A Kidney Xenotransplantation Milestone



Radical prostatectomy (RP) is associated with better cancer-related survival compared with radiation therapy (RT) among patients with prostate cancer who have unfavorable intermediate- and high-risk nonmetastatic disease and those who have clinically positive nodal disease, according to separate studies presented at the 2024 congress of the European Association of Urology in Paris. Both studies are distinguished by their use of other-cause-mortality (OCM) matched cohorts to mitigate the selection bias of previous studies whereby patients with worse health status are referred for RT, according to investigators.
In one study, investigators analyzed Surveillance, Epidemiology, and End Results (SEER) data from 6506 patients diagnosed with nonmetastatic prostate cancer from 2004 to 2009 who underwent RP or RT. The 10-year cancer-specific mortality (CSM) rates were significantly higher for the RT group compared with the RP group among patients with unfavorable intermediate-risk disease (8.8% vs 0.6%) and those with high-risk disease (7.9% vs 3.9%), according to results reported by Marco Finati, MD, from the Henry Ford Health System’s Vattikuti Urology Institute in Detroit. The CSM rates did not differ significantly between the RP and RT
continued on page 7
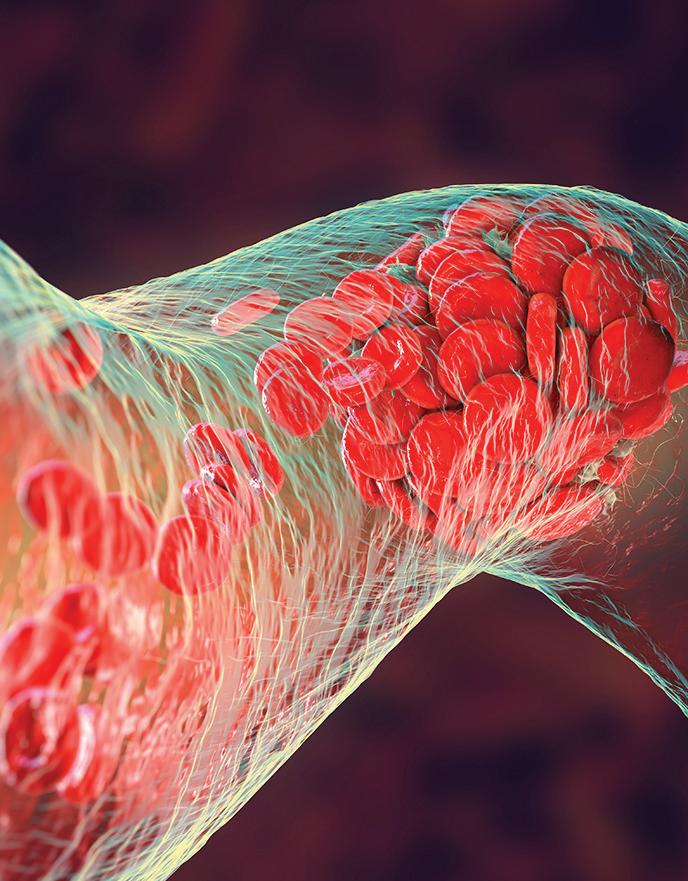
BY JODY A. CHARNOWTransplant surgeons at Massachusetts General Hospital in Boston have performed the first successful transplantation of a genetically modified pig kidney into a living patient.
During the 4-hour-long surgery that took place on March 16, the patient, a 62-year-old man from Weymouth, Massachusetts, received a pig kidney that was genetically edited to remove pig genes and add helpful human genes for a total of 69 gene edits to improve its compatibility with human beings, according to a Mass General press release. The procedure was performed under the US Food and Drug Administration’s Expanded Access Protocol, also known as compassionate
Longer periods of sustained clinical remission of lupus nephritis (LN) are associated with decreasing risks for flares and kidney function decline, a new study finds.
Among 303 patients with LN, 257 (84.8%) achieved sustained clinical remission after a median 1.4 years after treatment initiation. Sustained remission was defined as a Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) score of 0 along with an estimated glomerular filtration rate (eGFR) above 60 mL/min/1.73m2 for 1 or more years.
The probabilities of achieving sustained clinical remission increased from 40% at 1 year to 60%, 70%, 80%, and 90% at 3, 5, 10, and 15 years, respectively, “suggesting that a long-term treatment is necessary to achieve remission in LN,” Gabriella Moroni, MD, of IRCCS Humanitas Research Hospital in Milan, Italy, and colleagues reported
use. The patient received infusions of the novel immunosuppressant medications tegoprubart and ravulizumab.
The patient was discharged from the hospital on April 3.
“The procedure marks a major milestone in the quest to provide more readily available organs to patients,” the hospital said in the release.
In the United States alone, more than 89,000 people are waiting for a kidney, according to the Organ Procurement and Transplantation Network.
Previously, teams at NYU Langone Transplant Institute in New York and the University of Alabama at Birmingham (UAB) successful transplanted genetically modified pig kidneys into brain-dead
continued on page 7 continued on page 7
3 Fewer dialysis technicians linked to worse outcomes
5 Researchers have identified predictors of SLE renal flares
5 CKD ups the risk for kidney and urothelial cancer

11 Kidney stone prevalence is rising among US women
13 Pruritus in CKD patients tied to cardiovascular events
MEDICAL DIRECTOR, UROLOGY
Robert G. Uzzo, MD, MBA, FACS
G. Willing “Wing” Pepper Chair in Cancer Research
Professor and Chairman Department of Surgery
Fox Chase Cancer Center
Temple University School of Medicine
Philadelphia
UROLOGISTS
Christopher S. Cooper, MD
Director, Pediatric Urology Children’s Hospital of Iowa Iowa City
R. John Honey, MD
Head, Division of Urology, Endourology/Kidney Stone Diseases
St. Michael’s Hospital University of Toronto
Stanton Honig, MD Department of Urology
Yale University School of Medicine New Haven, CT
J. Stephen Jones, MD Chief Executive Officer Inova Health System Falls Church, VA
Professor and Horvitz/Miller Distinguished Chair in Urologic Oncology (ret.) Cleveland Clinic Lerner College of Medicine Cleveland
Jaime Landman, MD Professor of Urology and Radiology Chairman, Department of Urology UC Irvine School of Medicine Orange, CA
James M. McKiernan, MD
John K. Lattimer Professor of Urology Chair, Department of Urology Director, Urologic Oncology Columbia University College of Physicians and Surgeons New York
Kenneth Pace, MD, MSc Assistant Professor, Division of Urology St. Michael’s Hospital University of Toronto Vancouver, Canada
Anthony J. Bleyer, MD, MS Professor of Internal Medicine/Nephrology
Wake Forest University School of Medicine Winston-Salem, NC
David S. Goldfarb, MD Professor, Department of Medicine Clinical Chief New York University Langone Medical Center Chief of Nephrology NY Harbor VA Medical Center
Kamyar Kalantar-Zadeh, MD, MPH, PhD
Professor of Medicine, Pediatrics, and Public Health, and Chief of Nephrology, at the University of California-Irvine School of Medicine Orange, CA
Adjunct Professor of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, CA
Csaba P. Kovesdy, MD Chief of Nephrology Memphis VA Medical Center
Fred Hatch Professor of Medicine University of Tennessee Health Science Center Memphis, TN
Edgar V. Lerma, MD
Clinical Associate Professor of Medicine Section of Nephrology Department of Medicine
University of Illinois at Chicago College of Medicine Chicago, IL
Allen Nissenson, MD
Emeritus Professor of Medicine
The David Geffen School of Medicine at UCLA Chief Medical Officer, DaVita Inc. Denver, CO
Rulan Parekh, MD, MS
Associate Professor of Pediatrics and Medicine University of Toronto
Robert Provenzano, MD
Associate Professor of Medicine Wayne State University School of Medicine Detroit, MI
Vice President of Medical Affairs, DaVita Healthcare Denver, CO
Editor Jody A. Charnow
Digital content editor Natasha Persaud
Production editor Kim Daigneau
Group creative director Jennifer Dvoretz
Senior production manager Krassi Varbanov
Vice president, sales operations and production Louise Morrin Boyle
National accounts manager William Canning
Vice president, content, medical communications Lauren Burke
Chief commercial officer James Burke, RPh
President, medical communications Michael Graziani
Chairman & CEO, Haymarket Media Inc. Lee Maniscalco
The science of kidney transplantation has taken a momentous step forward (see our cover story). In a medical first, surgeons at Massachusetts General Hospital in Boston successfully transplanted a genetically engineered pig kidney into a living patient. It apparently went well, as that patient, a 62-yearold man, was discharged from the hospital on April 3. It is an auspicious first step on the way to making kidney xenotransplantation routine. This would be a worthy goal.

As the time of this writing, more than 89,000 individuals in the United States are awaiting a kidney transplant, according to the Organ Procurement and Transplantation Network. It can take years for patients with kidney failure to receive an organ. Genetically engineered pig kidneys potentially could eliminate concerns about donor-recipient compatibility, a common obstacle in kidney transplantation. A number of obstacles need to be worked out before that point is reached. The Mass General experience and previous experiments with transplanting pig kidneys into braindead humans show that pig kidneys can be genetically engineered so they are not immediately rejected by human recipients, but whether this would be the case for all recipients remains unclear.
Vineeta Kumar, MD, professor of medicine and medical director of the Incompatible Solid Organ Transplant Program at the University of Alabama at Birmingham, explained in an email that the genetic engineering now being performed makes all pig kidneys blood type O (universal donor). “Therefore, all donor/ recipient pairs will be blood-group compatible.”
