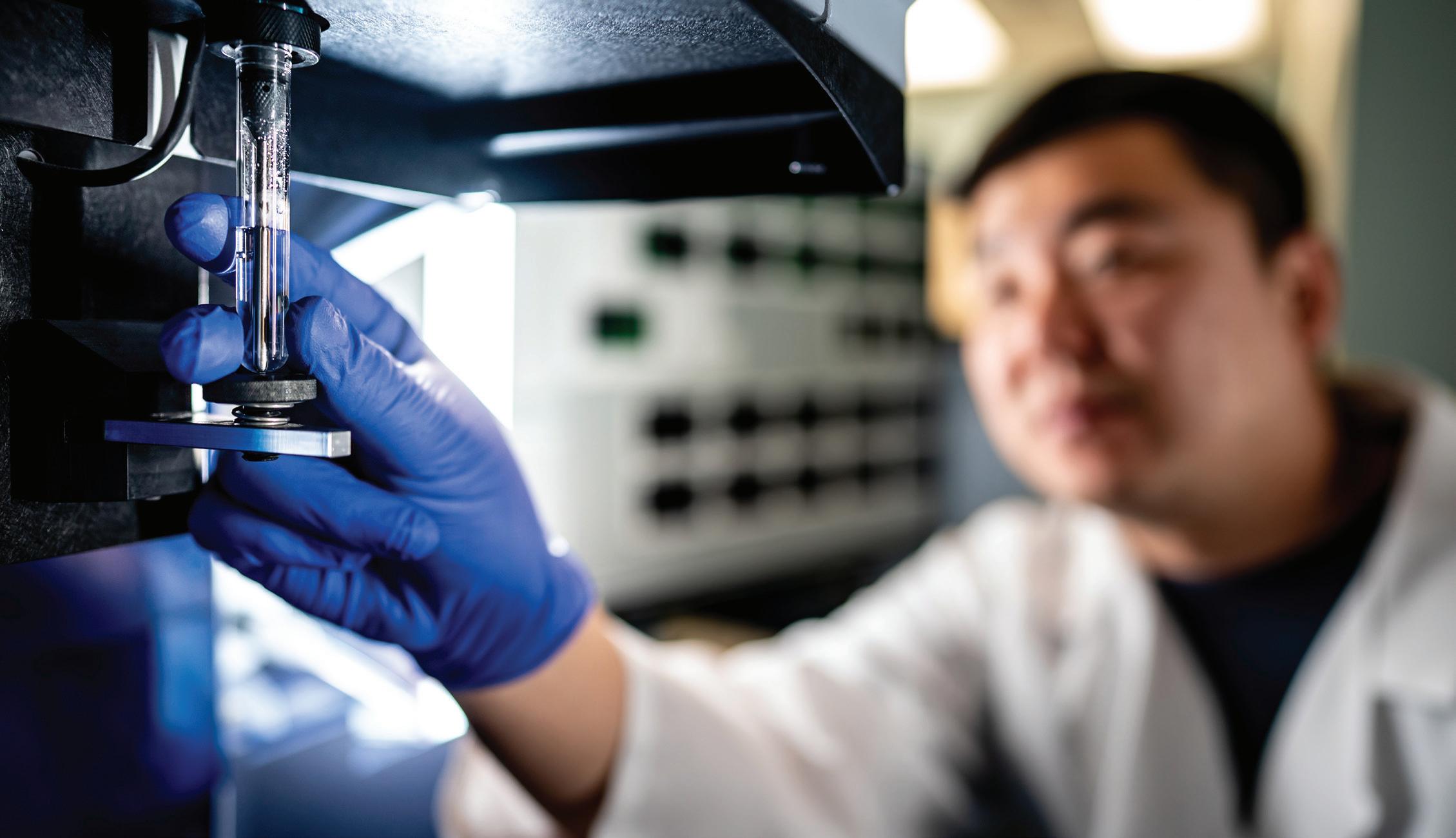
St. Jude researchers, backed by extraordinary resources and support teams, are focused on making big discoveries.






St. Jude researchers, backed by extraordinary resources and support teams, are focused on making big discoveries.

Discovering a molecular driver of lethal outcomes for viral respiratory disease
Improving long-term academic achievement through early interventions 52
A breakthrough in battling resistance with next-generation antibiotics 53 A blueprint for translating genome-editing strategies to clinical trials 54
Characterizing approaches to treatment decision-making for children presenting with advanced cancer in resource-limited settings 55


Solving the decades-long mystery of NLRC5 sensor function in inflammation and disease 56
Epigenetic insights help reveal the causes of unsolved epileptic neurological disorders 57
Discoveries are ‘one click’ away with the St. Jude survivorship portal 58
‘Molecular putty’ properties of biomolecular condensates coded in protein sequence 59
Scientists combine novel CAR design and AI to improve CAR T–cell immunotherapy 60
Switching gears in glutamine metabolism is key to red blood cell development and disease 61



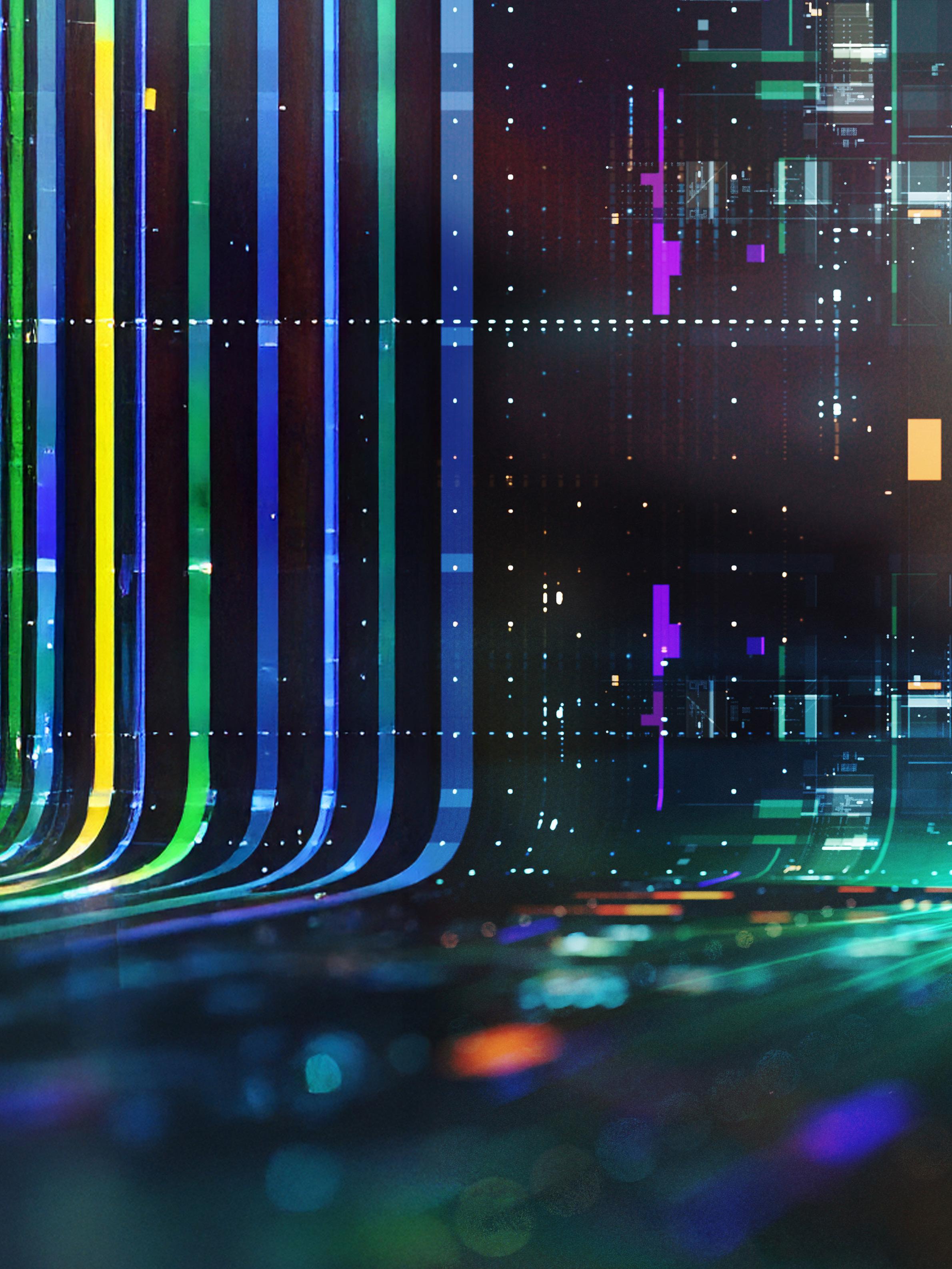
Light is a powerful force that fuels, illuminating discoveries and transforming our understanding of biological processes, molecular dynamics, human health, and disease. Modern microscopes and imaging techniques allow St. Jude researchers to manipulate light and energy to visualize aspects of science that can be leveraged to create novel treatments for catastrophic diseases. At the heart of fluorescence microscopy is the filter cube, which controls the path of light. The filter cube facilitates sample excitation and fluorescence signal detection, illuminating the target molecule(s). This artistic rendering of light at a specific wavelength passing through a filter cube to excite fluorophores embodies the concept of “lighting the way to knowledge.” The cube, sitting amidst a stream of computational data, represents how this technology integrates within a suite of scientific methods to generate impactful science. Artwork by Leena Xaypanya
Privileged communication. Copyright © 2025 St. Jude Children’s Research Hospital. No part of this communication may be cited, reproduced, stored in a retrieval system, or transmitted by electronic or other means without prior written permission of the President and CEO and the appropriate investigator.
This report reflects the activities of St. Jude Children’s Research Hospital during 2024.


When Danny Thomas founded St. Jude Children’s Research Hospital in 1962, he envisioned a place where science and medicine could work together to achieve the extraordinary — to ensure that no child dies in the dawn of life from a catastrophic disease. That vision continues to guide us today as we generate knowledge to transform the outlook for children with cancer and other life-threatening illnesses, not only in the United States but around the world.
Since we opened our doors more than six decades ago, St. Jude has made remarkable progress in curing the incurable, treating the untreatable, and improving the quality of life for patients and survivors. Yet, significant challenges remain. At St. Jude, we are uniquely positioned to address these challenges, leveraging unparalleled talent and resources to push the boundaries of science and medicine. We are committed to building systems that ensure the cures we develop reach children everywhere.

The Scientific Report 2025 celebrates the advancements made by St. Jude faculty and staff over the past year. These achievements reflect the institution’s unique scientific culture — one that encourages bold ideas and collaboration to tackle the hardest problems and answer the toughest questions. By combining fundamental biological research with extensive clinical expertise, we generate knowledge that drives transformative discoveries and changes the way medicine is practiced.
This year’s report showcases groundbreaking advancements across disciplines, from precision genomics transforming pediatric leukemia care to predictive medicine reducing symptom burdens, from immunotherapy innovations enhancing T-cell functionality to improving outcomes for survivors and at-risk children. In fundamental biology, cutting-edge tools are revealing new mechanisms of cellular communication and molecular interactions, reshaping
our understanding of complex systems. St. Jude is also accelerating progress through intelligent solutions, including the launch of the Office of Data Science and the integration of advanced technologies for translational impact. Together, these achievements reflect our commitment to generating knowledge that improves outcomes and ensures cures reach children worldwide.
As we reflect on the progress of the past year, we celebrate the dedication, talent, and collaboration that make these achievements possible. Together, we continue to honor Danny Thomas’s vision by transforming hope into reality for children with catastrophic diseases.
James R. Downing, MD President and Chief Executive Officer
St. Jude Children’s Research Hospital




are knowledge hunters who seek an objective understanding of the world.
Acquiring this understanding relies on the tools a scientist has in their toolkit. Light is a critical tool. It illuminates the material world and can reveal what is hidden by darkness. St. Jude researchers work on the cutting edge of science, often butting up against physical boundaries that limit the types of biological questions they can answer. However, researchers have shown that they can push past the boundaries of what has been possible, creating new approaches to peer into the unknown. The resulting discoveries illuminate science, lighting the way to knowledge.
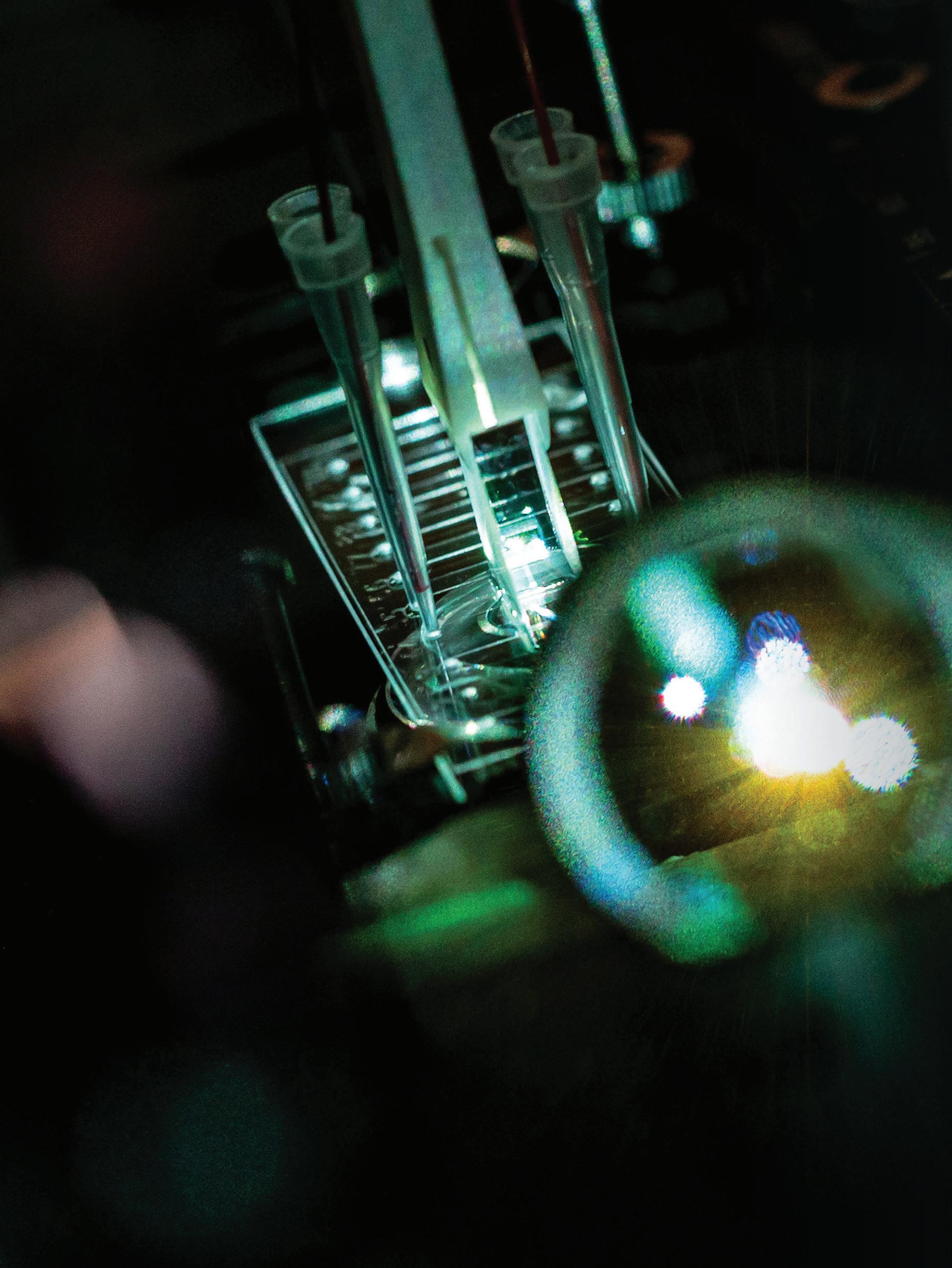
Fluorophores are molecules that can absorb visible light, which in turn enables electrons to jump to higher energy states. Upon relaxation of the electron, that energy is sometimes released as glowing light (fluorescence). Combining fluorescence with microscopy is a powerhouse pairing that can detect cellular structures and biological processes, which can inform foundational biology and the diagnosis and treatment of human diseases.
Biomolecules change their shape, or conformation, to interact with binding
partners and complete physiological functions. These movements can be subtle and localized — occurring on a time scale around one quadrillionth of a second — or more exaggerated, on a time scale of microseconds to seconds. Understanding how biomolecules move while they work is key to understanding their function.
Technological advances in microscope mechanics, improved data processing, and reimagined fluorophores have increased the speed and precision of fluorescence microscopy. Scientists can now study the movements of individual molecules in real time by using singlemolecule Förster resonance energy transfer (smFRET). This method works by placing two or more fluorophores on different parts of a molecule, exciting the sample with light, and measuring the energetic communication among the fluorophores. Quantifying the energy transfer between fluorophores informs scientists about the distance between them, which can be on the scale of one-billionth of an inch. This level of sensitivity makes this technique ideal for measuring biological processes at the molecular scale.
One limitation of fluorescence-based imaging methods is that fluorophores can fail to fluoresce because of a change in a fundamental property of the excited electron called its spin state. “Every time an electron is excited, there’s a probability that it will lose memory of its spin and adopt an inverted spin state,” said Scott Blanchard, PhD, Department of Structural Biology. “If this occurs, it cannot relax back to its ground state and becomes trapped in a highly reactive, nonfluorescent triplet state that is 100,000 times longer-lived.”
Triplet states, called “dark states,” impact a fluorophore’s brightness and durability and cause phototoxicity. Dark states also reduce data quality and accuracy.

choice but to try to find solutions.”
The need to succeed led Blanchard’s team to intramolecularly tether triplet state quenchers to fluorophores. This discovery gave researchers a generalizable strategy to reduce dark state lifetimes in fluorophores by as much as 1000fold. Fluorophores imbued with this property are called “self-healing.”
Published in Nature Methods, this study by Blanchard’s team demonstrated for the first time that self-healing fluorophores enable more robust and precise molecular-scale measurements. This transformative work substantially advances smFRET imaging and helps ascertain the function of biological molecules. However, the self-healing technology has the potential to benefit all forms of fluorescence imaging, which

What the field believed was that triplet states were an immutable reality. But we had no other choice but to try to find solutions.
Scott Blanchard, PhD Department of Structural Biology
Blanchard hopes will be advantageous to fluorescence microscopy pursuits at St. Jude and around the world.

Necessity is the mother of invention, and Lindsay Schwarz, PhD, Department of Developmental Neurobiology, agrees with that ancient Greek proverb. Schwarz researches norepinephrineexpressing (NE) neurons, which represent about 0.00003% of brain cells. These cells modulate anxiety, attention, memory, and stress responses.
Aberrant responses by NE neurons can cause mental health issues, including anxiety and depression. “We treat anxiety and depression with drugs that target norepinephrine signaling, but these drugs act globally, meaning there’s often a detriment to other important functions for norepinephrine that you don’t want to see,” explained Schwarz. “Targeting these neurons more specifically could help ameliorate that.”

subpopulations expressing overlapping elements or genetic features, a userfriendly intersectional approach — something that did not exist.
Writing in Nature Neuroscience, Schwarz and former St. Jude graduate student Alex Hughes, PhD, detailed the development of Conditional Viral Expression by RibozymeGuided Degradation (ConVERGD).
ConVERGD is an intersectional expression platform pairing adenoassociated virus vectors, which insert genetic material called transgenes, with ribozymes (RNA strands that catalyze reactions) to express desired traits in specific cellular subsets.
ConVERGD constructs activate transgenes and fluoresce only when two protein recombinases, Flp and Cre, are present.

the transcribed mRNA and prevent protein production. Flp and Cre can be introduced into many cells and organisms and can be activated independently through functional programs that are distinct to specific cells. Utilizing these molecular elements in the way that ConVERGD does allows specificity in identifying cell lineages and subsets in living organisms based on multiple parameters, highlighting the versatility of this approach. ConVERGD can also be used in other systems beyond the brain.
As proof of concept, Schwarz’s team looked for NE neurons that also expressed prodynorphin (Pdyn), which was thought to be involved in anxiety. Using ConVERGD, the researchers fluorescently labeled a targeted subpopulation of neurons expressing both Pdyn and Dbh, which makes

These methods are now being used by other labs to study important processes in the brain in ways that haven’t been done before.
Lindsay Schwarz, PhD Department of Developmental Neurobiology



ConVERGD-based viral tools made it possible for Schwarz’s team to identify the anatomical connectivity and behavioral influence of Pdyn+/ Dbh+ NE neurons and helped the field understand how this unique population of neurons provokes such diverse behavioral states — a question that has fascinated researchers for years.
Schwarz continues to expand the ConVERGD toolkit. She said, “These methods are now being used by other labs to study important processes in the brain in ways that haven’t been done before.”
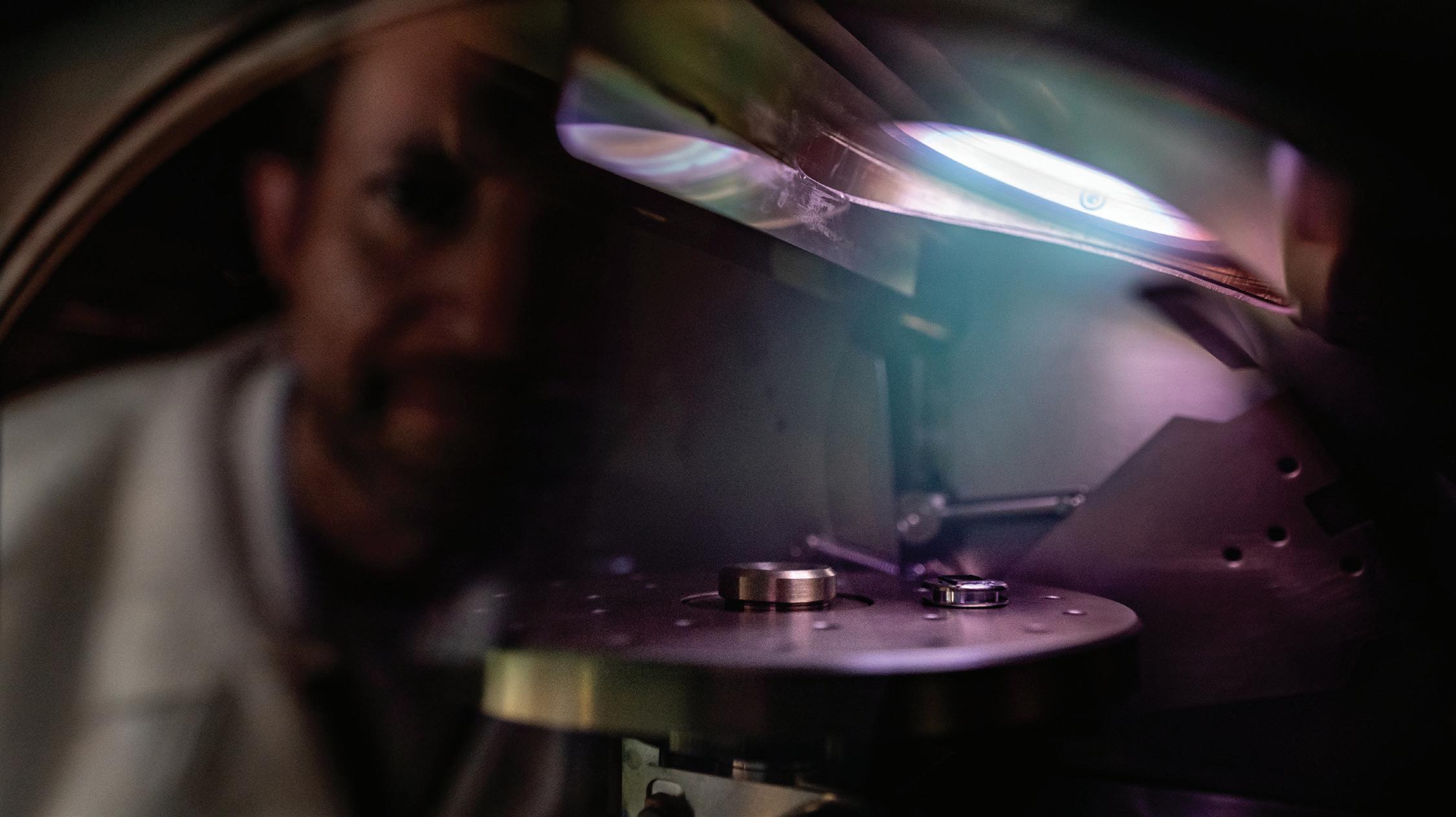
How researchers experimentally use illumination varies as technology advances. This is the case in the laboratory of Stacey Ogden, PhD, Department of Cell & Molecular Biology, who studies the role of signaling molecules such as Sonic Hedgehog (SHH).
Precisely when and where a cell receives an SHH signal is tightly regulated during development to ensure tissues and organs pattern properly. Still, scientists were unclear about how SHH reaches target cells with appropriate precision.

For a long time, visualizing these structures in complex developing mammalian tissue has been challenging, but we’ve finally found a way.
Stacey Ogden, PhD Department of Cell & Molecular Biology
Some wondered if thread-like cellular projections called cytonemes were involved, but no one had visualized the structures in mammalian tissue — not until Ogden reevaluated the capabilities of imaging science and, quite literally, saw cytonemes in a new light.
“For a long time, visualizing these structures in complex developing mammalian tissue has been challenging,” Ogden said. “But we’ve finally found a way.”
In Cell, Ogden described combining modern microscopy with optimized sample preparation to see fluorescent thread-like protrusions extending from cells. Ogden’s team systematically tested various methods of sample preparation, fixation, and imaging to ascertain the most conducive protocols for imaging in mammalian tissue.
To effectively visualize the cellular membrane extensions, the team leveraged a genetic lineage tracer in which membranes of SHH-expressing cells are labeled with a fluorescent protein. To preserve the 3D structure, tissues expressing the fluorescent marker were sectioned with a device called a vibratome, which allowed the researchers to create tissue sections that were thick enough to preserve cytonemes but thin enough to facilitate imaging of the membrane marker. Sectioning with the vibratome also minimized the fracturing of cytonemes that typically occurs when sectioning tissue with a more standard device called a cryostat.
Vibratome sections were visualized using a confocal microscope that combines super-resolution imaging with the ability to track fluorescence lifetime. This approach allowed the
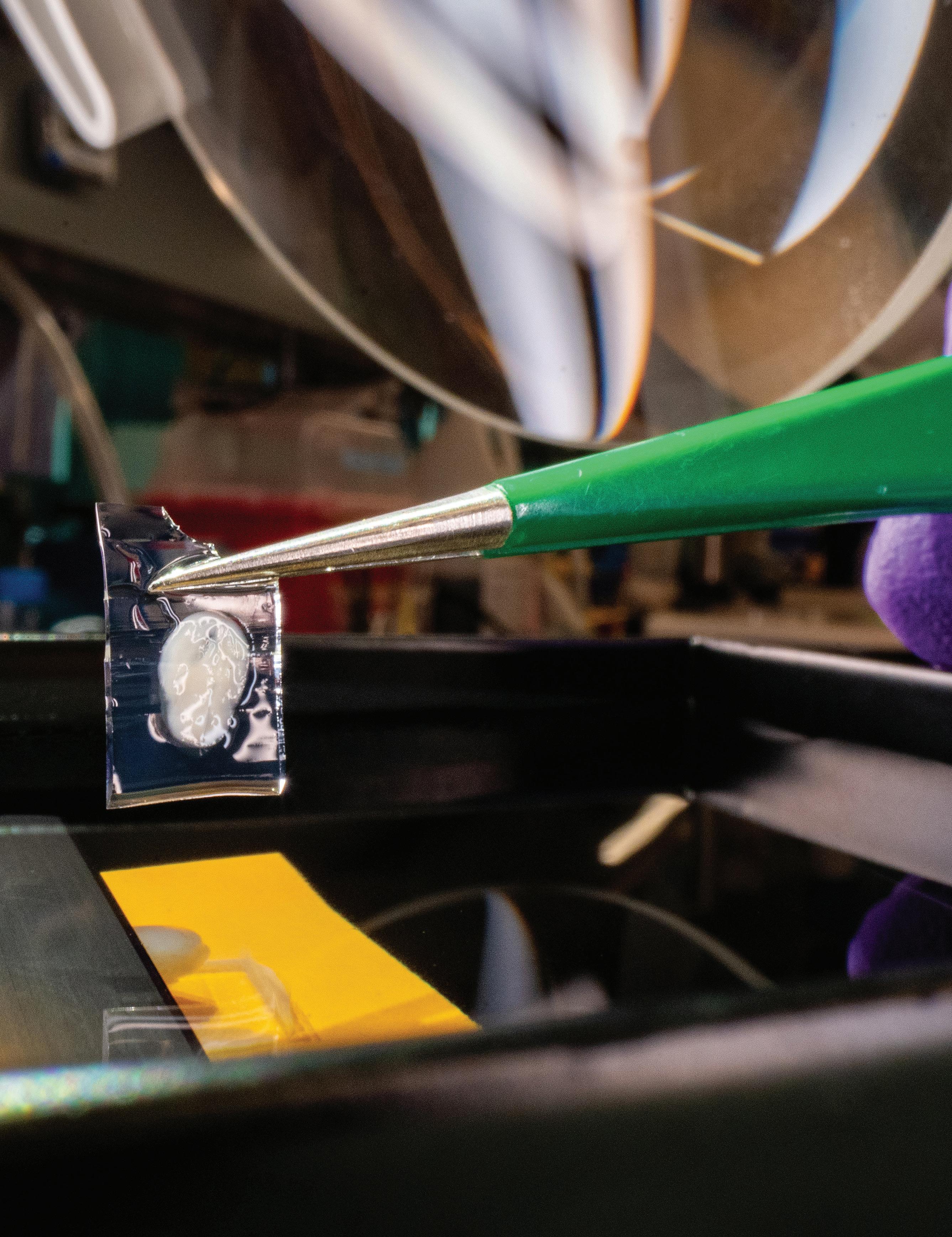

researchers to obtain images with lower background noise and higher spatial resolution. Ogden’s team also used scanning electron microscopy for additional validation that what they observed using light microscopy was occurring at a larger scale.
The researchers were able to observe the tip-to-tip connections made by these cellular extensions in the neural tube, a structure found early in development that eventually becomes the brain and spinal cord. These tipto-tip connections appeared to join cells at the apex of the membranes lining the lumen (hollow space within the neural tube) to primary cilia at the apex of adjacent cells.
Comprehensively, Ogden’s work showed that cytonemes are key contributors to SHH deployment and rapid delivery for tissue patterning. Furthermore, the work showed that when cytoneme function was disrupted, aberrant SHH signaling ensued.
“This is the first demonstration of these cytoneme-based transport processes occurring during the development of a complex mammalian tissue such as the neural tube,” Ogden said.
Illuminating discoveries are often made by pushing past the boundaries of what is known or what already exists to gain new understanding. This mindset of exploration is what enables researchers to gain fundamental biologic insights, whether improving smFRET, creating new tools such as ConVERGD, or seeing structures such as mammalian cytonemes for the first time. By lighting the way forward, these St. Jude researchers are forging the next generation of discoveries.
Clinician scientists gather data about every patient who is treated at St. Jude, ranging from genome sequencing to treatment regimens to medical imaging.
Each experiment performed in St. Jude laboratories — from cell assays to cryo-electron microscopy to transcriptomics — also generates data. Given the amount of information generated, how does St. Jude process, understand, and use these data in the most meaningful and impactful ways? Traditionally, scientists and clinicians have focused only on the data that is relevant to their specific projects. The drawback of this approach is that it can isolate data from other researchers, thereby limiting its potential impact on a broader scale. To unify data across St. Jude, streamline analysis, develop skill and understanding, and unearth patterns that can be useful for biomedical research, St. Jude formed the Office of Data Science.

