SUMMIT







































Greetings from Rocky Mountain University of Health Professions (RMU)!
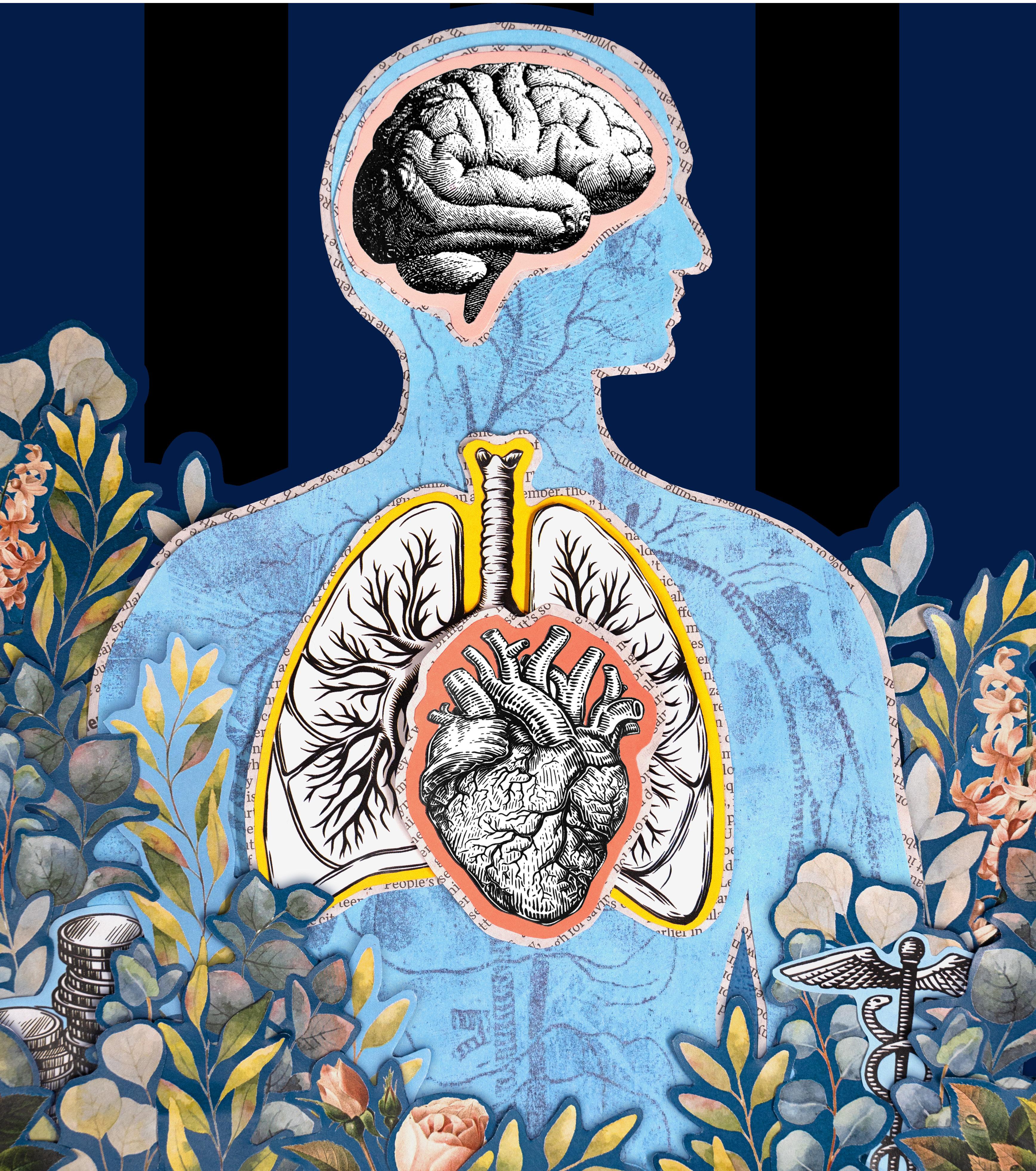
At RMU, we are deeply committed to preparing healthcare professionals who not only provide expert, evidence-based care but also understand the importance of holistic well-being—for their patients, their communities, and themselves. This year’s issue of The Summit is centered on the Wheel of Wellness and how RMU integrates a holistic approach into every aspect of education, training, and professional development.
The Wheel of Wellness reminds us that optimal health goes beyond physical care. Occupational, environmental, intellectual, spiritual, emotional, physical, financial, and social well-being all play a role in achieving balance. RMU embraces this philosophy, ensuring our students are equipped to deliver compassionate, patient-centered care while also fostering their own resilience and success in the healthcare field.
In this issue, you’ll read inspiring stories about how RMU students, faculty, staff, and alumni are applying these principles—whether through our student services, our holistic approach to healthcare education, or innovative research that promotes whole-person care. At RMU, we’re shaping healthcare leaders committed to treating the whole patient.
I invite you to take our wellness assessment within this issue and find areas in your life to help achieve balance and better well-being. Enjoy the stories of our different professions and how holistic health is applied on campus, in clinics, and in our daily lives.
Catch up on what RMU has been up to since last year’s issue with our University Updates, and be inspired by the service our students, faculty, and staff provide to the community.
Together, we are not just educating healthcare professionals—we are transforming the future of healthcare itself by loving and lifting those in need.
Sincerely,
Dr. Cameron K. Martin PRESIDENT & CEO

dr. cameron k. martin UNIVERSITY PRESIDENT & CEO
dana l. costa VICE PRESIDENT OF ENROLLMENT, MARKETING & COMMUNICATIONS
rachel richards DIRECTOR OF UNIVERSITY COMMUNICATIONS / MANAGING EDITOR
jody genessy SENIOR CONTENT WRITER
shari warnick ART DIRECTOR
alayna nichols GRAPHIC DESIGNER/ILLUSTRATOR
dustin winter UNIVERSITY VIDEOGRAPHER & PHOTOGRAPHER

SEND COMMENTS ON THIS ISSUE AND STORY IDEAS FOR FUTURE ISSUES TO:
&
ROCKY MOUNTAIN UNIVERSITY OF HEALTH PROFESSIONS AFFIRMS ITS COMMITMENT TO FAIRNESS AND EQUITY, AND DOES NOT DISCRIMINATE ON THE BASIS OF RACE, ETHNICITY, COLOR, NATIONAL ORIGIN, CITIZENSHIP, PERSONAL APPEARANCE, RELIGION (INCLUDING NO RELIGION) OR FAITH, POLITICAL AFFILIATION, ECONOMIC STATUS, DISABILITY (PHYSICAL OR MENTAL), AGE, MARITAL STATUS, SEX, SEXUAL ORIENTATION, GENDER IDENTITY, GENDER EXPRESSION, PREGNANCY, VETERAN STATUS, PREDISPOSING GENETIC CHARACTERISTICS, DOMESTIC VIOLENCE VICTIM STATUS, OR ANY OTHER PROTECTED CATEGORY OR GROUP UNDER APPLICABLE LOCAL, STATE, OR FEDERAL LAW, INCLUDING PROTECTION FROM THOSE OPPOSING DISCRIMINATION, ATTEMPTING TO PREVENT RETALIATION, OR PARTICIPATING IN ANY RESOLUTION PROCESS. FOR MORE INFORMATION, VISIT RM.EDU/COMPLIANCE



RMU Shines: Triple Win at the 2025 Utah Best of State Awards!
RMU has been honored with three 2025 Utah Best of State awards, recognizing excellence in student achievement, curriculum development, and university leadership. As a leading graduate healthcare institution, RMU received accolades in the categories of:
Best University Student Garrett Parry, physician assistant program (Pictured left)
Best Curriculum Development
RMU Occupational Therapy Department
(Pictured lower left, Dr. Bryan Gee, Founding Chair, Department of Occupational Therapy)
Best University Administrator
President Cameron K. Martin, PhD
(Pictured below, with First Lady Julie K. Martin at the 2024 gala)
These awards reflect RMU’s dedication to advancing healthcare education and making a meaningful impact through innovation, leadership, and service.


At the end of 2024, RMU renamed its College of Optometry to the College of Optometric Medicine. This change reflects the institution’s unwavering commitment to advancing healthcare by emphasizing the medical and clinical foundations of the profession of optometry.
At RMU, the Doctor of Optometry curriculum equips future optometrists with an in-depth foundation in medical sciences—such as anatomy, physiology, immunology, pharmacology, biochemistry, and microbiology—on par with the training provided in medical schools.
Additionally, RMU optometry students receive education in primary care, internal medicine, dermatology, radiology, and surgery. They learn how to diagnose/treat diabetes, hypertension, and high cholesterol—all symptoms that could affect vision and can be treated by an optometrist.
RMU’s Doctor of Philosophy (PhD) in Health Sciences program has transitioned from a four-year model to an accelerated three-year structure. Students use a hybrid learning format, combining asynchronous online coursework with immersive on-campus experiences. This aligns with the University’s commitment to provide cutting-edge, evidence-based education that adapts to the needs of students and the healthcare workforce.

The PhD in Health Sciences prepares students for leadership roles in academia, research, and clinical practice. The program emphasizes:
Rigorous Research Training Developing expertise in quantitative and qualitative methodologies for impactful and ethical research.
Innovative Teaching Strategies Equipping students to design evidence-based educational experiences and assessments. Leadership Development Building competence in roles spanning clinical practice, research, and education.
Mentorship and Support Offering personalized guidance throughout the program, including dissertation development.
A distinctive feature of the PhD program is its student-centered approach, which empowers students to choose their own dissertation topic based on their individual interests and passions. Once a topic is selected, students are matched with a mentor from an extensive in-house database of more than 150 nationally recognized healthcare experts.
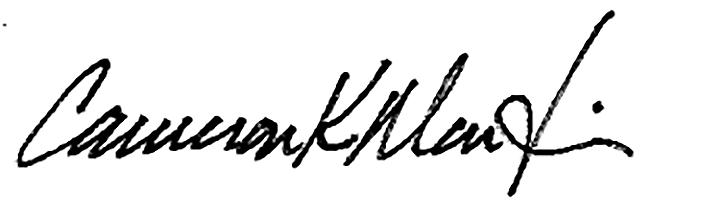
In May 2025, eight RMU students had an unforgettable and unique experience—they went to prison. The group, accompanied by two faculty members from the RMU College of Optometric Medicine, administered free eye exams and glasses prescriptions to 50 incarcerated individuals at the Utah State Correctional Facility in Salt Lake City.
Each diagnosis was reviewed and approved by faculty, who are licensed optometric physicians. Along with the exams, incarcerated individuals who needed corrective lenses were allowed to select a new pair of glasses. The screenings bring to light other health conditions, resulting in helpful referrals to other healthcare specialists.
RMU plans to conduct monthly exams at the prison.
“At Rocky Mountain University, we believe access to healthcare is a fundamental right—regardless of circumstances,” said Dr. Adam Hickenbotham, founding dean of RMU’s College of Optometric Medicine. “This partnership with the Utah State Correctional Facility not only helps meet a critical need for eye care, but also provides our students with meaningful, hands-on experience that reinforces the importance of compassion and service in healthcare.”