Tissue compatibility is harder, said Dr Kumar, who has been the lead nephrologist for kidney xenotransplantation into brain-dead individuals at UAB. “Unlike blood-group antigens where there are only 2 (A and B), there are many cell types and thousands of tissue antigens.” In addition, human have naturally occurring antibodies to tissues of other animal species gained during the neonatal period and into early childhood, and these do not seem to go away. In fact, some humans are presumed to have very high levels of antibodies to these pig antigens, and adding more human transgenes may not compensate for transplants performed in recipients with high levels of various anti-pig antibodies.
“The human immune system has evolved over millions of years, and the secret sauce has not all been coded and figured out yet, and thus despite genetic engineering, the pig-to-human transplant still requires immunosuppression to prevent rejection at present,” she said.
JODY A. CHARNOW Editor jody.charnow@haymarketmedia.com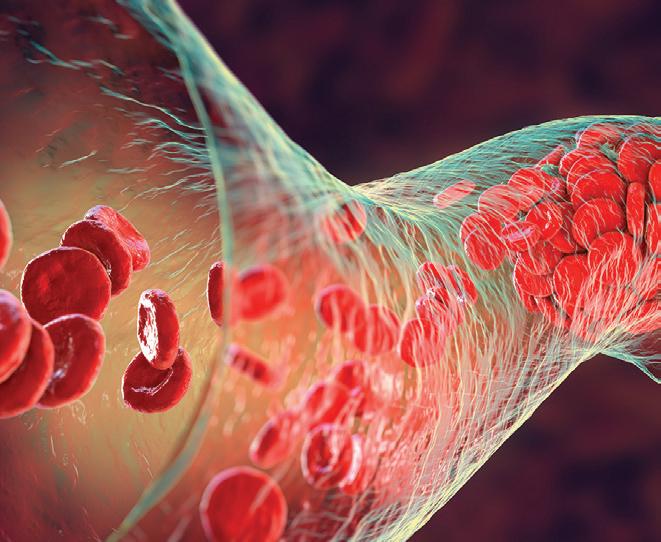


1 From the Editor A Historic First in Kidney Xenotransplantation
3 News in Brief Fewer dialysis technicians associated with worse outcomes
4 PPT May Lower Symptomatic Stone Risk A recent study showed a potential benefit of adhering to guideline-concordant pharmacotherapy.
4 Post-RN Kidney Cysts Ups Risk of Progressive CKD Progression risk is stronger when cysts are in the medulla rather than the cortex.
5 SLE Renal Flare Predictors Identified Risk factors included current/former renal involvement, low C3 levels, and high proteinuria.
5 LN Patients Have Inferior KT Outcomes
Patients who have lupus nephritis as a cause of ESKD have a 6% greater risk for graft failure.
5 Kidney, Urothelial Cancer Risk Higher in CKD Patients They have a 2.0- and 4.0-fold increased risk for kidney cancer and urothelial cancer, respectively, compared with patients without CKD.
6 VTE Risk Varies by Cancer Surgery Type The 1-year absolute risk was highest after bladder cancer surgery.
6 Novel BCG Strategy Proposed for NMIBC A clinical trial demonstrated that 2 sequential induction courses of intravesical BCG had an “excellent” response rate.
12 Post-RNU Adjuvant Chemotherapy Benefits in UTUC Cases Confirmed
Final results from the phase 3 POUT trial demonstrate improved disease-free survival compared with surveillance.
13 CKD Pruritus Common, Tied to CV Events
Patients extremely bothered by the condition, compared with those who were not bothered, had an 84% higher risk for cardiovascular events.
14 Renal Nutrition Update
Thyroid problems can adversely affect the kidney but are often underrecognized in patients with CKD.
15 Ethical Issues in Medicine
Physicians need to weigh various ethical considerations to determine whether accepting a gift is appropriate.
16 Practice Management
Physician groups are increasingly using artificial intelligence to improve patient care and practice efficiency.

Radical prostatectomy (RP) for prostate cancer can be performed in kidney transplant recipients (KTRs), but the complication rate is significantly higher in these patients, according to study findings published in European Urology.
Giancarlo Marra, MD, of AOU Città della Salute e della Scienza and the University of Turin in Italy, and colleagues compared outcomes between 102 KTRs and 408 non-transplant patients who underwent RP. Oncologic outcomes did not differ significantly between the groups, but the postoperative complication rate was 12% in the KTRs compared with 3% in the nontransplant group. The KTRs had a higher estimated blood loss (400 vs 200 mL), longer hospital stays (6.0 vs 3.5 days), longer times to catheter removal (11 vs 5 days), and a lower continence recovery rate (75% vs 89%).
A study of 848 patients with newly diagnosed ANCA-associated vasculitis (AAV) showed that 21% of them progressed to end-stage kidney disease (ESKD) after a median followup of 8 years, according to findings published
in Nephrology Dialysis Transplantation. The cumulative incidence of ESKD at 5 and 10 years was 16.9% and 22.5%, respectively, Kerstin Westman, MD, PhD, of Lund University in Sweden, and colleagues reported. Older age, lower baseline hemoglobin, and lower estimated glomerular filtration rate were factors significantly associated with an increased risk for ESKD. The ESKD group had a 2.8-fold increased risk for death compared with those who had preserved kidney function.
Elevated levels of C-reactive protein (CRP), a nonspecific inflammatory marker, are associated with an increased risk for kidney stones among US adults, Mei Yang, MD, of the People’s Hospital of Chongqing Liang Jiang New Area in Chongqing, China, and colleagues reported in BMC Nephrology Individuals in the highest CRP quartile had significant 64% increased odds of experiencing kidney stones compared with those in the lowest quartile after adjusting for age, sex, race, and other variables. The finding is based on an analysis of data from 11,033 participants in the National Health and Nutrition Examination Survey (2007-2010).
According to the US Renal Data System 2023 Annual Data Report, the adjusted mortality rates among adult patients on hemodialysis varies by race and ethnicity, with the highest rate among White patients. Shown here are the 2021 rates per 1000 person-years.
Understaffing of hemodialysis patient care technicians is associated with worse patient outcomes, including early mortality, more frequent hospitalization, and less transplantation, a new study finds.
In the study of 236,126 patients (mean age, 63.1 years; 61.9% with diabetes), the top vs bottom quartile of patient-to-dialysis technician ratio — reflecting dialysis facilities with the highest number of patients per technician — was significantly associated with a 7% higher rate of patient mortality, Laura C. Plantinga, PhD, of the University of California San Francisco, and colleagues reported in JAMA Network Open. Facilities in the top quartile of understaffing also had a 5%, 8%, and 15% higher rate of overall hospitalization, sepsis-related hospitalization, and vascular access-related hospitalization, respectively.
The top quartile facilities had a significant 8% lower rate of transplant waitlisting and a significant 20% lower rate of receiving a kidney transplant.
The top quartile facilities had 12.34 or more patients per technician and the bottom quartile had 8.60 or fewer patients per technician, the investigators reported.
Among kidney transplant recipients (KTRs) with kidney or ureteral stones, the rates of hospitalization with or without acute kidney injury (AKI) are “clinically significant,” investigators report.
In a study of 1436 KTRs with recent stone events recorded in the US Renal Data System (USRDS), 65% were diagnosed with stones as inpatients compared with 35% as outpatients, Calyani Ganesan, MD, MS, of Stanford University School of Medicine in Palo Alto, California, and colleagues reported in the Clinical Journal of the American Society of Nephrology. Within 90 days of outpatient diagnosis, 32% were hospitalized. AKI developed with hospitalization in 27% of recipients.
The median time to a stone event was 7.3 months after kidney transplant surgery. Kidney stones were more prevalent among men (59%) than women.
Within 90 days of a stone event in any setting, 13% of recipients were diagnosed with urinary tract infections, 67% of which were pyelonephritis.
Older donor age was significantly associated with a 14% increased risk of hospitalization in recipients who experienced an outpatient stone event, according to Dr Ganesan’s team.
Oral ondansetron increases the risk of sudden cardiac death (SCD) among patients receiving maintenance hemodialysis, a new study finds.
In a study of 119,254 patients in the 2012-2019 US Renal Data System, 64,978 patients (54.5%) initiated oral ondansetron, and 54,276 (45.5%) initiated a comparator oral antiemetic (promethazine, metoclopramide, or prochlorperazine).
The risk for SCD within 10 days was a significant 44% higher among patients receiving ondansetron rather than another antiemetic, Jennifer E. Flythe, MD, MPH, of the University of North Carolina Kidney Center at Chapel Hill, and colleagues reported in the Journal of the American Society of Nephrology. The number needed to harm was 1688 patients. The results applied to adults younger than 65 years and patients without heart failure.
Intravenous ondansetron is known to prolong the QT interval and carries a risk of torsades de pointes, but less is known about the oral formulation, the investigators pointed out.
Patients with urolithiasis may have a lower risk for symptomatic kidney stone events if they receive preventive pharmacological therapy (PPT), according to a retrospective cohort study.
In a study of 13,942 Medicare recipients with urolithiasis, of whom 31% were prescribed PPT, patients who adhered to treatment with thiazide diuretics for hypercalciuria and alkali for low urinary pH had a significant 26.4% and 19.6% lower risk for symptomatic stone events, respectively, compared with untreated patients. The reduced risk was driven mainly by emergency department (ED) visits. These patients had a significant 44.7% and 41.2% lower risk for ED visits for symptomatic stone events, respectively, compared with untreated patients.
