


The City of Crest Hill and area residents gave Silver Cross Hospital a warm welcome at the ribbon-cutting and grand opening celebration of the hospital’s new Silver Cross Health Center | Urgent Care Center in the Crestlake Commons in June!
The location features the newest member of the hospital’s expansive ambulatory network and its 3rd Urgent Care Center – which includes urgent care for adults and children, ages 6 months and up, and X-ray services 7 days a week. Future plans include lab services, mammography and primary care.

Silver Cross Urgent Care in Crest Hill is located at 16127 S. Weber Road. It features 5 large exam rooms, a procedure room and on-site X-ray. Patients can schedule their visit online or walk in.
More than 200 community residents and local officials attended the ribbon-cutting.
“This brand-new facility features the third urgent care center we’ve opened in just five years,” Silver Cross President and Chief Executive Officer Michael Mutterer said. “Our other centers are located in New Lenox and Mokena, and from the day they opened, they’ve been very well-received – and very busy! Why? Because they answer a very important need: immediate, easy access to care when and where people need it most. Like our other centers, this new facility is staffed by highly trained advanced practice providers ready to provide care seven days a week, including evenings.”
Crest Hill Mayor Ray Soliman shared, “On behalf of the City of Crest Hill, we extend a very warm welcome to Silver Cross Hospital. We’re grateful to have a healthcare organization of your stature and national reputation right here to care for our residents and the residents of neighboring communities. And we hope this new facility is just the start of our partnership with you to bring truly exceptional healthcare close to home.”
Will County Executive Jennifer BertinoTarrant, who helped Silver Cross secure a valuable ARPA (American Rescue Plan Act) grant to help cover some of the costs of this project, added, “Your continued expansion demonstrates your dedication to all of us – whether we live in suburban, urban or rural Will County. Will County continues to grow, and more and more people are making our 32 communities their home. The need to continue to invest in accessible healthcare is greater now more than ever, not just with our growing population, but our aging population as well. Thank you, Silver Cross, for your support, your vision, your leadership and your staff for helping make Will County a better place to live.”
Rep. Natalie Manley, 98th District, and Sen. Meg Cappel, 49th District, also shared their congratulations and support of this important new addition, which will provide walk-in and urgent care for constituents in their respective districts.










•Back Pain
•Nausea












































Silver Cross Urgent Care in Mokena, New Lenox and Crest Hill is your choice for non-emergency situations. For life-threatening conditions, choose our Silver Cross Emergency Departments in New Lenox or Homer Glen. When an emergency happens, know where to go. Visit us at SilverCross.org/urgent-care
For more information or to make an appointment, scan the QR code.

