




Advocating for people 50 and over living with HIV l
This is only a brief summary of important information about BIKTARVY® and does not replace talking to your healthcare provider about your condition and your treatment.
BIKTARVY may cause serious side e ects, including:
` Worsening of hepatitis B (HBV) infection. Your healthcare provider will test you for HBV. If you have both HIV-1 and HBV, your HBV may suddenly get worse if you stop taking BIKTARVY. Do not stop taking BIKTARVY without fi rst talking to your healthcare provider, as they will need to check your health regularly for several months, and may give you HBV medicine.
BIKTARVY is a complete, 1-pill, once-a-day prescription medicine used to treat HIV-1 in adults and children who weigh at least 55 pounds. It can either be used in people who have never taken HIV-1 medicines before, or people who are replacing their current HIV-1 medicines and whose healthcare provider determines they meet certain requirements.
BIKTARVY does not cure HIV-1 or AIDS. HIV-1 is the virus that causes AIDS.
Do NOT take BIKTARVY if you also take a medicine that contains:
` dofetilide
` rifampin
` any other medicines to treat HIV-1
Tell your healthcare provider if you:
` Have or have had any kidney or liver problems, including hepatitis infection.
` Have any other health problems.
` Are pregnant or plan to become pregnant. Tell your healthcare provider if you become pregnant while taking BIKTARVY.
` Are breastfeeding (nursing) or plan to breastfeed. Talk to your healthcare provider about the risks of breastfeeding during treatment with BIKTARVY. Tell your healthcare provider about all the medicines you take:
` Keep a list that includes all prescription and over-thecounter medicines, antacids, laxatives, vitamins, and herbal supplements, and show it to your healthcare provider and pharmacist.
` BIKTARVY and other medicines may a ect each other. Ask your healthcare provider and pharmacist about medicines that interact with BIKTARVY, and ask if it is safe to take BIKTARVY with all your other medicines.
BIKTARVY may cause serious side e ects, including:
` Those in the “Most Important Information About BIKTARVY” section.
` Changes in your immune system. Your immune system may get stronger and begin to fight infections that may have been hidden in your body. Tell your healthcare provider if you have any new symptoms after you start taking BIKTARVY.
` Kidney problems, including kidney failure. Your healthcare provider should do blood and urine tests to check your kidneys. If you develop new or worse kidney problems, they may tell you to stop taking BIKTARVY.
` Too much lactic acid in your blood (lactic acidosis), which is a serious but rare medical emergency that can lead to death. Tell your healthcare provider right away if you get these symptoms: weakness or being more tired than usual, unusual muscle pain, being short of breath or fast breathing, stomach pain with nausea and vomiting, cold or blue hands and feet, feel dizzy or lightheaded, or a fast or abnormal heartbeat.
` Severe liver problems , which in rare cases can lead to death. Tell your healthcare provider right away if you get these symptoms: skin or the white part of your eyes turns yellow, dark “tea-colored” urine, light-colored stools, loss of appetite for several days or longer, nausea, or stomach-area pain.
` The most common side e ects of BIKTARVY in clinical studies were diarrhea (6%), nausea (6%), and headache (5%).
These are not all the possible side e ects of BIKTARVY. Tell your healthcare provider right away if you have any new symptoms while taking BIKTARVY.
You are encouraged to report negative side e ects of prescription drugs to the FDA. Visit www.FDA.gov/medwatch or call 1-800-FDA-1088.
Your healthcare provider will need to do tests to monitor your health before and during treatment with BIKTARVY.
Take BIKTARVY 1 time each day with or without food.
` This is only a brief summary of important information about BIKTARVY. Talk to your healthcare provider or pharmacist to learn more.
` Go to BIKTARVY.com or call 1-800-GILEAD-5.
` If you need help paying for your medicine, visit BIKTARVY.com for program information.














Scan or visit BIKTARVY.com to learn more.
People featured are compensated by Gilead.
















†For commercially insured eligible patients only. Restrictions apply. Subject to change. See terms and conditions at GileadAdvancingAccess.com.










Person featured is compensated by Gilead.






Our roster of bloggers spans the diversity of the HIV community. Go to poz.com/blogs to read varying points of view from people living with the virus as well as from HIV-negative advocates. Join the conversation in the comments section. Visit the blogs to nd hope and inspiration from others.
D POZ OPINIONS

Advocates, researchers, politicians, thought leaders and folks just like you all have ideas worth sharing. Go to poz.com/ opinions to read about topics such as living with HIV, improving care and treatment, increasing prevention e orts and ghting for social justice.
#UNDETECTABLE

The science is clear: People who have an undetectable viral load don’t transmit HIV sexually. In addition to keeping people healthy, e ective HIV treatment also means HIV prevention. Go to poz.com/undetectable for more.

