STANFORD UNIVERSITY
SCHOOL OF MEDICINE
Department of Otolaryngology
Head & Neck Surgery
RESIDENT HANDBOOK 2023-2024
1 Table of Contents 1. INTRODUCTION ................................................................................................................................................ 3 2. STANFORD UNIVERSITY OTOLARYNGOLOGY FACULTY ROSTER ........................................................ 4 3. OTOLARYNGOLOGY RESIDENCY APPLICATION REQUIREMENTS ....................................................... 5 4. RESIDENT ROTATION SCHEDULE ................................................................................................................ 7 5. POLICY ON RESIDENT PROMOTION......................................................................................................... 10 6. POLICY ON RESIDENT DISMISSAL ............................................................................................................ 10 7. 360° EVALUATIONS ...................................................................................................................................... 10 8. POLICY ON SUPERVISION ........................................................................................................................... 11 9. MENTORSHIP PROGRAM ............................................................................................................................ 12 10. ACADEMIC CURRICULUM ............................................................................................................................ 13 11. DESCRIPTION OF ACADEMIC CONTENT, CONFERENCES AND RESPONSIBILITIES ..................... 14 12. RESIDENT TRAVEL AND CONFERENCE FUNDING POLICY .................................................................. 18 13. PERSONAL TIME-OFF ................................................................................................................................... 19 14. RESIDENT WORK HOURS AND CALL ........................................................................................................ 19 15. DEPARTMENTAL HAND-OVER POLICY..................................................................................................... 21 16. OPERATIVE CASE LOGS ............................................................................................................................... 21 17. COMMUNICATION ......................................................................................................................................... 22 18. GUIDELINES FOR ONLINE PROFESSIONAL OR PERSONAL ACTIVITY ............................................. 22 19. POLICY AND GUIDELINES FOR INTERACTIONS WITH INDUSTRY ..................................................... 23 20. STANFORD DEPARTMENT OF OHNS GUIDELINES FOR CONSULTATIONS .................................... 24 21. OTOLARYNGOLOGY POST -GRADUATE EDUCATIONAL PROGRAM ................................................... 26 GOALS AND OBJECTIVES PGY 1 - NON-OHNS ROTATIONS ................................................................................................ 26 STANFORD HEALTH CARE HEADMIRROR SERVICE ................................................................................................................. 33 Goals and Objectives PGY 1: SHC Headmirror Service 33 Goals and Objectives PGY 2/3: SHC Headmirror Service .................................................................................... 35 Goals and Objectives PGY 4: SHC Headmirror Service 41 STANFORD HEALTH CARE SCALPEL SERVICE ......................................................................................................................... 49 Goals and Objectives PGY 1: SHC Scalpel Service 49 Goals and Objectives PGY 2/3: SHC Scalpel Service ............................................................................................ 50 Goals and Obj ectives PGY 4: SHC Scalpel Service 56 Goals and Objectives PGY 5: SHC Scalpel Service ................................................................ ................................ 61 LUCILE PACKARD CHILDREN’S HOSPITAL STANFORD 66 Goals and Objectives PGY 1: PEDIATRIC Otolaryngology ................................................................................. 66
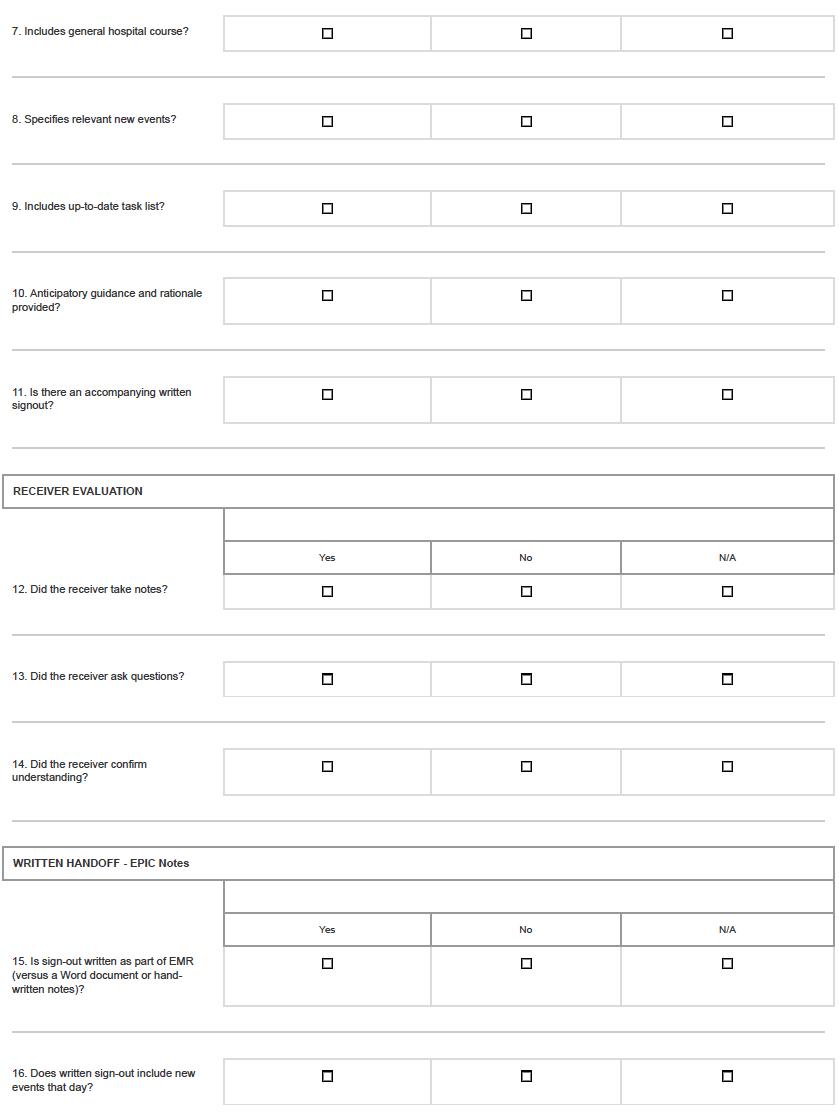
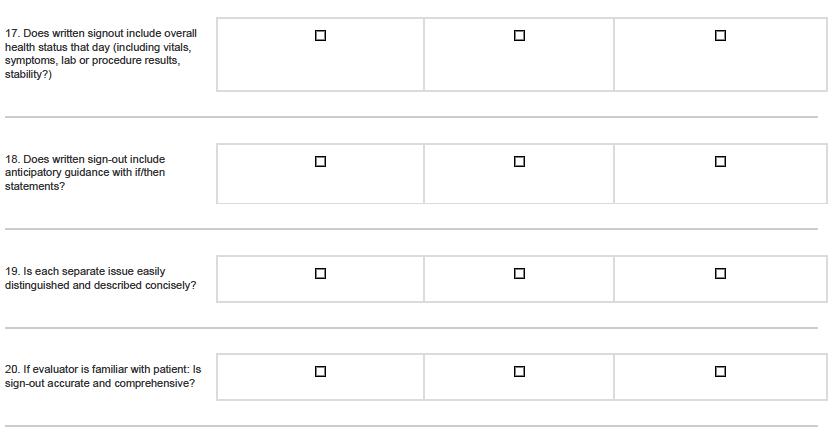
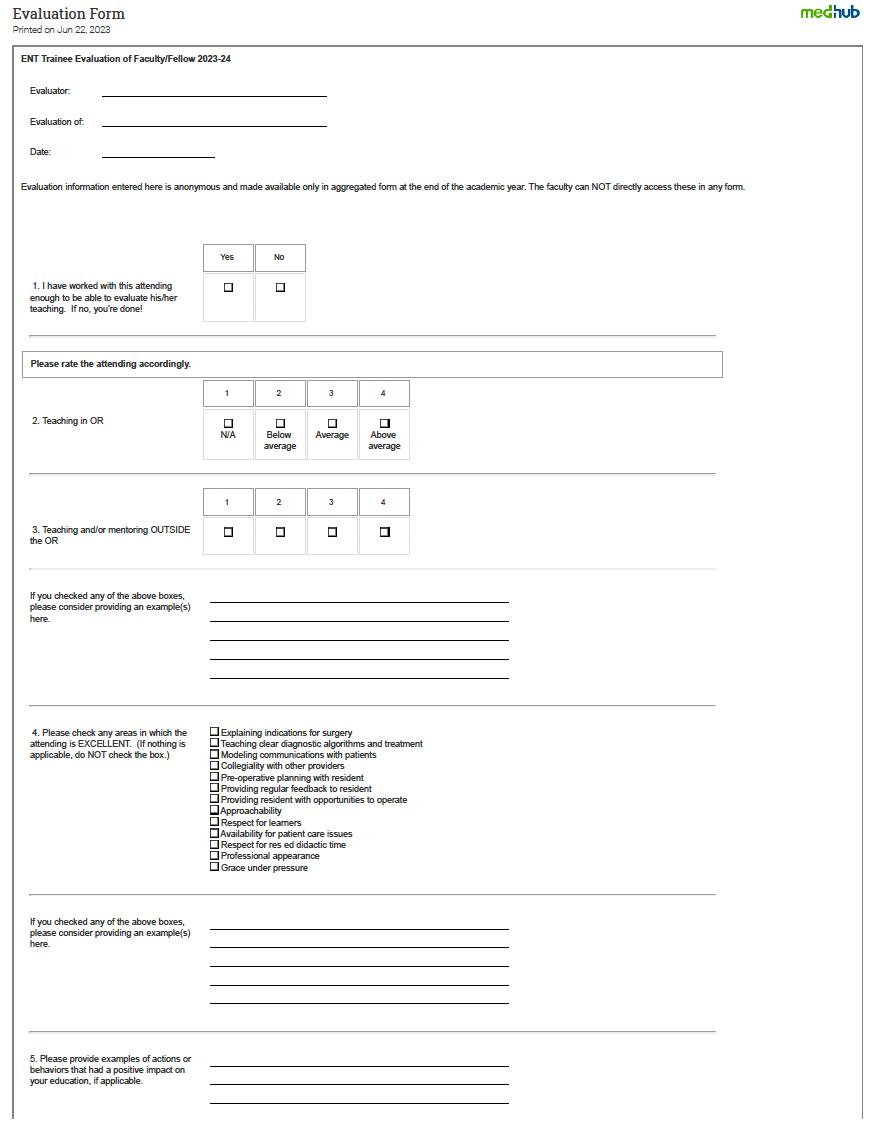
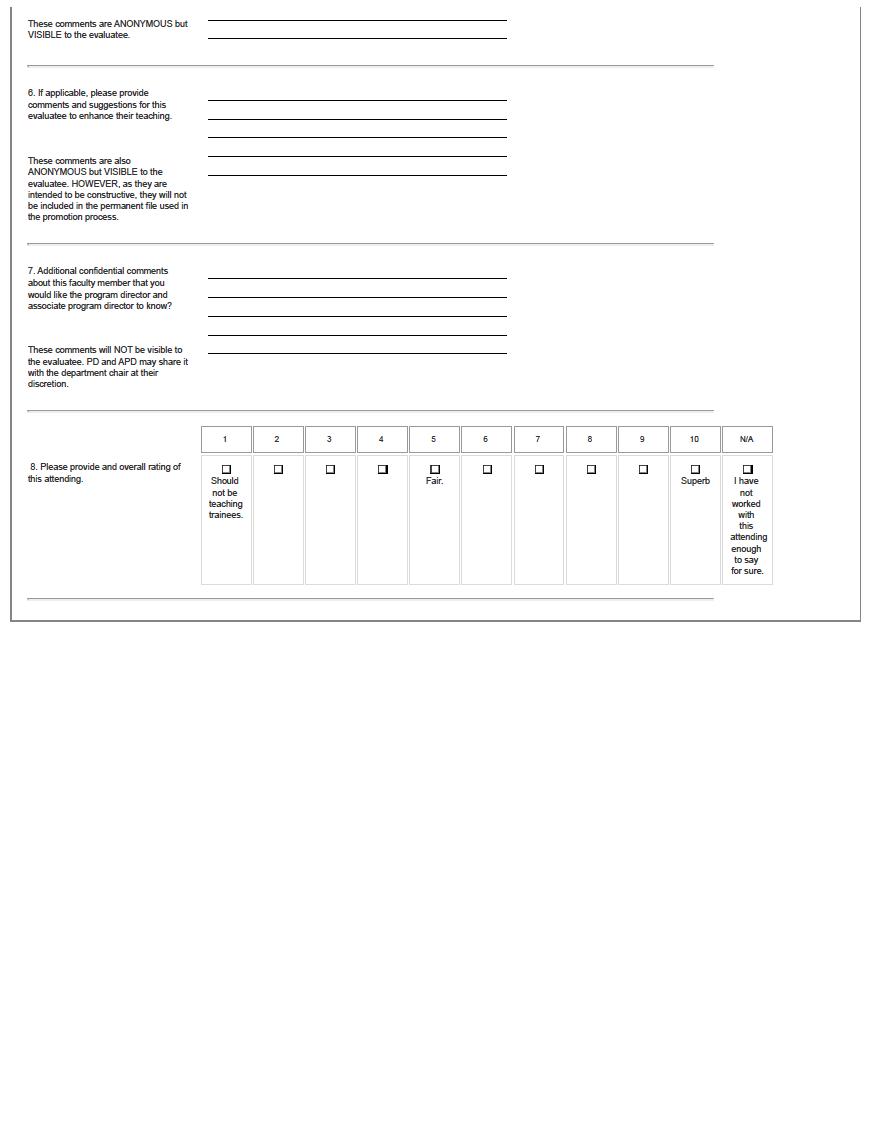
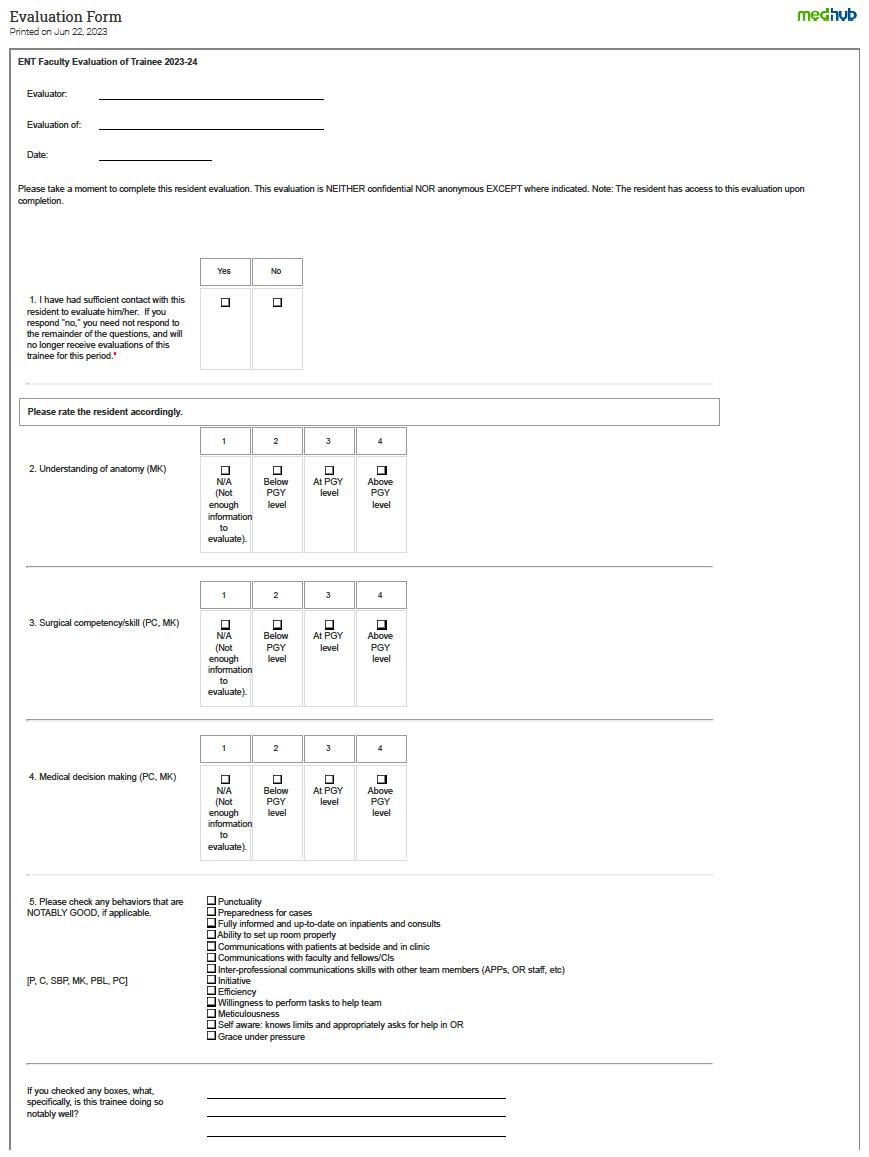
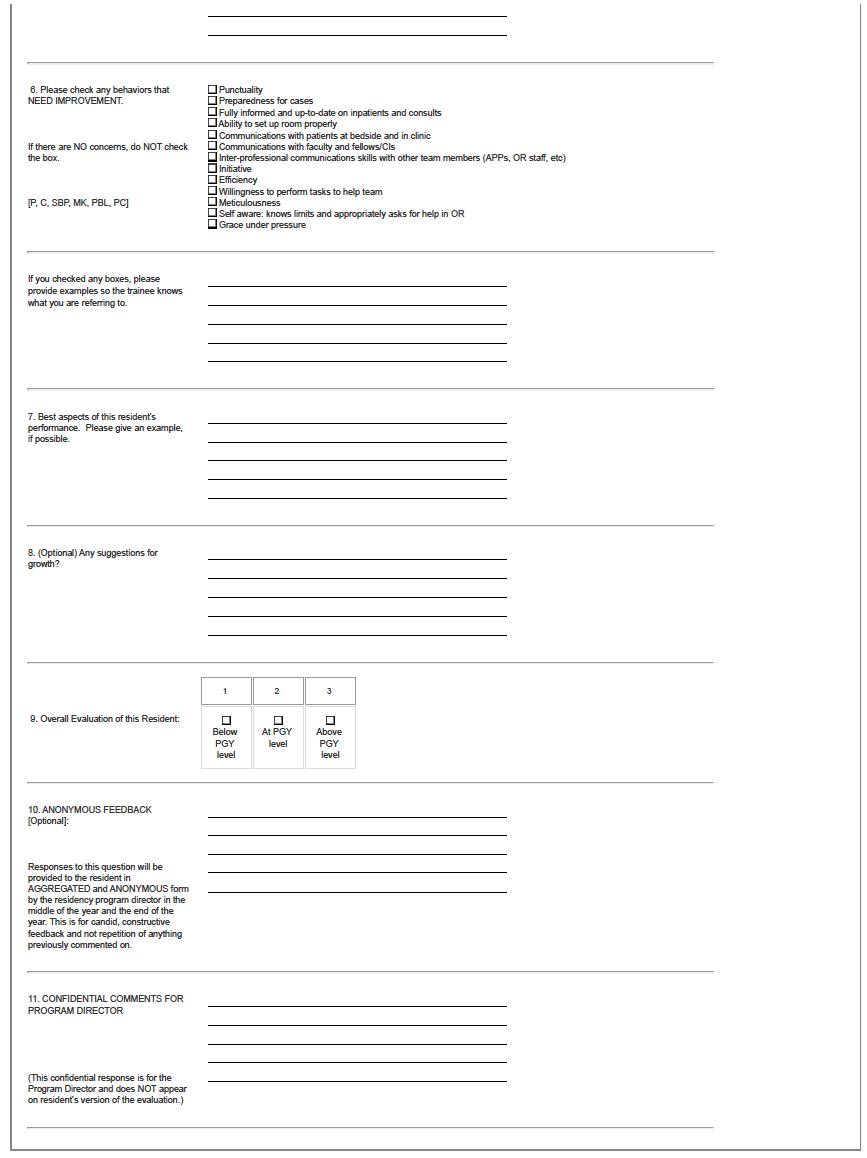
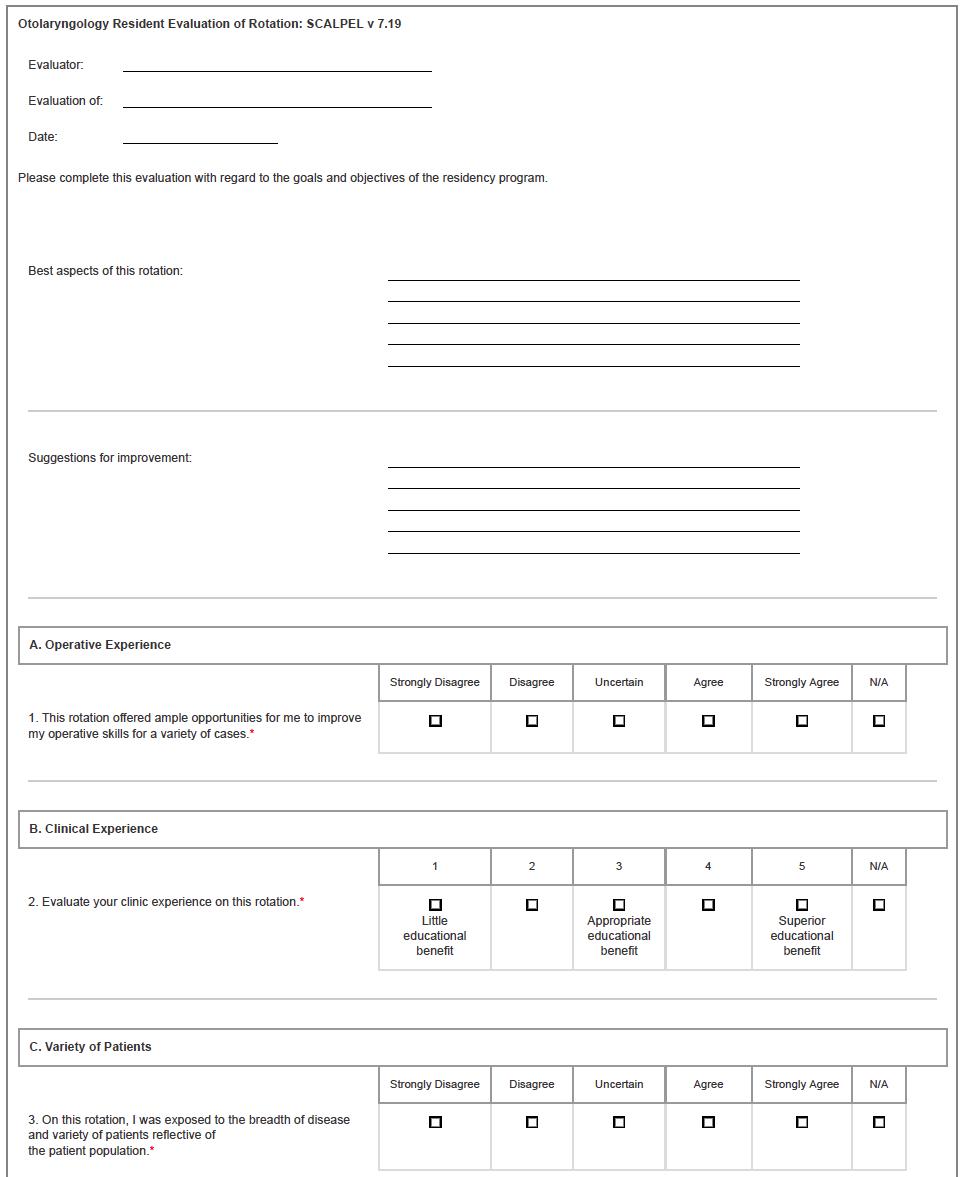
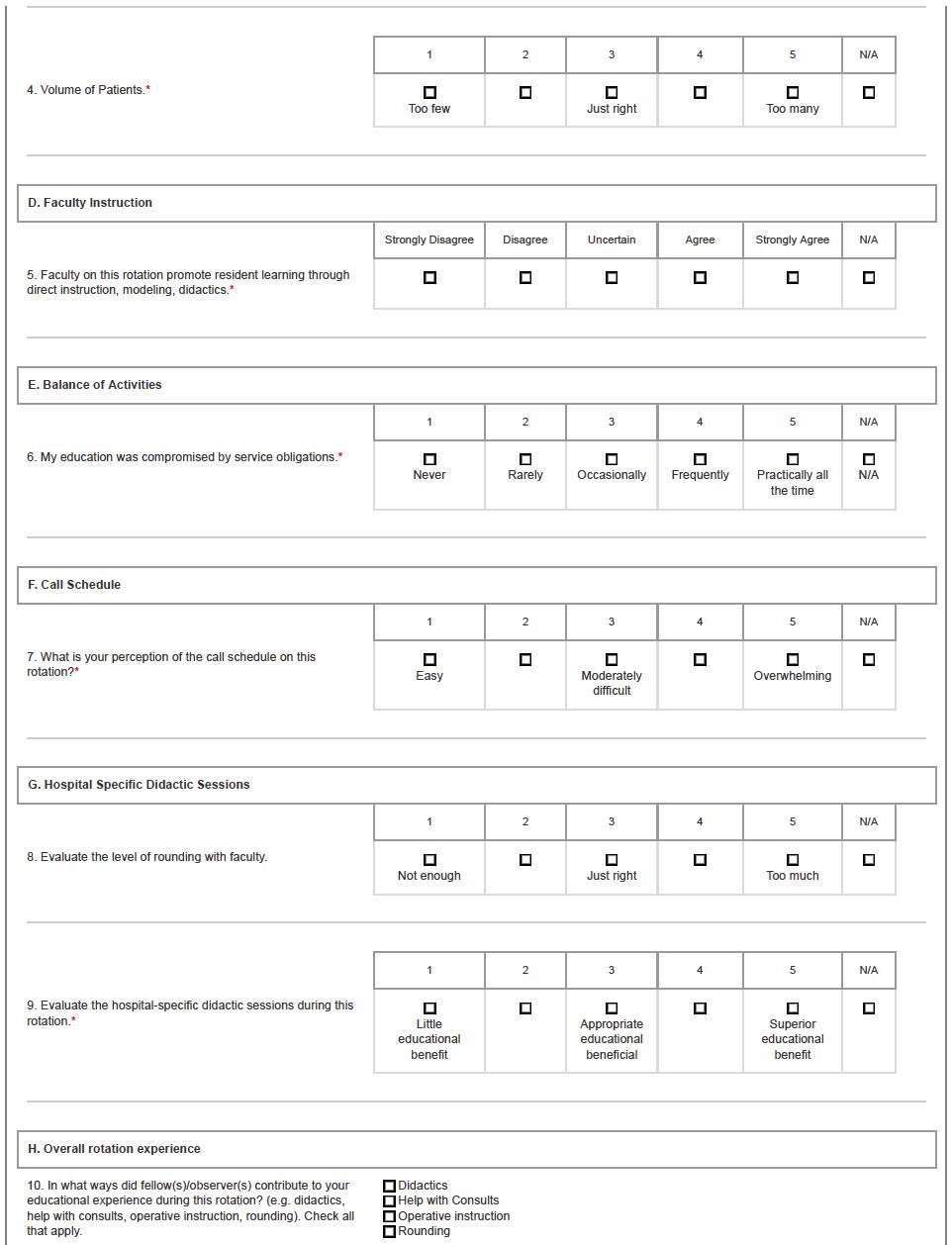
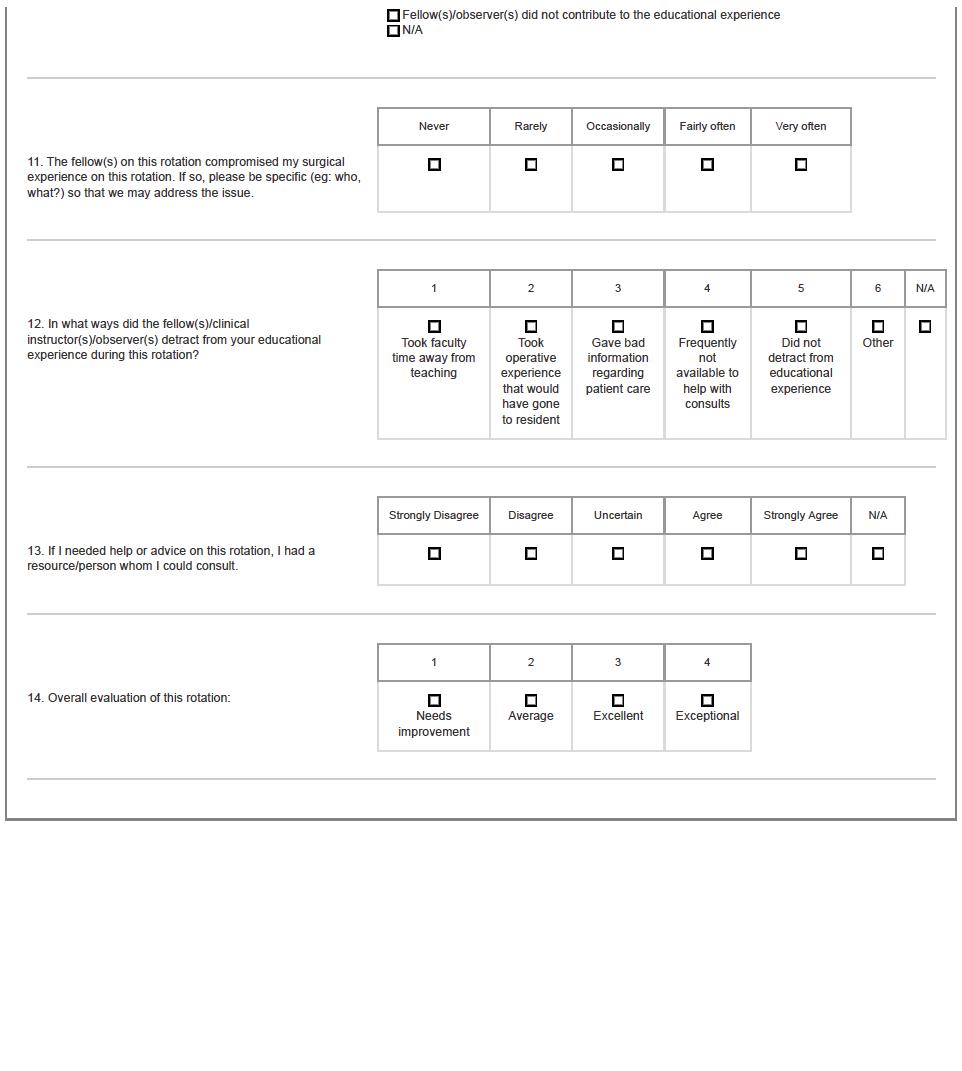
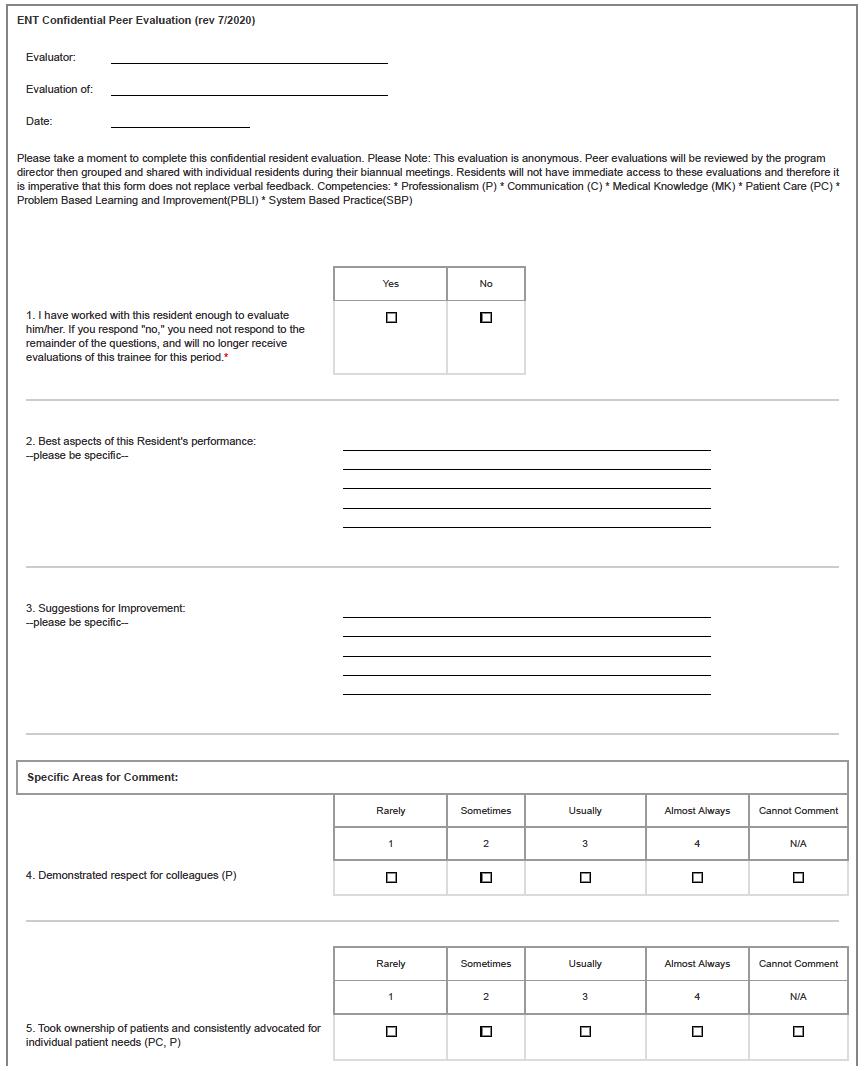
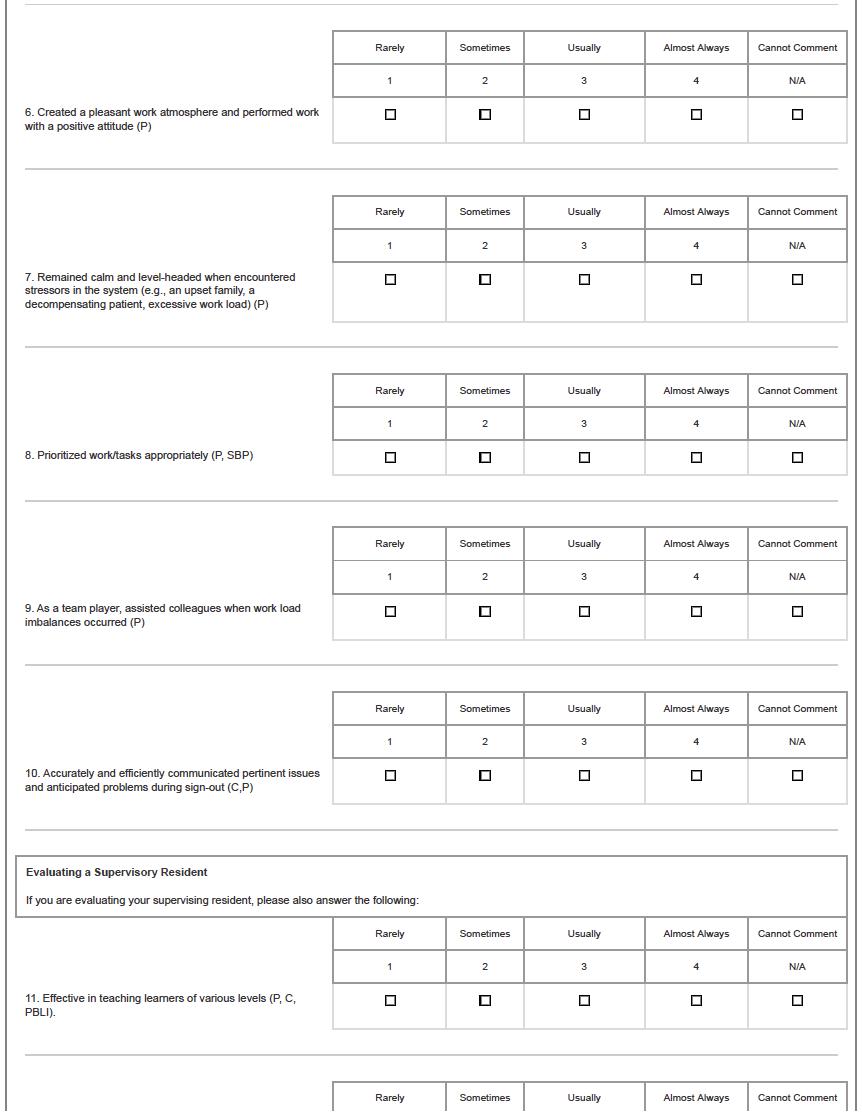
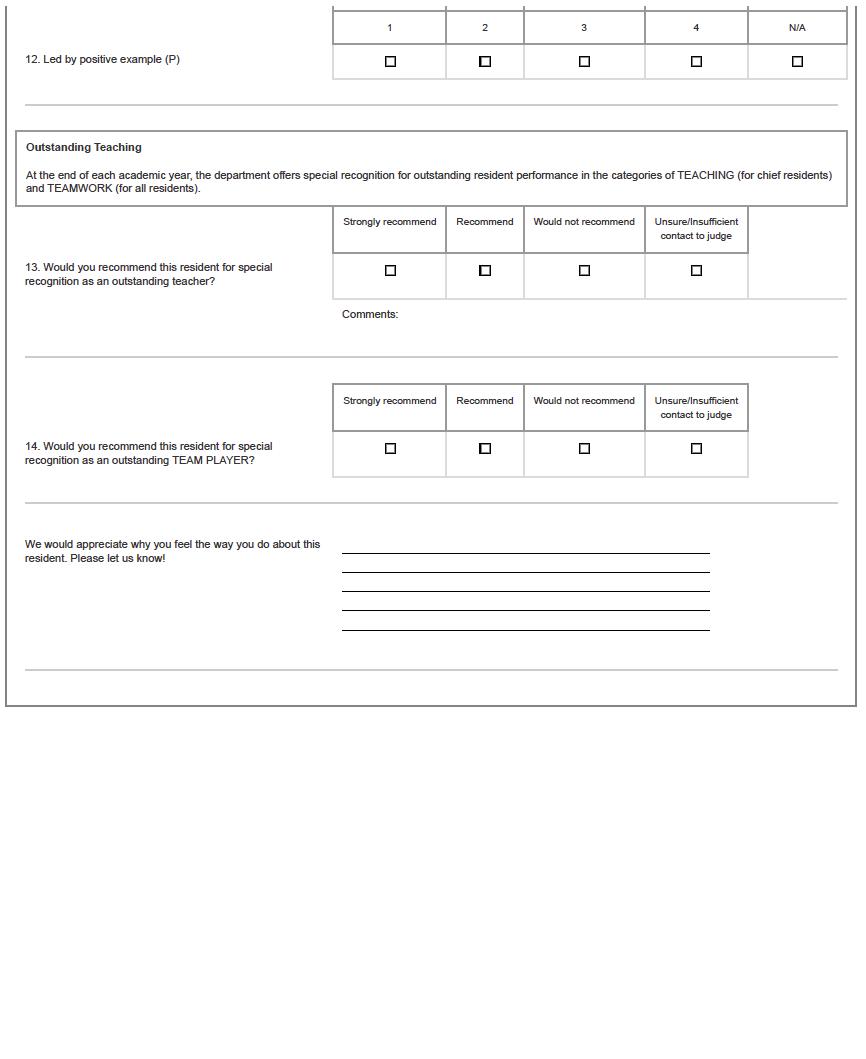
2 Goals and Objectives PGY 2/3: PEDIATRIC Otolaryngology ............................................................................. 67 Goals and Objectives PGY 4: PEDIATRIC Otolaryngology 73 VETERAN’S ADMINISTRATION PALO ALTO .............................................................................................................................. 78 Goals and Objectives PGY 3: VAPA 82 Goals and Objectives PGY 5: VAPA ............................................................................................................................ 88 STANFORD HEALTH CARE: SPECIALTIES TEAM (SCOPE) 92 Goals and Objectives PGY 1: SHC Specialty Service ............................................................................................ 94 Goals and Objectives PGY 2/3: SHC Specialty Service 95 Goals and Objectives PGY 4: SHC Specialty Service ..........................................................................................104 Goals and Objectives PGY 5: SHC Specialty Service 114 SANTA CLARA VALLEY MEDICAL CENTER ............................................................................................................................. 124 Goals and Objectives PGY 2: SCVMC .......................................................................................................................127 Goals and Objectives PGY 5: SCVMC .......................................................................................................................131 STANFORD HEALTH CARE AND LUCILE PACKARD CHILDREN’S HOSPITAL NIGHT FLOAT ROTATION ........................... 135 OHNS RESIDENT RESEARCH PROGRAM 137 CHIEF RESIDENT MINI-FELLOWSHIP AND ELECTIVE ROTATIONS 140 22. APPENDICES ...................................................................................................................................................142 APPENDIX A – CONFERENCE DATES 143 APPENDIX B – KEY INDICATORS 144 APPENDIX C – HANDOVER EVALUATION FORM 145 APPENDIX D – EVALUATION FORM OF FACULTY BY RESIDENT ..................................................................................... 148 APPENDIX E – EVALUATION FORM OF RESIDENT BY FACULTY 151 APPENDIX F – EVALUATION FORM OF SERVICE/ROTATION BY RESIDENT .................................................................. 154 APPENDIX G – RESIDENT PEER EVALUATION FORM 157 APPENDIX H – EVALUATION FORM OF RESIDENT BY STAFF .......................................................................................... 160 APPENDIX I – EVALUATION FORM OF RESIDENT BY PATIENT 162 APPENDIX J – OTOLARYNGOLOGY MILESTONES 2.0 ..................................................................................................... 164 APPENDIX K – FACIAL TRAUMA CALL POLICY .................................................................................................................. 165 APPENDIX L – MEDICINE/ENT/FACE/ED INTER-SERVICE AGREEMENT ................................................................... 167 APPENDIX M – AFTERHOURS OUTPATIENT MEDICAL ADVICE ...................................................................................... 170 APPENDIX N – PAGING SYSTEM 171 APPENDIX O – VERBAL ORDERS PROCESS CLARIFICATIONS FOR NURSES AND PHYSICIANS 172 APPENDIX P – TEMPORAL BONE LAB 174 APPENDIX Q – SHC INFECTION CONTROL ....................................................................................................................... 176 APPENDIX R – VAPAHCS ENT RESIDENT HANDBOOK 2023-2024 177
1. Introduction
The Stanford Department of Otolaryngology Head & Neck Surgery is dedicated to providing the highest level of training to its residents and fellows.
