

2025
LEGISLATIVE WRAP UP

Healthcare Symposium Delivers HOD Wrap Up
Richard Waters, MD Honoring a Legacy
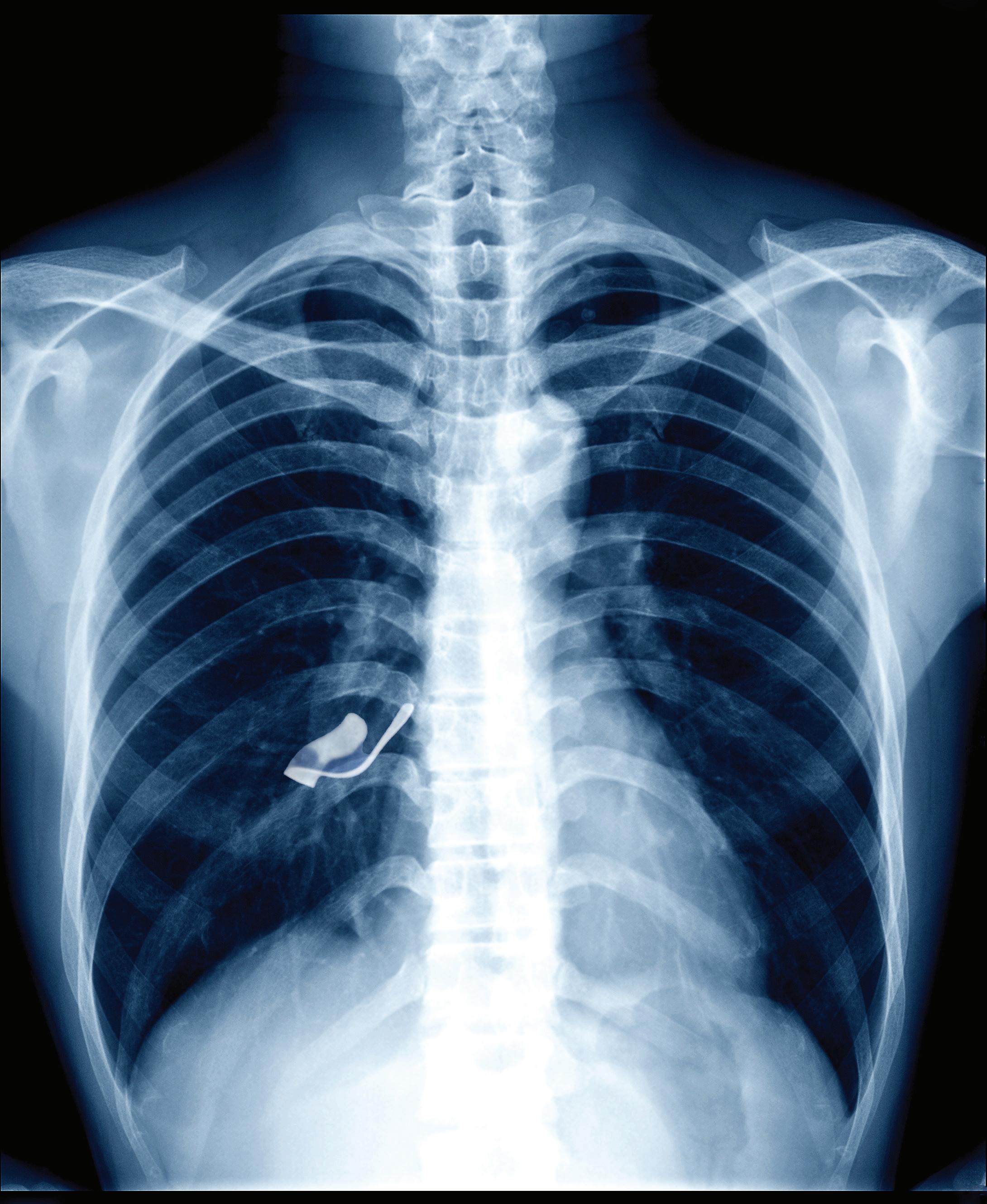
11 days after appendectomy, tests for acute abdominal pain revealed a
retained object
left inside the patient.
Surgical miscounts are considered never events because they are usually preventable by following established procedures.
ProAssurance offers risk assessments designed to help practices minimize errors by establishing and evaluating safety procedures and communication protocols.
With reliable procedures in place, our insureds are more likely to reduce errors in their medical practice, avoid claims, and make claims more defensible if they do occur.



PRESIDENT Sujeeth Punnam, MD
PRESIDENT ELECT Stephen Tsang, MD
TREASURER Sanjeev Goswami, MD
BOARD MEMBERS Maggie Park, MD, Alain Flores, MD, Manreet Basra, MD, Kinnari Parikh, MD, Bhagya Nakka, MD, Sunny Philip, MD, Rahuljit Bajwa, MD, Neelesh Bangalore, MD and Dheeraj Nandanoor, MD
MEDICAL SOCIETY STAFF
EXECUTIVE DIRECTOR Lisa Richmond
MEMBERSHIP COORDINATOR Jessica Peluso
COMMITTEE CHAIRPERSONS
CMA AFFAIRS COMMITTEE James Halderman, MD
CMA TRUSTEE Ramin Manshadi, MD
DECISION MEDICINE Kwabena Adubofour, MD
MEDICAL EDUCATION PROGRAMS Kelly Savage, MD
SCHOLARSHIP LOAN FUND Alexander Fodor, MD
CMA HOUSE OF DELEGATES REPRESENTATIVES
Aisha Chaudhry, MD, Dheeraj Nandanoor, MD, James R. Halderman, MD, Raissa Hill, DO, Richelle Marasigan, DO, Philip Edington, MD, Sujeeth Punnam, MD, Ripudaman Munjal, MD, Stephen Tsang, MD, Alberto Del Pilar, MD
SAN JOAQUIN PHYSICIAN MAGAZINE
EDITOR Lisa Richmond
EDITORIAL COMMITTEE Lisa Richmond, Sujeeth Punnam, MD
MANAGING EDITOR Lisa Richmond
CREATIVE DIRECTOR Sherry Lavone Design
CONTRIBUTING WRITERS Sujeeth Punnam, MD, Joan Duwve, MD, MPH, King Lomotos, MPH, CIC, Pooja Vyas Patel, MS RDN and Wendy Howard, CLE THE SAN JOAQUIN PHYSICIAN MAGAZINE is produced by the San Joaquin Medical Society
SUGGESTIONS, story ideas are welcome and will be reviewed by the Editorial Committee.
PLEASE DIRECT ALL INQUIRIES AND SUBMISSIONS TO: San Joaquin Physician Magazine 3031 W. March Lane, Suite 222W Stockton, CA 95219
Phone: (209) 952-5299 Fax: (209) 952-5298
E-mail Address: lisa@sjcms.org
MEDICAL SOCIETY OFFICE HOURS: Monday through Friday 8:00am - 4:00pm


The 2026 AMG GLE 53 Coupe
Performance. Precision. Presence.
Whether you’re driving through the city or escaping to the Sierra Mountains, the 2026 AMG GLE 53 Coupé delivers performance, safety, and luxury in every mile. Its handcrafted AMG engine and 4MATIC+ all-wheel drive provide power and confidence on any road, while the sleek coupe design blends athletic style with everyday versatility. Inside, premium materials and advanced technology create a cabin that’s both refined and connected. Every drive in the AMG GLE 53 Coupe is an experience in power, precision, and pure Mercedes-Benz luxury.



THE VALUE OF MEMBERSHIP
Advocacy. Education. Community.
SJMS is always looking for opportunities to better serve its members. We know physicians join for many reasons—personal benefits, leadership development, networking, and more. This year, the board proudly added a continuing medical education event to that list. Our inaugural Fall Symposium, Cardiology Updates for Non-Cardiologists, was held on Saturday, September 27, and was a tremendous success. I hope you’ll enjoy the feature story on page 32, and we look forward to welcoming you again next year.
Advocacy remains one of the most meaningful—though sometimes less visible— benefits of membership in SJMS and the California Medical Association. Each year, seven dedicated SJMS Delegates represent our region at the CMA House of Delegates, joining hundreds of physicians from across the state to shape policy and guide the future of medicine. This year, delegates examined the impact of federal proposals affecting healthcare coverage, workforce development, and public health programs. We are grateful to Delegates Drs. Sujeeth Punnam, James Halderman, Raissa Hill, Richelle Marasigan, Alberto Del Pilar, and Dheeraj Nandanoor, and to our CMA Trustee, Dr. Ramin Manshadi. Thank you for your service!
If you are passionate about policy, governance, and legislation, we are currently recruiting leaders to serve as Alternate Delegates. Please contact Lisa Richmond at Lisa@sjcms.org for more information.
Don’t miss our most popular annual presentation, Medicare Changes for 2025 and Beyond, by Cheryl Bradley, Associate Director of the CMA Center for Economic Services. Join us on Wednesday, December 10, at Papapavlo’s for important Medicare updates delivered with Cheryl’s unique brand of humor (laughs guaranteed!). If you are not receiving invitations to our quarterly Office Managers’ Forum meetings, please contact Jessica Peluso at Jessica@sjcms.org. These educational events are open to physicians, office managers, and staff.
Finally, we hope to see you at our annual Holiday Party on Thursday, December 11, at Stockton Golf & Country Club as we gather to enjoy fellowship with friends and colleagues and celebrate another successful year. I wish you laughter, joy, good cheer, and meaningful time with those who matter most. Thank you for the privilege of leading the Society for another year.
Happy Holidays,

Lisa Richmond
LISA RICHMOND





Celebrating 60 years of excellence and unwavering commitment to businesses and families in California’s Central Valley and East Bay communities


21, 1965.
Formed in Brentwood, CA, BAC first opened for business May
Photos from left to right: Ron Berberian, President; Dana Bockstahler, Board Chairman and former CEO; Dante Tosetti, Chief Executive Officer; Jackie Verkuyl, Executive Vice President and Chief Operating Officer; Bill Trezza, Board Vice Chairman and former CEO.
Building Momentum: A Year of Progress and Partnership
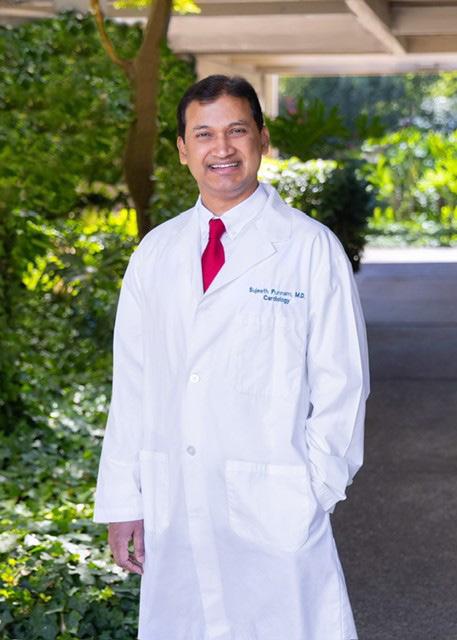
ABOUT THE AUTHOR
Sujeeth Punnam, MD is the current president of the San Joaquin Medical Society and practices interventional cardiology at Sutter Gould Medical Group
When I stepped into this role, I envisioned a medical society that not only leads the charge in cutting-edge healthcare innovation but also serves as a nurturing force for its members and the communities we cherish. That vision began to take shape with the launch of our very first Healthcare Symposium—an inspiring milestone for the San Joaquin Medical Society (SJMS).
A Day of Discovery and Dialogue
On September 27th, the Hilton Stockton buzzed with energy as we hosted our inaugural Fall Symposium. I had the honor of chairing the event alongside three exceptional committee members, with unwavering support from our board. The day unfolded like a symphony of ideas and collaboration. Esteemed speakers traveled from across Northern California and the Central Valley, bringing with them a wealth of expertise and passion. Over 100 physicians registered, filling the venue with curiosity and camaraderie. What struck me most was the hunger for knowledge—the audience remained engaged and eager, even as the clock ticked past 3 PM. The speakers, too, were invigorated by the lively exchange, their presentations met with thoughtful questions and genuine enthusiasm.
A heartfelt thank you to Dr. Bobby Mukkamala, President of the American Medical Association, whose personal message to our attendees was both motivating and affirming. His call to stay involved in society activities resonated deeply. You’ll find a detailed recap of the symposium in this issue.
Advocacy in Action: CMA House of Delegates
In October, I had the privilege of attending the California Medical Association’s House of Delegates Meeting in Los Angeles. The gathering was nothing short of inspiring—nearly 800 physicians convened with

a shared sense of purpose, lending their voices to critical discussions and casting votes that shape the future of healthcare. Advocacy is the lifeblood of organizations like CMA and AMA, and it’s worth noting that 31% of your membership dues go directly toward these efforts. These meetings are more than procedural—they’re a testament to our collective power to influence policy and protect public health.
A Legal Victory and a Legislative Battle
One of CMA’s landmark victories this year was a California court ruling that clarified the use of the title “doctor,” ensuring transparency for patients. Equally significant was the formation of a 50-state coalition to oppose HR-1, a federal proposal threatening $990 billion in Medicaid cuts over the next decade. For California alone, that translates to a staggering $187 billion loss, potentially stripping coverage from 1.3 million Medicaid enrollees and driving up premiums for nearly 2 million ACA participants by 97%.
Investing in Future Healers
SJMS continues its commitment to cultivating local talent through our Scholarship Loan Fund, which supports academically gifted students pursuing medicine with the hope they’ll return to serve our region. In a move toward greater transparency, we opened a board position for this fund to all society members. After a thoughtful nomination process, Dr. Babu Sagireddy was elected via secret ballot. I extend my warmest congratulations and best wishes to him in this vital role.
Legislative Update Highlights
Federal Shutdown Impact: As of September 30, 2025, the federal government shut down due to a budget impasse. While physician payments remain intact, Medicare telehealth waivers have expired—limiting access except for mental health, substance use treatment, and certain ACO participants. Fortunately, Medi-Cal services and telehealth claims remain unaffected thanks to state-level protections.
Proposition 35 Progress
After months of delay, California is finally implementing voterapproved measures to expand Medi-Cal access:
• Retroactive reimbursement for Emergency Department billing codes (99282–99285)
• $90 million allocated for Family Planning and Abortion Services
• $75 million in Graduate Medical Education funds via CalMedForce
• Supplemental payments for Emergency Transportation Services
Looking Ahead
SJMS remains steadfast in its partnership with CMA to restore telehealth flexibilities, protect workforce funding, and extend ACA premium tax credits. As autumn paints our region in golden hues, I look forward to celebrating with you at our Winter Holiday Party.

