SAN FRANCISCO MARIN MEDICINE
JOURNAL OF THE SAN FRANCISCO MARIN MEDICAL SOCIETY

Local And State Policy Updates / Physician Wellness Healthcare As A Right
SPECIAL SECTION: Medical Aid in Dying Update


Local And State Policy Updates / Physician Wellness Healthcare As A Right
SPECIAL SECTION: Medical Aid in Dying Update
Heyman
Lonny
SFMMS Interview With David Smith, MD: "Healthcare Is a Right, Not a Privilege" Steve Heilig, MPH 20 How Are Federal Cuts Going to Impact Your Healthcare? As a Doctor, I'm Not Going to Sugarcoat it.
Gerald Hsu, MD
Geriatrics: A Rising Priority for Physicians Across All Specialties
Marek Brzezinski, MD, PhD, FASA and Jasleen Kukreja, MD, MPH 23 SFMMS Members Bring Their Message to Sacramento
Adam Francis, CAE
April/May/June 2025
Volume 98, Number 2
Membership Matters
President's Message Jason Nau, MD
Executive Memo: The Expertise of Physicians Is a Cure for Political Polarization
Amenta
24 You Don't Need Another Lecture On Self-Care. You Need to Do Things That Make You Feel Cared For.
Jessie Mahoney, MD
Sarita Satpathy, MD
CMA Federal Alert: Medicaid Still on the Chopping Block - Join the Texting Campaign!
US House Republicans have advanced a bill that would slash Medicaid by over $700 billion—threatening coverage for millions, including 3.4 million Californians, while cutting provider payments and destabilizing state health systems. In response, CMA and all 49 state medical associations launched Physicians for Medicaid to urge Congress to reject these devastating cuts. If you haven’t yet, send a message to your members of Congress – and share our graphics and videos on social media.
Thanks to support from Kaiser Permanente, CMA and the Protect Our Health Care Coalition have also launched a national voter-to-voter texting campaign. Physicians have already sent over a million texts, but with the bill now in the Senate, your voice is more important than ever. Join the texting campaign today and make your voice heard before it’s too late. See: Protectourhealth.org
Speaker Emeritus Nancy Pelosi Quotes CMA on The US House of Representatives Floor:
Mr. Speaker, the California Medical Association President issued the following statement regarding House Republicans’ proposed care cuts in Medicaid:
‘The latest federal proposal to gut Medicaid is reckless. Physicians and hospitals will be pushed to the brink, forced to close their doors and unable to continue care for their patients.’'These would be the largest Medicaid cuts in history and will leave veterans, seniors, the disabled, children and working families without health care coverage.'…. 'Congress must reject these cuts and instead focus on strengthening the safety net that protects us all. Otherwise, at least 13.7 million people will lose health care coverage.'
SFMMS Leaders Attend Mayor Lurie & Supervisor Dorsey’s Signing of Recovery First Legislation

SFMMS Leaders, Drs. John Maa, Jason Nau, Anthony DiGiorgio, Heyman Oo, and Christina Wang with San Francisco Mayor Daniel

SFMMS President-Elect, Dr. Sarita Satpathy speaks at the SF Wear Orange Gun Violence Awareness Rally.
SFMMS Sponsors Northern California Planned Parenthood Acts of Courage 2025 Event
SFMMS Community Foundation supports community health partners such as Planned Parenthood with donations and sponsorship. On May 30, 2025 SFMMS was a sponsor of the Planned Parenthood Acts of Courage 2025 event.
Jodi Hicks, the President and CEO of Planned Parenthood Affiliates of California, lamented the Dobbs decision and the current climate for reproductive health and rights. She gave an Acts of Courage Award to Gilda Gonzales, the current President and CEO of Northern California Planned Parenthood, who is stepping down. Ms. Gonzales focused on resilience, expansion of services, gender affirmation care, service to the undocumented and working with local and state politicians. She urged the audience to resist attempts to defund Planned Parenthood nationally and protect reproductive freedom.
SFMMS was represented by Board members Dr. Melinda Aquino, Dr. Dawn Rosenberg, and Dr. Michael Schrader. There is a current proposal within SFMMS to enhance our support for community health groups by forming a Community Health Committee.
April/May/June 2025
Volume 98, Number 2
Editor Michael Schrader, MD, PhD
Managing Editor Steve Heilig, MPH
Production Maureen Erwin
SFMMS OFFICERS
President Jason Nau, MD , MD, DDS
President-Elect Sarita Satpathy, MD
Secretary Ian McLachlan, MD
Treasurer Sarita Satpathy, MD
Immediate Past President Dennis Song, MD, DDS
SFMMS STAFF
Executive Director
Conrad Amenta
Associate Executive Director, Public Health and Education
Steve Heilig, MPH
Director of Operations and Governance
Ian Knox
Director of Engagement
Molly Baldridge, MPH
Senior Director, Advocacy and Policy
Adam Francis, CAE
2024 SFMMS BOARD OF DIRECTORS
Edward Alfrey, MD
Melinda Aquino, MD
Julie Bokser, MD
Kristina Casadei, MD
Clifford Chew, MD
Esme Cullen, MD
Anthony DiGiorgio. MD
Manal Elkarra, MD
Mihal Emberton, MD
Cindy Greenberg, MD
Tracey Hessel, MD
Cynthia Lin, MD
Ian McLachlan, MD, Treasurer
Jason Nau, MD, President
David Pating, MD
Dawn Rosenberg, MD
Sarita Satpathy, MD, President-Elect
Michael Schrader, MD, Editor
Yalda Shahram, MD
Neeru Singh, MD
Dennis Song, MD, DDS, Immediate Past-President
Ranna Tabrizi, MD
Kenneth Tai, MD
Melanie Thompson, DO, Secretary
Christina Wang, MD
Kristin Wong, MD
Andrea Yeung, MD
Helen Yu, MD
For questions regarding journal, including possible submissions, contact Steve Heilig: Heilig@sfmms.org
Jason Nau, MD
In April, the RAND Corporation released its report, Strategies for Sustaining Emergency Care in the United States Much like patients scrutinizing their own diagnostic test results, I read it closely, curious to see how its findings aligned with my own experience. After 26 years at Kaiser Permanente, I’ve begun to wonder: how typical is our emergency department? According to the report, while every shop has its quirks, we’re all straining under the same pressures.
Emergency Departments (EDs) are society’s diagnostic black box, the healthcare system’s safety net, and medicine’s front line. We are where the undifferentiated patient meets the undaunted physician—where chaos meets calm, with a splash of caffeine. No one is turned away. And yet, despite this vital role, emergency medicine is under siege.
Visits have rebounded to near pre-pandemic levels, but patients are sicker, more complex, and harder to disposition. Meanwhile, resources are dwindling, and financial challenges are multiplying. As the report emphasizes, EDs—often the only 24/7 option for unscheduled acute care regardless of insurance status—are dangerously strained.
Rising acuity, growing demand, and insufficient capacity have led to worsening crowding, extended wait times, and increased safety risks for patients and staff. These stresses are driving physician burnout and attrition. At the same time, EDs are doing more: managing geriatric care, coordinating follow-up, absorbing mental health system failures—all while being paid less.
Thanks to EMTALA, the ED is open to all—insured, uninsured, undocumented, or just out of options. When the PCP can’t see you for three weeks, when the specialist says, “go to the ER,” or when Grandma feels funny at 3 AM, we are there. EDs offer 24/7 access to advanced diagnostics, acute treatments, and often, crucial social support.
Our value extends beyond individual patients. EDs care for the unhoused, veterans, frail older adults, and people at the edges of society. We’re frontline responders to the opioid crisis, gun violence, and mental health emergencies. We’re essential infrastructure in public health crises—Ebola, COVID, and mass casualty events.
For the broader healthcare system, EDs provide access, triage, and continuity. We keep the wheels turning, make real-time decisions about inpatient admissions, and innovate constantly to improve flow, reduce crowding, and improve outcomes. For payers, we deliver cost savings by treating and safely discharging many who would otherwise be admitted.
Emergency medicine is the shock absorber of a fragile system—and increasingly, the glue holding it together.

Despite all this, we’re in crisis. Patient acuity is up, and we now routinely manage cognitive decline, trauma, addiction, and homelessness. Payments, however, are falling: from 2018 to 2022, emergency physician reimbursements declined 3.8% (Medicare/ Medicaid), 10.9% (in-network commercial), and a staggering 47.7% (out-of-network commercial). Unpaid claims total nearly $6 billion annually. Financial viability is slipping away.
And then there’s boarding : the accumulation of admitted patients stuck in the ED for hours or days, waiting for inpatient beds. It’s the root cause of crowding, delays, poor outcomes, and even violence toward staff. Boarding is not an emergency department problem—it’s a system failure. When hospitals hold empty beds or can’t discharge in a timely way, EDs become makeshift wards. Everyone suffers.
Physicians, drowning in complexity and short-staffed hallways, are burning out and leaving. We’re losing experienced doctors faster than we can train their replacements.
If we don’t act, the model collapses. Independent ED groups are folding or being absorbed into hospital systems. Burnout is rampant. Medical students are turning away from the specialty. The pipeline is narrowing.
What happens if we lose emergency medicine? The consequences are dire. When EDs close, mortality rises, wait times balloon, and the strain on nearby hospitals becomes unbearable. Communities lose critical access. The system grows brittle.
We could face a patchwork of overworked midlevel providers managing critical cases in hallways, with no physician oversight and no margin for error.
Solutions: Pay Fairly, End Boarding, Protect the
So how do we preserve this beautiful, dysfunctional miracle? How do we keep emergency medicine sustainable, physician-led, and high-quality? RAND’s recommendations, along with our own experience, suggest a clear path forward:
• Fight for Fair Payment: Advocate for Medicaid expansion and parity with Medicare. Push for emergency physicians to receive a fair share of facility fees. Demand federal and state support for EMTALA compliance. It’s absurd to mandate 24/7 access but refuse to pay for the cost to keep the doors open.
• Crush Boarding: Implement full-capacity protocols, distribute admitted patients throughout the hospital, and smooth elective admissions. Partner with post-acute facilities and increase capacity at inpatient psychiatric facilities,
continued on page 8
As we celebrate the 250th anniversary of the American Revolution I have been thinking about the heroism of the people who fought for our country against unjust governance They risked everything to create the values and rights we hold today.
Recently we have seen the Trump administration threaten to revoke accreditation of medical schools and graduate medical education programs over use of diversity, equity and inclusion (DEI) measures in selecting candidates for medical school and residency, respectively. In addition, some of our medical journals have received notices that they must publish research driven by political agendas rather than fact-based medical research. And the vaccine industry has been given notice that the federal government will place an onerous regulatory burden on mRNA technology.
Equality is a key value expressed in our Declaration of Independence. June is Pride Month where San Francisco and the rest of the country celebrate diversity. Baron von Steuben who drilled our Continental Army at Valley Forge was an openly gay man. Without his preparation we would have lost the pivotal Battle of Monmouth Courthouse.
DEI has accepted benefits for our profession and our patients. Our profession and our country have long struggled with the legacy of racism and sexism that have given the privileged class of white men unfair advantage in advancement and earning. If anything this is anti-meritocratic. Our patients are diverse and we are diverse.
Freedom of the press is one of our core rights protected by the First Amendment along with freedom of speech, the right to assemble peaceably, and freedom of worship. The basis for this was the prosecution of John Peter Zenger, a printer, prior to the American Revolution who was sued for libel for criticizing the Royal Governor of New York. Diversity of opinion, reasonable discourse, and, propagation of ideas are a tenet in America. Censorship precludes the dissemination of knowledge, ideas and opinions.
Vaccination has always been controversial. It requires cooperation to achieve herd immunity and prevention of communicable disease. General George Washington required his troops to be vaccinated against smallpox during the American Revolution because losing his soldiers to disease could cost him victory and the freedoms he and his patriots desired. As we physicians
Michael Schrader, MD, PhD
know, there is no conquering of infectious disease. Our recent Covid epidemic and ongoing endemic cases serve as a warning that we must be vigilant and prepared. Vaccines and induced immunity are a bulwark of community health.
So in these three instances of federal policy we see deliberate wrongheadedness to cause trepidation in our medical training, inhibit dissemination of medical knowledge, and obstruct the use of the latest medical technology. The threat of censorship becomes intimidation. Already I have heard warnings that SFMMS should be careful and avoid any possible scrutiny from the federal government. And that our scope should not reach beyond the borders of our two counties.
This may be a strategy that other groups in organized medicine use but not SFMMS. We do not receive federal funding so we do not need to fear cuts or recision of funds. Our patients and our members are dependent on federal policy for their lives and livelihoods respectively—national decisions affect our lives. And the ethos of SFMMS is not to remain silent and not fight back. We have impacted state and national policy about smoking and vaping, firearms, reproductive health, sugary beverages, treatment of detained migrant children seeking asylum, and many other issues.
Equality, freedom of expression, and acceptance of the benefits of scientific ideas were key components of the American Revolution. The documents and attitudes and resilience of the American patriots made the United States what it is today. Physicians were heroes of the American Revolution including Drs. Joseph Warren, Samuel Prescott, Benjamin Rush, Benjamin Church (complicated legacy) and many others. Our profession has always produced trusted leaders. We will not let ourselves be intimidated by tyrants.

