INNOVATIONS





In this latest edition of the Innovations Magazine, we are pleased to share some of the wide-ranging efforts that Riverside University Health System (RUHS) has taken to address Disparities. Nationally, there has been a recent awakening with regard to health equity, disparities, and systemic racism. Pandemicrelated remote schooling, telecommuting, and economic uncertainty have exacerbated the gaps among socioeconomic quartiles. And tracking of COVID-related infections and vaccinations has led to increased dialogue about concerning differences in health outcomes among racial and ethnic groups.
in greatest need, those who are most vulnerable, and those who often face the greatest disparities in health outcomes and social determinants. This is remarkable and something of which we should never lose sight.
While the notion of addressing disparities has always been a core value in our organization, over the past several years, there has been a convergence of forces and events that has elevated the topic of disparities to the forefront of our collective consciousness. Past and present state Medi-Cal waiver programs, including DSRIP (Delivery System Reform and Incentive Payment), PRIME (Public Hospital Redesign and Incentives in Medi-Cal), QIP (Quality Incentive Program), and now Cal-AIM (California Advancing and Innovating Medi-Cal) have incentivized organizations like RUHS to recognize and reduce disparities in an increasingly holistic manner. In August 2020, the Riverside County Board of Supervisors unanimously passed a resolution declaring racism as a public health crisis. Around this same time, the RUHS Leadership Team and the RUHS Community Health Center Board tasked the RUHS team with developing a systematic and organization-wide approach to addressing and reducing disparities.
While the national conversation about disparities may seem recent or reinvigorated, we would like to point out that RUHS has been focused on reducing disparities since the opening of Riverside County Hospital in 1893. While some organizations are rightfully recognized for devoting a portion of their time, energy, and resources to community work and helping the underserved, we sometimes overlook how the entirety of our team, our effort, and our entire organization (RUHS Medical Center, RUHS Community Health Centers, RUHS Behavioral Health, and RUHS Public Health) is devoted to those

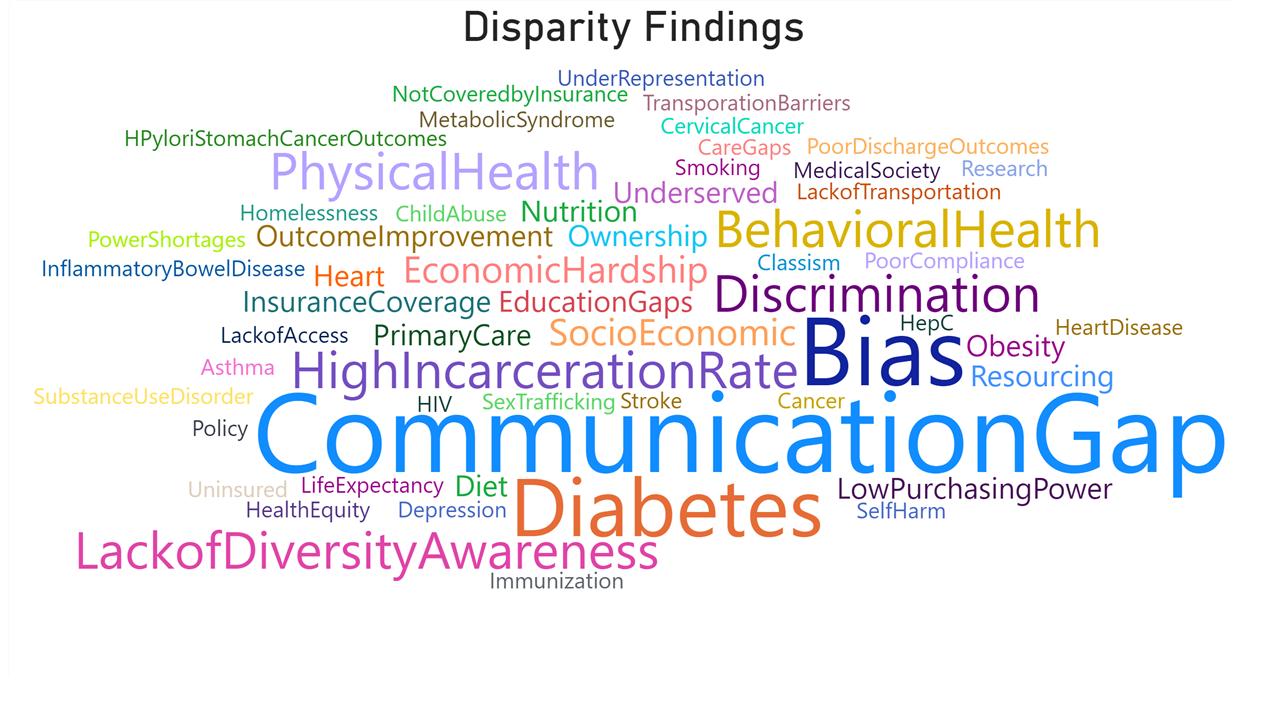
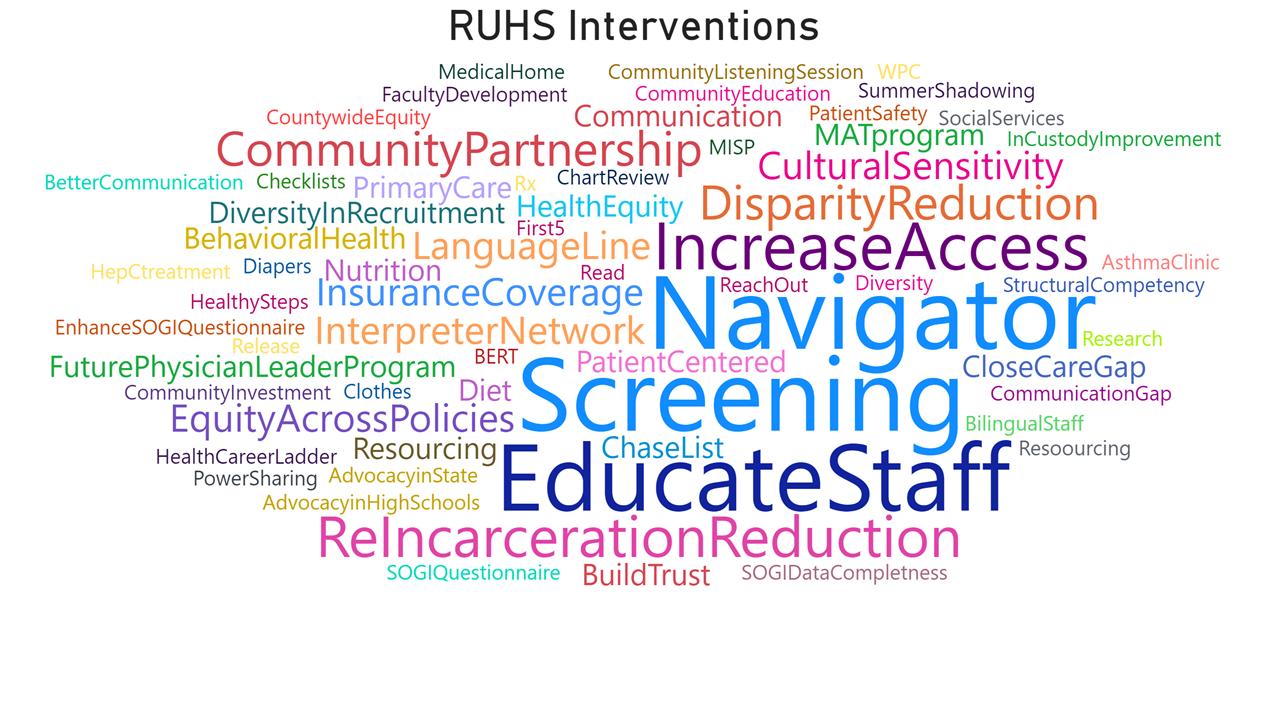
In November 2020, the first RUHS Disparities Workshop was convened in order to highlight and share disparities work among RUHS colleagues, programs, and services. At least 17 RUHS teams presented their disparities-related projects during this workshop, including but not limited to: Behavioral Health, Comparative Effectiveness and Clinical Outcomes Research Center, Dietary and Nutrition Services, Gastroenterology, Information Technology, Integrated Care Management Services, Language and Cultural Services, Media, Pediatrics, Pharmacy, Public Health, Quality and Incentive Programs, Transportation, Whole Person Care, and Whole Person Health Score.
Leveraging and building upon the energy, interest, and dialogue from the Disparities Workshop, the RUHS Equity and Diversity Advisory Taskforce was formed. The overall mission of this taskforce is to

