

Rarity
Dear Reader,
We have been working hard on issue 13 of Rarity Life magazine these past few months, and as always we really hope that you enjoy reading it just as much as we have enjoyed the process of bringing it to life. It is a true honour and a privilege to be entrusted to share your stories.
We are delighted to be able to share that we have secured funding to build on the work of our pilot project, ‘What matters most?,’ which amplified the voices of individuals with a life shortening illness as well as those of caregivers and healthcare professionals. ‘Dying to be Heard’ will seek to implement impactful discussions and provide essential support to communities through focusing on compassionate care, effective communication, and the dignity of the individual. The aim is to ensure that every voice is heard during the end-of-life process.
Rarity Life is an online publication that offers those affected by rare disease, disability and cancer the opportunity to create content that is truly inclusive. A platform to unify our collective experiences and to celebrate and share our differences.
As ever, we’re so grateful to everyone who contributes their time, effort and stories to this magazine, and to Same but Different. Thank you for taking the time to read Rarity Life, and please do share it far and wide. As always we welcome your thoughts and ideas for future publications, we love hearing from you.
Happy reading,
Same but Different




conversation with Nancy Di Salvo, Director of International Affairs for The GBS
conversation with Kate Farnell MBE, Founder & CEO of the Butterfly Thyroid Cancer Trust
to the Artist Charlie French
Dying to be Heard
We are delighted to announce that Same but Different have secured funding to build on the work of our pilot project ‘What matters most?’ which amplified the voices of individuals with a life shortening illness as well as those of caregivers and healthcare professionals.
The success of our initial pilot project revealed the urgent need for improvements and highlighted the necessity for more open conversations about death and end-oflife care. Building on that foundation, ‘Dying to be Heard’ seeks to implement impactful discussions and provide essential support to communities. Focusing on compassionate care, effective communication, and the dignity of the individual, the aim is to ensure that every voice is heard during the end-of-life process.
Through this project we aim to further work with the end-of-life care (EOLC) community and use our creative approach to

amplifying the voices of those within the community. We wish to collaborate with the incredible organisations that work in this landscape with the aim of improving the living with dying experience and make it accessible to everyone. Our initial focus will be on North Wales, however, that does not preclude us from building on relationships in other areas.
Through our work we would like to use our creative approach to further develop our exhibition to include a diverse library of powerful images, impactful written narratives and raw and honest films that can be utilised in collaboration with our partners. Some of the ways that we can do this includes:-
• Working with partners we can share our resources

for use at conferences, community events and as discussion points.
• Co-hosting events around the theme of Living well, Dying better.
• Promoting partner events, information and raising awareness of the work done to support the EOLC.
• Create a local route map of community support and services for when someone is dying to support them and their carers.
We are grateful to National Lottery Community Fund Wales for their support.
In this image you can see one of the scenes we created to highlight the themes identified as part of the ongoing project. It highlights the difficulties patients face when they fall between services during their end of life journey.
You can see the ‘What matters most?’ exhibition on our website:
View here
If you would like to collaborate with us on this project please contact us

A LIFE BY PAIN
In conversation with Janneke Peperzak
“The friends that I have nowadays know that if I’m tired and I have to cancel the plans we made that it is not because of them. They know, and understand, that although I would love to go out and to do things with them, sometimes I just can’t.”
When the video connects on our call the first thing that strikes me about Janneke is how well she looks; a beautiful and immaculately presented twenty-five-year old with a warm smile which radiates a positive energy. But, as is so often the case with rare diseases and invisible disabilities, her reality is a far more complex one.
Janneke lives with her parents and her dog in Wijchen, a small village near a city called Nijmegen in Holland. She also has three older brothers, and a small, supportive circle of friends. Over the years she has had to learn how to balance her dreams of living a full and active life with taking care of herself, and giving her body the rest it needs. Accepting that the dreams you have for your future are not dreams that your body can sustain is an incredibly hard thing to do, but it is something that she has had to do.
“In 2008 when I was eight-and-a-half years old my mum saw that I was not really able to control my feet properly, that I had to look at them to lift them up so I could step forwards. I had also had a lot of pain in my muscles for the previous couple of weeks, but my mum had thought it was just that I was growing, but when she saw that I was looking
where to place my feet she made an appointment at the doctors. When they were assessing me, they saw that my reflexes did not work, so that set off an alarm bell for them and they sent me to the hospital. I went to see a doctor who was a specialist in GBS/CIDP (for a description of both see pop-out box below). He asked me to walk in the hallway, and after just a few metres he said ‘I think your daughter has GuillainBarré syndrome, or GBS.’”
Janneke explains that as she was so young she didn’t truly understand, or know much about what was going on. But she immediately knew that there was something very wrong, because her parents both cried, and she could see the impact of these words on them, and their fear, shock and worry. “The doctor said ‘your child has GBS.’ They asked him what it was, as they had never heard of it and he explained that ‘your daughter is going to be paralysed, all of her muscles can stop working because of it, so it can also affect her lungs and heart.’ And when they were told that they cried a lot.” As part of the tests needed, she had to undergo a painful lumbar puncture (a procedure used to collect a sample of spinal fluid for analysis), and just 24 hours later paralysis set in.
“I was fully paralysed from my head to my toes, I couldn’t do anything. They put me on the heart monitor, I remember that they put me on the wrong one, it was for babies so it kept going off. My Dad stayed with me, he slept next to me so I was not alone, but it was a very

frightening, hard time, and a bit of a roller coaster. After about ten days I could stand a little bit and walk, though I couldn’t lift my feet properly. I was given physiotherapy, occupational therapy for my hands and some infusions and I slowly got a bit better.” Her recovery was not a complete recovery, and she experienced frequent relapses. “There were many periods when I was in so
much pain, and I was so tired, that I slept for twelve hours a day, I only really woke up for something to eat, or to go to the toilet or brush my teeth, and then I had to go back to bed.”
GBS is an acute autoimmune condition, which occurs when the immune system attacks the peripheral nerves, and typically an individual experiences a rapid onset
of muscle weakness which can lead to paralysis.
“Mostly its adults who get the disease and not children, and when they get GBS even if they get paralysed, like me, they recover and get better, though they might be left with some more mild symptoms like pain in the hands or feeling more tired. For me every time I got a little bit better, I relapsed and that’s not a typical
thing for GBS, so they sent me to a specialist Children’s Hospital in another city. Once there they did many more tests, and then they found out that I actually have CIDP.” The symptoms of CIDP tend to develop more slowly, and continue over a longer period, and they are also far more likely to reoccur, as such CIDP is considered to be the chronic form of GBS.
Unsurprisingly the pathway that Janneke’s life was on changed with the onset
of her rare disease, and CIDP has demanded much from her. When she was well enough to return to education this was initially at home, “for my homeschooling they had a screen in the classroom, and then using Skype I could follow the lessons. I had a walkie talkie near me, so if I needed to go to the toilet, I could call my mum to come upstairs and help me.” During her periods of better health she could return to school, but even when physically present
she was not always able to join in fully. Inevitably this had an impact on her friendships, because as she notes “there were a couple of friends that didn’t want to see me again, but I think it was because we were so young that it was more that they felt ‘oh she can’t play with me so I’ll go to look for someone else who can,’ rather than it being because they didn’t like me.”
After school Janneke began a course at college

studying to become a makeup artist, a dream course in many ways as doing makeup is one of her favourite activities, and the course represented an opportunity to turn a hobby into a job. She explains that one of the things that brings her the most joy is sitting in her studio at home, and working on looks. “When I work on a look it might take six hours, so I need to plan for a whole day. Beforehand I will have an idea, I research on Pinterest, Tik Tok and Instagram and get some of my inspiration there, but then I put it together and make something that is my own. The whole process gives me joy, and although I’m very tired afterwards it also gives me energy.” She continues, explaining that as doing makeup largely only involves using her hands, ‘which are the only part of me where I have no pain’ it felt like it might be possible to manage, but the reality proved to be different.
Although the college tried their best to offer suitable accommodations to make it work for her, the daily travel there and back took over an hour each way, and it proved to be a huge stumbling block for her. “I needed to go on the train to get there, and when it was busy I often couldn’t sit anywhere. I was too ashamed to ask someone that I didn’t know if I could sit down because I have this disease. I worried that they would look at me and think I didn’t really need a seat, because you can’t see anything obvious.
When I walk with crutches, or if I’m in a wheelchair then it is obvious, but when I’m having a good period all you can see is my feet when I walk. Because if I’m really tired I walk a little bit like I’m drunk, but that would be the only visible difference.” As well as the toll the daily commute and the course took on her, Janneke also realised that the industry itself would prove difficult for her to cope with. “If you work in the makeup industry often you might need to stand in small, cramped spaces, for example in a small dressing room backstage in the theatre, and you can’t always sit down to work. Or you might need to travel to the other side of the country and work long hours, and I can’t do that.”
Accepting that the life and career you dream of is not one that your body can support is hard, and over the years Janneke has had to work at finding a balance that she can manage, a way to live her life to the fullest, whilst also giving her body the rest and care it needs. She has also had to learn how to live with pain, without allowing it to shade and colour her life. “It can be hard when people think or say that they have it worse than me, because you can’t see pain. You can’t see it, and everyone experiences and feels pain differently too.”
Still living with her parents she’d like her own place, but being at home does mean “I can have a little bit of help from my parents. When I have a bad day,
my mum can help me with washing my hair, or showering.” Having the love and support of her close family and friends is very important, and helps to make it easier to accept the impact her health has on her day to day life.
Dreaming of the future can be hard too, because although some people with CIDP go on to have a spontaneous recovery, others may see their symptoms improve only to return later. For the more severe cases, like Janneke, not only will they experience frequent relapses, their day to day life is marked by pain and disability, making it hard to truly know what the future might hold. “I would love to be a mum someday, but recently I’ve started to think about what that might mean. What would happen if I had a child who runs towards a busy road for example, because I couldn’t run after him. I worry that I couldn’t do anything alone and would need help. So that part is hard.” It has also proved hard to meet anyone she explains, especially as she can only rarely manage to attend parties or busy social events where she might meet someone in person. “There are a lot of parties I need to cancel going to, and if I’m chatting to someone online and I tell them that I have a disability often they will just block me. When I was younger I found it harder, but now I think if someone does not respect me then they are not worth my time.”


Today Janneke volunteers three days a week in a lovely, small local primary school, and takes on private makeup jobs as well.
Recently she has discovered a love of shooting, having joined a local shooting club which offered seated sessions, and which she now attends twice a week.
It is also hugely important that she tries to maintain her daily step count on her good days, because even after five surgeries her feet and ankles are left weakened and need to be constantly rehabilitated as well as rested. Above all, Janneke has learnt to plan and manage her time carefully, to give herself the best chance of doing the things she wants to do each day.
“If I have a busy morning then I’ll rest. Or if I have plans to go out with friends for dinner or something then I’ll save my energy for that.”
There is a chance that her health will improve as she gets older, but she has also come to realise that it is also important to not only learn to live with her rare disease, but to talk about it too, although this is not always something she finds easy or comfortable to do.
“Sometimes I get a little emotional about it, and it’s hard to explain what you have, especially to people that I don’t know, but I also want to get more information about CIDP out there into the world, so that more people can learn about it.”