Dr. Schrader, an internist at Dignity Health, is Chair of the SFMMS delegation to the CMA and a past-president of the SFMMS.
Conrad Amenta, SFMMS Executive Director
Politics in San Francisco and Marin Counties is often the product of dialogue between entrenched interests Coalitions of advocacy groups who might otherwise share a long-term goal will disagree on the best path to achieve it, and, over time, their preferences harden into ideologies. We see this playing out again and again, whether the issue be ensuring adequate housing, reducing food insecurity, eliminating gun violence, or providing pathways out of addiction. These are complex policy issues, and finding a balance of approaches can be difficult in the supercharged environment of local politics.
I was recently reminded of the power of the physician’s expertise to carve new paths through inflexible ideology. In April 2025, the San Francisco Marin Medical Society was asked to take a position on a San Francisco ordinance proposed by Supervisor Matt Dorsey. This ordinance was an aspirational policy outlining the city’s approach to drug-addiction recovery. The dialogue around this ordinance seemingly pitted advocates for harm reduction against advocates for an “abstinence-first” approach.
As the debate played out, terminology like “recovery” was co-opted by all sides, and emptied of its meaning as defined in medical evidence. SFMMS was asked to take sides in a deliberation that was becoming increasingly charged and political, to participate in a zero sum proposition.
It’s important to point out the best intentions of everyone in this vital debate. San Francisco continues to face intractable suffering at the intersection of addiction, behavioral health, health equity, and housing. All involved wish to reduce the suffering of some of the most vulnerable members of our community. Despite these good intentions, the different sides were talking past one another.

SFMMS offered to support the ordinance if its authors accepted amendments, including introducing the term “Remission,” which means overcoming the illness of substance use disorder to the point of living a self-directed and healthy life, free from illicit drug use. This amendment, seemingly small, reoriented the thrust of the policy away from tactics and toward outcomes, while injecting nuance to a debate that had become intractable and de-emphasizing terms that had become politically loaded.
What this experience helps clarify is the role medicine has to play as a good-faith, evidence-driven voice in local politics. Physicians remain a trusted voice, and for good reason: medical training and practice is designed to allow physicians to make patient-centered decisions, free from political interference.
We are living in deeply polarized times, during which people who live in the same community have become more likely to view shared problems through the lens of politics. San Francisco and Marin have proud traditions of local advocacy and organizing, a testament to the engagement of their citizens, but sometimes also a risk to our ability to put aside differences in one area to collaborate in another.
Now, more than ever, there is a role for physicians as a trusted, evidence-driven profession, deeply in touch with the needs of their community, to provide objectivity, clarity and nuance in public policy debates. For more information about getting involved in the Medical Society and bringing your medical expertise to bear on seemingly intractable issues, visit www. sfmms.org and click on ‘Leadership Opportunities’ under the ‘Advocacy’ tab.
While state and national issues have garnered significant attention and advocacy efforts, SFMMS has also continued to fight for physicians and patients at the local level. Physicians have firsthand knowledge of the health challenges their communities face. Because we are embedded in our communities, physicians have firsthand knowledge of the health challenges their patients and their neighbors face, our involvement in advocacy ensures that local public health policies are informed by real-world experience and scientific evidence. As we know, health outcomes are influenced by non-medical factors like housing, education, transportation, food access, and environmental conditions. Physicians can advocate for policies that address these social determinants of health, improving our patients’ health outcomes by looking beyond the clinic or hospital. Local advocacy also gives physicians a say in how the systems that affect our practice of medicine are designed, implemented, and regulated. This leads to better alignment between what our patients need, what our practices provide, and the policies passed by public officials.
Below are a few examples of local issues SFMMS has played a decisive role in influencing over the past few months.
In early 2025, Supervisor Matt Dorsey introduced an ordinance that would make “cessation of illicit drug use and attainment of long-term Recovery from substance use disorders” as the “primary objective of the City’s drug policy.” It defined ‘Recovery’ as “abstinence from illicit drugs.” Several organizations and patient advocates opposed the measure, disagreeing with its “singular focus on the abstention and cessation of drug use,” and believed it represented a “drastic departure from San Francisco’s long-established data-driven drug and harm reduction policies.” Supporters argued that those fighting against this ordinance have been irresponsible in their harm reduction strategies and their zealot nature has blinded them to the public safety dangers on San Francisco streets. An increasingly polarized public debate oversimplified the complex issues involved, leading to a false-choice narrative that policymakers must choose between supporting “abstinence” based approaches or “harm reduction” based approaches, with no room for nuance. This narrow view caused substance use disorder-related terms (e.g., abstinence, harm reduction, recovery) to become politically and emotionally charged.
SFMMS consistently affirmed that harm reduction efforts, abstinence, and treatment/recovery are not in opposition with one another or mutually exclusive. If properly supported and provided, they are complementary components of optimal substance use disorder systems. SFMMS also stressed that, given the severe lack of facilities, beds, and the staff to provide behav-
Heyman Oo, MD
ioral health services, none of these strategies will be effective, whether coerced, voluntary or otherwise.
Guided by input from the SFMMS Advocacy and Policy Committee, the SFMMS Board offered Supervisor Doresy a set of amendments that, if he agreed to incorporate into his legislation, would earn SFMMS’s support. The amendments included changing the definition of ‘Recovery’ to “the process by which an individual suffering from substance use disorder strives to make positive changes that become part of a voluntarily adopted healthy lifestyle. This may include participation in a MedicationAssisted-Treatment program administered by a licensed healthcare provider in accordance with applicable laws and medical guidance, outpatient residential treatment, contingency management, and injury prevention services as determined by the individual in need.” It also called for the goal of the city’s substance use disorder treatment policy to be “long-term remission of substance use disorders for individuals, with the help of fully supported and staffed evidence-based recovery and behavioral health services.”
Supervisor Dorsey agreed to these amendments, thanking SFMMS for its helpful input that successfully removed the organized opposition to the ordinance and garnered unanimous support from the Board of Supervisors. Several SFMMS members and I were honored to join the Mayor at the ordinance’s signing ceremony where our efforts to advocate for increased investment in behavioral health workforce and facilities was met with applause from community members.
For the past six months, the San Francisco Department of Homelessness and Supportive Housing (HSH) has implemented a policy with a well-intentioned goal: ensure the most vulnerable families experiencing homelessness are given access to the limited supply of shelter beds in San Francisco. However, this policy is having unintended consequences, creating avoidable stress and dire mental health conditions for some of San Francisco’s most at-risk families. The policy requires families to leave their shelter within 90 total days unless they can meet requirements for an up-to-30-day extension. The policy aims to “increase the flow” of families moving from shelters to more long-term housing and reinforces the use of shelter beds for emergencies. While it is a laudable goal to get more families into long-term housing, the current policy comes at the cost of increased family traumatization through miscommunication and the constant threat of a return to homelessness.
Parents and children suffering from homelessness are among the most at-risk populations that physicians encounter. Aside from not knowing whether they will have a roof over their head,
continued on page 8
Christina Wang, MD
Each year in May, hundreds of bills face the gauntlet of the Senate and Assembly Appropriations Committees’ Suspense File The bills on this File are ones that would cost the state money, and the Committees have a special hearing to determine these bills’ fate In a mix of high stakes political and fiscal decisions, many bills are held back, essentially eliminating their prospects of becoming law
SFMMS’s priority legislation came out relatively unscathed, with only three supported bills no longer moving forward in the legislative process:
• AB 371 (Haney) would have required dental insurers to provide access to in-network dentists near a patient’s home or workplace, and would have ensured that patients aren't stuck paying upfront for services their insurance should cover.
• AB 384 (Connolly) would have prohibited health insurance plans from requiring prior authorizations for a patient to be admitted to medically necessary 24-hour inpatient care for mental health and substance use disorders, and would have prohibited health plans from requiring prior authorizations for the medical care patients receive from a physician while enrolled in a 24-hour inpatient setting.
• AB 510 (Addis) would have required that appeals of prior authorization denials be performed by a provider of the same or similar specialty.
SFMMS’s prioritizes bills authored by the legislators that represent our two counties and would make a positive change in health care policy. This year, SFMMS’s three top priority bills are:
• AB 255 (Haney) – This bill will allow state funding for supportive-recovery residences that emphasize substance use abstinence. The bill would also prohibit eviction based on relapse.
• AB 1363 (Stefani) –This bill will ensure protective orders are properly transmitted and verifiable, with clear records accessible to families, survivors, and law enforcement, helping to prevent the purchase of firearms by individuals prohibited from doing so..
• SB 363 (Wiener) – This bill will require health plans to report the number of treatment denials or modifications they make. If more than half of them result in an overturning or reversal of a treatment denial, the plan or insurer faces administrative penalties.
SFMMS is also supporting six CMA-sponsored bills that recently passed out of their houses of origin, covering a wide range of critical issues including, physician wellness, prior authorization
reform, maternity access, and the risks of unregulated artificial intelligence in health care.
Other SFMMS-supported bills that continue to move toward the Governor’s Desk include:
• AB 544 (Davies) – This bill will require a person under the age of 18 to take an electric bicycle (e-bike) safety course if they receive a violation for failing to wear a proper helmet and want to avoid a court-imposed fee. It will also require e-bikes to have red reflectors at all hours of the day and night. SFMMS has prioritized improving safety related to e-bikes.
• AB 669 (Haney) – This bill will prohibit concurrent or retrospective review of medical necessity for the first 28 days of an inpatient substance use disorder stay during each plan or policy year, and prohibits retrospective review of medical necessity for the first 28 days of intensive outpatient or partial hospitalization services for substance use disorder. The bill also prohibits the imposition of prior authorization or other prospective utilization management requirements for outpatient prescription drugs to treat substance use disorder that are determined medically necessary by the enrollee's physician or psychiatrist.
• AB 824 (Stefani) – This bill will clarify that, for procedures relating to protective or restraining orders, a restrained person is required to relinquish any firearm and ammunition in their immediate possession. SFMMS has been a strong supporter of efforts to reduce gun violence.
• SB 40 (Wiener) – This bill will prohibit health plans from imposing a co-pay of more than $35 for a 30-day supply of insulin or imposing a deductible, coinsurance, or any other cost-sharing on insulin. It will also prohibit a health plan from imposing step therapy protocols as a prerequisite to authorizing coverage of insulin.
• SB 41 (Wiener) – This bill will require pharmacy benefit managers (PBMs) to obtain a license from the Department of Insurance, and it establishes qualifications, regulations, and fees for licensure. The bill will also prohibit health plans from charging enrollees more than the actual cost of prescription drugs.
• SB 418 (Menjivar) – This bill will prohibit health plans and insurers in California from discriminating against individuals based on race, color, national origin, age, disability, or sex. The bill will also prohibit health plans from actions like canceling, limiting, or refusing coverage, denying claims, or imposing extra costs based on protected characteristics.
continued on page 18
continued from page 3
thereby opening the flow. Boarding is the blaze that will consume us unless we act.
• Protect the Workforce: Reduce documentation burdens using scribes and AI. Utilize APPs under meaningful physician supervision. Support well-being with rest spaces, food access, and flexible scheduling. We must treat emergency physicians like the critical resource they are.
• Bolster Public Health Readiness: Secure funding for disaster preparedness, public health, and mass casualty response. EDs are our civilian front line. Just as we fund the military, we must fund readiness against pandemics, mass shootings, and disasters—natural or man-made. We have fire departments for fires. Who’s ready when society itself catches flame?
continued from page 3
these families’ concerns are compounded by other challenges such as parental employment, childcare and education, physical and emotional health, and personal safety. Parents have reported suicidal ideation, anxiety, depression, and feelings of hopelessness and desperation when faced with notices of losing shelter for themselves and their children. Burdensome administrative rules that require parents to secure repeated shelter extensions inflict unnecessary pressure and anxiety on an already difficult situation. Extending shelter stays and providing comprehensive support services are crucial steps toward ensuring that families can transition to stable, permanent housing successfully. Access to housing and shelter will not eliminate all the mental and physical health challenges these families face, but it creates a solid foundation from which they can improve and stabilize their lives.
SFMMS is urging immediate steps to reform the policy and its processes, including 1) Lengthening timelines and/or reforming the extension process to reduce the administrative and psychological burden on families; 2) Improving guidance and/or caseworker training given the number of HSH-overturned eviction decisions; 3) altering messaging to families (with their input) to avoid unnecessary and anxiety-inducing notices; 4) Prioritizing efforts to increase the availability of homeless family shelters and rental subsidies.
After alarm raised by Marin physicians, Assemblymember Damon Connolly introduced legislation to address safety concerns related to the use of electronic bicycles. After support from SFMMS, the bill was signed into law in 2024. The decision to implement these regulations was driven by a significant increase in e-bike-related accidents among youths and the lack of rider training and helmet use among adolescents. Between 2019 and 2022, youth bicycle accidents in Marin County surged by 110 percent. Notably, 10- to 15-year-olds experienced accident rates five times higher than other age groups. Physicians
The Bottom Line: Avoid Asystole
Emergency medicine is the heart of healthcare—sometimes racing, sometimes irregular, always essential. It’s a place where coffee and Diet Coke are the unofficial pressors, and no two days are ever alike.
However, the current trajectory—unsustainable workloads, plummeting payments, endemic boarding, and burnout—is untenable. If we don’t fight to fix this, we will lose not just a specialty, but a foundational part of healthcare itself.
Embrace the spirit of emergency medicine: resourceful, relentless, and dedicated to service. Let’s save this system—not with adrenaline and defibrillators—but with advocacy, policy, and purpose.
Jason Nau, MD, is an emergency physician at Kaiser Permanente in San Rafael, CA, where he’s been caring for his community for 26 years. A self-proclaimed serial hobbyist and amateur philosopher, he’s driven by curiosity, always eager to explore new ideas, and unafraid to have his beliefs challenged—and occasionally overturned.
and safety advocates were also concerned that Class 2 e-bikes can be modified to allow speeds up to 50 mph, a fact not widely known by parents purchasing these bikes for their children.
The new law grants local authorities within Marin County the power to implement specific safety regulations for Class 2 electric bicycles, including prohibiting individuals under 16 years of age from operating Class 2 e-bikes (throttle-assisted bikes that can reach speeds up to 20 mph without pedaling) and mandating helmet use for all Class 2 e-bike riders, regardless of age. The pilot program will remain in effect until January 1, 2029, during which time Marin County is required to collect and report data on enforcement and safety outcomes. As of June 2025, seven municipalities (Tiburon, Belvedere, Mill Valley, Corte Madera, Larkspur, Fairfax and San Anselmo) have adopted ordinance aligning with AB 1778 provisions, and four others (Sausalito, Novato, San Rafael, and Ross) plan to soon. Whenever possible, SFMMS member physicians have gone to these city council meetings to provide testimony in support of these measures and have been met with appreciation for their insights and perspectives.
When so much attention is paid to state and national news, it is sometimes easy to forget the profound impact our voices as physicians can have on our local communities. Many of these issues only come to the attention of SFMMS leadership through the involvement of our physician members. To learn more about state and local legislation, and how you can be involved, please consider joining the SFMMS Advocacy and Policy Committee: https://tinyurl.com/SFMMS-APC.