Aria University to Launch First Medical School in San Joaquin County
French Camp campus to repurpose county facility near San Joaquin General Hospital
A new medical school is on the horizon for San Joaquin County, marking the first of its kind in the region and a major step forward in addressing the community’s ongoing shortage of healthcare professionals.
The school, operated by Aria University, a private nonprofit institution, will give local students the opportunity to pursue medical education close to home while helping meet the county’s growing need for physicians and other healthcare providers.
The campus will be located in French Camp, repurposing an existing county-owned building near San Joaquin General Hospital. Under a 30-year lease agreement, Aria University will pay one dollar per year to the county. Renovations are expected to begin soon, and the school plans to open within two years.
“We have the facility available; they don’t have to build it from the ground up,” said San Joaquin County Supervisor Sonny Dhaliwal, who represents District 3. “It’ll be an easy renovation, and it’ll be up and running in two years.”
San Joaquin County Health Care Services Director, Genevieve Valentine emphasized the importance of investing in the local healthcare workforce.
“We are underserved to an extreme place,” Valentine said. “In fact, we will not have enough nurses by 2030 to just serve our current community, and we already don’t have enough psychiatrists or primary care doctors.”
The medical school will also complement the county’s
upcoming Be Well Campus, a centralized health and social services complex planned nearby and expected to open within two years. Together, these projects will create a vital hub for healthcare training and delivery in French Camp.
Stockton Mayor Christina Fugazi praised the new school as a critical step toward improving access to care for residents across the region.
“We have a community that is in desperate need of healthcare,” Fugazi said. “By having this medical school here, a teaching hospital, people will finally be able to get the care that everyone is so desperately in need of.”
Local leaders hope the school will not only prepare the next generation of healthcare professionals but also encourage them to stay and practice in the region.
“When students are taught in our backyard, they stay in our backyard,” Dhaliwal said. “This will help reduce, or even stop, the brain drain.”
With Aria University expected to begin operations at the French Camp campus in 2027, San Joaquin County’s vision of training, retaining, and supporting homegrown physicians is moving closer to reality. The project represents an investment not only in medical education but also in the health and vitality of the entire Central Valley community.
For more information, please contact Aria University President, Anand Kuchibhotla at Anand@aria.edu or (408) 667-1518.

Navigating cancer is a big journey. A personal guide is a big help.
Hearing the words “you have cancer” can be overwhelming. At St. Joseph’s Cancer Institute, our patient navigators can answer questions, explain treatment options, and help guide you through your cancer journey. St. Joseph’s is the only accredited cancer center and NAPBC®-accredited breast center in San Joaquin County. With certified oncology specialists, state-of-the-art technology, and comprehensive support services, you can be assured St. Joseph’s is the right place for care.
Learn more at dignityhealth.org/stockton/cancercare or call our Cancer Patient Navigator at (209) 939-4526.


House of2025Delegates
CMA elects new officers, honors physician leaders and advances a united agenda
The California Medical Association (CMA) convened its 154th annual House of Delegates (HOD) in Los Angeles, bringing together more than 800 physicians and medical students to debate policy and chart the profession’s path forward. This year’s meeting centered on a single major issue: responding to federal funding cuts and other attacks on health care, public health and medicine—with delegates reaffirming CMA’s commitment to protecting access, strengthening the physician workforce and defending science-based care.
Policy and Governance
Major Issue: Responding to Federal Funding Cuts and Attacks on Health Care
Delegates examined the impact of sweeping federal proposals to reduce funding for health care coverage, workforce development and public health programs. Policy discussions focused on CMA’s strategies to safeguard MediCal and Medicare resources, preserve graduate medical education funding, and maintain essential federal research and public health infrastructure.
CMA reaffirmed its commitment to advocate aggressively for state and federal policies that ensure equitable access to care for all Californians, while protecting the viability of physician practices and the safety net on which millions depend.
CMA adopts governance reforms to modernize House and resolution process
The CMA Governance Technical Advisory Committee (GTAC) presented its final report at CMA’s 154th Annual Session, outlining a comprehensive set of reforms to strengthen CMA’s governance, streamline the flow of resolutions and elevate member engagement in the policy-making process.
The adopted recommendations refine how the House of Delegates conducts business, modernize the resolution submission and sorting process, and establish a new twointerval model that allows for timely policy action throughout the year while preserving deliberation on high-priority issues during Annual Session.
The proposal reflects more than a year of study, stakeholder engagement and feedback from delegations across the state. It was adopted by the House with only minor amendments, and implementation planning will now begin.
CMA extends its appreciation to GTAC Chair Holly Yang, M.D., and all members of the committee for their extensive work and commitment to strengthening the association’s governance framework. Members will receive regular updates as planning and implementation move forward.

Elections
San Luis Obispo pediatrician René Bravo, M.D., installed as CMA’s 157th president
San Luis Obispo pediatrician René Bravo, M.D. , was installed as the 157th president of CMA, the nation’s largest and most influential state medical association representing more than 50,000 physicians. Addressing hundreds of delegates and health care leaders, Dr. Bravo reflected on his journey from the working-class neighborhoods of southeast Los Angeles County to leading the House of Medicine in California.
“My path here was improbable,” Dr. Bravo said. “My parents were hardworking immigrants—a union welder and a clerical worker—and I honor their memory today. But this isn’t about me—it’s about you and the sacred profession we share.”
In his inaugural address, Dr. Bravo called for unity, vigilance, and moral clarity amid intensifying challenges to health care access, physician autonomy, and the safety net.
“The government cannot solve every problem,” he said. “It is up to us—the governed—to tell government and those elected by us what is just and acceptable. We must be relentless in our defense of the underserved, the disadvantaged, and the most vulnerable among us. In this struggle, we are on the side of the angels.”
As CMA president, Dr. Bravo said he will focus on strengthening the association’s influence in Sacramento and Washington, D.C.; revitalizing ties with the American Medical Association (AMA); and protecting all modes of medical practice—from solo and small-group physicians to those within large health systems.
CMA thanks outgoing president Shannon Udovic-Constant, M.D., for her dedicated leadership over the past year. Dr. UdovicConstant will continue to serve on the Executive Committee as Immediate Past President.

René Bravo, M.D., and his wife, Debra.

Newly elected CMA President, René Bravo, M.D., addresses physicians during his inaugural speech.
Elections

Los Angeles family physician Jack Chou, M.D., elected CMA president-elect
Los Angeles family physician Jack Chou, M.D. , was elected by the House of Delegates to serve as president-elect of CMA. He will serve on the Executive Committee in that role for one year and will be installed as CMA president at the conclusion of the 2026 annual meeting.
Dr. Chou previously served as Speaker of the House of Delegates, a position he held since 2022 after three years as Vice-Speaker. For the past six years, he has helped guide the House through an extraordinary period of change — from the shift to virtual sessions during the pandemic, to hybrid meetings, and now fully back together in person.
“I could never imagine six years ago what we would experience as a House together,” Dr. Chou said, reflecting on how the pandemic “changed everything for this House. We went from virtual sessions to hybrid meetings, and somehow we kept it all together.”
He thanked the delegates for their resilience, patience, and unwavering engagement throughout these transitions. “I look forward to working with all of you in the years ahead. I’m deeply grateful for your work and your trust — so let’s go further together,” Dr. Chou said.
A practicing family physician with Kaiser Permanente Baldwin Park Medical Center since 1999, he divides his time between
primary care, urgent care, and hospitalist duties and has served as Chief of Service for the Family Medicine Department since 2018, overseeing five medical office locations.
A partner in the Southern California Permanente Medical Group (SCPMG), Dr. Chou also serves as regional chair for Health Information Management and regional cochair for the Scanning Oversight Committee. A longtime CMA and Los Angeles County Medical Association (LACMA) leader, he has represented LACMA in the House of Delegates since 2001 and previously served on the CMA Board of Trustees and Council on Ethical Affairs. He is also active in the California Academy of Family Physicians, where he has served as president and speaker of its Congress of Delegates.
Originally from a small rural town in Taiwan, Dr. Chou earned his bachelor’s degree in biology from the University of Miami and his medical degree from the University of Southern California, followed by a family medicine residency at Kaiser Permanente Woodland Hills.
CMA congratulates Dr. Chou on his election as president-elect and thanks him for his years of service guiding the House of Delegates and advancing the voice of organized medicine in California.
Elections
Los Angeles psychiatrist George Fouras, M.D., elected Speaker of the House; UC Davis emergency physician Anna
Yap, M.D., elected Vice-Speaker
Los Angeles psychiatrist George Fouras, M.D. , was elected Speaker of the House of Delegates, succeeding Dr. Chou. A CMA member since 1996, Dr. Fouras has served in the House of Delegates for more than a decade and brings a long record of leadership to his new role guiding CMA’s policy-making body.
Dr. Fouras’s leadership within organized medicine spans decades. He previously served as Vice-Speaker of the CMA House of Delegates, Secretary-Treasurer of the California Medical Association Political Action Committee (CALPAC), and chair of the Los Angeles County Medical Association Political Action Committee (LACPAC), and continues to represent California physicians as a delegate to the American Medical Association. He has also led several professional societies, including the San Francisco Marin Medical Society, the Northern California Regional Organization of Child and Adolescent Psychiatry, and the Southern California Psychiatric Society.
Dr. Fouras earned his medical degree from Ohio State University and completed his residency in general psychiatry and fellowship in child and adolescent psychiatry at the Los Angeles County/USC Medical Center. He spent over two decades with the San Francisco Department of Public Health’s Foster Care Mental Health Program, where he helped create California’s first organized psychotropic medication oversight system. Since returning to Los Angeles in 2017, he has continued his work in specialized foster care for the county’s Department of Mental Health.

"I am honored to assume the role of speaker after Dr. Chou. Nothing is more important to me than ensuring that physicians across California feel empowered to participate in the processes that shape our policy and lead our profession,” Dr. Fouras said. “The strength of our House of Delegates lies in the diversity of our members and the unity of our purpose.”
Anna Yap, M.D. , an emergency physician and assistant professor at UC Davis Health, was elected Vice-Speaker of the House of Delegates. At UC Davis, she directs the Administration and Health Policy Fellowship, training early-career physicians to become effective health-policy leaders.
A former CMA Trustee, Dr. Yap currently chairs the CMA Early Career Physicians Section (formerly the Young Physicians Section) and serves as Vice Chair of the Council on Medical Services. She has authored more than 40 adopted policies and has served as Speaker of two AMA Sections; nationally, she now serves as Chair-Elect of the AMA Young Physicians Section.
“The House of Delegates is one of CMA’s greatest assets,” Dr. Yap said. “It is where our members’ voices are heard and ideas become action. Together, we can protect our profession, our workforce, and the patients who depend on us.”

Dr. George Fouras
Dr. Anna Yap
Executive Committee
THE FULL 2025–2026 CMA EXECUTIVE COMMITTEE INCLUDES:

René Bravo, M.D. President

Sergio R. Flores, M.D. Chair, Board of Trustees

George Fouras, M.D. Speaker of the House

Shannon Udovic-Constant, M.D. Immediate Past President

Jack Chou, M.D. President-Elect

Eric Hansen, D.O. Vice-Chair, Board of Trustees

Anna Yap, M.D. Vice-Speaker of the House
Read more about all of our CMA officers at cmadocs.org/executive-committee.
Awards and Honors
Merced family physician Salvador Sandoval, M.D., receives Plessner Award
Salvador Sandoval, M.D., MPH, a family physician whose career spans more than 45 years serving Merced and the surrounding Central Valley, received the Frederick K.M. Plessner Memorial Award, honoring the California physician who best exemplifies the ethics and practice of a rural county practitioner.
Dr. Sandoval’s commitment to health equity began early, shaped by his own summers in farm labor and formative experiences serving migrant workers. His advocacy has focused on farmworker and migrant health, pesticide exposure prevention, opioid overdose prevention, and care for unhoused patients. He led Golden Valley’s Medical Outreach Mobile (MOM) services, bringing care to hard-to-reach residents, and served as
Medical Director of a respite clinic for patients experiencing homelessness.
As Merced County Public Health Officer during the COVID-19 pandemic, Dr. Sandoval provided steady, science-driven leadership, using wastewater surveillance to predict surges and protect vulnerable populations. He continues to mentor future physicians as a preceptor in the Merced Family Medicine Residency.
“Dr. Sandoval’s legacy is etched into the very fabric of rural health care in the Central Valley,” said Kristynn Sullivan, Director, Merced County Department of Public Health. “He has delivered care under bridges, on farms, in shelters, and clinics—always with humility, integrity, and a deep belief in human dignity.”