MISSION AND PHILOSOPHY
• Provide patient care with both expertise and compassion
• Foster dedication to life -long learning and teaching
• Excel at state-of-the art medical care for patients with otolaryngological diseases
• Take an investigative approach to the scientific and policy questions in medicine
• Invent new approaches to diagnosis and therapy
• Implement and optimize emerging technologies
• Be active world citizens in the provision of health care to those most in need
This handbook describes policies and procedures associated with the Otolaryngology Head & Neck Surgery residency, as well as the expectations for successful completion of the program. It is updated annually.
The Graduate Medical Education Office’s House Staff Handbook is available for download at: https://med.stanford.edu/gme/policy.html
3
2. Stanford University Otolaryngology Faculty Roster
Department Chair
Vice Chair
Residency Program Director
Associate Program Director
Stanford
Konstantina M. Stankovic, MD, PhD
Peter Hwang, MD
C. Kwang Sung, MD, M.S.
Jennifer Alyono, MD, M.S.
Iram Ahmad, MD, MME
Fred Baik, MD
Karthik Balakrishnan, MD, MPH
Nikolas H. Blevins, MD
Robson Capasso, MD
Kay W. Chang, MD
Michael Chang, MD
Alan Cheng, MD
Michelle Chen, MD, MHS
Edward J. Damrose, MD
Seth Davis, MD
Elizabeth DiRenzo, PhD
Vasu Divi, MD
Andrey Finegersh, MD, PhD
Matthew Fitzgerald, PhD
Nicolas Grillet, PhD
Stefan Heller, PhD
Floyd Christopher Holsinger, MD
Peter H. Hwang, MD
Robert K. Jackler, MD
Michael J. Kaplan, MD
Grace Kim, MD
Peter J. Koltai, MD
Jennifer Lee, MD
Stanley Liu, MD, DDS
Dáibhid Ó Maoiléidigh, PhD, MS
Kara Meister, MD
Uchechukwu Megwalu, MD, MPH
Lloyd Minor, MD
Sam P. Most, MD
Jayakar Nayak, MD, PhD
Teresa Nicolson, PhD
Brian Nuyen, MD
Lisa Orloff, MD
Zara Patel, MD
Jon-Paul Pepper, MD
Nathan Reticker-Flynn, PhD, S.M.
Anthony Ricci, PhD
Peter Santa Maria, MBBS, PhD
George Shorago, MD
Douglas Sidell, MD
Davud Sirjani, MD
Heather Starmer, MA
Kristen Steenerson, MD
4
John Sunwoo, MD
Mai Thy Truong, MD
Tulio Valdez, MD, MSc
Fellows & Clinical Instructors
Pediatrics – Daniel Penaranda Garcia, MD, MSc & Z. Jason Qian, MD
Facial Plastic – Monica Rossi Meyer, MD
Laryngology – Christina Ng, MBBS, MRCS, MM
Rhinology – Zechariah Franks, MD, MPH & Axel Renteria, MD, MSc
Sleep – Pedro Martins Gomes de Oliveira, MD & Vikram Padhye, MBBS, PhD
Head & Neck – Zipei Feng, MD, PhD & Guolan Lu, MD, PhD
Otology-Neurotology – Richard Baron, MD, Minjin Jeong, MS, PhD, Peter Kullar, MBBChir, MA, PhD & Lindsay Moore, MD
Research - Nesrine Benkafadar, PhD, Marie Kubota, MD, PhD & Sheth Sam George, PhD
Affiliated Faculty
Santa Clara Valley Medical Center
M. Lauren Lalakea, MD (Section chief)
Kimberly Shepard, MD
Micah Saste, MD
Amanda Muñoz, MD
Misha Amoils, MD
Julia Noel, MD
Veterans Administration Palo Alto
Davud Sirjani, MD (Chief)
Michell Chen, MD, MHS
Andrey Finegersh, MD, PhD
Jayakar Nayak, MD, PhD
Bohdan Makarewycz, MD
Monica Rossi Meyer, MD
Hamed Sajjadi, MD
C. Kwang Sung, MD, MS
3. Otolaryngology Residency Application Requirements
• The Stanford Department of Otolaryngology Head & Neck Surgery welcomes qualified applicants for consideration for appointment to its ACGME -accredited residency program. Please see the “Resident eligibility – recruitment” section of the Stanford House Staff Policies & Procedures for details of eligibility. The department encourages residency applications from all qualified individuals regardless of age, sex, ethnic background, religious beliefs, or sexual orientation with an interest and a proven track record of excellence in scholarly pursuits.
5
• Stanford participates in the Electronic Residency Application Service (ERAS) for otolaryngology. Rank lists are submitted by both the program and the resident applicants, and a matching algorithm is applied.
• All applications received by Stanford are individually reviewed. Candidates are selected for interviews based on this initial review. Once interviews are conducted, decisions about candidate selection are made by consensus among the faculty. Approximately 45 invitations for interviews are offered from among more than 300 applications. Interviews tak e place on two days in January.
6
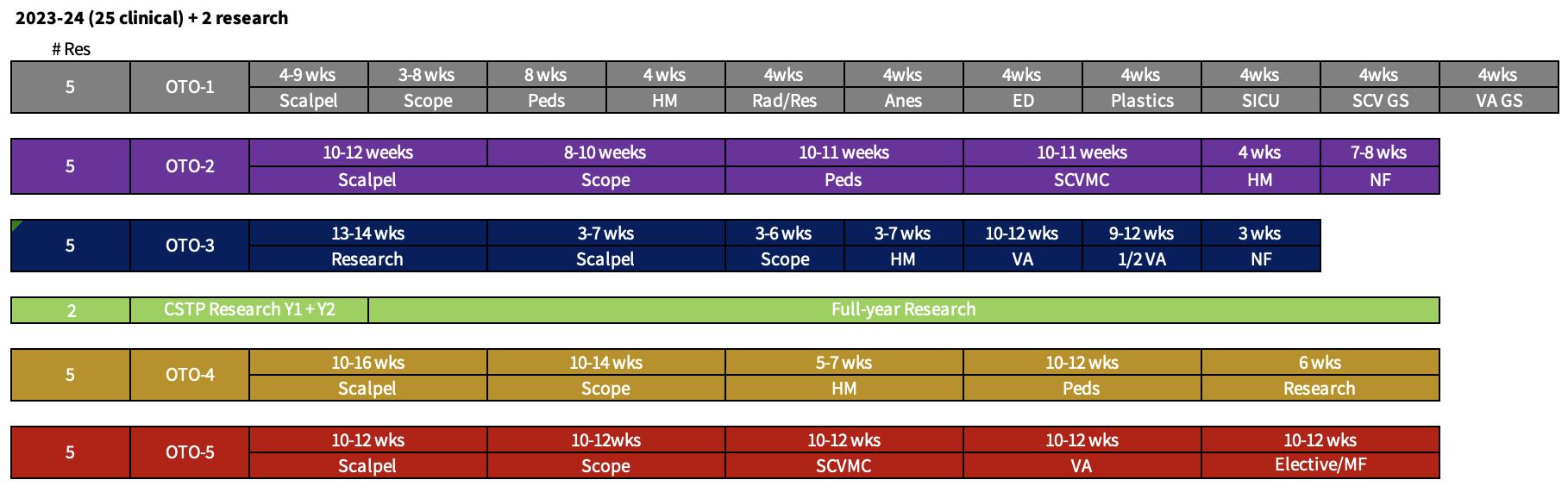
4. Resident Rotation Schedule
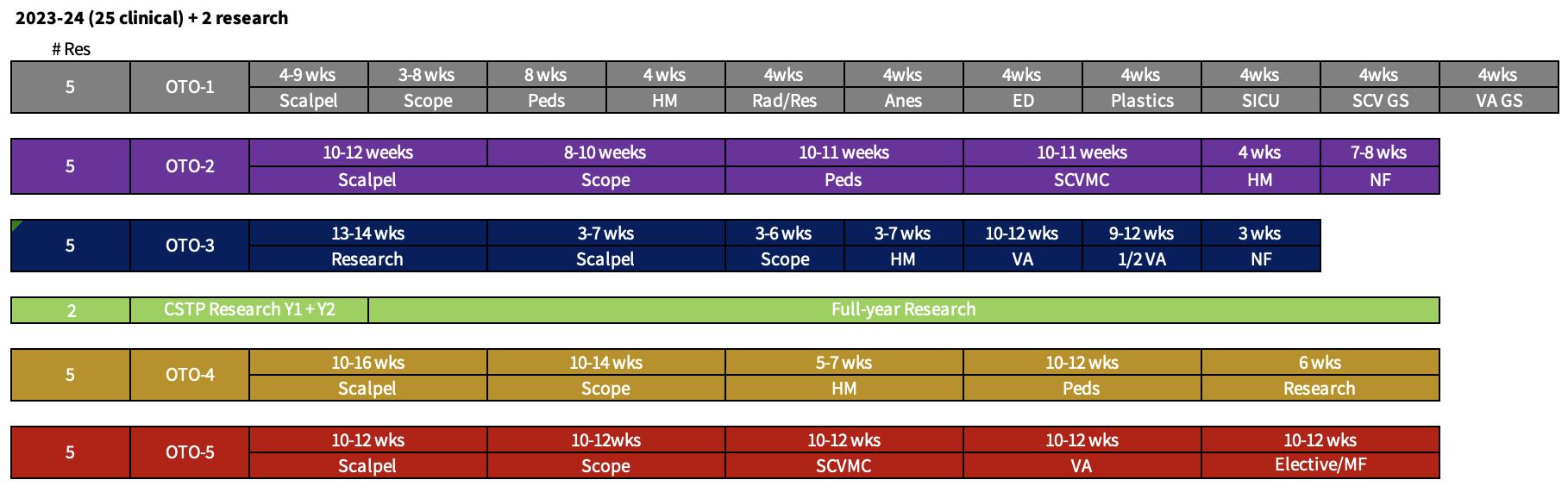
Key:
Scalpel: Head and Neck Surgery
Scope: Specialties (Otology, Rhinology, Facial Plastic Surgery)
HM: Headmirror (Laryngology, Sleep Surgery, Comprehensive Otolaryngology)
Peds: Pediatric Otolaryngology
NF: Night Float
SCVMC: Otolaryngology department at Santa Clara Valley Medical Center
VA: Otolaryngology department at Veterans Affairs Palo Alto Health Care System
MF: Mini Fellowship
Elective: Options for rotating on sub-specialties, or extra-departmental rotation
Rad/Res: Radiology (neuroradiology) / Research
Anes*: Anesthesia, Stanford Health Care
ED*: Emergency Department, Stanford Health Care
Plastics*: Plastic Surgery, Stanford Health Care
SICU* Stanford Health Care Intensive Care Unit
SCV GS*: General Surgery, Santa Clara Valley Medical Center
VA GS*: General Surgery, Veterans Administration Palo Alto
* PGY1 rotations with General Surgery Department
7
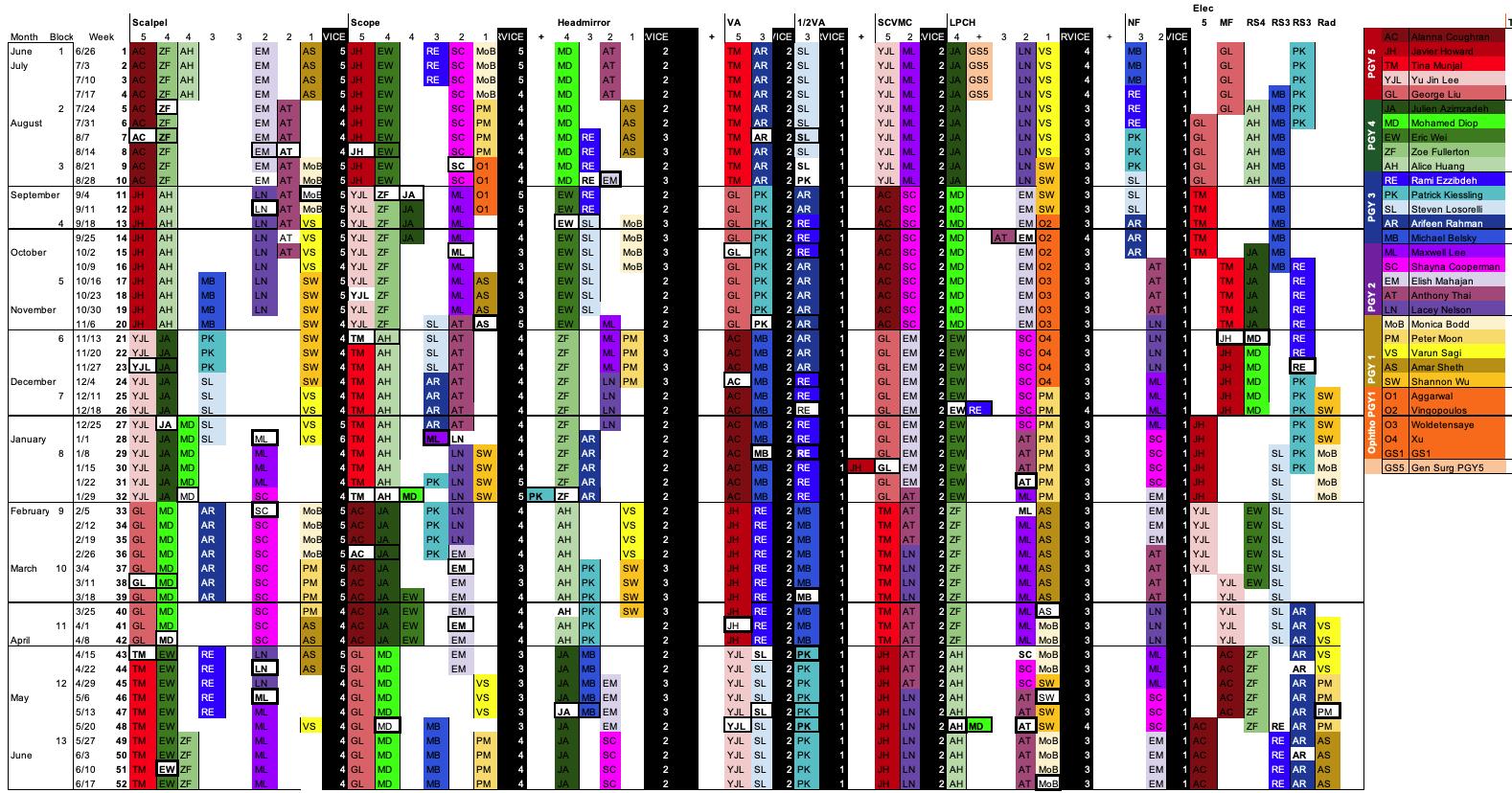
2023- 24 OHNS Residents Rotation Schedule
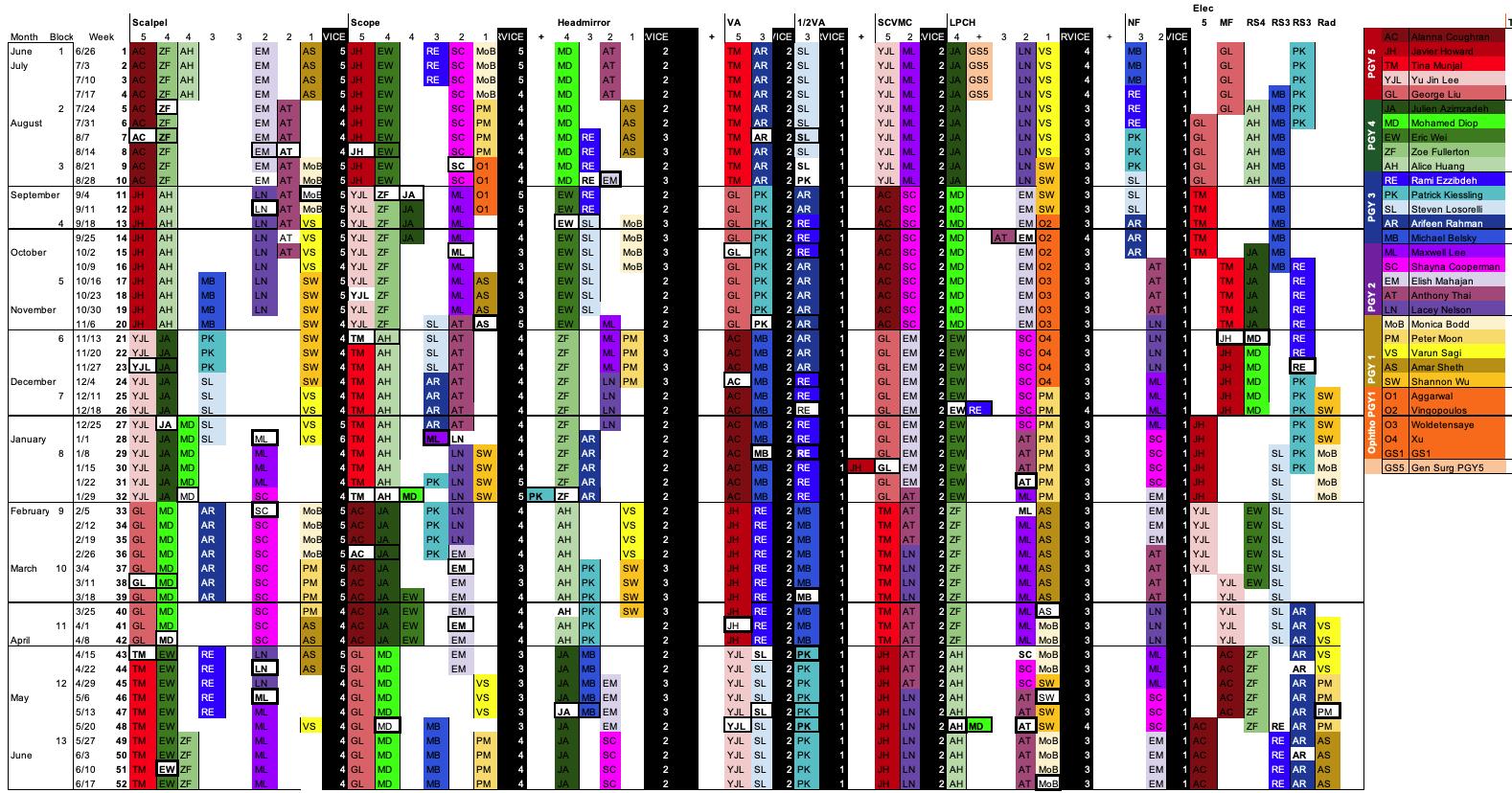
8

9
5. Policy on Resident Promotion
Stanford is fortunate to attract the highest caliber of residents in the nation. It is expected that each resident has the necessary skills and intellect to be promoted through the residency and graduate successfully. Prior to completion of the program, otolaryngology residents are expected to demonstrate compe tence in patient care, medical knowledge, professionalism, system-based practice, practice-based learning and improvement, and interpersonal and communication skills. They are likewise expected to complete and excel in the research requirements of the program.
Twice a year, the program director conducts a meeting with each resident to discuss resident performance and educational development. At these meetings, evaluations of the resident (that have been completed by the resident, faculty, nurses/adjunct personnel, and patients) are discussed at length. Attendance record at conferences, resident research projects, operative logs, and planned/completed portfolio projects will be reviewed.
6. Policy on Resident Dismissal
Residents are expected to satisfy a t least a minimum level of competence in order to be promoted.
Residents failing to achieve the minimal level of competence as determined by the evaluations will be given written notice of that fact. Depending on the nature of the deficiency, they may then be placed on probation. This period of probation will last at least three months and will be accompanied by a detailed plan to address any deficiencies in the resident’s performance.
Residents who are on probation for a minimum of three months and who h ave not successfully improved their performance to meet at least the minimal level of competence may be dismissed.
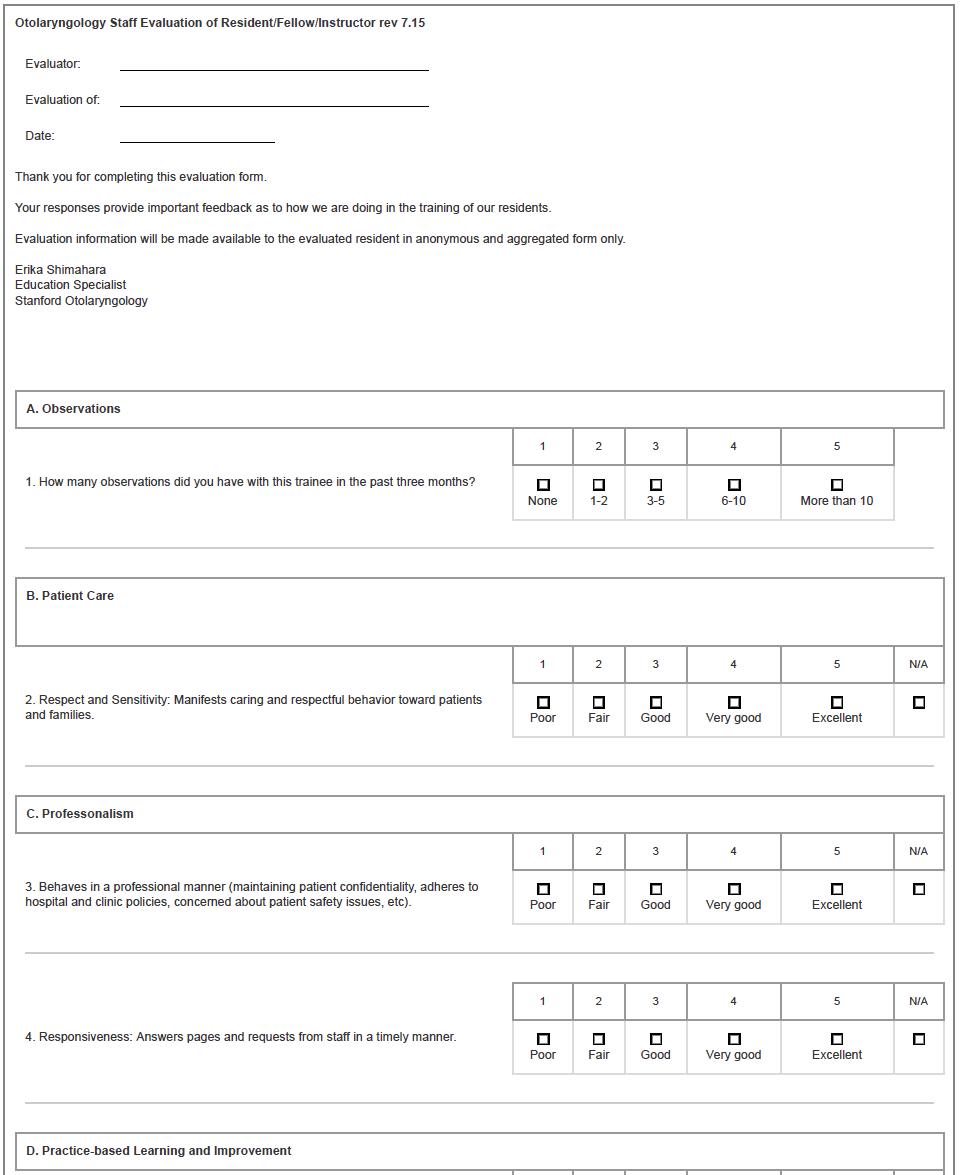
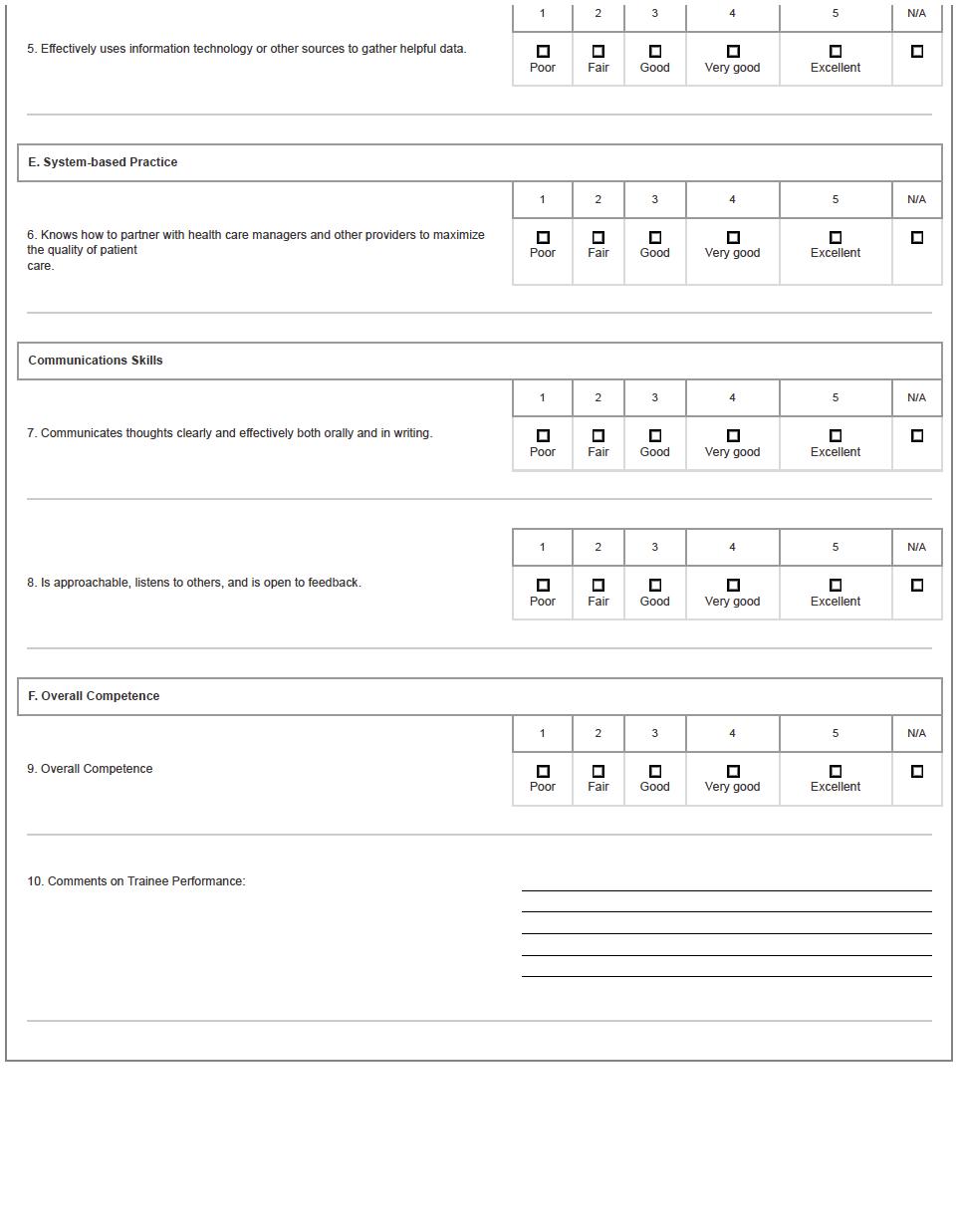
7. 360° Evaluations
Performance evaluations are completed by various members of the healthcare team including faculty, staff (nurses, MAs, physicians’ assistants, nurse practitioners, technicians, anesthesiologists, etc), patients and peers. These evaluations address performance in the core competencies and are sent to evaluators after every rotation, including the research block. Evaluations are conducted on-line via the MedHub system to assure anonymity. In an effort to obtain a 360-degree evaluation, patients are also randomly asked to compete evaluations based on their interactions with residents.
10
Peer evaluations are held from resident -access until the end of the year to protect anonymity. However, at the semi-annual review meeting, the program director will share aggregated feedback of these evaluations verbally. Resident(s) with the highest peer ratings for outstanding teaching will be awarded the “Resident Teacher of the Year” award at the end of the year. An award will also be given for the resident rated highest as an outstanding team player by their peers.
Meaningful evaluation of the faculty and the program is a critical aspect of the residency program; it is a tool for improving educational quality and the resident learning environment. Residents are therefore expected to complete faculty and rotation eval uations in a timely fashion after the end of each rotation.
Residents will have access to their evaluations by faculty upon completion of their faculty/rotation evaluations. To assure anonymity, the evaluations of faculty and rotations will not be collated or made available to faculty until the end of the academic year. Evaluations by residents are always anonymous.
8. Policy on Supervision
See GME handbook for policies.
Stanford OHNS
System Triggers for Attending Communication
• Admission/discharge
• Transfer in/out of ICU
• Unplanned intubation
• Cardiac arrest or hemodynamic instability
• Neurological changes
• Wound complications
• Any medication or therapeutic error that leads to a change in patient management
• Unplanned transfusion
• Any clinical problem requiring an invasive procedure
• ER visit
• Any concern by a trainee that a situation is more complicated than he or she can manage
• Any request that an attending surgeon be contacted
• Any situation in which a parent requests attending notification or feels that an issue has not been adequately resolved or addressed
• Any new onset/worsening of symptoms out of proportion to expectations
11
9. Mentorship Program
Beginning July 2020, the faculty mentoring program has been restructured . Rather than 1:1 faculty to resident pairings, r esidents are now assigned to cohorts of five to six residents representing each post-graduate year, and these cohorts are assigned to one faculty member.
The cohorts will meet at least three times a year for activities (eg dinner, outings ) with their mentors.
The goals of this program are to encourage more routine interactions, develop closer group dynamics and friendships, and foster supportive social and professional network s.
The resident may consult the faculty mentor as needed on any issues either professional or personal. The resident should also feel free to consult the Program Director regarding any such subjects.
The faculty mentors will function as liaisons to the rest of the faculty for issues regarding resident academic, clinical and operative performance as well as well-being.
12
Group # Resident PGY Track Mentor 1 1 Sagi 1 CT Orloff 2 Losorelli 3 CT 3 Wei 4 CT 4 Munjal 5 CSTP 5 Soo 5 CSTP 2 6 Sheth 1 CSTP Sunwoo 7 Cooperman 2 CT 8 Kiessling 3 CSTP 9 Fullerton 4 CT 10 Coughran 5 CT 3 11 Moon 1 CT Patel 12 Lee, Maxwell 2 CT 13 Ezzibdeh 3 CT 14 Rahman 3 CT 15 Huang 4 CT 16 Howard 5 CT 4 17 Thai 2 CT Divi 18 Nelson 2 CT 19 Park 4 CSTP 20 Azimzadeh 4 CT 21 Lee, Yu Jin 4 CSTP
Resident Mentors
The otolaryngology peer -mentoring program was started in 2009 to provide a formalized career and personal support system to junior residents. Incoming interns are paired with midlevel residents, based on consideration of their common interests. Senior residents have an opportunity to offer professional guidance, moral support, process decisions and the like. Notifications of these pairings are made in the spring prior to incoming inte rns’ arrival to Stanford.
Class beginning 2022
Shayna Cooperman – Alice Huang
Maxwell Lee – Mohamed Diop
Lacey Nelson – Zoë Fullerton
Elish Mahajan – Ki Wan (Roy) Park
Anthony Thai – Eric Wei
Class beginning 2023
Monica Bodd - Michael Belsky
Peter Moon - Rami Ezzibdeh
Varun Sagi - Steven Losorelli
Amar Sheth - Patrick Kiessling
Shannon Wu - Arifeen Rahman
10. Academic Curriculum
Required Assignments
The following is a list of the principle required projects and talks during the course of the residency:
All five years of residency
❑ Otolaryngology In-training Exam
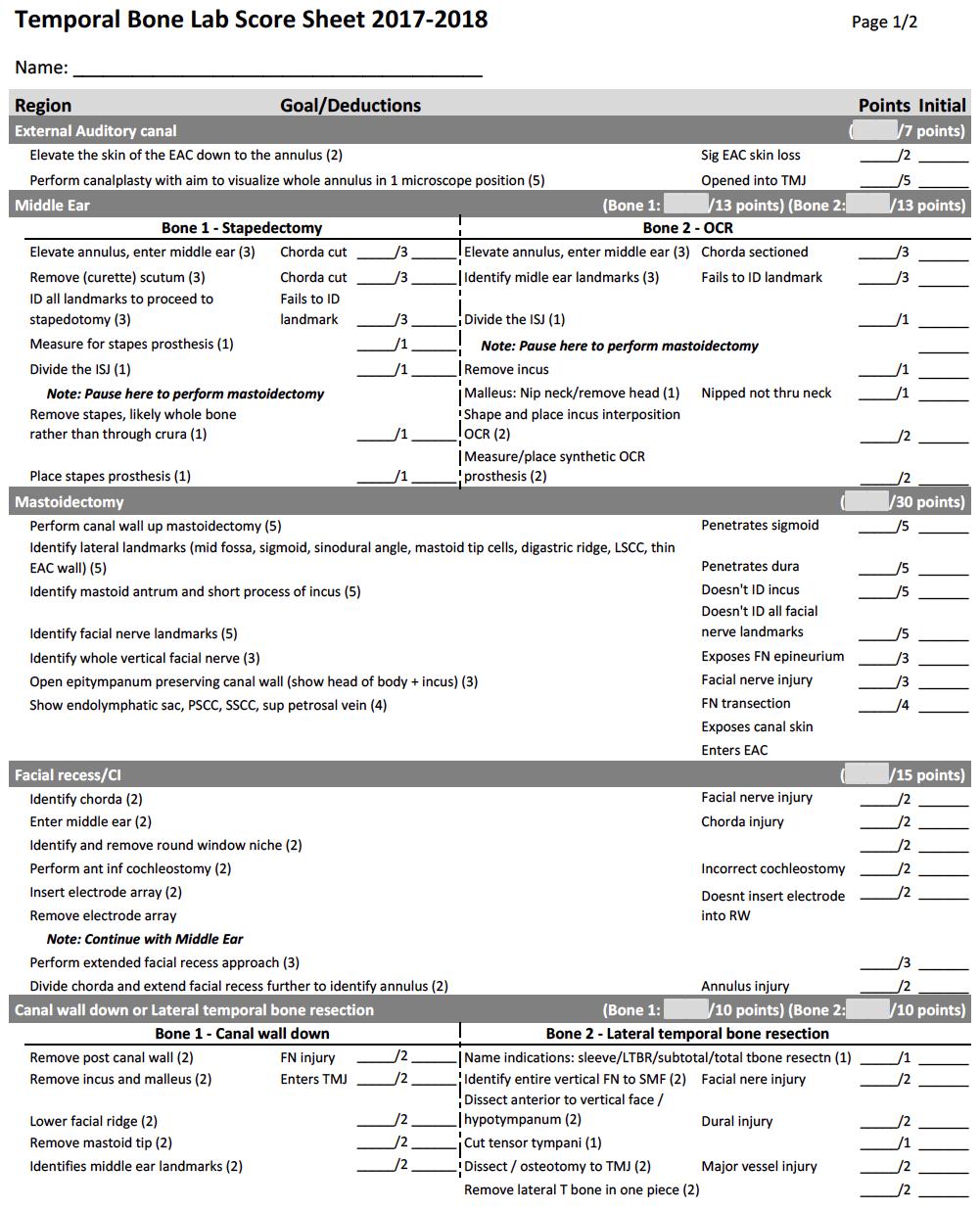
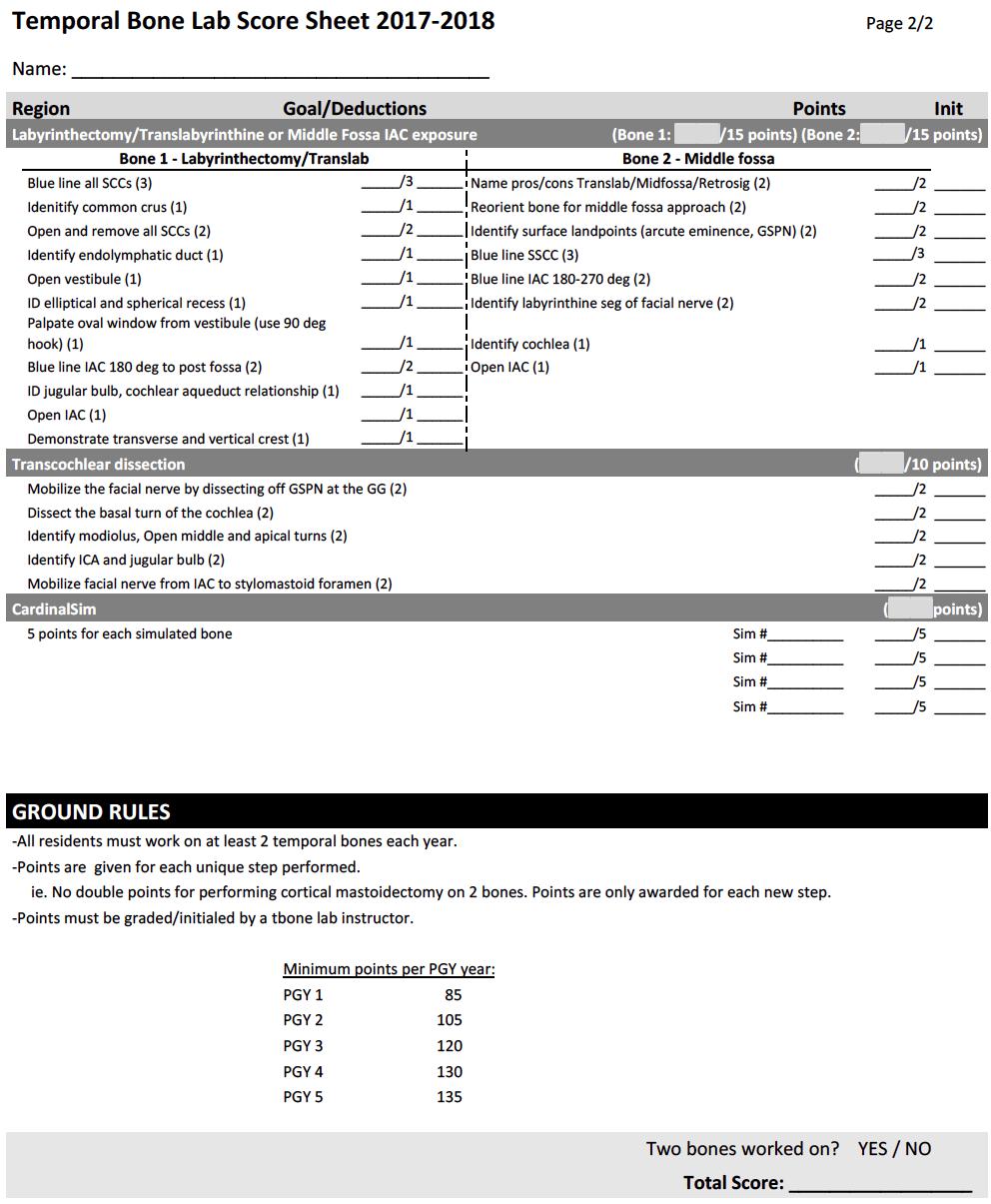
❑ Temporal bone lab
13 5 22 Bodd 1 CT Hwang 23 Wu 1 CT 24 Mahajan 2 CSTP 25 Belsky 3 CT 26 Diop 4 CT 27 Liu 5 CT
PGY1
❑ Radiology case presentation assembled during Radiology/Research Rotation
PGY2
❑ Research proposal, due at semi -annual meeting with program director in January/February.
❑ Residency Research Symposium Presentation
❑ Radiology case presentation for Resident Education
PGY3
❑ Residency Research Symposium Presentation
❑ Abstract submission to the Bay Area Residency Research Symposium
❑ Quality Improvement Project
PGY4
❑ Residency Research Symposium Presentation
PGY5
❑ Grand Rounds
❑ Residency Research Symposium Presentation
11. Description of Academic Content, Conferences and Responsibilities
The academic curriculum is based on a rotating two -and-a-half year cycle so that each resident is exposed to each topic at least twice during his/her residency. Weekly Residency Education conferences are held on Mondays 8:00-10:00 AM. Residents are expected to be on time for 75% of sessions (except for cases of pre -approved excused absences). Residents at SCVMC and VAPA will be expected to participate in person when possible, or via Zoom videoconference when necessary. Attendance records will be tracked, and will be reviewed by residents and faculty.
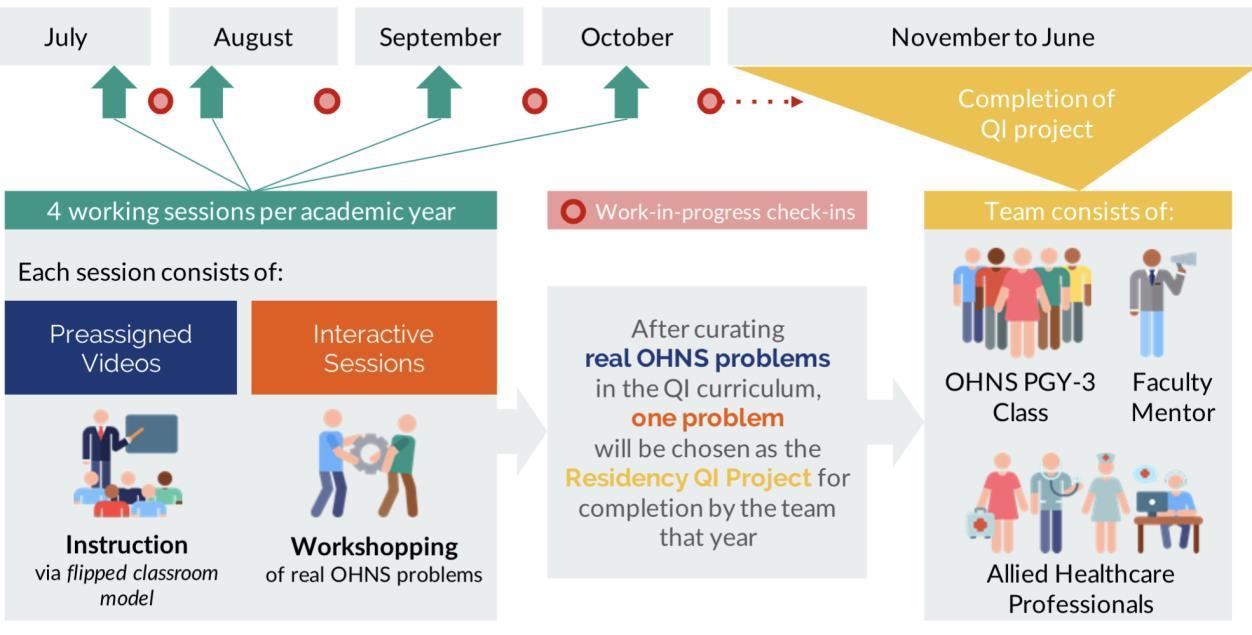
The Thursday evening conferences (Grand Rounds and Quality Improvement) begin at 6:00 PM. In addition, there will be at least one book club, and journal clubs are held on weekday evenings (usually on Mondays) four times a year. Residents will be assigned to help organize the journal clubs. Residents are expected to practice drilling in the temporal bone lab on their own to meet required competencies. See appendix (Temporal Bone Lab) for more information. The Quality Improvement Project, whose curriculum has been redesigned, will be a requirement of all residents in their PG3 year.
