How PBM Scrutiny Threatens

Self-Insurance
State action seen as challenge to ERISA protection, while a crackdown on revenue sharing could drive up service costs
A SIPC PUBLIC A TION SIPCONL I NE.N E T SEPTEMBER 2023
Accident & Health Insurance

We’ll focus on risk, so you can take care of your business
Get the peace of mind and support it takes to self-fund your healthcare.
Self-insuring your healthcare benefits can open up new possibilities for your business — affording you greater flexibility in how you manage your healthcare spend. Trust the expert team at QBE to tailor a solution that meets your unique needs.

We offer a range of products for protecting your team and assets:
• Medical Stop Loss
• Captive Medical Stop Loss
• Organ Transplant
• Special Risk Accident
We’ll find the right answers together, so no matter what happens next, you can stay focused on your future.
QBE and the links logo are registered service marks of QBE Insurance Group Limited. ©2023 QBE Holdings, Inc. This literature is descriptive only. Actual coverage is subject to the terms, conditions, limitations and exclusions of the policy as issued. Crop Specialty Commercial
To learn more,
us at
Download now: Accident & Health Market Report 2023
visit
qbe.com/us/ah
FEATURES
4 HOW PBM SECURITY THREATENS SELF-INSURANCE STATE ACTION SEENS AS CHALLENGE TO ERISA PROTECTION, WHILE A CRACKDOWN ON REVENUE SHARING COULD DRIVE UP SERVICE COSTS
By Bruce Shutan
14 PSYCHEDELIC-ASSISTED THERAPY EXPANDS EMPLOYER OPTIONS FOR MENTAL HEALTH
 By Laura Carabello
By Laura Carabello

ARTICLES
31 ACA, HIPAA AND FEDERAL HEALTH BENEFIT MANDATES THE AFFORDABLE CARE ACT (ACA), THE HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT OF 1996 (HIPAA) AND OTHER FEDERAL HEALTH BENEFIT MANDATES
36 SIIA CONFERENCE EXPERTS LOOK AT 2023 TRENDS
42 3M MASS TORT SETTLEMENT REMINDS US THAT SUBROGATION MATTERS
50 SIIA ENDEAVORS
57 NEWS FROM SIIA MEMBERS
The Self-Insurer (ISSN 10913815) is published monthly by Self-Insurers’ Publishing Corp. (SIPC). Postmaster: Send address changes to The Self-Insurer Editorial and Advertising Office, P.O. Box 1237, Simpsonville, SC 29681,(888) 394-5688
PUBLISHING DIRECTOR Bryan Irland, SENIOR EDITOR Gretchen Grote, CONTRIBUTING EDITORS Mike Ferguson and Ryan Work, DIRECTOR OF ADVERTISING Shane Byars, EDITORIAL ADVISOR Bruce Shutan, CEO/Chairman Erica M. Massey, CFO Grace Chen

SEPTEMBER 2023 VOL 179 WWW.SIPCONLINE.NET
2023 3
TABLE OF CONTENTS
SEPTEMBER
How PBM Scrutiny Threatens Self-Insurance
State action seen as challenge to ERISA protection, while a crackdown on revenue sharing could drive up service costs
Written By Bruce Shutan
Acrackdown on pharmacy benefit managers, three of which control about 80% of the market, may prove to be a double-edged sword for self-insured health plans.
On the one hand, new or proposed laws at both the federal and state level are designed to transform an opaque part of the U.S. health care system with transparency for payers and patients alike. They are in lockstep with federal Transparency-in-Coverage rules, No Surprises Act and Consolidated Appropriations Act – all of which have been fully supported across the self-insurance community.

FEATURE A
4 THE SELF-INSURER
A growing appetite to regulate PBMs stem from a larger effort to curb out-of-pocket Rx costs for health plan members that keep rising 13 years after the Affordable Care Act was enacted. It doesn’t help that the cost of specialty drugs coming down the R&D pipeline are expected to further raise prices.
Another culprit is consolidation of these services. The so-called Big Three PBMs – CVS Caremark, Express Scripts and Optum – boast massive scale and ownership that includes health insurers, physician practices, retail pharmacies and specialty pharmacies.
But with PBMs now firmly in the crosshairs of U.S. congressional representatives, regulators, statehouses and jurists, well-intentioned reform efforts also pose a serious threat to Employee Retirement Income Security Act (ERISA) protections for self-insured employers. Moreover, employers worry that curtailing or eliminating PBM revenue-sharing agreements will result in higher-priced services.
Since a 2020 U.S. Supreme Court decision pertaining to PBMs, industry observers fear that an invitation to unintended consequences could widen. An overly broad interpretation of Rutledge v Pharmaceutical Care Management Association is responsible for a fresh assault on ERISA. In upholding an Arkansas law requiring PBMs to pay pharmacies no less than their acquisition costs for prescriptions, the high court ruled that it was not preempted by ERISA. That decision allows states to regulate health care costs, including health plan contractors such as PBMs.

Ryan Work, SIIA’s VP of government relations, says the case to some extent opens the floodgates for states to regulate PBMs, “and what they’ve done along the way is started cracking at that ERISA firewall. You can regulate PBMs and pharmacy benefits, but at what point does that stop and then it starts actually regulating ERISA-protected selfinsured plans?”
His hope is that at some point the federal court is going to better define the Rutledge decision, “take up some of these ERISA arguments and create buttresses and firewalls around it that, while providing more transparency in the pharmacy space, will offer better protections for risk of self-insured plans.” The case is currently seen as a way for state regulators to get their hands
on self-insured plans, he explains, noting that Louisiana and Texas are among a few states that have tried to eliminate the word ERISA from some of their insurance statues related to PBMs.
Some regulators are using the decision to test how far they can go, he adds, while others are targeting PBMs without actually understanding that they’re just a tool to help mitigate costs.
There has been growing scrutiny of PBMs at the state level. A dozen states enacted 19 pieces of legislation last year that imposed a variety of restrictions for PBMs, including licensing and reporting requirements, prohibitions on spread pricing and rules aimed to make costs more transparent enrollees. These bills, among a whopping 135 measures introduced in state legislatures across the nation, seek to curtail the influence that PBMs have
SEPTEMBER 2023 5
“Pharmaceutical manufacturers are responsible for the high costs of drugs, and the PBMs are providing them the plans,” Work notes, “and they’re both pointing the finger at each other.”
PBM Scrutiny & Self-Insurance
Ryan Work
Complete, customizable TPA solutions
From locally-focused to national-scale programs, AmeriHealth Administrators offers a full spectrum of third-party administration and business process outsourcing services. Our scalable capabilities service many unique customers, including self-funded employers, Tribal nations, international travelers, and labor organizations.
We offer innovative solutions, insight, and expertise to help you manage your health plan and capabilities, control costs, and support employees’ health.
Visit amerihealth.com/tpa

to learn more about how we can work with you.
over both pharmacies and drug pricing.
Much of the state legislation is being driven by community pharmacists who feel under attack by the role of PBMs and the large retail pharmacy chains, according to Work. In Louisiana, for instance, they have shopped around model legislation for every state to pass. He references a campaign to file a complaint with the Louisiana Department of Insurance every time a PBM claim from a self-insured plan was submitted, which generated 30,000 cases in the past year.
“One of the problems that I’ve seen is that patients will go in with a prescription, and their community pharmacy is requiring that they pay in cash,”
Work reports.
Similar efforts to regulate PBM activity are also afoot on Capitol Hill, including the Pharmacy Benefit Manager Reform Act (S. 1339), which was introduced in late April. Led by Sens. Bernie Sanders (I-VT) and Bill Cassidy (R-LA), it proposes several reforms that are universally reflected in other bills. They include a ban on spread pricing and certain PBM claw backs, as well as require rebates paid to PBMs be passed through to health plan sponsors.
Work predicts that Congress will pass federal PBM transparency legislation by the end of this year – an area that has garnered rare bipartisan support in divisive times. The wheels are already in motion. He says PBM legislation has been introduced in the Senate Finance Committee and Senate Health, Education, Labor and Pensions Committee, as well as the House on Ways and Means Committee,
SEPTEMBER 2023 7
“In some cases, they are saying, ‘we’re not even going to take insurance. You do that on your own, and if you want to get reimbursed by your insurance, you need to do it on your own.’”
PBM Security & Self-Insurance
House Committee on Education and Labor and House Committee on Energy and Commerce.
But there’s no guarantee that any reform efforts will actually lower prices. In fact, it may do just the opposite. If PBMs aren’t able to share in claw backs, rebates or spread prices, then Work worries about higher fees being imposed on their services for self-insured customers. “You can bring transparency, but at the end of the day, is that really going to move the needle on cost? And the answer is probably no,” he suggests. “It’s just going to be a cost shift.”

EDUCATION AND ADVOCACY

Given the elevated level of misunderstanding, or no understanding at all, about ERISA and how the nearly 50-year-old landmark law benefits self-insured plan sponsors and participants, Work points to the importance of education and advocacy. As this issue went to press, SIIA planned to release to an ERISA white paper to help policymakers and congressional staffers at both the federal and state level understand the importance of ERISA protection. It also will serve as a resource for SIIA members.
While SIIA’s Drug Pricing Taskforce disbanded after several years of producing helpful checklists for members, other opportunities are expected to rise with regard to assessing PBMs. “One of the things that I’m trying to do is kind of create a smaller working group to better understand where our members come down on PBMs and regulation,” Work says.
Marien Diaz, VP of stop-loss claims and medical management for Symetra who was part of the taskforce, expresses a related concern about state oversight. “The No. 1 concern that I see from a claims angle is how are employers able to even comply with some of these state regulatory requirements?” she wonders. “If you have a selffunded employer with multiple locations across the board, these reporting requirements may change from state to state. Anytime that you have to program or invest in meeting those requirements, there’s additional cost.”
8 THE SELF-INSURER
PBM Security & Self-Insurance
Marien Diaz
Somebody has to come in second. Make sure it’s not you.
There are no insurance MVP trophies, no best PowerPoint awards, no fantasy broker leagues. You show up first with the best option for your client, or you lose. We never take this for granted. That’s why we leverage all of our people, data and relationships to reach one goal: We help you win.
We help you win.
BENDING THE COST CURVE


importance of providing transparency alongside eliminating hidden fees associated with direct and indirect remuneration, Baldzicki explains.


Plan sponsors, particularly TPAs, also are stepping away from brokers who pocket money from the large PBMs.
While lawmakers and regulators hope that reining in PBMs ultimately will help reduce costs, it’s clear that certain marketplace practices can have an immediate effect.
In the face of tremendous influence the Big Three PBMs wield, for example, some self-insured employer groups are peeling away from them contractually and embracing regionalized or midsize entities known as pharmacy benefit administrators, according to Mike Baldzicki, chief commercial officer, specialty pharmacy for Premier Pharmacy Services and member board of directors for the National Association of Specialty Pharmacy.
He says PBAs, whose business model reflects the service’s late 1980s roots before layers of complexity were added, are driving fiduciary duties and defining clinically appropriately utilization. They understand the
Advanced technology has powered the rise of PBAs to provide deeper insight beyond pharmacy claims to also include overall medical claims.

10 THE SELF-INSURER
“I even see brokers changing the way their model works to bring in other regionalized PBMs like CAP RX or App Rx and win some business for the smaller guys that are doing the right things to change the model,” he reports.
Learn More 8 88-248-8952 selffunding@benefitmall.com ©2023 BenefitMall. All Rights Reserved. Stop-Loss Management Services Claim Risk Solutions Premier Broker Support Expect More FROM YOUR STOP-LOSS PARTNERS PBM Security & Self-Insurance
Mike Baldzicki
Don’t face your obstacles alone. Whether you’re facing benefits loading issues, limited reporting, integration problems, or any other challenges—we’ll conquer them by your side.
Rise above your hurdles with cloud-based software fully customized for you.

( Experience quick implementation ( Optimize your software with AI integration ( Maintain full compliance with the No Surprises Act ( Leverage price transparency and reference-based pricing tools Software that Rises to Any TPA’s Challenge Looking for a foundational partner to grow your business? Schedule a demo today. 908.813.3440 sales@hi-techhealth.com hi-techhealth.com
“I’ve seen it where medical benefits for an infusion drug still ranges gross profit margin 19% to 66%, depending on the drug, if you’re truly not gaining insight on that claim,” he says.
Diaz says it’s important to create greater alignment between PBMs and claims administrators that support self-funded health plans, as well as offer transparent pricing. The Big Three have an opportunity to willingly create more disclosure in their billing practices and provide reasonable incentives to help employers mitigate their plans rather than rely on the regulatory environment to force them into adapting, she observes.
But there’s another area where self-insured employers can gain considerable traction: having a solid contractual arrangement in place when engaging the services of a PBM.

“When we are underwriting stop-loss risk, one of the basic questions that we ask is, ‘when was the last time that you reviewed and updated your PBM contract?’” notes Diaz, suggesting that an annual review be done. “It is shocking to me that although pharma expenses continues to grow exponentially, the review of contracts doesn’t happen with enough frequency and discipline… So it’s very difficult for us to provide competitive pricing in a meaningful way unless those agreements are reviewed and updated regularly. Sometimes we find employers that haven’t even looked at their PBM arrangement in the past five years.”
It all comes down to pursuing a proactive approach to engage in a meaningful relationship with PBMs, which Diaz believes “is in the long run a much better prescription, no pun intended, as an industry than to have to wait on regulatory mandates.”
Whatever direction the Rx industry takes, experts agree that cooperation and collaboration need to displace divisiveness. Adds Baldzicki: “We have to stop bashing PBMs, which have a place in the healthcare ecosystem, because if you really rip that away the disruption would be huge.”
Bruce Shutan is a Portland, Oregon-based freelance writer who has closely covered the employee benefits industry for more than 30 years.
12 THE SELF-INSURER
PBM Security & Self-Insurance

www.bhspecialty.com/msl A trusted business name. A stellar balance sheet. An executive team with 30 years of experience. Creative, tailored solutions. Berkshire Hathaway Specialty Insurance is proud to bring our exceptional strength, experience and market commitment to the medical stop loss arena. A medical stop loss grand slam. It’s a home r un for your organization. Atlanta | Boston | Chicago | Columbia | Dallas | Houston | Indianapolis | Irvine | Los Angeles | New York | Plymouth Meeting | San Francisco | San Ramon | Seattle | Stevens Point Adelaide | Auckland | Barcelona | Brisbane | Brussels | Cologne | Dubai | Dublin | Frankfurt | Hong Kong | Kuala Lumpur | London | Lyon | Macau | Madrid | Manchester | Melbourne | Munich Paris | Perth | Singapore | Sydney | Toronto | Zurich
PsychedelicAssisted Therapy Expands Employer Options for Mental Health Treatment
Written By Laura Carabello