The Office of Data Science facilitates integrating and analyzing the vast amounts of data collected at St. Jude and helps researchers and clinicians extract meaningful, actionable insights. This innovative approach stands to make St. Jude a global leader in applying data science to biological discovery.
Leading this initiative is M. Madan Babu, PhD, FRS, Chief Data Scientist and Senior Vice President for Data Science. As a member of the Department of Structural Biology and the Director of the Center of Excellence for DataDriven Discovery, Babu will expand the role of data science and data-driven approaches throughout St. Jude.
“With our intellectual ecosystem of talented clinical, experimental, and


With our intellectual ecosystem of talented clinical, experimental, and data scientists united under the same mission, there’s no better place than St. Jude to build a data science enterprise of this magnitude.
M. Madan Babu,
PhD, FRS
Chief Data Scientist & Senior Vice President for Data Science
data scientists united under the same mission, there’s no better place than St. Jude to build a data science enterprise of this magnitude,” said Babu.
The power of this comprehensive institutional approach is in the collection of large, complex, and unique datasets that can be analyzed to answer a broader scope of biological questions. The Office of Data Science is working with the Information Services department to create an institutional hub in which data are securely housed and easily accessible for researchers wishing to tap into the power of “big data.” Furthermore, Babu and his team are developing ways to ensure the institution has the capacity to meet researchers’ current and future computing needs.
Alongside these endeavors, the Office of Data Science embraces innovation by developing novel computing technologies and optimizing preexisting technologies for
researchers’ computational workflows. With the establishment of the Office of Data Science, St. Jude will grow its capacity in the areas of artificial intelligence (AI), large language models, computational protein design, and quantum computing.
The push to incorporate innovation has already paid off, as Babu and his team are working to increase the efficacy and predictive power of an AIbased method called AlphaFold2. This software has been integral in predicting protein structure and function. Data scientists successfully integrated this software into the computational

We use AI in radiology to enhance image quality, increase diagnostic accuracy and detection of disease, reduce errors, and improve efficiency and communication.
Andrew Smith, MD, PhD Department of Diagnostic Imaging (Radiology as of Q3 of 2024)

pipeline at St. Jude, and this effort has already shown promise in accelerating the projects of researchers studying a variety of biological questions.
The power and potential of AI have implications across departments at St. Jude, including in the Department of Radiology. As the new department Chair, Andrew Smith, MD, PhD, is

integrating AI technology with medical imaging. When speaking of the impact of AI in radiology, Smith said, “Our field leads all other medical fields in the use of AI. We use AI in radiology to enhance image quality, increase diagnostic accuracy and detection of disease, reduce errors, and improve efficiency and communication.”
With assistance from AI, sedation time for patients undergoing positron emission tomography, computed tomography, or magnetic resonance imaging could be decreased as imageprocessing speeds improve. The technology can also ensure that tumor measurements are as accurate and precise as possible, providing valuable information to clinicians creating treatment plans and determining prognoses. An AI approach to pediatric radiology will be transformative, positioning St. Jude as a global innovator of pediatric cancer imaging.
The breadth of work at St. Jude is vast and interconnected. The data generated from the clinical and research enterprises are a tremendous asset that needs a team able to shepherd, cultivate, and make the data readily available. Through the
Office of Data Science and the work of Babu, Smith, and other St. Jude researchers invested in these technologies, the insights buried in data can be brought forth. With the true impact of data revealed, we can better understand human health and better serve our mission of advancing cures — and means of prevention — for pediatric catastrophic diseases through research and treatment.


St. Jude was established in 1962, in part to tackle the daunting task of improving childhood cancer survival, which was just 4%.
Today, with treatment protocols innovated at St. Jude, the five-year survival of the most common pediatric cancer, acute lymphoblastic leukemia (ALL), exceeds 90% in the United States. However, more work remains.
Our scientists are now putting every facet of the rarest and most treatmentresistant leukemia subtypes under the lens to find even the subtlest vulnerabilities and opportunities to improve outcomes for the remaining 10% of pediatric ALL cases.
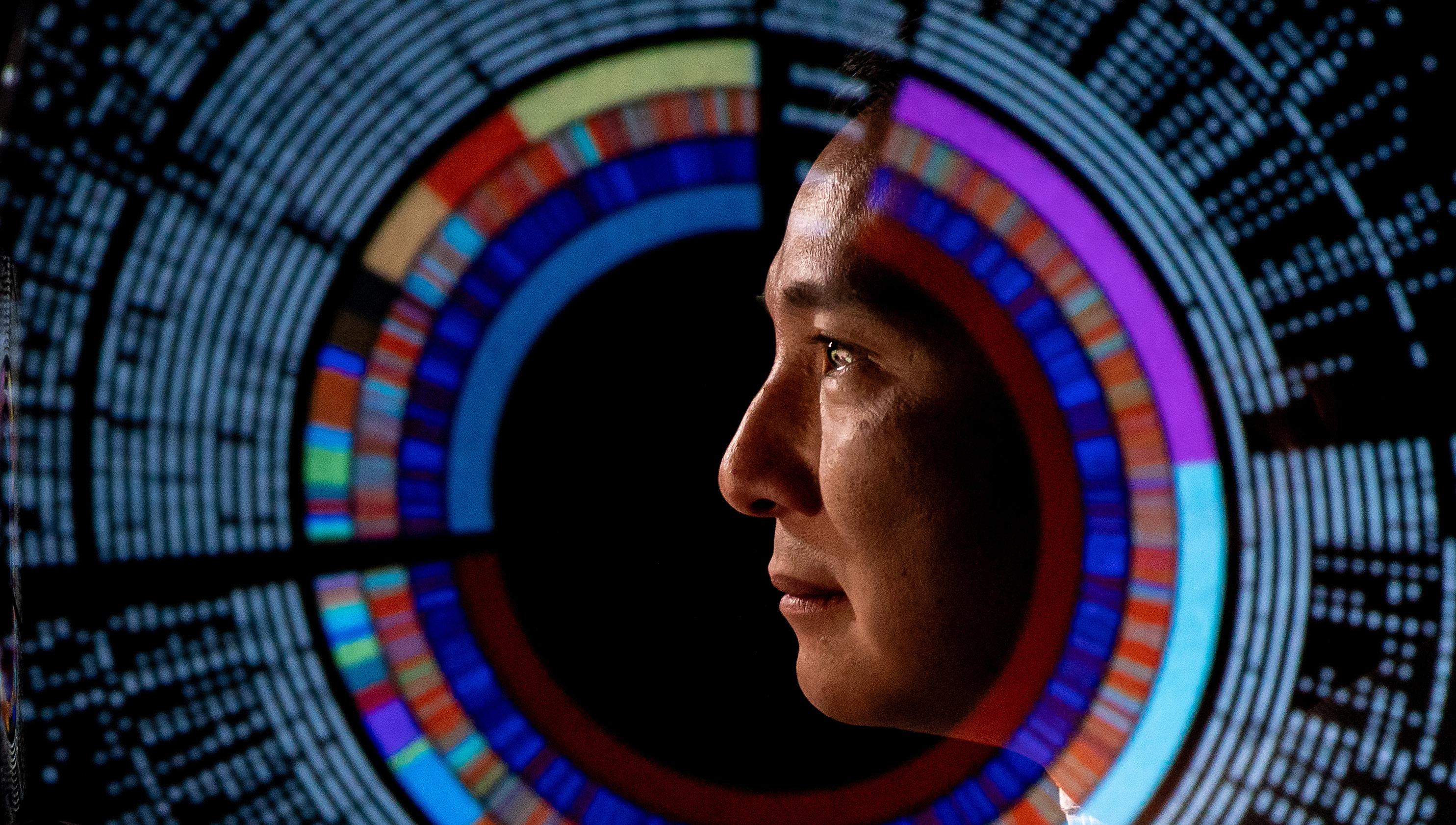
“ALL treatment is a great success story, but there remains a population of children whose disease is not fully cured,” said Charles Mullighan, MBBS (Hons), MSc, MD, Department of Pathology.
Mullighan co-led a study published in the Journal of Clinical Oncology that addresses the differences in survival
among children with standard-risk B-cell ALL (SR B-ALL) by identifying the genetic predictors of relapse. SR B-ALL is the most common form of pediatric ALL, and as such, nearly half of all relapsed pediatric ALL cases are SR B-ALL. Survival among patients with relapsed or resistant B-ALL falls between 30% and 50%, indicating a dire need for a better understanding of this subgroup.
The scientists conducted wholegenome and -transcriptome sequencing on SR B-ALL samples and compared data from patients who experienced relapse with patients who remained in complete remission. They found that B-ALL subtypes, genetic alterations, and patterns of aneuploidy (extra or missing chromosomes) were associated with the risk of and time to relapse. Some B-ALL subtypes, such as hyperdiploid ALL and ETV6::RUNX1 ALL, had a low frequency of relapse, but others, including PAX5altered, TCF3/4::HLF, ETV6::RUNX1-like, and BCR::ABL1-like ALL, were associated with an increased risk of relapse.
Based on these results, Mullighan suggested, “Children with SR B-ALL should have their tumor cell genome sequenced upon their initial diagnosis to identify if their tumor cells have these high-risk features so that their initial therapy intensity can be increased.”

ALL treatment is a great success story, but there remains a population of children whose disease is not fully cured.
Charles Mullighan, MBBS (Hons), MSc, MD Department of Pathology


Understanding the biology of drug resistance in cancer is one of the top research priorities for St. Jude scientists. In Cancer Cell, Jun J. Yang, PhD, Department of Pharmacy & Pharmaceutical Sciences vice-chair, and colleagues reported which B-ALL cells resist treatment and why, as well as a potential counter approach.
“We found a new explanation of B-ALL sensitivity to asparaginase, a drug commonly used for this disease,” said senior co-corresponding author Yang.
“We found leukemic B cells are stuck in two major stages,” said cocorresponding author Jiyang Yu, PhD, Department of Computational Biology interim chair, whose lab investigated gene expression from thousands of cancerous B cells. “One is an earlier stage that is more resistant to asparaginase and another later stage that is more sensitive to it.”
Leveraging single-cell network analysis and drug-sensitivity profiling, Yu and his colleagues discovered that treatment-resistant cancer cells exploit the cell death protein BCL-2 to evade self-destruction. The protein is also downstream of mTOR, asparaginase’s target. This resistance mechanism prompted the scientists to investigate the therapeutic usefulness of venetoclax, a BCL-2 inhibitor. They showed that combining asparaginase with venetoclax was more effective than either drug alone in laboratory models of three high-risk B-ALL subtypes.
“Administering asparaginase alongside venetoclax may reduce the risk of ALL relapse, which is the leading cause of treatment failure,” said co-author Ching-Hon Pui, MD, Department of Oncology. “These findings merit further investigation in future clinical trials.”
“We strive to be mindful, using only the necessary treatments to achieve a cure, so that we can minimize the risk of enduring side effects from a child’s cancer treatment,” said Katelyn Purvis, MD, a pediatric hematologyoncology fellow in the Department of Oncology and first author on a clinical trial study published in Blood designed to determine whether certain B-ALL subtypes can be cured with lower-intensity treatments.
Results showed that patients with ETV6::RUNX1 and high-hyperdiploid B-ALL, which, according to the National Cancer Institute risk assessment, would receive a highintensity treatment regimen, can be treated with a low-intensity regimen and still have positive outcomes.
“In the St. Jude Total Therapy XV and XVI studies, we incorporated genetic information and response criteria into our risk assessment. This risk classification system allows us to identify patients who can be treated with lower-intensity therapies while

We incorporated genetic information and response criteria into our risk assessment [which] allows us to identify patients who can be treated with lowerintensity therapies while ensuring those who require more intensive treatment receive it.
Hiroto Inaba, MD, PhD Department of Oncology
ensuring those who require more intensive treatment receive it,” said corresponding author Hiroto Inaba, MD, PhD, Department of Oncology.


Patients who would have otherwise received high-risk therapy experienced fewer side effects, such as thrombosis and pancreatitis. The findings suggest that clinicians can accurately identify patients likely to benefit from less intensive treatment by using genome- and early treatment response–guided risk classification.
While much research focuses on understanding B-ALL genetics after diagnosis, scientists can apply the same techniques to predict if a child is at a higher risk of cancer before it develops. In a study published in Blood, St. Jude researchers characterized variants in a single gene in children with B-ALL to determine which were risk factors for the disease.
“We found NBN is a key B-ALL risk gene,” Yang, the corresponding author, said. “We identified many genetic variants in this gene that seemed to be linked to B-ALL, and
we meticulously characterized their functional consequences.”
The researchers sequenced NBN in 4325 patients with B-ALL and found 25 unique, putatively damaging coding variants in 50 patients. These variants were overrepresented in children with this form of leukemia, suggesting that they predispose people to the disease.
Testing these variants in the lab, the scientists found that 14 variants caused severe loss of function of the protein encoded by NBN. NBN is involved in double-stranded DNA repair, so the loss of its activity provides a plausible mechanism for increased cancer incidence. However, NBN loss also represents a potential challenge for treating leukemia.
“As NBN is involved in DNA repair and many leukemia drugs cause DNA damage, we did worry that patients with variants would experience higher treatment-related toxicity,” Yang said. “But that did not seem to be the case, although the number of patients we studied was relatively small.” The researchers found that the survival of these patients was comparable


to that of patients without NBN variants, suggesting that patients with NBN variants can safely receive standard B-ALL care and experience a reasonable treatment outcome.

We found NBN is a key B-ALL risk gene [and] identified many genetic variants in this gene that seemed to be linked to B-ALL, [then] we meticulously characterized their functional consequences.
Jun J. Yang, PhD
Department of Pharmacy & Pharmaceutical Sciences



Childhood T-cell ALL (T-ALL) is an aggressive cancer that typically responds well to initial treatment, but relapsed T-ALL and treatment-resistant disease have dismal prognoses. Given its relative rarity, studying T-ALL genetics has been difficult. To address that need, St. Jude collaborated with other pediatric research hospitals to profile the whole germline and cancer genomes of more than 1300 children, adolescents, and young adults with T-ALL.
As published in Nature, T-ALL was classified into 15 subtypes with distinct gene expression and genomic drivers, including previously undefined subtypes. The researchers also refined the classification of known subtypes and showed that driver lesions, other genetic changes, and the original cell type cooperate to define the genomic subtype and a condition’s clinical and biological characteristics. They also observed a significant link between the kind of gene alterations and outcomes in T-ALL.
The study found that approximately 60% of the genetic changes driving T-ALL cells are noncoding changes.
“It was striking how abundant these noncoding changes were and how many of them were enhancer-

perturbation events,” Mullighan, a co-corresponding author, said. “We now have a much stronger framework to take these alterations back to the lab, build the right models to understand the biology, and test therapy.”
Investigators from St. Jude and an international collaborative group of more than 50 researchers joined forces to understand the rare but aggressive gamma delta T-cell ALL (γδ T-ALL). In Cancer Discovery, they reported identifying 200 children with γδ T-ALL, the largest cohort of the disease.
“We needed a large collaborative effort to understand the genetics in these cases to figure out how to potentially treat them,” cocorresponding author Inaba said.
The researchers found that genetic alterations resulting in activation of LMO2, a gene commonly altered in other types of T-ALL, and inactivation of STAG2, a gene more commonly altered in acute myeloid leukemia (AML) and solid tumors, were associated with worse outcomes.
“This alteration switches STAG2 off, taking the STAG2 promoter and moving it proximal to LMO2, switching it on,” Mullighan, a co-corresponding author,

said. “This dual mechanism is unusual and provides insight into what happens at the genomic level in this rare cancer.”
That insight also highlighted potential treatment strategies, informing drug-screening design to identify therapeutics that may help treat γδ T-ALL. PARP inhibitors, which target dysfunctional DNA-repair pathways in cancer cells, showed some promise. STAG2 is an important protein that acts as a subunit of the cohesin complex, which stabilizes DNA replication forks and helps maintain chromosomes. When STAG2 is mutated, doublestranded DNA breaks become more common. PARP inhibitors could plausibly target STAG2’s functional defect, accelerating DNA damage accumulation and driving cancer cells toward self-destruction.
Inaba expressed optimism about PARP inhibitors, “This is very exciting to identify a potential targeted therapy for these patients who have typically poor outcomes.”
Despite constituting only 20% of pediatric acute leukemias, pediatric acute myeloid leukemia (pAML) remains the leading cause of mortality among children with leukemia. However, “most of what we know about classifications

Most of what we know about classifications of AML comes from the adult field. Many of the AML types we see here at St. Jude, you just don’t see in adults.
Jeffery Klco, MD, PhD Department of Pathology
of AML comes from the adult field,” said Jeffery Klco, MD, PhD, Department of Pathology, who led a study published in Nature Genetics to define the molecular underpinnings of pAML.
“Many of the AML types we see here at St. Jude, you just don’t see in adults.”
Therefore, the researchers examined 887 unique pAML cases via transcriptome and gene profiling. The findings established 23 distinct molecular categories, including 12 not included in the current classification systems.
Their results showed that while the normal accumulation of mutations during aging may explain many adult AML cases, fusion oncoproteins are major drivers in more than 70% of pAML cases. “Some categories show very similar transcriptional profiles, indicating that the background biology is similar and can potentially be treated by similar drugs,” said first author Masayuki Umeda, MD, PhD, a postdoctoral fellow in the Department of Pathology.
By combining the transcriptome and gene profiling analysis with clinical data, the researchers determined a strong association between the new pAML subtypes and clinical outcomes.
“The study fills many gaps in the current classification of pAML,” first author
Jing Ma, PhD, a principal bioinformatics research scientist in the Department of Pathology, confirmed. “It provides a risk-stratification strategy we hope will provide clinicians with a simpler road to accurate diagnosis and optimal treatment in the future.”
A gene fusion called PICALM::MLLT10 (PM) is a rare but recurring genetic driver associated with different acute leukemia subtypes. PM-positive AML (PM-AML) is uncommon and accounts for less than 1% of pediatric cases but has particularly poor outcomes. St. Jude scientists compared the genetic and transcriptomic profiles of PM-AML and T-cell acute lymphoblastic leukemia/ lymphoma with PM fusions (PM –T-ALL/ LLy) to “identify subtype-specific molecular signatures that could offer insights into disease development, progression, and potential therapeutic targets,” said co-author Rebecca Voss, MD, an associate scientist in the Department of Pathology.
Published in Leukemia, results show that among patients with PM-AML, there is a high frequency of alterations in TP53 and NF1, which normally help prevent cancer. “The most compelling finding from our study was that patients with AML with this fusion typically have cooperating mutations in the TP53 gene, which you don’t particularly see in T-ALL cases,” co-author Klco said.
Additionally, investigators found that PHF6 was the most frequently mutated gene in this study cohort, occurring in both PM-AML (approximately 70%) and PM–T-ALL/LLy (37.5%). PHF6 is an epigenetic remodeler that regulates gene expression.
“PHF6 alteration is commonly associated with T-ALL, so finding its high frequency in PM-AML cases was quite surprising, suggesting it plays a key role cooperating with the PICALM::MLLT10 fusion in leukemogenesis, particularly in PMAML,” said corresponding author
Lu Wang, MD, PhD, Department of Pathology. The elevated expression of specific HOXA genes and XPO1 demonstrated in this study supports the potential use of Menin inhibitors and SINEs (short, interspersed nuclear elements) for treating these rare and challenging forms of leukemia.

Our study reveals a unique molecular landscape in PMAML and underscores the need for further investigation into its underlying molecular pathogenesis.
Lu Wang, MD, PhD Department of Pathology

“Overall, our study reveals a unique molecular landscape in PM-AML and underscores the need for further investigation into its underlying molecular pathogenesis,” said Wang.
By looking ever more closely at rare and relapsed leukemia subtypes, investigators at St. Jude are discovering how to treat these cancers more effectively. Until the cure for leukemia reaches 100%, scientists will keep putting leukemia under the lens — increasing scrutiny to detect the smallest features of these diseases that can be leveraged therapeutically.
From bank statements to email, computer programs use passwords to secure important information. Cellular programs also secure information in chromatin, the complex of DNA and its associated proteins.
Cells use “biochemical passwords” comprising chemical modifications and interactions among proteins to allow or restrict access to specific genes within chromatin. St. Jude researchers are identifying how cancer cells crack the chromatin code to steal or mimic these passwords and how scientists can hack that same code to stop — or even revert — pediatric cancers.
Ependymoma, the third most common type of brain tumor in children, has no known effective therapeutic targets. In collaboration with Baylor College of Medicine, Stephen Mack, PhD, Department of Developmental Neurobiology, and his colleagues engineered a mouse model of the cancer and found how aberrant neuronal activity impacts ependymoma cells by regulating pro-tumor genes wrapped in chromatin. The study, published in Nature, revealed an unexpected mechanism that may be a target for future therapies.
The research revealed that serotonin transporters are enriched within tumor cells with the ZFTA–RELA gene fusion, implying that the tumor cells forage serotonin from their environment. Serotonin was imported into ependymoma cells and attached to the histones that make up chromatin, a process called serotonylation. The presence of the ZFTA–RELA fusion protein and serotonylation allowed full access to the proliferative genes, thereby aiding tumor growth.

Finding that histone serotonylation regulates tumorigenesis and that it’s being driven by neurons in the microenvironment is remarkable, it could apply to other tumor types too.
Stephen Mack, PhD Department of Developmental Neurobiology

“Finding that histone serotonylation regulates tumorigenesis and that it’s being driven by neurons in the microenvironment is remarkable,” said Mack. “It could apply to other tumor types too.” Neuromodulatory agents, such as selective serotonin reuptake inhibitors (SSRIs), are currently used to treat certain mental health conditions. Although these agents have not been tested on brain tumors, the findings suggest they are an avenue worth exploring.

Therapeutic targeting of mutant genes is a promising frontier in the fight against cancer; however, many cancers are caused by the complete loss of a gene. This is a challenge for researchers because, in those cases, the protein encoded by the gene is no longer present to be targeted. Loss of the tumor-suppressor protein SMARCB1 is implicated in rhabdoid tumors, which comprise aggressive cancers that primarily affect infants and very young children. St. Jude researchers led by Charles W.M. Roberts MD, PhD, executive vice president and St. Jude Comprehensive Cancer Center director, were looking for a way to treat aggressive rhabdoid tumors caused by the loss of SMARCB1 when they found a new approach to treatment.
Published in Nature, the study showed that a little-studied protein, DCAF5, is essential to rhabdoid tumors missing SMARCB1. Initially, the team identified DCAF5 as a target by using the Dependency Map (DepMap) portal, a database of cancer cell lines and genes critical for their growth. When the scientists genetically deleted or chemically degraded DCAF5, the cancer cells reverted to a noncancerous state, resulting in the sustained remission of the cancer in the mouse model. “We saw a spectacular response,” said Roberts. “The tumors melted away.”
Normally, SMARCB1 is an essential component of a larger chromatinregulating complex of proteins called the SWI/SNF complex. Unexpectedly, the study found that in the absence of SMARCB1, DCAF5 recognizes SWI/ SNF as abnormal and destroys the complex. The researchers showed that when DCAF5 is degraded, SWI/ SNF re-forms and maintains its ability to open chromatin and regulate gene expression to an extent sufficient to reverse the cancer state fully.
“The mutation of SMARCB1 shuts off gene programs that prevent cancer. By targeting DCAF5, we’re turning those

Myriad types of cancers are caused by tumor suppressor loss. We hope we have opened the door to thinking about new ways to target at least some of these by reversing, instead of killing, cancer.
Charles W.M. Roberts, MD, PhD
Executive Vice President, Director of the St. Jude Comprehensive Cancer Center
gene programs back on,” said first author Sandi Radko-Juettner, PhD, a former St. Jude Graduate School of Biomedical Sciences student, now a research program manager for the Hematological Malignancies Program.
“We have demonstrated a beautiful proof of principle,” Roberts said. “Myriad types of cancers are caused by tumor suppressor loss. We hope we have opened the door to thinking about new ways to target at least some of these by reversing, instead of killing, cancer.”
In another study, Roberts’s team again leveraged DepMap to systematically identify genes that become essential to cancer cells when SMARCB1 is absent because those genes present potential routes for future targeted therapies.
“We discovered PHF6 as another one of those genes,” said Roberts. “We found that in healthy cells, PHF6 co-
localizes with SMARCB1 and helps the SMARCB1-containing SWI/SNF complex keep chromatin open, which then becomes aberrant without SMARCB1.”
In healthy cells, SMARCB1 and PHF6 act like two-factor authentication, both of which are necessary for genes to be turned on. Although SMARCB1 loss promotes cancer, its absence should shut down the expression of so many genes that the cell would die. When SMARCB1 is lost, PHF6 keeps many of those genes turned on, allowing the cancer cells to survive. Removing PHF6 from these cells caused cell death and slowed or stopped tumor growth, revealing a potential vulnerability to target in rhabdoid tumors and possibly other cancers.
“Twenty percent of cancers have mutations in SWI/SNF subunits,” Roberts explained. “This work on dependencies could advance the opportunity to find therapeutic interventions far more broadly than just rhabdoid tumors.”
The tight regulation of chromatin protects cells from carrying out potentially harmful gene expression programs while promoting the expression of protective genes, such as tumor suppressors. These fundamental processes often go awry in pediatric cancer, highlighting the tremendous opportunity to leverage chromatin control therapeutically.
St. Jude scientists are well poised to continue cracking the chromatin code, finding new targeted therapies for some of the most difficultto-treat pediatric cancers.


Living things all have needs, such as water, sunlight, or nutrients. Tending to the root of health means addressing the foundational factors, such as genetics or the environment, that shape these needs and impact health.
Predicting, preventing, and intervening against disease ensures that children at risk of negative health outcomes receive the proper care under the right conditions to thrive. At St. Jude, scientists are studying how to predict who is at risk of disease and which interventions will be most beneficial to prevent diseases from occurring in the first place.
Disease detection is entering a golden era where sophisticated classification strategies and genetic screening panels fuel the development of novel detection methods that can lead to better outcomes for patients.
Physicians use this knowledge to tailor targeted treatments to the specific cancer-causing mutations affecting each patient. However, current high-quality wholegenome sequencing requires physical and computational infrastructure that most institutions lack. To address this bottleneck, Xiaotu Ma, PhD, Department of Computational Biology; Jeffery Klco, MD, PhD, Department of Pathology; and John Easton, PhD, Computational Biology Genomics Laboratory director, developed SJPedPanel. Published in Clinical Cancer Research, SJPedPanel is a sequencing platform focusing on genes involved in childhood cancer instead of looking at the entire genome.


Even though adult cancers are genetically distinct from childhood malignancies, all available genetic screening panels were designed for adult cancers and then adapted for pediatric cancers. St. Jude was one of two institutions that conducted the Pediatric Cancer Genome Project, which sequenced the genomes of 800 patients whose diagnoses included 23 types of cancer to provide the most detailed overview of the genomic landscape of many pediatric cancers. The SJPedPanel covers the risk-related genome regions, occupying just 0.15% of the genome, to provide a comprehensive assay to detect the full spectrum of mutations in pediatric cancers.
“We compared this panel with six commercially available panels,” Ma said. “SJPedPanel provides the most coverage of pediatric cancer driver genes, providing close to 90% when others are closer to 60% coverage.”
In addition to working better than adapting adult-focused cancer
gene panels, the SJPedPanel outperforms gold-standard wholegenome sequencing in some circumstances. Whole-genome sequencing interrogates the entire human genome, making detecting low–cell-count cancers difficult.
“There are certain situations, such as low tumor purity samples or even testing after bone marrow transplantation, where current clinical whole-genome sequencing approaches don’t work,” Klco said.
“This fills an important clinical gap for our patients.” SJPedPanel is now part of the routine clinical service at St. Jude and will soon be used to monitor patient response during therapy.
The panel will give institutions without resources, such as wholegenome sequencing, a better chance at identifying cancers.
“Panels like the SJPedPanel are easier for clinical or research labs to implement than whole-genome sequencing,” Easton said.

SJPedPanel provides the most coverage of pediatric cancer driver genes, providing close to 90% when others are closer to 60% coverage.
Xiaotu Ma, PhD Department of Computational Biology


Detecting cancer before it can spread is critical to ensuring overall and longterm health. Even if interventions work on most of a tumor, biological resistance means small populations of cancer cells often survive, and those cells are more challenging to treat. Determining how these robust malignant cells escape treatment is key to true prevention.
The survival of children with relapsed or recurrent ALL is 30% to 40%, often due to therapy resistance. In research published in Nature Communications, Daniel Savic, PhD, Department of Pharmacy & Pharmaceutical Sciences, identified and investigated mechanisms behind functional variants within the noncoding region of the genome and explored their contribution to resistance using six drugs that treat leukemia. Despite being devoid of genes, the noncoding region of the genome comprises 98% of DNA and contains a vast number of gene

We harnessed innovative tools and technologies to systematically examine the noncoding genome and understand its functional effects on ALL pharmacogenomics.
Daniel
Savic, PhD Department of Pharmacy & Pharmaceutical Sciences
regulatory elements, some of which could contribute to resistance.
By combining massively parallel reporter assays and three-dimensional chromatin looping assays, the St. Jude researchers identified more than 1600 inherited noncoding variants associated with drug resistance in ALL with gene-regulatory roles. This comprehensive study, the largest of its kind to date, prioritized 556 functional noncoding DNA variants that affected gene regulation related to ALL drug resistance in at least three ALL cell lines, identifying a previously unknown resistance mechanism to the chemotherapy drug vincristine. This finding was based on a functional interrogation of the most robust variant, linking its proximity to the gene for EIF3A, a protein involved in cell proliferation and survival, to its resistance mechanism.
“In any genome-wide association study, nearly all associated genetic variants reside in the noncoding genome, so connecting that variation to gene function and an actual trait, such as



chemotherapy resistance or disease predisposition, is challenging,” Savic said. “We harnessed innovative tools and technologies to systematically examine the noncoding genome and understand its functional effects on ALL pharmacogenomics. We hope to utilize our findings to improve clinical outcomes in ALL patients.”
Genetics can directly affect how patients respond to treatments and interventions. Acute lymphoblastic leukemia (ALL) affects both children and adults. Children with ALL have a better chance of being cured than adults; long-term survival of childhood ALL exceeds 90%, compared to that of adults, which is 50% to 75%. However, whether ALL has an age-related drugresponse profile is unclear. In a study published in the Journal of Clinical Oncology, a team led by Jun J. Yang,
PhD, Departments of Pharmacy & Pharmaceutical Sciences and Oncology, examined 767 children and 309 adults with B-cell ALL, assessing the sensitivity of leukemia cells to 21 drugs.
“We found that, for most of the cytotoxic drugs with differential activity between adult and pediatric, it’s largely explained by the age-related differences in the underlying genomic abnormalities of their cancer, namely molecular subtypes,” Yang said.
However, the molecular subtypes of ALL did not explain all the differences in antileukemia drug sensitivity between children and adults. The researchers found that some children had “adultlike” ALL based on their gene expression profiles, making them more resistant to treatment and leading to poorer outcomes. This finding suggests that age and individual genomics beyond the ALL subtype must be considered to predict treatment response.
“There’s a lot of heterogeneity within each age group,” explained Yang. “You cannot simply divide patients
into older than or younger than 18 years and offer therapy based on the legal age of majority; you have to look at their underlying molecular characteristics and pharmacogenomic features.” Together, the group’s findings suggest the need for tailored treatment strategies for both children and adults with B-cell ALL.
Genetic predispositions are found in 5% to 15% of children with cancer. In a study published in JAMA Oncology, Kim Nichols, MD, Division of Cancer Predisposition director, Department of Oncology, showed that beginning surveillance soon after recognizing a patient’s predisposition often leads to discovering one or more early-stage asymptomatic tumors, most of which could be removed after chemotherapy and/or radiation therapy, and about half of which could be removed surgically.


