Meet our Honorary Fellows

ISSN 2632-0185 COLLEGE FOR MEMBERS OF THE ROYAL COLLEGE OF PHYSICIANS AND SURGEONS OF GLASGOW EDITION 15


2 RCPSG.AC.UK ADVERTISEMENTS













Voice is the magazine of the Royal College of Physicians and Surgeons of Glasgow. If you are interested in contributing to Voice please email: media@rcpsg.ac.uk Copyright 2023. The text and images in this publication may not be reproduced without permission from the Royal College of Physicians and Surgeons of Glasgow. To request permission, please contact the Creative Manager. Produced by Communications and Marketing. Editor Elaine O'Connor Writers Hannah Parker, Fiona Hooker, Steven Shanahan, Kat Hannah Design Craig Gallacher Print Winter and Simpson Print Photography Jamie Simpson, Fiona Winter, John Camilleri-Brennan, Elaine O'Connor Royal College of Physicians and Surgeons of Glasgow 232-242 St. Vincent Street, Glasgow, G2 5RJ +44 (0) 141 221 6072. Registered Charity SC000847. EDITION 15 NEWSBITES 6 UPDATE FROM THE PRESIDENT 5 BUILDING SUSTAINABILITY INTO EVERY DAY REPRESENTING OUR COLLEGE IN BANGLADESH 14 REFLECTING ON THE NHS AT 75 12 harder ever workforce Wanting to work differently Leading and innovating Still feeling valued S ill fli 2022 CENSUS OF CONSULTANT PHYSICIANS 16 8 CELEBRATING AT OUR DIPLOMA CEREMONY INEQUALITIES IN HEALTH 21 19 MEMBERS' AREA 24 EDITION 15 3
 The staircase leading up to College Hall at our College building in St. Vincent Street, Glasgow
The staircase leading up to College Hall at our College building in St. Vincent Street, Glasgow
RCPSG.AC.UK
Welcome to College Voice, which I hope will offer a message of support and optimism during a time of significant challenge for all who work in the health service. Over the past year, we have been faced with sustained workforce pressures, record backlogs for elective and outpatient care, delayed access to social care, and ever-increasing demand. It is, therefore, unsurprising that our health service, and its workforce, are not in a healthy position. Our College is committed to actively addressing the current crisis through discussions with governments, devolved administrations, the GMC, other Colleges, specialty associations, and others about the steps we can take to support our Fellows and Members during the challenging period ahead.
Despite the challenges within the NHS, let's not lose sight of its great value and wonderful history. We recall its groundbreaking innovations as we mark the NHS’s 75th birthday (p.14) with personal reflections from our Vice President (Surgical) John Scott. With the introduction of a universal system, free at the point of delivery, the founding principles sought to tackle health inequalities in the UK. However, 75 years on the gap in healthy life expectancy across the nation remains. Urgent change is needed to protect the health of the population and the NHS, and I believe that we have the power to enact this change. For this reason, I have dedicated this year’s President’s Conference to understanding Health Inequalities (p.23) and exploring the practical steps we can take to close the gap. I hope to see you in November to discuss these issues.
Our recent Diploma Ceremony (p.8) served as a warm reminder of the passion and dedication that persists within the healthcare professions. We welcomed leading figures who have carried out outstanding work to improve health across the globe, reminding us of the privilege we have in making a lasting impact on peoples’ lives.
As our new Members and Fellows began a new chapter in their careers, we took a moment to focus on what is most important: their wellbeing. In the most recent survey of consultant physicians in the UK (p.18), we learned that almost one in five are at risk of burnout and a similar number almost never feel in control of their workload. As we usher in a new generation of doctors, we also welcome new ways of working that give medical professionals better support and work life balance – one of the many interventions our College will advocate for to retain our valued workforce. As we continue to reform the system, we remain cautious of the impact it is having on our planet’s health and we will continue to work to embed sustainable practices in medicine (p.12).

In our College community, you have a voice – and our upcoming elections (p.28) ensure the voices of our members are heard. Please let me know if our College can be of more specific assistance in any situation that you or your colleagues are facing by contacting me at: president@rcpsg.ac.uk.
Mr Mike McKirdy President of the Royal College of Physicians and Surgeons of Glasgow

EDITION 15 5 FROM THE PRESIDENT
NEWSBITES
VOW TO TACKLE ‘COMPLETELY UNACCEPTABLE’ BEHAVIOURS
In September, the Working Party on Sexual Misconduct in Surgery published its report ‘Breaking the Silence –Addressing Sexual Misconduct in Healthcare’. Over 1,400 registered surgeons from across the UK responded to the survey. Of female responders, 63% had been the target of sexual harassment from colleagues, and a third had been sexually assaulted by a colleague. 90% of women, and 81% of men had witnessed some form of sexual misconduct. College President, Mike McKirdy, said: "The findings in the report are deeply disturbing. They describe completely unacceptable behaviours which have no place in surgery or the wider NHS.
“All staff have a fundamental right to safety in the workplace. Abuse and misconduct must not be tolerated.”
The report sets out recommendations for the Department of Health and Social Care, healthcare providers and other organisations including medical Royal Colleges and the GMC. “As a Royal College, we are actively looking at the actions we can take to prevent further harm and put support in place for those affected,” Mr McKirdy continued.
“We welcome the recommendations put forward by the Working Party and will take these on fully, while also working closely with the GMC, to address the problems of misconduct in medicine.”
LEADERSHIP PROGRAMME ALUMNI REUNITE AT ROYAL COLLEGE

Alumni of our Leadership Development Scholarship Programme reunited at the College this summer at a special celebration.
The programme was established in 2019 by Professor Jackie Taylor, then President of the College, and Professor Dame Anna Dominiczak, Regius Professor of Medicine at the University of Glasgow and Scotland’s Chief Scientist (Health). Since then, 20 talented clinicians and academics have benefited from bespoke leadership learning and training, to support them in the next phase of their careers. On the final day of this year’s programme, participants from each year gathered together at the College.
The fully-funded programme is open to those in the early stages of a leadership position, including clinical academics, of any health-related discipline. It includes three days of intensive leadership training, an assessment of personal leadership style, experiential learning and support, mentorship training, and access to personal mentorship from a senior clinician. Keep an eye on the Awards and Scholarships section of our website as applications for the next course, which will take place in early 2024, will open this autumn.
rcp.sg/awards
6 RCPSG.AC.UK
TWO SURGICAL EXAM CENTRES TO OPEN IN INDIA
Two new examination centres for surgical trainees are set to launch in India, with the first exams expected to take place early next year.
The College will work in partnership with Symbiosis International in Pune and KIMS Health in Thiruvananthapuram to offer the MRCS Part B examination – an intercollegiate exam run by the four surgical Royal Colleges in the UK and Ireland.
President Mike McKirdy announced the new centres during his visit to India this summer.
He said: “We are extremely proud of our international College community, and it is such a pleasure to return to India this year to meet with colleagues and the physicians and surgeons of the future.
NHS WORKFORCE PLAN REVEALED
The UK Government’s long-awaited NHS Workforce Plan was published in June. Set to be implemented over 15 years, the plan will see ‘record numbers’ of doctors, nurses and other healthcare staff being trained in England.
College President Mike McKirdy said: “The NHS has long needed a workforce plan and I particularly welcome the expansion of medical student and trainee doctor numbers and commend the commitment to retain our greatest resource – those currently working in the NHS.
“Wellbeing, and compassionate leadership, should be key priorities for the NHS in the years ahead if we are to create the workforce our NHS needs and deserves.”
“Our new partnerships with Symbiosis International and KIMS Health are an exciting development which will provide easier access to this important exam for trainee surgeons in India and the Middle East. Our experienced examination team is very much looking forward to meeting with the centre’s first candidates in early 2024.” While visiting India, the President met with colleagues, including Fellows and Members of the College in New Delhi, Hyderabad and Ahmedabad. Over the course of the visit, he delivered a series of talks on global citizenship in the NHS and reflected on the approach to breast cancer treatment and management, based on his own career as an NHS surgeon.
NEW MASTER’S QUALIFICATIONS LAUNCHED FOR TRAVEL MEDICINE PROFESSIONALS
We’ve launched two new qualifications – MSc Advanced Practice (Travel Medicine) and MSc Advanced Practice (Expedition and Wilderness Medicine) – in collaboration with Glasgow Caledonian University.
Taught by travel and expedition medicine leaders, these courses respond to the need for formal qualifications which demonstrate professionalism and ultimately, protect patient safety.
Dr Sam Allen, Dean of the Faculty of Travel Medicine at the College, said: “The new Master's qualifications combine practical learning and academic capability, and the travel medicine Master's is believed to be the first of its kind in Europe. This is a monumental achievement driven by our valuable partnership with GCU, and the hard work of educators, trainers and leaders.”
DAVID WYLIE APPOINTED AS DEAN OF THE FACULTY OF PODIATRIC MEDICINE
At the Faculty of Podiatric Medicine AGM in May, David Wylie was appointed Dean of the Faculty of Podiatric Medicine, succeeding the position from Christine Skinner. David has been a Fellow of the Faculty since 2013, and managed podiatry services in the NHS for over 30 years. He is Associate NMAHP Director at NHS Education for Scotland, and prior to that was Head of Podiatry at NHS Greater Glasgow and Clyde.
up the
EDITION 15 7
On taking
post of Dean,
David said: The international profile of the College offers the podiatry profession in the UK an unparalleled opportunity to develop shared learning opportunities and mutual educational support globally.
CELEBRATING NEW FELLOWS AND MEMBERS AT OUR DIPLOMA CEREMONY
 Photos: Jamie Simpson / Royal College of Physicians and Surgeons of Glasgow
Photos: Jamie Simpson / Royal College of Physicians and Surgeons of Glasgow
RCPSG.AC.UK 8
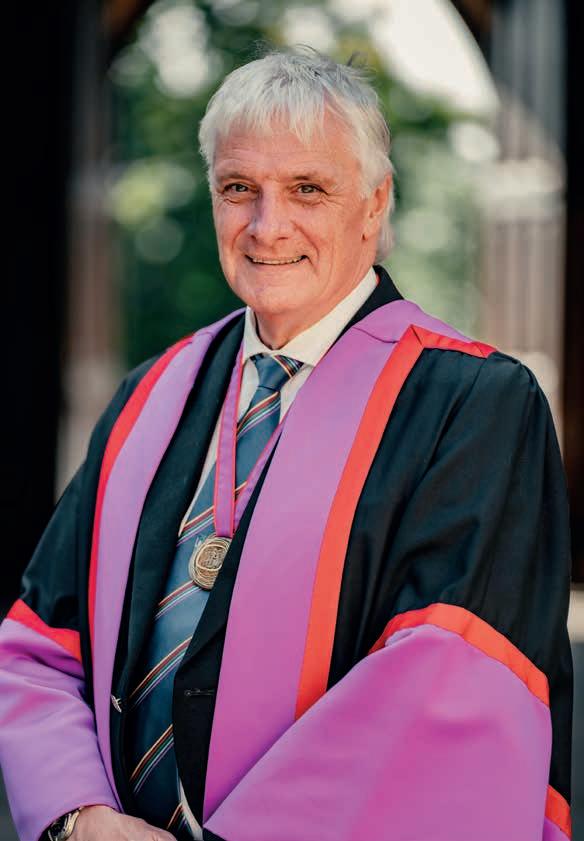
Sir Tom Hunter, Dr Adar Poonawalla, Professor Dame Sarah Gilbert, Professor Chris Lavy
On a warm September day, more than 300 new Fellows and Members from 27 different countries travelled to Glasgow to take part in our Diploma Ceremony.

The events took place at the University of Glasgow’s Bute Hall, where we celebrated the achievements of hundreds of physicians, surgeons, dentists, and travel and podiatric medicine professionals.