WithWgrowing mainstream media coverage surrounding Psychedelic-Assisted Therapy (PAT) and its benefits to address staggering mental health issues such as anxiety, depression, substance use disorder (SUD) and chronic, unresolved posttraumatic stress disorder (PTSD), it’s no wonder that selffunded organizations are now paying attention to and adopting this treatment option.
PAT refers to therapeutic practices that involve the ingestion of a psychedelic drug, and since the early 1990s, a new generation of scientists has revived the research to support this treatment. A growing body of research is helping to dispel the social stigma surrounding “psychedelics” and employers are taking a healthcare perspective on covering this treatment as a meaningful health benefit.
FEATURE
14 THE SELF-INSURER
As science now better understands the health and wellness improvements derived from the medicinal use of psychoactive compounds, such as Ketamine, this novel, innovative approach introduces opportunities for cost effective mental health treatment that deviates from traditional pharmacological interventions.
“The effectiveness of ketamineassisted therapy has been demonstrated through multiple research studies and more than twenty years of accumulated clinical experience,” says Dan Rome, MD, chief medical officer at Enthea, the first and only licensed, turn-key third-party administrator (TPA) of psychedelic healthcare in the United States offering psychedelic healthcare as a workplace benefit.
Clinical trials have shown that ingesting a psychedelic in a carefully prescribed and monitored setting can induce an experience that is medically safe and that provokes profound, durable psychological and behavioral change.
Researchers have conducted highly regulated studies, using careful screening, therapeutic preparation, controlled settings and with trained monitors. Innovative therapies, such as Ketamine, are now FDA-approved and state-legal for use to effectively treat a range of behavioral disorders.
Several reports show that psychedelics have surged in popularity over the past few years. According to National Survey on Drug Use and Health, prepared for the Substance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department of Health and Human Services (HHS), 1.4 million Americans tried hallucinogens for the first time in 2020.
This level of enthusiasm, as reported in the New England Journal of Medicine, is partially the result of clinical trials showing that the drugs, notably psilocybin and ketamine, hold real promise in treating some mental health disorders, particularly depression. In fact, two states, Oregon and Colorado, have now legalized psilocybin for therapeutic use, and additional states are expected to follow suit.
Here’s the caveat: specialists who study these substances strongly urge that people only use them in supervised therapeutic settings, such as in a clinical trial or at an established ketamine clinic.
There are safety concerns attached to these substances and they are illegal outside of these venues.
Experts at Lancet advise that psychedelics have an extremely low chance of lethal overdose and there is little likelihood of addiction. As a result, authors classify them as some of the least harmful recreational drugs. But they do caution that they are not entirely without risk. Because of this, psilocybin trials and ketamine clinics have strict exclusion criteria to try to protect people who have physical or psychological vulnerabilities. The newest research published in Nature offers promise that psychedelic drugs may “reopen” the brain to help it recover from trauma. Scientists at Johns Hopkins University were investigating the drugs’ effects on “critical periods” for social learning, times when the brain is more open to new information that diminish as we age. They also anticipate that the therapeutic horizon for psychedelics could expand to other opportunities to retrain the brain, including recovery from a stroke, traumatic brain injury and even hearing loss and paralysis.
Some medical professionals and researchers say that PAT can be lifesaving when other traditional medications and therapies have failed. Researchers point to their remarkable efficacy in treating conditions that are often resistant

SEPTEMBER 2023 15
Assisted Therapy
Psychedelic
Dan Rome, MD
Psychedelic Assisted Therapy
to conventional treatments, with one promising arena in the treatment of substance abuse.
Employers are often ill-equipped to address these treatmentresistant conditions and welcome proven solutions. Given the current shortage of mental health providers and compromised access to care, this option is resonating among health decision-makers.
CALL FOR MORE EDUCATION AND MARKET AWARENESS
Don McCully, founder, Medical Captive Underwriters LLC, makes a good point: “Psychedelic assisted therapy is not widely known as an excellent treatment source. Education about the groundbreaking work in this area is largely muted. Employer decision making in this area requires additional education to allow for better informed decisions. PTSD and cancer were the first disease states approached for use of PAT and both experienced amazing outcomes. This needs amplification.”
He observes the inertia in health care for adoption of new and better treatments, saying, “It took 20 years to get sleep apnea patients assigned to pulmonologists. While there are no similarities or comparison between sleep disorders and PAT psychedelic assisted therapy, this is an example of the delayed response among decisionmakers.”
Emphasizing that the first step in any behavioral health treatment plan is a referral from the trusted family physician, preferably a Direct Primary Care provider, he highlights the importance of a referral for PAT from a provider with enough knowledge to pair up the patient with an estimable good fit. McCully says he has heard about a few employers that make this treatment available, noting that many first responders are aware of PAT and are incorporating it into plan offerings.
“The only way to offset the significant cost I estimate this treatment will run, it is only logical to have covered members contribute in the form of a deductible, co-pay or co-insurance,” he says.

Enthea counters this statement by demonstrating the cost-savings of ketamine-assisted therapy:

WHAT IS KETAMINE?
Ketamine is legal in the U.S. in all 50 states to clinically treat patients suffering from not only serious mental illness who have tried other medications with little or no relief, but also others who are struggling to a lesser severity.
Ketamine is a synthetic pharmaceutical compound, classified as a dissociative anesthetic. It is one of the most widely used drugs in modern medicine and is on the World Health organization’s List of Essential Medicines. It was developed in 1963, approved by the Food and Drug Administration for certain surgical procedures in 1970, and adopted by many hospitals and medical offices because of its rapid onset, proven safety, and short duration of action.
16 THE SELF-INSURER
Source: 2023 Enthea
Donald McCully

Is your payments solution delivering more to your bottom line? Expect more with ECHO® echohealthinc.com
Psychedelic Assisted Therapy
More recently, a growing body of research has found that lower doses of ketamine may be effective to treat a variety of mental health conditions. During the 1990s, investigators at the National Institute of Mental Health started to explore the antidepressant potential of ketamine while looking for alternatives to anti-depressants, commonly known as SSRIs and SNRIs.
In conjunction with this growing body of research, ketamine clinics and clinicians have proliferated across the United States, offering ketamine sessions for a range of psychiatric disorders either using ketamine-only treatments or ketamine in conjunction with psychotherapy (i.e., KAT).

Ketamine can induce a state of sedation -- feeling calm and relaxed – as well as relief from pain. Ketamine is an FDAapproved medical product as an injectable, short-acting anesthetic for use in humans and animals and esketamine (Spravato®; the active form of the drug) which was granted FDA-approval as a nasal spray for treatmentresistant depression.
(esketamine) nasal spray version (Spravato®) for treatment-resistant depression that is only available at a certified doctor's office or clinic.
According to Dr. Rome, “Unlike existing medicines, these compounds have a unique “neuroplastic” effect, meaning they put the brain in an unusually fresh, open and flexible state that is freed of longestablished assumptions and routines – ways of seeing things and experiencing ourselves, others and the world around us.”
He says to imagine the mind of a 2-year-old – curious, open, unburdened by anxiety and depressive thoughts:
In 1999, Ketamine became a Schedule III non-narcotic substance under the Controlled Substances Act. Ten years later, the FDA approved the S(+) enantiomer of Ketamine
18 THE SELF-INSURER
On average, aequum r esolves c laims within 297 days of p lacement aequum has generated a savings of 95.5% off disputed c harges f or self-funded pl ans aequum ha s ha ndled claims in all 50 states 297 95.5% 50 No Guarantee of Results – Outcomes depend upon many factors and no attorney can guarantee a particular outcome or similar positive result in any particular case. Protecting plans and patients across the U.S. 1111 Su perior A venue E ast Suite 1360 Cleveland, OH 44114 P 2 16-539-9370 www.aequumhealth. com
“Exploiting this neuroplastic effect combined with gently guiding talk therapy, many are finding lasting relief from depression, anxiety, PTSD and addictive disorders.”
KETAMINE-ASSISTED THERAPY (KAT)
KAT is a treatment that integrates prescribed doses of sub-anesthetic ketamine under the supervision of a clinician. Combined with integration sessions with KAT-trained therapists, this treatment improves mental health conditions. In low doses, ketamine can serve as an adjunct to psychotherapy, as it provides an opportunity for the temporary softening of psychological defenses, which may result in deeper self-reflection and psychotherapeutic processing.
Together, these components may help patients break long-standing, deeply ingrained thinking patterns associated with a variety of mental health conditions and, in turn, develop new ways of thinking and being. In this way, KAT involves the use of ketamine to enhance and deepen the therapeutic process, and the use of psychotherapy to amplify and prolong the curative effects of ketamine.
Ketamine is fast-acting and short-lived, making it very conducive to working with a therapist.

SEPTEMBER 2023 19 Psychedelic Assisted Therapy
Psychedelic Assisted Therapy
EMPLOYER ADOPTION OF PAT
A sure-fire sign that PAT has hit the self-funded community is the creation of Enthea as a TPA to help self-funded organizations, brokers, benefits consultants and other intermediaries with new choices, new and better ways to treat mental health issues that are apparent in the workplace.
Established in 2020 and thereafter re-organized as a Public Benefit Corporation, Enthea advocates for the safe and effective clinical use of psychedelics.
The Enthea approach is to offer employer-sponsored benefit plans new and better mental health treatment options that are proven to be safe. Standards of care emanate from Enthea’s evidenced-based medical policy, with treatment delivered through its proprietary network of KAT/ PAT therapists.
Sherry Rais, CEO and cofounder, Enthea, says, “Our goal is to make it easy for employers to expand their mental health package and offer psychedelic healthcare to their employees. Employers need and rely upon our developed protocols, guidelines and frameworks for integrating psychedelic therapy into their benefit program design. This practical perspective is vital for the industry as it moves towards broader adoption of psychedelic therapy.”

Rais points to Enthea data and scores over the past year which demonstrate the impact of KAT treatment for members:
• Post-traumatic stress disorder (PTSD) diagnosis reported an average of 86% symptom reduction
• Major depressive disorder (MDD) diagnosis reported an average of 67% symptom reduction
• General anxiety disorder (GAD) diagnosis reported an average of 65% symptom reduction.
“This is astounding considering that only 15% of people who use SSRIs find them highly effective, and the SSRIs, in contrast to ketamine therapy, come with many, many unwanted side effects,” says Rais.
POST TRAUMATIC STRESS DISORDER (PTSD)
PTSD is defined as a disorder that develops in some people who have experienced a shocking, scary, or dangerous event. Anyone can develop PTSD at any age, including combat veterans and people who have experienced or witnessed a physical or sexual assault, abuse, an accident, a disaster, or other serious events.
“As psychedelic treatments become better understood and widely accepted and practiced within healthcare, they will provide critical support to self-insured participants,” says Rais, noting that Enthea is building a nationwide network of credentialed providers. “We vet each clinic to ensure that they are staffed by credentialed PAT providers and follow guidelines that include:
• Evidence-based medical policies for psychedelic therapies that are regularly updated based on clinical developments and FDA approvals.
• Standards of care and credentials across the network to assure quality, positive patient experiences and positive treatment outcomes.
• Easy treatment authorization and reimbursements to providers, while shielding employers from Protected Health Information.
20 THE SELF-INSURER
Sherri Rais
Pharmaceutical Expertise Helps Clients Better Manage Costs

HM Insurance Group’s Pharmacy Operations Team Is Essential in Helping to Assess and Address Risk
Pharmacy expertise is critical to smart claims management, especially with high-cost gene therapies now entering the market regularly. The claims associated with these highcost treatment options can be catastrophic to self-funded employers without the right Stop Loss coverage in place.
Consider, for example, that a one-time infusion of Elevidys costs $3.2 million to treat a type of muscular dystrophy, and a one-time infusion of Hemgenix® costs $3.5 million to treat hemophilia B.1
That’s why HM Insurance Group (HM) has a Pharmacy Operations (RxOps) component among its Stop Loss solutions — to help with cost-containment opportunities, risk assessment, and client education.
Identifying Potential Financial Challenges
The RxOps team, led by our two expert PharmDs, watches the market and HM’s book of business to help anticipate how current and future advancements may impact financial risk for its client base in the current plan year and into the future. They review and audit current policies, monitor trends, and implement appropriate cost-saving techniques for specialty pharmaceuticals and gene and cell therapies.
Helping Clients Manage High-Cost Claims
Pharmaceutical developments continue to keep everyone — carriers, brokers, and employers alike — on alert, and HM has prioritized working together to better aid in managing claims expenses without compromising care, helping to achieve improved outcomes now and in the future.
Visit hmig.com to access a range of pharmacy-related informational publications, including our Pharmacy Focus articles, and other Stop Loss resources.
About HM Insurance Group
HM Insurance Group (HM) works to protect businesses from the financial risk associated with health care costs. A recognized leader in Employer Stop Loss, the company delivers protection for a range of group sizes. HM also offers Managed Care Reinsurance, including Provider Excess Loss and Health Plan Reinsurance, as well as accident and health specialty reinsurance.
HM Life Insurance Company, HM Life Insurance Company of New York and Highmark Casualty Insurance Company are all rated “A” (Excellent) by AM Best Company.* Through its insurance companies, HM Insurance Group holds insurance licenses in 50 states and the District of Columbia and maintains sales offices across the country.
For more information, contact your HM sales representative or visit hmig.com. MX2804006 (8/23) 800.328.5433 | hmig.com *AM Best Company, Best’s Rating Reports, August 2022. 1HM Insurance Group’s Pharmacy Focus: Elevidys – A New Gene Therapy for Duchenne Muscular Dystrophy (DMD), June 2023, hmig.com; and HM Insurance Group’s Pharmacy Focus: Hemgenix® – A New Gene Therapy for Hemophilia B, December 2022, hmig.com Stop Loss coverage is underwritten by HM Life Insurance Company, Pittsburgh, PA, in all states except New York under policy form series HMP-SL (08/19) or HMP-SL (06/20) or similar. In New York, Stop Loss coverage is underwritten by HM Life Insurance Company of New York, New York, NY, under policy form series HMP-SL (06/20) or similar. In all states except New York, Managed Care Reinsurance coverage is underwritten or reinsured by HM Life Insurance Company, Pittsburgh, PA, or Highmark Casualty Insurance Company, Pittsburgh, PA, under policy form series HM PEL 1105, HC PEL 1105, HMP PEL (08/19), HMP PEL (09/20), HML 1105 ELR, HMC 1105 ELR, HM 1005-ELR or similar. In New York, Managed Care Reinsurance coverage is underwritten under policy form series HMNY PEL 1105 or similar or reinsured by HM Life Insurance Company of New York, New York, NY.
Psychedelic Assisted Therapy
• A range of customizable options based on the company’s business and personnel needs.”
MICRODOSING OF PSYCHEDELIC SUBSTANCES
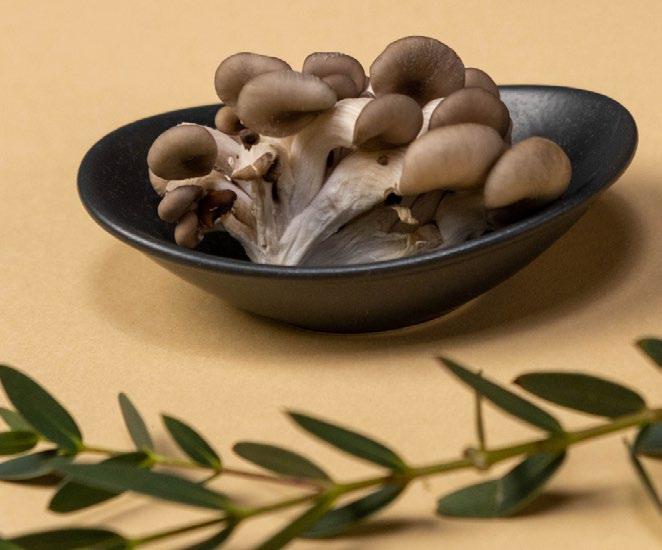
Microdosing involves taking sub-perceptual doses of psychedelic substances, such as psilocybin-containing mushrooms, in order to experience subtle cognitive and emotional benefits without the typical hallucinogenic effects associated with higher doses.
Psilocybin or magic mushrooms are naturally occurring and are consumed for their hallucinogenic effects. They are psychedelic drugs, which means they can affect all the senses, altering a person›s thinking, sense of time and emotions.
Robert A. Mines, Ph.D., Chairman and Chief Psychology Officer of MINES and Associates, an international business psychology firm providing behavioral health services for self-insured organizations, explains, “While there has been a growing interest in microdosing, it’s important to note that the scientific research on its effects and efficacy is still limited.”