The use of laptops is not permitted during Grand Rounds.
The PGY5 chief residents will be assigned to give one grand rounds session during the year.
14
All residents rotating at Stanford and LPCH are expected to attend Monday morning conference from 7:15-8:00 AM. The course subjects include Otology, Radiology, Laryngology, Rhinology, Facial Plastic Surgery, Head & Neck, Sleep Surgery, and Pediatric Otolaryngology conference. The residents rotating at SCVMC and VAPA are expected to participate in the Monday morning conferences via Zoom videoconference.
All residents on the Scalpel Service are required to attend the Head & Neck Resident Case Conference every Thursday 4:00-4:30 PM, followed by Head & Neck Tumor Board 4:30-5:00 PM.
All residents are required to complete an allergy course either online or in person at some point during their residency. In addition, all residents must spend a minimum of two halfdays in the Allergy Clinic to gain hands-on experience with skin testing. Contact Dr. Meng Chen at least one month in advance to schedule your clinic time. These requirements can be completed in any PGY year. Due to travel restrictions, the requirements may be completed online through the World Allergy Organization website: https://www.pathlms.com/wao/
The following allergy sessions should be completed:
https://www.pathlms.com/wao/courses/585
https://www.pathlms.com/wao/courses/4114
https://www.pathlms.com/wao/courses/1771
https://www.pathlms.com/wao/courses/572
https://www.pathlms.com/wao/courses/586
https://www.pathlms.com/wao/co urses/576
https://www.pathlms.com/wao/courses/581
All residents are required to take the in -training exam each year of residency, held the first Saturday of each March, including residents in their dedicated research years of the CSTP track.
Attendance Policy
Conferences
Attendance will be taken at each of the Monday conferences at 8:00 AM and other required conferences (eg journal club, grand rounds, etc) and other events (residency meetings, symposium, etc).
Mandatory Events
Residents are required to be present for the following annual events. Vacation time should be scheduled accordingly:
15
• Residency graduation
• Residency Research Symposium
• In-training exam (first Saturday of March)
• Residency Annual Program Evaluation/Retreat (first Monday in June)
Annual In- training Exam
All residents, including the PGY1 residents , including residents in their dedicated research years of the CSTP track, are required to sit for the in -training exam, administered the first Saturday of March. Residents who achieve scores in the 7 th-9th group stanines will receive prizes of $500 for academic purposes. Those in the bottom three stanines will be required to submit a written study plan to the program director and their assigned mentor, and to meet with their mentor on a quarterly basis to discuss progress.
Residency Research Symposium
Every year, on graduation Friday, the department hosts a day -long symposium to showcase research conducted by residents over the year. Maximum time for the presentation is 7 minutes (with an additional three minutes of question and answer time). Presentation s are judged by selected faculty and the guest of honor using a criterion -based rubric, which is provided to the residents in advance. PGY2-5 are required to give a presentation. A grand prize of $500 in academic funds is given to the best overall present er; there are two runners up, receiving $250 in academic funds each in the categories of presentation and content , respectively.
To be eligible for these prizes, the material presented must constitute original research conducted by the resident (which h as also not been previously presented in years past, but may have been presented at a national conference or the Bay Area Residency Research Symposium). An abstract of the talk is due two weeks before the symposium date.
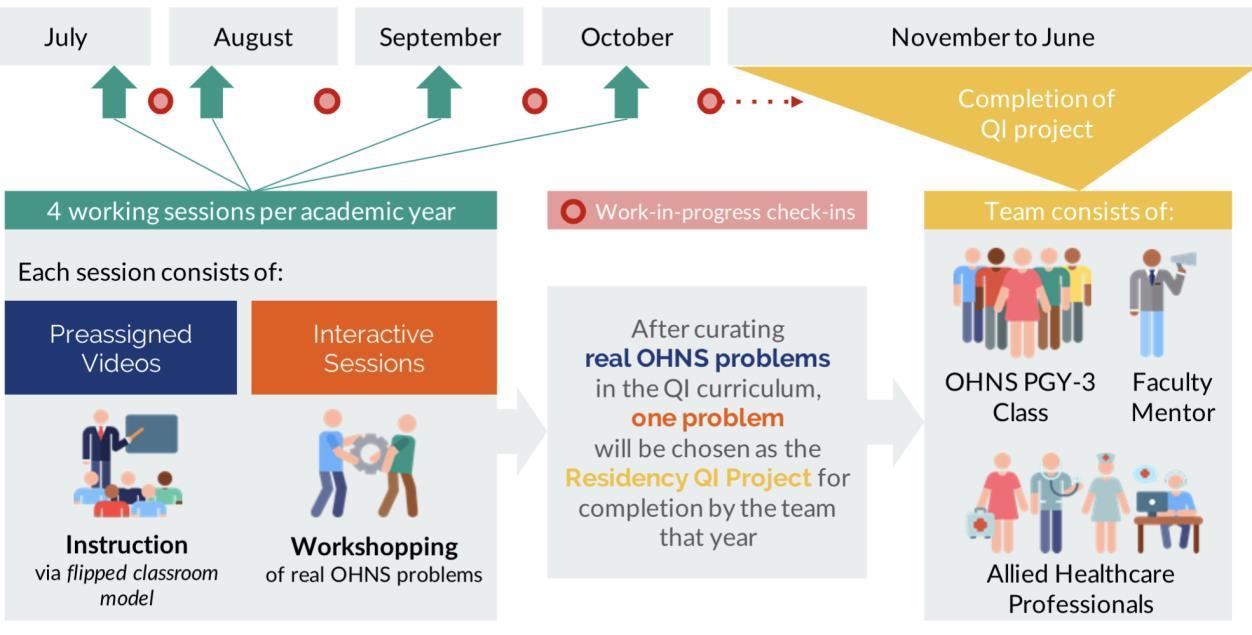
Quality Improvement (QI) Curriculum
Effective July 1, 2020, the QI curriculum has been revamped. While its purpose remains the same, this learning requirement has been restructured, is now being overseen by Dr. Alyono, and is a collective rather than indi vidual resident projec t of PGY3’s
The aim of the QI project is to develop a plan to support a hospital or clinical performance improvement or patient safety measure by:
• Reflecting on practice and practice analysis
• Critically analyzing the current literature
• Developing a plan for implementation of the proposed change
• Developing an outcomes’ assessment (performance measure)
16
Its overall purpose is to foster an understanding of the complexities of health care delivery and develop the skills to address t hem as is described by the core competency, SystemsBased Practice.
The program is illustrated in the image below. Working sessions will take place on weekday evening, four times a year between July and October. Thereafter the team will meet on its own for completion of the project in the following June.
National Academic Conferences
Every attempt will be made to relieve the PGY2 or PGY3 residents from their clinical duties so that they may attend the Combined Otolaryngology Spring Meeting sponsored by the Department one time .
In addition, all residents who have abstracts accepted for podium presentation at a regional or national meeting will be relieved of their clinical responsibilities to attend the meeting and present their data. PGY1 -3’s who have abstracts accepted for poster presentation at a regional or national meeting will be relieved of their clinical responsibilities, if possible, to attend the meeting. They will be eligible to receive funding to offset the costs of the meeting (currently set at a maximum of $1,400 per conference). There is no maximum on the number of conferences a resident may attend. See Policy on Resident Travel.
Fellowship Interviews
17
Many otolaryngology residents pursue fellowships in otolaryngology subspec ialties after their residency. The faculty recognizes that residents need to interview for these fellowships and will make every effort to release residents from their clinical duties so that they may attend these interviews. Fellowship applicants are ask ed to try to minimize the days away from their rotation as their absence places an undue burden on their fellow residents.
12. Resident Travel and Conference Funding Policy
Note: Check the latest updates on University-sponsored travel.
Resident travel to the following scientific meetings will generally be approved for departmental support: American Association for Research in Otolaryngology (A RO), Combined Otolaryngological Spring Meetings (COSM), American Academy of OtolaryngologyHead & Neck Surgery Annual Meeting (AAO -HNS), and Section Meetings of the Triological Society. Travel to other meetings may be approved on a case -by-case basis by the program director.
In addition, funding approval will require that the following three circumstances exist:
The resident must be the podium speaker, course lecturer, or poster presenter. Poster presentations are generally acceptable only for PGY1 -3 residents (at the time of the presentation). If a poster of a PGY4-PGY5 resident is accepted the resident may be eligible for travel funding but this must be approved by the program director ahead of time . However, posters on laboratory basic science topics a re acceptable at any training level.
In addition, the work must be original and presented for the first time and, the presentation must be accompanied by a manuscript that is submitted to a peer reviewed journal before the time of the meeting.
Major Expense Guidelines (Note: Beginning Jan. 2022, residents are also required to book their travel, including flight and hotel, through the Stanford Travel program for sponsored trips):
• Roundtrip airfare will be reimbursed at the lowest available fare purchased through Egencia: https://stanfordtravel.stanford.edu/ (using your SUNet ID and pw) .
• Hotel lodging should also be booked through Egencia (except for conference hotels) or use the itinerary-forwarding service. and rates should be reasonable and follow university’s Hotel Lodging Rate Guidance: https://web.stanford.edu/group/fms/fingate/staff/travel/policy_notes/lodging.html
• Meeting registration reimbursement will be b ased on early pre-registration, not at-the-door fees.
• All ground transportation reimbursement is based on actual expenses and should be reasonable and necessary. Per AGM 5.4.2, use Stanford Travel to book rental cars.
• Meals will not be reimbursed.
• Total departmental reimbursement for a given meeting will be a maximum of $1,400 per domestic trip.
18
• Poster expenses are reimbursed up to $100. This is considered separate from the travel expenses.
NOTE: The ultimate approval of all resident travel at departmental expense is at the discretion of the program director and departmental chair. Approval of reimbursement for travel not meeting the above criteria may be possible under certain circumstances and will be evaluated on a case-by-case basis.
13. Personal Time-off
House staff are permitted to take up to three weeks of personal time off with pay during each one-year period. Vacation should be scheduled in 1-week blocks unless prior approval is obtained from the program director and the rotation director (fo r example if 2 weeks are requested together or if a partial week is requested) . Personal time off must be requested and subsequently approved through the MedHub system. Stanford University Medical Center believes that personal time away from the residency program is important to the welfare of house staff, so unused personal time off does not accumulate from year to year and there is no provision to pay in lieu of time off.
Residents should not plan on taking vacation at the time of the in -training exam, during the time of the Annual Program Evaluation (Residency Retreat), or during the week of the chief residents’ graduation dinner and the annual Resident Research Symposium. At a minimum, rotation directors and the PD should be notified no less than 2 weeks before the rotation starts. All time off must be recorded in MedHub
So-called “terminal leave,” vacation as the final week of residency, will be considered on an individual basis for residents who will be pursuing a fellowship. A resident who i s taking terminal leave should not take an additional week of vacation during the same rotation block.
Time off for fellowship/job interviews
Residents are not permitted to take vacation in any quarter in which they will be gone for more than five days due to interviews. Residents must report the number of days they will be taking off to the program director. To avoid patient care coverage issues, PGY2 ’s should try not take vacation when a resident on the same rotation is interviewing.
14. Resident Work Hours and Call
The Department of Otolaryngology Head & Neck Surgery is committed to following the current ACGME policies on duty hours. See GME handbook for policy.
19
The resident call schedule will be determined by the chief residents. First call is shared among junior and senior residents; the second call is by the chief resident, or in the event of the chief resident’s absence, by the most senior resident on the service. Third call is staffed by a faculty member. Recognizing the individual resident circumstances and needs and acknowledging the autonomy of the specific si tes within the residency program, it is understood that the residents will be allowed to determine their own call schedule, to the extent that this does not create any undue hardship for any individual resident and it follows the above guidelines. As much as possible, no resident should be on call 2 weekends in a row. Resident work hours are monitored on a weekly basis and any potential issues are addressed immediately.
The following guidelines were adopted starting the 2020-2021 Academic Year to address duty hour concerns:
All Residents:
• All day residents should leave the hospital by 9 :00 pm weekdays. May voluntarily elect to stay (if working within 80 hours/week, 1 in 7 days off guidelines):
– to continue to provide care to a single severely ill or unstable patient
– humanistic attention to the needs of a patient or family
– to attend unique educational events
• The night float resident should actively take over day residents’ work (e.g., in the OR) to allow them to leave by 9 :00 pm, if there are no active consults.
• Attending or fellow to dictate cases when finishing after 9 :00 pm when the day resident has left.
Junior Residents
• Chiefs may allow junior residents on call for the weekend (PGY 2 –4) to skip morning rounds during the week.
– These residents should also leave the hospital each day as soon as their clinical responsibilities are completed.
• Peds Weekend Rounds: The post-call resident rounding must leave the hospital by 10:00 am to finish their shift within the 24 hours + 4 hours of transition time guidelines.
– The SHC junior resident or chief should take over any remaining work to allow for the resident to leave on time.
– Attending on weekend call must round no later than 8 :00 am.
Interns
• SHC intern on for the weekend can work a maximum of 14.5 hours/weekday and 7 hours/weekend day (6 :00 am – 1:00 pm) (86.5 hours total. This will be balanced out by weeks where they are not on call to remain under the 80 hour/week average ).
• LPCH intern can work a maximum of 14.5 hours/weekday and 7 hours on Saturd ay (6:00 am – 1:00 pm) (79.5 hours total).
20
– LPCH intern is on every Saturday during the rotation.
• Chiefs should ensure these hours are adhered to by scheduling clinical responsibilities accordingly and releasing interns by 7:30 pm even if PM rounds have not been completed.
Valley/VA Night and Weekend Call
• Full-time research residents will take 1 weekend of call per month. They may also take up to 1 weeknight call on the other weeks.
• PGY4s on research time may take 1 weeknight call per week
– When there are no full-time PGY3 residents, the PGY4 on research will follow the call schedule for full-time research residents.
• Frequency of weeknight call for research residents may vary depending on the number of residents on research at one time.
On-call rooms are pr ovided.
All residents are required to enter their work hours into the MedHub system on at least a weekly basis.
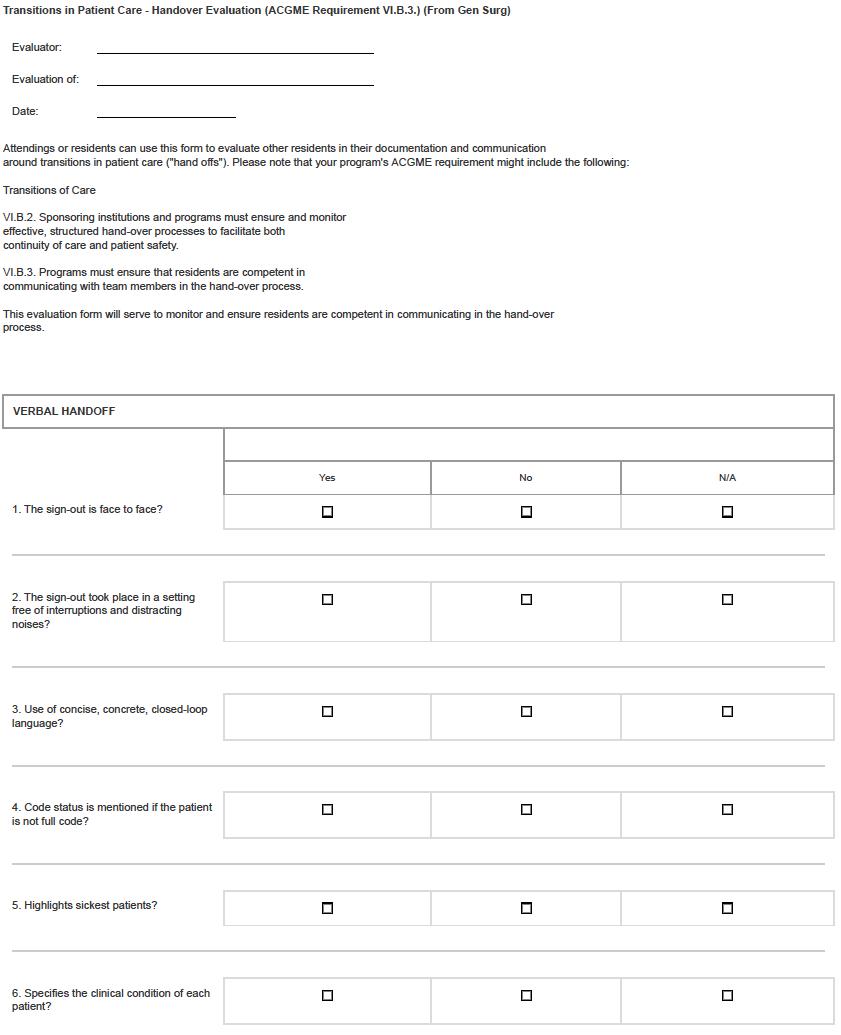
15. Departmental Hand-over Policy
When on-call, residents typically cover patients at more than one hospital. For this reason, a verbal check-out procedure via phone is currently used by the resident staff. Elements of this policy include:
Prior to leaving the hospital each day:
• Junior residents check -out to on-call junior resident or to night float resident every patient via I-PASS (I: Illness severity; P: Patient summary; A: Action items; S: Situation awareness and contingency planning; S: Synthesis by receiver).
• After checking out, the Junior resident(s) with the ghost consult and floor pagers will reassign the pagers to the on-call resident. In the morning the resident assuming the consult pager will reassign the ghost pager, and each resident covering the floor ghost pagers will reassign the pagers.
• Senior/chief residents check out to senior/chief residents regarding all unstable/concerning patients.
• Faculty members check out all concerning patients to faculty member on call.
16. Operative Case Logs
21
All residents are required to enter data on their surgical cases into the ACGME system in a timely manner (every week recomm ended, operative logs must be up-to-date at the time of the semi-annual resident meeting with the program director or associate program director .)
Residents are responsible for keeping track of the surgical cases in which they participate.
A Resident Supervisor instructs, and assists as needed, a more junior resident during a procedure during which the junior resident performs greater than or equal to 50% of the operation, including the key portion(s) of the procedure. The attending functions as an assistant or observer.
A Resident Surgeon performs greater than or equal to 50% of the operation with the attending surgeon (and resident supervisor, if applicable), including the key portion(s) of the procedure.
An Assistant Surgeon performs less than 50% of the operation, or greater than or equal to 50% of the operation but not the key portions(s) of the procedure.
Residents are responsible for entering all data into the ACGME database. Accuracy in this endeavor is critical, both for justifying a residen t’s suitability for sitting for the board examination, as well as accurately reflecting the volume of surgery done in the program.
The required minimum number of key indicator procedures is listed in Appendix D. Coding guidelines are listed at:
https://medwiki.stanford.edu/display/ent/Protocols+and+Forms
17. Communication
Addresses: The resident home addresses, email addresses, home phone numbers and cell phone numbers should be provided to the administrative staff within the department and updated on Medhub.
E-mail: Residents are required to maintain an active Stanford e -mail address that is checked regularly (at least every 48 hours). All clinical and academic e-mail should be sent through this system. All e-mail with protected health information (PHI) must be sent securely (this is done by typing “SECURE:” at the beginning of the e-mail subject line).
18. Guidelines for Online Professional or Personal Activity
These guidelines apply to Stanford OHNS residents in social medical venues such as professional society blogs, LinkedIn, Google+ , Instagram, Twitter, and/or Facebook, etc. for deliberate professional engagement or casual conversation.
22
• Protected Health Information, including photographs, may not be placed on social media sites.
• For the purposes of education, descriptions of patient cases and clinical images may be posted to password protected professional sites once the data has been deidentified.
• By virtue of identifying oneself as a part of Stanford in social media, residents connect themselves to, and reflect upon, Stanford colleagues, Stanford patients and supporters.
• Remember that all content contributed on all platforms becomes immediately searchable and can be shared. This content leaves the contributing individual’s control forever.
19. Policy and Guidelines for Interactions with Industry
The above policy may be accessed at: https://med.stanford.edu/siip/home.html Highlights of this policy include:
1)Medical staff, faculty, students, and trainees may not accept gifts from Industr y anywhere at the Stanford SOM, SHC, LPCH, or other clinical facilities operated by either hospital. It is strongly advised that no form of personal gift from Industry be accepted under any circumstances.
2)Free drug samples given directly to members o f the SUMC are considered gifts and may not be accepted, except by the pharmacy for use for needy patients.
3)Gifts or compensation may not be accepted a) at any Stanford or non -Stanford facility such as other hospitals and outreach clinics, b) for liste ning to a sales talk by an industry representative, c) for prescribing or changing a patient’s prescription, d) for simply attending a CME or other activity or conference, including the defraying of costs.
4)Meals or other types of food directly funded by Industry may not be provided at Stanford SOM, SHC, LPCH, or Menlo Clinic.
5)Sales and marketing representatives are not permitted in any patient care areas except to provide in-service training on devices and other equipment and then only by appointment. They are permitted in non-patient care areas by appointment only.
6)Industry support of students and trainees in the SOM educational programs should be free of any actual or perceived conflict of interest, must be specifically for the purpose of education and must comply with several provisions: a) The Department selects the student or trainee, b) The funds are provided to the School, department, program, division, or institute and not directly to the student or trainee or to an individual faculty member; c) The department, program, division, or institute has determined that the funded conference or program has educational merit, d) the recipient is not subject to any implicit or explicit expectation of providing something in return for the support.
23
SOM faculty, students, staff and trainees should evaluate carefully their attendance at meetings and conferences that are fully or partially sponsored or run by Industry because of the potential for perceived or real conflict of interest.
20. Stanford Department of OHNS Guidelines for Consultations
General guidelines for all consults:
◼ Otolaryngology is a service oriented specialty where relationships with practitioners of other services are established and maintained.
◼ ALL consults should be seen the day they are received unless it is late in the day and the referring provider expressly states that it is fine to see the next day. If the consult is received but not seen on that day, please see the consult yourself on the following day so another resident i s not left with your work.
◼ If a consult is received and you think it is truly an inappropriate consult , an OHNS Chief Resident MUST hear about the consult and give permission for the OHNS resident to not see the consult.
◼ Consults take priority over the O R.
◼ All consults must be staffed with the on call attending the day of the consult.
◼ A consult note must be entered on the day of the consult (including vocal fold consults). This includes any consult you see, even ones that are immediately signed off on.
◼ A full consult note must be entered for every consult patient. It is not OK to only enter a procedure note without a consult note (for example: a full consult note needs to be entered for a patient with possible vocal fold paralysis – not just the laryngoscopy note.)
◼ During the day, the consult note may (and should) be started but not completed (i.e. don’t put the assessment and plan) until the consult has been seen/discussed with the attending.
◼ All outpatient calls should be returned in a timely fash ion and have a telephone encounter documented in the appropriate EPIC.
◼ The night float residents should see and document all consults - even ones that are not urgent.
◼ Referring providers should be treated with respect – just as we want to be treated when we call in a consult. Inevitably, we will receive some consults for conditions we think are “silly” or “a waste of time”. Remember that we sometimes call in these types of consults too. A consult is a request for help. BE NICE.
Emergency Department Consultations:
◼ Should be seen within 1 hour of receiving the call (obviously , quicker for urgent consults)
◼ Always check out with the ED physician- don’t leave without talking to them.
24
Consults at SHC:
◼ The Consult PGY 2 (and occasionally 1) serves as the front-line consult resident.
◼ Consults will be added to the team of the staffing attending (ie a consult staffed by a Scope attending will go to the Scope service.)
◼ Trach consults will go to the service of the staffing attending.
◼ Vocal fold consults go to the Headmirror service.
◼ Existing H&N patients with a H&N issue will go to Scalpel even if not yet staffed with the H&N attending (i.e. laryngeal tumor patient followed by Kaplan in the past but staffed with rhinology fellow will go to H&N)
◼ New H&N patients will go to team of staffing attending unless directed otherwise by the chief (i.e. new tongue SCC consult staffed by FPRS fellow will go to Scope at first.)
◼ If you want a consult to be seen in a fellow/instructor clinic (i.e. mandible fracture to be seen in FPRS clinic) you must email, call or text that attending. A STAFF MESSAGE ALONE IS NOT SUFFICIENT!
Consults at LPCH: Please refer to Peds Service Guidelines provided by the division.
25
21. Otolaryngology Post-Graduate Educational Program
Goals and Objectives PGY 1 - Non-OHNS rotations
Rotation Contacts and Scheduling Details
Rotation Director: Kwang Sung, MD, MS
NOTE: All residents, including the PGY1 residents, will take the in - training exam on the first Saturday in March.
Rotation details:
The daily schedules will be determined by the chief residents/faculty on each individual rotation. While on other rotations residents should attend the resident education sessions for that specialty. Residents should attend the OHNS education sessions when feasible.
Radiology/Research Rotation
This rotation is comprised of neuroradiology, audiology, neurology and research.
Rotation Contacts & Addresses
Rotation Directors: Mrudula Penta, MD (Neuroradiology)
Matt Fitzgerald, PhD
Clinics: Besides Stanford and LPCH, the locations for this rotation include:
• 451 Sherman Ave
• Hoover 2 Pavilion (SNHC, Stanford Neurosciences Health Center, 213 Quarry Rd)
• VAPA
26
• Stanford Ear Institute (Watson Court)
Rotation Details:
• One week before the rotation, resident is to touch base with Dr. Mrudula Penta for orientation plan and sharing of documents, including upcoming faculty/fellow schedules and conference schedules.
• At least one week before the rotation, resident is to make an appointment with Drs. Kara Meister or Iram Ahmad, residency research committee faculty, to discuss research goals.
• At least two half-days are to be spent in neurology clinic shadowing Dr. Kristen Steenerson (on Mondays, Tuesdays, Thursdays or Fridays). Please contact Dr. Steenerson one month in advance to arrange.
• Residents will attend OHNS conferences on Monday mornings and neuroradiology conferences (see list) as appropriate and as possible. The mornings will generally be spent in the neuroradiology reading rooms at Stanford, LPCH, Sherman Ave and/or Hoover.
• One afternoon (Wednesday or Friday) a week will be spent in audiology, primarily at the Stanford Ear Institute at Watson Court.
• Afternoons not spent in audiology or neurology are to be utilized to develop research plans.
Residents are required to complete the project specified in the G&Os.
Conferences: In addition to attending Monday morning and Thursday afternoon OHNS conferences, the resident is encouraged to attend the following conferences, depending on appropriateness of content. Current schedules can be provided by Dr. Penta or by neuroradiology program coordinator Malika Curry (mcurry18@stanford.edu).
27
Conference Time Locations Mondays – Neuroradiology Fellows Conference 1:30 PM Zoom at present (Zoom info available
Tuesdays – Neuroradiology Fellows Conference 7:30 AM Zoom at present (Zoom info available on the monthly conference schedule)
Neurosurgery Skull Base Conference 5:30
Zoom at present (Zoom info available on the monthly conference schedule)
on the monthly conference schedule)
Tuesdays –
PM
Wednesday – Third Wed of month (usually): Peds ENT Radiology Conference
5-6pm
Thursdays – Radiology Resident didactic block Noon-5pm (if Neuro lectures, typically at 12:30 and 1:30 p.m.)
Thursdays – Head & Neck Tumor Board 4:30-6:30 PM
Radiology readouts:
LPCH Conference Room
Zoom at present (Zoom info available on the monthly conference schedule)
Zoom at present (Zoom info available on the monthly conference schedule)
• 8:30 am to 11 am is likely the best time for a consistent read-out experience
• Additional one-on-one Radiology review time via Zoom might be available during preparation of the Tuesday Skull Base conference (Dr. Fischbein) or the Thursday Head and Neck Tumor Board (Dr. Fischbein, Dr. Penta, or Dr. Nancy Pham)
• Observation of image-guided biopsy procedures might also be possible – touch base with Dr. Pham for this option
Other Resources:
• Diagnostic Imaging: Head & Neck, 3 rd Edition by Koch, et al
• Expert Differential Diagnoses: Head & Neck, by Harnsberger
• AJNR (Am J Neuroradiol) Special Collections:
-link to H+N papers: http://www.ajnr.org/site/specCol/SpecColl7TOC.xhtml
-note: a bound copy can be ordered for $50 if one wants to
Competency-based Goals and Objectives
General & Plastic Surgery rotations: To be able to provide pre -and postoperative care to the surgical patient.
Resident Objectives: ACGME Competency Goals
Be able to take a detailed surgical history and review relevant medical records.
Be able to perform a detailed physical examination.
Patient Care
Interpersonal and Communications Skills
Patient Care
Medical Knowledge
28
Be able to write/dictate a thorough and succinct history & physical.
Patient Care
Interpersonal and Communications Skills
Understand the process of obtaining a surgical informed consent.
Be able to complete a thorough clinical note in the inpatient record.
Understand NPO guidelines.
Understand fluid management in the NPO patient.
Understand the basic laboratory and radiologic tests performed for the pre -operative and post-operative patient.
Understand the basics of nutritional support for the surgical patient.
Understand operative sterility principles.
Understand the diagnosis and basics of management of surgical related infections.
Understand the guidelines and use of prophylactic antibiotics.
Learn how to effectively utilize the “EPIC” computerized medical record.
Patient Care
Systems-Based Practice
Interpersonal and Communications Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Systems-Based Practice
Goal for Surgical Intensive Care Unit rotation: To understand the basics of care for the critically ill surgical patient.
Resident Objectives:
Understand the different types of shock.
Understand the various types of monitoring catheters and how to interpret the data obtained
Understand the basic principles of mechanical ventilation.
Understand effective preventive measures for deep vein thrombosis and pulmonary embolus.
Understand the basics of EKG interpretation
ACGME Competency Goals
Medical Knowledge
Medical Knowledge
Medical Knowledge
Medical Knowledge
Patient Care
Medical Knowledge
29
Understand the basics of renal physiology and electrolyte disturbances.
Understand the basics of pulmonary physiology
Be able to manage the nutritional needs of the surgical patient.
Learn about optimal communication between the intensivists and surgical teams.
Medical Knowledge
Medical Knowledge
Patient Care
Professionalism
Systems-Based Practice
Goals of Emergency Medicine rotation: To understand the basics of care in the emergency department.
Resident Objectives: ACGME Competency Goals
Learn about the process of E.D. triage.
Know how to evaluate the most common disorders seen in E.D. patients.
Learn how to work with the E.D. personnel and other medical professionals to evaluate and treat patients.
Learn the basics of laceration closure.
Goals for Anesthesia Rotation: To become familiar with the basics of anesthesia care.
Resident Objectives:
Know basic laryngeal anatomy.
Know appropriate indications for general versus local versus regional anesthesia.
Know the important features of the most common surgical anesthetics used in the operating room.
Understand appropriate preoperative tests for patients undergoing anesthesia.
Be able to interpret the anesthesia record.
Be familiar with various types of intraoperative monitoring.
Medical Knowledge
Patient Care
Systems-Based Practice
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Systems-Based Practice
Patient Care
Medical Knowledge
ACGME Competency Goals
Medical Knowledge
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Medical Knowledge
Patient Care
Medical Knowledge
Medical Knowledge
Patient Care
30
Be able to perform orotracheal intubation.
Learn about optional communication between anesthesia and surgical teams.
Learn how to participate in a “time out” session and understand the importance of surgical checklists.
Patient Care
Patient Care
Professionalism
Systems-Based Practice
Patient Care
Systems-Based Practice
Goals of Neuroradiology/Audiology/Neurology/Research rotation : To become facile at ordering and reading imaging studies of the head and neck, to understand the basics of audiology and vestibular testing, become familiar with basic neurological assessments, and learn the fundamentals of conducting medical research.
Resident Objectives: ACGME Competency Goals
Know the anatomy of the head and neck as seen on CT and MRI.
Understand which type of imaging study is best for which type of clinical disorder.
Understand the appearance of common head and neck disorders as seen on radiologic images.
Learn how to best interact with members of the radiology department.
Spend at least two sessions observing a CT/MRI technologist to develop familiarity with scanning processes, radiation dosing and safety.
Attend OHNS and neuroradiology education conferences
Project: Assemble 10 to 15 cases of interest. These should be in PowerPoint format and presented as teachable cases. In their PGY2 year, the resident will present this at a residency education session.
Spend time in audiology a minimum of one afternoon/week learning about audiologic testing for all ages, hearing aids and cochlear implants.
Learn the basics of audiology evaluation in adults. Be able to perform an audiogram.
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Systems-Based Practice
Medical Knowledge
Patient Care
Medical Knowledge
Practice Based Learning
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
31
Learn and observe the types of audiologic testing in children.
Medical Knowledge
Patient Care
Understand the types of newborn hearing screens and the associated laws regarding screening.
Observe the various types of vestibular testing and understand when each type is indicated.
Learn to take a detailed vertigo/dizziness history.
Become familiar with how to conduct a thorough vestibular physical exam
Begin to understand the workup of a vestibular patient
Obtain exposure to how to interpret results of vestibular/balance testing, including VEMP, VHIT, VNG, rotary chair, CDP
Describe vestibular pathologies, both central and peripheral.
Learn management options in the treatment of patients with dizziness.
Attend or view online research training course
Medical Knowledge
Medical Knowledge
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Systems-Based Practice
Medical Knowledge
Medical Knowledge
Medical Knowledge
Patient Care
Medical Knowledge
32
Stanford Health Care Headmirror Service
Rotation Directors: Laryngology
C. Kwang Sung, MD, MS
Weekly Schedule
AM
Sleep Medicine
Robson Capasso, MD
Comprehensive Uchechukwu Megwalu, MD, MPH
Monday Tuesday Wednesday Thursday Friday
Megwalu OR Lee clinic
Capasso OR (RWC)
Nuyen clinic (RWC)
Sung OR Capasso clinic (RWC)
Megwalu clinic
Sung clinic
Capasso OR Lee clinic Liu clinic (RWC)
Lee OR (alternate weeks)
Damrose clinic
Capasso clinic (RWC)
Megwalu clinic
Lee OR (alternate weeks)
Damrose OR
Sung OR (4th & 5th Fri)
Liu clinic (RWC)
PM
Megwalu OR Lee clinic
Nuyen clinic (RWC)
Sung procedure clinic
Capasso clinic (RWC)
Liu OR
Megwalu clinic
Sung clinic
Capasso OR Lee clinic
Liu clinic (RWC)
Lee OR (alternate weeks)
Damrose clinic
Capasso clinic (RWC)
Megwalu clinic
Goals and Objectives PGY 1: SHC Headmirror Service
Lee OR (alternate weeks)
Damrose OR
Sung OR (4th & 5th Fri)
Liu clinic (RWC)
The PGY-1 will participate in otolaryngology rounds and under the direction of the chief/senior resident will be responsible for care of inpatients.
Call duties: The PGY1 resident will take call for in -house floor patients from 6:00 am until after rounds are complete and residents are released by the chief resident. On assigned weekends, they will take floor call during the day. PGY -1 residents will not take overnight call.
NOTE: All residents, including the PGY1 residents, will take the in - training exam on the first Saturday in March.
33
Evaluation and Feedback
The OHNS Faculty on the Headmirror Service (and selected ancillary medical personnel) will complete written evaluations at th e end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Faculty Member and the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interacti ons.
Competency-based Goals and Objectives
Goal 1: Otolaryngology (“Headmirror”) Rotation: To be able to provide pre - and post-operative care for the otolaryngology surgical patient.
Resident Objectives: ACGME Competency Goals
•Know the important aspects of history and physical examination of the otolaryngol ogy patient.
•Begin to understand the diagnosis and treatment of common otolaryngologic disorders.
•Become familiar with the ACGME resident case log system.
•Demonstrate self-awareness and time management/organizational skills.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Systems-Based Practice
Practice-Based Learning and Improvement
Goal 2: Otolaryngology (“Headmirror”) Rotation: To begin to develop otolaryngology surgical skills.
Resident Objectives: ACGME Competency Goals
•Resident will know the names of common surgical instruments.
•Resident will learn basic suturing and knot tying techniques.
•Resident will know how to set up the OR for routine otolaryngology cases.
•Resident will learn the basic techniques of Direct laryngoscopy, Esophagoscopy, Bronchoscopy.
• Resident will learn the basic techniques of DISE/flexible nasopharyngoscopy, inferior turbinate reduction, frenulotomy, arch bar removal, tonsillectomy.
•Resident will gain experience by assisting with surgical procedures.
•Resident will be introduced to flexible laryngoscopy.
•Resident will learn basics of dissection of soft tissue of the face and neck.
Patient Care
Goal 3: Otolaryngology (“Headmirror”) Rotation: To begin to organize a plan for a research project during residency .
Resident Objectives: ACGME Competency Goals
• Meet with at least three faculty members about possible research projects during the otolaryngology research rotation in the PGY3 year .
Professionalism
34
Objectives
Rotation Contacts and Scheduling Details
Please coordinate schedules and care with Attending Surgeons from Head and Neck Surgery (Capasso, Damrose, Lee, Liu, Megwalu, Nuyen, Sung)
Rotation Specifics
1. Rounding expectations: team is to round together in the morning with the chief resident leading. All members of the team are expected to know what is going on with each patient. On discharge, patients should have a date and time for follow -up. The team should establish this prior to discharge by calling the clinic or communicating with the P.A. The chief resident is expected to be teaching the juniors on rounds.
2. Communication with faculty regarding patients after rounds/weekends:
• Communication of some sort is expected each day with each attending. For some, a text message is fine; for others, a phone call. At the start of the service, the chief should establish the best mode of communication with each attending.
• When talking with patients, residents should avoid relaying care plans if there is uncertai nty. They should tell the patient that they will check with the attending.
3. Communication with faculty regarding night-time contact with patients
For serious issues (e.g. should a patient go back to the OR), it is ideal if calls go up the chain of command. R2s and R3s on call should call their chief resident to evaluate, who should notify the fellow, and then the attending. The R2 or R3 should NOT bypass senior residents and go directly to the attending. This is for teaching purposes.
4. Residents are expected to make entries into medical records for night -time patient contacts. A note should be entered into Epic for each contact with patients.
5. Residents should strike a balance between learning in the clinic and operating room. However, the chief resident should anticipate and plan in advance so that clinics can be covered as much as possible. This may require asking residents from oth er services to help. It may be advisable to limit vacation during the months of heavy R4 interviews.
6. A brief operative note should be entered within an hour of completion of the surgery by the resident. Dictation of operative reports: within 24 hours.
35
Goals and
PGY 2/3: SHC Headmirror Service
7. Preparation for OR: Decide a personal goal to achieve in each case. Discuss case with attending the day before. Read about the case. Know the patient and why the operation is being performed, the labs, etc. Seek feedback from faculty by directly asking faculty.
8. When faculty is out of town, continue to communicate with attending daily if available by cell phone. If not, then, communic ate with the covering attending or instructor (designated by the attending prior to leaving).
Evaluation and Feedback
The OHNS Faculty on the Headmirror Service (and selected ancillary medical personnel) will complete written evaluations at th e end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Faculty Member and t he rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interact ions.
Competency-based Goals and Objectives
Goal 1. Consults in an adult tertiary care hospital. Learn about the most common consults requested from other medical and surgical services regarding laryngeal and general otolaryngology problems in adults.
Resident Objectives:
Be the initial contact person for all consults from other SHC services and the emergency department.
ACGME Competency Goals
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Perform initial evaluation of all consult patients when designated and for all laryngology consults.
Be familiar with the S HC electronic medical record (EPIC) and be able to access information appropriately. Understand the importance of confidentiality in patient medical records.
Evaluate consult patients with senior resident or fellow and faculty member and communicate recommendations and plan to primary team. Consistently demonstrate courtesy when interacting with clinical and non -clinical staff members.
Patient Care
Medical Knowledge
Patient Care
Professionalism
Systems-Based Practice
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Perform a literature search to learn more about unusual patient problems.
Medical Knowledge
36
Create a complete and coherent consultation note and dictate it in a timely fashion. This objective applies to all patients seen in the clinic setting as well as the outpatient setting.
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Professionalism
Utilize translation services to communicate with non-English speaking patients as needed. Interpersonal and Communication Skills
Systems-Based Practice
Demonstrate effective time -management skills.
Follow-up on consult patients as needed.
Prepare and present at the weekly Head and Neck Case conference.
Practice-Based Learning and Improvement
Professionalism
Patient Care
Systems-Based Practice
Professionalism
Medical Knowledge
Systems-Based Practice
Goal 2. Hoarseness. Screen, diagnose and manage patients with symptoms secondary to vocal fold/laryngeal pathology.
Resident Objectives:
Be able to describe the anatomy, physiology, and pathophysiology of the larynx.
Take a history with focused questions that assist in the diagnosis of hoarseness.
Describe the use of diagnostic tests for assessing hoarseness (e.g. airway films, sleep studies, laryngeal endoscopy, videostroboscopy).
Be able on physical examination to assess abnormalities of the vocal folds (ie, paralysis).
Describe how to identify a paralyzed vocal fold.
Be able to counsel patients/parents about the pathophysiology of conditions associated with vocal fold paralysis.
Understand the indications for medialization (e.g., injection, thyroplasty) and alternative therapies.
Be able to counsel parents about the risks and benefits of vocal fold medialization.
Know the perioperative management and expected postoperative course of patients who undergo vocal fold medialization.