• Minor Fractures
•S hort-term Vomiting and Diarrhea
•Minor Headaches
• Mild Injuries
•Cuts and Scrapes
•Mild Adult and Child Fevers
•Ear or Sinus Pain
•Cough or Sore Throat
•Minor Burns
•Animal Bites
•Stitches
•Sprains and Strains
•Mild Asthma
•Objects in Eyes or Nose
•Allergies
•Rashes
•Cold or Flu Symptoms
•Burning with Urination
•Eye Irritation
•Swelling or Pain
•Minor Allergic Reactions
•Work-related Injuries
The Midwest Institute for Neurosciences at Silver Cross Hospital is pleased to announce the arrival of Dr. Ravi Garg.
Dr. Garg specializes in neurology and neurocritical care. He earned his Doctor of Medicine degree from the Lewis Katz School of Medicine at Temple University and is board-certified in both Neurology and Neurocritical Care.
In addition to his clinical work, Dr. Garg holds a Master’s Degree in clinical research methods and epidemiology and is interested in improving health outcomes for patients through best evidencebased practices.
His office is located in Pavilion A, Suite 450, 1890 Silver Cross Blvd., New Lenox, on the campus of Silver Cross Hospital.
At the Midwest Institute for Neurosciences at Silver Cross Hospital, our goal is to make sure that you receive the right treatment at the right time for brain and spine care.
You’ll find highly trained experts that include board-certified neurologists, neurosurgeons, emergency medicine doctors, and physical medicine and rehabilitation specialists who can diagnose and treat all types of neurological conditions that include:
• Preventing strokes and halting them in their path.
• Diagnosing and treating neck and back injuries, brain tumors, cerebral vascular malformations, aneurysms and blockages in the arteries of the neck or carotid arteries.
• And providing the necessary rehabilitation.
You can feel confident you’ll get top-quality brain and spine care at The Neuroscience Institute at Silver Cross Hospital because we:
• Provide the very latest in stroke care, starting with a prompt diagnosis; clot-busting therapies; remote monitoring through our tele-stroke program; and minimally invasive neuroendovascular procedures.
• Offer the latest rehabilitation services through our partnership
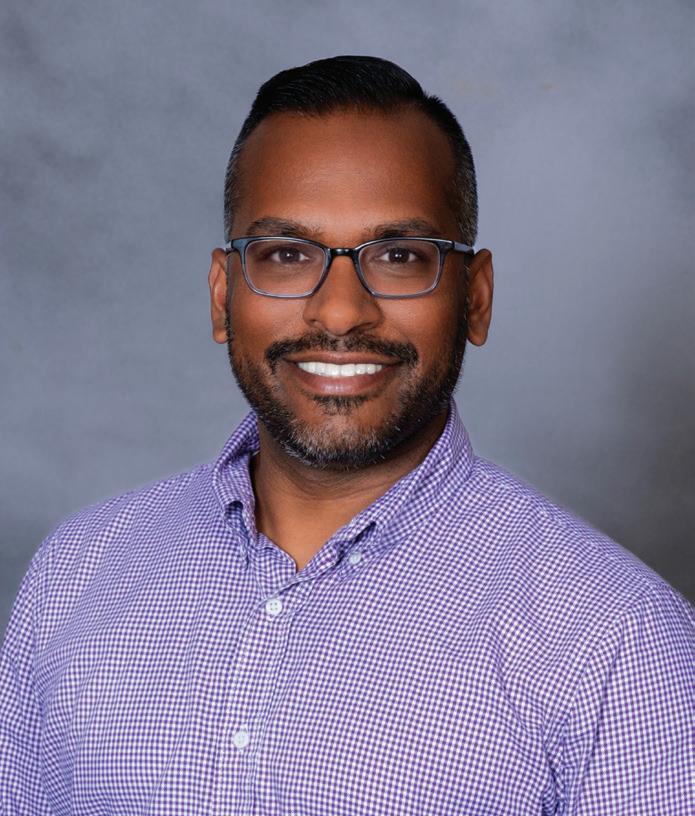
Ravi Garg, M.D.
with the Shirley Ryan AbilityLab —ranked the best rehabilitation hospital in the U.S. by U.S. News & World Report every year since 1991, allowing patients to recover close to home at Silver Cross Hospital.
• Are designated as a Primary Stroke Center by The Joint Commission and The American Heart Association/American Stroke Association.
• Received the American Heart/American Stroke Association’s Get with the Guidelines Stroke Silver Plus Quality Achievement Award.
• Recognized Blue Distinction Center for Spine Surgery by Blue Cross and Blue Shield of Illinois.
For more information about neurosciences at Silver Cross, visit silvercross.org. For a referral to Dr. Garg, call (815) 723-4387.



Sclerotherapy is a well-established, minimally invasive treatment commonly used to treat spider veins and small varicose veins. While often effective on its own, it can also serve as a complementary procedure to laser therapy, enhancing overall results for patients seeking both medical relief and cosmetic improvement.
The procedure involves injecting a specialized solution directly into the affected veins. This solution irritates the vein lining, causing it to collapse and eventually be reabsorbed by the body. Blood flow is naturally rerouted to healthier veins, improving circulation and reducing the visible appearance of unwanted veins. At Eterna MedSpa and Laser Vein Center, sclerotherapy is typically performed in an outpatient setting, requires no anesthesia, and involves minimal downtime.