About GBS & CIDP: Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a rare autoimmune disorder caused by inflammation of the peripheral nerves— those located outside the brain and spinal cord. CIDP occurs when an individual’s immune system has an abnormal response, potentially triggered by an infection or illness, and starts attacking the myelin sheath. This sheath is the fatty, protective covering around nerves, and when it is damaged, it can lead to muscle weakness, numbness, and pain.
CIDP generally progresses slowly and may be present for months or even years before diagnosis. Initial symptoms—such as slowed nerve responses and sensory changes—often go unnoticed until they become more pronounced. Typically, CIDP develops over at least eight weeks, with symptoms gradually worsening. As the condition progresses, muscle weakness often begins in the arms and spreads to the legs, while reflexes may become slower than normal. In severe cases, swallowing and breathing can be affected, increasing the risk
of pneumonia, lung tissue collapse, or respiratory failure. If the autonomic nervous system is involved, gastrointestinal function or bladder control may also be impaired.
Treatment options may include corticosteroids, immunotherapy, and physical therapy to manage symptoms and improve function. CIDP has a high risk of relapse—while some individuals go into remission, others continue to experience symptoms that impact daily life.
CIDP is also considered the chronic form of GuillainBarré syndrome (GBS), an acute inflammatory disease of the peripheral nerves.
To find out more, visit the GBS | CIDP Foundation International website: www.gbs-cidp.org

The Importance of Connection
In conversation with Nancy Di Salvo, Director of International Affairs for The GBS | CIDP Foundation International
“No patient should walk alone”
The GBS | CIDP Foundation International is a global non-profit organisation which was co-founded in 1980 by Estelle Benson, it was known then as the Guillain-Barré Syndrome Foundation International. She was motivated by the experiences she’d had when her husband, Robert, was diagnosed with Guillain-Barré Syndrome, or GBS. Nancy Di Salvo, the Director of International Affairs for the Foundation, describes how Estelle and Robert found themselves “in a terrible situation
in which they had no information, no support, and she vowed that it would not happen to any other patients. No patient should walk alone. So she started creating this patient organisation, that basically started in her living room, and to this day she still actively supports the foundation’s work.”
The Foundation works tirelessly to support the global GBS/CIDP community, and as Nancy explains, central to their work are the four pillars which inform their mission; “support,
education, research and advocacy. We help educate our patients to better understand their condition, to learn about what they can do to improve their health, how to raise awareness and also to navigate through the healthcare systems that are in place, which of course are different in each country.” She continues, describing how at the very heart of their work is the belief in the importance of human connection.
“We have a peer-to-peer support system in which we try to make sure that each patient that contacts us can connect with another volunteer who is, or has also been, a patient. We have around 80 volunteers and supporting allied organisations worldwide, and this way a patient who is facing this new diagnosis can speak to a person that has already been on that journey, and can be guided and supported in a more human way. Because we all need human contact, and we want to make sure that nobody feels alone with their diagnosis.”
Guillain-Barré Syndrome is a rare, inflammatory neurological disorder of the peripheral nerves - the nerves located outside of the brain and the spinal cord, where the body’s own immune system mistakenly attacks the peripheral nerves. An early and accurate diagnosis is critical to try to treat and manage GBS effectively, unfortunately however it is, or can be, very challenging to diagnose as the symptoms
often overlap with other neurological disorders. In addition, it typically has a very rapid onset, and symptoms might include numbness, weakness, and often paralysis of the legs, arms and it can even impact the muscles needed for breathing. In some instances, Nancy explains “GBS can be deadly, and most patients do end up in the ICU with a tracheostomy to help them breathe. However, if diagnosed and treated in a timely manner with either plasmapheresis or immunoglobulins, then the patient can overcome the condition, and the paralysis, and slowly regain their physical abilities. Of course they need to be supported with not only medical treatments, but also with occupational and physical therapy, and recovery is a slow process. But for some patients a residual, or possibly even
severe, disability might remain, but the outcome can be positive as well.”
A combination of clinical evaluations and diagnostic tests are used to diagnose GBS, including a clinical evaluation by a neurologist, nerve conduction studies using various electrical tests, an electromyography (EMG) which can help distinguish GBS from other neuromuscular disorders. A lumbar puncture, blood tests and at times imaging studies might also be used. It is, Nancy notes, important to get the correct diagnosis as there are many variants and related conditions, including Chronic inflammatory demyelinating polyneuropathy, or CIDP. “CIDP is in the name of the Foundation now, as it is a chronic condition, and one of all of the related variants that we support. It is described as chronic

because it’s not like GBS which you can overcome, and where you can get back to a normal life. Instead the majority of CIDP patients will have ongoing treatments for the rest of their life. It is also a condition that has a much slower onset, and so it is unlike the quick, acute version of GBS. Unfortunately, it is often misdiagnosed, in those cases it leads to more damage.”
CIDP is also an autoimmune condition, which means that the immune system attacks the nervous system, which leads to damage of the myelin sheath that covers that nerve. Nancy qualifies this further; “Once a nerve is no longer protected then the electrical signals to the nerves does not reach the limbs, for example to the hand or the foot, so slowly you lose the function and control of your body. Early diagnosis can lead to less damage, because once the
damage is done, it’ll take more to regain that ability. CIDP treatments are usually based on corticosteroids, or high doses of intravenous immunoglobulins and plasma exchange. Ideally treatment with intravenous immunoglobulin would be the most important treatment, because if it is administered in the correct way in line with the international treatment protocols, then a CIDP patient might regain a good level of function.”
As above both GBS and CIDP are autoimmune disorders, but although the exact cause of both diseases is still not fully understood, they appear to have different triggers. Over 50% of GBS cases seem to occur after a bacterial or viral infection, but in CIDP the exact cause of this immune response is, as yet, not fully understood.
Ensuring that the global GBS and CIDP patient communities have access to both a timely diagnosis and the best possible treatment is at the centre of the work that the Foundation is building on. Whilst it might have started as a small support group who met around Estelle’s dining room table back in 1980, today it has become an international organisation which includes 30,000 members, supported through 200 chapters in 49 countries, each dedicated to providing support and assistance to GBS | CIDP patients and their families. ”The Foundation is very much focused on moving outwards to help all patients, we really want to be present, and able to advocate within national and local contexts, ideally even being invited to sit at the table when important regulatory processes are discussed. Because we want to make sure that regulators and policy makers, truly understand the rarity and realities of this condition. We are very passionate about helping our community to grow, not in numbers, but as advocates.”
The reality is, as with so much in life, that whilst the Foundation is a global organisation supporting patients from around the world, the patients they are supporting do not have access to the same medical infrastructures. Each country, indeed often each local health authority, will have very different budgets in place, and this can make operating globally


Nancy on the first of many awareness benches, photograph courtesy of Nancy Di Salvo and the GBS | CIDP Foundation International
quite difficult in terms of advising and supporting a global patient community. This conflict is one that can at times weigh heavily on Nancy, and the Foundation, as they try to build a fairer world. “There are times when I’m talking to patients from countries where the current political or economic situation is very complicated, and I’m trying to help them access treatment but it is incredibly hard to do. At the moment I have a patient for whom I’ve reached out to Doctors Beyond Borders, and to the United Nations because we need to do something to try to help. We can see that it’s a privilege to live in one country compared to another country, because if you’re unlucky enough to live in a country where you don’t have access to treatment then the outcome is very, very difficult.”
Nancy sighs, before continuing, “It can be sad, and very frustrating. I have to be honest, at times I feel helpless. This is why the Foundation is so committed to trying to help these patients, through creating local committees, and connecting our volunteers in these continents, to support them in creating these committees, and to develop effective advocacy in their countries. We all need to fight for equitable diagnosis and treatment of rare diseases.” It is the experiences of her own diagnostic journeys and access to treatment that drives her forward, and that gives her the strength to carry on - even on the days when the burden feels heavy. “I had GBS when I was 20 years old. I was diagnosed here
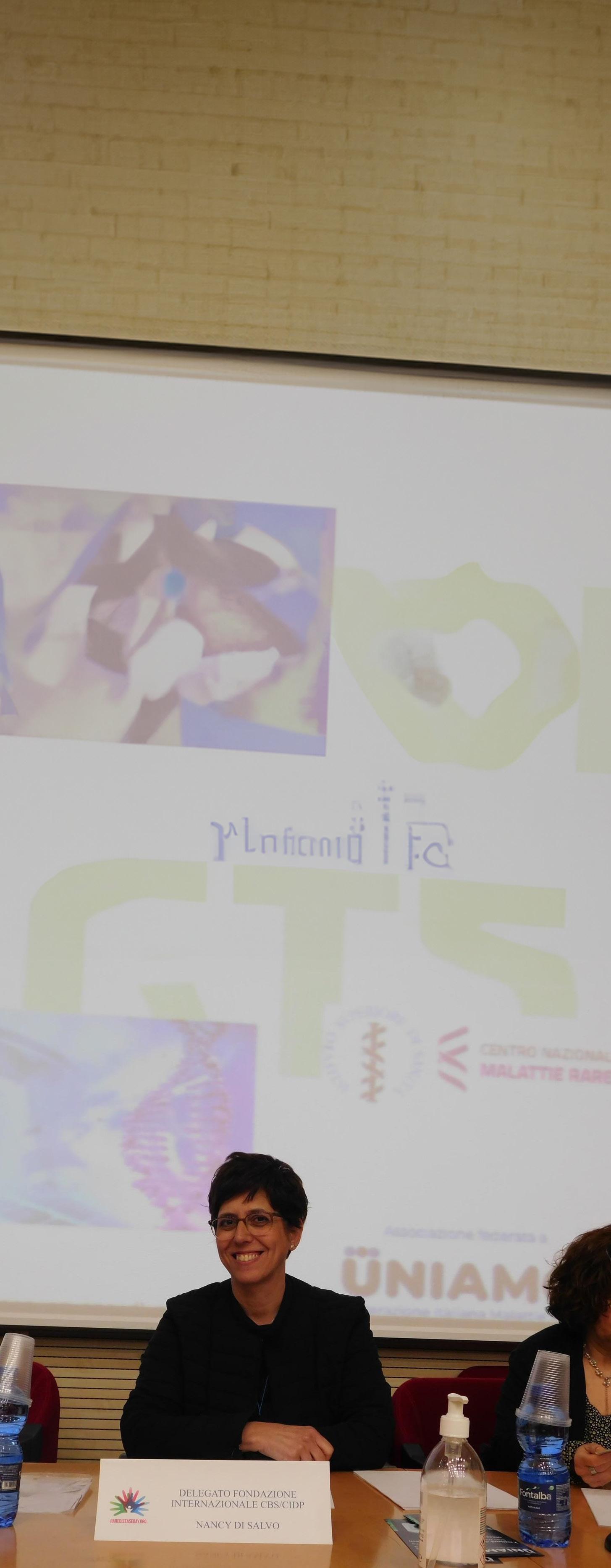
in Italy where I live, and with treatment I overcame it, and I got well again. It was an experience that left me not only with the determination to get well again but also to help other patients. I wanted to make sure that they didn’t feel lost, that they would have the right support because it is a devastating condition. Because it is such a rare condition, it’s almost always unknown, and so when you are suddenly paralysed and you don’t know the reason why, it is incredibly scary and frightening, for both the patient and their loved ones.”
After her recovery from GBS Nancy was living a full and busy life when, at around the age of 35, she started to experience some sensitivity and numbness. Despite being told by her doctor that it was likely just part of ‘ageing’ she was not convinced. “I was already a member of the GBS | CIDP Foundation, I was one of the patients being supported through their resources, and so from reading through their educational newsletters I had heard about CIDP, and I just had a sense that that was it, because I could connect the dots. But even still I saw four doctors until finally the fourth one understood that it was CIDP, and I was admitted into the hospital. But by that point I was in an acute situation because it took so long to get that diagnosis.”
Nancy at Rare Disease Day, University of Palermo, photograph courtesy of Nancy Di Salvo and the GBS | CIDP Foundation International
It is incredibly rare to be diagnosed with both GBS and CIDP, and occurs in only around 5% of cases. Despite the huge odds stacked against her today Nancy is doing well, and she can “live a normal life. I’m able to do almost anything other than running and jumping, but I can live my life well enough without those activities.”
It was after her own CIDP journey that Nancy first started volunteering for the Foundation, a role she continued for over 10 years until she took on a paid position within the organisation. Being involved with the Foundation has been, she feels, more than anything else “the most important step in my life, because it gave my life sense, and it gave my experiences of rare disease a meaning. It became my mission - a mission I am still very committed to, that all patients should have access to diagnosis, treatment, care and support, and that they know that they are not alone.”

Nancy at Walk and Roll in Washington DC, photograph courtesy of Nancy Di Salvo and the GBS | CIDP Foundation International

To find out more about The GBS | CIDP Foundation International visit: www.gbs-cidp.org

Finding small moments of happiness (or hygge moments) Time with a loved one.
Sharing a freshly made brew with a friend, old or new.
at photographs that hold the best memories.
Moving plants into the sun.
The smell of fresh bread from a local bakery, or the oven if you bake.
The creases in the spine of a book that shows you are currently enjoying reading.
The smell and delight of freshly cut flowers arranged beautifully. Neatly folded fresh blankets and plumped up cushions on the sofa. The smell of fresh laundry. An afternoon spent doing your version of nothing, be that reading, a TV binge, knitting, snoozing or anything else.
Holding a perfectly shaped mug in your hand, looking out at a view that moves you. Listening to music that you love, and that always moves you.
Watching the delight on someone’s face when they receive an unexpected and thoughtful gesture or gift from you.
A walk, because it really is true that ‘you never regret a walk.’
The first night in your freshly made bed.