Mines points to the “pros” of microdosing:
1. Enhanced Mood and Emotional Well-being: A study found that microdosers reported improvements in mood
Have you heard about our Premier Solution?
We’re partnering with local and national organizations to create customized plans that put the control back in employers’ hands.
The solution:
• Prevents unnecessary care
• Reduces plan spend
• Provides access to best-in-class providers
• Advocates for the members
• Distrups the status quo!
We love what we do. That’s the HPI difference.
22 THE SELF-INSURER
HPI Premier Solution HPI Premier Solution Healthcare navigation organizations Transparancy programs Local healthcare systems Member advocacy solutions
hpiTPA.com
Rober Mines
and emotional stability. Participants reported increased positive affect, reduced depressive symptoms, and enhanced emotional regulation.
2. Increased Creativity and Cognitive Flexibility: Research suggests that microdosing may enhance cognitive abilities associated with creativity. Microdosers reported improved divergent thinking, increased fluency, and enhanced cognitive flexibility, potentially leading to enhanced problem-solving skills.
3. Heightened Focus and Productivity: Microdosing has been associated with improved focus and concentration. Researchers found that microdosers reported increased energy levels and improved productivity, leading to enhanced work performance and efficiency.
4. Reduction in Anxiety and Stress: Preliminary evidence suggests that microdosing may have potential therapeutic effects on anxiety and stress. Researchers observed a reduction in anxiety symptoms among microdosers, indicating its potential as an alternative
approach for managing anxiety disorders.
Mines also cites some of the “cons”:
1. Lack of Standardized Protocols: One of the challenges with microdosing is the lack of standardized protocols. One study emphasized the need for careful dosage control, as individual responses to microdoses can vary. The absence of precise guidelines may lead to inconsistent effects and potential risks.
2. Potential Side Effects: While microdosing aims to avoid the acute psychedelic effects, some individuals may still experience side effects. One study reported increased irritability and restlessness in a subset of participants, suggesting the importance of monitoring individual responses to microdoses.
3. Legal and Regulatory Considerations: It’s important to note that the legal status of psilocybin-containing mushrooms varies across jurisdictions. In many places, their possession and use are still illegal. Individuals considering microdosing should be aware of the legal implications and potential risks involved.
4. Lack of Long-Term Safety Data: Although the existing research on microdosing is promising, the long-term safety and potential risks associated with prolonged microdosing are yet to be fully understood. Further research is needed to evaluate the potential long-term consequences and safety profile of microdosing practices.
“Microdosing with mushrooms has gained popularity due to anecdotal reports of positive experiences and potential benefits,” continues Mines. “While the available peer-reviewed literature on microdosing is still limited, it suggests potential advantages such as enhanced mood, creativity, and focus. However, it is essential to consider the lack of standardized protocols, potential side effects, legal considerations, and the need for long-term safety data.
Mines asserts that science advantages from an initial clinical observation and set of case studies through preliminary peer reviewed studies to gold standard double blind studies.
“Microdosing has received significant social media attention with many individuals self-microdosing and sharing their experiences,” he states. “How these experiences translate to treatment for depression, generalized anxiety or PTSD much less other conditions is unknown regarding the actual dosage levels. Furthermore, as in many areas of psychotropic medications, the actual causal pathways of deficiencies
SEPTEMBER 2023 23
Psychedelic Assisted Therapy
Bringing the Power of Consumerism to Healthcare
A first-of-its-kind healthcare SuperApp for self-funded plan sponsors that helps members make better decisions around quality medical care delivery, so everyone wins.


The only self-funded healthcare engagement platform of its kind.
Hercules Health rewards habitual app utilization by giving cash incentives earned through intelligent healthcare shopping tied to quality and cost. More app use equals more savings for members and plan sponsors alike.

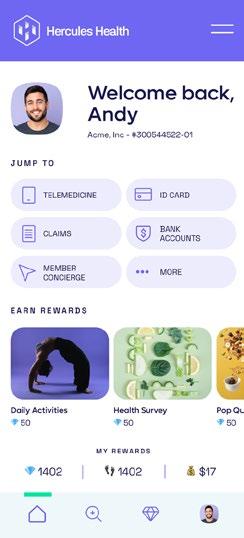
Comprehensive Compliance
Hercules Health delivers best-in-class price transparency that is fully compliant with the Transparency in Coverage (TiC) and the No Surprises Act (NSA) rules and regulations.
Contact us today.
info@herculeshealth.com herculeshealth.com
at the neurochemical level is not known in the research to date”
He says there are a number of correlational studies that associate improvement in symptoms with taking psilocybin. The basis for the effects could be a number of factors ranging from actual biochemical positive changes to placebo effects.
“We just do not know at this time,” he advises. “From the selfinsurance perspective, I suggest the industry proceed with its usual caution on experimental medications. It is premature to endorse the use of microdosing until the research clarifies what does may be effective -- assuming further research does support the next step related to effectiveness, for whom, and at what dose levels, plus long term effects, and for those who it may be contraindicated.”
COMPANIES INTRODUCE PAT
“By building a provider network for safe and legal clinical pathways to psychedelic therapy, Enthea services come at a critical time when self-funded companies recognize that mental health issues are significantly impacting the workplace in terms of employee wellness, attendance and productivity,” says Rais, referring to the companies
that offer PAT to their employees via the Enthea network:
Dr. Bronner’s
Dr. Bronner’s is leading the way as an early adopter and advocate of psychedelic medicine. The USbased, family-owned company expanded its healthcare benefits as a first step in prioritizing their support of employee mental health and wellness. Founded in the U.S. in 1948, Dr. Bronner’s is the top-selling natural brand of soap in North America and a leading brand worldwide.
“The health and wellbeing of our employees is the primary driver in how we think about benefits and compensation,” explains

For


SEPTEMBER 2023 25
product
Amalgamated Life Insurance Company Medical Stop Loss Insurance— The Essential, Excess Insurance Amalgamated Family of Companies Amalgamated Life ▲ Amalgamated Employee Benefits Administrators ▲ Amalgamated Medical Care Management ▲ Amalgamated Agency ▲ AliGraphics Group • Stop Loss • Voluntary Amalgamated Life Insurance Company 333 Westchester Avenue, White Plains, NY 10604 914.367.5000 • 866.975.4089 www.amalgamatedbenefits.com As a direct writer of Stop Loss Insurance, we have the Expertise, Resources and Contract Flexibility to meet your Organization’s Stop Loss needs. Amalgamated Life offers: VOLUNTARY SOLUTIONS—KEEPING PACE WITH TODAY’S NEEDS • Accident • AD&D • Critical Illness • ID Theft • Dental • Disability • Hearing • Whole Life Insurance • Specialty Rx Savings Programs and Discounts • “A” (Excellent) Rating from A.M. Best Company for 47 Consecutive Years • Licensed in all 50 States and the District of Columbia • Flexible Contract Terms • Legal • Portable Term Life • Excellent Claims Management Performance • Specific and Aggregate Stop Loss Options • Participating, Rate Cap and NNL Contract Terms Available Policy Form ALSLP-2020* *Features & form numbers may vary by state. A M BEST S A E F nan ia St ength Rat ng Psychedelic Assisted Therapy
information, contact: marketing@amalgamatedbene ts.com
Psychedelic Assisted Therapy
Michael Bronner, president, Dr. Bronner’s. “Offering coverage for ketamine-assisted therapy is in the interest of providing tools to our workforce to have the best quality of life and best options for mental health care.”
Dr. Bronner’s employees and their dependents receive assistance from Enthea, either electronically or by phone, to connect with a ketamine-assisted therapy provider. Once a patient/provider relationship is established, 100% of services are covered for Dr. Bronner’s benefit eligible employees.
Bronner continues, “Our family and Company are no strangers to depression and anxiety. We are deeply concerned about the mental health crisis society is facing, especially in the context of the Covid-19 pandemic. Considering all our advocacy on this issue, this employee benefit is the next logical step.”
Dr. Bronner’s supports a number of public education efforts, advocacy organizations, and political campaigns around the country working to advance the acceptance and availability of psychedelic-assisted therapy and medicines to treat depression, anxiety, PTSD, and other conditions.
PLEXIS Healthcare Systems
PLEXIS Healthcare Systems is a leading payer technology company delivering trusted enterprise core administration
and claims management solutions to healthcare payers and delivery systems worldwide. More than 100 organizations trust PLEXIS core administrative enterprise solutions to manage over 55 million lives in all 50 states and around the world. PLEXIS provides mission-critical solutions that catalyze efficiencies and connect evolving business ecosystems to a wide range of payer organizations.
“The reality is the vast majority of all illnesses and diseases are psychosomatic,” says Jorge Yant, founder and CEO, PLEXIS Healthcare Systems. There are things that we can heal with our minds just as much as we can create with our minds. And so, tools that help expand consciousness and help you see more clearly the truth of how things are will help you just naturally heal effortlessly.”
He says we’re just at the beginning, adding, “I see several reports from our insurance companies that give me a sense of the types of medications and the types of services, in general, that our employees and their family members are using. It’s shocking the number of people on antidepressants. Psychedelic therapeutics could change this dependency.”
Yant believes that KAT, if properly administered and applied in in the right setting, can be extremely helpful and useful to people, not only for mental illness issues, but also physical problems.
“We’re covering the cost of the benefit which is included our very rich benefits package,” he explains. “My aim is always to try to find new benefits to give our employees. A healthier healthy employee is a productive employee.”
PAT: A BETTER SOLUTION FOR MENTAL HEALTH
Novel Treatment Approach: Psychedelic therapy introduces a novel treatment approach that deviates from traditional pharmacological interventions. By combining the administration of psychedelic substances, such as psilocybin, MDMA, or LSD with prescribed dosage under doctor-supervision and with therapeutic support, this treatment offers a unique and potentially more effective way to address mental health conditions. This shift from symptom management to a more holistic, transformative approach can revolutionize the field of mental healthcare.
Breakthrough in Treatment-Resistant Conditions: Psychedelic therapy has shown remarkable efficacy in treating conditions that are often resistant to conventional treatments. For example, clinical trials have
26 THE SELF-INSURER
“You have become a key partner in our company’s attempt to fix what’s broken in our healthcare system.”
- CFO, Commercial Construction Company
“Our clients have grown accustomed to Berkley’s high level of customer service.”
- Broker
“The most significant advancement regarding true cost containment we’ve seen in years.”
- President, Group Captive Member Company
“EmCap has allowed us to take far more control of our health insurance costs than can be done in the fully insured market.”
- President, Group Captive Member Company
“With EmCap, our company has been able to control pricing volatility that we would have faced with traditional Stop Loss.”
- HR Executive, Group Captive Member Company
People are talking about Medical Stop Loss Group Captive solutions from Berkley Accident and Health. Our innovative EmCap® program can help employers with self-funded employee health plans to enjoy greater transparency, control, and stability.

Let’s discuss how we can help your clients reach their goals.
This example is illustrative only and not indicative of actual past or future results. Stop Loss is underwritten by Berkley Life and Health Insurance Company, a member company of W. R. Berkley Corporation and rated A+ (Superior) by A.M. Best, and involves the formation of a group captive insurance program that involves other employers and requires other legal entities. Berkley and its affiliates do not provide tax, legal, or regulatory advice concerning EmCap. You should seek appropriate tax, legal, regulatory, or other counsel regarding the EmCap program, including, but not limited to, counsel in the areas of ERISA, multiple employer welfare arrangements (MEWAs), taxation, and captives. EmCap is not available to all employers or in all states.
Stop Loss | Group Captives | Managed Care | Specialty Accident ©2022 Berkley Accident and Health, Hamilton Square, NJ 08690. All rights reserved. BAH AD2017-09 2/22 www.BerkleyAH.com
Psychedelic Assisted Therapy
demonstrated the potential of psychedelics in reducing symptoms of treatment-resistant depression, PTSD, addiction, and anxiety.
Accelerated Therapeutic Process: Psychedelic therapy has the potential to accelerate the therapeutic process by facilitating deep introspection, emotional breakthroughs, and heightened states of consciousness. The psychedelic experience can help individuals gain new perspectives, access repressed memories, and confront underlying emotional traumas. This accelerated process can potentially lead to profound insights, personal growth, and lasting therapeutic benefits in a shorter time frame compared to traditional therapy approaches.
Shift towards Personalized Medicine: Psychedelic therapy aligns with the growing emphasis on personalized medicine and patient-centered care. The treatment is tailored to the individual’s unique needs, focusing on their personal experiences, traumas, and aspirations. This personalized approach recognizes the multidimensional nature of mental health and aims to address the underlying causes rather than merely suppressing symptoms. The shift towards personalized medicine holds the potential to revolutionize the healthcare industry, leading to more tailored and effective treatments.
Subrogation Management
Potential Cost Savings: While the cost-effectiveness of psychedelic therapy is still being studied, early evidence suggests that it may lead to tremendous cost savings in the long term. Therapy
session costs are dependent on location, provider, and type of service, however, a typical session can range from $150-$400 per session.

By potentially reducing the need for long-term medication use, hospitalizations, and ongoing therapy sessions, PAT
Reach out for more information on how we can help your insurance business.