We welcomed seven new Honorary Fellows and presented three individuals with the President’s Medal on the day.
Sir Tom Hunter, founder of the Hunter Foundation, was recognised for the impact he has made on tackling poverty and inequality and promoting entrepreneurship in Scotland and beyond.
Joining him was Chris Lavy, Professor of Orthopaedic and Tropical Surgery at the University of Oxford. His inspirational work supporting the development of orthopaedic training and services and clubfoot
treatment in East, Central and Southern Africa was recognised.
Two people who have been instrumental in developing vaccines and making them accessible were also honoured at the event. Dr Adar Poonawalla, CEO of the Serum Institute of India, was made an Honorary Fellow recognising his commitment to affordable prices for vaccines and work to make them accessible for all. And Professor Dame Sarah Gilbert, the world-leading vaccinologist who led the development of the Oxford vaccine during the Covid-19 pandemic, was awarded the President’s Medal.
Our President’s Medal was also awarded to Dr David Ritchie and Dr Patrick Grant for their outstanding work on the Bridges Programme, based in Glasgow. The Programme supports doctors who are refugees to work in the NHS through education and advisory services. You can find out more in the Members’ Area.
A member of our Faculty of Dental Surgery celebrates at the Diploma Ceremony
Faculty of Dental Surgery member with guest
EDITION 15 9
Dean of the Faculty of Podiatric Medicine David Wylie welcomes new Fellow Jayne Robbie
In the spirit of collaborative working and celebrating our connections with other institutions, we welcomed as Honorary Fellows Professor Cathal Kelly, Vice-Chancellor and CEO of the Royal College of Surgeons in Ireland; Professor Meegahalande Durage Lamawansa, Vice-Chancellor and Chair Professor of Surgery at the University of Peradeniya in Sri Lanka; and Professor Rowan Parks, President of the Royal College of Surgeons of Edinburgh.
Professor Sir Jim McDonald, Principal and Vice-Chancellor of the University of Strathclyde and President of the Royal Academy of Engineering, was also made an Honorary Fellow – marking his contribution to education in the city of Glasgow, where our College is based, and further afield.

It was a day of much celebration for all of our attendees – who were given a warm welcome to our College family from President Mike McKirdy.
He said: “As the UK’s only multidisciplinary Royal College, we are incredibly proud of the impact our College community is making by bringing together different perspectives and experiences to tackle global challenges.

“Our newest Fellows, Members, Honorary Fellows and Medal Winners build on a great legacy of innovation and collaboration over almost 425 years.”

College
Registrar Professor Abhay Rane
“I am extremely proud to be associated with the Royal College. The talent and the collaboration that the College drives through its Fellows, Members and staff is very evident, and I am delighted to be here today.”
Professor Sir Jim McDonald
10 RCPSG.AC.UK
David Wylie, Christine Goodall, John Camilleri-Brennan, Mike McKirdy, Eric Livingston and Sam Allen


 Dr David Ritchie and Dr Patrick Grant celebrate with their President's Medals
New members of our Faculty of Travel Medicine
Dr David Ritchie and Dr Patrick Grant celebrate with their President's Medals
New members of our Faculty of Travel Medicine
EDITION 15 11
New Fellows and Members applaud at the end of the Ceremony
BUILDING SUSTAINABILITY INTO EVERY DAY
In the last edition of Voice, we explored the relationship between environmental sustainability and healthcare. Here, Dr Eleanor Murray, consultant nephrologist at NHS Greater Glasgow and Clyde and former College/NHS Scotland Clinical Sustainability Fellow, considers how we can incorporate sustainability into everyday practice.
This is not an instruction manual to a sustainable professional life, they are personal reflections from my year spending one day a week focusing on sustainable healthcare. I have taken three broad approaches:
STARTING CONVERSATIONS AND BUILDING NETWORKS
We’re all keen to live and work more sustainably. But our best intentions can easily be derailed by overbooked clinics, staff shortages, or any number of competing pressures. When I first started asking colleagues what environmental sustainability activities were happening in our department, the answer was none. But the majority were keen to explore what we could do.
Conversations are the first step. Ongoing conversations keep the momentum going when competing pressures threaten to dampen enthusiasm. Networks facilitate these ongoing
conversations: sharing ideas, resources and practical advice, positive reinforcement and motivation.
I found my communities through setting up a departmental sustainability committee, on social media and online platforms such as the Centre for Sustainable Healthcare (sustainablehealthcare.org.uk), through a national kidney-care working group, and a cross-discipline committee within my health board. The set up doesn’t matter, so long as the contacts and conversations are there. A College sustainability steering group has also been established, which welcomes ideas and suggestions.
12 RCPSG.AC.UK
NORMALISING SUSTAINABILITY AND STEWARDSHIP
Healthcare professionals are familiar with a finite amount of appointment slots, hospital beds, or theatre space. We’re also familiar with the concept of stewardship from microbiology. Constraining the use of antibiotics allows us to treat infections in an individual, whilst managing microbial resistance profiles and preserving sensitivities in the population. Curbing inappropriate antibiotic use has required leadership at a national level. This shows we can protect and future-proof whilst still offering high quality care.
We must start to apply the same principles of resource stewardship to all aspects of healthcare.
It is our decisions and behaviours that drive health systems’ contribution to climate change – every investigation or intervention needs energy to extract resource, to process, manufacture, transport and package.1 We may not have much direct impact on our supply chain, but we do determine procurement and disposal through our clinical decisions.
Looking at your day-to-day practice, you can identify the low-value activity that consumes resource without contributing to patient care. By cutting these, we can improve efficiencies in patient pathways, save money, and improve environmental impacts.
For example, we requested that glucose was removed from our standard electronic ordering ‘set’ of bloods. The standard set is ordered for every inpatient and outpatient, but staff rarely deleted items they didn’t require. Glucose could still be ordered when required, but removing it from the set meant the number of glucose tests sent fell by 83% across 50 inpatient beds and approximately 500 outpatient appointments per week.
This saved cost and carbon by avoiding the energy use and carbon embedded in manufacturing, packaging and distributing glucose bottles; cutting down the reagents and energy involved in transporting and analysing the sample; and avoiding associated waste. For patients, venesection time was reduced, and where appropriate, daily glucose was replaced with a one-off HbA1c, of higher clinical value for diagnosis and monitoring of diabetes.
SUSTAINABLE QUALITY IMPROVEMENT
Projects such as this are specific to your department, as every service will have its own inefficiencies and ‘carbon hotspots’. You can find tools to identify potential projects, and learning resources on undertaking Sustainable Quality Improvement (SusQI) at susqi.org and other websites.
Where able, we have implemented change through SusQI approaches. This provides standardised structure to a project,
and the concepts of QI are widely understood in healthcare. SusQI reflects a ‘shift of narrative’, including environmental, financial, and social outcomes as well as those of the patient.
We reviewed project ideas and considered potential impact and feasibility. We selected some ‘easy fixes’, and targeted other high-impact ones. To target our carbon hotspot of haemodialysis, we set up a protocol to permit greater individualisation of dialysis prescribing. Patients meeting certain criteria could dialyse twice instead of thrice weekly, bringing environmental and financial benefits as well as improved quality of life. We generated calculators to ensure that these patients were still receiving adequate dialysis according to internationally set standards. We provided patient information sheets, and focused on required staff behaviour change with communications.
Such changes require more effort in planning, implementing, and measuring outcomes, but have potential for greater impact, reducing healthcare burden on the patient and on the service.
We have had mixed results across different projects. We achieved changes that were in our ‘circle of influence’ much more easily that those heavily dependent on supply chain, procurement, or involvement of infection control or estates departments. These took additional time, to build wider networks and tackle regulations.
This is where health system leadership is required, to create a working environment that facilitates SusQI across traditional silo working. Advocacy and engagement with management is important to push a ‘green agenda’ and to ensure that the health system enables staff to choose the more sustainable option in their professional life.
National or international specialty-based societies can also amplify the sustainability voice for advocacy, offer leadership, and co-ordinate larger networks. This has been highly effective within renal medicine, in addition to electronic platforms to share projects and events (sustainablehealthcare.org.uk), and using meetings and conferences to increase awareness of climate change, environmental sustainability, and healthcare.
Whilst many of my examples are unique to kidney-care, starting conversations, building networks, practicing resource stewardship, and incorporating environmental sustainability into QI projects are not. I would urge you to consider how these approaches could be incorporated into your own practice.
The time for action is now.
I’d like to add my thanks to the College for supporting my sustainability fellowship last year, and participation in the Leadership Development Scholarship Programme.
(1) Health care climate footprint report. Health Care Without Harm (noharm-europe.org)
EDITION 15 13
“We must start to apply the same principles of resource stewardship to all aspects of healthcare.”
NHS AT
July marked 75 years of the National Health Service in the UK. When it was founded in 1948, the NHS was the first universal health system which was available to all, free at the point of delivery.
It’s a significant milestone – serving as a point of reflection following a particularly challenging few years for the health service. Vice President (Surgical) John Scott shares some of his experiences from a career in the NHS.
STARTING A CAREER IN THE NHS
The vast array of specialties that the NHS encompasses provides an excellent environment for medical graduates to experience different options, and make choices about where their career might go. For John Scott, those early experiences led to his career in Plastic Surgery.
“I was fortunate to experience working in a number of surgical specialties in the West of Scotland,” he said. “Of note was my rotation to the internationally acclaimed Canniesburn Plastic Surgery Unit.
“The raison d’être of the plastic surgeon is to restore form and function after ablative oncological surgery, trauma, or congenital anomalies. The teamwork, enthusiasm, dedication and skill were inspiring.
“The socialised philosophy of NHS care enables the best possible care to be provided without consideration of the patients’ financial status.”
MOMENTS OF PRIDE
“Patients place enormous trust in their doctors. In Plastic Surgery, this is exemplified when undertaking surgical procedures that, without successful reconstructive surgery, have the potential to create permanent loss of form and function.
“Achieving success in this environment requires high levels of performance from all the team – surgeon, anaesthetist, nurses, allied health care professionals. The surgeon is in a privileged position to take the patient through the whole process.
“Witnessing the successful navigation of this journey, with the restoration of a patients’ quality of life, is always an immensely proud moment.”
FOCUSING ON THE FUTURE
Looking to the future, we know that changes and improvements are needed to protect the NHS.
“Talented and dedicated staff are one of the organisation's major assets,” said John. “Retention of the staff both in training and senior clinical roles is key to the future of the health service, particularly as the retirement age inexorably rises.
“The NHS has to appreciate the dynamic changes that occur during a consultant’s career. A senior consultant has a huge amount to offer in terms of teaching and mentoring. Appropriately structured job plans are required to facilitate teaching of the expanding number of medical students and nurturing the enormously talented trainees – the future custodians of NHS care.”
HOW OUR COLLEGE CAN SUPPORT THE NHS
Like the NHS, our College models itself on the collaborative delivery practiced within healthcare teams and between specialties, which is essential to effective care. Of course, we also support our Fellows and Members working in the NHS to deliver the best care.
“Successful performance of NHS staff is inextricably linked to their health and wellbeing,” John said. “Recent surveys of both junior and senior NHS doctors note alarmingly high levels of work-related health issues.
“A focus of our College in recent years has been the promotion and discussion of health and wellbeing amongst medical staff. It is imperative that this issue remains foremost in our activity and is highlighted to both regional health authorities and Departments of Health.”
“The teamwork, enthusiasm, dedication and skill were inspiring.”
14 RCPSG.AC.UK
Milestones through the years*
20th Century: 1948 – 1999
1948
The NHS is launched by Aneurin 'Nye' Bevan, then health secretary, providing free healthcare for all at the point of delivery
21st Century: 2000 – present day
2006
NHS Bowel Cancer Screening Programme launched for those aged 60-69
1956
The first kidney dialysis is performed by Frank Parsons at Leeds General Infirmary
2006
The Smoking Ban is introduced in Scotland – followed by England, Wales and Northern Ireland in 2007
1958
Ian Donald, Professor of Midwifery at the University of Glasgow, publishes findings on ultrasound in the Lancet
2007
Introduction of robotic arm leads to ground-breaking heart operations
1968
Measles vaccine is introduced and the first heart transplant is carried out at the National Heart Hospital in London
2008
CT scans revolutionise the way doctors can examine the body 1972
Development of the Glasgow Coma Scale by Sir Graham Teasdale, former President of the College 1974
1978
Louise Brown is born as a result of in-vitro fertilisation (IVF), developed by Dr Patrick Steptoe
2012
The HPV vaccine, to prevent cervical cancer, is available for all schoolgirls 12 and over
The 100,000 genomes project launched. This research has helped find actionable results for patients with rare diseases and cancer
First known case of Covid-19 reported in the UK 2020
2020
MRI (magnetic resonance imaging) scans are introduced and keyhole surgery is used successfully for the first time 1980
2020
Britain’s first ever purpose-built AIDS ward is opened at the Middlesex Hospital 1987
2022
Free breast screening is introduced to reduce breast cancer deaths, the first of its kind in the world
Covid-19 vaccination campaign begins with 90-year-old grandmother Margaret Keenan, the first person in the world to receive the Pfizer Covid-19 jab
The NHS becomes the first health system in the world to commit to become carbon net zero
The NHS conducts the first net zero operation at Solihull Hospital
The NHS Organ Donor Register is set up
*Source: NHS England
1988
1994
“Talented and dedicated staff are one of the organisation's major assets”
EDITION 15 15
THE UK 2022 CENSUS OF CONSULTANT PHYSICIANS
In recent years, the UK has faced immense challenges in its health service. The impact of the Covid-19 pandemic is still felt in hospitals across the nation as we continue to work towards recovery. It has introduced healthcare professionals to new ways of delivering care, but has also amplified pressures within the workforce that were present before the pandemic began.
Each year, the annual Physicians’ Census, conducted jointly with our College, the Royal College of Physicians of Edinburgh and the Royal College of Physicians of London, provides vital information needed to understand the issues on the ground. The latest census of consultant physicians in the UK reiterates the need for long-term strategic planning to grow the medical workforce and for robust retention policies to reduce the pressure on existing staff.
Keys trends from the 2022 census:
FILLING THE GAPS