Traveling the World for a Diagnosis
Written & contributed by Renee Bruns
It was a cold day in February 1984 when my story began. Mom hadn’t had an ultrasound – they weren’t common then. There was no reason for her to think that anything would be different with her firstborn child. But the moment I came into this world, I was, in fact, different.
I was born with a rare skeletal condition called autosomal recessive multiple epiphyseal dysplasia (rMED). But… it took 39 years for my family and me to learn what was different about my skeletal system. It started on that cold day over 40 years ago. My feet were curved up, the bottoms touching my buttocks. “She has clubfeet,” the doctors said. “It’s an easy procedure and a specialist should be able to fix them in a few weeks.” There were dozens of doctor’s appointments, referrals, x-rays. At the end of the day, there was something different about my skeletal system. And no one knew what it was.
My family and I started to accept that there was something different about me, and that we may never know exactly what it was. I had half a dozen operations on my feet before I stopped walking completely. My feet never took ‘normal’ shape, and my knees and hips started to contract so that I could no longer extend my legs straight. Eventually, my legs had little movement, and I was ‘stuck’ in the seated position. I had intense bouts of arthritis and pain in my joints, especially my legs. When I was 26 years old, I underwent a double hip replacement to alleviate some pain – and it helped tremendously!
We traveled all over the United States in search of a diagnosis – we received over half a dozen along the way – and treatment for my condition. But there was never a definitive answer, so we learned to live in a space that was uncertain
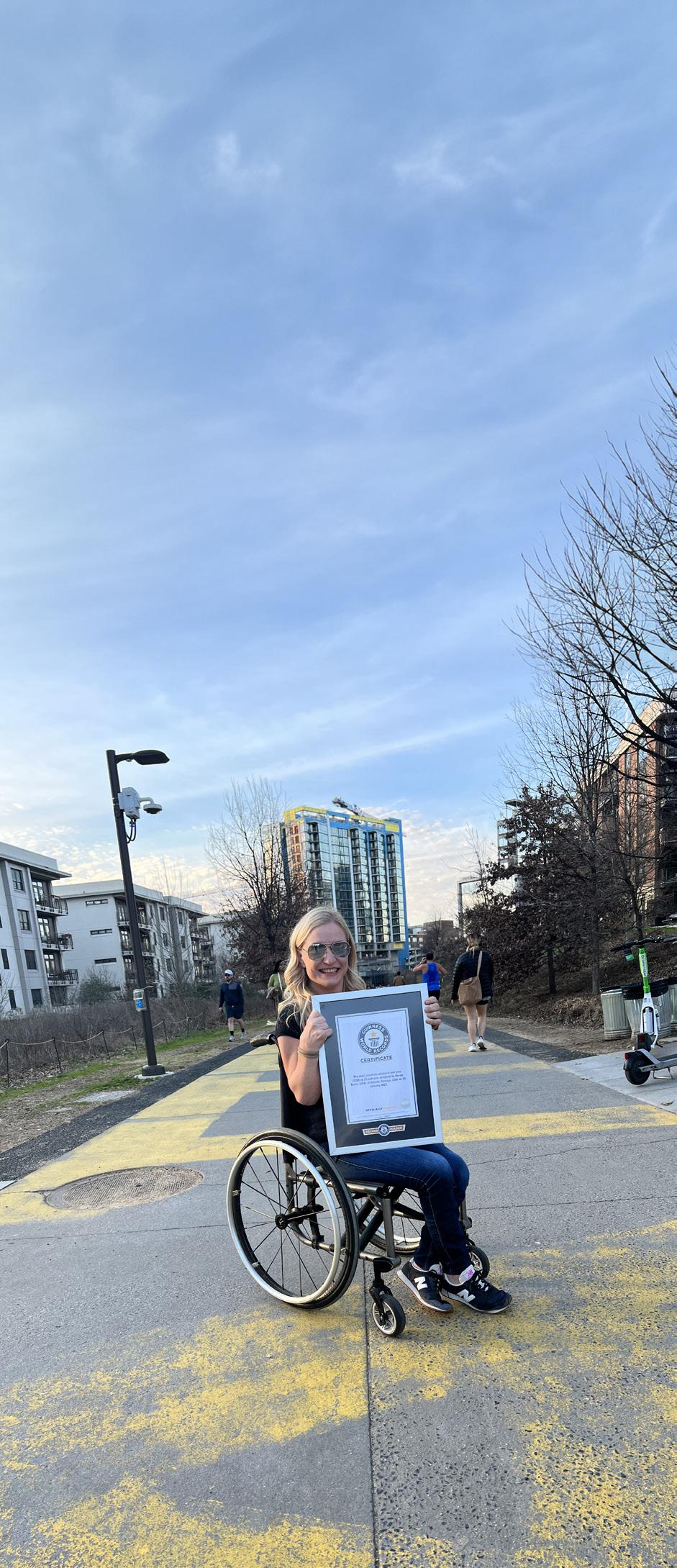
and unknown to anyone. I remember my first airplane ride to New York City, to see a specialist when I was around 5 years old, and falling in love with the culture and experience of seeing the world. It was that trip that sparked the joy of travel in me. It was something I could do, even using a wheelchair, and a few years later, I set an ambitious goal for myself: I would see all 50 states before I died!
By the time I was in my early 20s, I had reached my goal. I finished college and thought, “now what?” I took my first trip to Europe, and then Africa, and then Asia. I completed a Master’s Degree and built a career – something I longed for – while traveling during my time off. In early 2022, after struggling from post-pandemic burnout, I made the difficult decision to leave my executive level role in corporate insurance. I had spent years struggling to find my place in the world, always feeling different and alone. I have the most amazing family ever, and tremendous friends, but there was never anyone quite like me and that left me feeling abandoned in a world where everyone seemed to fit in. Coupled with employment discrimination at various points throughout my career, disability prejudice in my day-to-day world, and my own self-hate, I knew I needed to make a change in my life. I set out to see the world with one goal in mind: I wanted to experience humanity and try to find the good in people!
I asked everyone I knew if they wanted to travel with world with me. To no surprise, none of my family or friends wanted to leave their careers behind and jet set around the world with me. It was clear that this was a journey I’d need to make on my own. With much speculation, I booked a one-way ticket to Bali, built spreadsheet upon spreadsheet to help me plan and stay on budget, and began my research about solo traveling as a disabled female. I found few resources for someone like me, and I started wondering if I was the only person doing something so adventurous and unique. I messaged Guinness World Records shortly before I left, asking if there was a world record I could compete for. If I was the only one traveling the world solo and using a wheelchair, surely there must be an award for what I was about to do! We exchanged messages a few times before a new record was opened for me: How many countries can you visit in one-year using your wheelchair?
Guinness World Record, February 2023. Image courtesy of Renee Bruns

I was already on my trip, exploring the world, when I received news of the opportunity to become a world record holder. My objective was changing, but I promised myself that I wouldn’t lose sight of my original goal: to experience the people in our world. I was finding kindness in people at every corner – men in Fiji who carried me in my wheelchair up a flight of stairs when there wasn’t an elevator, a young man in Kyrgyzstan who pushed me up a mountain so we could meditate at the top, a couple in Bulgaria who walked with me in the middle of the night through dark streets to make sure I made it to my hotel safely. I left on my trip needing to know that there was good in this world, that there were people who could see me for me, and not for my
wheelchair or my disability. I was finding it tenfold. It was working – my view of humanity was resetting itself.
About six months into my journey, I started to get curious about the ‘thing’ – my disability – that had defined so much of my life. I had undergone DNA testing many times before, as a child and an adult, and eventually stopped trying to find answers there. The results always came back inconclusive, and I was always left disappointed. While I was touring the islands of the South Pacific, away from the rest of the world and with little access to the internet, I had a sudden urge to know more. I was becoming so comfortable with who I am, and the experiences I was
having around the world allowed me to accept the challenges I had in life. But I desperately wanted to know what my condition was. What was it called?
I promised myself, while swimming in the crystal clear Pacific Ocean waters surrounding the Kiribati islands, that I was going to figure this out. Weeks later, I ordered an at-home DNA test. The website promised to scan my DNA for over 1,200 rare diseases. This is it! I will finally know what I have! I thought to myself. I mailed in a saliva sample and waited. Months later, I received an email. “Inconclusive.” I didn’t want to give up this time. I started reaching out to genetic specialists around the country. Eventually, I received a response from a genetics team at Johns’
Hopkins University in Baltimore, Maryland. I met with them as soon as I could, took more DNA tests, asked my family to undergo DNA testing, and almost a year after I committed to finding out what my condition was, I listened intently as my medical team told me, “you have a rare genetic variant that we’ve never seen before in any scientific literature. You have a form of autosomal recessive multiple epiphyseal dysplasia.”
A new, unexpected wave of acceptance and self-worth overcame me. I had a new peace with those words, something I didn’t think I needed to find when I left my career months earlier. I really was different, down to a unique genetic variant never before seen. All of those times that I felt so isolated and alone weren’t made up. There really wasn’t anyone else like me. I had always known that I was living my life differently than others. But I always thought it was because of my disability, of the special ways I got around the world. Now I know that it’s more than just a disability, or a diagnosis, or the device I use to navigate the places I go.
Because I was born different, and no one knew what was going on with my skeleton, I started to accept that being different was okay. And I started to live my life differently. I stopped worrying what other people thought of me and my outlandish dreams, and I created my own goals, devoid of society’s expectations. I learned at a young age that our health can be taken from us without warning, and sometimes without ever having it in the first place, and so I set out to experience as much of the world as I possibly could.
I left my job in search of kindness. I found that and so much more. I received my Guinness World Record after visiting 66 countries in one year. I found adventure. I found kindness around the world. I found a diagnosis – 39 years later! And I found love. For the people who supported me. For the strangers who became friends. For humanity. I found love for myself.


About Autosomal Recessive Multiple Epiphyseal Dysplasia (rMED).
Multiple epiphyseal dysplasia (MED) is a rare, inherited, skeletal dysplasia caused by a malformation of the growing ends of the long bones. However, there is an even rarer form of MED, rMED, or Autosomal recessive multiple epiphyseal dysplasia.
rMED is a recessive, inherited genetic disorder. A recessive gene disorder occurs when both parents are carriers of a recessive gene and pass it on to their child. Often people will not know that they are a carrier of a recessive gene until their child is diagnosed, as typically they will possess one copy of the recessive gene and one copy of the dominant gene, so they often do not have any identifying symptoms.
rMED is characterised by an abnormal skeletal development, which mainly affects the growth of the long tubular bones, including the bones in the hands, hips, knees and feet, which can lead to malformation of the hands, feet and knees and scoliosis. Joint pain, especially in the hips and/or knees, is fairly common and typically begins during childhood.
For more detailed information visit: www.rarediseases.org
Find out more
To find out more about Renee or to follow her social media platforms visit her website here: www.reneebruns.net
Renee is passionate about giving back, and supports the charity Free Wheelchair Mission, linked here: www.freewheelchairmission.org
You can find Renee’s fundraiser here: www.give.freewheelchairmission.org

The Transformative Possibilities of Gene-silencing Medications
In conversation with Liz Gill and Sue Burrell, Co-CEOs of the British Porphyria Association (BPA)
“People say that when they found the British Porphyria Association (BPA), they found a family.”
For so many people in the rare disease community this observation will resonate. When you have a rare condition the road to finding your community can often be a long, exhausting and confusing one, and the relief of finding people who not only truly understand but can also offer support and insights can feel like a coming home of sorts.
Liz Gill and Sue Burrell are the Co-CEOs of the British Porphyria Association, they are also sisters, and they both live with acute, recurrent porphyria. Porphyria, Liz explains, “Is a rare genetic condition which can often be hard to diagnose. The symptoms that people initially experience tend to be pain, sickness, and other quite non-specific symptoms, and although in more extreme cases paralysis can also occur, the main symptoms can be very general and so people can go an awfully long time without being diagnosed.” She continues, describing how “porphyrias are a group of rare genetic disorders caused by a gene defect, or mutation, which means that we can’t produce the right kind of
proportions of chemicals in our heme biosynthetic pathway. This is an instrumental part of the biochemical function of the body, and if there are errors in this multi-step process it results in a buildup of porphyrins, which are essential for producing haem, a key component of haemoglobin. This buildup is toxic for the body, and can therefore lead to severe symptoms, including abdominal pain, vomiting, and various neurological issues.”
At this point Liz asks Sue to add her thoughts, so she continues; “Individuals can and likely will experience different levels of attacks and symptoms as well. Some people often might have had some kind of ‘grumbling’ symptoms for a while before it develops into something that might be a full blown attack. The pain, as Liz said, can often
sometimes even in their legs. We know of patients around the world who have had treatment or even procedures and operations, for example things like having their appendix removed, because their medical teams think that it’s causing the issues. In addition, there are a number of medications which are unsafe to use for porphyria, but as this has not been diagnosed, people are being treated with them which in turn can exacerbate the symptoms even more.”
Put simply, it is the buildup of the body’s naturally produced chemicals that causes a toxic overload, which in turn causes an attack which results in inflammation of, or damage to the nerves which is what creates the symptoms experienced. What makes porphyria so difficult to live with, especially if still
BPA website states that “Acute porphyria attacks are often triggered by exposure to commonly prescribed drugs, illegal drugs, alcohol, dieting, stress, infections, viruses and hormonal fluctuations.” This often means that whilst someone is still undiagnosed, their recurrent attacks are being triggered either by the efforts to treat the symptoms, by their life or lifestyle, or even the body’s own hormones. Added to this the difficulty and delay in diagnosing this rare condition can, in severe cases, mean that by the time a patient is finally diagnosed the impact of the disease is not only profound, but also irreversible. It was, Sue explains quietly, this way for Liz. “We didn’t know we’d inherited this condition, which meant that by the time Liz was finally diagnosed the