When combined with treatments such as RFA (Radiofrequency Ablation), a minimally invasive technique which uses heat created by radiofrequency to shut down the vein and redirect the blood flow to the healthy veins.—sclerotherapy can be used to target the surface veins that remain after the deeper, underlying vein issues have been treated. RFA is highly effective for larger varicose veins caused by venous reflux, but it may not eliminate smaller surface veins. In these cases, sclerotherapy provides a valuable finishing touch to complete the treatment process and achieve more refined cosmetic results.
Patients may undergo sclerotherapy to improve skin appearance or reduce any residual discomfort caused by surface-level veins. The treatment is relatively quick, and most patients return to normal activities shortly afterward, although wearing compression stockings is often recommended to support healing and optimize results.
Understanding how sclerotherapy complements laser therapy helps patients make more informed decisions about their vein care. By addressing both the functional and aesthetic aspects of vein disease, this combination approach offers comprehensive and long-lasting results. Consulting with an experienced vein specialist at Eterna MedSpa and Laser Vein Center is essential to determine if sclerotherapy is the right option for your individual needs and how it fits into your overall vein treatment plan.









Even before you have all the details, just hearing the word “cancer” triggers fear and uncertainty... for you and your loved ones.
At Silver Cross Hospital, you’re never alone in your cancer journey. Our cancer experts are with you every step of the way. From diagnosis through treatment and beyond, we’re by your side. Answering questions. Discussing treatment options. And, most importantly, listening.
The UChicago Medicine Comprehensive Cancer Center at Silver Cross offers you access to one of the nation’s foremost cancer programs. In fact, UChicago Medicine is one of only two cancer centers in Illinois officially designated by the National Cancer Institute.
NCI designation is the gold standard for cancer programs and is bestowed upon the nation’s top cancer centers in recognition of their innovative research and leading-edge treatments. Because of our partnership with UChicago Medicine, you can receive most of those services right here in New Lenox!
We also collaborate with Rush University System for Health, bringing you the very latest in lung cancer surgery and treatment.
Through the Shirley Ryan AbilityLab at Silver Cross, you have access to comprehensive rehabilitation services, including lymphedema therapy to treat swelling in the extremities, which can result from cancer treatments including surgery and radiation.
Finally, for treatment of skin irritation or wounds that may result from radiation therapy, Silver Cross Wound Healing and Hyperbaric Medicine offers a variety of treatment modalities, including hyperbaric oxygen therapy that enhances the body’s natural ability to heal.

•Comprehensive care for adult cancers in one convenient location.
•Clinical trials and investigational therapies from the University of Chicago’s NCI-designated comprehensive cancer care team of over 150 clinical care specialists and subspecialists.
•Advanced treatment options, including chemotherapy, radiation therapy and stereotactic radiosurgery, which delivers high doses of radiation in a single session, or a few sessions, while minimizing damage to surrounding tissue.
•Supportive programs for patients and their families, including cancer support groups, preventive screenings and a comprehensive cancer resource center.
The University of Chicago Medicine Comprehensive Cancer Center at Silver Cross is pleased to announce Dr. Linda Chen, boardcertified radiation oncologist, is now providing expert radiation oncology services at the cancer center as the Medical Director of Radiation Oncology.
Dr. Chen, an Associate Professor of Radiation and Cellular Oncology, has an impressive background of treatment experience, clinical trials and research, and has brought it to Silver Cross. She earned her medical
degree at Duke University School of Medicine and performed her internship and residency training in radiation oncology at Johns Hopkins University.