reduce disparities within RUHS using three main strategies – namely, Education and Engagement, Data-Driven Improvement, and Partnerships. Some of the short-term goals include: hosting a Disparities Grand Rounds, developing or selecting a curriculum for implicit bias training, and developing an inventory of disparities measures already collected at RUHS.
In addition to the creation of the RUHS Equity and Diversity Advisory Taskforce, we are excited that RUHS Public Health recently created and filled a new Deputy Director position focused on Health Equity. Inhabiting this new position, Dr. Marshare Penny will serve as an invaluable resource and pioneer not only for Public Health but also for RUHS and the community as a whole.

COVID-19 has significantly impacted communities and local health jurisdictions across the nation. The reduction in the transmission of COVID-19 is possible with concentrated efforts on vaccination and containment. According to the California Department of Public Health, important elements of containment include testing, contact tracing, protecting the vulnerable, engaging the community, meeting the needs of essential workers, and acute care surge.
Successful case investigation and contact tracing for COVID-19 is dependent on a robust and welltrained public health workforce. Many are familiar with case investigation and contact tracing as a core strategy used in outbreak investigations. To be most effective, case investigation and contact tracing requires staff with adequate training, language skills, cultural sensitivity, supervision, and access to social and medical support for clients and their contacts. During the summer of 2020, the Riverside University Health System –Public Health, experienced a dramatic increase in department staffing levels through the recruitment and training of more than 350 contact tracers. It was important to public health leadership that contact tracers hired were representative of the Riverside County population of which they would serve.
COVID-19 case and mortality rates disproportionately impact communities of color
(CDC, 2020), with the risk of COVID-19 exposure disproportionately represented among essential workers (Hawkins, 2020), and those educationally, socially, and geographically disadvantaged (Selden & Berdahl, 2020). In collaboration with Riverside County Human Resources, RUHSPublic Health worked to onboard staff that were representative of the Riverside County community to better engage and support efforts to tackle COVID-19 disparities. In a demographic survey of our contact tracers, most (78.4%) were female, and an average age of 35 years. Although age and sex may not have been representative characteristics, contact tracers were demographically diverse with the majority (49.7%) self-identifying as Hispanic, Latino, or of Spanish origin, followed by White (47.6%), Asian (14.6%), multi-Racial (13.4%), and African American (8.5%). This level of diversity among contact tracing teams was greater than that documented among county residents overall in 2019, where 50% identified as Hispanic or Latino, followed by White (34.1%), Asian (7.2%), African American (7.3%) and multi-Racial (3.6%) (United States Census Bureau, 2019). The contact tracer demography appropriately represented the rich diversity found in Riverside County as well as the cultural and linguistic needs of the population served. This serves as an excellent example of the ability to establish a workforce that is derived from the population served.
CENTERS FOR DISEASE CONTROL AND PREVENTION (2020). Disparities in COVID-19 illness. Racial and ethnic health disparities. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/ racial-ethnic-disparities/increased-risk-illness.html
HAWKINS D. (2020). Differential Occupational Risk for COVID-19 and Other Infection Exposure According to Race and Ethnicity. Am J Ind Med. 2020;1-4. DOI: https://doi.org/10.1002/ajim.23145external icon. SELDEN TM, BERDAHL TA. (2020). COVID-19 And Racial/Ethnic Disparities in Health Risk, Employment, and Household Composition. Health Affairs. 2020: DOI: https://doi org/10.1377/hlthaff.2020.00897external icon











According to the CDC, the best COVID-19 vaccine for you is the first authorized vaccine available to you as they all have been tested for safety, effectiveness, and have reduced risk of severe illness.

Since the first plane harboring the COVID-19 virus landed at March Air Force Base, epidemiologists at Riverside University Health System (RUHS) have been involved in every phase regarding the COVID-19 virus from testing to tracking the number of cases to administering the vaccine. Today, there are three vaccines that are authorized and recommended by the United States: Pfizer-BioNTech, Moderna, and Johnson & Johnson/Janssen. According to the CDC, the best COVID-19 vaccine for you is the first authorized vaccine available to you as they all have been tested for safety, effectiveness, and have reduced risk of severe illness.
In order to efficiently vaccinate as many people as possible, the Vaccine Priority Index (VPI) was created using data such as the rate of COVID-19 cases, deaths, vaccination, and the Healthy Places Index (HPI). The HPI was already being used to identify areas in need of more accessible healthcare by tracking 25 different community characteristics related to economic, education, clean environment, and housing conditions. These characteristics along with the statistics
associated with the COVID-19 virus were the key components in creating the map for the VPI that was being used by the epidemiologists at RUHS.

When vaccines became available there was an understanding that they were in high demand but low in supply. The VPI is used to strategically place mobile sites or teams to administer the vaccine, in order to reach communities that have low accessibility to the vaccine. Communities include those with limited access to transportation, childcare, time off work to go to a vaccine site, or those working in agricultural areas. With the help of trusted messengers getting the word out in their communities and various organizations opening their doors to be used as vaccine sites, it allowed the vaccine to reach more arms as quickly as possible. There are still more places that need to be reached but the VPI is continually being improved as well as the County Vaccination rate.

Riverside County women and their babies in-utero are severely underserved when it comes to high-risk pregnancy care. A lack of Maternal Fetal Medicine (MFM) Providers, geography that makes it difficult to access the one hospital-based MFM Provider available, and no centralized information service are all significant systemic issues that are being addressed to improve health outcomes.
Since arriving in 2017, Dr. Bryan Oshiro, the sole full-time MFM Provider in Riverside County, and Dr. Ronald Johnson, Chair of Obstetrics and Gynecology, have demonstrated that implementing systematic process improvements at RUHS can

optimize resources and create cultural change that improves the health of mothers and their children. RUHS is uniquely positioned to lead the way in developing this approach that will improve the health of high-risk pregnant mothers and their unborn children by utilizing 13 Community Health Centers that are strategically placed throughout the county as well as the Medical Center located in Moreno Valley.
Drs. Oshiro and Johnson have partnered with First5 Riverside, a California state program, that has awarded them a $6.3 million dollar grant to address the following:
Part 1: Offer a competitive MFM Provider salary HeRCARe will provide yearly salary support for a newly recruited MFM, Dr. Sarah Smithson for a 4-year period. The new MFM Provider is building a practice, so the salary will be sustained in the future without further need for outside funding.
Part 2: Establish a research endowment, focused on pregnancy and 0-5 age projects

RUHS Medical Center has a burgeoning research program, but no consistent funding for such endeavors. As part of the recruitment incentive, the RUHS Foundation, a 501c3 supporting RUHS Medical Center, is establishing a research endowment for future projects and investigations into novel programs. Such research topics will include but are not limited to the development of novel programs to care for patients with diabetes, hypertension, substance abuse disorder, and health disparities, and trialing new methods of care delivery, and integration and linking of existing programs within the region. Research and development of a perinatal/neonatal call center and county-wide maternal transport system will be high priority.
Part 3: Optimize MFM Provider Practice-Care Manager, Project Manager and Ultrasound Technician
Critical to increasing provider capacity is bringing on the support needed to do the work. RUHS Medical Center has hired a Project Manager responsible for the oversight and implementation of all projects developed under this plan. In addition, to care for the highest risk patients, a registered nurse to care manage this population will be utilized as a Care Manager. An Ultrasound Technician dedicated to doing the scans at the local CHCs will bring care to the patient’s unique geographic location.