Watch Dr. Sandoval's video profile at https://youtu.be/mPJJ_GjyTJw.
2025 Plessner Award Winner Salvador Sandoval, M.D., accepting his award.
Awards and Honors
Bay Area physician and health advocate Shagun Bindlish, M.D., receives Compassionate Service Award
Bay Area internist and diabetologist Shagun Bindlish, M.D. , received CMA’s Compassionate Service Award, recognizing extraordinary dedication to community and charity care. Dr. Bindlish is founder and president of the Golden State Obesity Society (GSOS), which advances obesity and lifestyle medicine through community-based education and multidisciplinary engagement in underserved communities across California. As Medical Director at One Medical (Dublin), she delivers inclusive diabetes and obesity care and trains teams in patient-centered practice.
A powerful policy advocate, Dr. Bindlish partnered with the American Diabetes
Association and Senator Scott Wiener to champion SB 40, making insulin more affordable and accessible—a measure passed unanimously and signed into law by Governor Gavin Newsom. She also teaches as adjunct faculty at Touro University California and created the GSOS Youth Ambassador Initiative to engage students in public health advocacy.
“Her commitment extends beyond direct care to meaningful structural change,” said Irene J. Lo, M.D., president of the Alameda-Contra Costa Medical Association. “She champions policy initiatives to improve access to obesity and diabetes treatment.”
Sutter physician P.T. Koenig, M.D., honored with Nye Award for Physician Health and Wellness
P.T. Koenig, M.D. , a family physician with Sutter Medical Group in Dixon, received the Gary S. Nye Award for outstanding contributions to physician health and wellness.
A practicing family physician since 2001, Dr. Koenig has led transformational wellness initiatives as Sutter Medical Group’s Lead Well-Being Champion since 2016, creating a network of peer Well-Being Champions across hospitals and clinics. He helped elevate clinician wellness to an enterprise priority through Sutter’s Joy of Work Initiative, hosted the organization’s first Well-Being Summit, and launched the popular Daily Dose of Well-Being newsletter during the pandemic.


He also collaborated with the Sierra Sacramento Valley Medical Society and other organizations to improve cross-institutional well-being programs aimed at reducing burnout and improving professional fulfillment.
“For over two decades, Dr. Koenig has modeled servant leadership in every sense,” said Edward M. Yu, M.D., Vice President for Value/Population Health at Sutter’s Palo Alto Foundation Medical Group.
“He has always been a brave voice for clinician well-being,” added Elizabeth Ward Pham, M.D., Medical Director of Recruitment and Retention at Sutter Health. “His candor and deep commitment have earned him the respect of our entire medical group.”


CMA honors longtime advocate Elizabeth McNeil with the Speaker’s Recognition Award
Elizabeth McNeil, CMA Vice President of Federal Government Relations, received the Gary F. Krieger Speaker’s Recognition Award. Presented each year by the Speaker of the House, this award recognizes exceptional contributions to CMA and its House of Delegates.
The honor comes as McNeil retires after more than 34 years with CMA, concluding a career that has defined the organization’s advocacy at the federal level. An unflappable strategist and trusted advisor, McNeil has been a driving force behind CMA’s efforts to strengthen physicianled care and elevate California’s influence in Washington, D.C.
“Elizabeth has been the steady hand guiding CMA’s federal advocacy for more than three decades,” said CMA CEO Dustin Corcoran.
“She’s done an absolutely incredible job representing California’s physicians in both Sacramento and Washington, D.C. It’s hard to
imagine CMA without her—because, frankly, none of us have ever known CMA without her.”
Throughout her tenure, McNeil played a pivotal role in shaping every major federal health policy debate of the modern era— from Medicare reform and Affordable Care Act implementation to pandemic relief and telehealth expansion. Her calm intelligence, deep policy expertise and bipartisan credibility have made CMA a trusted voice on Capitol Hill.
“Elizabeth’s knowledge, strategic instincts, and unwavering commitment to physicians have elevated our entire profession,” said Speaker of the House George Fouras, M.D.
“Her work has defined what excellence in advocacy looks like.”
CMA is proud to honor McNeil’s extraordinary service and enduring legacy of integrity, influence, and compassion as she embarks on her well-earned retirement.
Read more about Elizabeth McNeil’s remarkable career and contributions in our companion feature, “A Legacy of Integrity and Influence.”
Advocacy and Engagement
Physicians rally for advocacy: CALPAC shatters fundraising record at CMA HOD
CMA’s Political Action Committee (CALPAC) once again broke records, raising $300,320 at the House of Delegates—its sixth record in seven years and a 22% increase over 2024. The total marks a doubling of event fundraising in less than a decade, underscoring the success of CALPAC’s sustained engagement strategy. Four delegations—the Organized Medical Staff Section and geographic Districts 1, 2 and 8— achieved 100% participation among delegates and alternates. District 2 and District 8 received CALPAC’s Victory Bell Awards for the highest total and average contributions, respectively.

CALPAC begins the 2025–26 year with a record 11 Diamond Level ($6,500) donors: René Bravo, M.D.; Jack Chou, M.D.; George Fouras, M.D.; Brian Grady, M.D.; John Maa, M.D.; Ramin Manshadi, M.D.; Tanya Spirtos, M.D.; Shannon Udovic-Constant, M.D.; Robert Wailes, M.D.; Timothy Watson, M.D.; and the Balboa Nephrology Medical Group.
CALPAC funds power CMA’s political advocacy and efforts to elect more physicians to office— including Los Angeles cardiologist and longtime CMA member and delegate Sion Roy, M.D., who is currently running for the State Senate.
"This year’s record performance shows that physicians understand what’s at stake,” said CALPAC Chair Vimal Nanavati, M.D. “Legislators are making decisions every day that impact how we care for patients and CALPAC ensures physicians are at that decision-making table, not watching from the sidelines. When physicians show up, we don’t just influence the debate—we drive it."
Renew or donate today at calpac.org/donate.
Stay involved with CMA
The House of Delegates meets annually, but advocacy continues year-round. Physicians can stay engaged by volunteering, serving on councils and committees, contributing to grassroots campaigns, and supporting CALPAC.
Learn more about engagement opportunities at cmadocs.org/opportunities.
Thank you to our delegates
CMA extends its deepest gratitude to the hundreds of physicians, residents, and medical students who served as delegates and alternates at this year’s House of Delegates. Your time, expertise, and spirited debate continue to shape the policies that strengthen our profession and improve the health of all Californians. The collaboration and leadership displayed in Los Angeles exemplify the best of organized medicine—and ensure that CMA remains a powerful, unifying voice for physicians and their patients across the state.
Around the House








IN THE NEWS

San Joaquin County Breaks Ground on Transformational Behavioral Health Campus
San Joaquin County leaders joined State officials and health care providers in September to break ground on the SJ BeWell Campus, a new behavioral health care facility designed to expand access to care and strengthen the County’s commitment to building a healthier future.
The campus has been in development among multiple County departments for more than two years and is located on 18.6 acres of County-owned land in French Camp near San Joaquin General Hospital. The SJ BeWell Campus will feature two distinct areas: a South Campus and a North Campus.
Providing staff, physicians, and patients with relevant & up to date information
South Campus
• Community and Outpatient Services building (76,000 sq. ft.)
• Urgent Care Services building with 42 beds (35,250 sq. ft.)
• Residential Treatment Program buildings (two, totaling 132 beds)
• Urgent Care Clinic operations by SJ Health Centers
North Campus
• Supportive Transitional Housing with 252 beds (150,360 sq. ft.)
The four-building campus will provide a full spectrum of behavioral health services, integrating mental health and substance use disorder treatment from outpatient care to residential treatment and crisis stabilization. Having this range of services in one location will allow individuals to seamlessly transition through various stages of recovery, from crisis intervention to long-term care and outpatient follow-up.
Genevieve Valentine, Director of San Joaquin County Health Care Services, said the project represents a new chapter in care delivery. “The SJ BeWell Campus is more than buildings; it is a promise to deliver compassionate, innovative care in a setting designed to heal.”
The total project cost is estimated at $261 million. Site work for construction began in early November 2025, with the first building anticipated to open in July 2027. The remaining three buildings are expected to open at six-month intervals, with the entire campus projected to be complete and fully operational in 2029.
Genevieve Valentine
St. Joseph’s Medical Center
Completes Milestone of 700th Minimally Invasive TAVR Procedure
Dignity Health St. Joseph’s Medical Center has reached the milestone of completing 700 transcatheter aortic valve replacement (TAVR) procedures, led by surgeons Dr. James Morrissey, Dr. Jerome McDonald, and Dr. Mahbub Jamil.
TAVR is a minimally invasive procedure that focuses on replacing a thickened aortic valve that has difficulties fully opening, due to either aortic valve stenosis or aortic valve regurgitation, both of which cause reduced blood flow from the heart to the rest of the body.

“We are proud to continuously provide the highest quality of cardiac care to the Stockton and surrounding community,” said Tina Munoz, St. Joseph’s Director of Cardiac Services. “Everyday, I am privileged to work with our highly trained team of Interventional Cardiologists and Cardiothoracic Surgeons who work together to provide this specialized procedure to our patient population, helping increase the quality of life for countless individuals.”
Healthgrades Names St.
Joseph’s
Medical Center a 2026 Leader in Specialty Care
Dignity Health St. Joseph’s Medical Center has achieved numerous 2026 accolades for clinical excellence from Healthgrades, the #1 site Americans use when searching for a doctor or hospital. Among St. Joseph’s distinctions is the Critical Care Excellence Award for the fifth consecutive year (2022-2026), placing the hospital among the nation’s top 10% Critical Care. SJMC was also rated five stars for four service areas, including Coronary Interventional Procedures, Carotid Procedures, Treatment of Bowel Obstruction, and Treatment for Sepsis.
“We are honored to be recognized for our efforts in achieving the highest standard of care by Healthgrades, placing us in the top 10% in the nation for Critical Care for the fifth consecutive year,” said David Ziolkowski, President and CEO of St. Joseph’s Medical Center. “These specialty acknowledgments are a true testament to our staff and physicians’ continued commitment to providing San Joaquin County with nationally-recognized care, with humankindness, right here in our community.”
St. Joseph’s Medical Center Holds Blessing of the Rigs for Local First Responders
Dignity Health St. Joseph’s Medical Center (SJMC) held their third annual Blessing of the Rigs & Responders event on Tuesday, October 28th, in recognition of National First Responders Day. Nearly 80 first responders and 43 different rigs attended, including 16 patrol vehicles, 15 ambulances, 4 fire trucks, 2 boats, 2 jet skis, 2 motorcycles, 1 BearCat, and 1 Watch Commander, with Chaplains from the Spiritual Services Department performing the blessings for the first responders and their respective rigs.
SJMC offered a county-wide invitation to all city and county fire, police, sheriff, and highway patrol departments, and county ambulance companies to attend. Festivities entailed an interfaith blessing of the vehicles and first responders, which also included specialty units and motorcycles.
“We are immensely proud to stand alongside our first responders, who embody compassion and courage every day,” shared Tammy Shaff, Director of Community Health at St. Joseph’s Medical Center. “Their unwavering dedication as frontline partners in health is vital in creating a healthier and safer San Joaquin County for everyone, and we are delighted in recognizing them in a special way today.”
SJMC’s Annual Blessing of the Rigs















St. Joseph’s Foundation of San Joaquin
Releases Annual Impact Report
St. Joseph’s Foundation of San Joaquin’s 2024-25 Annual Impact Report is now live and can be found on the Foundation’s website. Each year, St. Joseph’s Foundation of San Joaquin publishes their Impact Report to highlight how philanthropy elevates care quality in our community. With the support of over 1,300 donors they’ve raised $8,927,000 to further their mission and enhance access to quality health care for all.
Throughout fiscal year 2025, this tremendous donor backing has enabled St. Joseph’s to achieve wrap-around services for cancer patients and celebrate major milestones at the Morrissey Family Heart and Vascular Institute, including WATCHMAN FLX™ cases and transcatheter aortic valve replacement (TAVR) procedures. They have also expanded the number of medical learners on campus, actively transforming St. Joseph’s into a true teaching hospital.
Introducing Rapid Risk Review, a Podcast from ProAssurance
ProAssurance Risk Management professionals and guests discuss timely and practical issues affecting today’s healthcare professionals. Each monthly episode examines real-world examples and offers actionable strategies to help clinicians and practice leaders make informed, defensible decisions while navigating the clinical, ethical, and legal complexities of care. Topics include patient safety, professional liability, emerging risks, communication strategies, and lessons learned from claims. Discussions range from artificial intelligence in healthcare to informed refusal and the culture of safety. Episodes are available on Spotify, Apple Podcasts, and iHeartRadio. Visit RiskManagement.ProAssurance.com/ Rapid-Risk-Review-Podcast.