ACGME Competency Goals
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Patient Care
Patient Care
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Professionalism
Interpersonal and Communication Skills
Patient Care
37
Be able to safely and efficiently perform a flexible nasolaryngoscopy and videostroboscopy.
Be able to discuss the treatment of and provide care to patients with complications of laryngoscopy.
Goal 3. Swallowing. Be able to evaluate and treat swallowing disorders in adults.
Patient Care
Patient Care
Interpersonal and Communication Skills
Resident Objectives: ACGME Competency Goals
Be able to describe the anatomy, physiology, and pathophysiology of the pharynx and esophagus.
Be able to take a history related to the pharynx and esophagus as regards swallowing problems.
Understand the available treatments for dysphagia.
Be able to discuss the indications, risks, benefits and alternatives to dilation and to cricopharyngeal myotomy.
Be familiar with the endoscopic and open methods of treating Zenker’s diverticulum.
Understand the available bedside and radiographic methods of assessing swallowing.
Be able to discuss and treat complications from esophagoscopy.
Goal 4. Expand ability to perform surgical procedures
Resident Objectives:
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Patient Care
Patient Care
ACGME Competency Goals
Patient Care such as:
Be able to competently and efficiently perform mid -level procedures with attending assistance
• Microdirect laryngoscopy
• Flexible and rigid Esophagoscopy.
• Injection laryngoplasty
• Tonsillectomy
• Septoplasty
• Turbinate reduction
• Tracheostomy
• Panendoscopy
38
• Submandibular gland excision
• Excision of congenital cysts
• Eustachian tube dilation
• Resection of small carcinomas (e.g. tongue, floor of mouth)
Goal 5. Sleep Medicine. Know about normal sleep/wake neurobiology and respiratory physiology
Resident Objectives: ACGME Competency Goals
Be familiar with the sleep/wake neural centers and connections associated with normal sleep/wake cycles.
Know the sleep stages and architecture.
Understand options for treatment of nasal septal deviation and turbinate hypertrophy..
Goal 6. Know about common sleep disorders and their consequences
Medical Knowledge
Medical Knowledge
Medical Knowledge
Patient Care
Resident Objectives: ACGME Competency Goals
Be able to define and describe the following sleep disorders:
Sleep related breathing disorders (SRBD)
Insomnia
Circadian rhythm sleep disorders
Hypersomnias, parasomnias and sleep related movement disorders
Insufficient sleep syndrome.
Medical Knowledge
Patient Care
Goal 7. Know how to obtain a sleep history and comprehensive physical examination in patients with sleep complaints
Resident Objectives: ACGME Competency Goals
Be able to obtain a sleep history including the ability to identify associated comorbidities from poor sleep: mood and cognitive dysfunction, hypertension, atrial fibrillation, cerebrovascular accidents.
Know the Epworth sleepiness scale and be able to administer and interpret the results.
Be able to identify craniofacial and soft tissue abnormalities associated with SRBD.
Patient Care
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Goal 8. Understand the options for evaluating patients with sleep disorders and how to interpret the appropriate clinical stu dies.
Resident Objectives: ACGME Competency Goals
39
Understand technological tools involved in polysomnographic and home monitoring devices, including EEG, EMG, EOG, EKG, airflow sensors, respiratory effort belts, oximetry/gas monitoring, esophageal pressure, arterial pletismography.
Be able on a polysomnogram to identify respiratory events including apneas/hypopneas, RERAs and hypoventilation.
Understand the indications and interpretation of the multiple sleep latency test.
Understand the use of imaging studies in patients with sleep disorders.
Goal 9. Improve general otolaryngology knowledge
Resident Objectives:
Develop competence in the interpretation of head and neck imaging studies through regular review of all patient imaging and attendance at radiology rounds.
Learn to set-up and use the facial nerve integrity monitor.
Demonstrate competence in the safe and appropriate use of various lasers.
Learn the nuances of correctly coding surgical procedures, consultations, and outpatient visits (CPT and ICD -9).
Be able to appropriately document patient care to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of healthcare.
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
HALF-TIME RESEARCH RESIDENT
• Research Resident must have at least 2.5 days of research time per week on average.
Medical Knowledge
Medical Knowledge
Medical Knowledge
Medical Knowledge
ACGME Competency Goals
Patient Care
Medical Knowledge
Patient Care
Patient Care
Patient Care
Systems-Based Practice
Patient Care
Systems-Based Practice
Professionalism
Systems-Based Practice
Professionalism
Professionalism
Practice-Based Learning and Improvement
• During PGY2/3 or PGY4’s vacation/conference/interview period, Half -time Research Resident usually works as full time.
40
Goals and Objectives PGY 4: SHC Headmirror Service
Rotation Contacts and Scheduling Details
Please coordinate schedules and care with Attending Surgeons (Capasso, Damrose, Lee, Liu, Megwalu, Nuyen, Sung)
Note: if there is no O.R. going on ( e.g., attending physician is out of town), the resident is expected to attend clinic.
Rotation Specifics
1. Rounding expectations: team is to round together in the morning with the chief resident leading. All members of the team are expected to know what is going on with each patient. On discharge, patients should have a date and time for follow -up. The team should establish this prior to discharge by calling the clinic or communicating with the P.A. The chief resident is expected to be teaching the juniors on rounds.
2. Communication with faculty regarding patients after rounds/weekends:
• Communication of some sort is expected each day with each attending. For some, a text message is fine; for others, a phone call. At the start of the service, the chief should e stablish the best mode of communication with each attending.
• When talking with patients, residents should avoid relaying care plans if there is uncertainty. They should tell the patient that they will check with the attending.
3. Communication with faculty r egarding night-time contact with patients
For serious issues (e.g. should a patient go back to the OR), it is ideal if calls go up the chain of command. R2s on call should call their chief resident to evaluate, who should notify the fellow, and then the a ttending. The R2 should NOT bypass senior residents and go directly to the attending. This is for teaching purposes.
4. Residents are expected to make entries into medical records for night -time patient contacts. A note should be entered into Epic for each contact with patients.
5. Residents should strike a balance between learning in the clinic and operating room. However, the chief resident should antic ipate and plan in advance so that cases can be covered as much as possible. This may require asking residents from other services to help . It may be advisable to limit vacation during the months of heavy R4 interviews.
6. A brief operative note should be entered within an hour of completion of the surgery by the resident. Dictation of operative reports: within 24 hours.
7. Preparation for OR: Decide a personal goal to achieve in each case. Discuss case with attending the day before. Read about the case. Know the patient and why the operation is being performed, the labs, etc. Seek feedback from faculty by directly asking faculty.
41
8. When faculty is out of town, continue to communicate with attending daily if available by cell phone. If not, then, communicate with the covering attending or instructor (designated by the attending prior to leaving).
Evaluation and Feedb ack
The OHNS Faculty on the Headmirror Service (and selected ancillary medical personnel) will complete written evaluations at th e end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Facult y Member and the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interactions.
Competency-based Goals and Objectives
Goal 1. Expand knowledge in the area of laryngeal oncology
Resident Objectives: ACGME Competency Goals
Be able to identify clinically suspicious lesions of the larynx and esophagus, perform appropriate biopsies and imaging studies to make a diagnosis in a cost effective and time efficient manner.
Understand risk factors for head and neck cancer, be able to assess patients for risk factors and be able to counsel patients about managing the risk factors.
Be able to acquire appropriate information to stage laryngeal cancers, to present cases in the Head and Neck Tumor Board and to determine the best treatment modality or modalities. When presenting the cases in Tumor Board, up -to-date literature will be used to support treatment decisions.
Be able to discuss the treatment options with the patient and make the appropriate consultations (medical oncology, radiation oncology, dentistry, speech pathology, physical therapy, nutrition, and or social work) based on the patient’s needs and wishes. This will require consideration of the patient’s rights and a sensitivity to cultural, age, gender and disability issues.
Administer care for the post-operative oncology patient.
Be able to describe principles about and perform interventions for early laryngeal cancer.
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Professionalism
Systems-Based Practice
Professionalism
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
42
Be able to perform interventions for advanced laryngeal cancer.
Goal 2: Be competent in evaluating and managing otolaryngology patients.
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Expand and refine evaluation and management skills of otolaryngology patients. Such knowledge should allow the R4 resident to confidently and independently care for otolaryngology patients by the end of the year.
Expand participation to include a leadership role in teaching conferences facilitating the learning of the junior residents and medical students.
Expand knowledge of Otolaryngology literature for diseases and disorders of the larynx and sleep surgery.
Understand the limits of surgical and medical treatment.
Understand indications for urgent operative decisions, such as a performing a surgical airway and decompressing an expanding neck hematoma
Recognize and manage surgical risk -factors.
Administer care for the post-operative patient.
Expand the capacity to recognize and treat post -surgical complications effectively, and learn to recognize preoperative risk factors.
Gain a healthy appreciation for the dangers inherent in medical intervention, and learn how to be appropriate in selecting patients for surgery.
Assume a leadership role in postoperative care of complications such as salivary fistula, wound infection, hematoma, cerebrospinal fluid leak, airway compromise, and hemorrhage. Teach the junior residents and medical students to manage these complications.
Medical Knowledge
Patient Care
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Practice-Based Learning and Improvement
43
Be able to successfully transition from supervision by faculty to primary decision making with faculty oversight.
Supervise presentation of complications on the service at monthly Morbidity and Mortality conference.
Demonstrate competence and organizational skills in directing the resident team in the daily management of in-house patients and OR activities.
Demonstrate ability and commitment in the day -to-day informal teaching and mentoring of students and junior residents.
Be able to competently supervise/assist junior residents performing common OTO/HNS surgical procedures.
Be able to demonstrate excellent interpersonal skills, effectively setting the tone for other members of the resident team, clinical and non -clinical staff.
Patient Care
Patient Care
Practice-Based Learning and Improvement
Practice-Based Learning and Improvement
Practice-Based Learning and Improvement
Practice-Based Learning and Improvement
Professionalism
Goal 3. Airway. Be able to evaluate and form treatment plans for adults with airway obstruction due upper airway and tracheal lesions.
Resident Objectives:
ACGME Competency Goals
Be able to describe the anatomy, physiology, and pathophysiology of the larynx. Medical Knowledge
Be able to recognize, describe and categorize stridor in adults. Know the most common causes of stridor and dyspnea in adults.
Be able to describe the various methods for managing a complex airway patient (i.e. awake fiberoptic intubation, hi -flow nasal cannula, jet ventilation, laryngeal mas k airway, rigid bronchoscopy, awake tracheostomy); their indications and their possible complications.
Be able to discuss routine care of a tracheostomy and describe how to recognize tracheostomy obstruction or decannulation. Be able to educate a patient about the risks/benefits and care of a tracheostomy. Be knowledgeable about how to obtain the needed tracheostomy related equipment for patient use at home.
Be familiar with the principal lesions that can affect vocal fold function in adults (i.e. papilloma, polyp, nodule, cancer).
Patient Care
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Systems-Based Practice
Patient Care
Medical Knowledge
44
Be able to identify the various methods for laryngeal framework surgery (e.g. thyroplasty, arytenoids adduction); their indications and their possible complications.
Know the instrumentation used to resect laryngeal lesions (i.e. endoscopic scissors, graspers, laser).
Patient Care
Medical Knowledge
Patient Care
Goal 4. Videostroboscopy. Be able to utilize and to interpret videostroboscopy in the diagnosis of laryngeal disorders.
Resident Objectives: ACGME Competency Goals
Be familiar with the setup and technique of videostroboscopy.
Understand the various components of laryngeal function which can be assessed with videostroboscopy (ie, vocal fold waveform, amplitude, glottic gap, etc).
Recognize the characteristic features of various disorders as diagnosed by videostroboscopy (ie, nodules, polyps, cysts, granulomas, spasmodic dysphonia).
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Goal 5. Sleep Medicine. Be able to effectively evaluate and treat a patient with a sleep related breathing disorder.
Resident Objectives: ACGME Competency Goals
Know the indications for PAP therapy, and different modalities including CPAP, auto PAP, BiPAP, Auto BIPAP, AVAPS, and ASV.
Evaluate and stimulate PAP compliance through clinical history and data downloaded from PAP machine.
Understand and be able to recommend methods to improve PAP compliance including mask refitting, use of EPR, referral to behavioral desensitization.
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Systems-Based Practice
Be able to integrate with other members of a sleep center, and know how to adequately refer patients for medical, dental, and behavioral management of sleep disorders.
Be able to analyze data from the history, physical examination, sleep test, nasal endoscopy, drug induced sleep endoscopy, and imaging tests and identify who will benefit from some sort of therapy and which therapy should be recommended.
Patient Care
Systems-Based Practice
Patient Care
Medical Knowledge
45
Be able to select appropriate candidates for oral device therapy.
Be able to inform the patient about weight loss, behavioral and positional management of SRBD.
Be able to ethically and thoroughly provide all available data to patients and help him/her make the best possible decision on surgical care of OSA.
Understand the indications, role and realistic goals of surgery. Be able to perform an adequate psychosocial assessment and explain why no surgical intervention may be the best choice for some patients. Be able to formulate an independent plan for surgical management of obstructive sleep apnea. Performing septoplasty, turbinate reduction, uvulopalatopharyngoplasty.
Understand the indications, techniques, benefits and risks of sleep surgery involving the facial skeleton (maxillomandibular advancement, maxillary expansion/DOME, genioglossus advancement). Performing critical parts of the procedure. Incorporate virtual surgical planning.
Understand the inclusion criteria of hypoglossal nerve stimulation. Performing critical Parts of the procedure. Understand the activation protocol after implantation.
Understand and describe risks and complications of OSA surgery, including voice and swallowing changes, complex pain management, facial paresthesias, infection, need for HGNS explant, facial profile and cosmetic changes and need for revision surgery. Be able to effectively and compassionately counsel patients of these details.
Effectively and comprehensively manage primary inhouse, post -operative and consult patients with obstructive sleep apnea with the junior and senior residents.
Demonstrate appropriate surgical technique for uvulopalatopharyngoplasty, be able to perform most of the cervical approach in hypoglossal nerve stimulation cases. Be able to perform Lefort osteotomies during maxillomandibular advancement
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Professionalism
Patient Care
Interpersonal and Communication Skills
Professionalism
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Medical Knowledge
Goal 6. Improve competency in the performance of laryngology, sleep, and general otolaryngology surgeries
Resident Objectives: ACGME Competency Goals
46
Be adept in performing the following procedures:
· Diagnostic endoscopy
· Operative microlaryngoscopy
· Tracheotomy
· Submandibular gland excision
. Sublingual gland excision
· Endoscopic dilatation and CO2 laser resection for subglottic stenosis and posterior glottic stenosis
· Uvulopalatopharyngoplasty and its multiple modifications
· Tongue surgery-volume reduction and/or tongue suspension/suture
Become increasingly skilled in performing the following procedures:
· Neck Dissection
· Laryngectomy (total and partial)
· Laryngopharyngectomy
· Parotidectomy
· Thyroidectomy
· Parathyroidectomy
· Type I thyroplasty
· Arytenoid adduction
· Cricotracheal resection
· Tracheal resection
· Maxillomandibular advancement, maxillary expansion/DOME, genioglossus advancement
· Hypoglossal nerve stimulator implant
Know the indications, perioperative care, expected outcomes and possible complications for all procedures listed above.
Demonstrate competence in the safe and appropriate use of various lasers.
Patient Care
Patient Care
Patient Care
Patient Care
Goal 7. Be able to take care of patients in an ethical, efficient and caring manner within the current medical system
Resident Objectives: ACGME Competency Goals
47
Develop competence in the interpretation of head and neck imaging studies through regular review of all patient imaging and attendance at radiology rounds.
Learn the nuances of correctly coding surgical procedures, consultations, and outpatient visits (CPT and ICD -9).
Be able to appropriately document patient care to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
Patient Care
Systems-Based Practice
Professionalism
Patient Care
Interpersonal and Communication Skills
Systems-Based Practice
Professionalism
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of healthcare.
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Prepare and guide junior residents presentation at weekly Head and Neck Case conference.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
Professionalism
Interpersonal and Communication Skills
Professionalism
Practice-Based Learning and Improvement
Medical Knowledge
Systems-Based Practice
Medical Knowledge
Practice-Based Learning and Improvement
48
Rotation Director: Fred Baik, MD
Stanford Health Care Scalpel Service
Goals and Objectives
PGY 1: SHC Scalpel Service
The PGY-1 will participate in otolaryngology rounds and under the direction of the chief/senior resident will be responsible for care of inpatients.
Call duties: The PGY1 resident will take call for in -house floor patients from 6:00 am until after rounds are complete and residents are released by the chief resident. On assigned weekends, they will take floor call during the day. PGY -1 residents will not take overnight call.
NOTE: All residents, including the PGY1 residents, will take the in- training exam on the first Saturday in March.
Evaluation and Feedback
The OHNS Faculty on the Scalpel Service (and selected ancillary medical personnel) will complete written evaluations at the e nd of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Faculty Member and the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interactions.
Competency-based Goals and Objectives
Goal 1: Otolaryngology ( “Scalpel”) Rotation: To be able to provide pre - and post-operative care for the otolaryngology surgical patient.
Resident Objectives:
•Know the important aspects of history and physical examination of the otolaryngology patient.
•Begin to understand the diagnosis and treatment of common otolaryngologic disorders.
• Demonstrate proficiency in medical documentation (progress notes, discharge summaries) with comprehensive physical examinations, assessments and differential diagnoses
ACGME Competency Goals
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Systems-based practice
49
• Become familiar with the ACGME resident case log system.
Patient Care
Medical Knowledge
Systems-Based Practice
• Demonstrate self-awareness and time management/organizational skills. Practice-Based Learning and Improvement
• Prepare and present at the weekly Head and Neck Case Rounds
Goal 2: Otolaryngology (“Scalpel”) Rotation: To begin to develop otolaryngology surgical skills.
Medical Knowledge
Systems-Based Practice
Resident Objectives: ACGME Competency Goals
• Resident will know the names of common surgical instruments.
• Resident will learn basic suturing and knot tying techniques.
• Resident will know how to set up the OR for routine otolaryngology cases.
• Resident will learn the basic techniques of Direct laryngoscopy, Esophagoscopy, Bronchoscopy.
• Resident will gain experience by assisting with surgical procedures.
• Resident will be introduced to flexible laryngoscopy.
Patient Care
Goal 3: Otolaryngology (“Scalpel”) Rotation: To begin to organize a plan for a research project during residency.
Resident Objectives: ACGME Competency Goals
• Meet with at least two faculty members about possible research projects during the otolaryngology research rotation in the PGY3 year .
Professionalism
Goals and Objectives PGY 2/3: SHC Scalpel Service
Rotation Contacts and Scheduling Details
Please coordinate schedules and care with Attending Surgeons from Head and Neck Surgery (Baik, Chen, Divi, Finegersh, Holsinger, Orloff, Sirjani, Sunwoo)
Rotation Specifics
1. Rounding expectations: team is to round together in the morning with the chief res ident leading. All members of the team are expected to know what is going on with each patient. On discharge, patients should have a date and time for follow -up. The
50
team should establish this prior to discharge by calling the clinic or communicating wi th the P.A. The chief resident is expected to be teaching the juniors on rounds.
2. Communication with faculty regarding patients after rounds/weekends:
3. Communication of some sort is expected each day with each attending. For some, a text message is fine; f or others, a phone call. At the start of the service, the chief should establish the best mode of communication with each attending.
4. When talking with patients, residents should avoid relaying care plans if there is uncertainty. They should tell the pati ent that they will check with the attending.
5. Communication with faculty regarding night-time contact with patients For serious issues (e.g. should a patient go back to the OR), it is ideal if calls go up the chain of command. R2s on call should call their chief resident to evaluate, who should notify the fellow, and then the attending. The R2 should NOT bypass senior residents and go directly to the attending. This is for teaching purposes.
6. Residents are expected to make entries into medical records for n ight-time patient contacts. A note should be entered into Epic for each contact with patients.
7. Residents should strike a balance between learning in the clinic and operating room. However, the chief resident should anticipate and plan in advance so that cl inics can be covered as much as possible. This may require asking residents from other services to help. There should never be a chief and the R4 gone at the same time. It may be advisable to limit vacation during the months of heavy R4 interviews.
8. A brief operative note should be entered within an hour of completion of the surgery by the resident. Dictation of operative reports: within 24 hours.
9. Preparation for OR: Discuss case with attending the day before either verbally or by email. Read about the case. Know the patient and why the operation is being performed, the labs, etc.
10. When faculty is out of town, continue to communicate with attending daily if available by cell phone. If not, then, communicate with the covering attending or instructor (des ignated by the attending prior to leaving).
11. The resident is required to attend weekly attending rounds on Fridays . At this conference, the PGY-2 will present a case assigned by the chief resident and know the tumor stage and basic management strategies.
12. The resident will also attend H&N tumor board in addition to the regularly scheduled resident education conferences.
Evaluation and Feedback
51
The OHNS Faculty on the Scalpel Service (and selected ancillary medical personnel) will complete written evaluatio ns at the end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Faculty Member an d the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur thro ugh clinical interactions.
Competency-based Goals and Objectives
Goal 1. Expand knowledge in area of head and neck oncology.
Resident Objectives:
Be able to accurately stage cancers of the head and neck.
Develop an understanding of the role of chemotherapy and radiation therapy in the treatment of head and neck cancer.
Begin to be able to formulate a treatment plan for head and neck tumors with supervision, and be able to effectively counsel patients regarding treatment options including risks associated with surgical treatment.
ACGME Competency Goals
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Patient Care
Adequately assess flap viability and recognize venous congestion or arterial insufficiency
Progress in ability to counsel patients regarding head and neck cancer risk factors.
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Develop an understanding of the role of surgery in the treatment of squamous cell carcinoma of the head and neck.
Begin to understand the appropriate surgical procedures for the treatment of head and neck cancers.
Be able to work-up and treat patients with thyroid and parathyroid diseases.
Be able to work-up and treat patients with melanoma of the head and neck.
Be able to work-up and treat patients with salivary gland tumors.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
52
Be able to recognize the histopathologic appearance of common head and neck neoplasms, including parotid and thyroid pathology.
Medical Knowledge
Goal 2. Consults in an adult tertiary care hospital. Learn about the most common consults requested from other medical and surgical services regarding otolaryngology problems in adults.
Resident Objectives:
Be the initial contact person for all consults from other SHC services and the emergency department.
ACGME Competency Goals
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Perform initial evaluation of all consult patients.
Be familiar with the SCH electronic medical record (EPIC) and be able to access information appropriately. Understand the importance of confidentiality in patient medical records.
Evaluate consult patients with senior resident or fellow and faculty member and communicate recommendations and plan to primary team. Consistently demonstrate courtesy when interacting with clinical and non -clinical staff members.
Patient Care
Medical Knowledge
Patient Care
Professionalism
Systems-Based Practice
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Perform a literature search to learn more about unusual patient problems.
Medical Knowledge
Practice-Based Learning and Improvement
Create a complete and coherent consultation note and dictate it in a timely fashion. This objective applies to all patients seen in the clinic setting as well as the outpatient setting.
Utilize translation services to communicate with non -English speaking patients as needed.
Demonstrate effective time -management skills.
Follow-up on consult patients as needed.
Interpersonal and Communication Skills
Professionalism
Interpersonal and Communication Skills
Systems-Based Practice
Practice-Based Learning and Improvement
Professionalism
Patient Care
53
Systems-Based Practice
Professionalism
Prepare and present at the weekly Head and Neck Case conference or Attending rounds. Medical Knowledge
Systems-Based Practice
Goal 3. Expand ability to perform head and neck surgical procedures
Resident Objectives: ACGME Competency Goals
Be able to competently and efficiently perform mid -level procedures with attending assistance
Patient Care such as:
• Direct laryngoscopy and biopsy
• Flexible and rigid esophagoscopy.
• Tonsillectomy
• Tracheostomy
• Panendoscopy
• Submandibular gland excision
• Excision of congenital cysts
• Resection of small carcinomas (e.g. tongue, floor of mouth)
• Resection of melanoma of the head and neck
• Sentinel lymph node biopsy
• Skin graft and flap reconstruction of head and neck defects
• Assist with neck dissections and begin to understand the anatomy and principles governing neck dissections
Goal 4. Improve general otolaryngology knowledge
Resident Objectives: ACGME Competency Goals
Develop competence in the interpretation of head and neck imaging studies through regular review of all patient imaging and attendance at radiology rounds.
Learn to set-up and use the facial nerve integrity monitor.
Demonstrate competence in the safe and appropriate use of various lasers.
Learn the nuances of correctly coding surgical procedures, consultations, and outpatient visits (CPT and ICD -9).
Patient Care
Medical Knowledge
Patient Care
Patient Care
Patient Care
Systems-Based Practice
54
Be able to appropriately document patient care to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of healthcare.
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
HALF-TIME RESEARCH RESIDENT
• Research Resident must have at least 2.5 days of research time per week on average.
Patient Care
Systems-Based Practice
Professionalism
Systems-Based Practice
Professionalism
Professionalism
Practice-Based Learning and Improvement
• During PGY2/3 or PGY4’s vacation/conference/interview period, Half -time Research Resident usually works as full time.
55
Rotation Contacts and Scheduling Details
Please coordinate schedules and care with Attending Surgeons from Head and Neck Surgery (Baik, Chen, Divi, Finegersh, HolsingerOrloff, Sirjani, Sunwoo)
Note: if there is no O.R. going on (e.g., attending physician is out of town), the resident is expected to attend clinic.
Rotation Specifics
1. Rounding expectations: team is to round together in the morning with the chief resident leading. All members of the team are expected to know what is going on with each patient. On discharge, patients should have a date and time for follow -up. The team should establish this prior to discharge by calling the clinic or communicating with the P.A. The chief resident is expected to be teaching the juniors on rounds.
2. Communication with faculty regarding patients after rounds/weekends:
3. Communication of some sort is expected each day with each attending. For some, a text message is fine; for others, a phone call. At the start of the service, the chief should establish the best mode of communication with each attending.
4. When talking with patients, residents should avoid relaying care plans if there is uncertainty. They should tell the patient that they will check with the attending.
5. Communication with faculty regarding night-time contact with patients For serious issues (e.g. should a patient go back to the OR), it is ideal if calls go up the chain of command. R2s on call should call their chief resident to evaluate, who should notify the fellow, and then the attending. The R2 should NOT bypass senior residents and go directly to the attending. This is for teaching purposes.
6. Residents are expected to make entries into medical records for night -time patient contacts. A note should be e ntered into Epic for each contact with patients.
7. Residents should strike a balance between learning in the clinic and operating room. However, the chief resident should antic ipate and plan in advance so that clinics can be covered as much as possible. This may require asking residents from other services to help . There should never be a chief and the R4 gone at the same time. It may be advisable to limit vacation during the months of heavy R4 interviews.
8. A brief operative note should be entered within a n hour of completion of the surgery by the resident. Dictation of operative reports: within 24 hours.
56
Goals and Objectives PGY 4: SHC Scalpel Service
9. Preparation for OR: Discuss case with attending the day before. Read about the case. Know the patient and why the operation is being performed, the labs, etc.
10. When faculty is out of town, continue to communicate with attending daily if available by cell phone. If not, then, communicate with the covering attending or instructor (designated by the attending prior to leaving).
11. Resident are required to atten d the Thursday H&N teaching conference (H&N team) and tumor board in addition to the regularly scheduled resident education conferences.
Evaluation and Feedback
The OHNS Faculty on the Scalpel Service (and selected ancillary medical personnel) will complete written evaluations at the end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Faculty Member an d the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interactions.
Competency-based Goals and Objectives
Goal 1. Expand knowledge in the area of head & neck surgery, as well as general concepts in surgical oncology
Resident Objectives:
Be able to identify clinically suspicious lesions of the head and neck, perform appropriate biopsies and imaging studies to make a diagnosis in a cost effective and time efficient manner.
Understand risk factors for head and neck cancer, be able to assess patients for risk factors and be able to counsel patients about managing the risk factors.
ACGME Competency Goals
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Be able to acquire appropriate information to stage head and neck cancers, to present cases in the Head and Neck Tumor Board and to determine the best treatment modality or modalities. When presenting the cases in Tumor Board, up-to-date literature will be used to support treatment decisions.
Recognize flap complications (flap failure, salivary fistula, hematoma) and initiate appropriate intervention
Be able to discuss the treatment options with the patient and make the appropriate consultations (medical oncology, radiation oncology, dentistry, speech pathology, physical
Patient Care
Professionalism
Systems-Based Practice
Patient care
Medical Knowledge
Systems-based practice
Professionalism
Practice-Based Learning and Improvement
57
therapy, nutrition, and or social work) based on the patient’s needs and wishes. This will require consideration of the patient’s rights and a sensitivity to cultural, age, gender and disability issues.
Become more familiar with ablative and reconstructive options.
Understand the role of adjuvant therapy.
Be able to work-up and treat patients with thyroid and parathyroid diseases. Become familiar with the endocrinology of these disorders and how to decide when intervention is appropriate.
Learn the fundamentals of neck ultrasound, to include optimization of machine settings and accurate identification of pathology.
Be able to work-up and treat patients with melanoma of the head and neck.
Be able to work-up and treat patients with salivary gland tumors.
Prepare and present at the weekly Head and Neck Case conference or Attending rounds.
Administer care for the post-operative oncology patient.
Goal 2. Improve competency in the performance of head and neck surgeries
Resident Objectives:
Be adept in performing the following procedures:
· Diagnostic endoscopy
· Operative microlaryngoscopy
· Tracheotomy
· Oral cavity cancer resections
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Systems-Based Practice
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Medical Knowledge
Systems-Based Practice
Patient Care
Medical Knowledge
ACGME Competency Goals
Patient Care
58
· Removal of skin cancers
· Sentinel lymph node biopsy
Become increasingly skilled in performing the following procedures:
· Neck Dissection
· Laryngectomy (total and partial)
· Laryngopharyngectomy
· Composite resection
· Regional flaps for reconstruction
· Maxillectomy
· Parotidectomy
· Thyroidectomy
· Parathyroidectomy
Know the indications, perioperative care, expected outcomes and possible complications for all procedures listed above.
Demonstrate competence in the safe and appropriate use of various lasers.
Patient Care
Patient Care
Patient Care
Goal 4. Be able to take care of patients in an ethical, efficient and caring manner within the current medical system
Resident Objectives: ACGME Competency Goals
Develop competence in the interpretation of head and neck imaging studies through regular review of all patient imaging and attendance at radiology rounds.
Learn the nuances of correctly coding surgical procedures, consultations, and outpatient visits (CPT and ICD-9).
Be able to appropriately document patient care to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
Patient Care
Systems-Based Practice
Professionalism
Patient Care
Interpersonal and Communication Skills
Systems-Based Practice
Professionalism
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of healthcare.
Professionalism
Interpersonal and Communication Skills
59
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Professionalism
Practice-Based Learning and Improvement
Prepare and guide junior residents presentation at weekly Head and Neck Case conference or Attending rounds.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the l evel of medical knowledge.
Medical Knowledge
Systems-Based Practice
Medical Knowledge
Practice-Based Learning and Improvement
60
Rotation Contacts and Scheduling Details
Please coordinate schedules and care with Attending Surgeons from Head and Neck Surgery (Baik, Chen, Divi, Finegersh, Holsinger, Orloff, Sirjani, Sunwoo)
Note: if there is no O.R. going on ( e.g., attending physician is out of town) resident is expected t o attend clinic.
Rotation Specifics
1. Rounding expectations: team is to round together in the morning with the chief resident leading. All members of the team are expected to know what is going on with each patient. On discharge, patients should have a d ate and time for follow -up. The team should establish this prior to discharge by calling the clinic or communicating with the P.A. The chief resident is expected to be teaching the juniors on rounds.
2. Communication with faculty regarding patients after rounds/weekends:
3. Communication of some sort is expected each day with each attending. For some, a text message is fine; for others, a phone call. At the start of the service, the chief should establish the best mode of communication with each attending.
4. When talking with patients, residents should avoid relaying care plans if there is uncertainty. They should tell the patient that they will check with the attending.
5. Communication with faculty regarding night-time contact with patients For serious issues (e.g. should a patient go back to the OR), it is ideal if calls go up the chain of command. R2s on call should call their chief resident to evaluate, who should notify the fellow, and then the attending. The R2 should NOT bypass senior residents and go directly to the attending. This is for teaching purposes.
6. Residents are expected to make entries into medical records for night -time patient contacts. A note should be entered into Epic for each contact with patients.
7. Residents should strike a balance between learning in the clinic and operating room. However, the chief resident should antic ipate and plan in advance so that clinics can be covered as much as possible. This may require asking residents from other services to help. There should never be a chief and the R4 gone at the same time. It may be advisable to limit vacation during the months of heavy R4 interviews.
8. A brief operative note should be entered within an hour of completion of the surgery by the resident. Dictation of operative reports: within 24 hours.
9. Preparation for OR: Discuss case with attending the day before. Read about the case. Know the patient and why the operation is being performed, the labs, etc.
61 Goals and Objectives PGY 5: SHC Scalpel Service
10. When faculty is out of town, continue to communicate with attending daily if available by cell phone. If not, then, communicate with the covering attending or instructor (designated by the attending prior to leaving).
11. The resident is required to attend the Thursday H&N teaching confe rence (H&N team) or the Friday Attending rounds. At this conference, the chief resident will assign upcoming cases to junior residents.
12. Chief resident is expected to attend the monthly faculty meeting.
Evaluation and Feedback
The OHNS Faculty on the Scalpel Service (and selected ancillary medical personnel) will complete written evaluations at the end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each faculty member an d the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interactions
Competency-based Goals and Objectives
Goal 1: Be competent in evaluating and managing head & neck otolaryngology patients.
Resident Objectives:
Expand and refine evaluation and management skills of otolaryngology patients. Such knowledge should allow the R5 resident to confidently and independently care for otolaryngology patients with conditions involving head and neck oncology by the end of the year.
Expand participation to include a leadership role in teaching conferences facilitating the learning of the junior residents and medical students.
Expand knowledge of Otolaryngology literature for diseases and disorders of the larynx and cancers of the head and neck .
ACGME Competency Goals
Medical Knowledge
Patient Care
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Be able to identify clinically suspicious lesions of the head and neck, perform appropriate biopsies and imaging studies to make to make a diagnosis in a cost effective and time efficient manner.
Be able to acquire appropriate information to stage head and neck cancers, to present cases in the Head and Neck Tumor Board and to determine the best treatment modality or modalities. When presenting the cases in Tumor Board, up to date literature will b e used
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Medical Knowledge
62
to support treatment decisions. Be able to discuss the treatment options with the patient and make the appropriate consultations (medical oncology, radiation oncology, dentistry, speech pathology, physical therapy, nutrition and/or social work) base d on the patient wishes. This will require consideration of the patient’s rights and a sensitivity to cultural, age, gender, and disability issues.
Demonstrate competency in performing comprehensive neck ultrasound to assist in diagnosis, surgical planning, and image guided procedures. Be able to recognize common pathologies (thyroid nodules/cysts, malignancy, normal and abnormal lymph nodes, parathyroid adenoma, ranula, thyroglossal duct cyst).
Develop a comprehensive understanding of the common ablative and reconstructive options.
Understand the limits of surgical and medical treatment.
Understand the role of adjuvant therapy.
Understand indications for urgent operative decisions, such as a performing a surgical airway and decompressing an expanding neck hematoma
Recognize and manage surgical risk -factors.
Administer care for the post-operative oncology patient.
Expand the capacity to recognize and treat post -surgical complications effectively, and learn to recognize preoperative risk factors.
Gain a healthy appreciation for the dangers inherent in medical intervention, and learn how to be appropriate in selecting patients for surgery.
Practice-Based Learning and Improvement
Systems-Based Practice
Interpersonal and Communication Skills
Professionalism
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Assume a leadership role in postoperative care of complications such as salivary fistula, wound infection, hematoma, cerebrospinal fluid leak, airway compromise, and
Patient Care
Practice-Based Learning and Improvement
63
hemorrhage. Teach the junior residents and medical students to manage these complications.
Be able to effectively incorporate radiologic studies in assessing patients with head and neck tumors in a cost effective and time efficient manner.
Be able to successfully transition from supervision by faculty to primary decision making with faculty oversight.
Supervise presentation of complications on the service at monthly Morbidity and Mortality conference.
Demonstrate competence and organizational skills in directing the resident team in the daily management of in-house patients and OR activities.
Demonstrate ability and commitment in the day -to-day informal teaching and mentoring of students and junior residents.
Be able to competently supervise/assist junior residents performing common OTO/HNS surgical procedures.
Be able to demonstrate excellent interpersonal skills, effectively setting the tone for other members of the resident team, clinical and non -clinical staff.
Goal 2: Be able to safely and efficiently perform advanced head & neck surgical skills.
Resident Objectives:
Refine operative skills and gain expertise in advanced surgical procedures of the head and neck, as well as laryngology. The R5 Otolaryngology residents are expected to assume a graduated responsibility in more complex operative cases. Through their rotation they should become comfortable with taking an active role in the technical procedures such as:
• Head and Neck Surgery
o Neck Dissection
o Laryngectomy (total and partial)
o Laryngopharyngectomy
o Composite resection
• Endocrine Surgery
o Thyroidectomy
o Parathyroidectomy
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Patient Care
Practice-Based Learning and Improvement
Practice-Based Learning and Improvement
Practice-Based Learning and Improvement
Practice-Based Learning and Improvement
Professionalism
ACGME Competency Goals
Patient Care
64
o Central neck dissection
• Reconstructive Surgery
o Regional flaps for reconstruction
o Maxillectomy
o Anterior skull base resection
o Parotidectomy
o Oral cavity cancer resections
o Melanoma of the head and neck
o Sentinel lymph node biopsy
Learn the nuances of correctly coding surgical procedures, consultations, and outpatient visits (CPT and ICD -9).
Be able to appropriately document patient care to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of healthcare.
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statis tical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
HALF-TIME RESEARCH RESIDENT
• Research Resident must have at least 2.5 days of research time per week on average.
Patient Care
Systems-Based Practice
Patient Care
Systems-Based Practice
Professionalism
Systems-Based Practice
Practice-Based Learning and Improvement
Practice-Based Learning and Improvement
• During PGY2/3 or PGY4’s vacation/conference/interview period, Half -time Research Resident usually works as full time.
65
Rotation Director: Iram Ahmad, MD, MME
Lucile Packard Children’s Hospital Stanford
Goals and Objectives
Welcome to the Pedi OHNS Rotation !
Faculty: Ahmad, Balakrishnan, Chang, Cheng, Meister, Sidell, Truong, Valdez
Rotation Specifics: Please refer to Peds Service Guidelines provided by the service.
Goals and Objectives PGY 1: PEDIATRIC Otolaryngology
NOTE: All residents, including the PGY1 residents, will take the in - training exam on the first Saturday in March.
Competency-based Goals and Objectives
Goal 1. Pediatric Otolaryngology Hospital service. Learn the common pediatric otolaryngology disorders which require childr en to be in the hospital, the basics of how to manage these patients, and basic surgical skills.
Resident Objectives:
Round with the pediatric otolaryngology team 2 times a day and know the common entities that require a child to be hospitalized.
ACGME Competency Goals
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Systems-Based Practice
Learn the basics of how to perform flexible laryngoscopy on a child. Learn how to operate the Machinery on the scope cart.
Be familiar with the LPCH electronic medical record (EPIC) and be able to access information appropriately. Understand the importance of confidentiality in patient medical records.
Perform a literature search to learn more about unusual patient problems.
Patient Care
Systems-Based Practice
Patient Care
Professionalism
Systems-Based Practice
Medical Knowledge
66
Create a complete and coherent consultation note and dictate it in a timely fashion. This objective applies to all patients seen in the hospital setting as well as the outpatient setting.
Utilize translation services to communicate with non -English speaking patients as needed.
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Professionalism
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Demonstrate effective time-management skills.
Begin to acquire the following surgical skills: Suturing and knot tying techniques.
Practice-Based Learning and Improvement
Patient Care Microscope set up. Cerumen removal.
Tonsillectomy and Adenoidectomy steps. Myringotomy and tube placement steps.
Goal 2. Pediatric Otolaryngology Clinics. Learn the common pediatric otolaryngology disorders seen in pediatric otolaryngol ogy clinics and how to evaluate these patients.
Resident Objectives:
Learn how to evaluate a child with sleep-disordered breathing.
Learn how to evaluate a child with recurrent ear infections.
Practice pneumatic otoscopy.
Learn how to evaluate a pediatric neck mass, particularly congenital neck masses.
ACGME Competency Goals
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Goals and Objectives PGY 2/3: PEDIATRIC Otolaryngology
Competency-based Goals and Objectives
Goal 1. Consults in a pediatric hospital. Learn about the most common consults requested from other medical and surgical se rvices regarding otolaryngology problems in children.
Resident Objectives:
ACGME Competency Goals
67
Be the initial contact person for all consults from other LPCH services and the emergency department.
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Systems-Based Practice
Perform initial evaluation of all consult patients.
Be familiar with the LPCH electronic medical record (EPIC) and be able to access information appropriately. Understand the importance of confidentiality in patient medical records.
Evaluate consult patients with senior resident or fellow and faculty member and communicate recommendations and plan to primary team. Consistently demonstrate courtesy when interacting with clinical and non -clinical staff members.
Patient Care
Medical Knowledge
Patient Care
Professionalism
Systems-Based Practice
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Professionalism
Perform a literature search to learn more about unusual patient problems.
Medical Knowledge
Practice-Based Learning and Improvement
Create a complete and coherent consultation note and dictate it in a timely fashion. This objective applies to all patients seen in the clinic setting as well as the outpatient setting.
Utilize translation services to communicate with non -English speaking patients as needed.
Interpersonal and Communication Skills
Professionalism
Interpersonal and Communication Skills
Systems-Based Practice
Professionalism
Demonstrate effective time -management skills.
Follow-up on consult patients as needed.
Attend at least one “care conference”
Practice-Based Learning and Improvement
Patient Care
Systems-Based Practice
Professionalism
Systems-Based Practice
Goal 2. Tonsillar and Adenoidal Hypertrophy. Screen, diagnose and manage patients with symptoms secondary to their tonsils and adenoids
68
Resident Objectives: ACGME Competency Goals
Be able to describe the anatomy, physiology, and pathophysiology of the tonsils/adenoids/eustachian tube.