Prior to her appointment at UChicago Medicine, Dr. Chen served as a Radiation Oncology attending physician at Memorial Sloan Kettering Cancer Center (MSKCC), where she developed clinical expertise in head
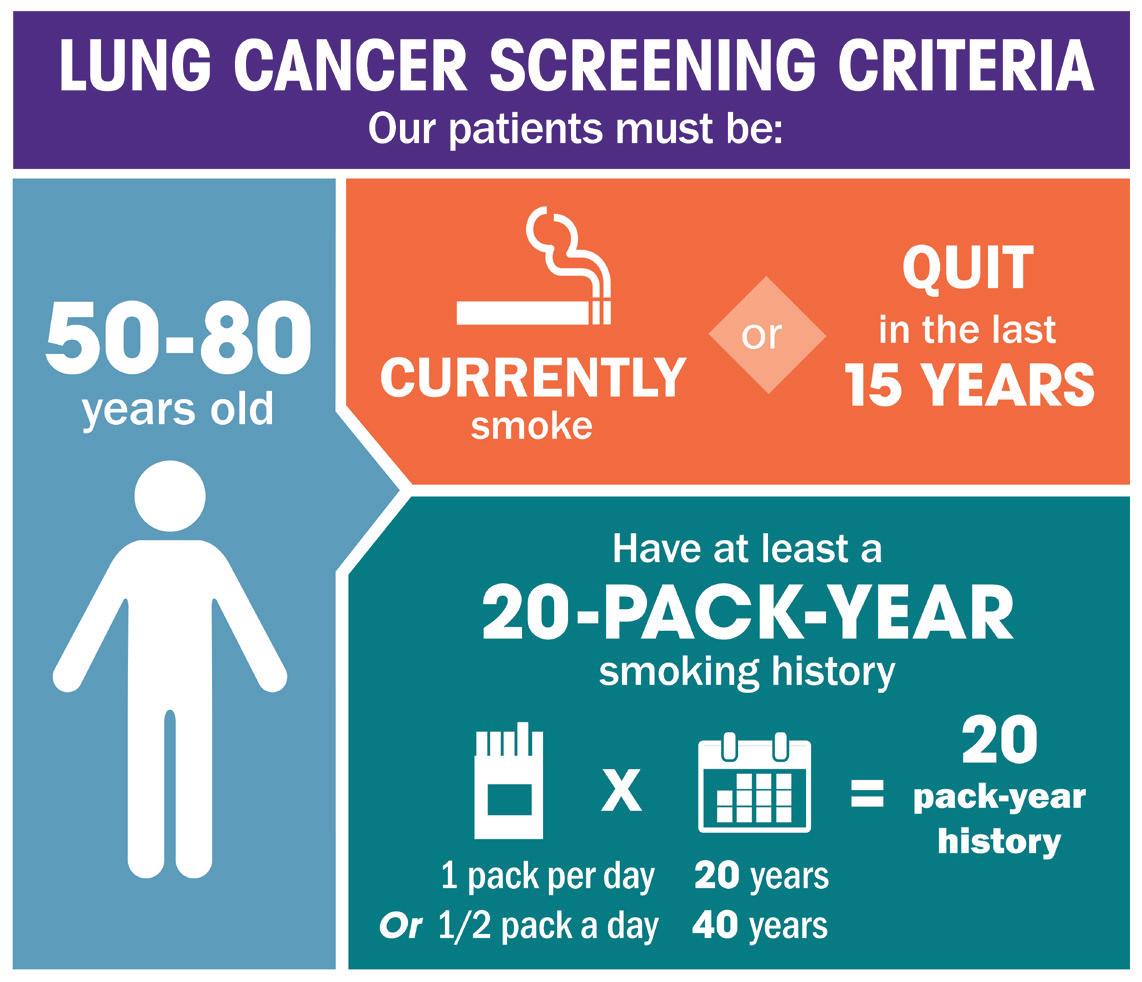
According to the American Lung Association, lung cancer is the leading cause of cancer death in the U.S. and remains a silent epidemic.
Lung Cancer Screening is a quick, painless, and non-invasive low-dose CT scan that we offer. The screening can detect nodules or spots on your lung that might be early indicators of lung cancer. It takes only a few minutes to have a scan which can potentially save your life.Low-Dose CT Lung Cancer Screening can reduce the lung cancer death rate by 20%. At this time, only low dose CT scans are recommended for screening; chest X-rays are not effective.
If you meet the following criteria and do not exhibit typical symptoms of lung cancer (i.e. cough, chest pain, weight loss) you maybe at high risk of getting lung cancer and are a candidate for this screening. For more information, call 815-300-LUNG.
and neck cancers as well as cancers affecting the brain and spine.
Dr. Chen was awarded a research grant from MSKCC’s Human Papilloma Virus Cancer Research Center and served as principal investigator or co-principal investigator in numerous clinical trials, including studies focused on HPV-related head and neck cancers, breast cancer/brain metastases, and skin cancer. She has also authored or coauthored dozens of research papers and publications.

