HEALTH, LIFE & HIV
HIV Is Not a Crime
The Sero Project marks 10 years of advocacy



A SMART+STRONG PUBLICATION MARCH 2023 POZ.COM $3.99
Tami Haught (left) and Kamaria Laffrey
IMPORTANT FACTS FOR BIKTARVY®
This is only a brief summary of important information about BIKTARVY and does not replace talking to your healthcare provider about your condition and your treatment.






MOST IMPORTANT INFORMATION ABOUT BIKTARVY
BIKTARVY may cause serious side effects, including:
` Worsening of hepatitis B (HBV) infection. Your healthcare provider will test you for HBV. If you have both HIV-1 and HBV, your HBV may suddenly get worse if you stop taking BIKTARVY. Do not stop taking BIKTARVY without first talking to your healthcare provider, as they will need to check your health regularly for several months, and may give you HBV medicine.
ABOUT BIKTARVY

BIKTARVY is a complete, 1-pill, once-a-day prescription medicine used to treat HIV-1 in adults and children who weigh at least 55 pounds. It can either be used in people who have never taken HIV-1 medicines before, or people who are replacing their current HIV-1 medicines and whose healthcare provider determines they meet certain requirements.
BIKTARVY does not cure HIV-1 or AIDS. HIV-1 is the virus that causes AIDS.
Do NOT take BIKTARVY if you also take a medicine that contains:
` dofetilide






` rifampin



` any other medicines to treat HIV-1
BEFORE TAKING BIKTARVY
Tell your healthcare provider if you:
` Have or have had any kidney or liver problems, including hepatitis infection.
` Have any other health problems.
` Are pregnant or plan to become pregnant. It is not known if BIKTARVY can harm your unborn baby. Tell your healthcare provider if you become pregnant while taking BIKTARVY.
` Are breastfeeding (nursing) or plan to breastfeed. Do not breastfeed. HIV-1 can be passed to the baby in breast milk.
Tell your healthcare provider about all the medicines you take:
` Keep a list that includes all prescription and over-thecounter medicines, antacids, laxatives, vitamins, and herbal supplements, and show it to your healthcare provider and pharmacist.
` BIKTARVY and other medicines may affect each other. Ask your healthcare provider and pharmacist about medicines that interact with BIKTARVY, and ask if it is safe to take BIKTARVY with all your other medicines.
POSSIBLE SIDE EFFECTS OF BIKTARVY
BIKTARVY may cause serious side effects, including:


` Those in the “Most Important Information About BIKTARVY” section.
` Changes in your immune system. Your immune system may get stronger and begin to fight infections that may have been hidden in your body. Tell your healthcare provider if you have any new symptoms after you start taking BIKTARVY.
` Kidney problems, including kidney failure. Your healthcare provider should do blood and urine tests to check your kidneys. If you develop new or worse kidney problems, they may tell you to stop taking BIKTARVY.
` Too much lactic acid in your blood (lactic acidosis), which is a serious but rare medical emergency that can lead to death. Tell your healthcare provider right away if you get these symptoms: weakness or being more tired than usual, unusual muscle pain, being short of breath or fast breathing, stomach pain with nausea and vomiting, cold or blue hands and feet, feel dizzy or lightheaded, or a fast or abnormal heartbeat.
` Severe liver problems, which in rare cases can lead to death. Tell your healthcare provider right away if you get these symptoms: skin or the white part of your eyes turns yellow, dark “tea-colored” urine, light-colored stools, loss of appetite for several days or longer, nausea, or stomach-area pain.
` The most common side effects of BIKTARVY in clinical studies were diarrhea (6%), nausea (6%), and headache (5%). These are not all the possible side effects of BIKTARVY. Tell your healthcare provider right away if you have any new symptoms while taking BIKTARVY.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.FDA.gov/medwatch or call 1-800-FDA-1088.
Your healthcare provider will need to do tests to monitor your health before and during treatment with BIKTARVY.
HOW TO TAKE BIKTARVY
Take BIKTARVY 1 time each day with or without food.
GET MORE INFORMATION
` This is only a brief summary of important information about BIKTARVY. Talk to your healthcare provider or pharmacist to learn more.
` Go to BIKTARVY.com or call 1-800-GILEAD-5
` If you need help paying for your medicine, visit BIKTARVY.com for program information.
(bik-TAR-vee)
US-BVYC-0008 01/22
BIKTARVY, the BIKTARVY Logo, GILEAD, the GILEAD Logo, and GSI are trademarks of Gilead Sciences, Inc., or its related companies. Version date: February 2021 © 2022 Gilead Sciences, Inc.
All rights reserved.
































Please see Important Facts about BIKTARVY, including important warnings, on the previous page and visit BIKTARVY.com. BIKTARVY® is a complete, 1-pill, once-a-day prescription medicine used to treat HIV-1 in certain adults. BIKTARVY does not cure HIV-1 or AIDS. Ask your healthcare provider if BIKTARVY is right for you. Because HIV doesn’t change who you are. ONE SMALL PILL, ONCE A DAY Pill shown not actual size (15 mm x 8 mm) | Featured patient compensated by Gilead. #1 PRESCRIBED HIV TREATMENT * *Source: IQVIA NPA Weekly, 04/19/2019 through 05/28/2021. Scan to see Zach’s story. Because HIV doesn’t who you are. KEEP EXPLORING. ZACH LIVING WITH HIV SINCE 2009 REAL BIKTARVY PATIENT
EXCLUSIVELY ON POZ.COM

#ADVOCACY
Fighting against HIV and AIDS has always been a struggle. Much work remains to end the epidemic. POZ encourages you to get involved in advocacy. Go to poz.com/ advocacy to find the latest news and learn how you can make a difference in the fight.
#CRIMINALIZATION
Opinions still vary on whether criminal law should apply to HIV disclosure, exposure and transmission. However, there is a growing consensus to make laws reflect current science. Go to poz.com/ criminalization for more on how you can get involved in reform efforts.



#UNDETECTABLE
The science is clear: People who have an undetectable viral load don’t transmit HIV sexually. In addition to keeping people healthy, effective HIV treatment also means HIV prevention. Go to poz.com/undetectable for more.
POZ DIGITAL
Scan the QR code (left) with your smartphone camera or go to poz.com/digital to view the current and past issues online.

The Well Project’s Krista Martel with her dog, Simba

22 EVOLVING THE HIV DECRIMINALIZATION
MOVEMENT For 10 years, the Sero Project has fought HIV criminalization laws—and it’s not done yet.
BY TIM MURPHY
28 INCREASING PrEP UPTAKE IN THE SOUTH
Women are the focus of new programs. BY
3 FROM THE EDITOR Is It a Crime?
4 POZ Q & A
Anthony Fauci, MD, discusses his retirement from government, COVID-19 and HIV with Mitchell Warren of AVAC.
6 POZ PLANET
“Bounce to Zero” to end HIV • mobilizing Black gay men to fight mpox • ads for HIV meds upset viewers • “Keep on Loving” to prevent HIV • POZ Stories: Lashanda Salinas • Everyday: milestones in the HIV epidemic
11 VOICES
Winners of the 7th Annual POZ Awards, and Cleve Jones is honored with a lifetime award from the National AIDS Memorial.
14 SPOTLIGHT
World AIDS Day 2022
LAURA SCHMIDT
16 NUTRITION & FITNESS
Salmon with grapefruit vinaigrette
• get ready to get fit
17 BASICS
Switching HIV treatment
18 CARE & TREATMENT
IAS-USA releases new HIV treatment and PrEP guidelines • antiretrovirals and weight gain • COVID vaccine response in people with HIV • COVID disrupted HIV care
20 RESEARCH NOTES
bnAb HIV vaccine shows promise • Sunleca approved for people with multidrugresistant HIV • CRISPR may remove HIV genome from cells • people with HIV can benefit from lung cancer screening
32 HEROES
Krista Martel, executive director of The Well Project, marks 10 years at the helm.
CONTENTS POZ (ISSN 1075-5705) is published monthly except for the January/February, April/May, July/August and October/November issues ($19.97 for an 8-issue subscription) by Smart + Strong, 157 Columbus Avenue, Suite 525, New York, NY 10023. Periodicals postage paid at New York, NY, and additional mailing offices. Issue No. 266 POSTMASTER: Send address changes to POZ/Smart + Strong, 157 Columbus Avenue, Suite 525, New York, NY 10023. Copyright © 2023 CDM Publishing, LLC. All rights reserved. No part of this publication may be reproduced, stored in any retrieval system or transmitted, in any form by any means, electronic, mechanical, photocopying, recording or otherwise without the written permission of the publisher. Smart + Strong® and POZ® are registered trademarks of CDM Publishing, LLC.
COVER: OCTAVIO JONES; THIS PAGE; (MARTEL) BILL WADMAN; (GAVEL/BOOKS, BARBED WIRE AND MAGNIFIER) ISTOCK
D
D
D
EDITOR-IN-CHIEF
ORIOL R. GUTIERREZ JR.
MANAGING EDITOR
JENNIFER MORTON
DEPUTY EDITOR
TRENT STRAUBE
SCIENCE EDITOR
LIZ HIGHLEYMAN
COPY CHIEF
JOE MEJÍA

EDITORIAL ASSISTANT
LAURA SCHMIDT
ART DIRECTOR
DORIOT KIM
ART PRODUCTION MANAGER
MICHAEL HALLIDAY
CONTRIBUTING WRITERS
SHAWN DECKER, OLIVIA G. FORD, ALICIA GREEN, MARK S. KING, TIM
MURPHY, CHARLES SANCHEZ
CONTRIBUTING ARTISTS
JOAN LOBIS BROWN, LIZ DEFRAIN, ARI MICHELSON, JONATHAN
TIMMES, BILL WADMAN
FOUNDER
SEAN STRUB
LEGACY ADVISER
MEGAN STRUB
ADVISORY BOARD
A. CORNELIUS BAKER, GUILLERMO
CHACÓN, SABINA HIRSHFIELD, PHD, KATHIE HIERS, TIM HORN, PAUL KAWATA, NAINA KHANNA, DANIEL
TIETZ, MITCHELL WARREN
PRESS REQUESTS
NEWS@POZ.COM
SUBSCRIPTIONS
HTTP://ORDER.POZ.COM
UNITED STATES: 212-242-2163
SUBSCRIPTION@POZ.COM
FEEDBACK
EMAIL WEBSITE@POZ.COM OR EDITOR-IN-CHIEF@POZ.COM
SMART + STRONG
PRESIDENT AND COO
IAN E. ANDERSON
EDITORIAL DIRECTOR
ORIOL R. GUTIERREZ JR.
CHIEF TECHNOLOGY OFFICER
CHRISTIAN EVANS
VICE PRESIDENT, INTEGRATED SALES
DIANE ANDERSON
INTEGRATED ADVERTISING MANAGER
JONATHAN GASKELL
INTEGRATED ADVERTISING COORDINATOR
SARAH PURSELL
SALES OFFICE 212-938-2051; SALES@POZ.COM
CDM PUBLISHING, LLC

CEO JEREMY GRAYZEL
CONTROLLER
JOEL KAPLAN
Is It a Crime?
IDON’T REMEMBER EXACTLY when it happened, but I do recall my first in-depth conversation about HIV criminalization. It was with POZ founder Sean Strub. I was the deputy editor at the time. He was in the process of launching a new nonprofit called the Sero Project.
I was sitting in the office of our managing editor, Jennifer Morton. Sean was visiting the office for a meeting, so he came to say hello to us. His appointment was delayed, which gave us all a chance to talk about the injustice of HIV criminal laws and the need for advocacy against such laws.
Before that chat, I admit that I had not thought about this topic in any great detail. I knew such laws existed, but I hadn’t considered how badly they had aged, since most had been implemented before effective treatment. HIV was no longer an automatic death sentence. Regardless, I confess that it took me quite some time to get past my own hang-ups about this issue.
My reasons were very personal. I tested HIV positive in 1992. Since I had tested HIV negative in 1991, I was confident that only one person could have transmitted the virus to me. When I confronted him that I had tested HIV positive, he didn’t disclose his own status right away, but eventually, he did. He died of AIDS-related illness in 1994.
Needless to say, I was angry at him for years. That anger did diminish over time, especially as I repeatedly encountered the stigma and discrimination he must have experienced. I never once considered involving the legal system in what I believed to be a personal matter, but for years, I could not fault others for making a different choice. That changed soon after my chat with Sean.
I went through the same process most people do when they start to think more deeply about HIV criminalization. At least that’s how Sean described it during that talk, as a process. Realizing step by step that every objection to repealing these laws has a compelling counterpoint only leads folks
to one conclusion: HIV is not a crime; therefore, these laws must be abolished.
Since its launch in 2012, the Sero Project has led the way on this topic. Many states have already modernized their HIV criminalization laws, notably states that once imprisoned people simply for not disclosing, even if they were undetectable and HIV wasn’t transmitted. As a measure of that success, in May, Sean will be stepping down as executive director. Longtime advocates Tami Haught and Kamaria Laffrey will become co–executive directors. Go to page 22 to read more about their efforts.