Take a sleep history with focused questions that assist in the diagnosis of sleep apnea.
Describe the use of diagnostic tests for assessing tonsils and adenoids (e.g. airway films, sleep studies, nasal endoscopy).
Be able on physical examination to assess obstruction by tonsils, adenoids, turbinates and nasal septum.
Describe how to identify a submucous cleft palate.
Be able to counsel parents about the pathophysiology of conditions associated with tonsillar and adenoidal hypertrophy, tonsillitis and adenoiditis.
Understand the indications for tonsillectomy and/or adenoidectomy and alternative therapies.
Be able to counsel parents about the risks and benefits of tonsillectomy and/or adenoidectomy.
Know the perioperative management and expected postoperative course of patients who undergo tonsillectomy and adenoidectomy.
Be able to safely and efficiently perform an adenoidectomy using the following techniques: microdebrider, coblation, curette.
Be able to safely and efficiently perform a tonsillectomy using the following techniques: cold snare, electrocautery, microdebrider, coblation.
Be able to discuss the treatment of and provide care to patients with complications of a T&A procedure.
Goal 3. Ears. Be able to evaluate and treat ear disease in children.
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Patient Care
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Professionalism
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Patient Care
Patient Care
Interpersonal and Communication Skills
Resident Objectives: ACGME Competency Goals
Be able to describe the anatomy, physiology, and pathophysiology of the ear and eustachian tube.
Be able to take a history related to the ears and hearing.
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
69
Know how to perform microscopic otoscopy and pneumatic otoscopy.
Understand the available treatments for acute otitis media and chronic serous otitis media.
Be able to discuss the indications, risks, benefits , and alternatives to tympanostomy tube placement.
Be able to counsel parents about the risks and benefits of tympanostomy tube placement.
Be able to safely and efficiently place tympanostomy tubes.
Be able to discuss and treat complications from tympanostomy tube placement.
Counsel patients and families about preventing noise exposure and hearing loss in the well child/adolescent setting (e.g. avoiding music and sounds that lead to high frequency hearing loss, wearing ear protectors for noisy tasks.)
Goal 4. Airway. Be able to evaluate children with breathing problems.
Resident Objectives:
Be able to obtain an appropriate airway history.
Be able to recognize, describe and categorize stridor in children.
Know the most common causes of stridor in children.
Be able to perform and interpret flexible laryngoscopy in a child.
Know the most common cause of stridor and weak voice in a child who has undergone cardiac surgery, and the procedures associated.
Be able to assemble the equipment needed to perform a laryngoscopy, bronchoscopy and esophagoscopy.
Begin to know how to perform a direct laryngoscopy and bronchoscopy in a child.
Discuss routine care of a tracheostomy and describe how to recognize tracheostomy obstruction or decannulation.
Understand and be able to describe to parents the risks of a tracheotomy in a child.
Patient Care
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Patient Care
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
ACGME Competency Goals
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Patient Care
Patient Care
Patient Care
Patient Care
70
Medical Knowledge
Interpersonal and Communication Skills
Goal 5. Nose. Diagnose and manage pediatric patients with nasal problems.
Resident Objectives: ACGME Competency Goals
Know the anatomy, physiology, and pathophysiology of the nose in children.
Be able to obtain a history related to the nose and nasal problems.
Understand the signs, symptoms and differences between chronic adenoiditis and sinusitis in children.
Understand the etiology, presentation, diagnosis and therapy of sinusitis in children with cystic fibrosis.
Understand and be able to recommend and interpret ancillary tests (e.g. plain films, CT scans) to evaluate nasal problems in children.
Be able to evaluate a neonate with nasal obstruction, and understand the possible causes of neonatal nasal obstruction.
Be able to describe and recognize complications of acute sinusitis in children.
Identify the signs and symptoms of allergic rhinitis.
Be able to describe and compare pharmacologic options for treatment of acute and chronic adenoiditis, and sinusitis, and allergic and nonallergic rhinitis.
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Goal 6. Pediatric Audiology. Understand the methods available to test the hearing in children, and how to interpret the tests.
Resident Objectives: ACGME Competency Goals
Be familiar with the principal methods for screening the hearing of a newborn (automated auditory brainstem response, Otoacoustic emissions).
Know the age-appropriate way to behaviorally test the hearing of infants and children.
Be able to interpret routine tympanograms and audiograms.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
71
Describe general principles about interventions for hearing -impaired children (speech training, sign language, amplification devices, communication boards, cochlear implants).
Goal 7. Neck. Be able to diagnose and treat common problems which occur in the neck in children.
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Be able to describe the natural history, clinical presentation, evaluation and treatment options of neck abscesses (retropharyngeal, peritonsillar, parapharyngeal & lymph node) in children.
Know the symptoms, signs, and physical examination findings of a thyroglossal duct cyst and branchial cleft cyst.
Understand the differential diagnosis of Vascular anomalies in the head and neck in children, just as infantile hemangiomas, lymphatic malformations, and venous malformations.
Goal 8. General Pediatric Otolaryngology
Resident Objectives:
Be able to obtain an appropriate history regarding possible foreign body ingestion.
Be able to describe and recognize the signs of symptoms of ear, nose, larynx, esophageal and bronchial foreign bodies.
Be able to describe the risks and benefits of foreign body removal from the head and neck.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
ACGME Competency Goals
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Be able to describe the signs and symptoms of ankyloglossia and the indication for frenotomy.
Be able to counsel patients about the indications, risks, benefits and alternatives to frenotomy.
Be able to safely and efficiently perform a frenotomy.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
72
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of healthcare.
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Continue to participate in the quality improvement process and to follow -up postoperative patients whenever possible.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
Develop an understanding of OHNS coding and compliance issues in pediatric otolaryngology.
Professionalism
Systems-Based Practice
Professionalism
Professionalism
Practice-Based Learning and Improvement
Systems-Based Practice
Professionalism
Practice-Based Learning and Improvement
Professionalism
Systems-Based Practice
Goals and Objectives PGY 4: PEDIATRIC Otolaryngology
Competency-based Goals and Objectives
Goal 1. Be able to provide a thorough evaluation and create a treatment plan for consult and otolaryngology patients in a pe diatric hospital.
Resident Objectives: ACGME Competency Goals
Will provide back -up to the R2 resident for all inpatient and emergency room consults. If R2 resident is not available will be initial contact person for all consults. R4 to work with the R2 in seeing the consults and providing guidance re a treatment plan. In conjunction with the R2 the R4 will communicate with the fellow and attending physician re the consult.
Will lead twice-daily rounds on all inpatients on the otolaryngology service and at least once-daily rounds on all consult patients. Will work together with pediatric OHNS fellow and attending faculty to provide optimum care.
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Patient Care
73
Will work to educate the R2 resident and medical st udents re patient problems. (For example, discussing the details of care with them on morning rounds and encouraging them to read about pertinent patient issues.)
Will aid the R2 in performing a literature search to learn more about unusual patient problems.
Attend at least one “care conference”
Interpersonal and Communication Skills
Systems-Based Practice
Medical Knowledge
Medical Knowledge
Practice-Based Learning and Improvement
Systems-Based Practice
Goal 2. Be able to evaluate pediatric patients in the clinic with a wide range of problems.
Resident Objectives:
Be able to take a history from more complicated pediatric patients such as those with multiple congenital anomalies and more complex otolaryngology problems such as those with airway obstruction, tracheostomy dependent, veloopharyngeal insufficiency, sensorineural hearing loss.
Know the features of common sequences and syndromes seen in pediatric otolaryngology patients such as: Down syndrome, velocardiofacial syndrome, oculoauriculovertebral syndrome, Treacher-Collins syndrome, Crouzon syndrome, Pierre Robin sequence, Usher’s syndrome, Pendred syndrome.
Know the common genetic abnormalities found in children with sensorineural hearing loss. Know how to order these tests and interpret them.
Be adept in performing nasal endoscopy and flexible laryngoscopy in neonates.
Be able to initiate an evaluation of a child with hypernasality. Understand the importance of coordinating care with a speech pathologist knowledgeable about velopharyngeal insufficiency.
Know the surgical and non-surgical options for treatment of velopharyngeal insufficiency. Be able to assist with VPI procedures and to understand the perioperative course.
Know the options for treatment of different vascular anomalies, including surgical and medical management options.
ACGME Competency Goals
Medical Knowledge
Medical Knowledge
Medical Knowledge
Patient Care
Systems-Based Practice
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
74
Goal 3. Ears. Be able to evaluate and treat ear disease in children.
Resident Objectives: ACGME Competency Goals
Know the common presenting symptoms and findings in pediatric patients with a tympanic membrane perforation, severe atelectasis, cholesteatoma, microtia and sensorineural hearing loss.
Be able to formulate appropriate treatment plans for all patients with the above clinical conditions.
Know the indications for aural habilitation (and rehabilitation) in children with hearing loss. Understand the types of hearing aids available and the difficulties in treating children with these devices.
Understand the indications for bone-anchored hearing aids and cochlear implants in children.
Be able to counsel families of children with ear disease regarding appropriate surgical and non-surgical management of their child’s condition.
Be able to perform an underlay tympanoplasty, and simple Mastoidectomy. Be able to assist with canal atresia reconstruction. Understand the expected perioperative course and potential complications of these procedures.
Understand the treatment options and treatment timeline for microtia and canal atresia. Be able to assist in rib cartilage harvest and auricular reconstruction.
Goal 4. Be able to evaluate and treat children with breathing problems.
Medical Knowledge
Patient Care
Patient Care
Interpersonal and Communication Skills
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Know the common causes and treatments for children who present with a complaint of chronic throat clearing and/or cough. Be able to counsel families regarding these treatments.
Be able to formulate a treatment recommendation for children with airway obstruction including children with laryngomalacia, subglottic stenosis, tracheal stenosis, laryngeal cleft, subglottic hemangioma, subglottic cysts.
Know the indications, risks and benefits for the following procedures including; microdirect laryngoscopy with excision of lesion, supraglottoplasty, laryngotracheal reconstruction, slide tracheoplasty. Be able to counsel patients regarding these procedures.
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
75
Be able to discuss the post-operative care for the patient who has undergone a Laryngotracheal reconstruction.
Know the most common causes of acute onset of stridor and how to treat them (eg croup, supraglottitis, foreign body aspiration, deep neck abscess.)
Know the etiology of perioperative laryngospasm in children and how to treat it.
Know the etiology, typical patient, and treatment options for vocal fold dysfunction syndrome (paradoxical vocal fold motion).
Goal 5. Diagnose and manage pediatric patients with nasal problems.
Patient Care
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Know the presenting symptoms of a child with choanal atresia, nasal dermoid, nasal glioma, nasal encephalocele.
Know the different options for repair of choanal atresia and understand the indications, timing, risks and benefits of repair.
Understand the causes of chronic sinusitis in children and the indications for endoscopic sinus surgery. Be able to discuss with families the expected perioperative treatment course. Be able to perform endoscopic sunus surgery under direct supervision.
Be able to set up and utilize the surgical navigation system in the operating room.
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care Systems-Based Practice
Goal 6. Neck. Be able to diagnose and treat common problems which occur in the neck in children.
Resident Objectives: ACGME Competency Goals
Be able to describe the natural history, clinical presentation, evaluation and treatment options of different types of vascular malformations.
Know the presentation, work-up, and treatment for congenital torticollis (fibromatosis colli) in young children.
Be able to formulate a differential diagnosis for any type of neck mass in a child.
Goal 7. General Pediatric Otolaryngology
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Patient Care
76
Be able to perform a microdirect laryngoscopy, and bronchoscopy in a neonate. Be able to perform a routine bronchoscopy with foreign body removal, and esophagoscopy with foreign body removal.
Continue to develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor -patient relationship and the delivery of healthcare.
Continue to develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Continue to participate in the quality improvement process and to follow -up postoperative patients whenever possible.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
Continue to develop an understanding of OHNS coding and compliance issues in pediatric otolaryngology.
HALF-TIME RESEARCH RESIDENT
• Research Resident must have at least 2.5 days of research time per week on average.
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Professionalism
Practice-Based Learning and Improvement
Professionalism
Professionalism
Practice-Based Learning and Improvement
Professionalism
Systems-Based Practice
• During PGY2 or PGY4’s vacation/conference/interview period, Half -time Research Resident usually works as full time.
77
Veteran’s Administration Palo Alto
Rotation Contacts and Scheduling Details
Rotation Director: Davud Sirjani, MD
Attendings who need Resident clinic coverage: Chen, Finegersh, Nayak, Sajjadi, Sirjani, Sung
Private Attendings- residents do not cover: Makarewycz
Fellows- do not need Resident clinic coverage: Facial-Plastics – Monica Rossi Meyer
Important Contacts: Main # 650-493-5000 (dial 1→1→ ext#)
Location: PAD, Bldg 100, 2nd Floor ENT Clinic. Mailstop code 112ENT
ENT fax number: ( 650) 496-2502. If you need to send a fax, you can
• Use the Xerox machine (will need to use your PIV card)
• OR send from your computer if you already have an ecopy. If you do not have an ecopy, you can scan a copy using the Xerox machine. The link to efax is
• https://oitpalappfax01.va.gov/RightFax/User /
78
Additional Required Conferences Clinic rules
▪ Wednesday (every other week) at the Radiology Conference Room (Building 102) from 8:30 -9:30 am
▪ Clinic starts promptly at 9 am and 1pm
▪ Please complete inpatient rounds and workload prior to start of clinic
▪ All documentation must be done accurately and in a timely fashion (within 24 hours)
▪ Please see PAVAPGY3andPGY5.pdf for details on specific rotation goals and objectives
79
Weekly Schedule
A- NON-OPERATIVE WEEK (starting 6/26/23)
R: Research Resident **1 resident to scrub out PRN
Chen Clinic: PGY 3,5,NP Mak
Sirjani Clinic: PGY 3,5,NP Mak
Tumor Board- NP (8:30-9:00am)
Nayak Clinic: PGY 3,5,R,PA Mak
**OR- Sajjadi: PGY 3 or 5
Time Monday Tuesday Wednesday Thursday, OR 7:45am Friday, OR 7:45am AM 08001200
Sung Minor: PGY 3 or 5, PA
Finegersh Clinic Mak
OR- Sirjani/Chen: PGY 3, 5
FPF clinic
Annie clinic (RNP)
Sirjani Clinic: PGY 3, 5, NP
Nayak Clinic: PGY 3,5,R,PA
Team3- pre/postops
OR- Sung: PGY 3 or 5
Team5- as needed PM 12001700 Team1- FPF postops Mak
Sajjadi Clinic: PGY 3or5, PA, R
Team4- pre/postops Mak
B- OPERATIVE WEEK (starting 7/3/23)
R: Research Resident **1 resident to scrub out PR N
OR- Sirjani/Chen: PGY 3, 5 FPF clinic
OR- FPF: PGY 3or5
Chen clinic: PGY 3or5, NP
Sirjani Clinic: PGY 3,5,NP Mak
Tumor Board – NP (8:30—9:00am)
**OR- Sajjadi: PGY 3 or 5
Time Monday , OR 8:45am Tuesday Wednesday , OR 7:45am Thursday , OR 7:45am Friday , OR 7:45am AM 08001200
OR- Chen/Sirjani: PGY 3, 5
Sung Clinic: PA, R Mak
**OR- FPF: PGY 3or5
Sung Clinic: PA, R Mak
Sirjani Clinic: PGY 3,5,NP
**OR- Nayak: PGY 3, 5
Resident clinic: R Mak
**OR- Nayak: PGY 3, 5
Resident clinic: R
Sung Minor: PGY 3 or 5, PA
Finegersh clinic Mak
OR- Sung: PGY 3 or 5
Team5- as needed PM 12001700
Sajjadi Clinic:PGY3or5, PA, R
Team4- pre/postops Mak
OR- Chen/Sirjani: PGY 3, 5
80
Additional Notes:
• Monday OPERATIVE WEEK : check-in patient at 8AM, case starts at 8:45AM
• All other OPERATIVE WEEK : check-in patient in at 7AM, case starts at 7:45AM
• ALL PATIENTS: Surgical site MUST be marked, even bilateral or midline cases need a wrist band stating the procedure to be done.
RESEARCH RESIDENT (R: RESEARCH RESIDENT)
• If clinic needs extra-help from Research Resident please give those dates in advance.
• Research Resident must have at least 2.5 days of research time per week on average.
• During PGY3 or PGY5’s vacation/conference/interview period, Research resident usually works as full time.
• Check to see if help is needed for Monday procedures in M. Chen clinic the week before.
Non-Operative Week Wednesdays: COCLIA
• COCLIA is the Comprehensive Otolaryngologic Curriculum Learning through Interactive Approach provided by the American Academy of Otolaryngology – Head & Neck Surgery Foundation. It can be found at: https://www.coclia.org.
• The VA residents and all residents on full-time or ½-time research will participate in the bi -weekly COCLIA session.
• The VA PGY5 will pick a topic from the curriculum and assign questions for each resident cover.
• Each resident will provide a handout summarizing the answers to their assigned questions.
• Research residents may participate via Zoom if they are not scheduled to be at the VA that day.
Rotation Specifics
See APPENDIX Q (VAPAHCS ENT Resident Handbook) for comprehensive details.
Evaluation and Feedback
The VAPAHCS faculty and selected ancillary medical personnel will complete written evaluations at the end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Faculty Member and the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interactions.
81
Goals and Objectives PGY 3: VAPA
Competency-based Goals and Objectives
Goal 1. Expand knowledge in area of head and neck oncology.
Resident Objectives:
Be able to accurately stage cancers of the head and neck.
Develop an understanding of the role of chemotherapy and radiation therapy in the treatment of head and neck cancer.
Begin to be able to formulate a treatment plan for head and neck tumors with supervision, and be able to effectively counsel patients regarding treatment options including risks associated with surgical treatment.
Progress in ability to counsel patients regarding head and neck cancer risk factors.
ACGME Competency Goals
Medical Knowledge
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Be able to work-up and treat patients with thyroid and parathyroid diseases.
Be able to work-up and treat patients with salivary gland tumors.
Be able to recognize the histopathologic appearance of common head and neck neoplasms, including parotid and thyroid pathology.
Goal 2. Expand knowledge of common otologic complaints.
Resident Objectives:
Be able to outline the assessment, work -up, and management of sudden sensorineural hearing loss.
Progress in the ability to systematically evaluate the dizzy patient.
Be able to formulate operative and non-operative treatment plans for patients with chronic otitis media.
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
ACGME Competency Goals
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
82
Demonstrate facility with counseling patients regarding the expected risks and benefits associated with surgery for chronic ear disease.
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Be able to describe the pathophysiology of cholesteatoma.
Develop the ability to recommend ‘for’ or ‘against’ hearing amplification based on audiometric considerations, and be able to effectively advise patients regarding appropriate amplification options.
Goal 3. Expand knowledge of common rhinologic disorders.
Resident Objectives:
Progress in the ability to evaluate and treat patients with epistaxis, including nonoperative and operative management as well as counseling patients regarding risk reduction.
Be able to successfully evaluate patients with chronic sinusitis, and be able to counsel patients regarding medical and surgical treatment options.
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
ACGME Competency Goals
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Demonstrate increasing facility and diagnostic skill with rigid nasal endoscopy.
Progress in the ability to successfully interpret sinus imaging studies.
Be able to competently counsel patients regarding the risks associated with sinonasal surgery.
Patient Care
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Goal 4.
Expand knowledge of voice and swallowing disorders
Resident Objectives:
Be able to describe the anatomy, physiology, and pathophysiology of the larynx.
ACGME Competency Goals
Medical Knowledge
83
Take a history with focused questions that assist in the diagnosis of hoarseness and dysphagia.
Be able to subjectively assess and describe hoarseness (i.e. GRBAS scale)
Describe the use of diagnostic tests for assessing hoarseness (e.g. CT scans, laryngeal endoscopy, stroboscopy).
Be able on physical examination to assess dysfunction of vocal folds (i.e. paralysis).
Be able to counsel parents about the pathophysiology of conditions associated with vocal fold paralysis.
Understand the indications for vocal fold medialization (e.g. injection, thyroplasty, arytenoid repositioning) and alternative therapies.
Be able to counsel parents about the risks and benefits of vocal fold medialization.
Be able to safely and efficiently perform a flexible fiberoptic nasolaryngoscopy and stroboscopy.
Be familiar with the principal lesions that can affect vocal fold function in adults (i.e. papilloma, polyp, nodule, cyst, cancer).
Be able to identify the various methods for laryngeal framework surgery (e.g. thyroplasty, arytenoid adduction); their indications and their possible complications.
Know the instrumentation used to resect laryngeal lesions (i.e. endoscopic scissors, graspers, lasers).
Patient Care
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Professionalism
Interpersonal and Communication Skills
Patient Care
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care Goal 5. Increase knowledge of sleep medicine.
Understand the available radiographic and endoscopic methods of assessing swallowing.
Resident Objectives:
Increase competence in the assessment of patients with suspected sleep apnea.
Progress in the ability to interpret polysomnographic data in adults.
ACGME Competency Goals
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
84
Be able to effectively counsel patients regarding the consequences of untreated sleep apnea, and regarding appropriate treatment options.
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Goal 6. Increase knowledge in the area of facial trauma and reconstruction.
Resident Objectives: ACGME Competency Goals
Be able to perform a thorough physical examination in the facial trauma and reconstruction patient with a command of positive signs to be sought and their significance.
Be able to effectively counsel facial trauma and reconstruction patients regarding treatment options, potential complications, and expected post -operative course.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Goal 7. Expand knowledge of head and neck infectious disorders.
Resident Objectives: ACGME Competency Goals
Be able to successfully evaluate and recognize cases of deep neck infection, and be able to outline an appropriate treatment plan.
Be able to describe the pathophysiology of necrotizing fasciitis, and the treatment of this disorder.
Demonstrate an understanding of the clinical presentation of mycobacterial infection in the head and neck, including organisms involved and appropriate management.
Be able to describe the stages of orbital infection in complicated sinusitis, and outline appropriate treatment options.
Goal 8. Expand ability to perform surgical procedures
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Be able to competently and efficiently perform mid -level procedures with attending assistance such as:
o Laryngology
Microlaryngeal excision of papillomas, polyps, leukoplakia
Injection laryngoplasty
Patient Care
85
o Otology/Neurotology
Tympanoplasty
Straightforward simple mastoidectomy
o Head and Neck
Submandibular gland excision
Excision of congenital cysts
Resection of small carcinomas (e.g. tongue, floor of mouth)
Uvulopalatopharyngoplasty
o Rhinology
Septoplasty
Turbinate reduction
Selected endoscopic sinus surgery (concha bullosa, polypectomy, partial ethmoidectomy, maxillary antrostomy)
o Facial Plastic and Reconstructive Surgery
Closed nasal reduction
Open nasal reduction (straightforward)
Closure of complex facial lacerations
Local flaps
Goal 9. General knowledge
Resident Objectives: ACGME Competency Goals
Develop competence in the interpretation of head and neck imaging studies through regular review of all patient imaging and attendance at radiology rounds
Gain an understanding of the set-up and use of the image-guidance system.
Learn to set-up and use the facial nerve integrity monitor.
Demonstrate competence in the safe and appropriate use of various lasers.
Learn the nuances of correctly coding surgical procedures, consultations, and outpatient visits (CPT and ICD -9).
Be able to appropriately document patient care to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
Patient Care
Medical Knowledge
Patient Care
Patient Care
Patient Care
Patient Care
Systems-Based Practice
Patient Care
Systems-Based Practice
86
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of healthcare.
Professionalism
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
Systems-Based Practice
Professionalism
Professionalism
Practice-Based Learning and Improvement
87
Objectives
Competency-based Goals and Objectives
Goal 1. Know how to care for the otolaryngology patient.
Resident Objectives:
The R4/5 will be able to efficiently execute the evaluation of most patients without major changes being suggested by supervising faculty.
Demonstrate a command of relevant literature and be able to apply it in the development of an evaluation and (surgical and/or non-surgical) treatment plan for the full spectrum of OTO/HNS problems such as:
o Head and neck malignancy
o Complicated sinonasal disease
o Complex facial reconstruction
o Complex oto-neurotologic complaints
o Advanced voice and swallowing disorders
o Obstructive sleep apnea
ACGME Competency Goals
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
88
Goals and
PGY 5: VAPA
Demonstrate confidence and competence in the management of OTO/HNS emergencies.
Patient Care
Medical Knowledge
Exhibit leadership and clear thinking while efficiently mobilizing appropriate resources to care for such problems as airway emergencies, hemorrhage, and OTO/HNS trauma.
Demonstrate the ability to think ahead and contingency plan to avoid errors caused by lack of equipment, lack of staff, or lack of appropriate attending or specialty back -up.
Demonstrate proficiency in the recognition and management of surgical risk factors.
Patient Care
Medical Knowledge
Systems-Based Practice
Systems-Based Practice
Patient Care
Medical Knowledge
Demonstrate proficiency in the recognition, management, and avoidance of surgical complications.
Be able to successfully transition from supervision by faculty to primary decision making with faculty oversight.
Supervise presentation of complications on the service at monthly Quality Assurance conference.
Demonstrate competence and organizational skills in directing the resident team in the daily management of in-house patients and OR activities.
Demonstrate ability and commitment in the day-to-day informal teaching and mentoring of students and junior residents.
Be able to competently supervise/assist junior residents performing common OTO/HNS surgical procedures.
Be able to demonstrate excellent interpersonal skills, effectively setting the tone for other members of the resident team, clinical and non -clinical staff.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
89
Goal 2. Be able to perform standard otolaryngology procedures.
Resident Objectives: ACGME Competency Goals
Be able to competently and efficiently perform advanced otolaryngology procedures such as: Patient Care
o Otology/Neurotology
Tympanomastoidectomy
Ossicular chain reconstruction
Stapedotomy
o Head and Neck
Maxillectomy
Partial laryngeal surgery
Composite resection
Total parotidectomy with nerve grafting
Surgical management of aggressive thyroid malignancy
o Rhinology
Revision endoscopic sinus surgery
Orbital decompression
Repair of CSF leaks
o Laryngology
Microlaryngeal excision of cancer with laser and cysts with microflap technique
Endoscopic and open cricopharyngeaus and Zenker’s diverticulum surgery
Thyroplasty and arytenoid repositioning surgery
In office injection larygoplasty, laser surgery, and trans -nasal esophagoscopy
o General
Advanced techniques in obstructive sleep apnea surgery
o Facial Plastic and Reconstructive Surgery
Complex facial trauma, such as Le Fort fractures, naso-orbital-ethmoid fractures, and comminuted mandible and midface fractures
90
Functional rhinoplasty
Repair of post-traumatic and post-ablative defects
Skin resurfacing for malignancy prophylaxis
Goal 3. Have a comprehensive otolaryngology knowledge base.
Resident Objectives: ACGME Competency Goals
Develop competence in the interpretation of head and neck imaging studies through regular review of all patient imaging and attendance at radiology rounds.
Learn the nuances of correctly coding surgical procedures, consultations, and outpatient visits (CPT and ICD -9).
Be able to appropriately document patient care to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of healthcare.
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise cl inical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
Patient Care
Medical Knowledge
Patient Care
Systems-Based Practice
Patient Care
Systems-Based Practice
Professionalism
Systems-Based Practice
Professionalism
Professionalism
Practice-Based Learning and Improvement
91
Stanford Health Care: Specialties Team (Scope)
Rotation Contacts and Scheduling Details
Rotation Directors: Otology/Neurology
Nikolas Blevins, MD
Rhinology
Peter Hwang, MD
Facial Plastics
Sam Most, MD
Attendings: Alyono, Blevins, Chang, Hwang, Jackler, Most, Nayak, Patel, Pepper, Santa Maria, Stankovic, Steenerson
Weekly Schedule (effective Nov. 2023)
Monday Tuesday Wednesday Thursday Friday
Blevins OR Most OR
Hwang clinic
Hwang OR Stankovic OR Most clinic
Jackler clinic
Most MRP
Jackler OR
Blevins OR Hwang OR
Santa Maria OR
Alyono OR Chang OR/clinic
AM
Pepper OR (1st/3rd Mondays)
Alyono clinic
Steenerson clinic
Nayak OR
Capasso clinic (RWC)
Alyono clinic
Patel clinic
Santa Maria clinic
Patel OR Blevins clinic
Hwang clinic
Pepper clinic
Alyono clinic
Nayak clinic
Patel clinic
Stankovic clinic
Steenerson clinic
Most OR Patel OR (2nd Friday only)
Pepper OR Allergy clinic
Blevins clinic
Blevins OR Most OR
Hwang clinic
Pepper OR (1st/3rd Mondays)
Alyono clinic
Steenerson clinic
NOTE: Every resident is expected to attend:
Steenerson clinic
Hwang OR Stankovic OR Jackler clinic
Capasso clinic (RWC)
Most clinic
Alyono clinic
Patel clinic
Santa Maria clinic
Steenerson clinic
Most MRP
Jackler OR
Patel OR Blevins clinic
Hwang clinic
Pepper clinic
Alyono clinic
FP fellow clinic
Blevins OR Hwang OR
Santa Maria OR
Nayak clinic
Patel clinic
Most clinic
Stankovic clinic
Steenerson clinic
o Each skull base/rhinology conference while on their rhinology rotation (5:30-7:00 PM Tuesdays)
Alyono OR Chang OR/clinic
Steenerson clinic PM
Most OR Patel OR (2nd Friday only)
Pepper OR Blevins clinic Steenerson clinic Rhinology fellow clinic Jane Wang clinic
92
o 1 Cochlear Implant conference each rotation (7:30-8:30 am the 2nd and 4th Wednesdays of the month).
o 1 Stanford Balance Center conference each rotation (7am – 8 am), typically the 3rd Tuesday of the month.
Rotation Specifics
1. The team is expected to round together on all patients. “Splitting” the team to cover rounds on different patients is not acceptable. Rounds should occur two times daily.
2. During the week a resident should have a conversation with each attending re his/her patients. On the weekend some kind of formal notification (phone, text, etc) is expected daily.
3. All phone calls/patient contacts should be entered into EPIC. Contact attending directly if needed.
4. The R2 resident is the initial contact person for all consults. All consults should be seen by an attending - presented the same day and signed off by the next day. Discuss the consult list on rounds daily.
5. There should be a culture of teaching at all levels.
6. Chiefs can assign appropriate coverage of OR’s. When OR is complete residents should go to clinic. “Key indicator cases” should take precedence. Residents should see post -op cases in the clinic whenever possible.
7. Residents need to go to scheduled educational sessions and should break out of cases as needed. On time attendance is expected except for emergencies.
8. Residents are expected to read about cases in advance and check on important clinical info (CT, MRI, Audio, Path etc).
9. When faculty are out of town resi dents should extend coverage to other clinics/OR’s which are usually uncovered. Chiefs can make assignment for otherwise unassigned time.
10. Rhinology-Specific
a. For no leak/no drain patients (who usually leave the hospital POD2-3 anyway)- we think rounding for two days post-op and then chart checking is ok. Although rare, post-operative leaks that were not detected intra-operatively do occur.
b. For leak and flap/no drain patients – we would like you to round as a team for two days post-operatively, and then continue to have a senior resident see the patient daily until discharge.
c. For leak and flap/+drain patients – we would like you to round as a team for two days post-operatively, and then continue to have a senior resident see the patient through the day after the drain is removed, then chart checking is ok.
d. Please alert us when the transition to chart checking occurs on each of our patients.
93
e. For patients who remain in house over the weekend, they should be seen by the resident team for at least one of those two weekend days.
Evaluation and Feedback
The faculty, and selected ancillary medical personnel will complete written evaluations at the end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Faculty Member and the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interactions.
Goals and Objectives PGY 1: SHC Specialty Service
Competency-based Goals and Objectives
Goal 1. OHNS specialty service inpatients. Learn about the most common surgeries and disorders requiring admission to the ho spital.
Resident Objectives:
Round with the inpatient team 2x daily. Learn the most common surgeries and OHNS disorders requiring admission to the hospital. Understand the expected hospital course and requirements for discharge.
ACGME Competency Goals
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Become familiar with the Stanford EMR (EPIC) and how to input orders.
Patient Care
Medical Knowledge
Systems-Based Practice
Begin to develop surgical skills in the following areas:
Facial Plastics service: suturing/soft tissue handling, squire knot-tying, patient positioning, identify of common surgical instruments and handling techniques.
Sinus/rhinology: Inferior turbinate reduction, zero-degree rigid nasal endoscopy, polypectomy, allergy clinic (shot skills and interpretations - at least 6 visits)
Otology: in-clinic binocular microscopy, cerumen removal, mastoid bowl cleaning, basic audiologic testing and interpretations. Perform a literature search to learn more about unusual patient problems.
Patient Care
Medical Knowledge
Medical Knowledge
94
Create a complete and coherent consultation note and dictate it in a timely fashion. This objective applies to all patients seen in the clinic setting as well as the outpatient setting.
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Professionalism
Utilize translation services to communicate with non -English speaking patients as needed. Interpersonal and Communication Skills
Systems-Based Practice
Demonstrate effective time -management skills.
Practice-Based Learning and Improvement
Goals and Objectives PGY 2/3: SHC Specialty Service
Competency-based Goals and Objectives
Goal 1. Consults in an adult hospital. Learn about the most common consults requested from other medical and surgical servic es regarding otolaryngology problems.
Resident Objectives:
Be the initial contact person for all consults from other SHC services and the emergency department.
ACGME Competency Goals
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Perform initial evaluation of all consult patients.
Evaluate consult patients with senior resident or fellow and faculty member and communicate recommendations and plan to primary team. Consistently demonstrate courtesy when interacting with clinical and non -clinical staff members.
Perform a literature search to learn more about unusual patient problems.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Medical Knowledge
Practice-Based Learning and Improvement
95
Create a complete and coherent consultation note and dictate it in a timely fashion. This objective applies to all patients seen in the clinic setting as well as the outpatient setting.
Utilize translation services to communicate with non-English speaking patients as needed.
Demonstrate effective time -management skills.
Follow-up on consult patients as needed.
Interpersonal and Communication Skills
Professionalism
Interpersonal and Communication Skills
Systems-Based Practice
Practice-Based Learning and Improvement
Patient Care
Systems-Based Practice
Professionalism
Goal 2. Nasal cavity and sinuses. Diagnose and manage patients with nasal problems.
Resident Objectives: ACGME Competency Goals
Be familiar with the EMR at Stanford (EPIC) to confidentially access appropriate patient information, past culture results, pathology reports and past imaging studies.
Evaluate consult patients with sinonasal disorders with the senior residents and faculty. Be able to document and communicate recommendations and plan with the primary team in a professional and courteous manner.
Know the anatomy, pathophysiology, and development of the nasal cavity and sinuses.
Perform literature searches to investigate common and rare patient presentations, and to obtain evidence for current practice paradigms in patient care.
Understand principles and utility of CT versus MRI imaging of the sinuses. Understand and describe anatomic variations of the 4 pairs of paranasal sinuses, patterns of uncinate process attachment and sinus drainage patterns.
Be able to obtain a detailed history related to the nose and nasal problems related to sinus disease and allergic rhinitis.
Perform safe, informative routine office nasal endoscopy with 0 degree and 30 degree rigid endoscopes.
Patient Care
Professionalism
Systems-Based Practice
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Medical Knowledge
Medical Knowledge
Practice-Based Learning and Improvement
Professionalism
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
96
Access and understand AAO descriptive guidelines for acute, subacute and chronic sinusitis, and know the major and minor symptoms associated with diagnosis of sinusitis.
Evaluate patients with chronic sinusitis with and without polyposis – and distinguish which patients may require surgery or medical therapy.
Be able to describe and recognize complications of acute sinusitis.
Identify the signs and symptoms and differences between allergic rhinitis and acute/chronic sinusitis.
Understand indications for safe intranasal office biopsy.
Be proficient with the evaluation and management algorithms for treating epistaxis.
Understand options for treatment of nasal septal deviation and turbinate hypertrophy.
Learn the assembly of equipment needed to perform nasal endoscopy, and intraoperative image guidance.
Complete basic aspects of endoscopic approaches to the nasal cavity – including use of zero-degree and 30 degree endoscopes, safely navigating the nasal cavity with mucosal preserving technique, performing septoplasty, turbinate reduction, maxillary antrostomy, and anterior ethmoidectomy.
Systems-Based Practice
Patient Care
Medical Knowledge
Professionalism
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Goal 3. Allergy – Contact Dr. Meng Chen (mengchen@stanford.edu) at least one month prior to your visit.
Resident Objectives:
Proper history/evaluation and assessment of the allergy patient
Knowledge of therapies for the general allergy patient, including medication classes, dosages, side effects, and combination therapies
Proper administration of a skin-prick test x 1
ACGME Competency Goals
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
97
Proper interpretation of a skin prick test, and historic end point titration test interpretation
Proper design of an immunotherapy strategy based on prick testing (Each resident will receive instruction in immunotherapy design from the allergy team).
Understanding the goals, principles and practice of ASA desensitization therapy, and how
AERD/ASA intolerance differs from classic allergic reactions.
Advantages/disadvantages/principles of intradermal vs. sublingual immunotherapy
Goal 4. Understand the basics of the aesthetic patient consultation
Medical Knowledge
Medical Knowledge
Patient Care
Medical Knowledge
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Perform initial contact with outpatient facial plastics patient consultation.
Understand pathophysiology of aging process.
Goal 5. Understand the approach to the rhinoplasty patient
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Perform initial contact with outpatient consultation for nasal obstruction and/or aesthetic rhinoplasty.
Understand pathophysiology of nasal obstruction.
Goal 6. Understand the approach to the facial trauma patient
Resident Objectives:
Provide effective specialist consult services to trauma team/ED for facial trauma.
Patient Care
Medical Knowledge
ACGME Competency Goals
Patient Care
Medical Knowledge
Professionalism
Interpersonal and Communication Skills
Understand wound healing.
Understand concepts of occlusion.
Evaluate patients with facial paralysis.
Understand pathophysiology of facial paralysis.
Goal 7. Chronic Otitis Media. Screen, diagnose and manage patients with symptoms
Medical Knowledge
Medical Knowledge
Patient Care
Medical Knowledge
Medical Knowledge
secondary to their chronic ear infections
Resident Objectives: ACGME Competency Goals
98
Be able to describe the anatomy, physiology, and pathophysiology of the middle ear and mastoid.
Medical Knowledge
Take a directed history focused on issues related to recurrent and chronic ear infections. Patient Care
Describe the use of diagnostic tests for assessing otologic disease (e.g. CT and MRI imaging, audiology, tympanometry).
Be able to assess the external and middle ear on exam, including the use of the binocular microscope.
Differentiate middle ear from external ear disease
Be able to counsel parents about the pathophysiology of conditions associated with chronic otitis, its risks, and treatment options.
Understand the indications for surgical intervention, its risks and potential complications
Be able to counsel parents about the risks and benefits of tympanomastoid surgery.
Know the perioperative management and expected postoperative course of patients who undergo tympanomastoid surgery.
Be able to safely and efficiently perform the approach for tympanomastoid surgery (postauricular incisions, canal incisions, harvesting graft materials).
Be comfortable with mastoidectomy techniques ( bony landmarks, use of drill for cortical bone removal, effective use Suction-irrigation system).
Be able to discuss the basics of tympanomastoid surgery patients including potential complications and postoperative expectations.
Goal 8. Vertigo. Be able to evaluate and treat peripheral vestibular disease.
Resident Objectives:
Be able to describe the anatomy, physiology, and pathophysiology of the peripheral vestibular system.
Be able to take a history related to balance and vertigo.
Know how to perform clinical examination of patients with vestibular complaints.
Patient Care
Medical Knowledge
Patient Care
Patient Care
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Professionalism
Interpersonal and Communication Skills
Patient Care
Patient Care
Patient Care
Patient Care
Interpersonal and Communication Skills
ACGME Competency Goals
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
99
Understand treatments available for acute vestibular dysfunction in the clinic and emergency room.
Be able to discuss factors involved in vertigo and balance dysfunction with patients and families.
Be able to counsel parents about the various treatment options available for management of Meniere’s disease, paroxysmal positioning vertigo, and vestibular neuronitis, superior semicircular canal dehiscence, etc
Be able to interpret the basics of vestibular function tests.
Be able to discuss care of vertigo patients with providers from other specialties to formulate a care plan involving a number of disciplines.
Counsel patients and families about compensatory strategies for minimizing risks in chronic vestibulopathy including the role of vestibular rehabilitation and physical therapy.
Goal 9. Hearing Loss
Resident Objectives:
Be able to obtain an appropriate hearing loss history.
Be able to recognize, describe and categorize acquired and congenital hearing loss.
Know the most common causes of sensorineural vs conductive hearing loss.
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
ACGME Competency Goals
Patient Care
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Be able to perform and interpret appropriate physical examination for hearing loss, including tuning fork exam, otomicroscopy, cranial nerve exam, pneumo -otoscopy.
Patient Care
Patient Care Understand the basics of audiometry, and how to interpret common audiometric tests.
Medical Knowledge
Be able to counsel patients about hearing aids and assistive listening devices.
Patient Care
Medical Knowledge
100
Understand the basic options involved in the surgical correction of conductive hearing loss (stapedectomy, ossiculoplasty).
Gain basic capacity for evaluating ossicular chain mobility intraoperatively, and gain a foundation for bimanual manipulation of prostheses under the surgical micr oscope.
Be able to discuss the basics of cochlear implantation with patients and families, including the basics of surgery, postoperative expectations, and need for rehabilitation services.
Goal 10. Neurotology. Diagnose and manage patients with skull base disease
Patient Care
Patient Care
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Resident Objectives: ACGME Competency Goals
Know the basic anatomy, physiology, and pathophysiology of the skull base.
Be able to obtain a history related to extra -axial neoplasms and other lesions of the internal auditory canal, cerebello -pontine angle, temporal bone and posterior fossa.
Understand the basic anatomy, signs, symptoms and clinical diagnosis of lesions of the petrous apex.
Understand the basics of radiologic studies used to diagnose lesions of the posterolateral skull base.
Understand the indications of ancillary tests (e.g. angiography, electrodiagnostic studies) to evaluate skull base lesions.