The researchers examined 274 pediatric patients at St. Jude who carried 35 different cancer-predisposing syndromes over a median of three years. Surveillance revealed 35 tumors in 27 patients, representing a broad array of solid and central nervous system cancers. This group included a subset of about 17% of children who had a new tumor identified while they were still undergoing treatment for a prior cancer. This finding suggests providers should not wait until a child has finished treatment for their first cancer before they start screening for other potential malignancies.
To find potential cancers and guide treatment, clinicians used various surveillance methods. For example, a predisposition for a solid tumor may lead to annual full-body magnetic resonance imaging (MRI). Standard surveillance methods had minuscule false positive and false negative rates.

Understanding whether children have an underlying genetic risk for cancer can greatly impact their clinical care. Proactive surveillance for new tumors is an important component of this care.
Kim Nichols, MD Department of Oncology
data collections, such



“We’ve shown that standardized surveillance protocols provide a very effective way to detect new tumors at their earliest and most treatable stages,” Nichols said. “Understanding whether children have an underlying genetic risk for cancer can greatly impact their clinical care. Proactive surveillance for new tumors is an important component of this care.”
The study may enable more providers to order these effective, yet sometimes expensive, tests. It can be challenging for providers to get insurance companies to pay for early screening. Historically, this has created a difficult cycle where providers could not order the tests, which meant there was no strong evidence of their value, preventing their use. Patients at St. Jude are treated regardless of insurance coverage, thus enabling physicians to order the appropriate tests. The excellent performance of the standard screening methods is evidence that early testing can improve detection and outcomes. This may give insurance companies the evidence needed to cover the tests for children with a predisposition.
Cancer has lifelong effects. Survivorship research focuses, in part, on predicting and preventing these long-term adverse effects. Published in the Journal of Clinical Oncology, a study led by Yadav Sapkota, PhD, Department of Epidemiology & Cancer Control, identified four previously unknown genetic variants associated with diabetes risk in childhood cancer survivors. Furthermore, the genetic risks for diabetes appeared to be not only magnified by childhood exposure to alkylating agents (a common class of chemotherapeutics) but also exacerbated by ancestry.
“The genetic risk disproportionately affected survivors of African or African American ancestry previously treated with alkylating agents,” Sapkota said.
“The same variant is implicated in both European and African ancestry groups, but the amount of risk conferred by carrying the variant differs.”
In addition to individual genetic variants, combinations of many genetic variants previously associated with diabetes risk in the general population, considered as a score, have been studied to assess disease risk in childhood cancer survivors. However, these scores have been derived typically from studies involving only individuals of European descent. Thus, the researchers compared three scores: one based on those of European descent only and two others developed by including individuals of different ancestries. The more inclusive scores more accurately predicted diabetes risk in survivors of both European and African ancestries.

Now we know how to identify childhood cancer survivors most at risk of diabetes so we can provide more personalized opportunities for interventions and prevent cardiovascular complications down the road.
Yadav Sapkota, PhD Department of Epidemiology & Cancer Control
“We hope this information will help reduce differences in the diabetes burden,” Sapkota said. “Now we know how to identify childhood cancer survivors most at risk of diabetes, so we can provide more personalized opportunities for interventions and prevent cardiovascular complications down the road.”
While detecting disease risk is at the root of improving clinical outcomes, long-term monitoring is required for quality-of-life improvements to endure. Treatment for medulloblastoma, a type of childhood brain tumor, is associated with neurocognitive impairments. The outlook for patients with medulloblastoma has improved over time. However, Tara Brinkman, PhD, Departments of Psychology & Biobehavioral Sciences and Epidemiology & Cancer Control, and her colleagues showed in research published in Neuro-Oncology that the risk of neurocognitive impairment remains a concern.
The researchers surveyed 505 survivors of medulloblastoma from the Childhood Cancer Survivor Study (CCSS), a multiinstitution retrospective cohort with prospective follow-up led by Gregory Armstrong, MD, MSCE, Department of Epidemiology & Cancer Control chair. They categorized the participants based on the treatment received.
Childhood medulloblastoma survivors who were treated between 1970 and 1999 experienced as much as a fivefold increased risk of cognitive deficits compared to that of their healthy siblings. Notably, the researchers observed that the survivors’ ability to achieve independence in adulthood is adversely impacted by the development of neurocognitive problems and chronic health conditions after treatment for medulloblastoma.
“Routine surveillance of neurocognitive functioning in survivors remains critical



to understanding the long-term effects of contemporary therapies,” Brinkman said. “Surveillance efforts further inform our ability to prevent and manage disease and treatment-related late effects to optimize quality of life.”
In addition to how clinical factors affect patient outcomes, research on how contextual factors such as low socioeconomic status, unstable housing, and transportation barriers affect the health of childhood cancer survivors mainly focused on those survivors who reached adulthood. This approach has left a gap in understanding the experiences of children and adolescents at least five years postdiagnosis and younger than 18 years.
Published in JAMA Network Open, a study by I-Chan Huang, PhD, Department of Epidemiology & Cancer Control, examined the physical and psychological symptoms in children and adolescents aged 8 to 18 years and explored the contextual factors’ impacts. This involved identifying associations with sociodemographic, clinical, and psychological resilience skills and health-related quality of life. The study provides a comprehensive portrait of the challenges faced by young survivors and suggests ways to develop targeted interventions.
By examining contextual factors in 302 young childhood cancer survivors, the investigators found that nearly 40% of the cohort self-reported moderate or high cumulative overall symptom burden. Factors that correlated strongly with symptom burden included caregiver anxiety and neighborhood deprivation, which cover aspects such as income and living environment. “If parents have anxiety, there is almost a two-fold higher risk that survivors will have a higher symptom burden,” Huang explained. This conclusion is compounded by evidence showing that children living in high-vulnerability neighborhoods have a five-fold higher risk of experiencing high symptom burden.
The study identified preventative factors that can mitigate symptom

Routine surveillance of neurocognitive functioning in survivors remains critical to understanding the long-term effects of contemporary therapies.
Tara Brinkman, PhD Departments of Psychology & Biobehavioral Sciences and Epidemiology & Cancer Control
burden. For example, “We found the association between parents’ anxiety and the survivor’s disease burden decreases with high levels of survivor resilience,” said Huang. A sense of resilience reduced the impact of negative contextual factors on symptom burden by 30% to 40%.
However, while the survivor’s resilience can mitigate personal and family issues, community factors need broader solutions. “We need to find a way to identify and screen for the origin of their symptoms, then provide the necessary intervention,” Huang said.
Patient-reported outcomes are a key metric to understanding symptom burden, but clinicians are limited by the frequency of assessments — often only once every couple of years. “I don’t believe using these snapshots to understand symptom burden is enough,” Huang said. “I want to see the dynamics of the symptoms and how they evolve over time.”
In a pilot study of 41 participants published in Cancers and a larger



study protocol involving 600 survivors described in Frontiers in Oncology, Huang explored utilizing mobile health technology (mHealth) to achieve this. The researchers collected daily symptom data, momentary digital biomarkers (e.g., heart rate variability, respiratory rate, skin temperature, etc.), and overall progression of late effects over five years. The mobile platform enabled the researchers to send symptom and quality-of-life surveys to participants daily, which prompted them to report on 20 symptoms. They also tracked digital biomarkers through wearable activity monitors.
The researchers noted that some symptoms remained stable, but many demonstrated high variability from day to day, month to month, and even between individuals. “It suggests that we need more frequent symptom assessments rather than relying on yearly or less frequent clinic visits,” said Huang. “This also means that intervention strategies should be tailored to account for this variability.”

I want to see the dynamics of the symptoms and how they evolve over time.
I-Chan Huang, PhD Department of Epidemiology & Cancer Control
To collect robust data, using wearable devices represents a key feature of the study to Huang. “Combining wearable device data, such as heart rate, activity levels, and sleep patterns, with selfreported symptom data allows us to
identify patterns,” Huang said. “We can then predict various disease progression outcomes and integrate this prediction algorithm into the clinical workflow as a key component of the clinical warning system for managing late effects.”
While there is no exact blueprint for human health that will tell providers exactly who is at risk of disease or how to treat them, scientists are working to fill in gaps in knowledge, giving providers clues about the factors that influence health and how they can be assessed, modified, and used to tailor care for each person. A vast array of factors shape a person’s health, and with the right interventions, challenges can be overcome. Just as a plant with proper care can flourish despite harsh conditions, children can thrive when the root factors that shape their health care outcomes are understood.



A healthy heart is vital, but for survivors of catastrophic pediatric illnesses such as cancer and people with sickle cell disease, maintaining a healthy heart can be a challenge.
Sickle cell disease causes red blood cells to clump together and clog blood vessels, potentially resulting in heart injury and myocardial fibrosis (scar tissue buildup). “Sickle cell disease chips away at the wall of your health one brick at a time,” said Akshay Sharma, MBBS, MSc, Department of Bone Marrow Transplantation & Cellular Therapy.
Bone marrow transplantation is used to cure sickle cell disease, but myocardial fibrosis was thought to be irreparable by the treatment. Research published in Blood by Sharma and collaborators showed that not only did heart function recover, but myocardial fibrosis damage was reversed, which no disease-modifying treatment has previously achieved.
While myocardial fibrosis can be reversed, cardiovascular risk in survivors of pediatric cancer may not be fully realized until they are older. A study in The Lancet Oncology led by Greg Armstrong, MD, MSCE, Department of Epidemiology & Cancer Control chair, showed that by age 50, survivors experience a cumulative incidence of major adverse cardiovascular events (MACE) almost 20 times higher than average. Frequent screening was shown to detect this increased risk for

MACE. This suggests that proactive screening can help risk management since these conditions are detectable by electrocardiogram or echocardiography.
“Clinicians need to be aware that cancer survivors are at higher risk than the general population,” said Armstrong. “They should screen survivors appropriately and maintain a low threshold for referral to a cardiologist.”
Early detection can also help prevent other long-term heart risks among survivors. In the Journal of Clinical

Oncology, Stephanie Dixon, MD, MPH, Department of Oncology, showed a high prevalence of prediabetes in young adult survivors, which increases their risk of diabetes and related cardiovascular and kidney disease.
“We need to help survivors understand that prediabetes is an early warning sign that should lead to a change, whether that’s lifestyle, medication, or close primary care follow-up,” Dixon said. “But that change starts with physicians identifying when a survivor has developed prediabetes.”

it manifests
Estimating the risk of cardiovascular diseases isn’t straightforward, as many are asymptomatic until a severe event occurs. In a study published in the Journal of Clinical Oncology, Matthew Ehrhardt, MD, MS, Department of Oncology, found that two common biomarkers, global longitudinal strain (GLS) and N-terminal-pro-
B-type natriuretic peptide (NTproBNP), could identify survivors with normal appearing heart function at elevated risk of heart disease.
GLS measures the heart muscle’s ability to contract and relax with each cycle via echocardiogram. NT-proBNP is a serum biomarker released into the bloodstream when the heart is injured or overworked.
“The increased risk of developing cardiac dysfunction observed in individuals with abnormal GLS and

Clinicians need to be aware that cancer survivors are at higher risk than the general population. They should screen survivors appropriately and maintain a low threshold for referral to a cardiologist.
Gregory Armstrong, MD, MSCE Department of Epidemiology & Cancer Control

NT-proBNP supports investigating early interventions to prevent heart failure progression,” said Ehrhardt.
By studying the impact of treatments, early detection, and interventions, St. Jude researchers are making significant strides toward preserving and protecting the heart health of survivors of pediatric disease.



T cells are the body’s frontline protectors, pivotal in the immune system’s defense against disease.
Understanding T-cell biology is of great significance for immunotherapy, in which genetically modified T cells have demonstrated potential to treat cancers once considered incurable.
However, while these therapies have offered a chance at remission to some patients, they have not been universally successful.
The challenge of immunotherapy lies in optimizing T-cell performance — enhancing their activation, longevity, and function to ensure they respond robustly and sustainably.
Understanding these processes is central to improving immunotherapies as researchers explore ways to “finetune” T cells, thereby preventing their limitations and ensuring they function at their peak for longer periods.
At St. Jude, researchers harness the power of T cells by diving deep into their biology and discovering how to enhance their precision and persistence. These advances are opening the door to more effective therapies, bringing us closer to harnessing the power of the immune system to target and destroy tumors with minimal side effects.

Our research uncovers the mechanisms by which T cells adjust to extracellular nutrient conditions and connects these mechanisms to a key intracellular organelle, the lysosome.
Hongbo Chi, PhD Department of Immunology



To better understand and optimize the therapeutic application of T cells in cancer and other diseases, researchers at St. Jude use fundamental T-cell biology to unlock new ways to enhance immune efficacy. Hongbo Chi, PhD, Department of Immunology, studies metabolic systems and signaling pathways in T cells and capitalizes on those pathways to harness T cells’ antitumor and tissue immunity functions.
“T cells migrate to various tissues and must adapt to the local nutrient environment. Our research uncovers the mechanisms by which T cells adjust to extracellular nutrient conditions and connects these mechanisms to a key intracellular organelle, the lysosome,” Chi explained.

immune responses to nutrient availability and lysosomal function.
These findings, published in Immunity, highlight the complex interplay between metabolism and T-cell function and offer new insights into how T cells can be optimized to improve immune responses in tissues.
T-cell function is governed by metabolism and the ability to distinguish self from non-self, a process overseen by regulatory T (TREG) cells. The protein Foxp3 serves as a gatekeeper, or master regulator, determining what the immune system recognizes as “self” to protect from attack. However, the exact mechanism behind this process has remained elusive.

Tissue-resident memory (TRM) and TRM–like cells provide rapid, localized immune responses at the site of infection or tumor growth. Chi’s team used CRISPR-Cas9 genetic screens to uncover critical signaling pathways influencing TRM cell development and differentiation. They found that TRM cell formation depends on processes in cellular organelles called mitochondria. Additionally, signaling nodes at the lysosome, such as Folliculin (Flcn), Ragulator and Rag GTPases, restrict TRM formation and development.
Apart from organelle signaling, the study also found that nutrient availability played a role in tissue immunity. Specifically, Flcn modulates the activity of transcription factor EB (Tfeb). Flcn–Tfeb signaling, induced by amino acid deprivation, contributes to TRM cell development. The relationship links nutrient stress to cell fate decisions. Therefore, the Flcn–Tfeb axis is a regulatory pathway that coordinates

As immunologists, we don’t just want to understand the mechanisms; we want to know how we can take advantage of this knowledge to engineer better therapies.
Yongqiang Feng, PhD Department of Immunology
A study led by Yongqiang Feng, PhD, Department of Immunology, and published in the Journal of Experimental Medicine, examined Foxp3. For decades, Foxp3 has been considered a transcription factor, a protein that coordinates gene expression. The tunable nature and broad swath of responses that Foxp3 controls led Feng to question the biochemical nature of how this transcription
factor itself was regulated. How did Foxp3 know whether to coordinate a suppressive immune response?
The researchers studied the relationship between Foxp3’s protein-binding partners and its function, making a surprising discovery. “We found that when the environmental conditions changed, the ability of Foxp3 to interact with DNA also changed,” Feng said. “We found the Foxp3 does not directly interact very much with the DNA but rather binds to other DNA-binding proteins. In this sense, it is a transcriptional cofactor.”
These findings suggest that environmental triggers activating regulatory T cells drive the expression of Foxp3’s binding partners, which then coordinate with Foxp3 to establish the appropriate immune response. Foxp3 swaps out these binding partners depending on the environmental cue. These environmental triggers help Foxp3 regulate TREG cell function, control immune responses, and prevent autoimmune disease, but they can also promote tumor growth. This new paradigm proposes druggable strategies to modulate TREG cell function.
“By exploring the configuration of Foxp3 protein, we hope to identify new druggable targets and design a better protein, leading to better TREG cells, meaning better treatments,” said Feng. “As immunologists, we don’t just want to understand the mechanisms; we want to know how we can take advantage of this knowledge to engineer better therapies.”
In a separate study, Benjamin Youngblood, PhD, Department of Immunology, and Caitlin Zebley, MD, PhD, Department of Bone Marrow Transplantation & Cellular Therapy, in collaboration with researchers at the University of Minnesota, discovered that T cells can proliferate indefinitely without the typical functional decline seen in most cell types. This work, published in Nature Aging, revealed that T cells can outlive an organism, potentially enduring multiple lifetimes.
To study this phenomenon, the researchers used specific biomarkers known as epigenetic markers that accumulate over time. This “epigenetic clock” tells a retrospective story about the life cycle of a cell independent of the organism itself. The accumulation of genetic mutations, the shortening of telomeres (the protective caps

on chromosomes) and methylation patterns are currently regarded as the most accurate ways to interrogate the process of aging.
Through a collaboration with investigators at the University of Minnesota, the researchers utilized a mouse model that maintained the same line of T cells through several life cycles. Based on the markers of the epigenetic clock, the researchers found that the T cells were not bound by the reasonable limits of organism lifespan, surviving for up to four lifetimes. This study underscores the pivotal role of epigenetics in T-cell aging and function, revealing how molecular mechanisms extending beyond chronological age can influence cellular memory and longevity.
Immunotherapies face challenges impacting their effectiveness, particularly maintaining functional persistence, which ultimately reduces the long-term efficacy of such treatments. When T cells


are overstimulated, they become exhausted, a nonfunctional phase that significantly impairs their ability to destroy tumors. T-cell exhaustion has emerged as one of the primary reasons many T cell–based immunotherapies fail.
In a paper published in Nature Immunology, Youngblood and his colleagues identified the level of stimulation that leads to optimal anti-cancer performance. They found that preventing T-cell exhaustion requires precise stimulation. The study also revealed that how tightly a parental T cell binds to a cancer protein determines if its daughter cells will be anti-cancer effectors or exhausted. If binding strength is not just right, the progenitor T cells develop into exhausted cells.

We showed Asxl1 disruption endows T cells with superior long-term therapeutic potential, which could be a promising strategy for the design of future T cell–based immunotherapies.
Caitlin Zebley, MD, PhD Department of Bone Marrow Transplantation & Cellular Therapy

exhausted state will allow us to develop engineering approaches that improve the longevity of T cell–based immunotherapies for solid and liquid tumors.”
“We wanted to know how signal strength contributed to either the maintenance or the progression of T cells to a terminally exhausted state,” said Youngblood. “Understanding what controls the transition between progenitor to the dysfunctional
Checkpoints are signals that tell T cells how to react to diseased cells or pathogens. Tumors can hijack these checkpoints to turn off the immune system. One type of immunotherapy, immune checkpoint inhibitors, blocks tumors’ ability to suppress T-cell function, thereby helping the immune system find and kill cancer cells.
Although the approach has shown remarkable success, it does not

work for all patients. To understand why, Zebley and Youngblood collaborated with colleagues at the Van Andel Institute. The researchers explored what is different about the T cells of patients who respond to immune checkpoint inhibitors.
“Looking at clinical trial data from myelodysplastic syndrome patients treated with checkpoint inhibitors, we saw that while most didn’t respond well, a small subset had long-term survival,” explained Zebley. “These patients had an ASXL1 mutation in the T cells, which led us to question whether the mutation could drive response to immune checkpoint inhibition.”


Our research efforts defining barriers limiting immunotherapy will guide our future efforts to engineer more effective treatments and grow our pediatric immuneoncology program.
Benjamin Youngblood, PhD Department of Immunology
In a paper published in Science, the researchers reported that intentional Asxl1 disruption in murine T cells improves tumor control during immune checkpoint inhibition. The investigators also discovered that Asxl1 regulates the epigenetic checkpoint governing terminal T-cell differentiation into the exhausted state. Asxl1-depleted T cells resisted exhaustion for the animal’s lifespan and controlled a range of tumors, compared to T cells with Asxl1 intact, which become exhausted and control only a limited type of tumors.
“We showed Asxl1 disruption endows T cells with superior longterm therapeutic potential, which
could be a promising strategy for the design of future T cell–based immunotherapies,” Zebley said.

Breakthroughs in understanding fundamental T-cell biology pave the way for more precise and effective immunotherapies. “Support for fundamental science is one of the many things that makes St. Jude special,” explained Youngblood. “Our research efforts defining barriers limiting immunotherapy will guide our future efforts to engineer more effective treatments and grow our pediatric immune-oncology program.”
An example of how fundamental insights lead to tangible improvements is findings from a phase 2 clinical trial published in the Journal of Hematology & Oncology. The study, led by Brandon Triplett, MD, and Swati Naik, MBBS, both of the Department of Bone Marrow Transplantation & Cellular Therapy, shows promise in enhancing the donor immune attack on the host’s leukemic cells, called the graft-versus-leukemia effect, without causing excessive dangerous graft-versus-host disease (GVHD).
Patients with leukemia or other blood cancers who do not respond to chemotherapy often need hematopoietic cell transplantation, also called bone marrow or stem cell transplantation, to treat their cancer. Although potentially lifesaving, transplantation carries substantial risks.
from the donor’s bone marrow identify the patient’s tissues as foreign and launch a harmful immune attack. The researchers minimized this complication by selectively removing naïve T cells, which are defined as T cells that have not yet encountered the specific protein they were designed to recognize and which generally drive GVHD. By targeting only naïve T cells, the researchers could leave mature memory T cells behind. These memory T cells harness the beneficial graftversus-leukemia effect and can protect patients against infections while minimizing the risk of GVHD.

In this study, even without total body irradiation, the leukemia-free survival rates were comparable, if not better, than those seen in studies that used it.
Swati Naik, MBBS Department of Bone Marrow Transplantation & Cellular Therapy
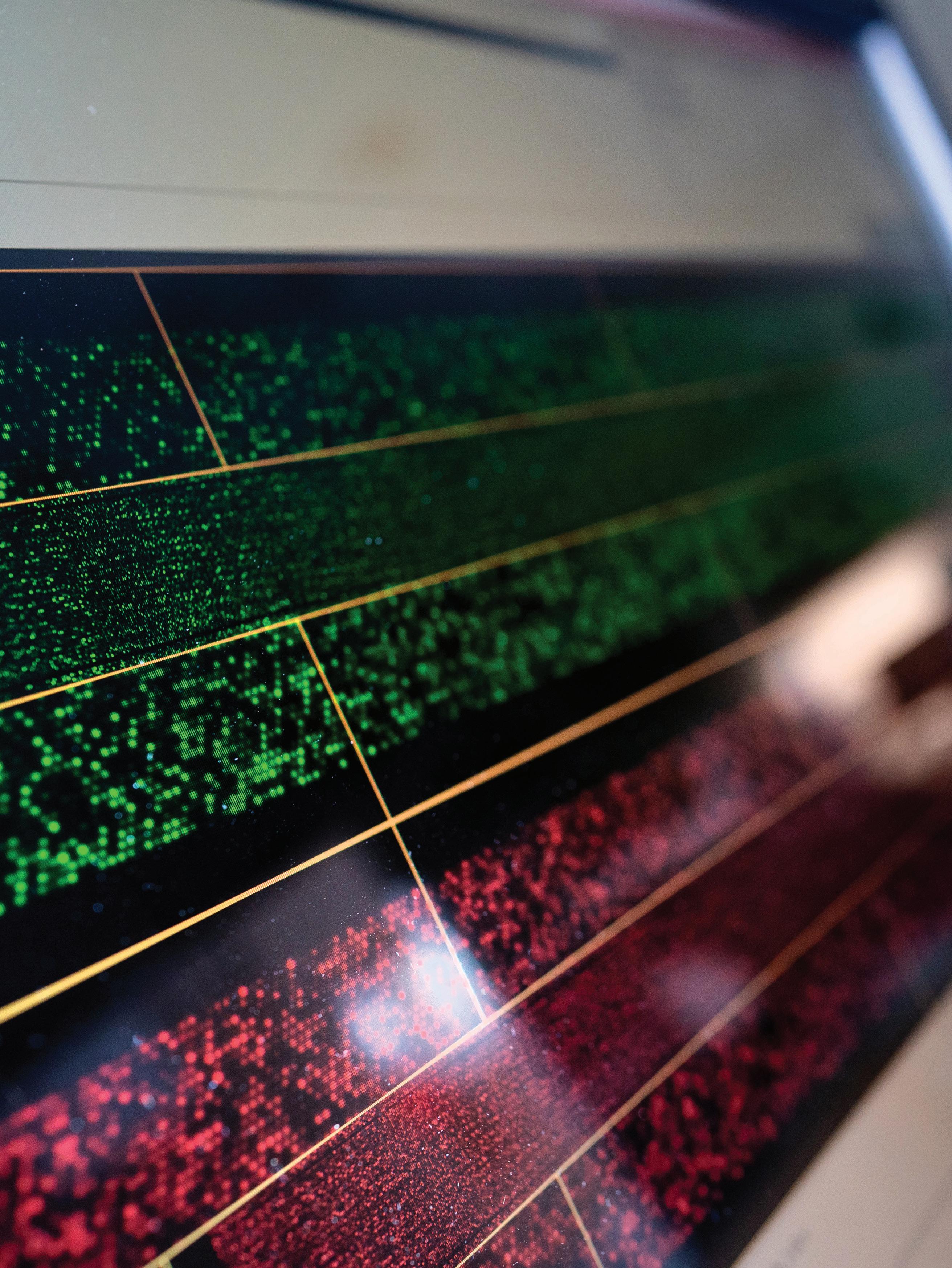
A scientist analyzes fluorescent signals on a microarray to gain insights into molecular activity in ongoing research.


We’re designing [the immune system] to be as robust as possible against infections and leukemia while carefully minimizing the risk of graftversus-host disease.
Brandon Triplett, MD
Department of
Bone Marrow Transplantation & Cellular Therapy
“In bone marrow transplantation, total body irradiation is typically considered essential to achieve favorable outcomes,” explained Naik. “However, in this study, even without total body irradiation, the leukemia-free survival rates were comparable, if not better, than those seen in studies that used it.”
“The thing about transplantation is that you’re building a whole new immune system in the recipient from the donor cells,” added Triplett. “We’re designing it to be as robust as possible against infections and leukemia while carefully minimizing the risk of graft-versus-host disease.”
As scientists deepen their understanding of T-cell biology and immune system activity, breakthroughs advance the development of finetuned and effective therapies. By enhancing the power of T cells and other immune components, St. Jude researchers are laying the foundation to improve immunotherapy treatment for patients with even the most intractable cancers.


For four decades, the HIV and Translational Medicine Program at St. Jude has advanced treatment and prevention options for children and youths living with and striving to prevent HIV.
Yet from initial treatments, which required taking multiple pills several times a day, to one pill daily, to two intramuscular injections given once every two months, St. Jude has played a role in the progress that has transformed HIV from a life-threatening disease into a manageable chronic condition.
St. Jude has helped accelerate the U.S. Food and Drug Administration (FDA) and Canada Health approval timeline for the combined administration of the

long-acting injectable antiretrovirals cabotegravir and rilpivirine in adolescents (aged 12 to 18 years). The approach was tested through the phase 1/2 International Maternal Pediatric Adolescent AIDS Clinical Trials (IMPAACT) Network clinical trial co-led by Aditya Gaur, MD, Division of HIV and Translational Medicine director and Department of Infectious Diseases, and his colleague Carolyn BoltonMoore at the Centre for Infectious Disease Research in Zambia, Africa.
Results from the study, also referred to as the More Options for Children and Adolescents (MOCHA) study, were published in The Lancet HIV. The study, which involved participants from 15 centers across four countries, showed positive safety, acceptability, and tolerability of this two-drug injectable regimen in youths aged 12 to 17 years.
“There will always be a little bit of lag between when promising drugs or discoveries get approved for adults versus children and youths,” said Gaur. “But for this first all-injectable HIV

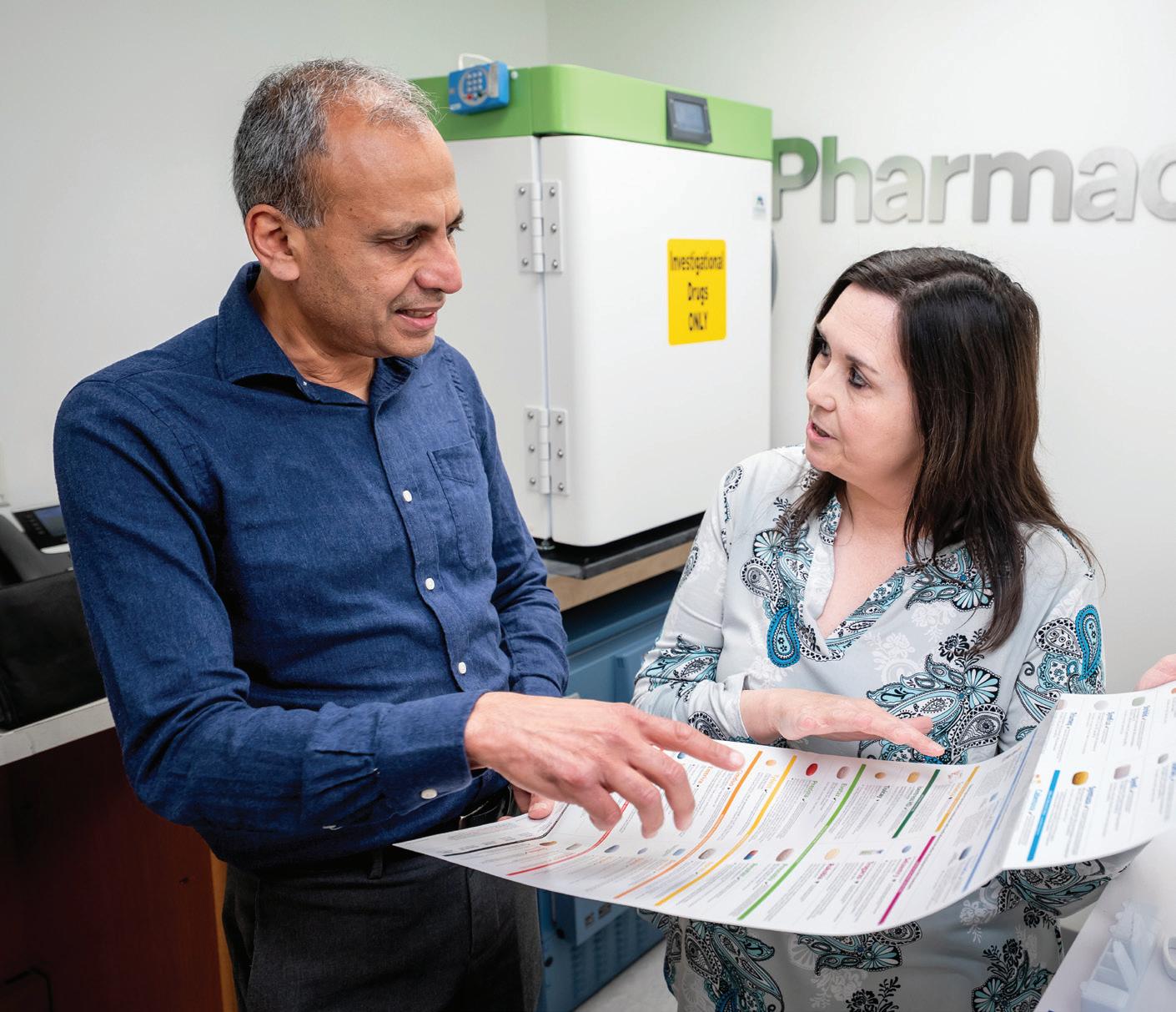

treatment regimen, approval for use for adolescents in the United States and Canada was relatively soon after the approval for adults, a credit to the IMPAACT 2017 study participants and the collaboration of the National Institutes of Health, ViiV Healthcare, and Janssen R&D, who sponsored the study.”
The approval brings a new treatment option to adolescents who may struggle with adhering to a one-pill-a-day regimen, the current standard of care.
“When we think of any chronic disease, be it HIV, diabetes, or high blood pressure, people struggle with taking medicine every day,” Gaur explained. “Additionally, when you have a condition stigmatized in society, where the act of taking a pill in the presence of someone else may be a reminder that you have HIV, one can see why adhering to a simple, potent, safe one-pill-a-day combination can become even harder.”
St. Jude also participated in a pharmaceutical company–led and sponsored phase 2/3 multicenter trial
to assess the safety of co-formulated bictegravir, emtricitabine, and tenofovir alafenamide administered in single-tablet form for 48 weeks in children aged 2 years or older living with virologically suppressed HIV in South Africa, Thailand, Uganda, or the United States.