Scan the QR code (le ) with your smartphone camera or go to poz.com/digital to view the current issue and read past issues online.

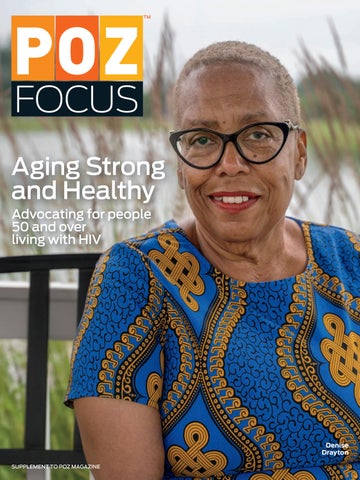
Denise Drayton is an advocate for people 50 and over living with HIV.

Magic Johnson to headline the 2025 United States Conference on HIV/AIDS • awareness day honors long-term survivors • new center for HIV cure research unveiled • raising awareness of fatty liver disease • advocating for access to Medicare without penalties • getting stuck in the health appeals process
Editor-in-Chief: Oriol R. Gutierrez Jr.
Managing Editor: Jennifer Morton
Deputy Editor: Trent Straube
Science Editor: Liz Highleyman
Copy Chief: Joe Mejía
Art Director: Doriot Kim
Production Manager: Michael Halliday
POZ Focus is independently produced by Smart + Strong.
Taurine is an inconsistent biomarker of aging • eating healthier in midlife tied to less chronic disease as people age • guiding lifestyle changes to improve health • new drugs may slow biological aging for those living with HIV
Aging With Power: People living with HIV growing older don’t have to do so alone.
SMART + STRONG
President & COO: Ian E. Anderson
VP, Integrated Sales: Diane Anderson
Integrated Advertising Manager: Jonathan Gaskell
Integrated Advertising Coordinator: Sarah Pursell
The long-term survivor will headline the conference.
HIV organization NMAC, in partnership with Alchemy, which builds and operates in-house pharmacies, has announced that the basketball legend Earvin “Magic” Johnson, a renowned entrepreneur and advocate for people living with HIV, will headline this year’s United States Conference on HIV/AIDS (USCHA) in Washington, DC, which will take place from September 4 to 7. He’s currently chairman and CEO of Magic Johnson Enterprises.
Johnson’s celebrity stature and his lived experience underscore 2025 USCHA’s theme of “Aging With HIV,” which will celebrate the lives of people living with HIV as a testament to the biomedical progress in HIV antiretroviral treatment. USCHA will also highlight racial and health disparities that drive up HIV rates in communities of color and defy the stigma that deters people from accessing effective prevention and treatment options.
“I’ve lived through every phase of the HIV epidemic—from the fear and grief of the early days to the transformative breakthroughs that have turned HIV into a manageable chronic condition,” said Johnson. “For decades, I’ve worked to raise awareness around HIV treatment and prevention through my foundation, and partnering with Alchemy is the next chapter in that mission. Together, we’re building pharmacies inside HIV-focused clinics and making sure everyone, no matter where they live, has access to the highquality, affordable care they deserve.”
Johnson continued, “As someone who’s been living with HIV for more than 30 years, I’m honored to now extend that partnership through Alchemy to work with NMAC and keynote this year’s USCHA and speak about what it means to age—and thrive—with HIV.”
Harold Phillips, deputy director of programs at NMAC, said, “HIV may not be making headlines the way it once did, but it remains a pressing crisis—especially for communities of color and LGBTQ individuals, who continue to face systemic barriers to health care. The lack of mainstream coverage can make it seem like the epidemic is behind us, but the reality is far different. And now, with unprecedented funding cuts and the erosion of bipartisan support for the programs that have held our HIV infrastructure together, we find ourselves at a critical crossroads.”
Phillips added, “That’s why I am especially grateful for our growing partnership with Alchemy, which has created an incredible opportunity to bring USCHA to the forefront as a platform to amplify the voice of Earvin ‘Magic’ Johnson. As someone who is also living and aging with HIV, I deeply understand the importance of visibility and leadership. More than 50% of people living with HIV are now over 50, and Johnson’s unwavering advocacy resonates profoundly with the work we do at NMAC. His dedication reflects the mission of USCHA—uniting the HIV community, celebrating resilience and driving action. His voice, alongside ours, is a powerful reminder that this fight is far from over.” —NMAC





Honoring
An awareness day addresses their journeys.
Thursday, June 5, marked HIV Long-Term Survivors Awareness Day (HLTSAD), an annual observance that honors long-term survivors of HIV and raises awareness about their unique needs and journeys.
“Leading With Legacy” was this year’s theme.