The census revealed that unfilled vacancies for consultant physicians across the UK are rising. Compared to data from the previous year (52%), this year 58% of consultant physicians reported having vacant consultant posts, with an average of 2.2 vacant posts per department. Recruitment gaps remain at a record high, as 81% reported that a consultant vacancy went out to advert but was not filled.

The impact of unfilled vacancies is putting significant strain on consultants to manage increasing workloads. As demand for the health service is higher than ever before, we are also battling the effects of a growing backlog for elective and outpatient care. Consultants surveyed are recognising the impact of vacancies




Illustrations: Royal College of Physicians of London

on their ability to deliver care: 73% felt rota gaps had impacted patient care, with reduced access to outpatient care (26%), inpatient care out of hours (23%) and increased length of stay (23%).
As doctors usually working in hospitals, physicians are at the forefront of bringing down waiting lists, including for diagnostic tests, procedures and imaging. Widespread staff shortages make it increasingly challenging to meet rising demand. Despite over two million diagnostic imaging and tests being delivered by NHS staff in April 2023, there were still over one and a half million patients waiting for one of 15 key investigations at the end of that month with 430,800 patients waiting six weeks or more for a test or scan from referral.

FOCUS ON PHYSICIANS:
Working harder than ever A changing workforce Wanting to work differently Leading and innovating
feeling valued S ill fli
Still
16 RCPSG.AC.UK
Consultants and job satisfaction
Percentage who said they ‘always’ or ‘often’ felt satisfied with different areas of their work:
Expanding training and driving recruitment to build strength in the workforce is important, however this is not an immediate solution. It takes on average six to eight years for a doctor to train for a consultant-level position. It is vital that the health service retains existing experienced staff. The majority of consultant physicians (84%) felt valued by their patients – but 44% reported having an excessive workload almost always or most of the time. Worryingly, almost one in five (18%) said they almost never feel in control of their workload and the census estimates that a similar proportion (19%) are at risk of burnout.
WORKING AND LEARNING
It is important to acknowledge that the majority of consultants still feel valued in the health service among both medical (77%) and non-medical (74%) colleagues. One of the most valuable aspects to retaining staff is that people feel a sense of job satisfaction, a sentiment which is felt most from their specialty (86%) but also through the opportunity to engage in education (42%) and leadership (50%) roles. Workforce planning should be focused on ensuring that consultants have adequate time available to pursue these opportunities.

As reflected by the data in previous years, less-than-full-time (LTFT) working continues to rise for both consultants and higher specialty trainees. Although job-plans are in place, currently consultants (86%) are routinely working past these arrangements due to staff shortages, most commonly to do administrative work related to patient care (68%) or to provide direct patient care (54%). Excessive workloads are further impacting the ability for consultants engage with continued professional development (CPD) with the main reasons for not taking leave being the inability to find cover or being too busy.
It is not surprising therefore, that the popularity of LTFT working is growing among consultants, as 28% are now working less than full time, with over half (53%) saying they’d like to reduce their programmed activities which will have notable
implications for workforce planning. Paired with this trend, is a higher proportion of women aged between 35-44 (49%) opting for LTFT compared to men (10%). However, it is predicted the proportion of men taking up LFFT working will increase. The census projects that by 2027, a third (31%) of consultants and a quarter (25%) of higher specialty trainees will be working less than full time.
Less than full time working offers doctors a better worklife balance, childcare opportunities and is an effective means of preventing burnout. However, barriers to access for LTFT working in both workforce planning and hospital culture may risk its effectiveness to retain experienced staff in the short term.
NEXT STEPS
Reflecting on the census results, long-term solutions are still required to balance the number of consultants with the high demand for care in the UK. In June 2023, the UK Government released its long-awaited workforce plan for NHS England, under the principles of Train, Retain and Reform. To be implemented over the next 15 years, the plan sets out to boost an additional 60,000 doctors into clinical practice by 2036/37.
Primarily, this is being done through the expansion of medical school places and the creation of new medical schools across the UK. This in itself will present problems, developing the necessary teaching resource from the existing stretched consultant body and coping with the lag between a student entering training, graduating and then attaining higher specialist training.
Temporary staff and international recruitment have long been relied upon to ensure safe staffing levels within the NHS, however, the plan acknowledges that this cannot be a primary solution to the workforce crisis. We reiterate there is a need for this recruitment to continue in the short term to uphold safe staffing. Although the drive to train more doctors is necessary, the proposals regarding existing staff will set out how we can protect the NHS and its workforce in the years to come.
85% 33% 50% 42% Specialty GIM Leadership
role Educational / training role
EDITION 15 17
Managing staff workload and job plans effectively must be at the centre of workforce planning, to ensure staff have protected time for education, teaching, research and quality improvement across all specialties and career stages. We further stress the need to provide NHS staff with access to affordable childcare and opportunities to enable flexible working.
Despite LTFT working becoming more attractive for trainees, higher specialty trainees and consultants, attitudes from trusts and workplace culture must be addressed, to appropriately integrate this with workforce planning. The workforce plan has set out guidance for implementing ‘culture reviews’ in NHS hospitals to assess how staff improvements can be made. This should include enforcing a culture of compassionate leadership with zero tolerance for bullying and poor professional behaviour. However, the plan is presented as a baseline to be driven locally by individual trusts, limiting implementation at the national level.
Equally, ensuring that staff have access to the basics during shift hours; facilities to rest, nutritious hot food and drink at all hours and time off for significant life events are all immediate interventions which are vital to retention.
Interventions should be prioritised which target the retainment of staff at the end of their career or allow those
Next
who have retired to return. Pension tax reform introduced in the Spring Budget 2023 was welcome to financially support consultants to stay in the NHS. However, improvements are still required to streamline processes for retired staff who wish to return to work.
Retaining this staff pool is vital to training and was evidenced to be of upmost importance during periods of significant stress in the NHS, as shown by the uptake in retired staff working during the Covid-19 pandemic. A more efficient and straightforward process for GMC registration, appraisal and revalidation for retired staff to match appropriate jobs should be developed to meet clinical need and facilitate training of junior doctors. Success will depend on fostering a change in culture within health boards and the GMC to retain highly experienced staff at the end of their career or in retirement, including attitudes to additional training.
With the workforce plan for England now published, the College will continue to advocate for the interventions mentioned here through subsequent reviews. We further anticipate the publication of workforce plans for Scotland and Wales in the near future, which we expect to address the strategies outlined above.
1
Use the census data in our discussions with governments about the need for accountability and transparency in workforce planning 2
Work with governments across the UK and our partners to streamline the process of revalidation to retain doctors at the end of their career and encourage those who have retired to return if they wish to 3
steps We will continue to: £0
Highlight the urgent need for transparent job planning and scrutiny of the amount of work that goes unpaid 5
4
Identify and promote 'here and now' interventions to improve retention and wellbeing, while working towards embedding a culture of compassionate leadership across the NHS
Work with governments to ensure ethical recruitment of doctors from other countries and make the case for the UK to be an accessible and welcoming place to work
18 RCPSG.AC.UK
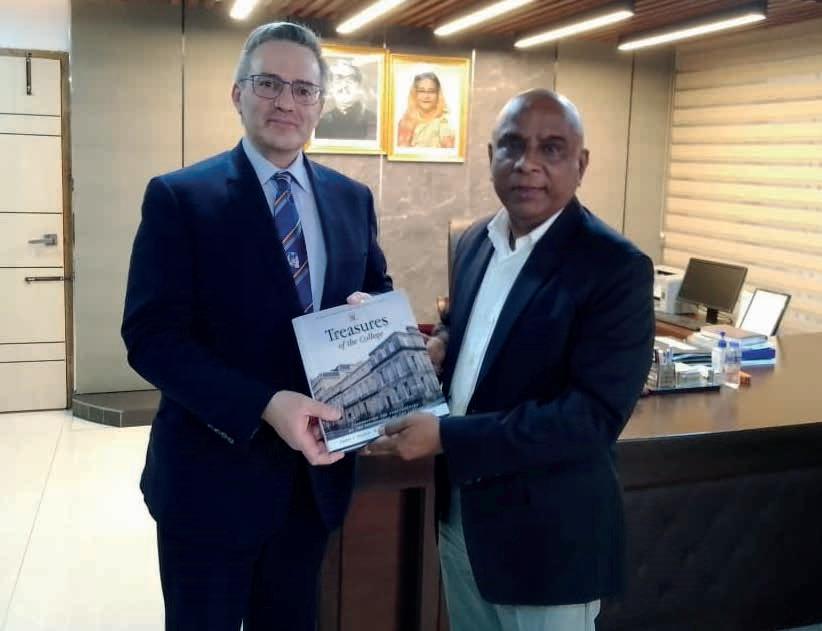
REPRESENTING OUR COLLEGE IN BANGLADESH
Vice-President (Surgical) John Camilleri-Brennan visited Dhaka, the capital city of Bangladesh. He represented our College for the Surgical Fellowship exams by the Bangladesh College of Physicians and Surgeons (BCPS). He shares some of his experiences here.


Earlier this year, I had the honour of meeting the BCPS College Presidents, Professor Quazi Deen Mohammad in January, and the newly elected Professor Shahidullah in July.
With both Presidents and members of their College Council, I discussed many topics of mutual interest, including Global Health, our College’s international work, surgical training and examinations, and collaboration between the two Colleges going forward.
The clinical examinations that I was directly involved in took place at the Sir Salimullah Medical College Mitford Hospital and the Bangabandhu Sheikh Mujib Medical University.
Both of these institutions are known for their commitment to medical education and research. They are significant players in the development of the healthcare sector and the advancement of medical science in the country.
Bangladesh Folk Art and Crafts Museum at the Sadarbari Palace EDITION 15 19
Mr John Camilleri-Brennan with Examiners at Sir Salimullah Medical College Mitford Hospital (Professor Mottalab Hossein, Chief of the Surgical Unit and Fellow of our College, second from left)
Bangladesh is a truly enchanting place to visit. First of all, I was impressed by the warm hospitality that I received. Bangladesh boasts a rich cultural heritage and history, and beautiful natural landscapes. Dhaka has a mix of modern and traditional architecture, with a blend of ancient Mughal structures, British colonial buildings, and contemporary high-rises. Some notable landmarks include the National Parliament House (Jatiya Sangsad Bhaban), Lalbagh Fort, Ahsan Manzil (Pink Palace) and the Dhakeshwari Temple.
I was particularly intrigued by Sonargaon, a historic town located about 25 kilometres south-east of Dhaka. Sonargaon was the ancient capital of Bengal during the medieval period, particularly under the reign of the Hindu Sena dynasty and later the Muslim rulers. The town served as an important trading and administrative centre.
One of the main attractions in Sonargaon is Panam City. Established during the 19th Century, Panam City was a thriving hub for the cotton trade. The area consists of several dilapidated but beautifully adorned buildings that reflect the architectural style of that period.
Another prominent site in Sonargaon is the Bangladesh Folk Art and Crafts Museum. It displays traditional folk art, crafts, and artifacts that showcase the cultural heritage of the region. The museum provides insights into the artistic traditions, rural lifestyle and craftsmanship of Bangladesh. In addition, Sonargaon has some picturesque natural landscapes, offering opportunities for boat rides, picnics, and leisurely walks.
Dhaka is one of the world’s most densely populated cities, with a vibrant and chaotic street life and a diverse cuisine. The infrastructure is in development, yet I noted a remarkable

progress in the construction of the motorways and the new subway. It has been a privilege to serve as External Examiner on behalf of the Royal College of Physicians and Surgeons of Glasgow. I look forward to continuing to strengthen the links established between our Colleges, for our mutual benefit.
BECOME AN EXAMINER
Examiners like Mr Camilleri-Brennan play a key role in supporting the next generation to progress to specialty training, by ensuring trainees have the required knowledge, skills and attributes. Visit our website for details of all examiner positions available: rcp.sg/vacancies
Mr John Camilleri-Brennan with Professor Quazi Deen Mohammad, Immediate Past-President BCPS
Mr John Camilleri-Brennan visited Bangladesh as an External Examiner
20 RCPSG.AC.UK
INEQUALITIES IN HEALTH: WHAT DO WE KNOW AND WHAT CAN WE DO?