In concert with the recruitment of the new MFM Provider and research opportunity, RUHS has identified eight of thirteen Community Health Centers strategically positioned to implement telehealth capabilities. By investing in telehealth,
pregnant women and their providers anywhere in the county will have better access to RUHS’s two MFM Providers. Each of the eight sites include telehealth equipment, a state-of-theart GE Voluson 10 ultrasound, and revamped infrastructure for information systems. Patients, in locations spanning the county, have access to high-risk pregnancy care not otherwise available. By utilizing telehealth, the challenges of transport, time, funds, and access are greatly eased.
Part 1: Equip Eight Community Health Clinics-telehealth equipment, ultrasound, and IS infrastructure Sites will be chosen for the telehealth rollout based on the current volume of gynecological and obstetric care and because the locations provide geographically optimized access points (they are easy to get to). Currently seeing patients are the RUHS Community Health Clinics in Hemet, Banning, Corona and Lake Elsinore with Riverside Neighborhood and Jurupa opening as soon as fall 2021.
a
Part 1: Link existing county resources
They are developing centralized partnerships with programs such as Black Infant Health, Nurse Family Partnership, Adolescent Family Life, Loving Support, WIC, Public Health Nursing, SU Cares, BHI and more by developing centralized partnerships. The Care Coordinator will be responsible for linking patients with services.
Part 2: Liaison with hospital and clinics
Women’s Health, under the leadership of Dr. Oshiro and Dr. Johnson, are visiting and discussing RUHS’s high-risk pregnancy offerings with hospitals and clinics throughout the region, most urgently MFM Provider access and telehealth, and sharing guidelines of care including referral guidelines.
A call center will provide easy and timely access for perinatal consults and referrals for outside providers and hospitals. This effort is connected to the research endowment for planning and implementation. The center will be designed for real time access for urgent medical questions,

referrals and hospital transfers. Email access will also be available for non-urgent questions, concerns or referrals. Establishing the call center will be the precursor to the future maternal-fetal transport system for Riverside County.
RUHS Medical Center, under the leadership of Drs. Oshiro and Johnson, has a vision of mothers and babies throughout Riverside County served through a coordinated system of care that allows pregnant mothers to access medical advice and health services at multiple locations around the county. Through the development of additional provider capacity and patient access as proposed in the plan, RUHS’s Women’s Health Program is partnering with hospitals county-wide through outreach and education to maternity centers. Telehealth, as processes develop and the system is refined, will pave the way for accessibility currently lacking in the system and ultimately a Call Center will coordinate services and care throughout Riverside County.
3: Interconnect hospitals, providers, existing perinatal services through Riverside County

RIVERSIDE COUNTY
MAY 8, 2021 12:57 AM
Riverside County COVID-19 Survivor Welcomes Baby



This Mother’s Day will be special in more ways than one for a Riverside County mom. That’s because she survived a series of health scares during pregnancy including COVID-19.


TONY SHIN reports for NBC4 News at 4 p.m. on May 7, 2021.

It all began in September of 2019. Lataria Polk was pregnant and was experiencing increasing abdominal pain. Concerned, she drove herself to RUHS Medical Center where she passed out in the parking lot. Her next memory was getting rolled into the hospital and seeing bright lights. It happened to be Dr. Lenorre Clarke’s first day as a new obstetrician on-call at the hospital, when she was called to the emergency room. She quickly recognized the signs of shock due to a ruptured ectopic pregnancy and immediately transferred Lataria to the operating room. Dr. Clarke was able to remove the ruptured fallopian tube that had contained the pregnancy and stopped the bleeding. It was an experience that frightened Lataria who shared, “That’s it. No more. I’m done. I was terrified”. Hearing that it would be more difficult to achieve pregnancy due to the loss of a tube with increased risk of a repeat ectopic pregnancy, she accepted that she would likely never conceive another child. Less than a year later, Lataria was informed she was pregnant with twin girls. As a mother of four boys and wanting a little girl, she was thrilled. Unfortunately, one of the twins did not survive early in the pregnancy but she knew she had to be strong to carry the remaining twin to term. The pregnancy was further complicated when she acquired COVID-19. Dr. Clarke described the situation as “High risk upon high risk, but this is what we do.” In March of 2020, Kyra was born happy and healthy. Her middle name Journey is a reminder of how she got here and how her journey was harder than others, but worth the risk. Riverside University Health System Medical Center (RUHS- MC) focuses on serving the under-served women in the county and the HeRCARe program is dedicated to women like Lataria, who experience high risk problems in their pregnancy. Their work has allowed stories like Lataria Polk and her little miracle, Kyra Journey, to come to light.

Her middle name Journey is a reminder of how she got here and how her journey was harder than others, but worth the risk


 CONTRIBUTORS: SHANNON McCLEERY-HOOPER AND BRANDON JACOBS
CONTRIBUTORS: SHANNON McCLEERY-HOOPER AND BRANDON JACOBS
For the past two and half years, a California statewide collaborative project known as Help@Hand has had the goal of bringing technology-based emotional wellness solutions to the public behavioral health system. The Collaborative is made up of twelve counties and two cities across California, including Riverside County. Each county or city has a project, or projects, they plan to implement, and a specific population of people they want reach. Help@Hand, the CalMHSA Collaborative, supports counties and cities in bringing innovative digital emotional wellness solutions and minimizing the digital divide in the community.
RUHS -- Behavioral Health is implementing projects partnered with Help@Hand, such as informational kiosks and a web-based Peer Chat service called Take My Hand™. The informational kiosks utilize devices with touchscreens that have access to preloaded emotional wellness apps, allowing community members to use the technology created for their emotional support. RUHS -- BH has one of these kiosks located on the second floor of the Medical and Surgical Center located on the main Medical Center campus for anyone who wants access to digital wellness resources.
Take My Hand™ lets people receive support using a data-or Wi-Fi-supported laptop, phone, tablet, or kiosk. It is a live Peer Chat service that is available for free weekdays from 8am to 5pm, except holidays. Take My Hand™ was rapidly implemented in April 2020 because of the distressing impact of the COVID-19 pandemic. With everyone isolating at home, it became especially important that individuals have access to emotional connection and support. Take My Hand™ allows the Visitor to remain anonymous, which eliminates any barriers due to mental health stigma. The Peer Chat Operators have experienced the challenges that come with maintaining good behavioral health, and
are able to create an environment where people feel safe discussing the struggles they deal with on an everyday basis. Peer Operators are trained to provide support, help connect people with resources and to just “walk alongside someone” as they find their own recovery path to wellness.
The Help@Hand Collaborative and projects such as Take My Hand™ hope to detect mental health symptoms sooner, reduce stigma and increase access to the appropriate level of support. Sometimes we take emotional wellness for granted, but access to tools like these provides essential resources and support for better emotional health and overall well-being. If you stop by the Medical and Surgical Center anytime soon, please feel free to try out Take My Hand™ Live Peer Chat at one of
Trying to serve patients with diagnostic treatment and preventative care poses a challenge, especially during a pandemic. Dr. Serrao, Chief of Gastroenterology & Hepatology at Riverside University Health System, emphasizes that “innovation comes under duress…sometimes you have to innovate quickly in order to survive, and that’s why I use the analogy of the ‘fog of war.’ Because in the fog (COVID-19), initially it’s confusing, but when it starts to lift, then opportunity to readjust. And that’s where innovation takes place.” Cancer is a crisis within a crisis and the “magic pill” for colon cancer is to have a robust screening process. When patients have competing health concerns, family responsibilities, work and financial obligations, where does colon cancer screening fall into that priority list? How can RUHS create a system to assist and be less of a barrier to accessing care? As a result of responding to limited visits with patients during COVID-19 and its surges, and the challenges faced by RUHS patients, a new patient navigation program was needed to reach more patients in the community, and not just in the times of COVID restrictions.
During the COVID-19 surges, fewer screenings were conducted and fewer cancers were diagnosed. The limited procedures resulted in a difference of 275 procedures per month pre-COVID to as low as 70 procedures per month during COVID. Patients were prioritized based on the severity of symptoms instead of family history or being part of a high-risk group. Because “the wind got taken out of screening” during surges, the amount of cancers caught per month went from 8-9 cancers pre-pandemic to 5-6 cancers a month in spring 2021 at 80% capacity. The reduced amount of cancers detected heightened Dr. Serrao’s concern. In order to combat the 75% decrease in care and the COVID surges, RUHS had to quickly
innovate in order to help patients and RUHS team members survive.
One of the identified obstacles was the old prescreening patient protocol and a new patient navigation program needed to be established. The pandemic forced the team to review operations. In the past, patients attended an in-person education class before their colonoscopy which was ineffective especially when many patients had to take time off work to attend. In order to combat this “artificial barrier” of having the education class in-person, a “concierge service” was developed to establish new patient navigation. This strategy had two approaches. First, RUHS began holding pre-procedure classes via Zoom, in English and Spanish, to educate patients on how to prepare for a colonoscopy. This also included sessions with RUHS pharmacists to clarify the medications they should be discontinued in preparation for the procedure. The second was a pre procedure follow up call with our patients to remind them about the procedure and refresh how to take the prep. The results of the new patient navigation program were pleasantly surprising for Dr. Serrao and his team. The recent changes to their operations dropped the no-show rate from over 20% to less than 5%. Additionally, patients have been prepping better with better patient compliance to medications, allowing for a high-quality screening colonoscopy.
The team approach from RUHS has allowed the Zoom classes to be successful and create a permanent way of preparing patients for a colonoscopy. The team effort from those who worked behind the scenes, the physicians, and the staff allowed RUHS to be successful in serving patients amidst the pandemic to the highest capacity.