We are taking steps to achieve the goal of ending the HIV epidemic [and are] fortunate to walk alongside patients, research participants, and their families as we work toward this future.
Aditya Gaur, MD Department of Infectious Diseases
Initial results published in The Lancet HIV — the first report to assess the safety and dose of a single-tablet option in young children — found the fixed-dose combination of the three medications to be efficacious and well tolerated with good adherence. The findings supported the FDA and European Medicines Agency approval of the low-dose, single-tablet co-formulation as a treatment for HIV in children aged at least 2 years and weighing 14 kg to less than 25 kg. The use of this new formulation was also added to the recommended-use guidelines issued by the U.S. Department of Health and Human Services.
Reflecting on the importance of advancing HIV treatment options to all age groups, Gaur stated that “the HIV Program at St. Jude is committed to providing the best multidisciplinary care and access to research independent of a person’s ability to afford or access care, and we are taking steps to achieve the goal of ending the HIV epidemic in collaboration with our community partners. We are fortunate to walk alongside patients, research participants, and their families as we work toward this future.”
Every year, the breadth and depth of the research enterprise at St. Jude expands. The Scientific Highlights capture a snapshot of the diversity of fields, departments, and researchers charting new discoveries at St. Jude. These high-impact publications provide a window into the scientific accomplishments of St. Jude investigators in 2024.

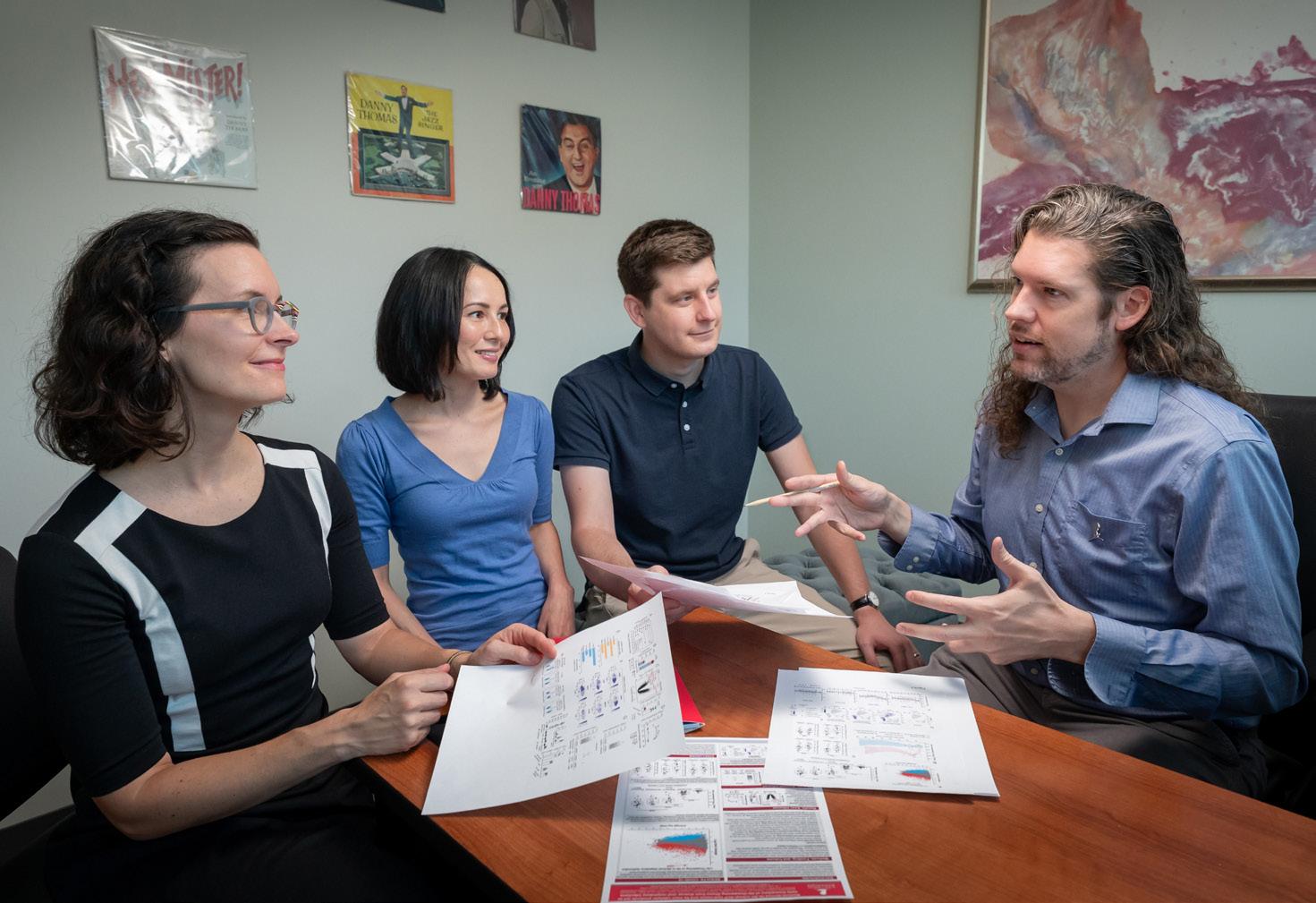
What drives infections to become severe, perhaps even fatal, in some individuals but not in others is an area of infectious disease research that has been difficult to study. Collaborative research between St. Jude, the Peter Doherty Institute for Infection and Immunity, Harvard University, and other institutions, published in Cell, has shed light on the problem, revealing that oleoyl-ACP-hydrolase (OLAH), an enzyme involved in fatty acid biosynthesis, is a driver of severe disease outcomes.
“It took years of working closely with basic scientists and clinicians from across the world, all studying different infections and diseases, for OLAH’s important role in the immune response to come to light,” said co-first and co-corresponding author Jeremy Chase Crawford, PhD, Department of Host-Microbe Interactions.
The lack of recognition for OLAH’s important role was due to difficulties in collecting unbiased datasets during severe disease. Because OLAH is rarely expressed, even in healthy tissue, scientists have long focused on panels of genes with presumed roles in disease. To overcome these barriers and better understand how OLAH works, the researchers assembled comprehensive datasets covering as many genes as possible from years of collaborative projects that examined multiple diseases.
Researchers turned their attention to OLAH when transcriptomic analysis of blood from hospitalized patients infected with avian A (H7N9) influenza first showed a link between the expression of OLAH — present early after hospital admission and throughout disease progression — and fatal disease.
This initial finding led Crawford to expand the datasets, examining the enzyme in different cohorts of individuals who experienced respiratory infections and in mouse models of disease.
“We generated transcriptomic datasets from several projects through years of studying distinct patient cohorts. It occurred to us to look at OLAH, and that’s how we started to see these amazing associations across different diseases,” explained Crawford, a founding member of the St. Jude Center for Infectious Diseases Research (CIDR).
While subsequent studies of patients hospitalized for seasonal influenza, SARS-CoV-2, respiratory syntactical virus, and multi-system inflammatory syndrome in children found high expression of OLAH, mouse models demonstrated that a lack of OLAH expression correlated with infections that became survivable. The explanation for why lies in how OLAH produces elevated levels of fatty acids, namely oleic acid. These findings support previous research that showed viral infections in cell lines become worse when oleic or palmitic acid levels increase.
The findings advance the understanding of respiratory viruses and have broad health implications. Not only could OLAH become an indicator of disease severity, but the knowledge that it is present shortly after symptom onset means it could be used as a biomarker to determine initial treatment responses.
“This is just the beginning of our exploration of OLAH,” Crawford said. “There is much more work to be done in infectious disease and other potential applications.”

Having and undergoing treatment for a brain tumor can impact a survivor long after concluding therapy, including reduced academic readiness. Scientists at St. Jude found that very young children treated for brain tumors were less prepared for school (measured by academic readiness scores) than their peers, emphasizing a need to intervene before they start to struggle in school.
In one of the first studies to examine academic readiness in infants and young children (less than 3 years old) after brain tumor treatment, the scientists observed an increasing gap between the patients treated for brain tumors and their same-age peers. The study, published in the Journal of the National Cancer Institute, followed a group of 70 patients who had developed brain tumors and
underwent treatment, assessing them six months after diagnosis and then annually for five years.
“Even in very young children, we found academic readiness was starting to lag behind healthy children their age,” said corresponding author Heather Conklin, PhD, Division of Neuropsychology chief and Department of Psychology & Biobehavioral Sciences member. “They were gradually falling behind their same-age peers in academic fundamentals, such as learning their letters, numbers, and colors.”
Previous research focused on schoolaged children also observed gaps in academic skills, but such gaps in younger children revealed an early and pervasive challenge. “Early academic readiness was predictive
of long-term reading and math outcomes,” said Conklin. “These children don’t catch up naturally.”
To address these concerns, the team proposed early intervention before a child enters elementary school. “We now know that we don’t need to wait until patients are struggling with math and reading; we can intervene earlier,” said Conklin. “We showed that the variability we’re seeing early on predicts long-term academic skills, which highly suggests earlier interventions will be beneficial and make a real difference.”
However, the researchers recognized that it was not enough to implement early interventions without first understanding what increased young learner’s vulnerability to or protected against the academic readiness gap. They examined myriad potential factors involved, such as treatment type and demographics, and found one standout determinant.
“The only clinical or demographic factor we found that predicted academic readiness was socioeconomic status,” explained Conklin. “Being from a family of higher socioeconomic status had a protective effect on children’s academic readiness.”
The finding that higher socioeconomic status is partially protective suggests that investing in resources to replace lost early enrichment experiences can mitigate the readiness gap. By increasing access to those opportunities, more children could be protected.
“Our results suggest that families can make playtime meaningful,” Conklin said. “By making small changes in how they interact with their child, with the support of their medical team and receiving appropriate resources, they can make a difference in their child’s cognitive and academic outcomes.”

Mycobacterium abscessus (Mab) infections are becoming increasingly common in health care settings. Such infections can be hazardous for patients with compromised lung function, such as in cystic fibrosis, or who are immunologically compromised, such as in childhood cancer. These infections are treated with long courses of antibiotics and can result in poor outcomes. The emergence of Mab and other similar pathogens presents a growing and deeply concerning public health threat because there are few effective therapeutic options and a limited drug development pipeline.
When treating Mab, clinicians have a limited number of effective antimicrobials from which to choose. However, resistance has emerged to these drugs, limiting the available treatment options and leaving very few viable alternatives.
Furthermore, this naturally antibioticresistant pathogen is becoming more prevalent, highlighting the urgent need for novel therapeutics.
“We chemists are in a race against the pathogens. We make stronger antibiotics, and the pathogens become more resistant,” said Richard Lee, PhD, Department of Chemical Biology & Therapeutics.
Scientists at St. Jude are tackling Mab antibiotic resistance, designing new versions of the drug spectinomycin that overcome resistance mechanisms. In the study, published in Proceedings of the National Academy of Science, the researchers modified the naturally occurring antibiotic spectinomycin to create analogs, comparable but structurally distinct N-ethylene linked aminomethyl spectinomycins (eAmSPCs).
These synthetically created eAmSPCs are up to 64 times more potent against Mab than standard spectinomycin.
The scientists unraveled the mechanism of action by which eAmSPCs are more effective: They circumvent efflux. Efflux is the process that cells use to eliminate a drug — imagine pumping water out of a flooded basement— and is a significant mechanism by which cells become resistant to therapy. Cells use specific drug efflux pumps to expel drugs.
The N-ethylene linkage structure of the eAmSPCs plays a critical role in how the compounds avoid efflux, suggesting that longer linkages modify how the compound is pumped out of the cell. This ultimately shifts the balance toward higher concentrations of eAmSPC within the cell and thus enhances antimicrobial efficacy.
“By re-engineering the molecule through structure-based drug design, we and our collaborators have adapted the antibiotic to increase its activity,” Lee added.
The researchers also found that eAmSPCs work well with various antibiotic classes used to treat Mab and retain their activity against other mycobacterial strains. Collectively, this work demonstrates that eAmSPCs should be further studied and developed. Once issues of tolerability and safety are addressed, these compounds could become next-generation therapeutics.
“Over the past two decades, we’ve seen a massive increase in infections caused by nontuberculous mycobacteria like Mab,” said co-first author Gregory Phelps, PharmD, Graduate School of Biomedical Sciences. “If we can boost the drug pipeline against these hardto-treat bacteria, we can potentially make a difference for patients like the ones we have here at St. Jude who are increasingly faced with limited or no therapeutic options.”
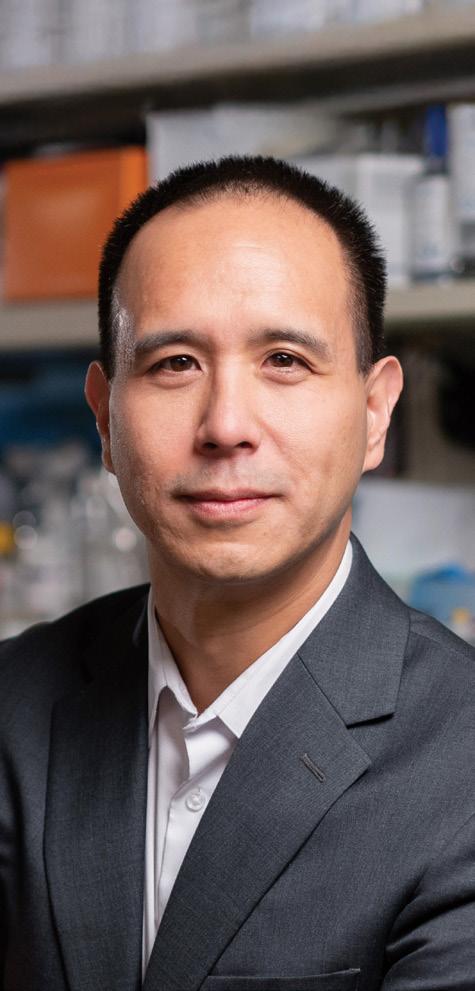


Treatments for sickle cell disease, a genetic blood disorder associated with chronic anemia, severe pain crises, progressive multiorgan damage, and early mortality, have limitations because currently approved drugs, such as hydroxyurea, are only partially effective. Allogenic bone marrow transplantation is potentially curative but is associated with immune toxicities, such as graftversus-host disease and graft rejection. Matched donors for the procedure are also limited; less than 20% of patients with sickle cell disease find a match. Genome editing of patients’ stem cells could circumvent these challenges.
Published in Molecular Therapy, St. Jude scientists detailed the safety and efficacy of a gene editing approach that induces fetal hemoglobin. Hemoglobin is a red blood cell protein that carries oxygen throughout the body.
Sickle cell disease affects this protein, but fetal hemoglobin (present before birth) offers an alternative. By editing blood stem cells to express fetal hemoglobin, researchers may be able to treat sickle cell disease.
The approach, initially developed in the lab of co-corresponding author Mitchell Weiss, MD, PhD, Department of Hematology chair, uses a CRISPRCas9 genome editor programmed to make targeted DNA double-stranded breaks. The researchers used this editor to interfere with the target of a repressor protein called BCL11A, which ceases fetal hemoglobin expression in adult blood cells.
“We compared different possible editing targets and identified a lead target that was not only highly effective at inducing fetal hemoglobin but also highly specific,”
said co-corresponding author Shengdar Tsai, PhD, Department of Hematology. “To understand where Cas9 was acting in the edited cells’ genome, we used an approach my lab developed called CHANGE-seq; it selectively sequences DNA modified by genome editors.”
The lab of co-corresponding author Jonathan Yen, PhD, Department of Hematology, optimized the cellediting process at the clinical scale by collaborating with the Children’s GMP, LLC. They demonstrated they could edit cells at the quantity and quality required to treat patients in a clinical trial.
Preclinical studies showed that Cas9 editing at the targeted binding site induced fetal hemoglobin to levels predicted to be therapeutically effective with no detectable offtarget effects in the edited human hematopoietic stem cells. These results prompted the team to open the first genome editing clinical trial at St. Jude, called St. Jude Autologous Genome Edited Stem Cells (SAGES-1).
In addition to providing the foundation for future St. Jude studies, this work supplies a blueprint for other researchers. “We described the complete story of developing a genome editing strategy to treat sickle cell disease from preclinical studies to scaling up the editing process to clinical readiness and understanding of safety and potential toxicities,” said Tsai. “By publishing these studies, we hope to help other groups by providing an example of studies required to clear an investigational new drug application.”
The team anticipates this study will be the first of a series of advances in genome editing medicines at St. Jude. They hope to catalyze similar efforts both at St. Jude and elsewhere.

More than 80% of children who receive cancer treatment in countries with significant resources survive their illness. At diagnosis, the provision of cure-directed therapy is considered the norm for most of these children. However, the global burden of pediatric cancer is not distributed equitably. Approximately 90% of children diagnosed with cancer live in resourcelimited countries. Children presenting with advanced cancer are particularly vulnerable, as many face barriers to accessing the health care they need, resulting in adverse outcomes.
In a study published in Supportive Care in Cancer, St. Jude researchers investigated approaches to clinical decision-making for children presenting with advanced cancer in resource-limited countries. “We identified a research gap. We had a poor understanding of how physicians
approach decision-making for these children and recognized the importance of using qualitative research methods to explore this topic. This was a key first step toward designing interventions to improve patient outcomes and clinician workflows,” said first author Marta Salek, MD, MPH, Department of Global Pediatric Medicine.
Eleven participants from the St. Jude Global Alliance community, representing each World Health Organization–designated region, were invited to participate in focus groups. As experts in pediatric oncology, the group offered unique insights into their treatment decision-making processes within their local contexts.
“We asked participants to brainstorm factors that influence their treatment decision-making for a child presenting with advanced cancer at diagnosis,
which were then reviewed and debated,” Salek explained. “This was followed by discussions regarding whether physicians considered treatment with noncurative intent for these children at diagnosis, including when it could or could not be appropriate. We also asked them to reflect on local definitions of ‘poorprognosis cancer’ at diagnosis.”
The focus groups identified many multi-level health system factors involved in decision-making, including family preferences, available resources, family health care access, local culture, and national payment structures for delivering childhood cancer therapy. These results illustrated that participants experienced difficulties with complex decision-making at diagnosis. Furthermore, the data suggested these challenges may be magnified by diverse factors underrepresented in existing decisionmaking frameworks or childhood cancer treatment guidelines. Inconsistent definitions of a “poor prognosis” amplified these difficulties.
Salek and her team plan to explore treatment decision-making in greater depth by leveraging diverse perspectives from patients, families, and multidisciplinary clinicians. With this qualitative research, they aim to develop pragmatic strategies to support treatment decision-making in resource-limited settings adaptable to local contexts and empower physicians to offer the best available treatment options. In instances when curative-intent treatment at diagnosis is not possible, such insights could highlight areas within health systems that need strengthening.
Improving outcomes for children diagnosed with cancer regardless of where they live is at the heart of this work. “We want to ensure that, in the future, all children presenting with cancer can be offered treatment with curative intent safely,” said Salek.

Innate immune sensors are an integral part of the immune system, acting as a first line of defense to protect against disease and infection. Activated sensors trigger a cascade of events that can be beneficial and provide host defense but can also cause inflammation and disease.
As part of their response, innate immune sensors assemble complexes that integrate signals and respond to threats. One such complex is the PANoptosome, which drives a prominent inflammatory cell death type called PANoptosis. However, how specific innate immune sensors work and what triggers them to act have remained mysterious for decades.
Chipping away at the mystery, scientists at St. Jude, led by ThirumalaDevi Kanneganti, PhD, Center of Excellence for Innate Immunity and Inflammation director and Department of Immunology vice chair, published research in Cell showing how a member of the nucleotide-binding
oligomerization domain-like receptor (NLR) family, NLRC5, plays a previously unidentified role driving PANoptosis.
To understand its role in disease and elucidate the triggers of NLRC5, the scientists screened combinations of immune-system threats, including pathogen-associated molecular patterns (PAMPs), damage-associated molecular patterns (DAMPs), and cytokines (immune signaling molecules) that can be released by or mimic an infection, injury, or illness. This comprehensive approach is built on extensive research that has shown the multifaceted nature of innate immunity; this contrasts with the conventional single ligand-receptor model of study, which has historically oversimplified the complex interplay of innate immune signaling.
Through this process, the researchers examined heme, a hemoglobin component that binds oxygen to carry the molecule throughout the body. However, “free heme”
can also be released when red blood cells rupture, leading to inflammation and organ damage.
“We identified that the combination of heme plus PAMPs or cytokines specifically induces NLRC5-dependent PANoptosis,” said co-first author Balamurugan Sundaram, PhD, Department of Immunology. “This showed for the first time that NLRC5 is central in responding to hemolysis, which can occur during infections, inflammatory diseases, and cancers.”
The results led the team to investigate how NLRC5 is regulated. They found that depletion of a key molecule for cellular energy production — nicotinamide adenine dinucleotide (NAD) — signals to the immune system that there is a threat, driving NLRC5 protein expression.
“Supplementing with the NAD precursor, nicotinamide, blocked NLRC5-mediated PANoptosis,” said co-first author Nagakannan Pandian, PhD, Department of Immunology. “Therapeutically, nicotinamide has been used as a nutrient supplement, and our findings suggest it could help treat inflammatory diseases.”
With this knowledge, the team searched for how NLRC5 could be a target in therapeutic approaches to mitigate PANoptosis associated with diseases. They found that deleting Nlrc5 protected against inflammatory cell death and prevented disease pathology in hemolytic and inflammatory disease models, making NLRC5 an exciting therapeutic prospect.
“The concepts of PANoptosomes and PANoptosis are fundamental to our understanding of how innate immune sensing works and can be translated to numerous diseases and conditions,” said Kanneganti. “For conditions with no targeted therapies — inflammatory disorders, infectious disease, cancers, aging — targeting PANoptosis could be an option.”

To effectively treat a disease or disorder, doctors must first know the root cause. Such is the case for developmental and epileptic encephalopathies (DEEs), whose root causes can be complex and heterogeneous. DEEs affect 1 in 590 children in the United States each year and involve more than 825 genes.
When a child is diagnosed with DEE, linking the encephalopathy to a specific gene can help facilitate appropriate treatment or symptom control. However, current testing methods can clinically identify the root cause, or etiology, of only 50% of individuals’ DEEs. Unfortunately, the remaining half of patients’ encephalopathy remains unexplained.
Addressing the genetic root causes for DEEs has been a long-term goal for Heather Mefford, MD, PhD, Pediatric Translational Neuroscience Initiative
and Department of Cell & Molecular Biology. Mefford was instrumental in raising the number of diagnosable cases to 50%, up from approximately 5% just a decade ago.
Today, 80% of identifiable DEEs can be explained by 27 genes. To tackle the remaining unsolved cases, the numerous rare occurrences of these disorders must be identified, a challenge that Mefford and her team embrace. The team is exploring epigenetics, the changes in gene expression, as a potential solution. One such epigenetic change involves a process called DNA methylation. This process regulates gene expression by adding a methyl group to a gene’s promoter region, which prevents transcription factors from binding to the DNA, ultimately leading to gene silencing or reduced expression.
In a study published in Nature Communications, Mefford and her team demonstrated that DNA methylation patterns can help identify the cause of DEEs. Their findings highlight how specific gene and genome-wide methylation “epi-signatures” can help pinpoint genes responsible for the disorder.
“For some genetic disorders, everyone with a mutation in the same gene has a methylation profile across their genome that puts them in a category with all the others with the same genetic disorder,” said Mefford. This methylation landscape is called an “epi-signature” and is akin to a DEE fingerprint.
While epi-signatures allowed the researchers to broadly identify DEEcausing variants, taking a closer look at the individual methylation instances, referred to as rare differential methylation analyses, revealed further insights. “The underlying cause of the disease manifests in an epi-signature that can serve as a marker for that gene,” explained cofirst author and Graduate School of Biomedical Sciences student Christy LaFlamme. “With rare methylation events, their analysis can point directly to the cause of the disease.”
Exploring these rare methylation events across the genome using longread DNA sequencing pointed the researchers toward DNA regions that are not commonly assessed, offering an answer to the cause of some cases. This allowed the researchers to identify the causative and candidate etiologies of DEEs in 2% of previously unidentified cases. This research represents another significant step in identifying rare instances of DEEs and another tool to aid in diagnosing children with DEEs.



The population of pediatric cancer survivors is growing — around 85% of childhood cancer patients survive to five years post-diagnosis in the U.S., with most living decades beyond that. But with more survivors comes more people at risk of adverse health effects caused by cancer or their cancer treatment.
Researchers are studying childhood cancer survivors to learn how to tailor improved therapies, provide screening, and support patients later in life. However, this research hinges on access and the ability to analyze collected comprehensive survivorship data systematically. In a boon to such studies, scientists at St. Jude created the St. Jude Survivorship Portal, the first data portal of its kind dedicated to sharing, analyzing, and visualizing cancer survivorship data — all open
access and free to use as part of the St. Jude Cloud ecosystem.
Poised to offer significant contributions to survivorship research thanks to its two large survivorship cohorts, the Childhood Cancer Survivor Study (CCSS) and the St. Jude Lifetime Cohort (St. Jude LIFE), St. Jude already possessed a rich data source for investigators to mine new survivorship insights. The creation of the survivorship portal serves as a tool that leverages this wealth of data and offers a resource that has the potential to propel the field of survivorship research forward.
“We aren’t just sharing data,” said cocorresponding author Yutaka Yasui, PhD, Department of Epidemiology & Cancer Control. “We are facilitating the analysis and visualization of data and making it free to anyone —
that’s a tremendous resource for the cancer survivorship community.”
Published in Cancer Discovery, scientists at St. Jude unveiled the big-data platform incorporating clinical and genomic information. The unprecedented research system integrates three sets of data: whole genomic sequencing, treatment exposure, and outcomes, in which there are 1,600 phenotypic variables and 400 million genetic variants from over 7,700 childhood cancer survivors.
Maintaining such an expansive data platform is a commitment the St. Jude team willingly assumes, ensuring access to a vast resource is sustained.
“Continued enhancement of the portal architecture is key to enabling on-the-fly analysis, which integrates data on treatment exposures, whole genome sequencing, and long-term outcomes,” said co-corresponding author Xin Zhou, PhD, Department of Computational Biology. “There are half a billion clinical data points in the portal and hundreds of terabytes of genetic data supported by dynamic and interactive visualization analysis.”
Among the various use cases that served to illustrate the discovery potential of the portal, the research team highlights their comparison of associated outcomes for two types of platinum chemotherapies, cisplatin and carboplatin, reaffirming that cisplatin is associated with greater auditory toxicity than carboplatin.
“By enabling the study of the mechanisms underlying toxicity, the portal can inform investigators how to prioritize drugs for treatment,” said cocorresponding author Jinghui Zhang, PhD, Department of Computational Biology. “Investigators can come to the portal with different interests, genetics, drug usage and exposure, or survivorship — these perspectives can all be explored in the portal.”