The UK’s National Health Service was designed in response to visible health inequalities, pushed forward by collectivist attitudes in the post-war era. Widening access to healthcare for all people removed the fear of ill-health, which had plagued lowincome communities. As a nation, we became healthier thanks to its interventions.
But despite the best intentions, 75 years after the NHS was established, we have not yet been able to eradicate health inequalities.
At the beginning of his medical degree in 1980, College President Mike McKirdy encountered the Black Report. It uncovered a mortality gap across the UK, which revealed that health outcomes were significantly worse and lifespans much shorter for people living in the most underserved communities.1 Findings from the Black Report stuck with him throughout his career. However, over 40 years later, health inequalities continue to persist. In his native Glasgow, healthy life expectancy at birth is only 54.6 years for men and 57.6 years for women2, compared
to the national average of 76.6 (men) and 80.8 (women) years.3 Faced with the lack of change, this year’s President’s Conference is dedicated to addressing health inequalities, focusing on unpacking its complexities and spotlighting effective interventions which empower clinicians to take action.
SPOTLIGHT ON ECONOMICS
On the frontline, healthcare professionals deal with the impact of health inequalities in their daily practice. Instances of chronic disease are rising among those in the most deprived areas of the UK, and in turn, the demand for health service is greater than ever before. However, this problem extends beyond the NHS. Key experts Sir Michael Marmot, Dr David Walsh, Marion Devaux and Professor Gerry McCartney will join the discussions at the conference, assessing what we know about health inequalities and what is preventing change. In their view, economics and social policy holds the key to understanding why this remains a problem for public health.
EDITION 15 21
In 2010, Sir Michael Marmot published his landmark report ‘Fair Society, Healthy Lives’. It revealed the social gradient of health in which the most affluent in England were living on average seven years longer and 17 years more in good health than those in the poorest communities. Further, it estimated the public cost of health inequalities to be between £36 billion to £40 billion through lost taxes, welfare payments and costs to the NHS.4 Although these findings made a concrete case for urgent action, Dr David Walsh argues that the lack of political will to implement policies are preventing change. He notes:
“Health inequalities are an extension of broader societal inequalities: to narrow them, therefore, you need government policies which fundamentally make society more equal. In the UK, we don’t have those policies – indeed in recent years we have had the opposite in place, and as a consequence, health inequalities have widened dramatically.”
Although the economic policies introduced alongside the launch of Marmot’s report have had a lasting impact on health today, at the conference Dr David Walsh will discuss how similar polices have taken effect over the last one hundred years in Scotland. Coupled with this, Marion Devaux will look at the economic map of health inequalities in Europe, to assess how they are tackled in various different health systems.
RETHINKING OUR DELIVERY
Healthcare professionals and by extension, Royal Colleges, also have their part to play in reducing health inequalities. Within the NHS, service design and clinical intervention has introduced successful mechanisms to improve public health in local communities. In November, President Mike McKirdy will welcome leading practitioners Professor Kiran Patel, Professor David Conway, Dr Camilla Kingdon and Professor Andrea Williamson who are all rethinking the delivery of care to achieve health equity.
This starts with understanding how people access healthcare and Professor Andrea Williamson joins us to discuss ‘missingness’ in the system through appointment uptake.
She argues ensuring people don’t fall through the cracks is one step to addressing health inequalities. Additionally, she believes in empowering doctors in their ability to deliver care and using this to advocate for patients, adding:
“Personally, my key one would be a trauma informed practice approach to care – when that is enacted at all levels of the system from managers to frontline clinicians then many of the barriers to care that currently drive inequalities will vanish. Also, importantly the advocacy role that doctors can have for patient groups. Doctors have power and are listened to – use it to achieve health equity!”
In striving for equality in health, service design works in the context of wider determinants of health which requires intervention from both those on the ground and at the top. Professor Kevin Fenton joins us to highlight how racism plays an intrinsic role in health outcomes and access to health. We will also be hearing from Medics Against Violence navigator Alan Gilmour to explore violence prevention in a health care context, particularly among youth, and Sir Harry Burns will further emphasise the importance of early interventions to reduce health inequalities.
Both Professor Tom Lloyd Goodwin and Professor Gerry McCartney will look at how we reshape our thinking on economics through community wealth building. We will also hear from the Directors of all four health systems, including Professor Bola Owolabi, Director of Healthcare Inequalities, NHS England, on the actions governments in the UK are currently taking to build a national response to health inequalities.
NOTES AND ACKNOWLEDGEMENTS
We’d like to thank Dr David Walsh and Professor Andrea Williamson for their contributions to this article. The annual President’s Conference is a hybrid event taking place on 16 November 2023. We’d like to further thank all of our speakers for their participation in this event.
(1) Gray A. M. (1982). Inequalities in health. The Black Report: a summary and comment. International journal of health services : planning, administration, evaluation, 12(3), 349–380. https://doi.org/10.2190/XXMM-JMQU-2A7Y-HX1E
(2) ONS Geography Open Data, ONS, Health state life expectancies, UK: 2017 to 2019. Avaliable at https://www.health.org.uk/evidence-hub/health-inequalities/map-ofhealthy-life-expectancy-at-birth
(3) National Records of Scotland, 2022, Life Expectancy in Scotland 2019-2021. Avaliable at https://www.nrscotland.gov.uk/files/statistics/life-expectancy-in-scotland/19-21/ life-expectancy-19-21-report.pdf
(4) Marmot, M. (2010) Fair society, healthy lives : the Marmot Review : strategic review of health inequalities in England post-2010. ISBN 9780956487001
22 RCPSG.AC.UK
Mr Mike McKirdy President, Royal College of Physicians and Surgeons of Glasgow
 Professor Sir Michael Marmot Professor of Epidemiology at University College London, Director of the UCL Institute of Health Equity
Professor Sir Michael Marmot Professor of Epidemiology at University College London, Director of the UCL Institute of Health Equity
 Professor Bola Owolabi Director of Healthcare
Professor Bola Owolabi Director of Healthcare
 NHS England
NHS England


PRESIDENT’S CONFERENCE 2023 What do we know and what can we do? At this year’s President’s Conference, you can hear from national and international healthcare leaders about how they have overcome the challenges of turning evidence into action, to reduce health inequalities. Attend in College or online: Thursday 16 November 2023 9am - 5pm GMT
Inequalities in Healthcare Visit our website to book your place: rcp.sg/presidentsconf23 SPEAKERS INCLUDE:
Inequalities,
MEMBERS’AREA
“We try to make sure the content is useful revision for the Professional and Linguistic Assessments Board exams – the test required for GMC registration and the right to practice. But it’s also just providing hints on UK-specific things, which are helpful as preparation for working here.”
Andrii, from Ukraine, attends the sessions in the College. He arrived in Scotland about a year ago and at first, was uncertain about the steps he needed to take to start working as a doctor.
“I was quite confused and lost,” he said. “But when I came to Bridges for the first time, and had a conversation with Dr David Ritchie, it gave me hope.
“It’s given me a lot of useful information about how the NHS works, and the differences between the health service here and in my own country. It’s given me confidence. I look forward to every meeting – it’s the highlight of my week.”
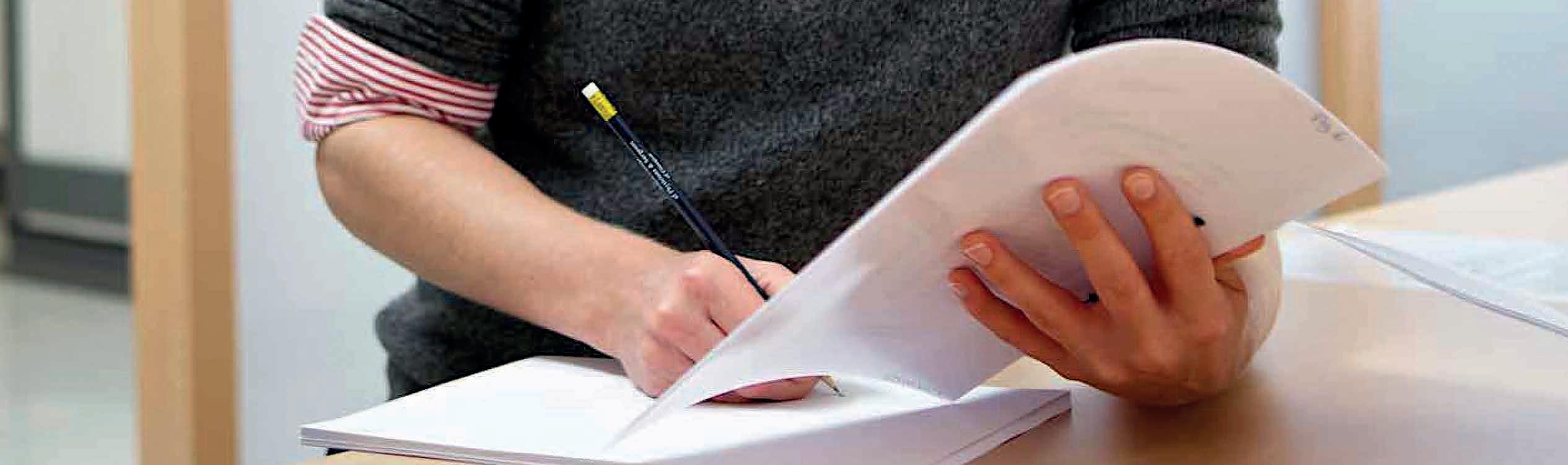
BUILDING BRIDGES
At September’s Diploma Ceremony (see p.8-11), Dr David Ritchie and Dr Patrick T Grant received the President’s Medal for their work with the Bridges Programme.
Bridges is an independent organisation which supports refugees, asylum seekers, migrants and people for whom English is a second language living in Glasgow – helping them into work, education or training. After retiring, David and Patrick started volunteering with the programme and set up a teaching programme for doctors.
The College has supported the programme since 2019 and we provide space in our library for free each Tuesday, for training sessions.