In addition to highlighting the efforts of Tami and Kamaria, this issue also features the stories of other women advocates, such as Krista Martel. In 2023, she marks 10 years at the helm of The Well Project. Go to page 32 to read more about Krista.
Another advocate is Lashanda Salinas. Go to page 10 to read about why she is fighting against Tennessee’s HIV criminal laws.
Please also take a look at our poster about HIV criminalization in the back of this issue.
ORIOL R. GUTIERREZ JR. EDITOR-IN-CHIEF editor-in-chief@poz.com
Want to read more from Oriol? Follow him on Twitter @oriolgutierrez and check out blogs.poz.com/oriol.

FROM THE EDITOR
poz.com MARCH 2023 POZ 3 (ILLUSTRATION) ISTOCK; (GUTIERREZ) JOAN LOBIS BROWN POZ.COM/TWITTER POZ.COM/FACEBOOK POZ.COM/INSTAGRAM
STILL MUCH TO DO
AVAC looks ahead with Anthony Fauci, MD, to what’s next in the fight against HIV and COVID-19.
PRIOR TO HIS DEPARTURE AS HEAD OF THE NATIONAL INSTITUTE of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health (NIH), Anthony Fauci, MD, spoke with Mitchell Warren, executive director of AVAC, on November 28, 2022, in advance of World AIDS Day. In the interview, they discuss what has been accomplished so far in the fight against HIV and COVID-19 and what’s ahead for Fauci and pandemic preparedness. Below is an edited excerpt.
Warren: What do we need to do differently in the next three to five years to meet the ambitious HIV goals set by the global community for 2030?
Fauci: We need to get back on track at the pace that we were on before we got hit with COVID—from the availability and ease of testing to the treatment supply chain, from outreach to the community to even the research endeavor itself.
Many people who otherwise would have been involved in HIV research essentially switched emphasis temporarily out of necessity. Many clinical trials came to a standstill because of the restriction of getting people into the clinic or into the hospital to study. We have to reset and reenergize.
Despite the stress of the last three years on the system, much has been accomplished. Particularly as an example is the proof of the extraordinary efficacy of long-acting injectable drugs for both HIV prevention and treatment. These could be game changers for us.
For the immediate future, it will be very exciting to apply to HIV the advances in vaccine technology that were hugely successful with COVID. We now have a number of trials that are going on from preclinical to Phase I using an mRNA platform for an HIV vaccine.

We also are seeing applications of some of the immunogen design that was so successful with COVID, where we utilize the stabilization of the prefusion configuration

of the viral spike protein, which turned out to be extraordinarily effective.
These are all lessons that we learned from COVID in the same way that HIV informs some of the successes that we got with COVID.
To what degree as researchers and as funders of research do we need to turn from biomedical product development to the often harder work of delivery? As far as pre-exposure prophylaxis (PrEP), if you look at the numbers, it is not being maximally utilized, particularly amongsomeofourminoritypopulations, which is really unfortunate.
We’ve got to get user-friendly PrEP to them. That’s going to involve implementation that integrates itself into the health care delivery system. Otherwise, we’re going to have highly effective interventions that are not being used, and that would really be a big mistake.
A very critical point in the success or not of ending the HIV epidemic is continuing with new discoveries. There are always new things that we need to discover. And we’ve done a very good job of that. But it’s important that we implement them, and that’s something
4 POZ MARCH 2023 poz.com
BY AVAC POZ Q & A BOTH IMAGES: ISTOCK
HIV (left) and SARS-CoV-2, the virus that causes COVID-19
that we are going to be making significant investments in.
We’ve got to keep everybody’s feet to the fire, including the appropriators, who might think, We’re doing so well, we don’t need new resources. We need increases in HIV commensurate to at least and maybe more in some respects than for other areas.
Remember, we went through a very disturbing period where everything was flat for a very long period of time with the misperception that you don’t want to get above a certain percentage of the budget, which is nonsense. It should be determined by the scientific opportunity and the public health need. Hopefully, that’s what we’ll be doing.
You’ve been such an effective spokesperson to policymakers and the public, what are we going to do without you? There are a lot of good people that can do this. I want to emphasize that I am not stepping away from my passion for ending the epidemic and getting attention to the importance of resources. I’ll be doing it in a different venue, but that venue could perhaps be equally if not more effective. I’m not disappearing.
Is it still possible in our lifetimes to see an HIV vaccine? And can we end the HIV epidemic without one?
Is it still possible? Of course. Is it difficult? Extremely.
It violates that rule of vaccinology that the best way to get a successful vaccine is to mimic a natural infection. When you get naturally infected with measles or polio, for example, when you recover, you develop a degree of immunity that protects you against reinfection from the same pathogen.
The correlate of immunity is unfortunately, and I might say tragically, not the case with HIV. Natural infection does not provide an adequate degree of immunity, which is why people can get reinfected and superinfected and virtually no one ever spontaneously gets cured of HIV by their immune system.
We’ve got to do better than natural infection immunity, and I think we can. We have the will and the wherewithal and the scientific commitment.
As for ending the epidemic without a vaccine, I also believe we can. If we implement long-acting injectables for PrEP and for treatment, I believe we can do it. We should not give up on the possibility of ending the outbreak by saying until we get a vaccine that we’re not going to achieve it.
It gets back to the principles of undetectable equals untransmittable. We need consistent widespread testing. If you are HIV negative, go on PrEP. If you are HIV positive, go on therapy. If we were able to do that 100% effectively, you would see the end of the epidemic without a vaccine. In that regard, a vaccine would be a bonus.
when it comes to people who are spreading misinformation.
The only thing that I would say is that we can’t give up. People throw up their hands and say there’s so much antiscience filled with myths. We can’t give up, because if we do, there’s no counter.
In your career, what are some of the biggest successes and regrets?
At NIAID, it was developing the AIDS program that has been responsible, with industry, for the development of most of the drugs that have now saved millions of lives. As a policy person, it clearly was helping to develop the President’s Emergency Plan for AIDS Relief (PEPFAR).
Coming out of COVID, where there was so much misinformation, what do we do to get out of this?
This may be one of the most important topics looking forward, not only for HIV but for all elements of science and public health. The divisiveness in this country, which feeds into the misinformation and disinformation, is truly profound. I have never in all of my career of 54 years here at NIH and 38 years as the director of NIAID ever seen this level of misinformation and disinformation.


I’ve always said that the best way to counter misinformation and disinformation is to flood the system with correct information. But it’s a very interesting situation that I’ve observed.
Usually, people have a lot of responsibilities, or, as they say colloquially, have day jobs. However, the people who are out there spreading ridiculous nonsense seem to have all the time in the world to spread misinformation.
It’s almost like we’re outnumbered
PEPFAR is a great example of what can be done when you have leadership and commitment from the highest levels of the country.
My biggest disappointment is that I wanted to be in this position when we developed a safe and effective HIV vaccine. It is just not turning out that way. But we’re not giving up.
Thank you for all that you’ve done. I’m going to let you have the last word. It’s been such a great privilege, a pleasure and an honor to be leading this organization and to be getting involved, particularly with the relationships that we’ve developed along the way, with so many people and organizations.
I look forward to continuing to interact with you in a different capacity, which is soon to be determined but not quite yet known. ■
AVAC advances global advocacy for HIV prevention. Go to AVAC.org to learn more.
poz.com MARCH 2023 POZ 5
“I am not stepping away from my passion.”
—Anthony Fauci, MD
Anthony
Fauci, MD
(FAUCI) NATIONAL INSTITUTE OF ALLERGY AND INFECTIOUS DISEASES; (WARREN) COURTESY OF MITCHELL WARREN
Mitchell Warren
“BOUNCE TO ZERO” TO END HIV

A New Orleans campaign aims to reduce new cases.
A New Orleans campaign aims to reduce new cases.

Inspired by bounce music—the highenergy hip-hop style that originated in New Orleans—the Southern city known as NOLA launched the HIV campaign “Bounce to Zero,” which aims to “reduce new HIV cases by 95% by 2030 and create a world with zero new HIV infections and zero people out of care.”
The campaign, which is headquartered on BounceToZero.com, includes Queen of Bounce Big Freedia and urges folks to #NOLAYourStatus (a play on “know your status”) and to take a pledge to stop HIV stigma.
“We hope this campaign will get the word out to Black residents all across the region and help them feel more comfortable with HIV testing and treatment as needed,” Jennifer Avegno, MD, director of the New Orleans Health Department and an official at the Louisiana State University School of Medicine, told Louisiana Weekly, adding that African Americans are disproportionately affected by HIV and its stigma.
“There has been much progress in HIV diagnosis and treatment over the
past several decades so that now individuals who are in care can live long, healthy lives,” Avegno says. “However, stigma around the disease persists and is a killer—by being afraid to know your status or seek treatment, individuals can present later in the course of the illness and suffer tremendously.”
“Bounce to Zero” launched in conjunction with events such as a wreathlaying ceremony marking World AIDS Day (WAD), held each December 1 (see page 14 for more WAD events), and is part of the federal Ending the HIV Epidemic (EHE) initiative, which aims to reduce new HIV cases in the country by 75% by 2025 and by 90% by 2030.
Launched in 2019 by President Donald Trump, the EHE initiative invests
federal and
federal funding and resources in 57 key jurisdictions. These are the 48 counties nationwide plus Washington, DC; San Juan, Puerto Rico; and seven rural states with high HIV burdens (Alabama, Arkansas, Kentucky, Mississippi, Missouri, Oklahoma and South Carolina) that together account for 50% of new HIV cases.
New Orleans, with its high HIV rates, received federal EHE funding. As Louisiana Weekly reports, 8,642 people are known to be living with HIV in the city, which amounts to 38% of the total number of cases in Louisiana. Nationwide, about 1.2 million people have HIV.
“Bounce to Zero” promotes HIV testing, education, prevention, access to care and awareness of Undetectable Equals Untransmittable, or U=U, which refers to the fact that people living with HIV who maintain an undetectable viral load do not transmit the virus sexually. —Trent
Mobilizing Black Gay Men to Fight Mpox
The #FactsAndVax campaign enlists Black influencers.

One of last year’s biggest health stories was the outbreak of monkeypox, now referred to as mpox, which primarily affects men who have sex with men. Although cases have dramatically decreased since its peak during the summer, disparities remain among people of color and in the South. To engage African-American gay men, the LGBTQ advocacy group GLAAD teamed up with influencers in the community for a series of Instagram Reels and a social media campaign.
The first video in the #FactsAndVax influencer campaign launched November 20 with a humorous Reels in which life coach Obio Jones, playing multiple roles, brings up the topic with a friend who says he got vaxxed two years ago—he is likely confusing the mpox shots with COVID-19 vaccines, because mpox vaccines weren’t out in 2020. When he’s corrected on the facts, he disappears, presumably off to his health care provider.