Adherence to guideline-concordant PPT for hypocitraturia (alkali) and hyperuricosuria (uric acid-lowering medications) did not lower the risk for symptomatic stone events.
“As the lack of data on clinically relevant outcomes has dampened enthusiasm for PPT, these findings may inform patients and clinicians regarding the potential benefits of these treatments,” John M. Hollingsworth, MD, of NorthShore
University HealthSystem in Evanston, Illinois, and the University of Michigan Medical School in Ann Arbor, and colleagues concluded in a paper published in the American Journal of Kidney Diseases. Investigators categorized patients as adherent or nonadherent to guidelineconcordant PPT or untreated. The primary outcome was a composite measure indicating the first occurrence of a
Patients
hypercalciuria was 3.8% among those who adhered to guideline-concordant treatment compared with 6.9% for untreated individuals. For patients with low urine pH, the adjusted 2-year predicted probabilities of an ED visit were 4.3% and 7.3%, respectively.
Dr Hollingsworth’s team noted that their study provides a blueprint for additional needed research. “Although our
symptomatic stone event, defined as an ED visit or hospitalization for urolithiasis or stone-directed surgery.
The adjusted 2-year predicted probabilities of an ED visit for patients with
sensitivity analyses suggested a lower hazard of symptomatic stone events with combination therapy and increasing doses of a thiazide diuretic and alkali therapy, these associations were not
statistically significant, possibly due to limited statistical power.”
The authors acknowledged that the observational nature of the study limited interpretation of the findings. “While we used a rich set of patient-level controls, including baseline 24-hour urine collection data, we cannot exclude the possibility of unmeasured differences between the treated and untreated.” Patients who are prescribed PPT, however, would be expected to have higher levels of underlying disease severity compared with untreated patients, “such that our analysis would be biased towards showing a higher risk of symptomatic stone events in the treated,” the investigators noted. They also pointed to the potential for misclassification bias “whereby patients in the untreated group actually received an intervention.” The investigators noted, for example, that hydration and other dietary modifications are frequently used as first-line treatment for preventing stones, and some types of alkali preparations are available over the counter, “but we have no way of knowing whether either were prescribed.” ■
Among patients who undergo radical nephrectomy (RN) for kidney cancer, those who have cysts in the remaining kidney are at increased risk for progressive chronic kidney disease (CKD), investigators report. The risk of progression is stronger when cysts are in the medulla rather than the cortex.
In a study of 1195 patients who underwent RN for cancer, 50 patients experienced progressive CKD over a median 4.4 years of follow-up. Progression was defined as dialysis, kidney transplantation, a sustained estimated glomerular filtration rate (eGFR) less than 10 mL/min/1.73m 2 or a more than 40% decline in eGFR that was at least 5 mL/min/1.73 m2 below the postnephrectomy baseline. On preoperative contrast-enhanced CT, 37% of patients displayed at least 1 cyst sized at 5 mm or more. By location, 34% of patients had at least 1 cortical cyst, and 8.3% had at least 1 medullary cyst.
The overall number of cysts were significantly associated with a 13% to 18% increased risk of progressive CKD in adjusted analyses. The number of cortical cysts were significantly associated with a 26% increased risk only in unadjusted analyses.
Progression risk is stronger when cysts are in the medulla rather than the cortex.
The number of kidney cysts overall or cortical cysts did not meaningfully improve risk assessment for progressive CKD over standard clinical testing and evaluation, Andrew D. Rule, MD, of Mayo Clinic in Rochester, Minnesota, and colleagues reported in the American Journal of Kidney Diseases. Medullary cysts, however, continued to be significantly associated with a 54% to
61% increased risk of progressive CKD after adjustment for traditional CKD risk factors, baseline eGFR, nephron size, and nephrosclerosis, compared with the absence of cysts.
“Unlike cortical cysts, the risk of progressive CKD with medullary cysts showed no evidence of being via the same pathways as reduced eGFR, proteinuria, common CKD risk factors, larger nephron size, or nephrosclerosis,” Dr Rule’s team explained. Medullary cysts, which typically originate in the distal tubules or collecting ducts, might impair more nephrons than cortical cysts, which arise from the proximal tubule, they suggested.
Patients with 2 or more medullary cysts had a significant 4-fold increased risk of progressive CKD compared with patients without a medullary cyst.
The investigators suggested that medullary cysts may have a genetic origin, noting that a COL4A3/4/5 or ALG8
mutation can cause cysts. Genetic testing was not performed, however. The study excluded patients with evidence of autosomal dominant polycystic kidney disease.
According to Dr Rule’s team, “these analyses suggest that presence of a few cortical cysts should not be considered an important independent prognostic factor for progressive CKD when considering a nephrectomy. However, this is not the case for medullary cysts.”
The authors acknowledged a number of study limitations. For example, they noted that RN “may accelerate the risk of progressive CKD due to hyperfiltration in the remaining kidney, and this may potentially interact with pathways of kidney cyst formation.”
Further, they pointed out that their study cohort was predominantly White, “and findings may differ with more diverse race and ethnic groups.” ■
Investigators have identified characteristics that signal impending renal flares among patients with systemic lupus erythematosus (SLE).
In a post-hoc analysis of 4 phase 3 clinical trials of belimumab involving 3225 patients with SLE, 192 patients experienced at least 1 renal flare, with the first occurring after a median 197 days.
In the overall cohort, current/former renal involvement was significantly associated with a 15.4-fold increased risk of renal flare. Low C3 levels and high proteinuria at baseline also were significantly associated with a 2.9and 1.6-fold increased risk, respectively, Ioannis Parodis, MD, PhD, of Karolinska University Hospital in Stockholm, Sweden, and colleagues reported in Rheumatology. The presence of anti-double stranded DNA also was associated with renal flares, but the
association was attenuated after multivariable adjustment.
The investigators looked for additional prognosticators among the groups treated with belimumab vs placebo on top of standard therapy. Anti-Sm was significantly associated with a 3.7-fold increased risk for renal flares in the placebo group only, which
Low serum albumin levels were significantly associated with a 10% lower risk of renal flare.
coincides with results from a previous study. Anti-ribosomal P positivity was significantly associated with a 2.8-fold increased risk of renal flares in the belimumab group only.
Patients with nondialysis-dependent chronic kidney disease (CKD) have increased risks for kidney cancer and urothelial cancers, according to a systematic review and meta-analysis of observational data.
“Even moderate CKD is associated with elevated risk of kidney cancer and urothelial carcinoma,” Stella K. Kang, MD, of NYU Grossman School of Medicine in New York, and colleagues concluded in a paper published in Nephrology Dialysis Transplantation. “Providers should consider these elevated risks when managing individuals with CKD, particularly when considering evaluation for the presence and etiology of hematuria.”
In an adjusted analysis of 6 mostly good-quality cohort studies including 8,617,563 individuals, patients with CKD had a significant 2.0-fold increased risk of kidney cancer and a 4.0-fold increased risk of urothelial cancer compared with those without CKD. By CKD severity, stage 3 CKD was significantly associated with a 1.9-fold increased risk of kidney cancer and a 1.4-fold increased risk of urothelial carcinoma. Stage 4-5 CKD was significantly
associated with a 2.3-fold increased risk of kidney cancer and a 1.2-fold increased risk of urothelial carcinoma.
The incidence rate ratio for kidney cancer was 3.1- and 3.3-fold at CKD stage 3 and 4-5, respectively. The incidence rate ratio for urothelial cancer was 4.4- and 3.1-fold at CKD stage 3 and 4-5, respectively.
“To our knowledge, no prior systematic review and meta-analysis has provided summary risk estimates for kidney or urothelial malignancies in persons with non-dialyzed CKD,” Dr Kang’s team wrote. “Restricting our analysis to exclude dialyzed persons and kidney transplant recipients reduced confounding by the associated immunocompromised state when examining CKD and risks of incident urinary tract cancers.”
They concluded that the “numerous healthcare providers across a wide range of specialties who encounter hematuria in patients with CKD may consider these risk estimates for malignancy in initial evaluation or surveillance after detection of microhematuria, and with particular vigilance in cases of persistent or worsening hematuria.” ■
“Even though further investigation is needed regarding the presence of anti-ribosomal P protein antibodies in patients with SLE in relation to kidney involvement, our findings point towards predictive properties for these autoantibodies, which may prove useful in monitoring renal flare development, especially in patients starting belimumab therapy,” Dr Parodis’ team wrote. Low serum albumin levels were significantly associated with a 10% lower risk of renal flare.
Patients with current or former renal involvement had a more than 9-fold increased risk for a new renal flare. Flare was more likely among younger and Asian patients. Renal flares were defined as a proteinuria rise to more than 1 g/day from a baseline value of less than 0.2 g/day; a rise to more than 2 g/day if the baseline value was 0.21.0 g/day; or a doubling if the baseline
Patients with lupus nephritis (LN)related end-stage kidney disease (ESKD) are more likely to be evaluated for kidney transplantation, but their graft and patient survival appear worse compared with patients who have other causes of kidney failure, according to new research.