Earvin
“Magic” Johnson
Launched in 2014 by Let’s Kick ASS—AIDS Survivor Syndrome, HLTSAD coincides with a significant milestone in history: the date in 1981 when the Centers for Disease Control and Prevention (CDC) published the first report of what would come to be known as AIDS.
The report detailed five cases of a mysterious disease affecting young gay men and as such is considered by many to mark the start of the AIDS epidemic. Effective treatment for HIV— combination antiretroviral therapy—did not become available until 15 years later, in 1996.
Several decades later, the narrative surrounding HIV has evolved from one characterized by fear and stigma to one marked by hope and progress.
Today, about 50% of people with HIV in the United States are over 50 years old, according to the CDC. By 2030, 70% of people with HIV will be over age 50. —Laura Schmidt
The Wistar Institute unveiled a new center dedicated to finding a cure for HIV and other viral diseases, according to Philly Voice.
Philadelphia-based Wistar is a top independent nonprofit specializing in researching HIV and other infectious diseases, cancer and immunology. Wistar’s new $24 million center, the HIV Cure and Viral Diseases Center, aims to advance HIV cure research and boasts more than 25,000 square feet, including laboratories. This expansion marks the first in Wistar’s more than 130-year history and comes at a critical time for biomedical research, as the Trump administration continues to slash funding in several areas of research.
Led by executive vice president Luis Montaner, DVM, DPhil, the center brings together top scientists, community leaders and public health champions to address some of the world’s most pressing health challenges.
“I am confident we will advance toward an HIV cure in my lifetime,” Montaner told Philly Voice. “With the launch of this center, Wistar makes a clear and bold statement that the time to get us to an HIV cure is now.”
Worldwide, more than 39 million people are living with HIV, including more than 18,000 in Philadelphia.
Medical advances have made HIV highly treatable with

antiretroviral medications, which have enabled many people living with HIV to achieve and maintain an undetectable viral load, which means they cannot transmit HIV to others (known as Undetectable Equals Untransmittable, or U=U). What’s more, safe and effective prevention options for HIV-negative people include pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP).
Despite these lifesaving advancements in HIV research, scientists worldwide continue to search for a lasting cure that doesn’t require daily medication.
With support from world-renowned scientists, research experts and community leaders, the new center aims not only to find a cure for HIV but also to yield insights into the treatment of other viral infections. —Laura Schmidt
Advocates seek to elevate liver health.
On the second Thursday in June, Global Fatty Liver Day (formerly International NASH Day) spotlighted one of the most widespread yet under-addressed health threats of our time: fatty liver disease, increasingly referred to as steatotic liver disease in clinical settings.
Hosted annually by Global Liver Institute (GLI), this public awareness campaign raises awareness of this silent epidemic and its deep roots in global metabolic health challenges.
Fatty liver disease, including