High blood pressure in Riverside County is prevalent and exceeds the state and national average based on the data from 2017. In order to address this statistic regarding hypertension, Riverside University Health System (RUHS) developed a project known as “Healthy Hearts Healthy Homes.” The project was first implemented at the Indio clinic in the beginning of 2020 and was meant to make patients more aware of their hypertension and reduce financial disparity for those who are low income, have Medi-Cal, or are uninsured. The original plan was to utilize reference cards on vital machines to educate patients on the ranges of blood pressure and engage leaders, providers, and staff in the initiative. Unfortunately, like the rest of the world, the project was impacted by the COVID-19 pandemic. The plan had to change the way it reached the community as in-person was no longer an option. Utilizing grant funds to purchase bloodpressure kits seemed to be the best solution. The idea came from discovering that blood pressure kits are a covered benefit for IEHP Managed Medical Patients but are not covered for those with other benefit plans or have no benefit plan. Based on the last quarter statistics for 2020, there were 3000 hypertension (HTN) patients covered by IEHP, while 2131 HTN patients were covered by other plans. The initiative allowed patients access to a blood pressure cuff and the ability to self-monitor their blood pressure. Although, there was a detour from the original course the solution became a beginning step in combating financial disparity.

THE RUHS TEAM RECEIVED A QUALITY LEADERS AWARD HONORALBLE MENTION FOR THEIR EFFORTS.
 CONTRIBUTORS: CORINNE MATTHEWS, LATRICE CARRILLO AND KIRSTEN O’DELL
CONTRIBUTORS: CORINNE MATTHEWS, LATRICE CARRILLO AND KIRSTEN O’DELL
The California Public Hospital Redesign and Incentives in Medi-Cal (PRIME) Program is a five-year initiative under the Medi-Cal 2020 section 1115 waiver that builds upon the Delivery System Reform Incentive Payment (DSRIP) program established under the Bridge to Reform waiver. The goal of PRIME is to continue significant improvement in the way care is delivered through California’s safety net hospital system to maximize health care value and to move toward alternative payment models (APMs), such as capitation and other risk-sharing arrangements.
In Riverside County, health disparities are welldocumented and often linked to race, ethnicity, language, sexual orientation, and gender identity, among other socio-economic factors. Riverside University Health System (RUHS)- Medical Center and Ambulatory Care Clinics serve a diverse, lowincome patient population who are at greater risk for health disparities and poor health outcomes. Through the Public Hospital Redesign and Incentive Medi-Cal (PRIME) program, RUHS has participated in statewide efforts to standardize the approaches used to identify and reduce disparities in health care. Systematic approaches
for quality improvement and change management were adopted to ensure cultural competency in implementing PRIME projects and the strategies to reduce healthcare disparities.
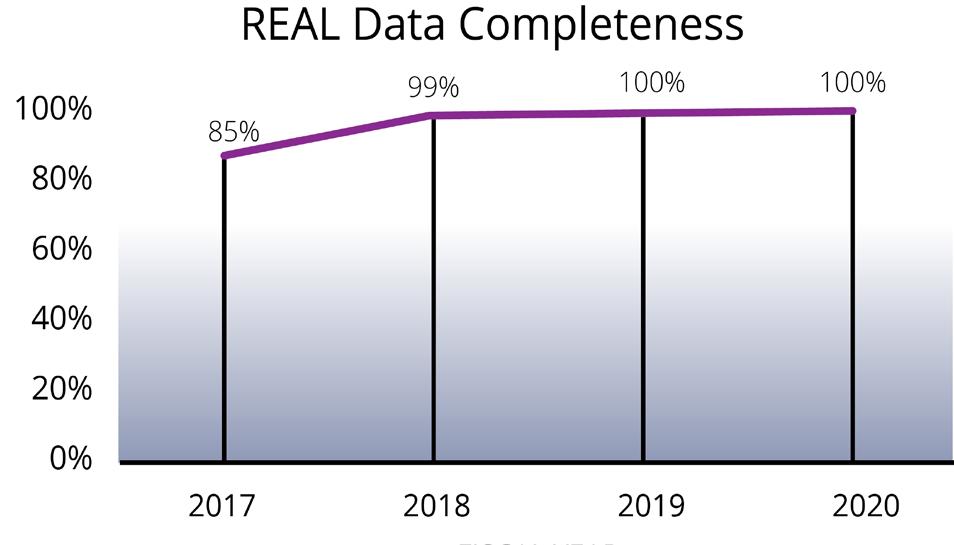
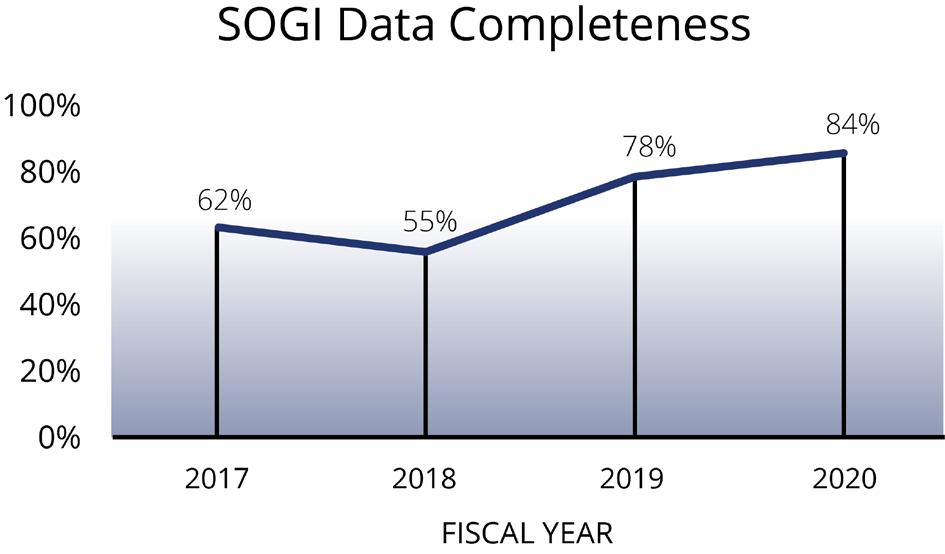
Through PRIME initiatives, RUHS optimized capabilities to improve the collection and stratification of detailed Race, Ethnicity, and Language (REAL) data and proactively collect Sexual Orientation and Gender Identity (SOGI) data. Adding this granular data to the demographic data collection processes and training front-line registration staff to gather complete and accurate REAL/SO/GI data, provided RUHS with the ability