silvercross.org/cancer

Cancer is a prolific group of diseases that affects millions of people across the globe. The American Cancer Society indicates that approximately 20 million cancer cases were newly diagnosed, and 9.7 million people died from the disease worldwide in 2022.
The day a patient’s successful cancer treatment ends is a cause for celebration, but the happiness that comes from a clean bill of health can soon be overshadowed by anxiety regarding what the future may bring. Many cancer survivors wonder what happens if the cancer comes back. These tips can help guide cancer survivors looking to protect their long-term health and overall well-being as they seek to reclaim their lives.
It’s time to kick the tobacco habit. The Mayo Clinic warns that smoking or using chewing tobacco puts people at risk for several types of cancer. Quitting also lowers the risk of developing a second type of cancer. Smoking causes significant damage to the heart and blood vessels, increasing the risk of heart disease.
Smoking impairs the body’s immune system, making smokers more susceptible to infection. Quitting and avoiding secondhand smoke is instrumental to better health and longevity.
Regular physical activity improves overall health for everyone, including cancer survivors. Exercise boosts energy and mobility and strengthens the immune system. Research suggests exercise is a natural way to boost the body’s immune responses to reduce inflammation and vulnerability to illness.
A gradual buildup of exercise tolerance helps people avoid injuries that can derail workout plans. The goal is to do 30 minutes or more of daily activity, plus strength activities two or more times a week, according to Siteman Cancer Center.
Always consume alcohol in moderation, if at all. That means no more than one drink a day for women, and no more than two for men. The Mayo Clinic notes it’s hard to definitively say alcohol consumption causes cancer recurrence, but it can increase the risk of a second primary cancer.
A healthy diet for cancer survivors prioritizes consumption of fruits, vegetables, whole grains, beans, and healthy fats, like olive oil. Protein sources should be lean, and consumption of red meat, processed foods, and full-fat dairy should be limited. Avoid processed meats. According to the World Health Organization, the link between processed meats and cancer has been strongly established. Eating a healthy diet helps to control body weight, which also is an important step to maintaining health.
Prioritizing mental health is also important. Cancer survivors may need a little extra help working through their feelings, and utilizing a mental health professional can help.
Surviving cancer is a monumental achievement. Remaining healthy after successful treatment requires commitment and a new approach to daily living.
It should come as no surprise that the weight we carry on our bodies impacts our hip and knee joints. In fact, the forces experienced across the joint surfaces inside our hips and knees can be the equivalent of more than seven times our body weight, according to the American Academy of Orthopaedic Surgeons.
Studies have also shown that approximately 30% of obese patients will require knee replacement surgery in their lifetime. This is why individuals needing a hip or knee replacement are sometimes told they need to lose weight before proceeding with surgery. Instead of expecting patients to lose weight on their own, the orthopedic surgeons with Morris Hospital Orthopedics & Sports Medicine are referring patients to a new orthopedic weight loss program that was created in collaboration with the Morris Hospital YMCA. Called Joint Effort, the 12week program is for individuals with a Body Mass Index (BMI) over 30 who have been advised to lose weight in order to become eligible for hip or knee replacement surgery.
BMI is the ratio that compares a person’s weight to their height. While a BMI of 25-29.9 is considered overweight, a BMI of 30 or above falls into the obesity classification.
Lacey Carls, a certified physician assistant with Morris Hospital Orthopedics & Sports Medicine, shares more about the program:
What inspired Morris Hospital to launch the Joint Effort program?
Lacey: In orthopedics, we see many patients whose mobility is limited by joint pain. This often keeps them from being active and living a healthier lifestyle. Part of my role as a physician assistant is to see surgical patients pre-operatively and assess if they are ready for surgery. Unfortunately, there are times when you have to tell a patient that they are not approved for surgery until they achieve weight loss. This can be a difficult conversation because many patients are having surgery due to chronic pain, limited mobility, and an impacted overall quality of life. I explain to them the elevated risks to
having the surgery with the excess weight and help them understand the importance of losing weight as part of their health journey. We created the Joint Effort program in collaboration with the Morris Hospital YMCA to further support our patients by helping them lose weight in a healthy way while also teaching skills they can use after their joint replacement. Our goal is to be a true partner in each patient’s health journey. Instead of simply telling someone we cannot proceed with surgery due to their weight, we offer this program as a solution to help them lower their BMI and move forward with their care.
How does the Joint Effort program work?
Lacey: Joint Effort is a guided, 12-week orthopedic weight loss program for people preparing for joint replacement surgery. It’s led by a dedicated team of wellness professionals from Morris Hospital and the Morris Hospital YMCA and combines lowimpact exercise, nutrition education, and personalized support. The goal is to help patients lose weight safely and improve their joint health and overall well-being. With a focus on both physical activity and nutrition, Joint Effort supports patients in achieving sustainable, health-focused weight loss while improving their mobility and quality of life. Specifically the program includes:
• A 3-month facility membership to the Morris Hospital YMCA
• A personal fitness orientation to help navigate the YMCA wellness center
• Weekly water fitness classes designed to be gentle on joints
• Weekly support group sessions for motivation and accountability
• Monthly check-ins with the Morris Hospital Wellness Manager for progress tracking and weigh-ins
Who is eligible to participate?
Lacey: Participants must be referred to the program by a Morris Hospital orthopedic