metabolic dysfunction-associated steatotic liver disease (MASLD), metabolic dysfunction-associated steatohepatitis (MASH) and metabolic dysfunction-associated alcoholrelated liver disease, impacts millions globally—yet most remain undiagnosed and untreated. Once considered rare, fatty liver disease has surged in parallel with rising rates of obesity, diabetes and other metabolic conditions.
An estimated 30.2% of the global population now lives with MASLD, with rates soaring to 57.5% among adults with obesity. In the United States alone, more than 122 million adults are projected to be affected by 2050.
Larry R. Holden, president and CEO of GLI, stated, “The liver is no longer the silent organ. Fatty liver disease is now one of the clearest and most urgent signs of global metabolic dysfunction. On Global Fatty Liver Day, we call on health
care leaders, policymakers and the public to recognize the liver’s central role in preventing not just liver disease but cardiovascular disease, diabetes and other noncommunicable diseases. Liver health must rise to the top of public health agendas globally.”
Fatty liver disease develops when excess fat accumulates in the liver, o en without symptoms in its early stages. Le unaddressed, it can progress to inflammation, fibrosis, cirrhosis, liver cancer and even death. In fact, MASH is now one of the leading causes of liver transplantation in the United States.
But fatty liver disease doesn’t occur in isolation: Up to 75% of people with type 2 diabetes also have MASLD; over 70% of people with MASLD also live with obesity; and between 20% and 80% of individuals with high cholesterol or triglycerides are also affected by fatty liver disease. —GLI
These penalties are burdensome
At NMAC, we celebrate the courage of those who fought through the darkest days of the epidemic and now stand as pillars of our movement—advocates, elders and mentors in the ongoing fight to end the HIV epidemic. But celebration also requires action.
Many long-term survivors face unique challenges as they age, especially when it comes to navigating the health care system and psychosocial services. One critical issue is accessing Medicare without penalty.
For some long-term survivors— especially those who returned to work, lost access to disabilitybased Medicare or are retiring and enrolling in Medicare later than expected—reenrolling can come with unexpected costs.
If you delay enrollment in Medicare Part A, B or D without having other creditable coverage, you may face late enrollment penalties,
some of which last a lifetime:
• Part B (doctor visits, outpatient care): Delaying enrollment can result in a lifetime 10% increase in premiums for each 12 months you were eligible but did not enroll.
• Part D (prescription drug coverage): The penalty adds 1% of the national base premium for each uncovered month, again, for life.
• Part A (hospital insurance): If you buy it late, your premium can rise by 10% for twice the number of years you delayed.
These penalties are especially burdensome for older survivors living on fixed incomes who may have been uninsured or underinsured at key moments.
No one who has lived through this epidemic, who has fought for survival and dignity, should be penalized for system gaps or outdated policies. We call on federal policymakers to:
• Create waivers or exemptions for late enrollment penalties for older people living with HIV;
• Expand outreach and education so long-term survivors understand their Medicare rights and deadlines;
• Ensure special enrollment periods are better publicized and accessible to all.
As we celebrate the strength and stories of long-term survivors, we must also fight for the policy chang-

Doctors complain that insurance denials are worse than ever.
Health insurers issue millions of denials every year. Many patients find themselves stuck in a convoluted appeals process marked by long wait times, frustrating customer service encounters and decisions by medical professionals they’ve never met who may lack relevant training.
Recent federal and state efforts as well as changes undertaken by insurance companies themselves have attempted to improve a 50-year-old system that disproportionately burdens some of the sickest patients at the worst times. And yet many doctors complain that insurance denials are worse than ever, as the use of prior authorization has ramped up in recent years, reporting by KFF Health News and NBC News found.

While the killing of UnitedHealthcare chief executive Brian Thompson in 2024 incited a fresh wave of public fury about denials, there is almost no hope of meaningful change on the horizon, said Jay Pickern, DBA, an assistant professor of health services administration at Auburn University.
Prior authorization varies by plan but o en requires patients or their providers to get permission (also called precertification, preauthorization or preapproval) before filling

prescriptions or scheduling imaging, surgery or an inpatient hospital stay, among other expenses.
The practice isn’t new. Insurers have used prior authorization for decades to limit fraud, prevent patient harm and control costs. In some cases, it is used to intentionally generate profits for health insurers, according to a 2024 U.S. Senate report. By denying costly care, companies pay less for health care expenses while still collecting premiums.
For most patients, though, the process works seamlessly. Prior authorization mostly happens behind the scenes, almost always electronically, and nearly all requests are quickly, or even instantly, approved.
But the use of prior authorization has also increased in recent years. That’s partly due to the growth of enrollment in Medicare Advantage plans, which rely heavily on prior authorization compared with original Medicare. Some health policy experts also point to the passage of the Affordable Care Act in 2010, which prohibited health insurers from denying coverage to patients with preexisting conditions, prompting companies to find other ways to control costs. —KFF Health News
The amino acid gained popularity as a dietary supplement.
Scientists at the National Institutes of Health (NIH) have found that levels of circulating taurine, a conditionally essential amino acid involved in multiple important biological functions, is unlikely to serve as a good biomarker for the aging process. In blood samples from humans, monkeys and mice, scientists found that circulating taurine levels o en increased or remained constant with age.
Analysis of longitudinal data showed that within-individual differences in taurine levels o en exceeded age-related changes. Researchers also found that taurine levels were inconsistently associated with health outcomes across age, species and cohorts, suggesting that declining taurine is not a universal marker of aging. Instead, its impact may depend on individual physiological contexts shaped by genetic, nutritional and environmental factors. Results are published in Science.
Taurine recently gained popularity as a dietary supplement due to recent research that found supplementation with taurine improved multiple age-related traits and extended lifespan in model organisms (worms and mice). However, there is no solid clinical data that shows its