The campaign directs folks to GLAAD’s “Factsheet for the LGBTQ Community on Mpox,” which includes answers to questions
such as “Am I eligible to be vaccinated against Mpox?” and “Are people “living with HIV/AIDS more likely to get Mpox?”
Seven other reels have been posted since the debut.
The influencers are:
Kvng David, an Atlanta-based musician


Clockwise from top right: Reggie Rich, Dustin Ross, Kenni Javon, Maria Van Cartier, Henry Philyaw, Antonio “Forever Mistah,” Obio Jones and Kvng David
Reggie Rich, a Washington, DC–based party promoter
Obio Jones, an Atlanta-based life coach and LGBTQ advocate

Dustin Ross, a New York City–based actor, writer and television host
Antonio “Forever Mistah,” an Atlanta-based party promoter
Kenni Javon, a New York City–based DJ and party promoter
Henry Philyaw, a New York City–based writer
Maria Van Cartier, a New York City–based actor and producer. —TS
Straube



UPDATES ON HIV & AIDS POZ PLANET (CANTRELL) YOUTUBE/LOUISIANA HOMETOWN; (LOGO) BOUNCETOZERO.COM; INSTAGRAM INFLUENCERS: (RICH) @REGGIERIICH; (ROSS) @LOOKATDUSTIN; (JAVON) @KENNIJAVON; (CARTIER) @DEARMARIANYC; (PHILYAW) @JUSTXHENRY; (MISTAH) @FOREVER_MISTAH; (JONES) @OBIOOJONES; (DAVID) @KVNGDAVIDSWORLD 6 POZ MARCH 2023 poz.com
New Orleans Mayor LaToya Cantrell
Alexandra Billings


ADS FOR HIV MEDS UPSET VIEWERS





The commercials aired on the Great American Family Channel.
TV commercials for prescription meds are about as common nowadays as ads for fast food. But for some viewers enjoying holiday movies on the Great American Family channel (GAC TV), encountering ads for HIV meds featuring same-sex couples felt like getting a lump of coal for Christmas. They complained on social media about the HIV ads, and the network apologized.
“Love the movies! But have you removed the very non-family friendly aids drug ad with 2 men kissing,” a viewer asked GAC TV via social media.


“Unfortunately, we don’t have control over local commercials,” the company responded, “and we sincerely apologize.”









Transgender actress Alexandra Billings, pictured above, who has been living with HIV for decades, used the opportunity to discuss HIV stigma and history. As LGBTQ news outlet The Advocate reported, Billings tagged GAC TV and wrote via Instagram:

“Dear @gactv

“I have been living with HIV for over 30 years now. I buried most of my friends in my 20s and I live with an illness that gets more and more difficult to manage and navigate with each passing year.


“The stigma of this disease is alive and well, as long as there are humans who attempt to pass off misinformation, fear or ignorance as normal conversation and acceptable social behavior.”
“I remember when my best friend Ginger died. She was 24 years old and had been sick for a few years. Back in the ’80s, when this first appeared, you got sick and you died. There was no treatment. There was no alternative, and there was no hope. Because funeral homes were terrified to put us in the ground because no one really knew how you got this thing, and because family members ostracized us and because the mainstream of society was working off misinformation there was nowhere to put her dead body. So my friend Gloria and I sewed her up, put her in the back of our Volkswagen and dropped her off at the Cook County emergency room exit in Chicago, Illinois, in the middle of winter.
“I’m not assigning blame. And I’m not trying to suggest this is all of who you are. Your channel professes love, tolerance and family, and I simply don’t see any of those attributes in your response to this viewer.

















“I only hope this holiday brings everyone at your channel clarity of heart. And that as you continue to tell stories about love and tolerance, and the American family, that you allow everyone into that divine space…and not just the humans you believe deserve to be there.
“Happy holidays, and may everyone in your family find inclusion and grace and, moreover, be both safe and healthy.” —TS
“Keep on Loving” to Prevent HIV
Philadelphia launches a free virtual PrEP program.
Folks in Philadelphia at risk for HIV can now access both pre-exposure prophylaxis (PrEP) and postexposure prophylaxis (PEP) at no cost, even without insurance or leaving the comfort and privacy of their own home. This month, the city launched a virtual program called Philadelphia TelePrEP to make the HIV prevention drug available to its residents.
It’s a program of the AIDS Activities Coordinating Office (AACO) of the Philadelphia Department of Public Health, which partnered with the Albert Einstein Medical Center for the initiative.
What’s more, reports Metro Philadelphia, the program aims to make PrEP prescriptions available to clients within seven days—a major improvement over the wait times people often have to endure to see a health care provider in person.
“A lot of these providers are really overwhelmed, and they don’t have the capacity to deliver PrEP services to the people who are seeking them,” says Javontae Williams, a prevention program manager with AACO. Another objective is to help retain clients in the prevention program once they begin. Many folks, Williams says, abandon PrEP after about eight or nine months.
Philadelphia TelePrEP is the “first of its kind in the region and a true opportunity to bring PrEP to people where they live,” said AACO’s director, Kathleen Brady, MD, in a press statement from the city health department.
Philadelphia TelePrEP is part of the “Philly, Keep on Loving” campaign, which provides condoms, lube, public awareness, and testing and treatment for sexually transmitted infections, including syphilis and mpox.
More than 18,000 people are living with HIV in the city, and nearly 300,000 Philadelphians are at risk of contracting HIV, estimates the Philadelphia health department, noting that about 8,200 of these individuals have already been deemed good candidates for PrEP.
In addition to offering PrEP, the telehealth program also offers PEP, a regimen of HIV meds taken after potential exposure to keep the virus from taking hold in the body. PEP must be initiated no later than 72 hours after a potential exposure. It’s hoped that a virtual program will allow people to access the antiretrovirals much faster.


Please visit PhillyKeeponLoving .com for more about TelePrEP and other campaigns, including links to sign up for PrEP and PEP. —TS










(BILLINGS) @THEREALALEXANDRABILLINGS/INSTAGRAM; ALL OTHERS: ISTOCK poz.com MARCH 2023 POZ 7
MY WORLD STOPPED


Lashanda Salinas wants to reform HIV criminalization laws.




When I was 25 years old, I was in a relationship with a guy for about a year, and after we broke up, he filed a police report saying that I didn’t tell him that I was HIV positive. I think he did this for revenge, because he knew I was receiving HIV care and he never tested positive.

The police arrested me. I had no one to bail me out, and my father was in the hospital dying of brain cancer. It was the most terrifying time of my life.
At the time, I had a job as a hotel front desk clerk, so I could not afford to hire an attorney, and there was no way I could afford a $100,000 bond. I kept thinking, How did this happen to me?





I was appointed a public defender who came to me with two plea options: 1) a three-year prison sentence in which I would spend 18 months in prison and a year and half on probation; 2) three years on probation, which meant I would

EVERYDAY
get out of jail that day. I took the latter deal because my father passed away while I was in jail and I was able to attend his funeral the following day.
I had to report to my probation officer within 24 hours. Since I was living in another city, I had to get my probation transferred. When I got a call from my new probation officer, she told me that I had to register as a sex offender. My world stopped.
I was never informed that if I pled guilty to the charges against me, I would be considered a sex offender for the remainder of my life! If I was told about the lifetime sex offender registration, I would have fought the charges.
Since I registered as a sex offender, I have to follow certain rules and requirements. I have to take classes for sex offenders. I have to pay a $150 fee once a year, which I cannot afford. I can’t be around any kids, and I can’t be within 1,000 feet of a school, daycare or anywhere children will be. When I see a child in a grocery store, I have to go in the opposite direction. I would love to go to a football game and watch my cousin play. I want to go to his graduation and see him walk across the stage.
Being charged with criminal exposure to HIV and put on the sex offender registry has been a nightmare. I want to wake up from this bad dream and have
in Tennessee never

my life be normal again. But my life and the lives of other people living with HIV in Tennessee will never be the same until this unjust law is changed. I am asking for help to do that by modernizing Tennessee’s HIV criminal laws.
What three words best describe you? Caring, fighter, strong.
What is your greatest achievement? Finding the courage to share my story and becoming an advocate.
What keeps you up at night?
Wondering if I’m fighting hard enough.
What’s the best advice you’ve received? Let go and let God.
What person(s) in the HIV community do you most admire? Ryan White and his mother, Jeanne White-Ginder.
What is your motto?
“Changing laws and lives.”
Read other POZ Stories or share your own at poz.com/stories.



4 21
At the 2019 Conference on Retroviruses and Opportunistic Infections, researchers announce that THE LONDON PATIENT (Adam Castillejo) is the second person to be cured of HIV after receiving a bone marrow transplant from a donor who is genetically immune to the virus. (2019)
20 , in which he


6 10
The Sero Project and GMHC present a screening of the short film HIV IS NOT A CRIME, followed by a discussion on HIV criminalization. (2013)

NATIONAL WOMEN AND GIRLS HIV/AIDS AWARENESS DAY


Tom Hanks wins the Academy Award for Best Actor for the film PHILADELPHIA, in which he plays a lawyer living with HIV who sues his employer for wrongful termination. (1994)



KARL SCHMID, an Australianborn television entertainment reporter, reveals on Facebook that he’s been living with HIV for more than 10 years. (2018)

(SALINAS) COURTESY OF LASHANDA SALINAS; (CASTILLEJO) JON ATTENBOROUGH; (OSCAR AND PHILADELPHIA POSTER) WIKIPEDIA; (SCHMID) FACEBOOK/KARL SCHMID
March NATIONAL NATIVE HIV/AIDS AWARENESS DAY
23
to learn more about the
of
and AIDS. BY JENNIFER MORTON
These dates represent milestones in the HIV epidemic. Visit poz.com/aidsiseveryday
history
HIV
8 POZ MARCH 2023 poz.com
Lashanda Salinas UPDATES ON HIV & AIDS POZ PLANET
, followed a
BEST CELEBRITY ADVOCATE
Demetre Daskalakis, MD
If you do a Google image search for “Dr. Demetre Daskalakis,” the first pic that appears is a sexy shot of the Columbiaand Harvard-educated doc, who is currently director of the Division of HIV/AIDS Prevention for the Centers for Disease Control and Prevention. The sex-positive, openly gay, tattooed doctor has been working on behalf of the health of the LGBTQ community for years. When monkeypox (mpox) began to spread, he was called on to serve as a member of the White House Monkeypox National Response Team.
BEST IN FILM OR TELEVISION Don Quixote in Newark (Documentary Film)
The impact of illness has always been acute among poor minority youth. In the early days of HIV, when many medical professionals shied away from the mysterious illness, James Oleske, MD, a young immunologist and infectious disease specialist in Newark, stepped up. Directed by Joseph Dorman, this film tells the story of Oleske and his work in the early 1980s. Before the virus even had a name, he noticed that babies were suffering from the illness that at the time was being seen only in gay men and IV drug users. Medical specialists and even his mentor thought Oleske’s discovery was medically
impossible, but the independent doctor refused to back down. He was the first to discover HIV in kids, which rendered him a leader in combating the virus in children around the world.
BEST IN VISUAL ARTS

Tub Talks With Damon L. Jacobs
Licensed family therapist, national pre-exposure prophylaxis (PrEP) and harm reduction champion and sexpositive HIV advocate Damon L. Jacobs launched this series of interviews on YouTube in 2021. What makes these videos extra exciting is that Jacobs and his guests shed their clothing and conduct their conversations while sharing a bubble bath. As a result, they are more vulnerable and have real and honest conversations about everything, including sex, love, connection, HIV, gender and more. Jacobs has interviewed major players in the HIV community, sex workers and friends, and the conversations are frank, funny and smart—not to mention a little titillating.
BEST IN LITERATURE
The Viral Underclass: The Human Toll When Inequality and Disease Collide by Steven
W. Thrasher
Groundbreaking LGBTQ scholar, social critic and journalist Steven W. Thrasher, PhD, has spent his career studying HIV criminalization and how the virus has been policed in marginalized communi-
ties. This vital and potent book explores how viruses can expose the vast inequalities in our society, something we witnessed all too recently during the COVID-19 pandemic. Friends, activists and teachers shared their heartbreaking stories of navigating the coronavirus, HIV and other viruses with Thrasher, uncovering the devastating effects of the lack of privilege. The Viral Underclass helps us to understand more fully the differences that determine who receives care when society is facing the deadly effects of a mysterious virus.
BEST REASON TO KEEP ACTING UP HIV Criminalization
Acquiring a virus should not be a crime, but 30 states still have laws on the books that criminalize HIV. These laws were implemented during the early days of the AIDS epidemic, designed to discourage high-risk behavior and promote safer sex. They were also written at a time when little was known about HIV and no treatments were available. In the current age of PrEP, post-exposure prophylaxis (PEP) and the fact that people living with HIV on successful treatment do not transmit the virus (Undetectable Equals Untransmittable!), the only reason laws criminalizing people living with HIV remain on the books is to promote fear and stigma. They must be abolished. Q
BLOGS AND OPINIONS FROM POZ.COM VOICES ISTOCK poz.com MARCH 2023 POZ 11
CONGRATS CLEVE