Among 192,318 patients with ESKD from the eastern United States, 0.4% had LN-ESKD. The median time from ESKD diagnosis to transplant referral was similar between the LN and nonLN groups: median 2.9 vs 2.6 months. Approximately 58% of patients with LN were referred, and two-thirds of these patients started transplant evaluation. In adjusted analyses, patients with LN had a 13% higher likelihood of transplant evaluation, Laura McPherson, MPH, of Emory University in Atlanta, Georgia, and colleagues reported in Lupus. “While providers may no longer be delaying the early steps in the kidney transplantation process among this patient population, there is still room for improvement in the rates of preemptive referral,” the investigators wrote.
value was more than 1 g/day. Other criteria included a serum creatinine rise of 20% or more or 0.3 mg/dL, along with proteinuria, hematuria, or red blood cell casts. The third definition was new hematuria of glomerular origin, along with proteinuria or red blood cell casts. Dr Parodis’ team noted that C3 was more reflective of renal activity than C4. In a separate study published in Kidney International Reports , Lubka T. Roumenina, PhD, of Cordeliers Research Center, INSERM UMRS in Paris, France, and colleagues also found that autoantibodies to C3 were more strongly associated with disease activity and future flares in a cohort of 85 patients with established lupus nephritis. C3 antibodies were associated with hypocomplementemia, anti-dsDNA, class 4 lupus nephritis, and active disease according to British Isles Lupus Assessment Group renal score. ■
Qichun Yin, MD, and colleagues from HuZhou University in Huzhou City, China, performed a separate systematic review and meta-analysis of 15 studies involving 6456 kidney transplant recipients with LN and 168,529 patients without LN as their cause of ESKD. The LN group had a significant 6% greater risk of graft failure and a significant 15% greater risk of death compared with patients with ESKD due to other causes, the investigators reported in Renal Failure The systemic nature of LN and comorbidity burden may make the LN group more prone to transplant complications and earlier death, the investigators noted. The “complex immune milieu” may lead to graft inflammation and
Patients who have lupus nephritis as a cause of ESKD have a 6% greater risk for graft failure.
dysfunction. “Living donor transplantation may offer a better outcome, and healthcare providers should consider this option when possible,” they wrote. The researchers urged multidisciplinary care of patients with lupus nephritis involving rheumatologists, nephrologists, and transplant specialists to address systemic autoimmune manifestations and transplant-related factors. ■
The 1-year absolute risk was highest after bladder cancer surgery, according to investigators
Investigators have provided precise estimates of excess venous thromboembolism (VTE) risk after major cancer surgery by cancer type.
Using multiple Swedish nationwide registers such as the national cancer register, they determined the risk for VTE (pulmonary embolism or deep vein thrombosis) in 432,218 patients who underwent major surgery for cancer of the urinary bladder, breast, colon or rectum, gynecologic organs, kidney or upper urinary tract urothelial cancer, lung, prostate, or stomach or esophagus from 1987 to 2016. Each patient with cancer was matched to 10 cancer-free adults.
The 1-year absolute risk of pulmonary embolism and deep vein thrombosis was lowest after prostate cancer surgery and highest after bladder cancer surgery, Johan Björklund, MD, PhD, of Karolinska Institutet, in Stockholm, Sweden, and colleagues reported in JAMA Network Open
For pulmonary embolism, the 1-year absolute excess risks were 2.69% for
bladder cancer, 0.59% for breast cancer, 1.57% for colorectal cancer, 1.32% for gynecologic organ cancer, 1.38% for kidney and upper urinary tract cancer, 2.61% for lung cancer, 2.13% for gastroesophageal cancer, and 0.57% for prostate cancer.
For deep vein thrombosis, the 1-year absolute excess risks were 4.67% for bladder cancer, 1.36% for breast cancer, 2.15% for colorectal cancer, 2.02% for gynecologic organ cancer, 2.14% for kidney and upper tract urinary cancer (UTUC), 1.40% for lung cancer, and 2.19% for gastroesophageal cancer. VTE risk was highest just after surgery, then declined and held steady at approximately 90 to 120 days, the investigators reported. The highest VTE risk was observed after lung cancer surgery: a significant 25.7-, 18.6-, and 8.9-fold higher at 30, 90, and 365 days, respectively, for patients compared with cancer-free adults. After bladder cancer surgery, VTE risk was a significant 16.3-,
9.6-, and 5.2-fold higher for patients at 30, 90, and 365 days, respectively. For kidney cancer and UTUC, VTE risk was significantly elevated 12.2-, 4.2, and 3.3-fold at the respective time periods, according to the investigators. For prostate cancer, VTE risk was significantly
A novel strategy for using bacillus Calmette-Guérin (BCG) for high-risk nonmuscle-invasive bladder cancer (NMIBC) may provide a workaround that addresses an ongoing shortage of the therapy, according to a recent report in JAMA Oncology
The 5-year outcomes from a prospective phase 2 clinical trial found that 2 sequential induction courses of intravesical BCG (12 instillations) “demonstrated an excellent response rate,” according to corresponding author Harry W. Herr, MD, of Memorial Sloan Kettering Cancer Center in New York, and colleagues.
Of 81 patients who consented to participate in the trial, 75 remained evaluable for long-term follow-up analysis. At a median follow-up of 4.4 years, high-grade recurrence developed in 21 patients, for a 5-year recurrence-free survival rate of 69%. The 5-year cancerspecific survival rate was 97%.
Using 2 induction courses decreased the amount of BCG per patient from 27 vials to 12, according to the investigators.
“Using 12 instillations of BCG was a viable alternative to standard induction with 3 years of maintenance therapy, which may provide an alternative
treatment option during the BCG shortage,” the authors wrote.
BCG has been in short supply globally since 2011, they noted.
The investigators acknowledged study limitations. In addition to being conducted at a single-institution, it had a small sample size and a single study arm, “which precludes direct comparisons between 2 induction courses and induction plus maintenance.” They added, however, that based on historical rates of 6-month complete response and 5-year recurrence-free survival, these results appear to have similar outcomes compared with standard therapy. ■
Cancer diagnoses fell substantially during the first 10 months of the COVID-19 pandemic in the United States, with prostate cancer accounting for the largest number of potentially missed cancers, according to a recent study.
An estimated 134,395 cancer cases went undiagnosed from March 1 through December 31, 2020, corresponding
author Krystle A. Lang Kuhs, PhD, MPH, of the University of Kentucky in Lexington, and colleagues reported in JAMA Oncology. Observed rates of cancer at all sites were 13.0% lower than expected based on pre-pandemic rates, according to investigators.
“The findings from this analysis can inform the US health care system as
elevated 13.9- and 1.7-fold only at 30 and 90 days, respectively.
Individualized Evaluation Needed
“The results highlight the need for individualized venous thromboembolism risk evaluation and prophylaxis regimens for patients undergoing surgery for different cancers,” Dr Björklund’s team concluded. Key decisions include timing, duration, dosage, and choice of prophylaxis.
Both surgery and systemic treatments, such as chemotherapy, may contribute to thromboembolism, Dr Björklund’s team pointed out. The study lacked information on nonsurgical treatments, precluding analyses. They noted that pelvic lymph node dissections have been associated with VTE, which may explain why prostate, bladder, and gynecologic cancer surgery have higher peak rates than colorectal cancer surgery. What’s clear is that VTE risk persists beyond in-hospital or 28-day extended thromboprophylaxis. ■
The Food and Drug Administration (FDA) has approved once-daily aprocitentan (Tryvio, Idorsia Pharmaceuticals US) for the treatment of hypertension in combination with other antihypertensive drugs to lower blood pressure (BP) in adult patients who are not adequately controlled on other drugs.
The approval was based on data from the phase 3 PRECISION study (ClinicalTrials. gov Identifier: NCT03541174), which evaluated the safety and efficacy of aprocitentan, an endothelin receptor antagonist, in adults with uncontrolled BP (systolic BP 40 mmHg or higher) despite at least 3 background antihypertensive medications.
decisions are made to recover the deficit through focused cancer screening and detection,” the authors wrote.
Dr Lang Kuhs and colleagues pointed out that “a decline in new cancer diagnoses in 2020 does not indicate that cancer occurrence in the US decreased, but rather that new cancers were undetected.” ■
The most frequently reported adverse reactions to aprocitentan during a 4-week double-blind placebo-controlled treatment period in the PRECISION trial were edema/fluid retention and anemia. The drug, which is supplied as a 12.5 mg tablet, is expected to be available in second half of 2024. ■
continued from page 1
individuals. Investigators reported no hyperacute antibody-mediated rejection and comparable physiologic function of the pig kidneys.
“This first-ever transplantation of a genetically modified pig kidney into a live human is an enormously important step in the progress towards human xenotransplantation,” said Vineeta Kumar, MD, professor of medicine and medical director of UAB’s Incompatible Solid Organ Transplant Program, who has been the lead nephrologist for the experiments with xeno kidneys and brain-dead humans at UAB. “This opens the door to ask the next set of crucial questions towards making human xenotransplantation a reality.”
What remains to be learned next is the immediate and longer-term
continued from page 1
groups among patients with favorable intermediate- and low-risk disease.
In the other study, researchers analyzed 2004-2017 SEER data from 5778 men with prostate cancer and clinically positive nodal disease (cN1). Of these, 4739 (82%) underwent RP and 1039 (18%) had RT. The 10-year CSM rate was 32.2% in the RT group compared with 17.1% in the RP group, Firas Abdollah, MD, also from the Vattikuti Urology Institute, reported. Compared with the RP group, the RT arm had a significant 86% increased risk for CSM even after adjusting for known confounders, including cancer stage and
remission, SLE flares
continued from page 1
in Kidney International Reports On multivariable analysis, arterial hypertension was significantly associated with a 31.1% decreased probability of achieving sustained remission. Hydroxychloroquine use was significantly associated with a 1.4-fold increased probability of remission, confirming guideline recommendations.