Samantha Gaw, an Intensive Care Trainee, is a volunteer coordinator. “We ask consultants or senior trainees to volunteer their time to come and do a bit of teaching, and we look for people from different specialties,” she explained.
AWARDS AND SCHOLARSHIPS
Are you keen to travel, and gain experience by visiting other countries or specialist centres? One of the benefits you have as a member of our College is access to apply for our awards and scholarships. These are designed to support you to progress your research, or build on your skills and knowledge.
Here’s a sample of some upcoming awards and scholarships –you can find many more and further details on our website: rcp.sg/awards
Ethicon Foundation Fund Travelling Fellowship
Offering surgeons grants of up to £900 to support you with overseas travel (closing date: 24 November 2023).
The sessions at the College are relatively informal – providing a sociable, relaxed environment where people can share their own experiences and advice.
“I have been working only in surgery since I graduated,” Andrii said, “so covering different specialties helps me revise the material which will come up in my exams. Meeting my peers also gives me an opportunity to discuss steps towards getting a licence as a doctor here.”
“We do a lot of teaching within the NHS, and for me, it’s slightly different being part of a community like this,” Samantha added.
“You get loads of interesting stories about people’s backgrounds, and their experiences. I learn a lot from them.
“It really becomes a community. It feels quite special.”
If you want to learn more about the Bridges Programme or volunteer, get in touch by emailing samantha.gaw@nhs.scot
College Travelling Fellowship
Up to £2,000. Open to all Members of the College – including students, affiliates and associate members – for travel to support learning opportunities (closing date: 24 November 2023).
The Tuanku Fauziah Fellowship in Rural Medicine
For physicians, up to £2,000 for travel to Malaysia, to gain further experience and training in rural medicine (closing date: 24 November 2023).
J C MacDougall Travelling Fellowship
For specialists in Oral Medicine, Oral Surgery or Oral Pathology, up to £1,500 to assist with travel and accommodation for training and to build experience (closing date: 1 December 2023).
24 RCPSG.AC.UK MEMBERS' AREA
IMG INDUCTION: A WARM WELCOME TO GLASGOW
In August, the College held a dedicated induction session for International Medical Graduates (IMGs) starting at NHS Greater Glasgow and Clyde. It was a collaborative event with NHS Education Scotland, made possible through a link with Professor Mo Al-Haddad, Associate Postgraduate Dean for IMGs in Scotland.

More than 30 delegates, most of whom are starting as new FY1s in Glasgow-area hospitals, came along to the College building at St. Vincent Street for the full day session.
Attendees had an introduction to training grades, pathways and other types of health professionals they’ll be working with in multidisciplinary teams. They also heard about how the NHS differs from other countries’ healthcare systems, and what to expect in terms of workplace culture.
But the event was also about welcoming the group to working life in the West of Scotland. Attendees learned about living and working in Greater Glasgow and Clyde, getting around, the local culture and got tips on surviving their first few weeks in post.
OBITUARY
Marjorie E M Allison MD FRCP(Glasg) FRCP(Edin)
1940–2023
Marjorie Allison entered the Univeristy of Glasgow in 1958, graduating with first-class honours BSc Physiology 1962; then MB ChB with honours 1965; and MD with honours 1976. Her prizes included most distinguished woman medical graduate of her year. She trained in the University Department of Medicine at Glasgow Royal Infirmary, specialising in nephrology with Professor Arthur Kennedy. From 1969 to 1973, as a research fellow in renal physiology at the University of North Carolina, she performed meticulous, pioneering work in animal models relevant to human problems.
Returning to Glasgow Royal Infirmary in 1973, and despite cancer and four major operations, she became senior lecturer and consultant nephrologist in 1977. Retaining her interest in clinical research, she devoted most of her time to clinical work and teaching. Her determination to do the very best she could for every patient was renowned.