to identify disparities for targeted interventions. For REAL data, RUHS committed to identifying a disparity, implementing an intervention to reduce the disparity, and demonstrating year-over-year improvement throughout PRIME program. Over the past five years, RUHS has made significant advancements in its’ ability to collect detailed REAL data (See Figure 1). The PRIME program helped RUHS advance data collection efforts so that RUHS could better identify the diversity of its’ patients and provide more customized care. By the end of the PRIME program, RUHS collected detailed REAL data for more than 108,000 patients- an additional 59,434 more patients since program year one.
RUHS, like many healthcare systems in California, began the PRIME program in the early stages of collecting SOGI data. The PRIME program helped lay the groundwork for collecting SOGI data. By the end of the five-year PRIME program, SOGI data collection was embedded into the ambulatory care workflows, included in staff trainings, and integrated into organizational equity and strategic goals and priorities.
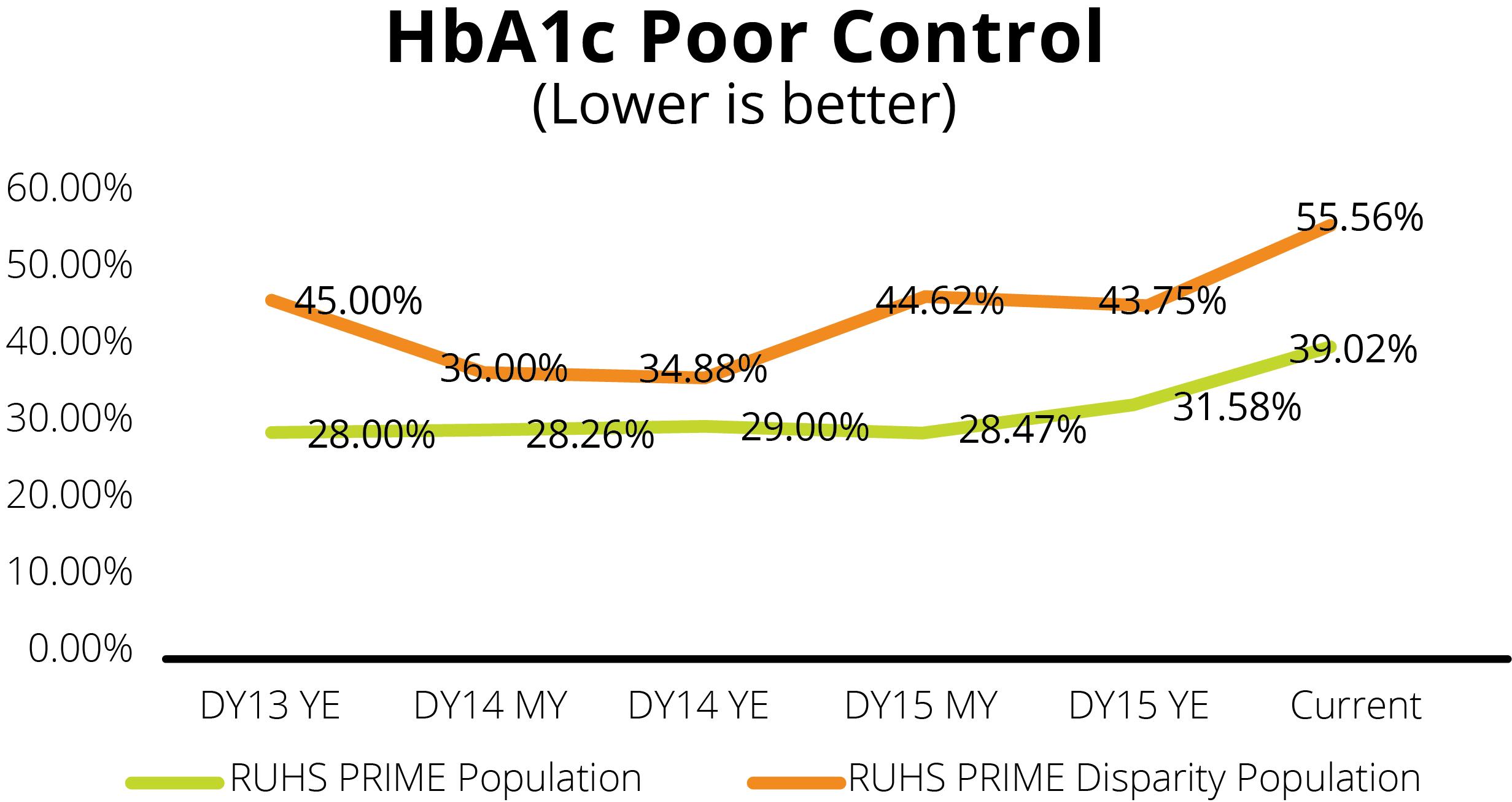
control blood glucose, reduce risks for complications and prolong life. Through thoughtful data analysis, it was identified that diabetes poor control was prevalent in the Riverside County community. The national NCQA measure “Comprehensive Diabetes Care: HbA1c Poor Control (>9.0%)” was chosen to measure the rate of diabetes patients at who has their most recent Hemoglobin A1c at or above 9.0 or was not performed during the measurement year.
To identify a disparity population, the population data was stratified by REAL and SOGI filters. Through this stratification process, RUHS learned that Hispanic males, age 18-39, who are Spanish speaking had much larger rate of poor control (44%) with their diabetes when compared to the total diabetic population (28%). Glucose, reduce risks for complications and prolong life. Through thoughtful data analysis, it was identified that diabetes poor control was prevalent in the Riverside County community. The national NCQA measure “Comprehensive Diabetes Care: HbA1c Poor Control (>9.0%)” was chosen to measure the rate of diabetes patients at who has their most recent Hemoglobin A1c at or above 9.0 or was not performed during the measurement year. To identify a disparity population, the population data was stratified by REAL and SOGI filters. Through this stratification process, RUHS learned that Hispanic males, age 18-39, who are Spanish speaking had much larger rate of poor control (44%) with their diabetes when compared to the total diabetic population (28%).
PRIME required annual improvement in a disparity reduction project. RUHS leadership quickly realized that proper diabetes management is essential to

A workgroup consisting of members of the clinic and staff and ambulatory quality staff lead by Dr. Shunling Tsang set out to reduce disparities in diabetes control. Assisted by consultants from IHQC (Institute for High Quality Care) and Keene Insights.
In order to understand the reasons for poor control in this population, the workgroup decided to conduct a focus group with this population in order to gain insights to better understand what prevents patients. The largest distribution of disparity population was found in the Jurupa Valley, so we chose to conduct focus group at one of RUHS’s clinics in that area.
The workgroup held a pre-focus planning session to identify strategies for conducting the focus group. Then Patient volunteers from the disparity population were recruited to participate.