Heyman Oo, MD, MPH is a primary care pediatrician who believes in taking a whole family, whole child approach to health. She is passionate about public health advocacy, social justice, reversing the effects of toxic stress and helping every child, regardless of social circumstances, reach their full potential. She is Chair of the SFMMS Advocacy and Policy Committee.
Ameena Ahmed, MD and Steve Heilig, MPH
The elected delegation to the CMA House of Delegates (HOD) acts year-round to help CMA formulate medical and public health policy As seats in the HOD are allocated in proportion to medical society membership, the size of our SFMMS delegation to the HOD has expanded substantially in recent years, and there are currently a few open positions in our delegation. We have long made a significant, outsized contribution to CMA policymaking on important issues. If you are interested in learning more about this work or applying to run for an open seat, please reach out to Ian Knox at IKnox@sfmms.org.
CMA’s House of Delegates (HOD) convenes annually in October to debate on the most important issues affecting members, the CMA, and the practice of medicine. The Major Issues to be considered by the House each year are determined by the Committee of Delegation Chairs, the Speakers, and the Board of Trustees. Our delegation submitted a Major Issues proposal, “Health and Human Rights: Best Practices to Protect Vulnerable Patients (and Physicians) Under Attack.” Physicians and the health care system are under grave, foundational threat. We propose a CMA HOD major issue studying and providing best practice guidance for ensuring evidence-based care for all our patients, particularly those who are threatened due to their gender, nativity, sexual orientation, ethnicity, or other minoritized category; for protecting our medical institutions; safeguarding the independence of medical researchers; and for upholding medical ethics in these challenging times.
The Committee on Delegation Chairs approved Responding to Federal Funding Cuts and Other Attacks on Health Care, Public Health and Medicine as the major issue for the 2025 House of Delegates. This major issue subsumes many of the points made in our delegation’s proposal. While the scope and scale of changes being pursued at the federal level are significant and widespread, there are three main areas that could impact medicine broadly. These include efforts to cut federal programs that provide or support health care coverage, restructuring the federal government’s public health and research infrastructure and priorities, and undermining the physician education and workforce pathways.
Three policy resolutions introduced by the SFMMS delegation to HOD were recently adopted as CMA Policy. The first, Hate Speech is a Public Health Threat, was adopted by CMA in 2024. This resolution was advanced to the AMA, which adopted this resolutions as AMA policy at the June 2025 AMA House of Delegates meeting.
The second, Tobacco/Nicotine Endgame: Supporting A Generational Phaseout of Sales, calls for CMA to support the concept of generational nicotine/ tobacco phaseouts of sales, such that sales of commercial tobacco and nicotine products other than those used for nicotine replacement/ cessation therapy are prohibited to those born after a defined year, throughout their lifetimes. A similar resolution was introduced
at the June 2025 AMA conference by the New England delegation, and was adopted in modified form by the AMA.
A third SFMMS-authored resolution, Restricting the Use of Electronic Medical Records for Patient Criminal Prosecutions, is a timely response to ongoing actions in other states and at the federal level. This resolution, which was adopted as CMA policy, calls for the CMA to support federal legal restrictions on using electronic health records for investigation and criminal prosecutions of patients seeking and clinicians providing reproductive and gender affirming care across state lines, and to protect patients from out-of-state legal actions based on lawfully provided care in California; and to include reproductive and genderaffirming health privacy as part of certified system functionality; and that this be sent to the AMA for review and adoption.
The CMA GTAC has proposed a comprehensive reform package to modify the business of the House of Delegates and overhaul the year-round resolutions process. These proposals seek to improve member engagement in policy development, including expanding the voice of the House on issues of prioritization. These proposed changes are grounded in principles of good governance and to respond directly to member feedback about the current process. We thank Drs. Roger Eng and George Fouras for their participation on the GTAC. SFMMS members are encouraged to log on to the CMA website and submit feedback to the GTAC proposal. This will be taken up as business of the October 2025 House of Delegates meeting.


Dr. Ahmed practices at Kaiser Permanente San Francisco and is Chair of the SFMMS delegation to the CMA House of Delegates.
Steve Heilig is an editor, ethicist, epidemiologist, environmentalist and educator based at the San Francisco Marin Medical Society, and co-editor of the Cambridge Quarterly of Healthcare Ethics.
Lonny Shavelson, MD, and Thalia DeWolf, RN, CHPN
Legal medical aid in dying — allowing terminally ill patients with decision-making capacity to take medications to die at the time of their choice — was born in Oregon in 1997, had a 23-year adolescence growing from legal rules to bedside care, and on February 14, 2020 it matured. Now, in 2025 — with 22% of the U.S. population living in aid-in-dying states — medical aid in dying is an increasingly wise adult, guided by evidencebased best clinical practices.