 Marie Noble, MBA, AIC VP of Subrogation Management
Marie Noble, MBA, AIC VP of Subrogation Management
Marie.Noble@us.davies-group.com
28 THE
SELF-INSURER
At Davies, we provide thorough investigations and subrogation support specifically tailored to all classes and entities within the insurance sector.
davies-group.com/us
has the potential to alleviate the financial burden on individuals and healthcare systems. Health economists are calculating a $25,000 savings per individual with effective treatment.
PAT: ADDRESSING MENTAL HEALTH TREATMENT ACCESS CHALLENGES
Accessing mental health services remains a challenge for employees. A recent report, based on a survey of 2,794 patients conducted by NORC, a nonpartisan research organization at the University of Chicago, found:
• More than half of patients (57%) who sought mental health or substance use care were unable to access any care on at least one occasion between January 2019 and April 2022.
• Of patients in employersponsored health plans, 39% reported using at least one out-of-network provider for mental health or substance use outpatient care, compared to just 15% for physical health care.
• Of patients using out-ofnetwork provider, 80%
reported using out-of-network mental health or substance use providers “all of the time” versus only 6% for physical health care.
• Even among patients who successfully made an appointment with a new in-network mental health or substance use provider, 40% had to contact four or more providers.
Immediate access to PAT can help employers to resolve these challenges by providing a meaningful solution that can be rapidly and cost-effectively implemented.
Laura Carabello holds a degree in Journalism from the Newhouse School of Communications at Syracuse University, is a recognized expert in medical travel, and is a widely published writer on healthcare issues. She is a Principal at CPR Strategic Marketing Communications. www.cpronline.com
SEPTEMBER 2023 29
Psychedelic
Therapy
Assisted
Psychedelic Assisted Therapy
Sources
https://www.thelancet.com/journals/lancet/article/PIIS01406736(10)61462-6/fulltext
Psychedelics for Therapy: What to Know About Benefits and RisksThe New York Times (nytimes.com)
https://www.nejm.org/doi/full/10.1056/nejmoa2032994
https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/ NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.pdf
https://www.nature.com/articles/s41586-023-06204-3
https://www.psychologytoday.com/us/basics/habit-formation
https://www.dea.gov/factsheets/ketamine
https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsdchecklist.asp#:~:text=The%20PCL%2D5%20is%20a,Making%20 a%20provisional%20PTSD%20diagnosis
https://www.psychiatry.org/psychiatrists/practice/dsm
https://adf.org.au/drug-facts/psilocybin/#:~:text=Psilocybin%20 or%20magic%20mushrooms%20are,sense%20of%20time%20 and%20emotions.
https://pubmed.ncbi.nlm.nih.gov/30604183/
https://pubmed.ncbi.nlm.nih.gov/31152167/
https://pubmed.ncbi.nlm.nih.gov/31778967/
https://pubmed.ncbi.nlm.nih.gov/30357434/
https://pubmed.ncbi.nlm.nih.gov/30478716/
https://www.psychologytoday.com/us/basics/ocd
https://www.psychologytoday.com/us/basics/alcohol
https://www.psychologytoday.com/us/basics/depression
https://www.psychologytoday.com/us/basics/shyness
https://www.psychologytoday.com/us/articles/201705/radical-newapproach-beating-addiction
https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC3363299/
https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC9053551/
https://jamanetwork.com/ journals/jamapsychiatry/ fullarticle/668195
https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC6767816/
https://www.ncbi.nlm.nih.gov/ books/NBK470357/
https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC8959757/
https://www.dea.gov/sites/ default/files/2020-06/ Ketamine-2020.pdf
https://norc.org/
https://www.maketheconnection. net/conditions/ptsd/
30 THE SELF-INSURER
ACA, HIPAA AND FEDERAL HEALTH BENEFIT MANDATES:
PRACTICAL Q & A

Q & A
TheAffordable Care Act (ACA), the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and other federal health benefit mandates (e.g., the Mental Health Parity Act, the Newborns and Mothers Health Protection Act, and the Women’s Health and Cancer Rights Act) dramatically impact the administration of self-insured health plans. This monthly column provides practical answers to administration questions and current guidance on ACA, HIPAA and other federal benefit mandates.
Attorneys John R. Hickman, Ashley Gillihan, Carolyn Smith, Ken Johnson, Amy Heppner, and Laurie Kirkwood provide the answers in this column. Mr. Hickman is partner in charge of the Health Benefits Practice with Alston & Bird, LLP, an Atlanta, New York, Los Angeles, Charlotte, Dallas and Washington, D.C. law firm. Ashley, Carolyn, Ken, Amy, and Laurie are senior members in the Health Benefits Practice. Answers are provided as general guidance on the subjects covered in the question and are not provided as legal advice to the questioner’s situation. Any legal issues should be reviewed by your legal counsel to apply the law to the particular facts of your situation. Readers are encouraged to send questions by E-MAIL to Mr. Hickman at john.hickman@alston.com.
SEPTEMBER 2023 31
AGENCIES ISSUE FAR-REACHING RULES RELATING TO MENTAL HEALTH PARITY COMPLIANCE OBLIGATIONS FOR NQTLS

On July 25, 2023, the tri-agencies (Internal Revenue Service, Department of Labor, and Department of Health and Human Services) released new proposed regulations under the Mental Health Parity and Addiction Equity Act (MHPAEA) that, if finalized, would provide significant clarifications and new compliance obligations for group health plans and issuers subject to the MHPAEA’s provisions. These rules are part of a Biden Administration push to improve access to in-network mental health care. Comments on the proposed rule will be due 60 days after publication in the Federal Register.
In addition to the Proposed Rules, the agencies released the second report to Congress on the MHPAEA comparative analysis for nonquantitative treatment limitations. This report for the first time, as required by the Consolidated Appropriations Act, 2021, names specific plans that were found by the agencies to not be compliant with the comparative analysis requirement.
BACKGROUND
Under current law, group health plans and health insurance issuers subject to the MHPAEA must comply with detailed compliance obligations for both quantitative treatment limitations (QTLs) and nonquantitative treatment limitations (NQTLs) that impact mental health and substance abuse disorder (MH/ SUD) benefits.
While guidance for the QTL obligations (such as monetary caps or limitations on the number of days of treatment) has been in place for some time, significant recent agency attention and guidance has addressed NQTL obligations (such as provider contracting, network

Get All the Tea on Advanced RBP Let’s talk more control, less cost. imagine360.com Your company’s health plan can do better. We promise. 32 THE SELF-INSURER
requirements, and utilization review). The Proposed Rules expand and clarify the NQTL requirements.
WHEN ARE THE NEW REQUIREMENTS EFFECTIVE?

If finalized as proposed, the new requirements would be generally effective starting the first plan year starting on or after January 1, 2025. However, certain clarifications of existing rules are currently effective.
WHAT ARE THE MAJOR PROPOSED RULE CHANGES FOR NQTLS?
Upon initial review, notable provisions include the following:
• Application of substantially all/ predominant test to NQTLs. The Proposed Rules require that the “substantially all/ predominant” test currently applicable to QTLs also apply to NQTLs. This means that for an MH/SUD NQTL to be permissible, it must apply to at least two-thirds of the medical benefits in the same classification (i.e., inpatient, in-network;
inpatient, out-of-network; outpatient, in-network; outpatient, out-of-network; emergency care; and prescription drugs). In addition, only the predominant (most frequent) variation of the NQTL can apply. This will likely significantly limit the issuer’s or plan’s ability to apply certain NQTLs, such as clinical utilization review techniques, to MH/SUD benefits.
• Meaningful benefit requirement. Under the Proposed Rules, if a plan provides any benefits for an MH/SUD condition in any classification of benefits, meaningful benefits for that MH/ SUD condition must be provided in every classification in which medical/surgical benefits are provided, as determined in comparison to the benefits provided for medical/surgical conditions in the classification.
• Design and application requirement. Under the Proposed Rules, NQTLs are subject to a new “design and application” requirement under which the NQTL analysis will also apply “in designing and applying the limitation.”
• Data gathering requirement as part of the NQTL process. There is a specific data collection requirement for network composition that “includes, but is not limited to, innetwork and out-of-network utilization rates (including data related to provider claim submissions), network adequacy metrics (including time and distance data, and data on providers accepting new patients), and provider reimbursement rates (including as compared to billed charges).”
SEPTEMBER 2023 33

The Technical Release issued at the same time as the Proposed Rules provides technical details, includes a request for information concerning this data gathering, and discusses a possible safe harbor on network composition based on this data gathering.
• For NQTLs other than network composition, a “material difference” in the metrics/data gathering for the NQTL as applied to MH/SUD and medical/surgical benefits would be a “strong indicator” of a violation, and the Proposed Rule details action that should be taken.
• As to network composition, the Proposed Rule goes beyond a “strong indicator” and provides that there would be an NQTL violation if “the relevant data show material differences in access to in-network mental health and substance use disorder benefits as compared to in-network medical/surgical benefits in a classification.”
• Further clarification on comparative analysis demonstrations. The Proposed Rules contain further detail on the contents of an NQTL comparative analysis and the timing to respond to a request for a comparative analysis from one of the agencies.
We will expand our analysis of these far-reaching rules in a forthcoming article.
Comprehensive self-funded plan management, including medical, dental, vision, COBRA, and reimbursement account administration combined with:



• Award-winning support
• Experienced, dedicated partnership and guidance

• Health plan performance management approach
• Optimized costs and health trends
• URAC-accredited UM and CM with in-house clinical team
SEPTEMBER 2023 35
YOUR SITUATION IS UNIQUE. YOUR HEALTH PLAN SHOULD BE TOO.
Looking for a better way? We’ll help you find it. AskNova@novahealthcare.com novahealthcare.com/services
2023 Nova Healthcare Administrators, Inc.
©
SIIA CONFERENCE EXPERTS LOOK AT 2023 TRENDS
Written By Caroline McDonald
Witha widening knowledge of captives and a greater need for them in an ever-changing environment, businesses and a growing number of insurance industry professionals are looking to captives for long term stability for their risks.

At SIIA’s 2023 National Conference, Oct. 8-10 in Phoenix, Arizona, industry experts will discuss different areas and trends in the captive insurance industry. Results of SIIA’s 2023 Captive Survey will also be released.
Some preliminary observations of conference panel experts are discussed below.
W
36 THE SELF-INSURER
EMERGING TRENDS
Bailey Roese, partner at Dentons Bingham Greenebaum LLP, who will serve on the panel for Emerging Trends in Captive Insurance, believes that captives are a well-established and valuable risk management tool.
“We are still seeing a lot of growth in the captive space,” she said. “I’m getting tons of calls.” This includes cyber and errors & emissions policies as well as growth in traditional coverages like general liability and property-casualty.
In the past, Roese said, “We had a niche of small captives, but we’re getting calls from larger insurers that want to form a bigger captive, so that speaks to the increased interest in captives.”
Their interest, she said, is partially driven by the hard market and the economy, “and certain lines of coverage disappearing in Florida and California, due to the extreme climate events we’re having.”
In hard-hit areas, insurers are pulling out of certain markets, because of extreme weather events and wildfires. “State Farm announced in January that it is stopping property coverage in Florida and has also exited the market in California,” Roese said.
This has led more companies to explore options to self-insure. “Captives are one of those options,” she said. “In the big picture I think there will continue to be a trend of more captives formed for property lines of coverage, and anything that is difficult to get in the commercial market for a consistent premium.” Added to that is the growing number of exclusions, Roese said.
Another trend, she noted, is the move away from § 831(b) captives –which have been targeted by the Internal Revenue Service – towards § 831(a). “It’s not clear whether the IRS will finalize rules surrounding § 831(b) captives as is or with some tweaks,” she said, “but we might see companies looking harder at whether they want to set up an § 831(b) or exit the one they have.
As it stands, she said, the only way to exit one “is to get a private letter ruling from the IRS, or they can wind down the captive. I think we will see people considering that. They can then start fresh with an § 831(a).”
Overall, “It’s an exciting time to be in the industry, it’s going to continue to grow,” Roese said. “It’s such a creative industry and people are always striving to answer questions, and it moves faster than the commercial market in response to emerging risks. It’s a great option for a lot of industries and businesses.”
UNDERSTANDING CAPTIVE STRUCTURE
Jeff Fitzgerald, vice president, employee benefits at Innovative Captive Strategies is a member of the panel, Understanding Captives: Structure, Risk and Ownership, which will discuss major issues facing captive owners, brokers, and captive management firms.
“While captive owners are more knowledgeable than they have been in the past,” he said, “The brokerage community is now the bigger driver of people’s participation in captives.” Brokers, he said, “are much more aware of captives as an option and more comfortable presenting them to their clients.”
Informed brokers know that captives are a viable option, “and for some clients it’s the primary option,” Fitzgerald said.
The vast majority of growth in the captive space, he added, has been through smaller groups moving into group captives. “Five or 10 years ago, the questions were about the captive—is it sustainable, is it something I can trust, what happens if we have a bad year?” he said, “Now, I hear that somebody who is already looking at one type of captive wants to know how it compares to another.”
The current situation is, less about explaining the basics of the captive, “and more about comparing what else is out there in the captive world or in the larger self-funded world,” Fitzgerald said.
SEPTEMBER 2023 37
IF YOU PLAN PLANNING TIME WITH YOUR PLANNER
We know what it’s like to feel FOMA, or Fear Of Missing Anything. That’s why we invented Curv®, so you can zero in on catastrophic claims risks with the industry’s most predictive and trusted risk score, making it easier than ever to see more stop loss risks and opportunities—and competitively price plans across your spectrum of underwritten groups.

Traditionally the type of captive used is determined by the type of risk that it will cover, he said. “Captives are a broad term that covers a lot of risks, a lot of different opportunities and a lot of industries.”
Currently, most people’s conception of a captive is very specific to their past experience. “So, one of the things that’s interesting on the SIIA captive committee is that we have two very related, but individualized groups that we try to support,” Fitzgerald said.
One group are those involved in the medical stop loss fund management, “The others are what we call enterprise risk captive arrangements, which is really more about balancing the risk that individual companies face, that they can’t find in the marketplace,” he said.

He noted that the two populations are both using single captives and are both self-insured, “but the risks up front that they are being used for are very different.”
So, the first questions he asks those considering a captive, are “What is your concern, your pain and your frustration?” He said. “And then seeing if there is a captive out there that can solve it, or that we can create for them.”
DOMICILES AND REGULATION
When considering regulation or a domicile, Fitzgerald said, the domicile’s location doesn’t make a big difference. Some domicile meetings, for example, are
beneficial, but attendance at every meeting isn’t a necessity.
The most important thing, he said, is how well the regulator understands what the captive is set up to achieve, “because there are multiple ways these issues can be looked at.”
Most importantly, he said, is that “most people, including regulatory bodies and many in the insurance agency world don’t understand selfinsurance.”
So, while self-insurance is broader than the captive world, “it all is under the same umbrella. Self-insurance has been around for a long time,” Fitzgerald said.
he said. “So, the more the larger population, including regulatory bodies, agencies and the general public, understands that there is a self-insurance option for them, the more the perceptions of captives can be clarified.”
SEPTEMBER 2023 39
“There are multiple risks self-insurance can cover and the majority of the time, once somebody does self-insure, they are appreciative that they did,”
We Know ... Risk
We study it, research it, speak on it, share insights on it and pioneer new ways to manage it. With underwriters who have many years of experience as well as deep specialty and technical expertise, we’re proud to be known as experts in understanding risk. We continually search for fresh approaches, respond proactively to market changes, and bring new flexibility to our products. Our clients have been benefiting from our expertise for over 45 years. To be prepared for what tomorrow brings, contact us for all your medical stop loss and organ transplant needs.