For each 1-year increase in age at LN diagnostic biopsy, the probability of sustained clinical remission significantly increased 1.7%, supporting the “need for a closer monitoring of young patients from the beginning of the disease.”
postoperative course with regard to rejection of the kidney, infection risks with the novel immunosuppression, and physiologic function of the pig kidneys in humans. Pig kidneys have some fundamental differences from human kidneys and recipients of these modified pig kidneys will require
transplant at Massachusetts General and prior transplants of pig kidneys into nonhuman primates and braindead individuals will form the basis of the first pig-to-human kidney transplant clinical trials, Dr Kumar said. “Selecting the appropriate patients for these first human clinical trials,
‘This opens the door to ask the next set of crucial questions towards making human xenotransplantation a reality.’
careful monitoring and management, said Dr Kumar, who co-chaired a recent session on xenotransplantation that was part of the National Kidney Foundation’s Patient-Focused Drug Development Meeting on Kidney Xenotransplantation.
The knowledge and experience gained from this first in human xeno kidney
defining the research parameters, and successfully conducting the trials will remain vital in genetically edited pig xenotransplantation to truly realize all the benefits as we enter a new era in kidney transplantation and will require the medical and patient community to work together collaboratively to make this a reality,” Dr Kumar said.
“Moving forward, if this clinical approach is successful, it will need to be applied to more kidney disease patients before we can say that dialysis will be obsolete,” said Roslyn B. Mannon, MD, Chair of the American Society of Nephrology’s Policy and Advocacy Committee. “But it is an important step in that direction, and kudos to the team but importantly, [gratitude] to the patient who took a pioneering step for the field.”
Dr Mannon noted that the posttransplant therapy used is unique in that it included both costimulatory blockade as well as infusion therapy aimed at complement inhibition.
She pointed out that the risks for infection and antibody- or cell-mediated rejection will be important key barriers to overcome over the next few months. ■
Radical prostatectomy is significantly associated with lower cancer-specific mortality (CSM) compared with radiation therapy for patients with clinical nodal disease and unfavorable intermediateand high-risk disease, according to study results presented at EAU24. Shown here are the 10-year CSM rates.
grade. The researchers found no significant difference in 10-year OCM between the treatment arms.
In a paper published in The Journal of Urology in 2022, investigators reported on a study showing that RP was significantly associated with a
Among patients who achieved sustained clinical remission, 55.3% experienced a lupus flare after a median 3.6 years, the investigators reported. Flare risk progressively decreased from 10% to 5% and 2% in patients with less than 5 years of clinical remission, 5 to 10 years, and more than 10 years, respectively. The probability that remission would persist to 15 years was 38%.
Patients who achieved sustained clinical remission had a significant 82% lower risk for impaired kidney function to an eGFR less than 60 mL/min/1.73m2 compared with patients who never achieved remission, the investigators reported. As the years in remission increased, the probability of impaired kidney function decreased. Approximately one-third of patients maintained long-lasting clinical
32% lower CSM risk compared with external beam radiation therapy (EBRT) in men with high-risk prostate cancer as defined by National Comprehensive Cancer Network criteria. The 5-year CSM rate was 2.3% with RP compared with 4.1% with EBRT. The
remission up to 13.2 years after induction therapy.
Withdrawal of glucocorticoids (26.1% vs 61.7%) and immunosuppressive drugs (19.0% vs 42.6%) was significantly
Arterial hypertension is associated with a lower likelihood of sustained remission, study finds.
less frequent in patients who experienced flares compared with patients who maintained clinical remission.
At last follow-up, 57 patients (18.8%) had impaired kidney function. Achieving remission and sustaining it long-term were significantly associated with a 72% and 17% decreased risk
■ Unfavorableintermediate risk
■ High risk ■ Clinical nodal disease
study included 24,407 patients: 9823 (40%) who underwent RP and 14,584 (60%) who had EBRT. The researchers assessed CSM after 1:1 propensity score matching between the treatment arms according to age, biopsy Gleason score, PSA, and clinical T and N stages. ■
of impaired kidney function (eGFR less than 60 mL/min/1.73m2). Impaired kidney function was 3.4-fold more likely with nephritic vs proteinuric flare.
“Our results highlight the value not only of achieving but also of maintaining longer [sustained clinical remission] to avoid kidney damage,” Dr Moroni’s team wrote.
The authors pointed out some study limitations. As the data were collected from a real-world LN cohort, treatment, time to data collection, and duration of followup were not standardized, and the indication to discontinue glucocorticoids and immunosuppressants was based on clinical judgment, they wrote. In addition, most patients were White, thus limiting the generalizability of the results. ■
Focal therapy such as high-intensity focused ultrasound (HIFU) for localized prostate cancer results in treatment outcomes comparable to those of radical prostatectomy, according to findings from separate studies presented at the European Association of Urology 2024 Congress in Paris, France.
One study was the HIFI trial, the first prospective multicenter study comparing HIFU to RP as first-line treatment for prostate cancer. The trial included 1967 consecutive HIFU and 1361 RP patients with low- or intermediaterisk prostate cancer from 42 centers. Investigators followed up patients for 30 months.
The primary oncologic endpoint was survival without salvage treatment (SWST) for significant prostate cancer after post-HIFU biopsies or biological recurrence of significantly positive margins after RP.
HIFU was associated with a lower risk for requiring salvage treatment vs RP.
At 30 months, the SWST rate was 89.6% in the HIFU group compared with 86.2% of the RP arm, with the HIFU-treated patients having a significant 24% lower risk for salvage treatment, Guillaume Ploussard, MD, PhD, of La Croix du Sud Clinic, QuintFonsegrives, France, and colleagues reported. After adjusting for age, body mass index, and other variables, the HIFU group had a significant 29% lower risk for salvage treatment compared with the RP group.
The cancer-specific survival rate was 100% in both study arms. The overall survival rate was 97.7% and 99.5% in the HIFU and RP arms, respectively, at 30 months, with no significant difference between the groups after adjusting for age, which was significantly higher in the HIFU group (median 74.7 vs 65.1 years).
After HIFU, patients had a median PSA nadir of 0.25 ng/mL and a positive biopsy rate of 12.5%. After RP, patient had a positive surgical margin rate of 26% and median PSA level of 0.01 ng/mL.
Dr Ploussard concluded that HIFU was not inferior to RP with respect to salvage therapy-free survival at the 30month follow-up.
In a separate presentation, Eduard Baco, MD, PhD, of Oslo University Hospital in Norway, reported on a
randomized trial showing that focal ablation (HIFU or transurethral ultrasound ablation) was not inferior to RP with regard to treatment failure.
Investigators randomly assigned 213 patients to receive focal ablation (107 patients) or RP (106 patients). After randomization, 6 patients declined
treatment, leaving 207 patients for a per-protocol analysis (131 in the focal ablation group and 76 in the RP group). That analysis showed that the proportion of treatment failures at 2 years was 6.1% in the focal ablation group and 7.9% in the RP group, a nonsignificant difference.
For the focal ablation group, Dr Baco’s team defined treatment failure as the need for secondary RP or radiation therapy due to the presence of highrisk prostate cancer ineligible for repeat focal ablation. For the RP group, they defined treatment failure as a posttreatment PSA level higher than 0.2 ng/mL. ■
Positive surgical margins (PSMs) following partial nephrectomy, but not radical nephrectomy, for renal cell carcinoma (RCC) independently predict an increased risk for disease recurrence, according to study findings presented at the European Association of Urology 2024 congress in Paris.
The multi-institutional retrospective study included 5827 patients who underwent either partial nephrectomy (PN) or radical nephrectomy (RN) and had a median follow-up of 45 months. Of these, 251 (4.3%) had PSM. Compared with patients without PSMs, those with PSMs were significantly more likely to have under-
gone PN than RN (75.3% vs 51.9%), Cesare Saitta, MD, of UC San Diego Health System in California, and colleagues reported. On multivariable analysis, PSMs after PN were significantly associated with a 75% increased risk for recurrence. PSMs after RN were not significantly associated with recurrence. Other signifi-
cant risk factors for recurrence following PN included tumor necrosis, increasing tumor size, and high-grade disease. PSMs after RN were significantly associated with a 5.3-fold increased risk for cancer-specific mortality (CSM) compared with no PSMs. PSM after PN was not significantly associated with CSM. ■
Men with primary organic erectile dysfunction (ED) are less likely than those with primary psychogenic ED to adhere to treatment with phosphodiesterase type 5 (PDE5) inhibitors, according to study findings presented at the 2024 congress of the European Association of Urology in Paris.
Christian Corsini, MD, of IRCCS Ospedale San Raffaele in Milan, Italy, and colleagues studied 1252 men diagnosed with ED: 1040 (83%) with primary organic ED and 212 (17%) with primary psychogenic ED. Men in the primary organic group had a significant 81% increased risk for nonadherence to PDE5
inhibitor treatment compared with those in the primary psychogenic group. The primary psychogenic group was significantly younger than the primary organic group (44.6 vs 53.9 years). At baseline, compared with the primary psychogenic group, the primary organic group had significantly
worse International Index of Erectile Function (IIEF) scores for both sexual desire and orgasmic function. The investigators found no significant differences between the groups with respect to the IIEF-erectile function, IIEF-intercourse satisfaction, and IIEFoverall satisfaction domains. ■
Kidney stone prevalence is rising among women in the United States, investigators reported at the 2024 congress of the European Association of Urology in Paris.
Investigators identified the trend using 2007-2020 data from 38,329 individuals aged 20 years or older who
participated in the National Health and Nutrition Examination Survey (NHANES). The weighted prevalence of kidney stones rose from 8.9% in 2007-2008 to 9.9% in 2017-2020, a difference that was not significant, Naeem Bhojani, MD, of the University of Montreal in Canada, reported on be-
half of his team. The prevalence of kidney stone among women, however, increased significantly from 6.5% to 9.1% during the same period. The prevalence remained stable among men (11.5% in 2007-2008 and 10.8% in 2017-2020).