OBAMACARE IS HERE
THE NATIONAL AIDS Memorial marked World AIDS Day 2022 with a national observance at the 10-acre National AIDS Memorial Grove in San Francisco honoring AIDS activist and founder of the AIDS Memorial Quilt Cleve Jones with its Lifetime of Commitment Award.
The two days of events brought together leaders on the front lines of the epidemic for powerful conversations and events focused on “Changing the Pattern for a Future without AIDS,” referencing a major initiative of the Memorial that is bringing the Quilt to the South to address the growing crisis of rising HIV rates among communities of color and marginalized populations.
Jones, who founded the Quilt 35 years ago, was recognized for his visionary leadership, activism and powerful voice in the fight for health and social justice. He remains an inspirational force for change and action today, standing up without hesitation and using his voice for those who are often overshadowed and not heard.
Speaker Nancy Pelosi praised Jones in a special video tribute, saying, “Cleve, you are a force of nature—unshakable in the face of adversity, overflowing with a passion for serving others.
“When the AIDS crisis tightened its grip on San Francisco—when pain and despair grew rampant— you kept hope
alive,” Pelosi continued. “You were a shining light in the dark, building community out of grief and spurring action out of anguish. From the halls of power to union halls and picket lines, you have never relented in your mission: empowering the oppressed, tearing down injustice and honoring the dignity and beauty of every person.”
Former San Francisco mayor and mentor Art Agnos presented the award to Jones in front of an audience of more than 600 members of the community, who gathered on the eve of World AIDS Day for a gala to support the Memorial’s programs. “I’m honored to receive this award, but, more importantly, I’m so pleased that the Quilt now has a permanent home with the National AIDS Memorial and that it is continuing its mission of activism and justice. One thing I’ve learned is that through hope one finds courage, and through courage we find love. Love is at the core of what we do, and that is what this Quilt represents.”

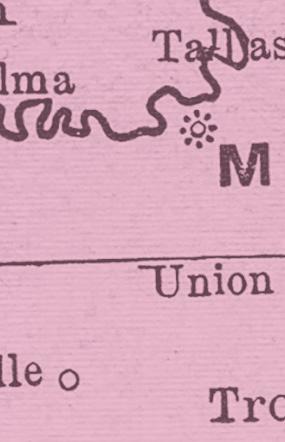
The National AIDS Memorial worked with local partners from across the country to display hundreds of Quilt sections featuring more than 3,500 individual panels in nearly 100 communities on World AIDS Day. The largest Quilt display ever in Alabama took place in Montgomery and surrounding areas as part of the Memorial’s Change the Pattern initiative. The
program, funded through a $2.4 million grant from Gilead Sciences, is organizing quilting workshops, displays and educational programming with the Southern AIDS Coalition throughout the Southern United States.
The National AIDS Memorial’s World AIDS Day Observance panelists highlighted the importance of the work being done around the country, the interconnectivity of issues to reach zero HIV diagnoses and the importance of education and outreach to at-risk populations during three powerful conversations (available for viewing at AIDSMemorial.org): “Reflections with Cleve Jones and 35 Years of the Quilt,” “The State of the Epidemic Today with Leaders on the Frontlines” and “Young Leaders Making an Impact.”
“As our community comes together this World AIDS Day, it’s hard not to look around and see who’s missing—our friends, lovers and family we’ve lost over four decades of this horrific, cruel disease,” said National AIDS Memorial CEO John Cunningham. “Today, people are still dying, and there should have been a cure long ago. We are angry because bigotry, hate and stigma persist today in society. And we carry shame because communities of color and marginalized populations continue to be disproportionately impacted by HIV and discrimination, and it shouldn’t be this way. It’s time to change the pattern.” ■
COURTESY OF NATIONAL AIDS MEMORIAL/ONYX AND ASH PHOTOGRAPHY 12 POZ MARCH 2023 poz.com
Below is an edited excerpt of a blog post by the National AIDS Memorial titled “Cleve Jones, Activist and Founder of the AIDS Memorial Quilt, Honored with Lifetime of Commitment Award on World AIDS Day.”
BLOGS AND OPINIONS FROM POZ.COM VOICES
Cleve Jones (right) accepts a lifetime award from former San Francisco Mayor Art Agnos.
Leverage HIV science into policy and practice
IAS 2023, the 12th IAS Conference on HIV Science, will take place in Brisbane, Australia, and virtually from 23 to 26 July.



Register now at ias2023.org
Join thousands of professionals at the world’s most influential meeting on HIV research and its applications.
WORLD AIDS DAY 2022




Founded in 1988 by the World Health Organization, World AIDS Day, observed annually on December 1, was the first international day designated for global health. The day marks a chance to show support for those living with HIV and to commemorate those lost to AIDS. Globally, 40.1 million people have died of AIDS, and 38.1 million people are living with HIV worldwide, including 1.2 million in the United States.
World AIDS Day also represents an opportunity to raise awareness of the issues many of those living with the virus face, including stigma, unjust laws and lack of access to treatment. By providing services and care, raising funds and awareness and offering support, love and so much more, these folks help remind us how much progress has been made in the fight against HIV while driving home the point that AIDS is not over.
14 POZ MARCH 2023 poz.com
SPOTLIGHT (1) @RCZIMLER/@THEAIDSMEMORIAL/INSTAGRAM; (2) @MICHAEL_KERNER_SF/INSTAGRAM; (3) @HOPEHOUSMEMPHIS/INSTAGRAM; (4)@ASICOPHOTO/INSTAGRAM
BY JOE MEJÍA
1 2 3 4
1. The Instagram account @TheAIDSMemorial pays tribute to those lost to AIDS by sharing photos submitted by users. Richard Zimler shared a picture of him (left) and his brother Jerry as kids in their family home in New York. Jerry died of AIDS in 1989 at age 35. 2. Photographer Michael Kerner documented the results of a screen printing workshop led by the SF Poster Syndicate at San Francisco’s Strut clinic. 3. Hope House Memphis staffers shared information about the organization’s services for families affected by HIV and AIDS at an event held at Memphis’s FedEx Forum. 4. At Washington, DC’s Kennedy Center, the AIDS Healthcare Foundation’s concert It’s Not Over honored those lost to AIDS as well as survivors and featured soul sisters Patti Labelle and Gladys Knight.
5.
welcomed by
Councilwoman
as
Beach, Florida’s World AIDS Day speaker at an event that featured free HIV testing. 6. Minnesota’s The Aliveness Project held its Third Annual Red Undie Run and raised a record $34,000 for HIV care and prevention services. 7. Ken Pinkela, a former Army lieutenant colonel, who was convicted in June 2012 of aggravated assault under an HIV crime law, shared a photo of Fordham University and NYU students standing up against HIV stigma and criminalization at the NYC AIDS Memorial. Pinkela is on the board of the Sero Project (see page 22).

8. Sporting red surgical masks instead of red ribbons, Erie Family Health staffers provided HIV education and resources in the waiting areas at one of Erie’s Chicago centers.

9. The AIDS Support Group of Cape Cod marked World AIDS Day and the agency’s 40th year with the opening of an expanded drop-in center, which, in addition to offering HIV testing and treatment and housing and food assistance, will be able to host large community events.



(5) @ARAELT/INSTAGRAM; (6) @ALIVENESSMN/INSTAGRAM; (7) @KENPINKELA/INSTAGRAM; (8) @ERIEFAMILY/INSTAGRAM; (9) AIDS SUPPORT GROUP OF CAPE COD/FACEBOOK
Author and long-term HIV survivor Rae LewisThornton (right) was
District 3
Shirley Lanier (left)
Riviera
Send your event photos to POZ at website@poz.com or tag us on Facebook, Instagram or Twitter. For a list of community events, visit poz.com/calendar. 5 6 7 8 9 poz.com MARCH 2023 POZ 15
SALMON WITH GRAPEFRUIT VINAIGRETTE
This easy recipe includes nutrient-rich broccoli rabe.
THIS RECIPE IS ONE OF THE SIMPLEST WAYS to cook salmon and an even more delicious way to eat it. The pleasantly bitter-tasting broccoli rabe and tangy vinaigrette contrast beautifully with the richness of the fish.

SERVINGS: 4 / INGREDIENTS: 7 / PREP: 20 MINUTES
INGREDIENTS FOR MEAL
4 (4-ounce) salmon fillets
Salt and pepper, to taste
1 tablespoon olive oil

1 bunch broccoli rabe, any thick stalks trimmed
4 tablespoons grapefruit pistachio vinaigrette
¼ cup pistachios, lightly toasted and chopped
DIRECTIONS FOR MEAL
1. Rub salt and pepper onto the salmon fillets.
INGREDIENTS FOR VINAIGRETTE
2 tablespoons olive oil

½ grapefruit, juiced


1 teaspoon cider vinegar

½ teaspoon honey



Salt, to taste
2 tablespoons pistachios, toasted
GET READY TO GET FIT
By Craig Ramsay
Your gym workout should be tough, but fitting it into your morning routine can be easy.
Try these three quick tips:



1. Gather your workout clothes, athletic shoes and any accessories (toiletries, hair band, towel) the night before.
2. Set your coffee maker to start five minutes before your alarm clock. The smell of the coffee brewing will help you wake up.
2. In a wide skillet with a lid, heat the oil over medium-high heat. Add the salmon to the pan, skin side up. Cook for 5 minutes, then flip and cook for another 3 to 5 minutes, or to desired doneness.

3. While the salmon is cooking, drop the broccoli into a pot of boiling salted water. Boil for 3 minutes, then drain.
4. Divide the broccoli among 4 plates, then top with salmon and evenly drizzle over the vinaigrette. Garnish with pistachios, if using. Serve.
DIRECTIONS FOR VINAIGRETTE
1. Whisk all ingredients until combined. Taste and adjust seasonings.
CHEF TIPS
A good way to cook salmon while reducing fishy smells is to bake it instead. Place salmon fillets skin side down on parchment paper on a baking sheet coated with olive oil. Sprinkle fillets with salt and pepper. Bake in a 425° F oven for 10 to 15 minutes or until a food thermometer reads 145° F when inserted into the thickest part of the fish.
NUTRITION FACTS (per serving)

Calories: 361; fat: 26 g; saturated fat: 8 g; polyunsaturated fat: 0 g; monounsaturated fat: 8 g; carbohydrates: 0 g; sugar: 1 g; fiber: 6 g; protein: 29 g; sodium: 573 mg
©2023 Fred Hutchinson Cancer Research Center, a 501(c)(3) nonprofit organization. Used by permission.
3. Keep a full water bottle in the fridge so it’s ready to grab on your way out.
expert, an author and the winner season 8 The Race on at
Craig Ramsay is a fitness expert, an author and the winner of season 8 of The Amazing Race Canada. Follow him on Instagram at @craigramsayfit.

16 POZ MARCH 2023 poz.com (SALMON) COURTESY OF COOK FOR YOUR LIFE/JOE GAFFNEY; (BOARDS) ISTOCK; (RAMSAY) COURTESY OF CRAIG RAMSAY
ADVICE ON DIET AND EXERCISE NUTRITION & FITNESS
SWITCHING HIV TREATMENT
SOME PEOPLE LIVING WITH HIV, especially those who start treatment promptly using modern antiretrovirals, can stay on their first regimen for a long time. But others are unable to keep their viral load suppressed or have trouble with side effects—or they may simply want a more convenient regimen.