Marjorie’s approach to medicine was influenced by her strong Christian beliefs. She enjoyed being active in the local church, entertaining visiting trainee doctors, visiting family in England and foreign travels.
In 1995, Marjorie took early retirement from the Royal Infirmary, working on the new undergraduate curriculum for the Medical School. She taught as a facilitator, clinical skills instructor, then third year coordinator.
HAVE YOU VOTED YET?
Voting for our College Executive Board and Council Elections is open from 9 October to 9 November 2023. Key positions in this election include President Elect, Vice President (Medical), Vice President (Surgical) and Honorary Secretary.
As with her clinical work, she was dedicated and meticulous, caring enormously for individual students, especially those who required additional support.
Retiring in 2005 at the age of 65, she continued her interest in medical history, collecting the story and instruments of James Bouglas, a country doctor in Lanarkshire. These were the basis of a Micromuseum in the Medical School, opening in 2009. Marjorie gave so much to her patients and students and is fondly remembered by them and her colleagues.
Obituary supplied by Gordon Lowe, James McKillop and Harry Gray
Don’t miss your chance to have your say. To vote, visit: hub.ukevote.uk/rcpsg
Our election and online portal is being managed on behalf of the College by UK Engage. If you have any general or technical queries about the election process, please contact: support@uk-engage.org
EDITION 15 25
EDUCATION CALENDAR
For more information, visit: rcp.sg/events
Courses: In Person
Basic Surgical Skills
9–10 November 2023
21–22 March 2024
12 CPD Approved
This course is for trainees anticipating a career in surgery and preparing for basic surgical examinations. To help support your training journey all delegates enrolling on this course will automatically receive 30% off any further MRCS Preparatory Course.
Basic Orthopaedic Procedural Skills
24 October 2023
30 January 2024
26 March 2024
Learn the principles of skin suturing, plastering, digital nerve blocks, joint aspiration, emergency fracture treatment and spinal immobilisation.
Principles of Intramedullary Nailing
26 October 2023
This practical, one-day course introduces the principles of intramedullary nail fixation for fractures of the tibial and femoral shaft. The course will be taught by experienced orthopaedic surgeons with an interest in orthopaedic trauma.
Basic Surgery Cadaver Skills
30–31 October 2023
22–23 February 2024
This course is aimed at CT1 / ST2 level and will cover areas of the ISCP curriculum required for entry to ST3. Candidates should have previously undertaken a Basic Surgical Skills course.
IMPACT
30–31 October 2023
5–6 December 2023
23–24 January 2024
19–20 February 2024
4–5 March 2024
IMPACT (Ill Medical Patients’ Acute Care and Treatment) is a two-day course introducing the principles and practice of acute medical care and related knowledge, skills, understanding and attitudes.
Conscious Sedation in an Increment
7–8 November 2023
14 CPD Approved
This two-day course will provide a comprehensive overview of conscious sedation for the dental team. This will total 14 hours of verifiable CPD, fulfilling the 5-year IACSD requirement.
Surgical Skills for the Emergency Department Resuscitation Room
8–9 November 2023
9 CPD Approved
This is an innovative practical training course on the surgical techniques that can save lives. Experienced faculty members from a variety of clinical backgrounds will utilise cadaver, and other specially designed clinical models, to maximise the practical experience for course participants.
Basic Laparoscopic Skills
19 December 2023
11 March 2024
This one-day course is aimed at CT1 level with an interest in general surgery, paediatric surgery, urology and gynaecology. Delegates will become familiar with equipment and instruments used in laparoscopic surgery and can practise simulated procedures.
GI Anastomosis Techniques
22 November 2023
This one-day course provides exposure to the theoretical principles and practical techniques of gastrointestinal anastomosis. It gives an opportunity to perform a variety of surgical procedures on tissue models under the expert guidance of consultant surgeons.
Vascular Anastomosis Techniques
23 November 2023
This one-day course provides exposure to the theoretical principles and practical techniques of vascular anastomosis. It gives an opportunity to perform a variety of surgical procedures on tissue models under the expert guidance of consultant surgeons.
Endodontic Microsurgery Masterclass
7–8 December 2023
6 CPD Approved
This cadaveric course has been designed for dentists, specialist and speciality trainees with an interest or experience in endodontics and oral surgery.
Expert Witness Training for Medical Professionals
14–15 December 2023
12 CPD Approved
A comprehensive two-day training course to equip senior medical professionals from all specialties with the essential knowledge, confidence and support needed to succeed as a medical expert witness.
Events for all Physicians Surgeons Dental Surgery
Travel Medicine Podiatric Medicine
26 RCPSG.AC.UK MEMBERS' AREA
MRCS Part B Preparation
11–12 January 2024
This two-day course will prepare surgical trainees for the MRCS Part B OSCE Exam. The course combines online, flexible and independent learning with classroombased scenarios and preparation that benefit from direct interaction and feedback from faculty.
Surgical Approaches to the Upper Limb
12 January 2024
6 CPD Approved
This intensive cadaveric course is for experienced orthopaedic trainees (ST4 and above) and consultants to learn surgical approaches to the upper limb, with a focus on the management of trauma.
Head and Neck Dissection
18-19 January 2024
12 CPD Approved
This is a two-day, hands-on dissection course aimed at ST level trainees in Otolaryngology. The main aim of the course is to teach the surgical anatomy and steps of important head and neck procedures, using cadaveric material.
Vertigo Made Simpler – A practical course to stop you spinning in circles
6 February 2024
5 CPD Approved
This popular, practical course is designed for physicians, trainees and associated health care professionals seeing the dizzy patient in Acute Admissions Unit, Emergency Department, Syncope units, Falls services, TIA clinics and Outpatients.
Foot and Ankle Cadaveric Masterclass
16 February 2024
6 CPD Approved
This cadaveric course aims to equip trainees in approaches to the foot and ankle as well as modern surgical management of challenging conditions.
Prostate Cancer Training and Update Day
23 February 2024
Discover the latest clinical news and best practice on the surgical treatment of prostate cancer. Suitable for urology trainees, specialist nurses and consultants, with subsidised places available.
Foundation Skills in Surgery
16 March 2024
This course provides an introduction to the specific skills needed in the early stages of surgical training. It is suitable for foundation year doctors and final year medical students considering a career in surgery.
Procedural Skills for Medical Trainees
28 March 2024
This course is an excellent opportunity to develop your practical skills and gain knowledge in common IMT procedures.
Courses: Online
Royal College Advanced Certificate in Clinical Education
8 and 22 November 2023
31 January and 14 February 2024
27 March and 10 April 2024
A comprehensive two-day microteaching course suitable for postgraduates (CT1/ ST1/equivalent) and consultants involved in teaching delivery at advanced level
Training the Clinical Trainer
Various dates
12 CPD Approved
This course aims to enhance your knowledge of, and skills in, educational practice within a clinical setting. Designed for senior trainees across all specialties and mapped to CCT requirements, it will provide attendees with skills to meet the trainer criteria as set out in the GMC recognition of trainers’ requirements.
Performance Support for Doctors in Training
21 and 24 November 2023
19 and 22 March 2024
4 CPD Approved
This two-part course for senior clinicians focuses on how to manage doctors experiencing difficulties. The course will support you to identify concerns early, diagnose the issues and ensure effective intervention and support.
Urology ST3 Interview Preparation
2 February 2024
In this course, candidates preparing for the ST3 Urology National Interview Selection can gain a full understanding of what to expect and can optimise their interview technique.
EDITION 15 27
Developing the Clinical Trainer: Teaching skills for early stage trainees
20 February 2024
4 and 5 March 2024
Through online individual learning and live sessions, this course will provide foundation doctors and medical students with an overview of teaching, learning and feedback in the clinical environment
Orthopaedic and Trauma ST Interview Preparation
26 January 2024
This focused course aims to prepare candidates for the ST Orthopaedic interview. It offers a unique 1:1 real time experience of the interview process, to maximise exposure and potential.
General Surgery ST3 Interview Preparation
16 February 2024
This course aims to prepare candidates for the ST3 General Surgery interview, with in-depth understanding of what to expect, and a chance to refine interview technique.
Conferences: Hybrid (College and Online)
Medicine24
26–27 October 2023
12 CPD Approved
Returning for its ninth year, our flagship medical conference will provide upto-date information on the optimal management of acutely ill patients within the first 24 hours of admission.
TC White Conference: Problem Solving Leadership
10 November 2023
5 CPD Approved
This conference will cover a wide range of topics to aid optimising the patient experience and promoting staff wellbeing and morale. Throughout the day, you will hear from inspiring speakers focusing on problem solving leadership.
President’s Conference: Inequalities in Healthcare – What do we know and what can we do?
16 November 2023
6 CPD Approved
This hybrid conference brings together national and international healthcare leaders to hear how they have overcome the challenges of turning evidence into action, to reduce health inequalities.
Medical problems in pregnancy: optimising multi-disciplinary care
1 December 2023
6 CPD Approved
The programme is delivered by expert speakers and includes interactive casebased learning and engaging panel discussions. Topics to be covered include cardiac disease, renal disease, perinatal mental health and rheumatological disease, with an emphasis on collaborative cross-disciplinary working, and how to achieve this.
Scottish Orthodontic Conference
26 January 2024
6 CPD Approved
This event will provide an update on current topics and will give orthodontic teams an opportunity to get together and to focus on areas of fundamental importance to the delivery of contemporary orthodontics.
Respiratory Conference
2 February 2024
6 CPD Approved
This conference will update you on topical issues within respiratory medicine including COPD and lung cancer. Our keynote lecture will cover multi-morbidity along with an update on interstitial lung diseases.
Syncope Conference: Everyone's Problem
7 February 2024
5 CPD Approved
Syncope can go across many areas of medicine and involve any physicians in unscheduled care. This conference will serve to update your knowledge on acute assessment of syncope, how to risk stratify and emerging areas of interest.
Robotics in Colorectal Surgery Conference
1 March 2024
This one-day hybrid conference will feature up-to-date presentations from experts in colorectal surgery and robotics, case-based talks and panel discussions.
Orthopaedic and Trauma Conference
17 May 2024
6 CPD Approved
This one-day meeting, for all clinicians involved in orthopaedics and trauma, will feature clinical updates, topical presentations and lively panel discussions.
For more information, visit: rcp.sg/events
28 RCPSG.AC.UK MEMBERS' AREA
EXAMINATIONS CALENDAR
Physicians
MRCP(UK)
The Membership of the Royal Colleges of Physicians of the United Kingdom diploma is essential for all physicians who train in a medical specialty in the UK.
The three Royal Colleges of Physicians of the UK share this common membership examination in general medicine.
When all three exams are passed, successful candidates are eligible to become a Member of the Royal College of Physicians and Surgeons of Glasgow, and use the postnominals MRCP(Glasg).
MRCP(UK) Part 1
This entry-level exam is for doctors with a minimum of 12 months' postgraduate experience.
It covers a broad range of topics to ensure the level of knowledge is appropriate to physicians at this stage of their career. The exam is taken online (in the UK) or at a test centre (if based internationally).
Exam date: 24 January 2024
UK registration: 6–13 November 2023
Exam date: 17 April 2024
UK registration: 5–12 February 2024
MRCP(UK) Part 2 Written
This exam can be taken by physicians in training who have passed the MRCP(UK) Part 1 exam.
It builds on the knowledge assessed in Part 1 and tests the acquisition of medical knowledge, skills and behaviour.
The exam is taken online (in the UK) or at a test centre (if based internationally).
Exam date: 21 February 2024
UK registration: 4–11 December 2023
MRCP (UK) Part 2 Clinical (PACES)
The Practical Assessment of Clinical Examination Skills (PACES) is designed to test the clinical knowledge and skills of trainee doctors who hope to enter higher specialist training (ST3).
The exam, which takes place in person, sets rigorous standards to ensure that trainees are competent across a range of skills and they are ready to provide a high standard of care to patients.
Exam period:
Late January to 31 March 2024
UK registration: 13–20 November 2023
MRCP(UK) PACES ONLINE PREPARATION
Our comprehensive eLearning material contains guidance and top tips from examiners on the new PACES23 format. rcp.sg/paces23prep
MRCP(UK) SPECIALTY EXAMINATIONS
ESEGH
The European Specialty Examination in Gastroenterology and Hepatology (ESEGH) is a high-quality examination which ensures that certified specialists have sufficient knowledge of gastroenterology and hepatology.
Exam date: 3 April 2024
UK registration: 14 December 2023–10 January 2024
Respiratory Medicine
Candidates in UK training posts would normally take the Specialty Certificate Examination (SCE) in Respiratory Medicine in their penultimate year of higher specialty training.
Exam date: 17 April 2024
UK registration: 27 December 2023–24 January 2024
To find out more about sitting an MRCP(UK) exam with the Royal College of Physicians and Surgeons of Glasgow, visit our website: rcpsg.ac.uk/physicians/exams
EDITION 15 29
Surgeons
MRCS
The Intercollegiate Membership of the Royal College of Surgeons examination is run jointly with the other Colleges of Surgeons in Great Britain and Ireland.
Award of the MRCS diploma indicates that a candidate has enhanced their knowledge, understanding, experience and clinical competence well beyond primary qualification level.
Candidates will be eligible for election as a Member of our College if they successfully complete Part B of the examination with us, at one of our exam centres.
MRCS PART B OSCE PREPARATION COURSE
This course combines online, independent learning with two days of practical, in-person scenarios and a mock exam. Candidates benefit from direct interaction and feedback from faculty, so they feel well-prepared when taking their exam.
For the latest course dates, visit rcp.sg/events and search ‘MRCS Part B Preparation Course’.
Dental Surgery
MFDS
Award of the Diploma of Membership of the Faculty of Dental Surgery (MFDS) indicates that a dental surgeon has enhanced their knowledge, understanding, experience and clinical competence well beyond primary qualification level to the standard required to proceed into specialist training.
On passing Part 2, candidates will be invited to proceed to admission to the College as a Member.
MFDS Part 1
This online exam is for trainees in the first two years of postgraduate training. It aims to test the range of knowledge and understanding that underpins direct patient care.
Exam date: 9 April 2024
Closing date: 5 February 2024
MRCS Part A
The Part A examination takes place online at a test centre, and consists of a three-hour paper (Applied Basic Science) followed by a two hour-paper (Principles of Surgery in General).
Exam date: 9 January 2024
Closing date: 19 October 2023
MRCS Part B OSCE
The Objective Structured Clinical Examination (OSCE) uses examined stations to test candidates’ knowledge of anatomy, surgical pathology, applied surgical science and critical care, plus their applied skills (communication, history taking, clinical and procedural skills). In the UK, we use two excellent venues: Hampden Park Stadium in Glasgow and Ashton Gate Stadium in Bristol.
Exam dates:
UK: 8–9 February 2024 in Glasgow, 16 February 2024 in Bristol
Closing date: 16 November 2023
International: 27–28 February 2024 in Pune, India
Closing date: 30 November 2023
Further dates and exam centre locations will be announced on our website.
MRCS (ENT) OSCE