The prevalence increased slightly among racial and ethnic groups, but
not significantly. For example, from 2007-2008 to 2017-2020, the prevalence rose from 10.2% to 11.1% among Whites, 4.3% to 5.8% among Blacks, and 5.7% to 7.8% among Mexican-Americans.
“While the overall lifetime prevalence of kidney stones in American adults has not changed significantly over the last decade, there is a concerning trend in kidney stone disease among females that warrants further investigation,” the investigators concluded. ■
Testosterone deficiency is associated with an increased likelihood of nocturia, especially among patients aged 60 years or older and those with cardiovascular disease, according to data presented at the European Association of Urology 2024 congress in Paris.
Overall, testosterone deficiency was significantly associated with 21.1% increased odds of nocturia compared with no deficiency, Sungjin Kim, MD, of Hallym University Kangnam Sacred Heart Hospital in Seoul, South Korea, and colleagues reported. Testosterone deficiency in men with cardiovascular disease, hypertension, and dyslipidemia was significantly associated with 42.9%, 28.5%, and 28.8% increased odds of nocturia, respectively.
Among men aged 60 years or older, testosterone deficiency was significantly associated with 36.8% increased odds of nocturia. The investigators found no significant association between testosterone deficiency and nocturia among men younger than 60 years.
The cross-sectional study included 6137 participants in the National Health and Nutrition Examination Survey (NHANES; 2011-2016 data): 1709 with testosterone deficiency and a control arm of 4428 patients without the condition. Of the 6137 participants, 1730 (28.2%) experienced nocturia (2 or more urinations per night). The deficiency group was significantly older than the control arm (mean 52.3 vs 47.5 years) and had a significantly higher proportion of patients with cardiovascular disease (23.1% vs 15.0%), hypertension (42.4% vs 28.0%), and dyslipidemia (44.9% vs 30.8%). ■
Final results from the phase 3 POUT trial further support the use of adjuvant chemotherapy for patients with upper tract urothelial carcinoma (UTUC), according to a recent report in the Journal of Clinical Oncology Adjuvant chemotherapy given after radical nephroureterectomy (RNU) was significantly associated with improved disease-free survival (DFS) compared
muscle-invasive or lymph node-positive nonmetastatic UTUC. Following RNU, investigators randomly assigned 132 patients to receive platinum-based chemotherapy and 129 to undergo surveillance. DFS was the primary outcome measure.
The chemotherapy regimen consisted of four 21-day cycles of gemcitabine and either cisplatin or carboplatin.
Adjuvant chemotherapy after UTUC surgery significantly improved 5-year disease-free survival. The 5-year overall survival rate was higher with vs without adjuvant chemotherapy, but the difference was not statistically significant after adjusting for multiple variables.
with surveillance, Alison Jane Birtle, MD, MBBS, of Royal Preston Hospital in Preston, UK, and colleagues concluded POUT was a randomized, open-label trial that included 261 patients with
At a median follow-up of 65 months, 50 and 67 DFS events had occurred in the chemotherapy and surveillance groups, respectively. The 5-year DFS rate was significantly higher in the chemotherapy
group compared with the surveillance arm (62% vs 45%). Patients in the chemotherapy group had a restricted mean survival time (RMST) that was 18 months longer than in the surveillance arm.
The chemotherapy and surveillance groups had 46 and 60 deaths, respectively. The 5-year overall survival (OS) rate was 66% vs 57%, respectively. On multivariable analysis, OS did not differ significantly between the chemotherapy and surveillance arms. The RMST, however, was a significant 11 months longer in the chemotherapy group.
Treatment effects were consistent across disease stage and chemotherapy regimens. Toxicities were similar to those previously reported, with no clinically relevant differences in quality of life (QoL) between study arms.
“In the current analysis, data on both clinician-report toxicity and patientreported QoL provide reassurance that there are no important long-term adverse impacts, which might offset the benefits,” the investigators wrote.
The authors concluded that “updated outcomes from the POUT trial added further support to the value of adjuvant systemic gemcitabine:platinum combination chemotherapy after nephroureterectomy for UTUC.” ■
High levels of bone turnover biomarkers predict shorter overall survival in men with newly diagnosed metastatic hormone-sensitive prostate cancer (mHSPC), not just castration-resistant disease, a new study finds.
Investigators assessed biomarkers of bone formation (C-terminal collagen propeptide [CICP] and bone alkaline phosphatase [BAP]) and bone resorption (C-telopeptide [CTx] and pyridinoline [PYD]) at baseline in men in the SWOG S1216 trial. Using a training set of 316 patients, the investigators used models to determine prognostic thresholds for each biomarker and validated these thresholds in 633 patients.
Men with high vs low BAP had a significant 43% increased risk for allcause mortality, Primo N. Lara Jr., MD, of the University of California Davis Comprehensive Cancer Center in Sacramento, and colleagues reported in European Urology. Median overall
survival was 3.3 vs 6.8 years. High vs low CICP was significantly associated with a 92% increased risk of all-cause mortality. Median overall survival was 2.4 vs 7.6 years.
High vs low CTx was significantly associated with a 37% increased risk of all-cause mortality. Median overall
Men with high vs low BAP had a 43% increased risk for all-cause mortality.
survival was 4.0 vs 7.7 years. High vs low PYD was significantly associated with a 77% increased risk of all-cause mortality. Median overall survival was 3.4 vs 8.2 years.
“Elevated levels of each of the four bone biomarkers — using cut-points derived from a training set and subsequently tested in a validation set —
Although low testosterone levels are associated with increased risks for prediabetes and type 2 diabetes in men, testosterone replacement therapy (TRT) will not reduce these risks, according to new research.
Investigators conducted a substudy of the TRAVERSE trial (Testosterone Replacement Therapy for Assessment of Long-Term Vascular Events and Efficacy Response in Hypogonadal Men). Of 5204 men aged 45 to 80 years with hypogonadism, 1175 had prediabetes and 3880 had diabetes. In the prediabetes group, mean hemoglobin A1c level was 5.8% at baseline.
Progression to diabetes did not differ significantly between men receiving testosterone gel vs placebo at 6 months (0.7% vs 1.4%), 12 months (7.8% vs 10.7%), 24 months (10.1% vs 14.6%), 36 months (12.8% vs 15.8%), or 48 months (13.4% vs 15.7%). Further, hemoglobin A1c, glycemic remission, and fasting glucose reduction were comparable, Shalender Bhasin, MB, BS, of Brigham and Women’s Hospital, Harvard Medical School in Boston, Massachusetts, and colleagues reported in JAMA Internal Medicine.
showed statistically significant association with worse survival outcomes, independent of traditional clinical risk factors,” Dr Lara’s team wrote.
The investigators distinguished low-, intermediate-, and high-risk groups based on a combination of 2 of these bone biomarkers. Median overall survival was 8.2, 5.1, and 2.1 years, respectively. Median all-cause mortality was significantly increased 1.4- and 2.2fold for the intermediate- and highrisk groups, respectively, compared with the low-risk group, according to Dr Lara and colleagues.
The low-risk group had a CTx less than 0.6 ng/mL and CICP less than 161 ng/mL. The intermediate-risk group had a CTx less than 0.6 ng/mL and a CICP of 161 or greater or a CTx of 0.6 ng/mL or more and a CICP less than 286 ng/mL. The high-risk group had a CTx of 0.6 ng/mL or more and a CICP of more than 286 ng/mL. ■
“Testosterone replacement therapy did not improve glycemic control in men with hypogonadism and prediabetes or diabetes,” Dr Bhasin’s team concluded. Previous research has found that testosterone therapy does not increase the risk for cardiovascular events, fracture, or prostate cancer. It may improve anemia, but not cognitive function. TRT is associated with increased risks of venous thromboembolism, polycythemia, atrial fibrillation, and acute kidney injury.
In an accompanying editorial, Lona Mody, MD, MSc, and Kenneth E. Covinsky, MD, MPh, of the University of Michigan, Ann Arbor, commented: “Thus, the only indication for TRT in men with hypogonadism remains treatment of bothersome symptoms of hypogonadism, generally sexual dysfunction. Further, results of this study suggests that TRT will not benefit glycemic control in men without hypogonadism, despite the inappropriately high rates of use in this group.” ■
Real-world study demonstrates 51% lower death risk vs TKI therapy
BY JOHN SCHIESZERFirst-line immuno-oncology (IO)-based regimens and intensive focal therapies are associated with significantly prolonged overall survival (OS) among patients with brain metastases from renal cell carcinoma (RCC), new findings suggest.
In a real-world study, median OS was 32.7 months for patients who received first-line IO-based combination regimens compared with 20.6 months for those who received tyrosine kinase inhibitor (TKI) monotherapy, Kosuke Takemura, MD, of the Tom Baker Cancer Centre at the University of Calgary in Alberta, Canada, and colleagues reported in European Urology Patients who received intensive focal therapies with stereotactic radiotherapy or neurosurgery have significantly longer OS compared with those who receive whole-brain radiotherapy alone or no focal therapy (31.4 vs 16.5 months).