There are several reasons for switching medications, including the following:
• Viral load is not suppressed
• Inadequate CD4 cell recovery
• Difficulty taking medications
• Too many pills or too frequent dosing
• Poor tolerability (side effects)
• Drug interactions
• Pregnancy
• Medication cost or insurance.
Treatment failure means some medications in a regimen are not doing their job. The best way to tell whether medications are working is to measure viral load, or HIV RNA level. If your viral load does not fall to an undetectable level—or if it does not stay suppressed— not only are you at risk for disease progression, but you could also transmit the virus to others and could develop drug resistance that limits future treatment options. A single detectable viral load, known as a “blip,” is usually nothing to worry about, but if two consecutive tests show a rising virus level, it might be time to adjust your regimen.
Virological treatment failure can happen if HIV develops mutations that make it resistant to medications. This can occur when drug levels are too low, allowing the virus to replicate—for example, if a regimen is not potent enough, if drugs are poorly absorbed (some meds must be taken on an empty stomach or with food for proper absorption) or if interactions with other medications reduce drug levels.
HIV medications only work if you take them, and poor adherence is a common cause of treatment failure. Factors that can interfere with adherence include side effects, inconvenient regimens, forgetfulness, a hectic or unpredictable schedule, unstable housing and interrupted access due to cost or insurance issues. Tell your doctor or pharmacist if you don’t understand how to take your meds or are having trouble taking them as directed. Some drugs are more “forgiving” of an occasional missed dose.
WHAT TO USE NEXT
Which new regimen to use depends on your treatment history and why you are switching. In many cases, people who have been taking more than one pill a day can switch to a more convenient singletablet regimen. Standard HIV regimens include three drugs, but people who have achieved an undetectable viral load may be able to switch to a two-drug
maintenance regimen, such as Juluca (dolutegravir/rilpivirine) or Dovato (dolutegravir/lamivudine). Another option is Cabenuva (cabotegravir/rilpivirine), long-acting injections administered once monthly or every other month.
When switching due to virological failure, resistance tests can show which drugs are not working and which alternative antiretrovirals are likely to work best. Switching treatment is more challenging for people who have already used many drugs and have developed resistance to multiple medications (known as multidrug-resistant HIV).
Ideally, a new regimen should contain at least two, preferably three, fully active drugs, but this is not always possible. Some people may be able to add novel antiretrovirals that work in different ways, such as the monoclonal antibody entry inhibitor Trogarzo (ibalizumab) or the twice-yearly injectable capsid inhibitor Sunlenca (lenacapavir). Another option is joining a clinical trial, but currently, there are few experimental antiretrovirals in the pipeline.
Modern antiretrovirals are more potent, better tolerated, less likely to lead to drug resistance and more convenient than older meds. With the newest drugs, even people who have been living with HIV for years and have highly resistant virus can usually find a regimen that keeps their HIV in check.
ISTOCK BY LIZ HIGHLEYMAN BASICS poz.com MARCH 2023 POZ 17
Most people can find a well-tolerated regimen that maintains viral suppression.
NEW HIV TREATMENT AND PrEP GUIDELINES
Coinciding with World AIDS Day, the International Antiviral Society–USA released updated guidelines on the use of antiretroviral therapy for HIV treatment and pre-exposure prophylaxis (PrEP).
The guidelines recommend starting treatment as soon as possible after an HIV diagnosis, since early treatment leads to better outcomes. For most people, integrase inhibitor regimens “remain the mainstay of initial therapy.” For people with viral suppression on a daily oral regimen, switching to long-acting injectable Cabenuva (cabotegravir plus rilpivirine) is now an option. Current PrEP options include tenofovir disoproxil fumarate/emtricitabine (Truvada and generic equivalents), tenofovir alafenamide/emtricitabine (Descovy) and long-acting Apretude (cabotegravir) injections.

The guidelines address barriers to care, treatment simplification and adherence support as well as screening for and management of other health conditions, including substance use disorders and weight gain (see next item). Finally, they discuss how recent global health emergencies, including COVID-19 and monkeypox (mpox), affect people living with HIV (see item on page 19).
“Ending the HIV epidemic will require an equity approach that focuses resources on addressing societal disparities (for example, tackling poverty as an HIV prevention strategy), addressing stigma as a root cause of HIV risk, eliminating laws that target people with HIV and ensuring access to care for all,” the authors wrote.
Studies Shed More Light on Weight Gain

Switching from the newer tenofovir alafenamide (TAF) to the older tenofovir disoproxil fumarate (TDF) may help people with HIV lose weight, but doing so because of weight gain is not recommended, according to new guidelines.
In recent years, there’s been growing concern about weight gain after starting or switching antiretrovirals. Some of the largest increases have been seen in people who start potent integrase inhibitors, such as dolutegravir, and TAF, especially when used together. In the ADVANCE trial in South Africa, which compared first-line regimens, people who started on dolutegravir, TAF and emtricitabine gained about 19 pounds over four years.
But integrase inhibitors and TAF may not be entirely to blame. TDF can lead to reduced cholesterol and triglyceride levels and either weight loss or absence of expected weight gain over time. TAF lacks this weight-suppressing effect, so people who switch from TDF to TAF may experience weight gain and rising blood fat levels.
Researchers analyzed weight and metabolic changes among a subset of ADVANCE participants who switched to dolutegravir, TDF and lamivudine when national treatment guidelines changed. People who switched from either dolutegravir, TAF and emtricitabine or efavirenz, TDF and emtricitabine to the new regimen saw declines in body weight, cholesterol and triglyceride levels and blood sugar. A related study in Finland found that people who switched from TAF to TDF while keeping their other antiretrovirals unchanged maintained a stable weight after two years, while those who stayed on TAF gained about 3 pounds.
Some people might benefit from switching—or switching back—from TAF to TDF, but this must be balanced against the risk of kidney impairment and bone loss due to TDF, side effects TAF doesn’t share. Until there’s more evidence, “switching regimens because of weight gain is not recommended,” according to new guidelines from the International Antiviral Society–USA (see item above). “Instead, lifestyle modifications, like exercise and diet intervention, are recommended.”
BY LIZ HIGHLEYMAN CARE & TREATMENT 18 POZ MARCH 2023 poz.com
COVID VACCINE RESPONSE IN PEOPLE WITH HIV
With more than two years’ worth of data, most HIV-positive people can feel confident that COVID-19 vaccines provide good protection, especially if they receive booster shots. However, individuals with poorly controlled HIV or moderate to advanced immune suppression may not fare as well.

The Corona-Infectious-Virus Epidemiology Team looked at the risk for severe illness among 1,214 HIV-positive and 2,408 HIV-negative adults in the United States who experienced breakthrough COVID after vaccination. Most had an undetectable viral load and a high CD4 count. All had received two doses of the Pfizer-BioNTech or Moderna messenger RNA (mRNA) vaccines or a single dose of the Johnson & Johnson vaccine.
Overall, people with and without HIV had low and comparable rates of severe breakthrough illness (7.3% and 6.7%, respectively). However, the risk was 59% higher for people with a CD4 count below 350 compared with HIV-negative people. What’s more, HIV-positive people with fewer than 200 CD4 cells had more than a twofold greater risk than those with a count of 500 or higher. Another study of HIV-positive adults in Denmark found that people who received a third vaccine dose were less likely to be hospitalized with COVID than those who got only two doses.
Other recent research showed that people with well-controlled HIV have antibody, memory B-cell and T-cell responses after vaccination and boosters that are comparable to those of HIV-negative people, but people with a low CD4 count may have weaker or less durable responses.

Based on these findings, HIV-positive people with moderate or severe immune suppression “should be included in groups prioritized for additional vaccine doses and risk-reduction strategies,” the authors of the first study suggest. The Centers for Disease Control and Prevention now advises that the primary vaccine series for moderately or severely immunocompromised people—including those living with HIV—should consist of three doses of the mRNA vaccines, to be followed by recommended boosters.
How Did COVID Affect HIV Care?
The nation’s ability to prevent HIV was “dealt a hard blow” early in the COVID-19 pandemic, according to a new Centers for Disease Control and Prevention (CDC) analysis. But a rapid rebound in services “is a testament to quick, resourceful local innovations that, if scaled up and sustained, could help reach national HIV prevention goals.”
Nationwide, HIV testing declined by about 32% and pre-exposure prophylaxis (PrEP) prescriptions fell by about 6% during the early months of the pandemic as cities imposed stay-at-home orders, medical services were curtailed and many people lost their jobs and health insurance. Reported HIV diagnoses fell by 26%, but this is thought to be a consequence of less testing rather than a real drop in new HIV cases. Testing and PrEP prescriptions started to rebound during the second half of 2020, but they did not reach pre-pandemic levels until 2021.
While HIV testing and PrEP prescriptions were disrupted, the provision of HIV treatment remained strong. The proportion of people who were linked to care after an HIV diagnosis, received prescriptions for antiretroviral therapy and achieved an undetectable viral load all remained stable.
To maintain access to critical HIV services, some providers launched or expanded programs to substitute for traditional in-person care, including telehealth, HIV self-testing and home delivery of HIV medications and PrEP.
“Investment in local community innovation is vital to strengthening our nation’s HIV prevention and care systems to endure future public health emergencies,” according to the CDC. “Expanding those innovations can also help achieve national goals to end the HIV epidemic.”
poz.com MARCH 2023 POZ 19 ALL IMAGES: ISTOCK (MODELS USED FOR ILLUSTRATIVE PURPOSES ONLY)
BY LIZ HIGHLEYMAN
bnAb HIV Vaccine PREVENTION
A new type of HIV vaccine that teaches the immune system to produce broadly neutralizing antibodies (bnAbs) looks promising in an early study. Scientists have spent nearly four decades studying vaccines to prevent and treat HIV, with little success. The virus mutates rapidly, making it difficult to develop a broadly effective vaccine. A novel approach known as germline targeting uses a series of vaccines in a stepwise manner to spur the development of specialized B cells and train them to produce bnAbs, antibodies that target hidden parts of the virus that don’t change much. All but one of the 36 participants in the Phase I IAVI G001 trial who received a vaccine containing eOD-GT8 60mer —an immunogen consisting of 60 engineered copies of HIV’s gp120 envelope protein—developed specialized precursor B cells. After a booster, these cells produced antibodies with greater affinity for the HIV proteins. The results offer proof of concept that this approach could work, but it will likely take years of research before it can be tested in large clinical trials.

Sunlenca Approved TREATMENT
On December 22, the Food and Drug Administration approved Gilead Sciences’ Sunlenca (lenacapavir), a new option for treatmentexperienced people with multidrug-resistant HIV who are unable to maintain viral suppression on their current regimen. The first approved HIV capsid inhibitor, Sunlenca disrupts the cone-shaped shell that surrounds the viral genetic material and essential enzymes. In the Phase II/III CAPELLA trial, 36 participants added either Sunlenca or placebo pills to their failing regimen for 14 days, and then everyone was offered Sunlenca injections every six months plus an optimized background regimen. After 52 weeks, 83% had an undetectable viral load, and CD4 counts increased by an average of 82 cells. Sunlenca is now the longest-acting HIV medication, but it can’t be used alone. Currently, no other antiretrovirals can be taken as infrequently as once every six months, so it is not yet possible to construct a complete twice-yearly regimen. Gilead is also testing Sunlenca for first-time HIV treatment and for pre-exposure prophylaxis (PrEP).
CRISPR Cuts CURE

Excision BioTherapeutics recently announced that the first participant in a Phase I/ II clinical trial has received a CRISPR-based gene-editing therapy designed to snip HIV out of human cells, potentially leading to a functional cure. Antiretroviral therapy can keep HIV replication suppressed, but the virus inserts its genetic blueprints— known as a provirus—into the DNA of human cells and establishes a long-lasting reservoir that is unreachable by antiretrovirals and invisible to the immune system. The therapy, dubbed EBT-101, uses an adeno-associated virus to deliver CRISPR-Cas9 nucleases—enzymes that act as “molecular scissors”— and dual guide RNAs targeting three sites in the HIV genome that tell the enzymes where to cut. This study is evaluating a single IV infusion of EBT-101 in nine men with an undetectable viral load on daily antiretroviral therapy. The first participant was treated last July, and the therapy has been well tolerated so far. The man is expected to start a carefully monitored antiretroviral treatment interruption to see whether his HIV rebounds.