Visit us online at tmhcc.com/life Tokio Marine HCC - Stop Loss Group A member of the Tokio Marine HCC Group of Companies TMHCC1189 - 09/2023 HCC Life Insurance Company operating as Tokio Marine HCC - Stop Loss Group
SIIA CAPTIVE SURVEY
SIIA’s 2023 survey results will be released at the annual conference in October. The survey is designed to increase knowledge and understanding of the captive insurance industry.
Questions for service providers include the areas of interest in captive use, types of and numbers of structures formed most, numbers of closures, areas of growth, numbers of captives redomiciled and where they are domiciled.
Questions for captive owners include how they first heard of captives, how many captives they have set up for business, the risks covered, the type of captive formed, whether they were able to find coverage for their risk in the commercial market, and their board meetings.
Prospective owners’ questions include the company’s gross revenues, number of employees, hurdles encountered when looking at a captive and unusual risks that insurers cannot or will not cover.
HIGHLLIGHTS FROM SIIA’S 2022 SURVEY
• Captive formation growth significantly outpaced captive closures, with survey results showing positive signs for the industry.
• A sharp increase in the average number of captives under management was shown, reflecting growing confidence in the captive model.
• A wide range was seen in the total captive premium amount, raising questions about the disparity.
• 36% of captives reported COVID-related claims in the past year.
• The average COVID-related claim amount was down.
• IRS audits were slightly lower.
• Roughly 40% of respondents had clients settle with the IRS.
• 66.7% of respondents reported adding staff in the past year–including a significant number of legal specialists.
Caroline McDonald is an award-winning journalist who has reported on a wide variety of insurance topics. Her beat has included in-depth coverage of risk management and captives.
SEPTEMBER 2023 41
3M MASS TORT SETTLEMENT REMINDS US THAT SUBROGATION MATTERS
Written By Ron E. Peck
OnThursday, June 22, 3M followed other companies’ example by announcing that it had reached an agreement to settle claims that their polyfluoroalkyl and perfluoroalkyl substances (PFAS), known as “forever chemicals,” had contaminated water supplies in the United States.
Specifically, the settlement will see 3M pay up to $10.3 billion over 13 years to municipalities in the U.S. that have detected these chemicals in their drinking water. This is only the most recent in a series of settlements regarding water contamination by PFAS producers, who also announced that they would pay over $1 billion to settle similar lawsuits; with this likely heralding a new series of litigation and settlements, akin to the well-known asbestos proceedings.

O
42 THE SELF-INSURER
Many are familiar with the recent advent of PFAS testing conducted by municipal water authorities, and the resultant identification of unacceptable PFAS levels in drinking water. This in turn led to various lengthy and costly remediation procedures, to remove the offending chemicals from public drinking water.
The aforementioned settlement is primarily meant to address abatement claims, compensating municipalities for damage suffered to property and costs incurred in said remediation projects.
As entities funding and/or servicing self-funded health benefit plans, the importance and relevance of this news to our industry cannot be overstated. That is because these settlements are not focused on potential illness caused by exposure to and consumption of PFAS chemicals, nor do they resolve what promises to be a substantial number of medical claims.
The lawsuits and settlements we are witnessing now are more likely than not just the tip of the iceberg. That is why it is so important for health benefit plans to act now and assert their and their participants’ rights – at the beginning of what promises to be a long process.
Furthermore, this type of lawsuit – and opportunity – is not unique. Class actions, and the lesser-known toxic tort and mass tort cases, represent substantial chances for health benefit plans to recoup funds they had previously paid – sometimes years prior – through specialized subrogation.
As a refresher, whenever a third party causes – or potentially causes – an illness or injury to a participant of a health benefit plan, and that plan pays to treat those illnesses or injuries, subrogation enables the aforementioned benefit plan to either “step into the shoes” of the injured participant – and pursue a claim against the liable third party –or, seek to recoup what the plan paid from the plan participant; (after that participant has recovered from a liable third party funds that are meant to pay for illness or injuries that are deemed to be the liable third party’s responsibility, but were already paid by the plan).
Subrogation is a legal concept grounded in fairness. It is one of those few rights, supported by both statute and equity, that has repeatedly withstood judicial review at every level.
The reason why subrogation is so durable is because society recognizes the justice inherent in ensuring parties pay for the damages they cause; guaranteeing that victims and their health benefit plans are not left paying for damages caused by someone else.
The most common and recognizable “type” of subrogation case usually involves one victim, one liable party, and one incident. These often take the form of a car accident, slip and fall at a place of
business, or injury at one’s place of employment… resulting in subrogation against automobile insurance carriers, businesses, and workers’ compensation. There exist other types of subrogation cases which, despite being far less common, represent a massive opportunity for health benefit plans and their participants to recoup substantial funds. These cases are often called class action, toxic tort, or mass tort cases, and they occur when a substantial entity – such as 3M – is deemed to be responsible (or avoids liability through settlement) for injuries or illnesses caused to a large population over a meaningful period.
These lawsuits usually occur in Federal Court, following consolidation into multi-district litigation (“MDL”) by the judicial panel on multidistrict litigation (“JPML”). As a result, there are many plaintiffs involved, at least one – but sometimes more than one – sizeable defendant organization, and a lot of money at stake.
Identifying such subrogation opportunities is no easy feat. Unlike a motor vehicle accident – where the accident, injury, and treatment all occur within days (if not hours) of each other –with mass torts, exposure to the hazard, development of the illness or injury, identification of the link between the two, and filing of the case can take years or even decades to unfold.
SEPTERMBER 2023 43
Your employer stop loss partner
A true partnership means you have a passionate team of experts who collaborate with you to bring cost effective solutions for managing your medical risk. Our streamlined organizational structure creates a quick and transparent decision-making process – because the best solutions should come without red tape.
Discover the advantages of true partnership. www.partnerre.com/health

That means plans and their service providers must remain aware of developing cases, know which conditions are deemed to be caused by the accused tortfeasors, and exercise a capacity to audit old claims to flag treatments that are indicative of said conditions, before investigating whether the affected participants encountered the accused tortfeasors’ substance or device in question.
Is it worth the effort? Absolutely. Setting aside the tremendous plan funds at stake, consider also every plan administrator’s fiduciary duty to prudently manage plan assets and enforce the terms of the plan. As such, it is arguably every plan administrator’s duty to investigate and pursue such cases.
Admittedly, it requires more sophistication than most plan sponsors and even third-party administrators may possess; but fortunately, fiduciaries can satisfy their duty by utilizing agents acting on their behalf.

HOW MUCH IS AT STAKE, AND WHAT DO THESE CASES LOOK LIKE?
In June of 2012, the FDA announced a voluntary recall of Stryker Orthopedics’ Rejuvenate Modular-Neck and ABG II ModularNeck Hip Stems. Litigation ensued, and a subsequent settlement followed. In total, the proceedings only addressed an estimated 20% of the failed devices, meaning an estimated 80% of the episodes were not addressed.
This is particularly worrisome, given that just the revision surgeries associated with the removal of the recalled devices cost health plans approximately $45,000.00 per procedure.
Similarly, another case involved the Exactech knee replacement systems. Like Stryker, Exactech launched a recall in February of 2022 of more than 140,000 Optetrak, Optetrak Logic and Truliant knee replacement systems, after it discovered a defect in its packaging that exposed a polyethylene insert component to oxygen.
Focused on Clients. Dedicated to Results. Our Complex Claim Consulting Practice is committed to making your business better. www.lockton.com We have a team of Clinicians and risk managers working to simplify your most complex claims In s u ran ce • R isk Manag e m e n t • S u re ty Ex p ert i s e 2100 Ross Ave. Suite 1200 W E L I V E SE RV I C E ! Dallas, TX 75201 • 214.969.6100 © 2021 Lockton Companies A rights eserved Medical Benefits Complex Claims Pharmacy Analytics Risk Management
SEPTEMBER 2023 45
A lawsuit was filed, with 27 complaints pending in 11 different federal district courts – as well as a motion to centralize the cases. Again, this represents only a fraction of the estimated patients and health plans that expended money to pay for procedures that should be funded by Exactech. Likewise, in 2002, a study suggested that the long-term use of Wyeth Pharmaceuticals’ Prempro (a hormone therapy drug used to treat menopausal symptoms) significantly increased the likelihood of developing breast cancer.

After several years of litigation, a settlement was reached to pay patients who developed hormone-receptor positive breast cancer¹, however, only about 10,000 individuals² (a mere 5% of the estimated 200,000 women who developed this type of breast cancer), ever asserted a claim.
The average cost in these instances is estimated to be $50,000,³ meaning that the unrecovered medical expenses associated with treating breast cancers caused by Prempro and similar drugs –payments made by health plans – are estimated to exceed $9.5 billion. These, along with other examples – such as the Chantix recall, Paragard IUDs lawsuits, and Elmiron MDL – represent billions of dollars spent by health plans, and only a fraction in reimbursement being paid back.
Finally, many readers are likely familiar with the recent lawsuits involving RoundUp. In 2015 the World Health Organization’s (WHO) International Agency for Research on Cancer classified glyphosate – a key component of RoundUp – as a probable cancercausing agent.
Additional research over the years subsequently suggested that RoundUp exposure increases the risk of developing NonHodgkin’s Lymphoma and other cancers. As with the other examples of mass tort described herein, here too the matter became an MDL, instituted by the Federal Courts.
Some claims have settled, whilst many others remain open.
Specifically, as of December
46 THE SELF-INSURER
Ringmaster is dedicated to developing cloud-based software that will improve your Stop-Loss and PBM administration and the reporting capabilities for Carriers, Managing General Underwriters (MGUs), Third Party Administrators (TPAs), Brokers and PBMs.

By automating the manual processes, you will:
• Reduce processing time and complexity
• Access extensive data warehouse
• Receive real-time actionable analytics
• Minimize turn-around time
330.648.3700 • rmtsales@ringmastertech.com
www.ringmastertech.com Step Into the Ring and Start Realizing the Possibilities by Utilizing Ringmaster’s Cloud-Based Solutions to Make Your Business Thrive!
to one destination to connect partners across the entire PBM & Stop-Loss ecosystem. Start Realizing the Possibilities!
•
Come
2022, Bayer reached an agreement to settle about 100,000 cases, with $10.9 billion being paid out.
These are just a few examples of mass tort cases. Looking again at the recent claims involving PFAS, chemical seepage into drinking water may not be the only target for mass tort consideration. PFAS that is present in household items may soon also become a subject of litigation, including items which may more easily introduce potentially harmful substances into human bodies – such as feminine hygiene products and baby wipes.

Likewise, extensive use of PFAS chemicals by airports, firefighters, and all divisions of the military, promises to result in more claims and more damages arising from this issue. The amount of potential
recovery health benefit plans could be pursuing are substantial and meaningful.
These assets, once returned to the plan, could be used to fund other claims and simultaneously prevent contribution, co-pay, and deductible increases. It therefore behooves all self-funded plans, administrators, and fiduciaries to investigate what their plans are doing to identify and manage these types of claims.
How does this impact self-funded health benefit plans, and the entities that service them?
Great question. In a word: money.
These types of cases almost always impact numerous participants, and result in a lot of funds changing hands. Self-funded benefit plans almost certainly have spent substantial amounts of plan assets on treatments about which these cases relate.
Every plan administrator has a fiduciary duty to identify opportunities to recoup such funds for their plan. The question, then, is how to do it.
With traditional subrogation and third-party liability work, the process is fairly straightforward. You monitor claims as they come in, and flag those that – based on a diagnosis code – tend to relate to an accident or injury which, more often than not, entails third party liability.
48 THE SELF-INSURER
In other words, if claims arrive for a broken bone, an ambulance, whip lash, facial injuries, and other similar trauma codes – all within the same 24 to 48 hour period – it’s a safe bet that these injuries all relate to one accident for which a third party may be responsible. With mass tort claims, however, it’s much less straightforward.
In 2015, a plan member may have incurred $200,000 in claims for the treatment of Non-Hodgkin’s Lymphoma. In 2015, there was no reason to think these claims relate in any way to third party liability.
Then, in 2020, someone proves that the use of a chemical herbicide causes Non-Hodgkin’s Lymphoma.
Then, in 2022, a lawsuit is filed against the producer of said herbicide. To maximize this opportunity, self-funded plans must themselves – or with a partner – monitor instances like this, where some substance or product is tied to an illness or injury.
When instances like this arise, the plan – or their partners –must then identify the illness or injury caused by the substance or product and audit their historical claims to identify if and when participants treated for (and the plan paid for) such illness or injury.
Then, they must communicate with the impacted participant, or their family, to identify if that
patient came in contact with the substance or product in question.
Then (phew) the plan or the plan’s partner must work with the attorney’s managing the mass tort case, to assert the plan – and if at the patient’s behest, the patient’s – rights. It’s not easy, but with the right process and partners in place, it is more than worth it.
Sources:
¹ Feeley, Jef, Pfizer Paid $896 Million in Prempro Settlement, Bloomberg Business, June 19, 2012
² Id.
³ See e.g. Campbell, J.D. and Ramsey, S.D. The Costs of Treating Breast Cancer in the US: a Synthesis of Published
Evidence, Pharmacoeconomics 2009 27(3): 199-209. (“The estimates of lifetime per-patient costs of breast cancer ranged from $US20 000 to $US100 000.”)
SEPTEMBER 2023 49
SIIA ENDEAVORS S
SIIA’S 43RD NATIONAL EDUCATIONAL CONFERENCE & EXPO
WILL BE OCTOBER 8-10TH AT THE JW MARRIOTT DESERT RIDGE RESORT & SPA IN PHOENIX, AZ.

Drawing thousands of thought leaders, innovators and product/ service providers, SIIA’s National Conference is widely accepted as the self-insured and captive industry’s largest and most influential gathering of industry professionals.
Attendees representing multiple industry sectors including Employers, TPAs, Brokers, Captive Managers, Stop-Loss Carriers, and Solution Providers connect to learn from experts, build relationships and explore cutting-edge solutions.
ENDEAVORS
50 THE SELF-INSURER
We should note that SIIA produces this event for the benefit of registered attendees. To ensure this exclusive value, access to most of the host hotel space, including the lobby bar, will be restricted to registered attendees during conference hours…another important reason to sign up now if you have not already done so.
With over 1,500 attendees already registered, this year’s National Conference promises to be one of the best attended in our history!
NETWORKING OPPORTUNITIES HIGHLIGHTS
Golf Tournament
You are invited to participate in the annual fundraising event to benefit the Self-Insurance Educational Foundation (SIEF)!
SIEF is a 501 C3 non-profit organization affiliated with SIIA. Its mission is to raise the awareness and understanding of self-insurance among the business community, policymakers, consumers, the media and other interested parties. SIEF is dedicated to providing the tools and resources needed to promote self-funding.
The SIEF Golf Tournament Fundraiser, scheduled on October 8th at the Wildfire Golf Club, is open to all conference registrants and promises to be an excellent opportunity to network with executive-level industry colleagues and peers.
Registration for the SIIA Conference is required to participate in the tournament, and golf fees are not included in conference registration fees.
Golf Tournament fees include green fees for 18 holes, golf cart, grab & go breakfast and lunch, beverages, and various prizes. Golf clubs can be rented and picked up from the Pro Shop on the morning of the tournament.