The Board of Trustees directs RMU in its mission to educate current and future healthcare professionals for outcomes-oriented, evidence-based practice. In 2024, the Board of Trustees welcomed new members Dr. Michael Nelson, Mr. Roy Zwhalen, and Mr. James Suel.



Wendy Chase Appointed Program Director of RMU’s MS MedSLP Program

Wendy Chase, MA, CCC-SLP, was named program director for RMU’s Master of Science in Medical Speech-Language Pathology program.
Chase joined RMU as a professor and clinic director in 2017. She has three decades of experience in clinical positions, treating clients from infancy through geriatrics and in locations from home care to hospitals.
Her classroom teaching has focused on dysphagia and clinical methods. She believes that critical thinking and evidence-influenced practice are hallmarks of an excellent speech-language pathologist and strives to support student acquisition of these core skills through quality clinical education.
Chase took the helm after the retirement of Linda Spencer, PhD, CCC-SLP, who served as program director from 2016-2024.

Sandra Combs, PhD, CCC-SLP, became the new Doctor of Speech-Language Pathology (SLPD) program director at the end of 2024. Dr. Combs, a graduate of the University of Kentucky, the University of Cincinnati, and RMU, has been the SLPD capstone coordinator and an associate professor at RMU since 2021. She has more than 30 years of clinical experience and almost 20 years of teaching and research experience.
Dr. Combs took over after the retirement of Sandra Shigetomi-Toyama, ClinScD, CCC-SLP. Dr. Shigetomi-Toyoma held many roles at RMU, including SLPD program director, teacher’s assistant, an instructor for the capstone courses, and as capstone coordinator. Both are alumnae of RMU’s SLPD program.
Jeffrey Fisher Named Senior Executive Director of RMU Foundation

Jeffrey Lynn Fisher was named the new Senior Executive Director of the RMU Foundation, a role essential to advancing its mission to improve the human condition through education, research, and providing healthcare to underserved populations in our communities.
With deep expertise in both public and private fundraising—including working with federal agencies, healthcare systems, and higher education institutions—Fisher is uniquely positioned to grow the Foundation’s strategic partnerships and philanthropic reach. Fisher leads the RMU Foundation, a registered 501(c)(3) public charity and nonprofit organization that supports the academic and clinical initiatives of RMU—including the RMU Health Clinics.
Through the RMU Health Clinics, the RMU Foundation provides essential healthcare services to Utah County’s most vulnerable populations, delivering compassionate, high-quality care across multiple disciplines. Patients receive specialized treatment in physical therapy, mental health counseling, optometry, speech-language pathology, occupational therapy, and electrophysiology.
In 2024, the health clinics facilitated 9,533 patient visits, helping uninsured and underinsured individuals, immigrants, refugees, and those experiencing homelessness access critical medical care. With 17 licensed clinicians and a commitment to patient-centered service, the clinics continue to bridge healthcare gaps and improve the well-being of the community.
Alongside healthcare delivery, the RMU Foundation remains steadfast in its mission to support education and professional development. Student-learning clinics provide RMU students with invaluable hands-on experience, fostering the next generation of healthcare leaders. Additionally, grants, scholarships, and mentorship programs strengthen academic opportunities, allowing students to advance their expertise and contribute to evidence-based medical practices. Through the generosity of donors, volunteers, and community partners, the Foundation continues to make a profound impact, ensuring that quality healthcare and education remain accessible to those who need it most.
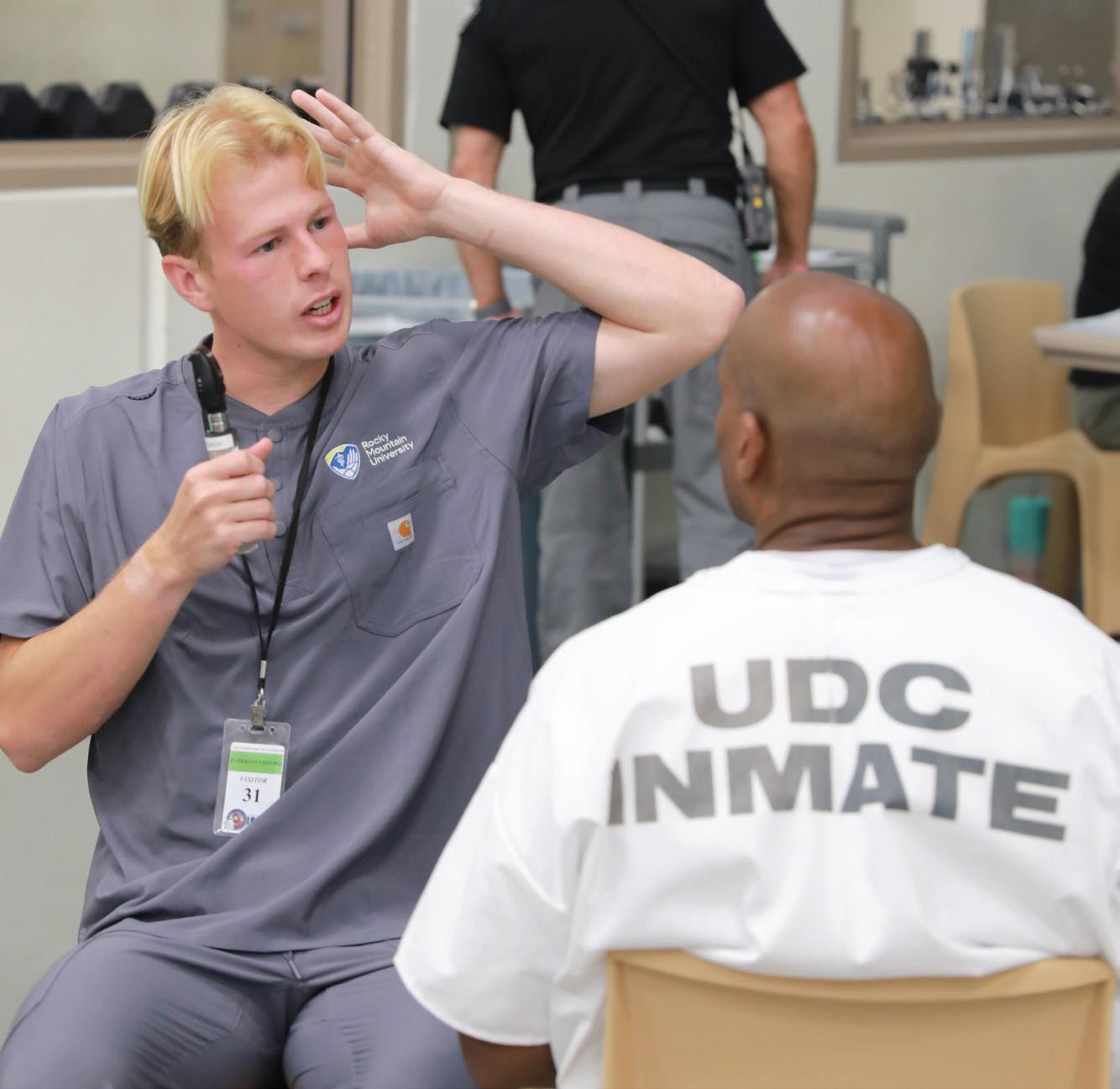
Reader’s Theater is an annual summer camp run by RMU Master of Science in Medical Speech-Language Pathology (MS MedSLP) students and the RMU Center for Communication Disorders (CCD) to help children develop academic and reading skills. Under the guidance of MS MedSLP students and CCD clinicians, the children rehearsed and performed in the play “The Three Pirate Pigs” last summer. The cast and crew used creativity to make props and costumes, had fun while learning vocabulary and improving articulation, and bravely stepped out of their comfort zones.
9,533 Patient Visits $1,525,859 Annual Community Value
17 Licensed Clinicians Institutional Partnerships We
mentorship and training opportunities for students.

In September 2024, RMU partnered with the United Way of Utah County and the South Franklin Community Center in Provo to host its annual health fair for underserved and uninsured individuals and families in Utah County. Every year, local children and adults receive healthcare assessments, testing, and information. Some attendees are referred to community clinics for further care.


The RMU Doctor of Optometry program was awarded $20,000 from the Seva Foundation to support technology and learning for Native communities in the United States. A select team of optometric researchers, translational biochemists, and RMU optometry students works with the Navajo Nation and Tsé Bii’ Ndzisgaii Community Center in Monument Valley, Utah, to conduct a series of studies focused on improving diabetic eye care for Native Americans. This generous grant allowed the program to acquire a fundus camera. This will help improve care for diabetic patients and perform mass spectrometry-based plant proteomics experiments in collaboration with Brigham Young University.

“Instead of just treating a specific disease, wholeperson health focuses on restoring health, promoting resilience, and preventing diseases across a lifespan.”