months. The disease doesn’t come up on any of the routine or normal tests that you might do, and there’s no way to test for it in a standard blood test, there will be nothing visible on a scan, or a CT scan. There’s simply nothing obvious which makes it very complex, and it means that you can go for months and months without a diagnosis.” Although she is largely well today Liz lives with the damage caused by many, many years of suffering with recurrent acute attacks of porphyria. When I look at Liz she chimes in, noting pragmatically that she’s “been left with quite damaged kidneys, as one example, and residual paralysis.”
Those familiar with the challenges of the rare disease community will of course recognise this story, because it is one that is told time and again. Rare conditions with symptoms that are not immediately, or easily diagnosable, are hard to diagnose because the very fact of their rareness means that inevitably doctors will have maybe only read a paragraph or two about them during the course of their training. “It’s often about luck” Sue explains, and although it is getting better, the majority of the people they support through the BPA “have had a very long journey to diagnosis. It’s still about finding that initial doctor who is willing to look deeper to try to find what might be causing the symptoms.”
However, if people have a known family history of porphyria then they might either have already had genetic testing themselves, or if not would at least be more aware of porphyria if they develop any potential symptoms. This was the experience that Sue had, she describes how “It took ages for Liz to be diagnosed, and by then she was very ill. Once we knew, I had genetic testing, and so by the age of fifteen I knew what I had. I was lucky and didn’t experience any symptoms until I was twenty-seven, and we knew exactly what doctor to go to, and they could start with treatment straight away.” Until her first attack Sue tried, as best she could, to avoid or minimise any possible triggers. For example, “I didn’t touch any alcohol, and I also never had any unsafe medications. I wear a medical alert bracelet in case of emergencies, and I would make sure that I had the ‘safe medicines’ list with me when I went to the dentist, or to the doctors, so I avoided every potential trigger.”
However, the range of ways in which an attack could be triggered means that avoiding them all is not easily possible, but the delayed onset for Sue also brought with it the benefits of a much more robust and informed treatment protocol once she needed it. Liz takes over, describing how she had been an early patient
to be given a medication called Normosang, and it had helped to bring her out of an attack.
“I had treatment on a named patient basis (also known as compassionate use), and it worked very effectively to bring me out of an attack when I had one. But at that point, we’re talking thirty odd years ago, I had to wait until I went into an attack, and then they would give me the treatment. But eventually they were no longer easily able to get the drugs into my veins properly because they were collapsing, so they fitted me with a portacath and started giving me a preventative dose in an attempt to pre-empt the attacks and try to control them. That did actually help for a good long while.” At this point Sue adds that because it was an uncommon treatment, it was not always administered exactly how it should have been;
“In the early stages, Liz didn’t always get the full treatments as it was being infused into a small vein. We know a lot more now and are aware that it has to be infused within an hour.”
Dr Vicky McGuire (Chair of Board of Trustees), Liz Gill (Co-CEO) and Sue Burrell (Co-CEO) at the International Congress of Porphyrins and Porphyrias in Pamplona, Spain, September 2024. Photograph courtesy of the British Porphyria Association (BPA)
Despite receiving treatment both more swiftly and more efficiently than had been the case for Liz, Sue still lived with the utterly debilitating effects of frequent, acute porphyria attacks, and was often hospitalised. However in 2017 she was one of 94 patients from 18 different countries invited to take part in a clinical trial that was part of ongoing research into the treatment possibilities that ‘gene-silencing,’ and gene-silencing medications, might offer. But what are gene silencing medications? In brief, they work by blocking, or modifying and/or inhibiting the specific genes that contribute to a disease, essentially silencing them. In the case of porphyria specifically, the trial drug Givosiran worked by interfering with the processes through which harmful proteins are produced, leading to a build-up of toxic porphyrins in the patient. As such it is not a cure,

as it does not remove the cause of the disease, but it did prove to be an incredibly effective treatment for it.
In April 2019 the BBC excitedly reported that ‘Gene-silencing: ‘New class’ of medicine reverses disease porphyria’ and quoted Sue in the article, explaining that her ‘life had been transformed.’ This exciting development was one which was being anxiously awaited by the wider global porphyria community. However, the reality is that whilst gene silencing therapies offered hope for a number of previously untreatable diseases, they were, and are still, very expensive. In addition, the medicine development process is invariably long, and even once a medicine has been trialled, it still needs to be approved and assessed by the different national and global regulatory bodies. In the case of the
UK, it was only in October 2021 that the National Institute for Care and Excellence (NICE) issued draft guidance which recommended the use of Givosiran on the NHS, but only for the treatment of severe recurrent attacks of acute porphyria. In reality this has meant that only a relatively small set of recurrent attack patients (which means people who experience 4+ attacks in a 12-month period) are eligible, something which the BPA is fighting tirelessly to address.
Liz explains, “We are delighted with the impact gene silencing treatments have had on the course of acute porphyria for those with recurrent attacks. It’s a powerful reminder that progress is possible, and hope is real! But there is still much to be done: raising awareness, improving diagnosis and supporting those with sporadic attacks or chronic pain. We are still looking for ways to improve quality of life for everyone living with porphyria. One of the things we are focused on is supporting those porphyria patients that don’t fit the current treatment criteria. For example, some people who experience sporadic attacks may well be having a really tough journey, and their symptoms during a full blown attack might really affect their lives, and make it incredibly hard to
cope, but they don’t qualify for the gene silencing treatment that is offered to those diagnosed with recurrent attacks. Because the reality for many of the porphyria community here in the UK is that unless you fit a very narrow criteria, you don’t get the treatment and that’s hard, really hard.” But despite this huge discrepancy in terms of access to treatment between those diagnosed with sporadic or recurrent porphyria in the UK, it is, Sue and Liz explain, one of the leading countries in terms of access to treatment and support.
Since 2018 Liz has served as a patient representative on the Executive Board of Ipnet (International Porphyria Network – a clinician-led non-profit association that aims to improve healthcare services for porphyria patients), and she is also a key member of a working group which aims to create clinical guidelines for the acute porphyrias globally. Sue is similarly invested, serving as the President of the Global Patient Advocacy Coalition, a global patient network of national porphyria patient advocacy organisations. They note that “Overall what we have here in the UK is actually pretty amazing, there are patients around the world that do not have access to diagnostics, testing or any
form of support. Indeed, in some cultures porphyria is still completely hidden, and patients are kept in the house so that their communities do not know that they are ill.” It is for those hidden, forgotten patients, as well as for the patients whose diagnosis means they do not meet the treatment funding criteria in place, that they continue to work tirelessly to fulfil the mission at the very heart of the BPA.
“The BPA is committed to advocating for, supporting and educating porphyria patients, relatives and medical professionals, so as to improve the quality of life for those living with the different types of porphyria. We promote disease awareness and the advancement of research into new therapies. Patients often experience exceptionally negative effects on their physical health, family and social relationships, financial stability and psychological and emotional wellbeing. By providing families with the tools and resources to be informed about their condition, we can help to improve the lives of those affected.” It is this, this heartfelt and sincere commitment that Liz and Sue extend towards the global porphyria community that means that they are often told by people that “when they found the BPA, they found a family.”
Photograph by Sangharsh Lohakare, Unsplash

About Porphyria
The BPA website notes that ‘The porphyrias are a group of relatively rare genetic disorders. They are called the porphyrias because they cause a build-up of chemicals called porphyrins, or the simpler chemicals used by the body to make porphyrins’ in the body. High levels of porphyrins that have built up can cause major problems, mainly in the nervous system and skin. As such they are broadly categorised into acute and cutaneous (skin). The severity of symptoms varies dramatically in all types of porphyria. But no matter which type, the more knowledgeable about their condition a patient is, the more it is that they stay well.
To find out more visit the BPA website here: www.porphyria.org.uk


CRETE CAPTIVATING
Where Myth Meets Paradise: Exploring Crete’s Legendary Beauty
Crete, Greece’s largest island, is a captivating blend of ancient myths, breathtaking landscapes, and vibrant Mediterranean culture, making it a must-visit destination for everyone. Home to the legendary Palace of Knossos, the island’s rich history intertwines with Greek mythology, offering a glimpse into Europe’s earliest civilisation. Its stunning beaches boast crystal-clear waters and pink-hued sands, and charming villages, warm hospitality, and mouthwatering cuisine create an unforgettable experience. Whether wandering through historic streets, basking in golden sunsets, or seeking adventure, Crete caters to every type of traveller with its unparalleled beauty, authentic experiences, and increasing accessibility for visitors with mobility needs. With a little planning, anyone can discover its magic, embrace the welcoming atmosphere, and make lifelong memories on this extraordinary island.


Things to Do
Accessible Beach Days
For many travellers, a day at the beach is an essential part of any getaway, and Crete offers several accessible beaches designed for visitors with limited mobility. Many feature smooth pathways, ramps, and designated parking areas, with some even providing beach wheelchairs for easier navigation on the sand. Popular choices include Agia Pelagia Beach, known for its calm waters and accessibility, Ligaria Beach, which offers direct sea access and adapted facilities, and Preveli Beach, famous for its palm forest and scenic beauty, with accessible pathways leading to the shore.
Exploring Chania’s Old Town
Chania’s Old Town is a captivating blend of Venetian, Ottoman, and Greek influences, offering a rich historical experience for all visitors. While the area is known for the charming cobblestone streets, wheelchair users can still enjoy much of its beauty, particularly around the Venetian Harbor, which features smoother pathways and ramped access. Some streets have gentle inclines, and certain areas may require careful navigation, but accessible tours with adapted vehicles ensure a comfortable experience. Visitors can stroll along the picturesque waterfront, admire the historic lighthouse, and soak in the lively ambiance of local cafés and shops.
Discover Cretaquarium
Cretaquarium is a fantastic destination for marine enthusiasts, offering accessibility features that ensure a welcoming experience for all visitors. The aquarium is wheelchairfriendly, with ramps and elevators providing smooth navigation through the exhibits. Guests with disabilities can even opt for private tours with adapted transportation for added convenience. Inside, over 2000 sea creatures across 200 species—including stingrays, jellyfish, and sea turtles—showcase the rich biodiversity of the Mediterranean. With accessible restrooms and seating areas, Cretaquarium delivers a comfortable and engaging experience.
www.cretaquarium.gr


Must
See
The Palace of Knossos
Crete’s most famous archaeological site, the Palace of Knossos, features accessible pathways and ramps, allowing visitors to explore around 50% of the ancient ruins. While some areas may pose challenges, wooden decks and solid ground pathways make navigating the site easier. The entrance offers accessible toilets, and tickets are free for visitors with disabilities. Private tours with adapted vehicles provide a fully accessible experience, ensuring smooth transportation between sites. As the legendary home of King Minos and the Minotaur, Knossos blends mythology and history, offering an unforgettable journey into Crete’s rich past.
www.knossos-palace.gr

Where to Stay
Crete offers a diverse range of accommodation, from charming boutique hotels to luxurious five-star resorts, many of which prioritise accessibility. Several properties provide adapted pools, beach access, and tailored services to ensure a comfortable stay for visitors to the Island. Whether seeking a cosy retreat or a grand resort experience, Crete caters to a variety of preferences while embracing inclusivity. It’s always recommended to check directly with the accommodation to ensure it meets specific accessibility needs.
Creta Maris Resort - Located in Hersonissos, Creta Maris Resort offers accessible rooms, ramps, and adapted facilities for wheelchair users, ensuring smooth mobility throughout the property. Guests can enjoy a Blue Flagawarded beach, multiple restaurants, pools, and entertainment options, all designed with accessibility in mind. The resort provides assistance from lobby staff and club cars to help guests move around comfortably. With its blend of luxury and thoughtful accessibility, Creta Maris Resort ensures a relaxing and inclusive experience for all visitors.
www.cretamaris.gr
Mitsis Selection Laguna in Hersonissos, Crete, is a luxurious five-star ultra-all-inclusive resort, offering an exceptional stay with superb amenities and accessibility features. Located on a Blue Flag-awarded beach, the resort boasts 351 elegant rooms, six themed restaurants, and six stylish bars, including a Champagne, Wine & Sushi Bar for a refined dining experience. Guests can unwind in the Venice-style pool landscape or indulge in treatments at the state-of-the-art spa. The resort also provides customised rooms for wheelchair users, featuring spacious layouts, adapted bathrooms, and barrierfree access, ensuring a comfortable and inclusive stay. With its breathtaking design, world-class hospitality, and commitment to accessibility, it is a standout destination for visitors to Crete seeking both luxury and convenience.
www.mitsis.com/en/hotels/laguna-resort
Stella Island Luxury Resort & Spa - Nestled in Aposelemis, this Luxury Resort & Spa is an exclusive, adults-only, five-star retreat that prioritises both sophistication and accessibility. The resort features spacious pathways, ramps, and accessible accommodations, ensuring a comfortable experience for guests with mobility needs. With its lagoon-style pool, overwater bungalows, and world-class spa, Stella Island creates an atmosphere of pure indulgence. Attentive staff and tailored services enhance the experience, making it a refined and inclusive escape for anyone seeking relaxation and elegance.
www.stellaisland.gr