Be able to evaluate a patient with vestibular schwannoma in the clinic, including history, physical examination, audiometric data, and radiologic studies.
Be able to describe and recognize complications of cranial base surgery.
Be able to collaborate with a multidisciplinary team to provide comprehensive care for patients with skull base lesions.
Understand the basic management options for benign lesions of the posterio-lateral skull base including watchful waiting, focused radiation, and microsurgical resection.
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Goal 11. Audiology. Understand the methods available to test the hearing, and how to interpret the tests.
Resident Objectives: ACGME competency goals
101
Be familiar with the principal methods and indications for various audiometric tests including pure-tone testing, word recognitions scores, reflex testing, tympanometry).
Be familiar with the basics of assessing reliability in audiometric testing.
Be able to interpret routine tympanograms and audiograms.
Understand the basics of most specialized electrodiagnostic studies and their indications (including ABR, ECOG, VEMP, rotational chair, posturography testing, VNG, etc).
Goal 12. Facial nerve. Be able to diagnose and treat common facial nerve problems.
Resident Objectives:
Be able to describe the basic anatomy of the facial nerve and its common disorders, including their natural history, clinical presentation, evaluation and treatment.
Understand the management of acute facial paralysis, especially as it applies to the postoperative patient.
Goal 13. General Otology
Resident Objectives
Be able to obtain an appropriate history regarding external ear disease, including acute and chronic otitis externa and cerumen impaction.
Become comfortable with otoscopic examination and procedures involving the external auditory canal including canal debridement and cerumen removal.
Be able to discuss the procedure, risks, benefits, and expectations of myringotomy with aspiration, and myringotomy with tube placement.
Be able to discuss the basics of tinnitus diagnosis and management.
Be able to perform a directed history and physical examination for patients with otalgia.
Know how to obtain consultation from other related services for patients with otologic disorders.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
ACGME competency goals
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
ACGME competency goals
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
102
Develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor-patient relationship and the delivery of otologic care.
Develop an understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Become an intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
Develop an understanding of OHNS coding and compliance issues in otology/ neurotology.
Professionalism
Systems-Based Practice
Professionalism
Professionalism
Practice-Based Learning and Improvement
Professionalism
Systems-Based Practice
103
Goals and Objectives
PGY 4: SHC Specialty Service
Competency-based Goals and Objectives
Goal 1. Consults in an adult hospital. Continue to learn about consults requested regarding otologic problems.
Resident Objectives: ACGME Competency Goals
Be the backup or initial contact person for consults from other SHC services and the emergency department.
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Perform initial or backup evaluation for consult patients.
Be familiar with the subtleties of the SHC electronic medical record (Epic) and be able to access information appropriately. Understand the importance of confidentiality in patient medical records.
Evaluate consult patients with chief resident, fellow, and faculty member and communicate recommendations and plan to primary team. Consistently demonstrate courtesy when interacting with clinical and non -clinical staff members.
Patient Care
Medical Knowledge
Patient Care
Professionalism
Systems-Based Practice
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Perform a literature search to learn more about unusual patient problems, and teach other residents, and medical students.
Create or review a complete and coherent consultation note and dictate it in a timely fashion. This objective applies to all patients seen in the clinic setting as well as the outpatient setting.
Utilize translation services to communicate with non -English speaking patients as needed.
Medical Knowledge
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Professionalism
Interpersonal and Communication Skills
104
Demonstrate effective time -management skills.
Follow-up on consult patients as needed.
Attend multidisciplinary Skull Base Tumor rounds.
Systems-Based Practice
Practice-Based Learning and Improvement
Patient Care
Systems-Based Practice
Professionalism
Systems-Based Practice
Goal 2. Chronic Otitis Media. Screen, diagnose and manage patients with symptoms secondary to their chronic ear infections
Resident Objectives: ACGME Competency Goals
Be able to describe the anatomy, physiology, and pathophysiology of the middle ear and mastoid, and the variations seen that may influence optimal treatment options.
Take a refined history focused on issues related to recurrent and chronic ear infections.
Describe and assess the use of diagnostic tests for assessing otologic disease (e.g. CT and MRI imaging, audiology, tympanometry). Refine efficiency in ordering tests.
Be able to assess the external and middle ear on exam, including the use of the binocular microscope and otoendoscopy. Refine the interpretation of clinical findings to formulate a treatment plan.
Differentiate middle ear from external ear disease.
Be able to counsel parents about the pathophysiology of conditions associated with chronic otitis, its risks, and treatment options.
Understand the indications for surgical intervention, its risks and potential complications. Understand how history and anatomy influence surgical treatment planning.
Be able to counsel parents about the risks and benefits of tympanomastoid surgery, and obtain informed consent for planned procedure.
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Patient Care
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Professionalism
Interpersonal and Communication Skills
105
Know the perioperative management and expected postoperative course of patients who undergo tympanomastoid surgery. Be able to answer the majority of postoperative questions/ concerns.
Be able to safely and efficiently perform the majority of tympanomastoid surgery including mastoidectomy, transcanal procedures, ossiculoplasty, etc.
Refine comfort with mastoidectomy and bone removal techniques; increase safety and efficiency.
Be able to assess outcomes over time and formulate plans based on the evolution of the underlying disease.
Goal 3. Vertigo. Be able to evaluate and treat peripheral vestibular disease.
Resident Objectives:
Be able to describe the anatomy, physiology, and pathophysiology of the peripheral vestibular system, and how it impacts clinical presentation.
Be able to take a history related to balance and vertigo. Formulate a directed and practical differential diagnosis.
Know how to perform clinical examination of patients with vestibular complaints. Differentiate peripheral from central pathology.
Understand treatments available for acute vestibular dysfunction in the clinic and emergency room.
Refine ability to discuss factors involved in vertigo and balance dysfunction with patients and families.
Patient Care
Patient Care
Patient Care
Patient Care
ACGME Competency Goals
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Be able to counsel parents about the various treatment options available for management of Meniere’s disease, paroxysmal positioning vertigo, and vestibular neuronitis, superior semicircular canal dehiscence, etc. Discuss medical vs surgical approaches, and formulate an understanding of the role of surgery in these disorders.
Be able to interpret vestibular function tests, and use them in forming a treatment plan.
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
106
Be able to discuss care of vertigo patients with providers from other specialties to formulate a care plan involving a number of disciplines. Understand the role of otolaryngologist and other specialists in the management of vestibular disorders.
Be familiar with the surgical management of peripheral vestibular disease, and be able to perform the majority of the steps necessary for their successful completion.
Goal 4. Hearing Loss
Resident Objectives:
Be able to obtain a comprehensive hearing loss history and formulate a treatment plan.
Refine the ability to recognize, describe and categorize acquired and congenital hearing loss.
Know the most common causes of sensorineural vs conductive hearing loss.
Perform an efficient physical examination for hearing loss, including tuning fork exam, otomicroscopy, cranial nerve exam, pneumo -otoscopy, and know whn additional testing is needed
Understand audiometric testing, and how to fully interpret their findings to direct care. Refine the ability to discuss patient data with audiologists to optimize care.
Understand the basics of hearing aid types, styles, limitations, and the fitting process.
Understand the options of surgical correction of conductive hearing loss (stapedectomy, ossiculoplasty) including their indications, limitations, and the relevant anatomic variations that could be encountered intraoperatively.
Gain additional familiarity with intraoperative evaluation of ossicular chain mobility, and understand the reconstructive options that are available for a given patient. Be able to place the majority of ossicular prostheses.
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
ACGME competency goals
Patient Care
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Patient Care
107
Be able to assess patients for possible cochlear implantation. Be able to discuss the indications, surgery, postoperative expectations, and need for rehabilitation services. Be able to perform the majority of cochlear implantation with intraoperative supervision.
Goal 5. Neurotology. Diagnose and manage patients with skull base disease
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Resident Objectives: ACGME Competency Goals
Refine the understanding of skull base anatomy to understand the influence of anatomic and pathologic variability on treatment options and patient care.
Be able to obtain a detailed history related to extra-axial neoplasms and other lesions of the internal auditory canal, cerebellopontine angle, temporal bone and posterior fossa. Incorporate relevant patient data into an efficient and optimized care plan.
Understand the surgical anatomy, signs, symptoms and clinical diagnosis of lesions of the petrous apex. Refine an understanding for which lesions require immediate treatment, and which do not.
Understand the interpretation of radiologic studies used to diagnose lesions of the posterolateral skull base. Be able to combine different modalities in formulating a diagnosis.
Be able to effectively use ancillary tests (e.g. angiography, electrodiagnostic studies, nuclear studies) to evaluate skull base lesions.
Be able to evaluate a patient with vestibular schwannoma in the clinic, and formulate a reasonable treatment plan based on findings, radiology, and patient preferences.
Be able to recognize complications of cranial base surgery, including vascular injury, spinal fluid leak, cranial neuropathy, infection, and CNS injury. Recognize the causative factors, and formulate a basic management plan.
Refine the ability to collaborate at a high level with a multidisciplinary team to provide comprehensive care for patients with skull base lesions.
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
108
Understand the options for benign lesions of the postero -lateral skull base including watchful waiting, focused radiation, and microsurgical resection. Have a basic understanding of treatment planning for stereotactic radiosurgery.
Patient Care
Medical Knowledge
Goal 6. Audiology. Understand the methods available to test the hearing, and how to interpret the tests.
Resident Objectives: ACGME competency goals
Be familiar with the indications for various audiometric tests including pure -tone testing, word recognitions scores, reflex testing, tympanometry). Understand how to use these tests efficiently in the context of clinical findings.
Be familiar with interpreting audiometric testing, including their accuracy, reliability, and impact on clinical care.
Be able to perform routine tympanograms and audiograms.
Understand specialized electodiagnostic studies and their indications (including ABR, ECOG, VEMP, rotational chair, posturography testing, VNG, etc). Understand how they can guide further treatment.
Goal 7. Facial Nerve
Resident Objectives:
Understand the surgical anatomy of the facial nerve and its common disorders, including their natural history, clinical presentation, evaluation and treatment.
Be able to identify and decompress the intratemporal facial nerve with supervision as clinically indicated. Be able to perform the majority of facial nerve neurorrhaphy, including donor graft harvest.
Goal 8. General Otology
Resident Objectives
Be able to obtain an appropriate history regarding external ear disease. Understand cutaneous disorders that may be related and the indications for biopsy.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
ACGME competency goals
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
ACGME Competency Goals
Patient Care
Interpersonal and Communication Skills
109
Become more comfortable with clinical otologic procedures including myringotomy, and intratympanic injections. Be familiar with local anesthetic used for outpatient otologic procedures.
Be able to discuss the basics of intratympanic treatment, including the procedure, its risks, benefits, and expectations.
Be able to effectively evaluate and treat the majority of patients complaining of tinnitus.
Refine the approach to patients with otalgia, including an understanding of when to involve consultation for non-otologic etiologies.
Refine the interaction with other related consult services for patients with otologic complaints.
Further develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor -patient relationship and the delivery of otologic care.
Develop an improved understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Become a more intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and statistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
Develop an understanding of OHNS coding and compliance issues in otology/ neurotology.
Goal 9. Nasal cavity and sinuses. Diagnose and manage patients with nasal problems.
Resident Objectives
Be familiar with the EMR at Stanford (EPIC) to confidentially access appropriate patient information, past culture results, pathology reports and past imaging studies.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Professionalism
Professionalism
Practice-Based Learning and Improvement
Professionalism
Systems-Based Practice
ACGME Competency Goals
Patient Care
Professionalism
Systems-Based Practice
110
Evaluate consult patients with sinonasal disorders with the senior residents and faculty. Be able to document and communicate recommendations and plan with the primary team in a professional and courteous manner.
Know the anatomy, pathophysiology, and development of the nasal cavity and sinuses.
Perform literature searches to investigate common and rare patient presentations, and to obtain evidence for current practice paradigms in patient care.
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Medical Knowledge
Medical Knowledge
Practice-Based Learning and Improvement
Professionalism
Understand principles and utility of CT versus MRI imaging of the sinuses. Understand and describe anatomic variations of the 4 pairs of paranasal sinuses, patterns of uncinate process attachment and sinus drainage patterns.
Be able to obtain a detailed history related to the nose and nasal problems related to sinus disease and allergic rhinitis.
Perform safe, informative routine office nasal endoscopy with 0 degree and 30 degree rigid endoscopes.
Access and understand AAO descriptive guidelines for acute, subacute and chronic sinusitis, and know the major and minor symptoms associated with diagnosis of sinusitis.
Evaluate patients with chronic sinusitis with and without polyposis – and distinguish which patients may require surgery or medical therapy.
Be able to describe and recognize complications of acute sinusitis.
Identify the signs and symptoms and differences between allergic rhinitis and acute/chronic sinusitis.
Understand indications for safe intranasal office biopsy.
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Medical Knowledge
Professionalism
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
111
Be proficient with the evaluation and management algorithms for treating epistaxis.
Patient Care
Medical Knowledge
Understand options for treatment of nasal septal deviation and turbinate hypertrophy.
Patient Care
Medical Knowledge
Learn the assembly of equipment needed to perform nasal endoscopy, and intraoperative image guidance.
Complete basic aspects of endoscopic approaches to the nasal cavity – including use of zero-degree and 30 degree endoscopes, safely navigating the nasal cavity with mucosal preserving technique, performing septoplasty, turbinate reduction, maxillary antrostomy, and anterior ethmoidectomy.
Goal 10. Understand the basics of the aesthetic patient consultation
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Understand and be able to perform psychological assessment for potential aesthetic surgery patients.
Describe how to perform outpatient filler or botulinum toxin injections.
Know literature regarding efficacy of facial rejuvenation procedures.
Understand basic medical photography.
Goal 11. Understand the approach to the rhinoplasty patient
Medical Knowledge
Patient Care
Medical Knowledge
Medical Knowledge
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Understand and provide psychological assessment for potential rhinoplasty patients.
Understand anatomy of the internal and external nasal valve and repair.
Know literature regarding efficacy of nasal surgical procedures.
Understand basic aesthetic nasal analysis.
Goal 12. Understand the approach to the facial trauma patient
Medical Knowledge
Patient Care
Medical Knowledge
Medical Knowledge
Medical Knowledge
Resident Objectives: ACGME competency goals
112
Be able to assess and perform soft tissue repair.
Understand pathophysiology of facial fractures and provide effective plan of care.
Understand the biomechanics of fixation for fractures
Know literature regarding facial trauma.
Goal 13. Understand the approach to the facial nerve trauma patient
Resident Objectives:
Be able to explore the extratemporal facial nerve.
Be able to discuss options for treatment of facial nerve paralysis.
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
ACGME Competency Goals
Medical Knowledge
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
113
Competency-based Goals and Objectives
Goal 1. Consults in an adult hospital. Continue to learn about consults requested regarding otologic problems.
Resident Objectives:
Provide backup resident evaluation for all consults from other SHC services and the emergency department. Effectively oversee the discussion of all consults on daily rounds.
ACGME Competency Goals
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
See consult patients as indicated, and formulate a plan for care. Discuss with attending staff as needed. Oversee the implementation of all clinical plans.
Develop a comprehensive understanding of the SHC electronic medical record (Epic) and be able to access information appropriately. Understand the importance of confidentiality in patient medical records. Provide backup and instruction for the other resident team members for its use.
Learn to effectively run an inpatient service. Understand how to assign duties appropriate for each resident’s level of training. Provide administrative leadership to cover consults, operative cases, and outpatient clinic.
Patient Care
Medical Knowledge
Patient Care
Professionalism
Systems-Based Practice
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Establish competency as a leader for teaching on rounds and assigning academic duties to the resident team.
Understand how to oversee all communications between the resident service and other services who share common patients. Learn how to be accurate, professional, and efficient in these interactions.
Medical Knowledge
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Professionalism
114
als
Go
and Objectives PGY 5: SHC Specialty Service
Establish leadership skills in planning academic meetings, conferences, and schedules. Interpersonal and Communication Skills
Systems-Based Practice
Refine effective time-management skills given expected additional time constraints imposed by academic duties.
Learn to integrate varied patient care styles from different attendings, and use these to develop personal preferences.
Lead Skull Base Tumor rounds discussions, understand issues examined, and implement decisions as required.
Practice-Based Learning and Improvement
Patient Care
Systems-Based Practice
Professionalism
Systems-Based Practice
Goal 2. Chronic Otitis Media. Screen, diagnose and manage patients with symptoms secondary to their chronic ear infections.
Resident Objectives:
Develop a comprehensive understanding of the surgical anatomy, physiology, and pathophysiology of the middle ear and mastoid. The depth of understanding should allow the resident to operate independently in the great majority of chronic ear procedures.
Take a refined history focused on issues related to recurrent and chronic ear infections, and formulate an optimized plan of care.
Order and interpret diagnostic tests for assessing otologic disease (e.g. CT and MRI imaging, audiology, tympanometry). Refine efficiency in ordering tests and establish individualized protocols for managing chronic ear disease.
Be able to assess the ear on exam. Develop mastery of the binocular microscope and otoendoscopy. Understand what findings necessitate operative intervention, and which can be treated in the outpatient clinic.
Be able to teach junior residents and medical students the basics of middle ear disease.
Refine the ability to counsel parents regarding the pathophysiology of conditions associated with chronic otitis, its risks, and treatment options.
ACGME Competency Goals
Medical Knowledge
Patient Care
Patient Care
Medical Knowledge
Systems-Based Practice
Patient Care
Patient Care
Patient Care
Interpersonal and Communication Skills
115
Understand the indications for surgical intervention, its risks and potential complications. Understand how history and anatomy influence surgical treatment planning. Be able to formulate an independent plan for management of broad categories of middle ear disease.
Patient Care
Be able to appropriately manipulate even difficult ears in the clinic with a minimum of patient discomfort. Develop the confidence and reassuring tone to enable this.
Know the management and expected postoperative course of patients who undergo tympanomastoid surgery. Be able to answer the postoperative questions/ concerns, and arrange for appropriate follow -up care.
Be able to safely and efficiently perform the majority of tympanomastoid surgery including mastoidectomy, transcanal procedures, ossiculoplasty, etc.
Be able to safely work in anatomically challenging middle ears with unconventional anatomy.
Be able to take junior residents through the basic steps of tympanomastoid surgery.
Develop a comprehensive understanding of the natural history of chronic ear disease and its response to treatment.
Goal 3. Vertigo. Be able to evaluate and treat peripheral vestibular disease.
Resident Objectives:
Refine the understanding of the anatomy, physiology, and pathophysiology of the vestibular system (both peripheral and central), and how it impacts clinical presentation.
Be able to take a history related to balance and vertigo. Formulate a directed and practical differential diagnosis.
Know how to perform clinical examination of patients with vestibular complaints. Differentiate peripheral from central pathology. Incorporate the interpretation of specialized vestibular tests.
Be able to formulate, present and carry out an incremental approach to treating peripheral vestibulopathy.
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Patient Care
Patient Care
Patient Care
Patient Care
Patient Care
ACGME competency goals
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Patient Care
Medical Knowledge
116
Refine the ability to discuss factors involved in vertigo and balance dysfunction with patients and families.
Be able to counsel parents about the various treatment options available for management of Meniere’s disease, paroxysmal positioning vertigo, and vestibular neuronitis, superior semicircular canal dehiscence, etc. Discuss medical vs surgical approaches, and formulate an understanding of the role of surgery in these disorders.
Be able to interpret the subtleties of vestibular function tests (VNG, VEMP, ECOG, etc), and use them in forming a treatment plan.
Be able to discuss care of vertigo patients with providers from other specialties to formulate a care plan involving a number of disciplines. Understand the role of otolaryngologist and other specialists in the management of vestibular disorders.
Be familiar with the surgical management of peripheral vestibular disease, and be able to perform the majority of the steps necessary for their successful completion – including selective canal plugging, vestibular neurectomy, and labyrinthectomy.
Goal 4. Hearing Loss
Resident Objectives:
Be able to obtain a comprehensive hearing loss history and formulate a treatment plan.
Refine the ability to recognize, describe and categorize acquired and congenital hearing loss.
Be able to formulate an appropriate and cost -effective work-up for retrocochlear diagnosis, and evaluation of congenital hearing loss.
Perform an efficient physical examination for hearing loss, including tuning fork exam, otomicroscopy, cranial nerve exam, pneumo -otoscopy, and know when additional testing is needed.
Understand audiometric testing, and how to fully interpret their findings to direct care. Refine the ability to discuss patient data with audiologists to optimize care.
Patient Care
Interpersonal and Communication Skills
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
ACGME competency goals
Patient Care
Patient Care
Medical Knowledge
Patient Care Systems-Based Practice
Patient Care
Patient Care
Medical Knowledge
117
Understand the basics of hearing aid types, styles, limitations, and the fitting process. Have a basic understanding of how to incorporate hearing aid dispensing into an otolaryngologic practice.
Understand the options of surgical correction of conductive hearing loss (stapedectomy, ossiculoplasty) including their indications, limitations, and the relevant anatomic variations that could be encountered intraoperatively.
Patient Care
Medical Knowledge
Patient Care
Gain clinical competence in the intraoperative evaluation of ossicular chain mobility, and understand the reconstructive options are available for a given patient. Be able to place the ossicular prostheses. Be able to perform the majority of uncomplicated stapes surgery.
Patient Care
Patient Care Be comfortable in evaluating cochlear implant candidates. Be able to disc uss the indications, surgery, postoperative expectations, and need for rehabilitation services. Present the different type of devices available, and understand current areas of clinical research that may implant care. Be able to perform the majority of c ochlear implantation.
Medical Knowledge
Interpersonal and Communication Skills
Goal 5. Neurotology. Diagnose and manage patients with skull base disease
Resident Objectives: ACGME Competency Goals
Refine the understanding of skull base anatomy to understand the influence of anatomic and pathologic variability on treatment options and patient care. Be able to list the clinical and radiographic presentation of skull base lesions.
Refine the ability to obtain a detailed history related to extra -axial neoplasms and other lesions of the internal auditory canal, cerebellopontine angle, temporal bone and posterior fossa. Incorporate relevant patient data into an efficient and optimized care plan.
Understand the surgical anatomy, signs, symptoms and clinical diagnosis of lesions of the petrous apex, clivus, and jugular foramen. Refine an understanding for which lesions require immediate treatment, and which d o not.
Understand the interpretation of radiologic studies used to diagnose lesions of the posterolateral skull base. Be able to combine different modalities in formulating a diagnosis and appropriate treatment plan.
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
118
Be able to effectively order and interpret ancillary tests (e.g. angiography, electrodiagnostic studies, nuclear studies) to evaluate skull base lesions. Discuss the findings effectively with radiologists.
Be able to evaluate a patient with vestibular schwannoma and similar lesions, and formulate a reasonable treatment plan based on findings, radiology, and patient preferences. Formulate a work -up and treatment plan for patients with NF-2.
Be able to recognize complications of cranial base surgery, including vascular injury, spinal fluid leak, cranial neuropathy, infection, and CNS injury. Recognize the causative factors, and formulate a basic management plan. Understand methods and tehniques to avoid such complications.
Refine the ability to collaborate at a high level with a multidisciplinary team to provide comprehensive care for patients with skull base lesions.
Understand the options for benign lesions of the postero -lateral skull base including watchful waiting, focused radiation, and microsurgical resection. Be familiar with treatment planning for stereotactic radiosurgery for uncomplicated lesions of the cranial base.
Be able to perform the majority of surgical approaches to the cranial base including transmastoid approaches to the jugular foramen, petrous apicectomy, translabyrinthine approaches, and middle fossa craniotomy.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Goal 6. Audiology. Understand the methods available to test the hearing, and how to interpret the tests.
Resident Objectives:
Be familiar with the indications for all used audiometric tests including pure -tone testing, word recognitions scores, sentence testing, reflex testing, tympanometry). Understand how to use these tests efficiently in the context of clinical findings.
Be familiar with interpreting audiometric testing, including their accuracy, reliability, and impact on clinical care.
Be able to perform routine tympanograms and audiograms.
ACGME Competency Goals
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
119
Understand specialized electodiagnostic studies and evokes responses and their indications (including ABR, ECOG, VEMP, rotational chair, posturography testing, VNG, etc). Understand how they can guide further treatment.
Goal 7. Facial Nerve
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Understand the surgical anatomy of the facial nerve and its common disorders, including their natural history, clinical presentation, evaluation and treatment.
Be able to find and decompress the intratemporal facial nerve with supervision as clinically indicated. Be able to perform the majority of facial nerve neurorrhaphy, including donor graft harvest. Be comfortable with techniques of facial nerve re -routing.
Goal 8. General Otology
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Resident Objectives: ACGME Competency Goals
Be able to independently manage uncomplicated cutaneous lesions of the external ear canal and pinna. Be able to communicate the treatment options and expectations with the patient.
Be able to perform clinic-based otologic procedures including myringotomy, and intratympanic injections. Be familiar with local anesthetic used for outpatient otologic procedures.
Be able to discuss the basics of intratympanic treatment, including the procedure, its risks, benefits, and expectations.
Be able to effectively evaluate and treat the majority of patients complaining of tinnitus and the spectrum of other non-surgical otologic complaints.
Further refine the care of otalgia, including an understanding of when to involve consultation for non-otologic etiologies and when to consult other specialists (pain service, oral surgery, laryngology, etc).
Be able to teach junior residents and medical students in the approach to outpatient otology.
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
120
Further develop an understanding of and sensitivity to the impact of cultural, economic and ethnic factors in the doctor -patient relationship and the delivery of otologic care.
Develop an improved understanding of one’s own abilities and limitations including awareness of signs of fatigue.
Become a more intelligent user of the academic literature in otolaryngology. Demonstrate the ability to apply knowledge of study designs and sta tistical methods to appraise clinical studies. Perform literature searches as needed to continuously improve the level of medical knowledge.
Develop an understanding of OHNS coding and compliance issues in otology/ neurotology.
Goal 9. Understand the basics of the aesthetic patient consultation
Resident Objectives:
Be able to perform a blepharoplasty (upper or lower).
Goal 10. Understand the approach to the rhinoplasty patient
Resident Objectives:
Be able to perform an effective functional or aesthetic septorhinoplasty.
Goal 11. Understand the approach to the facial trauma patient
Resident Objectives:
Be able to perform repair of frontal sinus, naso-orbito-ethmoidal, maxillary, orbital, and mandibular fractures.
Goal 12. Understand the approach to the facial trauma patient
Resident Objectives:
Be able to perform a canthoplasty and gold weight procedure.
Goal 13. Nasal cavity and sinuses. Diagnose and manage patients with nasal problems.
Resident Objectives:
Professionalism
Systems-Based Practice
Professionalism
Professionalism
Practice-Based Learning and Improvement
Professionalism
Systems-Based Practice
ACGME Competency Goals
Medical Knowledge
Patient Care
ACGME Competency Goals
Patient Care
Medical Knowledge
ACGME competency goals
Patient Care
Medical Knowledge
ACGME competency goals
Medical Knowledge
Patient Care
ACGME Competency Goals
121
Be familiar with the EMR at Stanford (EPIC) to confidentially access appropriate patient information, past culture results, pathology reports and past imaging studies.
Effectively comprehensively manage primary inhouse, post-operative and consult patients with sinonasal disorders with the junior and senior residents.
Patient Care
Professionalism
Systems-Based Practice
Patient Care
Medical Knowledge
Systems-Based Practice
Interpersonal and Communication Skills
Know the endoscopic anatomy and pathophysiology of the sinuses, paranasal skullbase, and extended skullbase including pterygopalatine fossa, infratemporal fossa, orbit, sella, lateral sphenoid recess, clivus and anterior skullbase.
Perform literature searches to prepar e for public presentations on rhinology topics, and effectively present in quality assurance conferences in a professional and composed manner.
Understand radiographic nuances of sinonasal disease processes using both CT versus MRI imaging – sinonasal neoplasms, intraorbital pathology, pneumocephalus, suprasellar intracranial disease.
Understand the posterior, lateral, inferior, and superior limits of endoscopic approaches to the skullbase
Understand fungal sinusitis, including fungal ball versus allergic fungal sinus disease versus invasive fungal sinusitis.
Evaluate patients with chronic sinusitis with and without polyposis – and distinguish which patients may require surgery or medical therapy.
Evaluate patients with chronic sinusitis who have received prior surgery. Understand indications for revision surgical procedures versus use of medical therapies.
Perform proper office debridement of the maxillary, ethmoid, sphenoid and frontal sinuses in the immediate post-operative setting with minimal patient discomfort.
Medical Knowledge
Medical Knowledge
Practice-Based Learning and Improvement
Professionalism
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Medical Knowledge
Systems-Based Practice
Patient Care
Medical Knowledge
Professionalism
Patient Care
Medical Knowledge
Professionalism
Patient Care
Medical Knowledge
Professionalism
122
Understand the etiology of sinusitis in the setting of immunosuppression, and surgically manage patients with invasive fungal sinus disease.
Identify the signs and symptoms of more rare intranasal pathology, such as autoimmune disease (Wegener’s) and granulomatous (Churg -Strauss) disease.
Understand and describe complications of endoscopic sinus surgery, including orbital injury, CSF leak, synechiae formation, middle turbinate lateralization and need for revision surgery. Be able to effectively and compassionately counsel patients of these details.
Utilize more advanced equipment and instrumentation to access the nasal cavity –including use of 30, 45, and 70 degree endoscopes to access areas of the nasal cavity, use of hand instrumentation and powered instruments such as microdebriders and drills, and endoscopic cautery tools.
Perform safe and methodical endoscopic sinus surgery, including skullbase dissection, frontal sinusotomy, modified Lothrop procedure, and revision endoscopic sinus surgery.
Understand principles and techniques for performing open skullbase surgery, including frontal sinus obliteration, cranialization, and Reidel procedures.
Demonstrate appropriate surgical technique for advanced endoscopic orbital surgery, including endoscopic dacrocystorhinostomy (DCR) and orbital decompression. Work effectively with the Opthalmology service to coordinate patient intraoperatively and on the floors.
Understand and appropriately use reconstructive ladders for intranasal and skullbase lesions, including free tissue grafts, pedicled mucosal tissue flaps, pericranial flaps, and free flaps.
Perform safe and efficient endoscopic resection of anterior midline skullbase pathology with reconstruction. Work closely and effectively with a neurosurgical service in coordinated surgical efforts when required.
HALF-TIME RESEARCH RESIDENT
• Research Resident must have at least 2.5 days of research time per week on average.
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
• During PGY2 or PGY4’s vacation/conference/interview period, Half -time Research Resident usually works as full time.
123
Rotation Contacts and Scheduling Details
Rotation Director: Misha Amoils, MD
Santa Clara Valley Medical Center
Attendings: Amoils, Lalakea, Munoz, Saste, Shepard, Noel
Introduction
Santa Clara Valley Medical Center is located 25 minutes south of Stanford University, and is a county hospital facility. Rota tions at this facility complement the residency experience by providing exposure to a culturally diverse, medically indigent popula tion with a broad range of OTO/HNS pathology.
The R2 resident should review the R3 Research Rotation Goals and Objectives. The research plan must be completed during the R2 year.
Additional Required Conferences:
o All VMC OTO/HNS Teaching Conferences:
o OTO/HNS Radiology Conference, OTO/HNS Pathology Conference (each conference once monthly).
o Monday AM Stanford teaching conferences
124
Weekly Schedule
6:00- 7:00 Rounds Rounds Rounds Rounds Rounds
8:00- 10:00 Res Ed at Stanford
All Day
6:00- 18:00 Inpatient consults for R2 and R5 residents
Gen Clinic Gen Clinic Gen Clinic Gen Clinic Gen Clinic
8:00- 12:00
12:00-16:00
Amoils, Saste Saste, Noel Lalakea, Munoz Shepard, Munoz Saste, Lalakea
Gen Clinic Gen Clinic Gen Clinic Gen Clinic Gen Clinic
Amoils, Lalakea Amoils, Shepard Lalakea Munoz, Noel Amoils
Radiology conference
(Every 4th Thursday)
12:00-13:00
Pathology conference
8:30- 17:30 OR Shepard (4th Saste)
7:30- 17:30 OR Lalakea
7:30 -17:30 OR Amoils
(Every 2nd Thursday) OR
7:30 -17:30 OR 1st, 3rd, 5th: Saste
7:30 -17:30 OR Munoz/Noel
18:00-19:00
2nd resident to assist in OR M, T, W, Th, F afternoons at conclusion of clinic .
Rotation Specifics
Grand Rounds at Stanford
1. Rounding: Residents are expected to round daily before O.R. and daily after clinic/OR. Residents are expected to round daily on weekends in the AM. The chief resident is expected to teach junior residents while on rounds.
125
Time Monday Tuesday Wednesday Thursday Friday
Clinic
2. The attending on call should be phoned after rounds and given the patient update. Call other attendings as needed for specif ic patient issues.
3. The attending on call should be called about all admissions to the hospitals, all patients going to the operating room and all complicated evening or nighttime consults.
4. Consult patients should be seen and evaluated within ½ day of receiving the consult and discussed with the attending. Attend ing will sign off within 24 hours.
5. OR cases should be covered by the appropriate level residents with attending faculty present. Residents are expected to hand down cases as appropriate. Operative reports should be dictated/typed the day of the procedure.
6. Cases going on after 5 pm should be covered by the on-call resident if local to Valley, otherwise the appropriate level resident. If a senior level case is going on and no clinics are in process then a junior resident is encouraged to scrub in and assis t with case.
7. Pre-ops should be reviewed the week prior. Residents are expected to know the patient information.
8. Residents are released from duty when the work is done with attention to resident work hours and patient care.
Evaluation and Feedback
The Santa Clara Valley Medical Center faculty, and selected ancillary medical personnel will complete written evaluations at the end of the rotation. Selected clinic patients will evaluate the residents. Residents will be asked to evaluate each Faculty Member and the rotation. Daily feedback on physical findings, assessment, plan, and surgical technique will occur through clinical interactions.
126
Goals and Objectives PGY 2: SCVMC
Competency-based Goals and Objectives
Goal 1: Learn how to evaluate and counsel otolaryngology patients with common conditions related to the head and neck.
Resident Objectives:
Regularly attend outpatient clinics and learn a complete head and neck history and examination on adult and pediatric patients with attending supervision/verification of positive/negative findings.
Begin to attain an understanding of appropriate work -up and available medical and surgical treatment options for adults with common conditions such as chronic otitis media, nasal obstruction, sleep apnea, chronic sinusitis, gastroesophageal reflux, asymmetric sensorineural hearing loss, vocal cord paralysis, epistaxis, head and neck malignancy, and otitis externa.
Be able to effectively counsel patients regarding the treatment alternatives, indications, risks, benefits, and expected post-operative course of basic surgical procedures such as:
o Uvulopalatopharyngoplasty
o Septoplasty
o Turbinate reduction
o Tracheotomy
o Tympanostomy tube placement
o Intracapsular versus total tonsillectomy
o Excisional biopsy of neck mass
o Laryngoscopy, esophagoscopy, and bronchoscopy
Be able to effectively counsel patients regarding medical ENT topics such as presbycusis, tinnitus, control of seasonal allergies, head and neck cancer risk factors, and smoking cessation.
Learn basic audiologic principles and understand the interpretation of audiologic tests.
Begin to develop a practical and cost -effective approach to providing excellent care within the constraints of resources available to uninsured/under -insured patients.
ACGME Competency Goals
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Medical Knowledge
Systems-Based Practice
Patient Care
127
Begin to develop competency in recognizing emergencies in the adult and pediatric patient, including airway emergencies.
Patient Care
Learn the nuances of performing fiberoptic nasopharyngoscopy and laryngoscopy. Patient Care
Learn to perform pneumatic otoscopy to improve accuracy in the diagnosis of middle ear effusion.
Learn the ways in which normal pediatric anatomy may differ from adult anatomy, and the appearance of common pediatric disorders.
Learn to obtain a directed history and exam for common pediatric problems such as sleep apnea, hearing loss, speech delay, epistaxis, and stridor.
Be able to discuss appropriate work -up and management for pediatric conditions such as otitis media, sleep disorders, sinusitis, laryngomalacia, recurrent respiratory papillomatosis, and neck masses.
Be able to effectively counsel patients/families regarding the treatment alternatives, indications, risks, benefits, and expected postop recovery of the following procedures:
o Pressure equalizing tube placement
o Tonsillectomy
o Adenoidectomy
o Laryngoscopy and bronchoscopy
o Excision of neck mass (e.g. thyroglossal duct cyst)
o Tracheostomy
o Tympanoplasty
Be able to effectively counsel patients/families regarding medical ENT topics such as congenital hearing loss, risk factors for otitis media, second -hand smoke risks, epistaxis prevention.
Develop a sense of empathy regarding the barriers that conspire to prevent patients from receiving optimal healthcare (lack of transportation, language barriers, socioeconomic status, cultural differences, education level, family support, etc.).
Understand the importance of confidentiality in patient medical records, patient care, and patient related communications.
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Professionalism
Professionalism
Interpersonal and Communication Skills
128
Begin to develop an understanding of one's own abilities and limitations, including fatigue-management, and a commitment to life -long learning and improvement.
Become a competent user of the literature in otolaryngology, through targeted literature searches and critical review of literature, to direct patient care and improve medical knowledge.
Develop an understanding of OHNS documentation, coding and compliance issues.
Goal #2: Learn to perform basic otolaryngology procedures
Resident Objectives:
Be able to competently perform the following procedures with direct attending supervision:
o Tympanostomy tube placement
o Tonsillectomy and adenoidectomy, both total and intracapsular
o Endoscopy, including direct laryngoscopy, suspension laryngoscopy, esophagoscopy, and bronchoscopy in children and adults
o Routine tracheotomy
o Removal of simple neck masses/cysts
o Repair of complex facial lacerations
o Removal of uncomplicated esophageal foreign bodies
o Incision and drainage of neck abscess
o Inferior turbinate reduction
o Nasal fracture reduction
Be able to assemble the equipment needed to perform a laryngoscopy, bronchoscopy and esophagoscopy.
Practice-Based Learning and Improvement
Professionalism
Practice-Based Learning and Improvement
Systems-Based Practice
Professionalism
ACGME Competency Goals
Patient Care
Patient Care
Goal #3: Begin to appreciate systems-based understanding of otolaryngology practice and general OHNS issues
Resident Objectives:
Begin to appreciate importance of E&M and procedure coding, surgical procedures, consultations, and outpatient visits (CPT and ICD -10).
Begin to understand the importance of documentation to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
ACGME Competency Goals
Systems-Based Practice
Professionalism
Systems-Based Practice
Professionalism
Patient Care
129
Begin to develop sense of empathy regarding the barriers that conspire to prevent patients from receiving optimal healthcare (lack of transportation, language barriers, socioeconomic status, cultural differences, education level, family support, etc.)
Understand the importance of maintaining confidentiality in patient medical records, patient care, and patient related communications.
Interpersonal and Communication Skills
Professionalism
Professionalism
Interpersonal and Communication Skills
130
Goals and Objectives
PGY 5: SCVMC
Competency-based Goals and Objectives
Goal #1: Know how to evaluate, counsel and treat otolaryngology patients.
Resident Objectives: ACGME Competency Goals
Exhibit confidence and independence while pursuing a well -reasoned approach to the evaluation and management of the full spectrum of OTO/HNS patients.
The R5 will be able to efficiently execute the evaluation of most patients without major changes being suggested by supervising faculty.
Demonstrate a command of relevant current literature and be able to apply it in the development of an evaluation and (surgical and/or non -surgical) treatment plan for the full spectrum of OTO/HNS problems such as:
o Head and neck malignancy
o Complicated sinonasal disease
o Complex facial trauma
o Complex oto-neurotologic complaints
o Structural and functional voice/swallowing disorders
o Thyroid and parathyroid disorders
Demonstrate confidence and competence in the management of OTO/HNS emergencies, along with the skills needed to effectively lead the patient care team.
Professionalism
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Medical Knowledge
Patient Care
Practice-Based Learning and Improvement
Demonstrate the ability to think ahead and contingency plan to avoid errors caused by lack of equipment, lack of staff, or lack of appropriate attending or specialty back -up, and to communicate effectively while leading the patient -care team .
Patient Care
Medical Knowledge
Professionalism
Interpersonal and Communication Skills
Systems-Based Practice
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
131
Recognize and anticipate complications such as airway compromise, hemorrhage, hematoma, infection, CSF leak, and fistula.
Develop and execute a treatment plan to manage such complications, while taking responsibility as appropriate, and using such experiences to improve patient care.
Patient Care
Medical knowledge
Patient Care
Medical Knowledge
Professionalism
Practice-Based Learning and Improvement
Be able to apply information gained from radiographic studies in the assessment of head and neck lesions, congenital anomalies, paranasal sinus pathology and temporal bone pathology, and understand the appropriate use, overuse, and limitation of these studies.
Demonstrate competence in the interpretation of the full range of audiologic studies including ABR, Enog, and OAEs.
Be able to successfully transition from supervision by faculty to primary decision-making with faculty oversight.
Take primary responsibility for co -directing monthly pathology and radiology teaching conferences with the Pathology and Radiology Departments.
Supervise presentation of complications on the service at monthly Quality Improvement conference, including review of relevant literature.
Develop the resident call schedule and weekly OR schedule.
Demonstrate competence and organizational skills in directing the resident team in the daily management of in-house patients and OR activities.
Demonstrate ability and commitment in the day -to-day informal teaching and mentoring of students and junior residents.
Be able to competently supervise/assist junior residents performing common OTO/HNS surgical procedures.
Systems-Based Practice
Medical Knowledge
Patient Care
Medical Knowledge
Professionalism
Medical Knowledge
Patient Care
Interpersonal and Communication Skills
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
Medical Knowledge
Interpersonal and Communication Skills
Patient Care
Professionalism
Interpersonal and Communication Skills
Interpersonal and Communication Skills
Medical Knowledge
Interpersonal and Communication Skills
Medical Knowledge
132
Successfully demonstrate excellent interpersonal skills, effectively setting the tone for other members of the resident team, clinical and non -clinical staff.
Demonstrate competence in OHNS coding, compliance, documentation and confidentiality issues.