By Rachel Richards
Modern medicine is evolving rapidly. New technology is transforming healthcare research, treatment, and procedures. Part of this transformation is a shift among healthcare providers to treat the whole person, not just their symptoms.
According to the National Institutes of Health, “Instead of just treating a specific disease, whole-person health focuses on restoring health, promoting resilience, and preventing diseases across a lifespan.” This approach acknowledges that health isn’t just about fixing problems—it’s about maintaining overall well-being.
A popular way to understand whole-patient health is through the Eight Dimensions of Wellness, often called the Wheel of Wellness. This model helps patients and healthcare providers understand the importance of balancing all aspects of health to achieve overall wellness.
This concept isn’t new. In 1948, the World Health Organization defined health as “a complete physical, mental, and social well-being, not merely the absence of disease.” This was one of the first global acknowledgments that health goes beyond physical symptoms.
In 1976, Bill Hettler, co-founder of the National Wellness Institute, introduced six dimensions of wellness: physical,
emotional, intellectual, social, spiritual, and occupational. By 1996, two more— environmental and financial—were added to create the Eight Dimensions of Wellness we recognize today.
Public health organizations like the Substance Abuse and Mental Health Services Administration recognized that factors like environmental conditions and financial stability play critical roles
in an individual’s well-being. It was essential to add these to help address health disparities (see page 26 for more).
The Affordable Care Act in 2010 emphasized preventative healthcare and holistic wellness, which contributed to integrating these dimensions into patient care. Today, universities, hospitals, and corporate wellness programs worldwide use this model to promote well-being.
Level of satisfaction and enrichment from one’s work and the extent to which a person’s occupation allows for the expression of personal values.
Based on the idea that balance in eight key areas of life build to better health and well-being, The Eight Dimension of Wellness include the areas of occupational, environmental, intellectual, spiritual, emotional, physical, financial, and social well-being.
RMU alumna (2013) Dr. Alisa Ward explored this concept in her dissertation, The Conceptualization and Measurement of Wellness: The Perceived Wellness Survey (read more about Dr. Ward on page 40).
The common theory is that true wellness is only achievable when the person

has established a healthy balance of all the dimensions of wellness. Some may require more attention than others at different times, but the goal is to create harmony in one’s life.
The Eight Dimensions of Wellness are not standalone pillars—they often overlap and influence each other in realworld settings. For instance, someone struggling with financial instability may also experience heightened stress and anxiety, which can affect emotional and

even physical wellness. Healthcare providers, wellness coaches, and educators are using this model to help patients set realistic, personalized goals. By visually mapping out which dimensions need more attention, patients can better understand which areas of life need improvement.
Wellness is dynamic, and using tools like the Assess Your Wellness Survey (see page 16) helps people gain a more holistic understanding of areas of life that need improvement.
Emotionally well people can bounce back from setbacks and failures and are resourceful when responding to difficult situations.
Gives meaning and purpose in life and a connection to something greater than yourself.
With this shift toward holistic health, more medical providers are utilizing whole-patient assessments to address lifestyle, mental health, and social factors during medical visits. These surveys help healthcare providers understand a patient’s overall health before discussing specific issues or ailments.
Some commonly used assessments include:
• Patient-Reported Outcome Measures: Evaluating a patient’s self-reported health status.
• Comprehensive Geriatric Assessment: Addressing physical, mental, and functional well-being in older adults.
• Functional Medicine Matrix: Examining lifestyle, diet, and environmental influences.
• Social Determinants of Health Screenings: Identifying factors like food security, housing, and financial stability.
• Mental Health and Behavioral Assessments: Screening for depression, anxiety, and stress.
Clinics adopting a whole-person approach are also investing in inte-

grated electronic health records that include social and behavioral health data. This integration allows providers from different specialties to access and update shared patient profiles, fostering more coordinated and informed care. For example, if a physician notes signs of chronic stress during a routine visit, they can refer the patient to an in-house behavioral health specialist or connect them with community support resources. At some clinics, patients are even paired with wellness navigators who act as liaisons between medical care and lifestyle support—ensuring recommendations are culturally relevant, achievable, and aligned with the patient’s personal goals.
Refers to one’s perception of physical health, physical activity levels, nutrition, self-care, vitality or longevity, and is a wellness dimension included in all models.
A commitment to lifelong learning and a desire to share knowledge.
Effective collaboration in healthcare depends on interprofessional communication across disciplines. There has been a rise in collaborative healthcare teams to serve patients better. These teams unite healthcare professionals such as doctors, nutritionists, mental health professionals, and wellness coaches, ensuring patients receive comprehensive care in a single setting. These team-based care models reduce redundancy, minimize gaps in service, and create a seamless experience for the patient.

Research supports the value of interprofessional collaboration in improving healthcare delivery. A systematic review published in the Journal of Interprofessional Care found that collaborative practice models lead to improved patient satisfaction, enhanced health outcomes, and even reduced hospital readmission rates. As the healthcare system grows more complex, collaboration is essential to achieving efficient, equitable, and patient-centered care.

At RMU, students participate in cross-disciplinary experiences to prepare for this integrated model. Opportunities like the Parkinson’s Clinic (see page 42), Multiple Sclerosis labs, and the annual mass-casualty simulation allow students to work together to provide better patient outcomes. This kind of training not only mirrors real clinical settings but fosters a mindset of shared responsibility and empathy—critical for delivering whole-person care.
One’s sense of belonging and connection to family, friends, and community.
Income determines one’s living conditions and access to food and safe housing. It also includes distribution of wealth, poverty rates, income volatility, and economic security.


The future of healthcare is shifting to comprehensive, patient-centered care that understands the interconnectedness of physical, emotional, social, and environmental well-being. By integrating the Eight Dimensions of Wellness into medical practice, healthcare providers can offer better preventive care and improve long-term health outcomes.
As modern medicine embraces the whole-patient model, institutions like RMU are preparing healthcare professionals to adopt this approach. This new generation of providers will be equipped to deliver truly integrated holistic care, ensuring that patients receive the support they need to thrive in all aspects of life.
Incorporating balance between home and work life and one’s relationship with nature and resources.
“By embracing a holistic approach, healthcare professionals can deliver comprehensive, patient-centered care that fosters resilience, prevents disease, and enhances quality of life,” said RMU President Cameron K. Martin. “RMU is committed to preparing the next generation of providers to integrate these principles into their practices, ensuring better health outcomes for all.”
Wellness isn’t just the absence of illness or stress—it’s the pursuit of positive physical, mental, and social well-being. When was the last time you sat and looked at all areas of your life? Where are you thriving? What area needs a little TLC?
In this section, we encourage you to grab a pen, set aside some time, and assess the areas of your personal Eight Dimensions of Wellness. This self-
assessment tool, from the Substance Abuse and Mental Health Services Administration is utilized by RMU Student Affairs, and can help identify the areas of wellness where you’re thriving, as well as those that may need more attention. This self-assessment helps you consider aspects of your health that you might not have focused on before.
Instructions:
1. Carefully review and answer all the questions for each Dimension of Wellness sections on pages 17 and 18.
2. Total your points for each section.
3. Color in the wheel based on these scores for a visual interpretation of where you are in each area.
Examples
“Spending time with friends has been such a priority that I haven’t balanced my work and learning. I also realized that they are not always the emotional support I thought I needed.”
—Example Person 1
“I have spent so much time at my job trying to get ahead that I have neglected just about everything else in my life. Now I realize how much it has been affecting my overall health for quite some time now.”
—Example Person 2
Involves your ability to cope with life stress, express emotions, and maintain a positive outlook on life. It includes being aware of and accepting your thoughts, feelings, and behaviors, and managing them in a healthy way.
Involves developing healthy habits related to nutrition, sleep, exercise, appropriate health care, stress management, and overall physical health. It also includes building awareness of your body and taking personal responsibility for your health. Consists of personal beliefs and values that give your life meaning and purpose.
exploring the deeper meaning of human existence while cultivating
and a connection to something greater than yourself. It is not necessarily
I consider the feelings of others and do not act in hurtful or selfish ways.
I try to see good in my friends and do whatever I can to support them.
I
Involves engaging in creative and stimulating activities to expand your knowledge and skills. It means recognizing your potential to contribute and engage with different viewpoints.
Consists of balancing the various aspects of your relationship with money. It includes understanding financial processes related to savings, income, and debt, and using resources to achieve long-term financial goals.
Involves creating safety in all of your surroundings. It includes respecting nature and ensuring your living, working, and learning environments
of your well-being.
Consists of finding activities that align with your individual purpose, and reflect your goals and beliefs. It includes being aware of the balance between work and personal time, building relationships, exploring various career options, and engaging in ongoing training.
(Ideal score: 28 in each area)
Scores of 20-28: Outstanding! Your answers demonstrate that you’re already taking positive steps in this dimension of wellness. You’re improving your own well-being and setting a good example for those around you. Although you achieved a high overall score in this domain, consider reviewing any lower scores on individual items to identify specific areas for improvement. You might also want to focus on other areas where your scores weren’t so high.
Scores of 15-19: Your behaviors in this area are good, but there is room for improvement. Look at the items where you scored lower and think about what changes you can make to improve your score. Even small adjustments in behavior can lead to better health and well-being.
Scores of 14 and below: Your answers suggest potential health and well-being risks.
Suggestions from RMU Student Affairs on Ways to Improve Each of the Eight Dimensions of Wellness
Emotional wellness involves your ability to cope with life stress, express emotions, and feel positive about your life.
• Stay positive
• Practice gratitude and self-compassion
• Avoid overthinking or ruminating on mistakes or negative thoughts
• Incorporate self-care into your busy schedule
• Practice being mindful to increase your awareness and positive effects
• Reframe and befriend stress
• Seek or accept support from others around you
Social wellness consists of having positive, healthy, and meaningful relationships with friends, family, and the community.
• Join a club or organization
• Connect with supportive friends and family
• Set healthy boundaries
• Practice good communication skills and be assertive
• Treat others with respect
• Practice self-disclosure and be authentic with others
Spiritual wellness consists of personal beliefs and values that provide a sense of meaning and purpose in life.
• Practice meditation
• Join a faith-based community
• Spend time in nature
• Increase self-reflection and explore your inner self
Physical wellness consists of healthy habits towards nutrition, sleep, exercise, appropriate healthcare, stress reduction, and overall physical health.
• Engage in physical activity every day for 30 minutes
• Recognize the signs when your body begins feeling ill or tense and take actions to take care of your body
• Annual physicals with your primary care physician
• Eat a variety of healthy food
• Get adequate sleep between 7-9 hours each night
For more tips and resources, scan the QR code or visit bit.ly/RMU_wellnesstips
Environmental wellness promotes physical and emotional safety in all of your surroundings, and includes respect and preservation of nature.
• Recycle
• Conserve energy
• Participate in an environmental organization
• Carpool or use public transportation
• Plant a personal or community garden
• Purchase products with minimal packaging
• Organize neighborhood watches
Intellectual wellness encourages interacting in creative and stimulating activities to expand your knowledge and skills, as well as understanding diverse points of view.
• Be curious and open-minded
• Listen to and consider the perspectives of others to improve critical thinking skills
• Participate in activities that cultivate mental growth
• Attend conferences, talks, and programs that increase your knowledge
• Try a new hobby or learn a new language or musical instrument
• Teach or mentor others
• Travel more to increase your knowledge and appreciation for another culture
Financial wellness consists of finding an equilibrium among the psychological, physical, and spiritual aspects of your relationship with finance.
• Track your expenses, create a financial budget, and stick with the plan
• Use coupons and take advantage of sales and discounts
• Make weekly meal plans ahead of time to maintain your budget goals
• Utilize the library for free books
• Adopt the minimalist mindset in your lifestyle
• Reorganize your belongings and utilize what you have currently
• Attend financial management workshops or seminars
Occupational wellness consists of exploring and determining activities that align with your individual purpose and meaning that mirrors personal goals, belief systems, lifestyle, and values.
• Balance work and leisure time
• Manage workplace stress
• Explore volunteer opportunities that interest you
• Practice communication and conflict management with colleagues
• Attending conferences and trainings in your chosen profession

By Jody Genessy
“I think all of these aspects are just vital to true wellness, and since they overlap tremendously, you can’t really be a disaster in one area and be perfectly well in all the other areas. It’s a good framework for really looking at our own wellness, looking at the wellness of others, and helping everyone be more well.”