Where to Eat
Crete’s culinary scene is a delicious blend of fresh local ingredients and traditional recipes, making it one of Greece’s most flavourful and authentic gastronomic destinations. The island is renowned for its olive oil, cheeses, and hearty specialties like dakos (barley rusks with tomato and cheese) and antikristo lamb, which is slow-cooked over an open flame. Seafood lovers can enjoy freshly caught delicacies, while sweet treats such as kaltsounia (cheese pies with honey) and bougatsa (filo pastry with creamy filling) provide the perfect finish. Whether dining in a seaside taverna or a rustic mountain eatery, Crete’s food is a true celebration of its rich culinary heritage.
Petousis Restaurant - Located in Heraklion, Petousis Restaurant is a beloved spot for authentic Cretan cuisine, offering a warm and inviting atmosphere. Known for its traditional family recipes, the restaurant serves standout dishes such as antikristo lamb, gamopilafo (wedding pilaf), and grandma Kalliopi’s dolmadakia. Guests can savour freshly grilled meats, homemade appetizers, and locally sourced ingredients in a setting that effortlessly blends tradition with comfort. With its welcoming service and rich flavours, Petousis Restaurant delivers a true taste of Crete’s culinary heritage
www.petousis-tavern.gr/en
Estrella - Located in Chania, Estrella is a vibrant all-day restaurant known for its creative brunch, specialty coffee, and Mediterranean-inspired dishes. It offers a stylish yet relaxed atmosphere, perfect for enjoying fluffy Japanese pancakes, Thessaloniki-style bougatsa, and fresh seafood. The restaurant blends modern flavours with traditional Greek ingredients, making it a standout spot for food lovers. Its seaside setting in Chania enhances the experience, whether indulging in a leisurely breakfast or a late-night cocktail.
www.instagram.com/estrella_chania
7 Thalasses - With locations in Heraklion and Rethymno, these are highly recommended Mediterranean seafood restaurants, offering a refined yet welcoming ambiance with a focus on fresh, high-quality ingredients. The restaurant in Rethymno is situated by the sea, it provides a stunning backdrop for an elegant dining experience. The menu showcases expertly prepared seafood, complemented by an extensive wine list curated for perfect pairings. With impeccable service, stylish decor, and dedication to the Cretan-Mediterranean diet, this place is a must-visit for seafood lovers seeking both authenticity and sophistication.
www.7thalases.gr/en
A classic Greek salad. Photograph by Loes Klinker, Unsplash



FOLLOW YOUR DREAMS
An introduction to the artist Charlie French
Charlie French was born in 1991 in New York. The oldest of three siblings, he has a younger brother and sister. Over the years the close-knit family have lived all over the US, and even in Europe too. He recently relocated to Boulder, Colorado with his parents, because as he explains “although I have lived away from them a couple of times. I prefer to be with them, and they like that too.”
When Charlie was just sixteen years old he developed Down Syndrome Regression Disorder (DSRD), a very rare and serious disorder that can affect individuals with Down syndrome in their late teen years, or even into early adulthood. DSRD causes a loss of skills, and whilst these vary from person to person this might include an acute loss of speech and the inability to perform activities needed in daily life amongst other things. And so he lost his ability to communicate, and to engage with the world for a period which spanned over five years. It was as he gradually emerged from this difficult time that his love of painting truly blossomed.
“I loved to paint when I was in high school, but in my early twenties I started taking painting classes and working with art tutors, and it was then that I discovered I loved painting and wanted to become a professional ARTIST!” Over the following years Charlie continued to work with different tutors, he attended classes and began painting every day at home. As he explains “I love painting. I work with acrylic paints, and I do lots of drawing before, during and after I cover a canvas with paints. I like to draw as a warm-up especially. I have also tried ceramics, printing, watercolours and using oil sticks. I love trying new materials and new techniques, but when I am done trying something new, I prefer to get out my pencils and acrylics and just ‘Let Go and Be Free’ with a canvas: painting whatever I want!”
By 2018 Charlie was selling his work online, and had set up a beautiful website and his social media platforms where he was able to both showcase his work, and share his story with the world. As with many artists his work is influenced by many things, including the space and
the seasons around him. In a 2023 interview in Canvasa blog by Saatchi Art, about his work he explained how the view of the changing seasons through the skylight in his studio in London inspired his series ‘It is Almost Spring.’ As he is currently building a new art studio in their backyard in Boulder it will be exciting to see how the city, which is nestled in the foothills of the impressive Rocky Mountains, may influence and inspire him over the coming years. He explains that “the studio should be finished this summer. I cannot wait!!! My first studio was in Dallas, TX and I also had one in London. It will be exciting to get to work in my own space again.”
Charlie describes that whilst he is influenced by “other artists who inspire me with their energy and creativity,” his creativity is sparked by the world around him. “My Life. My experiences. My adventures with the world. My travel. And also my relationships, especially with people I love. All of this makes me feel happy. And when I am happy, I can ‘Let Go and Be Free.’ That is the best creative process for me.”
Charlie’s website describes him as ‘an intuitive abstract painter, known for his compositions of bright and colourful shapes,’ and goes on to explain how his ‘process is to be free, and embrace a blank canvas as an adventure in imaginative freedom. He loves textures, layers, geometric shapes and freeform markings he calls Charlie’s Designs.’




It concludes by noting how although recently he ‘has been inspired to create abstract landscapes he always returns to his beloved and sought-after series: In the Fathoms Below, Morning in Paris and Snowy Day.’ Over the years he has been featured in a number of articles across a range of media, he has worked on brand commissions and collaborations and has even had his work featured in both the US and abroad in private and corporate collections. When asked what he is most proud of, he answers simply “my career as a professional Artist! My ART is in a sports stadium, a hotel, corporate offices in London, New York, California and many other cities. And my ART is in homes around the world. I am pretty proud of that!”
But he is also not one to rest on his laurels, as although he has already exhibited in the US, Mexico, and the UK he is working hard towards his ‘biggest dream’, which is “for my ART to be in the Tate Modern museum.” And it is a dream he will doubtless realise, because above all Charlie lives by the advice which he would share with others, and that is to simply go out and “Do it. Follow your dreams. Think about what makes you happy, what inspires you and LET GO!!”


About Charlie French
To visit Charlie’s beautiful website click here: Visit Charlie’s website
About Down Syndrome Regression Disorder (DSRD):
To learn more about DSRD visit the National Down Syndrome Society (NDSS) website here: Visit the NDSS website

“The hospital radioactive isolation rooms are pretty grim, and you’re in there on your own. No one can stay in there with you, not even your family, as you’re giving off radiation.”
For some people it is their most difficult challenges in life which go on to not only change them, but also to change the world around them in unexpected and remarkable ways. In 2025 the Butterfly Thyroid Cancer Trust will celebrate its twenty-fifth anniversary, a huge milestone for any charity, but perhaps more so for one which started with one thyroid cancer patient kindly agreeing to have a chat with someone whose world had just been turned upside down by their own diagnosis.
In June 2000 Kate was 42 years old, and as she recalls, “Life was good. My husband Steven and I ran two very busy NHS dental practices, and we had a gorgeous 12-year-old boy, Daniel. When he went on a school trip to Paris we took the opportunity to go to the North East Coast for a few days on our own. One morning, after my shower I started to blow dry my hair, and I could
The Shape of a Butterfly
In conversation with Kate Farnell MBE, Founder & CEO of the Butterfly Thyroid Cancer Trust
see that the left side of my neck was protruding a little bit, it had happened overnight.” She wasn’t overly alarmed, indeed looking back she notes that had she found a lump in her breast she’d have called the GP immediately, but instead she showed Steven. He suggested she see one of his colleagues at the hospital, where he also taught part-time, on their return, which she did. An ultrasound followed, as the doctor felt that there was a possibility she might have thyroid disease.
“The ultrasound on the right side took seconds, but he spent ages looking at my left side. Eventually he just said that there was a tumour in the left side of my thyroid gland. He went on to say ‘but they’re always benign, so no need to worry, it’s not doing any harm and it’s only about two centimetres in size, so we will probably just leave it.’” But, Kate explains, as a nurse this simply did not sit comfortably with her, and so at her request he agreed to refer her on to a surgeon. “When he examined my neck his exact words were ‘there’s a considerable mass in your neck.’ He asked my age
and then explained that 42 was right in the age range for it to be a thyroid cancer. I knew what a thyroid gland was, but like a lot of people I’d never heard of thyroid cancer, it’s so rare. He went on to add that it might not be thyroid cancer, but when you hear that news you just go into a kind of free fall, fearing the worst but hoping for the best.”
Kate was admitted to hospital to have the left side of her thyroid gland out, and when the surgeon came to visit her once she was awake he explained that the tumour had been ‘a bit big and a bit messy,’ but that he’d managed to remove it. He went on to ask how her voice was, and on hearing that it was fine he was relieved, as he had been concerned that it might have been damaged during the operation. A week later
Kate and Steven returned to the hospital to discuss the pathology results following a biopsy on the tumour.
“I was anxious, but I still had hope. But by then I had lost my voice, and so I thought ‘what’s going on?’ When I went in the surgeon stood up from behind his desk, and he came round and he put his arm around my shoulder, and you just
know then. He said, ‘you’ve got thyroid cancer, I’ve also damaged the nerve to your voice box, and that’s why you’ve lost your voice. I looked at Steven and he looked at me, and we both had tears in our eyes. Then the surgeon said, quite famously, ‘what are you worried about? You’re fine. You’ll be fine.’”
Although Thyroid Cancer is rare the numbers are rising, and currently there are approximately 3,700 new cases in the UK each year. In the main the prognosis is excellent, with a 95% cure rate for the most common types of thyroid cancer. However, coming to terms with a cancer diagnosis is never easy, and for Kate, as for so many, telling those who loved her that she had cancer was devastating. “Telling my son and my elderly parents I had thyroid cancer remains one of the hardest things I’ve ever had to do.” The treatment protocols for thyroid cancer vary, and each patient will have a personalised treatment plan. Her medical team opted for a complete thyroidectomy (the removal of the entire thyroid gland), as they wanted to be sure that they had removed all of the cancer. So a week later she returned to the hospital for a second operation to remove ‘the other side.’
It proved to be a hugely difficult time for Kate. After her first operation and following a thorough examination at her follow up appointment, it was explained to her that she had sustained a laryngeal nerve injury during her surgery, which had produced a vocal cord palsy. Her surgeon explained to her that although the nerve was damaged, it might recover, but that this could take up to a year. Although she could still speak, she could no longer project her voice. The resulting quietness of her voice meant that it was hard for people to hear her at times, leaving her struggling to engage in day-to-day interactions in many situations. She reflects how “it isn’t until you don’t have a voice that you realise how integral it is to everyday life.” Her second operation led to her developing hypocalcemia, which is caused by the disruption of, or damage to, the parathyroid glands beside the

thyroid which manage and regulate the calcium levels in the blood. This can be a medical emergency, and in Kate’s case it was severe, resulting in a five day stay in hospital to receive urgent medical treatment.
After her second operation Kate then had to wait for seven weeks for her radioactive iodine (RAI) treatment, which is used to destroy any remaining thyroid tissue in the neck after a thyroid operation. During this time, she was not given any thyroid hormone replacement therapy, and she ended up developing hypothyroidism. “I was feeling very depressed by this stage and not being allowed to have my husband come into the room to visit me was the final straw. For me personally, the four days I spent in isolation were just the worst, and I was very anxious and depressed during the initial six months while I waited for my follow up scans.” Fortunately, her scans were clear, and life slowly returned to a new, if slightly altered, normal. “Everything was as good as it could be, and I thought that I should try to move forward, but it was hard and I was on antidepressants.”
It was around a year after her shock cancer diagnosis that Kate received a call from her surgeon, which would change the course of her life once again. “I’m a firm believer that once you experience something personally, like profound grief, a traumatic divorce, a
horrible accident or ill-health, then you know how it feels to go through it. One day, when I was at a supermarket checkout, my surgeon rang me and explained that he’d ‘just had to tell a 23 year old that she has what you’ve got. Will you speak to her?’ I said yes, and that was the start of what is now the Butterfly Thyroid Cancer Trust.”
That first phone call turned out to be exactly that, just the first of many. Initially, the calls would be made to one of the dental practices that the Farnells ran. But it soon became evident that the support that Kate was able to offer was truly invaluable and that the need for it would likely only grow, so they decided to install a dedicated telephone line for it. “Initially, it was just the doctors here in Newcastle that had the phone number, and every time they got a new patient, they would tell them about me. They’d explain that ‘Kate went through this herself a year ago, if you want to talk, here’s the number.’ That’s really how it started.” Eventually, Kate

was asked if she would consider attending the thyroid cancer clinic as a volunteer to meet patients in person. This proved to be a success as people valued having the opportunity to talk to someone with lived experience of what they were going through themselves. Over time, the demands on Kate grew, after three years they decided it was time to become a registered charity. Today the Butterfly Thyroid Cancer Trust remains ‘the first national charity in the UK dedicated solely to the support of patients with thyroid cancer.’
The following years were ones of huge growth, both for Kate personally and for the Butterfly Thyroid Cancer Trust. As well as the vital volunteer peer support offered via their dedicated helpline the charity began work on producing leaflets and QR code cards for distribution to other hospitals and clinics and creating and maintaining an online resource providing reliable and up-to-date written information about the disease. Kate began attending national and global conferences, adding that much needed, and hugely important, patient voice to conversations around the disease. Through the network of relationships that Kate and the trust built up over the years, she was able to contribute to two editions of the Practical Management of Thyroid Cancer book, and she was invited to join the NICE (National Institute for Health and Care