This two-part exam tests the breadth of knowledge, the clinical and communication skills and the professional attributes of doctors wishing to join an otolaryngology department in a trainee position, or for GPs who wish to offer minor ENT surgery.
Exam dates:
19 February 2024: Online
28 February 2024–1 March 2024: Edinburgh
Closing date: 30 November 2023
FRCS(Ophth) Part 1 and 2
Award of the Diploma of Fellowship of the Royal College of Physicians and Surgeons of Glasgow indicates that a candidate has a sound knowledge of the scientific basis of ophthalmology and is experienced and competent at applying that knowledge.
Exam date: 12 March 2024
Closing date: 5 January 2024
To find out more about sitting a surgical exam with the Royal College of Physicians and Surgeons of Glasgow, visit our website: rcpsg.ac.uk/surgeons/exams
MFDS Part 2
The Objective Structured Clinical Examination (OSCE) uses examined stations to test candidates’ clinical competence by assessing their communication skills and their knowledge, understanding and management of a range of common conditions. Our exam centres are typically in Glasgow and Manchester, UK, and in various locations internationally. Future dates and exam centre locations will be announced on our website.
MFDS REVISION MODULES
These modules have been developed to give candidates the necessary knowledge about key areas of the exam: rcp.sg/mfds1revision
MFDS QUESTION BANK
The Example Question Bank is designed to prepare candidates for the exam: rcp.sg/mfds1questions
To find out more about taking an MFDS exam with the Royal College of Physicians and Surgeons of Glasgow, visit our website: rcpsg.ac.uk/dental-surgery/exams
30 RCPSG.AC.UK MEMBERS' AREA
NEW MEMBERS WELCOME TO ALL OUR
JANUARY - JULY 2023
PHYSICIANS
Fellow qua Physician
Mohamed Salah Eldin Mohamed Abdel Kader
Mohamed Mahmoud Abdelghany
Pramod Kumar Agrawal
Kazi Abdullah Al Mamun
Nithyanandam Allimuthu
Mustafa Alqaysi
Sajid Ansari
Tahir Ansari
VijayKumar Antappa
Ravi Arora
Bapilal Bala
Smarajit Banik
Ayman Sharafeldin Ibrahim Bannaga
Yashodhara Byagoti Math
Yap Hang Chan
Yu Ho Chan
Saleh Muhammad Channa
Mei Chih Cheng
Asok Cheriyan
Md. Niamul Gani Chowdhury
Arup Dutta
Hazem El-Bilbeisi
Mahmoud Farouk Elmahdi
Mohammed Fareeduddin Farooqi
Dilip Kumar Ghosh
Raja Ramesh Gummalla
Arvind Gupta
Rizwan Hameed
Deepa Mohan Lal Hemnani
Nai Chien Huan
Muhammad Khalid Idrees
Hing Lung Ip
Meenakshi Jain
A. K. M Shamsul Kabir
Amin Lutful Kabir
A T M Rezaul Karim
Kashif Khan
Zahoor Aslam Khan
Md. Nur-A-Alom Khan
Salman Khwaja
Ryan Lap Yan Ko
Sudheer Koganti
Praveenkumar Korothu Parambil
Yew Fung Kwan
Chun Kit Kevin Kwok
Ka Luen Lui
Debkrishna Mallick
Lucy Elizabeth McGeoch
Md. Nurul Amin Miah
Riyaz Mohammed
Hanif Muhammad Mustafa
Kei Yan Andrew Ng
Yong Muh Ng
Andrew Agada Okpe
Nagaraja Rao Padaki
Kok Wei Poh
Prasannakumargupta Pokal
Matthew Mammen Puliyel
Malik Anas Rabbani
Arunkumar Radhakrishnan
Shabbir Khan Rajan Rawther
Nadeeka Rathnamalala
Sameh Emil Sadek Zaky
Syamlal Sasidharan
Sarbani Sengupta
Syed Ibrahim Ali Shah
Kai Cheuk Sin
Santosh Singh
Thein Htat Thein
Sunny Chun Fung Tsang
Md. Salahuddin Ulubbi
Khin Thandar Win
Sze Wai Yeung
Member qua Physician
Ghada Osman Abdelrahim Ahmed
Anand Alagappan
Nadia Al-tameemi
Osagioduwa Mike Atoe-Imagbe
Mohamed Ibrahim Bayoumy
Jaclyn Elizabeth Carberry
Laura Duffy
Annu Susan George
Kerri-Marie Heenan
Sourab Hiremath
Khin Myat Hla
Lijo James
Phyu Hnin Khaing
Md. Shahjalal Khan
Fasiha Kiran
Eleanor Klejnow
Chin-Yong Kok
Rachel Mauchlen
Jothiswaran Namasoo
Robert Osborn
Agbonmeire Awele Osiki
Nithya Rajendran
Sankanika Roy
Katie Sadler
Talal Safdar
Nazar Ulla Syed
Patrick Harold Thompson
Rebekah Toner
Lindsay Whyte
Kyaw Zay Ya
Rebecca McCall
Max Reiser
Member of the College
Anand A.
Samy Abdellatif
Muhammad Abedur Rahman Bhuyan
Akhtar Ali
Sophie Victoria Barrett
Darren Dookeeram
Mohamad Habli
Mohammed Emdadul Haque
Alice Harpur
Muhammed Kamrul Hassan
Muhammad Irfan
MD. Atikul Islam
Aneesh Bava K
AKS Zahid Mahmud Khan
Ramaning Loni
Ahmed Mahmoud Attia
Karan Malhotra
Rida Mansoor
Omer Aziz Mirza
Hassan Mortagi
Muhammad Aneel Razzaq
Muhammad Umer Salim
Muhammad Shahzad Shabir
Sharker Mohammad Shahadat Hossain
Asif Zaidi Syed
Aman Yadav
Saba Zartash
EDITION 15 31
SURGEONS
Fellow qua Surgeon
Mohamed Abdelazeem
Timothy Averch
Sara Best
Brendan Carr
Abhideep Chaudhary
Prof Dr Ravi Kumar Chittoria
Mohammad Ismail Hossain
Sanjay Kumar Jain
Sujit Jos
Badrinath Konety
Bhaskara Mallipudi
Chander Mohan Mittal
Mujeeburahiman Musliyarakath
Probal Neogi
Nalin Ruvinda Palehepitya Gamage
Jay Raman
Prashanth Rao
Surya Rao Rao Venkata Mahipathy
Kumar Ratnesh
Siddharth Mahesh Shah
Pravin Suryawanshi
Alaaeldin Tawfik
Nirmal Coumare Venkataramamujam
Nishantha Laksman Weerasinghe
Peter Wiklund
Lee Zhao
Mohammad Hassan Abbas Abdallah
Ahmed Hamid Ibrahim Al-Tameemy
Belal Mosaad Mohammmed Elber
Chi Heng Fung
Pranaw Kumar
Fellow qua Surgeon in Ophthalmology
Amani Mohammed Abd El Salam Abd
Elhalem
Dalia Salah Elsayed Abdelrahman
Fayrouz Mohamed Aboalazayem Mohamed
Abo Alhassan
Mohammed Abouelsaad
Hima Bindu Adusumilli
Manar Hamad Alnajjar
Ali Al Mafrachi
Mohamed Asem Alemary
Divya Alex
Mustafa Saber Hafez Mohamed Ali
Moataz Ahmed Khairy Mohammed Ali
Raghad Bdewi Mohmmad Al-Kubaisi
Amani Suleiman Abdelhalim Almanasrah
Zainab Qayssar Mahdi Al-nidawi
Haydar Rahman Shakir Alramahy
Yasser Kasim Rumy Al-Rubiay
Sarah Alshamarti
Ashraf Alzboon
Tamanna Binthu Abdul Azeez
Sanjana B Singh
Ahmed Said Ahmed Abdel Aziz Bardalah
Mohammad Hasan Awwad Bayoumy
Syed Imran Burhan
Ali ElHussainy Ali Mohamed ElAnwar
Mostafa Amr Azzab El-Bahrawy
Rania Abdelfattah Hussein Mahmoud
Eldakhs
Mohamed Hassan Husseini Elmesalami
Hala Abdulmula Elmosrati
Moustafa Mohamed Mohamed Amin
Mohamed Elsayed
Abdelrahman Magdy Farahat Farahat
Mona Abdelfatah Mohamed Gadalla
Sumatee Gerald
Jylan Ahmed Mohamed Gouda
Sahana Gowda M
Mohammad Husni Ahmed H.Dawood
Mustafa Hasoun
Mohamed Amin Mahmoud Abdelhamid
Heikal
Ismael Mostafa Ismael Ibrahem
Vivekaraj Jairaj
Maria Javed
Yamen Jazaeri
Keerthana K. E.
Rama Purushottam Kalantri
Mohammed Mahmoud Mohammed
Mahmoud Hassan Kaoud
Ahmed Mahmoud Mohamed Omer Kenawy
Bayan Awni Mohamad Khasawneh
Ghada Basouney Ghareep Hussein
Khomkhom
Logandran Vijaya Kumar
Anala Maharaj
Ashish Markan
David J Mathew
Yasmin Mohamed
Hend Mohammed Safwat Ahmed
Mohammed
Ahmed Amr Mohamed Mohssen
Kieron Garrett Naguar
Walid Osama Abdel Rahman Nour El Din
Ahmed Obaidi
Sushma Sadashiva Poojary
Qirat Qurban
Faheem Raja
Ramya Ramachandran
Mahmoud Ashour Ramadan
Sonali Rao
Evangeline Rao
Ahmed Reda Hasan Aly Donia
Arshiya Saini
Shanthini Sathiaraj
Mai Nasser Abdelmohsen Sayed
Ankit Shah
Ahmed Ibrahim Ahmed Elsayed Shokr
Rita Mary Tomy
Saji Valiparambil Krishnanunny
Nisrein Basem Husni Yaaqba
Saumya Yadav
Ziad Zidan
Fellow in Plastic Surgery
Karima Medjoub
Fellow qua Surgeon in Plastic Surgery
Nursheila Izrin Bte Abu Zaki
Teck Ree Law
Fellow qua Surgeon in Urology
Yeap Siu Hui Amelia
Ling Sing Ch'ng
Ooi Chin Chuan
Arvind Vashdev Jagwani
Arshvin Kesavan
Jia Lun Kwok
Li Yi Lim
Benjamin Lim Tze Ying
Shu Hui Neo
Kanesh Kumaran Seevalingam
Suzliza Shukor
Fellow in General Surgery
Peter Gordon Alexander
Muhammad Shahzad Javid
Katrina Anne Knight
Erin Catherine McIlveen
Anu Sandhya
Stacy Wardle
Fellow in Otolaryngology
Mohammad Adeel
Patrick Daragh Chakravarty
Kasirajan Saravanan
Fellow in Trauma & Orthopaedics
Fraser John Henderson
William Thomas Wilson
Fellow in Urology
Waduthanthri Supun Lakmal De Silva
Kenneth Tze Seng Hiew
Alastair Crawford McKay
Mark Salji
Member of the College
Naveed Ali Shair
Akshay Agnihotri
32 RCPSG.AC.UK MEMBERS' AREA
Zeeshan Ahmad
Salman Ahmed
Mehtab Ahmed
Muhammad Ahsan
Mohad Asim Aideh
Firas Attallah Razej Al UBaidy
Syed Danish Ali
Rao Nouman Ali
Hasanain Al-Tamimi
Hafiz Salman Asif
Saadia Aslam
Nasir Bakhtiar
Dnyanesh Belekar
Nishant Bhatia
Md. Mukhlesur Rahman Bhuiya
Tofael Hossain Bhuiyan
Durr-I- Chaman
Sumant Naginbhai Chavda
Majid Dastgir
Bashar Dawud
Muhammad Ammar Hafeez Dogar
Nilotpal Dutta
Muhammad Zoha Farooq
Tayyaba Fatima
Mazhar Ul Hassan
Ahmed Hussein Alhaaj
Osamah Ibrahim
Maryam Iftikhar
Mohammad Inam
Muhammad Waqas Iqbal
Vikas Jain
Usba Jameel
Tamoor Ahmed Jatoi
Farrukh Javeed
Syed Muhammad Khalid Karim
Rajiv Kaul
Sher dil Khan
Awais Ali Khan
Aamir Imtiaz Khan
Muhammad Farhan Khan
Noman Khan
Ramish Kumar
Hammad Afzal Malik
Akram Muhammad Aliuddin
Areej Muhammad Salim Habib
Rubab Nafees
Hafiz Ahmed Nazmul Hakim
Iffat Noureen
Jitenkumar Harshadbhai Panchal
Adam Carl Philipoff
Muhammad Taqi Pirzada
Ramesh Radhakrishnan
Kumar Rahul
Usama Bin Saeed
Dr. Heemel Saha
Kazi Shameemus Salam
Maria Saleem
Ayyanathan Shivanraj
Lakshmanan Somu
Sivaviganesh Subramanian
Zaeem Sultan
Shah Tahir
Najam Ul Hassan
Sajjad Ullah
Fazali Wahid
Imdad Ahmad Zahid
Sohail Zia
Member qua Surgeon in ENT
Reda refaat Elsaid Abdelaal
Tan Dexian Arthur (Chen Dexian)
Satnam Singh Rehal
Helen Rooney
Prateek Soni
Rayah Ahmad Ibrahim Tarawneh
Member qua Surgeon
Hasan Mohammad Ali Abdallah
Ahmed Abdelfatah Abdelaziz Basha
Mohamed Sameem Abdul wajeed
Amir Faliq Abdullah
Mutaz Gumaa Mohamed Ahmed
Abdiaziz Ahmed Mohamed
Samuel Akintunde
Ezzat Al badawi
Ali Alhamdi
Sattar Al-Husseini
Almigdad Ali
Kamal Al-Jawdah
Kaluwelle Mudalige Vishva Randhara Alles
Anniestan Antonyrajan
Matthew Arnold
Arulprashanth Arulanantham
Pragalathan Balakrishnan
Landekumbura Mudiyanselage Prasad
Madushanka Bandara
Mohit Bhatia
Kamran Faisal Bhopal
Rachael Boardley
Caitlin Brennan
William Joseph Brown
Emmanuvel Shanthakumar Croos
Chathura Shalitha Madushanka Dampe
Gamage
Hewa Fonsekage Damitha Gihan De
Fonseka
Mahee Jeewantha Dissanayake
Samath Theeraka Ekanayake
Lauren Anne Elliot
Mowafag Elsayed
Maysara Hassan Ibrahim Elsiddig
Dinesh Karna Emmaneni
Palamandadige Chamal Shanura Fernando
Giovanni Preciado Ferrara
Christy Denyraj Francis Xavier
Nityanandan G
Chloe Louise Gelder
Asma Ahmed Yahya Hassan
Bruce Hay
Herath Mudiyanselage Kasun Bandara
Herath
Herath Mudiyanselage Mahendra Neranjan
Bandara Herath
Riham Ibrahim
Abdurrahman Islim
Assaddume Gedara Nalaka Pradeep
Jayasinghe
Ahmad Kaleem
Jayasundara Mudiyanselage Sathyajith
Karunarathna
Anuj Lal
Fiona Elizabeth MacDonald
Prabath Madhuwantha
Nuwan Darshana Masakorala
Luke McElroy
Megan McWade
Mohammed Nabil Mohammed Nassardeen
Harivallavan Nagenthiram
Rebecca Nail
Gowcikan Navanesan
Ashwani Kumar Nugur
Stephen Olphert
Bronte Paice
Alasdair William MacMillan Pollock
Razick Mohamed Raayiz
Layth Rasool
Chiran Rathnaweera Patabendige
Amr Mohsin Tahsin Rifaat
Iona Robertson
Ruwanpathirana Neranga Samarasinghe
Achala Samarasinghe
Dishan Randika Samarathunga
Theivaagar Santherasegaram
Keddagoda Gamage Vinod Saranga
Shiyanth Selvantharajah
Ramy Shaalan
Rajesh Babu Shrestha
Abhimanyu Singh
Sivakaran Sinnathurai
Robert James Spencer
Sivagnanasundarampillai Thivvika
Prabuth Dulanjan Weeraddana
Chamini Dilupa Priyadarshanie Weerasinghe
Pathirathnahalage
Halgaha Withanage Thushara Dananjaya
Wijayaratne
EDITION 15 33
Member qua Surgeon in Ophthalmology
Noor Hussain Abady
Majdi Abdulhamid Miftah Abdala
Maab Abdelgwad
Noor Jahan Lashkaran Ghulam Al Belushi
Yasmin Mohsen Saeed Albatarny
Ahmed Najm Abdullah Alfdhieh
Alia Fathi Ali
Eman Sayed Ahmed Ali
Humaid Sulaiman Khalfan Al-Kalbani
Asmaa Mohamed Ismail Abdelkader Alkolfat
Mustafa Dhafer Yasir Almarzooq
Salwa Alsaadoun
Hend AlSafran
Laylay Andeesh
Ann Tresa Antony
Zahra Arsalan
Muhammad Imran Asif
Sanaullah Askaney
Meenakshi Ct
Keerthi Duggineni
Mohamed Eid
Mohamed Usama Kamal Elabbasy
Omar Elbaha
Marwa Ebrahim Elsebaay Eldesouky
Mohamed Gamal Fahmy
Fizzah Farooq
Hosam Mohammad Salaheldeen Atef
Mohammad Salaheldeen Gad
Ranpati Dewayalage Gaveesha Gayashan
Gunasekara
Munawar Habib
Sherein Hagras
Hossam Eldin Hasan Soliman Ebrahim
Shimaa Hashish
Su Myat Hlaing
Mohammad Ali Imtiaz
Manishka Indunil Jayasundera
Priyanka Kakar
Muhammad Rizwan Khan
Lawrence Kindo
Abhinav Loomba
Ashish Mahobia
Mariya Nazish Memon
Rahul Menon
Rabbia Mirza
Ahmed Gamal Elsayed Mohamed
Hameed Obedulla
Ajibola Toyin Oluwaniyi
Zezawar Oo
Thet Nwe Oo
Kochami P A
Feriyal P M
Vaishnavi Ravishankar
Abdullah Ragab Abdullah Saad
Paula Sedhom
Marco Albert Erian Seif
Saba Shaikh
Mary Atef Prince Shaker
Mustafa Ali M Shata
Nair Soman Sukumaran
Yamon Thant Syn
Bashar Hussein Theyab Al-Majali
Mina Magdy Berty Wanis
Sisira Kumara Welahettige
Heather Krystal White
Nang Yamon Khin
Seng Hong Yeoh
Royala Zaka
Mohammad Shaban Mohammad Zidan
Hsu May Zin
Associate Membership of the College
Stephen Novak
DENTAL SURGERY
Fellow in Dental Surgery
Anirudh Balakrishna Acharya
Salah Al-Din Al-Azri
Yasin Alavi Aruveetil
Josephine Camilleri
Naseer Ahmad Chaudhry
Daniel Tak Sang Fang
Nyer Firdoose Chintamani Subhan
Mohammed Zakir Hossain
Mohammed Ibrahim
Islam Mohamed El-Said Kassem
Praveen Kumar S
Dae Hyun Lee
Tsun Ma
Natashekara Mallesh
Farzin Mirzaeeyan
Ciaran Eoin Moore
Faisal Muhammad
Sathish kumar Nadanasigamani
Rajesh P
Shankargouda Patil
Alexandra Claire Perks
Dr Suneel Kumar Punjabi
Saravanan Rethinam
Abdelfattah Sadakah
Hamed Shaheen
Jayakara Shetty
Dania Tamimi
Tulika Tripathi
Fellow in Dental Public Health
Sarah Kaddour
Fellow in Oral Medicine
Daniel Joshua Finn
Sandra Marina Soeima Goncalves
Fellow in Restorative Dentistry
Hamzah Ahmed
Sarah Garner
Member of the Faculty of Dental Surgery
Kareem Abou el Neel
Sara Adel Ismail Youssef
Abayen Ahilan
Deepal Ajmera
Ali Al Bayati
Mohamed Sayed Mohamed Aly
Lewis Arbuckle
Andrew Aschaber
Zartash Ashraf
Dr. Muhammad Aqeel Aslam
Anuj Bhargava
Amy Browne
Chris Cairns
Lue Hang Chan
Ching Yi Chan
Tai Wai Chan
Lucy Charles
Chun Hei Alvin Chau
Yu Hin Cheng
Venetia Cheung
Wing Yan Cheung
Tsz Tsun Chiu
Cho Kiu Chung
Mollie Clark
Sean Daley
Rajesh Damarasingu
Heather Dawar
Carlos Fernando de Almeida Barros
Mourao
Pankaj Dhawan
Kirsty Skye Dickson
Huda El Wahed
Abdelrahman Elbeltagy
Mohamed Elsayed
Mohideen Salihu Farook
Helen Fegan
Caitlin Finney
Wing Yan Fong
Man Man Fong
Jacqueline Fraser
Padmashini Gnanam
Khyati Gupta
Hany Harby
Sana Haye
Katie Huane
34 RCPSG.AC.UK MEMBERS' AREA
Ka Po Hung
Yuen Man Hung
Hira Iqbal
Emily Elizabeth Jane Ireland
Joshua Jackson
Sadia Kaleem
Yee Ting Alice Kan
Muhammad Kashif
Taranjit Kaur
Ross Malcolm Keat
Polly Kent
Muhammad Adnan Khan
Ahmed Saeed Abdelkader Khayamey
Mehreen Anam Khokhar
Rahail Kumar
Martin Laird
Vanessa Lam
Chi Yan Lau
Yee Ting Lau
Ka Wing Law
Ngo Hin Lee
Yan Yan Lee
Catherine Ka Wing Lee
Tsz Yan Leung
Tsz Choi Alvin Li
Yee Man Li
Sahrish Liaqat
Yuen Ting Liu
Wing Lam Luk
Fathima Hafila M I
Shorouk Mahgoub
Chung Kan Mak
Wing Hang Bella Mak
Pui Ying Mak
Yu Hei Mak
Karolina Justyna Maluga-Siek
Rupert Mazareanu
Aoife Alexandra McDougall
Niamh McGirr
Rashid Mehmood
Arshad Mir
Ayesha Mohamed
Kathryn Ruth Morrow
Ahmed Mostafa
Rhyanna Mughal
Maria Mullerat-Pigem
Aristotelis Mylonas
Saqib Naeem
Monica Nathan
Ashiwin Nehrudhas
Chi Tsam Ng
Clarissa Ju Cheng Ngiam
Heather Sze Yan Pang
Christine Park
Hemish Patel
Anouska Patel
Minesh Popat
Prathibha Prasad
Navya Keerthana Rajupalem
Sajjad Salam
Shakirah Samsuri
Graeme Shaw
Raeed Mohammed Sheikh
Samarth Shetty
Megan Shields
On Ki Shum
Kwan Kit Sin
Har Amrit Singh
Yasser Soliman
Hannah Son
Stella Stasiak
Nessma Sultan
Mustafa Tahir
Lok Yan Tam
Sonam Thakkar
Amy Thomson
Man Wai Tsang
Pak Chuen Tsui
Yahya Turki
Muhammad Uzair
Satish Vasanth
Sathyadeep Vijayendra
Richard Walton
Kayleigh Marie Whyte
Harriet Grace Wilson
Yan Ting Wong
Fung Yee Wong
Hoi Shuen Wong
Ka Chai Kevin Woo
Felix Ho Won Wu
Cindy Xie
Elvin Yip
Member in Orthodontics
Ahmed Muhamed Esmael Saad Abusen
Manar Algindy
Muhammad Farhan Ali
Hasan AL-Nuaimi
Wasila Jamil Alsadi
Mohamed Sayed Mohamed Aly
Diana Ashok
Jun Ai Chong
Amr Mohamed Maher Ali Ebrahim Daoud
Mohamed ElGhamry
Mostafa Adel Mohamed Ali Hassan
Mahmoud Khedr
Ashwin Kumar
Maha Ahmed Shehata Abdel Aziz Mohamed
Basil Mahmoud Mumtaz
Niha Naveed
Robin Mathew Neerumtharappel
John Thomas
Abraham Thomas
Haytham Abdehamid Hasanin Tony
Nisha Varughese
Jasleen Kaur Walia
Mina Zakhary
Member in Paediatric Dentistry
Hilton Hiu Chun Chiu
Yuxin Yang
Member in Periodontics
Melissa Fok
Member in Prosthodontics
Mohideen Salihu Farook
Member in Restorative Dentistry
Jun Fay Low
TRAVEL MEDICINE
Fellow in Travel Medicine
Hamad Eid H R Al-Romaihi
Jason Biswas
Theodore Cieslak
Mark Kortepeter
Member of the Faculty of Travel Medicine
Martin Anthony Williams
PODIATRIC MEDICINE
Fellow in Podiatric Medicine
Matthew Carroll
Johann Francois Goyvaerts
Amanda Killeen
Ji Soo Kim
Caroline Leverett
Eric Lullove
Simone Karen McConnie
Tiziana Mifsud
Liam Stapleton
Phillip Ward
Daniel Aharon Weisz
Member of the Faculty of Podiatric Medicine
Amy Jessica Curran
Wasim M Dar
EDITION 15 35
Leading the way in Non-Clinical Skills Training
Develop your teaching, coaching and leadership skills at every stage of your career with our range of non-clinical skills courses.
Education and Supervision
Developing the Clinical Trainer Teaching skills for early-stage trainees
Training the Clinical Trainer Teaching skills for senior trainees
Royal College Advanced Certificate in Clinical Education
Leadership and Professional Development
Introduction to Mentoring
Discover the principles of mentoring; for all in the healthcare sector