Morris Hospital Orthopedic Surgeon Ahmed Eldib, M.D., and Wellness Manager Becca Evola are helping patients prepare for hip and knee replacement surgery through a new orthopedic weight loss program developed in collaboration with the Morris Hospital YMCA
surgeon. The program is currently accepting hip and knee replacement patients, with a goal of expanding the program in the future to include spine surgeries.
For individuals living with joint pain, Morris Hospital Orthopedics & Sports Medicine is here to help, with a goal of supporting patients through every phase of their joint health journey. By combining expert surgical care with programs like Joint Effort, the team at Morris Hospital Orthopedics & Sports Medicine is committed to helping individuals achieve better outcomes, regain mobility, and improve their overall quality of life. To schedule an appointment with a Morris Hospital orthopedic surgeon, call 815-9424875. Offices are located in Morris, Joliet, Diamond and Ottawa.

Most people expect to undergo rehabilitation after a surgical procedure, injury, or stroke. What’s not as commonly know is that a number of medical conditions can benefit from a round of physical, occupational or speech therapy, or a combination of the three. With six locations, Morris Hospital’s Rehabilitation Services is here to help.
What’s the difference between PT, OT and Speech?
In general, physical therapy (PT) can help improve physical limitations caused by a variety of medical problems, with a goal of helping patients return to work, activities and hobbies. Occupational therapy (OT), on the other hand, focuses more on improving safety and independence in everyday living activities.
Speech therapy involves evaluations and treatment of swallowing disorders, cognitive disorders, and speech/language and voice problems resulting from strokes, head injuries, respiratory issues, and other medical complications.
Before a patient gets started, the Rehabilitation Services team at Morris Hospital conducts an evaluation to help identify the right treatment and plan of care depending on the patient’s specific needs.
How do I know if rehab services can help me?
If you are struggling with any of the following conditions, there’s a good chance you might benefit from physical, occupational or speech therapy:
• Pain
• Falls
• Recovery from an orthopedic injury or surgery
• Walking or moving around
• Performing activities that you previously

enjoyed because of weakness or fatigue
• Performing daily tasks such as getting dressed, cooking or bathing
• Using your hands when writing, keyboarding, or opening jars
• Bladder or bowel control
• Pelvic pain
• Vocal loudness or sound quality
• Speaking or understanding speech
• Difficulty or pain when chewing or swallowing
• Coughing or choking when eating food or drinking liquids
• Memory
In addition, Morris Hospital offers specialized Rehabilitation Services for:
Parkinson’s disease – Morris Hospital has therapists who are specially certified in Lee Silverman Voice Treatment (LSVT), which includes LSVT Loud speech therapy and LSVT Big physical therapy for fine and gross motor skills. The intense, four-week program helps to “re-wire” the brain so actions are performed with purpose and drive.
Concussion symptoms – Concussion is a type of traumatic brain injury that may require specialized treatment to heal properly. As
part of the Concussion Management team, Morris Hospital physical therapists help individuals suffering from concussion who are experiencing visual problems, balance or vestibular issues, or even cervical spine deficits.
Dizziness or balance problems – If you have a vestibular condition that causes dizziness, room spinning, nausea, or feeling off balance, a specialized physical therapy program may help improve the debilitating symptoms that interfere with day-to-day activities.
Pelvic health concerns – When you’re dealing with issues like bladder leaks, pelvic pain or core weakness, pelvic floor physical therapy can be life-changing. Specially trained physical therapists from Morris Hospital treat the root cause to help women get back to living confidently and comfortably.
Lymphedema – Lymphedema is a chronic, often progressive condition that can cause swelling of the head, arm, leg and/or trunk due to disruption of the lymphatic system. The condition is most effectively managed with a combination of treatments known collectively as Complete Decongestive Therapy that involves specialized lymphatic massage, compression, exercise and skin care.
Morris Hospital offers rehabilitation services at locations in Channahon, Diamond, Joliet, Morris and Ottawa. Services may vary by location. Ask your provider for a referral, or call 815-705-7828 and a patient service representative will assist you with the process.
For more information, visit morrishospital.org/ rehabservices.