Excellence) Committee, which was working on thyroid cancer guidelines. The charity also funded and produced the first patient film about thyroid cancer. This film is now given to all new patients in the UK to watch, and remains one of her proudest achievements. It has been followed by more films, including one that has just been released, which was created specifically for young people living with thyroid cancer. All of the hard work has undoubtedly paid off, both in terms of the vital work that the charity and Kate do, but also in the recognition that their efforts have justly received. “We started to win prizes, we won five in a row, one after the other. I won Inspirational Woman of the Year award, and then after ten years, I was awarded an MBE 1 which was just amazing.”
One of the projects that Kate is most passionate about has been the trust’s campaign to make the
isolation suites, typically known as an RAI or iodine suite, less cold and clinical. The majority of thyroid cancer patients will need to receive a secondary radioiodine therapy treatment to destroy any remaining thyroid tissue in the neck after their thyroid operation. As this treatment is radioactive, patients will need to be admitted to the hospital and will have to stay in isolation for one to three days whilst their treatment is given. From her own experience, she knew that “generally the rooms are pretty grim, and you’re in there on your own. As you’re giving off radiation, no one can come in, not even family, and that’s so hard. I thought that we have got to be able to do this better. Does everything in the room really need to be covered in plastic? I sat down with the unit manager and explained that while I understood about radiation protection, I felt we could review what this needs to
really look like again. They agreed, so we formed a working party with all the top nuclear medicine teams from across the UK and we got it changed!” To date, the team at the Butterfly Thyroid Cancer Trust have redecorated 40 isolation suites across the country using beautiful bespoke vinyl wraps, which the ward staff choose from several themes. In addition they go a step further for children, recognising how hard it is for them to be isolated in this way. “We personalise the room as much as possible, buying bedding, cushions, throws and pyjamas, as well as presents and treats all based on a theme that is important to that child –most recently this included a ‘Stranger Things’ room which 11 year old Ollie absolutely loved.”
For many years, the charity operated on a shoestring, with the Farnells running it voluntarily, and simply
1 MBE stands for ‘The Most Excellent Order of the British Empire’, and it is a recognition given to reward contributions to charitable and welfare organisations amongst other categories.
incorporating the dayto-day running costs into their domestic bills, and largely managing it from their home office. Over time, however, some of the patients they had supported, along with their families and the communities around them, began to fundraise and it is these vital funds that will help ensure the future of the charity. As the charity continued
to grow, Kate explains that the trustee board were concerned that such a huge workload would eventually prove too much to juggle alongside her work, life and other commitments. “They explained to me that we’ve got to bring somebody in to run the charity, to ensure it remains sustainable even once you are no longer able to do it.” They proposed that

they would like to formally employ her as the first CEO of the charity, a role which she was of course best placed to fulfil. The covid-19 pandemic brought a huge increase in workload with it, and Kate was often still working late at night to try to respond to the, understandably desperately worried, thyroid cancer community. Once again, the trustee board recognised that this enormous demand on the charity would be too much eventually, and worked hard to be able to introduce a new patient support worker role to the charity.
What started with a phone call from one thyroid cancer patient to another has grown into a vital national patient support organisation, in large part due to the unwavering determination, drive and commitment that Kate has given over the last twentyfive years. But now, whilst she has no immediate plans to retire or step back, she is reassured to know that the awesome responsibility that the charity brings with it no longer rests entirely on her shoulders. “The charity was my baby from day one, but I know that I could walk away from it now and it will continue to be successful, because everything is in place.” What could be a better way to celebrate twenty-five brilliant years than the knowledge that your life’s work, the charity to which you have given your all, can continue to offer its vital support services to the wider thyroid cancer community for many, many more years to come.
What is Thyroid Cancer?
The thyroid gland is a small, butterfly-shaped organ located in the front of the neck, straddling the windpipe (trachea). It is part of the endocrine system and produces hormones that regulate various functions in the body.
Cancer occurs when cells in a specific part of the body divide and begin
to grow and reproduce uncontrollably, and thyroid cancer occurs when the abnormal cells are located in the thyroid gland.
The symptoms of thyroid cancer can vary and can also be missed or misdiagnosed as something else, as they can include a hoarse voice, difficulty in
swallowing as well as more obvious signs such as a lump in the neck. Likely treatments include surgery, radiotherapy and targeted drugs .
For more information and support please visit the Butterfly Thyroid Cancer Trust here:
www.butterfly.org.uk

What We’re Into
Film Review:
Out of My Mind
Directed by Amber Sealey
Having seen many posts on different SEN (Special Educational Needs) related social media platforms about the film ‘Out of My Mind’, we knew we had to watch it! Released on Disney+ in late 2024 the film is directed by Amber Sealey, and based on the hugely popular book of the same name written by Sharon M. Draper, and published in 2010.
The film is set in the US, and tells the story of Melody Brooks, a sixth-grader in middle school who lives with cerebral palsy, is nonverbal and uses a powered wheelchair to navigate the world. Despite having beyond average intelligence and a photographic memory, she has been placed in a mixed-ability SEN block, and is both bored and frustrated by the world around her. The film follows Melody as she is allowed to try taking part in a mainstream class, and tries hard to make friends and to show the world who she really is. In some ways, the film could be criticised for being a bit of a Hollywood cliché, with the inevitable highs and lows that are to be found in any good coming-of-age drama. There is a real truth to the film however, in large part because of the utterly compelling debut by British actress Phoebe-Rae Taylor, who is absolutely brilliant.
She has a huge screen presence, and her ability to convey a range of, at times conflicting, emotions is beautiful to watch.
Having not read the book, it’s not clear how closely the film follows it, but it was interesting to learn that although it is a piece of fiction Draper’s daughter has cerebral palsy, and she also worked as a speech therapist for many years. Perhaps it is because Melody’s story is firmly rooted in the author’s personal experiences that there are many aspects of the film that felt like a

realistic portrayal of the challenges faced by some children with disabilities, and not just another ‘feelgood’ film. We cried, we felt angry, then hopeful, and throughout we also laughed. Especially when Melody’s neighbour, one of the few people who seemed to be able to truly see Melody for who she is, uttered the brilliant line “You’re going to have people taking care of you for the rest of your life. At some point you better learn that just because someone wipes your arse it doesn’t mean you have to kiss theirs.”
Book Review:
What to Do When I’m Gone:
A Mother’s Wisdom to Her Daughter
Written by Suzy Hopkins and illustrated by Hallie Bateman, published by Bloomsbury
“Funny and pragmatic and fully illustrated in gouache paintings by me”
After I read this great little book, which was written and illustrated by a mother and daughter, I decided to visit both of their Instagram accounts. I loved the way the illustrator, Hallie, summed up the book in the above quote, because it really is exactly that. The advice that the Mum, or Mom, Suzy, shares with her daughter really is both pragmatic and funny. And as the term ‘gouache’ has been used to describe both a product and a technique which was used as far back as the fifteenth century to paint images for written manuscripts, it too is the perfect way to describe the bright and accessible images created to illustrate the wisdom that this book shares.
The idea for the book came about after Hallie had the painful realisation that her Mum would one day die, and
not always be there to help guide her through life. So she asked her to write some concrete advice, or even instructions really, out for her that would help her to know what to do and how to cope once she was gone. The resulting book offers the reader some very real, and practical advice, and whilst the examples given are undoubtedly those which Suzy really feels will help her daughter to cope when she dies, they could easily be reinterpreted as needed. For example, the list begins with “pour yourself a stiff glass of whiskey and make some fajitas” but it could as easily be ‘make yourself a hot cup of sweet tea and bake yourself a cake/some scones’ or whatever food you turn to for comfort. Because really, it is about getting back up, and making yourself engage in the reassuring and daily routines and rhythms of cooking, not what is being cooked, that is the real wisdom being shared. The book begins with very clear suggestions for the days, weeks, then months and finally years that follow the loss of a loved one, starting with day one and ending on day 18,000 when the
daughter is herself an old lady reflecting on her own life. It is this final part of the book that I found truly moving, the realisation that we must all live and navigate our own lives. That “Even though it comforts you to get my advice and trust me, I have no shortage of it, you already know all the answers. In fact, you don’t really need this book. I was happy to write it with you, but you don’t need it. You already have what it takes to carry on without me.”
Available from all good booksellers.
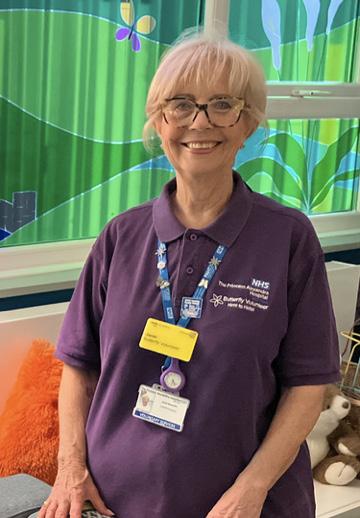
Meet the Professional
In conversation with Janet Granville, Butterfly Volunteer at the Princess Alexandra Hospital.
‘No-one
deserves to die alone’
For our ‘Meet the Professional’ feature we talked to Janet, a Butterfly Volunteer at the Princess Alexandra Hospital in Essex. The very first team of Butterfly Volunteers was launched in June 2017 at the hospital in partnership with the Anne Robson Trust.
The Anne Robson Trust received charity status in 2018, but the story that led to this milestone began in 2010, when Anne was admitted to hospital following a series of falls. The hospital was hugely overstretched, and the under-resourced NHS staff ‘failed to deliver the care Anne needed.’ In addition, there was a norovirus outbreak at the time and so her family were not allowed to visit, and the hospital also failed to ‘communicate sufficiently with her family,’ further adding to the enormous difficulty of that time. Anne died just hours after she was discharged, and the serious lack of appropriate care that she received was felt to have contributed to her death. Her devastated daughter, Liz Pryor, was determined that no other family should go through such
a challenging experience, and over the coming years she went on to work with numerous charities in and around the NHS.
The Anne Robson Trust works alongside 25 partner healthcare organisations to provide companionship and support through a network of trained end of life volunteers. Their work is driven by the belief that no one should have to face their final days alone. And it is the wonderful volunteers like Janet who help turn this mission into action, and whilst the motivation that each volunteer brings with them will doubtless vary, for Janet it was also her experiences with her mum in her final days that have led her on this Butterfly volunteer journey. She explains that when her beloved mum was 93, and living in a care home that supported people living with dementia, she had had a fall. She was admitted to hospital where it was established that she would need to have an operation on her hip which was broken. Unfortunately she became immobile after the surgery, and her health rapidly deteriorated.
“When she went downhill, they put her in a side room, and me and my daughter stopped with her the whole
week, and by then we realised that she was dying, and it was beautiful because we were with her on that journey. The hospital staff were fantastic, and their Butterfly volunteers came in and saw to us, but at the time I didn’t know what they did, and we didn’t need their assistance.”
“When I used to walk into the ward, I saw lots of people who were in the same situation as my mum, but they didn’t have anybody with them, and nobody came to see them. I used to just sit by their bed, hold their hand and talk to them. I think it taught me something about myself, and I really enjoyed being with these other people. Mum was there for a week before she died, and it was a beautiful death, peaceful. But I’d cared for her for so long and I was left thinking ‘what am I going to do now? My life is empty.’ It was almost like a lightbulb moment because I realised that this is what I needed to do. I needed to be with people who need help, who just need the company, and the empathy that my mum had had.”
Over the course of her career Janet had always worked with people, first as a hairdresser, then teaching hairdressing before setting up and
managing her own busy salon. After a period of illhealth, during which she had briefly stopped working Janet knew she needed to be back out in the world. She began working in a dental practice where she stayed for many years, before eventually leaving to care for her mum. She has always “Loved being with people, as I love having conversations about all sorts of different things with all sorts of people.” After her mum had passed away, and she had learnt about the work of the Butterfly volunteers she knew that it was the right fit for her. She describes how she wrote to the hospital explaining
that she was interested in volunteering, however the global Covid-19 pandemic hit and her plans were put on hold whilst the world, and the NHS especially, was turned upside down. But, once the hospital was able to begin training volunteers again, and had done all of the necessary background checks, she was finally able to begin her Butterfly volunteer journey.
Janet explains that each hospital setting manages their own volunteer teams, with the core training provided by the