The focus group was held on July 24, 2018 at

“I


want to get rid of the medications, that is my challenge.”
The workgroup use themes from the focus group along with recommendations from the participants to begin to design interventions to address the specified needs of the disparity population. Some of the strategies included increasing Health Literacy of our target population, providing additional education around diabetes, providing support and increasing cultural competency of clinicians. The workgroup met with nutrition staff and pharmacy staff to outreach patients and provide additional contact and support through nutrition counseling, health coaching and medication management. In 2020, the workgroup recruited the assistance of the newly formed centralized outreach department called the Healthy Patient Outreach Program (HPOP). These bilingual team members were able to provide more intensive outreach strategies for patients difficult to contact, establish report and trust to motivate patients to complete appointments and A1c testing, schedule patients appointments at RUHS after-hours clinics for patients who are not able to come during work hours as well as utilize mobile phlebotomy services for qualified patients with transportation barriers.
RUHS saw an initial reduction in the disparity of HbA1c control in the first year. Over time, however A1c rates began to rise along with the total diabetes population.
Moving into QIP: As RUHS leaves the PRIME program behind and moves into the QIP (Quality Incentive Pool) program year 4, Disparity Reduction will continue as a new Improving Health Equity Measure. The metric will be aimed at addressing diabetes control for both the Black/African American and Latinx populations. RUHS Quality/Incentive Payment workgroups are now beginning data analysis of both populations and will soon be on the way to creating a health equity plan.
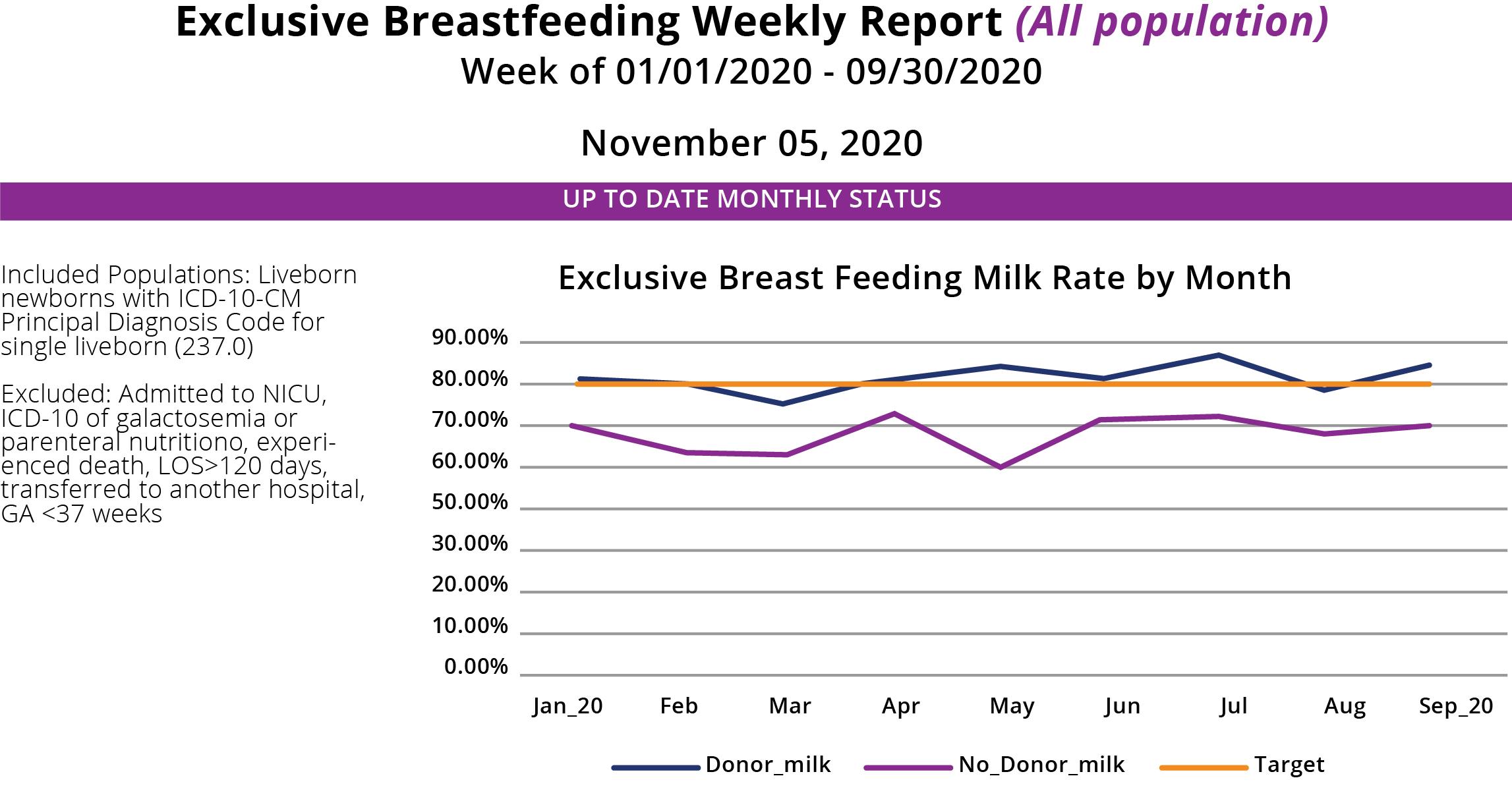
Exclusive breast milk feeding for the first 6 months of neonatal life has long been the expressed goal of World Health Organization (WHO), Department of Health and Human Services (DHHS), American Academy of Pediatrics (AAP) and American College of Obstetricians and Gynecologists (ACOG). Exclusive breastfeeding (newborns that were fed breast milk only during their hospitalization) rates at RUHS have consistently increased over the five-year PRIME Waiver period, from a low of 61.8% in 2016 to a rate of 78.6 % in 2020 (these data exclude the NICU population). The PRIME population closely mirrored the RUHS entire birthing population during these years and data from the Maternal Data Center demonstrates that RUHS compares very favorably with other birthing facilities regionally and throughout California.
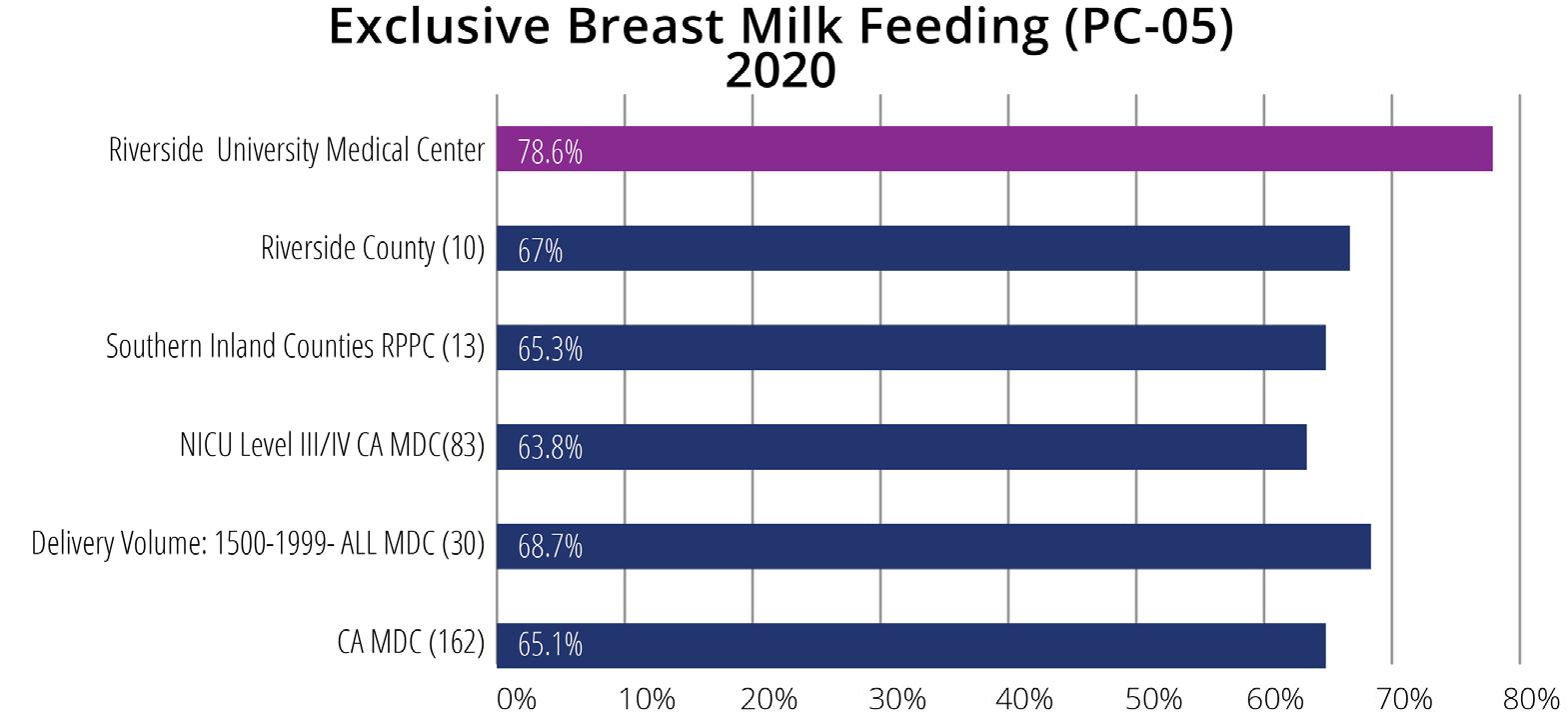
RUHS achieved the prestigious designation of Baby Friendly in 2015, providing the foundation for implementing many of the strategies that would ultimately benefit so many of our mothers, their newborns. A few of these efforts are highlighted in this article.
One of the first changes instituted to support mothers and infants was “Quiet Time” occurring for two hours during the day to allow mothers more time to rest, anticipating irregular sleep during the night. To support “Quiet Time” signage was created and placed near the elevators and throughout the unit, and education was provided to perinatal physicians and nurses and to departments interacting with mothers on the unit such as lab and housekeeping.