Kaiser Permanente Addresses Hunger and Loneliness Among Older Adults
Kaiser Permanente is supporting five Northern California organizations that are working to alleviate hunger and decrease social isolation among older adults.
With the support of grants totaling $450,000 from a Kaiser Permanente fund at the East Bay Community Foundation, organizations in Fresno, the Central Valley, Sacramento, and the Bay Area will distribute food, conduct wellness checks, and organize activities for older adults over the next year. The goal: to improve the quality of life for aging populations in their communities.
According to the California Department of Aging, one in four California residents will be over the age of 60 by 2030. Californians are living longer than ever before, and the increased cost of living is causing many older adults to struggle with purchasing enough nutritious food.
In 2023, more than one-third of low-income adults 60 or older (with household incomes equal or less than 200% of the federal poverty line) were found to be food insecure, according to the California Department of Aging. Further, social isolation and loneliness are on the rise across the country and about 20% of older adults in the state live alone, according to the Public Policy Institute of California.
Kaiser Permanente recognizes that everyone needs and deserves access to healthy food. When people are hungry, lack proper nutrition or cannot access the food they need to address medical needs, they are less likely to get or stay healthy. In addition, research indicates that loneliness can lead to serious health consequences, including an increased risk of dementia, depression, anxiety, heart disease, and stroke.
Grants will support home delivery of nutritious foods and programs that provide social connections. The $450,000 in grants provide much-needed support to five key organizations focused on enhancing access to nutritious food and providing programs and services to reduce social isolation and loneliness that will serve more than 6,000 people.
IN THE NEWS
Health Plan of San Joaquin Launches DualEligible Special Needs Plan
Starting January 1st, 2026, Health Plan of San Joaquin/ Mountain Valley Health Plan (“Health Plan”) will offer Advantage D-SNP, a new Dual Eligible Special Needs Plan (D-SNP) for eligible members in Stanislaus, San Joaquin, El Dorado, and Alpine counties. Often called Medi-Medi plans, D-SNPs serve individuals who qualify for both Medicare and Medi-Cal, combining benefits into one coordinated plan for simpler, more connected care.
Members will receive one health plan card, one number for all support, and dedicated care coordination across medical, pharmacy, and community-based services. This integrated approach reduces fragmentation and promotes personcentered care.
Care coordinators play a key role by helping members schedule appointments, understand prescription coverage, arrange transportation, and access community resources—improving engagement, adherence, and quality of life.
Providing staff, physicians, and patients with relevant & up to date information
What Providers Should Know
• Contracting: Providers interested in becoming part of the Advantage D-SNP Network may contact Health Plan’s Provider Relations team.]
• Case Management: Dedicated care team to support your Health Plan patients with appointment scheduling, coordination of medication refills, transitions of care, and other services.
• Patient Conversations: Providers may share CMSapproved materials and refer patients to trusted resources.
Resources:
• DHCS Medi-Medi Plan Webpage – fact sheets
• Visit our website: www.hpsj-mvhp.org
Health Plan is currently engaging prospective Advantage D-SNP members during the annual election period through December 7th. The new plan is effective January 1, 2026. Questions? Call Provider Services at (209) 942-6340.
Office Space Available for Lease
Office space available now to be leased for medical/dental/medically relevant professional office. The space is 1367 square feet for immediate occupancy in the established Medical Doctor’s Complex, Weber Ranch Professional Park at East March Lane, with 7 rooms and waiting area. Call now (209) 951-8830.

San Joaquin General Hospital introduces Dr. Sobya Hashmi, Infectious Disease
Attending Physician
Dr. Hashmi completed her fellowship in Adult Infectious Diseases at Tulane University, where she served as Chief Fellow and was honored with both the Best Collaborator Award and the VA Medical Center’s Trainee of the Year award. Her clinical expertise encompasses antibiotic stewardship, infection prevention, HIV care, and infectious diseases related to transplant.
At the heart of her practice, Dr. Hashmi believes that curiosity, community, and compassion are the true pillars of medicine. She is a welcome addition to our family of caregivers. Dr. Hashmi is currently accepting patients for bone and joint infections, C. diff management, diabetic foot infections, HIV and PrEP management, sexually transmitted infections (STIs), Tuberculosis (active and latent), and more. For more information, please contact (209) 468-6820.




Dr. Sobya Hashmi
Save time, check into our ER online.

We’re here with 24-hour emergency care. And, with InQuicker, you can let us know you’re on your way.
When an emergency changes your plans, plan to get great care. Our experienced ER team is ready at any time to diagnose and treat a variety of emergency conditions, including lifethreatening illnesses, injuries, broken bones, burns, stroke, heart conditions and more.
In addition, as part of Central Valley Doctors Health System, we can enhance patient-care coordination and provide access to additional specialized services and resources provided by Doctors Medical Center and Emanuel Medical Center.
When an emergency strikes, you can trust the ER team at Doctors Hospital of Manteca.
To check in online, scan the code or visit DoctorsManteca.com/ER For life-threatening emergencies, call 911.





















HEALTHCARE SYMPOSIUM DELIVERS

LEADING EXPERTS SHARE CARDIOLOGY UPDATES for NON-CARDIOLOGISTS
BY JO ANN KIRBY
The Inaugural Fall Healthcare Symposium Cardiology Updates for Non-Cardiologists presented a unique challenge for Dr. Sujeeth Punnam, president of the San Joaquin Medical Society, who spearheaded the event.
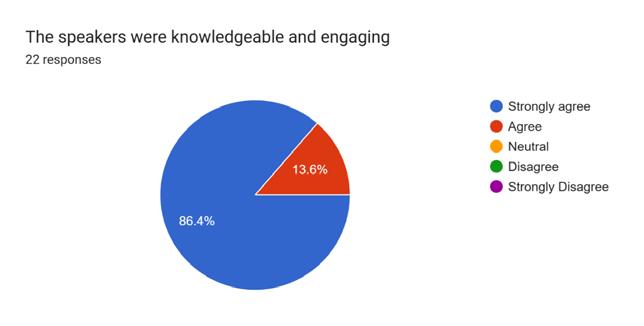
“I wanted to pull in good speakers. I really tried to cherry pick who I thought would be the best because a lot of times an excellent physician isn’t a good teacher,” Dr. Punnam said. As a physician specializing in interventional cardiology, he attended presentations by the very cardiologists he invited to be faculty at the symposium. He was quite pleased when the impressive list of presenters all accepted his invitation.
They included leading experts in their field from UC Davis Cardiology, Stanford Medicine, UCSF Fresno and Dignity Health Sacramento. Seven of the eight physicians also serve as professors, making them ideal teachers for the symposium. Physicians, nurse practitioners, residents, fellows and other health providers attended the event. >>
PLANNING COMMITTEE:
SUJEETH PUNNAM, MD, COURSE DIRECTOR


MANREET BASRA, MD
CYRUS BUHARI, DO
KINNARI PARIKH, MD


The symposium, which was held September 27 at the Hilton Stockton, included breakfast, lunch, exhibits and eight 30-minute sessions that featured the speaker and a cardiologist moderator who facilitated a Q-and-A. “The moderator was in sync with the speaker,” Dr. Punnam said. “It was a great chance for our cardiologists to meet primary care physicians who refer their patients to them. For the primary care physician, this was an opportunity to listen to speakers who are an authority on the topic.”



“ The good old-fashioned way of interacting with speakers, listening, having a discussion, getting your questions answered is time-tested.”
— Dr. Sujeeth Punnam
Dr. Punnam said the San Joaquin Medical Society has about 700 dues-paying members and the symposium was an effort to provide an important opportunity for its members. “We need to bring all the physicians under one umbrella and provide them with opportunities whether it is education, networking or advocacy to fight for what is right,” he said. “What we realized is the education part was missing. There are a lot of educational opportunities online. The good old-fashioned way of interacting with the speakers, listening, having a discussion, getting your questions answered is time tested but we haven’t been doing it. We thought it’s a good way to contribute to the members at large and at the same time encourage a pursuit of excellence in medical care.”
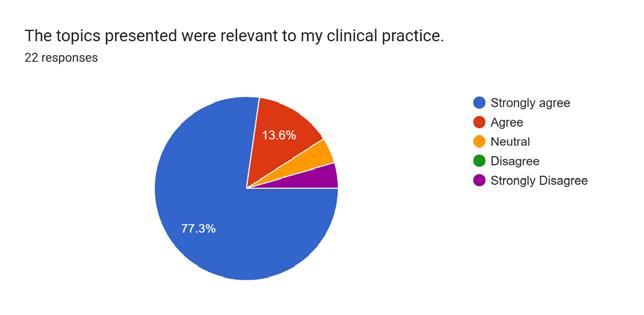
For the 100-plus who registered for the event, it was a unique opportunity to earn a maximum of six Continuing Medical Education credits while learning about the latest advancements in cardiology. Physicians are lifelong learners and must keep up to date on the latest advancements to best care for their patients. Session topics included “Updates on Coronary Artery Disease,” and “Contemporary Diagnosis and Management of Hypertension.’
Primary care physicians are on the front line of identifying heart-related conditions in patients who may seek care for what turns out to be high-blood pressure, high cholesterol, diabetes and other ailments that are risk factors for heart disease. “Cardiovascular


diseases are the leading cause of death worldwide and are responsible for nearly one in three deaths,” Dr. Anureet Gill, a family medicine physician in Stockton, said of why she felt compelled to attend. “One thing, which is most important, is to identify the patients at high risk and early treatment to prevent complications from the cardiovascular issues.”
She found the session on “Contemporary Management of Lipids in Clinical Practice” most informative. “Focusing on preventing the disease should take precedence and treat early to prevent death,” she said.
Dr. Gill appreciated the opportunity to attend an event locally so that she didn’t have to travel far from home and be away from her children for long. She recommends that her colleagues take advantage of attending the event next year. “It was exciting to see different providers in audience including primary care physicians, cardiologists, APPs and residents,” she said.
Dr. Omar Masarweh, who is in the class of 2028
Cardiovascular Disease Fellowship Program at Dignity Health St. Joseph’s Medical Center, said the symposium was a unique opportunity to learn from experts in their fields from leading institutions. “It was both valuable and inspiring to hear them share their experiences and perspectives. Their presentations offered timely insights into the latest clinical guidelines and evidencebased recommendations for patient care,” he said. “The information they provided was not only cutting-edge but also highly relevant to the challenges and patient populations we encounter in daily practice.”
“While we’ve made significant strides in understanding cardiovascular disease and refining best practices for treatment, there remain substantial knowledge gaps to address,” Dr. Masarweh said, praising the event for bringing leading cardiology experts to share the latest findings with physicians. “The ongoing evolution of clinical evidence highlights the importance of continued research, education, and collaboration to ensure we’re delivering the most effective, up-to-date care across the full spectrum of cardiovascular conditions,” he said.
A bonus was the in-person nature of the event, which allowed physicians to make connections and network. “The symposium offered a valuable opportunity to connect with peers as well as established leaders in the medical community during structure lectures as well as Q&A’s and small group discussions during the break periods allowing us to exchange ideas and see how others tackle challenge clinical scenarios,” Dr. Masarweh said. “It
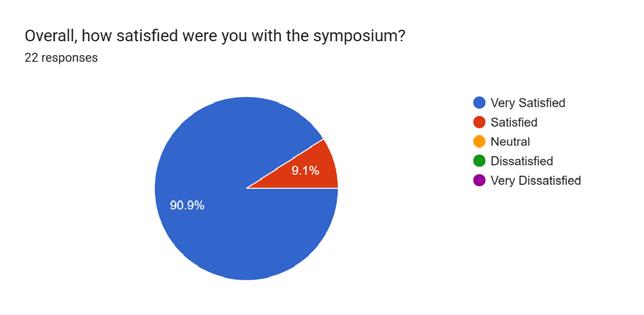
POST SYMPOSIUM SURVEY RESULTS


fostered a sense of professional community, collaboration and helped build connections that could lead to future learning and potential partnerships to improve patient care.”



That is so often missing when physicians take advantage of online learning opportunities. “The most beautiful aspect of it, was we went 45 minutes over with the schedule but even then, they were hanging on,” Dr. Punnam said. “Everyone sat through until it was done. No one left early. I am surprised and so much grateful to see the audience come and then also enjoy it.”
He added that the symposium met all of his expectations, and he hopes the planning committee builds on the success of the inaugural event and can register even more attendees next year. “It worked out well and it was very successful,” Dr.
said. “The planning committee recognizes that physicians are busy and have families. We thought a Saturday, instead of a crammed workday, would give them time to learn and interact in a relaxed atmosphere.”
The event was followed up with a survey. “We are talking about where we want to make it a general theme or keep it specialized,” Dr. Punnam said. Survey respondents were split on that question, so it is something for the planning committee to decide.
Dr. Gill and Dr. Masarweh both said they look forward to attending future symposiums not just for the valuable learning opportunity but also for chance to forge professional relationships with others in the medical community.