supplementation benefits humans.
“A recent research article on taurine led us to evaluate this molecule as a potential biomarker of aging in multiple species,” said Rafael de Cabo, PhD, study coauthor and chief of the Translational Gerontology Branch at NIH’s National Institute on Aging (NIA).
Researchers also found that the relation between taurine and muscle strength or body weight was inconsistent. For example, analyses of gross motor function highlight the limitations of considering solely circulating taurine changes as indicative of biological aging, as comparatively low motor function performance can be associated either with high or low concentrations of taurine, whereas in other cases, no relation at all is found between these variables.
“Identifying reliable biomarkers to predict the onset and progression of aging and functional decline would be a major breakthrough, enabling more effective, personalized strategies to maintain health and independence into old age,” emphasized Luigi Ferrucci, MD, PhD, study coauthor and scientific director at NIA. This study was funded by the in-house research program at NIH/NIA. —NIH
Eating healthier in midlife is tied to less chronic disease as people
Several studies have shown links between healthy eating and prevention of chronic diseases, like diabetes or heart disease. Others have found ties between a high-quality diet and longer life. But less common are studies that examine the links between various dietary patterns and healthy aging overall, including the longterm impact of midlife food choices.
A research team examined data gathered in two long-term studies of health


and lifestyle. The Nurses’ Health Study enrolled women ages 30 to 55 years, and the Health Professionals Follow-Up Study enrolled men ages 40 to 75 years.
The team assessed participant data every four years beginning in 1986 for up to 30 years. Participants were excluded if they had a serious chronic disease at the start. The final study population included about 70,000 women and 35,000 men, for a total of more than 105,000 participants. Results appeared in Nature Medicine.
The researchers first examined how closely each participant’s selfreported eating patterns adhered to eight different
healthy diet patterns. Among these were the Alternative Healthy Eating Index, the DASH diet (Dietary Approaches to Stop Hypertension, which is supported by the National Institutes of Health, or NIH), the MIND [Mediterranean Intervention for Neurodegenerative Delay] diet, the Planetary Health Diet Index and a Mediterranean diet. They also looked at intake of ultra-processed foods.
The team then assessed the links between adherence to each eating pattern and healthy aging at age 70 or older. They found that over 9% of participants, about 9,800 people, had achieved healthy aging. That is, they were free of
major chronic disease and had positive measures of cognitive, physical and mental health.
Those who most closely followed the Alternative Healthy Eating Index were most likely to have healthy aging by age 70. The same held true by age 75. Those who mostly closely adhered to any of the other healthy eating patterns also boosted their odds. Regardless of diet, people who ate more fruits, vegetables, whole grains, unsaturated fats, nuts, legumes and low-fat dairy were more likely to have healthy aging. Healthy aging was less likely in those who ate more trans fats, salt, sugary drinks and red or processed meats. —NIH
The goal is to guide lifestyle changes that improve health.
Age and health are clearly connected. Yet people of the same age can show vast differences in overall health. Some have chronic conditions by midlife, while others have a clean bill of health into their 70s and beyond.
One theory holds that such differences stem from variation in biological aging. This is the extent of damage that builds up across tissues and organs, leading to chronic conditions, physical decline and disability.
Existing measures of biological age, such as the Frailty Index, try to capture a person’s health based on the number of health deficits they have. But these approaches don’t fully capture the complexity of biological aging.
Researchers from the University of Washington School of Medicine and National Institute on Aging at the National Institutes of Health (NIH) wanted to develop a better way. Their method, called the Health Octo Tool, is described in Nature Communications.
To develop the tool, the team turned to data from multiple long-term studies that included more than 40,000 people. First, the researchers defined disease states and their severity for each of 13 major organ systems based on accepted medical criteria. These systems included cardiovascular, kidney, metabolic, gastrointestinal and liver, respiratory, thyroid, blood, oral health, bones and muscles, sensory and the central nervous system. The team also considered whether a person had a history of stroke or cancer.
The analysis of organ-specific disease was used to predict what the researchers call Bodily Organ-Specific Clocks. Then, by combining all the organ systems together, they created a measure, called the Body Clock, that captures a person’s overall health state without regard to chronological age.
The team found that the Body Clock accurately predicted a person’s performance on a short assessment used to gauge physical functioning, including balance, walking speed and strength. It also predicted disability and mortality with more than 90% accuracy. The Body Clock predicted health outcomes better than the Frailty Index.