On multivariable analysis, IO-based regimens were significantly associated with a 51% reduced risk for death compared with TKI regimens. Stereotactic radiotherapy or neurosurgery was significantly associated with a 52% lower risk for death compared with wholebrain radiotherapy alone or no focal therapy.
pembrolizumab/axitinib, avelumab/ axitinib, nivolumab/cabozantinib, pembrolizumab/lenvatinib, or atezolizumab/bevacizumab) or TKI monotherapy (sunitinib or pazopanib) and had data available on brain metastases before initiation of systemic therapy. Of the 389 patients, 99 (25%) received IO-based regimens.
Outcome by Risk Group
IMDC favorable- or intermediate-risk disease was significantly associated with a 60% lower risk for death compared with poor-risk disease.
The patients with brain metastases were more likely to be younger (63 vs 65 years) and to have metastases to the lung (80% vs 67%), spleen (2.0% vs 0.8%), and multiple sites (96% vs 80%). The group with brain metastases had a shorter median OS compared with patients without brain metastases (22.8 vs 34.7 months).
The study was limited by its retrospective design and absence of data on PD-L1 expression or intracranial/ extracranial disease status.
“This is a very important study and highlights that this patient population should be considered as the focus of future innovative clinical trials, and there definitely should not be an exclusion simply because they are not anticipated to have a favorable outcome,” said genitourinary surgical
Of 389 patients with RCC brain metastases, 99 (25%) received immuno-oncology-based regimens for first-line treatment.
The findings are from an analysis of data from the International Metastatic Renal Cell Carcinoma Database Consortium (IMDC). Of 4799 patients with metastatic RCC, 389 (8.1%) had brain metastases at initiation of systemic therapy. The goal of the study was to define the clinical effectiveness of modern multimodal cancer treatment for patients with brain metastases from RCC. The investigators did not investigate the causal pathways between treatments and outcomes.
The study included patients who received first-line IO-based combination therapy (nivolumab/ipilimumab,
oncologist Philippe E. Spiess, MD, assistant chief of surgical services and high-volume kidney cancer surgeon at the Moffitt Cancer Center in Tampa, Florida. “Up until this point, these patients were never eligible for clinical trial participation, as it was thought they would do poorly, but now with promising outcomes with new treatment combinations along with sitedirected brain radiation, our clinical approach to these patients needs to adapt to one offering more hope and personalization.”
In addition, the morbidity and mortality of these therapeutic modalities
are improving, he said, “and now our focus should be in knowing which of these systemic therapies when used in combinations along with radiation can offer a curative potential to a subset of patients.”
Scott S Tykodi, MD, PhD, Director of Kidney Cancer Research at the University of Washington’s Fred Hutchinson Cancer Center in Seattle, said the real-world data used in the study are informative because the outcomes are likely closer to what is seen in the clinic versus clinical trial results, which usually exclude patients with comorbidities and unfavorable disease presentations like brain metastases.
“The trends observed in the IMDC data are consistent with our expectations that front-line IO-based regimens are better than TKI monotherapy, and an oligometastatic pattern of brain metastases amenable to surgery or stereotactic radiation is a better prognosis than widespread disease managed by whole brain radiation or no localized therapy at all,” Dr Tykodi said. “While this study reinforces our usual treatment patterns, it also confirms the survival penalty associated with brain involvement by the metastatic disease burden.”
Marc A. Bjurlin, DO, MSc, Director of Clinical Trials at the Lineberger Comprehensive Cancer Center at the University of North Carolina, Chapel Hill, said the new study provides a context in which clinicians can better counsel patients with RCC brain metastases in terms of expected OS by taking into account both focal therapy options and systemic therapy.
The IMDC database enabled investigators to capture a broad selection of clinically important and informative variables in a cohort of patients with a relatively long follow-up, Dr Bjurlin said. He pointed out, however, that there is a selection bias in that only patients who were suitable for stereotactic radiotherapy or neurosurgery were selected for those interventions, whereas those who were unable to receive these treatments due to such issues as the presence of more or larger tumors might have been steered toward whole brain radiotherapy. ■
Pruritus is common among patients with nondialysis-dependent chronic kidney disease (NDD-CKD), and it is associated with a higher risk for cardiovascular (CV) events and death.
Among 4410 patients with NDD-CKD in the 2013-2021 Chronic Kidney Disease Outcomes and Practice Patterns Study (CKDopps), 51% reported bothersome pruritus, Jennifer S. Scherer, MD, of NYU School of Medicine in New York, New York, and colleagues reported in Kidney Medicine. The proportion of patients who were somewhat, moderately, very much, and extremely bothered by itchy skin was 27%, 13%, 7%, and 3%, respectively.
More than half of the NDD-CKD patients studied reported bothersome pruritus.
The prevalence of pruritus and degree of bother increased with advancing CKD stage, older age, and comorbidity burden.
Among patients at least moderately bothered by pruritus, 23% overall were prescribed at least 1 pharmacotherapy, including 35% in the United States, 19% in France, and 4% in Brazil. The most common prescriptions were antihistamines (10%), gabapentin (6%), topical corticosteroids (4%), pregabalin (3%), and sedating antihistamine (3%). Systemic medication was used more often than less harmful options, such as topical corticosteroids.
Difelikefalin is only approved for patients receiving dialysis. However, clinical studies are evaluating the safety and efficacy of oral difelikefalin in advanced CKD.
Patients who were extremely bothered by pruritus had a significant 74% increased risk for all-cause mortality, an 84% increased risk for CV events, and a 56% increased risk for all-cause hospitalization compared with those who had no bother. Infections were also more prevalent among patients with pruritus. Severe pruritus was not associated with CKD progression or initiation of kidney replacement therapy.
“These findings are important because the associations of pruritus with increased mortality, infections, and hospitalizations have been described in the maintenance hemodialysis population but never in the CKD population,” according to Dr Scherer’s team. ■
Chronic kidney disease (CKD) has a well-known impact on many body systems, but less appreciated is the link between the kidney and the thyroid. Increased understanding of this relationship offers a largely unexplored opportunity to improve management of patients with CKD, in whom thyroid problems are frequently underrecognized.
An estimated 20 million Americans have some type of thyroid disease. Disconcertingly, it is also estimated that 60% of those with a thyroid condition are unaware of it.1 Regarding CKD, subclinical hypothyroidism has been found to increase from 7% to 17% in patients whose glomerular filtration rate (GFR) drops to 60 mL/min/1.73 m2 from 90 mL/min/1.73 m 2 or higher. 2 Recent research indicates that subclinical hypothyroidism can be considered an independent predictor of CKD in the
injury.4 CKD is thought to impair thyroid function through multiple pathways. One such pathway is reduced expression of type 1 5′-deiodinase that leads to decreased conversion of T4 to T3. Indeed, the most common finding is not an elevated thyroid stimulating hormone (TSH) level, but low T3.2 However, TSH is the most common and typically only laboratory measure used to assess thyroid function, which can result in underdiagnosis of thyroid disease. This is significant because it is estimated that GFR is reversibly reduced by about 40% in more than half of adults with hypothyroidism.4
Providers can improve CKD care by: Regularly screening for thyroid issues by ordering a full thyroid panel. Because TSH is not a reliable marker of thyroid issues in patients with CKD, a full thyroid panel including TSH, free T3, free T4, and thyroid peroxidase
Proper thyroid function requires various micronutrients, including zinc, iodine, selenium, choline, iron, folate, and essential amino acids.
general population, even when adjusting for other common risk factors such as age, hypertension, and obesity.3
The effects of poor thyroid function on the kidney are widespread, including reduced renin-angiotensin-aldosterone system (RAAS) activity, reduced GFR, and decreased heart rate and cardiac output that leads to diminished renal blood flow and ischemic kidney
antibodies would be more informative. It is important to recheck thyroid function as GFR changes as well.2
• Considering patient symptoms. Subclinical hypothyroidism is common in those with CKD, which may mean laboratory values look normal but patients present with common hypothyroidism symptoms and signs like cold intolerance, fatigue, brain fog, hair loss, joint and muscle pain, increased cholesterol and triglyceride

levels, unintentional weight gain, or difficulty sleeping.5 These findings can be common in patients with CKD as a result of anemia or other common coexisting conditions, so testing is important to properly identify the root cause.
• Ensuring adequate micronutrients and amino acids. T4 to T3 conversion and thyroid function require several micronutrients, such as zinc, iodine, selenium, choline, iron, folate, and essential amino acids. This is an important consideration if the patient is on a T4-only thyroid medication or on a low-protein or plant-based diet.6 A dietitian can play an important role in assessing nutrient need, guiding diet changes, and recommending appropriate supplements. Managing stress. Cortisol can inhibit conversion of T4 to T3 and actually increase conversion of T4 to reverse T3.7 While stress management support is not a typical responsibility of nephrology providers, providing tools or referrals to support patients is appropriate. Measures that can reduce stress include meditation, counseling, and vagus nerve stimulation.8
Because thyroid disease can affect kidney health (and vice versa), nephrology providers are uniquely poised to investigate and identify thyroid issues. As with many connected issues in CKD,
An estimated 20 million Americans have some type of thyroid disease.
nephrology providers need not shoulder the responsibility of treating thyroid disease, but refer out to dietitians, endocrinologists, and other appropriate providers to ensure the patient is getting the best care possible. Although it is not fully understood how much of an impact supporting thyroid health can have for those with CKD, with a few simple proactive steps providers can begin to see possibilities. ■
Lindsey Zirker MS, RD, is a renal dietitian and Director of Clinical Services for the Kidney Nutrition Institute in Titusville, Florida. She specializes in autoimmune kidney disease and advanced practice medical nutrition therapy for people with kidney disease.