“ The information they provided was not only cutting-edge but also highly relevant to the challenges and patient populations we encounter in daily practice.” — Dr. Omar Masarweh
Punnam
Robert Kucejko, M.D.
Enhanced referrals, closer to home


Our team of surgeons in the multidisciplinary UC Davis Colorectal Surgery Program offer laparoscopy, robotics, transanal minimally invasive surgery and advanced endoscopy for routine and complex conditions.
Your referred patients benefit from the only university based Nationally Accredited Program for Rectal Cancer in Northern California, and the academic expertise of our National Cancer Institute-designated UC Davis Comprehensive Cancer Center and nationally ranked UC Davis Medical Center. Plus the convenience of care closer to home and lodging on our Sacramento campus.
Our physician referral liaisons are here to help navigate referrals and:
■ Facilitate access to our secure EMR system, PhysicianConnect
■ Keep you abreast of new services and providers; assist with clinical trials and telemedicine; and more
Connect with your local Physician Referral Liaison: Joaquin Muñoz 916-701-7161 joamunoz@health.ucdavis.edu
California wrapped up its 2025 legislative session on October 12, sending 1,247 bills to the Governor’s desk –just over half of the 2,416 that were introduced this year. Amid shifting political priorities and an ever-changing policy landscape, each year feels more chaotic and frenetic than the last, and 2025 was no exception.
California lawmakers returned in January thinking the big issue of the year would be the budget deficit, which would grow to $12 billion by May, only to be faced with the catastrophic wildfires in Los Angeles – the most expensive disaster in the state’s history and one that hit close to home for many physicians who were both victims and first responders. Only a few months after these fires, Congress began debating HR 1, a sweeping tax and spending bill that drastically reduced health care funding. The ramifications of its passage will be felt in the California budget for the foreseeable future.
The summer recess – a period typically devoted to negotiating lingering amendments to myriad bills – was spent laying the groundwork for Proposition 50, which would drastically redraw California’s congressional district lines. The national debate has largely dominated the legislative discussion in Sacramento, and many of the state’s new policy proposals were aimed at responding to federal actions.
The end of session also saw a leadership change in the Senate with Pro Tem Mike McGuire being replaced by Senator Monique Limón, who represents Santa Barbara, Ventura and Oxnard. Senator Limón takes the reins November 17, and we expect allies like Senator Christopher Cabaldon, Senator Angelique Ashby and Senator Akilah Weber Pierson, M.D., to be elevated into important leadership and committee positions.
On the following pages are highlights of the California Medical Association’s (CMA) major legislative priorities this year.
California Medical Association 2025 Legislative Wrap Up
Prior Authorization
After years of roadblocks to prior authorization reform, CMA introduced four bills to reform the state’s prior authorization systems. CMA’s prior authorization reform package included common-sense reforms to streamline prior authorization processes, expedite critical care for patients and free up physicians’ time to focus on patients, not paperwork.
Earlier iterations (SB 277, SB 516) were previously held because of cost and implementation concerns raised by the California Department of Managed Health Care (DMHC), so we tailored this year’s four-bill prior authorization reform package to be efficient to implement in light of the state’s budget deficit. Ultimately, we were successful in sending two bills to the Governor’s desk, SB 306 and AB 512, with the former signed and the latter vetoed. SB 306 gives the administration the authority to remove prior authorizations on a code-by-code basis, as well as to require reporting from the health plans to give us a better picture of how prior authorization is being deployed at the ground level. Another bill in the package, AB 539, advanced to the Senate Health Committee. CMA will resume working to advance it through the legislature in the 2026 legislative session. The bills in CMA’s prior authorization reform package included:
+ SB 306 (Becker): Requires annual reporting of prior authorization data from health plans and gives DMHC the authority to remove prior authorization statewide on a code-by-code basis.
Signed by the Governor.
+ AB 512 (Harabedian): Shortens the decision timeline for prior or concurrent authorization requests for health plans and health insurers to be no longer than three business days for standard requests (instead of five days in existing law) if the request is made by electronic submission, and 24 hours for urgent requests involving an imminent and serious threat to the enrollee’s health if the request is made by electronic submission or 48 hours.
Vetoed by the Governor.
+ AB 510 (Addis): Requires that appeals of prior authorization denials be performed by a provider of the same or similar specialty. This will help ensure that providers can discuss prior authorization denials with a professional peer who understands the recommended treatment and underlying condition.
Held in Assembly Appropriations Committee.
+ AB 539 (Schiavo): Extends the validity of an approved prior authorization to one year (current industry standard is between 60-90 days). This will provide patients with a longer window of time to receive medically necessary care and avoid cumbersome prior authorization review (and ultimately appeal) processes.
Currently in Senate Health Committee.
Liability Protections
CMA was successful in stopping a bill (twice!) sponsored by the Consumer Attorneys of California that would have increased medical malpractice costs.
SB 29 (Laird) would have extended pandemic-era legal exceptions that make it easier to sue for pain and suffering damages – including in medical malpractice cases – undoing the careful balance struck in AB 35’s historic reforms to the Medical Injury Compensation Reform Act (MICRA). Unless amended to exclude medical malpractice claims, this bill would have significantly increased litigation, settlement and damages
costs across California’s health care system – costs that would have been passed on to physician practices, health plans and the state itself. These increased costs would have further destabilized a system already reeling from drastic state and federal budget cuts, including the devastating multibillion-dollar Medicaid cuts under HR 1.
CMA was successful in getting the bill held in Assembly Appropriations due to its high costs to both the state and the health care system. However, in an unusual procedural move, the bill was resurrected on the evening of September 2, the very last day for bills to be amended. The CMA Government Relations team quickly sprang into action, ensuring that every single Assemblymember had been contacted by a CMA representative by 10 a.m. the following morning. The bill did not have the required votes to pass and was placed on the inactive file on the very last day of session. This bill will likely return next legislative session, but CMA will continue working with legislators to ensure that any bill that passes does not affect medical malpractice cases.
Private Equity
CMA also sponsored SB 351 (Cabaldon), which codified Medical Board of California guidance restricting non-physicians from making business decisions that infringe upon the clinical determinations of physicians. The bill also gives the California Attorney General authority to bring its own enforcement actions, which is a critical new policy. Currently, violations of the corporate practice of medicine either have to be enforced through costly private litigation or through regulatory actions taken by the medical board. Private lawsuits, even if they are successful, typically do not provide financial remuneration, and the medical board has not devoted any resources to enforcing this law. Giving the Attorney General this power means the state can take enforcement action without having to rely solely on civil lawsuits filed by physicians.
Artificial Intelligence
The rapid rise of artificial intelligence emerged as a major new policy front in the California Legislature this year. Last year’s CMA-sponsored SB 1120 (Becker) established a requirement that health plans maintain physician oversight when using AI to approve or deny claims. Building on that foundation, CMA this year sponsored AB 489 (Bonta), which prohibits AI systems or similar technologies, such as internet-based chatbots, from misleading patients into thinking they are interacting with licensed health professionals.
CMA also led a health care coalition to defeat AB 1018 (Bauer-Kahan), a sweeping proposal that would have imposed complex disclosure, auditing and reporting mandates on anyone using automated decision-making tools. As written, the bill would have treated every physician in California as a “deployer of AI,” subjecting routine technology use to onerous compliance requirements and potential enforcement actions. Had it become law, the bill would have severely disrupted the current use of AI in health care and deterred future innovation and technological advancement.
Thanks to CMA’s advocacy, the bill was placed on the inactive file, preserving physicians’ ability to adopt innovative tools while policymakers continue working toward a more balanced regulatory framework.
On the following pages, you will find summaries of many of the key bills that CMA was involved with in 2025.
Priority Opposed
AB
280
(Aguiar-Curry) – Provider Directories
Status: Two-Year Bill – Held on the Senate Floor Inactive File.
This bill would have imposed new mandates related to the accuracy and maintenance of health plan provider directories. As written, this bill would have significantly increased administrative burdens without guaranteeing improved directory accuracy and would have put providers at risk of being reimbursed at the out-of-network amount – set unilaterally by the plan and often significantly below market value – when a consumer is misled by inaccurate or outdated provider directory information.
AB 396 (Tangipa) – Needle and Syringe Exchange
Status: Two-Year Bill – Held in the Assembly Health Committee.
This bill would have required every needle provided through a needle exchange program to carry a unique identifier and required all needles through exchange programs to be properly disposed of. Any needle that had not been properly disposed of could be traced back, and the offending entity that donated the needle would be fined $10,000 per needle. This bill would have created significant costs that threatened the existence of needle exchange programs.
AB
1018
(Bauer Kahan) – Artificial Intelligence
Status: Two-Year Bill – Held on Senate Floor Inactive File.
This bill would have required incredibly burdensome administrative regulations on both developers and deployers of AI. As written, every physician in the state would have been considered a “deployer of AI.”
AB 1215 (Flora) – Hospitals: Medical Staff Membership
Status: Two-Year Bill – Held in the Assembly Business and Professions Committee.
This bill would have required that dentists, podiatrists, clinical psychologists, nurse practitioners, nurse anesthetists, nurse midwives and other health care professionals be admitted to an organized medical staff. This bill failed to account for the diverse circumstances and requirements of different health care facilities and would have put a physician’s licensure at risk by linking enforcement of this bill to disciplinary actions by the Medical Board.
AB 1453 (Tangipa) – Contraception Information
Status: Two-Year Bill – Held in the Assembly Higher Education Committee.
This bill would have required the California State University (CSU) and requested the University of California (UC) to provide all students with adoption information when they receive contraception or emergency contraception from their campus health center or pharmacy. This was an inappropriate mandate that would have undermined efforts to provide students with the reproductive health care they need.
AB 1450 (Hoover) – California Children’s Services Program: Providers
Status: Two-Year Bill – Held in the Assembly Health Committee.
This bill would have allowed the Department of Health Care Services to approve advanced practice providers – including nurse practitioners, physician assistants and certified registered nurse anesthetists – to practice independently within the California Children’s Services program. Allowing advanced practice providers to practice independent of physician supervision is inappropriate, dangerous and at odds with delivering the safest and most effective patient care.
SB 29 (Laird) – Civil Actions: Decedent’s Cause of Action
Status: Two-Year Bill – Held on the Assembly Floor Inactive File.
This bill would have made permanent the ability for a surviving descendant or spouse to recover non-economic damages (pain and suffering) that otherwise would have been awarded to the plaintiff had they survived. As written, this would have included medical malpractice claims, which should be excluded in light of MICRA modernization negotiated through AB 35 (Reyes, 2022).
SB 579 (Padilla) – Mental Health and AI Working Group
Status: Two-Year Bill – Held in the Senate Appropriations Committee.
This bill would have required the Government Operations Agency to appoint a working group to study the impacts and role of artificial intelligence in mental health treatment environments, but did not require a physician to be appointed. CMA requested amendments to ensure that the working group included a physician; however, the bill was held before amendments could be taken.
SB
747
(Wiener) – Wages: Behavioral Health and Medical-Surgical Employees
Status: Two-Year Bill – Held in the Senate Rules Committee. This bill would have required a “covered employer” to report confidential behavioral health employee and medical-surgical employee compensation information to the Department of Industrial Relations. This bill would have diverted resources away from patient care and posed privacy and data security concerns. In September, this bill was amended and no longer pertains to the practice of medicine.
Successfully Negotiated
AB 277 (Alanis) – Behavioral Health Centers, Facilities, and Programs: Background Checks
Status: Two-Year Bill – Held in the Assembly Human Services Committee.
This bill requires any person providing behavioral health treatment to undergo a background check. CMA ensured that this would not apply to physicians holding a current and valid license, as the California physician licensure process includes a fingerprint-based background check.
AB
290 (Bauer-Kahan) – Emergency Services: Physician Fines
Status: Signed by the Governor (Chapter 475, Statutes of 2025).
This bill would have increased penalties for physicians who fail to provide emergency health care by raising monetary penalties from $5,000 per violation to $1 million per violation and establishing additional civil liability for physicians that violate injunctions related to a prior failure to provide emergency health care. Due to opposition, the bill was ultimately gutted and amended and no longer pertains to the practice of medicine, moving CMA to a neutral position.
AB 316 (Krell) – Artificial Intelligence
Status: Signed by the Governor (Chapter 672, Statutes of 2025). This bill would prohibit a defendant that developed or used AI from asserting a defense that AI autonomously caused harm to the plaintiff in a legal action. While not intended to target physicians, this bill unintentionally would have put physicians at risk any time they are in a practice environment that uses AI tools. Amendments were taken that allow defendants to present information for any other affirmative defense, including evidence relevant to causation or the comparative fault of any other person or entity. CMA’s amendments to explicitly exempt physicians from this bill were rejected, but the recent amendments provide a pathway for physician liability protection.
AB 348 (Krell) – Full-Service Partnerships
Status: Signed by the Governor (Chapter 688, Statutes of 2025).
This bill establishes criteria for serious mental illness to presumptively be eligible for a full-service partnership through their county and funded by the Mental Health Services Act. CMA collaborated with the California State Association of Psychiatrists to address concerns and ensure those with behavioral health conditions would also be presumptively eligible.
AB 360 (Papan) – Menopause Survey
Status: Two-Year Bill – Held in the Assembly Appropriations Committee.
This bill would have created a menopause training survey to be provided to all physicians and surgeons upon license renewal to determine the level of menopausal training they have received. While the survey would have been anonymous and optional, mandating the creation of an overly broad survey at license renewal was an inappropriate avenue to gather such information and would have likely resulted in costs to the Medical Board of California and therefore increased licensing fees. Amendments were taken that instead create a study on menopausal training by the Department of Health Care Access and Information and the medical board, removing CMA’s opposition.
AB 432 (Bauer-Kahan) – Menopause CME Mandate
Status: Vetoed by the Governor.
This bill would have imposed an ongoing continuing medical education (CME) mandate on menopause for all general internists, family physicians, obstetricians and gynecologists, cardiologists, endocrinologists, and neurologists who have a patient population composed of 25 percent or more adult women under 65 years of age. CMA supports the author’s efforts to improve access to educational opportunities; however, CMA opposes mandatory CME requirements, as physicians are best positioned to determine which CME courses will provide the most pertinent knowledge relevant to their practice and patient population. This bill would have broadly captured a wide range of physicians whose practices do not involve diagnosing or managing menopause. The bill now creates an incentive program that allows physicians who take a CME course in menopause to receive two credits for every one hour, removing CMA’s opposition.
AB 583 (Pellerin) – Death Certificates
Status: Signed by the Governor (Chapter 271, Statutes of 2025).
This bill allows nurse practitioners to be the attesting provider on death certificates when practicing in a skilled nursing or intermediate care facility. Amendments re-drafted the bill in different code sections to enable implementation. A neutral position was recommended because the overwhelming majority of nurse practitioners still practice under physician supervision. CMA offered amendments that would have only allowed independently practicing nurse practitioners to complete and attest on a death certificate.
AB 601 (Jackson) – Child Abuse Reporting
Status: Two-Year Bill – Held in the Senate Appropriations Committee.
This bill introduces a variety of changes to mandated reporting for general neglect, including establishing an alternative response approach and creating a new standardized curriculum for mandated reporters that must be completed within the first three months of employment. CMA worked to ensure that physicians – who already undergo mandated reporting training – were exempted from this new requirement, moving us to neutral.
AB 669 (Haney) – Substance Use Disorder Coverage
Status: Two-Year Bill – Held in the Senate Appropriations Committee.
This bill prohibits concurrent or retrospective review of medical necessity for the first 28 days of an inpatient substance use disorder stay during each plan or policy year. However, the bill also granted psychologists the ability to prescribe drugs. CMA moved to neutral after psychologists were removed from the list of those who can prescribe drugs.
AB 692
(Kalra) – Employment Contracts
Status: Signed by the Governor (Chapter 703, Statutes of 2025).
This bill makes certain contract terms unlawful, including a term requiring a worker to pay an employer for a debt if the worker’s employment is terminated. Amendments moved CMA to neutral by addressing concerns that employers would be prohibited from collecting amounts paid for training in instances where the employee was stealing or engaged in insubordination, sexual harassment or other misconduct. Amendments now allow for termination of employment prior to the retention period at the election of the employer for material noncompliance or misconduct.
AB 849 (Soria) – Medical Chaperones
Status: Signed by the Governor (Chapter 442, Statutes of 2025). This bill would have required licensed health facilities to provide a medical chaperone to patients during sensitive examinations and required that both a hard copy and electronic notice be given to the patient or their legal guardian. CMA had concerns after the bill was amended to include “providers,” creating redundant requirements for physicians. CMA moved to neutral once amendments were taken that provided a mechanism to reschedule patient exams if a medical chaperone was not available and reduced administrative burdens by requiring only a onetime notification.
AB 876 (Flora) – Nurse Anesthetists: Scope of Practice
Status: Signed by the Governor (Chapter 169, Statutes of 2025). This bill would have allowed certified registered nurse anesthetists (CRNAs) to practice independently, without physician oversight, in hospitals, outpatient facilities and dental offices across California. This bill would have fundamentally changed how anesthesia care is delivered by removing critical safeguards. Recent amendments, as a direct result of CMA advocacy, struck many of the concerning provisions that would have allowed CRNAs to practice independently of any physician order or supervision. These amendments clarify that when CRNAs are providing anesthesia care in any health care setting, it must be under an order from a physician – including preoperative, intraoperative, postoperative and pain management care. This largely clarifies existing CRNA practice in California.
AB 970 (McKinnor) – Child Abuse and Neglect Reporting
Status: Two-Year Bill – Held in the Assembly Public Safety Committee.
This bill proposes a pilot program to evaluate a new model for mandatory child abuse reporting. The program would incorporate internet-based tools and decisionsupport systems to assist mandated reporters in assessing whether a report should be made. Amendments clarify that participation in the program is voluntary and affirm that mandated reporters – particularly physicians – retain full authority and discretion in making reporting decisions.
AB 1172 (Nguyen) – Antiseizure Medication
Status: Signed by the Governor (Chapter 448, Statutes of 2025).
This bill would have authorized a licensed adult program facility to administer inhalable seizure medication to disabled adults at the facility by trained volunteers in emergency situations. CMA had concerns regarding physician liability for incorrect administration of these medications by volunteers and worked with the author to clarify that participating physicians cannot be held liable for the actions of volunteers following their administration and observation instructions, moving CMA to neutral.
AB 1196 (Gallagher) – Health Facilities: Cardiac Surgery
Status: Two-Year Bill – Held in the Assembly Appropriations Committee.
This bill would have changed the requirements for cardiac surgical teams performing extracorporeal bypass to consist of a minimum of one surgeon and two additional medical staff persons, down from three surgeons. CMA coordinated with the California Society of Cardiologists to narrow the bill and ensure that requirements reflect current professional standards of care.
AB 1415 (Bonta) – California Health Care Quality and Affordability Act
Status: Signed by the Governor (Chapter 641, Statutes of 2025). This bill would have broadened the definition of entities captured under the California Office of Health Care Quality and Affordability Act by including management service organizations (MSOs), hospital systems, and hedge funds under the definition of applicable entities. Additionally, this bill specified that a physician organization would be captured if it is under the same ownership or control as a hospital. Amendments, taken in collaboration with CMA, deleted the bill’s newly created definition of a health system. This change was adopted in response to CMA’s concerns that the bill would have subjected physician organizations that are part of larger health systems to onerous data and reporting requirements under the Office of Health Care Affordability.
SB 297 (Hurtado) – Valley Fever Screening
Status: Two-Year Bill – Held in the Assembly Appropriations Committee.
This bill would have required the Department of Public Health to track and identify regions with Valley Fever and mandate that adult patients receiving primary care services in high-incidence regions be offered a Valley fever screening test in a culturally competent and linguistically appropriate manner. CMA opposed this testing mandate as
it overrides a physician’s clinical judgment in determining whether testing is appropriate for a given patient. Amendments were negotiated that remove the mandate that every adult patient be offered a test, instead clarifying that patients in high-risk areas need to be screened according to current clinical standards, and ensuring that physicians are not subject to any licensing actions if they decide – based on their professional judgment – not to screen or offer a test for Valley fever.
Priority Support
AB
82
(Ward) – Health Care: Legally Protected Health Care Activity
Status: Signed by the Governor (Chapter 679, Statutes of 2025).
This bill extends existing privacy laws and protections to health care professionals providing gender-affirming care and services. Additionally, this bill prohibits testosterone and mifepristone from being reported to the Controlled Substances Utilization Review and Evaluation System.
AB 260 (Aguiar-Curry) – Sexual and Reproductive Health Care
Status: Signed by the Governor (Chapter 136, Statutes of 2025). This bill allows a pharmacy to dispense abortion medication without a physician’s name or pharmacy information, so long as a log with this identifying information is maintained. The bill specifies that this log may only be accessed via subpoena. AB 260 also protects healing arts practitioners from civil or criminal actions for prescribing or furnishing abortion medication and prohibits healing arts boards from taking any licensing or disciplinary action against a practitioner solely because they were disciplined or convicted in another state for prescribing abortion medication.
AB 408 (Berman) – Physician Health and Wellness Program
Status: Two-Year Bill – Held in the Senate Judiciary Committee.
This bill would establish a physician health and wellness program under the Medical Board of California to support physicians’ health and protect patients. The bill would align California with national best practices to address mental health and burnout issues. This bill would protect patients by connecting impaired or at-risk physicians with treatment.
AB 416 (Krell) – Involuntary Commitment
Status: Signed by the Governor (Chapter 691, Statutes of 2025).
This bill empowers emergency department physicians to authorize 5150 holds on patients suffering from severe mental illness and in crisis.
AB 447 (Gonzalez, Mark) – Involuntary Commitment
Status: Signed by the Governor (Chapter 363, Statutes of 2025).
This bill allows physicians or authorized prescribers to dispense an unused portion of a medication to an emergency department patient upon discharge, as long as the drug is not a controlled substance, has been ordered and administered specifically to the patient, and is required for continued treatment of the patient.
AB 544 (Davies) – Electric Bicycles
Status: Signed by the Governor (Chapter 36, Statutes of 2025).
This bill updates existing law to align electric bicycles with regular bicycles regarding required safety equipment. It adds requirements for minors to wear a properly fitted and fastened helmet that meets certain safety standards when operating an e-bike and prohibits the sale of a helmet for an e-bike that does not meet those standards.
AB 951 (Ta) – Health Care Coverage: Behavioral Diagnoses
Status: Signed by the Governor (Chapter 84, Statutes of 2025).
This bill prohibits insurance companies from requiring patients to undergo repeated re-diagnoses for pervasive developmental disorders and autism as a condition of maintaining their insurance coverage.
AB 1127 (Gabriel) – Firearms: Converter Pistols
Status: Signed by the Governor (Chapter 572, Statutes of 2025).
This bill would prohibit the sale of certain semi-automatic handguns that can be easily converted to automatic machine guns.
SB 40 (Wiener) – Health Care Coverage: Insulin
Status: Signed by the Governor (Chapter 737, Statutes of 2025).
This bill prohibits health plans from imposing a copay of more than $35 for a 30-day supply of insulin and prohibits plans from imposing step-therapy protocols as a prerequisite to authorizing coverage of insulin.
SB 41 (Wiener) – Pharmacy Benefits
Status: Signed by the Governor (Chapter 605, Statutes of 2025).
This bill would prohibit pharmacy benefit managers (PBMs) from requiring use of an affiliated pharmacy or imposing conditions that would discourage the use of a non-affiliated pharmacy. It would also limit a PBM’s income to the fee for the pharmacy benefit management services provided. SB 41 bans spread pricing and mandates that drug rebates go to payers, not PBM profits.
SB 439 (Weber-Pierson) – California Health Benefit Review Program
Status: Signed by the Governor (Chapter 318, Statutes of 2025).
This bill extends the operation of the California Health Benefit Review Program and the Health Care Benefits Fund and authorizes the continued assessment of the annual charge on health plans for that purpose through fiscal year 2032–2033.
CMA-Sponsored
AB 489 (Bonta) – Health Care Professions: Deceptive Terms or Letters: Artificial Intelligence
Status: Signed by the Governor (Chapter 615, Statues of 2025)
This bill would ban companies from marketing artificial AI chatbots as licensed medical professionals. AI can be a useful tool for physicians and patients; however, patients need to know when they’re communicating with an AI chatbot versus a trained health care professional.
AB 510 (Addis) – Prior Authorization: Same or Similar Specialty
Status: Held in the Assembly Appropriations Committee. This bill would have required that appeals of prior authorization delays, modifications, or denials be performed by a provider of the same or similar specialty. This would have helped ensure that providers can discuss prior authorization denials with a professional peer who understands the recommended treatment and underlying condition.
AB 512 (Harabedian) – Prior Authorization: Shortened Timelines
Status: Vetoed by the Governor.
This bill would shorten urgent prior authorization request timelines from 72 hours to 24 hours for electronic submissions and 48 hours for non-electronic submissions. For non-urgent requests, the timeline
would be shortened to three business days for electronic submissions, while maintaining the existing five business days for non-electronic submissions. This change will ensure more patients can receive care or appeal denials in a timely fashion.
AB 539 (Schiavo) – Prior Authorization: One-Year Duration
Status: Two-Year Bill – Held in the Senate Health Committee. This bill would extend the validity of an approved prior authorization to one year (current industry standard is 60–90 days). This will provide patients with a longer window of time to receive medically necessary care and avoid the cumbersome prior authorization review and appeal processes.
AB 967 (Valencia) – Physicians and Surgeons: Licensure: Expedited Fee
Status: Two-Year Bill – Held in the Senate Business, Professions, and Education Committee.
This bill would streamline the process for licensing outof-state physicians looking to practice in California. This will ensure that physicians can be recruited to move to California and have certainty that they will have an active license to practice when they relocate.
SB 32 (Weber-Pierson) – Health Care Coverage: Timely Access to Care
Status: Held in the Assembly Appropriations Committee. This bill would enhance access to maternity care services by requiring the Department of Health Care Services, the Department of Managed Health Care, and the California Department of Insurance to establish unique time and distance standards for perinatal units in collaboration with stakeholders.