Lung Cancer CONCERNS
People living with HIV who are current or former heavy smokers may be at high risk for lung cancer and could benefit from regular screening, according to the Forum of International Respiratory Societies. People with HIV may have impaired cancer-fighting immune function, even if they’re on treatment, and studies have shown that they are more likely to develop several types of cancer. Lung cancer is the leading cause of cancer death for HIVpositive people in the United States and worldwide, as it is for HIV-negative people. What’s more, people living with HIV are more likely to smoke than those who are HIV-negative. The U.S. Preventive Services Task Force recommends annual lung cancer screening using low-dose CT scans for people ages 50 to 80 who have at least a 20 pack-year smoking history. A recent study found that people living with HIV tend to develop lung cancer at a younger age and with a less extensive smoking history than those in the general population, suggesting that people with HIV may benefit from earlier screening.

RESEARCH NOTES ALL IMAGES: ISTOCK 20 POZ MARCH 2023 poz.com



















A daily resource for people living with and affected by HIV and AIDS
information
A SMART + STRONG PUBLICATION Award-winning consumer health care information Follow us on: us on:
•
• Clear, comprehensive prevention and treatment
• News, personal stories, blogs, HIV-specific resources and more • Sign up for free email newsletters POZ.COM
EVOLVING THE HIV DECRIMINALIZATION MOVEMENT

THE SERO PROJECT HAS BEEN MOBILIZING ADVOCATES ACROSS THE COUNTRY TO FIGHT HIV CRIMINALIZATION LAWS FOR 10 YEARS— AND IT’S NOT DONE YET.
BY TIM MURPHY
FOR A DECADE, THE PIONEERING Sero Project has led the push for the repeal—or at least the modernization—of outdated laws that criminalize people living with HIV for having sex without disclosing their status, even in cases where HIV is not transmitted. The national nonprofit does serious work. If Sero’s story were to be dramatized, its tale could be told in two chapters.
22 POZ MARCH 2023 poz.com
OCTAVIO JONES
 Tami Haught (left) and Kamaria Laffrey are living with HIV.
Tami Haught (left) and Kamaria Laffrey are living with HIV.
The first chapter, “When Sean Met Tami,” would take place in 2013. That’s when Iowa native Sean Strub met fellow Iowan Tami Haught. Strub, who has been living with HIV since the 1980s, founded POZ magazine in 1994 and sold it a decade later. Haught was diagnosed with HIV in 1993, a day before her 25th birthday, and had since become involved in HIV activism in Iowa, including advocating for more funding for the AIDS Drug Assistance Program (ADAP) in the mid-2000s, when more than 1,000 Iowans were on the ADAP waiting list to access HIV meds.
Strub’s anger at the injustice of HIV criminalization laws—many of which apply even if HIV is not transmitted and focus on the accusation of nondisclosure, which is hard to prove—led him to launch Sero in 2012. He asked Haught to coordinate Sero’s first HIV Is Not a Crime (HINAC) conference at Iowa’s Grinnell College in 2014. And she did.
That was also the year that Iowa—thanks to a coalition led by Haught—became the first state since the founding of Sero to modernize its HIV criminalization law by factoring in an undetectable viral load or the use of a condom into a case and increasing the burden on the prosecution to prove that the person with HIV demonstrated an intent to transmit HIV—a high bar to clear. The modernization also removed from the state sex offender registry everyone who had been placed on it due to an HIV crime.
The second chapter, “When Tami Met Kamaria,” would take place shortly after, in 2016, when Florida’s Kamaria Laffrey—who was diagnosed with HIV in 2003 and subsequently became a local activist, speaking at National Black HIV/AIDS Awareness Day events and fighting the era’s ADAP shortage in her state—attended the second HINAC conference in Alabama.
“I went and never looked back,” Laffrey says. Back in Florida, she led a coalition to decriminalize HIV in her state—the effort is ongoing—and in 2017 joined Sero’s fulltime staff.
In May, Strub will retire as Sero’s founding executive director and become a senior adviser, while Haught and Laffrey, currently co–managing directors, will become co–executive directors.
HAUGHT AND LAFFREY HAVE THEIR WORK CUT out for them. As of the summer of 2022, according to the Center for HIV Law and Policy (CHLP), 30 states still have HIV-specific criminal laws or sentence enhancements applicable to people living with HIV.
However, it’s also true that over the past decade, 13 states have reformed or repealed one or more parts of their HIV-specific crime laws. (Texas, somewhat notably, repealed its HIV-specific crime law back in 1994.)
That’s a lot of hard-won legislation in only a decade. Sero has had a guiding hand in all of it. It has nurtured coalitions of people living with HIV and their care and service providers and other allies and urged each coalition to push for the changes it felt were within reach for a particular state. “It’s a different strategy in every state,” says Strub. “No one state
becomes the model, because each has its own political realities.”
Sero has amassed many partners and admirers over the years. “They’ve been an amazing model of courage,” says Charles Stephens, founder and executive director of The Counter Narrative Project, which works to create better attitudes toward and policies benefiting Black gay and bisexual men, including HIV decriminalization. “They’ve built a movement, raised awareness and changed laws.”

Stephens particularly applauds Sero’s focus on the disproportionate impact of HIV crime laws on Black people, especially Black gay men. “In HIV criminalization, we can really see how the forces of racial disparities in the criminal justice system converge,” he says. “We have to address criminalization as a racial justice issue.”
Sero has also been instrumental in putting people living with HIV at the forefront of decriminalization efforts, says Naina Khanna, co–executive director of Positive Women’s Network–USA (PWN-USA), which has often collaborated with Sero, including on the HINAC conferences, since 2016.
“They’ve centered the voices of survivors of HIV crimi-
24 POZ MARCH 2023 poz.com
(CONFERENCE) COURTESY OF SERO PROJECT/JENNIE SMITH-CAMEJO
Clockwise from above: Attendees of the HINAC3 conference; Sean Strub, founder of POZ and the Sero Project; promotional poster from Sero
nalization, making sure that their stories and priorities are reflected in our efforts to abolish these laws,” Khanna says. She also says Sero introduced the state-by-state strategy of changing laws, helping nurture coalitions in each state as early as the first HINAC conference in Iowa, when it asked groups from each state to announce aloud what their next steps would be once they returned home.
“Nobody had been doing that before,” she says, “especially while making sure that people living with HIV, not just lobbyists from big organizations, were prioritized in the process.”
In the broadest sense, Sero has played a huge role in a social trend away from the attitudes of the 1980s and ’90s—when people living with HIV were largely seen as dangerous and rarely were given the benefit of the doubt in an HIV criminal-


ization case—and toward an era of greater understanding that people on effective treatment do not transmit HIV through sex and that the vast majority of people with the virus do everything possible not to expose their sexual partners, even if not all of them disclose their status before sex.
“It’s been a huge learning curve and helped me identify a fire inside me that I didn’t know I had,” says Laffrey of her Sero experience. “If anyone had come to me a decade ago and told me I’d be doing this work, I’d have laughed in their face.”
WHEN SERO WAS FOUNDED IN 2012, HUNDREDS, perhaps thousands, of Americans living with HIV—it appears that no one has an exact number—had been prosecuted under HIV-specific statutes since states began instituting them in the AIDS-phobic mid-’80s.
“I was alarmed by the growing stigmatization and criminalization of people living with HIV, along with the declining strength of networks of people with HIV” with every passing year of better antiretroviral treatment, says Strub. Although CHLP had started the anti-criminalization Positive Justice Project, “actual people living with HIV needed a voice in the movement, like a labor union,” he says.
Strub particularly wanted to center the voices of people

poz.com MARCH 2023 POZ 25 (STRUB)
BILL WADMAN
living with HIV who had been prosecuted, so he reached out to three such individuals: Robert Suttle in Louisiana, Nick Rhoades in Iowa and Monique Howell in South Carolina. A grant from Broadway Cares/Equity Fights AIDS (BC/EFA) allowed Strub to produce the eight-minute documentary HIV Is Not a Crime, which became Sero’s most valuable teaching tool.
The film showed how the three of them were living under suffocating legal penalties and stigma despite not having transmitted HIV to their partners. The doc included a shot of Suttle’s driver’s license with “SEX OFFENDER” stamped across it in large red letters.

Funds from BC/EFA, the Elton John AIDS Foundation and the philanthropist Henry van Ameringen allowed Strub to produce an informational brochure, hire two interns and start speaking at colleges, universities and law and medical schools about HIV crime laws. “People didn’t even know what the phrase ‘HIV criminalization’ meant, and many of them, when they first learned of the statutes, believed they served a purpose,” he says.
In 2013, a research working group on HIV criminalization funded by the National Institutes of Health concluded: “Findings from empirical studies on the impact of these laws suggest that they do not decrease HIV infections or have any other positive public health impacts.”
By the time Strub brought Haught into Sero, she had already started the coalition that led to the modernization of Iowa’s HIV law in 2014. To celebrate the law change, including its removal of those harmed by it from the state’s sex offender registry, a reception was held at the first HINAC conference during which the law change’s legislative champion, state Senator Matt McCoy, used a bolt cutter to remove the sex offender ankle bracelet that Rhoades had been forced to wear.

“Watching that was very moving, nourishing and inspiring” for the budding movement, recalls Strub. “There was an ecstatic reaction in the room.” Recalls Haught: “That will always be the greatest advocacy moment in my life, along with getting emails from other Iowans who’d left the state and were removed from offender registries in their new state, where they’d been required to register after Iowa.”
But as much as the new Iowa law put the burden of proof of “intention to transmit” on the accuser rather than the accused—an important change, to be sure—it retained “exposure with intent to transmit” as a felony charge and “exposure with reckless disregard” as a felony if transmission occurred and a misdemeanor if not.




It was an early lesson for Sero that such laws would be easier to modernize than outright repeal, which since 2014
has happened in only two of the 14 states where law changes have occurred—Illinois in 2021 and New Jersey in 2022.
GALVANIZED BY SERO’S BIENNIAL HINAC CONference, coalitions of people living with HIV and their allies, including service providers and public health professionals, did indeed manage to modernize and soften laws—not only in Iowa (2014), but in Colorado (2016), California (2017), Michigan, Louisiana and North Carolina (2018), Washington (2020), Missouri, Virginia, Illinois, Indiana and Nevada (2021) and Georgia and New Jersey (2022).
“When COVID hit and we were all sheltering in place, figuring out what we were going to do, advocates were still meeting virtually with legislators” and changes still went through, recalls Laffrey. “That kept me from falling under. Whenever I thought, This is too hard, our advocates were relentless, which makes me so damn proud to be a part of this movement.”
She particularly remembers the exhilaration of the legislative vote in Virginia, which came down to the wire. “We each had a chunk of a long list of lawmakers we needed to reach out to over a weekend via phone and email—then waiting on that Monday to find out how the vote was going. It was an adrenaline rush. Folks want to put their hands on something, and you don’t always get to feel you’re making the sausage like that. Usually, you do community engagement, make a move and wait—but it’s exciting when you finally get the bill on the table, and it’s all hands on deck.”
At the heart of efforts in every state, says Strub, “you have to explain to people what HIV criminalization actually is, which is the inappropriate use of one’s HIV status in a criminal