Within cells lie membraneless hubs of concentrated proteins and nucleic acids called biomolecular condensates. Like liquid droplets, these condensates are centers of reaction for the spatial organization of biomolecules. Beyond cellular organization, these condensates play roles in disease, including neurodegenerative diseases such as amyotrophic lateral sclerosis (ALS) and frontotemporal dementia.
Understanding how these reaction hubs function and change over time is key to better understanding the mechanisms that drive disease. Studies of biomolecular condensates have uncovered layers of complexity, including their changing material properties, known as “aging.” In these aging processes, the condensates change from having viscoelasticliquid properties into a viscoelastic solid over time. To better understand
these changing material properties, St. Jude scientists, in collaboration with the State University of New York at Buffalo and Washington University at St. Louis, studied the interaction networks within condensates to better understand the rules associated with their unique material properties. The study was published in Nature Physics
“Condensates have often been described as liquid-like, but their material properties can vary quite a bit,” says co-corresponding author Tanja Mittag, PhD, Department of Structural Biology. “That depends on the sequences of the proteins within them and the lifetime of the interactions being formed.”
Mittag leads an effort to understand how the amino acid sequence of proteins that form these biomolecular condensates determine these material
properties through the St. Jude Research Collaborative on the Biology and Biophysics of RNP Granules. Previous work published in Science established a “stickers-and-spacers” model for predicting phase separation behavior in proteins. “Stickers” are amino acids that connect with other stickers, while “spacers” are amino acids necessary for the arrangement of stickers and interactions with water.
Building upon this “sticker-and-spacers” model, the researchers found that the material behavior of biomolecular condensates depends on the strength of these sticker–sticker interactions.
“What we call ‘sticker’ amino acids make pairwise interactions that form a network fluid,” Mittag said. “Now, we understand that these pairwise contacts that are forming — how stable they are and what their lifetime is — determine the condensates’ viscoelastic properties, and we can push their behavior toward elastic properties if we make stronger interactions. We now understand the protein sequence encodes this.”
The team’s work further explored how condensates age, identifying a new path in aging by building on the “stickers-and-spacers” model.
“If we exchanged spacer amino acids for ones that like to interact more with water, we could get condensates to age into a viscoelastic solid,” says co-first author Wade Borcherds, PhD, Department of Structural Biology. “This is like putty becoming a rubber ball. They can both bounce, but one is solid, and one is not.”
Now that the scientists understand how the aging process is encoded in the protein sequence, they can test whether this is the basis for certain neurodegenerative diseases’ development.

design to enhance CAR T–cell therapy for leukemia in a study published in Cell Reports Medicine
Chimeric antigen receptor (CAR) T–cell therapy redirects a patient’s own immune cells to target a cancerspecific protein. Optimizing CAR T–cell therapy for different pediatric cancers requires an improved understanding of T–cell biology and immune processes. One challenge in the field has been identifying tumor-specific targets that are both uniformly expressed and not essential in healthy tissues. St. Jude scientists are addressing this issue by designing and developing CARs with more sophisticated targeting abilities. The work provides a foundational understanding that may guide future CAR T–cell design across cancer types.
The study, published in Cell Reports Medicine, showed how a computational approach incorporating AlphaFold2,
an AI-powered protein folding prediction tool, could shed light on how structure impacts CAR T–cell function in acute myeloid leukemia (AML). Combining this improved CAR design with computational prediction could potentially expand treatment options for AML and other malignancies traditionally resistant to current therapies.
“One of the most exciting aspects of the approach is that although we focused on leukemia, it can be widely extrapolated to other tumors such as solid and brain tumors,” said senior corresponding author Paulina Velasquez, MD, Department of Bone Marrow Transplantation & Cellular Therapy.
The researchers created a unique single-molecule CAR, which includes the region of an antibody that binds a specific target (its antigen) and one short peptide that binds a separate target. These two binding domains are connected by a linker, enabling the CAR to target two different cancer-related proteins.
This approach overcomes inefficiencies in CAR T–cell therapy caused by the inability to target large antibody fragments. “Our approach added a small peptide, enabling our CAR to engage either target to prevent immune escape,” said first author Jaquelyn Zoine, PhD, Department of Bone Marrow Transplantation & Cellular Therapy.
The dual-targeted CARs outperformed single-targeted CARs in both in vitro and in vivo experiments, demonstrating their promise. However, the researchers struggled to determine the optimal linkers to use between the binding domains. The physical structure of the targeted molecule and its linker can interfere with target binding on the cancer cell, so identifying the most effective linker could further improve the therapy.
Using computational structure prediction and comparing structures with experimental results, the researchers found that shorter, more flexible linkers improve binding and efficacy. “A linker of sufficient flexibility and shorter length can scan a larger volume and is more likely to find the target proteins on the cancer cell,” said co-author M. Madan Babu, PhD, FRS, Chief Data Scientist and Senior Vice President for Data Science.
As one of the few groups in the world employing AI-based structure prediction tools for CAR T–cell design, the researchers hope their method will encourage others to improve CAR designs and enhance treatments for pediatric cancers.
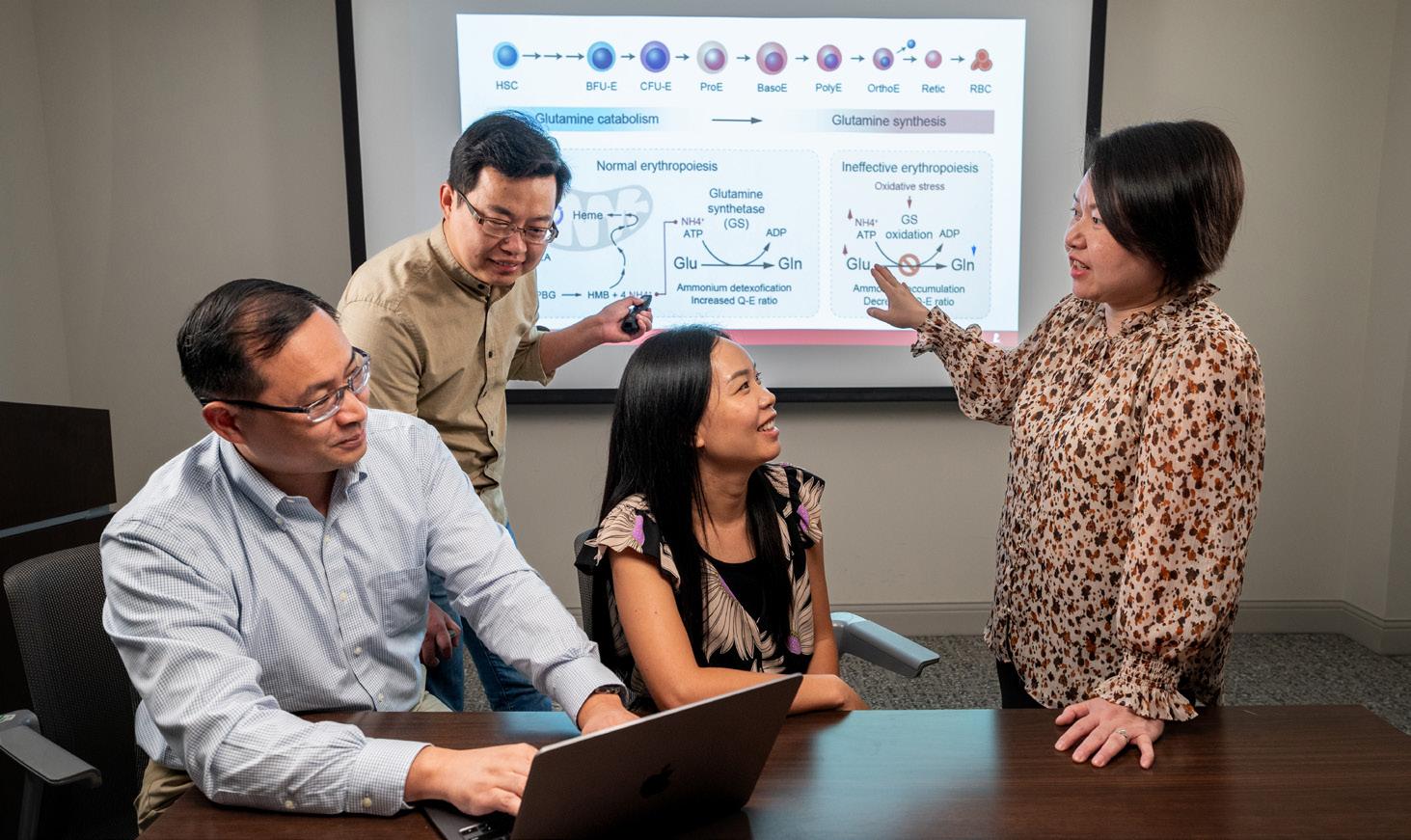
During mature red blood cell formation, a process called erythropoiesis, blood stem cells develop through many different stages. This fundamental biological process includes complex metabolic pathways, which are often dysregulated in blood disorders such as sickle cell disease and β-thalassemia. However, these metabolic pathways and how their dysfunction contributes to disease are not fully understood.
A collaborative research team led by Jian Xu, PhD, Department of Pathology and Center of Excellence for Leukemia Studies, and Min Ni, PhD, Department of Oncology, set out to understand the metabolic pathways regulating normal red blood cell maturation and how this might be altered in various disorders.
The scientists systematically profiled metabolic changes through each red blood cell maturation stage and identified a previously unrecognized role for the amino acid glutamine.
The work, published in Science, reveals modulating glutamine metabolism is a potential therapeutic route for common red blood cell disorders. It may also serve as a tool for evaluating therapeutic efficacy.
Early blood cell maturation processes break down glutamine as an energy source, but the researchers made a surprising finding about the amino acid’s metabolism in the later stages of development. “We found this process is completely reversed during later differentiation. The cells stop breaking down glutamine and begin synthesizing it by completely reversing the reaction,” Xu explained.
Heme is the main component of hemoglobin, the protein in red blood cells that carries oxygen. Red blood cell maturation depends on heme production, but ammonium (a heme production byproduct) can accumulate if not removed, causing oxidative stress.
The researchers found red blood cells begin producing glutamine synthetase to facilitate ammonium’s removal by combining glutamate with the ammonium to produce glutamine.
Through conditional inactivation of glutamine synthetase, the researchers identified a direct link between disruption of glutamine metabolism and red blood cell disorders, such as β-thalassemia. This link causes a metabolic phenotype resembling a glutamine synthetase deficiency, characterized by increased glutamate and ammonia levels and decreased glutamine levels. They identified glutamine synthetase oxidation as the cause of this metabolic phenotype in β-thalassemia and were able to treat the condition by restoring enzyme activity.
The link between glutamine synthase deficiency and other red blood cell disorders in which the enzyme is inactivated is further supported by a recent report describing a selective impairment of erythropoiesis in a human patient with inherited glutamine synthetase deficiency, an ultra-rare inborn error of metabolism.
The researchers carried their study further, investigating how the drug luspatercept, currently used to treat β-thalassemia, works. They found the drug likely acts to restore glutamine levels. Similarly, the study suggests that the mechanisms behind other red blood cell disorder treatments, such as L-glutamine supplementation to alleviate sickle cell disease symptoms, likely involve fixing defective glutamine metabolism.
Beyond its direct impact on treating red blood cell disorders, the findings suggest metabolic features, such as glutamine-to-glutamate ratios, can be used as biomarkers for these conditions, offering a means to diagnose, monitor disease progression and evaluate therapeutic efficacy.




Comprising five research programs and 10 shared resources, the Comprehensive Cancer Center is designed to foster interdisciplinary basic and translational research, clinical trials, and population science focused on childhood cancer and survivorship.
The National Cancer Institute (NCI) supports 72 Cancer Centers in the United States. The St. Jude Comprehensive Cancer Center, under the direction of Charles W.M. Roberts, MD, PhD, is the first and only NCI-designated Comprehensive Cancer Center solely focused on pediatric cancer.
CANCER BIOLOGY PROGRAM
co-led by: Douglas Green, PhD; Richard Kriwacki, PhD
The diverse nature of pediatric cancers, coupled with the complex molecular, genetic, and developmental contexts in which they form, necessitates a broad spectrum of discovery research to build a strong foundation for translational studies. This program aims to explore and understand the cell and molecular biology of cancer at a fundamental level. In working toward this goal, program members lead integrated and transdisciplinary efforts to define pathways related to cancer, identify genomic and epigenetic drivers of cancer, explore key cellular processes underlying cancer maintenance and progression, understand the cancer immune microenvironment, and facilitate the translation of discoveries.
CANCER CONTROL & SURVIVORSHIP PROGRAM
co-led by: Gregory Armstrong, MD, MSC; Kristen Ness, PT, PhD, FAPTA
As treatments for childhood cancers improve, the number of long-term survivors of childhood cancer increases.
This multidisciplinary program aims to conduct innovative clinical, genetic, and observational research and translate the findings into effective strategies to avert or mitigate treatment-related complications and improve the quality of life of childhood cancer survivors. Leading two of the world’s largest pediatric survivorship research studies, the St. Jude Lifetime Cohort Study and the Childhood Cancer Survivor Study, program members have influenced the design of contemporary pediatric cancer treatment strategies and provided critical data to guide health surveillance and health-preserving interventions for long-term survivors.
DEVELOPMENTAL BIOLOGY & SOLID TUMOR PROGRAM
co-led by: Michael Dyer, PhD; Alberto Pappo, MD
Some of the most devastating and poorly understood cancers that affect children and adolescents arise in the peripheral nervous system, muscles, and bones. This program aims to improve the survival and quality of life of children with solid tumors by integrating basic and clinical research. Clonal selection
contributes to disease recurrence, so this program is targeting rare tumor cell populations that survive treatment via three key areas: precision medicine, cancer immunotherapy, and translational research. Research extends from basic mechanistic development studies to therapeutic studies in preclinical models, ultimately translating these discoveries to the clinic and altering the standard of care.
co-led by: Charles Mullighan, MBBS(Hons), MSc, MD; Ching-Hon Pui, MD
The program’s overall goal is to improve cure rates for hematological malignancies while minimizing therapy-related toxicity. This established, highly interactive, transdisciplinary program has a long track record of significant discoveries in cancer biology. Translation of these findings into new diagnostic and treatment approaches has changed the standard of care for children with hematological malignancies. Program members have pioneered efforts to transform childhood acute lymphoblastic leukemia (ALL) into a curable condition and defined many subtypes of ALL and acute myeloid leukemia with profound practicechanging implications now incorporated into the International Consensus and World Health Organization classifications of ALL, ultimately driving global advances in cancer research.
NEUROBIOLOGY & BRAIN TUMOR PROGRAM
co-led by: Suzanne Baker, PhD; Giles Robinson, MD
Brain tumors are the leading cause of cancer-related death in children. The goal of the Neurobiology &
Brain Tumor Program is to improve the survival and morbidity of children with brain tumors by developing the most effective, least toxic therapies through a better understanding of disease pathogenesis and normal brain development. Program members have illuminated mechanisms of oncogenesis and developmental origins of pediatric brain tumors, altered diagnostic practice worldwide by identifying refined molecular subgroups that are now incorporated into the new World Health Organization tumor classification guidelines, developed innovative clinical trials with risk-stratified design or immunotherapy approaches, and identified mitigating approaches to neurocognitive and long-term effects of therapy.










Charles W.M. Roberts, MD, PhD Director
Charles Mullighan, MBBS(Hons), MSc, MD Senior Deputy Director of Strategic Initiatives
Suzanne Baker, PhD Deputy Director of Strategic Initiatives
Hongbo Chi, PhD Associate Director, Basic Research
Heather Brandt, PhD Co-Associate Director, Outreach
Elizabeth Fox, MD, MS Associate Director, Clinical Research
Melissa Hudson, MD Associate Director, Population Sciences
Julie Park, MD
Associate Director, Translational Research
Shondra Pruett-Miller, PhD Associate Director, Shared Resources
Carlos Rodriguez-Galindo, MD Co-Associate Director, Outreach
Shared resources include: Bioinformatics and Biotechnology, Biostatistics, Cell and Tissue Imaging, Center for Advanced Genome Engineering, Center for Spatial Omics, Center for Translational Pharmacology, Flow Cytometry and Cell Sorting, Genetically Engineered Mouse Models, and Viral Vector Technology



Carolyn Russo, MD Associate Director
Dana Wallace, MS
Associate Director, Administration
Gerard Zambetti, PhD
Associate Director, Education & Training


Providing pediatric patients with cancer or blood diseases equal access to care, regardless of their geographic location, is a central goal of the Affiliate Program. The affiliate clinics support participant recruitment for clinical trials and the geographic extension of St. Jude clinical care.
Carolyn Russo, MD, medical director of the Affiliate Program, led a task force with leaders from the Strategic Planning, Affiliate Program, Clinical Operations, and Legal Services teams to determine how the hospital’s eight affiliate clinics across the country could better meet the needs of patients residing in those areas.
As of November 1, 2024, the clinic in Huntsville dropped the “affiliate” name and is now a St. Jude clinic in Huntsville, the first St. Jude satellite clinic. The new arrangement provides a closer alignment with St. Jude in Memphis. The St. Jude clinic in Huntsville will be overseen by both Clinical Operations and the Affiliate Office in Memphis to provide more of the look and feel of a St. Jude clinic. The goal, as always, is to provide more St. Jude care close to home, and this new approach offers the flexibility and resources to meet the St. Jude mission. A few years in the making, we are excited to begin this new journey.
Baton Rouge, LA
Our Lady of the Lake Children’s Hospital – Our Lady of the Lake Regional Medical Center
Jeffrey Deyo, MD, PhD Medical Director
Kacie Sims, MD
Sakshi Bami, MD
Alexandria Broadnax, MD
Katherine Helo, NP
Jessica Templet, PA-C
Joseph Kent, PA
Charlotte, NC
Novant Health Hemby Children’s Hospital
Christine Bolen, MD Medical Director
Jessica Bell, MD
Jenny McDaniel, MD
Joanne McManaman, MD
Felipe Bautista, MD
Holly Edington, MD
Courtney Saine, NP
Jennifer Weisner, NP
Andria Kokoszka, NP
Courtney Carr, NP
Huntsville, AL
Huntsville Hospital for Women & Children – Huntsville Hospital
Marla Daves, MD Medical Director
Sana Mohiuddin, MD
Jamie Musick, MD
Heidi Simpson, NP
Megan Vann, NP
Emily Clawson, NP
Ameila Jantz, NP
Johnson City, TN
Niswonger Children’s Hospital – Ballad Health
East Tennessee State University
Marcela Popescu, MD
Medical Director
Myesa Emberesh, MD
Meghan Srinivas, MD
Angela Willocks, RN, MSN, CFNP
Lauren Wyatt, NP
Amy Shaw, NP
Peoria, IL
OSF HealthCare Children’s Hospital of Illinois
University of Illinois College of Medicine at Peoria
Brinda Mehta, MD
Medical Director
Prerna Kumar, MD
Mary Beth Ross, MD, PhD
Jennifer Light, MD
Maggie Nagel, MD
Kay Saving, MD
Beth Speckhart, NP
Sue Gaitros, NP
Diana Simmons, NP
Dana Stephens, NP
Shreveport, LA
Ochsner LSU Health – Shreveport
Ayo Olanrewaju, MD
Medical Director
Elizabeth Wadhwa, MD
Alejandra Rosales, MD
Diana Townsend, NP
Amanda Saunders, NP
Springfield, MO
Mercy Children’s Hospital – Springfield
Mercy Health System
Francisca Fasipe, MD
Medical Director
Batool El-Atoum, MD
Carolyn Sullivan, NP
Danielle Lee, NP





Carolyn Russo, MD Medical Director
Jennifer Morgan, MSN Nursing Director
Nica Graunke, MPH Clinical Operations Director
Linda Stout, MD Rotating Physician
Patti Pease, NP, APN, RN Advanced Practice Provider Lead
Tulsa, OK
The Children’s Hospital at Saint Francis
Ashraf Mohamed, MD Medical Director
Martina Hum, MD
Shilpa Shukla, MD
Jill Salo, MD
Sara Mednansky, MD
Cori Ryan, NP
Allison Taylor, NP

Cancer
develops in about 400,000 children worldwide annually, and 90% of those children live in resource-limited countries. Fewer than 30% have successful outcomes.
When St. Jude launched the St. Jude Global initiative in 2018, it was an effort to build on the institution’s decades of mentorship and collaboration with hospitals around the world, with the vision that every child who receives a diagnosis of cancer or another catastrophic disease has access to quality care and treatment.
In 2024, St. Jude Global continued solidifying its work with medical institutions and foundations around the world through seven regional and 15 transversal programs and a growing number of projects, research initiatives, and educational opportunities.
Among these efforts is the St. Jude Global Alliance, which connects and empowers institutions and foundations worldwide. Launched in December 2018, the Alliance is a global community working to advance care for children with cancer or other catastrophic diseases. It takes a multilevel approach to developing global, national, regional, and hospital-based initiatives centered on its member institutions. In 2024, the Alliance grew to 324 members, including medical institutions and foundations from more than 80 countries.
At the sixth annual Global Alliance Convening, which took place December 10–12, 2024, in Memphis, more than 240 Alliance members from 185 organizations representing 68 countries came together. More than 800 members attended hybrid plenary sessions. The St. Jude Global team co-designed the program with Alliance members to include 11 general sessions, 54 interactive breakout sessions, and 116 posters and exhibition items. The theme, “Global Voices Exchanging Knowledge,” encouraged and empowered attendees to connect through knowledge sharing, amplifying successes, and inspiring action to transform care for children everywhere.
In 2003, St. Jude began working with partner institutions around the globe to create fellowship training programs at those institutions to build capacity and improve access to care for children with cancer. This effort has grown to include the development of fellowship training programs across eight institutions in seven countries. To strategically fill the specialist gaps across regions, trainees are selected according to country- or facilitylevel needs, with a plan for employment to begin immediately after completing training. These fellowships are modeled after those at St. Jude and consist of two- or three-year training programs that physicians enter after completing a pediatric residency. Beginning with the academic year in July 2024, the St. Jude Global Academy became an official ACGME-I (Accreditation Council for Graduate Medical Education–International)–sponsoring institution. To date, 130 specialists have graduated from St. Jude Global collaborating programs.
The St. Jude Global Academy seminars are skill-setting, certificate-based short training programs that enroll about 300 individuals per year. These seminars provide structured learning experiences in key areas that are relevant globally and are offered either as hands-on experiences at St. Jude or through blended formats that are both online and in person. In 2024, St. Jude Global Academies focused on neuro-oncology, critical care, and palliative care. Across these seminars and other educational opportunities, the online platform Cure4Kids provides critical resources. In September 2024, the platform relaunched to provide even more educational resources in a streamlined and easy-to-use new design.
The Department of Global Pediatric Medicine, in collaboration with the St. Jude Children’s Research Hospital Graduate School of Biomedical Sciences, developed the Master of Science in Global Child Health degree program in 2019. The sixth class of 10 students began its two-year program of study in 2024.
Following graduation, the Global Scholars conduct projects that the Global Pediatric Medicine department funds for two years. More than 10 of these projects were launched in 2024, and 12 were approved.
St. Jude Global and the St. Jude Comprehensive Cancer Center continued their partnership on a phase 2 clinical trial titled “Entrectinib as a Single Agent in Upfront Therapy for Children <3 Years of Age with NTRK1/2/3 or ROS1-fused CNS Tumors” (GLOBOTRK) (NCT06528691).
The study was activated in 2024 and includes seven Alliance partner hospitals in five countries (Brazil, Egypt, India, Jordan, and Peru). An external clinical research organization was selected in 2024 to manage the study, and the St. Jude Institutional Review Board and the Clinical Trials Scientific Review Committee have approved the protocol, which is now active for accrual.
The SJCARES implementation platform continued to grow its suite of tools in 2024, including the Adapted Resource and Implementation Application (ARIA) Guide, which enables St. Jude Global to provide essential guidance to the clinicians who need it most. These childhood cancer management guidelines are made possible through the partnership between St. Jude Global and the International Society of Paediatric Oncology, along with ongoing global support from the Paediatric Radiation Oncology Society, the International Society of Paediatric Surgical Oncology, and Childhood Cancer International. The ARIA Guide can be applied across a range of geographic and resource-diverse settings and is freely available to health care providers worldwide through the ARIA Guide web portal. So far, 22 guidelines are available, and more than 50 are in progress.
The SJCARES Registry, PrOFILE, Global Packages, and Systems & Policies tools continued to expand during 2024. As part of these comprehensive efforts, the National Cancer Control Planning integrating Children, Adolescents, and
Young Adults, a policy science–driven workshop series delivered in four languages to help health ministries develop national cancer control plans that include childhood cancer, enrolled its third cohort of ministry-led teams, helping reach 39 countries.
The St. Jude Global Diagnostic Innovations Using Value-based Implementation Models to Increase Access (DIVIA) Project made great progress in 2024. In partnership with the Department of Pathology and the Center for Applied Bioinformatics, the project has established and executed feasibility-assessment endeavors at two Alliance sites: Tata Memorial Center in Kolkata, India, and Hospital do Amor Barretos in Barretos, Brazil. Each site has cleared regulatory, legal, and financial hurdles, and sequencing quality control work has been successfully completed toward generating the quality FASTQ files (i.e., text-based files that store raw DNA and RNA sequencing data and quality scores) needed for the successful classification of pediatric cancers.
Addressing disparities in access to and quality of care for children with catastrophic diseases requires a systemic approach that addresses the multilayered dimension, from micro to macro, with a focus on the empowerment of partners. In 2018 and again in 2022, the World Health Organization (WHO) designated St. Jude as the first and only WHO Collaborating Centre for Childhood Cancer. St. Jude supports this work across three areas: 1) Support the WHO in including childhood cancer in national cancer control plans through tools for prioritization, costing, and framework for monitoring and evaluation. 2) Support the
WHO in developing tools and platforms for innovation, including diffusion in childhood cancer management, research, and education. 3) Support the WHO in strengthening childhood cancer control through technical support, training materials, and stakeholder engagement.
In 2018, St. Jude worked with the WHO and global partners to launch the Global Initiative for Childhood Cancer (GICC), with the goal of reaching at least 60% survival for children with cancer and saving 1 million more children by 2030 while reducing suffering. St. Jude serves as a technical and implementation partner, providing subject matter expertise, supporting technical tools and packages, and facilitating workshops and projects with national and global stakeholders. Through 2024, 76 countries were engaged in GICC, including 44 that have a signed Memorandum from their Ministry of Health as a focus country.
In 2021, St. Jude and the WHO announced the creation of the Global Platform for Access to Childhood Cancer Medicines to provide an uninterrupted supply of quality-assured cancer medicines to lowresource countries. Co-designing with the first six pilot countries (Ecuador, Jordan, Mongolia, Nepal, Uzbekistan, and Zambia) took place throughout 2024, with a target of the first medicines to arrive in early 2025. This work included collaborative readiness assessments of supply chain and clinical capacity, as well as country governance to foster ownership opportunities. The Global Platform saw the largest joint tender in global oncology medicines conducted by UNICEF and the PAHO Strategic Fund. It included 69 essential medicines and formulations after two rounds of requests for proposals.


Doctorate of Philosophy in Biomedical Sciences (PhD-BMS) training young scientists to advance our understanding of the molecular basis of disease and therapy
Master of Science in Global Child Health (MS-GCH) developing a global community of agents of change and leaders dedicated to improving children’s health worldwide
Master of Science in Clinical Investigations (MS-Cl) training clinicians and medical professionals to perform clinical research and conduct clinical trials
In the fall of 2025, the Graduate School will launch its newest graduate program, a Master of Science in Applied Biomedical Data Sciences, which will train students to be effective and collaborative biomedical data scientists. Approximately 220 faculty members and staff at St. Jude are now formal Graduate School faculty members involved in teaching, mentoring, serving on committees, and continuing to enhance the school’s future. In 2024, 78 PhD-BMS students, 21 MS-GCH students, and 17 MS-Cl students were actively enrolled.
Drawing on the deep expertise of a leading biomedical research faculty focused on the eradication of catastrophic childhood diseases and state-of-the-art infrastructure and technological support available at St. Jude, the PhD-BMS Program has now graduated 24 doctoral awardees, who have begun to contribute to diverse fields, including professional and industry research, scientific policy, academic postdoctoral studies, scientific writing and communications, and faculty at St. Jude. The program is led by Associate Dean Wilson Clements, PhD, associate member in the Department of Hematology; Assistant Dean Cassandra VanDunk, PhD; and Program Specialist Alex Frawley, MS. In the fall of 2024, the PhD-BMS Program welcomed 16 new matriculants.
Led by Associate Dean Shaloo Puri, MBBS, DTCD, MPH, MPA; Assistant Dean Julie Laveglia, EDD;
and Program Specialist Whitney Horton, MPS, who joined the staff in 2024, the MS-GCH Program has a mission to provide transformative education, facilitate collaborative opportunities, build capacities, and cultivate a diverse community of agents of change with the overall aim of enhancing equity, access, and quality of health care for children globally. The program completed its fifth academic year in 2024 and admitted another cohort of 11 health care professionals. The Winter Intersession welcomed back 20 students who attended leadership, management, and communication workshops on campus. In May, the fourth cohort participated in the Commencement ceremony to receive their diplomas. During the summer, multiple cohorts (students and alumni) came to Memphis for two weeks to participate in Orientation, Summer Intersession, Professional Development, Convocation, and Commencement. The MS-GCH Program has 38 alumni living in more than 20 countries.
Co-led by Associate Deans Patricia Flynn, MD; and Victor Santana, MD; Assistant Dean Sally Utech, PhD; and Program Specialist Jimmi Lampley, MS, the MS-CI Program provides students with a transformative education that will generate a cadre of health care professionals who are adept at designing, conducting, and reporting clinical investigations that promote human health. The program creates a unique opportunity to understand these concepts in a pediatric and young adult research setting, leveraging the expertise of St. Jude faculty and staff in undertaking clinical research. The MS-CI Program graduated its second class of five students in 2024, all remaining active in clinical research and patient care. In the fall of 2024,
the program matriculated its third class of ten students, composed of postdoctoral fellows, St. Jude faculty, and research and medical staff members.
Renovation of the Graduate School space in the Marlo Thomas Center was completed in the spring of 2024, adding additional administrative offices and cubicles needed to accommodate the Graduate School’s growing staff. The Graduate School has leased new space for student study carrels in the Inspiration4 Advanced Research Center, doubling the previous study capacity. New student activity center space is also being leased on the plaza level of the Danny Thomas Research Tower.
Under the leadership of Steven Varga, PhD, Dean of the Graduate School of Biomedical Sciences, the school submitted its initial application for membership to the Southern Association of Colleges and Schools Commission on Colleges in February of 2024. This crucial step begins the accreditation process, which ensures a school maintains the highest educational standards, as judged by external evaluators.
Finally, none of these activities and accomplishments would have been possible without the support of our Board of Trustees. The Graduate School relies heavily on the advice and insight this group of dedicated volunteers provides.