Mentorship Programme
Learn how to coach and support others as a mentor
Performance Support for Doctors in Training
Learn how to manage trainees who are experiencing difficulties
Practical Advice for New Consultants
Guidance for a smooth progression to being an established consultant
Patient Safety and Quality Improvement
Expert Witness Training for Medical Professionals
For senior medical professionals
A comprehensive course for senior trainees and consultants teaching at an advanced level Visit
Leadership Development Scholarship Programme
Fully funded programme for individuals from underrepresented groups to develop leadership skills both in clinical practice and positions of academic study

our website to see upcoming course dates and book your place:
rcp.sg/nonclinical
















 The staircase leading up to College Hall at our College building in St. Vincent Street, Glasgow
The staircase leading up to College Hall at our College building in St. Vincent Street, Glasgow




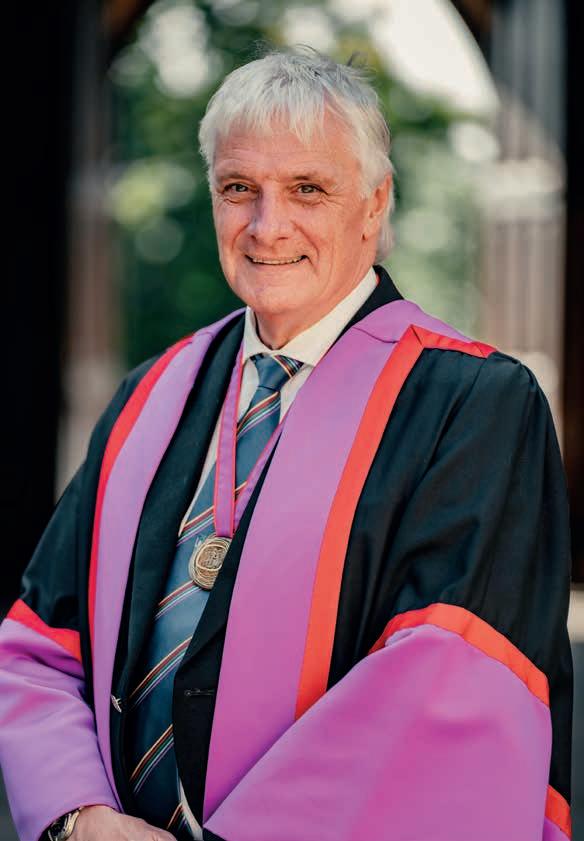
 Photos: Jamie Simpson / Royal College of Physicians and Surgeons of Glasgow
Photos: Jamie Simpson / Royal College of Physicians and Surgeons of Glasgow








 Dr David Ritchie and Dr Patrick Grant celebrate with their President's Medals
New members of our Faculty of Travel Medicine
Dr David Ritchie and Dr Patrick Grant celebrate with their President's Medals
New members of our Faculty of Travel Medicine









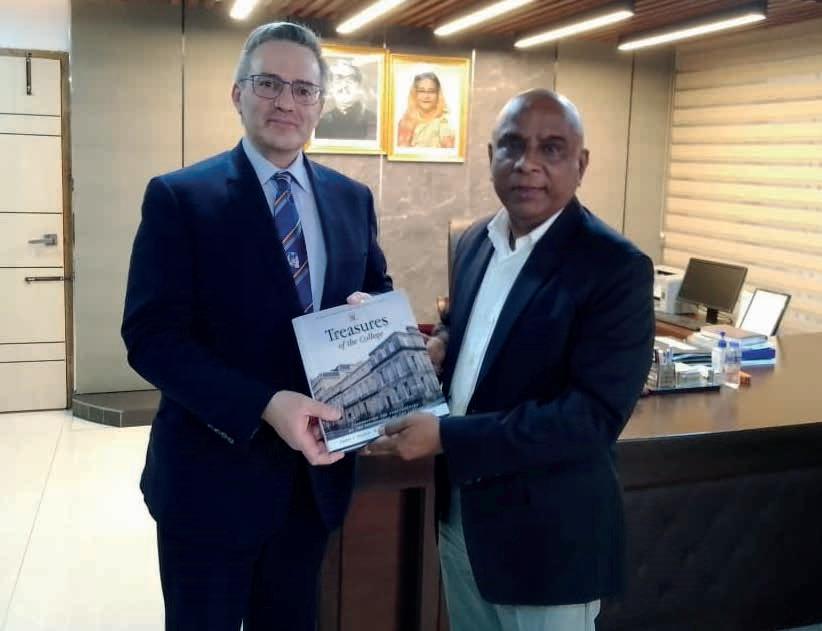

 Professor Sir Michael Marmot Professor of Epidemiology at University College London, Director of the UCL Institute of Health Equity
Professor Sir Michael Marmot Professor of Epidemiology at University College London, Director of the UCL Institute of Health Equity
 Professor Bola Owolabi Director of Healthcare
Professor Bola Owolabi Director of Healthcare
 NHS England
NHS England