SEPTEMBER 2023 51 ENDEAVORS
Depend on Sun Life to help you manage risk and help your employees live healthier lives

By supporting people in the moments that matter, we can improve health outcomes and help employers manage costs.
For over 40 years, self-funded employers have trusted Sun Life to help them manage financial risk. But we know that behind every claim is a person facing a health challenge and we are ready to do more to help people navigate complicated healthcare decisions and achieve better health outcomes. Sun Life now offers care navigation and health advocacy services through Health Navigator, to help your employees and their families get the right care at the right time – and help you save money. Let us support you with innovative health and risk solutions for your business. It is time to rethink what you expect from your stop-loss partner.
Ask your Sun Life Stop-Loss Specialist about what is new at Sun Life.
The content on this page is not approved for use in New Mexico. For current financial ratings of underwriting companies by independent rating agencies, visit our corporate website at www.sunlife.com. For more information about Sun Life products, visit www.sunlife.com/us. Stop-Loss policies are underwritten by Sun Life Assurance Company of Canada (Wellesley Hills, MA) in all states except New York, under Policy Form Series 07-SL REV 7-12. In New York, Stop-Loss policies are underwritten by Sun Life and Health Insurance Company (U.S.) (Lansing, MI) under Policy Form Series 07-NYSL REV 7-12. Product offerings may not be available in all states and may vary depending on state laws and regulations. © 2023 Sun Life Assurance Company of Canada, Wellesley Hills, MA 02481. All rights reserved. Sun Life and the globe symbol are trademarks of Sun Life Assurance Company of Canada. Visit us at www.sunlife.com/us. BRAD-6503-y SLPC 29427 01/22 (exp. 01/24)
Don’t miss this exclusive opportunity to better your handicap, refine your putting skills and support the foundation dedicated to ensuring the development of tomorrow’s leaders in the self-insurance/ captive industry.

SIPAC TAILGATE & CRAFT BEER LUNCHEON
Please join us for a networking luncheon benefiting the SelfInsurance Political Action Committee (SIPAC).
The event is being held at the Meritage Restaurant - JW Marriott Desert Ridge and is open to all SIIA members. A contribution to SIPAC is required to attend the event. There will be lunch, drinks, and games provided.
For more information, please contact Anthony M. Murrello at amurrello@siia.org or (732) 853-5825. RSVPs are requested at least 10 days prior to the event.
Contributions to SIPAC are used for political purposes and are not tax deductible for federal income tax purposes. All contributions to SIPAC are voluntary and must be made with personal funds. Federal law prohibits contributions from corporations. You may refuse to contribute without reprisal. SIPAC will not favor or disadvantage anyone by reason of the amount contributed or the decision not to contribute. SIPAC participants must be US citizens or permanent resident aliens.
ENDEAVORS
SEPTEMBER 2023 53
ENDEAVORS
BLUE EAGLE LOUNGE
The Blue Eagle Lounge is back! Located in the foyer between the Exhibit Hall and Main Ballroom, this is the place for attendees to relax between sessions, chat with friends or take a load off after roaming the Exhibit Hall.
SIIA FUTURE LEADERS RECEPTION - CORNHOLE TOURNAMENT
Future Leaders will set aside their knowledge of self-insurance for a night to focus on competing in SIIA’s Inaugural Cornhole Tournament. The competition will be center stage during the opening night reception on Sage Court located outside the lobby bar. Teams of two will square off for trophies and bragging rights as SIIA 23 Cornhole Champions!
HULLABALOO 2 - NATIONAL CONFERENCE PARTY
Last year’s conference party was on fire…literally!! A huge fire pit and a fire engine shooting balls of fire 30’ into the air lit up a night of music and fun. This year we’re keeping with Hullabaloo’s festival environment with new and exciting entertainers, a band that will get you movin’ on the dance floor, and relaxed atmosphere to close out the conference. It’s not just a Hullabaloo…it’s HULLABALOO 2!
We look forward to seeing you in Phoenix! For more information, including registration, please visit www.siia.org.
Schedule-At-A-Glance:
Sunday, October 8
7:30 AM - 7:00 PM Conference Registration
8:00 AM - 12:30 PM Golf Tournament Fundraiser
Monday, October 9
Eagle Lounge 8:30 AM - 10:00 AM
Address: Planning For AI-Powered Organizations 10:00 AM - 10:15 AM Networking Break
10:15 AM - 11:30 AM Emerging Trends Impacting the Employer Stop-Loss Market
10:15 AM - 11:30 AM Emerging Trends in Captive Insurance 11:00 AM - 5:00 PM Lobby Bar
11:30 AM - 1:30 PM Luncheon / Exhibit Hall Open
1:30 PM - 2:45 PM SIIA Captive Insurance Industry Survey Results
1:30 PM - 2:45 PM Understanding Employer Expectations – The Boomer and Gen-X Perspectives
1:30 PM - 2:45 PM What’s Going Right & Wrong with Federal Price Transparency?
2:45 PM - 3:00 PM Networking Break
3:15 PM - 4:30 PM Health Systems and Self-Insured Payers – An Evolving Relationship
3:15 PM - 4:30 PM Specialty Pharmaceuticals: Remedy the Pain Points for Self-Insured Employers
3:15 PM - 4:30 PM Surprise Medical Billing and the Federal IDR Process: How’s It Going?
4:30 PM - 6:30 PM Evening Reception /Exhibit Hall Open
8:00 PM - 10:00 PM SIIA Future Leaders Reception - Cornhole Tournament
54 THE SELF-INSURER
2:30 PM - 4:30 PM SIPAC Tailgate & Craft Beer Luncheon 5:00 PM - 7:00 PM Welcome Reception / Exhibit Hall Open
7:00
Conference
Continental
Blue
AM - 7:00 PM
Registration 7:30 AM - 8:30 AM
Breakfast 7:30 AM - 5:00 PM
Keynote


Tuesday, October 10 7:00 AM - 4:00 PM Conference Registration 7:30 AM - 8:30 AM Continental Breakfast 7:30 AM - 10:00 AM Power Breakfast Meeting Time 7:30 AM - 5:00 PM Blue Eagle Lounge 10:15 AM - 11:30 AM Gag Clauses and Fiduciary Responsibilities: Where’s Our Claims Data? 10:15 AM - 11:30 AM The Artificially Intelligent TPA 10:15 AM - 11:30 AM Understanding Captives: Structure, Risk and Ownership 11:00 AM - 5:00 PM Lobby Bar 11:30 AM - 1:30 PM Luncheon / Exhibit Hall Open 1:30 PM - 2:45 PM Charting Successful Careers in the Self-Insurance Industry 1:30 PM - 2:45 PM Self-Insured Employer Strategies for Managing Oncology Care 2:45 PM - 3:15 PM Networking Break 3:15 PM - 4:30 PM Empowering Plan Participants to Leverage Cost Containment Strategies 3:15 PM - 4:30 PM SIIA Legislative & Regulatory Update 3:15 PM - 4:30 PM What’s Next for Employer Digital Health Strategies 7:30 PM - 10:00 PM Hullabaloo 2 - National Conference Party
times are listed in Mountain Time. Our Stop Loss Insurance mitigates the impact of devastating medical claims through flexible contracts, customizable plans and a consultative, client-focused approach. With more than 40 years of industry experience, we provide unparalleled guidance and protection for businesses – whether you’re carving out Stop Loss for the first time or an experienced client looking for cost containment. Trust the provider that’s stopped loss over and over again: visit voyastoploss.com for more information Stop Loss Insurance is underwritten by ReliaStar Life Insurance Company (Minneapolis, MN) and ReliaStar Life Insurance Company of New York (Woodbury, NY). Within the State of New York, only ReliaStar Life Insurance Company of New York is admitted, and its products issued. Both are members of the Voya® family of companies. Voya Employee Benefits is a division of both companies. Product availability and specific provisions may vary by state. ©2022 Voya Services Company. All rights reserved. 2225973 204657-06012022 Steadfast protection for the unpredictable Stop Loss coverage that weathers any storm SEPTEMBER 2023 55 ENDEAVORS
*All

Partner with Nationwide® to simplify Medical Stop Loss for you and your clients. Save time and effort with easy access to experienced underwriters who offer a broad range of solutions. Our flexible plans are tailored to fit your clients’ needs and reduce future risk. Plus, claims are backed by a carrier with A+ financial ratings.* Offer coverage from a brand clients can trust. Nationwide has been in the health business for 80 years and Medical Stop Loss for nearly 20 years. To learn why top Medical Stop Loss producers and underwriters choose Nationwide, call 1-888-674-0385 or email stoploss@nationwide.com We hope to see you at the SIIA National Conference. *A+ ranking from AM Best received 10/17/02, affirmed 12/1/22, and A+ ranking from Standard & Poor’s received 12/22/08, affirmed 4/19/22. Plans are underwritten by Nationwide Life Insurance Company, Columbus, Ohio 43215. Nationwide, the Nationwide N and Eagle, and Nationwide is on your side are service marks of Nationwide Mutual Insurance Company. © 2023 Nationwide NSV-0113AO.1 (06/23) Strong relationships. More solutions.
NEWS FROM SIIA MEMBERS
2023 SEPTEMBER MEMBER NEWS
SIIA Diamond, Gold, and Silver member companies are leaders in the self-insurance/captive insurance marketplace. Provided below are news highlights from these upgraded members. News items should be submitted to membernews@siia.org.

All submissions are subject to editing for brevity. Information about upgraded memberships can be accessed online at www.siia.org.
If you would like to learn more about the benefits of SIIA’s premium memberships, please contact Jennifer Ivy at jivy@siia.org.
SEPTEMBER 2023 57
NEWS
DIAMOND MEMBERS
AMWINS ANNOUNCES NEW HIRES JOINING STEALTH PARTNER GROUP AND AMWINS GROUP BENEFITS
CHARLOTTE, NC -- Amwins, a global distributor of specialty insurance products and services, announced three new additions to the firm. Brad Mathews and Todd Marcoux will be joining the sales team at Stealth Partner Group, the largest stop-loss wholesaler in the U.S., and Kathy Phillips will be joining the ancillary practice team for Amwins’ Group Benefits division, a leading provider of employee benefits products and services.
Brad Mathews will serve as vice president working in the southeast region and based out of Tampa. After graduating from the University of Georgia with a finance and risk management degree in 2006, Brad moved to Tampa and began his career with Genworth Financial which was acquired by Sun Life Financial in 2007.
Brad considers the highlight of his sales career being inducted into the Sun Life Distribution Hall of Fame in 2017. He has a passion for finance and has held his Certified Financial Planner (CFP) designation for more than 10 years.
Todd Marcoux will serve as vice president working in the
northeast region and based out of Boston. Todd earned his MBA from the University of Massachusetts and began his insurance career in 1993, bringing 30 years of industry experience to Stealth Partner Group. He spent the last 16 years with Tokio Marine HCC as vice president and manager for the northeast and mid-Atlantic territories.
“We are delighted to bring Brad and Todd on board,” said Harley Barnes, chief executive officer at Stealth Partner Group. “They have a tremendous level of experience and expertise that will enhance our ability to provide best-in-class support to our clients, carriers and retail broker partners.”
Kathy Phillips will serve as senior vice president and Ancillary Benefits national practice leader. With over 30 years of experience, she brings a wealth of knowledge and expertise in life, disability, extended sick bank transformation, supplemental health, dental and leave administration.
Kathy was a top-producing ancillary insurance wholesaler at Lincoln Financial Group, focusing on helping clients find solutions to their benefits challenges. She is a highly sought-after expert in the field, and her unwavering commitment to providing superior service and building strong, lasting relationships was a cornerstone of her 27 year tenure at Lincoln Financial Group.
“With her proven expertise in ancillary benefits, Kathy is a great asset to our growth strategy and ongoing mission to provide industryleading broker and client support,” said Riva Dumeny, chief operating officer at Amwins Group Benefits. “Kathy is an innovative leader, and we are looking forward to sharing the developments she brings to our products, services and carrier relationships.”
About Amwins
Amwins is the largest independent wholesale distributor of specialty insurance products in the U.S. dedicated to serving retail insurance agents by providing property and casualty products, specialty group benefit products, and administrative services. Based in Charlotte, N.C., the company operates through more than 155 offices globally and handles premium placements in excess of $33 billion annually. Visit amwins.com
TOKIO MARINE HCC ANNOUNCES AGREEMENT TO ACQUIRE GULF GUARANTY EMPLOYEE BENEFIT SERVICES, INC.
Tokio Marine HCC announced it has signed a definitive agreement to acquire Gulf Guaranty Employee Benefit Services, Inc., a third-
58 THE SELF-INSURER NEWS

You Can. Discover The Value Of Partnership A Full Service MGU Program Manager Custom Plans | EPO | RBP | PPO | Level Funding What If You Could Have The Value Of A Direct Carrier, With The Underwriting Expertise Of An MGU?
party administrator and managing general underwriter that designs, underwrites, and administers group gap medical plans for small and mid-sized businesses. The transaction is expected to close in the third quarter of 2023.