Steven Bares, PhD, MBA (Chair) Former President and Executive Director Memphis Bioworks Foundation
William Troutt, PhD (Vice Chair) President Emeritus Rhodes College
James R. Downing, MD President & CEO
St. Jude Children’s Research Hospital
Gabriel Haddad, MD Chairman, Department of Pediatrics University of California San Diego
Sarah Larsen, PhD Vice Provost and Dean of the Graduate School Interim Dean, Graduate College of Social Work Professor of Chemistry University of Houston


Ryan Potts, PhD Vice President Head of the Induced Proximity Platform Amgen, Inc.
Carolyn Smith, PhD Dean, Graduate School of Biomedical Sciences Vice President, Education Affairs
William R. Brinkley BRASS Chair Baylor College of Medicine

J. Paul Taylor, MD, PhD Executive Vice President and Scientific Director
St. Jude Children’s Research Hospital




CHAIR
Motomi Mori, PhD, MBA1; Endowed Chair in Biostatistics
Design and analysis of early phase clinical trials, biomarker discovery and validation, risk prediction models
MEMBERS
Cheng Cheng, PhD1
Statistical methods in cancer biology, clinical & translational studies
Meenakshi Devidas, PhD, MBA1,2
Biostatistics, pediatric hematology and oncology
Guolian Kang, PhD1
Statistical genetics/genomics, modeling of complex data
Yimei Li, PhD1
Statistical analysis of complex imaging data, survival data analysis & clinical trial design
Arzu Onar-Thomas, PhD1
Phase 1/2 designs, survival analysis, Bayesian statistics
Stanley Pounds, PhD1
Statistical cancer multi-omics; statistical pharmacogenomics
Deokumar Srivastava, PhD1
Clinical trials, robust methods, survival analysis
Li Tang, PhD1
Prediction, validation, diagnostic testing, microbiome analysis
ASSOCIATE MEMBERS
Sedigheh Mirzaei, PhD1
Statistical methods for incomplete survival data, cancer survivorship
Haitao Pan, PhD1
Bayesian dose-finding clinical trials design, adaptive design for single-arm and randomized clinical trials, pediatric extrapolation
ASSISTANT MEMBERS
Cai Li, PhD1
Statistical learning and computing methods for neurodegeneration
Qian Li, PhD1
High-dimensional multiomics, longitudinal modeling, statistical learning
Qijun Li, PhD1
Novel statistical methods to address statistical issues that widely arise in observational studies
Subodh Selukar, PhD1
Design and sequential monitoring of clinical trials
Yiwang Zhou, PhD1
Statistical methods for precision-medicine studies
INSTRUCTOR
Zachary Wooten, PhD
Enhancing contouring quality assurance in radiation oncology by using AI and machine learning
CHAIR
Stephen Gottschalk, MD1; Endowed Chair in Bone Marrow Transplantation & Cellular Therapy Cancer immunotherapy, cellular therapy, hematopoietic cell transplantation
MEMBER
Brandon Triplett, MD1; Deputy Clinical Director Hematopoietic cell transplantation
ASSOCIATE MEMBERS
Giedre Krenciute, PhD1 Cellular therapy for brain tumors
Ewelina Mamcarz, MD3
Swati Naik, MBBS
Cellular therapy for hematologic malignancies, hematopoietic cell transplantation
Amr Qudeimat, MD Hematopoietic cell transplantation
Akshay Sharma, MBBS1
Gene therapy and transplantation for nonmalignant hematologic diseases
Ashok Srinivasan, MD3
Paulina Velasquez, MD1 Cellular therapy for hematologic malignancies
ASSISTANT MEMBERS
Senthil Bhoopalan, MBBS, PhD1 Gene therapy & genome editing
Christopher DeRenzo, MD, MBA1
Cellular therapy for solid tumors
Rebecca Epperly, MD
Cellular therapy for pediatric malignancies
Ali Suliman, MD, MSc Hematopoietic cell transplantation
Aimee Talleur, MD1
Cellular therapy for hematologic malignancies
Caitlin Zebley, MD, PhD
Cellular therapy and T-cell differentiation

CHAIR
J. Paul Taylor, MD, PhD1; Executive
Vice President, Scientific Director, Edward F. Barry Endowed Chair in Cell & Molecular Biology
Molecular genetics of neurological diseases
VICE-CHAIR
Peter McKinnon, PhD1; Endowed Chair in Pediatric Neurological Diseases
DNA-damage responses in the nervous system
MEMBERS
Mondira Kundu, MD, PhD1
Autophagy-related proteins in health & human disease
Heather Mefford, MD, PhD1
Genetics of pediatric neurological disease
Stacey Ogden, PhD1
Mechanisms of Hedgehog signal transduction
ASSOCIATE MEMBERS
Joseph Opferman, PhD1
Regulation of cell death & mitochondrial function
Jasmine Plummer, PhD1,2
Multi-omics examination of genetic risk as a factor of oncogenesis
Shondra Pruett-Miller, PhD1
Genome-editing technologies
ASSISTANT MEMBERS
Fernando Cruz Alsina, PhD1
Molecular and cellular mechanisms that drive neural differentiation and maturation during brain development
Chi-Lun Chang, PhD1
Dynamic regulation of interorganelle communication
Bryan Gibson, PhD1
Impact of phase transitions on higher-order genome structure and human disease
Dolores Irala, PhD1
Role of astrocyte dysfunction in neurodevelopmental disorders
Andrew Kodani, PhD3
CHAIR
Aseem Ansari, PhD1; Robert J. Ulrich Endowed Chair in Chemical Biology & Therapeutics
Synthetic gene regulators for personalized medicine, artificial transcription factors to control stem cell fate choices
MEMBERS
Taosheng Chen, PhD, PMP1
Xenobiotic receptors and therapeutic responses
Richard Lee, PhD1; Endowed Chair in Medicinal Chemistry
Discovery of new antibiotic agents and structure-based drug design
ASSOCIATE MEMBERS
Marcus Fischer, PhD1
Protein conformational landscapes for ligand discovery
Anang Shelat, PhD1
Translational research & chemical biology
ASSISTANT MEMBERS
Daniel Blair, PhD1
Covalent inhibitors and automated synthesis
Tommaso Cupido, PhD1
Protein machines & chemical probe discovery
Hai Dao, PhD1
Development of novel chemical biology tools to study abnormal chromatin processes
INSTRUCTOR
Supriya Sarvode, MD
Therapeutic development


INTERIM CHAIR
Jiyang Yu, PhD1
Systems biology, systems immunology, & translational oncology
MEMBERS
Zhaoming Wang, PhD1,2
Genetic epidemiology of pediatric cancer & survivorship
Jinghui Zhang, PhD1; Endowed Chair in Bioinformatics
Cancer genomic variant analysis & visualization
ASSOCIATE MEMBERS
Xiang Chen, PhD1
OMICS integration & tumor heterogeneity by machine
Yong Cheng, PhD1,2 Cis-regulatory modules in hematopoiesis & its disorders
Paul Geeleher, PhD1
Computational methods and drug repositioning
Xiaotu Ma, PhD1
Mathematical modeling of cancer-initiating events
ASSISTANT MEMBERS
Brian Abraham, PhD1
Transcriptional control of cell identity and disease learning approaches
Samuel Brady, PhD1,2
Cancer genomics and pharmacology in pediatric cancer treatment
Xin Zhou, PhD1
Data visualization and real-time analysis

CHAIR
Michael Dyer, PhD1; Richard C. Shadyac Endowed Chair in Pediatric Cancer Research
Retinal development, retinoblastoma, & pediatric solid tumor translational research
MEMBERS
Suzanne Baker, PhD1; Endowed Chair in Brain Tumor Research
Genetic and epigenetic drivers of pediatric high-grade glioma
James Morgan, PhD; Edna and Albert Abdo Shahdam Endowed Chair in Basic Research Control of neuronal death & differentiation
Paul Northcott, PhD1; Endowed Chair in Molecular Neuro-Oncology Genomics & developmental biology of childhood brain tumors
Junmin Peng, PhD1,2 Proteomics & metabolomics in human disease
David Solecki, PhD1
Cell polarity in neuron precursor differentiation
J. Paul Taylor, MD, PhD1,2; Executive Vice President, Scientific Director, Edward F. Barry Endowed Chair in Cell & Molecular Biology
Molecular genetics of neurological diseases
Stanislav S. Zakharenko, MD, PhD1
Neural circuits of learning, memory, and their dysfunction in neurodevelopmental psychiatric disorders
ASSOCIATE MEMBERS Xinwei Cao, PhD1
Growth control during neural tube development
Fabio Demontis, PhD1
Protein homeostasis & stress sensing in skeletal muscle aging
Young-Goo Han, PhD1
Regulatory mechanisms of neural progenitors in brain development, diseases, & evolution
Khaled Khairy, PhD
Biomechanics-based computational models as priors for biological-image analysis
Stephen Mack, PhD1
Pediatric brain tumors, cancer epigenetics, therapeutics, models
Jamy Peng, PhD1
Epigenetic regulation of stem cell functions
Jasmine Plummer, PhD1
Multi-omics examination of genetic risk as a factor of oncogenesis
Elizabeth Stewart, MD1,2
Translational research of pediatric solid tumors
ASSISTANT MEMBERS
Jay Bikoff, PhD1
Neural circuits controlling movement
Yuuta Imoto, PhD1
Membrane trafficking during synaptic vesicle recycling
Lindsay Schwarz, PhD1
Mechanisms of neuromodulatory circuit organization
Jason Vevea, PhD1
Mechanisms of organelle quality control and organelle trafficking in neurons

(Radiology as of Q3 2024)
CHAIR
Andrew Smith, MD, PhD; Endowed Chair in Diagnostic Imaging
Clinical applications of artificial intelligence in radiology
MEMBERS
Sue Kaste, DO4
Robert Kaufman, MD4
Mary (Beth) McCarville, MD4
Wilburn Reddick, PhD1
CNS structural changes during and after therapy
Barry Shulkin, MD, MBA
PET imaging evaluation of pediatric tumors
Ranganatha Sitaram, PhD
Multimodal functional brain imaging & neurorehabilitation
Michael Temple, MD
Advancing pediatric interventional oncology techniques in children
ASSOCIATE MEMBERS
Allison Aguado, MD
Evaluating the safety and effectiveness of interventional radiology therapies for children with cancer
Asim Bag, MBBS, MD1
Response to immunotherapy & radiation therapy, cancer therapy–induced neuroinflammation & brain damage, imaging low-grade gliomas
Hedieh Khalatbari, MD3
Soft-tissue sarcomas and bone tumors
Noah Sabin, MD, JD
Imaging of brain tumors & side effects of therapy
Paul Yi, MD1
Human–computer interaction to augment collaboration between AI & humans in medicine
ASSISTANT MEMBERS
Zachary Abramson, MD, DMD
Quantitative imaging, computeraided three-dimensional modeling
Puneet Bagga, PhD
Metabolic imaging, MR spectroscopy, molecular MRI, & cancer metabolism
Kiel Neumann, PhD1
Translational Imaging and radiopharmaceutical development
Devendra Sawant, MD, PhD
Molecular imaging, radionucleotide therapy, and cancer biology
INSTRUCTORS
Stuart McAfee, PhD
Network interactions between cerebellum, brainstem, and cerebral cortex in normal development and disease
Soniya Pinto, MD
Imaging of neurologic complications of CAR T–cells therapy

CHAIR
Gregory Armstrong, MD, MSCE1; Endowed Chair in Epidemiology & Cancer Control Cancer survivorship & long-term follow-up
MEMBERS
Heather Brandt, PhD1
HPV vaccination and cervical cancer screening
Tara Brinkman, PhD1,2 Psychosocial outcomes of pediatric cancer
Joshua Burns, PhD1; Jeweler’s Charity Fund Endowed Chair in Cancer Survivorship Gait and movement disorders of childhood
I-Chan Huang, PhD
Patient-reported outcomes measurement after pediatric cancer
Melissa Hudson, MD1,2; The Charles E. Williams Endowed Chair of Oncology – Cancer Survivorship Health outcomes after childhood cancer
Kirsten Ness, PT, PhD, FAPTA1; Endowed Chair in Cancer Survivorship
Physical health and accelerated aging in childhood cancer survivors
Leslie Robison, PhD4
Zhaoming Wang, PhD1
Genetic epidemiology of pediatric cancer & survivorship
Yutaka Yasui, PhD1
Genetics & risk of therapyrelated outcomes
ASSOCIATE MEMBERS
Nickhill Bhakta, MD, MPH1,2
Global health, survivorship, epidemiology, childhood leukemias
Angela Delaney Freedman, MD2
Hypothalamic/pituitary dysfunction in childhood cancer survivors
Daniel Mulrooney, MD, MS1,2
Cardiovascular outcomes of cancer therapy
ASSISTANT MEMBERS
Yadav Sapkota, PhD1
Genomic basis of pediatric cancer outcomes
Carmen Wilson, PhD1
Late effects of childhood cancer therapy


MEMBERS
Alessandra d’Azzo, PhD1; Jewelers
Charity Fund Endowed Chair in Genetics and Gene Therapy Lysosomal/proteasomal function in health & disease
Gerard Grosveld, PhD4

CHAIR
Carlos Rodriguez-Galindo, MD1; Executive Vice President, Four Stars of Chicago Chair in International Pediatric Outreach Global medicine, pediatric solid tumors
MEMBERS
Miguela Caniza, MD, MPH1 Global health, infection care and control
Meenakshi Devidas, PhD, MBA1 Biostatistics, pediatric hematology and oncology
Jane Hankins, MD, MS1 Sickle cell disease, transition to adult care & health outcomes during adolescence & young adulthood
Sima Jeha, MD1
Global health, childhood leukemias, developmental therapeutics
Gaston Rivera, MD4
Victor Santana, MD1; Charles Pratt Chair in Solid Tumor Research Global health, novel therapeutics, neuroblastoma, research ethics
ASSOCIATE MEMBERS
Asya Agulnik, MD, MPH1
Global health, pediatric oncocritical care, quality improvement
Nickhill Bhakta, MD, MPH1 Global health, survivorship, epidemiology, childhood leukemias
Paola Friedrich, MD, MPH1 Global health, health disparities, health services, pediatric solid tumors
Catherine Lam, MD, MPH1 Global health, health systems, pediatric solid tumors
Ibrahim Qaddoumi, MD, MS1
Global health, brain tumors, telemedicine, retinoblastoma
Teresa Santiago, MD2 Laboratory quality improvement & assessment
Jeremy Slone, MD, MPH1 Global pediatric cancer epidemiology
ASSISTANT MEMBERS
Anita Arias Prado, MD2
Capacity building in pediatric critical care
Dylan Graetz, MD1
Global health, patientcentered care, solid tumors
Saman Hashmi, MD
Capacity building in global pediatric oncology
Michael McNeil, MD, MPH1
Defining the state of palliative care for children with cancer in resource-constrained settings
Daniel Moreira Ridsdale, MD1 Global pediatric oncology, evidence-based education, pediatric CNS tumors
Sheena Mukkada, MD, MPH1 Global health, infection care & control
INSTRUCTORS
Caitlyn Duffy, MD
Application of implementation science to address the global pediatric cancer survival gap
Marta Salek, MD, MPH
Optimizing care and quality of life for children with cancer on a global scale

CHAIR
Mitchell Weiss, MD, PhD1; Arthur Nienhuis Endowed Chair in Hematology
Blood development, red blood cell biology, novel therapeuticapproaches to sickle cell disease and β-thalassemia
MEMBERS
John Crispino, PhD, MBA1; Wall Street Committee Endowed Chair
Mechanisms of leukemogenesis, benign & malignant blood disorders
Shannon McKinney-Freeman, PhD1
Mechanisms of hematopoietic stem cell development & transplantation
Ellis Neufeld, MD, PhD; Executive Vice President, Clinical Director, John and Lorine Thrasher Endowed Chair in Pediatric Medicine Patient-oriented studies in nonmalignant hematology
Clifford Takemoto, MD1; Lemuel Diggs Endowed Chair in Sickle Cell Disease Hemostasis & thrombosis, vascular malformations, bone marrow failure
Winfred Wang, MD4
ASSOCIATE MEMBERS
Yong Cheng, PhD1
Cis-regulatory modules in hematopoiesis & its disorders
Wilson Clements, PhD1
Hematopoietic development & leukemia
Ulrike Reiss, MD1
Bleeding disorders, gene therapy for hemophilia, bone marrow failure
Carolyn Russo, MD
Quality improvement inclinical networks
Shengdar Tsai, PhD1
Genome-engineering technologies for therapeutics
Jonathan Yen, PhD1
Translation of therapeutic genome engineering technologies to treat hemoglobinopathies
ASSISTANT MEMBERS
Nidhi Bhatt, MD
Health communication & implementation science
Marta Derecka, PhD1
Hematopoiesis & the bone marrow microenvironment
Rohith Jesudas, MBBS Hemostasis, thrombosis, & immune cytopenias
Alyssa Kennedy, MD, PhD Molecular drivers behind bone marrow failure and leukemiapredisposition syndromes
Alexis Leonard, MD Curative strategies for sickle cell disease
Dirk Loeffler, PhD1 Cancer stem cells & clonal hematopoiesis
Yogindra Persaud, MD Advancing the knowledge of sickle cell disease
Parul Rai, MD Cardiac injury in sickle cell disease
Marcin Wlodarski, MD, PhD1 Inherited bone marrow failure & MDS-predisposition syndromes
Masayuki Yamashita, MD, PhD1 Cell death programs that control hematopoietic stem cell survival vs. elimination
INSTRUCTORS
Georgios Christakopoulos, MD Development of genome-editing strategies to cure β-thalassemia
Richa Sharma, MD3
RESEARCH ASSOCIATE Phillip Doerfler, PhD3
ADJUNCT MEMBERS
Kenneth Ataga, MD Sickle cell disease and related hemoglobinopathies, thalassemia and other red blood cell disorders
Francisca Fasipe, MD Leukemia, lymphoma, hemoglobinopathies, and solid tumors
Marcela Popescu, MD Clinical pediatric hematology

CHAIR
Victor Torres, PhD1; Albert and Rosemary Joseph Endowed Chair in Host-Microbe Interactions Interactions between antimicrobial-resistant bacteria and their mammalian host
MEMBERS
Jason Rosch, PhD1
Bacterial genomics & pathogenesis
Stacey Schultz-Cherry, PhD1 Pathogenesis of influenza & enteric virus infections
Paul Thomas, PhD1 Mechanisms of antiviral and antitumor immunity
Elaine Tuomanen, MD1 Pathogenesis of pneumococcal infection
Richard Webby, PhD1 Influenza virus pathogenicity
ASSOCIATE MEMBER
Charles Russell, PhD1
Respiratory viruses: disease, cures, and prevention
ASSISTANT MEMBER
Jeremy Crawford, PhD1
Translational immunology, immunotherapy, and immunoinformatics
INSTRUCTOR
Bradley Muller, MD2
Gamma-delta T-cell receptor biology in gamma-delta T-cell acute lymphoblastic leukemia


INTERIM CHAIR
Terrence L. Geiger, MD, PhD1,2; Endowed Chair in Pediatrics
T-cell regulation, adoptive immunotherapy
VICE-CHAIR
Thirumala-Devi Kanneganti, PhD1; Rose Marie Thomas Endowed Chair in Immunology
Mechanisms of host defense & inflammation
MEMBERS
Hongbo Chi, PhD1; Robert G. Webster Endowed Chair in Immunology
Immune signaling and metabolism
Peter Doherty, PhD4; Nobel Laureate
Douglas Green, PhD1; Peter Doherty
Endowed Chair in Immunology
Cell death, autophagy, and immune function
Benjamin Youngblood, PhD1
T-cell memory differentiation, exhaustion, and immunotherapy
ASSOCIATE MEMBERS
Yongqiang Feng, PhD1
Epigenetic & transcriptional basis of T-cell immunity
Bo Hu, PhD1
Neuroimmunology and interrogations of neuroimmune interactions in health and disease
ASSISTANT MEMBER
Yunlong Zhao, PhD1
Molecular and cellular cues that influence antitumor responses utilizing membrane-reconstitution systems and advanced imaging

CHAIR
Octavio Ramilo, MD1; Endowed Chair in Infectious Diseases Viral respiratory infections and early life immunity
MEMBERS
Miguela Caniza, MD, MPH1,2 Global health, infection care and control
Patricia Flynn, MD1; Arthur Ashe Endowed Chair in Pediatric AIDS Research HIV/AIDS in children & infections in children with cancer
Aditya Gaur, MD, MBBS1 Clinical research in HIV prevention & treatment
Hana Hakim, MD Infection prevention and control
Julia Hurwitz, PhD1 Pathogen/vaccine-induced immunity, nuclear hormones
Gabriela Marón Alfaro, MD1 Infectious complications in transplant patients
Asuncion Mejias, MD, PhD, MsCS Viral respiratory infections and perinatal infections
Steven Varga, PhD1; Endowed Chair–Dean Graduate School of Biomedical Sciences Immunopathogenesis of respiratory viruses
Robert Webster, PhD4
Joshua Wolf, PhD, MBBS1 Prediction, prevention, & treatment of infections in immunocompromised children
ASSOCIATE MEMBERS
Elisabeth Adderson, MD1 Epidemiology & treatment of infections
Diego Hijano, MD, MSc1
Host–pathogen interactions of respiratory virus
Katherine Knapp, MD
Perinatal HIV exposure/ HIV clinical trials
Nehali Patel, MD1 HIV clinical care
Megan Wilkins, PhD2
Clinical & research psychological services for youth with HIV/AIDS
ASSISTANT MEMBERS
Lisa Hiskey, DO
Optimizing antimicrobial use in immunocompromised pediatric patients through infectious diseases diagnostics
Ellie Margolis, MD, PhD1 Microbiome dynamics in immunocompromised patients
Sheena Mukkada, MD, MPH1,2 Global health, infection care and control
INSTRUCTOR
Amanda Green, MD
Human immune responses to co-infection and chronic viruses, including HIV and CMV
ADJUNCT MEMBERS
Nicholas Hysmith, MD, MS, FAAP Emerging infections & hospital epidemiology
Jonathan A. McCullers, MD
Interactions between viruses & bacteria

CHAIR
Julie Park, MD; Endowed Chair in Pediatric Oncology
Translational research to improve survival of children with cancer
MEMBERS
Gregory Armstrong, MD, MSCE1,2; Endowed Chair in Epidemiology & Cancer Control
Pediatric neuro-oncology & cancer survivorship
Sara Federico, MD1
Drug development, pediatric soft-tissue sarcomas
Elizabeth Fox, MD1
Developmental therapeutics in pediatric oncology
Wayne Furman, MD4
Amar Gajjar, MD2; Scott and Tracie Hamilton Endowed Chair in the Brain Tumor Program Novel treatments for children with brain tumors
Daniel Green, MD1
Adverse hepatic, renal, and reproductive effects of therapy
Alejandro Gutierrez, MD1
Molecular basis of chemotherapy resistance to advance novel therapeutics
Melissa Hudson, MD1; The Charles E. Williams Endowed Chair of Oncology – Cancer Survivorship Health outcomes after childhood cancer
Hiroto Inaba, MD, PhD1 New therapeutic strategies for leukemia
Sima Jeha, MD1,2
Global health, childhood leukemias, developmental therapeutics
Sue Kaste, DO2,4
Kim Nichols, MD1
Heritable cancers & primary immunodeficiency syndromes
Alberto Pappo, MD1; Alvin Mauer Endowed Chair New therapies for sarcomas & rare pediatric cancers
Ching-Hon Pui, MD1; Fahad
Nassar Al-Rashid Endowed Chair in Leukemia Research Biology & treatment of childhood leukemia
Raul Ribeiro, MD1
Hematological malignancies
Charles W. M. Roberts, MD, PhD1; Executive Vice President, Lillian R. Cannon Comprehensive Cancer Center Director Endowed Chair SWI/SNF (BAF) chromatin remodeling/tumor suppressor
Giles Robinson, MD1
Origin & genomics of medulloblastoma, translational studies
Jeffrey Rubnitz, MD, PhD3
Jun J. Yang, PhD1,2; Endowed Chair in Pharmacogenomics
Pharmacogenomics of anticancer agents & drug resistance
ASSOCIATE MEMBERS
Nickhill Bhakta, MD, MPH1,2
Global health, survivorship, epidemiology, childhood leukemias
Patrick Campbell, MD, PhD1 Histiocytic disorders, clinical informatics, patient safety
Matthew Ehrhardt, MD, MS1
Late effects of childhood cancer therapy
Paola Friedrich, MD, MPH1,2
Global health, health disparities, health services, pediatric solid tumors
Rebecca Gardner, MD
Development of cellular immunotherapy trials for pediatric cancer
M. Meaghan Granger, MD
Treatment of high-risk neuroblastoma in newly diagnosed and relapsed patients
Mark Hatley, MD, PhD1
Origins of pediatric sarcomas
Sara Helmig, MD1
Sarcoma, thyroid carcinoma, & quality improvement
Liza-Marie Johnson, MD, MPH, MSB1
Ethical issues in pediatrics
Seth Karol, MD1
Toxicity reduction during acute leukemia therapy
Erica Kaye, MD1
Prognostic communication, early integration of palliative care in oncology
Myriam Labelle, PhD1
The role of the microenvironment in cancer metastasis
Catherine Lam, MD, MPH1,2
Global health, health systems, pediatric solid tumors
Deena Levine, MD
Pediatric palliative & end-of-life care
Daniel Mulrooney, MD, MS1
Cardiovascular outcomes of cancer therapy
Ibrahim Qaddoumi, MD, MS1,2
Global health, brain tumors, telemedicine, retinoblastoma
Elizabeth Stewart, MD1
Translational research of pediatric solid tumors
Anna Vinitsky, MD, MS1
Pediatric neuro-oncology & process improvement
ASSISTANT MEMBERS
Aditi Bagchi, MD, PhD
Molecular and genomic characteristics of pediatric brain tumors
Kelsey Bertrand, MSc, MBBS Understanding ependymoma and high-grade glioma
Michael Bishop, MD3
Steven Carey, MD, PhD Management of central nervous system malignancies
Griffin Collins, MD1 Integration of palliative care
Brittany Cowfer, MD1 Prognostic communication in pediatric oncology
Stephanie Dixon, MD1 Pediatric cancer survivorship
Adam Durbin, MD, PhD1 Molecular biology of highrisk pediatric cancers
Aysenur Esen, MD Relapsed or refractory acute myeloid leukemia
Jessica Gartrell, MD
Early phase clinical trial development, sarcomas, liver tumors
Dylan Graetz, MD1,2 Global health, patient-centered care, solid tumors
Lillian Guenther, MD1 Novel genomic targets in osteosarcoma
Saman Hashmi, MD2
Capacity building in global pediatric oncology
Zhongbo Hu, MD, PhD3
Lauren Jerkins, MD
Cellular therapy, quality improvement, and patient safety
Michael McNeil, MD, MPH1,2
Defining the state of palliative care for children with cancer in resource-constrained settings
Daniel Moreira Ridsdale, MD1,2
Global pediatric oncology, evidencebased education, pediatric CNS tumors
Min Ni, PhD1
Genetic and metabolic regulation of childhood development and cancers
Esther Obeng, MD, PhD1
Myeloid malignancies & bone marrow failure syndromes
Anand Patel, MD, PhD1
Tumor recurrence in pediatric rhabdomyosarcoma
Melissa Perrino, MD
Germline predisposition and genetic drivers of cancer
Matthew Rees
Improvement science in the care of children with cancer
Linda Stout, MD
Pediatric oncology
Liqin Zhu, PhD2
Stem cells in normal & malignant development
INSTRUCTORS
Matthew Davis, MD
Acute care of hematology and oncology patients
Caitlyn Duffy, MD2
Application of implementation science to address the global pediatric cancer survival gap
Emily Hanzlik, MD2
Clinical pediatric neuro-oncology & neurologic complications of pediatric cancer
Supriya Sarvode, MD2
Therapeutic development
Dana Tlais, MD
Characterizing the molecular landscape of pediatric high-grade gliomas
Ruth Wang’ondu, MD, PhD
Integration of genetic data from diverse populations to inform treatment of B-cell acute lymphoblastic leukemia
ADJUNCT MEMBERS
Francisca Fasipe, MD
Leukemia, lymphoma, hemoglobinopathies, and solid tumors
Marcela Popescu, MD
Clinical pediatric hematology


CHAIR
David Ellison, MBBChir, MA(hons), MSc, MD, PhD; Joan and Roy Gignac Endowed Chair in Pathology & Laboratory Medicine
Pathologic/molecular classification of CNS tumors
MEMBERS
James R. Downing, MD; President and Chief Executive Officer; Donald Pinkel Endowed Chair in Childhood Cancer Treatment
The molecular pathology of acute leukemia
Terrence L. Geiger, MD, PhD1; Endowed Chair in Pediatrics
T-cell regulation, adoptive immunotherapy
Randall Hayden, MD
Clinical microbiology of immunocompromised hosts
Laura Janke, DVM, PhD
Pathology of mouse models of disease
Jeffery Klco, MD, PhD1
Genomic & functional characterization of pediatric myeloid neoplasms
Mondira Kundu, MD, PhD1,2 Autophagy-related proteins in health & human disease
Michael Meagher, PhD4
Charles Mullighan, MBBS(Hons), MSc, MD1; William E. Evans Endowed Chair
Genomic, experimental, & preclinical studies of acute leukemia
Kim Nichols, MD1,2
Heritable cancers & primary immunodeficiency syndromes
Brent Orr, MD, PhD1
Molecular classification of tumors of the nervous system
Jerold Rehg, DVM4
A. Peter Vogel, DVM, PhD1
Pathology of animal models of human disease
Jian Xu, PhD1
Gene regulatory processes controlling stem cell development and blood cancers
Gerard Zambetti, PhD1
The function of p53 in tumor suppression & tumorigenesis
ASSOCIATE MEMBERS
Jason Cheng-Hsuan Chiang, MD, PhD
Diagnosis & classification of CNS tumors
Larissa Furtado, MD Clinical genomics and data management systems
Gabriela Gheorghe, MD
Pediatric leukemias and lymphomas, histiocytic lesions
Yen-Chun Liu, MD, PhD Hematologic malignancies
Harshan Pisharath, DVM, PhD
Animal models of human diseases, preclinical safety
Teresa Santiago, MD
Laboratory quality improvement & assessment
Heather Tillman, DVM, PhD Comparative pathology
Lu Wang, MD, PhD
Genomic profiling & functional analysis of genetic alterations in pediatric tumors
Gang Wu, PhD1
Genome instability, neurodegeneration, brain transcriptomics
Yan Zheng, MD, PhD
Red blood cell genotyping & alloimmunization, cancer immunotherapy
ASSISTANT MEMBERS
Paula Arnold, PhD HLA and hematopoietic cell transplantation
Patrick Blackburn, PhD
Clinical laboratory genetics and genomics
Mohammed Eldomery, MD
Molecular oncology, cancerpredisposition syndromes
Heather Glasgow, PhD
Novel diagnostics for clinical microbiology
Anoop Murthy Kavirayani, DVM, DACVP
Comparative preclinical pathology, experimental/investigative discovery pathology, and toxicologic pathology
Alyssa Kennedy, MD, PhD2
Molecular drivers behind bone marrow failure and leukemiapredisposition syndromes
Mahsa Khanlari, MD
Diagnosis and classification of pediatric hematopoietic neoplasms
Selene Koo, MD, PhD
Molecular classification of pediatric solid tumors
Priya Kumar, MD
Diagnostic capacity building for hematologic malignancies in resource-limited settings
Julieann Lee, MD, MS Clinicopathologic and molecular characterization of pediatric brain tumors
Faizan Malik, MD
Morphologic and molecular characterization of bone and soft-tissue sarcomas and pediatric solid tumors
Denis Noubouossie, MD, PhD
Clinical pathology and transfusion medicine
RESEARCH ASSOCIATE
Lindsey Montefiori, PhD
Lineage-ambiguous leukemia and gene regulatory mechanisms of oncogenic transcription factor activity

CHAIR
Amar Gajjar, MD; Scott and Tracie Hamilton Endowed Chair in the Brain Tumor Program
Novel treatments for children with brain tumors
MEMBERS
Shannon Dean, MD, MMM; Chief Medical Information Officer Applied clinical informatics
Richard Finkel, MD; George J. Pedersen Endowed Chair in Neurotherapeutics, Director of the Center for Experimental Neurotherapeutics Pediatric neurologic and metabolic diseases
Andrea Gropman, MD; Michael F. Tamer Endowed Chair in Pediatric Neurology
Evaluating neurocognitive injury in inborn errors of metabolism by using multimodal neuroimaging
Raja Khan, MD; Division of Neurology Director
Effect of cancer on central & peripheral nervous systems
Kirsten Ness, PT, PhD, FAPTA1,2 Physical health and accelerated aging in childhood cancer survivors
Ellis Neufeld, MD, PhD2; Executive Vice President, Clinical Director, John & Lorine Thrasher Endowed Chair in Pediatric Medicine Patient-oriented studies in nonmalignant hematology
ASSOCIATE MEMBERS
Angela Delaney Freedman, MD; Division of Endocrinology Director Hypothalamic/pituitary dysfunction in childhood cancer survivors
Asya Agulnik, MD, MPH1,2 Global health, pediatric oncocritical care, quality improvement
Lama Elbahlawan, MD
Pediatric critical care, acute lung injury
Michael Frett, MD; Division of Anesthesiology Director Pediatric anesthesia
Saad Ghafoor, MD
Improvement of pediatric critical care outcomes
Ellen Grishman, MD
Quality of life in pediatric patients with diabetes
Melissa Hines, MD Pediatric critical care, hemophagocytic lymphohistiocytosis
Caitlin Hurley, MD Onco-critical care, HSCT/ immunotherapy patients, long-term care
Belinda Mandrell, PhD, RN, CPNP1; Division of Nursing Research Director Biological mechanism of symptoms associated with cancer & cancer therapy
Jennifer McArthur, DO1 Improving outcomes in critically ill pediatric patients
R. Ray Morrison, MD1; Division of Critical Care Medicine Director Pediatric critical care, myocardial protection
Kavitha Raghavan, MBBS, FRCA Patient safety & quality of care in pediatric anesthesia
Michael Rossi, DO Patient safety & cognitive effects of anesthesia
Luis Trujillo Huaccho, MD Regional anesthesia & anesthetic approach in high-risk cases
Christine Yu, MD Fertility after gonadotoxic therapy
ASSISTANT MEMBERS
Anita Arias Prado, MD Capacity building in pediatric critical care
D. Andrew Elliott, MD; Division of Psychiatry Director Psychiatric effects of cancer and its treatment
TeKesha Henry, DO3
Tzipa Zweig, MD, MS Pediatric pain and palliative care
INSTRUCTORS
Emily Hanzlik, MD Clinical pediatric neuro-oncology & neurologic complications of pediatric cancer
Andrea Heifner, MD Pediatric critical care medicine
ADJUNCT MEMBERS
Mark Corkins, MD Gastroenterology
Patricia Dubin, MD Pulmonology
Terri Finkel, MD, PhD Rheumatology
James Wheless, MD Neurology