Bartley Rust, DHSc, PA-C, RMU’s Doctor of Medical Science (DMSc) program director and a longtime practicing physician assistant (PA), is concerned that PAs are among the 50% of healthcare providers who will experience burnout at some point in their careers.
“It’s really a matter of when, not if, a PA is going to experience burnout,” he said. “That’s why it’s important to treat and teach individual strategies that a person could employ. We teach people self-care and resilience training, especially mindfulness, relaxation techniques, and physical activity. All that can help improve your emotional resilience.”
Knowing of the potential adverse effects of burnout on providers and patients, Dr. Rust and RMU are taking a proactive approach within the scope of the Wheel of Wellness to get in front of that situation.
Being aware of the causes of burnout is crucial. Risk factors include a variety of workplace stressors, including long hours, high patient loads, emotional demands (particularly for those on the front line in trauma or emergency settings), high stress levels, exhaustion, and a work-life imbalance.
“There are things that can be done at the organizational level as well, whether it’s a healthcare organization or a university,” he said. “They can foster a culture of open communication, well-being, emotional support, workload management, and getting involved with team-building activities.”
The Wheel of Wellness is a useful tool for PAs in assessing and enhancing well-being in personal and professional settings. That’s why RMU puts an emphasis on helping students learn how to cope and thrive in all dimensions—occupational, environmental, intellectual, spiritual, emotional, physical, financial, and social. It helps them as students during graduate school and carries over into providing skills for the rest of their careers.
“I think all of these aspects are just vital to true wellness,” Dr. Rust said. “And since they overlap tremendously, you can’t really be a disaster in one area and be perfectly well in all the other areas. It’s a good framework for really looking
at our own wellness, looking at the wellness of others, and helping everyone be more well.”
RMU’s DMSc program even includes a specific module on practitioner well-being and mindful practice during the Lifestyle Medicine course. Strategies taught include:
• Boundary setting
• Limiting work hours
• Taking breaks
• Managing workloads
• Peer support
• Connecting with mentors
• Seeking academic advising
• Getting professional help from a licensed provider DMSc students are encouraged to communicate openly upon entering the program. RMU’s attentive Student Affairs team (see page 38) provides additional resources. Students also have free 24/7 access to BetterHelp’s virtual counseling.
The DMSc psychiatry concentration includes instruction in Cognitive Behavioral Therapy and Motivational Interviewing to boost emotional and spiritual wellness.
“These courses are focused on motivational interviewing and cognitive behavior therapy, which obviously you can use to assist patients,” Dr. Rust said. “You can also use those techniques on yourself to effect behavior change in an effort to achieve a higher level of wellness.”
As healthcare demands grow, RMU’s holistic approach ensures PAs flourish, delivering exceptional and holistic care—a model for the future of medical education.
“It’s not wise to try to separate physical wellness, mental wellness, and spiritual wellness,” Dr. Rust added. “We used to talk about body, mind, and spirit as whole person healthcare, but the Wheel of Wellness model is even more helpful as it allows us to focus on the eight core dimensions of wellness.”
By Jody Genessy
Not only is it one of the most important rooms on a healthcare school campus, but the Cadaver Lab, of all places, is an intersection of dimensions of wellness, health education, and humanity.
It’s also where Anatomy Lab Director Kent Crossley, PhD, a 2025 Utah Best of State nominee, calls home while at RMU. Dr. Crossley’s anatomy instruction equips students across RMU’s health science programs to serve communities in multiple healthcare disciplines and emphasizes respect and empathy for donors from the University of Utah’s Body Donor Program.
“This is your first patient,” he tells students when they enter the cadaver lab for the first time. “This is where you start to learn good bedside manner.”
Here are ways well-being and science intertwine in an unlikely spot at RMU:
Physical Wellness Studying for long hours and on weekends comes with the territory of grad school. Dr. Crossley understands that. But he’s concerned about students’ physical and emotional well-being and advises them to work toward balance.
“Do something fun,” he recommends. “Go for a hike or go skiing. Get a little fresh air and a new start.”
Emotional Wellness The lab invokes a wide range of emotions and reactions: anticipation, curiosity, anxiety, trepidation, sadness, inquisitiveness, and respect. While some students are eager to acquire hands-on learning through dissection and observation, others can be emotionally affected by being in the same room as cadavers. That stems from a variety of reasons, including memories associated with the death of a loved one.
“With the emotional side of things, sometimes we find that students just struggle,” Dr. Crossley said.
The key, he said, is to patiently allow students to go at their own pace. At first, they simply spend time in the lab and look out the windows at the scenic view of Provo and the Wasatch Mountains. When they’re ready, they can approach the cadavers. If they need a break or to come back another day, that’s fine. One-on-one sessions can happen later if necessary.
Social Wellness In the lab, students usually work in groups, which fosters teamwork and collaboration.
“Invariably, they have to work with other individuals in the health profession to be able to take care of a patient,” Dr. Crossley said.
RMU even has a Dissection Club, which fosters group camaraderie and offers a social outlet for students.

Spiritual Wellness Along with studying the bodies, students get to know part of the deceased’s history, including their first name, occupation, and cause of death.
“You find these amazing things and students are wowed by it,” Dr. Crossley said. “You kind of get to know [the donors] personally because you spend a lot of time with them .”
It’s heartwarming for Dr. Crossley to see students pay their respects to the cadavers and tell them goodbye when the semester ends. They appreciate the donors’ posthumous participation in their health education and want to honor their humanity.
Occupational/Financial Wellness Anatomy is such an integral part of healthcare professions; it is the only department that offers courses to multiple programs at RMU. Dr. Crossley enjoys being able to make a difference in the education—and careers—of students in programs ranging from physical therapy to optometry.
“The support our Anatomy Department provides for the other programs is absolutely vital,” said Dr. Tyler Sommer, RMU alumnus and former director of RMU’s Master of Medical Science (MMSc) program. “I personally think Kent truly is the best in the state when it comes to lab instruction.”
“Best cadaver lab in the U.S.”
Dr. Jonathan Baird Assistant Professor, Master of Medical Science Program
Environmental Wellness It’s sometimes humorously mentioned that RMU’s cadaver lab has a better view than any other, and it quite possibly does. With a long wall full of windows on the eighth floor, natural light brightens the room in multiple ways. The unique setting and outdoor scenery adds to the effectiveness of the education that happens inside the integral room.
Intellectual Wellness RMU’s Anatomy Department has a two-prong approach; Students are taught in the cadaver lab and another classroom equipped with cutting-edge 3D monitors and state-of-the-art technology. That innovative approach allows students the invaluable opportunity to explore various parts of a body on a screen and then observe what it looks like in an actual body, and vice versa.
“Students always really love anatomy,” Dr. Crossley said. Those are among the myriad reasons why Dr. Jonathan Baird, an assistant professor in RMU’s MMSc program, echoes others in offering this observation: “Best cadaver lab in the U.S.”

By Rachel Richards






“Just go for a 30-minute walk.”