February, 14, 2020: A sunny winter morning on the Clark Kerr campus at UC Berkeley; more than 300 aid-in-dying clinicians from across the country gathered for the first National Clinicians Conference on Medical Aid in Dying. Prior to that day, they’d been working in relative seclusion, isolated by small numbers and the newness of aid-in-dying clinical care. The intense camaraderie at the conference formed a new medical community, and gave birth to the Academy of Aid-in-Dying Medicine. Clinical practice guidelines have rapidly evolved.
Clarifying and expanding the definition of medical aid in dying
Uniformly, in the lay press and medical literature, aid in dying was defined as variations of "(the) medical practice wherein a health care provider prescribes medication to a qualified individual who may self-administer that medication to bring about a peaceful death.” But quality patient care, we all know, should never be narrowly focused on just writing prescriptions. Yet it wasn’t until 2023 that the major clinical-practice resource UpToDate updated its prescription-focused definition of aid in dying to, “…the legal practice where a clinician cares for a terminally ill patient who considers and potentially follows through with hastening their imminent death…” The two major concept changes in that definition are (1) cares for a terminally ill patient, and (2) considers aid in dying.
Considering aid in dying has become the state-of-art term, acknowledging that terminally ill patients — novices at the dying process — are reviewing options, not just requesting lethal medications. Considering aid in dying is the all-encompassing term, from awareness of the option and simply wanting more information, through their journey in continued end-of-life care, ending only with death, whether by lethal medications or
not. The aid-in-dying provider, then, is an end-of-life clinician who also offers aid in dying, if that’s how the patient chooses to die.
This opened the nascent field of aid-in-dying medicine to include providing everything from information to life-ending medications, and all care in between. In fact, helping patients through the if , and if so , when dilemma is a major focus of compassionate aid-in-dying care, independent of whether the patient takes medications to die.
These conceptual advances led to our teaching about “interval care” — between contemplation and death. Terminally ill patients physiologic and psychosocial circumstances change as they get closer to dying; the patient’s condition at the beginning of the process is often very different by the end. The attending/ prescribing provider, then, doesn’t operate at a moment in time (qualifying the patient and giving them a prescription), but over a spectrum of evolving events and circumstances.
Hospices and nurses are central to aid-in-dying care
Each year, around 50% of terminally ill patients receive hospice care. For those who utilize aid in dying, hospice enrollment rates are remarkably high, in the 90% range. By now, virtually every hospice in states where aid in dying is legal has cared for patients who have considered or completed aid in dying. Hospice staff, then, play a vital role in supporting these patients, independent of outcome. As a result, policies and procedures have evolved.
Since aid-in-dying laws permit any clinician or organization not to participate in the practice, the range of care has been described as “opt-in” or “opt-out.” But that binary choice rapidly proved to be uninformative as a variety of care models developed. Similarly, non-specific but common expressions such as “We support aid in dying,” or “We take a neutral stance,” proved to be less than useful in understanding what, if any, aid-in-dying services a patient might expect. Unless accompanied by specific details about the care provided, imprecise phrases do not provide adequate information to patients, families, referring clinicians, or even hospice frontline clinical staff.
Only recently have hospices in some aid-in-dying states been required to make their policies public. Compliance has continued on page 12
been poor, so data is hard to come by. But extensive anecdotal information suggests that hospices have become increasingly knowledgeable about the processes and care involved. Most have found ways to compassionately work with patients considering this option, moving beyond the opt-in/opt-out binary into a variety of approaches to care.
Rare hospices, mostly religious based, still tell patients, “We don’t participate in any way and can’t talk about it.” The vast majority of these organizations have moved beyond that limitation and their staff now ask about and discuss the reasons behind the patients’ inquiries. They embrace compassionate conversations about goals of care and end-of-life needs — even when the patient continues on the path to medical aid in dying (typically by hiring an outside clinician). Some Catholic-based hospices now allow their nurses to be present with the patient on the aid-in-dying day (while an outside clinician organizes and monitors that care).
Hospice care variations form a continuum, from those which “support” patients considering aid in dying but provide no specific care (referring that to outside clinicians), to those which provide “integrated aid-in-dying care” within their agency. These hospices coordinate all care from contemplation to the final decision and, if the patient wishes to proceed, provide staff for medical and emotional support on the aid-in-dying day.
Other hospices have reached varied middle grounds. Some do not allow their doctors to be attending/prescribing physicians, while they permit the legally-mandated consulting/2ndopinions role. Frontline clinical staff policies vary, as well. For example, in many hospices, nurses, social workers, and chaplains may provide the crucial interval monitoring of patients considering aid in dying, and can be present on the aid-in-dying day. But those same hospices might forbid their nurses from preparing the medications — leaving the daunting task of adding liquid to a bottle of lethal powders to already anxious family members. And some ban all clinical staff from being in the room during medication ingestion. These hospices commonly cite legal restrictions prohibiting those activities, but no such limitations exist in any aid-in-dying law.
Hospice policies are still frequently outdated, originating from risk-management recommendations early in aid-in-dying history. They’ve persisted in spite of 28 years of clinical practice, during which no hospice, medical organization, or clinician has been sued or investigated for preparing the medications, complications of aid in dying, or being present during ingestion of the final dose. Of course, proving a negative (no lawsuits) is always difficult, but the Academy and multiple lawyers have searched for such cases, finding none. Of note, ethics reviews have found that “nurse leave the room policies” not only increase stigma against patients who choose aid in dying, they border on patient abandonment.
Yet signs of progress abound. When California’s law went into effect in 2016, hospices which provided integrated aid-indying care were extremely rare. They’ve since been increasingly common. Several large multi-location agencies provide fully-integrated care, successfully managing and coordinating workflows within their teams.
Since day-to-day clinical care in hospices concentrates on nurses, and quality aid-in-dying care means following patients over time, improved hospice and nurse outreach and training has become a major focus of the Academy of Aid-in-Dying Medicine. Follow their gut.
Aid-in-dying laws mandate (in varying language) that patients ingest the medications — injections of any type are prohibited. This creates a pharmacologic dilemma that, surprisingly, took years to realize: The intestinal tracts of seriously ill patients, especially as they get closer to death, are not healthy. At a minimum, gastric emptying and peristalsis decrease and absorptive surfaces atrophy — leading to impaired transport and absorption of medications. At the worst, dying patients develop bowel obstructions (mechanical or medical), inability to swallow, or what we now refer to as “global gut dysfunction” — as the body shuts down, so does the gastrointestinal tract. So the legally mandated “ingestion” of aid-in-dying medications is, from a clinical point of view, an extremely troublesome requirement.
Major advances in aid-in-dying medicine have, to a significant extent, mitigated (but not resolved) the gut dilemma. First, legal opinions clarified that “ingestion” — thought from 1997 to around 2017 to signify “swallow” — means the administration of medications into the gastrointestinal tract. That opened the possibility of working not only with swallowing, but feeding tube, ostomy, and rectal administrations. This means that aidin-dying clinicians, tasked with deciding which route would be the safest and most efficacious for each patient, have become experts in the oropharyngeal-esophageal-gastrointestinal tracts of dying patients — a changing functional capacity as they get closer to death. Again, aid-in-dying care moved from the original concept of a prescription-writing moment in time, to continued clinical care.
In journal articles, especially the Academy’s Journal of Aidin-Dying Medicine, at conferences, in continuing education materials, and by word of mouth and mentoring, aid-in-dying clinicians increasingly understand dying patients’ gut function, and clinical best practices have evolved.
At aid-in-dying’s birth in Oregon in 1997, clinicians assumed that since sleeping medications like barbiturates bring on sleep by broadly suppressing brain neuron activity, a huge dose of a barbiturate would reliably also inhibit brain stem neurons that drive respiration. Megadoses of barbiturates, then, would first put the patient to sleep and then cause death by respiratory suppression. This, it turns out, is far from true. For example, if a patient can rapidly and completely absorb X milligrams of a barbiturate, the same does not apply to X-thousand milligrams, especially in the dysfunctional gut of a terminally ill patient. Although ER clinicians, toxicologists, and the media have
reported about people dying from overdoses of various sedatives, including barbiturates, that doesn’t mean that everyone who takes such an overdose dies. But for aid-in-dying, reliability is crucial — and barbiturates, even in enormous doses, did not provide that.
Aid-in-clinicians have come to understand that megapharmacology differs from pharmacology — enormous overdoses don’t have the same absorption and pharmacokinetics of typical doses. As a result, a group of clinicians in Washington originated a system of three-system lethality — shutting down the brain, respiration, and heart — deeming such a protocol as necessary for the reliability of aid in dying. Over the 28-year history of these protocols, the pharmacology has advanced from admittedly ad-hoc word-of-mouth recommendations to sophisticated data-driven innovations and new medication combinations, as most recently described in the Journal of Palliative Medicine and extensively by the Academy.
Additionally, by using patient-report databases of the Academy, End of Life Washington, and End of Life Choices Oregon, predictive Clinical Factors Associated with Prolonged or Complicated Aid-in-Dying Deaths have been elucidated and widely distributed, mitigating complications and increasing the efficacy, reliability, and comfort of medical aid in dying.
The presently recommended medications are a combination of brain/respiratory/cardiac suppressants — DDMAPh, a mixture of diazepam, digitalis, morphine, amitriptyline, and phenobarbital in megapharmacologic doses that can be adjusted depending on the patient’s opiate/benzodiazepine resistance, extreme cardio-respiratory conditioning, and other risk factors. As well, the route of administration (oral, feeding tube, ostomy, rectal) can be changed depending on oropharyngeal-esophageal-gastrointestinal factors.
Autonomy
The moral imperative of aid-in-dying care rests in the clinician’s response to the autonomous decisions of patients considering aid in dying. And the very existence of autonomous decision making relies on information, readily provided, accurate, and detailed.
Autonomy thrives on information.
An interesting dilemma frequently comes up for clinicians, especially those in the attending/prescribing role, since those providers are the gatekeepers of aid-in-dying care. They determine if the patient qualifies, accepting or denying the possibility. But what if a patient legally qualifies, but the clinician disagrees with their motivations and reasoning?
For example, one author of this article, Lonny Shavelson, cared for a patient who’d been a Vietnam war pilot, fire-bombing forests with napalm, resulting in thousands of civilians sustaining life-altering burns. Now dying of lung cancer with an estimated three to four months to live, this ex-pilot resided in a skilled nursing facility, the cost eating through his life savings. The patient qualified for aid in dying by all legal criteria. He decided to hasten his death to save money so he could finance a hospital in Vietnam for victims of napalm burns. (I’m switching to first person, given the personal nature of the dilemma.) I
was deeply uncomfortable with and vociferously objected to his reasoning, even while understanding its foundation. I provided information and my own rationale for being distressed by his hastened death. As for any clinician, I, too had the right to autonomy. I considered denying or delaying his aid-in-dying request. But, I decided, his autonomy trumped mine.
I have since fielded questions from clinicians saying, “But this patient wants aid in dying so as not to be a burden to her family, even though they say she’s not a burden. I’m not comfortable with that.” Or, “This patient is having a pain-free hospice death and seems to me to have minimal suffering, with more than a month to live. Yet he wants me to help him die in a few days. That bothers me.”
After lengthy discussions with many clinicians, we agreed that a provider can decline care to a patient if they are morally uncomfortable with that care (and all aid-in-dying laws support this “opt-out” right). Those clinicians might decide to transfer the patient to a different practitioner. We also agreed that, after we provide patients with detailed information and the reasons for our discomfort, we should not impose our moral imperatives on theirs. Or, as I put it to my own patients: “We may disagree on some aspects of your death, and I’ll make it clear when that’s happening. But in the end, if we disagree — you get to decide.”
Clinicians are not mere providers of information, we also offer the knowledge of our experiences — personal, clinical, and ethical — in as non-judgmental a fashion as we can. In the end, though, whether our patients consider stopping potentially lifeextending chemotherapy, or are considering aid in dying, they get to decide.
So to further amend the UpToDate definition of aid in dying as where a clinician cares for a terminally ill patient who considers and potentially follows through with hastening their imminent death, we now add: The core of aid-in-dying medicine lies in respecting dying patients’ autonomy by providing evidence-based information and experienced knowledgeable opinions. And then, they decide if aid in dying is their chosen route to death, among many. The essence of our practice is to fulfill autonomy, not just provide medical aid in dying.