Demonstrate a high-level of empathy and 'cultural competence' regarding those factors that conspire to prevent patients from receiving optimal healthcare (lack of transportation, language barriers, socioeconomic status, cultural differences, education level, family support, etc.), and an understanding of resources that can be utilized to improve care in these situations
Demonstrate a high degree of self -knowledge, including personal strengths and weaknesses, including the ability to expand medical knowledge through literature review, to be appropriately self-critical, and to request assistance and/or consultation as needed.
Goal #2: Be able to safely and efficiently perform advanced otolaryngology procedures
Resident Objectives:
Be able to competently and efficiently perform advanced otolaryngology procedures with attending supervision such as:
o Laryngology
• Microdirect laryngoscopy with endoscopic intervention
o Otology/Neurotology
• Tympanomastoidectomy
• Ossicular chain reconstruction
• Stapedotomy
o Head and Neck
• Partial maxillectomy
• Modified radical neck dissection
• Composite resection
• Partial glossectomy
• Total or superficial parotidectomy
• Surgical management of aggressive thyroid malignancy
Interpersonal and Communication Skills
Professionalism
Professionalism
Systems-Based Practice
Patient Care
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Professionalism
Practice-based Learning and Improvement
ACGME Competency Goals
Patient Care
133
• Parathyroidectomy
o Rhinology
• Revision endoscopic sinus surgery
• Orbital decompression
• Repair of CSF leaks
• SPA ligation
o Facial Plastic and Reconstructive Surgery
• Complex facial trauma, such as Le Fort fractures and comminuted mandible and midface fractures
• Functional rhinoplasty
• Repair of post-traumatic and post-ablative defects
Goal #3: Develop systems-based understanding of otolaryngology practice
Resident Objectives:
Demonstrate competence in correctly coding surgical procedures, consultations, and outpatient visits (CPT and ICD -10).
Demonstrate competence in appropriately documenting patient care to support coding levels and to comply with insurance payor regulations (e.g. Medicare).
Demonstrate sense of empathy regarding the barriers that conspire to prevent patients from receiving optimal healthcare (lack of transportation, language barriers, socioeconomic status, cultural differences, education level, family support, etc.)
Continue to develop an understanding of one's own abilities and limitations, and a commitment to life-long learning and improvement, through activities such as case presentation at Morbidity and Mortality conference, including directed literature review and discussion of systems improvements as appropriate.
ACGME Competency Goals
Systems-Based Practice
Professionalism
Systems-Based Practice
Professionalism
Patient Care
Interpersonal and Communication Skills
Professionalism
Practice-Based Learning and Improvement
Professionalism
Systems-Based Practice
134
Stanford Health Care and Lucile Packard Children’s Hospital Night Float Rotation
Rotation Specifics:
1.Night float is on Sunday-Thursday nights from 6 pm to 6 am.
2.All call is in-house.
3.The night float resident will see all consults and take all outside calls which come in after 5pm; be the operative resid ent on any cases which start after 8:00 pm and will begin taking the floor calls once the hand -off from that team has occurred.
4.Beginning at 7:30 pm the night float resident will take over in any running ORs.
Goal 1. Consults. Know how to evaluate and treat inpatient and emergency department consult patients.
Resident Objectives: ACGME Competency Goals
Be the initial contact resident for all consults at SHC and LPCH services including the emergency department.
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Systems-Based Practice
Perform initial evaluation of all consult patients.
Be familiar with the EPIC medical record systems and be able to access information appropriately. Understand the importance of confidentiality in patient medical records.
Consistently demonstrate courtesy when interacting with clinical and non -clinical staff members.
Perform a literature search to learn more about unusual patient problems.
Create a complete and coherent consultation note in a timely fashion.
Utilize translation services to communicate with non-English speaking patients as needed.
Patient Care
Medical Knowledge
Patient Care
Professionalism
Systems-Based Practice
Interpersonal and Communication Skills
Professionalism
Medical Knowledge
Practice-Based Learning and Improvement
Interpersonal and Communication Skills
Professionalism
Interpersonal and Communication Skills
Systems-Based Practice
135
Demonstrate effective time -management skills.
Follow-up on consult patients as needed.
Professionalism
Practice-Based Learning and Improvement
Patient Care
Systems-Based Practice
Professionalism
Goal 2. Hand -offs. Know how to receive and give hand -offs.
Resident Objectives: ACGME Competency Goals
Receive and give hand -offs in a thorough and efficient manner.
Patient Care
Interpersonal and Communication Skills
Professionalism
Demonstrate effectiveness in following up all to -do items communicated through the handoff process.
Patient Care
Goal 3. Patient phone calls. Know how to appropriately communicate with patients via the phone.
Resident Objectives: ACGME Competency Goals
Be able to obtain an appropriate history from patients who call in through the hospital operators.
Be able to direct outside patients appropriately.
Be able to appropriately document patient phone calls in the medical record.
Patient Care
Interpersonal and Communication Skills
Patient Care
Interpersonal and Communication Skills
Patient Care
Systems-Based Practice
Goal 4. Operative experience. Know how to perform surgical procedures in the after business -hours setting.
Resident Objectives: ACGME Competency Goals
Be able to perform procedures which must be done on an urgent basis after normal business hours.
Be able to rapidly learn a patient’s history and step in to assist in surgery which is on -going.
Patient Care
Patient Care
Medical Knowledge
136
OHNS Resident Research Program
Introduction: Protected research time will be allotted to residents throughout the course of their training. As the main focal point of the research program, R3 resident will have one three -month block of dedicated research time to engage in one or more pr ojects. In addition, there will be three-months of half-time research time during the R3 year. Each resident must have a full-time Stanford faculty advisor and may have an additional direct research advisor if the research is performed outside the Otolaryngology department. This rotation is intended to give the resident maximum flexibility regarding the subject matter of the research project. Each resident is expected to publish at least one manuscript in a peer-reviewed journal during their residen cy.
PGY1 / PGY2
During the PGY1 rotations on Otolaryngology and the first few PGY2 rotations, the resident should investigate departmental projects and arrange to meet with at least three Otolaryngology faculty members to discuss possible research project s for the research rotation. The PGY1 residents have a four -week block of Radiology/Research to get to understand the basics of research and to facilitate their exploration of research opportunities. (See the Goals and Objectives for the PGY1 Radiology/Research rotation)
Deadline: January/February of PGY2 year (be prepared to discuss at the time of semiannual meeting with program director.)
After review and discussion, the resident selects a project and with the help of their advisor writes a two -page proposal detailing how the research block will be spent (see below for details). The proposal should be prepared for submission for the American Academy of Otolaryngology – Head & Neck Surgery Foundatio n CORE Grant.
The research proposal should consist of:
▪ Your faculty advisor’s name (must be Stanford full -time faculty). You may have an adjunct clinical faculty member or non -faculty member as your direct research advisor, with the approval of your facu lty advisor. Submit both names, if appropriate.
▪ Written proposal:
o Specific Aims and Significance . What question are you trying to answer and what is the significance of that question?
o Background and Literature Search . Summarize previous relevant work in t he area; demonstrate that you have done your homework with an annotated bibliography and explain how other studies have been lacking.
o Methodology . How do you plan to answer your question or questions? How many animals and what type and how did your choose that animal? What type of lab equipment will you be using? For those studies requiring a clinical chart review, how many char ts
137
Winter
PGY2
do you intend to review, where, and how will you get the charts? What problems do you anticipate and how do you think these can be overcome?
o Data. For all proposals, how will the data be analyzed? What statistical methods will be used?
o Budget . This must be detailed and appropriately justified. Rough estimates are not acceptable.
o Bibliography. PGY3
The R3 will carry out the research proposal submitted during the PGY2 year utilizing the dedicated full-time and half-time research blocks. PGY4/5
During the R4 year , there will be allotted 3-6 weeks of full-time research time to complete projects from the R3 year or work on new projects. The R5 will have one 5-week block of full-time research or elective time.
The goals and objectives of the research program are out lined in the following table.
Competency-based Goals and Objectives: PGY3/4/5 – Research
Goal 1. Be able to construct a plan for research
Resident Objectives: ACGME Competency Goals
Construct a research plan and create a research proposal (including Specific Aims and significance, Background and literature search, methodology, Data analysis plan, Budget, Bibliography). This should be done during the R1 and R2 years.
Complete the mandatory education programs for inve stigators involved in human and/or animal research.
Complete the Human Subjects and/or Animal subjects applications and submit in a timely fashion.
Systems-Based Practice
Professionalism
Systems-Based Practice
Professionalism
Systems-Based Practice
Present your research plan two months before the official research rotation begins. Interpersonal and Communication Skills
Goal 2. Know how to carry out a research project
138
Resident Objectives: ACGME Competency Goals
Complete the data acquisition portion of the research plan.
Demonstrate an ability to adapt the research plan (“troubleshoot”) based on unexpected results or difficulties.
Demonstrate an understanding of the various personnel who contribute to the research process. Coordinate and perform the research through cooperation and respectful communication with all members of the research team.
Demonstrate a commitment to research integrity including the highest ethical standards in gathering, analyzing, and reporting data.
Goal 3. Analysis and dissemination of results of research project
Resident Objectives:
Demonstrate an ability to analyze the data obtained in the research study and understand the statistical methods involved.
Write a manuscript to the specifications of the journal proposed for submission. Revise the manuscript based on commentary from advisory faculty. Submit the manuscript for possible publication.
Present the results of your research at the year -end research symposium. Talks will be 7 minutes long with 3 minutes of Q&A. Residents are expected to present a project at the end of their R2, R3, R4 and R5 years. Presentation at the end of the R2 year d uring the resident research symposium may be a case report.
Present a research project at the Bay Area Resident Research Symposium one time during your residency.
At the completion of the rotation, be able to reflect and describe intra/interpersonal and professional challenges and successes of the research project.
Systems-Based Practice
Professionalism
Interpersonal and Communication Skills
Interpersonal and Communication Skill s
Professionalism
ACGME Competency Goals
Systems-Based Practice
Systems-Based Practice
Interpersonal and Communication Skills
Interpersonal and Communication Skills
Interpersonal and Communication Skills
Practice-Based Learning and Improvement
139
Chief Resident Mini-Fellowship and Elective Rotations
Rotation Contact and Scheduling Details
Rotation Director: C. Kwang Sung, MD, MS
Introduction
The Mini-Fellowship rotation was created in 2021 -2022 as a way for the chief residents to take a deep -dive into a sub-specialty at Stanford prior to graduation and embarking on a fellowship or a comprehensive otolaryngology practice. The chief resident should identify one or two attendings in the chosen sub -specialty to serve as mentors. The resident should plan on sp ending a significant amount of time in clinic, as well as the operating room with the mentor. The rotation is also a chance for exposure to some o f the ancillary specialties or services that might have overlap with the chosen sub -specialty. The resident should plan in advance to spend time with these services for hands-on exposure, such as:
• Neurosurgery
• Neurology
• Plastic Surgery
• Ophthalmology
• Oncology
• Radiation Oncology
• Palliative Care
• Pain Medicine
• Gastroenterology
• Interventional Pulmonology
• Sleep Medicine
• Neuroradiology
• Pathology
• Allergy
• Dermatology
• Endocrinology
• Geriatrics
• Dentistry/Oral Surgery
140
• Audiology
• Speech Language Pathology
The chief resident elective rotation is a 5 -week block that can be utilized for wrapping up research projects or scheduling formal elective rotations, such as medical missions or visiting rotations at other institutions. The maximum amount of time spent aw ay from campus on the elective rotation is 3 weeks since the maximum total time away allowed by the American Board of Otolaryngology –Head & Neck Surgery is 6 weeks per year (including vacation).
The chief resident should submit a written plan for the Mi ni Fellowship and use of the elective/research block at least two months prior to the start of the rotation.
Competency-based Goals and Objectives: PGY5 – Mini-Fellowship and Elective
Goal 1. Gain in-depth knowledge in a sub -specialty
Resident Objectives:
Spend time in clinic and the operating room with a sub -specialty mentor to increase knowledge and learn nuances of the subject matter.
ACGME Competency Goals
Patient Care
Medical Knowledge
Interpersonal and Communication Skills
Professionalism
Systems-Based Practice
Obtain in-person experience with ancillary services and departments related to the chosen sub-specialty.
Patient Care
Medical Knowledge
Practice-Based Learning and Improvement
141
142 22
. Appendices
Appendix A – Conference Dates
Annual Meeting
Feb. 3-7, 2024 Association for Research in Otolaryngology (ARO) –Mid-Winter Meeting
Jan 25-27, 2024 Triological Society: Combined Sections Meeting
May 15-19, 2024
Combined Otolaryngology Spring Meetings (COSM)
CA
IL
9, 2023
June 14, 2024
Stanford OHNS Residency Research Symposium
IL
1, 2024
143
Date Event Location Abstract Due Sept
AAO-HNS
Nashville,
July
30 – Oct. 4, 2023
TN
5, 2023
Anaheim,
June
Chicago,
July
1 – Aug. 1, 2023
Chicago,
July
1 – Oct. 15, 2023
June
Stanford, CA
Appendix B – Key Indicators
Required Minimum Number of Key Indicator Procedures For Graduating Residents
Note: Case logs for 2017 program graduates will be reviewed for compliance with minimum numbers but no citations will be giv en. Residents graduating in 2017 are expected to achieve the required minimum numbers for all Key Indicator Procedures. Achievement of the required minimum numbers is an indicator of experience but is not considered an indicator of competence. Programs should continue to evaluate procedu ral competence in order to ensure that graduates are competent to enter practice without direct supervision.
144
Category Procedure Min # KEY INDICATOR: Head & Neck Parotidectomy (all types) 15 Neck Dissection (all types) 27 Oral Cavity Excision 10 Thyroid/Parathyroidectomy 22 KEY INDICATOR: Otology/Audiology Tympanoplasty (all types) 17 Mastoidectomy (all types) 15 Stapedectomy/Ossiculoplasty 10 KEY INDICATOR: FPRS Rhinoplasty 8 Mandible/Midface Fractures 12 Skin Flaps and Grafts 20 KEY INDICATOR: General/Peds Airway – Pediatric and Adult 20 Congenital Neck Masses 7 Ethmoidectomy 40 Bronchoscopy 22
Appendix C – Handover Evaluation Form
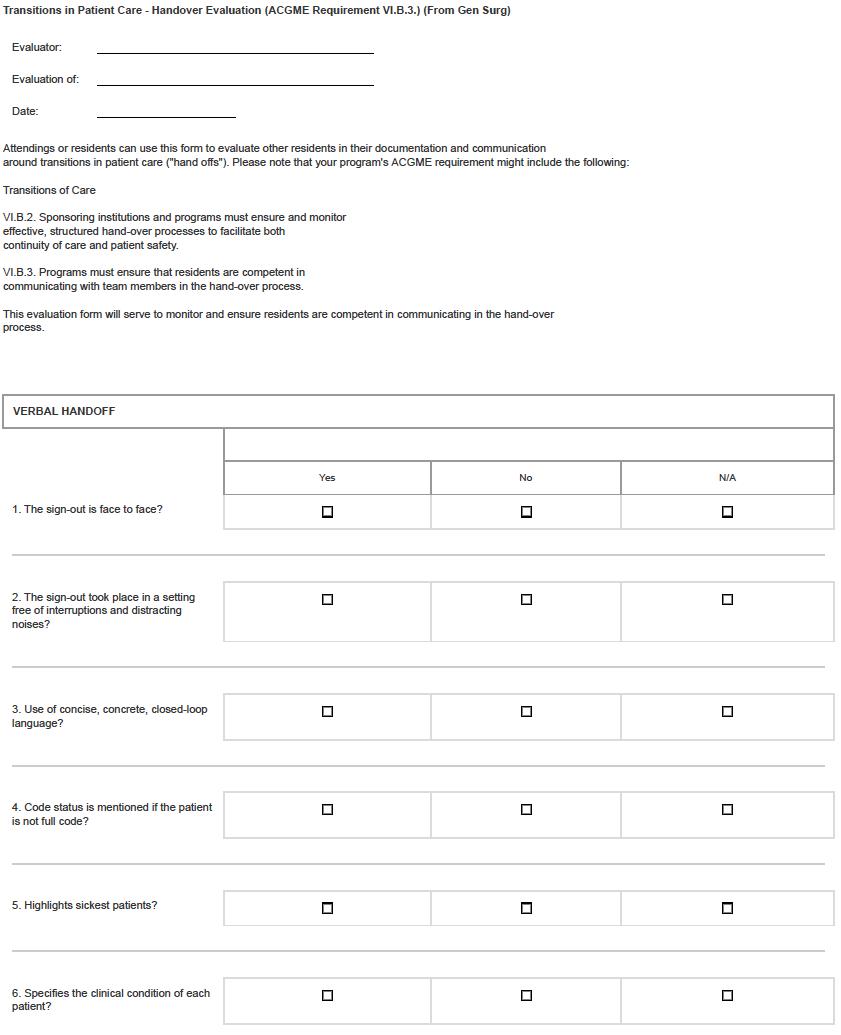
145
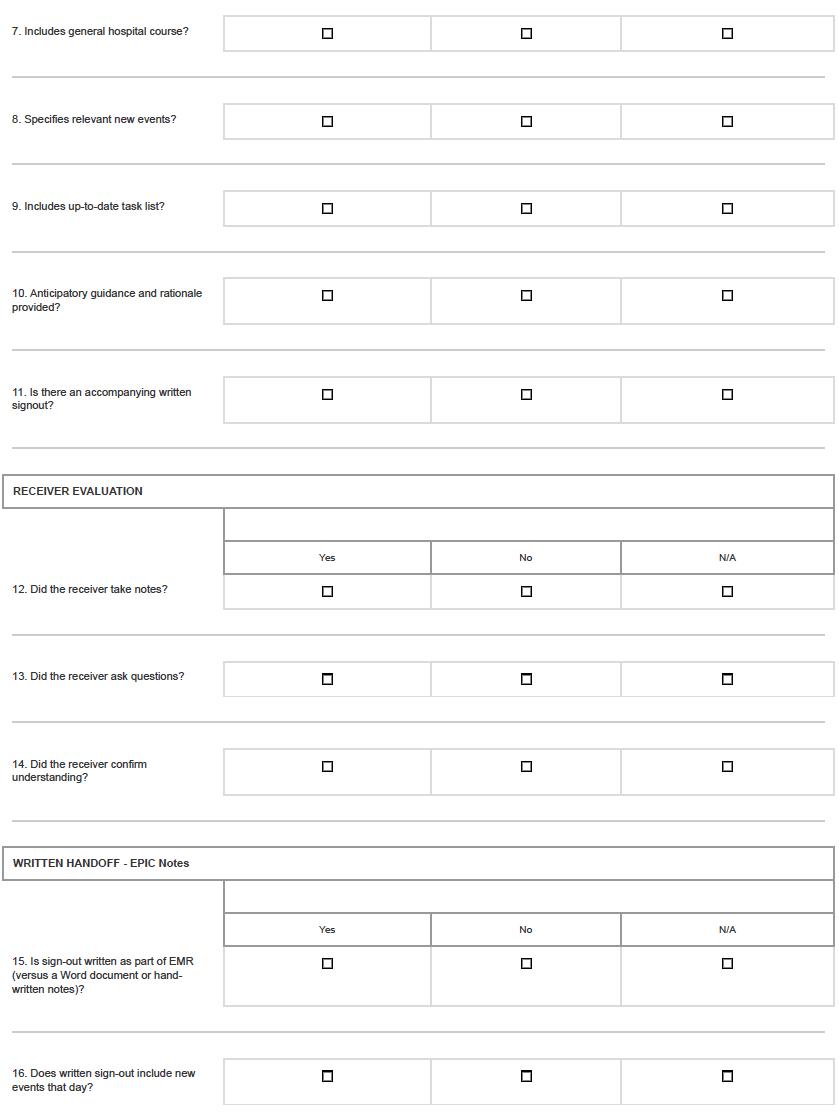
146
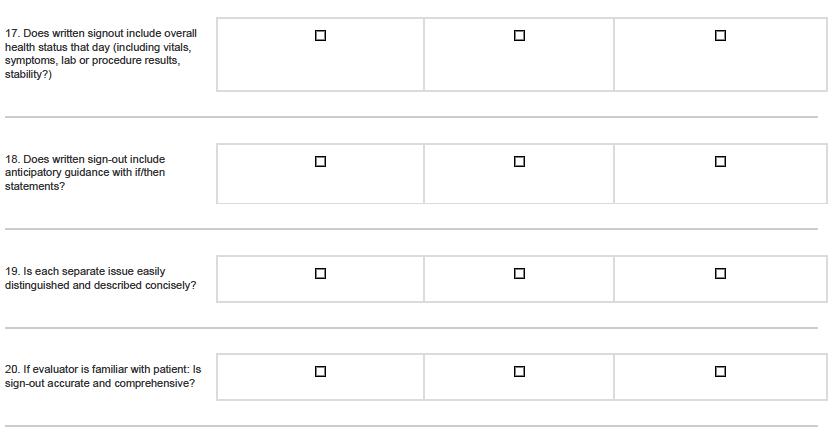
147
Appendix D – Evaluation Form of Faculty by Resident
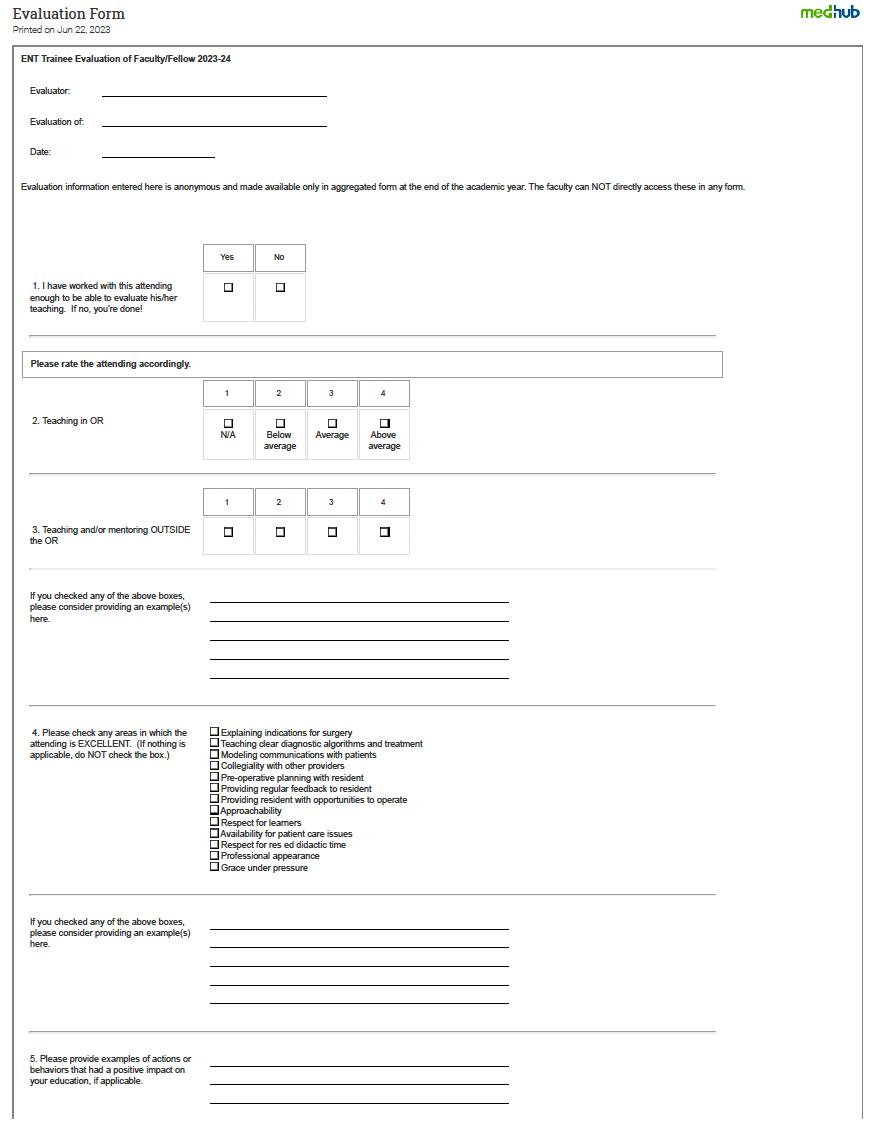
148
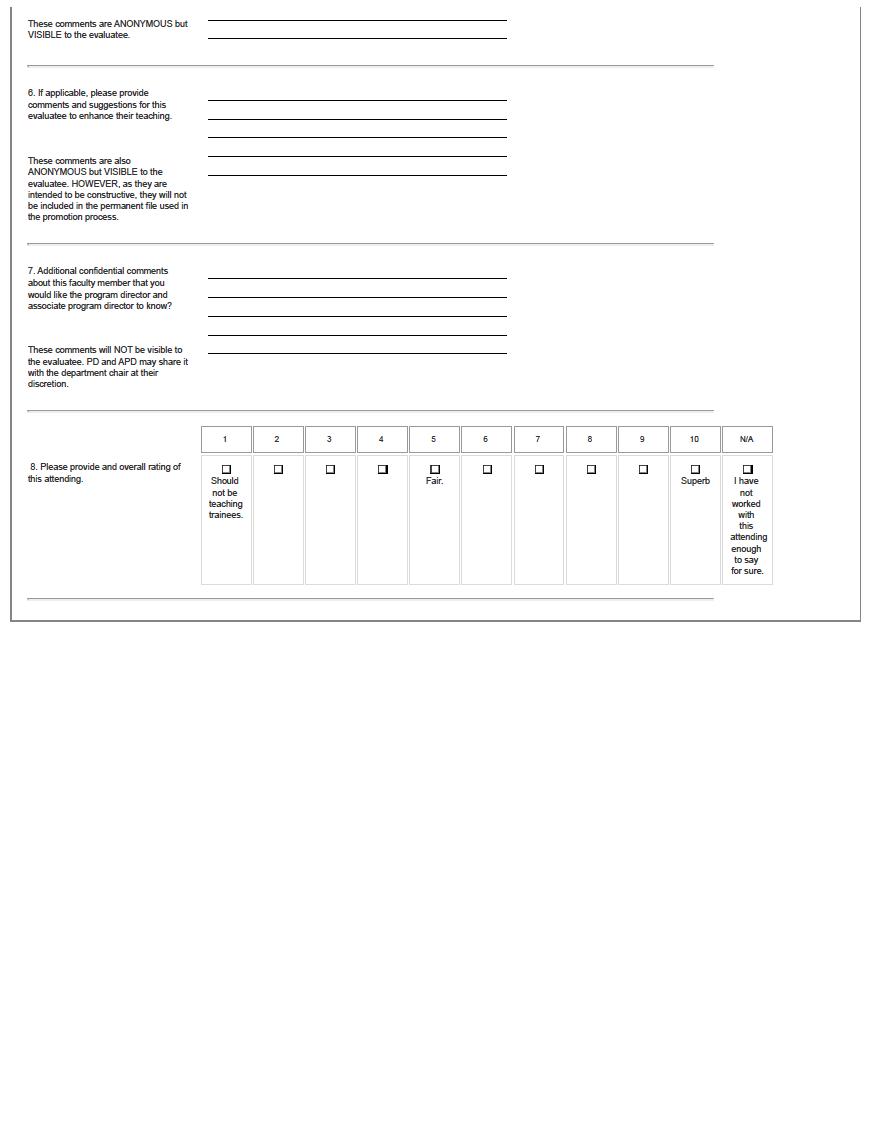
149
150
Appendix E – Evaluation Form of Resident by Faculty
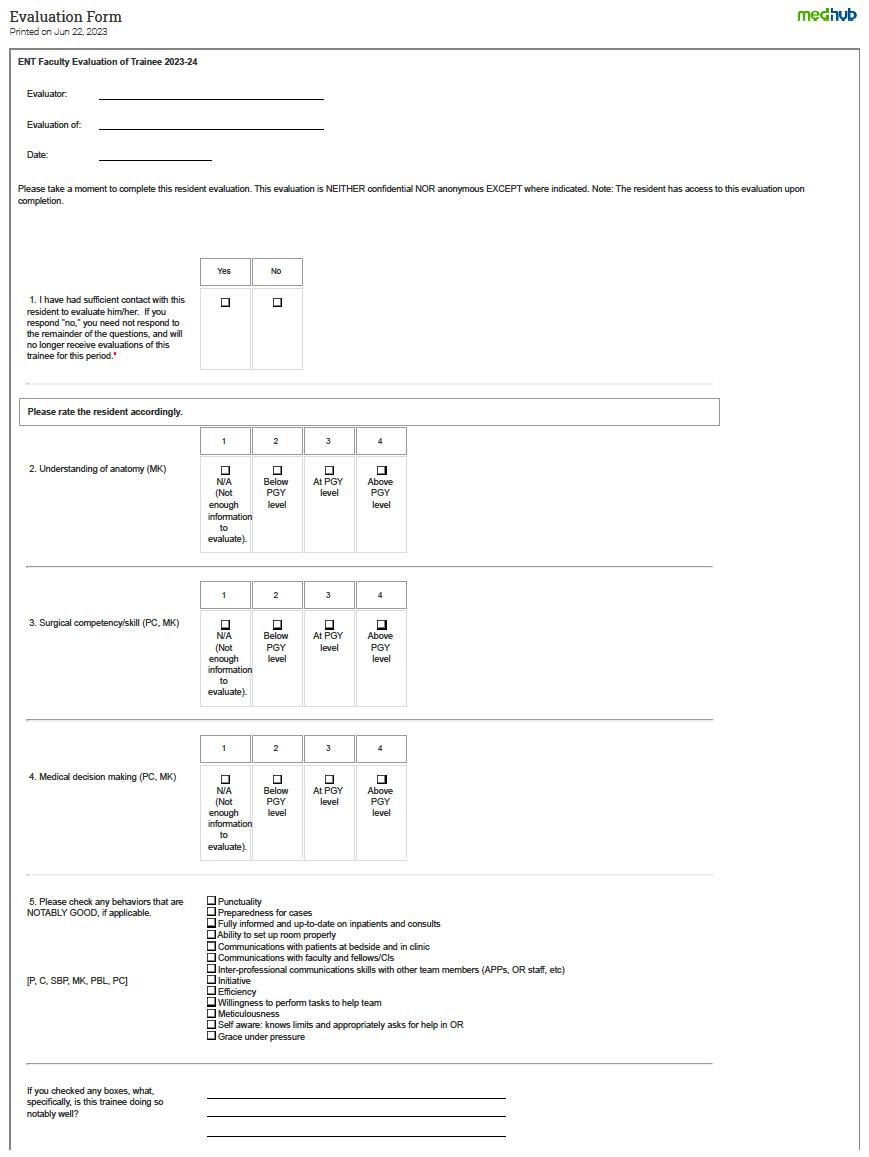
151
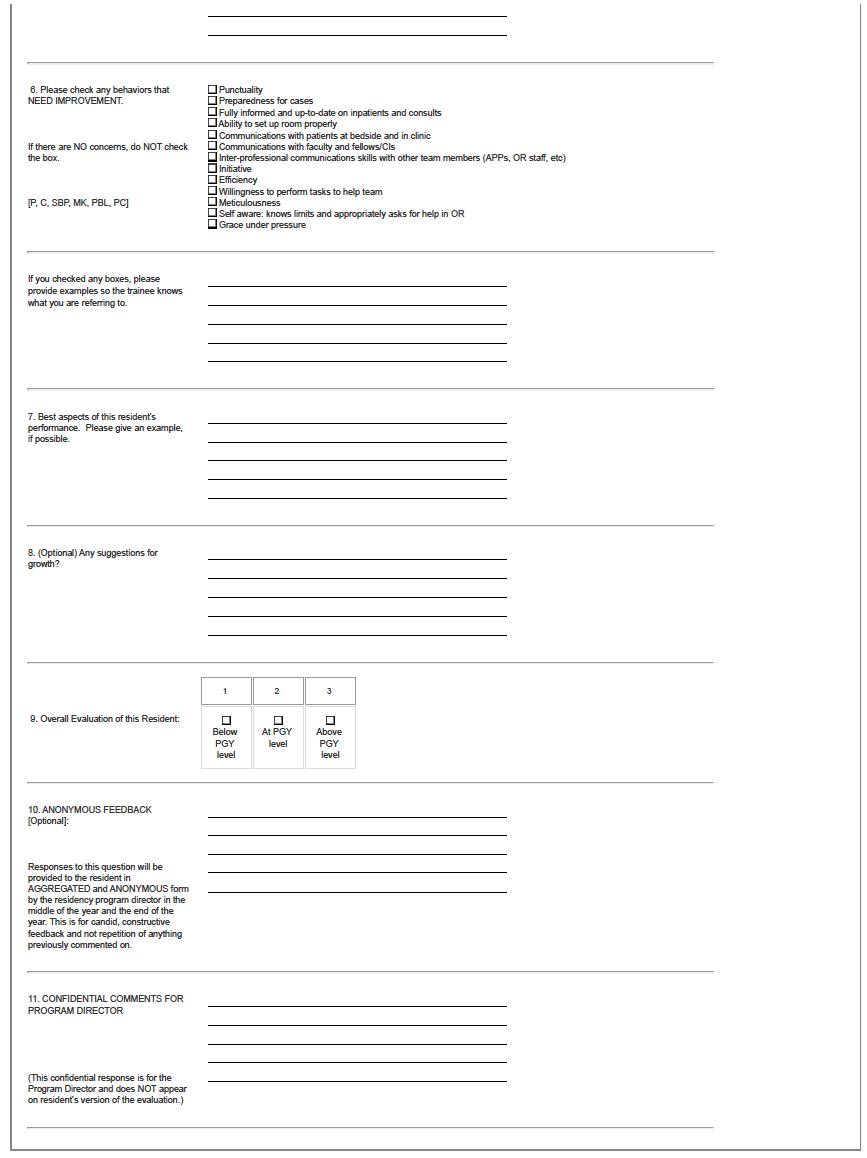
152
153
Appendix F – Evaluation Form of Service/Rotation by Resident
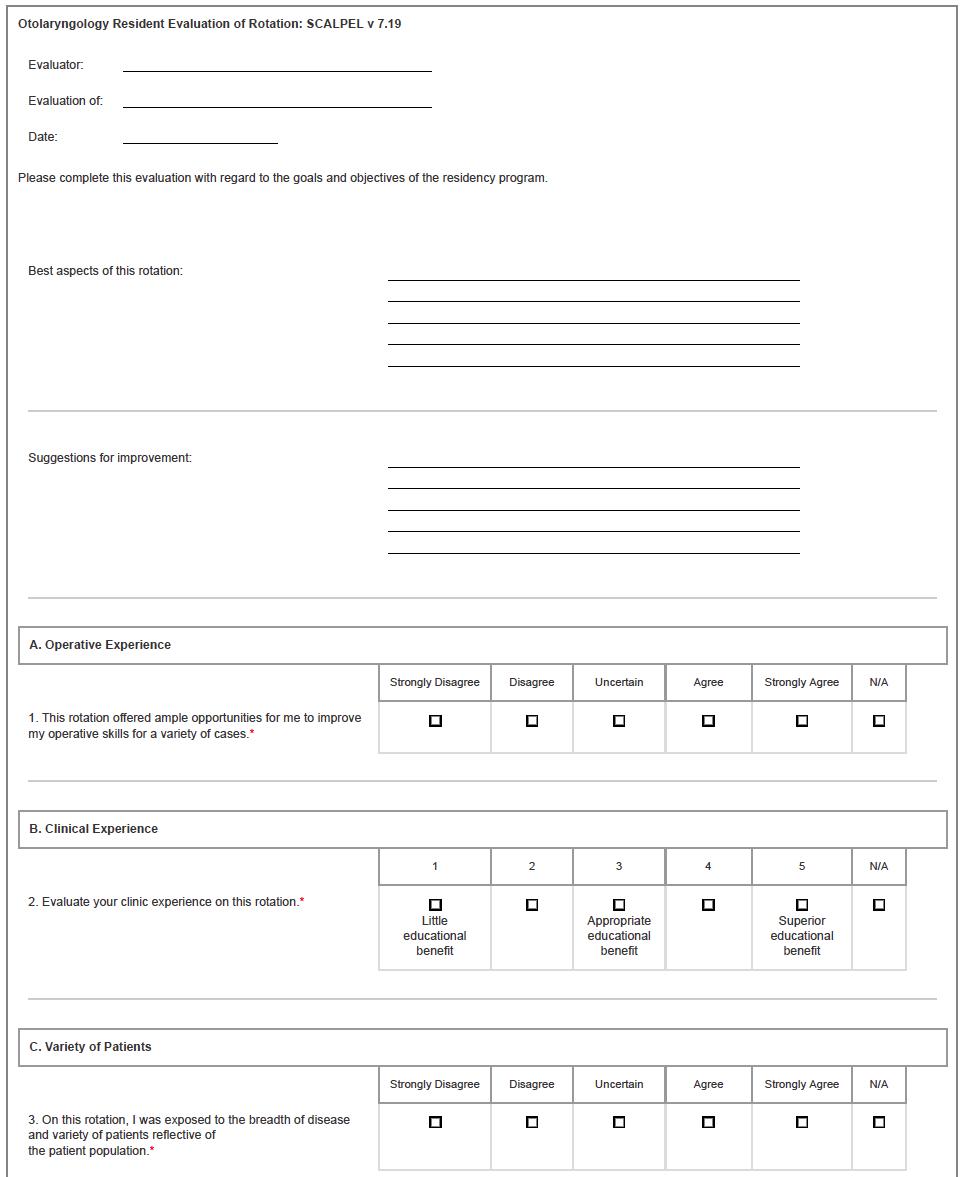
154
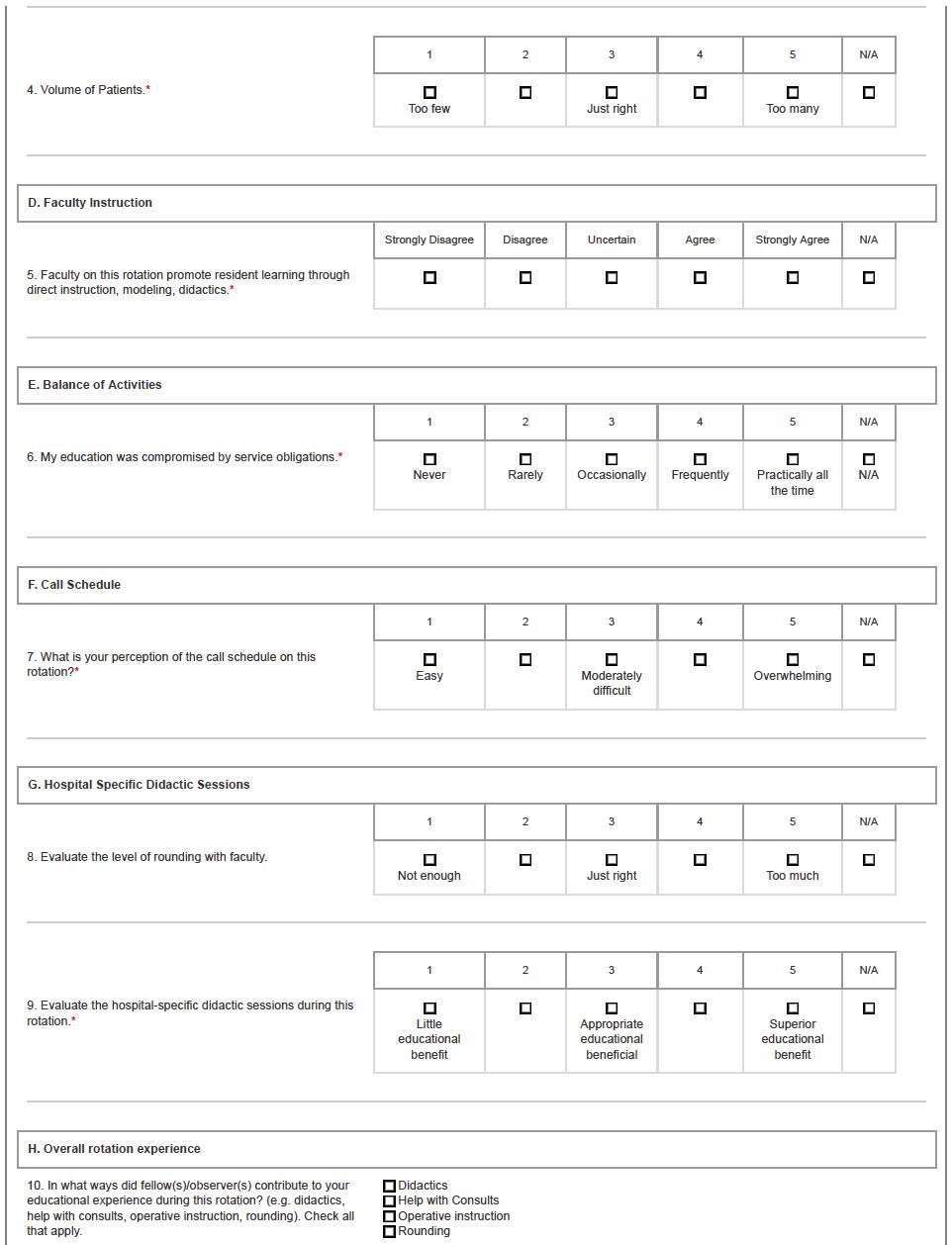
155
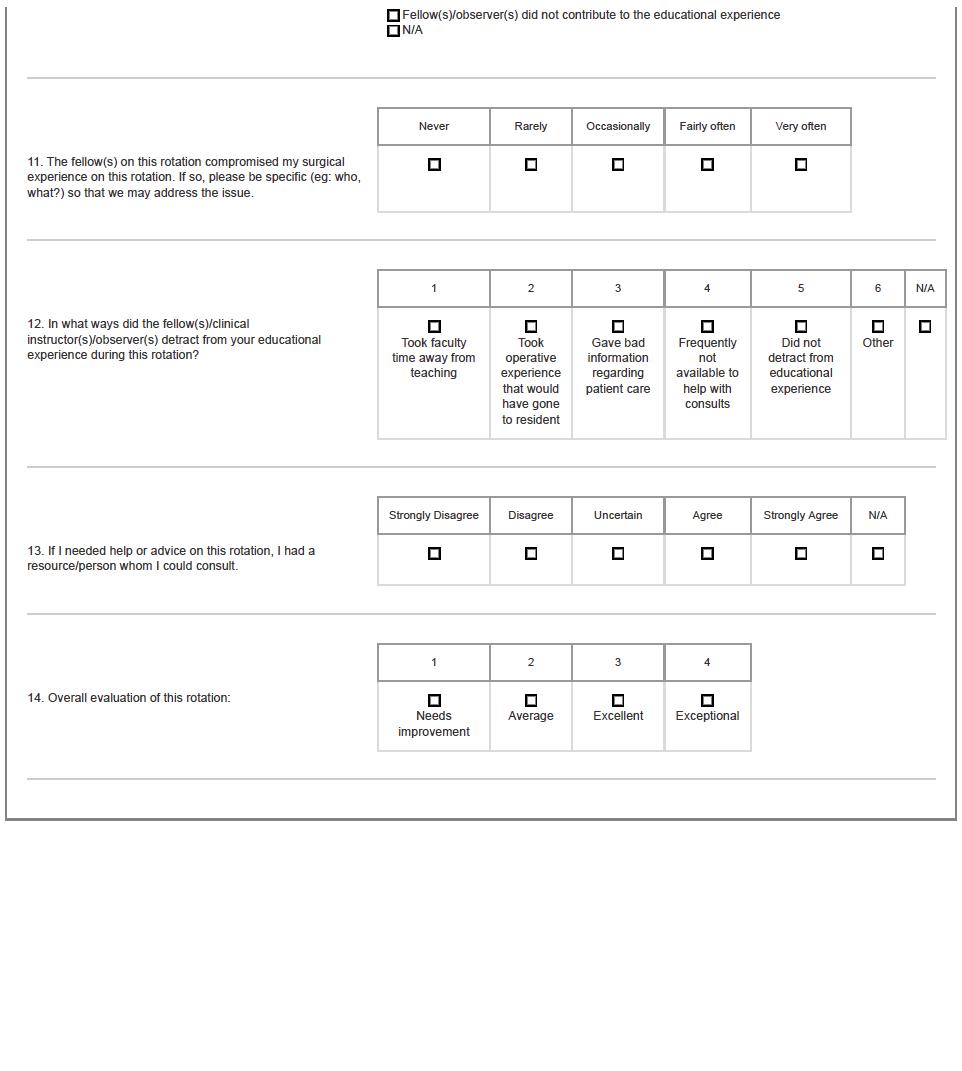
156
Appendix G – Resident Peer Evaluation Form
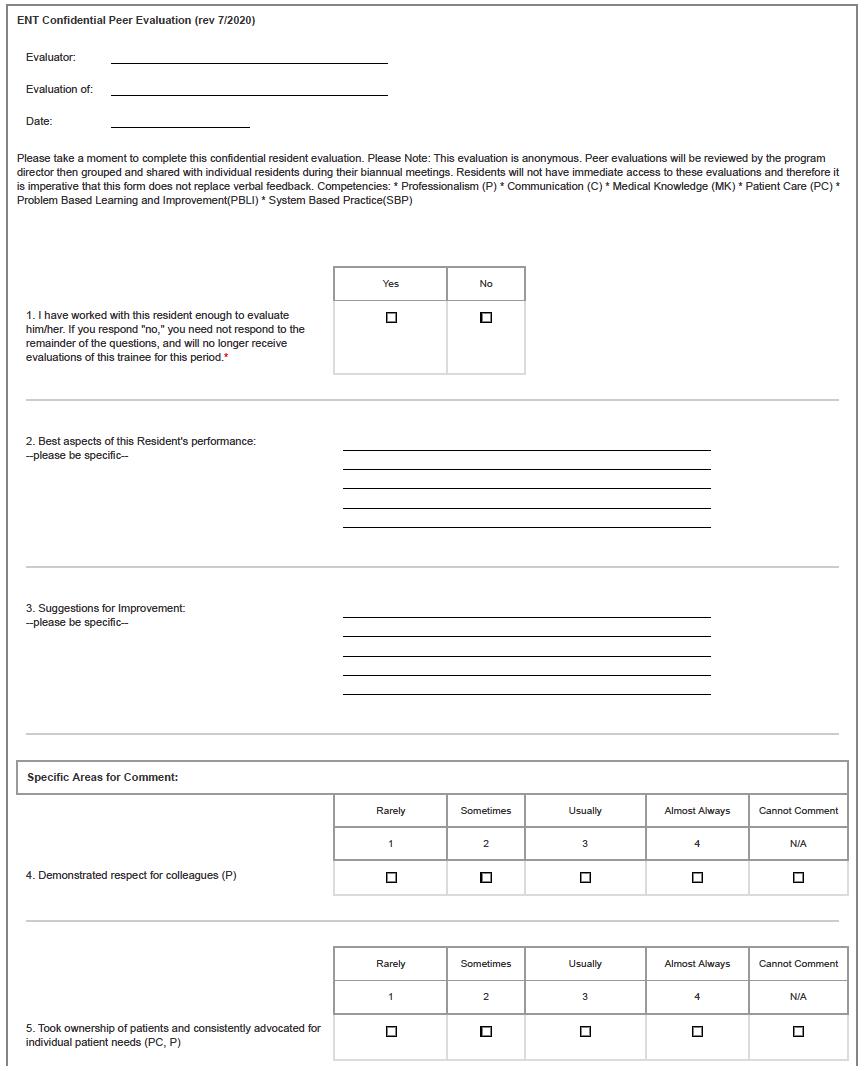
157
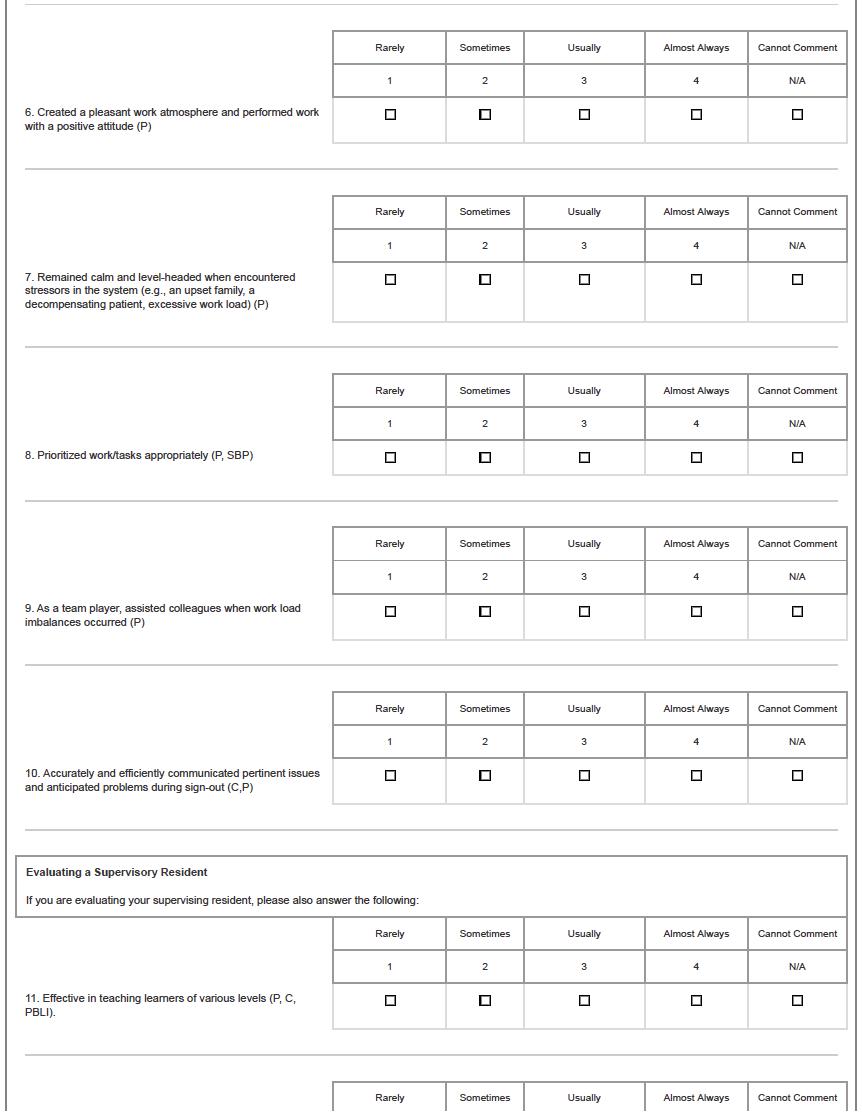
158
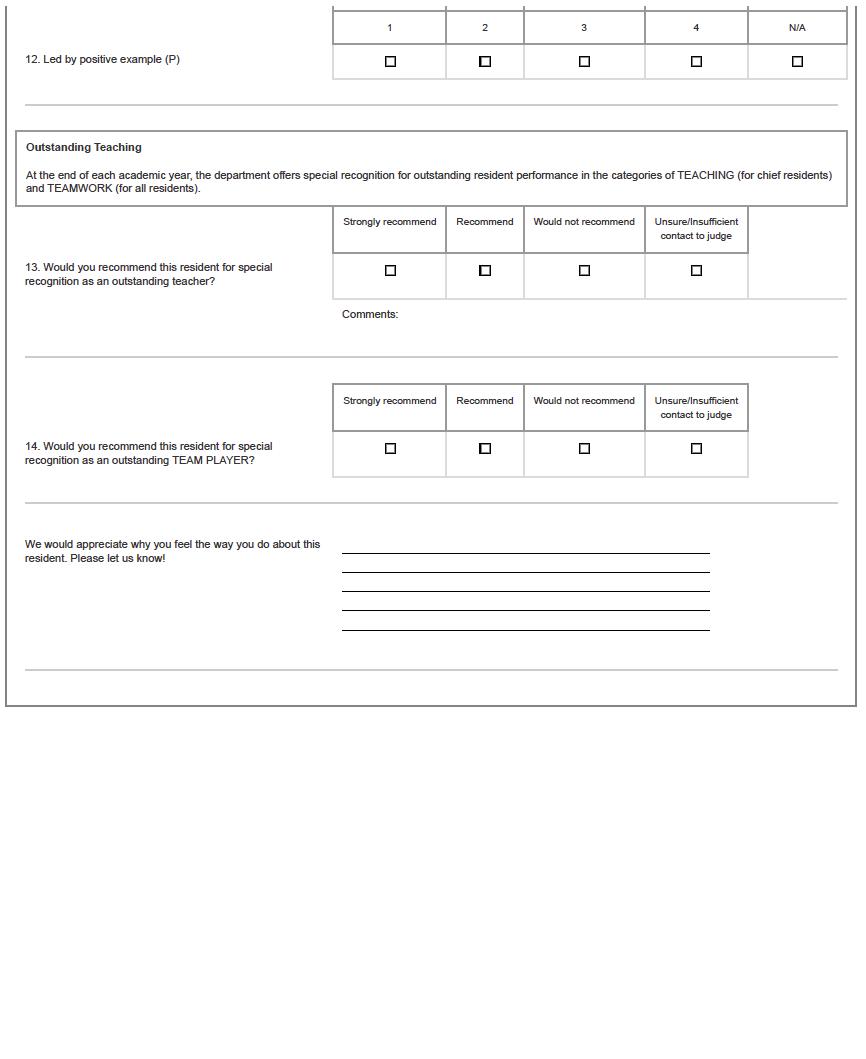
159
Appendix H – Evaluation Form of Resident by Staff
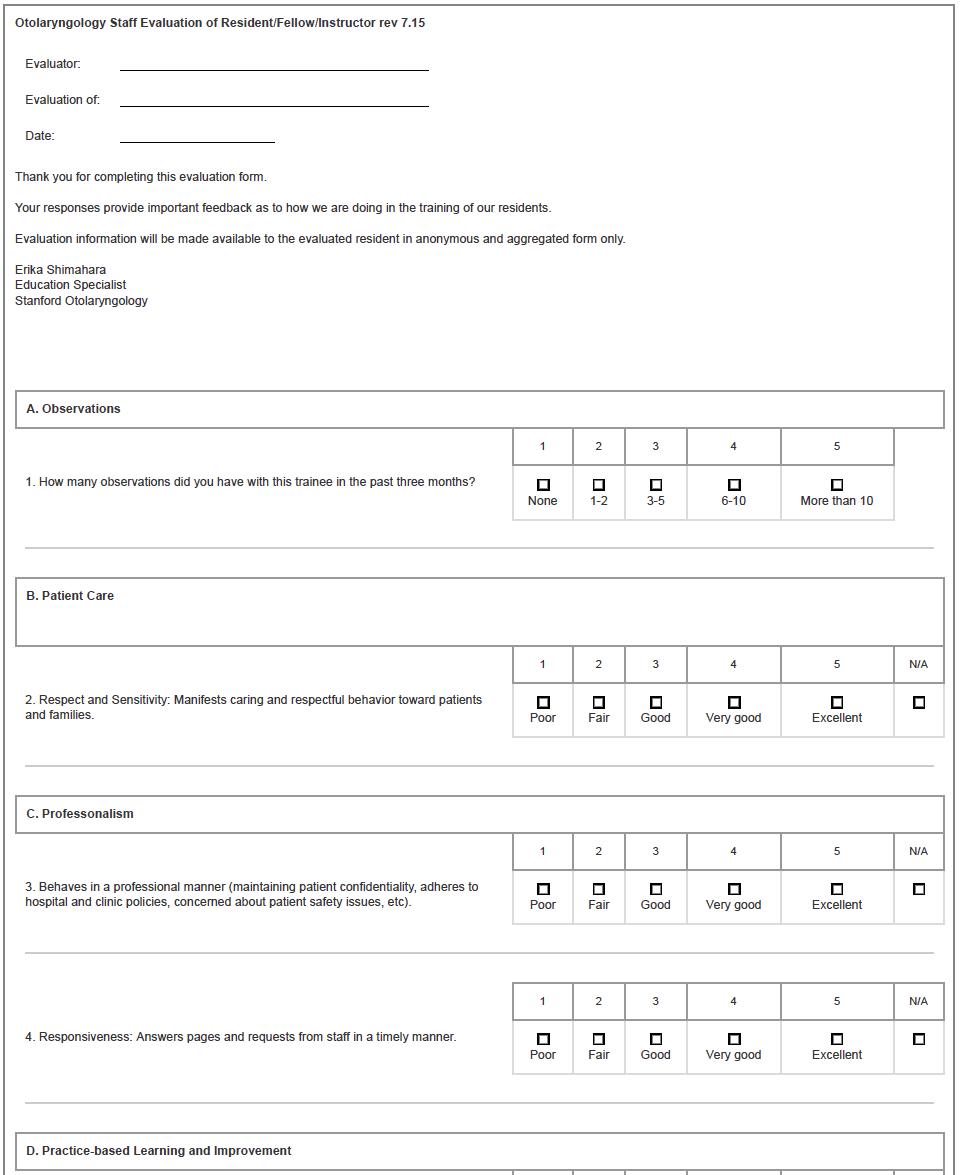
160
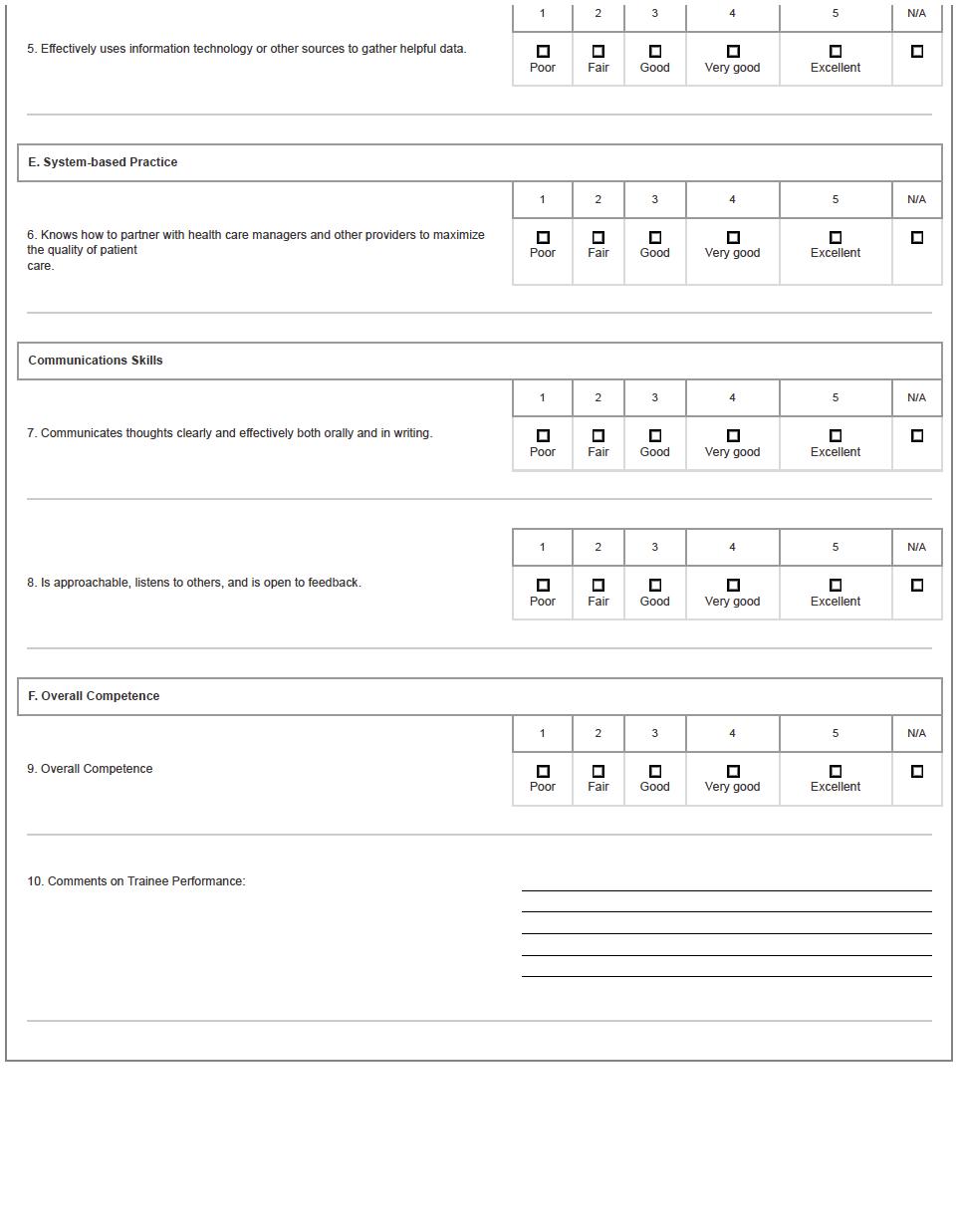
161
Appendix I – Evaluation Form of Resident by Patient

162
163
Appendix J – Otolaryngology Milestones 2.0
Otolaryngology – Head and Neck Surgery Milestones
The Accreditation Council for Graduate Medical Education
Implementation Date: July 1, 2022
Second Revision: July 2021
First Revision: October 2013

164