“Get eight hours of sleep.”
By Rachel Richards




“Eat fresh fruits and vegetables.”
“It’s important to help young professionals step outside themselves and start thinking about how environmental and financial factors impact their patients.”
What does it really mean to live a healthy life? The answer goes beyond diet and exercise, it’s shaped by the environment we live in, the resources we can access, and the barriers we face every day. Health isn’t experienced the same way by everyone, and the path to wellness often looks different depending on your zip code, income, or background. That’s why it’s crucial to recognize that personal responsibility is only one piece of a much larger puzzle.
There are many common “easy” health tips often given to the public. But health isn’t always that simple.
What if you don’t live in an area where it’s safe to go for a walk? Or reside in a food desert, where the nearest grocery store is miles away? Maybe you don’t have the luxury of getting eight hours of sleep because you’re juggling multiple jobs.
These scenarios are examples of social determinants of health—factors that extend beyond personal choices and fall within the environmental dimension of the Wheel of Wellness (see page 10).
According to the U.S. Department of Health & Human Services, “Social determinants of health are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”
Examples include:
• Safe housing, transportation, and neighborhoods
• Racism, discrimination, and violence
• Education, job opportunities, and income
• Access to nutritious food and opportunities for physical activity
• Clean air and water
• Language and literacy skills
Healthcare professionals need to recognize these determinants as real barriers that patients may be unable to overcome.
At first glance, it might seem obvious that physical therapists focus on the physical dimension of wellness. However, healthcare is far more complex. At RMU, physical therapy students receive training beyond clinical skills—they learn to understand and address social determinants of health.
“Where you live and your socioeconomic status are major determinants of your overall wellness,” said Steve Wilkinson, PT, PhD, program director for RMU’s Doctor of Physical Therapy program. “It’s important to help young professionals step outside themselves and start thinking about how environmental and financial factors impact their patients.”
Empathy and understanding from healthcare providers are necessary for improving patient outcomes.
“If you want a patient to come to the clinic twice a week, but they’re not showing up, we need to ask if there are barriers beyond motivation,” Dr. Wilkinson explained. “In the past, people assumed patients were lazy or didn’t care. But it could be so much more than that. Maybe they don’t have transportation, can’t afford time off work, or clinic hours don’t accommodate their schedule. We must be mindful of all these factors.”
RMU recognizes the need to improve access to physical therapy. That’s why the RMU Physical Therapy Clinic has been providing pro bono physical therapy services to the community for more than a decade.
The clinic is led by students from local universities who work alongside RMU’s licensed specialists, gaining hands-on experience while making a real impact in their community.
Since opening in 2014, the clinic has provided more than $800,000 in free physical therapy services and logged over 29,000 volunteer hours.
“Students are making a difference while still in school by volunteering at the RMU Physical Therapy Clinic,” Dr. Wilkinson said. “It gives them the opportunity to work directly with patients who need physical therapy but can’t afford it. We are actively improving access to care.”
By Jody Genessy
By integrating the Wheel of Wellness into a well-rounded medical and optometric curriculum, it’s safe to say Doctor of Optometry (OD) students at RMU gain an educational experience that’s comprehensive and eye-opening.
Rebranding from the College of Optometry to the College of Optometric Medicine magnifies RMU’s commitment to providing evidence-based, holistic eye care education and training optometrists who are a sight for sore eyes.
“Our students receive comprehensive training in foundational medical courses like physiology, pharmacology, biochemistry, anatomy, histology, and immunology,” said Dr. Adam Hickenbotham, RMU’s College of Optometric Medicine founding dean. “We wanted to reflect that in the name of our college.”
Not only are OD students educated in eye healthcare, they’re also instructed in primary care, internal medicine, dermatology, radiology, surgery, administering EKGs, and much more.
window is because when you look into the eye, you can see the blood vessels and nerves, things like that. When you’re able to see how the tissues and blood vessels are acting straight on without any barriers whatsoever, you can read how that person is doing health-wise.”
RMU students learn how to observe the blood flow through vessels in the eye, which can show plaque build-up and other issues. They’re trained to detect diabetes, high cholesterol, and high blood pressure through the eye. It’s even possible to determine how some medication is working through vision.
“There are a lot of systemic diseases that manifest in the eye,” Dr. Hickenbotham said.
“ONE OF THE GREATEST FEARS THAT
PEOPLE HAVE IS LOSING THEIR SIGHT.
IN TERMS OF EMOTIONAL WELL-BEING,
MAKING SURE THAT PEOPLE CAN SEE AND
FUNCTION WELL IS VERY IMPORTANT.”
RMU’s vision is to prepare them to be eye experts who can serve their patients in a wide range of wellness. After all, being an optometrist is so much more than just dealing with eye charts, glasses, and prescriptions.
“Everybody thinks they know what an optometrist does,” Dr. Hickenbotham said. “But they actually really underestimate the amount of things that we have to learn. We’re an eye doctor, and it’s not an easy task.”
As RMU students learn in classroom and clinical opportunities, they touch on each spoke of the Wheel of Wellness—occupational, environmental, intellectual, spiritual, emotional, physical, financial, and social—all through the lens of the eye.
“You’ve heard before that the eye is the window to the soul,” Dr. Hickenbotham said. “One of the reasons it’s such a good
This valuable information allows optometrists to offer treatment and/or refer patients to other healthcare providers, enhancing physical and emotional well-being. Occupational and intellectual wellness can also be improved through optometric care.
“Vision loss, like presbyopia (an age-related eye condition), costs societies millions,” Dr. Hickenbotham explained, “especially in underserved areas. It affects earning potential, careers, education.”
Children with corrected vision have increased opportunities in education, development, and life satisfaction. Proper eye care benefits adults with increased independence, safety, and reward in their careers. Vision issues can lead to devastating falls, driving incidents, self-care limitations, immobility, and isolation.
“Optometry is the primary caregiver for vision and for sight, and vision is such an important sense to people,” Dr. Hickenbotham said. “One of the greatest fears that people have is losing their sight. In terms of emotional well-being, making sure that people can see and function well is very important.”


By Jody Genessy
While teaching her classes at RMU, Wendy Chase, MA, CCC-SLP, will regularly take time to do something she refers to as a “temperature check.” Along with being a fun diversion from the daily classroom routine, the exercise is a useful method that helps her graduate-level students monitor and manage their stress levels and lives.
Chase, the director of RMU’s Master of Science in Medical Speech-Language Pathology (MS MedSLP) program, begins the temperature check by asking personal questions to gauge their emotional, mental, and physical well-being. Students give themselves a rating on a scale from 1-5 or 1-10 based on how they’re feeling.
The follow-up questions are critical:
“What is it that your friends can help you with?”
“What is it that we can help you with?”
“What is it that you need some outside resources to help you with?”
“And can you get that help?”
“It’s a process of saying, ‘You know, where is all of your stress?’” Chase said.
“The temperature check is important. It’s a way for them to put things in perspective.”
In the exercise, which aligns with the Wheel of Wellness’s holistic approach to health, it becomes apparent that some students are struggling more than others.
“It helps them understand that Susie
over there sounds a little worse off than you. Maybe you can redirect a little bit, and that’ll help you feel more balanced to provide some support to someone else,” Chase said. “Or, you’re rating pretty high right now. Do you have a little extra to hand off to someone else?”
“It’s a process of saying, ‘You know, where is all of your stress?’ The temperature check is important. It’s a way for them to put things in perspective.”
Occasionally, Chase will put an imaginative spin on the exercise. She’ll engage students by having them rate their stressors on a pizza topping scale—from sauce-only (one) to supreme with extra toppings (10)—to demonstrate how much life is piled on at the moment. They’ll raise their fingers to show their score and share what ingredients—pressure points like tests, work, clinical duties, family demands—are on their personal pizzas, which gives her an idea of their demands and workload.
This assessment allows for productive conversations about time management, prioritization, and finding help. It also
helps build community and opens the door for social wellness opportunities. Scores (i.e., their needs) change based on challenges presented at school or in the hands-on clinical situations they experience in the program.
“As an academic program, there’s only so much we can do. Having the University community help provide resources to students becomes critically important, particularly when they are further away from who they are and what they are,” Chase said. “RMU works very hard to help students, which is good.”
While RMU Student Affairs and the speech-language pathology faculty and staff provide beneficial resources for emotional resiliency, Chase has students keep lists of recommendations. This helps future cohorts become familiar with their new setting along with suggested local hair stylists, nail salons, massage therapists, food options, day-trip destinations, etc. It’s a thoughtful way to help students spend more time concentrating on their classroom studies, clinical experiences, and the other pizza toppings.
“They have to learn on two tracks at the same time. They have to learn all of this knowledge and all of these skills, and those are hard to do concurrently,” Chase said, referring to classroom and clinical settings for the MS MedSLP students. “In this profession, those are going to be skills that will be valuable to find. I don’t know if balance is ever achievable, but at least aim for some type of harmony.”


“Not all angels have wings— some have scrubs.”
This anonymous saying captures the profound impact that nurses have on others, a sentiment echoed by President Barack Obama: “America’s nurses are the beating heart of our medical system.”
Just as the heart pumps life throughout the body, nurses infuse care into every aspect of health. Their reach spans the Wheel of Wellness—encompassing occupational, environmental, intellectual, spiritual, emotional, physical, financial, and social dimensions—while providing well-rounded, holistic care.
Allyce Jones, DNP, APRN, PMHNP-BC, CNE, NCMP, PMH-C, witnesses this daily as a reproductive psychiatry specialist, advanced practice registered
By Jody Genessy
nurse, and program director of RMU’s Psychiatric Mental Health Nurse Practitioner (PMHNP) program. With a Doctor of Nursing Practice degree in psychiatric/mental health from the University of Utah, Dr. Jones sees the ripple effects of this approach with patients and passes the knowledge on to her students. As a PMHNP, Dr. Jones can assess, diagnose, and treat patients across the lifespan with mental health disorders.
“I think nursing has always been ahead of the game in this area,” Dr. Jones said. “Nurses recognize that it’s not just the person and the illness, but all of the other factors that go into it, like family, which would be social, relationships, financial resources, spirituality, mental health—all of those things.”
When evaluating patients, she looks beyond symptoms, assessing their physical health, activity levels, financial stability, social relationships, key support systems, career satisfaction, and whether their work gives them meaning and purpose. Dr. Jones recalled a patient whose health improved from getting a job, along with taking prescribed medication. Bolster one area, like occupational health, and emotional or financial wellness may follow. But neglect one, and others might suffer.
“I like to de-prescribe meds, which is part of this wellness wheel. The healthier they get and the more skills they build in these areas, the easier it is to take them off their meds,” Dr. Jones said. “If
they build in a lot of healthy routines, then they might not need meds for panic attacks or anxiety, or whatever.”
For those in a downward spiral, Dr. Jones suggests starting with social ties—reaching out to supportive people and limiting time with those who aren’t—because it’s something they can control.
“Everything is all interconnected all of the time,” she said.
Dr. Jones emphasizes sleep as vitally important to health.
“Sleep is a huge part of mental health and probably the foundation of wellness,” she said. “So that’s a common thing that we treat—issues around sleep.”
Spirituality, which she defines as “finding meaning and purpose in life and living according to your values,” plays a vital role.
“Lots of mental health issues come up when you’re not living in accordance to your values, or you don’t have any meaning or purpose,” she said.
In an ideal world, Dr. Jones envisions healthcare embracing a wellness model where seeking mental health support is as routine and stigma-free as dental check-ups. She’d love for people to evaluate their wellness every 3-6 months.
“Hopefully,” she added, “healthcare will move more towards wellness.”
Whether that shift happens or not, nurses will keep mending bodies, nurturing minds, and strengthening lives. They are, indeed, the heart of healthcare—or, as the saying goes, angels in scrubs.
By Rachel Richards
Garrett Parry, a physician assistant student at RMU, is no stranger to stress. Between academic demands, clinical rotations, and family responsibilities, Parry has experienced firsthand the challenges of balancing a busy lifestyle.
Originally from Salem, Utah, Parry transitioned from finance to medicine, guided by a simple but powerful principle: the most fulfilling careers are rooted in human connection. Today, he is pursuing a Master of Medical Science and a Doctor of Medical Science at RMU—earning top grades, conducting research, and mentoring peers as a teaching assistant and tutor.
“As a graduate student, maintaining physical wellness has been particularly challenging,” Parry shared. “The demands of academic responsibilities, clinical rotations, and family life often left little time for structured exercise.”
Recently recognized with the 2025 Utah Best of State award for Best University Student (see page 4), Parry has found creative ways to adapt.
“I started taking laps around campus during lunch or between classes,” he said. “These brief walks not only helped me stay active but also provided mental clarity and a moment of respite during busy days.”
His understanding of wellness has evolved significantly since beginning his studies at RMU.
“Initially, I believed that achieving balance meant allocating equal time and energy to every aspect of life,” he explained. “However, I’ve come to realize
that true balance involves prioritizing what is most important at any given moment and being adaptable to life’s changing demands. This perspective has allowed me to focus on areas that need attention without feeling overwhelmed by the pursuit of perfection.”
This shift in mindset has not only helped Parry navigate the pressures of graduate school—it’s shaped how he encourages others to approach their own wellness journeys.
“My advice to other students is to let go of the notion of being perfectly balanced,” he said. “Instead, identify the areas that require immediate attention and take small, manageable steps toward improvement. Remember that wellness is a dynamic process, and it’s okay to shift focus as needed.”
Parry knows about finding your focus. Outside of the classroom and clinic, Parry is equally devoted to service. He’s volunteered over 200 hours at a local food pantry, helping families in need access essential resources. He’s supported students with mental and social impairments as a peer tutor and as a Sunday School teacher, guiding youth to develop strong values and a sense of purpose. As a husband and father of two, Parry’s commitment to others is deeply personal and profoundly inspiring.
“Wellness will look and feel different for everybody, but it is important to find what works best for you,” Parry advised. “Be kind to yourself, celebrate small victories, and recognize that each step forward contributes to overall well-being.”

