HOUSTON
Hospital News pg.7

The AI Therapist Will See You Now
By Pooja Chettiar
Recently, I found myself pouring my heart out, not to a human, but to a chatbot named Wysa on my phone. It nodded—virtually—asked me how I was feeling and gently suggested trying breathing exercises.
As a neuroscientist, I couldn’t help but wonder: Was I actually feeling better, or was I just being expertly redirected by a well-trained algorithm? Could a string of code really help calm a storm of emotions?
Artificial intelligence-powered mental health tools are becoming increasingly popular—and increasingly persuasive. But beneath their soothing prompts lie important questions: How effective are these tools? What do we really know about how they work? And what are we giving up in exchange for convenience?
Of course it’s an exciting moment for digital mental health. But understanding the trade-offs and limitations of AI-based care is crucial.

game-based exercises.
Somewhere in the middle are chatbot therapists like Wysa and Woebot, using AI to mimic real therapeutic conversations, often rooted
influenced his son’s mental state. These cases raise ethical questions about the role of AI in sensitive situations. Where AI comes in
Neuroscientist Explores Whether Chatbots Can Really Improve Mental Health
Stand-in meditation and therapy apps and bots
AI-based therapy is a relatively new player in the digital therapy field.
But the U.S. mental health app market has been booming for the past few years, from apps with free tools that text you back to premium versions with an added feature that gives prompts for breathing exercises.
Headspace and Calm are two of the most well-known meditation and mindfulness apps, offering guided meditations, bedtime stories and calming soundscapes to help users relax and sleep better. Talkspace and BetterHelp go a step further, offering actual licensed therapists via chat, video or voice. The apps Happify and Moodfit aim to boost mood and challenge negative thinking with
in cognitive behavioral therapy. These apps typically offer free basic versions, with paid plans ranging from US$10 to $100 per month for more comprehensive features or access to licensed professionals.
While not designed specifically for therapy, conversational tools like ChatGPT have sparked curiosity about AI’s emotional intelligence.
Some users have turned to ChatGPT for mental health advice, with mixed outcomes, including a widely reported case in Belgium where a man died by suicide after months of conversations with a chatbot. Elsewhere, a father is seeking answers after his son was fatally shot by police, alleging that distressing conversations with an AI chatbot may have
Whether your brain is spiraling, sulking or just needs a nap, there’s a chatbot for that. But can AI really help your brain process complex emotions? Or are people just outsourcing stress to silicon-based support systems that sound empathetic? And how exactly does AI therapy work inside our brains?
Most AI mental health apps promise some flavor of cognitive behavioral therapy, which is basically structured self-talk for your inner chaos. Think of it as Marie Kondo-ing, the Japanese tidying expert known for helping people keep only what “sparks joy.” You identify unhelpful thought patterns like “I’m a failure,” examine them, and decide whether they serve you or just create anxiety.
But can a chatbot help you rewire your thoughts? Surprisingly, there’s science suggesting it’s possible. Studies have shown that digital forms of talk therapy can reduce symptoms of anxiety and depression, especially for
Legal Matters
Texas’s New IV Therapy Law – What It Means


By Stephen M. Angelette, J.D.
Laura D. Pone, J.D.
Polsinelli, PC
The
Capping a frenetic legislative session with an intense focus on medical spa services, Texas Governor Greg Abbot signed HB 3749, also known as “Jenifer’s Law”. The final version of Jenifer’s Law attempts to address shortcomings in Texas’s oversight of elective IV therapy, but leaves out several other key medical spa reforms that were originally proposed
as part of HB 3749 and other bills introduced this session.
Jenifer’s Law was introduced in response to the tragic death of Jenifer Cleveland, who passed away following an IV infusion administered under troubling circumstances. The original form of HB 3749 and other, similar bills, introduced a number of medical spa reforms, including patient notices, medical direction qualifications and other requirements, and even state licensure for personnel performing cosmetic medical procedures. Through the legislative process, these requirements were meaningfully narrowed to focus specifically on the provision of elective intravenous therapy, the root cause of the Jenifer Cleveland tragedy.
The final version of Jenifer’s Law, effective September 1, 2025, reforms Texas practices for elective IV therapy, but also leaves open significant

ambiguity for providers evaluating their current practices.
Key Issues
What is Elective IV Therapy?
Jenifer’s Law applies only to “elective intravenous therapy,” which the law defines as a procedure: “(a) to administer fluids, nutrients, medications, or blood directly into a patient’s bloodstream through a vein, (b) that is sought by the patient to alleviate symptoms of temporary discomfort or improve temporary wellness; and (c) that is not administered in (i) a physician’s office, (ii) a health facility licensed under Subtitle B, Title 4 Health and Safety Code; (iii) a mental hospital . . .; or (iv) a hospital maintained or operated by [the state].” This definition contains
several key features that providers must navigate to evaluate their current operations under these new provisions: 1. Elective IV therapy is “sought by the patient to alleviate symptoms of temporary discomfort or improve temporary wellness.” Under this definition, it is not difficult to imagine the legislature’s intent to regulate patient-driven access to hangover cures or vitamin infusions they might have learned about from their Instagram influencer du jour. But, in the sense that almost all care is sought by a patient, and the hope is that all symptoms are temporary


Heat-Related Illnesses Among Children on the Rise
Study Reveals 170% Increase Over 12 Years in Emergency Department Visits Among Children Exposed to Excessive Heat
Highersummer temperatures are resulting in more children seeking emergency care for heat-related illnesses, with nearly 1 in 5 needing hospitalization, according to new research from UT Southwestern Medical Center published in Academic Pediatrics.
A review of emergency department (ED) visits at Children’s Health campuses in Dallas and Plano during the months of May through September, 2012–2023, found that heat-related illness encounters, as a proportion of total ED cases, increased 170%, with the higher level of visits correlating with hotter weather.
“As extreme summer temperatures become more frequent, we’re seeing a rise in heat-related illnesses among children,” said study leader Andrew Yu, M.D., a pediatric hospitalist at Children’s Health and Assistant Professor of Pediatrics and Director of
the Pediatric Residency Program at UT Southwestern.
Heat-related illnesses range from mild heat cramps and fainting to heat stroke, heat exhaustion, and rhabdomyolysis – a severe and potentially fatal condition caused by prolonged exertion in extreme heat that leads to muscle breakdown.
While most prior research has focused on adults or high school athletes, little is known about how heat affects the broader pediatric population. Children are more vulnerable due to physiological and behavioral factors. They have a larger surface area relative to body mass, have lower sweat production, and often have difficulty determining when it’s time to rest or hydrate.
“This research strengthens the evidence linking extreme heat to pediatric health risks, helping define the burden and inform future prevention strategies,” said Taylor Merritt, M.D.,

a third-year pediatric resident at UT Southwestern and Children’s Health and the study’s lead author. “By identifying trends and demographic patterns, the study raises awareness among clinicians and caregivers to better recognize and protect children at increased risk.”
To evaluate the risk, researchers reviewed more than 2 million ED visits. More than 500 of those visits were linked to excessive heat, the effects of heat and light, or rhabdomyolysis. Because rhabdomyolysis differs significantly from other heat-related conditions, researchers assessed it separately.
Among other findings:
• Children living in low-opportunity neighborhoods — those with less access to quality schools, parks and playgrounds, clean air, access to
healthy food, health care, and safe housing — were disproportionately affected.
• Children with rhabdomyolysis were admitted to the hospital 63% of the time.
• Children with other heat-related illnesses were discharged from the ED in 96% of the cases.
• Compared with rhabdomyolysis patients, children with other diagnoses were more likely to be under age 12, Hispanic, on government insurance, or from very low-opportunity neighborhoods. Researchers said additional study is needed to understand how neighborhood factors such as tree canopy and urban heat islands could affect risk.



Oncology Research
Food Insecurity and Cancer Patients

By Samip R. Master, M.D., Texas Oncology–Deke Slayton Cancer Center
WhenCancer and cancer care
can take a heavy toll on the body, and getting proper nutrition and eating healthy foods can support both treatment and recovery. However, the extra burdens of cancer care can mean less time and money to purchase or prepare nutritious and healthy meals. Across the United States, 17 to 55 percent of cancer patients are affected by food insecurity, when a person cannot easily and regularly access high-quality food.
For patients, food insecurity can stem from several factors.
Limited access to healthy foods may result from having few grocery
stores nearby or challenges in reaching those stores.
Financial barriers, including high copays and increased travel expenses, can reduce the funds available for purchasing food.
Additionally, physical barriers such as difficulty finding and preparing healthy recipes, low energy to stand and cook, or trouble using utensils can further complicate securing nutritious meals.
Food Insecurity Affects Health
Access to nutritious food and a healthy diet can impact a person’s risk factors for health issues, as well as their outcomes. For patients with cancer, this may include:
Issues with Side Effects
Food choices can help reduce the side effects of cancer and cancer treatment. For patients experiencing weight loss, nausea, diarrhea, or other symptoms related to eating and digestion, it can be important to pick the right foods and prepare them in
a specific way. Similarly, when patients don’t meet their dietary needs, side effects can be worse.
Issues with Treatment
A 2020 study in the Journal of Clinical Oncology found cancer patients with financial barriers to food access were more likely to skip, delay, or change their prescription medications. Food insecure patients were less likely to be able to make their treatment a financial priority. Nutrition can also affect other conditions that make cancer treatment more complicated, such as diabetes and heart disease.
Issues with Recovery

income and access to food.
Finding Help for Food Insecurity
Adequate nutrition is an important part of staying healthy after cancer treatment. For many patients, the high cost of cancer care carries on even after treatment is finished. Making up missed work, paying medical bills, and getting out of debt can all cut into food budgets. Societal and policy issues can also make it harder for members of certain communities — influenced by factors such as race, ethnicity, location, income, and disability — to maintain
Because a nutritious diet is essential to maintain health, connecting to resources and support is an important part of cancer treatment and survivorship care. The US Oncology Network has partnered with find help, America’s leading social care network, to connect patients with resources, including financial assistance, transportation to your appointments, food pantries, childcare, services, and more. Search at usoncology.findhelp.com to connect with resources in your community.


Mental Health Study:
Nature-Inspired Virtual Reality Boosts Emotional Well-Being in Older Adults Living with Dementia
By Ann Kellett, PhD
That’sthe main finding from a pilot study led by Junhyoung “Paul” Kim, PhD, a health technology researcher with Department of Health Behavior in the Texas A&M University School of Public Health. It also sheds light on important challenges this population faces when using this virtual reality technology for the first time.
Published in the American Journal of Health Behavior, the study involved 11 residents of a long-term memory care facility who were diagnosed with mild to moderate Alzheimer’s disease.
Twice weekly over five weeks, participants engaged in nature-themed virtual reality sessions using Oculus Quest 2 headsets and the Nature Treks Virtual Reality application.
For each 20- to 30-minute session, users were immersed in calming, natural landscapes, including
forests, meadows, oceans and sunsets, and could interact with animated plants and animals.
“While research supports the benefits of nature-based activities for people living with dementia, these individuals often face significant barriers—such as limited mobility, environmental obstacles and safety concerns—that prevent them from engaging in real-life outdoor programs,” Kim said. “This intervention allowed participants to safely explore and connect with diverse nature-themed virtual reality settings in a personalized and meaningful way.”
The research team used a pretest-posttest approach to quantify changes in emotional well-being and perceived quality of life. Results showed a significant increase in feelings of pleasure and alertness, along with a reduction in negative emotions such as anxiety, sadness and anger. Participants reported a noticeable improvement
SHOULDN’T YOU BENEFIT

in overall quality of life following the intervention.
The team also collected qualitative data during the final week of the study through in-depth interviews with participants and their caregivers.
“Three core themes emerged from the interviews: participants’ enjoyment of exploring virtual natural environments, the novelty and excitement of the virtual reality experience and the triggering of fond memories and reminiscence,” Kim said.
The study also revealed several usability barriers, with some participants struggling to use the headsets and handheld controllers.
The researchers noted these difficulties point to a need for more age-friendly
design features.
“Simplifying the control interfaces and improving the ergonomic fit of headsets could significantly enhance accessibility for older adults with cognitive impairments,” Kim said.
Still, the results are promising, according to the researchers.
“Our findings underscore the therapeutic potential of immersive technology for older adults and supports the ongoing efforts to design virtual platforms for them,” Kim said.
“They offer a promising step forward, especially as the number of Americans living with Alzheimer’s disease— currently over seven million— continues to grow.”

Hospital News
Memorial Hermann Health System Among Nation’s Top Performing Hospitals for Treatment of Heart Attack Patients
Memorial Hermann Health System is pleased to announce that nine hospitals within the system have received the American College of Cardiology’s NCDR Chest Pain –MI Registry Platinum Performance Achievement Award for 2025. Additionally, two hospitals within the system have received the Silver Performance Achievement Award for 2025.
Only 323 other hospitals nationwide received the Platinum Performance honor, and 79 other hospitals received Silver Performance recognition.
“We are very proud that each one of our 11 facilities that treats patients for heart attack and chest pain have been recognized by the American College of Cardiology
for excelling in this area of care,” said Dr. Majid Basit, chair of Memorial Hermann’s Cardiology Clinical Programs Committee. “Achieving Platinum and Silver Award status on the Chest Pain – MI Registry underscores our system-wide pledge to maintaining excellent outcomes and consistent quality improvement in cardiovascular care.”
The award recognizes Memorial Hermann’s commitment and success in implementing a higher standard of care for heart attack patients across each hospital campus within the system, and signifies success in treating these patients to standard levels of care as outlined by the American College of Cardiology/ American Heart Association clinical guidelines and recommendations.
“It is an honor to award
Platinum Performance Achievement Award Winners:
• Memorial Hermann Cypress Hospital
• Memorial Hermann Greater Heights Hospital
• Memorial Hermann Memorial City Hospital
• Memorial Hermann Northeast Hospital
• Memorial Hermann Southeast Hospital
Memorial Hermann Health System with the Platinum Performance Award for their valuable national leadership and dedication to meeting comprehensive performance measures in patient care,” said Michael C. Kontos, MD, FACC, chair of the NCDR Chest Pain – MI Registry Steering Subcommittee, and cardiologist at Virginia Commonwealth University Medical Center. “The receipt of this award indicates that Memorial Hermann Health System remains committed to providing top quality, guideline-driven care for heart attack patients. Their success ensures patients are receiving the highest quality cardiovascular care.”
The Centers for Disease Control estimates that over 800,000 Americans suffer a heart attack each year. Chest Pain MI Registry empowers health care provider teams to consistently

treat heart attack patients according to the most current, science-based guidelines and establishes a national standard for understanding and improving the quality, safety and outcomes of care provided for patients with coronary artery disease, specifically high-risk heart attack patients.
• Memorial Hermann Southwest Hospital
• Memorial Hermann Sugar Land Hospital
• Memorial Hermann-Texas Medical Center
• Memorial Hermann The Woodlands Hospital
Silver Performance Achievement Award Winners:
• Memorial Hermann Katy Hospital
• Memorial Hermann Pearland Hospital
St. Luke’s Health Accepting 2026 Grant Applications
St. Luke’s Health encourages local nonprofit agencies to apply to its grant funds program to help improve the health, mental well-being and health equity of the Houston region.
For fiscal year 2026, St. Luke’s Health will fund agencies tackling issues related to access to healthcare, heart disease and stroke, cancer, mental health, preventive health and wellness
and social determinants of health.
“We look forward to partnering with local organizations committed to driving meaningful and measurable impact,” said Michael Lawson, Houston Market President of St. Luke’s Health. “Our aim is to strengthen local service systems and enhance the quality of life of people in underserved communities within St. Luke’s Health service areas.”
The deadline for nonprofits to
apply for the grants is September 12.
Funding priorities are based on the health system’s most recent Community Health Needs Assessment, a comprehensive process conducted every three years to better understand and respond to community needs.
St. Luke’s Health awarded $1.5 million in grants to area nonprofits during its 2025 fiscal year and $1 million in grants in 2024, the
program’s inaugural year. The CommonSpirit Health Community Health Improvement Grant program provides funding for the grants. St. Luke’s Health, a part of CommonSpirit Health, consists of 16 hospitals covering communities in Greater Houston, East Texas, and the Brazos Valley.
Healthy Heart
Whispering Pines Elementary Receives Financial Grant to Provide Heart Rate Monitors in PE Class
American Heart Association Grants Ignite New Health Initiatives in Schools
By American Heart Association
The American Heart Association’s school-based programs, Kids Heart Challenge and American Heart Challenge, awarded $2,500 to Whispering Pines Elementary in Humble, TX for heart rate monitors to create an inclusive, informed, and motivating physical education experience that encourages students to take ownership of their health and well-being from an early age. The annual grant program supports schools by funding resources to extend school wellness initiatives. Heart rate monitors empower students to take ownership of their cardiovascular health by helping them exercise in
the right intensity zones using an approach shown to improve heart function and reduce risk factors for heart disease.
“This grant marks a powerful step forward in transforming physical education through technology,” said Renita Searcy, Physical Education Teacher of Whispering Pines Elementary. “By tracking and understanding the heart using heart rate monitors, we’re not just teaching fitness—we’re empowering students to take ownership of their health, build lifelong wellness habits, and connect with their bodies in meaningful ways. This is innovation in motion.”
Schools nationwide that participated in either the Kids Heart Challenge or American Heart Challenge during the 2023-2024 school year were invited to apply for grants to fund resources to enhance their health and physical education

programs. Seventy-seven schools were awarded grants, which will be used for various projects, including adding physical activity equipment, installing water filling stations, and enhancing educator training opportunities. The grant initiative provides funding twice a year, mid-school year and year end. The next grant application deadline will be near the end of next school year.
“As we move into our second century of lifesaving work, the American Heart Association remains deeply committed to youth through our in-school programs,” said Lisa Fletcher, Senior School Engagement Director of the American Heart Association. “These programs are essential because they equip young people with the knowledge and habits needed to lead heart-healthy lives. Our future is about improving yours, and by investing in the health of our youth today, we are building a healthier future for everyone.”
Both the Kids Heart Challenge and American Heart Challenge are rooted in proven science, which has shown that kids who are regularly


active have a better chance of a healthy adulthood, more than 10 million students in 20,000 schools each year, these service-learning programs give students the opportunity to feel good, while doing good.
Participating students, families and staff learn valuable skills, including how to make smart food choices, the importance of avoiding vaping/tobacco and the lifesaving skill of Hands-Only CPR. Educators

www.dewberry.com
Equiply Enters Houston to Support Smarter Capital Planning in Texas Hospitals
By Oscar Misla Founder & CEO, Equiply
Hospitals across the U.S. are facing a growing challenge: aging medical equipment and limited visibility into when — or how — it should be replaced. Planning for these assets often happens through outdated tools like spreadsheets, disconnected departmental requests, and reactive budgeting. This creates friction and leads to missed opportunities for health systems trying to operate efficiently while preparing for the future. We built Equiply to solve that.
Equiply is a platform designed specifically for hospitals to modernize the way they plan, budget, and invest in medical equipment. Today, we’re excited to announce our expansion into Houston as our home base in Texas — a state filled with health
systems that lead through innovation and operational excellence.
Texas hospitals are navigating the same capital pressures we’ve seen nationwide: balancing infrastructure needs with tightening budgets, aging assets, and a growing demand to stretch capital further. Leadership teams are being asked to do more with less — and make faster, more data-informed decisions.
Equiply gives hospitals the tools to do just that. Our platform connects asset data, lifecycle analytics, departmental input, budgeting logic, and procurement workflows into one unified capital planning system.
With Equiply, hospitals can:
• Gain full visibility into asset age, condition, and lifecycle risk with CapitalMap
• Standardize and prioritize department needs through
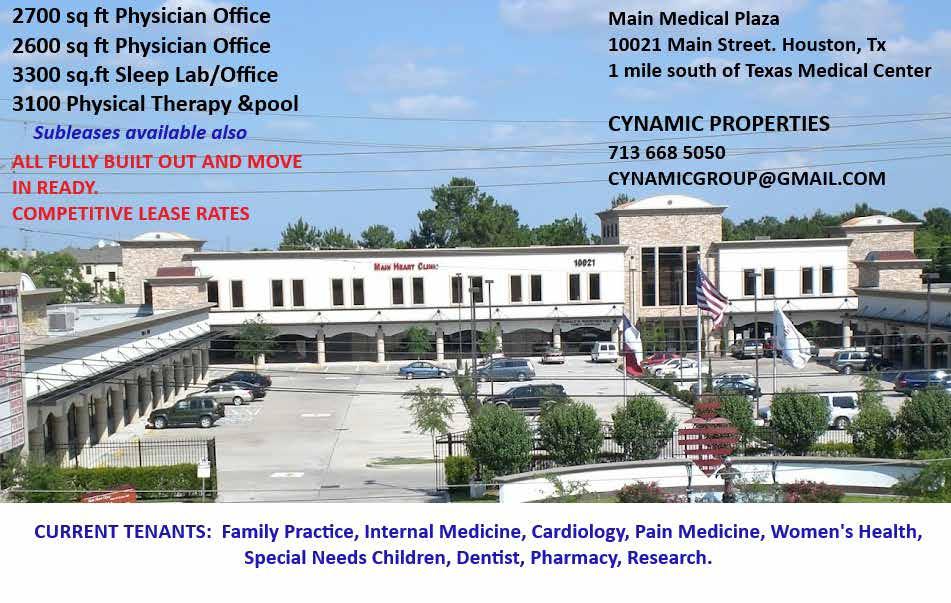
3100 WESLAYAN

WishlistIQ
• Automate procurement workflows and vendor comparisons with ProcureFlow
• Align teams across clinical, finance, and operations around a single, transparent process
The goal isn’t just to replace aging equipment — it’s to create structure around when, why, and how capital decisions get made. That structure helps hospitals reduce
Elevate Your
surprise costs, avoid emergency purchases, and plan strategically for both short-term needs and long-term growth.
We’ve already deployed Equiply with hospital partners in Puerto Rico and recently joined the Mayo Clinic Innovation Exchange, expanding our operations into Florida. Through that work, we’ve seen that hospitals of all

Practice
in Upper Kirby’s Premier Medical Office Building

A premier, four-story medical office building located in the heart of Upper Kirby, offering an array of movein ready suites with free initial test fits.

Expert Advice on Talking to Your Kids About Traumatic Events
By Betsy Kennard, Psy.D., and James Norcross, M.D.,
The tragic flooding that inundated summer camps in the Texas Hill Country over the Fourth of July weekend and claimed more than 100 lives is just the latest news story that can be frightening and confusing for children. With coverage of natural disasters, mass shootings, and other shocking events now widespread on television and social media, parents may find themselves trying to figure out the best way to talk to their kids about how they are feeling.
What to say is just as important as what not to say, according to experts at UT Southwestern Medical Center. Children are naturally curious and may have questions, or they may be worried about their own safety.
To learn how to best handle these discussions, we spoke with two faculty members in UT Southwestern’s Department of Psychiatry who have spent decades working with children.
Betsy Kennard, Psy.D., is a Professor of Psychiatry and member of the Peter O’Donnell Jr. Brain Institute. As a licensed psychologist, Dr. Kennard has more than 30 years of clinical experience with children and adolescents. She is also Director of the Suicide Prevention and Resilience Program at Children’s Health.
James Norcross, M.D., is a Professor of Psychiatry, Chief of the Division of Child and Adolescent Psychiatry, and a member of the O’Donnell Brain Institute.
Q&A with our experts
What should parents consider before talking about a sensitive topic with their child?
Dr. Norcross: The first thing to consider is the developmental level of the children so that you can provide answers and information at their level of understanding. All children, regardless of their age, should be encouraged to express their reactions to the event, and parents should feel free to talk about their emotions.

Children are typically worried about their personal safety after experiencing a traumatic event. As parents, you should provide reassurance that they are safe and that you are there to protect them from harm. How should I start a difficult conversation with my child?
Dr. Kennard: I typically start by asking children to tell me their understanding of what happened and what questions they have. This allows you to adjust your responses to their concerns and level of understanding. Additionally, assume that more questions will come after they begin
to process the event and/or experience others’ reactions to the event.
If it is an event that has been televised or shared across social media, try to limit your child’s repeated exposure to it.
What are some tips to ensure the conversation benefits my child?
Dr. Kennard: Reassure your children that they have your support and that you are there to take care of them.
As Fred Rogers of the long-running TV show “Mister Rogers’ Neighborhood” would say, “Look for the helpers; there
Healthcare & Education
From First – Generation Student to Physicianeer
By Krystel Johnson
Graduating from Texas A&M
University School of Engineering Medicine (EnMed) with both an M.D. and a master’s in engineering, Dr. Tarek Dawamne leaves behind a record of achievement and advocacy for first-generation doctors. As the first in his family to pursue higher education in the United States, he understands the challenges of navigating unfamiliar systems and the persistence required to succeed.
After realizing that students from similar backgrounds needed support, Dawamne helped launch the First-Generation Mentorship Program at EnMed. He recognized the importance of having support systems in place to help these students feel seen, understood, and empowered to succeed.
“Being a first-generation student means growing up with a unique set of
experiences and perspectives,” he said. “This viewpoint is rich in experiences that can be refined and distilled to provide unmatched strength, perseverance, and empathy in everything I do.”
Working closely with Drs. Erica Chance, Roderic Pettigrew, and Leslie Singleton, Dawamne transformed a simple conversation into a formal proposal.
The effort led to a university-wide task force focused on first-generation student support, a collaborative effort that engaged leadership from both EnMed and Texas A&M College of Medicine.
The program gained national attention, with Dawamne presenting the mentorship model at the Association of American Medical Colleges conference in San Francisco.
The session drew students and administrators from medical schools nationwide, all sharing strategies for
A Different Model for Medical Education
By Thomas J. Mohr, DO, Dean, SHSU-COM
Texas is facing a critical shortage of primary care physicians, particularly in rural and underserved areas. While the state’s 16 medical schools continue to graduate more each year, many of those graduates go on to pursue subspecialty training to practice in urban and suburban areas. These are regions that already have a high density
of providers.
It stands to reason that when the most accomplished medical school applicants are accepted into environments where cutting-edge research and subspecialty excellence are heralded, they are more likely to view professional success through that lens. Academic medical centers like those in the Texas Medical Center, one of the finest in the world, foster this environment. These institutions produce outstanding specialists and drive healthcare innovation, which are both essential to our profession. However, with 209 of the state’s 254 counties designated as Health Professions Shortage Areas (HPSA) we must also ask: how do we encourage more medical students to pursue primary care and serve in the communities that need them most?
One answer may lie in rethinking the traditional model of clinical education. Instead of concentrating clinical rotations in large academic hospitals, distributed, community-based medical education places student doctors in smaller hospitals and clinics. These are often located in the very communities facing the greatest
supporting first-generation students.
“We had a whole hall filled with students and administration personnel, all sharing what they have observed at their schools and how we, as a community in medical education, can surround this group with the resources they need,” Dawamne expressed.
Rather than public recognition, for Dawamne, the real impact lies in creating lasting support for first-generation students. During his time at EnMed, he pursued community service and research projects aimed at expanding access to medicine for underrepresented groups, all inspired by his own journey.
“Feeling the lack of sense of belonging, my aim is to help others belong, from patients to other health care professionals.”
Dawamne will begin his internal medicine residency at Mayo Clinic in Florida. There, he plans to apply
physician shortages. Students live, train, and become part of the fabric of the communities they serve. It’s a model designed not just to teach medicine, but to create connection.
When Sam Houston State University College of Osteopathic Medicine (SHSU-COM) opened its doors in 2020 with a mission to increase access to primary care for rural and underserved Texans, this model became central to its identity. From the start, the college recognized that expanding access would require more than curriculum tweaks. It would demand a cultural shift and a fundamentally different approach to where and how medical education happens.
SHSU-COM’s strategy is multi-pronged. Admissions prioritizes applicants from rural or underserved backgrounds who express an interest in primary care. It seeks to hire primary care physician faculty and administrators who can serve as role models from the start of a student doctor’s medical journey. And the osteopathic philosophy of whole-person, patient-centered care, while no longer unique to osteopathic physicians, is taught in addition to system-based education.
The most visible difference, though, begins in the third year and carries through the fourth year of medical education. SHSU-COM does

his experiences as a first-generation student to address healthcare gaps, focusing on delivering personalized care and developing practical solutions to improve patient access and treatment outcomes.
not center its clinical education around a single academic medical center. Instead, it partners with more than 4,000 community-based physicians across nearly 400 smaller hospitals and clinics throughout Texas. Student doctors move to their assigned communities for rotations, most of which are in rural and underserved areas. This is not a brief experience, but a fully immersive model of community-based medicine. Students live in these communities for at least one year, and often two, learning from primary care role models and building relationships with patients. The goal is that this type of exposure and connection will encourage graduates to practice primary care in similar communities.
Time will tell whether this model makes a lasting impact on the state’s primary care workforce, but the early results are encouraging. In its first two graduating classes, nearly 60 percent of SHSU-COM graduates went into primary care residency programs. That is a promising start.
The distributive model of clinical education may not be the norm, but it may be one of the most effective tools we have to meet the real healthcare needs of Texans and to help more future doctors find their calling in the heart of a community.
Dr. Tarek Dawamne

Home Financing Specific to Medical Professionals
At First Horizon, we understand the financial needs of medical professionals. Whether you’re still finishing your education or are a successful partner in a fastgrowing practice, our loans provide financing options to help you reach your goals.
Physicians – MD, DO, OMS, DPM
• 100% financing for loans up to 1.5M*
• No Mortgage Insurance
• Fixed and adjustable rates available
• Primary residences only
• Residents, fellowships or active physicians
DDS, DMD, Nurses, Pharmacists, Optometrists, Veterinarians:
• Up to 97%* financing available
• No Mortgage Insurance
• Loan amounts up to $806,500 for qualified buyers
• Primary residences only

NMLS 472329 Equal Housing Lender”
Craig Levin – NMLS 6066 | 678.469.9012 craig.levin@firsthorizon.com firsthorizon.com/mortgage/craig-levin
*Terms and conditions apply. *Subject to credit approval. Some restrictions apply. *For 97% LTV/CLTV, at least one borrower must be a first-time homebuyer. Borrower must have a minimum credit score of 700 to qualify.



Financial Forecast
How the One Big Beautiful Bill Could Impact Everyday Americans

TheBy Grace S. Yung, CFP Midtown Financial Group, LLC
recently passed One Big Beautiful Bill (OBBB) is one of the most comprehensive federal laws in recent memory. It touches everything from taxes and healthcare to energy and estate planning. Whether you’re working, retired, raising a family, or running a business, this bill will likely affect your finances in some way.
Here’s a plain-language summary of how the bill may impact Americans across various stages of life.
1. Lower Taxes for Most Households
The OBBB makes the individual tax cuts from the 2017 Tax Cuts and Jobs Act permanent. That means lower federal income tax rates will continue for most taxpayers.
What this means for you:
Whether you’re single, married, or supporting a family, you may continue to benefit from lower tax brackets. These changes help boost take-home pay and make it easier to save for shortand long-term goals.
2. Bigger Tax Breaks for Seniors
A new “senior deduction” allows individuals age 65 and older to take an additional $6,000 off their taxable income—or $12,000 for married couples.
Why it matters:
This change helps protect retirement income—especially Social Security— from federal taxation. Many older Americans will see their tax bills reduced or eliminated entirely.
3. Temporary Relief for Homeowners
The bill temporarily raises the cap on the state and local tax (SALT) deduction to $40,000 before gradually phasing back down.
How it helps:
This is especially beneficial for families and homeowners in high-tax states like California, New York, and New Jersey. By allowing more of these local taxes to be deducted on your federal return, your total tax burden may be lowered.
4. Changes to Medicaid and Social Programs

The OBBB reduces funding for Medicaid and certain federal assistance programs, including some clean energy incentives.
Why it matters:
Families who rely on Medicaid for healthcare—especially for children, seniors, or disabled individuals—may face more restrictive eligibility or reduced coverage. This could place more pressure on states or families to fill the gaps.
5. Impacts on Workers and Small Business Owners
The bill maintains business tax breaks and expands deductions for equipment purchases and business expenses. It also eliminates federal income tax on tips and overtime pay.
What this means:
If you work in hospitality, the service industry, or own a small business, these changes may result in more take-home pay or help you reinvest in your operations. However, the long-term impact of these tax cuts on the federal deficit remains a concern.
6. Estate Tax Changes for High-Net-Worth Families
The federal estate tax exemption has been increased to $15 million per person, or $30 million for married couples.
Why it matters:
While this change doesn’t affect most families, those with significant wealth may find it easier to pass assets to the next generation without triggering federal estate taxes. It also simplifies estate planning for many high-net-worth households.
7. Long-Term Economic Considerations
The bill is projected to add $2–3 trillion to the national debt over the next decade. While some economists argue it will stimulate growth, others caution it may lead to higher interest rates or
Legal Matters
Continued from page 3
with the correct management, this definition introduces unfortunate ambiguity to provider operations, including those of some traditional health care providers.
2. Elective IV therapy, by definition, takes place outside a physician’s office – but this term is not defined. A physician office could naturally be assumed to be the four walls of a physical office, but what if a physician practice entity has locations where no physician is
Equiply
Continued from page 9
sizes benefit from having the right infrastructure in place to plan capital proactively.
Houston stood out as the next step for us. With its world-renowned medical institutions, deep healthcare talent, and strong culture of innovation, the city is a natural fit
Expert Advice
Continued from page 10
are always helpers around.” Pointing out the positive responses in these events, such as communities uniting or people taking heroic actions, is also important. Let them know that there are no wrong feelings and that people can react differently. Be open to opportunities to talk about the event. Are there times when it’s better to avoid talking about a sensitive topic altogether?
Dr. Kennard: If your child becomes very emotional or disruptive, it is fine to pause the discussion with an invitation to revisit the conversation at a later time. Some families benefit from using an “emotional thermometer” as a way of assessing the distress level of their child. For example, ask, “On a scale of 1 to 10, with 10 being the highest level of distress, where are you on the scale right now?” If the child is very high on the scale, it might be good to discuss ways that the child can lower the distress. “What can you do to get the distress down to a 5?”
physically present? Or what about a physician practice that offers house calls to patients, rather than offering a brick and mortar location? Jenifer’s Law does not readily answer these questions.
3. The “health facility” exception also only applies to facilities licensed under a specific section of the Health and Safety Code. This exception incorporates hospitals, nursing facilities, ASCs, birthing centers, and assisted living facilities, among others. But Home and Community Support Services Agencies, the key licensure for home health agencies, are licensed under Title 2 of the Health and
Safety Code, and would not be expressly excluded from this definition. This means HCSSAs are not automatically exempt from the definition of elective IV therapy, and will need to consider whether their current IV protocols and procedures align with Jenifer’s Law.
What Now?
In advance of the September 1, 2025 effective date, Texas providers should carefully consider the following key issues:
1. Do we furnish elective IV therapy, or are we exempt?
2. If we are not exempt – do our current prescribing and administration
protocols align with the new requirements in Jenifer’s Law?
Overall, this new bill simultaneously expands and restricts aspects of elective IV treatment. On the one hand, it grants greater flexibility to both patients and providers in selecting and offering elective IV therapy. On the other hand, it limits physicians’ delegation authority by restricting administration to specific credentialed professionals. Providers offering elective IV therapy should remain vigilant, as future regulatory clarification or enforcement, particularly by the Texas Medical Board, could further narrow the scope of physician delegation or expand the reach of HB 3749.
for what we’re building. We’re not just opening a market—we’re establishing a presence, meeting directly with hospital leaders, and building long-term partnerships across the region.
We believe capital planning deserves the same level of sophistication as clinical or financial operations. At its core, Equiply turns capital planning from a once-a-year scramble into a continuous, collaborative process—rooted in real data and cross-functional alignment.
We’re excited to work with Texas hospitals ready to bring more clarity, structure, and confidence to the way they manage infrastructure. If your hospital is exploring how to better plan for upcoming equipment needs—or facing a backlog of aging assets without a roadmap—we’d love to connect.
Houston is a city known for leading in healthcare. We’re here to help make sure its hospitals continue to lead—with the tools and insights they need to plan smarter, invest wisely, and deliver excellent care. Oscar Misla Founder & CEO, Equiply contact@equiply.io equiply.io
Paid Advertisement
What are some ways that I can show my child that I am listening?
Dr. Norcross: I recommend using both verbal and nonverbal behavior to demonstrate you are listening. Maintain eye contact while the child is talking, and remain free from distractions such as cellphones or social media. Respond first by repeating what you heard the child say and maybe ask, “Did I get that right?” before responding. How should I respond to my child’s concerns?
Dr. Norcross: Let them know that it is normal to have negative emotions such as fear and anger. In addition, talk with them about ways that you manage these emotions and identify positive ways to cope, such as getting exercise, doing something active and fun, or getting together with friends. Any advice for what not to do when having these kinds of conversations?
Dr. Kennard: Parents should make a safe space to discuss their children’s reactions to the event. It can be hard to hear your children express their distress. Avoid the “pull” to tell them how to feel or to dismiss their feelings. Use active listening,
which is saying back to them what you heard them say and allowing space for them to correct your understanding. Demonstrate confidence in your ability to keep them safe, and model that it is OK to talk about emotions and about how to cope with difficult emotions. If I think my child might be anxious or scared, what signs or changes in behavior should I watch for?
Dr. Norcross: Changes in behavior such as regression to an earlier stage of development, changes in eating or sleeping patterns, somatic complaints such as stomachaches or headaches, or disruptive behaviors may be observed. In addition, some youth may not want to go to school, have poor school performance, have trouble concentrating, or have no interest in activities that were once pleasurable. What strategies for coping or reassurance would you recommend I give my child?
Dr. Kennard: Engaging in relaxation, participating in pleasant activities, and using problem-solving strategies can be important means of coping. Resist telling your children how to cope and instead allow them to come
up with some strategies that they can use to lower their level of distress. Try to maintain a normal routine and resist the temptation to allow your child to avoid fearful situations, which likely will compound the problem. How do I know when my child might need outside help?
Dr. Norcross: Persistent changes in mood or behavior may be a sign that additional help is needed. Talking with your pediatrician to screen for depressive or anxiety symptoms and the potential need for treatment can be helpful. Treatment with a mental health professional may be warranted if symptoms persist and result in impairment in school or outside activities, family conflict, or interpersonal problems.
AI
Continued from page 1
mild to moderate cases. In fact, Woebot has published peer-reviewed research showing reduced depressive symptoms in young adults after just two weeks of chatting.
These apps are designed to simulate therapeutic interaction, offering empathy, asking guided questions and walking you through evidence-based tools. The goal is to help with decision-making and self-control, and to help calm the nervous system.
The neuroscience behind cognitive behavioral therapy is solid: It’s about activating the brain’s executive control centers, helping us shift our attention, challenge automatic thoughts and regulate our emotions.
The question is whether a chatbot can reliably replicate that, and whether our brains actually believe it. A user’s experience, and what it might mean for the brain
“I had a rough week,” a friend told me recently. I asked her to try out a mental health chatbot for a few days. She told me the bot replied with an encouraging emoji and a prompt generated by its algorithm to try a calming strategy tailored to her mood. Then, to her surprise, it helped her sleep better by week’s end.
As a neuroscientist, I couldn’t help but ask: Which neurons in her brain were kicking in to help her feel calm?
This isn’t a one-off story. A growing number of user surveys and clinical trials suggest that cognitive behavioral therapy-based chatbot interactions can lead to short-term
Healthy Heart
Continued from page 8
improvements in mood, focus and even sleep. In randomized studies, users of mental health apps have reported reduced symptoms of depression and anxiety—outcomes that closely align with how in-person cognitive behavioral therapy influences the brain.
Several studies show that therapy chatbots can actually help people feel better. In one clinical trial, a chatbot called “Therabot” helped reduce depression and anxiety symptoms by nearly half—similar to what people experience with human therapists. Other research, including a review of over 80 studies, found that AI chatbots are especially helpful for improving mood, reducing stress and even helping people sleep better. In one study, a chatbot outperformed a self-help book in boosting mental health after just two weeks.
While people often report feeling better after using these chatbots, scientists haven’t yet confirmed exactly what’s happening in the brain during those interactions. In other words, we know they work for many people, but we’re still learning how and why. Red flags and risks
Apps like Wysa have earned FDA Breakthrough Device designation, a status that fast-tracks promising technologies for serious conditions, suggesting they may offer real clinical benefit. Woebot, similarly, runs randomized clinical trials showing improved depression and anxiety symptoms in new moms and college students.
While many mental health apps boast labels like “clinically validated” or “FDA approved,” those claims are often unverified. A review of top apps
found that most made bold claims, but fewer than 22% cited actual scientific studies to back them up.
In addition, chatbots collect sensitive information about your mood metrics, triggers and personal stories. What if that data winds up in third-party hands such as advertisers, employers or hackers, a scenario that has occurred with genetic data? In a 2023 breach, nearly 7 million users of the DNA testing company 23andMe had their DNA and personal details exposed after hackers used previously leaked passwords to break into their accounts. Regulators later fined the company more than $2 million for failing to protect user data.
Unlike clinicians, bots aren’t bound by counseling ethics or privacy laws regarding medical information. You might be getting a form of cognitive behavioral therapy, but you’re also feeding a database.
And sure, bots can guide you through breathing exercises or prompt cognitive reappraisal, but when faced with emotional complexity or crisis, they’re often out of their depth. Human therapists tap into nuance, past trauma, empathy and live feedback loops. Can an algorithm say “I hear you” with genuine understanding? Neuroscience suggests that supportive human connection activates social brain networks that AI can’t reach.
So while in mild to moderate cases bot-delivered cognitive behavioral therapy may offer short-term symptom relief, it’s important to be aware of their limitations. For the time being, pairing bots with human care—rather than replacing it—is the safest move. are also supported with lesson plans and resources to support their physical and mental well-being.
In addition to learning about heart health, participating students
Financial Forecast
Continued from page 12
inflation in the long run. What you can do:
It’s wise to build flexibility into
and families have the opportunity to give back to the community by raising funds for the American Heart Association. Dollars raised help advance cardiovascular research and outreach programs, paving the way for improved health outcomes for healthier communities.
your budget and savings plans. Keep an eye on inflation, interest rates, and future tax policy debates.
Final Thoughts
The One Big Beautiful Bill offers opportunities and challenges. While many Americans will benefit from lower taxes and expanded deductions,
Schools interested in the grant opportunity are encouraged to register now to participate in either Kids Heart Challenge or American Heart Challenge for the 2024-2025 school year. To learn more visit heart.org/ getstarted.

rising federal debt, healthcare funding changes, and shifting market dynamics may create longer-term risks. A thoughtful financial plan – and a periodic review – can help you make the most of the current environment..
Houston Medical Times is Published by Texas Healthcare Media Group, Inc. All content in this publication is copyrighted by Texas Healthcare Media Group, and should not be reproduced in part or at whole without written consent from the Editor. Houston Medical Times reserves the right to edit all submissions and assumes no responsibility for solicited or unsolicited manuscripts. All submissions sent to Houston Medical Times are considered property and are to distribute for publication and copyright purposes. Houston Medical Times is published every month
P.O. Box 57430 Webster, TX 77598-7430