• Quiet Time Guide developed to inform staff.
• Quiet Time Survey of moms to asses benefits and personnel adherence.
• Results and Mothers comments shared with staff.
Mother’s Comments:
“I like Quiet Time, it helps me and the baby get more rest.”
”I slept really well during that time.”
The Breastfeeding taskforce, a multi-disciplinary group formed when preparing for Baby Friendly designation, meets monthly and continues to be instrumental in promoting and supporting exclusive breastfeeding. As part of a large system with 12 outpatient clinics that provide prenatal care it is critical that mothers receive education regarding infant feeding prenatally. In collaboration with WIC, all outpatient clinic staff received three hours of education on breastfeeding and infant behavior supported by the Prime Nurse Coordinator and the Riverside County WIC Breastfeeding Liaisons.
• Trainings scheduled over a 9-month period.
• Breastfeeding and Baby Behavior, a glossy colorful book in English and Spanish, organized by weeks of pregnancy, are available for mothers to read at their prenatal visit.
• Pages can be printed as handouts.
• Books were provided for each exam room in every clinic.
Another example of collaboration with WIC was the RUHS/Medical Center support of the WIC “Grow your Own” course, a preparation course for the International Board-Certified Lactation Consultant (IBCLC) exam. RUHS/MC provided space and media support for the 9-month course in exchange for two Perinatal RN scholarships.
Instituting human donor milk availability for the term infant is perhaps the perinatal improvement that has most directly affected RUHS exclusive Breastfeeding Rates. Providing this service to our mothers and their newborns required endorsement from the Waiver Integration Team and took close to a year to accomplish. Human donor milk administration required a specific Tissue Bank license, policy development, logistics for donor milk administration, nursing, physician and patient education, and purchasing agreements. Monthly exclusive breastfeeding reports include donor milk administration. The report is shared with the perinatal team and incorporates race and ethnicity breakdown.
Thank you to all of those that care for RUHS mothers, newborns, and their families. This success is due to your expertise and caring.
RUHS is enormously proud of improvements in patient satisfaction for Care Transitions over the past year. RUHS started its PRIME journey with HCAHPS Care Transitions scores below the target rate. Our performance crept slowly closer to the benchmark, but never surpassed, while we worked to build a foundation of improved communication, continuity, and coordination of care. However, in November 2018, RUHS engaged its Hospital Patient Advocates in the care transition process. Since that time, patients are reporting significantly higher satisfaction in Care Transitions. RUHS HCAHPS scores have risen at the beginning of 2018 from 44.9% to 51.59% at year-end. It maintained to improve up to 54.9% in 2019.
The utilization of Hospital Patient Advocates to support care transitions is an innovative and patient-centered strategy that utilizes resources already in place at RUHS to impact patient care with very little investment. Hospital Patient Advocates have been a part of hospital administrative services for decades helping to resolve patient grievances. RUHS’s patient experience nurse coordinator collaborated with the Hospital Patient Advocate team to re-envision their role to enhance the patient experience in care transitions. In addition to our advocate rounding, our Nurse Coordinator in Patient Experience has aligned with National Research Corporation (NRC) to develop a Provider Shadowing Template. This template was designed as a tool to coach our health care teams on the meaning behind patient satisfaction questions and the importance of empathy, health literacy and teach-back, and effective communication resulting in enhanced
safety and improved relationships. The RUHS Provider Shadowing Template includes specific best practice tips and behaviors that will guide our teams to communicate efficiently and improve population health. The RUHS communication training included empathy, AIDET, Teach-Back, Bedside Reporting and Purposeful Rounding, resulting in more than 4,526 staff of all disciplines trained as our organization strives to standardize service excellence. Advocates now proactively round on newly admitted patients to offer a warm welcome, explain the role of the advocate and the management team and invite patients to resolve any concerns before they leave the hospital. They also advise patients and caregivers about the importance of understanding their responsibility in adhering to their post-discharge plan, the importance of knowing the reason for taking each of their medications and empower patients to ask questions if they do not understand. Advocates also help identify and communicate important patient preferences to the care team regarding their transition back to home.
Although HCAHPS is a measurement of the total patient population, over 80% of patients cared for at RUHS belong to Managed Care Medi-Cal. RUHS’s increasing satisfaction scores reflect the positive impact Hospital Patient Advocates are having on successful care transitions. The support to patients from an administrative level is strengthening patients and families’ involvement in their care during and after hospitalization and is helping to increase patients and caregivers’ level of understanding, comfort, and confidence in managing their care after discharge.
In August 2019, National Research Corporation recognized RUHS with an award for the Most Improved Large Hospital for HCAHPS performance. 2018 was the first demonstration year that RUHS has successfully met the PRIME target rate and the improvements are proving sustainable. One of the contributing factors for this success included the implementation of hospital patient advocate rounding on newly admitted patients. RUHS has focused on the expansion of the patient advocate rounding during 2019 to include our obstetrics department and utilization of our patient portal. Increased utilization of the patient portal enhanced patient experience by providing the client a direct method of contact with their provider and the ability to view upcoming appointments, schedule appointments, order medications, and access their laboratory results. This enhancement empowered patients to participate in their care and improve quality outcomes.