SB 306 (Becker) – Prior Authorization: Volume Reduction
Status: Signed by the Governor (Chapter 408, Statues of 2025) This bill would allow the Department of Managed Health Care to remove the requirement for prior authorization for the majority of services and lower tiers of prescription drugs that are approved at a high rate. DMHC will determine which services and items have prior authorization removed after health plans submit the required prior authorization statistics. This will reduce the overall volume of prior authorization requests and ensure that patients can receive the care they need with minimal delays and that physicians can spend more time focusing on patient care.
SB 351 (Cabaldon) – Health Facilities
Status: Signed by the Governor (Chapter 409, Statues of 2025) Private equity firms are gaining influence in our health care system, leading to rising costs and undermining the quality of care. This bill empowers the Attorney General to hold private equity groups accountable for interfering with the practice of medicine, allowing the Attorney General to investigate and take action against private equity firms that unlawfully interfere in the patient–physician relationship. The goal is to restore trust in the health care system, ensuring that medical decisions are made in the best interests of patients, not financial shareholders.
Save the Date: 2026 Legislative Advocacy Day!
April 8, 2026 | Sacramento
This event brings together more than 400 of physician and medical student leaders from all specialties and modes of practice. Attendees will have the opportunity to get hands-on experience meeting with legislators on priority health care issues and learn the ins and outs of advocating for their patients and profession.
Clear & Simple
Restore your vision with cataract surgery designed just for you — using the latest technology for clearer, brighter sight.
Our fellowship-trained physicians provide advanced care for diabetes-related eye conditions, the latest glaucoma treatments, eyelid surgery, tear duct procedures, and both medical and cosmetic eye treatments.




We o er laser vision correction and comprehensive eye exams for the whole family. Our on-site optical center features a wide selection of designer frames to suit every style.
Looking to refresh your appearance?
We also provide cosmetic injectables—including Botox and dermal fillers—to help you maintain a youthful, natural look.






STEPHEN A. LIN M.D.
STEVENS Y. KIM M.D.
DANIEL CHOI M.D.
ETHAN TITTLER M.D.
MICHAEL J. SAKAMOTO M.D.
MICHAEL C. YANG M.D.
KENNETH V. MISELIS M.D
VIKRAM GIRN O D
KELSEY PRICE O D
ANGELA MAHARAJ O.D.
HONORING A LEGACY
DR. RICHARD WATERS

Support the Legacy of Dr. Rip Waters
Your donation helps future physicians and healthcare professionals return to serve our community — the same mission Dr. Waters championed.
Give today: www.tinyurl.com/WatersPFP
Please note PFP in the memo line.