Thalia DeWolf, RN, is a certified hospice and palliative care nurse with extensive experience in end-of-life care. She is the Director of Nurse Education and Hospice Outreach Coordinator for the Academy of Aid-in-Dying Medicine.
Lonny Shavelson, MD, is the Director of Education for the Academy of Aid-in-Dying Medicine.
Monique Schaulis, MD, MPH, FAAHPM
Here are a few recent musings on Aid in Dying Medicine All in all, interesting times locally, nationally, and abroad
I attended several presentations on MAID at the National Hospice and Palliative medicine (AAHPM) conference last year. I noted what seem like persistent generational and coastal divides. At the conference, a young physician from a well-regarded academic East Coast program presented on MAID. She felt so ostracized by her older colleagues that she felt unable to share her employer on her slides. Afterward, her boss stood up and publicly berated physicians who offered aid in dying. The discomfort in the room was palpable.

At the upcoming AMA House of Delegates, conversations between supporters of AID and those who oppose the practice will take place. The CMA and the medical student section have proposed using the term Medical Aid in Dying instead of the older and more pejorative Physician Assisted Suicide. Additionally, the Board of Trustees will recommend opposition to the civil or criminal legal action against physicians, health professionals, and patients who legally engage in physician assisted suicide. This is similar to the language that the AMA has supported for physicians who provide full spectrum reproductive care.
In contrast, physicians from Washington, Oregon, California, and Hawaii discussed ongoing refinement of practical and ethical processes around aid in dying. Their compassionate and unwavering professionalism served as a clear rebuttal to those opposed. Most physicians reported that improving collaboration with hospice agencies has been very helpful to patients and families. The change in the California waiting period from two weeks to 48 hours also had a positive impact as it has decreased the number who die or become incapacitated during the waiting period.
From our northern neighbors, a Canadian AID practitioner offered her perspective that US aid in dying is “barbaric” since there is no legal IV administration, creating significant barriers for some patients. There was a collective gasp in the room when she used this adjective but it provided some food for thought given the barriers that some patients (often with ALS) face in self-administration. The ongoing difficulties that patients with dementia face in the US as they cannot legally access aid in dying medication were also discussed.
Here in the Bay Area, the Academy of Aid in Dying Medicine continues to be a source of education, clinical standards, and support for clinicians and patients. The Academy has published several issues of the Journal of Aid in Dying Medicine which is offered free of charge and firewalls. https://www.aadm.org/ journal
In California, there are concerns that the growing presence of faith-based hospitals and health systems restrict access to end of life medication (akin to reproductive services.) According to the Science Policy Group at UCLA, five California counties have exclusively faith-based acute, short-term care hospitals and faith-based hospitals have a majority market share in 25% of California counties. This is an exponential increase in the last decade. These organizations often explicitly prohibit their employees from participating in MAID. This increasing market share may represent an ominous shift in Californian’s access to aid in dying medication, particularly in counties where they are the only healthcare provider.
Overall, I see both steps forward and backward but a trend towards improved access to aid in dying.

Dr. Schaulis is an emergency and palliative physician at Kaiser San Francisco. She is a Past president of SFMMS and currently serves on the CALPAC board.
“I don’t want you to get stuck in traffic,” she said to me. Then, turning to her sons, she said “You guys go get something to eat. It will probably take the mortuary way too long to get here to take my body away.” Ever pragmatic, Allison lived her own way and she died on her own terms.
Just after her terminal cancer diagnosis, she started planning her path. Allison was no stranger to tragedy and death. In childhood and adolescence, her sister died in a drowning accident and her brother died in the Vietnam War. She watched her father, then her mother, decline and die. She even came close to death, herself, after falling from a tree. She just had to get that mistletoe from the treetop.

Her brother’s death surely shaped her views about war and peace, sparking her activism against war, hate and cruelty. She was a humanist, believing that the majority of people are good and kind.
But the best companions in Allison’s view were animals. She always had at least one dog. For a time, she had the smallest dog and the tallest dog ever seen at San Diego’s Fiesta Island Dog Park. Seeing their silhouettes against the bay, one could swear that she had both a horse and a small rat in tow.
Allison loved Great Danes, her little dog, and the beach. But most of all, she loved her family — especially her two sons and her granddaughter. She was determined to plan a peaceful death sparing herself and sparing her loved ones the indignities that would likely occur as her advanced esophageal cancer progressed.
She started on Hospice and she learned of the end of life option. As a very private person, the Hospice visits felt intrusive to her. As she started the evaluation for the end of life option, the number of assessments, reassessments, repeated visits and repetitive information greatly annoyed her. She called me often to vent her frustration. Did she really need to see the chaplain –again? Yet another visit from the social worker? Another doctors visit for yet another signature? Really?
She did come to understand that the thorough evaluation was necessary and she finally received the bottle with the mixture of medications that she was to eventually add water, shake to mix, bring to her lips and hold in her own hands to drink.
The timing must be right. Her ability to swallow was rapidly worsening. She must be strong enough to hold the bottle and drink it. She felt empowered by the bottle on her shelf. It represented self-determination. It represented freedom from pain, control of her destiny, and an end to hersuffering. She knew that the time was rapidly approaching, but she was not quite ready.
When I saw Allison on Monday together with younger son, she said that she had called her elder son and had asked him to
L. Nyberg, MD, MPH
fly out from Utah . She had decided to take the medication the following day. She wanted her two sons and me to be with her at the end of her life.
On Tuesday morning, I awakened filled with anxiety and misgivings about being a part of a person actively ending their life. Initially, I feared that I would not be able to be present during the process. But I quickly got a grip on my feelings and understood that this was about Allison, not me. It was Allison’s decision to end her life under her own terms as her natural death was rapidly approaching. I knew that this was the kindest path rather than allowing the cruel disease to rob her of the selfdetermination and dignity that she had left. I also understood that the fact that she would take the medication herself not only ensures that the decision is her own, but it also serves to absolve those who are present of any guilt feelings they may harbor as they do not administer the medication.
I have witnessed many deaths in my field in health care. Some deaths have been peaceful and good. Other deaths have been extremely painful and difficult. I have also lost three beloved family members recently. Their deaths were not entirely peaceful. I believe that our loved ones who died were not in pain, but it was excruciating for my family and me to witness the sights and sounds of a loved one in the throes of dying. Allison’s was a beautiful death. To be present when Allison passed away was one of the greatest privileges of my life. It was a courageous and selfless act.
“I’m ready", she said. She hugged and kissed her sons and me. With quiet serenity and shining eyes, she drank the mixture, smiled and put her head down on her pillow. I stepped out to give Allison and her sons privacy in her last moments of lucidity. Shortly after, I was told that she was sleeping. Soon, she took her last breath. The peaceful calm that followed allowed us to grieve her passing while also celebrating her life and joys.
After I gave Allison a last goodbye kiss I hugged her sons and got on the freeway.
I didn’t get stuck in traffic
Allison would have liked that.
Dr. Nyberg is a semi-retired gastroenterologist in San Diego, CA.
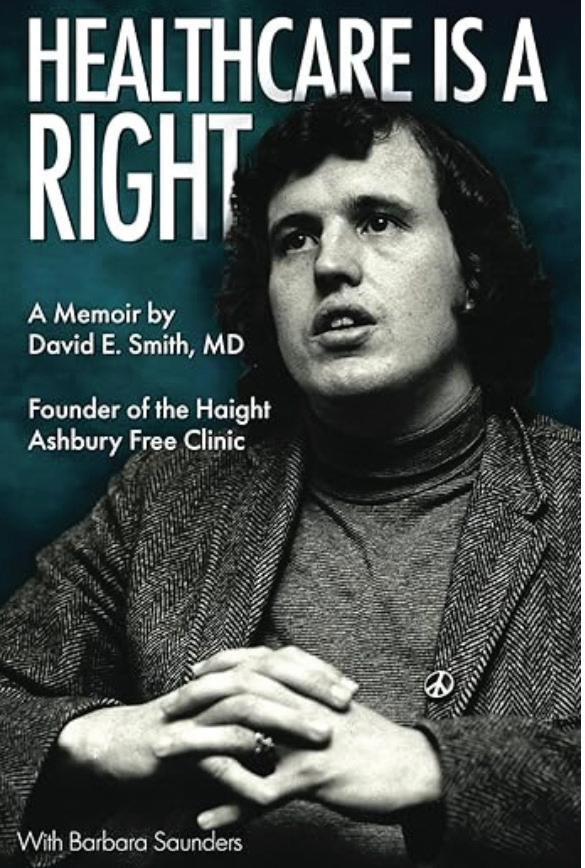
“David, you were such a promising young medical studentwhat went wrong?” – a UCSF professor and advisor to David Smith in the 1960s.
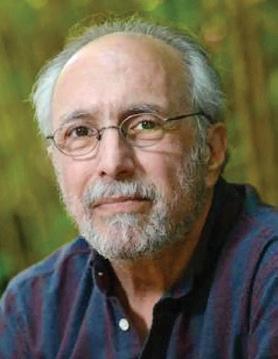
Dr. David Smith is now one of the longest-tenured members of the SFMMS, having first joined in 1968. He is also one of the most renowned, beginning with his unlikely path as young founder of one of the first “free clinics” in San Francisco’s HaightAshbury neighborhood in 1967. Out of that effort came a free clinic movement serving millions of patients, the specialty of addiction medicine, a guiding slogan quoted by United States Presidents, and much more. He’s been president of his state and national specialty societies and UCSF Alumnus of the Year and UC Berkeley’s Haas Public Service Award among many such recognitions. He’s published countless articles, many books, and founded the Journal of Psychoactive Drugs. You came to UCSF in 1960 from Bakersfield via undergraduatestudiesatUCBerkeley Atthatearlypointwhatdidyou thinkyourmedicalcareerplansmightbe?
My mother was a nurse, and my grandparents came from Oklahoma to settle in Bakersfield. They worked in the fields until they could stabilize their life, but my mother always said make something of yourself. She was the one that motivated me to go into medicine. I was privileged to be going to school in the 50s, which was the Golden era of California education with virtually free education for students born in California. I was a good student and went to UC Berkeley and then UCSF medical school. I was also in graduate school in pharmacology and took a real interest in psychopharmacology. It was my intent to be a biological psychiatrist being trained at Langley Porter. By the time you were finishing residency and postgraduate workthe“hippieexplosion”and1967“summeroflove”was underway How and why did you get the idea to open a free clinic in the Haight then?
In 1965 there was the war on poverty led by President Lyndon Johnson. Soon the counterculture revolution hit and I was surrounded by it in the Haight-Ashbury. I saw all the young people flocking to this area but my original idea of opening a
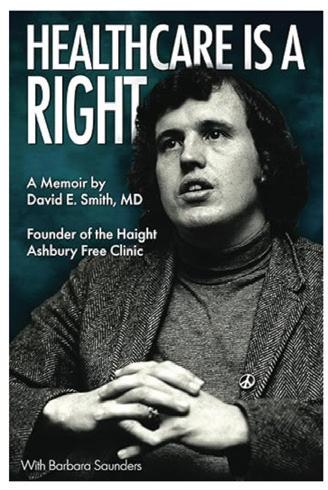
Dr. David Smith’s new memoir is available via Amazon, with proceeds going to his charitable foundation. Steve Heilig was honored to write the Foreward for his longtime mentor and friend.
Steve Heilig, MPH
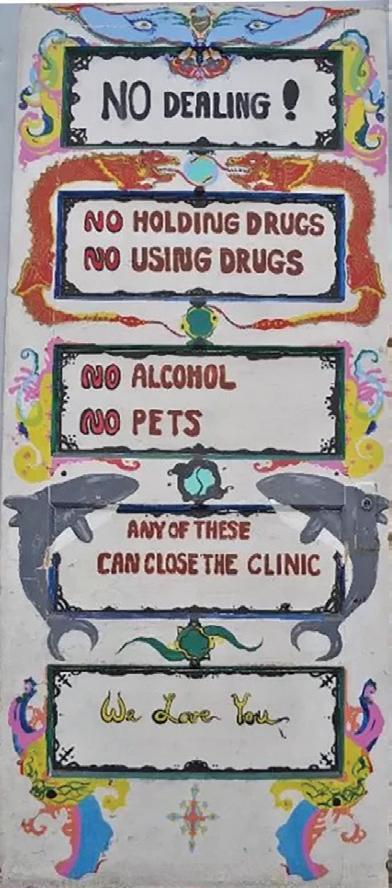
free clinic for hippies was rejected by the health department as they wanted the hippies to leave. I remembered seeing signs in Bakersfield that said “Okies go home” and decided to start a Free Clinic with the motto that “healthcare is are right not a privilege,” feeling that you should not deny healthcare to a population because you disagreed with their lifestyle and belief system
Howdidtheclinicoperate—volunteers,donations,etc—in those early years?
We were staffed primarily by volunteers, including physicians from the San Francisco Medical Society, medical student and faculty from all the schools at UCSF, including the pharmacy, medicine and nursing. During the 1967 “summer of love” the clinic operated 24/7, seeing about 300 patients a day. The primary problems that we saw included respiratory tract infections, sexually transmitted diseases, dermatological problems, psychiatric issues, and adverse effects of psychedelic drugs. Much funding came from rock music benefits, organized by Bill Graham that included the Grateful Dead, which lived in the neighborhood as well as a Jefferson Airplane, Janis Joplin, George Harrison, and Carlos Santana — our clinic was “built on rock ‘n’ roll.” In fact we founded Rock Medicine which continues to provide care at hundreds of concerts each year.
How did SFMMS first help save the clinic in the early years?
The original aim of the clinic was to provide care for the young hippies flooding into the city, which wasn’t that popular a mission. The San Francisco Medical Society was very helpful in the early days of the Haight-Ashbury Free Clinic, providing medical volunteers. Most noteworthy with Dr. Steve Walsh, who introduced our concept to the mainstream of the SFMMS and later became president. This became particularly important when I was receiving a great deal of publicity and my malpractice carrier decided to cancel my insurance. The SFMMS stepped in to provide insurance, so in a very real sense the SFMMS help save the clinic. And the clinic went on to provide over two 2 million client visits for all kinds of patients, not just hippies, prior to its merger into Healthright 360 where it is now part of their medical system.
Treating drug addicts at the start was still illegal How did youfirstgettheideaformainstreamingaddictiontreatment withanofficialspecialtyforthat,andwhatwerethebiggest challenges there?
The clinic developed a large community-based outpatient addiction treatment system, detoxing heroin addicts and dealing with methamphetamine psychosis as the Haight scene turned violent. At the time addiction was viewed as a crime and doctors who treated addiction were potentially guilty in abetting a
felony. In fact, a couple of physicians that used our detox techniques in other counties of California including Marin county were arrested. Addiction treatment was very narrowly focused, and viewed as outside the mainstream of medicine. I coined the term addiction medicine in order to get it viewed as a medical disease. the San Francisco Medical Society supported that concept and sponsored the resolution that introduced it to the AMA. Addiction medicine was finally accepted during the course of this evolution, and we came up with the idea of the California and American Societies of addiction medicine, dealing with all addictions, including alcoholism, and other drug dependencies. What are the biggest accomplishments and contributions in Addiction Medicine over the years as you now see them?
The concept of addiction medicine as a mainstream medical specialty has dramatically changed medicine. There are now addiction medicine fellowships at UCSF and other major universities and as a result the medical system is much more able to respond to the ongoing and growing problem of substance use disorder in United States. This is particularly important in light of the upswing in the potency of drugs, including fentanyl, which contributes to many of the overdoses, plus more potent forms of marijuana and pure forms of methamphetamine contributing to methamphetamine psychosis.
Harm Reduction is a major concept in the substance use disorder field. You were first opposed to syringe exchange efforts as possibly “enabling” substance abuse, but eventuallychangedyouropinion Howdoyouseethisdebatenow?
Yes, at first I was opposed to needle exchange and other harm reduction strategies as I felt they could enable addiction. However, evidence in studies from UCSF found that helping addicts at the point of contact, including needle exchange could increase the probability that they would engage in treatment and the overall therapeutic process, actually decreasing dysfunctional use of drugs. I believe harm reduction should be viewed as the point of the therapeutic engagement, reducing health consequences of addiction, but ultimately it should lead to recovery. Harm reduction, treatment and recovery should not be viewed as in conflict, rather part of a spectrum and response to the dysfunctional lifestyle associated with active addiction so apparent in San Francisco, where some streets have become open air drug markets, and overwhelmed emergency providers. These are all what the San Francisco health department and mayor Daniel Lurie are dealing with, and we met with him during his mayoral campaign after Dr. Bill Andereck, you and I wrote about this in the Chronicle. We remain hopeful that San Francisco can substantially expand treatment resources. Psychedelicdrugswereabigpartofthe“sixties”scene,with abacklashshuttingdownresearchforyears,butnowthere is a resurgence in mainstream interest and work How do you view this unfolding arena?
When I first began my studies in psychopharmacology at UCSF, I was very interested in the therapeutic potential of psychedelics. I then observed and participated in the psychedelic counterculture revolution and the Haight-Ashbury, seeing the flourishing, psychedelic art scene, but dealing with the bad trips associated with inappropriate use of LSD. The government