“True balance involves prioritizing what is most important ... and being adaptable.”
By Rachel Richards
“When you drive a car, are you perfect? No, but you recognize when you get off course and correct it. It’s the same with wellness—we accept a little wavering and give ourselves grace not to be perfect.”

Wellness is not just a priority; it’s an advanced degree at RMU. Students can earn a PhD in Health Sciences with a concentration in Health Promotion and Wellness (in addition to other specialties), making RMU a leader in health education. However, graduate school is demanding; even future wellness professionals need guidance in maintaining their health. Recognizing this challenge, RMU faculty, such as Mary Shotwell, PhD, OTR/L, FAOTA, NBC-HWC, actively work to promote finding a healthy balance and embracing emotional, physical, and intellectual wellness.

Consider setting time limits on news and social media apps or designating certain times of the day as “news-free.” You could also create a reading or podcast list focused on personal growth, professional development, or creative interests.
The popular saying goes, “I’ll start on Monday.” It typically applies to diets, workout routines, meditation plans, and earlier bedtimes. However, one of the most significant barriers to long-term wellness is the all-or-nothing mindset many believe is needed.
“When I think of wellness and health promotion in general, I use the analogy of driving a car,” said Dr. Shotwell. “When you drive a car, are you perfect? No, but you recognize when you get off course and correct it. It’s the same with wellness—we accept a little wavering and give ourselves grace not to be perfect.”
Self-compassion is directly linked to emotional wellness and is just as important as physical health. In the wellness world, “consistency over perfection” is a popular mantra. If things feel off in one wellness area, take Dr. Shotwell’s advice: Don’t give up entirely—course correct instead.
Wellness extends beyond physical and emotional health—it also involves intellectual well-being. One of Dr. Shotwell’s most effective strategies for managing stress and mental clutter is being intentional about media consumption. She decided to cut out cable and SiriusXM radio to improve her mental (and financial) well-being.
“I try to practice intentional disengagement,” Dr. Shotwell said. “I choose what information comes into my brain— through books and podcasts instead of the 24-hour news cycle.”
The constant influx of breaking news and social media updates can contribute to mental fatigue. Instead, choosing long-form content, such as books, educational podcasts, or research articles, allows for deeper engagement with meaningful topics.

Think about one small action you can take today to improve your well-being. Can you add an extra glass of water to your daily intake? Step outside for five minutes of fresh air? Replace five minutes of screen time with deep breathing? Small shifts help realign your wellness path without needing a complete overhaul.
Applying these lessons to everyday life can help anyone lead a happier, healthier, and more balanced life. Whether practicing self-compassion, making minor course corrections, or filtering media consumption, these simple adjustments can significantly improve overall well-being.
RMU’s commitment to wellness, led by faculty members like Dr. Shotwell, serves as a model for how small, intentional changes can create lasting health benefits.

Bryan Gee, PhD, OTR/L, FAOTA, lights up when asked how occupational therapy aligns with the Wheel of Wellness— covering occupational, environmental, intellectual, spiritual, emotional, physical, financial, and social health needs.
“We cover every single one,” said Dr. Gee, chair of the Department of Occupational Therapy and Doctor of Occupational Therapy program director at RMU. “It’s easy for us to talk about the role of occupational therapy in health and wellness because the scope of what we do is so broad, and we’re holistic, too.”
Occupational therapists (OTs) and occupational therapy assistants, Dr. Gee explained, use a three-fold intervention strategy that supports multiple aspects of well-being. The focus is on the person, the task, and the environment.
While working with patients, OTs assess patients’ strengths and weaknesses, evaluate the barriers, and modify tasks, which pay healthy dividends. They address physical, psychosocial, and mental health impairments, and get to the heart of whether what patients are doing is healthy and helpful or not.
Adjustments vary and could include teaching helpful stretches for a child with cerebral palsy, guiding parents in playtime, introducing picky eaters to nutritious foods, encouraging a
By Jody Genessy
10-minute walk, tweaking sleep routines, and offering tips on attending social gatherings.
“Let’s look at your habits and routines first and adjust those. Are they helpful?” Dr. Gee said. “From a health and wellness standpoint, it’s like a pebble in the pond. Those ripples go everywhere—if it’s healthy or not.”
These benefits ripple outward. Along with helping clients, OTs play a critical role in supporting caregivers’ emotional, physical, and social wellness. That’s particularly the case for people who help manage patients and loved ones with dementia. Dr. Gee welcomes billing and reimbursement changes that expand occupational therapy options for caregiver support and education.
“They’re the ones that have the burden of day-to-day care and they get burned out, right?” Dr. Gee said. “They need someone to help coach them. Educating these caregivers can help folks stay in their home longer.”
That education component can lead to improved overall safety and healthier outcomes for all communities.
“The wellness aspect for caregivers is just as, if not more, important than for some of our clients that are receiving skilled services,” Dr. Gee added.
Because of the high demand for OTs, RMU and Utah Valley University (UVU) partner on an accelerated pathway. In this unique option, eligible students begin RMU’s entry-level Doctor of Occupational Therapy program as seniors at UVU. This shortens how long it takes to become licensed occupational therapists, allowing passionate practitioners to go from the classroom to the clinic a year sooner.
The Wheel of Wellness guides students in blending evidenced-based methods with holistic participation and healing. While attending graduate school, students who are also practicing OTs get opportunities to find solutions to problems they face on a daily basis.
“In our approach at RMU, the wellness piece just comes up,” Dr. Gee said. “It’s what we do.”
By Jody Genessy
While Maslow’s Hierarchy of Needs (physiological, safety, love/belonging, esteem, and self-actualization) and William Glasser’s Five Basic Needs (survival, belonging, freedom, power, and fun) are often thought of as basic foundations for mental health, RMU Counseling Chair Verl Pope, EdD, identifies five immediate essentials that individuals can focus on:
Breathing • Eating • Sleeping Moving • Laughing
“All of these interplay with each other,” he said. “If we can find a balance— breathe, eat (appropriately), sleep, move (exercise), and laugh—then we’re building resilience for many of life’s difficulties.”
The counterbalance to wellness often starts with stress. Stress could be defined as “the byproduct of unresolved or unrelieved tension or the consequence of keeping the body and mind at a constant state of ‘red alert,” said Dr. Pope. “We all have different levels of ability to handle stress.”
Dr. Pope is a strong proponent of self-awareness, which he describes as “the foundation” for achieving balance and wellness. Knowing where you are can help you decide how to get where you’d like to be. That could include something as simple as returning to his five essentials and realizing that simply breathing is a healthy step forward.
Breathe: Focusing on breathing—in and out, slowly—can pause the body’s reaction and allow oxygen to reach the brain. This allows the brain to process what is happening in the moment.
Eat: Manage mealtime to be a little more regular and less “on the run.” Look for healthy (or at least healthier) food options.
Sleep: First, find a little extra time to get things done before bedtime. Ultimately, we all need sleep, so give yourself the appropriate amounts required—as much as possible.
Move: This may look like scheduled time at the gym, but it doesn’t have to be. Determine what physical movement is enjoyable for you and then find the time to take a walk, hike, or bike ride.
Laugh: Stress often comes from not seeing a way out—practice looking for the immediate joy of where you are right now. Laugh at yourself or the situation. Tell a dad joke; if you need one, just ask Dr. Pope, who can provide several.
However, we also recognize that some situations need more than these five essentials. We may need help, and that’s where talking to friends or family, ecclesiastical leaders, physicians, and mental health counselors can be helpful.
RMU’s Counseling program, which includes both mental health-related degrees and certificates, trains students to treat mental health issues. It helps individuals develop the capacity to recover from setbacks and empowers students with self-efficacy.
“We romanticize the path we didn’t take, believing that it would be way better than the one we are on,” Dr. Pope said.
“Counseling is a helping profession, and one of the paradoxes of my profession is trying to help smooth the path for another while also recognizing that we are very limited in our ability to smooth another’s path. However, if we walk beside someone and help them develop that level of resilience, perhaps they’ll be able to handle the rough path better.”
And hopefully, they’ll breathe, eat, sleep, move, and laugh to a healthy and happy life.
By Rachel Richards
Through its Department of Student Affairs, RMU helps students navigate the rigorous demands of graduate school in a healthy, balanced, and sustainable way.
One way Student Affairs does this is by focusing on supporting students in the Eight Dimensions of Wellness, with a special focus on occupational, intellectual, emotional, physical, financial, and social wellness.
“Remembering to prioritize wellness is so vital for graduate students and their success. They’ll forget because they get hyper-focused on studying and this leads to burnout,” said Lori Sisk-Robinson, former vice president of Student Affairs. “By teaching our students how to focus on the dimensions of wellness, they will be better healthcare providers because they’ll be able to do that with their patients.”
By guiding students through setbacks and equipping them with strategies for balance, RMU proves that success isn’t just about reaching the finish line—it’s about having the support to keep going.
Between graduate coursework, jobs, family responsibilities, and personal well-being, students often struggle to balance it all. Student Affairs focuses on helping students keep their lives well-balanced by utilizing the Wheel of Wellness. When students experience too much stress or burnout, Student Affairs will utilize the Eight Dimensions of Wellness self-assessment from the Substance Abuse and Mental Health Services Administration (see page 16) to help them identify areas that need focus.
Sisk-Robinson recalls the story of a student overwhelmed by his studies and constantly drained.
“I worked with him to evaluate the areas of his wellness that were hurting from hyper-focusing on studying and encouraged him to use time blocking to prioritize sleep and self-care,”
Sisk-Robinson said. “He didn’t want to decrease his study time, but I challenged him to try it out. Four weeks in, he was studying less but retaining more information because he gave himself breaks, and his grades went up.”
This small but powerful shift transformed his ability to manage stress, improve focus, and achieve academic success.
“When he came into our office, he was on academic probation,” Sisk-Robinson said. “After making those changes, he graduated and is practicing now.”
Life happens—unexpected challenges, personal struggles, and financial hardships can pull students away from their studies. But at RMU, stepping away doesn’t mean the end of the journey. The Student Success Program actively tracks and re-engages withdrawn students, ensuring they have the resources and support to return when ready.
“This University wants what’s best for students,” said Sisk-Robinson. “Sometimes it’s best if the student takes a few months off to take care of things, and we’re ready to help them when they return.”
RMU doesn’t just enroll students; it invests in them for the long haul. Whether a student needs time off for personal reasons or financial recovery, RMU’s approach is one of flexibility and care.
“The Student Success unit stays connected to each student. Last semester, our Student
Success team helped 29 students return to their studies,” said Sisk-Robinson.
By allowing students to step away without fear of losing their place, RMU fosters a culture of compassion and resilience.
At RMU, success isn’t just about earning a degree—it’s about becoming a stronger, healthier, and more capable healthcare professional ready to make a lasting impact. Student Affairs is helping accomplish this goal one student at a time.
RMU’s Student Affairs team provides many essential resources, such as:
ADA accommodations for students with disabilities
Civil Rights support for Title IX, ADA, Section 504, VAWA, and Clery
Counseling services for emotional wellness
Local student discounts to help save money
Student success coaching for academic, mentoring, and career guidance
Recreation services offer various sporting gear to get outside and take a break
Service projects that build a sense of community and purpose
Student leadership & engagement opportunities to connect and make a difference
Student lounge area where on-campus students can relax and enjoy snacks