THE DR. RIP WATERS PRINCIPAL FORGIVENESS PROGRAM
BY LISA RICHMOND
In late 2013, when the San Joaquin Medical Society’s Scholarship Loan Fund (SLF) had an opening for a physician on its Board of Directors, longtime board member Royce Northcott had an idea: she would recruit her beloved cardiologist, the late Dr. Richard “Rip” Waters. As a Stockton native and former recipient of an SLF loan during medical school, Dr. Waters understood firsthand the program’s impact. Royce knew he’d be a perfect fitand she was right.
The SLF provides annually renewable educational loans to students pursuing degrees in medicine, physician assistant studies, nurse practitioner programs, and nursing. Eligible applicants must have resided for a meaningful period of their lives in one of the five counties served by the San Joaquin Medical Society: Alpine, Amador, Calaveras, San Joaquin, or Tuolumne.
Dr. Waters went on to serve a decade on the SLF Board, where his leadership proved instrumental in modernizing the program. Among his many contributions was the creation of the Principal Forgiveness Program (PFP), an innovative incentive designed to encourage recipients to return to their hometowns and serve the communities that supported them, just as he had done.
Recognizing the region’s ongoing need for physicians and midlevel practitioners, the PFP allows eligible recipients who return to practice in an SJMS county to apply for forgiveness of 20% of their loan principal after each year of local service, for up to five years. Forgiveness requests are reviewed upon receipt of an application and granted at the discretion of the SLF Board based on an assessment of the Fund’s current finances. The board was proud to grant the PFP to its first two recipients, Stockton natives Drs. David Araiza and Vanessa Armendariz, who both moved home two years ago to practice family medicine at Community Medical Centers.
Following Dr. Waters’ sudden passing in the fall of 2024, the SLF Board sought a lasting way to honor his remarkable legacy and passion for strengthening the healthcare workforce in our community. In tribute to his vision and dedication, the program will henceforth be known as The Dr. Rip Waters Principal Forgiveness Program.
For more information about the Scholarship Loan Fund, visit www.sjcms.org/programs/scholarshiploanfund.
Exceptional orthopedic care. Exceptionally close by.
The new Sutter Alpine Care Center is bringing more top-quality orthopedic care to the Stockton and San Joaquin County community. Gould Medical Group is delighted to welcome the Alpine Orthopedics Group, a trusted name in orthopedics with deep roots in the community. Sutter is committed to delivering more access to timely, state-of-the-art care to help our patients feel their best.
See how we care at sutterhealth.org/alpine
2488 N California St., Stockton, CA 95204



RESID ENTS' REPORT

A PLACE FOR ALL NEWS HIGHLIGHTING RESIDENTS AND GRADUATE MEDICAL EDUCATION
The Resident’s Report is dedicated to all the good news related to our hard-working residents training at San Joaquin General Hospital and St. Joseph’s Medical Center. Please email your submissions, written in third person with accompanying photo to Lisa@sjcms.org.
DIGNITY HEALTH ST. JOSEPH’S MEDICAL
CENTER hosted its inaugural Fall Research Symposium on Monday, September 15, 2025 at the University Plaza Waterfront Hotel.
Funded by St. Joseph’s Foundation of San Joaquin, St. Joseph’s Graduate Medical Education Program was pleased to highlight researchers, clinicians, pharmacists, residents, fellows, medical students, faculty, and staff from across Northern California and the Central Valley to join us for a day dedicated to scholarly activity, networking, and innovation and insight sharing.


Practice News and Resources
Free to SJMS/CMA Members!

The Office Managers Forum empowers physicians and their practice manager staff with valuable tools via expert led education sessions from industry professionals who are committed to delivering quality healthcare. This quarterly forum is normally held on the second Wednesday of March, June, September and December at Papapavlo's in Stockton.
Registration is required!
If you don’t receive an invitation via E-Mail, please email Jessica@sjcms.org

December 10th, 2025: 11:00AM to 1:00PM
“Medicare Changes 2026 and Beyond”
Join us for our annual Medicare Update workshop for physicians and office staff. This 2 hour seminar will cover relevant information about current, future and proposed changes for the coming year!
Cheryl Bradley- Associate Director of CMA’s Center for Economic Services

January 27, 2026: 12:15pm to 1:15pm
"New Laws
Affecting Physicians 2026"
This one-hour webinar will discuss the new 2026 laws that are affecting physicians and their practices, highlight pending health legislation and explain CMA’s legal resources available to members.
Registration: https://tinyurl.com/NEWLAWS2026
Sheirin Ghoddoucy -Senior Legal Counsel and Director of Legal Advocacy for the California Medical Association

March 11th, 2026: 11:00AM to 1:00PM
“2026 Employment Law Updates”
Discover how to navigate complex employment law changes and stay on track for a successful year. This will help businesses navigate California’s challenging employment and labor laws.
Jamie Bossuat, a shareholder and employment lawyer at Kroloff will present an update on the most pressing issues in employment law and will offer practical suggestions for reducing liability. Issues will include recent changes in wage and hour requirements, updates to leave of absence laws, and current litigation trends.
CMA PRACTICE RESOURCES
DHCS DETAILS NEW MEDI-CAL RX POLICY
CHANGES EFFECTIVE JANUARY 2026
The California Department of Health Care Services (DHCS) has issued a 90-day notice announcing upcoming Medi-Cal Rx coverage changes that take effect January 1, 2026. The updates – authorized as part of the 2025-26 state budget – will limit reimbursement for select medications and over-the-counter (OTC) products and expand prior authorization requirements for certain therapies.
KEY UPDATES
COVID-19 Antigen Tests: All OTC COVID-19 antigen tests will require prior authorization unless prescribed by a California Children’s Services (CCS) Paneled Provider for a pediatric patient under age 21. Pharmacy claims for these tests may be approved on a case-by-case basis with medical justification demonstrating the need for suspected COVID-19 exposure or infection. Prior authorizations apply as one-time overrides and cannot be renewed. A new prior authorization is required for each claim. Additionally, approvals are limited to four tests per patient per month.
GLP-1 Drugs: Weight Loss Drugs: GLP-1 receptor agonists prescribed for weight loss or weight-related indications will no longer be covered under Medi-Cal Rx. Coverage will continue for GLP-1 drugs used to treat type 2 diabetes or other non-weight-loss indications with an appropriate ICD-10 code.
Continuation of Care Policies: Drugs currently approved under “continuation of care” exceptions will require a new prior authorization showing medical necessity. Before coverage is granted, prescribers must first try a therapeutic alternative listed on the MediCal Rx Covered Drugs List. The following drugs will be affected: chlorpromazine, fluphenazine, haloperidol (various forms), timolol (gel and solution), bimatoprost, and Adhansia XR (methylphenidate). This policy applies to all Medi-Cal members.
Select OTC Products: DHCS is also revising MediCal Rx coverage policies for several over-the-counter products for Medi-Cal patients 21 years of age and older. Beginning January 1, 2026, multivitamin combination products will no longer be covered. Single-ingredient vitamins and dry-eye treatments will require prior authorization to demonstrate medical necessity, while coverage of first- and secondgeneration antihistamines will be restricted to generic formulations. Additionally, OTC prenatal vitamins will be limited to use during pregnancy or lactation for Medi-Cal patients between ages 10 and 60. These
restrictions do not apply to prescriptions written by CCS Paneled Providers for a pediatric patient under age 21.
Implementation and Support
DHCS is framing these changes as part of a broader effort to control pharmacy costs while ensuring continued access to medically necessary treatments.
Providers with questions can contact the Medi-Cal Rx Customer Service Center at (800) 977-2273 (available 24/7) or email MediCalRxEducationOutreach@ primetherapeutics.com for more information.
The California Medical Association (CMA) will continue monitoring the rollout to ensure that patient access and continuity of care are not adversely affected by the new coverage restrictions.
CALIFORNIA BEGINS ROLLING OUT VOTER-BACKED PROP 35 HEALTH CARE INVESTMENTS
After months of delay, California has finally begun moving forward with implementation of Proposition 35, the voter-approved measure to increase Medi-Cal payments and expand access to care. While the 202526 state budget included budget allocations that were contrary to those required under Proposition 35, California Medical Association (CMA) advocacy and sustained pressure are now beginning to yield progress across four key areas, with the expectation of more to come.
Emergency Department Physician Payments
On September 30, the California Department of Health Care Services (DHCS) submitted a State Plan
Amendment (SPA) to CMS seeking approval to use Prop 35 funds for supplemental payments to emergency department physicians who treat Medi-Cal patients. The supplemental payments will be for four E/M billing codes (9928299285) and be retroactive to July 1, 2025.
Family Planning and Abortion Services
The state has begun distributing $90 million in Prop 35 funding for family planning and abortion care through grants administered by the California Department of Health Care Access and Information (HCAI). With federal funding for providers such as Planned Parenthood under attack in Washington, these state resources will help sustain critical reproductive health services.
Graduate Medical Education Expansion
In early September, the Newsom Administration confirmed that $75 million in Prop 35 funds for graduate medical education is available now. These dollars are being distributed through the state’s CalMedForce GME program, administered in a partnership between Physicians for a Healthy California and the University of California. CalMedForce/CalMedForce+ are currently accepting applications for residency and fellowship slots in primary care, as well as specialty and subspecialty training programs. The application window closes October 8.
Emergency Transportation Services
DHCS also submitted a SPA to CMS to support supplemental payments for ground emergency medical transportation for Medi-Cal enrollees. This change, too, would be retroactive to July 1, 2025.
Looking Ahead
CMA will continue to hold state leaders accountable to fully implement Proposition 35 as voters intended. Physicians and patients fought hard to pass this historic measure, and CMA will keep pressing to ensure that every voter-approved dollar is invested in strengthening the Medi-Cal program and improving access to care across California.
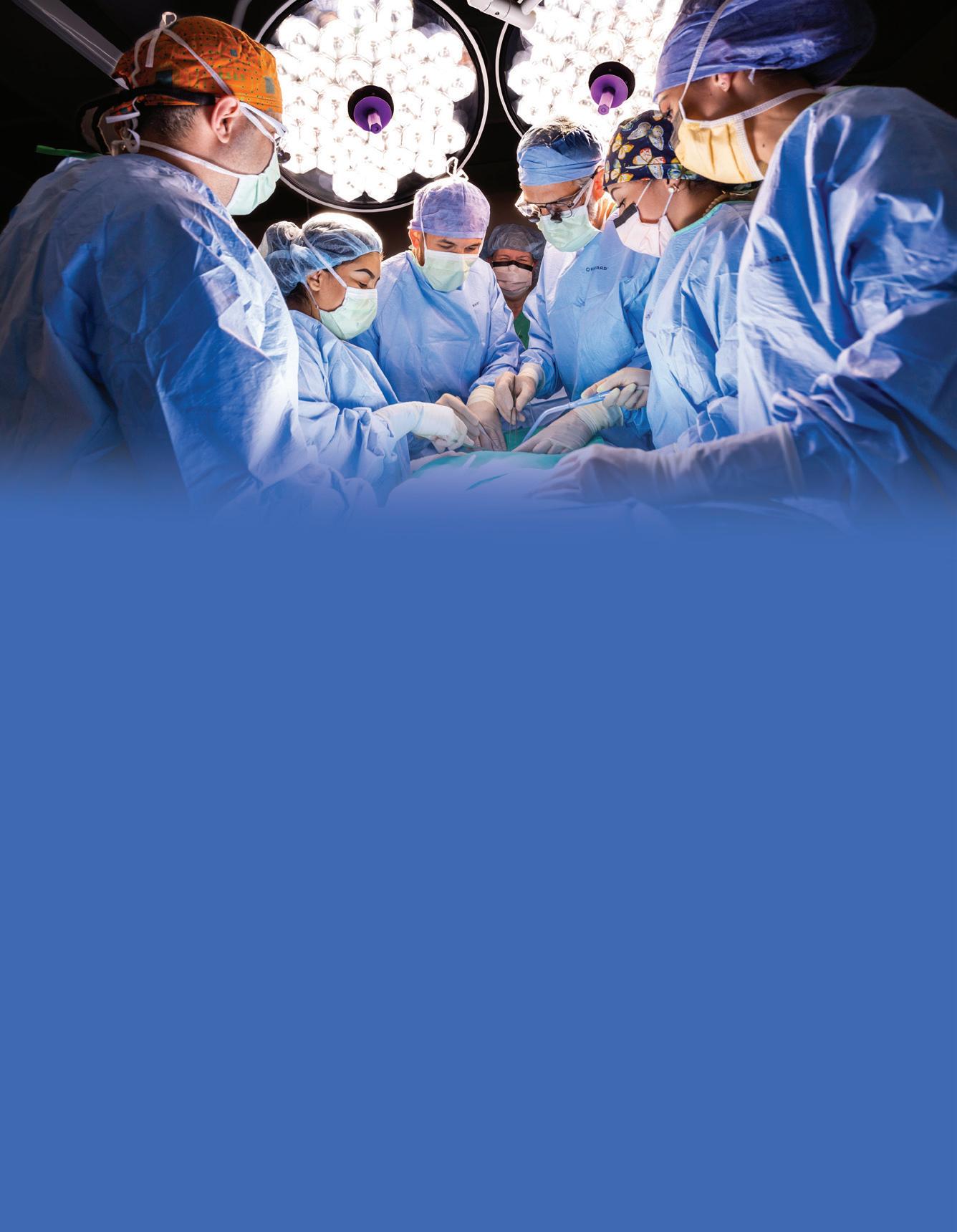
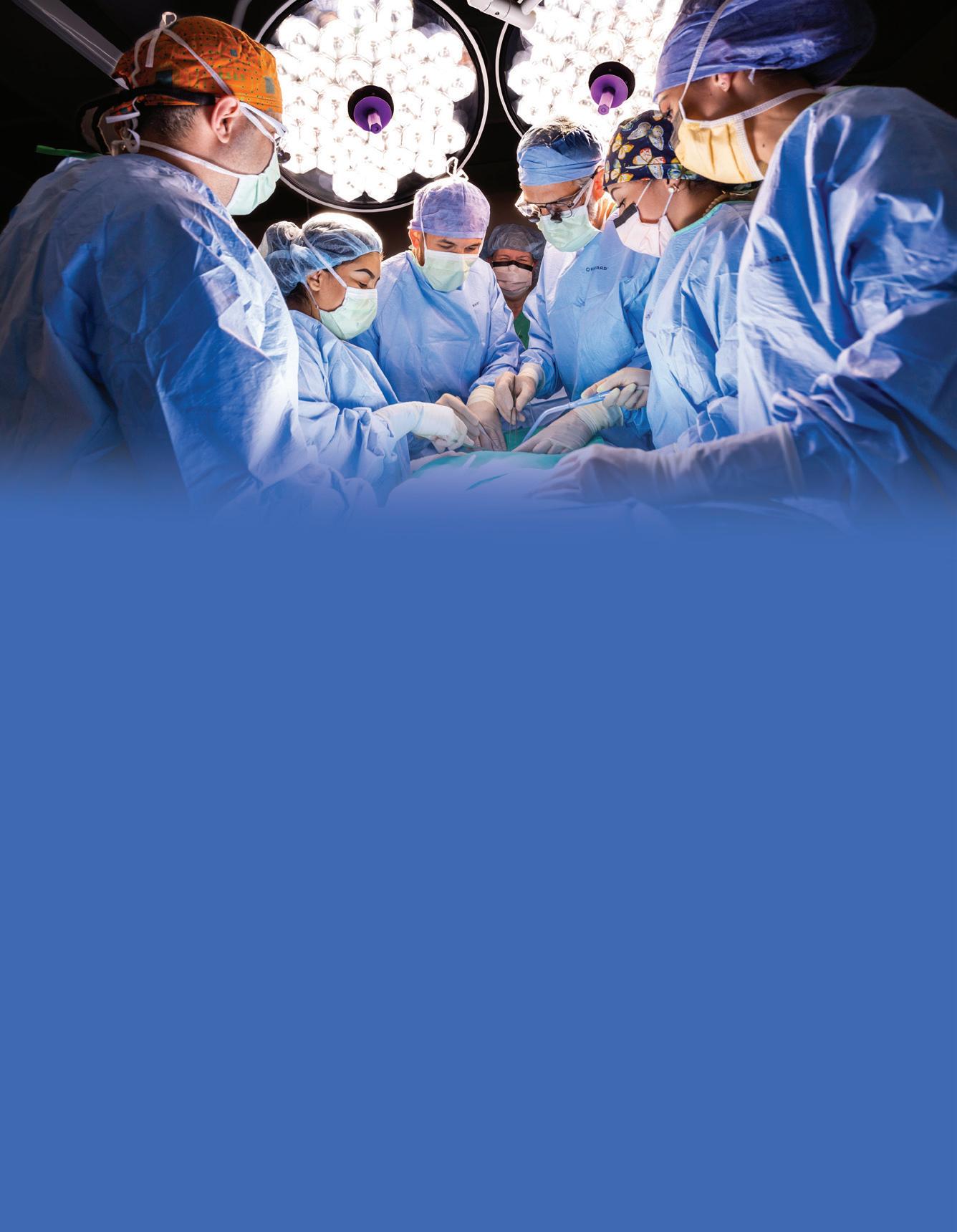