crackdown on and making LSD a schedule one drug seriously compromised mainstream research, but we’ve now entered into the third psychedelic research Renaissance and studies are showing much potential for carefully using substances such as psilocybin, MDMA and others for conditions including depression, PTSD and novel mechanisms in degenerative disorders such as Parkinson’s, and even, perhaps ironically, substance use disorder. The research is flourishing, and we have found it quite fascinating, synthesizing the spirituality of 12 step recovery and psychedelic spiritual enhancement and our psychedelics and recovery group that meets regularly in San Francisco. Your new memoir is titled “Healthcare is a Right ” How did you first come up with that slogan?
That was the founding slogan of our Haight-Ashbury Free Clinic, endorsed by then-UCSF Chancellor Dr. Phil Lee who had helped develop Medicare and Medicaid in the Johnson Administration, and later was quoted by President Obama when he announced the Obamacare and the parity act, revolutionizing the medical system to incorporate addiction treatment with appropriate insurance, but those advances are now being threatened by the current administration.
I hope that the book helps inspire a new generation of health activists as they complete their medical education to deal with the issues of healthcare inequality and access. We conduct a Haight tour for first-year UCSF Medical students and some are very interested in using their medical career to bridge this gap to underserve populations. We also have a small family foundation that gives scholarships to pre-nursing students with backgrounds in Bakersfield similar to mine or give them help with their nursing education. I’m proud that the San Francisco Marin Medical Society and CMA continue to be involved in these issues. I’m happy that the Haight-Ashbury clinic legacy continues on as part of HR 360 to carry this message through its addiction and primary care services around the city of San Francisco and now in other counties as well. These are the kind of the efforts that I have found so important in my career and my life.
Dr David E Smith's memoir, “Health Care is a Right”, is a powerful and persuasive narrative that ties in his personal journey as a physician with the evolution of community-based healthcare in America
As the founder of the Haight-Ashbury Free Clinic in 1967, Smith played a monumental role in starting accessible and nonjudgmental medical services during a transformative time in San Francisco. His story shows not only the challenges but the true triumphs of establishing the clinic amidst the counterculture movement. He was able to show the importance of providing care without stigma or shame. Dr. Smith's experiences truly expressed the way medicine, social justice as well as community activism interplayed during that era of the mid 1960’s. This memoir sheds light on the history of the HaightAshbury Free Clinic and also reflects on broader themes of healthcare accessibility as well as the ongoing struggle to view healthcare as a basic human right.
David Smith’s memoir provides insight into the origins and impacts of free clinics in the United States. He is able to offer such a unique perspective on various challenges faced by marginalized communities and the efforts made by physicians and other health care providers to address their healthcare needs.
The themes discussed in “Health Care is a Right” resonate so strongly with ongoing debates in modern healthcare. Today, the United States continues to grapple with issues of healthcare access, affordability, as well as equity. Despite the implementation of the Affordable Care Act and expansions in Medicaid, millions of Americans remain uninsured or underinsured, with the marginalized communities disproportionately affected.
continued from page 7
• SB 497 (Wiener) – This bill will expand California's shield laws by prohibiting provider, health plans, and other entities from complying with out-of-state or federal subpoenas that require them to disclose medical records or information that would disclose person is seeking or undergoing gender-affirming care, including mental health services.
The COVID-19 pandemic exposed more systemic weaknesses in the U.S. healthcare system such as disparities in treatment, access to vaccines, and health outcomes. These highlighted the same inequities that Smith tried to address years ago. His emphasis on community-based, compassionate care without stigma remains more relevant than ever.
Today's movements that advocate for universal healthcare, mental health reform, and the decriminalization of addiction closely represent the transformative spirit of the Haight-Ashbury Free Clinic. Dr. Smith's book serves not only as a historical account but also as a path to creating a more inclusive and just healthcare system.
In light of today’s challenges, “Health Care is a Right” remains a critical reminder that the fight for equitable healthcare is so far from over. This memoir encourages us all, physicians and other health care providers, to reexamine healthcare not as a privilege, but as an essential human right that must be upheld both in practice and policy change.

Sarita Satpathy, a hospitalist, is PresidentElect of the SFMMS.
To learn more about state and local legislation, and how you can be involved, please consider joining the SFMMS Advocacy and Policy Committee: https://tinyurl.com/SFMMSAPC.

Christina Wang MD is a San Francisco Department of Public Health physician, graduate of UCSF’s Internal medicine residency, and Vice Chair of the SFMMS Advocacy and Policy Committee.
Uninsured people who earn up to 400% of the federal poverty level ($5,217 per month for an individual, $10,717 for a family of four) are eligible for free specialty care.
Operation Access has immediate openings to provide donated surgical and specialty care through its network of participating medical volunteers and hospital partners. Visit operationaccess.org to refer someone or get involved as a volunteer.