Receiving a diagnosis of “heart failure” can be daunting. Not to mention scary. After all, those two words make it sound like the heart isn’t working anymore. Fortunately that’s not the case; however, a diagnosis of heart failure does mean that the heart no longer has the ability to adequately pump blood throughout the body.
And when that happens, all kinds of complications and difficulties can occur, making heart failure a complex and serious condition that results in frequent hospitalizations according to Sherese Pruss, Nurse Practitioner with Morris Hospital Cardiovascular Specialists.
While the heart and other parts of the body try to compensate when the heart fails to pump properly, eventually a person with heart failure tends to experience classic signs that indicate something is not right with the heart, including:
• Shortness of breath
• Persistent coughing or wheezing
• Swelling in the legs, feet, ankles, fingers, abdomen or other tissues and organs
• Weight loss or gain
• Fatigue that makes everyday activities difficult
• Lack of appetite or nausea
• Confusion or impaired thinking
• Increased heart rate or racing heart
“It’s really important to manage heart failure symptoms, and a lot of that falls on the patient,” says Pruss. “It starts with being aware of your body and how it’s working and monitoring your symptoms.”
As part of symptom management, individuals with heart failure are typically advised to weigh themselves every day.
“If a person with heart failure experiences rapid weight gain, that could be indicative that there are some issues related to the

Morris Hospital Cardiovascular Specialists Nurse Practitioner Sherese Pruss counsels a patient through the Heart Failure Management Program.
heart failure,” explains Pruss. “We also tell our heart failure patients to watch the salt intake in their diet. When someone with heart failure consumes a high salt diet, they tend to retain more fluids.”
Staying active is also important in managing heart failure symptoms.
“I always tell our patients, the heart is a muscle, and if you don’t use it you lose it,” says Pruss. “Trying to stay active and getting some daily exercise – such as walking every day -- helps keep your heart conditioned and helps with symptom management.
Morris Hospital Cardiovascular Specialists is working to improve heart failure symptom management and reduce hospitalizations through a special Heart Failure Management Program. The program was developed with the primary goal of providing specialized care and support for patients living with heart failure, with a key focus on reducing 30-day readmissions, preventing future hospitalizations, and enhancing overall patient outcomes by managing patients in an outpatient setting.
The ultimate goal is to improve outcomes for patients who have a heart failure diagnosis by being proactive about managing their condition. Through regularly scheduled office visits, the cardiology team with Morris Hospital Cardiovascular Specialists will review patient medications, provide education and resources specific to diet including dietitian consults, refer patients to cardiac rehab when indicated, and advise patients to promptly report any changes that could indicate a decline in their condition. Seeing patients with a heart failure diagnosis on a regular basis gives the Heart Failure Management Program team better ability to intervene before patients get to the point of needing hospitalization.
For more information about the Heart Failure Management Program at Morris Hospital, call Morris Hospital Cardiovascular Specialists at 815-705-1000. Or, ask your primary care physician for a referral to the program.



Are you experiencing:
• Abdominal pain and discomfort
• Heartburn or acid reflux
• Bloating or excess gas
• Constipation or diarrhea
• Hemorrhoids
• Change in bowel movements
These are signs that it may be time to see a Gastroenterologist.


Board-certified Gastroenterologist Afreen Hyder, M.D., is experienced in diagnosing and treating GI conditions related to your digestive system.
Whether you are experiencing symptoms or have a family history of gastrointestinal issues, Dr. Hyder offers compassionate, specialized care you can trust.
To schedule an appointment, call 815-941-9320.