trust. The Princess Alexandra hospital website outlines that ‘the role of the Butterfly volunteer is to provide support and companionship to our patients in the last days and hours of their life. They also provide respite and comfort to family members and relatives as they face the loss of their loved one… This is a particularly emotional role, yet very rewarding. Our Butterfly Volunteers are provided with bespoke training and support before being able to volunteer.’
It is vital that volunteers feel ready and able to meet the demands of the role, and as such the time it takes to train will vary for each volunteer, to be sure that when they begin their own visits they are confident and comfortable in offering the support that each individual patient might need. Janet describes how “After I’d had all my initial meetings and interviews, I began my training. Much of the initial learning process was online, and then I began by shadowing a lovely mentor who I was with for a month. We went onto the wards, and we saw people, and then over time as I gathered more knowledge and felt comfortable I took the lead with the patients we visited. After that month I worked with another mentor, learning so much from her as well, because we all work slightly differently. I was in my element, I loved being part of it, and it was just lovely to know that I was being able to do something to help other people.”
When a volunteer arrives for their shift they will go to the Butterfly hub, where they will have a chat with the Butterfly coordinator and discuss the patients that they will be visiting. Each patient will have been referred into the service by the palliative care team, and where applicable this will have been discussed with them and their loved ones so they will be expecting the volunteer’s visit. If the visit is to be the first one that a new patient receives then the Butterfly will take a lovely care package with them as a comforting gift. In it there will be a number of different items, which will include a beautiful, crocheted blanket made with love by volunteers, as well as essentials such as a toothbrush, toothpaste, comb, notepad and other small items. Janet explains how the way a visit unfolds will vary depending on the situation, for example if a patient


is conscious or not, or if they are alone or with family and friends, but she always begins by introducing herself, and explaining who she is.
“You assess the situation as it comes to you, on a first visit I could be there for ten minutes, or I could be there for an hour. If the patient is responsive, maybe talking to their relatives, then after I’d introduced myself I check if they are comfortable and have everything they need. Typically I’d then offer them all teas and coffees, and to answer any questions they might have. We will also make sure that families have parking permits for the hospital car parks. We have a beautiful hub which we are very proud of, so I encourage the family and friends of the patients to take respite breaks there. It means that they are able to relax, make themselves hot drinks and also use the bathroom facilities if needed. I explain that I’m more than happy to sit with the patients whilst family are using the hub, for however long they might need.”
Janet continues, noting that there are times when “Some people, some relatives, are so agitated they don’t want you there, so
we simply offer that should they need any help we can call back later. Or they might ask that I help them with something, perhaps even to advocate on their behalf with the hospital, as we get to know the nursing teams quite well.”
As Janet explains there are of course, also times when patients are alone. “If when I go into a room and there’s a patient on their own, and if they are unresponsive perhaps, I will still introduce myself, and then I will sit with them. If it feels right I will gently touch them, maybe their hand, or by resting my hand on their shoulder, just to let them know that I’m there. If they don’t want to be touched I will know as they will shift, or stiffen. I’ll talk about the weather, and make other conversation, and then I’ll maybe just sit quietly with my hand on theirs until I feel that they’re comfortable, and it’s time for me to leave. I know when it is the right time to go, and actually it’s the same when you’re with relatives, you just sense when it’s time to go.”
The main purpose of the Butterfly role is to be there, to offer compassion, empathy and support to individuals and families who are facing death, and the grief that this brings with it. Although it is undoubtedly true that death and dying are part of life they are not often talked about, and it is perhaps this very separateness with which we treat death, that makes the Butterfly volunteer role so incredibly special. To have someone who will sit with you and be there with you and your loved ones in those final weeks, days or even hours of life is a true gift. “There are times when I’ve been with patients, and they’ve died. If they’ve been on their own then I’ve just sat with them, I’ll hold their hand and I’ll wait with them until a doctor has come and certified the death. I won’t leave a patient on their own until I know that someone is with them, and it’s the same with patients who have their relatives or loved ones with them. After a patient has died I encourage the families to use the hub to take respite, to pause a little longer before they go back out into the world.”

For the Anne Robson Trust it is this which lies at the very heart of their work; ‘We believe that everyone should have the comfort and companionship they deserve at the end of life. They should also have the support to feel more prepared, whether they’re facing their own death or supporting someone close to them. We work with healthcare organisations to help make this possible.’ There can be no doubt that for volunteers such as Janet being a Butterfly is an honour, and so much more than a role, and their commitment to their patients speaks to the people that they are, and the values that they hold. “I’ve now been a Butterfly for three years, and I love being involved. It is such an honour to be allowed to be part of a patients journey into death. I love going to the hub, I love what we do, and I love being part of the Butterfly team.”
For more information please visit the Anne Robson Trust here: www.annerobsontrust.org.uk
You can visit the Princess Alexandra Hospital Butterfly team here: www.pah.nhs.uk/our-volunteers

Bits & Bytes:
Growing-up in Today’s Technological Age
Exploring the benefits and challenges of technology use in early years
In today’s world technology, and knowledge of technology, are essential parts of life. We increasingly rely on it in many industries, and of course to support and enhance our lives. The majority of the infrastructure of our work and homes use technology, from communications through to turning on the lights at home! Technology is here to stay, and as it is constantly changing and developing it is essential that children learn to use it well.
Some of us may have, or know, elderly friends and relatives who struggle with it, making their lives harder. Even we as adults can get a bit lost whilst using it, for instance, the faff of ordering food on an app, or a program that keeps giving error messages—not to mention remembering multiple complicated passwords - I am sure we all know the frustrations as well as the benefits it offers. But being comfortable using technology from childhood may have made life a little easier at times for us all.
Technology is designed to make our lives easier, but the instant access it offers can have negative effects on children too. It’s so important that we teach children to use it well from a young age, setting good lifetime habits
by promoting a healthy balance of technology use. Below are some insights into some of the positive and negative side effects of technology, and how to manage its use effectively for children.
The Positive Effects
Digital Literacy: The use of technology in childhood helps children to develop essential digital skills, and being tech-savvy from a young age will help prepare children for a world increasingly dominated by digital technologies. Familiarity with technology helps them navigate our ever-evolving tech-driven world.
Learning and Creativity: Educational apps and games can enhance cognitive skills like problem solving and critical thinking while having fun, and interactive learning experiences can also make education more engaging and fun. Digital art tools and music-making apps allow children to express their creativity and develop new talents. The internet offers a wealth of information at children’s fingertips, providing a valuable resource for learning about new subjects, completing school projects, and satisfying their natural curiosity about the world.




Social Connections:
Technology makes it easier to connect with others who share the same interests and hobbies, creating online communities. For marginalised or neurodivergent children online communication can provide a vital sense of belonging and connection if they can find or build safe online communities where they feel understood and supported.
Collaboration and Communication:
Technology facilitates a new form of collaboration and communication through tools like video calls, shared documents, and online classrooms. These tools help children work together on projects and communicate effectively, even when they are not in the same physical space.
Personalised Learning:
Adaptive learning technologies can tailor educational content to the individual needs and pace of each child. This personalisation helps ensure that all children, regardless of their learning style or ability, can succeed and progress at their own pace.
The Negative Effects
Screen Time: Excessive screen time can impact on children’s sleep, physical activity, and face-to-face interactions. The blue light emitted by screens can interfere with the body’s natural sleep cycle, leading to difficulties in falling asleep and poor sleep quality. Inadequate sleep can affect mood, behaviour, and cognitive functions. It’s important to ensure that
technology does not dominate their daily routines.
Health and Lifestyle: Too much time spent on screens can lead to sedentary lifestyles, increasing the risk of obesity and related health issues. Time spent on screens often replaces time that could be used for physical activities, affecting overall health, motor skills development, and physical fitness.
Behavioural Issues:
Overuse of technology can lead to reduced attention spans, trouble focusing, and increased aggression. Children might also become more irritable and less patient when accustomed to instant gratification from digital media.
Social Skills: Relying heavily on digital communication can hinder the development of essential social skills. Children may struggle with in-person interactions, understanding body language, and building strong interpersonal relationships.
Mental Health: Overexposure to social media and the internet can lead to issues such as anxiety, depression, and low self-esteem. Constant comparison with others, cyberbullying, and the pressure to maintain an online presence can negatively impact children’s mental health.
Online Safety: Children may be exposed to inappropriate content, cyberbullying, and online predators. Without proper guidance and supervision, they can easily fall victim to scams, phishing, and other online dangers.
Balancing Technology Use
By integrating technology thoughtfully into children’s lives, we can harness the positive effects to support their growth, development, and overall well-being. It’s all about striking the right balance and using technology as a tool to enhance their experiences while minimising its potential drawbacks. We know that balancing technology and life can be a challenge, but several strategies can help children use technology healthily and productively.
Set Boundaries: Establish clear rules for screen time and encourage offline activities, this can include setting times for using devices and promoting a balance with outdoor and/or physical activities. Consistent routines will help children understand and respect these boundaries.
Monitor Content: Supervise and monitor children’s technology use, particularly with online access and use parental controls to ensure children access age-appropriate content. Discuss what they watch and play, encouraging critical thinking about the media they consume - be involved and keep communication open.
Encourage Balance: Promote a healthy balance between technology use and other activities, such as board games, reading, sports, and family time. Creating a balance between online and offline activities fosters well-rounded development.
Be a Role Model: Children often emulate adult behaviour, so demonstrating a balanced approach to technology use yourself can encourage children to follow suit. We all know how
easy it is to spend time mindlessly scrolling through social media or watching cat videos. Show them how to enjoy life without constantly relying on screens, put down the phones and do something together that’s fun.
Promote Tech-Free Zones: Designate certain areas of the house as tech-free zones, like the dining room or bedrooms, this can help create spaces dedicated to family time, relaxation, and sleep, free from digital distractions.
Educational Use: Guide children towards educational apps and websites that promote learning and creativity and encourage them to use technology as a tool for gaining knowledge rather than just entertainment.
Physical Activity: Encourage regular physical activity to counterbalance sedentary screen time, activities like sports, dancing, or simply playing outside are crucial for physical health and overall well-being.
By implementing these strategies you can help children develop healthy habits and a balanced approach to technology use, ensuring it enhances rather than hinders their growth, development, and daily lives. Balancing technology use by setting clear boundaries, monitoring content, and encouraging offline activities is essential for mitigating possible negative side effects. By promoting a healthy balance, children can enjoy the benefits of technology, standing them in good stead as technology evolves throughout their lives. As with everything, moderation is key!


Photograph courtesy of the Roy Castle Lung Cancer Foundation, Like Me campaign – featuring 10 women diagnosed under 50

Lung Cancer can Affect Anyone
Contributed by Rachel Avery, Director of Communications and Engagement at the Roy Castle Lung Cancer Foundation
“The fact is lung cancer can affect anyone. It can affect men and women. It can affect people in their 20s and people in their 80s. It can affect people who smoke, who used to smoke and who have never smoked.”
Founded in 1990, Roy Castle Lung Cancer Foundation has remained as committed to improving outcomes for lung cancer