CHAIR
P. David Rogers, PharmD, PhD1; Endowed Chair in Pharmaceutical Sciences
Molecular and genetic basis of antifungal drug resistance
VICE-CHAIRS
Brooke Bernhardt, PharmD, MS, FCCP
Pharmacogenomics of treatment-related toxicity and outcomes in pediatric cancer
Jun Yang, PhD1; Endowed Chair in Pharmacogenomics
Pharmacogenomics of anticancer agents & drug resistance
MEMBERS
William Evans, PharmD4
James Hoffman, PharmD; Chief Patient Safety Officer Medication safety & outcomes
Markos Leggas, PhD1
Pharmacometabolomic methods to improve therapeutic outcomes and minimize toxicity in the context of pediatric clinical trials
Mary Relling, PharmD4
John Schuetz, PhD1
Regulation & function of ABC transporters
Clinton Stewart, PharmD1
Pharmacology of anticancer drugs in children
ASSOCIATE MEMBERS
Kelly Caudle, PharmD, PhD, BCPS, FCCP
Pharmacogenomics, implementation science, and clinical practice guideline development
Cyrine-Eliana Haidar, PharmD, BCPS, BCOP, FASHP
Clinical pharmacogenomics
Daniel Savic, PhD1
Pharmacogenomics & cis-regulatory architecture of pediatric leukemia
ASSISTANT MEMBERS
Samuel Brady, PhD1
Cancer genomics and pharmacology in pediatric cancer treatment
Peijun Ma, PhD1
Genetic markers for the development of effective therapies to treat bacterial infections
Jeffrey Rybak, PharmD, PhD1 Antifungal pharmacotherapy
Liqin Zhu, PhD1
Stem cells in normal & malignant liver development

CHAIR
Kevin Krull, PhD1; Endowed Chair in Psychology
Cognitive neuroscience approaches to outcomes and interventions in pediatric cancer survivors
MEMBERS
Tara Brinkman, PhD1
Psychosocial outcomes of pediatric cancer
Heather Conklin, PhD1
Cognitive outcomes of childhood cancer treatment
Valerie Crabtree, PhD1
Sleep disruptions and fatigue in pediatric oncology
Melissa Hudson, MD1,2; The Charles E. Williams Endowed Chair of Oncology – Cancer Survivorship Health outcomes after childhood cancer
Niki Jurbergs, PhD
Psychological & cognitive impact of pediatric cancer
Sean Phipps, PhD4
ASSOCIATE MEMBERS
Robert Ferguson, PhD
Treatment and rehabilitation of cancer-related cognitive impairment for cancer survivors
Ashley Fournier-Goodnight, PhD, ABPP-CN
Neurobehavioral outcomes in infants and toddlers with early brain pathology
Jennifer Harman, PhD3
Lisa Jacola, PhD
Neurobehavioral outcomes in children treated for cancer
Kendra Parris, PhD
Coping & adjustment in youth with cancer
Jerlym Porter, PhD, MPH1
Transition from pediatric to adult care in sickle cell disease
Brian Potter, PsyD
Neurocognitive outcomes in children with cancer
Megan Wilkins, PhD
Clinical & research psychological services for youth with HIV/AIDS
Victoria Willard, PhD5
ASSISTANT MEMBERS
R. Elyse Heidelberg Kenney, PsyD
Pain and symptom management in pediatric hematology/oncology
Andrew Heitzer, PhD
Neurocognitive outcomes in sickle cell disease
Anna Jones, PhD
Transition off therapy for oncology patients and families
Jennifer Longoria, PhD
Neurocognitive outcomes in sickle cell disease
Nicholas Phillips, MD, PhD
Neurocognitive late effects, cancer survivorship, functional and structural neuroimaging
Darcy Raches, PhD
Acute neurological injury & cognitive outcomes associated with childhood cancer treatment
Katianne Sharp, PhD
Cancer predisposition & adjustment in families of children with cancer
Rachel Webster, PhD
Promotion of healthy lifestyle behaviors in children with cancer & survivors of childhood cancer
INSTRUCTORS
Jessica Cook, PhD
Impact of child–caregiver interactions and caregiver wellbeing on patient psychosocial and medical outcomes
Ryan James, PhD
Pediatric pain and somatic symptoms & trauma-informed care in adolescents and young adults

CHAIR
Thomas Merchant, DO, PhD1;
Baddia J. Rashid Endowed
Chair in Radiation Oncology
Proton radiotherapy for CNS tumors and radiation-related CNS effects
MEMBERS
Chia-ho Hua, PhD
Improving proton therapy accuracy, advanced imaging for radiation therapy, normal tissue complication modeling
Matthew Krasin, MD1
Developing radiation therapy strategies and toxicity profiles for pediatric sarcomas
ASSOCIATE MEMBERS
John Lucas Jr., MS, MD
Brain tumors, neuroblastoma, proton therapy, clinical trial design
Carmen Perez, MD, PHD
Radiation-induced immune responses and to identify radiomitigation strategies
Christopher Tinkle, MD, PhD1
Preclinical evaluation of novel combination therapies and clinical trial development for high-risk brain tumors and sarcomas
ASSISTANT MEMBER
Ozgur Ates, PhD, DABR
Adaptive proton therapy & surface-guided radiation therapy

CHAIR
Charalampos Kalodimos, PhD1; Joseph Simone Endowed Chair in Basic Research Functional mechanisms of protein machineries
MEMBERS
M. Madan Babu, PhD, FRSC1; George J. Pedersen Endowed Chair in Biological Data Science Data science for discovery and personalized medicine
Scott Blanchard, PhD1; Endowed Chair in Molecular Imaging Examining structure–function relations in macromolecular assemblies
Mario Halic, PhD1
Regulation of genome expression
Richard Kriwacki, PhD1 Structural basis of tumor suppressor function
Tanja Mittag, PhD1
Molecular basis of liquid–liquid phase separation
Junmin Peng, PhD1 Proteomics & metabolomics in human disease
Georgios Skiniotis, PhD; Endowed Chair in Structural Cell Biology
Mechanistic aspects of signal recognition and propagation through G-protein–coupled receptors and their partner proteins
Stephen White, DPhil4
ASSOCIATE MEMBERS
Marcus Fischer, PhD1,2 Protein conformational ensembles
Elizabeth Kellogg, PhD1
Genome engineering, organization, and architecture
ASSISTANT MEMBERS
Christoph Gorgulla, PhD
Development of next-generation methods for computational biology and ligand/drug discovery
Chia-Hsueh Lee, PhD1
Molecular mechanisms of membrane-signaling complexes
Ji Sun, PhD3
ADJUNCT MEMBER
Brenda Schulman, PhD Cellular regulation by ubiquitin-like proteins


CHAIR
Andrew Davidoff, MD1; Endowed Chair in Surgical Research
Surgical management of solid tumors, gene therapy, angiogenesis inhibition, neuroblastoma, Wilms tumor
MEMBERS
Bhaskar Rao, MD4
Stephen Shochat, MD4
Martha Wells, DMD, MS
Dental materials and technology utilized in pediatric dentistry
ASSOCIATE MEMBERS
Andrew Murphy, MD1
Renal tumors, neuroblastoma, Wilms tumorigenesis, cancer stem cells
Jun Yang, MD, PhD1
Cancer epigenetics & targeted therapy
ASSISTANT MEMBERS
Abdelhafeez Abdelhafeez, MD3
Lindsay Talbot, MD Sarcomas, immunotherapeutic strategies against sarcoma & solid tumor metastases
ADJUNCT MEMBERS
Mary Ellen Hoehn, MD Pediatric ophthalmology
Paul Klimo Jr, MD Pediatric neurosurgery
Michael Neel, MD Pediatric orthopedic oncology
Anthony Sheyn, MD Pediatric otolaryngology
Matthew Wilson, MD; St. Jude Chair in Pediatric Ophthalmology Pediatric ophthalmology

CHAIR
Charles J. Sherr, MD, PhD; Herrick Foundation Endowed Chair in Tumor Cell Biology Tumor suppressor-dependent signaling networks
MEMBERS
Linda M. Hendershot, PhD4
Martine F. Roussel, PhD1; Endowed Chair in Molecular Oncogenesis Genomics & epigenomics in pediatric brain tumors
ASSOCIATE MEMBER Chunliang Li, PhD1
Three-dimensional genome and transcriptional regulation in cancer



Aseem Z. Ansari, PhD
Robert J. Ulrich Endowed Chair in Chemical Biology & Therapeutics

Gregory T. Armstrong, MD, MSCE
Endowed Chair in Epidemiology & Cancer Control

Alessandra d’Azzo, PhD
Jewelers Charity Fund Endowed Chair in Genetics & Gene Therapy

M. Madan Babu, PhD, FRSC
George J. Pedersen Endowed Chair in Biological Data Sciences

Suzanne J. Baker, PhD
Endowed Chair in Brain Tumor Research

Scott C. Blanchard, PhD
Endowed Chair in Molecular Imaging

Joshua Burns, PhD
Jeweler’s Charity Fund Endowed Chair in Cancer Survivorship

Hongbo Chi, PhD
Robert G. Webster Endowed Chair in Immunology

John D. Crispino, PhD, MBA
The Wall Street Committee Endowed Chair




Andrew Davidoff, MD
Endowed Chair in Surgical Research
James R. Downing, MD
Donald Pinkel Endowed Chair in Childhood Cancer Treatment
Michael A. Dyer, PhD
Richard C. Shadyac Endowed Chair in Pediatric Cancer Research
David W. Ellison, MD, PhD
Joan and Roy Gignac Endowed Chair in Pathology and Laboratory Medicine
Richard S. Finkel, MD
George J. Pedersen Endowed Chair in Neurotherapeutics

Patricia M. Flynn, MD
Arthur Ashe Endowed Chair in Pediatric AIDS Research

Amar J. Gajjar, MD
Scott and Tracie Hamilton Endowed Chair in the Brain Tumor Program

Terrence L. Geiger, MD, PhD
St. Jude Endowed Chair in Pediatrics

Stephen M. Gottschalk, MD
Endowed Chair in Bone Marrow Transplantation & Cellular Therapy

Douglas R. Green, PhD
Peter C. Doherty Endowed Chair in Immunology

Andrea L. Gropman, MD
Michael F. Tamer Endowed Chair in Pediatric Neurology

Melissa M. Hudson, MD
The Charles E. Williams Endowed Chair in Oncology–Cancer Survivorship






Charalampos G. Kalodimos, PhD
Joseph Simone Endowed Chair in Basic Research
Thirumala-Devi Kanneganti, PhD
Rose Marie Thomas Endowed Chair in Immunology
Kevin R. Krull, PhD
Endowed Chair in Psychology
Richard E. Lee, PhD
Endowed Chair in Medicinal Chemistry
Peter J. McKinnon, PhD
Endowed Chair in Pediatric Neurological Diseases
Thomas E. Merchant, DO, PhD
Baddia J. Rashid Endowed Chair in Radiation Oncology

James I. Morgan, PhD
Edna & Albert Abdo Shahdam Endowed Chair in Basic Research


Motomi Mori, PhD
Endowed Chair in Biostatistics

Charles G. Mullighan, MBBS(Hons), MD
William E. Evans Endowed Chair

Kirsten Ness, PT, PhD, FAPTA
Endowed Chair in Cancer Survivorship

Ellis J. Neufeld, MD, PhD
John & Lorine Trasher Endowed Chair in Pediatric Medicine

Paul Northcott, PhD
Endowed Chair in Molecular Neuro-Oncology

Alberto S. Pappo, MD
Alvin Mauer Endowed Chair

Julie Park, MD
Endowed Chair in Pediatric Oncology






Ching-Hon Pui, MD
Fahad Nassar Al-Rashid Endowed Chair in Leukemia Research
Octavio Ramilo, MD
Endowed Chair in Infectious Diseases
Charles W.M. Roberts, MD, PhD
Lillian R. Cannon Comprehensive Cancer Center Director Endowed Chair
Carlos Rodriguez-Galindo, MD
Four Stars of Chicago Endowed Chair in International Pediatric Outreach
P. David Rogers, PharmD, PhD
St. Jude Endowed Chair in Pharmaceutical Sciences
Martine F. Roussel, PhD
Endowed Chair in Molecular Oncogenesis

Victor M. Santana, MD
Dr. Charles B. Pratt Endowed Chair in Solid Tumor Research

Charles J. Sherr, MD, PhD
Herrick Foundation Endowed Chair in Tumor Cell Biology

Georgios Skiniotis, PhD
Endowed Chair in Structural Cell Biology

Andrew D. Smith, MD, PhD
Endowed Chair in Diagnostic Imaging (Radiology as of Q3 2024)

Clifford M. Takemoto, MD
Lemuel Diggs Endowed Chair in Sickle Cell Disease

J. Paul Taylor, MD, PhD
Edward F. Barry Endowed Chair in Cell & Molecular Biology

Victor Torres, PhD
Albert and Rosemary Joseph Endowed Chair in Host–Microbe Interactions

Steven M. Varga, PhD
Endowed Chair – Dean St. Jude Children’s Research Hospital Graduate School of Biomedical Sciences


Mitchell J. Weiss, MD, PhD
Arthur Nienhuis Endowed Chair in Hematology
Jun J. Yang, PhD
Endowed Chair in Pharmacogenomics
Jinghui Zhang, PhD
Endowed Chair in Bioinformatics

Diana Acevedo, PhD, Developmental Neurobiology
Anushree Achari, PhD, Chemical Biology & Therapeutics
Srijan Acharya, PhD, Pharmacy & Pharmaceutical Sciences
Sarada Achyutuni, PhD, Pathology
Adeleye Adeshakin, PhD, Bone Marrow Transplantation & Cellular Therapy
Himanshi Agarwal, PhD, Pathology
Farhan Ahmad, PhD, Center of Excellence - Leukemia Studies
Jemil Ahmed, PhD, Computational Biology
Shahbaz Ahmed, PhD, Structural Biology
Shelby Anderson, PhD, Chemical Biology & Therapeutics1
Konstantin Andreev, PhD, Host–Microbe Interactions
Hiroyasu Aoki, PhD, Host–Microbe Interactions
Amir Arabzade, PhD, Developmental Neurobiology
Cassie Argenbright, PhD, Psychology & Biobehavioral Sciences
Aahan Arif, PhD, Radiation Oncology
Emilia Asante, PhD, Strategic Communication, Education & Outreach
Anoop Babu Vasandan, PhD, Immunology
Lu Bai, PhD, Immunology
Seamus Balinth, PhD, Cancer Center Administration
Juan Barajas, PhD, Pathology
Stefanie Baril, PhD, Pharmacy & Pharmaceutical Sciences
Aditya Barve, PhD, Hematology
Jake Batchelder, PhD, Structural Biology1
Katelyn Baumer, PhD, Chemical Biology & Therapeutics1
Swarna Beesetti, PhD, Cell & Molecular Biology/Immunology 2
Numair Belgaumi, PhD, Global Pediatric Medicine
Declan Bennett, PhD, Computational Biology
Soumen Bera, PhD, Hematology
Amy Berkman, MD, Oncology
Wyatt Beyers, PhD, Cell & Molecular Biology
Akash Bhaskar, PhD, Pharmacy & Pharmaceutical Sciences
Akshita Bhatt, PhD, Developmental Neurobiology1
Kashi Bhattarai, PhD, Pharmacy & Pharmaceutical Sciences
Khaggeswar Bheemanapally, PhD, Structural Biology1
Weixiang Bian, PhD, Immunology
Caitlin Billiot, PhD, Infectious Diseases
Ramya Billur, PhD, Cell & Molecular Biology
Wade Borcherds, PhD, Structural Biology2
Austin Boucher, PhD, Hematology
Ryan Brady, PhD, Structural Biology2
Helena Brenes, MD, Infectious Diseases
David Brice, PhD, Host–Microbe Interactions
Pam Brigleb, PhD, Host–Microbe Interactions
Mark Brimble, PhD, Host–Microbe Interactions
John Bryant, PhD, Structural Biology
Ratnakar Bynigeri, PhD, Immunology1
Donghong Cai, PhD, Pathology
Zhongheng Cai, PhD, Biostatistics
Victoria Castro, PhD, Developmental Neurobiology
Kasturee Chakraborty, PhD, Diagnostic Imaging2,5
Saikat Chakraborty, PhD, Oncology
Bappaditya Chandra, PhD, Structural Biology1
Chih-Chiang Chang, PhD, Diagnostic Imaging1,5
Alexandra Chasse, PhD, Infectious Diseases
Kanokporn Chattrakun, PhD, Structural Biology
Letitia Chen, PhD, Host–Microbe Interactions
Wen Chen, PhD, Immunology
Xin-yan Chen, PhD, Tumor Cell Biology
Yantao Chen, PhD, Oncology
Peter Chockley, PhD, Bone Marrow Transplantation & Cellular Therapy
Jaesung Choi, PhD, Epidemiology & Cancer Control
Sk Mohiuddin Choudhury, PhD, Immunology
Mengqi Chu, PhD, Structural Biology
Chia-Lung Chuang, PhD, Developmental Neurobiology
Mellisa Clemons, PhD, Developmental Neurobiology
Jordan Cockfield, PhD, Oncology
Lisett Contreras, PhD, Pathology
Adam Cornwell, PhD, Hematology
Aaron Cruz Navarrete, PhD, Structural Biology
Chenxi Cui, PhD, Structural Biology1
Preeti Dabas, PhD, Chemical Biology & Therapeutics2
Jonathan Dabbs, PhD, Diagnostic Imaging5
Adithi Danda, PhD, Chemical Biology & Therapeutics
Tram Dao, PhD, Bone Marrow Transplantation & Cellular Therapy
Anuska Das, PhD, Structural Biology
Jitendra Das, PhD, Structural Biology
Tapojyoti Das, PhD, Structural Biology
Abhijit Dasgupta, Structural Biology1
Amy Davis, PhD, Infectious Diseases
Ian Delahunty, PhD, Oncology
Ashish Deshmukh, PhD, Structural Biology
Subhash Dhital, PhD, Cell & Molecular Biology
Thi Duyen Do, MD, Computational Biology
Esteban Dodero Rojas, PhD, Structural Biology
Priyanka Dogra, PhD, Structural Biology
Laura Doorley, PhD, Pharmacy & Pharmaceutical Sciences
Melodie Doute, PhD, Hematology
James Du, PhD, Structural Biology
Asaf Elazar, PhD, Structural Biology
Rebekah Eleazer, PhD, Oncology
Abdelrahman Elsayed, PhD, Biostatistics
Sally Elshaer, PhD, Oncology1
Carolin Escherich, MD, Pharmacy & Pharmaceutical Sciences1
Mansoore Esmaili, PhD, Structural Biology1
Tiffany Eulalio, PhD, Epidemiology & Cancer Control
Li Fan, PhD, Computational Biology
Esmat Fathi, PhD, Cell & Molecular Biology
Feng Feng, PhD, Developmental Neurobiology
Carlos Fernandez Pena Acuna, PhD, Developmental Neurobiology2
Michelle Fernando, PhD, Developmental Neurobiology
David Filipovic, PhD, Developmental Neurobiology
Leigh Fremuth, PhD, Genetics
Jennifer French, PhD, Epidemiology & Cancer Control
Kaustav Gangopadhyay, PhD, Structural Biology
Pritha Ganguly, PhD, Structural Biology
Karishma Gangwani, PhD, Computational Biology2
Megha Garg, PhD, Pharmacy & Pharmaceutical Sciences
Dusan Garic, PhD, Developmental Neurobiology
Mohamed Ghonim, PhD, Host–Microbe Interactions1
Aritra Ghosal, PhD, Biostatistics
Kyla Gibney, PhD, Psychology & Biobehavioral Sciences
Milica Gilic, PhD, Structural Biology
Prashant Giri, PhD, Immunology
Bryan Glazer, PhD, Chemical Biology & Therapeutics
Vanshita Goel, PhD, Tumor Cell Biology
Luisa Gomez Londono, PhD, Pharmacy & Pharmaceutical Sciences1
Abigail Gondringer, PhD, Chemical Biology & Therapeutics
Chelsea Goodenough, PhD, Epidemiology & Cancer Control
Xinrui Gui, PhD, Structural Biology
Omer Gullulu, PhD, Structural Biology1
Xuanming Guo, PhD, Immunology1
Yifeng Guo, PhD, Computational Biology
Samantha Hack, PhD, Cell & Molecular Biology
Priyanka Halder, PhD, GMP1
Eric Hall, PhD, Cell & Molecular Biology1
Trent Hall, PhD, Hematology
Liam Hallada, PhD, Developmental Neurobiology
Rawan Hammoud, MD, Epidemiology & Cancer Control1
Xiaolei Hao, PhD, Immunology
Yanhong Hao, PhD, Structural Biology
Walter Harrington, PhD, Host–Microbe Interactions
Minghong He, PhD, Immunology1
Elodie Henriet, PhD, Oncology
Taylor Hibler, PhD, Host–Microbe Interactions
Siarhei Hladyshau, PhD, Computational Biology
Cyrielle Holuka, PhD, Oncology
Jack Hopkins, PhD, Oncology
Madeline Horan, PhD, Epidemiology & Cancer Control1
Keito Hoshitsuki, PharmD, Pharmacy & Pharmaceutical Sciences1
Hadi Hosseini, PhD, Biostatistics/ Computational Biology/Structural Biology1
Ruida Hou, PhD, Pharmacy & Pharmaceutical Sciences
Maowei Hu, PhD, Chemical Biology & Therapeutics
Wenjun Huang, PhD, Immunology
Ya Huang, PhD, Structural Biology
Yan Huang, PhD, Structural Biology2
Yuanyuan Huang, PhD, Hematology
Brydie Huckestein, PhD, Host–Microbe Interactions
Michael Hughes, PhD, Cell & Molecular Biology
Jihye Hwang, PhD, Computational Biology
Jongchan Hwang, PhD, Oncology
Omkar Indari, PhD, Immunology
Siri Manasa Ippagunta, PhD, Developmental Neurobiology
Katelyn Jackson, PhD, Structural Biology
Laura Jamrog, PhD, Hematology
Thilina Jayasinghe, PhD, Chemical Biology & Therapeutics
Bohyeon Jeong, PhD, Developmental Neurobiology
Fubo Ji, PhD, Immunology1
Meiqin Jiang, PhD, Structural Biology1
Menglin Jiang, PhD, Immunology
Yanbo Jiang, PhD, Developmental Neurobiology
Kasey Jividen, PhD, Hematology2
Minjeong Jo, PhD, Structural Biology
Cydney Johnson, PhD, Host–Microbe Interactions
Jordan Johnson, PhD, Bone Marrow Transplantation & Cellular Therapy
Amber Jones, PhD, Bone Marrow Transplantation & Cellular Therapy
Kamal Jouad, PhD, Diagnostic Imaging1,5
Seunghyun Jung, PhD, Developmental Neurobiology1
Ahmed Kandeil, PhD, Host–Microbe Interactions
Suresh Kandikonda, PhD, Chemical Biology & Therapeutics1
Tae Gun Kang, PhD, Immunology
Priyanka Karmokar, PhD, Surgery
Sara Kassel, PhD, Oncology
Mangesh Kaulage, PhD, Chemical Biology & Therapeutics
Sukhmanjit Kaur, PhD, Bone Marrow Transplant & Cellular Therapy
Ahmed Khalaf, PhD, Hematology1
Suparna Khatun, PhD, Structural Biology
Hanane Khoury, PhD, Hematology
Jiyeon Kim, PhD, Immunology
Yoonji Kim, PhD, Epidemiology & Cancer Control
Shunsuke Kimura, PhD, Pathology1
Evan Kingsley, PhD, Developmental Neurobiology1
Kaitlin Koreski, PhD, Cell & Molecular Biology
Lili Kotmayer, MD, Hematology
Damian Krzyzanowski, PhD, Hematology
Aditya Kshirsagar, PhD, Spatial Transcriptomics Core1
Abhishek Kumar, PhD, Structural Biology1
Harsh Kumar, PhD, Cell & Molecular Biology
Prasanth Kumar, PhD, Immunology
Jesyin Lai, PhD, Diagnostic Imaging1,5
Xin Lan, PhD, Immunology1
Su Hyun Lee, PhD, Oncology
Dongfang Li, PhD, Cell & Molecular Biology2
Hanxia Li, PhD, Computational Biology
Miaomiao Li, PhD, Radiation Oncology
Siyu Li, PhD, Structural Biology

Zhenrui Li, PhD, Immunology
Chun-Yang Lin, PhD, Computational Biology
Jennapher Lingo VanGilder, PhD, Radiation Oncology
Danielle Little, PhD, Developmental Neurobiology
Beiyun Liu, PhD, Immunology
Fengming Liu, PhD, Developmental Neurobiology1
Jiaqi Liu, PhD, Pathology
Ke Liu, PhD, Pharmacy & Pharmaceutical Sciences1
Qiang Liu, PhD, Pharmacy & Pharmaceutical Sciences
Xueying Liu, PhD, Computational Biology
Yun Liu, PhD, Immunology
Zhaolin Liu, PhD, Cell & Molecular Biology
Nele Loecher, PhD, Psychology & Biobehavioral Sciences
Jianlin Lu, I PhD, mmunology
Joelle Magne, PhD, Immunology1
Arun Maharaj, PhD, Epidemiology & Cancer Control1
Kelsey Maher, PhD, Computational Biology
Maud Maillard, PhD, Pharmacy & Pharmaceutical Sciences1
Snigdha Maiti, PhD, Structural Biology
Efren Maldonado, PhD, Chemical Biology & Therapeutics1
Deepshikha Malik, PhD, Structural Biology
Alexandra Mandarano, PhD, Infectious Diseases
Mohammad Amin Mannan, PhD, Pharmacy & Pharmaceutical Sciences
Luigi Mari, PhD, Immunology
Maxwell Martin, PhD, Structural Biology2
Masihuzzaman, PhD, Structural Biology
Yurika Matsui, PhD, Developmental Neurobiology
Taylor Matte, PhD, Developmental Neurobiology
Eli McDonald, PhD, Structural Biology
Johanna Melo-Cardenas, PhD, Hematology1
Smrithi Menon, PhD, Host–Microbe Interactions
Audrey Mercier, PhD, Tumor Cell Biology
Robert Mettelman, PhD, Immunology
Bisi Miao, PhD, Pathology
Nicole Michmerhuizen, PhD, Pathology
Benjamin Minden-Birkenmaier, PhD, Developmental Neurobiology
Anastasia Minervina, PhD, Host–Microbe Interactions
Akhilesh Mishra, PhD, Computational Biology1
Priya Mittal, PhD, Oncology1
Mohammad Ali Mohammad Nezhady, PhD, Oncology
Jyotirmoy Mondal, PhD, Chemical Biology & Therapeutics
Lindsey Montefiori, PhD, Pathology2
Dorothea Morris, PhD, Host–Microbe Interactions
Janeala Morsby, PhD, Oncology
Tresor Mukiza, PhD, Cell & Molecular Biology
Bharath Muralikrishnan, PhD, Cell & Molecular Biology1
Saikat Nandy, PhD, Biostatistics
Ambuja Navalkar, PhD, Structural Biology1
Miguel Navarrete, PhD, Psychology & Biobehavioral Sciences
Stephany Navarro, PhD, Host–Microbe Interactions
Madeline Niederkorn, PhD, Hematology
Andrew Nishimoto, PhD, Host–Microbe Interactions
Kelsey North, PhD, Developmental Neurobiology
Jessica Nunes, PhD, Hematology
Greisly Nunez, PhD, Immunology
Shaikh Nurunnabi, PhD, Developmental Neurobiology
Dora Obodo, PhD, Biostatistics
Jennifer Ocasio Adorno, PhD, Research Education & Training Grant Support
Mary Cameron Ogg, PhD, Developmental Neurobiology
Faten Okda, DVM, PhD, Host–Microbe Interactions
Elisabet Olsen, PhD, Oncology
Han Wee Ong, PhD, Chemical Biology & Therapeutics
Eda Ozdemir, PhD, Host–Microbe Interactions
Tanya Paes, PhD, Psychology & Biobehavioral Sciences
Anasuya Pal, Chemical Biology & Therapeutics
Pankaj Pandey, PhD, Diagnostic Imaging5
Shubhant Pandey, PhD, Center for Pediatric Neurological Disease Research
Nagakannan Pandian, PhD, Immunology
Jung-Un Park, PhD, Structural Biology1
Seong Guk Park, PhD, Structural Biology
Christopher Patton, PhD, Host–Microbe Interactions1
Mary Patton, PhD, Developmental Neurobiology
Jing Pei, PhD, Cell & Molecular Biology
Shalmali Pendse, PhD, Hematology
Shashika Perera, PhD, Diagnostic Imaging5
Charles Perry, PhD, Developmental Neurobiology
Kateryna Petrykey, PhD, Epidemiology & Cancer Control
Sarayut Phasuk, PhD, Developmental Neurobiology
Adam Pickrum, PhD, Host–Microbe Interactions
Shabareesh Pidathala, PhD, Structural Biology
Anna Pittman, PhD, Developmental Neurobiology
Noel-Marie Plonski, PhD, Epidemiology & Cancer Control
Petri Polonen, PhD, Pathology
Pragya Poudel, PhD, HPV Cancer Prevention
Manisha Poudyal, PhD, Cell & Molecular Biology
Rojalin Pradhan, PhD, Cell & Molecular Biology
Rachel Prescott, PhD, Host–Microbe Interactions
Sashikantha Reddy Pulikallu, PhD, Structural Biology
Qiang Qin, PhD, Immunology
Zhuo Qu, PhD, Biostatistics1
Sabina Ranjit, PhD, Pharmacy & Pharmaceutical Sciences2
Meghdad Razizadeh, PhD, Developmental Neurobiology
Tyler Ripperger, PhD, Host–Microbe Interactions
Karen Ritter, PhD, Oncology
Sarah Robinson-Thiewes, PhD, Chemical Biology & Therapeutics
Stephanie Rockfield, PhD, Cell & Molecular Biology
Sarayu Row, PhD, Cell & Molecular Biology2
Sourav Roy, PhD, Chemical Biology & Therapeutics
Diana Sa da Bandeira, PhD, Hematology
Sushree Sahoo, PhD, Hematology
Julio Sanchez, PhD, Structural Biology
Laura Sanchez, PhD, Diagnostic Imaging1,5
Andrea Sanchez Corzo, PhD, Diagnostic Imaging1,5
Darian Santana, PhD, Pharmacy & Pharmaceutical Sciences
Gustavo Santiago-Collazo, PhD, Host–Microbe Interactions
Roman Sarkar, PhD, Immunology
Neha Sarodaya, PhD, Developmental Neurobiology
Jieun See, PhD, Developmental Neurobiology
Anna Seffernick, PhD, Biostatistics1
Justin Seffernick, PhD, Chemical Biology & Therapeutics
Jeremy Shaw, PhD, Immunology
Noha Shendy, PhD, Oncology1
Him Shrestha, PhD, Structural Biology
Rupesh Shrestha, PhD, Chemical Biology & Therapeutics1
Sauradeep Sinha, PhD, Bone Marrow Transplantation & Cellular Therapy
Oleksandra Sirozh, PhD, Structural Biology1
Adam Smiley, PhD, Structural Biology
Maria Smith, PhD, Host–Microbe Interactions
Hao Song, PhD, Immunology
Xirui Song, PhD, Bone Marrow Transplantation & Cellular Therapy
Jiao Sun, PhD, Biostatistics
Julianna Sun, PhD, Developmental Neurobiology
Renqiang Sun, PhD, Immunology
Xiang Sun, PhD, Immunology
Balamurugan Sundaram, PhD, Immunology
Luka Svet, PhD, Host–Microbe Interactions
Jeffrey Swan, PhD, Structural Biology1
Shannon Sweeney, PhD, Developmental Neurobiology
Kumari Sweta, PhD, Chemical Biology & Therapeutics
Kasia Szoltysek, PhD, Pathology
Meng Tang, PhD, Structural Biology
Justin Tanner, PhD, Psychology & Biobehavioral Sciences
Roshina Thapa, PhD, Oncology
Kristen Thomas, PhD, Developmental Neurobiology2
Sai Thulabandu, PhD, Developmental Neurobiology
Cheng Tian, PhD, Pharmacy & Pharmaceutical Sciences
Bailey Tibben, PhD, Pharmacy & Pharmaceutical Sciences1
Ricky Tirtakusuma, PhD, Host–Microbe Interactions
Kyla Tooley, PhD, Developmental Neurobiology
Carolina Torres Rojas, PhD, Diagnostic Imaging5
Despoina Trasanidou, PhD, Hematology1
Olivia Travis, PhD, Developmental Neurobiology
Alexandra Trevisan, PhD, Developmental Neurobiology
Sanja Trifkovic, PhD, Host–Microbe Interactions1
Uwemedimo Udoh, MD, PhD, Cell & Molecular Biology
Masayuki Umeda, MD, Pathology
Saurabh Upadhyay, PhD, Immunology1
Gintvile Valinciute, PhD, Tumor Cell Biology
Alanna Van Huizen, PhD, Hematology
Diego Velasquez Pulgarin, PhD, Hematology
Niveda Vellore, PhD, Hematology
Ashish Verma, PhD, Chemical Biology & Therapeutics
Kaitlin Victor, PhD, Bone Marrow Transplantation & Cellular Therapy
Paulina Villanueva, PhD, Diagnostic Imaging1,5
Eirinaios Vrettos, PhD, Chemical Biology & Therapeutics
Fnu Wahiduzzaman, PhD, Structural Biology
LaShanale Wallace, PhD, Oncology
Haolan Wang, MD, Structural Biology
Jingheng Wang, PhD, Chemical Biology & Therapeutics2
Ju Wang, PhD, Structural Biology
Kaili Wang, PhD, Pathology
Liang Wang, PhD, Structural Biology
Xiao Cui Wang, PhD, Structural Biology
Yan Wang, PhD, Immunology
Yaqiu Wang, PhD, Immunology
Abubakar Wani, PhD, Immunology
Grace Ward, PhD, Immunology
Meghan Ward, PhD, Bone Marrow Transplantation & Cellular Therapy
Megan Ware, PhD, Epidemiology & Cancer Control1
Zoe Watson, PhD, Structural Biology
Jayce Weesner, PhD, Genetics
Griffin Welfer, PhD, Structural Biology
Elizabeth Wickman, PhD, Bone Marrow Transplantation & Cellular Therapy
Kristin Wiggins, PhD, Surgery
Shyra Wilde, PhD, Host–Microbe Interactions
Andrew Willems, PhD, Computational Biology
Laura Wilt, PhD, Chemical Biology & Therapeutics2
Stephen Winston, PhD, Surgery
Tristen Wright, PhD, Developmental Neurobiology
Chengzhou Wu, PhD, Biostatistics
Jinjun Wu, Cell & Molecular Biology
Qiong Wu, PhD, Surgery2
Stephanie Wu, PhD, Developmental Neurobiology
Hui Xia, PhD, Immunology
Benjin Xu, PhD, Structural Biology
Lu Xu, PhD, Imaging Sciences
Lucy Xue, PhD, Host–Microbe Interactions
Chao Yang, PhD, Surgery
Jifeng Yang, PhD, Tumor Cell Biology
Jiyuan Yang, PhD, Computational Biology
Ke Yang, PhD, Hematology
Shu Yang, PhD, Structural Biology1
Zemin Yang, PhD, Scientific Director Office