The hope is that the Health Octo Tool will contribute to development of more effective lifestyle and health care strategies. Its use could suggest personalized interventions by identifying health declines early. —NIH



New drugs may slow biological aging for those living with the virus.
Semaglutide and related weight-loss medications may help reduce infl ammation, improve cognitive function and gut health, reduce alcohol use and even slow biological aging in people living with HIV, according to studies presented at this year’s Conference on Retroviruses and Opportunistic Infections.
Weight gain and metabolic abnormalities are a growing concern for people with HIV as they age, raising the risk for cardiovascular disease, fatty liver disease and other health problems.
Glucagon-like peptide-1 (GLP-1) receptor agonists, such as semaglutide (Ozempic or Wegovy), mimic a natural hormone that suppresses appetite, regulates insulin and blood sugar and slows emptying of the stomach. Originally developed to treat type 2 diabetes, these drugs are now widely used to manage obesity. They have been shown to reduce the risk of heart and kidney disease and some types of cancer, and ongoing research continues to show additional and sometimes unexpected benefits.
“While we know some of the types of benefits [related to] metabolic health, this new data points to potential aging benefi ts. It suggests that GLP-1 agonists may be helpful in stabilizing biological aging in a subset of people living with HIV,” investigator Michael Corley, PhD, of the University of California San Diego, said at the conference.
Case Western Reserve University researchers investigated the effect of semaglutide on neurocognitive function, asking whether changes in fat or inflammatory markers could explain the drug’s benefits.
“Semaglutide has shown a potential beneficial impact on cognitive function, specifically the visuospatial cognitive subdomain in people living with HIV,” the researchers concluded. “This effect appears to be mediated by the effect of the drug on attenuating infl ammation and not on adiposity [excess body fat].” —Liz Highleyman