Filling out our referral form is now optional but recommended to ensure we have a complete referral If more convenient, send referral via fax or email through your Electronic Health Records system along with a patient demographics page Include specific procedure requested and referral coordinator information. Attach relevant chart notes including the medical need for the procedure Include radiology reports (e.g. ultrasound, CT scan, X-Rays), lab results, or other necessary items indicated on the referral guidelines
We contact the patient to screen for eligibility by phone Patients are generally contacted within 10 days of referral receipt An appointment will not be scheduled in this call
We send a text to eligible patients to explain the program and outline the process. The referring clinic is notified of the eligibility status of all referrals in the semimonthly Referral Status Notification, requesting action on incomplete and unreachable referrals
*Eligibility: Uninsured and not covered by Medi-Cal, Medicare, and Workers Comp; Earn up to 400% of FPL; In need of outpatient procedure but not ongoing care.
4
1 2 3 5
Eligible patients are scheduled with a participating specialist Most referrals can be sent to a specialist within 1 month The average wait from referral to appointment is 1-3 months
When a specialist is available, an Operation Access case manager contacts the patient to confirm the appointment.
Our case managers try to coordinate appointments close to where the patient resides, but patients may need to travel to a specialist in another county
We notify clinics when cases are completed and provide information about the outcomes, where the patient was served, and how to obtain the medical records
Send referrals by fax to (415) 733-0019 or by email to referrals@operationaccess.org. Call us with any questions at (415) 733-0052 or visit www operationaccess org Direct address (within EMRs): operationaccess@direct.sacvalleymedshare.org
As a doctor, I’m not going to sugarcoat it.
At the end of a typical visit, I’ll ask my patients, “Do you have any more questions?” Of late, they’ll ask about the impact of executive orders and federal funding cuts on their care. As an oncologist, my reflex is to provide reassurance that has been some version of, “As long as we have a pharmacy and an infusion center with chemotherapy, I plan to keep your treatment on track.”
But my assurances are starting to feel hollow. With the announcement of cancellations of over $400 million in federal grants and contracts to Columbia University — and the prospect of similar action against other universities, including UC Berkeley, Stanford and UCSF — is it time for me and other health care providers to be more explicit about how federal funds have made possible the care my patients receive?
If I were to connect the dots for a patient of mine with melanoma, I’d tell him that the immunotherapy he is receiving, which has become widely used to cure a wide range of cancers, is only possible because federal funds supported research on how T-cells, a type of immune cell, are regulated. Understanding how T-cells are activated and inhibited made it possible to manipulate them to destroy cancer cells. This work began over 30 years ago in the laboratory of Dr. James Allison at UC Berkeley. It was funded by a grant from the National Institutes of Health long before its transformative potential became clear. Immunotherapy is why my patient and so many others are alive.
The treatments available to us today are the result of sustained investments over successive presidential administrations. Once at the point of being testable in patients, they require many more years of investment. Sequential clinical trials establish the optimal dose, safety and efficacy of novel treatments. As with basic scientific research, the federal government sponsors clinical trials and funds the Food and Drug Administration, which regulates them. While it is true that many scientific ideas and clinical trials fizzle out or fail, placing multiple bets increases the likelihood that one of them will pay off. It’s not waste or fraud. It’s the price of discovery.
I’d go on to tell my patient that it’s not just the treatments that depend on federal funds, it’s the training of doctors, too. After graduating from medical school — with an average of over $230,000 in student loans, mostly federal — newly minted physicians begin residencies and fellowships before becoming certified in a medical or surgical specialty. During this time, most pursue research funded by federal training grants. The spectrum of opportunities afforded by these grants is broad and reflects the need to produce a diverse physician workforce capable of meeting the health needs of our society and pushing the pace of progress across all areas of medicine.
In addition to fostering the environment for intellectual
Gerald Hsu, MD
growth, federal funding from Medicare and Medicaid provides the lion’s share of salary and benefits for physicians in training. Since its founding in 1965, Medicare has given direct payments to teaching hospitals to educate trainees. In 2021, this amounted to $17.8 billion. Every physician is the product of federal funding for their training and education.
After completing training, many physicians pursue careers at academic medical centers where they provide clinical care, teach and do research. To support this transition, they apply for highly competitive career development grants awarded based on a candidate’s likelihood of leading a successful independent research program. A physician in the training program I direct has spent the past 17 years — medical school, a doctoral degree, internal medicine residency, hematology/oncology fellowship and an additional three years as a post-doctoral research fellow — working toward a career development grant to fund her research on novel immunotherapies to treat leukemia. She got a score that in any other year would assure her this award. But due to the Trump administration’s decision to pause funding of these awards, her career hangs in the balance.
She is not alone. There are aspiring physician-researchers at every academic medical center across the country whose careers may never take off because of a funding freeze. And there is a pipeline of trainees behind them who will reasonably decide that the uncertainty of capricious funding streams makes a career path as a physician-researcher unfeasible. It’s a lose-lose scenario. They lose careers and society loses the intellectual capital that fuels discovery.
And so, the most transparent answer to my patient’s question is: Federal funding cuts are devastating and irreversible. The development of new approaches to treat your cancer will stall, the environment to train future doctors will be less intellectually rich, the potential of future doctors will fail to be realized and the knowledge and skills of future generations of physicians will deteriorate. These cuts jeopardize the care you receive today and the care of generations to come.
If I develop this new reflex for explaining the risks and benefits of medicines I prescribe, and how the doctors and the therapies available to treat their disease are the product of decades of federal funding, perhaps my patients will feel compelled to write their representatives, urging them to preserve federal funding for research and training. As beneficiaries of health care ourselves, it’s a prescription for us all.
Gerald Hsu is an oncologist and director of the hematology/oncology fellowship training program at UCSF. The original version of this article appeared in the San Francusco Chronicle.
Marek Brzezinski, MD, PhD, FASA and Jasleen Kukreja, MD, MPH
As the global population ages and life expectancy rises, geriatrics is becoming increasingly essential for physicians across all specialties Older adults require tailored care to meet their unique needs, presenting challenges that demand comprehensive and adaptive healthcare.1
With the complexities of aging more pronounced than ever, physicians must be prepared to manage these challenges. Whether it's addressing chronic conditions in primary care, providing perioperative care for older adults undergoing surgery, or considering lifestyle factors like diet and exercise, geriatrics intersects with nearly every aspect of healthcare.

The Need for a Greater Focus on Geriatrics
Regardless of specialty—whether surgery, internal medicine, general practice, or subspecialty—understanding the distinct needs of older patients is now crucial. Older adults are not only living longer but also managing multiple chronic conditions, with 60% of those over 65 having two or more. This requires a nuanced, multidisciplinary approach.
Patient expectations are also evolving. Many older adults now view their 70s-80s as a time for continued vitality, often seeking complex interventions like organ transplantation. Data from the Organ Procurement and Transplantation Network (OPTN) shows that in 2024, 26% of kidney transplants were performed on patients over 65, reflecting this trend.2 However, these expectations place a strain on healthcare systems, compounded by reduced reimbursement rates for the time-intensive care of elderly patients, challenging physicians to balance quality and efficiency.
To address these growing challenges, the SFMMS Journal is launching a series of educational articles tackling the most pressing issues related to the aging population. These articles will be relevant not only to geriatricians but also to physicians in all specialties, as older adults increasingly appear in every healthcare setting.
This series aims to equip healthcare providers with practical tools to manage aging effectively, enhance the quality of life for
older adults, and navigate the complexities of geriatric care.
This first article offers a broad overview of geriatrics, setting the stage for in-depth discussions on specific challenges in aging and elder care.
Human life expectancy has transformed dramatically over the past century. In ancient times, average life expectancy was 30–40 years, heavily skewed by high infant mortality and limited medical care. Those who survived childhood often lived into their 50s, 60s, or even 70s.
The 20th century brought remarkable gains. In 1900, U.S. life expectancy was about 47 years; by 2020, it had nearly doubled to 77.5 years, driven by advances in public health, medicine, and living standards, including antibiotics, vaccines, improved sanitation, and robust healthcare infrastructure.
These advancements have led to a profound global demographic shift: the aging population is growing rapidly. In the U.S., the population aged 65 and older is projected to exceed 95 million by 2060, comprising roughly 23% of the total population. Similar trends are evident in developed nations, particularly in Europe and East Asia. Japan leads with a life expectancy of nearly 85 years, followed closely by Switzerland and Spain. Notably, in 2018, the global population aged 65 and older (705 million!) surpassed children under 5 (681 million) for the first time in history.3
In contrast, countries with lower life expectancy face barriers like poor healthcare infrastructure, high rates of infectious diseases, malnutrition, and conflict, which significantly limit longevity.
Geriatrics is a relatively young medical specialty. The term “geriatrics” was coined in 1909 by Dr. Ignatz L. Nascher, an Austrian-born American physician widely regarded as the father of modern geriatric medicine. Nascher challenged the view that aging was merely a phase of disease, advocating for specialized care tailored to older adults. His 1914 book, Geriatrics: The Diseases of Old Age and Their Treatment, laid the foundation for the field. continued on page 22
In 1942, the American Geriatrics Society (AGS) was founded, cementing its place as the leading U.S. organization dedicated to geriatrics. Visionaries like Dr. Malford W. Thewlis and Dr. Lucien Stark were instrumental in shaping the society's mission. While there is no independent society solely focused on surgical geriatrics, the AGS has played a pivotal role in collaborating with surgical and other related specialties to foster interdisciplinary care for older adults.
Additionally, the Society for the Advancement of Geriatric Anesthesia (SAGA), established in 2001, has emerged as a key player in the field, specifically concentrating on enhancing anesthetic care for elderly patients.
Together, these organizations champion the importance of specialized, cross-disciplinary care for the aging population.
Life Expectancy in the Bay Area vs Other U S Areas
Life expectancy varies significantly across the U.S. The Bay Area, with an average of 83.5 years, ranks among the highest, thanks to access to high-quality healthcare, healthy lifestyles, and higher socioeconomic status. Cities like San Francisco and Palo Alto consistently lead in longevity. However, even in the Bay Area, challenges persist. Environmental factors, such as air pollution from traffic and industry, can reduce life expectancy. Social isolation, mental health issues, and limited transportation access for older adults also negatively impact health outcomes and quality of life.
Fun Facts About Aging and Life Expectancy
• The maximum human lifespan is estimated to be between 115 and 120 years, based on verified cases and influenced by genetics, lifestyle, and environment. On average, women live 5–7 years longer than men, thanks in part to biological factors like the protective effects of estrogen and lifestyle differences, such as lower rates of smoking and alcohol use. The longest verified lifespan belongs to Jeanne Calment, a French woman who lived to 122 years and 164 days (1875–1997). The oldest verified man, Jiroemon Kimura of Japan, lived to 116 years and 54 days (1897–2013). Some people carry genetic variations—such as certain forms of the FOXO3 gene—that are linked to longer lifespans and greater resistance to age-related diseases.
• A balanced diet plays a key role in long-term health. Large cohort studies suggest that both extreme carbohydrate restriction—such as in ketogenic diets (particularly when associated with high animal protein and fat consumption)—and high intake of refined carbohydrates are associated with increased risks of disease and early death.4-6
• Caloric restriction and interventions targeting conserved nutrient-sensing pathways—such as mTOR, IGF-1, AMPK, and sirtuins—represent the most consistently effective strategies for extending lifespan.7
• Starting around age 30, people naturally lose about 1% of their muscle mass each year, accelerating over time, contributing to frailty if not addressed.
• Importantly, many older adults maintain a positive outlook and adapt well emotionally to life’s challenges, which research suggests may contribute to longer lifespans.
This series will explore critical issues affecting older adults, including perioperative care, frailty, cognitive decline, transplant eligibility, nutrition, physical activity, and social engagement. These topics are vital for physicians across all specialties.
Understanding geriatric care is not just a professional necessity but a personal one, as we all aspire to age with vitality. Our shared goal is clear: not just to add years to life but to bring more life to those years.
Your insights and feedback will help shape this ongoing conversation, ensuring we meet the needs of an aging world.