©2021 Accreditation Council for Graduate Medical Education (ACGME) All rights reserved except the copyright owners grant third parties the right to use the Otolaryngology – Head and Neck Surgery Milestones on a non-exclusive basis for educational purposes
Full document at: https://www.acgme.org/Portals/0/PDFs/Milestones/OtolaryngologyMilestones.pdf
Appendix K – Facial Trauma Call Policy
Craniofacial Trauma & Oral Medicine (Dental) Call Policy Stanford Hospital & Lucile Packard Children’s Hospital
The Plastic Surgery Division and Otolaryngology/Head & Neck Surgery Department provides Stanford Emergency Department call coverage for Maxillofacial Trauma and Dental related problems.
1. Stanford: Otolaryngology (ENT) takes call on even days. Plastics ta kes call on odd days.
a. SCVMC: ENT takes call on odd days. Plastics takes call on even days.
b. VAPA: ENT takes call on even months. Plastics takes call on odd months.
2. Call switches at 6am at SHC.
3. Consult is assigned at the time the service is initially paged (not when the patient arrives in the ER/ICU or when the resident answers the page).
4. DAYTIME Oral Medicine & Maxillofacial Surgery Consults: The service will see all dental/OMFS consults during normal business hours (8a -5p, M-F); the plastics/ENT resident should direct referrals and calls to OMFS during this time. The smartpage schedule designates the daytime dental resident (if available) and dental attending with contact information.
5. NIGHTIME Regarding dental trauma (tooth luxations/avul sions with isolated alveolar bone fractures) or odontogenic infections: the ED should consult smart page to determine if a dental resident is on call (dental resident is on call approximately 20% of the time.) If no dental resident is on call then the de signated plastic surgery or ENT resident should be paged. The back-up attending dentist will be contacted by the Plastic Surgery/ENT/Dental designated resident as needed for consultation.
6. On their designated call days, ENT or Plastics will consult for c utaneous facial infections, TMJ dislocations, and ear lacerations. Plastics may defer to ENT for facial infections that are salivary gland, sinus- or ear-related.
7. Non-surgical infection admissions may be admitted to Internal Medicine, and ENT or Plastics will follow as needed. If internal medicine will not admit the patient with an infection of dental or possible dental origin then the patient should be admitted to the ENT or Plastic surgery service who is on for craniofacial trauma/dental for that day.
8. ENT is to see all deep space infections, ear hematomas, and temporal bone trauma. If a temporal bone trauma patient has other facial trauma and Plastics is on call, then Plastics is to address the other facial trauma.
9. ENT or Plastics may repair eyelid lace rations or retain the option to consult Ophthalmology for complex eyelid lacerations.
165
10. Consults that can be safely managed as an outpatient: nasal fractures (open or closed), mandible fractures (without airway concern), orbital floor fractures without entr apment or vision changes, maxillary sinus fractures. If patients are admitted for another reason with these injuries they can be seen on a non-urgent basis during the day.
11. If the ER or the patient has a specific request for Plastic Surgery and it is an EV EN day (ENT); or if there is a specific request for ENT on an ODD day (plastic surgery) the resident who is called can respond by indicating that the other service is on -call for facial trauma; Facial plastic surgery is included within the ENT call coverag e. HOWEVER, if the ER or patient specifically requests/insists that the nature of the problem requires a specific service (even though that service is not officially on call that day) then you should be available to see the patient, regardless.
12. ORBITAL FLOOR FRACTURES:
a. Days 1-10 of month:
i. For isolated orbital floor fractures (ie., no other facial trauma issues): oculoplastics will be the lead team for repair of orbit fractures - no need to involve plastics or ENT.
ii. For orbital floor fractures with other facia l trauma: ENT/Plastics will be the lead team for other facial trauma and will coordinate the care of the floor fracture with Ophthalmology. In these cases, Ophthalmology will be responsible for the orbital floor fracture and any repair will be performed a s a joint case.
b. Days 11-month end: ENT and plastics will be the lead team on any orbit fracture with ophthalmology help to clear the globe. If there is ocular compromise (globe not cleared) the patient will be managed by Ophthalmology and the orbital floo r fracture repair will be decided after the eye pathology is appropriately addressed. Orbital floor fractures should be referred to the ENT and plastics services, while Ophthalmology consults are obtained for vision and globe assessment only.
Rev
166
April 2018
Appendix L – Medicine/ENT/FACE/ED Inter-Service Agreement
Medicine/ENT/FACE/ED Inter-Service Agreement
(Effective September 2019)
Admissions
Patients with an ENT/FACE issue will be admitted to ENT/FACE, UNLESS the patient has one of the following medical conditions, in which case they will be admitted to a medical service: 1,2,3,4,5
1. Acute chest pain or EKG/enzyme evidence of ischemia (including troponin above upper limit of normal)
2. Dyspnea, or signs/symptoms of pulmonary edema, or >2 liter new O2 requirement (If these signs or symptoms are due to an upper airway obstruction then admit to ENT)
3. Decompensated Heart Failure
4. Uncontrolled arrhythmia or new arrhythmia with persistent/recurrent HR >110
5. DKA
6. Severe valve disease
7. EF <30% on most recent ECHO
8. Sepsis or any complicated active infections (e.g. diverticulitis or pneumonia but not bronchitis or uncomplicated UTI) Infections of the Ear/Mastoid/Nose/Throat/Epiglottis with sepsis would be admitted to ENT with medicine or ID consult if needed.
9. Acute kidney injury
10. Persistent/Recurrent systolic BP >180 or diastolic >100
11. Persistent/Recurrent systolic BP < 90 despite appropriate fluid challenge (ICU consult recommended)
12. Any signs of active internal bleeding (Except epistaxis alone would b e admitted to ENT. Epistaxis due to hematologic disorder would be admitted to Heme.)
13. Acute alcohol intoxication with significant behavioral disturbance or acute alcohol withdrawal
14. Decompensated liver disease including any of: hepatic encephalopathy, INR >1 .7, new onset jaundice
15. Focal central neurologic changes including stroke and TIA (admit to neurology)
1 Admitting medical service is dependent on active medical issues (e.g., decompensated heart failure to CCU/CSU instead of gene ral medicine) and will be determined as per the ED Admissions Grid
2 Patients with an active issue that is more appropriate for a non-ENT/FACE/medicine service will be admitted as per the ED Admission Grid (e.g., a patient with facial cellulitis, elevated creatinine, and acute appendicitis would go to general surgery).
3 Uncertainty regarding the appropriate primary admitting team should be resolved through a discussion between the otolaryngology/medicine admitting residents. If after discussion uncertainty persists, it should be resolved through an attending to attending discussion initiated by the service initially called by the ED for admission. (ED Decides on admit service; if a different service is felt to be more appropriate then a transfer to that service can be do ne per the workflow in this agreement after the admi t order)
4 Patients with invasive fungal sinusitis will be admitted to the medicine service with otolaryngology consulting.
5 Patients requiring direct admission after an elective otolaryngology surgery or directly from otolaryngology clinic are subject to this agreement.
167
16. Patients currently on hospice or requiring comfort care who will be managed nonoperatively
17. Patients in need of vulnerable adult or elder abuse evaluation
Consults
1. If the SCM hospitalist is consulted on a patient admitted to the otolaryngology service, they will see the patient within 3 hours (if called STAT within 1 hour).
2. For patients followed by the SCM hospitalist service, the SCM hospitalist will be paged directly regarding medical issues from 8 AM -5 PM. After 5PM, the 1st page for medical issues is to the otolaryngology resident on call, who after evaluating the patient ma y then contact the on-call SCM hospitalist (p24311). The SCM hospitalist may contact the in house nocturnist (N1; p12012) to perform bedside evaluation/treatment as necessary. If acute medical issues will require frequent monitoring/treatment decisions t hen a transfer request should be considered (see below Transfer Requests).
3. The consulted SCM hospitalist will write daily notes and orders for evaluation and management of medical issues (e.g., labs, medications, etc.). Notes will include full risk stratification for intra-operative intervention and will recommend additional consults when appropriate.
4. For non-emergent medical issues that develop overnight (5pm – 7am) in patients known to the SCM hospitalist, the on call SCM hospitalist will contact the in house nocturnist to perform evaluation/treatment. If non -emergent acute medical issues will require frequent monitoring/treatment decisions than a transfer request should be considered (see below Transfer Requests).
5. For non-emergent after hours (5pm – 7 am) consults on patients not followed by the SCM hospitalist, the otolaryngology resident should contact the on-call medicine consult resident (p27111) who then staffs the consult with the on -call SCM hospitalist.
6. For emergent medical issues, the ICU fellow should be contacted directly.
Otolaryngology Consult Role
1. If otolaryngology is consulted on a pat ient admitted to a medical service, they will see the patient within that day (if called STAT for an airway, they will be seen immediately).
2. Otolaryngology consults will write daily notes and will write recommendations pertaining to evaluation of the chief concern, anesthesia evaluation, OR scheduling, NPO status, equipment orders, PT/OT, perioperative antibiotics, wound care, and activity level.
Transfer Requests
From Otolaryngology to a Medical Service
168
Surgical Co-Management Hospitalist/Nocturnist/Medicine Resident Consult Role
1. Patients on the otolaryngology service should be co nsidered for transfer to a medical service if:
i. Any of the above criteria used to determine appropriate admission service develop.
ii. Other active medical issues that supersede active otolaryngology issues that cannot be reasonably/safely managed by the SCM Ho spitalist/Nocturnist develop.
2. For non-urgent transfer requests, the decision to request transfer should be discussed with the consulted SCM hospitalist prior to the request.
3. The on call chief medicine resident reviews/approves transfer requests to the gene ral medicine service. Transfer requests to sub -specialty medical services (e.g., general cardiology and CCU/CSU) are reviewed/approved by the respective service attending.
From a Medical Service to Otolaryngology
1. Patients whose medical issues are stable should be considered for transfer to the otolaryngology service in the post-operative period.
2. Patients originally admitted to the otolaryngology service, who were transferred to a medical service for an active medical issue, should be considered for transfer back to the otolaryngology service after stabilization of the medical issue.
3. Patients transferring from the medicine service to the otolaryngology service are expected to be verbally signed out to the SCM hospitalist at the time of transfer.
4. For patients transferred from the ICU overnight, the nocturnist (N1; p12012) should be contacted to physically see the patient and determine stability for transfer to otolaryngology.
Emergency Department Role
1. The Emergency department (ED) will page the approp riate admission service based on the above criteria.
2. The ED will not determine the appropriate admission service until an adequate workup is obtained to assess for the above criteria.
3. The service initially paged by the ED is responsible for admitting the patient if the above process has been followed .
Neera Ahuja, MD Program Director, Otolaryngology Medical Director, General Inpatient Medicine
C.Kwang Sung, MD
Sam Shen, MD Medical Director, Adult Emergency Medicine
169
Appendix M – Afterhours Outpatient Medical Advice
• PGY1s are not to take this type of call.
• Patients must receive a call back within 30 minutes of their contacting the hospital.
• If the resident does not respond or is unable to handle the call promptly (e.g., scrubbed in surgery) then the call goes to the attending physician on call (2nd call); after that the Clinic Chief/Division Chief (3rd call).
• Any medical advice given during these calls must be documented in E PIC.
170
Appendix N – Paging System
Effective June 2021
1.SmartPage now shows our 3 adult floor pagers (#27082 , #27083 and #27085) as separate entries. (This should hopefully minimize the number of errant floor and consult pages going to the wrong intern.)
2.Based on resident feedback, a second Peds pager number has been added to distinguish between floor and consults.
#25668 will remain the pager ID for floor issues and existing consults
#25670 is the new pager ID for new consults and STAT airways. This will also be the pager that gets outpatient phone calls.
The overnight resident should take the two consult pagers: #27087 for ad ults and #25670 for Peds — at 6:00 pm. The Peds floor pager (#25668) can remain assigned to the day team until they are ready to sign out.
171
Appendix O – Verbal Orders Process Clarifications for Nurses and Physicians
Verbal Orders Process Clarifications for Nurses and Physicians (Attendings & Housestaff)
Verbal orders (VOs) have an inherent degree of risk of error. While VOs are sometimes needed, it is important that the process build in safeguards to reduce risk. Optimal verbal order proc esses are built on mutual trust and respect between nurses and physicians. A collaborative process with built in checks and precautions is important.
VOs should be limited to urgent situations where immediate entry of orders into Epic is not feasible.
MD RN
When to use:
• Should use sound judgment about whether it is impractical (per policy) to enter order into Epic. (e.g., in a procedure, tied up in an emergency, on call out of hospital.)
• NOT for simple convenience
• Explain why a VO is needed.
Remain on the phone long enough for “read back” to be completed
Epic generated alerts may result in page back to clarify
Verbal Orders should not be used for:
• Blood transfusions (Type and hold and Massive Blood Transfusion Protocol OK)
• New PCA order
• Admission orders
• Order sets
• Chemotherapeutic agents
Use safety practices when giving order:
• Double ID of patient: name, MR#
• All parts of drug order (name, form, dose, frequency, route, duration)
• Spell out names of drugs
• Say units, not abbreviations (e.g., milligrams, not mgs)
Will accept verbal order in good faith that there is compliance with the Hospital policy/procedure.
Always perform a “read back”
Enter order into Epic as soon as possible; clarify any Epic generated questions with MD
Verbal Orders should not be used for:
• Blood transfusions (Type and hold, MTP OK)
• New PCA order
• Admission orders
• Order sets
• Chemotherapeutic agents
Use safety practices with “read-back”:
• Double ID of patient: name, MR#
• All parts of drug order (name, form, dose, frequency, route, duration)
• Spell out names of drugs
• Say units, not abbreviation (e.g., milligrams, not mgs)
172
• Say number digits (e.g., “fifty” becomes “Fifty - five zero”)
• Avoid abbreviations (e.g., every six hours - not q6 hours)
All VOs must be cosigned:
• Cosign within 48 hours – best on same day
• Team member should sign if MD off service, or otherwise not available
Education by MD leaders:
• When VO appropriate
• Name & SID required
• Read back required
• Orders not allowed as verbal
• Safety practices
• Cosign w/in 48 hours; same day cosign is best practice
• Any member of team should cosign
• Use caution to avoid errors
Cosign compliance management:
• Regular data reports at specialty and individual level
• Physician leaders/program directors improvement strategies
V6 10/19/18
• Say number digits (e.g., “fifty” becomes “fifty - five zero”)
• Avoid abbreviations (e.g., every six hours - not q6 hours)
Education by RN leaders:
• Name & SID required
• Perform read back
• Orders not allowed as verbal
• Safety practices
• Only if immediate need
• Use caution to avoid errors
Cosign compliance management:
• Not RN management responsibility
(This table does not apply to pharmacists who have their own standard work.)
These changes were created by a joint GME, nursing and physician work group with pharmacy input:
Neera Ahuja, MD, Hospital Medicine Division Chief
Gretchen Brown, RN, Nursing Director
Janjri Desai, PharmD, Assist Dir Pharmacy
Sharron Hampton, RN, Nursing Director
Joe Hopkins, MD, Assoc CMO
Larry Katznelson, MD, Assoc Dean GME
Marc Melcher, MD, General Surgery Residency Program Director
Elisa Nguyen, RN, PCM G1 – H1
Topher Sharp, MD, CMIO
Julie Tisnado, RN, Nursing Director
Hirut Truneh, RN, Nursing Director
173
Appendix P – Temporal Bone Lab
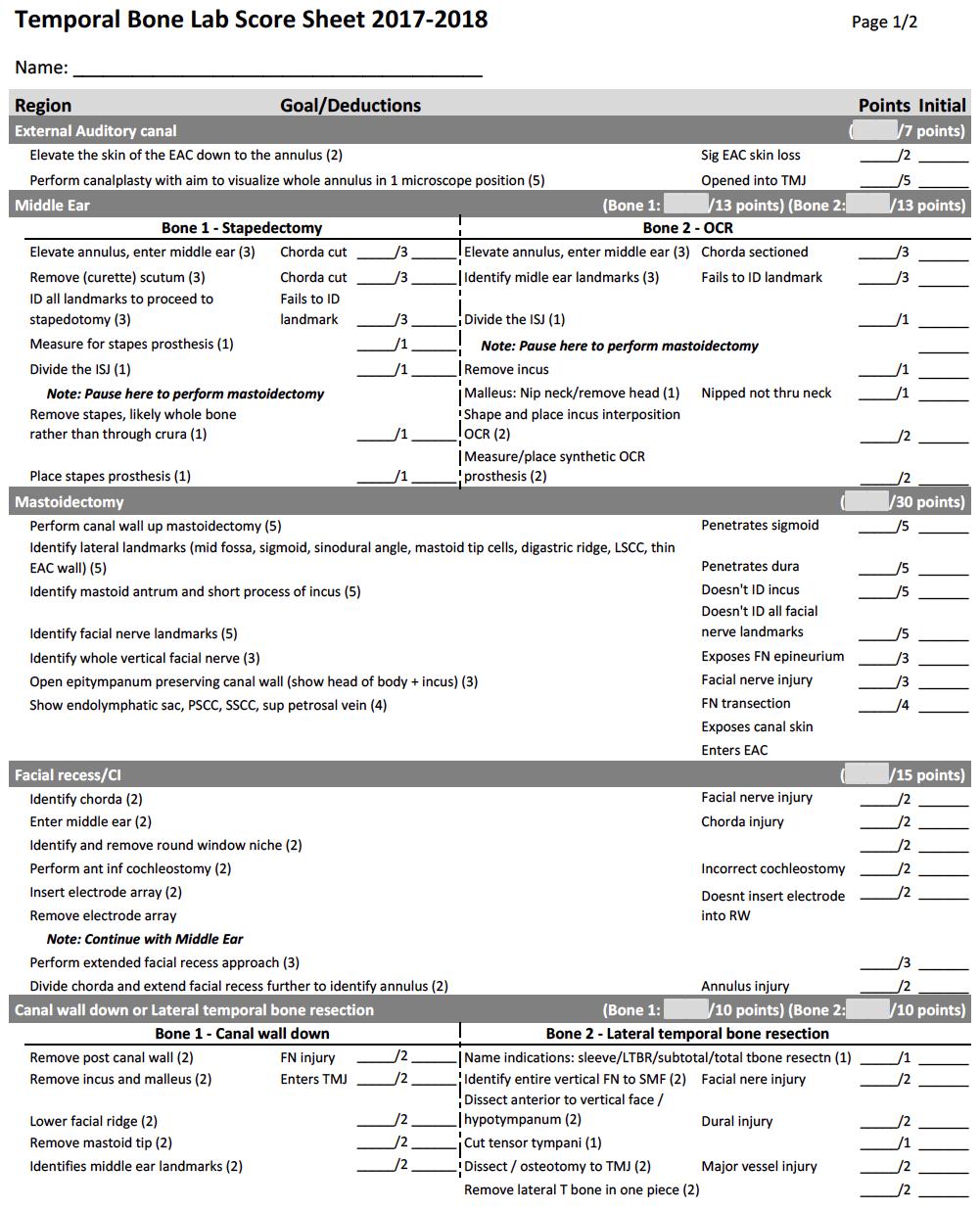
174
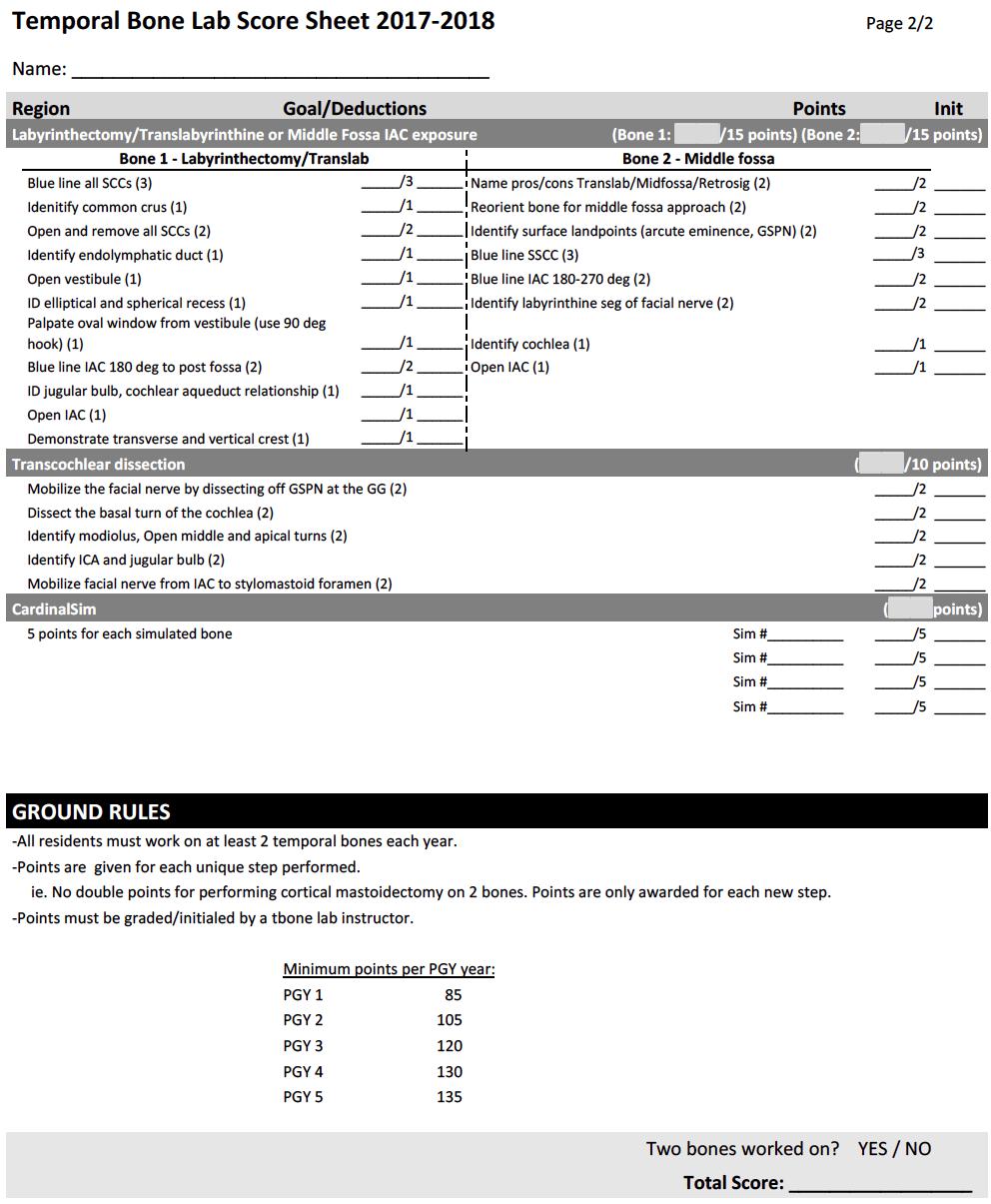
175
Appendix Q – SHC Infection Control
Goals and Objectives for SHC Infection Prevention and Control Department
1. Understand and perform necessary precleaning of used ENT endoscopes prior to reprocessing by Sterile Processing Department (SPD) or disposal
(https://stanfordhealthcare.policytech.com/dotNet/documents/?docid=13566 )
2. Follow Stanford Healthcare Infection Prevention and Control ‘ Quick Reference Guide for Infectious Diseases Conditions and Required Precautions’ when providing care to both inpatient and ambulatory care patients
(https://stanfordhealthcare.policytech.com/dotNet/documents/?docid=10907 )
176