BY TIM MURPHY
ARACELIS QUINONES, 60, of Queens, New York, who has been living with HIV since 1988, has been running a monthly Spanish-language support group for Latinos with HIV, Poder Latino, for the past 25 years. Thanks to 21stcentury treatment, her HIV has long been well managed.
But in recent years, she has felt overwhelmed by an accumulation of other health conditions—high blood pressure, osteoporosis, spinal stenosis, atrial fibrillation, arthritis— not to mention anxiety associated with managing the many medications she must now take in addition to her HIV meds. It’s a common scenario for folks aging with HIV, who often experience the onset of typical aging-related conditions up to a decade earlier than those without the virus, as ample research has shown.
“I feel like I’m getting a new diagnosis all the time, having new pains, and sometimes it gets scary,” she says. “It’s not just the stigma of having HIV but of aging in general.” She adds, “If it wasn’t for the network I have through NMAC’s 50+ Strong and Healthy and its National HIV & Aging Advocacy Network [NHAAN], I don’t know what I’d do.”
Quinones is referring to two groups at the longtime nonprofit NMAC (formerly known as the National Minority AIDS Council). The first is an aging-with-HIV peer support and information-exchange group; the second focuses on advocacy actions for that cohort, including how members can become educators and trainers in their own communities as well as lobby for programs at the federal, state and local levels.
Quinones says both groups empower folks aging with HIV to take action, because they enable them to meet others like them who’ve already done so. “You say to yourself, ‘Oh my goodness, if they’re doing it, I’m going to do it also,’” she says. “It motivates and inspires you because you feel safe and like you’re not the only one, especially at times when it feels like the world is ending.”
Since she became involved with the groups several years ago, Quinones has joined NHAAN’s executive committee, helping to organize quarterly Zoom meetings that draw, in her words, “huge attendance.” She’s also part of NHAAN’s subgroup for women—one of many groups within the group.
As part of NHAAN, she attended AIDSWatch, an annual meetup for people living with HIV in Washington, DC, organized by AIDS United that includes visits to Capitol Hill lawmakers to lobby for continued HIV funding (currently quite a challenge given a Trump-aligned GOP congressional majority’s ambition to slash social spending programs).
She’s also a recipient of an NHAAN $2,500 mini grant, which she’s used to spark education and advocacy efforts around aging with HIV in her own community.
With the money, she’s been able to invite groups of up to 60 people aging with HIV to discussions at the Latino Commission on AIDS, where she works the front desk. “We had a lawyer talk to us about immigration laws, HIV criminalization laws and how to survive and thrive and not feel that this is the end of days.”
And she has glowing words for Moisés Agosto, NMAC’s longtime director of treatment. “He’s our leader and an inspiration,” she says. “He’s been doing this work for so many years now, since the early ACT UP days, and he also shares his own story of aging with HIV. Thank you, Moisés, for opening your heart and showing that we cannot only survive but achieve our goals.”
AGOSTO, 60, A PUERTO RICAN GAY MAN WHO was diagnosed with HIV in 1986, has been an HIV advocate, especially for Latinos and communities of color, since ACT UP’s heyday in the late ’80s and early ’90s. (He was on the cover of POZ in 1997.) Agosto says starting both 50+ and NHAAN through his job at NMAC is one of his most important accomplishments ever.
In 2016, he says, “there was a lack of discussion of the issues facing older adults living with HIV and their visibility in the HIV community.” He notes that people living with HIV who are 50 and over are on track to make up 70% of all people living with HIV by 2030.
But the health systems that have been established for people with the virus, including via the Ryan White CARE Act (RWCA), were not designed to respond to the needs of older adults living with HIV. (For example, RWCA doesn’t necessarily cover visits to gerontologists, who can examine an aging patient in a holistic manner.)
He adds, “Research is showing that individuals with HIV often present with early and multiple comorbidities [health issues other than HIV], highlighting the need to build capacity in our health systems and increase health literacy and prevention efforts.”
Under Agosto’s leadership, the 50+ group made its public debut at the 2016 U.S. Conference on HIV and AIDS (USCHA, hosted annually by NMAC). “We made people over 50 very visible there and had them all come up onstage with their HIV 50+ Strong and Healthy T-shirts on,” he says. A few of them, like veteran activist Lillibeth Gonzalez of New York City, addressed the crowd.
After that, picking up the tab to get 50+ members to USCHA became a priority for the group. It then dispatched participants home with the aforementioned $2,500 grants to set up webinars and live events in their communities. The programs focused on issues related to diabetes, cardiovascular disease, mental health, polypharmacy [managing interactions among medications for many different conditions], HIV drug resistance, healthy living through exercise, diet and smoking cessation, and getting involved with federal, state and local advocacy for programs and funding.
NMAC also sends members of the 50+ and NHAAN cohort—which increases by roughly 50 new selected individuals every year—to different conferences throughout the year to deliver presentations. NHAAN was formed in 2019, says Agosto, because members of 50+ “thought that just building community wasn’t enough” and “there had to be some sort of a body to organize around policy and activism.” NHAAN now has close to 200 members, he says, and hosts quarterly online meetings. The group also holds a briefing day for AIDSWatch participants before they head to visit their representatives on Capitol Hill to bring them up to speed on the current status of key programs, including Medicaid, Medicare and RWCA.
Drayton is a member of NMAC’s 50+ Strong and Healthy group.
Agosto says the NMAC aging programs are distinct from national networks like

Aracelis Quinones tested HIV positive in 1988.