Marek Brzezinski, MD, PhD, FASA is a Professor in the Department of Anesthesia and Perioperative Care at UCSF and President, Society for the Advancement of Geriatric Anesthesia.
Jasleen Kukreja, MD, MPH is a Professor, Department of Surgery at UCSF and a cardiothoracic surgeon; and director of the Lung Transplant Program at UCSF Medical Center.
1. Fields B, Golden BP, Perepezko K, Wyman M, Griffin JM. Optimizing better health and care for older adults and their family caregivers: A review of geriatric approaches. J Am Geriatr Soc. 2024; 72(12): 3936-3940. doi:10.1111/jgs.19061
2. Organ Procurement and Transplantation Network. (2024). OPTN data. https://optn.transplant.hrsa.gov/data/view-data-reports/nationaldata/
3. United Nations Department of Economic and Social Affairs. (2019). World population prospects 2019: Highlights. https://population. un.org/wpp/Publications/Files/WPP2019_Highlights.pdf
4. Reynolds, A., et al. (2019). Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. The Lancet, 393(10170), 434-445.
5. Seidelmann, S. B., et al. (2018). Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. The Lancet Public Health, 3(9), e419-e428.
6. Dehghan, M., et al. (2017). Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study.The Lancet, 390(10107), 2050-2062.
7. Green, C. L., Lamming, D. W., & Fontana, L. (2022). Molecular mechanisms of dietary restriction promoting health and longevity. Nature Reviews Molecular Cell Biology, 23(1), 56-73.
This Spring, a delegation of dedicated SFMMS physician advocates gathered at the State Capitol to meet with their legislators as part of CMA’s Legislative Day The nine-member strong delegation included current CMA President (and past SFMMS president) Shannon Udovic Constant, along with CMA Trustees (and past SFMMS presidents) Man-Kit Leung and Kim Green, CalPAC Board member (and past SFMMS president) John Maa, SFMMS PAC Vice Chair (and past SFMMS president) Brian Grady, and SFMMS Advocacy and Policy Committee members Monisha Bhatia, Akash Shanmugam, and James Lawrence.
The delegation met with the offices of Assemblymembers Matt Haney (San Francisco), Catherine Stefani (San Francisco), and Damon Connolly (Marin), as well as State Senator Scott Wiener (San Francisco) and Senate President Pro Tem Mike McGuire (Marin).
The delegation spent most of their meetings advocating for CMA-sponsored bills that would reduce burdensome and unnecessary prior authorization requirement. Health plans overuse prior authorization as a blunt cost-control tactic, placing profits over patient safety and intruding on physicians’ ability to make health care decisions that best serve their patients’ needs. Patients

and their physicians are forced to wade through red tape, delays and denials, all while their medical conditions worsen. More than one in four physicians say that prior authorization burdens have led to a serious adverse event — such as hospitalization, permanent bodily damage, and even death — for a patient in their care. Physicians and medical professionals are also spending numerous hours a week on unnecessary paperwork — time they could otherwise be spending with patients. On average, practices complete 43 prior authorizations per week, spending nearly two working days out of the week completing prior authorizations. CMA’s legislation includes bills that would require health plans to respond to prior authorization requests within 24 hours for urgent requests or 48 hours for non-urgent requests, extend the validity of an approved prior authorization to 1-year from the current standard of 60-90 days, and require health plans to remove prior authorization from any service they approve more than 90 percent of the time.
The delegation also advocated for the reestablishment of a physician health and wellness program that provides a proactive approach to address mental health and burnout issues, enabling the Medical Board of California to prevent patient harm by connecting impaired or at-risk physicians with treatment. California is unconscionably one of only three states without a physician health and wellness program. Physicians experience high rates of burnout but often avoid seeking help due to stigma and fear of disciplinary action. These programs recognize mental health conditions as treatable medical conditions, not moral failings, encouraging recovery without unnecessary penalties. Studies show that physician health and wellness programs achieve long-term recovery rates of up to 90 percent for physicians with substance use disorders, demonstrating their effectiveness in ensuring physician wellbeing and safe patient care.
Organized medicine is most effective when more individual physicians speak up and are heard. The delegation’s advocacy that day helped elected officials make informed decisions about critical health care issues. To learn more about state and local legislation, and how you can be involved, please consider joining the SFMMS Advocacy and Policy Committee: https://tinyurl.com/ SFMMS-APC
YOU DON’T NEED ANOTHER LECTURE ON SELF-CARE. YOU NEED TO DO THINGS THAT MAKE YOU FEEL CARED FOR.
Mahoney, MD
There’s no shortage of wellness advice out there You’ve heard it all before: “Prioritize self-care ” “Set better boundaries ” “Take time for yourself ” You’ve likely attended a wellness lecture... You sat in a windowless conference room while someone clicked through PowerPoint slides on burnout. Maybe they handed out stress balls or suggested downloading a meditation app. Maybe you got an amazing lunch. And then?
You walked out, back into the same demands, the same pressures, and the same exhaustion. Talking about wellness isn’t the same as experiencing it. Most wellness programs fall short.
They offer quick fixes and surface-level solutions—strategies that don’t fit the reality of a demanding career in medicine, leadership, or caregiving. They tell you what to do, but they don’t show you how to feel differently. Real wellness is something you embody. Embodying wellness means you feel it in your body, in your breath, and in your nervous system.
It means:
• You notice tension release from your shoulders when you exhale fully for the first time all day.
• You feel a shift in your nervous system when you finally pause long enough to hear your thoughts.
• You realize that presence—not productivity—is what truly nourishes you.
• You experience a moment of clarity that changes how you move forward.
Real wellness is about deep restoration, nervous system regulation, and mindset shifts that don’t just help you cope—they help you change how you live, work, and show up in the world.
How We Were Taught to Move Through Medicine, No Longer Applies
Practicing medicine today is not what most of us envisioned when we chose it as a profession. We still love science. We still love health. We still love helping patients and being healers. But the practice of medicine has changed—and continues to evolve at an unprecedented pace. Navigating this shifting landscape requires a new mindset—one rooted in adaptability, selfawareness, and resilience. The way we were trained to practice medicine was for a different kind of medicine.
We were taught:
• Self-sacrifice and martyrdom—but burnout is now an epidemic.
• Service at all costs—this comes at the steep price of physician mental and physical well-being.
• Medicine as “a calling”—this often justifies unfair working conditions and unrealistic expectations.
• Avoiding discussions of compensation, we are told that advocating for fair pay undermines our commitment to patient care.
• Over-responsibility and toxic independence which now lead to unsustainable workloads and a culture of silent suffering.
These approaches are outdated. They are no longer sustainable. The pressures of electronic health records, administrative burdens, and corporate medicine demand a new approach.Our systems do need to change. But most of us can’t wait for that day. If we want to continue to do what we love, we must update and reshape our approach to medicine, to practice in a way that is both fulfilling and sustainable, given medicine today.
When you understand how you were trained to think—and how those thought patterns shape your lived experience—you gain the ability to make intentional changes:
• Recognize harmful conditioning and question outdated mental models.
• Set boundaries to protect your well-being without compromising patient care.
• Cultivate a growth mindset to navigate change effectively.
• Manage energy wisely instead of running on empty.
• Advocate for systemic change rather than passively accepting frustration.
The future of medicine isn’t just about enduring the system— it’s about transforming it. Practicing medicine in 2025, requires both navigating change and advocating with strategic intention. By shifting our mindset, we can be healthy enough to advocate strategically and effectively. When we are replete, we shift from feeling helpless, overwhelmed, and depleted to acting with agency, discovering solutions, and leading effective change. This is where mindset coaching comes in. It is an evidence-based approach to rewiring old thought patterns and developing new strategies for professional fulfillment. It is not taught in medical training and yet is essential for a sustainable career in medicine. It helps physicians show up caring while also reclaiming their energy, purpose, passion, and impact.

Jessie Mahoney is a pediatrician, a certified life coach for physicians, and a yoga instructor. She is the Chair of the SFMMS Physician Wellness Task Force. She practiced pediatrics and was a Physician Wellness leader at Kaiser Permanente for 17 years.

To learn more about our upcoming events and offerings, visit our SFMMS events page at https://www.sfmms.org/news-events/events.
SFMMS Financial Planning Roundtable & Mixer
In March, SFMMS gathered a group of 18 members for our first financial planning mixer. The goal of this first gathering was to help inform the financial planning needs of our physician members and future guest speakers for similar events. Stay tuned for our 2nd financial planning mixer, slated for November!
SFMMS Hosted Curbside Consults & Cocktails for Primary Care Physicians on May 28th in San Francisco
SFMMS hosted its second annual Curbside Consults and Cocktails, a fun and casual evening for SF and Marin physicians to mix and mingle Wednesday, May 28th at the Snug (one block from the 2100 Webster Pacific Professional Building & Medical Offices, at Fillmore & Clay).

SFMMS Sponsored Members Attend the Honoring Diastole Mindful Retreat at Pie Ranch on May 10th





“Thank you! This was so valuable. Forget the zoom wellness events, or free apps offered by many large medical institutions. What we need as physicians is this. A day AWAY from our usual place of work. To be outside, to be with others and to eat healthy food—all evidence based recommendations by the way for wellbeing and longevity. Thank you. I did not realize how much I needed this.”
– SFMMS Member & Retreat Raffle Winner
California Doctors in Retirement (CADRE) Gathers Monthly in Greenbrae
"The monthly CADRE meeting is always fun. This gathering is for special people, who have had unique lives. As retired SF and Marin physicians, we can be best understood by each other."
Join your fellow retired physician colleagues for CADRE (CAlifornia Doctors in REtirement) for casual conversation, connection, & free coffee, monthly (3rd Thursday of the month) at Peet's Coffee in Greenbrae. For more information, please contact Molly Baldridge at mbaldridge@sfmms.org. Special thanks to Dr. Joan Saxton for her coordination and leadership of the CADRE group!
Are you looking for Additional Resources?


The SFMMS Wellness page, curated by your SFMMS colleagues, includes upcoming and past wellness events, resources and more. Learn more by visiting the SFMMS Wellness page at www.sfmms.org/get-help/physician-wellness.
Would you like to Practice Mindful Yoga for Healers With Jessie anytime?
Join Dr. Mahoney on Zoom most Saturdays at 9 am or anytime on YouTube. For more information visit: https://mindfulyoga.jessiemahoneymd.com or https://youtube.com/c/JessieMahoney.