1. American Thyroid Association. Accessed February 7, 2024. https://www.thyroid.org/media-main/press-room/
2. Mohamedali M, Reddy Maddika S, Vyas A, Iyer V, Cheriyath P. Thyroid disorders and chronic kidney disease. Int J Nephrol. 2014;2014:520281. doi:10.1155/2014/520281
3. Kim HJ, Park SJ, Park HK, et al. Subclinical thyroid dysfunction and chronic kidney disease: a nationwide population-based study. BMC Nephrol 2023;24:64. doi:10.1186/s12882-023-03111-7
4. Basu G, Mohapatra A. Interactions between thyroid disorders and kidney disease. Indian J Endocrinol Metab. 2012;16:204-213. doi:10.4103/2230-8210.93737
5. National Institute of Diabetes and Digestive and Kidney Diseases. Hypothyroidism (underactive thyroid). Accessed February 7, 2024. https://www.niddk.nih.gov/health-information/ endocrine-diseases/hypothyroidism.
6. Krishnamurthy HK, Reddy S, Jayaraman V, et al. Effect of micronutrients on thyroid parameters. J Thyroid Res 2021;1865483. doi:10.1155/2021/1865483
7. Holtorf K. Peripheral thyroid hormone conversion and its impact on TSH and metabolic activity. J Restor Med 2024;23(1):30-52.
8. Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain-gut axis in psychiatric and inflammatory disorders. Front Psychiatry. 2018;9:44. doi:10.3389/fpsyt.2018.00044
“Don’t ever arrive emptyhanded,” my older sister advised me about the etiquette of gift-giving after I graduated college. Beyond the more obvious expectations with birthday parties, she recommended that whenever invited to a barbecue or a dinner party, I should bring a small token of my appreciation of the host’s generosity of the invitation. Although to my young brain she made it sound like a rule, she was describing existing norms that guide social behavior. Given this, it is not unusual that giftgiving from patients may sometimes confound both patients and their physicians.
Avoid Patient Exploitation
Ethical considerations can help inform the potential challenges of gift-giving in a professional setting. The relationship between patient and physician is bound by norms of professional behavior in part because it is ethically distinct from other social relationships. Physicians have an ethical and professional obligation to put patient’s interests above their own. This so called “frame” of the physician-patient relationship helps create boundaries that advance the goals of medical care by promoting the patient’s interests and avoiding patient exploitation.
Consider Patients’ Motivations
The physician-patient relationship is not simply transactional. Although there is insurance and potentially copays for services rendered, the basis for the relationship is fiduciary. Patients trust that their physician will care for them without regard to who they are, what illness they have, or whether they give gifts. Therefore, the physician should be mindful of the patient’s motivation
behind the gift-giving to evaluate when it appears to be primarily transactional. Does this patient believe that unless they provide the physician with a gift, the physician will not give them the time, attention, or individualized care they need? In this case, it is the physician’s responsibility to assure the patient of the fiduciary nature of their relationship and remind them that their care is never contingent on the provision of gifts.
Gift-giving is not likely to violate the same boundaries as a sexual relationship, but the ethical considerations in maintaining appropriate boundaries still applies. Furthermore, there are situations when gift-giving from a patient would be completely appropriate. From a patient’s perspective, gift-giving is often an entirely normal part of social interaction when showing appreciation. So how should clinicians approach this problem when confronted with a gift from a patient?
Clinicians should consider the ethics principles previously described and how they apply to a particular situation. Would accepting the gift be in the patient’s best interests? Does accepting the gift promote the physician’s interests far beyond those of the patients? Would accepting this gift contribute to or give the impression of exploitation? What are the patient’s potential motivations in giving this gift? The answers to these questions in specific scenarios may depend significantly on the context, suggesting that gift-giving would be ethically justifiable in some cases but not in others.
For example, it is unlikely to be ethically problematic for a physician to accept a patient’s gift of baked goods
during the holiday season as a token of the patient’s appreciation. Accepting a relatively inexpensive gift is not likely to exploit the patient and can promote the patient’s best interests by showing appreciation for the thoughtfulness of the gesture. In other words, rejecting a modest gift provided when gifts might normally be exchanged is more likely to harm the physician-patient relationship.
Alternatively, a patient who wishes to bequeath their physician with a sizable fortune after their death is likely to be ethically (and potentially legally) problematic. The size of the gift is far beyond a customary show of appre-
The more challenging cases may be somewhere in the middle of these extremes. Perhaps a patient wishes to gift their physician with expensive tickets to a sporting event or the arts. Again, physicians should discuss with the patient the principles above, trying to understand the patient’s motivation, assuring patient primacy, being mindful of potential exploitation, and assessing what the effect will be on the treatment relationship of accepting the gift. Depending on the answers to those questions, declining a gift might be as simple as saying, “I appreciate this lovely and thoughtful gesture. I can’t accept such large gifts from my patients.” Accepting the gift

The patient-physician relationship is bound by norms of professional behavior in part because it is ethically distinct from other social relationships.
ciation for the physician’s care and services. Accepting such a gift would overwhelmingly promote the physician’s interest and would raise concerns that it is exploitative. The motivation behind such a gift would be important to more fully understand. When an appreciative patient wishes to support a physician’s clinical care or research with an estate gift, the donation should be negotiated and managed through an institutional development office to minimize the potential ethical conflict with the individual physician.
might be as simple as saying, “Thank you for such a special gift,” and then remaining mindful of maintaining professional boundaries going forward. ■
David J. Alfandre, MD, MSPH, is a health care ethicist and an Associate Professor in the Department of Population Health at the NYU School of Medicine in New York. The views expressed in this article are those of the author and do not necessarily reflect the position or policy of the VA National Center for Ethics in Health Care or the US Department of Veterans Affairs.
As advancements in artificial intelligence (AI) continue to revolutionize health care, there appears to be a growing acceptance by patients and clinicians. A recent Cleveland Clinic national survey, for example, found that 3 in 5 Americans believe that AI will lead to better heart care. In addition, health care providers are spending heavily on IT and adopting new computergenerated tools.
Individuals are still cautious about how they use AI when it comes to their health. The survey showed that 72% of individuals believe the health advice they receive from a computer chatbot is accurate, but 89% said they would still seek doctor’s advice before acting on chatbot recommendations. The online survey was conducted among 1000 people aged 18 years or older. Respondents were nationally representative regarding age, gender, region, education, household income, race/ethnicity, and urban/rural residency.
Most Americans using health monitoring technology are experiencing significant physical and mental benefits. According to survey responses, 79% have noticed positive changes to their physical or mental health. The survey found that 60% of Americans track their daily step count and 53% monitor their heart rate/pulse. It also showed that 40% track their burned calories, 32% track their blood pressure, and 53% say they began exercising more regularly after using wearable technology to monitor their health.
The survey showed that due to monitoring technology, 50% are getting in
more steps per day and 34% are improving their eating habits. Further, 27% are more intentional about finding time to de-stress and relax.
Health care providers are spending heavily on IT, suggesting that technology is becoming a leading strategic
cycle management and clinical workflow optimization remain top areas of investment, according to the survey. However, patient engagement has moved up the list of priorities, particularly among more advanced or digitally mature providers.
E. Scot Davis, of Little Rock, Arkansas, a member of the LUGPA (Large Urology Group Practice Association) Board of Directors with nearly 30 years of experience in physician practice management, said the demand for urologic services is increasing while the supply of urologists available to treat patients is suboptimal. “Practices must find

In a Cleveland Clinic national survey, 60% of Americans track their daily step count and 53% monitor their heart rate/pulse.
priority for health care practices.
In a survey of 201 health care provider executives in the United States conducted in June 2023 by Bain & Company and KLAS Research, 56% of respondents cited software and technology as among their top 3 strategic priorities compared with 34% in 2022.
The survey showed that 75% of respondents expect growth in software and technology spending to continue over the next 12 months. Revenue
innovative ways to meet the needs of our patients,” he said. “Physicians and advanced practice providers can only see so many patient encounters in a day, and burnout among urologists is one of the highest of all specialties.”
The use of AI combined with emerging telephone technologies may offer solutions to ease this challenge.
“Perhaps the number 1 complaint heard among my colleagues is the vast number of phone calls that need to be answered on a daily basis,” Davis said.
“Practices might consider utilizing interactive voice recognition (IVR) software in conjunction with live operators to be able to meet the patients’ needs as well as reduce costs.”
Urology practices must evaluate each touchpoint, from initial patient contact to clinic visit and culminating with billing and follow-up, and consider how AI and technology can help improve the patient experience and reduce costs, according to Davis. Many electronic medical record systems have “bolt-on” products to improve pre-authorization processes. The systems also have automatic coding software, integrated patient responses directly into the patient chart, and methods to improve the collections process.
“Urology practices must embrace and implement AI and technology,” Davis said. “Obviously, any technology that improves the overall patient experience is good for the patient and the practice. Additionally, there will be a positive financial impact to the practices adopting AI and technology, if implemented correctly and timely.”
Emerging trends show technology is improving patient engagement through the use of IVR, triage software utilizing conversational chatbots, and self-scheduling tools for patient ease. From an administrative side, Davis said he foresees practices adopting more pre-authorization software technology combined with billing and coding applications to drop claims quicker with greater accuracy.
“This feature will feed well into an interactive dictation tool for providers to document more easily and efficiently, he said. “All of this technology and AI adoption will require an acceptance and change by the providers who must first believe the software will work, and secondly, will trust it can do it as well as they can do it. Without those, much time and effort and money will be spent without any useful benefits.” ■
John Schieszer is a medical journalist based in Seattle, Wash.
Learn about more ways to improve your day-to-day medical practice