The Reunion Project and Let’s Kick ASS—AIDS Survivor Syndrome, which serve HIV longterm survivors (including those born with HIV) who are not necessarily 50 and over. True to NMAC’s founding mission, members of the 50+ group and NHAAN are mostly people of color, although the groups welcome white members as well. Agosto says those interested in applying to be a 50+ fellow should check the NMAC home page (nmac.org) at the beginning of every year— this is where NMAC posts a call for applicants. Those in-
“IT’S NOT JUST THE STIGMA OF HIV BUT OF AGING IN GENERAL.” —ARACELIS QUINONES
terested in joining NHAAN, which has no selection process, should email him at magosto@ nmac.org or Audrianna “Dri” Marzette, the associate manager for NMAC’s treatment program, at amarzette@nmac.org.
Agosto says he’s proud that the 50+ group and NHAAN have meant that “people who weren’t very involved or visible have found a platform where they can develop themselves as leaders.” He acknowledges that the climate for HIV advocacy in Washington, DC, is currently challenging, which is one of the reasons that this year’s
USCHA, taking place September 4 to 7 in DC, will center the theme of aging with HIV.
“The climate is hostile right now, but that doesn’t mean you stop pushing,” he says. That’s not an option, he adds, at a time when Medicaid, which covers health care for 40% of Americans with HIV, is on the chopping block—potentially leading to cuts that would crowd countless people with HIV onto Ryan White’s AIDS Drug Assistance Program, the payer of last resort.
Because federal support is fragile right now, says Agosto, “we’re currently developing a training manual for folks to be active with their local and state reps.” The manual was born in part from a session NHAAN held at this year’s AIDSWatch on exactly that topic.
Agosto admits that his own anxiety about aging with HIV around the time he turned 50 helped inspire him to form 50+ and NHAAN. “A year or two ago, I was diagnosed with both neuropathy and diabetes, and I’ve always had cardiovascular disease,” he says. “I’m controlling the diabetes now with a GLP-1 agonist [a weight loss drug], but it also required a big adjustment in my diet, eliminating empty carbs and sugar and adding more fiber, vegetables and lean protein, like chicken and fish.”
He says his recent health challenges have triggered memories of getting opportunistic infections back in the ’80s and ’90s, before his HIV was well controlled. “I’m not trying to sound like a victim, but it’s still a challenge. I thought that after getting my HIV under control years ago, I was going to have a break from health scares.”
Drayton also credits the 50+ group with helping her get and stay on the Mediterranean diet, which research has found to be healthiest for aging folks, whether or not they are living with HIV. (The Mediterranean diet emphasizes the consumption of lean protein, fruits and vegetables and olive oil.) “A family of like-minded people are here to support and help one another,” she says of the members of the 50+ group.
Another member of the 50+ group and NHAAN is Joey Pons, 57, of San Juan, who was diagnosed in 1988 and is a longtime fellow Puerto Rican friend of Agosto. Formerly the head of the Puerto Rico office of the federal program Housing Opportunities for Persons with AIDS (HOPWA), Pons says he has helped fine-tune some education components of the 50+ group and NHAAN.
For example, he says, “the financial stability module used to only say ‘You need to have accessible housing,’ but it lacked the ‘How do I get it?’” The module, he says, has since been upgraded with resources specific to every region.
“A FAMILY OF LIKE-MINDED PEOPLE ARE HERE TO SUPPORT AND HELP ONE ANOTHER.”
—DENISE DRAYTON
at the nonprofit Ribbon—A Center of Excellence for Healthy Aging with HIV, where she supports initiatives concerning aging with HIV, is another member of the 50+ group and is part of NHAAN’s executive committee.
Diagnosed with HIV in 1993, Drayton moved a few years ago from her longtime Brooklyn home to the Maryland suburbs to be closer to her sister. She says the NMAC groups have “given me an opportunity to learn more about aging with HIV, so I can pass on that education in my day job.” (She’s also a member of the NHAAN Women of Color subgroup.)
The 50+ group has been particularly helpful for her, she says, because as a nondriver in the Maryland suburbs, where services are scattered, she’s had to rebuild an HIV and health support network for herself. Thanks in part to the 50+ group, she’s now connected with fellow long-term survivor Melanie Reese of Baltimore’s senior HIV network Older Women Embracing Life; she’ll also be joining her area’s RWCA Community Advisory Board.
He also helped the group record Spanish-language trainings on topics including diabetes, heart disease and advocacy—“like when a local or state budget is being negotiated, you can play a role in trying to expand services in rural areas.” The trainings will be released at USCHA in September.
Plus, he says, being in the 50+ group has helped him with some of his own aging issues, such as getting his drinking under control and dealing with depression from his own perception that he is not as desirable as he was in his youth.
“All of us are living under stress with this administration,” he says, so the 50+ group “is a way for us to socialize, vent and feel supported.”
Yet another 50+ and NHAAN member is Jeffery Haskins, 70, of Philadelphia, who was diagnosed with HIV in 1993. A major aging issue for him is exhaustion, even as he continues to work part-time for the clinical education division of the longtime HIV care and advocacy group Philadelphia FIGHT. “I emceed a program [recently], and I’m just wiped out now,” he says.
He says the 50+ group “has given me a purpose and centered me. And it has helped me deal with my own issues around aging because I’m in contact with so many people dealing with the same situations I have.”
According to Agosto, that’s exactly why he started 50+ Strong & Healthy in the first place. “If I hadn’t found community as a gay man living with AIDS a long time ago, I wouldn’t be here—honestly,” he says. “That’s how much I value community, because it helps us figure out ways to support one another, including those local referrals.”
He adds, “Community can give you many things—it all depends on what you need.” Q