BOTH IMAGES; OCTAVIO JONES 26 POZ MARCH 2023 poz.com
In May, Tami Haught (left) and Kamaria Laffrey will become co–executive directors of Sero.
prosecution. Most people don’t think there should be special crimes for people based on an immutable aspect of them, like their gender or race—but with HIV crime laws, we’re doing just that.”
But, he adds, “Ultimately, the most persuasive argument isn’t human rights, but public health. There’s zero evidence that these laws reduce HIV transmission.” On the contrary, he says, “We showed how these laws discourage people from getting tested for HIV,” because people fear that if they know they are HIV positive, it could be held against them in a legal proceeding.
Strub and other decriminalization advocates take pains to point out that the rare cases that result in HIV transmission or indicate malicious intent, sometimes involving several sexual partners, can be prosecuted under non-HIV-specific statutes, such as assault or reckless endangerment. They say that part of their work is trying to explain to people who contracted HIV from a partner who knew they had it—people who are understandably angry—why they should not press charges under HIV-specific laws.
“They feel a real harm has been done to them, and you have to let them feel that,” says Haught, whose HIV was transmitted by her husband, who died of AIDS in 1996. “But we encourage them to stop and think before they act, because many of them press charges and then feel they made a mistake when they see that the case is out of their hands with the prosecutors.”
Adds Laffrey: “I’ve known of women who felt, This person gave me HIV, and they must be arrested because they didn’t tell me. I ask them to consider the implications of these laws. I ask, ‘Do you know they could be used against you?’ The differences between possible exposure, intent and transmission are not considered. It could turn your life upside down.”
Sero has much work still to do in its second decade— including fighting off new HIV crime laws, such as the one some parties in Texas have been trying to pass during the past few years, as well as further softening or fully repealing laws that have already been modernized. Current grants from drugmakers Gilead Sciences and ViiV Healthcare as well as the nonprofit Wellspring Philanthropic Fund should go a long way toward furthering some of these goals.
Also important, says Haught, is the creation of more storytelling vehicles for the decriminalization movement, such as the short but powerful HIV Is Not a Crime documentary that got Sero started. “I want to tell the story of our success in various states so advocates pushing for law changes in other states can learn from them,” she says.
As for more state law changes, Sero is keeping an eye on
Tennessee, which will likely reintroduce a decriminalization bill, as well as on Ohio and Indiana. Also still in play is the push to pass the federal REPEAL HIV Discrimination Act—long sponsored by U.S. Representative Barbara Lee (D–Calif.)—which would have no teeth but would give states guidance on reexamining their HIV-specific crime laws.
Strub says Florida’s law will be a particularly tough nut to crack. “Usually, we feel apathy from legislators, but in Florida, we feel actual cruelty—anything to stick it to people living with HIV, Black people, queer people, just for its own sake.” He holds out hope because of the ground being laid there: “We’ve done so much organizing there, which shows you can make progress even in some of the bleakest political environments.”
Regardless of what the future holds, Sero’s principals all say the work has been transformative for them. “This is personal for all of us, for the burden of proof not to be on us,” says Haught. “We’ve had the honor of meeting survivors of criminalization, and, though the work can be emotionally draining, seeing how survivors continue to fight against incredible odds gives us strength.”
Khanna says that, as Strub fully hands over the reins to Haught and Laffrey, “I’d love to see from Sero an ongoing commitment to elevate and center racial justice, to think about how anti-Black racism, xenophobia and anti–sex work policies intersect” with efforts to soften or repeal HIV criminalization laws. “They’re already taking some great steps in that direction.”
Laffrey says being part of Sero “has really strengthened my view as a Black woman of my capabilities and how I can show up and hold myself accountable. I’m in a better position to support my community in a meaningful way. I lost my husband just before COVID hit, and I was in a very ‘I don’t give a damn’ space, but when I see other advocates say, ‘We have to keep at this because we’re worth it,’ that keeps my head above water.”
As for Strub, though he’s stepping down from Sero’s top position, he has no plans to step back from the work—especially as it becomes global, with organizations, including Sero, collaborating with the group HIV Justice Worldwide to soften or undo HIV criminalization laws around the world.
“This work has been incredibly satisfying personally,” he says. “And a lot of that is driven just by the inspiration and encouragement I get from people with HIV finding their voice, getting involved and realizing they have more power to influence policies that directly affect their lives than they realized.” ■
poz.com MARCH 2023 POZ 27
Go to SeroProject.com to find out how to get involved.
“THE DIFFERENCES BETWEEN POSSIBLE EXPOSURE, INTENT AND TRANSMISSION ARE NOT CONSIDERED.”

























































































































AIDS ALABAMA SOUTH PROMOTES PRE-EXPOSURE PROPHYLAXIS AMONG WOMEN.
BY LAURA SCHMIDT
Sucheffortshavehelpedtheclinicincrease the uptake of pre-exposure prophylaxis (PrEP) to prevent HIV among Black women, who make up nearly 35% of the clientele the clinic serves.
Shey Thorn, co–executive director of AIDS Alabama South, oversees all of the nonprofit’s prevention, education and outreach initiatives. As a high school teacher, Thorn had been struck by the lack of comprehensive sexual health education available in the South. So he quit teaching and ended up accepting a position at AIDS Alabama. “Passion makes purpose,” says Thorn. “I fell in love with the work and [AIDS Alabama’s] mission, and I found my passion.”
HIV MISINFORMATION IS STILL HIGHLY PREVALENT IN THE Southern United States. That’s why AIDS Alabama South—a fullservice sexual health clinic and a sister agency to AIDS Alabama—prioritizes meaningful relationships with its clients.
Doing so allows the clinic to provide education and outreach through courses designed to build community awareness about HIV, eliminate stigma and promote the health and well-being of people living with HIV and those who are HIV negative.
Soon thereafter, Thorn founded Sexual Health Education Learning and Living (SHELL) Health. “We cover all of those aspects of sexual health that, in the Deep South, don’t typically get covered,” says Thorn. SHELL Health, now located at AIDS Alabama South, started as a PrEP clinic that was open only once a week for four hours, but thanks to a grant, the clinic was able to hire full-time staff, open its doors five days a week and expand services to reach every corner of the community.
“We specifically focus all of our work on
poz.com MARCH 2023 POZ 29
ALL
IMAGES: ISTOCK
those who are most disproportionately affected by HIV, and, even more so, we focus our work within our minority community,” says Thorn. “So not only the LGBTQ community but also our African-American, Hispanic and Indigenous communities.”
TODAY, SHELL HEALTH HAS made community access to PrEP and post-exposure prophylaxis (PEP), which prevents infection after a potential exposure to HIV, “extremely easy,” according to Thorn.

“Creating that culture and that environment with equitable access and a focus on diversity and inclusion and being a radically inclusive space for all citizens of Mobile County and our surrounding areas,” says Thorn, “really brought a lot of people in through our doors and allowed them to see how important sexual health is.”
SHELL Health is just one part of AIDS Alabama South’s Prevention, Outreach, Testing, Education & Clinical Treatment (PrOTECT) Mobile, which addresses all aspects of sexual health. Project 1824, which offers prevention and education programs specifically for teenagers and young adults in southwest Alabama, is another part.
Project 1824, which Thorn also spearheaded, specifically prioritizes comprehensive sexual health education centered on HIV testing and PrEP education and access for young Black women between ages 18 and 24 in Mobile County.














“The point of [Project 1824] is to get larger groups of African-American women within our community together to just have simple, basic conversations so that we can eliminate their fears, eliminate HIV-related stigma in all of its forms and answer questions, and if we are unable to answer those questions, we link them to someone who can,” says Thorn.

Although Alabama is made up of 67 counties, the majority of African Americans newly diagnosed with HIV reside in Mobile, Montgomery, Madison and Jefferson counties, according to the Alabama Department of Public Health (ADPH).
Thorn encourages employees to make the most of the agency’s resources and partnerships and to get to know the people they serve through meaningful conversations “because that’s how we’re going to dispel these barriers: in between health care and community impact.”
NATIONWIDE, AFRICAN AMERICANS BEAR A disproportionate burden of HIV cases. In 2020, African Americans made up 42% of new HIV cases but only 13% of the U.S. population, according to the Centers for Disease Control and Prevention. HIV is especially prevalent in the Deep South. According to a study published in the Journal of Public Health, these states—Alabama, Georgia, Mississippi, North Carolina, South Carolina and Louisiana—have
a 30% Black population, yet African Americans in the Deep South account for 70% of HIV cases.









In Alabama, Black women are about nine times more likely to contract HIV than non-Black residents, according to ADPH. When it comes to equitable health care in Alabama, people of color historically have been disadvantaged.
As the coordinator of the Ending the HIV Epidemic initiative at AIDS Alabama South, Chance Shaw understands that transparency is key to chipping away at the Black community’s historic distrust of medical programs, which stems from years of systemic socioeconomic and cultural barriers in the United States.
Shaw and the agency aim to consistently provide culturally sensitive services because “a lot of the communities that we serve, especially our priority populations, are not only marginalized by the health care system, but they’re also typically distrustful, so we try to—and do—provide our services in a very transparent way so that we can dispel that distrust.”
Shaw points to historical events, such as the Tuskegee syphilis study, that have impacted how the Black community regards the health care system and health care providers. Conducted over the course of 40 years, the study lied to hundreds of Black men with syphilis, telling them that they were receiving treatment for the disease when in fact researchers were observing the natural progression of untreated syphilis.
The study, conducted by the Centers for Disease Control and Prevention, the Alabama State Health Department and the Macon County Board of Health, was exposed in 1972, yet no one has been prosecuted.
Shaw says “laying everything out so that they know what they’re getting into” is extremely important for Black men and women looking to start taking PrEP or to get tested for HIV.
To put clients at ease, nurse practitioners and other employees at the clinic prioritize being open and communicating about the whole process—for example, what they are testing for, what the test looks like and how long they must wait for test results.
“[People] know what we’re doing and know exactly how they can engage with us,” says Shaw. “They feel empowered when you do that because you’ve made them part of their treatment.
“Educating the people we come into contact with is almost secondary to the education they do in their own communities,” Shaw continues. “When they can get this proper education and take it back to their communities, they feel empowered to correct [misinformation] because they’ve had that education.”
30 POZ MARCH 2023 poz.com
(PILL) ISTOCK
Leaders at AIDS Alabama South recognize the importance of hiring culturally diverse employees who not only relate to clients and encourage education but also make difficult conversations about sexual health easier. They believe culturally sensitive services are key to dispelling misinformation and stigma surrounding HIV.
Shanmeshia “Shan” Thompson, the agency’s HIV testing and education outreach coordinator, says “a lot of people don’t really know or understand the importance of getting tested or know the definition of HIV.” She says a lot of people who come in for sexual health services simply need more information about HIV.
In her position, Thompson constantly builds trust with those in need of care. She reassures every person who enters the clinic that they are in a judgment-free zone and that PrEP is extremely safe and effective in preventing HIV. Thompson regards clients as her sisters and brothers.
“I’m not going to force you to get into details about anything,” says Thompson. “But as we sit there and talk, they start actually opening up to me. And I know that’s another reason why we do have a lot of people that do come in and get on either PrEP or get tested [for HIV].”
Thorn and Shaw both credit Thompson’s patience and calming energy for the increase in the number of Black women getting tested for HIV and going on PrEP.
“She is so vital to the agency. I just can’t express it enough,” says Thorn. “She creates truly impactful, compassionate, personal relationships with these clients that come through the door, and she gets to know them on a personal, first-name basis and checks in with them, and they share such a deep connection. I think that is really what initiated the acceptance within the [Black] community.”
ACCESS TO CARE IS ONE OF THE UTMOST HEALTH
concerns in Alabama, alongside mental health and substance use, according to ADPH. Rural Alabamians are especially unlikely to be able to access care in a timely fashion.
Shaw says many people who utilize the agency’s PrEP services “lack access to reliable transportation, especially in our more rural areas.” Distance paired with poor infrastructure prevents people in Alabama from accessing potentially lifesaving health care.
“They may have ways to get them around town, a few miles down the street, things like that, but maybe not necessarily two counties over,” says Shaw.
That’s exactly why AIDS Alabama South implemented a clinical van service that travels throughout the 12 counties
it covers in southwest Alabama. It provides people with all the services offered in-house, including free testing for HIV and other sexually transmitted infections, as well as PrEP services.
Thorn and Shaw are proud the agency and its employees are so responsive to clients in need. On numerous occasions, Shaw, along with nurse practitioners, will drive directly to a person in need of an HIV test, PEP or other services. “I’ll just grab a backpack and throw in a set of gloves and a test, and we’ll go meet them at their house,” says Shaw.
Furthermore, AIDS Alabama South has also partnered with specialty pharmacy Avita, a national health care services organization, to easily enroll clients in its ship-to-home pharmacy, which fills and delivers prescriptions to a person’s residence.
“We’re always looking for better ways to serve our community,” says Shaw.
AT AIDS ALABAMA
South, providers consider mental health to be as important as physical health. The agency offers individual, couples and group counseling to people living with HIV.
Sessions aim to help people adjust to and cope with their HIV-positive status as well as other challenges they may be facing, including anxiety, depression, low self-esteem and relationship issues.
The agency also offers individuals who misuse drugs and alcohol a safe space to explore sobriety and provides referrals to help with different forms of addiction.
Clients may also be connected to case managers, who can provide them with a continuum of care, including medical and dental care, housing resources, financial assistance, nutrition support via food pantries and more.
For those who have newly tested positive for HIV, the linkage to care program at AIDS Alabama South allows individuals to attend up to five sessions that cover topics including what to expect when you talk to your doctor, medications and their side effects, adherence, life span and more. The program prioritizes privacy and works with clients to identify the locations and times that work best for their schedule.
Looking to the future, AIDS Alabama South is seeking to add services, such as providing the overdose-reversing medication naloxone, sold under the brand name Narcan, as well as clean needles through a needle/syringe program.
“I believe that having dedicated staff and creating programs specifically for [Black women] to show how much we love and care for them and are here to support them,” says Thorn, “is what has allowed us to be so successful for the women in our community.” ■
poz.com MARCH 2023 POZ 31
“THAT’S HOW WE’RE GOING TO DISPEL THESE BARRIERS: IN BETWEEN HEALTH CARE AND COMMUNITY IMPACT.”
HEROES BY CHARLES SANCHEZ
Sisterhood for All
Krista Martel is the executive director of The Well Project, which educates and empowers women living with or vulnerable to HIV. This year, she marks her 10th anniversary as leader of the organization, which is over two decades old.