Public Health Update What Health Care Providers Need to Know about WIC
BY POOJA VYAS PATEL, MS RDN AND WENDY HOWARD, CLE
Every day, numerous health care providers across the nation see individuals and families who qualify for the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). The WIC program provides eligible families with healthy foods and expert advice on nutrition, health, and breastfeeding during critical periods of growth and development. Most health care providers are familiar with WIC, but many remain unaware of the vast array of services this public health cornerstone offers.
Brief History of the WIC Program
The federal WIC program was introduced as a pilot program in 1972 following an amendment to the Child Nutrition Act of 1966, providing supplemental foods to children up to age four and to breast-feeding mothers in the postpartum period. It was established as a national program in 1974 with the first site opening in January. By the end of the year, WIC was operating in 45 states. In 1975, federal legislation (P.L.94-105) was passed establishing WIC as a permanent program and expanding eligibility for WIC services to non-breastfeeding women who were up to 6 months postpartum and children up to age five.


Fifty years later, the WIC program stands strong and continues to be a leading pioneer in providing supplemental food packages, outstanding nutrition education, and support that helps pregnant and postpartum women, infants and children up to 5 years of age to eat well, be active, and stay healthy.
Breastfeeding Support – Setting WIC Apart
Beyond food packages and nutrition education, WIC is a critical ally in maternal and infant health, especially when it comes to breastfeeding support. Breastfeeding promotion and support are at the very heart of WIC’s mission. WIC proudly provides eligible new mothers with breastfeeding equipment and support and education about how breastfeeding benefits both mothers and their infants.
Most WIC agencies, including WIC in San Joaquin County, employ International Board-Certified Lactation Consultants (IBCLCs,) Breastfeeding Peer Counselors, and trained WIC Nutrition Assistants (WNAs) who provide support for breastfeeding parents, including individual nutrition and breastfeeding counseling, loaner breast pumps, group classes and ongoing encouragement.
with expertise in breastfeeding and community collaboration and include individuals from a wide variety of backgrounds. They are charged with increasing breastfeeding initiation and duration rates within communities and coordinating training for health care providers and health care provider staff on breastfeeding services offered by WIC programs. They also support adoption of the BabyFriendly Hospital Initiative by supporting implementation of the CDPH guidelines, “9 Steps to Breastfeeding Friendly Clinics: Guidelines for Community Health Care Centers and Outpatient Care Settings 2015.” In the community, RBLs encourage coalition building and community collaboration to support breastfeeding, and assist employers with lactation accommodation in local businesses, schools, and clinics.
Piecing it all together, WIC plays three major yet essential roles –
“Most families first learn about breastfeeding support through WIC—not the hospital—making early referrals essential for successful outcomes.”
1. Access Point of Support: In practice, most families first learn or hear about breastfeeding and lactation help through the WIC office, not the hospital or providers clinic. Providers are encouraged and empowered to refer patients early – ideally as soon as the pregnancy is confirmed and to start educating on the important benefits of Breastfeeding for both mother and the baby as to help bridge the gap between hospital discharge and home.
2. Community Alignment: WIC trained staff ideally speak and offer support via same language, background or lived / shared experiences with participating clients, helping them validate and normalize breastfeeding within the communities.
The California Department of Public Health (CDPH) WIC program created Regional Breastfeeding Liaisons (RBLs) to support collaboration among the community, public health and health care teams as we work together to improve awareness and education about breastfeeding. Regional Breastfeeding Liaisons are trained professionals
3. Continuity of Care: WIC program serves as a major consistent contact / platform for families starting from pregnancy, infancy and toddlerhood – something that we know clinical systems in the US often struggle to sustain.
WIC and Health Care Working Together
Despite years of continued effort, San Joaquin County Public Health WIC’s rates of exclusive breastfeeding have remained approximately 40% for the past five years (2020 -2025), so enhancing collaboration between health care providers and WIC staff is essential. Here are several key opportunities for alignment to consider:
1. Early Clear Messaging and Referrals –Refer eligible patients as soon as the pregnancy is confirmed by calling the WIC contact line or by completing the referral form – as to streamline the process. Phone number: (209)468-3280
2. Mutual Strategic Communication – When trained WIC staff or IBCLC or RBL reach out with updates or reminders, a timely response back ensures care continuity.
3. Shared Messaging – Consistent evidence-based advice – on latch, feeding practices and frequency, supplementation or weight checks – together builds a
strong parental confidence. Mixed messaging can lead to unsuccessful breastfeeding initiation and outcomes.
4. Pump & Formula Coordination – Developing and using internal protocols on determining the most appropriate use of a pump for a family’s needs or the need for baby formula depending on certain circumstances such as NICU discharges or mothers returning to work.
5. Hospital-WIC Linkages or Systems Integration –Developing and sharing two-way referral and discharge lists may allow WIC’s presence in overall patient care, leading to higher breastfeeding rates and smoother transitions in the perinatal period.
Healthcare providers can enhance these efforts by viewing WIC as part of the care continuum and not a separate system. Learn and know your community WIC contacts, refer early, and stay connected. Together we can achieve health equity from the very first feed.

6 NEW SJMS MEMBERS THIS
FALL! ...and even more on the way.
Grace Cavallaro, MD
Family Practice
1800 N California St Stockton, CA 95204
Rush Medical College, 1992
Rami Georgies, MD
Family Practice
8001 Lorraine Ave Stockton, CA 95210
Faculty of Medicine Univ of Aleppo, 1993

Anuja Oza, MD
Family Practice
599 E Valrico Rd. Tracy, CA 95376
Boston Univ School of Medicine, 2016
Alaa Gabi, MD
Interventional Cardiology
1801 E March Lane, Ste D400 Stockton, CA 95210
An-Najah National University, 2009
Pallavi Pothuri, MD
Internal Medicine
1800 N California St. Stockton, CA 95204
Gandhi Medical College, 2011
Dylia Pereira-Narvaez, MD
Family Practice
1801 E March Lane, Ste A170 Stockton, CA 95210
Faculty of Health Sciences of the University of the Witwatersrand, 1992
In Memoriam
LAWRENCE R. FRANK, MD
1944 - 2025
Lawrence “Larry” Robert Frank, M.D., born January 4, 1944, met his Savior shortly before he died & went to be with Him at the age of 81 on October 7, 2025.
He spent the last months of his life at Summerfield Memory Care in Stockton & the family thanks them for all the care given to “Doc”.
He is survived by his wife, Karen Janeen (Webb), sons David Michael & Alexander James, brother-in-law Ronald White (Carol), nephews Douglas (Samira) & Robert (Zepure), nieces Jessica (Bryan), Rebecca (Jordan) & Sarah along with their children, his cousins, 3 dogs, & dear friend Steve Schneider & his family. Larry was preceded in death by his parents Ernest Louis & Hilda Albers & his brother Allan.
Born in New York City, he was your typical New Yorker –quick-witted, direct & determined. He grew up the same as any city kid would, except he spent 12 summers on a farm owned by German immigrants. He knew from the time he was a child that he wanted to be a doctor & he always considered himself lucky to be able to fulfill that calling. He graduated from NYU School of Medicine, completed his residency in Internal Medicine at the VA in Martinez & fellowship in Nephrology at the University of California, San Diego. In 1972 he joined the USAF & was stationed as a medical officer in Panama during the Vietnam War where he also discovered a love of scuba diving.
Eventually he found his way to Stockton, which had been advertised as needing a nephrologist “in the Bay Area”. As the Medical Director of the Dialysis Unit at San Joaquin General Hospital since 1979, he became a familiar face in all 4 hospitals in the area. The time & dedication he poured into his job & patients was unmatched & he was also devoted to the Dialysis staff who cared for them. As the County grew, so did the need for Dialysis services & he oversaw the unit’s expansion to the area south of the Hospital. For the past 44 years he also served the medical profession through his work with the San Joaquin Medical Society & was awarded their Lifetime Achievement Award in 2019. He
continued to practice fulltime until his retirement in August 2024.
The Hospital also brought him together with his wife-to-be & her young son. An avid runner, you could often see Larry pushing the running stroller as they trained. He (finally) got on his knee & proposed after they finished a ½-marathon together. As the story goes, he wouldn’t have proposed if she hadn’t finished those 13 miles with him! A longtime member of the Sundance Running Club, he served as newsletter editor & also Race Director for the California 10-Mile for many years. He was particularly proud of finishing the 100th running of the Boston Marathon. Even though his runs eventually turned more into “walk-a-thons”, he still treasured the decades-long friendships he had with his fellow runners.

He also loved animals & probably would have taken in every dog in the city if possible. He would come up with his own silly names & made-up languages to talk to them & strangely enough they seemed to understand. Other passions were sailing, diving, woodworking, & astronomy, but really, he just enjoyed learning. He was a dedicated scientist & enjoyed cooking, which he viewed as just chemistry, but took forever to make a dish because he had to follow the recipe 1-step at a time & to a “tee”!
He had a laugh that can’t be forgotten, a dry sense of humor, & a quick wit. He was a friend & devoted husband & father & will be greatly missed by all who knew him.


San Joaquin Medical Society
3031 W. March Lane, Suite 222W
Stockton, California 95219-6568
RETURN SERVICE REQUESTED
SHARE THE LOVE NOT THE FLU.

Health Plan is engaging in flu prevention efforts now through March 2026 with local public health partners in San Joaquin and Stanislaus counties. This campaign covers all four of our service areas, targeting parents and caretakers of children under the age of two and the community at large.
As a valued Health Plan provider, you can join our efforts and be a flu prevention ambassador.
Go to www.hpsj.com/cold-flu-partnerships to access virtual campaign materials and get information on keeping your patients healthy all flu season. Health Plan providers can request flu prevention materials that can be mailed directly to your office.
Local partnership and collaboration is what makes our community great. Help us Share the Love, Not the Flu this season.
Get your campaign materials here:
