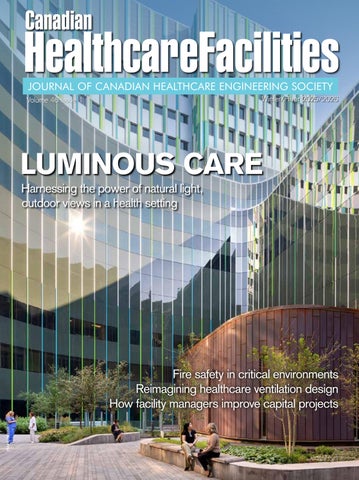
HealthcareFacilities Canadian LUMINOUS CARE
Harnessing the power of natural light, outdoor views in a health setting

Fire safety in critical environments
Reimagining healthcare ventilation design
How facility managers improve capital projects
2-Hour Fire-Resistive Cable System for Circuit Integrity







Ceramifiable silicone technology
RC90 Classified to ULC-S139 and FHIT7
Applications: Emergency Feeder Cables, Fire Pumps, Exit Lighting, Stairwell Pressurization, Ventilating Fans, Elevators / OEO
Scan to learn more about Lifeline® Fire-Resistive Cable Systems from

EDITOR/RÉDACTRICE Clare Tattersall claret@mediaedge.ca
PUBLISHER/ Jake Blanchard ÉDITEUR DU GROUPE jakeb@mediaedge.ca
PRESIDENT/PRÉSIDENT Kevin Brown kevinb@mediaedge.ca
SENIOR DESIGNER/ Annette Carlucci CONCEPTEUR annettec@mediaedge.ca GRAPHIQUE SENIOR
GRAPHIC DESIGNER/ Thuy Huynh-Guinane GRAPHISTE roxyh@mediaedge.ca
PRODUCTION Ines Louis MANAGER/ inesl@mediaedge.ca RESPONSABLE DE PRODUCTION
CIRCULATION MANAGER/ Adrian Holland DIRECTEUR DE LA circulation@mediaedge.ca DIFFUSION
CANADIAN HEALTHCARE FACILITIES IS PUBLISHED BY UNDER THE PATRONAGE OF THE CANADIAN HEALTHCARE ENGINEERING SOCIETY.
SCISS JOURNAL TRIMESTRIEL PUBLIE PAR SOUS LE PATRONAGE DE LA SOCIETE CANADIENNE D'INGENIERIE DES SERVICES DE SANTE.
CHES SCISS
PRESIDENT Kate Butler
VICE-PRESIDENT Vacant
PAST PRESIDENT Craig B. Doerksen
TREASURER Reynold J. Peters
SECRETARY Paul Perschon
EXECUTIVE DIRECTOR Penny Waddington
CHAPTER CHAIRS
Newfoundland & Labrador: Colin Marsh
Maritime: Steve Smith
Ontario: Beth Hall
Quebec: Mohamed Merheb
Manitoba: Stephen R. Cumpsty
Saskatchewan: Kendall Rathgeber
Alberta: Dave Attwood British Columbia: Mitch Weimer
FOUNDING
Rethink
Displacement ventilation as a keystone of future healthcare design
24 Transforming Mental Health Services
Collective effort delivers modern approach to mental health and addictions-based care
Reproduction or adoption of articles appearing in Canadian Healthcare Facilities is authorized subject to acknowledgement of the source. Opinions expressed in articles are those of the authors and are not necessarily those of the Canadian Healthcare Engineering Society. For information or permission to quote, reprint or translate articles contained in this publication, please write or contact the editor.
Canadian Healthcare Facilities Magazine Rate
Extra Copies (members only)
Canadian Healthcare Facilities (non members)
Canadian Healthcare Facilities (non members)
$25 per issue
$30 per issue
$80 for 4 issues
A subscription to Canadian Healthcare Facilities is included in yearly CHES membership fees.
H.
G.S.
J.
S.T.
4 Cataraqui St., Suite 310, Kingston, Ont. K7K 1Z7 Telephone: (613) 531-2661 Fax: (866)
La reproduction ou l’adaptation d’articles parus dans le Journal trimestriel de la Société canadienne d’ingénierie des services de santé est autorisée à la condition que la source soit indiquée. Les opinions exprimées dans les articles sont celles des auteurs, qui ne sont pas nécessairement celles de la Société canadienne d’ingénierie des services de santé. Pour information ou permission de citer, réimprimer ou traduire des articles contenus dans la présente publication, veuillez vous adresser à la rédactrice.
Prix d’achat du Journal trimestriel
Exemplaires additionnels (membres seulement)
Journal trimestriel (non-membres)
Journal trimestriel (non-membres)
$25 par numéro
$30 par numéro
$80 pour quatre numéros
L’abonnement au Journal trimestriel est inclus dans la cotisation annuelle de la SCISS.
NOT JUST ANOTHER FACILITY

THROUGHOUT ANY GIVEN YEAR, a multitude of healthcare facilities break ground or are completed. Then there are those that are recognized with awards. The Paul Myers Tower at Lions Gate Hospital in North Vancouver is just one project honoured in 2025. Part of the hospital’s phased redevelopment, the sixstorey tower garnered PCL Constructors Westcoast a gold award in the general contractor category, presented by the Vancouver Regional Construction Association. You can read about the project that brought modern clinical spaces and improved patient experience to one of the region’s busiest hospitals in Complex Achievement
Another noteworthy development covered in the ensuing pages is the recently finished Mental Health and Addictions Centre in St. John’s, Nfld. Opened in April of last year, the modern 240,000-square-foot, 102-bed facility is packed with recreation and fitness opportunities, art and music therapy and more, marking a monumental step forward to improving mental health care in Newfoundland and Labrador.
This issue’s key focus, healthcare development, addresses a myriad of topics beyond specific projects themselves. They include: why facility managers should be involved from a capital project’s get-go; the integration of light and nature into hospital public spaces; and displacement ventilation as a viable strategy in hospital environments.
A secondary theme this issue is emergency preparedness and response. Resilient Ready explores key challenges facing Canada’s healthcare system, with suggested actionable solutions to improve resiliency, while A Critical Priority delves into fire suppression systems.
Looking ahead to the spring 2026 issue, we are currently accepting editorial submissions that align with the topics of innovation and technology, infection prevention and control, and health and safety. I invite readers keen to write an article to submit a synopsis outlining what you might cover, for consideration.
Clare Tattersall claret@mediaedge.ca
BETTER TOGETHER


I CONTINUE TO BE INSPIRED by the strength and sense of community across CHES. December brought a personal highlight: our second annual Women in CHES year-end webinar. More than 100 women from across the country joined to listen and learn from two incredible presenters, and to share their own stories — both their journeys into healthcare and engineering, and the projects they are proud to lead. It was a powerful reminder of the talent and dedication that so many bring to our profession.
Hearing these stories made me reflect on how the work we do in healthcare facilities continues to evolve, especially as new technologies reshape the way we work. Whether digital tools, data insights or the early influence of artificial intelligence, the pace of change is real. It can feel exciting and, at times, a little daunting. But what reassures me is how willing CHES members are to learn, adapt and stay curious.
This commitment to learning shows up in so many ways. Our 2025 webinar series saw strong participation and exceptional speakers. In 2026, we remain committed to offering webinars designed to support your growth. The Canadian Healthcare Construction Course continues to be well-attended, and our medical gas training remains an important way to strengthen the technical side of the work we all do. Professional development, formal or informal, is one of the most powerful ways we prepare ourselves for whatever comes next.
Stepping into the role of CHES National president has been both humbling and a privilege. I am incredibly grateful for the support, patience and encouragement I’ve received from the board, chapter leaders and so many members. As we look forward, I feel hopeful about what we can continue to accomplish together. Healthcare will always face pressures but CHES members consistently show collaboration, steadiness and genuine support for one another.
Kate Butler CHES National president
CALL FOR YOUNG PROFESSIONALS GRANT NOMINATIONS & SPONSORSHIP SUBMISSIONS
CALL FOR SPONSORS
DEADLINE: April 30, 2026
• Who can sponsor? Organizations or companies.
• Apply online: www.ches.org/ches-young-professional-grant-sponsorship-application-form
• Cost: $2,500+tax
CALL FOR CANDIDATES
Eligibility criteria:
• Work full-time within a healthcare organization or a company supplying technical services to healthcare facilities or organizations.
• Be or will become an architect, engineer (ie. mechanical, electrical, power, civil, etc.), technician or work in a similar technical discipline.
• Have worked in the healthcare field for less than five (5) years, or have been a professional architect, engineer, technician or worked in similar technical discipline for not more than ten (10) years.
Application requirements:
• Complete the YPG Candidate Application Form on the CHES website: www.ches.org/young-professional-grantypg-application-form
• Submission must include a letter of endorsement of the nominee from the local CHES chapter.
What’s in it for the recipient?
• Level up your knowledge and plenty of networking. Complimentary registration for the CHES National Conference and reimbursement for travel costs (local transport, flights, accommodations and meals) for the successful candidate(s), up to a maximum of $2,500, with amounts above this value being the responsibility of the successful candidate(s). Reimbursement shall be in accordance with CHES policy B5.1.
• Recognition! The successful candidate(s) will agree to participate in the making of a short video interview at the CHES National Conference to share their experience while attending. An announcement will be made at the CHES National Conference recognizing the YPG recipient.
• Complimentary CHES membership for the successful candidate for one (1) year following the conference.
Full details about the YPG can be found on the CHES website at www.ches.org under the National page.
If you have any questions, e-mail us at info@ches.org.
NEWFOUNDLAND & LABRADOR CHAPTER
The shift from four health authorities to one provincial authority is starting to settle. Even though there have been bumps in the journey, we’re heading in the right direction.
Moving our local conference to fall is bearing fruit for our chapter. The 2025 conference was held in early November, at the Health Innovation Acceleration Centre in the eastern-urban zone. It was the largest in the chapter’s history — record-high attendance, the most vendor booths to date and strong participation from all health zones across the province.
For the first time ever, we held a separate CHES event on the day after the conference. It included a full-day of training and interactive activities, with more than 25 people in attendance and vendor representation.
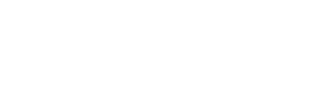
The chapter is in a strong financial position. In preparation for the 2026 CHES National Conference in St. John’s, we have allocated funds to support event planning. Members have been appointed to various planning committees to ensure a successful event. The venue has been confirmed — St. John’s Convention Centre — accommodations secured at the Delta hotel, and golf course reserved. Planning is underway for entertainment and the companion program.
—Colin Marsh, Newfoundland & Labrador chapter chair
MARITIME CHAPTER
The Maritime chapter held its 2025 fall education day Nov. 25, at the Glengarry Best Western in Truro, N.S. Planning is now underway for our 2026 spring conference in Moncton, May 3-5.
A big welcome to Glen Hughes, engineering manager at the Institute of Biomedical Engineering, University of New Brunswick, who has stepped up as vice-chair of New Brunswick, freeing up Kate Butler to focus on her role as CHES National president. Glen has also agreed to participate on the CHES National partnership and advisory committee.
I’d also like to welcome Janet Gomes, manager of redevelopment at IWK Health, who will represent the Maritime chapter on the Canadian Healthcare Construction Course (CanHCC) subcommittee. She is participating in planning the upcoming CanHCC session, rescheduled to take place Feb. 25-26, in Halifax. Janet will also be involved with the Women in CHES initiative.
The Maritime chapter is currently seeking members and executive representation from Prince Edward Island.
CHES Maritime continues to offer several financial incentives to members: Per Paasche bursary; contribution to Canadian Certified Healthcare Facility Manager exam fees, and spring and fall education days; various prize draws for participating members at conferences and education days; support for the Young Professionals Grant; and other membership benefits.
As well, the Maritime chapter has recently created an award to recognize outstanding achievement and performance in healthcare facilities management by a regular member.
ONTARIO CHAPTER
The chapter executive has hit the ground running, actively engaging in various initiatives to propel CHES Ontario forward.
Transitioning the treasurer role after many years has presented some challenges. However, thanks to Rudy Dahdal�s diligence and the support of our accounting and legal teams, we have successfully aligned all aspects of the corporation. Budget planning is currently underway and with past chair John Marshman’s assistance, we organized an in-person meeting in early December, to strategically review the Ontario chapter and plan for our future.
I am pleased to announce Sylvia Rodas as our education committee liaison. She is already exploring educational opportunities for members, while also supporting the Canadian Healthcare Construction Course and our student awards and bursary programs across nine colleges in Ontario.
Under Jeff Weir's leadership, we are prioritizing membership recruitment through a phone campaign targeting all provincial healthcare facilities. We are also committed to expanding our chapter into the long-term care sector and will have a booth at the AdvantAge conference this spring.
Larry Erwin remains committed to the CHES website as chair of communications, and ensuring social media feeds effectively promote CHES, both nationally and provincially. Alex Sullo continues to build partnerships with the Medical Device Reprocessing Association of Ontario and Infection Prevention and Control Canada, while secretary Dan Neaves brings a fresh new perspective and keeps us informed and focused on our goals.
The chapter executive has been diligently updating job descriptions and conducting a comprehensive review of our bylaws, with support from the law program at Queen’s University, thanks to Chris MacKay. We will be proposing bylaw changes to the membership, including the introduction of a member-at-large position to enhance succession planning.
Ron Durocher and his committee have initiated planning for the chapter’s 2026 spring conference in London, May 24-26. The event is shaping up to be highly successful, with strong interest in booths and sponsorships. Reach out to Ron directly if you wish to sponsor this forward-thinking conference.
Looking ahead, we are already planning for the 2029 CHES National Conference — the first-ever co-hosted event, with both Ontario and Quebec collaborating in Ottawa.
—Beth Hall, Ontario chapter chair

QUEBEC CHAPTER
As we transition from one year to the next, it is an important time to reflect on our current environment and prepare for what’s ahead. 2025 marked the first full year under the new Santé Québec governance structure. This transformation represents a major shift for the province, with many services under review or being restructured. More than ever, there is a strong need for leadership, technical expertise and support for healthcare facility teams that must adapt to increasing demand and operational pressures.
The Quebec chapter is now focusing on planning our spring 2026 education day. Details, including the theme, program and speakers, will be shared soon.
Unfortunately, the chapter had to cancel the Canadian Healthcare Construction Course that was to be held this past December, due to insufficient registration. While this outcome is understandable, given provincial changes and the fact that the course is only offered in English, we are actively working with the Quebec Construction Association to identify solutions and explore optimized offerings for 2026. Our objective remains to provide high-quality, accessible training that serves the needs of healthcare engineering professionals across the province.
CHES Quebec will launch a chapter-wide election process in early 2026, to fill several vacant positions on the executive committee. We strongly encourage members who wish to contribute to the evolution of the healthcare facilities sector in Quebec to submit their candidacy and get involved. Election results will be announced during our spring education day. Stay connected on our social media platforms for calls for participation, updates and announcements.
—Mohamed Merheb, Quebec chapter chair
BRITISH COLUMBIA CHAPTER
The B.C. chapter has issued its first call for elections for the new executive to take office at our annual general meeting in June.
The chapter executive has appointed three members to take on new roles as committee chairs. Julie Makranyi will cochair education with current chair Caroline Thomson, Darren Emes will replace Arthur Buse as membership chair, and Daryl Hoover has taken on communications.
CHES B.C.’s 2026 spring conference is scheduled for May 31June 2, in Whistler. Planning is well underway.
The majority of B.C. chapter committee members have reported they have attended all meetings and are actively participating in committee work.
CHES B.C. has successfully incorporated. We are currently working through the insurance and tax reporting process. By necessity through incorporation, our bylaws were updated to reflect provincial requirements. These bylaws will be provided to CHES National for updating on the website.
The B.C. chapter has secured the domain name chesbc.ca and is working on a conference webpage similar to that of the Ontario chapter.
CHAPITRE DU QUEBEC
Alors que nous passons d’une année à l’autre, il est important de prendre un moment pour réfléchir à notre environnement actuel et nous préparer pour l’année à venir. Cette année a marqué la première année complète sous la nouvelle structure de gouvernance de Santé Québec. Cette transformation représente un changement majeur pour la province, avec de nombreux services actuellement réévalués ou restructurés. Plus que jamais, il est essentiel d’offrir du leadership, de l’expertise technique et du soutien aux équipes responsables des installations de soins de santé, qui doivent s’adapter à une demande croissante et à des pressions opérationnelles importantes.
Notre équipe se concentre maintenant sur la planification de notre prochaine journée de formation, prévue pour le printemps 2026. Les details, incluant le thème, le programme et les conférenciers, seront communiqués au début de la nouvelle année.
Malheureusement, nous avons dû annuler la séance de décembre 2025 du cours Canadian Healthcare Construction Course en raison d’un nombre insuffisant d’inscriptions. Bien que ce résultat soit compréhensible compte tenu des changements provinciaux et du fait que le cours est offert en anglais, nous travaillons activement avec l’Association de la construction du Québec afin d’identifier des solutions et d’explorer des options optimisées pour 2026. Notre objectif demeure d’offrir une formation de haute qualité et accessible, qui répond aux besoins des professionnels en génie des installations de santé à travers le Québec.
Le chapitre Québec lancera un processus d'élection au début de 2026 afin de pourvoir plusieurs postes vacants au sein du comité exécutif. Les résultats seront annoncés lors de notre Journée de formation. Nous encourageons fortement les membres qui souhaitent contribuer à l’évolution du secteur des installations de santé au Québec à soumettre leur candidature et à s’impliquer. Restez connectés avec nous sur nos plateformes de médias sociaux pour suivre nos mises à jour, nos annonces et nos appels à participation.
—Mohamed
Merheb, chef du conseil d ’administration du Québec
SASKATCHEWAN CHAPTER
The Saskatchewan chapter had a successful 2025 conference. Held in October, in Saskatoon, we heard from many wonderful presenters and enjoyed another fun casino night. After the conference, three new board members were added to the executive team, which is now comprised of myself (chair), Steven Kemp (secretary/treasurer), Ted Cooke (director), Quang Pham (director), Mitch Empey (director), Peter Whiteman (director), Cameron Bantle (director), Connie Hogan (director) and Jim Allen (past chair). We are committed to continuing our efforts to look for new strategies to expand the chapter’s membership. Planning for the 2026 conference has begun. It will be held in Regina. We are currently looking at venues and will conduct walkthroughs before securing a location. Dates and further information will be relayed once there’s more to share.
—Kendall Rathgeber, Saskatchewan chapter chair
ALBERTA CHAPTER MANITOBA CHAPTER
The Alberta chapter has been enjoying the glow of the 2025 CHES National Conference that was successfully held in September. During the conference, the chapter formally made a motion to accept the results of the election that was held online last spring. Executive positions are now represented by myself (chair), Paul Perschon (vice-chair), Sarah Ahmed (treasurer), Sabrina McCormack (secretary) and James Prince (past chair).
On behalf of CHES Alberta, I would like to thank James for his leadership over the past two years and steering the chapter through some very tough roads leading up to the national conference. The executive is in a better place now, thanks to his guidance.
The executive committee held its first meeting and will be forming some exciting new subcommittees. We have several great volunteers that have put their names forth. An expression of interest will be sent out to our membership to seek committee chairs and members. We look forward to harnessing the energy of the new groups.
—Dave Attwood, Alberta chapter chair
The Manitoba chapter sponsored an award at Red River College Polytechnic’s construction trades awards for power engineering students. The recipient was Haki Osmani. Presented June 4, 2025, the awards ceremony was attended by myself and vice-chair Kevin Schmon.
CHES Manitoba’s 2026 spring education day has been scheduled for May 14, at the Victoria Inn in Winnipeg. Preparations for the event will start in the coming weeks. At this time, there is no planned theme or topics for presentations.
The chapter once again partnered with the Building Owners and Managers Association of Manitoba for its 2025 building conference in Winnipeg. We provided a presentation at the event, Oct. 21. The presentation and keynote speaker luncheon were provided to chapter members at no charge.
The Winnipeg Construction Association hosted the Canadian Healthcare Construction Course Nov. 4-5.
The Manitoba chapter has seen growth over the past year, with 27 new members for a total of 141.
—Stephen R. Cumpsty, Manitoba chapter chair
CALL FOR AWARD NOMINATIONS
Nomination Deadline: April 30, 2026
Nominations are now open for both the Wayne McLellan and Hans Burgers awards. This is your opportunity to recognize outstanding teams or individuals who have made significant contributions in the healthcare facility industry.
Wayne McLellan Award
Recognizes demonstrated leadership excellence by CHES members in a Canadian healthcare facility. The award may be granted annually to a healthcare organization that is judged to have the highest met criteria established for the award.
How to Nominate: Submit your nomination by completing the online form at www.ches.org/award/wayne-mclellan-award-ofexcellence-in-healthcare-facilities-management/

Why Nominate?
• Recognizing excellence inspires others and strengthens our community.
• Help us celebrate those who go above and beyond. Let's honour the best among us!
Hans Burgers Award
Recognizes an outstanding contribution to healthcare engineering by a CHES member. The award may be granted annually to a CHES member who is judged to have the highest met criteria established for the award.
How to Nominate: Submit your nomination by completing the online form at www.ches.org/award/hans-burgers-award-foroutstanding-contribution-to-healthcare-engineering

Award sponsored byrgrfgrfgrfgrggedge
Award sponsored byededdrgrfgrfgrfgrggedge
Full awards details can be found on the CHES website at www.ches.org under the National page.
CHES is a constituent society of the Engineering Institute of Canada and a Quality Learning Provider You may claim one (1) Professional Development hour for the webinar TIME: 1200 Eastern Register online: https://ches.org/2026-webinars/
Wednesday January 28, 2026
Improving the Sustainability of Healthcare Humidification Systems
Speakers: Nicholas Lea, B.Eng., LEED, Condair Ltd.
Nuno Silva, PhD, Condair Ltd.
Wednesday February 18, 2026
Preventive Maintenance versus Predictive Maintenance: Pros and Cons
Speaker: Daniel Golub, Head of Go-To-Market and Co-Founder of Click Maint
Wednesday March 18, 2026
IPAC in Construction for Long-term Care: Maneuvering the Complex Environment of LTC
Speaker: Youhanna Salib, CIC, BSc, MSc (Candid.), IPAC Consulting
Wednesday April 22, 2026
Energy and Sustainability
Speakers: William Gagnon, B.Eng., Building Engineering, MSc. Bioresource Engineering, Canadian Coalition for Green Health Care
Kristin Anstey, Canadian Coalition for Green Health Care
Wednesday May 20, 2026
Building Envelope: Maintenance and Upkeep Best Practices
Speakers: Andrew Epp, B.ASc (Honours), P.Eng. (Ontario, Alberta), PMPSpecialist, Management Consultant, TW, Pinchin Ltd.
Alexandru Olaru, DIPLENGT, Applied Science Technician (A.SC.T), Registered Roofing Observer (RRO), Pinchin Ltd.
Wednesday June 17, 2026
The Resilient Hospital: Future-proofing Critical Healthcare Systems
Speaker: Jamie Bardsley, Bachelor of Applied Science, Mechanical Engineering, Trane
Wednesday October 21, 2026
Time for an Air Change: Advancing Demand-controlled Displacement Ventilation
Speakers: Greg Allen, P.Eng., LEED AP, Rivercourt Engineering
Alex Hutton, P.Eng., CEM, LEED AP, Swordfern Strategic Sustainability
Tariq Amlani, P.Eng., LEED AP, Stantec
Wednesday November 18, 2026
Reusables in Healthcare: Cutting Waste, Costs and Carbon Footprints
Speaker: Emily Chin, BSc, Reeve Consulting
SERIES SPONSOR


COMPLEX ACHIEVEMENT
Une réalisation complexe
By/Par Cheryl Mah
BBuilding healthcare facilities is a highly complex undertaking. When the new facility is required to integrate seamlessly with existing infrastructure, that complexity is taken to a whole new level.
That was the task given to PCL Constructors Westcoast, general contractor for the Paul Myers Tower at Lions Gate Hospital in North Vancouver. The six-storey acute care facility was built between three existing facilities: the south tower and northern expansion building on one side, Hope Centre on the opposite side and Evergreen House to the north.
A major challenge was the physical constraints of the project site, according to construction manager Travis Prystai.
“The new building connects directly on the west to the existing hospital, and is in close proximity to existing buildings on the north
LLa construction d’établissements de santé est un défi complexe qui devient encore plus exigeant lorsque le nouvel établissement doit s’intégrer harmonieusement aux infrastructures existantes.
C’est exactement ce défi qui a été confié à PCL Constructors Westcoast, entrepreneur général de la tour Paul Myers à l’hôpital Lions Gate de North Vancouver. Celui-ci a réussi à implanter un établissement de soins intensifs de six étages au milieu de trois installations: d’un côté, la tour sud et le bâtiment d’extension nord, le Hope Centre sur le côté opposé, et l’Evergreen House au nord du site.
Selon Travis Prystai, responsable des travaux, la principale difficulté tenait aux contraintes physiques du site.
Il précise que “le nouveau bâtiment est directement relié à l’hôpital à l’ouest et jouxte, au nord et à l’est, des bâtiments existants,
and east, leaving only the south for the majority of the construction logistics,” he says. “These site constraints demanded careful planning, continuous communication with stakeholders and diligent execution by the construction team.”
For its exceptional work on the 258,000-square-foot acute healthcare facility, PCL was recognized with a 2025 Gold Award of Excellence in the top general contractor category, presented by the Vancouver Regional Construction Association.
“It’s a very nice recognition for our project team and stakeholders for all the effort put in,” says Prystai. “Building a hospital is a very challenging endeavour and while it’s rewarding to create a healthcare space and see it serve patients and the community, to be further recognized with this award is special validation for all those involved in building this beautiful facility.”
The tower is named after Paul Myers, former owner of Keith Plumbing and Heating Co., who donated $25 million to the Lions Gate Hospital Foundation. The new facility features 108 singleoccupancy patient rooms with ensuites, eight state-of-the art universal operating rooms, 39 patient pre- and post-operative bays, a medical device reprocessing department and outpatient clinic services.
PCL broke ground on the centre in 2021, with substantial completion achieved in December 2024. Challenges included significant change orders, scope additions, working on an active hospital site and integrating to existing infrastructure through 10 internal connections.
For the integration of the new tower and existing campus, several project elements also included work in the existing buildings.
A phasing plan, including building demolition, replacement of the oxygen tank farm, rerouting egress patterns and temporary facility


t
de sorte que seule la façade sud reste disponible pour l’essentiel des opérations logistiques du chantier. Ces contraintes sur le site ont nécessité une planification soignée, une communication constante avec les parties prenantes et une mise en œuvre rigoureuse de la part de l’équipe de construction.”
Pour la qualité remarquable de son intervention sur un centre hospitalier de soins intensifs de grande envergure, PCL a décroché en 2025 un Prix d’excellence or dans la catégorie des entrepreneurs généraux, décerné par la Vancouver Regional Construction Association.
Selon Prystai, “Cette distinction salue l’apport inestimable de notre équipe de projet et de l’ensemble des partenaires. Construire un hôpital représente un défi majeur. La création d’un espace de soins au service des patients et de la collectivité est en soi extrêmement gratifiante, mais cette reconnaissance constitue une récompense supplémentaire pour tous ceux qui ont participé à ce projet salutaire.”
La tour a vu le jour grâce à un don de 25 millions de dollars versé à la Lions Gate Hospital Foundation. Elle est baptisée en hommage à Paul Myers, ancien propriétaire de Keith Plumbing and Heating Co. Le nouvel établissement hospitalier est équipé de 108 chambres individuelles pour patients avec salles de bain, huit blocs opératoires universels de pointe, 39 unités de prise en charge pré- et postopératoire, un service de retraitement des dispositifs médicaux ainsi que des services cliniques ambulatoires.
Les travaux, entamés en 2021, se sont achevés en décembre 2024. Le projet a été confronté à de nombreuses contraintes: modifications importantes en cours de chantier, extensions de périmètre, interventions sur un site hospitalier pleinement opérationnel et intégration aux infrastructures existantes par dix liaisons internes.
YOUR TRUSTED PARTNER FOR TEMPORARY CONTROL FOR 30 YEARS.



“THESE
SITE CONSTRAINTS
DEMANDED CAREFUL PLANNING, CONTINUOUS COMMUNICATION WITH STAKEHOLDERS AND DILIGENT EXECUTION BY THE CONSTRUCTION TEAM.”
entrances, ensured ongoing operations during construction.
Opened to patients in March 2025, the acute tower has a variety of spaces to support patients, family and staff well-being, including lounges, new clinics, laboratory collection, amenity and administration spaces, additional bike storage, several new landscaped areas and a large rooftop garden with a walking path.
“The rooftop garden is a spectacular space that will serve patients, public and staff, with walking loops, places to sit, a fitness space and areas to gather,” says Prystai. “On a busy campus, it creates a tremendous opportunity for both views to nature and a convenient opportunity to experience the outdoors.”
Designed by HDR, the project is targeting LEED Gold. Features include a high-performance envelope and a highly efficient mechanical system that uses a heat recovery chiller to capture cooling loads and provide most of the tower’s heating. A sophisticated energy metering system enables operators to continue improving efficiency.
The design team also coordinated with First Nations representatives for interior colours, themes and artwork to ensure they accurately reflect the region’s Indigenous culture. Indigenous elements include welcome figures at the building entrance, ‘Tide-to-Sky’ themes for each floor, a sacred space and the House of Elders.
Prystai credits collaboration and teamwork for the successful delivery of the project.
“Large construction projects are a group effort and we had an excellent team at Lions Gate Hospital, from the architects and engineers to the subcontractors and suppliers to the Vancouver Coastal Health team and our PCL project team,” he says. “It was great to be part of something where everyone worked together to create a fantastic facility that will serve the community and region for a very long time.”
L’intégration de la nouvelle tour au sein des bâtiments du campus a par ailleurs nécessité des réaménagements des structures déjà en service.
Un plan d’échelonnement rigoureux des travaux a permis d’assurer la continuité des activités hospitalières tout au long du chantier. Ce plan prévoyait des démolitions ciblées, le remplacement des installations d’oxygène, la réorganisation des circuits d’évacuation et la création d’accès temporaires.
Ouverte aux patients en mars 2025, la tour de soins intensifs offre de nombreux espaces pensés pour le bien-être des patients, de leurs proches et du personnel. Elle est équipée de salons, de cliniques, d’un laboratoire de prélèvements, des bureaux administratifs, d’un espace supplémentaire pour les vélos, de plusieurs espaces verts nouvellement aménagés et d’un grand jardin de toiture avec un chemin de promenade.
Selon Prystai, “Le jardin de toiture est un espace exceptionnel qui permettra aux patients, au public et au personnel de se détendre, de marcher, de faire du sport ou de se rassembler. Dans un campus très fréquenté, il offre à la fois des vues sur la nature et une bonne occasion de profiter de l’extérieur.”
Conçu par HDR, le projet vise la certification LEED or. Il combine une enveloppe performante et un système mécanique efficace utilisant un refroidisseur à récupération de chaleur pour capter les charges de refroidissement et assurer l’essentiel du chauffage de la tour. Un système de comptage énergétique sophistiqué permet de garantir une bonne efficacité.
L’équipe de conception a travaillé avec des représentants des Premières Nations pour que les couleurs, thèmes et œuvres d’art reflètent fidèlement la culture indigène locale. Les éléments culturels englobent des figures de bienvenue à l’entrée, des thèmes ‘Tide-to-Sky’ pour chaque étage, un espace sacré et la House of Elders.
Prystai souligne que le succès du projet tient à la collaboration et au travail d’équipe.
Selon lui, “Les grands projets de construction exigent un travail d’équipe et nous disposions d’une équipe exceptionnelle à l’Hôpital Lions Gate: architectes, ingénieurs, sous-traitants, fournisseurs, équipe de Vancouver Coastal Health et notre équipe PCL. Tous ont contribué à créer un établissement fonctionnel et accueillant qui servira durablement la communauté et la région.”



EARLY INVOLVEMENT MATTERS
Capital projects perform better when facility managers take part from the start: study
By Rebecca Melnyk
FFacility managers are often integrated into capital projects during the commissioning or post-occupancy phases, after critical decisions affecting long-term operations have been made. Key findings from a new study highlight the importance of involving them earlier in a project’s development life cycle, rather than limiting their ability to influence design, procurement and construction choices.
Findings from the report, The Value of Early Facility Manager Involvement in Capital Projects, gleaned insight from in-depth interviews with 27 facility management professionals across 13 countries, including Canada, and various industries, such as healthcare, education, commercial real estate, government and corporate workplaces.
While a building’s operational and maintenance phase accounts for roughly 80 per cent of its overall life cycle cost, there is much decision-making during the earlier stages when facility managers’ insight is generally excluded, the interviewees shared. The consequences of omitting their expertise can amount to poor maintainability, increasing costs that exceed construction expenditures, long-term operational challenges and disappointed end-users.
Proactive input from facility managers brings an opportunity to shape infrastructure for efficiency and sustained performance, explained Dr. Jake Smithwick, research lead, professor at the University of North Carolina, and associate at Simplar, a global procurement and organizational management consultancy. He was speaking during
an event hosted by the International Facility Management Association this past summer.
BENEFITS OF EARLY INVOLVEMENT
Facility management encompasses many facets of knowledge that can flag issues and avoid costly mistakes. Ibilola Ogundare, graduate research assistant and civil engineering student at the University of Kansas, illustrated how facility managers can influence the planning phase with insights about project specifications, assessing operational feasibility, and evaluating site conditions, infrastructure constraints and integration requirements with other facilities.
“This is a phase where operational needs, staffing requirements and long-term costs can be built into the project strategy rather than
have them patched in later on,” she said. “A facility manager also brings a long-term perspective that other stakeholders might overlook on how the building would be used and maintained over time. This includes input on space planning, site access and system needs that may not have been top of mind for designers or even the owners at this early stage.”
Involvement in the procurement phase is becoming increasingly important for facility managers given current economic situations and increasing workloads for vendors.
“A key part of our value function as facility professionals is to identify and find expert vendors that can work inside our organizations,” said Smithwick. “We certainly shouldn’t minimize that because, when we do, we focus on low-bid cost, which leads to all sorts of other challenges.”
At this stage, facility managers expressed how they can review requests for proposals and guide vendor selections by evaluating specifications and contracts. This directly affects accountability and performance and helps avoid unreliable suppliers.
They can also bridge the gap between shortterm project cost and long-term operational and maintenance goals. What is being purchased must be both affordable and practical; for instance, making sure that equipment is serviceable, replacement parts are accessible and warranties cover what they need to. Proactive involvement brings a lower risk of purchasing systems that don’t integrate well with existing infrastructure or cost more to maintain.
As a project nears the design and pre-construction phase, facility managers can review plans and drawings to account for real-world conditions and focus on long-term use that goes beyond aesthetics. They can advocate for standardized building systems for operational consistency and fewer maintenance issues, as well as impact material selection and space allocation. As Ogundare explained, facility managers can identify what materials will maintain durability in local climates or how layouts will best suit future occupants.
Once construction commences, facility managers can participate in change order reviews, support quality control efforts and assist contractors by conducting periodic site visits to identify potential issues.
“There have been instances where access panels were blocked or equipment was installed in a way that would make it inaccessible for servicing,” said Ogundare.
While big decisions are often made before commissioning begins, at this stage, managers can still confirm warranty documentation and validate if systems are performing as intended and comply with other standards.
“Based on what the interviewees said, when facility managers are actively engaged in the early planning phases, it makes the handover process smoother,” said Ogundare. “They know the building because they have been part of the process and are better prepared to manage it from day one.”
MOVING BEYOND BARRIERS
A subtle bias persists during project development that prevents facility managers from being viewed as valuable contributors.
“They are seen as people who just fix things after the facility is handed over and this misconception actually limits their seat at the table,” said Ogundare. “One practical solution to overcome this barrier would be to position facility managers as strategic partners.”
A way forward is involving them in project steering committees to influence decisions, including them as voting members, and having them sign-off on designs and procurement packages alongside architects and engineers. At this point, they can share operational case studies that highlight how design flaws have impacted maintenance and operations.
Some interviewees working primarily in universities and healthcare noted how facility managers are starting to be invited to early capital planning meetings because the owners and other project stakeholders are beginning to see the long-term effects of these design errors, said Ogundare.
Fragmented delivery with no designated role for facility managers during project development also hinders their decision-making abilities. To overcome these obstacles, embedding facility manager checkpoints in contracts and project processes could mean adding clauses that require facility managers to review schematic design, construction documents and commissioning reports. Pilot projects could uncover valuable outcomes, such as reduced rework and smoother handovers, to be shared with senior leadership.
Short-term budget focus is another barrier drawn from the study.
“Many projects prioritize the lowest upfront cost, even if that leads to much higher operating expenses, which makes it really
hard for facility managers to recommend better systems or materials,” said Ogundare. “A very practical way to address this would be through life cycle cost analysis. Demonstrating our return on investment in real dollar terms or in years is one of the strongest ways to shift mindset and help re-orientate clients and project stakeholders.”
To further help facility managers actively participate in discussions with designers and builders, technical training and professional development require more investment. Many managers lack such expertise; however, they can upskill through building information modelling training, commissioning certificates, energy modelling and mentorship. Past research has shown that credentialed employees have higher ratings for performance appraisals, customer satisfaction and productivity.
FRAMEWORK BRINGS ADDED CLARITY
A practical tool emerging from the study is the RACI framework, an acronym for the different responsibility types within a project: responsible, accountable, consulted and informed. For facility managers, this would help offer clarity about where their input is essential and define their level of involvement across the phases of a project.
In the planning stage, for example, a chart based on the framework would show that the facility manager is ‘responsible’ for defining operational and maintenance requirements; should be ‘consulted’ when it comes to accessing the budget for operations, maintenance and life cycle cost analysis; and must be ‘informed’ about project approval meetings so they can comment as needed.
Using this tool integrates facility manager expertise more effectively, reinforces their value to other stakeholders, helps teams align facility manager activities with project deliverables, breaking those tasks down across different phases, and supports work training. Newly hired facility managers can visualize the areas where skills are lacking, while senior managers can mentor the younger generation through the responsibilities listed in the framework.
“Early decisions affect long-term cost,” concluded Ogundare. “The facility manager should be brought on earlier so their input, based on experience, can help maximize the project. Facility managers are strategic partners and not just maintainers. They should have a seat at the table.”

SIGHT AND LIGHT
Design beyond the patient room
By Rob Swart, Josh Bornia & Alyssa Young
IInside many healthcare facilities, access to daylight is hard to find and that’s tough on patients, staff and visitors. But a new day is dawning in healthcare design, as priority is placed on getting daylight deep into hospitals and other care facilities.
This daylight-driven approach is based on the fact that humans feel better when they have access to natural light, and healthcare facilities are places that, by definition, are supposed to help people feel better.
Studies further support the benefits of natural light in a health setting. The right exposure has been shown to shorten hospital stays and reduce stress among patients waiting to undergo medical tests and operations. Staff working in naturally lit environments report less fatigue and higher satisfaction, so much so that one study found increasing daylight in healthcare facilities would help reduce staff burnout during the pandemic. For families navigating large, unfamiliar hospitals, win-
dows and views help with orientation and wayfinding, reduce the sense of being trapped in a maze of corridors, and provide psychological relief when people might be extremely anxious or sad. In cancer centres, access to daylight has been shown to improve communication between family members and staff. But it is a challenge to get sunshine into healthcare facilities. It requires a thoughtful, multilayered approach that goes far beyond simply adding extra windows.

LEADING BY EXAMPLE
To optimize natural light exposure in healthcare settings, Dialog pulls together specialists from mechanical and electrical engineering, architecture, landscape architecture and clinical planning as part of an integrated design team. Using a combination of software tools, parametric modelling and interviews with staff and patients, the team works collaboratively to incorporate daylight into buildings in a meaningful way.
First, they assess the site for the proposed building and brainstorm ways to maximize views to the outside. The team studies the topography, solar exposure, existing vegetation and sightlines to inform the location and orientation of the building. This sometimes leads to unconventional building shapes. In Grand Prairie, Alta., for instance,

a 240-bed regional hospital sits on the highest point of the property to capture views over Bear Creek, a natural watercourse that runs through the site. The structure’s serpentine lines follow the bends of the creek, giving as many patient rooms as possible views of the water and wildlife wandering at its edge.
Arthur J.E. Child Cancer Centre in Calgary serves as another example. The largest cancer treatment and research facility in Canada features two J-shaped wings that create a heart shape, surrounding an all-season garden courtyard.
Next, the design team examines the way people are expected to move inside a building. They identify the ‘public spines’ — main thoroughfares inside a space — that connect major entrances and gathering areas. The team maximizes glass panels and views
along these public spines. That might mean floor-to-ceiling windows in waiting areas or a sun-soaked multi-level atrium at a main entrance. These public spines generally occupy a relatively small portion of a building’s overall footprint, but have an enormous effect on the way staff, patients and the public perceive a facility.
The team then looks for opportunities to integrate daylight into clinical planning, even in spaces historically left windowless. The goal is to get a healthy amount of natural light into places where patients are being cared for and staff are working. This represents a huge challenge for designers. Too much daylight might mean discomfort for a bedridden patient who can’t get up to adjust curtains, or glare in the eyes of a surgeon at a key moment in an operation. It can also lead to over- or
under-conditioned buildings, requiring increased HVAC and driving up capital and operating costs.
There’s no one-size-fits-all solution for getting natural light into a healthcare facility. Every building differs because of its location, regional climate and latitude. Temperature, humidity and sun angles vary over the course of a year and affect energy loss, glare and condensation.
For every facility, Dialog’s designers perform detailed analyses using a variety of tools to determine variables like the quality and quantity of daylight entering a building, and sun hours and angles at different times throughout the day or even across a year. They look at what can be adjusted to ensure light comes into the facility in the best way possible, taking views, energy use, cost, comfort and infection control into account.
For instance, operating rooms and medical device cleaning facilities are traditionally lit only with artificial light. Windows come with an increased risk of condensation, which creates an ideal environment for microbial growth. This can seriously affect the ability

to sterilize surgical instruments and maintain infection control.
At Dartmouth General Hospital in Nova Scotia, windows were added to both surgical suites and the medical device reprocessing department during an expansion project. The risk of condensation was minimized by amping up air circulation near windows and with planned windowsills, blinds and furniture so that air movement near window panels is unrestricted. In the medical device reprocessing department, designers added a bank of clerestory windows high on the wall with shelving below to help prevent the sun’s rays from hitting occupants at eyelevel. In operating rooms, vertical windows offer views to the outdoors. The surgical team reports that they find it valuable to pause in the middle of an operation to rest their eyes for a moment by looking out the window.
In other places, the design team adds frits onto windowpanes. These are tiny patterns of ceramic enamel baked on glass, which reduce solar heat and minimize glare. Frits can be helpful in places like pharmacies where ultra-violet degradation of pharmaceutical products is a concern.

REIMAGINING HOSPITAL DESIGN
Today, more jurisdictions require designers to integrate daylight into plans for healthcare facilities. These daylight-centred designs are more challenging than the old approach to healthcare settings, but they fundamentally change how staff and patients experience hospitals. With people in hospitals often having the worst days of their lives, the physical infrastructure of these spaces should not make things harder. Rather, they can be designed to make people feel better. And that, ultimately, is the goal.
Rob Swart is an architect and partner at Dialog. He has led a wide range of major healthcare projects in Alberta, including the Red Deer Regional Hospital Centre redevelopment, Edson Healthcare Centre and Gene Zwozdesky Centre at Norwood. Josh Bornia is an electrical engineer and associate at the firm, who has led electrical and lighting design on the same major healthcare projects as Rob. Alyssa Young is a mechanical engineer-in-training at Dialog. Alyssa applies her expertise in HVAC, plumbing, fire protection and building automation to major projects like the new patient tower at Toronto Western Hospital.


INDOOR AIR RETHINK
Displacement ventilation as a keystone of future healthcare design
By Alex Hutton, Greg Allen & Tariq Amlani

Across Canada, healthcare infrastructure is entering a once-in-a-generation renewal cycle. An unprecedented number of hospitals and long-term care homes are being planned, designed and built to meet demographic shifts, population aging and post-pandemic healthcare strengthening. Each new facility faces immense pressure to improve infection control, cut energy and carbon, step up resilience to extreme heat, accelerate schedules, and reduce both capital and operating costs.
Under such pressures, it’s natural for design teams to gravitate toward familiar templates. Familiarity feels safe. Incremental modifications — an added recovery coil, a higher-efficiency chiller — can address individual challenges without rethinking the overall system. Yet, as demands multiply, incremental changes often add complexity and cost. Sometimes the path to lower cost isn’t through cutting scope; it’s through rethinking the system itself.
There is a proven holistic design framework that embodies such a rethink and the keystone strategy that holds it together is displacement ventilation (DV). Other elements include 100 per cent outside air, radiant heating, improved
building envelope and superior control of solar gains. An emerging evolution of this framework is envisioned whereby demandcontrolled DV, or DC-DV, unlocks significant capital cost savings.
FIRST PRINCIPLES OF VENTILATION
The fundamental purpose of ventilation in healthcare facilities has always been clear: deliver fresh air and remove contaminants.
Florence Nightingale’s first canon of nursing was to “keep the air that the patient breathes as pure as the external air, without chilling them.” Her wards relied on natural buoyancy — warm, contaminated air rising and exiting through high openings, replaced by clean outdoor air at low-level and radiant heating for thermal comfort.
Over the past half century, however, hospital ventilation design and associated building codes evolved together around an overhead mixing ventilation (MV) approach. MV delivers cool air at high-velocity from ceiling diffusers intended to achieve complete mixing of air throughout the space to maintain a uniform temperature. This approach is familiar and predictable, but it takes a dilution
approach to contaminants, re-circulating rather than removing them. It also combines two distinct purposes: ventilation for health (fresh air supply and contaminant removal) and ventilation for thermal comfort (delivering heating or cooling).
DV is an evolution of enduring design logic — not a revolution. It represents a return to first principles and the core purpose of ventilation. DV supplies low-velocity air to the floor at a slightly cooler temperature than the room. Air warms when it encounters a heat source, such as people, equipment and lighting, rising naturally, carrying heat and contaminants up and out of the occupied zone to high-level exhausts. Thermal comfort is maintained primarily by regulating ventilation rates and supply air temperature augmented by radiant panels.
PRESCRIPTIVE VERSUS PERFORMANCE
In most hospitals, ventilation is the single largest contributor to energy use, typically accounting for more than half of total building consumption when reheat is included. Conventional MV systems push large volumes of air through extensive duct networks, condi-

tioning and reconditioning that air to maintain stable temperatures.
CSA standards prescribe both outside air and total air in terms of air changes per hour (ACH) for healthcare spaces; the difference between the two is often substantial. For example, a typical patient room requires two ACH of outside air and six ACH total air; a treatment room requires two ACH of outside air and up to 12 ACH total air. That gap is often two to six-fold — logical for mixing systems that rely on recirculation but less relevant for displacement systems designed to remove contaminants rather than dilute them.
This recognition invites a shift toward performance-based design, with ventilation volumes that are proportional to occupancy and actual contaminant generation.
STRATIFICATION REDUCES COOLING LOAD
In a DV room, cool air enters at low-level and spreads across the floor. As it encounters heat sources, it rises in thermal plumes. Warm, contaminated air collects at the ceiling and is exhausted, while the occupied zone remains supplied with clean, slightly cooler air.
Because only the lower occupied zone is conditioned, the system’s effective cooling load is dramatically reduced. Heat naturally stratifies to the upper zone, which can be
allowed to run warmer without affecting comfort. This cooling de-rating effect can reduce active cooling energy by 60 to 70 per cent, improving resilience to extreme heat and reducing central chiller capacity and associated electrical infrastructure.
On the other hand, since DV systems supply air at a warmer temperature — typically 19 to 20 C instead of the 13 C common in MV systems — the amount of cooling that can be delivered is reduced. With a combination of the cooling de-rating, attention to minimize internal gains (such as solar) and minor variations in supply air temperature depending upon outside air temperature, DV may be able to deliver sufficient cooling without the need for supplemental cooling systems. For DC-DV, the air flow can also be modulated with occupancy, which works well since the sensible and latent cooling load of occupants is proportional to carbon dioxide.
A KEYSTONE OF HOLISTIC DESIGN
DV cannot be considered in isolation, especially in a healthcare context, where it works best within a design framework that typically combines 100 per cent outside air with heat recovery, DV for directional contaminant removal, radiant heating for thermal comfort without reheat, and enhanced envelope and
solar control for load management.
This holistic design framework is not new — it has emerged over decades. DV has been applied for more than 40 years across many building types and its use in healthcare grew following a Stantec-Mazzetti research collaboration (2006-2009) that demonstrated strong performance advantages.
The Targeting 100! initiative, led by the University of Washington’s Integrated Design Lab, developed a foundational roadmap for healthcare decarbonization, targeting energy use intensity of 100 kBtu/sf/year or 315 kWh/m²/ year. This robust framework, published in 2012, methodically revealed the magnitude of reheat transfer (often more than 40 per cent of hospital energy), and a holistic and cost-effective archetype to eliminate it: 100 per cent outdoor air with DV, load reduction, and decoupled heating and cooling.
PROOF IN PRACTICE
Nanaimo Regional General Hospital’s emergency department, completed in 2012, exemplifies the holistic design philosophy illustrated through the Target100! initiative. The project introduced 100 per cent outdoor air DV across most of the department, supported by radiant panels and a unique thermal labyrinth design feature to precondition outside air.
Computational fluid dynamic (CFD) model ling conducted during design predicted reduced aerosol spread. Post-occupancy monitoring confirmed improved comfort and measurable reductions in nosocomial infection rates. Energy modelling predicted a 30 per cent reduction in total energy use intensity, reducing the code baseline from 747 kWh/m2/year to 524 kWh/ m2/year, while actual performance a few years after occupancy was confirmed at 301 kWh/ m2/year, placing measured performance on par with the best European healthcare facilities without deviating from CSA prescriptive venti lation rates.
The design also proved that DV integrates well into complex healthcare environments. Wall diffusers served patient rooms; cylindrical floor diffusers supplied open spaces, such as waiting areas; and anti-ligature ceiling grilles delivered supply air to mental health rooms via a ‘waterfall’ effect (where the cooler supply air falls to the floor).
CAPITAL COST SAVINGS POTENTIAL
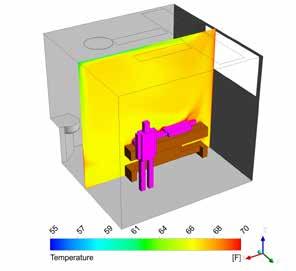
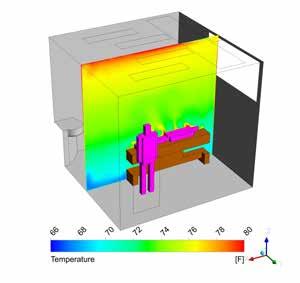
t CFD rendering of temperature stratification scenarios: mixing ventilation (left) and displacement ventilation (right). Images courtesy Price Industries
A BC Hydro energy study for Nanaimo Regional General Hospital’s emergency department estimated a modest incremental capital cost when compared to a building code baseline design, with the cost of higher performance envelope, automated exterior solar shades, thermal labyrinth, customized supply air grilles and radiant panels partially offset by elimination of return air ductwork and smaller plant equipment.
In general, capital cost savings with a DV design are not incremental – they’re structural. When DV uses 100 per cent outside air, return air ductwork is eliminated, simplifying coordination and reducing shaft space. Floor-to-floor heights can drop by at least 30 centimetres, saving building envelope and structural materials, as well as reducing embodied carbon.
When approached holistically, DV can deliver superior performance at comparable or lower capital cost compared with conventional MV. Adding DC-DV to the framework has the potential to magnify the cost-saving ripple effects of reduced ductwork through design for diversity, leading to a substantial decrease in capital cost.
CODES, STANDARDS AND READINESS
Both ASHRAE 170 (Ventilation of Health Care Facilities) and CSA Z317.2 (Special Requirements for Heating, Ventilation and Airconditioning Systems in Health Care Facilities) acknowledge DV as a permissible system.
The ASHRAE standard allows air change calculations for DV to be based on the occupied zone volume (floor to 1.8 metres) rather than the full room, explicitly recognizing that upper stratified air is not actively conditioned.
The CSA standard includes a clause that states “the use of displacement ventilation shall not be used as rationale for decreasing air exchange rates unless engineering studies have demonstrated an equivalent level of safety.” This clause is made clear by paraphrasing to remove the double negative: DV can be used to justify lower total airflows, provided equivalency in thermal comfort, humidity and infection control is demonstrated through CFD modelling and empirical validation. In short, the door is already open; what’s needed is shared understanding of how to walk through it.
A PATH FORWARD
Hospitals are built to heal, yet traditional ventilation systems often consume vast energy while circulating the contaminants they aim to remove. DV offers a practical, proven alternative that restores the original intent of ventilation — delivering fresh air and removing contaminants — while modernizing it for today’s carbon and resilience challenges.
Examples like Nanaimo Regional General Hospital’s emergency department and the Target100! archetypes show this approach is achievable today using available technologies. By embracing DV as part of a holistic framework, healthcare organizations can create environments that are healthier, more efficient, less costly and better prepared for the future. The
science is clear, the precedents exist and the path forward is open to those ready to take it.
The Displacement Ventilation Emergence in Healthcare (DiVE) initiative brings together diverse interest holders to explore how DV can move from rare pilot to mainstream practice by consolidating past research into a technology profile, additional CFD analysis to deepen understanding, and educational outreach to support design teams exploring DV and DCDV approaches. DV’s success depends not on complexity but on design literacy.
Additional funding is being sought to develop a DV application guide for healthcare, to build upon generic DV guides, such as one published by the American Society of Heating, Refrigerating and Air-Conditioning Engineers.
The DiVE project is made possible by funding from Vancouver Coastal Health, Fraser Health and BC Hydro as well as in-kind support from several partners, including Stantec and the Canadian Coalition for Green Health Care, whose website hosts the DiVE homepage. Interested parties are invited to participate in this important and ongoing effort.
Alex Hutton, P.Eng., is founding principal of Swordfern Strategic Sustainability and project manager for the DiVE initiative. Greg Allen, P.Eng., is a senior associate at Rivercourt Engineering with more than 40 years of experience advancing ventilation and sustainable design. Tariq Amlani, P.Eng., is the health sector engineering and Canada lead at Stantec, with nearly 20 years of Canadian healthcare design experience. They can be reached at alex@swordfernstrategic.com, greg.allen@rivercourt.ca and tariq.amlani@stantec.com, respectively.
TRANSFORMING MENTAL HEALTH SERVICES
Collective effort delivers modern approach to mental health and addictions-based care
By Jeff Card

This past April, a key step in the transformation of Newfoundland and Labrador Health Services’ (NLHS) mental health and addictions system was achieved with the transfer of patients from Waterford psychiatric facility to the recently finished Mental Health and Addictions Centre (MHAC) located on Health Sciences Centre’s campus in St. John’s.
Designed to destigmatize mental health, MHAC includes a 240,000-square-foot, sixstory, 102-bed hospital that features therapeutic terraces and daylight-filled rooms to foster comfort and community for clients, families and caregivers; a new 60-bed hostel (replacing Agnes Cowan Hostel that was demolished in 2019); and a parking garage with space for 1,000 vehicles.
Completed under a public-private partnership (P3) model, the design-build-financemaintain contract for the replacement of MHAC was awarded to Avalon Healthcare Partnership (AHP), a consortium consisting of 13 companies, in summer 2020. The team established service commencement in October 2024 (on time), which included early turnover of the parking garage in fall 2021. The project was delivered with significant local workforce participation and long-term maintenance commitments, overcoming pandemic challenges to reach financial close and provide sustainable, high-quality infrastructure for the province.
AHP took great care in the design, construction and commissioning of the project. The forensics unit is located on the ground floor to improve safety and security for staff, patients and visitors. The hostel is constructed on a single floor to reduce staffing requirements for NLHS, and to improve operational efficiency. The multiple outdoor terraces, a NLHS requirement for normative healing, were provided with snow melt systems to maximize use and minimize snow clearing impacts. The mechanical plant for the building is centralized in a penthouse with all air handling units in the interior, and

a 100 per cent outside air system to maximize fresh air exchange within the building. For maximum efficiency, heating is delivered from the existing campus annex.
Multiple user group meetings were held throughout the design development stages to ensure feedback from NLHS was implemented and then brought back for review before being constructed in the field. This resulted in fewer infrastructure changes postservice commencement.
Contracted with a 30-year operating mandate, the facilities maintenance team is responsible for a range of facility management and life cycle duties: help desk services and response; electrical systems maintenance; HVAC and building automation systems (BAS) control and maintenance; implementation of computerized maintenance management systems for maintaining assets; and oversight of all information, communication and automation technology, including, but not limited to, fire alarm, closed-circuit television, real-time locating systems, access controls, nurse call and enterprise service bus.
Given the long-term mandate of the project, several design elements were woven into the building to assist with future operations. For example, there was a provision for an isolation exhaust system that can be used to exhaust air from construction zones with only minor modifications. With this system in place, the operations team is able to create the necessary negative pressure zones required for construction/ remediation work without significant disruption to facility operations. This has led to faster response during construction change requests and when there have been incidental damage/ repair requirements for the facility.
Code grey (loss of essential service) programming related to air changeover was also incorporated into BAS architecture. It was fully designed and implemented for simpler operation during external events, and commissioned as part of building deployment. This included confirmation of airflow setbacks at all airflow stations to accommodate changes from outside air to recirculation. It has already been tested once as a result of

wildfires in Newfoundland and Labrador.
With respect to penthouse design and placement of generator and HVAC equipment, it was determined that indoor equipment would provide the lowest total cost of ownership for the application. Once selected, major equipment was located relative to overhead structural steel, and the generator ventilation design was facilitated to accommodate removal through the louvers. A concrete laydown pad and oversized access doors were incorporated into the southeast tower roof for future equipment removals/placements, as required.
The LEED Gold building was recognized with an award of merit in the P3 design and construction category at the 2025 National Awards for Innovation and Excellence in P3s, presented by the Canadian Council for PublicPrivate Partnerships (CCPPP). In 2021, MHAC won a silver award for project development, again from CCPPP.
Jeff Card, P.Eng., is vice-president of technology and services at The Cahill Group.
RESILIENT READY
Navigating Canadian healthcare amidst compounding crises
By Waseem Hamweyah

Canada’s publicly funded healthcare system is under increasing strain from a convergence of stressors. In order to anticipate, absorb and adapt to disruptions, healthcare leaders must embed resiliency into both project-level design and organizational strategies.
Here is a breakdown of key challenges facing this country’s healthcare system, with suggested actionable solutions to improve resiliency.
CLIMATE CHANGE DISRUPTION
Climate-related events are directly impacting
healthcare delivery. In 2023, wildfires in British Columbia led to air quality warnings, affecting more than 1.8 million residents. Emergency room (ER) admissions spiked and there was an increased risk of heart attacks or other cardiac events. That same year, flooding in Nova Scotia forced the temporary closure of multiple care facilities. Vulnerable populations — children, seniors and those with chronic conditions — were disproportionately affected.
Solution: At the project level, design resiliency into healthcare facilities, such as pas-
sive cooling, flood-resistant architecture and renewable energy systems. Organizationally, implement climate-health surveillance systems and integrate climate risk into capital planning. In addition, healthcare systems and facilities must have a common understanding of the ‘elevated risks’ that are expected in the future.
OPERATIONAL OVERLOAD AND DEFICITS
With more than half of Canadian healthcare facilities being more than 50 years old and built for a smaller population, the strain caused by increased demand and decaying
efficiency is only widening the gap between level of care needed and level of care expected. ERs have become overwhelmed, average ER wait times have increased (up to 20.7 hours in 2024, in Ontario), and surgical backlogs now exceed 200,000 procedures, according to Environics Research.
Solution: At the project level, build modular, scalable facilities with smart systems for energy, ventilation and patient flow. This should shift Canada’s healthcare model from major hospitals to a feeder system that provides care closer to home. Organizationally, use predictive analytics to optimize scheduling and resource allocation. Invest in interoperable digital platforms to streamline care coordination. This can extend to the use of telemedicine and 5G powered facilities. Such a change is not only due to physical infrastructure but rather legislative update that encourages sharing of resources.
DIGITAL VULNERABILITIES
Cybersecurity threats post a significant and growing risk to digital health systems. Recent years have seen an increase in cyberattacks on healthcare facilities, with ransomware incidents causing disruptions to patient care and potentially compromising sensitive data. Solution: At the project level, implement secure-by-design digital systems. This doesn’t only lower the severity of damage but serves as a stress test for governance and bylaws underlying healthcare facilities. What’s critical to achieve this is to pivot from using platforms as layered tools to building a digital organizational twin/data base, in line with the functional layout of the facility. Organizationally, integrate cybersecurity into operational risk management. This would become a natural
development of a healthcare system if adopted at the facilities level. However, there will be a need to define a unified ‘skeleton’ of this digital organization’s capabilities and services in order to ensure no divergence takes place, something that regulators should own at least at the very least.
DEMOGRAPHIC SHIFTS
Seniors now represent nearly 20 per cent of the population, reports Statistics Canada, and this is projected to increase. This is driving demand for long-term and home-based care.
Solution: At the project level, far more longterm facilities must be planned, built and operated. However, these facilities will need to be equipped for somewhat more productive senior communities rather than traditional senior homes. Organizationally, use demographic forecasting to guide service expansion and funding models. This may lead to more senior communities than homes where residents are still productive and help operate the community. This concept has been adopted in the Netherlands for a dementia village. While perhaps an extreme scenario, the principles of it may be worth investigating.
DESIGNING FOR RESILIENCY
Many healthcare systems remain reactive, with resiliency treated as a retrofit rather than a foundational principle. Fragmented governance and siloed services hinder coordinated responses to crises.
Solution: At the design level, design multi-use community hubs that integrate health, housing and social services. Organizationally, adopt integrated care models, reform governance for agility and institutionalize cross-sector collaboration.
BUILDING A RESILIENT FUTURE
Canada’s healthcare system must evolve to meet the demands of a changing world. By embedding resilience into every layer, from infrastructure and workforce to governance and equity, leaders can build a system that not only withstands disruption but thrives through it.
This doesn’t necessarily restrict integration to new systems and facilities. A resiliency assessment can be done for existing systems and facilities no matter their life span.
A three-phase approach can aid health systems to identify vulnerabilities, strengthen emergency preparedness and ensure care continuity, aligned with equity and sustainability goals. First, screen. Rapid self-assessment flags risks. Next, assess. This involves expert-led evaluation across key domains, such as infrastructure, cybersecurity, information technology, supply chain, emergency management, business continuity, followed by training. Then, plan. Tailor a roadmap for resilience. While this may not be a completely novel approach, it serves as a starting point for any healthcare facility or system that wants to challenge the status quo and make a lasting difference.
Waseem Hamweyah is a senior advisor at Jacobs. He is a seasoned sustainability professional with extensive global experience in healthcare resilience, particularly adept at translating international best practices to the Canadian context. Waseem’s portfolio includes numerous healthcare projects where he has implemented innovative sustainability solutions. He can be reached at 416-824-4584 and waseem.hamweyah@jacobs.com.

A CRITICAL PRIORITY
By Steve Bowers
In healthcare, fire protection is about more than meeting code — it’s about safeguarding lives, preserving critical infrastructure and ensuring uninterrupted patient care. Hospitals and other healthcare environments house advanced imaging equipment, surgical suites and data centres that cannot afford downtime or water damage. Traditional sprinkler systems, while effective for general fire protection, often pose risks in these spaces. This is where special hazard fire suppression systems become indispensable.
Over the past century, these systems have evolved dramatically, driven by technological innovation, environmental responsibility and stringent regulatory mandates. For healthcare leaders, understanding this evolution is key to balancing patient safety, operational continuity and sustainability.
EARLY ERA DOMINANCE
Introduced in the 1950s, Halon fire suppression systems were a breakthrough for environments where traditional sprinkler systems were not an option. Halon offered rapid fire suppression without leaving residue and did not damage sensitive electronics or medical equipment.
For decades, Halon was considered the gold standard for special hazard protection, as its ability to interrupt the chemical chain reaction of combustion made it highly effective for Class A, B and C fires. However, its negative environmental impact became a growing concern. Halon is a chlorofluorocarbon (CFC); its release into the atmosphere contributes significantly to ozone layer depletion.
By the late 1980s, scientific consensus and international pressure led to regulatory action. In 1993, the Montreal Protocol, an international treaty designed to protect the ozone layer, banned ozone-depleting substances like CFCs, forcing industries worldwide to rethink fire suppression strategies. This marked a significant turning point. Halon production
ceased in most countries by the mid-1990s, forcing healthcare and other industries to seek alternatives.
CLEAN AGENTS TAKE CENTRE STAGE
To fill the void left by Halon, the fire protection industry introduced clean agent systems, codified under National Fire Protection Association (NFPA) 2001: Standard on Clean Agent Fire Extinguishing Systems. These systems featured agents like HFC-227ea and FK-5-1-12, which offered similar benefits to Halon — rapid suppression, no residue and safety for sensitive equipment — while eliminating ozone depletion potential.
Clean agents work by absorbing heat or interrupting the chemical reaction of combustion. They are stored as liquids and discharged as gases, flooding the protected space to extinguish the fire.
However, while clean agent systems solved the ozone depletion problem, they introduced a new environmental challenge: global warming potential. Hydrofluorocarbons (HFCs), commonly used in clean agent systems, are potent greenhouse gases (GHGs). This concern led to further regulatory action, including the Kigali Amendment to the Montreal Protocol and, in the United States, the American Innovation and Manufacturing (AIM) Act.
The Kigali Amendment came into force Jan. 1, 2019, mandating a global phasedown of HFCs, including HFC-227ea, which was commonly used in clean agent fire suppression systems. It requires countries to incrementally reduce HFC production and consumption by more than 80 per cent over approximately 30 years, with legally binding targets for participating countries. Since HFC-227ea has a high global warming potential, reflective of its GHG strength, its availability has been curtailed under these schedules.
In the U.S., the AIM Act authorizes the Environmental Protection Agency to regulate HFC production and consumption, mandating an 85 per cent phasedown by 2036. The legislation ensures alignment with global climate goals while driving the adoption of next-generation fire suppression technologies that meet stringent environmental standards.
Additionally, Canada’s 2025 State of PFAS Report identified most per- and polyfluoroalkyl substances as toxic under the Canadian Environmental Protection Act due to their persistence and health risks. This finding has significant implications for fire suppression systems that historically relied on PFAS-based agents. The report signals a regulatory shift toward eliminating PFAS in fire protection, and accelerating the adoption of environmentallyfriendly alternatives to meet compliance and sustainability goals.
Regulatory uncertainty has pushed healthcare engineers and facility planners to exercise heightened caution when designing building systems. In sensitive sectors like healthcare, where patient safety and environmental stewardship are paramount, specifying fire protection agents is increasingly complex. A chemical approved today may face restrictions tomorrow, making long-term planning difficult. While engineering teams are adept at adapting to evolving standards, healthcare organizations rely on them to deliver solutions that not only meet current codes but also anticipate future regulatory shifts. The challenge is clear: create fire suppression strategies that protect patients, safeguard critical equipment and remain sustainable in an unpredictable regulatory landscape.
THE NEXT FRONTIER
As environmental regulations further tightened, the fire protection industry sought solutions with minimal climate impact. Enter NFPA 770:


Standard on Hybrid (Water and Inert Gas) Fire Extinguishing Systems. Hybrid extinguishing systems combine ultra-fine water droplets, which can be smaller than white blood cells, with inert gases to suppress fires efficiently while requiring far less water than traditional sprinklers.
Hybrid extinguishing systems offer several advantages in complex applications. They have zero ozone depletion potential and negligible global warming impact. Minimal water usage reduces the risk of damage to medical equipment and electronics. The fine water mist cools flames, while the inert gas dilutes oxygen, stopping combustion quickly. There is also no need for assurance of tight room integrity. Further, quick system recharge and minimal downtime means reduced interruption to patient care.
“We are already seeing proof that our updated restrooms are improving the user experience. The touchless, solar-powered Sloan products have been crucial in this successful effort.” - Briar Del Buono




For hospitals and healthcare environments, NFPA 770 systems represent a forward-thinking solution that aligns with sustainability goals, regulatory compliance and the need to protect critical infrastructure without compromising patient care.
A SAFER, GREENER FUTURE
Healthcare facilities face unique challenges in fire protection. Operating rooms, imaging suites, backup power rooms and data centres cannot tolerate downtime or equipment damage. At the same time, hospitals are under increasing pressure to meet environmental standards and reduce their carbon footprint. The transition from Halon to NFPA 2001 systems, and now to NFPA 770 solutions, reflects this balancing act between compliance, risk management and sustainability: regulatory mandates like the AIM Act and Montreal Protocol require healthcare organizations to phase out high global warming potential agents; fire suppression systems must protect life and property without introducing secondary risks, such as water damage or chemical exposure; and hospitals are adopting green building standards and sustainability initiatives, making eco-conscious fire protection a priority. For healthcare leaders, the message is clear: fire protection strategies must evolve alongside regulatory requirements and sustainability goals. By embracing modern technologies and standards, hospitals can ensure present and future compliance, safeguard critical assets and contribute to a greener future, without compromising the quality of care.
Steve Bowers is the Western Canadian business development specialist at Victaulic, a global leader in mechanical pipe joining and fire protection solutions. He can be reached at steve.bowers@victaulic.com.
DESIGNING FOR OPTIMAL PATIENT CARE AND OUTCOMES

No matter how simple or complex your goals are for your perioperative environment, the STERIS Healthcare Design Services team can help:

Design Development: Create the ideal layout for your facility, from equipment placement and single-room layouts, to department designs that ensure optimal performance and efficiencies.
Capacity Assessment: Analyze current capacity and understand future growth opportunities for your facility, including equipment, staff, and procedure types.
Construction Documentation: Provide detailed technical information to the architect, engineer, and construction team to facilitate a successful project and facility development.