Xiangyu Yao, PhD, Computational Biology
Jay Yarbro, PhD, Structural Biology
Rajesh Yetirajam, PhD, Pharmacy & Pharmaceutical Sciences
Siqi Yi, PhD, Hematology
Masanori Yoshida, MD, PhD, Hematology
Tomoko Yoshida, MD, PhD, Epidemiology & Cancer Control
Satoshi Yoshimura, PhD, Pharmacy & Pharmaceutical Sciences
Zhiyuan You, PhD, Immunology
Alexander Young, PhD, Immunology
Sarah Young, PhD, Chemical Biology & Therapeutics
Zehui Yu, DVM, Pharmacy & Pharmaceutical Sciences
Sujing Yuan, PhD, Immunology
Ugur Yurtsever, PhD, Cell & Molecular Biology Nan Zhang
Fatima Zaidi, PhD, Structural Biology
Nan Zhang, PhD, Structural Biology
Xiaohong Zhang, PhD, Immunology1
Xiaoyu Zhang, PhD, Immunology
Xue Zhang, PhD, Structural Biology
Yifan Zhang, PhD, Chemical Biology & Therapeutics
Yuhan Zhang, PhD, Structural Biology
Huanbin Zhao, PhD, Pharmacy & Pharmaceutical Sciences
Lanying Zhao, PhD, Hematology
Tuyu Zheng, PhD, Developmental Neurobiology
Immunocompromised Children & Adolescents Fellow
Lisa Hiskey, DO3
Infectious Diseases Fellows
Afreen Abraham, MBBS
Elspeth Bittle, MD
Sandra Castejon Ramirez, MD
Hayley Scheerer, MD
Kate Shapiro, MD
Neuropsychology Fellows
Lakia Kearson, PhD1
Bethany Schwandt, PhD
Alicia Travis
Ocular Oncology Fellow
William Evans, MD
Pediatric Hematology-Oncology Fellows
Margaret Cupit-Link, MD1
La’Ron Browne, MD
Stephanie Gehle, MD
Vidyasagar Jaiswal, MBBS, MPH1
Megan Lilley, MD
Ryan Lion, MD
Grace McKay-Corkum, MD
Margit Mikkelsen, MD
Bradley Muller, MD2
Sarah Mumanachit, MD
Devin Murphy, MD
Trisha Paul, MD
Katelyn Purvis, MD
Matthew Rees, MD3
Supriya Sarvode, MD3
Jasmine Smith, MD2
Alexandra Superdock, MD
Shruthi Suryaprakash, MD
Marleni Torres Nunez, MD
Pediatric Hematology-Oncology/ Adult Hematology Fellow
Tarun Aurora, MD1
Peipei Zhou, PhD, Immunology1
Qi Zhou, PhD, Surgery
Xuelin Zhou, PhD, Structural Biology
Changlei Zhu, PhD, Chemical Biology & Therapeutics
Hanwen Zhu, PhD, Structural Biology1
Jingwen Zhu, PhD, Pharmacy & Pharmaceutical Sciences
Mingrui Zhu, PhD, Computational Biology
Jaquelyn Zoine, PhD, Bone Marrow Transplantation & Cellular Therapy
Pediatric Surgery Oncology Fellows
Huma Faize Halepota, MBBS1
Zachary Morrison, MD
Pharmacy Infectious Diseases Fellow
Thanh Pham, PharmD1
Pharmacy Informatics Fellow
Nicholas Jantrakul, PharmD1
Pharmacy Oncology Fellows
Milre Matherne, PharmD4
Megan Wright, PharmD2
Pharmacogenomics Fellow
Kayla Thibodaux, PharmD1
Psychology Fellow
Emily Bernstein, MS1
Sickle Cell Disease Fellow
Khalid Elbashir, MBBS


St. Jude Graduate Students
Grace Adkins, Oncology
Korede Akindele, BH, Global Child Health
Victoria Akingbehin
Margaret Alexander
Khaled Al Habiba, RN, MSHA, Global Child Health
Zahangir Alom PhD, Clinical Investigations
Cassie Argenbright, PhD, Clinical Investigations
Tarun Aurora, MD, Clinical Investigations1
Tamar Bar Ziv
Ronnie Baticulon, MD, Global Child Health
Miguel Bayona, MD, MPPC, Global Child Health
Swarna Beesetti, PhD, Clinical Investigations
Bonn Belingon, Pharmacy & Pharmaceutical Sciences
Amy Berkman, MD, Clinical Investigations
Elspeth Bittle, MD, Clinical Investigations1
Mollie Black, Host–Microbe Interactions
Jordan Bondrowski
Alexandra Boyd, RN, Clinical Investigations
Jennyfer Bran, MD, Clinical Investigations
Joseph Brett, Structural Biology
Bailey Bridgers
Brett Brown
Kaitlin Budd, Developmental Neurobiology
Ashlyn Bugbee, Infectious Diseases
Taylor Bugbee, Developmental Neurobiology
Terri Cain, Oncology
Sandra Castejon Ramirez, MD, Clinical Investigations
Omar Chamdine, MD, Global Child Health
Jemma Clary
Sophie Cochiolo
Kristine Crews, PharmD, Clinical Investigations
Margaret Cupit-Link, MD, Clinical Investigations1
David Dachille, Immunology
Christina Daly, Cell & Molecular Biology4
Morgan Davis, Host–Microbe Interactions
Yogesh Dhungana, Computational Biology
Yuliana Diaz Tirado
Diana Dinh, Bone Marrow Transplantation & Cellular Therapy
Liezl Du Plessis, MD, MMD, Global Child Health1
Marygrace Duggar, Immunology
Christine Dunn, Host–Microbe Interactions
Angela Edwards, BHS, RT Clinical Investigations1
Mahmoud Elzembely, MD, Global Child Health
Nadine Emil
Mark Engelken
Rebecca Epperly, MD, Clinical Investigations1
Lauren Ezzell, Pathology
Mahwish Faizan, MBBS, Global Child Health
Arika Feils, Bone Marrow Transplantation & Cellular Therapy
Diego Figueredo, MD, Global Child Health
Abigail Fish, Chemical Biology & Therapeutics
Matthew Fisher
Teresa Fonseca, MD, MS, Global Child Health
Jake Friske, Tumor Cell Biology
Jessica Gaevert, Immunology
Lily Saladana Gallo, MD, Global Child Health1
Chelsea Goodenough, PhD, Clinical Investigations
Oliver Grants-Champman, Cell & Molecular Biology
Liam Hallada, Developmental Neurobiology4
Rawan Hammoud, MD, Clinical Investigations
Katie Han, Developmental Neurobiology
Lane Hartman
Sarah He
Blake Holcomb, Developmental Neurobiology
Job Huxford, Cell & Molecular Biology
Taiye Ibiyeye, MBBS, FMCS, FWACS, Global Child Health
Alissa Jackson, Hematology
Matthew Kieffer, Developmental Neurobiology
Sandra Kietlinska, Oncology
Aimee Kissou, MD, Global Child Health
Francine Kouya, MD, Global Child Health
Christy LaFlamme, Cell & Molecular Biology
Randolph Larsen, Oncology
Megan Lilley, MD, Clinical Investigations
Fuentes Lucia, MSc, Global Child Health
Zamokuhle Magagula, RN, BA, Global Child Health
JaQuel Maise, Oncology
Nidhi Mali, PhD, Clinical Investigations
Hayden Malone, Oncology
Milre Matherne, PharmD, Clinical Investigations
Aaron Mayo, Hematology
Ashton McKinnon, Infectious Diseases
Sanya Mehta, Bone Marrow Transplantation & Cellular Therapy
Vanessa Meza-Perez, Pharmacy & Pharmaceutical Sciences
Ramon Misla David, Center for Pediatric Neurological Disease Research
Erika Montalvo, MD, Global Child Health
Pablo Gonalez Montalvo, MD, Global Child Health1
Sarah Moore, Bone Marrow Transplantation & Cellular Therapy
Brendan Morrow, Host–Microbe Interactions
Mariam Ndagire, RN, Global Child Health1
Uma Neelakantan, Structural Biology
Adriana Ramirez Negron1
Amon Ngongola, MD, Global Child Health
Erienne Norton, Immunology
Hovaire Nsabimana, MD, Global Child Health1
Kiera O’Keefe, Hematology
Athena Olszewski, Center for Pediatric Neurological Diseases Research
Vivian Paintsil, MB, CHB, MSc, Global Child Health
Gabrielle Papp, Chemical Biology & Therapeutics
Claudia Pascual Morales, MD, Global Child Health1
Trevor Penix, Infectious Diseases
Nicolas Peterson, Immunology
Gregory Phelps, Chemical Biology & Therapeutics4
Soniya Pinto, MBBS, Clinical Investigations
Brittany Pioso, Structural Biology
Bilal Qureshi, MBBS, FCPS, Global Child Health1
Parul Rai, MD, Clinical Investigations
Revathi Rajagopal, MD, MMed, Global Child Health1
Auburn Ramsey
Isaiah Reeves, Surgery1
Logan Rice, Host–Microbe Interactions
Jordan Roach, Developmental Neurobiology
Lauren Rosenthal1
Samuel Rovito, Infectious Diseases
Kincaid Rowbotham, Structural Biology
Lauren Rowland, Infectious Diseases
Nihad Salifu, MBChB, Global Child Health
Austin Santhin, Infectious Diseases
Hayley Scheerer, MD, Clinical Investigations
Kate Shapiro, MD, Clinical Investigations
Sarah Sherman, Structural Biology
Jamaica Siwak, Cell & Molecular Biology
Jordan Skorupa, Oncology
Hannah Snoke, Chemical Biology & Therapeutics
Matthew So, Immunology
Bradley Stevens, Oncology
Morgan Sutton, Bone Marrow Transplantation & Cellular Therapy1
Shannon Sweeney, PhD, Clinical Investigations
Marta Zapata Tarres, MD, PhD Global Child Health
Robert Teis, Bone Marrow Transplantation & Cellular Therapy
Kim Hoa Nguyen Thi, MD, Global Child Health
Vinh Truong, Structural Biology
Sucharita Tuladhar, MD, MBBS, Global Child Health
Samantha Turk, Developmental Neurobiology
Carmen Uscatu, BSc, Global Child Health
Elena Valencia-Barbosa, Clinical Investigations
Holly Van Epps, Clinical Investigations
Dennis Voronin, Cell & Molecular Biology
Kyna Vuong, Oncology
Christina Wang, Cell & Molecular Biology
Nicholas Watkins, MD, Clinical Investigations
Kendall Whitt, Infectious Diseases
Elizabeth Wickman, Bone Marrow Transplantation & Cellular Therapy1
Kristin Wiggins, Infectious Diseases4
Benjamin Wilander, Immunology1
McLean Williamson, Hematology
Stephen Winston, Surgery1
Tristen Wright, Cell & Molecular Biology4
Milugeta Yimer, MD, Global Child Health1
Whitney Ziegenhorn, MD, Clinical Investigations
External Graduate Students
Osama Alaidi, Chemical Biology & Therapeutics
Amir Arabzade, Developmental Neurobiology4
Richard Begyinah, Chemical Biology & Therapeutics
Lauren Brakefield, Cell & Molecular Biology
Jingjing Chen, Hematology
Ashton Coker, Chemical Biology & Therapeutics
Andrew Cortes, Surgery
Erielle Culp, Computational Biology
Amy Davis, Infectious Diseases
Laura Doorley, Pharmacy & Pharmaceutical Sciences4
Ashley Gray, Pharmacy & Pharmaceutical Sciences
Ethan Hill, Diagnostic Imaging
Umamah Iram, Developmental Neurobiology
Alexander Jenner, Chemical Biology & Therapeutics
Menglin Jiang, Immunology4
Alisha Kardian, Developmental Neurobiology
William Kuenzinger, Developmental Neurobiology
Genevieve Lambert, Epidemiology & Cancer Control
Jimin Lee, Developmental Neurobiology
Song-Eun Lim, Computational Biology
Chun-Yang Lin, Immunology4
Michaela Meehl, Immunology
Joseph Miller, Pharmacy & Pharmaceutical Sciences
Kumar Niloy, Pharmacy & Pharmaceutical Sciences
Allison Norman, Immunology
Schyler Odum, Chemical Biology & Therapeutics
Homa Rezaei, Chemical Biology & Therapeutics
Christopher Rogers, Hematology
Dewan Shrestha, Hematology4
Utsav Shrestha, Diagnostic Imaging
Deryn St. James, Host–Microbe Interactions
Sadie Walker, Center for Advanced Genome Engineering
Jinjun Wu, Cell & Molecular Biology4
Zhen Xie, Computational Biology
Jingwen Zhu, Pharmacy & Pharmaceutical Sciences4



These volunteers served on the Board of Governors of St. Jude Children’s Research Hospital during 2024. Officers are indicated by the titles under their names.
Board of Governors
Joyce A. Aboussie
Steven J. Allen MD
Joseph S. Ayoub Jr.
Paul J. Ayoub
Frederick M. Azar, MD
Martha Perine Beard
Robert A. Breit, MD1
Terry L. Burman
Lisa R. Diller, MD
James R. Downing, MD2
St. Jude President and CEO
Joseph E. Eid, MD
John D. Farina Jr.3
Fred P. Gattas III, PharmD
Judy A. Habib
Chair
Gabriel G. Haddad, MD
Vice Chair
Charles C. Hajjar
Fouad M. Hajjar, MD
Frederick R. Harris Jr., MD
Secretary
Carla Z. Hassan3
J. David Karam II
Scott A. Kupor
Katherine N. Lapp3
Sharon L. McCollam
Samia Melhem
Robert T. Molinet
Neela M. Montgomery
Ramzi N. Nuwayhid
Thomas J. Penn III
Christina M. Rashid
Kathryne G. Reeves
Camille F. Sarrouf Jr.
Aarti S. Shah2
Richard C. Shadyac Jr.2
Joseph C. Shaker1
Joseph G. Shaker
George A. Simon II
Michael C. Simon
Tony Thomas
Paul H. Wein1
Tama H. Zaydon
Emeritus Members
Thomas G. Abraham
Susan Mack Aguillard, MD
Mahir R. Awdeh
James B. Barkate
Jack A. Belz4
Sheryl A. Bourisk
Stephen J. Camer, MD
Ann M. Danner
George Elias Jr.
Hasan M. Elkhatib
Fred P. Gattas Jr.
Ruth C. Gaviria
Christopher B. George, MD
Paul K. Hajar
Sam F. Hamra
Frederick R. Harris
Bruce B. Hopkins
Richard J. Karam
Salli E. LeVan
Paul J. Marcus
Michael D. McCoy
James O. Naifeh
Talat M. Othman4
Manal B. Saab
Frederick W. Smith4
Ronald A. Terry4
Terre Thomas
Pat Kerr Tigrett
Richard M. Unes
Thomas C. Wertz
Robert P. Younes, MD
Ramzi T. Younis, MD
Leah J. Domitrovic
Chief Governance Officer/ Corporate Secretary
James R. Downing, MD, Chair
President and Chief Executive Officer
Aseem Z. Ansari, PhD
Chair, Chemical Biology & Therapeutics
Gregory T. Armstrong, MD, MSCE
Chair, Epidemiology & Cancer Control Oncology
M. Madan Babu, PhD, FRSC
Director, Center of Excellence for Data Driven Discovery
Structural Biology
Suzanne J. Baker, PhD
Deputy Director of Strategic Initiatives, Comprehensive Cancer Center
Director, Division of Brain Tumor Research
Developmental Neurobiology
Shari M. Capers, MBA, MHA
Senior Vice President
Strategic Planning & Decision Support
Catherine I. Corbin, AIA
Senior Vice President
Chief Business Innovation Officer
John D. Crispino, PhD, MBA
Director, Division of Experimental Hematology Hematology
Sarah Currie, RNC, MSN, NEA-BC
Senior Vice President
Chief Nursing Executive
Andrew M. Davidoff, MD Chair, Surgery
Robyn Diaz, JD
Executive Vice President
Chief Legal Officer
Michael A. Dyer, PhD
Chair, Developmental Neurobiology
David W. Ellison, MD, PhD Chair, Pathology
Sarah M. Federico, MD
Director, Division of Solid Tumor Oncology
Richard S. Finkel, MD
Director, Center for Experimental Neurotherapeutics
Pediatric Medicine
Elizabeth Fox, MD, MS
Senior Vice President, Clinical Trials Research Oncology
Amar J. Gajjar, MD Chair, Pediatric Medicine
Terrence L. Geiger, MD, PhD
Senior Vice President
Deputy Director for Academic & Biomedical Operations
Interim Chair, Immunology Pathology
Stephen M. Gottschalk, MD Chair, Bone Marrow Transplantation & Cellular Therapy
Douglas R. Green, PhD Immunology
James M. Hoffman, PharmD
Senior Vice President, Quality and Safety
Chief Patient Safety Office
Pharmacy & Pharmaceutical Sciences
Melissa M. Hudson, MD
Director, Division of Cancer Survivorship
Oncology, Epidemiology & Cancer Control, Psychology & Biobehavioral Sciences
Charalampos G. Kalodimos, PhD
Chair, Structural Biology
Pat Keel, MHA
Executive Vice President
Chief Administrative & Financial Officer
Richard W. Kriwacki, PhD
Structural Biology
Kevin R. Krull, PhD Chair, Psychology & Biobehavioral Sciences
Mary E. (Beth) McCarville, MD1
Interim Chair, Diagnostic Imaging5
Chief, Clinical Radiation
Chief, Body Imaging Section
Jonathan A. McCullers, MD
Chair, Pediatrics, University of Tennessee Health Science Center
Pediatrician-in-Chief, Le Bonheur Children’s Hospital
Peter J. McKinnon, PhD
Director, Center for Neurological Disease Research
Vice Chair, Cell & Molecular Biology
Thomas E. Merchant, DO, PhD Chair, Radiation Oncology
Shondra Miller, PhD
Vice President, Cancer Center Shared Resources Cell & Molecular Biology
Motomi Mori, PhD, MBA Chair, Biostatistics
Charles G. Mullighan, MBBS(Hons), MSc, MD
Senior Deputy Director of Strategic Initiatives, Comprehensive Cancer Center Director, Center of Excellence for Leukemia Services
Pathology
Kirsten K. Ness, PT, PhD, FAPTA
Epidemiology & Cancer Control
Ellis J. Neufeld, MD, PhD
Executive Vice President
Clinical Director
Physician-in-Chief
Alberto S. Pappo, MD Oncology
Julie R. Park, MD
Chair, Oncology
Keith Perry, MBA
Senior Vice President
Chief Information Officer
Ching-Hon Pui, MD
Oncology
Octavio Ramilo, MD
Chair, Infectious Diseases
Charles W.M. Roberts, MD, PhD
Executive Vice President
Director, Comprehensive Cancer Center
Lori Spicer Robertson
Vice President
Carlos Rodriguez-Galindo, MD
Executive Vice President
Chair, Global Pediatric Medicine
Director, St. Jude Global
P. David Rogers, PharmD, PhD
Chair, Pharmacy & Pharmaceutical Sciences
Martine F. Roussel, PhD
Tumor Cell Biology
Charles J. Sherr, MD, PhD Chair, Tumor Cell Biology
Andrew D. Smith, MD, PhD
Chair, Diagnostic Imaging5
J. Paul Taylor, MD, PhD
Executive Vice President
Scientific Director
Chair, Cell & Molecular Biology
Director, Pediatric Translational Neuroscience Initiative
Victor J. Torres, PhD
Chair, Host–Microbe Interactions
Steven M. Varga, PhD
Chair and Dean, St. Jude Graduate School of Biomedical Sciences
Infectious Diseases
Mitchell J. Weiss, MD, PhD
Chair, Hematology
Jiyang Yu, PhD
Interim Chair, Computational Biology

This panel of physicians and scientists, serving during 2024, fostered the institution’s development through discussion with faculty members, reports to the Board of Governors, and advice to the President and CEO on scientific and clinical research directions.
John Maris, MD, Chair
Giulio D’Angio Chair in Neuroblastoma Research
Perelman School of Medicine at the University of Pennsylvania
Division of Oncology
Children’s Hospital of Philadelphia
Smita Bhatia, MD, MPH, Vice Chair
Gay and Bew White Endowed Chair in Pediatric Oncology
Distinguished Professor, Pediatric Oncology
Vice Chair for Outcomes Research, Department of Pediatrics
Director, Institute for Cancer Outcomes and Survivorship
University of Alabama at Birmingham School of Medicine
University of Alabama at Birmingham
Kevin Shannon, MD, Vice Chair
American Cancer Society
Research Professor
Roma and Marvin Auerback
Distinguished Professorship in Pediatric Molecular Oncology
University of California
– San Francisco
Helen Diller Family
Comprehensive Cancer Center
Susan Ackerman, PhD
HHMI Investigator
Stephen W. Kuffler Chair in Biology
Distinguished Professor, Departments of Neurobiology and Cellular and Molecular Medicine
University of California – San Diego
National Academy of Medicine
National Academy of Sciences
Scott Armstrong, MD, PhD
President, Dana-Farber/ Boston Children’s Cancer and Blood Disorders Center
Chair, Department of Pediatric Oncology
Associate Chief, Division of Hematology/Oncology, Boston Children’s Hospital
David G. Nathan Professor of Pediatrics, Harvard Medical School
Chief Research Strategy Officer
Senior Vice President for Drug Discovery
Dana-Farber Cancer Institute
National Academy of Medicine
Carsten Bönnemann, MD
Senior Investigator and Chief, Neuromuscular & Neurogenetic Diseases of Childhood
Acting Chief, Neurogenetics Branch
National Institute of Neurological Disorders and Stroke, National Institutes of Health
Adjunct Professor of Neurology, University of Pennsylvania Perelman School of Medicine
Michael Eck, MD, PhD
Professor of Biological Chemistry and Molecular Pharmacology, Harvard Medical School
Professor of Cancer Biology, Dana-Farber Cancer Institute
David Ginsburg, MD
James V. Neel Distinguished University Professor
Departments of Internal Medicine, Human Genetics, and Pediatrics University of Michigan Medical School
National Academy of Medicine
National Academy of Sciences
Nathanael Gray, PhD
Member, ChEM-H
Program Leader, Small Molecule Drug Discovery for the Innovative Medicines Accelerator
Co-Director, Cancer Drug Discovery
Co-Leader, Cancer Therapeutics Research Program
Krishnan-Shah Family Professor, Chemical and Systems Biology
Stanford University
Katherine High, MD
Emeritus Professor of Pediatrics, University of Pennsylvania Perelman School of Medicine
Visiting Professor, The Rockefeller University
National Academy of Medicine
National Academy of Sciences
Patrick Loehrer, MD
HH Gregg Professor of Oncology
Distinguished Professor
Indiana University School of Medicine
Sallie Permar, MD, PhD
Pediatrician-in-Chief, New York-Presbyterian/Weill Cornell Medical Center
Nancy C. Paduano
Professor and Chair
Professor of Immunology and Microbial Pathogenesis
Weill Cornell Medicine
Rob Pieters, MD, PhD, MSc
Board of Directors, Chief Medical Officer
Princess Maxima Center for Pediatric Oncology
Stanley Riddell, MD
Burke O’Reilly Family Endowed Chair in Immunotherapy
Professor, Department of Medicine
Fred Hutchinson Cancer Research Center
Kimberly Stegmaier, MD
Ted Williams Investigator, Dana-Farber Cancer Institute
Vice Chair of Pediatric Oncology
Research, Dana-Farber Institute
Co-Director, Pediatric Hematologic Malignancy Program, Boston
Children’s Hospital and DanaFarber Cancer Institute
Professor of Pediatrics, Harvard Medical School
Member, Broad Institute
Viviane Tabar, MD
Theresa C. Feng Professor in Neurosurgical Oncology
Chair, Department of Neurosurgery
Memorial Sloan Kettering Cancer Center
National Academy of Medicine
Sarah Teichmann, FMedSci FRS Professor
Wellcome – MRC Cambridge
Stem Cell Institute
Department of Medicine
University of Cambridge





1 Data represent the number of beds in use. St. Jude is licensed for 80 beds
2 Data include original data articles
3 Data include 59 full-time St. Jude fellows and 114 rotating fellows and residents from the University of Tennessee Health Science Center or other medical schools
4 Data represent the period July 1, 2022 to June 30, 2024
5 Average number of employees in 2024
Editorial Direction
Erin Podolak, MA
Jennifer L. Stripay, PhD
Creative Direction
Madison Newton-Rice, MS
Photography
Justin Veneman
Terrence L. Geiger, MD, PhD
Greg Armstrong, MD
M. Madan Babu, PhD, FRS
Scott Blanchard, PhD
Tara Brinkman, PhD
Hongbo Chi, PhD
Stephanie Dixon, MD
Matthew Ehrhardt, MD
Yong Feng, PhD
Aditya Gaur, MD
I-Chan Huang, PhD
Contributing Writers
Josh Dodson, PhD
LaToyia Downs, PhD
Matthew Gaschk
Alex Generous, PhD
Kathryn McCullough, MA
Brian O’Flynn, PhD
Jessica Rubino, PhD
Taylor Wewel
Lead Designer
Leena Xaypanya
Contributing Designers
Briana Williams
Rachel Byrd
Editing Support
Angela J. McArthur, PhD, ELS
Hiroto Inaba, MD, PhD
Jeffery Klco, MD, PhD
Xiaotu Ma, PhD
Stephen Mack, PhD
Charles, Mullighan, MBBS (Hons), MSc, MD
Kim Nichols, MD
Stacey Ogden, PhD
Ching-Hon Pui, MD
Charles Roberts, MD, PhD
Yadav Sapkota, PhD
Daniel Savic, PhD
Lindsay Schwarz, PhD
Akshay Sharma, MBBS
Andrew Smith, MD, PhD
Brandon Triplett, MD
Lu Wang, MD, PhD
Jun J. Yang, PhD
Benjamin Youngblood, PhD
Jiyang Yu, PhD
Caitlin Zebley, MD, PhD