Krista is a native of the Chicago area. In 1994, as she was preparing to move to New York City after college, her sister Ellen, then age 32, was diagnosed with HIV. “She had under 100 T cells, so they estimated that she’d had it for eight to 10 years,” says Martel. “This was pre–combination therapy. She was on monotherapy, [Retrovir], for a while, then they added [Videx] and [Zerit].”
Ellen was wasting away. Loved ones would ask whether she had cancer or an eating disorder. “My activism jumped in there,” says Krista, “I was like, If she had cancer, we wouldn’t be afraid. Why do we have to hide this from people?”
Krista advocated for Ellen not only to counter HIV stigma but also to alleviate the shame her sister felt for having had condomless sex. “I didn’t think she should feel guilty about that,” says Krista. Ellen also became an advocate. She participated in clinical trials, volunteered, educated the public and joined the HIV Coalition.



Krista moved to New York, where she waitressed, bartended and worked at flea markets until she interviewed for a receptionist position at a medical education company. “I interviewed with the president of the company, and she said they specialized in HIV education. I told her about my sister and that I was interested in the work.”
Krista had also interviewed for a job at MTV. “I took the job with the medical company and quickly moved up.” That role was just the beginning of what became her life’s work advocating for people living with HIV. “Some work came into the company to do a peer-based treatment program for women. I was able to get involved in that, and that was where I needed to be.”
Ellen died in 1998, just four years after testing HIV positive, of complications related to the virus. “It happened fast. I think ultimately from the ddI and d4T drugs and pancreatitis,” says Krista. “That fuels what I do, because both on the provider education and community-based education sides, having access to information about side effects and interactions is vital,” says Krista.
Krista joined The Well Project in 2009 and was named executive director in 2013. She has been a major force in the expansion of The Well Project and its success in shining a light on and giving voice to diverse women affected by HIV across the country and around the world.
“One of the first key things I did as executive director of The Well Project was to form a community advisory board,” she says. “I know the importance of having women living with HIV be part of all the decision-making.” ■
BILL WALDMAN
32 POZ MARCH 2023 poz.com
Krista Martel marks 10 years at the helm of The Well Project.
If your test result is positive (reactive)
Today, it’s recommended that people living with HIV start treatment as soon as possible. Starting and staying on today’s treatment can help you get to and stay at an undetectable status and prevent transmission of HIV to others through sex. Here are some steps you can take for yourself and your sexual partner(s):
1 3 2
Talk to your healthcare provider
Ask what your test results mean for you and find out about HIV treatments that could best fit your personal routine.
Find out everything you can
The more you know about HIV, the better. You can discover resources by scanning the QR codes, or even find helpful information on your own.
Maintain your sexual health
Use condoms, practice safer sex, and start and stay on the treatment discussed with your healthcare provider.
Help l terms to know
TasP Treatment as Prevention
If you’re living with HIV, current research shows that taking HIV treatment as prescribed and getting to and staying undetectable prevents transmitting HIV to others through sex. This is also known as U=U (undetectable=untransmittable).
PrEP
Pre-Exposure Prophylaxis
Undetectable
A major goal of HIV treatment is getting your viral load to undetectable. Undetectable means that there is so little virus in the blood that a lab test can’t measure it. If you have questions about your lab results and what it means to be undetectable, talk with your healthcare provider.
PrEP (pre-exposure prophylaxis) means routinely taking prescription medicine before you’re exposed to HIV to help reduce your chances of getting it. There are di erent PrEP options available, some of which are 99% e ective. Just remember, PrEP doesn’t protect against other STIs, so be sure to use condoms and other healthy sex practices.
HIV CRIMINALIZATION
HIV CRIMINALIZATION REFERS TO THE USE OF HIV-SPECIFIC LAWS TO PROSECUTE and punish people who have HIV because of their HIV status, not because of their actions. Such laws are outdated and don’t reflect the current science regarding how HIV is and isn’t transmitted. Instead, they put people with HIV at risk of prosecution for allegedly not disclosing their status during consensual sexual activity—even in situations where HIV is not transmitted. Some HIV-specific laws call for longer sentences for certain crimes, such as assault or sex work, simply because a person has HIV. In some states, individuals must register as a sex offender.
HIV criminalization reinforces stigma and discrimination against people living with HIV, which can discourage individuals from getting tested and accessing care and treatment. HIV criminalization also disproportionately impacts the Black, Latino and LGBTQ communities as well as people who engage in sex work.
In the United States, 25 states have HIV-specific laws on the books and nine states have sentencing enhancements that apply to people living with HIV.
STATES WITH HIV-SPECIFIC CRIMINAL LAWS
Arkansas, Delaware, Florida, Georgia, Idaho, Iowa, Kentucky,
Missouri, Nevada, North Carolina, North Dakota, Ohio,
South Dakota, Washington
STATES WITH ENHANCED SENTENCING FOR PEOPLE WITH HIV
Alaska, California, Colorado, Illinois, Wisconsin
STATES WITH HIV-SPECIFIC CRIMINAL LAWS AND ENHANCED SENTENCING FOR PEOPLE WITH HIV
Indiana, Nebraska, Tennessee, Utah
Source: HIV Criminalization in the United States, The Center for HIV Law and Policy, June 2022
Maryland, Michigan, Mississippi,
Pennsylvania, South Carolina,
Louisiana,
Oklahoma,
CA NV AZ WA MT ID OR ND WY SD CO UT NM NE KS OK TX IA WI MO AK HI AR MI MN IL OH IN KY TN FL GA AL MS LA SC NC VA W. VA NY ME PA NH MA VT RI CT NJ MD
DE WASHINGTON, DC
The good news is that there is a growing movement to reform these types of laws. Advocates are working together nationwide—and around the world—to change policies and legislation that discriminate against individuals based on their health status. Thirteen states have already reformed or repealed parts of their HIV-specific criminal laws. Visit poz.com/criminalization to find resources and learn the facts, and then help spread the word and advocate for change.
HOW TO PROTECT YOURSELF AGAINST HIV CRIMINALIZATION EDUCATE YOURSELF
Find out about the specific laws in your state.
DOCUMENT YOUR DISCLOSURE
Having your partner acknowlege your HIV status in writing or in front of a witness may help protect you from prosecution.
KNOW YOUR RIGHTS
If you are accused of an HIV-related crime, exercise your right to remain silent until you talk to a lawyer who is knowledgeable about HIV criminal law.
FEBRUARY 28
HIV IS NOT A CRIME NATIONAL AWARENESS DAY
This day is intended to raise awareness of and promote advocacy around unjust laws that criminalize people living with HIV and discriminate against or stigmatize individuals because of their health status.
1 2 3
If your test result is negative (non-reactive)
When it comes to HIV prevention, the Centers for Disease Control and Prevention (CDC) recommends that ALL sexually active adults and adolescents be informed about PrEP (pre-exposure prophylaxis). PrEP means routinely taking prescription medicine before you’re exposed to HIV to help reduce your chances of getting it. Here are some steps you can take for yourself and your sexual partner(s):
Talk to your healthcare provider
Have a conversation with your healthcare provider about all of your HIV prevention options, including PrEP.
Find out everything you can
Scan the QR codes and explore resources on your own to get tips on how to be proactive about protecting your sexual health, including understanding your HIV prevention options, like PrEP medications.
Maintain your sexual health
Regularly test for HIV and other sexually transmitted infections (STIs), use condoms, and communicate honestly with your partner(s). If you have been prescribed PrEP, continue to take it exactly as prescribed.
Whatever your results may be...
Speak with a healthcare provider:
1. How can I help protect myself and others?
2. How often should I get tested and retested?
3. How can I talk to my partner(s) about my status and theirs?
Share your status with partner(s)
It may not be easy, but having a conversation with your partner(s) about your HIV status can help:
• Normalize the conversation around status, sexual health, and testing
• Empower others to make informed decisions about their sexual health
• Encourage all people to have conversations and stay engaged with their healthcare providers
If your test result (reactive)
Today, it’s recommended that people living with HIV Starting and staying on today’s treatment can help status and prevent transmission of HIV to others take for yourself and your sexual partner(s):
Talk to your healthcare provider
Ask what your test results mean for you and find out about HIV treatments that could best fit your personal routine.
TasP
Find out everything you can
The more you know HIV, the better. discover resources scanning the QR even find helpful on your own.
Help l terms
Treatment as Prevention
If you’re living with HIV, current research shows that taking HIV treatment as prescribed and getting to and staying undetectable prevents transmitting HIV to others through sex. This is also known as U=U (undetectable=untransmittable).
PrEP
Pre-Exposure Prophylaxis
PrEP (pre-exposure prophylaxis) means routinely taking medicine before you’re exposed to HIV to help reduce of getting it. There are di erent PrEP options available, are 99% e ective. Just remember, PrEP doesn’t protect STIs, so be sure to use condoms and other healthy sex
1 2
HEALTHYSEXUAL, GILEAD, and the GILEAD Logo are trademarks of Gilead Sciences, Inc. All other marks are the property of their respective owners. © 2022 Gilead Sciences, Inc. All rights reserved. US-UNBC-1091 12/22
1 3 2
result is positive (reactive)
HIV start treatment as soon as possible. help you get to and stay at an undetectable through sex. Here are some steps you can

everything can know about better. You can resources by QR codes, or information own.
Maintain your sexual health
Use condoms, practice safer sex, and start and stay on the treatment discussed with your healthcare provider.
terms to know
Undetectable
A major goal of HIV treatment is getting your viral load to undetectable. Undetectable means that there is so little virus in the blood that a lab test can’t measure it. If you have questions about your lab results and what it means to be undetectable, talk with your healthcare provider.
taking prescription reduce your chances available, some of which protect against other sex practices.
No
what your
test
your
We can all ght against HIV Resources for you Visit the link above for more information and educational resources about PrEP. Visit the link above for more information and educational resources about HIV treatment. www.Healthysexuals.com www.HelpStopTheVirus.com If you are living with HIV, talk to your healthcare provider about treatment options.
Model portrayal
matter
HIV
results may be, staying educated on how to take care of yourself and
partner(s) is a key step to living a longer and healthier life.
3










































































































































































































 Tami Haught (left) and Kamaria Laffrey are living with HIV.
Tami Haught (left) and Kamaria Laffrey are living with HIV.