The implementation of the Patient Family Liaison (PFL) has been essential during Covid-19 when visitation was restricted to a select population like Compassion Visits. This provides the objective of the program, promoting patient and family-centered care. A Covid-19 nurse Liaison training was
also done which includes the workflow and their responsibility such as scheduling video calls to keep families as our priority. Also, a Covid-19 Welcome packet in both English and Spanish was designed to lessen patients’ fear during their Covid-19 hospitalization and provide them with an idea of what the hospital journey would look like for them. The packet is provided by the Patient Family Liaison during their rounding on COVID patients. In July 2020, the National Research Corporations go live for TELEHEALTH was implemented to measure our client’s perception of care in both video and telephone visits at the height of COVID. As RUHS continues to improve on the Net promoter Score, we have identified the following strengths such as clients feel the method of connecting was easy and we had a good quality of video/call.
In November 2020, the United States Food and Drug Administration authorized the early treatment of COVID-19 with REGEN-COV (casirivimab and imdevimab). This treatment reduces the impact of COVID-19 on the community by reducing disease progression, hospitalization, healthcare resource demand, and the risk of morbidity and mortality. Riverside University Health System (RUHS) Medical Center, RUHS Public Health, and the California Emergency Medical Services Authority (EMSA) have partnered together to open the hospital’s, and Riverside County’s, first Monoclonal Antibody Treatment Center to mitigate the disease effects early within COVID-19 patients. The Cal EMSA state support provides resources to facilitate services and treatment for earlydiagnosed high-risk unvaccinated and high-risk vaccinated COVID-19 patients.
What is “monoclonal antibody treatment (mAb)” and how is RUHS combatting the disparities of access of treatment care in offering this new treatment?
Monoclonal Antibody Treatment (mAb) “We have seen firsthand the impact the virus has had on patients,” said Dr. Mike Mesisca, Emergency Medicine Department Chair of RUHS Medical Center. “Offering this treatment gives our patients a chance to fight off a virus that has devastated our communities. By offering monoclonal antibody treatment, we are positioning ourselves in a way to protect some of the most vulnerable patients by working to prevent severe illness.”
Dr. Mesisca revealed that COVID-19 is now a pandemic of the unvaccinated. “It really has become a pandemic of the unvaccinated; the vast majority of our patients that are in our hospital and in our ICU are unvaccinated.”
Monoclonal antibody treatment’s purpose is to save lives from COVID-19 complications. It is an injection or an intravenous (IV) infusion designed to be administered early in the diagnosis. It provides antibodies that fight the virus and prevents the virus from getting into cells. “So, it is something you have to give early. You can’t wait till people get really sick and it’s already progressed, and the virus is throughout their system causing inflammation and other problems.” This treatment can help those who are within ten days of when their symptoms started.
Some of the identified challenges and or obstacles to helping those patients within ten days of symptoms and illness include the difficulty to:
• reach the at-risk communities; people in high-risk communities are not being educated to get monoclonals (Dr. Terese Hammond, Program Medical Director of Providence Saint John’s ICY and Sound Physicians),
• transportation, “It’s a rural location, so we have barriers as far as access, there’s transportation.” (Dr. Gary Wiltz, CEO/ Clinical CHO, Teche Actional Clinic, Franklin, Louisiana)
• availability of hospital beds per capita; “We have a critical access hospital that is an eighteen-bed facility serving about twenty thousand folks, and access is a big issue.” (Dr. Gary Wiltz, CEO/Clinical CHO, Teche Actional Clinic, Franklin, Louisiana)
• lack of tools to help the patients; (Dr. Gary Wiltz, CEO/Clinical CHO, Teche Actional Clinic, Franklin, Louisiana)
• identify which patient was eligible for the treatment (Dr. Jennifer Tuteur, Deputy Chief Medical Officer, County of San Diego, Health & Human Services Agency),
• overcoming a certain level of distrust; “The level of distrust that people of color across this country have with the institutions of their society is pervasive; it is deep, and it is damaging. It bleeds into healthcare. We now have a very specific and powerful reason for reaching out to every patient in our patient population. At least they will be well-armed with the information about monoclonal antibodies. These are really key elements that all of us have an opportunity to participate in enhancing.” (Dr. Reed Tuckson, Founding Member, Black Coalition Against COVID-19), and • discerning eligibility requirements: the need to meet one or more of the following criteria to be eligible for treatment.
Cal-EMSA and RUHS have implemented solutions borrowed from other equity-based strategies to combat some of these obstacles to care. Dr. Tutuer emphasizes that “it is so important that the ‘access in’ has to be the easiest possible, especially when the eligibility criteria is more complex.” For instance, in order to identify which patient that was eligible, Dr. Tutuer and the San Diego clinic modeled what was learned from a streamlined phone triage system. The clinic utilized a single phone number that provided a nurse interview and triage, physicians assisted when needed, and the nurse scheduled the appointment the same day. If an individual needed help with transportation, it was coordinated. At Geisinger Medical Group, their public relations teams met “people where they [were]” and used “proactive messaging in individuals’ preferred language.” (Dr. Keith Boell, Chief Quality Officer).
RUHS and Cal-EMSA have built on the prior experience of others to ensure access is simple, direct, and rapid to remove as many barriers as possible to time sensitive treatment of COVID-19.
The RUHS-MAB clinic team has utilized local media and news outlets to promote the clinic directly to the public. Presentations and promotion have been facilitated through the public health department and multiple county agencies. In tandem to these promotional
efforts, information has also been shared through Riverside County Medical Association (RCMA), Inland Empire Health Plan (IEHP), and the Hospital Association of Southern California (HASC). RUHS continues to look for multiple avenues to share the clinic resource and phone number to as many people as possible, particularly in underserved areas.
In order to make the “access in” easier, the clinic waived doctor referral, insurance requirements, and provided the opportunity for patients to call the MAB clinic directly. This way patients will not have to wait for insurance approval, provider referral, and scheduling. Since the center started welcoming patients on Monday, September 13, over twenty patients have been seen daily. The clinic is available from Monday through Saturday from 8 a.m. to 6 p.m. by appointment. It is available to people ages 12+ with mild-to-moderate COVID-19 who also meet the following criteria under the FDA’s Emergency Use Authorization.
In order to receive monoclonal antibodies at RUHS-MAB, a patient must meet three (3) of the following criteria:
• Positive SARS-CoV-2 test result
• Symptoms that started within the last ten days
• Among the third potential criteria patients must have risk factors for severe disease including Body Mass Index (BMI) ≥ 25, chronic kidney disease, diabetes mellitus, pregnancy, immunosuppressive disease, be receiving immunosuppressive treatment, OR be Age ≥ 65 years, OR Age ≥ 55 years AND have one of the following: o Cardiovascular disease, OR o Hypertension, OR o COPD/other chronic respiratory illness
The clinic is located on the lower level of the RUHS Medical Center. Patients should enter from Cactus Avenue. Designated parking for patients visiting the MAB Treatment Center is adjacent to the Emergency Department mobile office trailers. MAB clinic personnel will greet and escort patients from the parking area to and from the clinic by using a designated route.
For questions about scheduling, please contact the clinic directly at 951-486-6520.











 Dr. Edward Bacho EDITOR-IN-CHIEF
Ginny Jefferson PRODUCTION MANAGER
Dr. Edward Bacho EDITOR-IN-CHIEF
Ginny Jefferson PRODUCTION MANAGER
Ester Parada Bonilla
DESIGN DIRECTOR
ARTICLE CONTRIBUTORS:
Paula Carrillo
Latrice Carrillo
Isis Duran
Wendy Heatherington Dr. Ronald Johnson Dr.Vikram Kumar Dr.Geoffrey Leung
Corrine Matthews
INNOVATIONS WORKGROUP:
Edward Bacho, MD
Matthew Chang, MD, MMM
Raul Coimbra, MD, PhD
Parastou Farhadian, MD
Frank Flowers Jr, MD
Emily Hwang
Ginny Jefferson
Lenore Gallucci Stevenson
Emily Hwang
COPY EDITOR AND WRITER
Lesley Bellows DIGITAL CONTENT CREATOR
Kevin Meconis Dr. Mike Mesisca Kristen O’Dell Dr. Marshare Penny Dr. Shunling Tsang Salomeh Wegaw
Ronald Johnson, MD Mahbuba Khan, MD Vikram Kumar, MD
Geoffrey Leung, MD, EdM Michael Mesisca, DO
Adriana Rosato, MSc, PhD
Shunling Tsang, MD Chad Vercio, MD
RUHS MARKETING
26520 Cactus Avenue Moreno Valley, CA 92555 marketing@ruhealth.org ruhealth.org
Riverside University Health System - Medical Center 26520 Cactus Avenue Moreno Valley, CA 92555 ruhealth.org