By Jody Genessy

Alisa Ward, PhD, isn’t a stranger to being busy or balancing things in life. She’s a mom, a wife, an active member of her church and community, a national board-certified health and wellness coach, and a full-time college faculty member at Point Loma Nazarene University in San Diego, California. In recent years, she also managed to carve enough time out of her packed schedule to earn her doctoral degree at RMU, and graduated in 2023.
In her dissertation for her Doctor of Philosophy in Health Sciences, Health Promotion & Wellness concentration, Dr. Ward explored a variety of wellness models and discovered that a holistic, interconnected approach to well-being transcends a traditional physical health focus.
In other words, her research findings mirrored the balanced approach she strives for in her personal and professional life while juggling numerous responsibilities.
“The idea of balance is noted in many models of wellness. Each of the various dimensions of wellness are intertwined, and they’re impacting each other,” Dr. Ward said. “It’s hard to be physically well if you are socially isolated or lonely. Wellness models offer a visual that expands our understanding beyond just physical health. They provide a framework that broadens our thinking.”
“We are familiar with the data on physical health, exercise, and eating, but there is also data on the importance of sleep, social connection, and a spiritual sense of purpose. Even small attention to these dimensions plays a huge role in our health.”
Dr. Ward likes how the various iterations of the Wheel of Wellness offer a representation about how all of the dimensions are interconnected. This concept provides a visual that encourages people to consider and work on all aspects of health.
“They allow us to think more holistically about health beyond just exercise and diet,” she said. “It shows us we’re complex, multifaceted.”
Dr. Ward, who earned a BA in physical education at Point Loma and a master’s degree in kinesiology at Fresno State, went into her research focused on possible correlations of exercise adherence and people’s perception of wellness on personal and broad levels.
being. A balanced approach, where all dimensions are considered, can lead to a more sustainable state of wellness.”
While acknowledging the benefits of wheels that include eight dimensions, Dr. Ward focuses on five core foundational ones— emotional, intellectual, physical, social, and spiritual—in the “Lifestyle as Medicine” courses she teaches.
“When people are isolated, stressed, or struggling emotionally, it directly affects their physical health,” she said. “The emotional and physical dimensions are so intertwined— if you’re not emotionally healthy, it can undermine your ability to stay physically healthy.”
Having taught for
In an attempt to help improve her students’ lives, Dr. Ward has them ask themselves a few questions: What do you enjoy doing? What do you have access to? What are you currently doing? She asks them to consider what lifestyle behaviors they can work on or change in their current unique circumstances as part of their self-care efforts.
Having taught for 16 years, Dr. Ward gracefully teaches students that integrating wellness into real life isn’t simple or easy. There are challenges: lack of awareness, time constraints, resistance to change, and unequal access to resources like green spaces or mental health support.
“I wondered if we perceive ourselves to be unhealthy, are we less likely to be physically active? And if we perceive ourselves to be healthy, are we more likely to be physically active?” she said. “And if somebody has negative perceptions toward their overall health and well-being, how could we help to flip those perceptions or change their narrative? And could we statistically find some sort of correlation with people who are more likely to be physically active?”
There are challenges.
Encouraging progress over perfection through small, doable steps—being proactive rather than reactive—and implementing healthy habits can be empowering, especially when it involves doing things that you like to do. That’s why she encourages students to aim for incremental changes and to not try cramming a lifetime’s worth of self-improvement into a 15-week semester.
In her dissertation work, she investigated models of wellness and tools to measure wellness.
“The results showed that it’s almost impossible to parse out individual dimensions of wellness because they are so interconnected,” Dr. Ward said. “The interconnectedness of these dimensions shows that no single aspect can thrive without the support of the others. Focusing on one area—say physical health—might not be enough if you’re neglecting emotional or social well-
“Change takes a really long time and requires us to constantly and consistently be mindful toward those things,” Dr. Ward said. “Everybody’s view of health is slightly different. Our own wellness journeys can look vastly different, and we should be okay with that. We need to realize we can have grace with ourselves. We are not perfect beings. We’re humans.”
The wheel doesn’t need to be spinning at 100 mph to achieve wellness. It just needs to be moving forward.


EMontoya by wielding swords and going on the attack against a formidable foe.
The playful sword fighting—with foam swords, of course—is an entertaining and engaging part of a student-led exercise program that RMU hosts twice a week for people battling Parkinson’s disease. The lunging and laughing are among many activities they do to strike back at a neurodegenerative disorder that’s attacking them.
If he wanders by, the Six-Fingered Man—Montoya’s nemesis in “The Princess Bride”—needn’t fret … yet. He should at least prepare to die with a smile on his face if he sees all the colorful foam pool noodles and fencing fun.
“I come here for the exercise because it has throttled down the rate of progression of my Parkinson’s. It has made a definite difference,” said Santaquin resident Craig Barlow, a retired metallurgical engineer who was diagnosed four years ago. “I absolutely look forward to it.”
Launched in 2022 as an integrated clinical experience for physical therapy, the Parkinson’s exercise program expanded to include speech-language pathology. Occupational therapy will join soon. These programs teach students who collaborate to help patients manage Parkinson’s disease, a condition that impairs movement, balance, and other

“While Parkinson’s disease is a progres sive neurologic disorder without a cure, research suggests that regular, high-intensity activity can slow the progression and improve quality of life,” said RMU Associate Professor Christa Young, PT, PhD, NCS, who started the program with fellow physical therapy faculty member Tyler Luszeck, PT, DPT, NCS.
“This program aims to provide an opportunity for that regular activity while training student healthcare providers to deliver excellent, effective, and evidence-based care.”
Twice a week during lunchtime, the Parkinson’s patients arrive in their workout clothes and participate in a wide variety of exercises and activities. For an hour, the sixth floor of the RMU Tower bursts into a hive of carefully planned, supervised and safely executed activity. There’s hustling, bustling, memorizing, reciting, sweating, smiling, snorting, bonding, teaching, learning, encouraging and laughing—lots of laughing.
“It’s a whole lot of fun dancing, jamming to music, throwing things,” Dr. Young said, smiling. “People walk by and ask, ‘What’s going on?’”
This popular high-intensity, adaptive exercise and maintenance program serves dual (and duel) purposes.
It gives second-year Doctor of Physical Therapy and Master of Science in Medical Speech-Language Pathology students an

“While Parkinson’s disease is a progressive neurologic disorder without a cure, research suggests that regular, high-intensity activity can slow the progression and improve quality of life.”
opportunity to actively learn while helping people. It also provides a group of community members dealing with an incurable progressive condition the chance to stimulate their bodies, minds, and voices.
With guidance and feedback from faculty, students design the classes to address the
major mobility, speech, and cognitive concerns for individuals in lively and energetic ways.
“We work on incorporating with physical therapy as well as planning separate speech activities for them that focus on loudness and cognition and dual tasks in