Gulf Guaranty offers a group gap medical plan called MedPlus that pays limited benefits for expenses otherwise covered by an employer’s primary medical plan, but not payable due to the deductible and coinsurance provisions of the primary plan.
MedPlus is employer-paid, and every employee enrolled in the employer’s primary medical plan is automatically enrolled in the product. Group gap medical coverage is a new, profitable product addition to Tokio Marine HCC. The acquired operation produces gross written premium of approximately $60 million annually.
Sherman & Company served as financial advisor to Gulf Guaranty Employee Benefit Services, Inc.
About Sherman & Company
Sherman & Company is an investment banking firm dedicated to the convergence of the insurance, healthcare, technology, and asset &
wealth management industries. Visit sherman-company.com
About Tokio Marine HCC
Headquartered in Houston, TX, Tokio Marine HCC is a member of the Tokio Marine Group, a premier global company founded in 1879 with a market capitalization of $38 billion. Tokio Marine HCCStop Loss Group covers over 3,500 self-funded employers and union plans for medical stop loss and another 1,000 groups with organ transplant insurance. Visit tmhcc.com
60 THE SELF-INSURER NEWS
SUN LIFE LAUNCHES PROGRAM
WITH OPTIMED HEALTH PARTNERS TO MAKE SPECIALTY DRUGS MORE ACCESSIBLE AND AFFORDABLE
WELLESLEY, Mass., -- Sun Life U.S., the largest independent medical stop-loss provider in the country, has named OptiMed Health Partners as a preferred partner to further the company’s goal of improving healthcare access, while also managing rising healthcare costs.
The new program through OptiMed will identify opportunities to administer specialty drugs to members who need them - in a convenient setting, such as the member’s home or an infusion center - working in concert with the member’s physician and care team.
This type of highly coordinated and personalized delivery system reduces the risk of infections and complications for patients while decreasing the treatment costs for high-cost specialty drugs.
The new solution, Medical RX Management powered by OptiMed, is an extension of Sun Life’s Clinical 360 program, which combines innovative data analytics with superior clinical expertise to identify cost savings and ways to optimize patient care and outcomes.
At no additional cost to the client, OptiMed’s vast experience in effectively managing specialty medication trends will help those
who self-fund their health plans better manage their healthcare costs.
According to KFF, an independent non-profit organization focused on national health issues, 65% of covered workers in the U.S. are in a self-funded plan, where employers pay their own medical claims.
“Expensive specialty drugs are major contributors to escalating healthcare costs which can significantly impact self-funded plans,” said Jennifer Collier, president of Health and Risk Solutions, Sun Life U.S. “Through this collaboration with OptiMed, we will tackle two pressing issues in the healthcare ecosystem – access and cost. Medical Rx Management powered by OptiMed will provide more ways for members to receive vital healthcare while reducing unnecessary costs for our clients.”
“As therapeutic advancements continue, it is essential for plans to lean on industry experts and partnerships such as this, to promote sustainability and high levels of clinical support to members when they need it most” said Rusti Greis, Vice President, Business Development for OptiMed Health Partners. “Our passion to reimagine healthcare solutions that deliver unsurpassed value, leverages technology and concierge services; creating an exceptional patient experience and driving positive industry change.”
OptiMed provides specialty infusion medications and therapy management for many conditions including a large number of medications listed in Sun Life’s annual High-cost claims and injectable drug trends analysis of medical stop-loss claims.
OptiMed’s program has been reviewed and accredited by two nationally recognized accreditation bodies focused on patient care and safety.
Sun Life manages high-dollar medical claims for more than 2,800 self-funded employers covering more than 9 million people. Utilizing its extensive medical claims database, Sun Life provides expert insights each year on clinical conditions and medical trends that drive high-cost claims as well as how people utilize their healthcare.
Sun Life is the largest independent stop-loss provider in the U.S. according to data from the National Association of Insurance Commissioners. An independent stop-loss provider does not sell medical claim administration services.
About Sun Life
Sun Life is a leading international financial services organization providing asset management, wealth, insurance and health solutions to
NEWS SEPTEMBER 2023 61
A CLEAR PERSPECTIVE STARTS WITH TRANSPARENCY.

The big picture is always in our view – ensuring that you, your business and your members are strong, vigorous and healthy. From our vantage point, that’s possible only when you have open, accessible and accurate information – complete visibility across our Healthcare Ecosystem Optimization Platform.
We transparently share data used to identify cost, network and plan design opportunities, drive claim accuracy, and improve health outcomes for members – keeping a clear perspective on how to make better decisions, together.
That’s our promise to you. This is precisely why our customers stay with Vālenz® Health, because no one else does what we do. For true clarity on achieving smarter, better, faster healthcare, visit valenzhealth.com or call (866) 762-4455.
 Proud to be a Diamond Member
Proud to be a Diamond Member
individual and institutional Clients. Sun Life has operations in a number of markets worldwide, including Canada, the United States, the United Kingdom, Ireland, Hong Kong, the Philippines, Japan, Indonesia, India, China, Australia, Singapore, Vietnam, Malaysia and Bermuda. As of March 31, 2023, Sun Life had total assets under management of C$1.36 trillion. Visit www.sunlife.com
Sun Life Financial Inc. trades on the Toronto (TSX), New York (NYSE) and Philippine (PSE) stock exchanges under the ticker symbol SLF.
Sun Life U.S. is one of the largest providers of employee and government benefits, helping more than 50 million Americans access the healthcare and coverage they need. Through employers, industry partners and government programs, Sun Life offers a portfolio of benefits and services, including dental, vision, disability, absence management, life, supplemental health, medical stop-loss insurance, and healthcare navigation. Sun Life U.S. and affiliated companies in asset management employ approximately 8,000 people in the U.S. Group insurance policies are issued by Sun Life Assurance Company of Canada (Wellesley Hills, Mass.), except in New York, where policies are issued by Sun Life and Health Insurance Company (U.S.) (Lansing, Mich.). For more information visit our website and newsroom.
About OptiMed
OptiMed Health Partners, headquartered in Kalamazoo, Michigan, is an independently owned and operated national healthcare organization, leading the charge in the infusion and specialty space. For more than 30 years, OptiMed has leveraged personalized attention to detail to deliver customized solutions that optimize patient outcomes while partnering with other healthcare organizations to usher in a new standard of excellence. Email info@optimedhp.com and www.optimedhp.com.
Experience More Than Just Benefits Administration

Planned
with
to improve quality and lower costs while providing exceptional customer service, pharmacy benefits, stop loss, benefit ad ins, and additional perks. Contact us today to learn more: paisc.com/contact-us
Administrators, Inc. partners
clients
SEPTEMBER 2023 63 NEWS
GOLD MEMBERS
ADVANCED MEDICAL PRICING SOLUTIONS APPOINTS MATT BROW AS CHIEF EXECUTIVE OFFICER AND BOARD MEMBER
PHOENIX -- Advanced Medical Pricing Solutions (AMPS), a Cimmaron Healthcare Capital portfolio company focused on supporting self-insured employers and healthcare stakeholders in providing affordable, fair, and transparent medical and prescription benefits, announced the appointment of Matt Brow as Chief Executive Officer and Board Member.
Brow joins AMPS following nearly six years leading pharmacy software and life sciences advisory businesses for Inovalon, a leading provider of cloud-based software solutions empowering data-driven healthcare.
Prior to Inovalon, Brow spent nearly 14 years in leadership roles with US Oncology and McKesson focused on strategy, communications, policy, reimbursement, business development, mergers & acquisitions, and operations.
Brow succeeds Kirk Fallbacher who, over the past seven years serving as COO and then President & CEO of AMPS, led tremendous growth and expansion of the company during that time. Fallbacher will continue his leadership contributions to
AMPS as President of Drexi - the prescription benefits management subsidiary of AMPS, as an AMPS Board Member, as a member of the AMPS Leadership Team, and as executive sponsor for key strategic accounts.
“I am grateful for Kirk’s continued commitment to leadership at AMPS, and I am humbled by the trust and confidence that the Cimarron Healthcare Capital team and our investors have placed in us to fully maximize AMPS’ potential,” said Matt Brow, Chief Executive Officer of AMPS.
“I am honored to have the opportunity to join the exceptional team at AMPS and look forward to building strong relationships with both our team members and customers,” said Brow. “In a healthcare market desperate for innovative solutions, AMPS is well positioned to accelerate its growth and revolutionize employer-sponsored healthcare by providing affordable and transparent care to the benefit of patients and employers alike.”
James Nadauld, AMPS Board Chair stated, “The Board is excited to welcome Matt to the team. We are confident his growth-minded leadership will take AMPS and Drexi to the next level of their evolution in the months and years ahead.”
“Matt shares our deep passion for improving healthcare, and I enthusiastically welcome his leadership,” said Fallbacher. “To the exceptional teams at AMPS and Drexi, I cannot express enough how proud I am of all that we have achieved together over the years. I firmly believe that AMPS and Drexi are perfectly positioned for continued success.”
About Matt
Matt Brow is Chief Executive Officer of Advanced Medical Pricing Solutions (AMPS). With extensive experience managing crossfunctional teams, Matt has engaged internal and external healthcare stakeholders to find consensus and achieve stable business growth.
Prior to joining AMPS, Matt served as President & General Manager of Pharmacy, Life Sciences and Advisory at Inovalon, a leading provider of cloud-based solutions empowering data-driven healthcare.
Matt joined Inovalon in November 2017 to lead its subsidiary Avalere Health and then expanded his role in 2019 to also lead Inovalon’s Pharmacy software business which develops, markets, and supports
NEWS
64 THE SELF-INSURER
You want unparalleled customer service. Employers need the right stop loss coverage. At Swiss Re Corporate Solutions, we deliver both. We combine cutting-edge risk knowledge with tech-driven solutions and a commitment to put our customers first. We make it easy to do business with us and relentlessly go above and beyond to make stop loss simpler, smarter, faster and better. We’re addressing industry inefficiencies and customer pain points, moving the industry forward – rethinking employer stop loss coverage with you in mind. corporatesolutions.swissre.com/esl

Insurance products underwritten by Swiss Re Corporate Solutions America Insurance Corporation. © Swiss Re 2022. All rights reserved.
Advancing
Together.
Employer Stop Loss: Limit Health Care Exposure.
Self-funding
the pharmacy operational and workflow software ScriptMed. While at Inovalon, Matt led the successful divestiture of its Avalere Health business.

Before joining Inovalon, Matt was Senior Vice President, Operations, for The US Oncology Network at McKesson Specialty Health, responsible for developing, planning, and directing the operations of The Network across a multi-state territory.


Previously, he held roles at McKesson and its predecessor company, US Oncology, leading public policy, mergers and acquisitions, business development, go-to-market strategy, sales, reimbursement strategy, federal and state government relations, and communications.

Prior to joining US Oncology, he was a consultant, advising clients on state government affairs strategy across a wide range of healthcare and political issues.
Matt holds a BA in History and Political Science from the University of Richmond. He lives in McLean, Virginia with his wife Lauren and their two children.
About Kirk
Kirk Fallbacher brings more than 25 years of experience building teams and solutions serving the healthcare and health insurance industries.
Kirk has successfully grown multiple organizations / divisions from early-stage formation, focused on developing and launching new products, opening new market segments, and pure business growth, to preparation for scaling distribution and resultant enterprise value. He has overseen organic growth, combined with multiple acquisitions to establish flexible platforms with multiple products and services.
A SPECIALIST APPROACH TO HEALTHCARE

NEWS
risk-strategies.com/healthcare
The Risk Strategies National Healthcare Practice provides specialized expertise and solutions to the healthcare industry across all aspects of the business - Employee Benefits, Managed Care Risk, Reinsurance and Property, Casualty and Liability.
Risk Strategies.
Property & Casualty | Employee Benefits | Private Client Services | Consulting | Financial & Wealth 66 THE SELF-INSURER
By bringing together one of the largest teams of dedicated healthcare insurance and reinsurance professionals operating across the country, Risk Strategies offers its healthcare clients a focused, integrated and responsive liability and risk management service that is best-in-class.
A Specialist Approach to Risk.
Kirk joined AMPS in 2016 as COO and shortly thereafter assumed the President and CEO role, during which time he grew the employee base nearly 10x; opened offices in Phoenix and Hyderabad, India; established AMPS as a leading vendor in the individual health sharing segment; and completed multiple acquisitions, including Drexi, a pharmacy benefits manager and RX discount card provider.
Prior to AMPS, Kirk served in leadership roles at several technology and consulting firms, including: Netrix Global, ITR Mobility (acquired by Zebra Technologies), NVISIA, Swingtide, Alterian, Platinum Technology, Computer Associates, Novell and Ernst & Young.
Kirk holds a BS, computer science and mathematics degree from Western Illinois University.
About AMPS
AMPS provides market leading healthcare cost containment solutions serving self-funded employers, brokers, TPAs, health systems, health plans, and reinsurers. AMPS’ mission is to help clients attain their goals of reducing medical and pharmacy costs while keeping members satisfied with quality healthcare benefits. AMPS leverages its 18+ years of experience and data in auditing and pricing medical claims to deliver “fair for all” pricing. AMPS offers detailed analytics and transparency to
provide clients with insights based on plan performance. Visit amps.com
About Cimarron Healthcare Capital
Cimarron Healthcare Capital is a healthcare-focused private equity firm based in Salt Lake City, UT. Cimarron is led by a unique combination of seasoned healthcare investors and operators. The firm partners with owners and operators in the healthcare lower middle-market to build enduring businesses that improve the healthcare system and drive value for all stakeholders.
SILVER MEMBERS
BLACKWELL CAPTIVE SOLUTIONS ANNOUNCES CAPTIVE PLANNING ASSOCIATES AS ITS CAPTIVE INSURANCE MANAGER
Chicago, IL – Blackwell Captive Solutions, an innovative medical stop loss captive domiciled in South Carolina and sponsored by Carrick Capital Partners, announced that it has named Captive Planning Associates, LLC, as its captive manager to further enhance Blackwell’s services within the captive insurance and alternative risk markets.
“We are excited about the opportunity to work with Captive Planning Associates (“CPA”),” said Kari L. Niblack, President of Blackwell Captive Solutions. “Employer medical stop loss is a financial risk product at its core, and CPA has a demonstrated, successful track record of value creation and truly understands the comprehensive alternative risk ecosystem. This relationship will solidify Blackwell as a leader in the market for years to come.”
“We are grateful for the opportunity to develop and manage custom designed medical stop loss programs with Blackwell Captive Solutions,” said John Capasso, Chief Executive Officer of CPA. “Our years of experience in the employee benefit market, we believe, will greatly enhance Blackwell’s ability to implement unique captive structures for their clients.”
About Blackwell
Headquartered in Chicago, Blackwell Captive Solutions is a medical stop loss captive that differentiates by delivering essential stability with desired flexibility via access to cutting-edge health and well-being solutions for our clients. We’ve proven that combining employers’ buying power with tailoring freedom maximizes the impact of self-insurance and reduces market volatility associated with the ultimate cost of healthcare benefit delivery to employees. Visit blackwellcaptive.com
NEWS SEPTEMBER 2023 67
About Captive Planning Associates, LLC
Captive Planning Associates, LLC (CPA) is a boutique captive management firm specializing in providing innovative alternative risk solutions to closely-held family-owned businesses and large corporations to protect management, shareholders, and stakeholders from undue exposure to risk. Our firm is known for its holistic approach to the design, formation, and implementation of captive insurance companies. Visit captiveplanning.com
MARPAI LAUNCHES NEW HEALTH PLAN FOR SMALL SELF-FUNDED EMPLOYERS
Marpai, Inc. announced the launch of its new plan designed exclusively for small employers. The Marpai Vitality Plan is a unique offering in the rapidly growing segment of self-funded health plans, where small businesses are increasingly opting for greater control, cost savings, and better benefits for their employees.
According to the Kaiser Family Foundation Employer Health Benefits Annual Survey, an estimated 20% of workers employed by businesses with under two hundred employees are in self-funded plans as of 2022, versus only 13% of workers in this segment in 2011.
As small businesses recognize the benefits of transitioning from fully insured to self-funded health plans, the Marpai Vitality Plan provides an ideal solution. It combines ease of implementation, speed, and comprehensive coverage to meet the precise needs of small businesses seeking to maximize savings, enhance employee benefits, and provide value- based healthcare options.
Often smaller employers do not have the infrastructure to deal with complex, time-consuming implementations of self-funded health plans. Marpai Vitality Plan has been meticulously designed to simplify the process, ensuring a smooth and hassle-free experience for newly selffunded small employers. From initial setup to ongoing management, the streamlined approach allows organizations to get up and running quickly, enabling them to focus on what they do best - growing their business.
The Marpai Vitality Plan provides comprehensive healthcare for groups of less than 100 employees. It offers a wide range of services, including access to national and regional provider networks, compliance, banking, vision and dental options, telehealth, COBRA administration, out-of-network repricing (OON), utilization management (UM), pharmacy benefit management (PBM), care
management, subrogation, and stop-loss placement. With a strong emphasis on value-based benefits, the Marpai Vitality Plan enables smaller employers to prioritize the well-being and healthcare outcomes of their employees.
“We understand that small businesses are increasingly shifting towards self-funded health plans to take advantage of increased savings,” said Edmundo Gonzalez, CEO of Marpai.
“Our goal is to empower these organizations by providing a plan that is easy to implement, quick to set up, and offers comprehensive coverage for employees and their families.”
With the Marpai Vitality Plan, small businesses gain a competitive edge by offering robust benefits packages that attract and retain top talent, while promoting healthier lifestyles and more effective healthcare utilization. The tailored services cater to their needs, helping them navigate the complexities of benefits management effortlessly.
For more information about the Marpai Vitality Plan for smaller employers, please visit us here: https://info.marpaihealth.com/ clevenger_marpaivitalityplan
NEWS
68 THE SELF-INSURER
CONCERNED ABOUT MEDICAL INFLATION?