as the charity’s namesake was dedicated to breaking records! Many of us will remember the legendary entertainer, Roy Castlebe it for his outstanding musical talent, tap dancing prowess, his guest roles in Dr Who or Carry On Up the Khyber, or as the presenter on family favourite TV show, Record Breakers.
Equally, many will recall his brave and public battle with
lung cancer. It was in 1992 when Roy Castle revealed he had lung cancer. As someone who had never smoked, the news shocked the nation and shone a spotlight on the disease that, until then, had very much remained in the shadows.
In July 1994, Roy Castle teamed up with the then Lung Cancer Fund for the Tour of Hope, a 3-day
journey across the UK to raise awareness of the disease and raise money to build the first ever lung cancer research centre. Less than two months later, Roy Castle died and whilst he never saw the impact of his work, thousands have benefitted from it through the charity that today proudly bears his name.
Roy Castle Lung Cancer Foundation, renamed
in 1995 to commemorate Roy’s incredible legacy, is the UK’s leading lung cancer and only charity solely dedicated to supporting everyone affected by the disease. Its research – much of which was undertaken at the centre funded by Roy’s Tour of Hope endeavours – has successfully laid the groundwork for lung cancer screening, which is now rolling out across the country, as well as helping to identity new ways to diagnose and treat the disease.
The charity also provides practical and emotional support to all those affected, including the loved ones of those diagnosed. Through face-to-face, telephone and online support, the charity ensures no one goes through lung cancer alone. Because lung cancer can be a very lonely place, the intrinsic links to smoking shrouding the disease in stigma. Upon sharing a diagnosis, patients are inevitably met with the question “Did you smoke?”
For Roy Castle Lung Cancer Foundation, this question is as unhelpful as it is dangerous and why the charity has made campaigning a key area of its work as Rachel Avery, Director of Communications and Engagement, explains: “When you say the words lung cancer, I think many people would conjure up a similar picture. They would associate the disease with someone who is older, possibly male and probably someone who smokes. These assumptions are not wrong per se. The average age of a lung cancer patient is 74. The majority of cases are caused by smoking. However, where the danger lies, is failing to see beyond these stereotypes.”
“The fact is lung cancer can affect anyone. It can affect men and women. It can affect people in their 20s and
people in their 80s. It can affect people who smoke, who used to smoke and who have never smoked. And yet, someone’s smoking history remains the primary focus of their diagnosis. Whilst this is an issue in its own right (because the reasons why someone smokes or not are never black and white but that’s a whole different article!) this emphasis on smoking is stopping people from getting diagnosed earlier.”
“If someone has smoked, they can more reluctant to seek help because they feel guilty or ashamed whilst if someone has never smoked, they often face multiple visits to their GP or have their symptoms misdiagnosed because they don’t fit the profile. In either case, diagnosis is delayed and the chance to save their life diminished.”
For many years, the charity has set out to challenge these misconceptions, running awareness campaigns that demonstrate the reality of lung cancer and its diversity. From its Like Me campaign which featured 10 women all diagnosed under the age of 50, to its most recent venture, Let Go of the Labels, the aim remains consistent. Rachel continues, “Our campaigns may be dressed differently each time, but ultimately the message is the same – if
Photograph courtesy of the Roy Castle Lung Cancer Foundation, from the YOU’RE WRONG! social ad campaign
you have lungs, you can get lung cancer.”
“Smoking causes at least 16 types of cancer, but it is only lung cancer that has that immediate association. What we want is simply for everyone to recognise that just like other cancers, lung cancer is a disease that can affect anyone. But in order to convey this simple message, we must be innovative in our approach. The assumptions and suppositions mean people are less likely to engage with something about lung cancer, so we try to find ways to talk about it without directly talking about it! We have worked with a standup comedian. We’ve gone down the direct approach and simply stated YOU’RE WRONG! in a series of social media ads. We’ve featured stories of people who you would never in a million years expect to have lung cancer.”
“I think my favourite piece of work was part of our Still Here campaign which launched during the pandemic. As with all cancers, referral rates plummeted at the peak of Covid, but lung cancer faced an additional challenge. For years, people were told if they had a persistent cough to go their doctor. Now they were being told the exact opposite – if you have a continual cough, stay at home. The impact was devastating; people being referred for tests for suspected lung cancer fell by 75%. Lung cancer hadn’t gone away. It was just being allowed to thrive
under Covid’s shadow. Our Still Here campaign aimed to shine a spotlight back on lung cancer and remind everyone that a cough didn’t not just mean Covid.”
“We worked with shadow theatre company and past winners of Britain’s Got Talent, Attraction, to create a truly unique and beautiful performance to depict the impact of Covid-19 on lung cancer and highlight the importance of acting on symptoms even during the pandemic. And with over 2.2million views on social media, plus an airing on BBC 2, we were so proud of the impact it had. And that’s the reason we put so much hard work and effort into our campaigns. We don’t just devise clever or fancy campaigns for the sake of it. We do it because it can help people get diagnosed earlier, and when that happens, that person’s chance to surviving drastically increases.”
“This again is another misconception many people have. There is a belief that lung cancer is an instant death sentence. It isn’t. When lung cancer is caught early, it is possible to cure it. And now, thanks to advances in treatment and sustained investment into research, even later stage disease, whilst incurable, is still treatable - and liveable.”
Rachel expounds further, that really “It all comes back to that simple message we are trying to convey through every campaign we do (and the tagline to our 2023 Be Unforgettable campaign) –forget everything you think
you know about lung cancer. These are the facts. Lung cancer can affect anyone. You don’t have to have smoked to get lung cancer. There are many different symptoms, and you might not have a cough. Lung cancer can be cured. Nobody deserves lung cancer, and everybody deserves the chance to be diagnosed as early as possible.”
Rachel concludes with a return to one of the key messages that they share; ‘if you have lungs, you can get lung cancer.’ And at the very heart of what they do is the continued commitment to be there, because the “Roy Castle Lung Cancer Foundation is here to support everyone affected – and we’ll continue to think up new and inventive ways to talk about lung cancer until everyone finally sees past the typecast.”


About Lung Cancer
Lung cancer is the UK’s third most common cancer and the biggest cancer killer. Accounting for over a fifth of all cancer deaths, lung cancer takes the lives of more people than breast, prostate and pancreatic cancers combined.
Smoking remains the biggest cause of lung cancer, with approximately 72% of cases caused by smoking. However, smoking is by no means the only cause – a common misconception Roy Castle Lung Cancer Foundation continues to fight against by highlighting If you have lungs, you can get lung cancer. Other risk factors include air pollution and exposure to certain work-based chemicals, such as asbestos and silica.
Symptoms can include:
• A persistent cough that lasts three weeks or more
• Shortness of breath
• Repeat chest infections
• Coughing up blood
• Fatigue
• Weight loss or loss of appetite
• A cough that changes or gets worse
• Shoulder pain or back pain
• Wheezing or hoarseness.
Anyone experiencing any of these symptoms is urged to contact their GP.
For more information about lung cancer, the work of the charity or for help and support, visit www.roycastle.org

Please tell us a little bit about yourself:
My family is made up of my mum, older sister, my twin brother Matt, my dad and my step-mum. I was born first and weighed 2lbs, my brother weighed 3lbs. When I was around 6 months old my parents had taken us to watch some fireworks, and although I was watching them I wasn’t reacting to the sound, and my mum said to my dad that she thought I was deaf. I had already been diagnosed with cerebral palsy, and after my mum took me for tests it was confirmed that I was deaf when I was around 10 months old. My parents both cried when they found out, they were shocked and emotional. But they started learning BSL sign language, so that they would be able to communicate with me as I got older.
I had my first cochlear implant at 18 months old, and my second when I was 7 years old. I struggled wearing both, it was simply too much sensory overload, but I had to wear them both for school. Now I only wear one and it’s much better.
I was diagnosed with epilepsy at around 6 years old. It’s hard when you have epilepsy, it’s my main challenge really, but I try to put the epilepsy in a box and just focus on myself. I am happy and I don’t care about epilepsy! I’ve got my family, my friends and the people who I love - it’s important to be happy.
When did you start training in a functional fitness gym and what made you start?
I was bullied throughout secondary school because I’m disabled. When I was 13 or 14 my mum asked the PE teacher if I could get involved with school sports but he said no, that really hurt me a lot. My twin brother started going to the gym around that time and he agreed to take me, he is my best friend, the best brother in the world and always has my best interests at heart. But by then I’d lost my confidence, and was also struggling to stand and to walk. My mum found a personal trainer on Facebook, a man called Craig Graham, he was tall, covered in tattoos and just really cool, I was nervous but I thought ‘let’s do it’!
I was his first client with cerebral palsy, and he has helped me so much. He helped me build strength, I can stand straight now, he just really helped my confidence – and I have taught him how to sign. We started training in his garage gym, then had to go online during Covid which I hated, then after we

went back to training in person he decided to start Alternative Movement, and he asked me to join him. He explained that he wanted to create a space where people with all kinds of disabilities could train.
When did you decide to become an assistant coach, and why do you enjoy it?
When Craig first asked me if I wanted to help in the gym, and become an assistant coach I said yes! I was at college then, but in the half term I started helping with kit, and supporting him in classes with able-bodied clients and with disabled clients. When I met Freya, a new client who was just 5 years old I felt really emotional. She had cerebral palsy too, and was even more ‘wobbly’ then I had been and I just wanted to help her, and maybe be a role model to her, because it’s really, really important to see people like yourself. So working with disabled people is my passion. I want people to get involved, because it is so important to be included – I’m lucky I had the opportunity to work with Craig, and to be an assistant coach.
Which achievement are you most proud of?
I started CrossFit 4 years ago, and I love it. I’ve taken part in a number of competitions, including Wodadaptive, a mixed pairs competition, which means an adaptive athlete competing alongside an able-bodied athlete in a
team. I loved it, it is such a powerful community event! We’ve had the opportunity to become brand ambassadors which really gives me so much confidence. We were also filmed for a TV show called ‘ALT Jay’ which was even shown on Channel 4, and which tells mine and my brother’s story. When people contact me, and tell me I’ve helped them, it means so much. I work hard to have a strong body, and a strong mind and to build up my confidence, and if I can help people, both disabled and ablebodied, and get them involved with fitness then that means everything. When I work out I don’t feel like a disabled person,
I just do my workout and it feels like it does for anyone else – being active is just so important for all our futures. And when you work out you are building up your attitude and resilience too!
What advice would you give to other people?

Don’t give up on yourself! Keep pushing and keep chasing your dreams. Alternative Movement, Craig and all the team have become my second family.
Like my brother, Craig is my best friend as well as my coach, he also has my best interests at heart and is always there for me. I have found my place, and now I have big dreams –my dream is to compete in the Adaptive Division at the CrossFit Games one day!
You can follow Jay’s journey here:
Visit Jay’s Instagram
You can find out more about Alternative Movement here:
Learn more
About Cerebral Palsy:

5 QUESTIONS WITH
Cerebral palsy (CP) refers to a group of lifelong conditions that affect movement and co-ordination, also known as movement disorders. CP is typically caused by the abnormal development or damage to the brain, and most commonly develops before, during or soon after birth. The symptoms of cerebral palsy vary both in presentation and severity with each individual, but often include delays in reaching developmental milestones, increased or decreased muscle tone (seeming too stiff or too floppy), jerky, random and/or uncontrolled movements amongst others. This is because the areas of the brain that control movement, balance, and posture are often impacted. However, CP can also include a range of other problems, for example with the senses; vision, hearing, and speech.
To find out more please visit the NHS website resource, linked here:
Learn more
About deafness:
Deafness, or deafness, refers to the total or partial inability to hear sounds, typically if the word Deaf is capitalised it refers to people who have been Deaf since birth. Deafness can be caused by different factors, and there are also a number of different types of deafness, these include conductive, sensorineural, and mixed deafness, each with their own distinct causes and characteristics. Likewise symptoms vary, and can or might include difficulty understanding speech, muffled sounds, and trouble hearing in noisy environments. There are also different management options, include hearing aids, cochlear implants, and other assistive devices, as well as preventive measures to protect further hearing loss.
To find out more the National Deaf Children’s Society has some great resources, linked here:
Learn more
Dying to be Heard
A call for those at the end stages of life to share their journeys and experiences.
‘Dying to be Heard’ is an evocative and thought provoking project dedicated to exploring and amplifying the voices of those receiving palliative and end-of-life care. Recognising the unique experiences that accompany the final stages of life, we want to highlight the personal experiences during this time.
Each account will be transformed into powerful visual creative narratives and presented in an exhibition aimed at influencing improvement in healthcare policy and practice.
By taking part we hope it will provide a deeper understanding of what truly matters to individuals at the end of life and the narratives used are aimed at designing more empathetic and effective services for future generations.
Participants will engage in a heartfelt conversation about their lived experiences, cherished memories, and the decisions they face as they approach the end of life. These dialogues will be captured through film, written narratives and creative photography, ensuring that each story is honoured and preserved with dignity.
Your experiences really can help make a difference. We are happy to answer any questions you might have. If you or a loved one are navigating the final chapters of life and would like to take part please do contact enquiries@samebutdifferentcic.org.uk

www.samebutdifferentcic.org.uk/whatmattersmost
A LIFE SHADED BY PAIN
www.gbs-cidp.org
CAPTIVATING CRETE
www.cretamaris.gr www.cretaquarium.gr www.instagram.com/estrella_chania www.knossos-palace.gr www.mitsis.com/en/hotels/ laguna-resort www.petousis-tavern.gr/en/index.php www.stellaisland.gr www.7thalases.gr/en
DYING TO BE HEARD www.samebutdifferentcic.org.uk/ whatmattersmost www.tnlcommunityfund.org.uk/ funding/wales
LUNG CANCER CAN AFFECT ANYONE www.roycastle.org
FOLLOW YOUR DREAMS
www.charliefrenchfineart.com www.ndss.org/resources/ regression-down-syndrome
Supported by:


MEET THE PROFESSIONAL www.annerobsontrust.org.uk www.pah.nhs.uk/our-volunteers
THE IMPORTANCE OF CONNECTION www.gbs-cidp.org
THE SHAPE OF A BUTTERFLY www.butterfly.org.uk
THE TRANSFORMATIVE POSSIBILITIES OF GENE-SILENCING MEDICATIONS
www.porphyria.org.uk
TRAVELLING THE WORLD FOR A DIAGNOSIS
www.freewheelchairmission.org www.give.freewheelchairmission.org/ fundraiser/5272762 www.rarediseases.org www.reneebruns.net
5 QUESTIONS WITH www.altmovement.co.uk www.instagram.com/southernjj77 www.ndcs.org.uk www.nhs.uk/conditions/cerebral-palsy



Connect with meaning and honesty

We produce powerful films, strong imagery & compelling narrative; creating a visual storytelling experience that allows you to connect more closely with your audience.
We work with organisations, agencies and publications that love to make an impact. We can join as a creative partner and help shape the creative direction into an impactful photography campaign or film, or we can work to your brief.
Helping you connect to your audience with integrity.
Creativity. Collaboration. Empowerment.
Find out more by visiting: www.sbdcreative.co.uk