general,” said Jordan Pearson, an RMU speech-language pathology student.
“We’ve had to learn a lot about scaffolding because, especially in a group setting, there are some patients who are really quick, really fast cognitively, and there are others who are struggling a little bit more. It’s important to learn how to scale activities to meet patients where they’re at rather than pushing them too far out of that therapeutic zone.”
In addition, all physical therapy students are encouraged to be one-on-one helpers. They keep participants safe and individualize the intensity of activities, providing an opportunity for real-time application of the skills they are learning in coursework.
“The students are great. They keep us safe. They hold onto the belts so we don’t fall,” Barlow said. “They enjoy spurring us on, ‘Take a step higher, move a little faster.’ They encourage us.”
While physical therapy students help patients do activities that work on strength, endurance, balance, moving in all directions, and posture, the speech-language pathology volunteers give class members a mental workout and help them speak up.
Students plan and prepare for each hourlong session, making sure to include activities that simultaneously engage the seniors’ motor skills and mental acuity— all while having a ball.
“The interprofessional collaboration has been huge. We go through our plan together,” RMU physical therapy student Stephen Powers said. “While we’re doing exercises, we’ll have them do standing marches and then they’ll work the speech answering questions so that you have that dual tasking.”
Sometimes, the group will go on simulated backpacking and camping adventures. They’ll serve guests food and drinks from a platter they carried. They’ll stomp and clap while saying their own name and the name of another person. They’ll play floor hockey, walk like monsters, decorate rooms, go hunting, and make snowmen. Recently, group members transformed into Rocky Balboa clones and did boxing exercises.
“When I taught on Halloween, we had them run down the hall as if they were doing a ding dong ditch,” Powers said, grinning. “Then you would do monster walks. Other people have them climbing over tables (if able) or getting up and down.”
During the holidays, students helped seniors zig-zag, side-step, duck, and jump through an obstacle course in the hallway. Chuckles ensued as the patients repeated jokes: How did the reindeer learn to play the piano? He was elf-taught. What do gingerbread men use when they break their legs? Candy canes.
RMU speech-language pathology student Aubrey Huffaker also enjoys the aspect of getting to work with students and supervisors from other disciplines. It’s a model of interdisciplinary collaboration.
“It’s an interdisciplinary team, so it’s been really fun to learn how to work with physical therapists and their supervisors, as well as my supervisor and my team, and to be able to coordinate,” she said. “And it’s been extremely valuable because it’s real-life practice outside of the classroom.”
Getting to know the patients on a personal level has been rewarding, Huffaker admitted. She also loves how they benefit in multiple ways.
“The students are great. They make it fun. Exercising at home is just kind of ‘blah’ compared to what they do here. They make it a lot more enjoyable to exercise.”
“It’s extremely valuable for the patients,” she said. “It’s a huge social outlet.”
Perri Freeman values the forged friendships, including with the amicable Fred Nozawa.
“Fred and I have become kind of tight. I’m just like Fred,” the physical therapy student said while waving around a foam sword. “And then Deidre (Johnson) and I have gotten to be pretty good friends. I just smack her with a pool noodle as we walk by. Usually, I’m getting attacked, though.”
Building relationships and trust helps the students and the patients feel more comfortable with pushing limits to maximize progress and knowing when to let them take it at an easier pace. For instance, there are days when patients might use a walking stick and other days when they use a walker while doing the exercises. The familiarity allows students to know when to push harder because they know the patients can do more.
“It’s been stellar,” added Spencer Ochko, a physical therapy student. “You get to hang out with somebody who’s happy to be here, and you get to see them do awesome things.”
Students change each semester—allowing more volunteers the opportunity for hands-on service and learning about Parkinson’s and geriatric care—but most of the patients referred by local neurology offices keep coming back for more. Because of logistics, the free sessions are capped at 15.
“It’s just taken off,” Dr. Luszeck said. “A lot of people have been here since Day 1 and they don’t want to leave. It’s a passion.”
Karla Bowles is grateful for how the program has helped her husband, Jeff.
“The best time is when they push them to do more than they would probably do on their own,” she said.
Tracked data from testing at the beginning and end of each semester reveals positive results, even if it’s simply maintaining levels of mobility and cognition.
“It gets him moving, and that’s the best medicine for Parkinson’s—movement,” Bowles said. “It’s the only thing that really prolongs the downward spiral.”
Social interactions are an important part
of the program. Parkinson’s can lead to isolation and loneliness.
“The students are great. They make it fun,” Barlow said. “Exercising at home is just kind of ‘blah’ compared to what they do here. They make it a lot more enjoyable to exercise. We love the competitive stuff. We do volleyball sometimes, soccer, sword fights like today.”
With that, his friend Fred jokingly mentioned the famous sword-fighting secret that Montoya revealed in “The Princess Bride.” En garde, future foes: perhaps he’s also not really left-handed.
Either way, the fight against Parkinson’s disease will continue at RMU—one playful jab at a time.


By Jody Genessy
“Anything is possible” is the inspiring message embraced by the Ironman community—an empowering mantra for athletes who aspire to complete a three-fold endurance race that includes a 2.4-mile swim, a 112-mile bike ride, and a 26.2-mile marathon.
Fortunately for his students at RMU and for a group of triathletes with unique physical challenges, Stephen Black, PhD, embodies the ambitious spirit of that Ironman ethos for himself and instills it in others.
In his roles as an RMU adjunct professor of health sciences and as the coordinator of physically-challenged athletes for Ironman World Championship events, Dr. Black blends his medical expertise, logistical mastery, and deep compassion to help others achieve great things—on the race course, in graduate school, and in life.
Giving back comes as second nature to the Ironman finisher and RMU alumnus.
After earning his doctorate in sports medicine at RMU in 2005, Dr. Black felt compelled to pay it forward to the graduate healthcare institution that helped enrich his life and career so he began teaching remotely as an adjunct professor. He draws from his professional medical training and clinical experience to teach doctorate-level courses about subjects like orthopedic surgical procedures and therapeutic interventions. Teaching complemented the professional work he accomplished while managing a large sports medicine practice across four New England states.
Over the years, Dr. Black has found a way to beautifully blend his love for sports medicine, athletic inspiration, personal achievement, serving others, and the sport of triathlon.
Personally, he’s competed in more than 300 endurance events, including six Ironman World Championships. His triathlon roots trace to the mid-1980s, when the former collegiate gymnast turned to endurance sports for fitness.
“It’s a great sport,” Dr. Black said of triathlons. “The people involved are great. To me, it’s a lifestyle. It’s a great way to maintain your fitness, both physically and mentally. I was

always looking for a way to stay fit after college. I just kind of fell in love with it.”
After completing his first Ironman World Championship in Kona, Hawaii, in 1989, his athletic trainer and physical therapist career led him to sports medicine leadership. In 1997, Dr. Black aided wheelchair athlete John McCarthy through Kona. McCarthy was the first wheelchair athlete to complete the Ironman World Championship, leading the way for other athletes with disabilities to qualify and complete the grueling event. This led Dr. Black to take on coordinating care for challenged athletes at the World Championships. This role has sent him across the world—from Hawaii to France to New Zealand—to help support anywhere from four to 16 athletes per Ironman event.
“It’s a way that I can give back to a sport that’s given me so much,” Dr. Black said. “I’m so grateful and really take a lot of pride in assisting those athletes to the finish line.”
Months ahead of race day, Dr. Black connects with Ironman qualifiers and tailors plans for their specific needs. His athletes are required to complete the 140.6-mile race in the same amount of time (17 hours or under) as able-bodied athletes, and he makes it his personal goal to help them as much as he possibly can. With that knowledge, he gets onsite a week and a half before the race starts to offer them as much assistance as possible. He orients them to the course and game plans their strategy.
Some of his athletes have special needs as amputees. Others need coordination for their equipment, like handcycles and race wheelchairs, and communication with personal assistants who help transfer them from the water and transition on and off their bike. He lines up helpers and preps gear. He also assists with clothing changes, nutrition, treating injuries and, best of all, celebrating their triumphant finishes.
“It’s one thing for us as able-bodied athletes to be able to train and go that distance,” Dr. Black said. “But for
somebody that’s neurologically impaired, somebody with an intellectual disability, an amputee? It’s a whole different game for them.”
Thanks to Dr. Black and his team, it’s a more winnable game for people of all abilities and adversities.
One year, Dr. Black assisted a paralyzed cyclist who happened to suffer second-degree burns on her lower legs en route to an Ironman in St. George, Utah. She’d placed her bare feet, numb from a spinal injury, on the dashboard while driving from Las Vegas and didn’t feel them getting burned on the hot surface. His team offered care that enabled her to compete, and bandaged her wounds mid-race to help her keep going toward the finish line. His team helps with everything from cardiac emergencies


to swim-induced pulmonary edema to athletes accidentally gulping in too much water—all in the pursuit of conquering themselves and the course.
Dr. Black’s reward is the simple act of gratitude from the athletes—amputees, neurologically impaired individuals, and others who defy limits while taking the “Anything is possible” message to inspiring levels.
“The athletes are just so gracious for the care that they get. They’ve all got these unique stories, so to be able to assist them in completing an event like that is just so gratifying,” Dr. Black said. “It motivates me to continue doing what I’m doing. As I say, the sport has given me so much. I’m so grateful and really take a lot of pride in assisting those athletes to the finish line.”


HARTGRAVES AWARD FOR EXCELLENCE IN TEACHING
Rhodri Purcell, PT, MPT, EdD, OCS, CSCS

Dr. Rhodri Purcell is an associate professor for the Doctor of Physical Therapy program and supervises students at RMU’s pro bono Physical Therapy Clinic in Provo. His experience as a licensed physical therapist has included a variety of settings, including military, acute care, home health, pediatrics, and outpatient orthopedics.
With an average instructor rating of 4.72/5 from his students over the past three years and the comments from evaluations, it is clear that Dr. Purcell has positively impacted his students’ education and learning.
“Dr. Purcell’s feedback on assignments and practical exams is extremely helpful, and you can easily tell that he pays close attention and wants to make us better,” one student noted. “You can also really tell that Dr. Purcell cares about everyone in the class, and wants us to be successful.”
He is often praised for making complex concepts accessible, fostering confidence, and using innovative, hands-on teaching methods.
ADJUNCT FACULTY AWARD
Sara Nottingham, EdD, LAT, ATC

Dr. Sara Nottingham has been with RMU since 2021 and is an adjunct faculty member with the Doctor of Philosophy in Health Sciences (PhD) program. Dr. Nottingham is also a professor and the director of the athletic training program at the University of New Mexico.
Dr. Nottingham has received an average instructor score of 4.8/5 for the last three years.
She is recognized for engaging, professional delivery, and fostering a dynamic learning environment with real-world examples.
“This was a phenomenal class,” one student said. “It was incredibly well-organized, assignments were thoughtfully designed and provided in a manageable time frame. The assignments were just enough without being overwhelming and had just the right amount of challenge, which maximized my learning potential and did not make me feel overwhelmed.”
Raegan Furman, PhD, OTR/L

Dr. Raegan Furman has been with RMU since 2021 and is an assistant professor in the Doctor of Occupational Therapy program, facilitating pediatric, scholarly inquiry, and adult neurological courses. She received a PhD in Health Sciences with a concentration in neurological rehabilitation from RMU.
Her average instructor score has been 4.87/5 over the past three years.
Nomination letters submitted for Dr. Furman give evidence of the effort and dedication that go into her teaching.
“Dr. Furman consistently demonstrates a commitment to developing us as students academically and professionally by challenging us to engage in course materials in innovative ways and going above and beyond what is expected of her as a faculty member,” one student wrote. “Dr. Furman blends best teaching practices with the online model to provide the highest quality of education and engaging course materials.”
She specializes in pediatric and neurological occupational therapy, serving as chair of the Teaching Effectiveness and Faculty Development Committees.
Dr. Furman is noted for innovative teaching, mentoring, and creating a safe space for student inquiry.