CAN HELP WITH STARR ESL PREMIERTM: A STOP LOSS INSURANCE PROGRAM FOR EMPLOYERS OF ALL SIZES
are facing unprecedented financial uncertainty in the medical marketplace. Inflation, medical advancements, cutting edge delivery and evolving regulations are all contributing.
PremierTM from Starr Insurance Companies can help manage the financial impact in this challenging environment.
LEARN MORE CONTACT
Duchene
WE
Employers
ESL
TO
Mark
mark.duchene@starrcompanies.com 646.466.8485
About Marpai, Inc.

Marpai, Inc. (Nasdaq: MRAI) is a technology company bringing AI-powered health plan services to employers that directly pay for employee health benefits. Primarily competing in the $22 billion TPA (Third Party Administrator) sector serving self-funded employer health plans representing over $1 trillion in annual claims, Marpai maximizes the value of the health plan as measured in health outcomes. Marpai takes a member-centric approach that uses AI and big data to connect members to health solutions predicted to have a high probability of positive outcomes and aims to bring value-based
care to the self-insured market. With effective early intervention, disease management, claims processing and proactive member outreach Marpai works to deliver the healthiest member population for the health plan budget. Operating nationwide, Marpai offers access to provider networks including Aetna and Cigna and all TPA services. Visit marpaihealth.com
CLAIMSBRIDGE AND HIGHLIGHT HEALTH ANNOUNCE PARTNERSHIP TO DELIVER UNMATCHED COST CONTAINMENT SOLUTIONS
Philadelphia – ClaimsBridge, a leading healthcare technology company, and Highlight Health, an innovative firm specializing in cost containment strategies, are proud to announce their partnership to provide an unparalleled suite of cost containment solutions for selffunded employers.

The collaboration leverages Highlight Health’s unique cost containment methodology and ClaimsBridge’s robust Reference Base Pricing (RBP) platform, backed by advanced technology solutions.
At the heart of this partnership is a comprehensive RBP platform that integrates Medicare level pricing, member advocacy, legal
STOP LOSS | CAPTIVE | PAYOR | PROVIDER | GROUP ACCIDENT
starlinegroup.com | (508) 809-3179 70 THE SELF-INSURER NEWS
We love what we do and it shows in the relationships we cultivate with peers, partners and clients. Our stellar reputation is based on trust, expertise and an unparalleled team with eyes on innovation and collaboration. Reach out today and see how we can apply that thinking for you.
defense, and audit capabilities. By incorporating hospital financial and regulatory reimbursement policies, powered by the ClaimsBridge Connect technology platform, the joint offering ensures self-funded employers enjoy substantial savings while delivering an exceptional member experience.
“ClaimsBridge’s RBP platform and supporting technology are the gold standard in the industry,” said Josh Spivak, Chief Executive Officer of Highlight Health. “Integrating our product portfolios enables us to collectively offer a best-in-class cost containment solution for selffunded employers.”
Jeffrey Penn, Vice President of Business Development at ClaimsBridge, expressed excitement about the partnership, stating, “We are thrilled to join forces with Highlight Health. Their cost containment program perfectly complements our RBP platform. Together, we deliver an unmatched combination of cost containment expertise and cutting-edge technology solutions for payors.”
About Highlight Health
Highlight Health is an innovative firm dedicated to supporting selffunded health plans in achieving regulatory compliant coverage and implementing effective risk management strategies that substantially reduce healthcare costs. Visit highlight.health
About ClaimsBridge
ClaimsBridge is a leading healthcare technology company offering a range of services in the pre-adjudication claims lifecycle, including Clearinghouse, Reference Based Pricing, Network Access, Custom provider networks, and Network Hosting. As a SaaS-based company, we provide innovative technology solutions that help over 120 administrators and two million covered lives achieve best-in-class cost containment results. Our mission is to streamline healthcare operations and improve the overall healthcare experience for payors, providers, and patients alike.
Contact: Jeffrey Penn, Vice President of Business Development at jpenn@claimsbridge.com and visit claimsbridge.com
RINGMASTER TECHNOLOGIES® APPOINTS CHRIS BERLAND AS CHIEF FINANCIAL OFFICER
Boca Raton, FL -- Ringmaster Technologies®, Inc (RMT) a leading healthcare software provider in the U.S., in continuation of its growth strategy, is pleased to announce the appointment of Chris Berland as Chief Financial Officer and member of the Ringmaster Executive Team.
In his new role, Mr. Berland will utilize his extensive experience and outstanding record as a financial leader in both the technology and healthcare service sectors to guide Ringmaster to the fulfillment of its strategic and financial goals.
Prior to joining Ringmaster, Mr. Berland applied his entrepreneurial approach and financial leadership for companies in the mobile software, pharmaceutical manufacturing, and healthcare IT sectors to help these organizations achieve their growth objectives.
Additionally, as CFO of Datafile Technologies, he played a significant role in the strategic transformation of the company which led to the successful sale of the business.
“Helping early and growth stage businesses realize their potential and achieve their strategic and financial objectives is what gets me up in the morning,” stated Chris. “I am very excited
NEWS SEPTEMBER 2023 71
to be joining the Ringmaster® team comprised of like-minded visionaries whose individual and collective goals are focused on providing value to all of the stakeholders in the self-funded community.”
“Chris is a proven leader who brings an outstanding record in guiding companies to the fulfillment of their vision, mission and strategic goals,” said Todd Roberti, CEO of Ringmaster Technologies, Inc. “I am excited that Chris is now part of the Ringmaster family and I look
forward to utilizing his experience to help us expand our thriving business and deliver on our long-term targets.”
About Ringmaster Technologies, Inc.
Ringmaster is a cloud-based healthcare software provider created to simplify and enhance administrative processes by utilizing cutting edge technologies. Ringmaster offers the first fully automated workflow optimization solution that will drastically reduce processing time and complexity while minimizing the turnaround time for Stop-Loss quoting, contracting, and policy administration. Additionally, Ringmaster offers an end-to-end cloud-based operating system for pharmacy consulting.
Ringmaster Technologies – Realize the Possibilities – Step into the Ring. Contact Leo J. Garneau III, Chief Marketing Officer, at lgarneau@ ringmastertech.com and visit ringmastertech.com
Shared Values
Customer Service, Cost Controls, Quality Performance
We deliver value other TPAs can’t match. Our three-year medical trend is beating the industry at 2.6%, our claims reviews are finding an extra 15% in savings before network discounts, and our Excellent NPS Score tells us we’re keeping our clients very happy. Our people deliver incredible value for our customers. They can do it for you too.

NEWS
©2022 Trustmark Health Benefits® R450-2880 400 Field Drive • Lake Forest, IL 60045 | 800.832.3332 • TrustmarkHB.com
Scan the QR code with your smart phone to learn more 72 THE SELF-INSURER
SELF INSURANCE INSTITUTE OF AMERICA, INC. 2023
BOARD OF DIRECTORS
CHAIRWOMAN OF THE BOARD*
Elizabeth Midtlien
Vice President, Emerging Markets
AmeriHealth Administrators, Inc.
Bloomington, MN
CHAIRMAN ELECT & TREASURER AND CORPORATE SECRETARY *
John Capasso
President & CEO
Captive Planning Associates, LLC
Marlton, NJ
DIRECTOR
Stacy Borans
Founder/Chief Medical Officer
Advanced Medical Strategies
Lynnfield, MA
DIRECTOR
Matt Kirk President
The Benecon Group
Lititz, PA
DIRECTOR
Mark Combs
CEO/President
Self-Insured Reporting
Greenville, SC
DIRECTOR
Shaun L. Peterson
VP, Stop Loss
Voya Financial
Minneapolis, MN
DIRECTOR
Amy Gasbarro
Chief Operating Officer
Vālenz
Phoenix, AZ
DIRECTOR
Adam Russo CEO
The Phia Group, LLC
Canton, MA DIRECTOR
Deborah Hodges President & CEO Health Plans, Inc.
Westborough, MA
COMMITTEE CHAIRS
Captive Insurance Committee
Jeffrey Fitzgerald
Vice President
Innovative Captive Strategies
Waukee, IA
Future Leaders Committee
Erin Duffy
Director of Business Development
Imagine360
Wayne, PA
Price Transparency Committee
Christine Cooper CEO aequum, LLC
Cleveland, OH
Captive Insurance Advocacy Task Force
Jeffrey K. Simpson
Partner
Womble Bond Dickinson (US) LLP
Wilmington, DE
Workers’ Compensation Committee
Shelly Brotzge
Regional Underwriter, Group Self Insurance
Midwest Employers Casualty
Chesterfield, MO
SIEF BOARD OF DIRECTORS
CHAIRMAN
Nigel Wallbank
Preisdent
Leadenhall, LLC
Ocala, FL
PRESIDENT
Daniél C. Kimlinger, Ph.D.
CEO
MINES and Associates
Littleton, CO
DIRECTORS
Freda Bacon
Administrator
AL Self-Insured Workers' Comp Fund
Birmingham, AL
Les Boughner
Chairman
Advantage Insurance Management (USA) LLC
Charleston, SC
Alex Giordano
Chief Executive Officer
Hudson Atlantic Benefits
Bellmore, NY
Virginia Johnson
Strategic Account Director
Verisk/ISO Claims Partners
Charlotte, NC
* Also serves as Director
SEPTEMBER 2023 73
SIIA NEW MEMBERS
SEPTEMBER 2023
REGULAR CORPORATE MEMBERS
Tom Stein
Principal & CEO
American Trust Administrators, Inc.
Overland Park, KS
Keith LIetzke Advisor
Enthea
Lindsey Spector
Social Media Coordinator
BioTek reMEDys
New Castle, DE
Newton, MA Mike Bentz President
Optimyl Benefits
Milwaukee, WI
SILVER MEMBERS
Harry Tipper, III
Executive Vice President/Chief
Underwriting Officer
Alliance Captive Management, LLC
Nashville, TN
Tamara Marziani
Director, Specialty Solutions
CDPHP
Albany, NY
Ashley Johnson Executive Administrative Assistant
Semler Scientific Inc.
Santa Clara, CA
Christopher Santas
CEO and Co-Founder
ClearCost Health
Larkspur, CA
Amanda Rieger Green
Founder/CEO
Soul Pathology
Wimberley, TX
Jeb Dunkelberger
CEO
ClearPoint Health
Columbia, SC
74 THE SELF-INSURER

Connect with Zelis today at 888.311.3505 or visit zelis.com to get started.
Life Is Not Without Risk.
Catastrophic claims can arise unexpectedly. If the plan has the right Stop Loss protection in place, focus can remain on achieving business goals and welcoming Nadia back when it’s time. When you work with the experts at HM Insurance Group, you can have confidence that the claims will be paid. Find more on hmig.com

Nadia didn’t think her standard yearly check-up would lead to a cancer diagnosis. Neither did her self-funded employer. MTG-3456 (10/22) *Cost estimate based on HM Insurance Group historical Stop Loss data and additional industry observations, September 2022. In all states except New York, coverage may be underwritten by HM Life Insurance Company, Pittsburgh, PA, or Highmark Casualty Insurance Company, Pittsburgh, PA. In New York, coverage is underwritten by HM Life Insurance Company of New York, New York, NY. The coverage or service requested may not be available in all states and is subject to individual state approval. SECURE FINANCIAL PROTECTION WITH OUR INSURANCE AND REINSURANCE OPTIONS: Employer Stop Loss: Traditional Protection • Small Group Solutions • Coverage Over Reference-Based Pricing Managed Care Reinsurance: Provider Excess Loss • Health Plan Reinsurance
A discovery at a $200 annual exam could result in nearly $500,000 in cancer treatment protocol.*



 By Laura Carabello
By Laura Carabello



























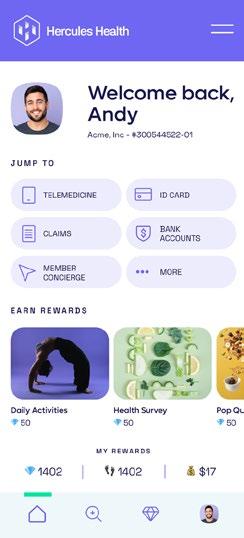



 Marie Noble, MBA, AIC VP of Subrogation Management
Marie Noble, MBA, AIC VP of Subrogation Management
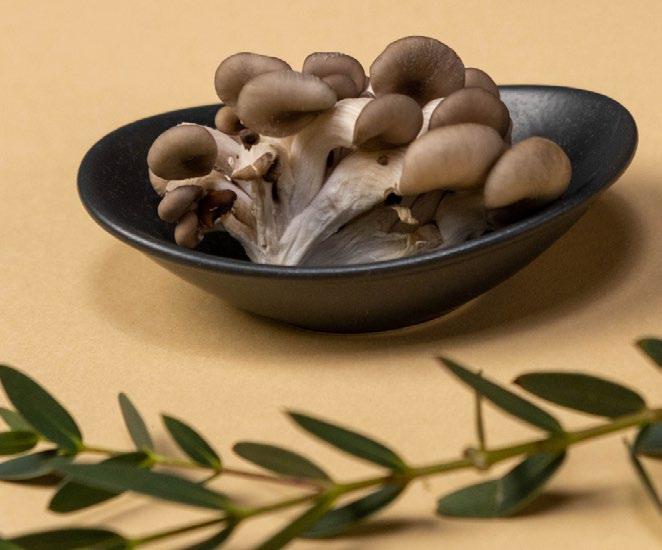





























 Proud to be a Diamond Member
Proud to be a Diamond Member








