

Volume 16 No 3 / June 2020 Quarterly publication of The Royal Australian and New Zealand College of Radiologists Our Advocacy: A Good News Story for Breast Cancer Patients Trainees Rise to the Challenge: NZ Interisland Coronoschool The COVID-19 Impact on Services and Practices Also Featured in this edition College Pandemic Response Update ➤
YOUR WELLBEING IN PUBLIC HEALTH CRISES An Examination of the Demands on the Professions
MAINTAINING

“We innovate and adapt” At I-MED Radiology, we have a vision: to be the most respected and trusted medical imaging specialists in the world. And at the heart of that vision is our commitment to innovation. If you are interested in finding new and improved ways of doing things, if you have the courage to adapt and deal with change, then come and talk to us. Discover what it’s like to work with a world-leading organisation with innovation in its DNA. Contact our careers team T: +61 2 8274 1080 E: careers@i-med.com.au www.i-med.com.au/careers
5 19 22
8 A Joint Message from President and CEO
Maintaining Your Wellbeing in Public Health Crises: An Examination of the Demands on the Professions
Trainees Rise to the Challenge: The New Zealand Interisland Coronoschool
The COVID-19 Impact on Services and Practices in Clinical Radiology and Radiation Oncology
Training and Assessment Reform: What's the Plan? Changes to Your Medical Registration Requirements
What are your thoughts?
Cardiac MRI Certification Update
RANZCR Workshops, Courses and Events 2020
College Honours 2020
Targeting Cancer
The State of Neurointervention Practice in Western Australia
From the Faculty of Clinical Radiology
Chief Censor Update: Clinical Radiology Training During the COVID-19 Pandemic Clinical Radiology Trainee Matters
Chief of Professional Practice Update
If you have thoughts or comments about one of the stories you have read in this issue, we want to hear from you. The submission of letters to the editor, articles and news items is encouraged. Please email any submissions to editor@ranzcr.edu.au
From the Faculty of Radiation Oncology
Chief Censor Update: Agility, Resilience and Lasting Change Radiation Oncology Trainee Matters
Supporting Quality Radiation Therapy in Regional Areas
Have you moved recently?
Log into the MyRANZCR portal and ensure your contact details are up to date at www.myranzcr.com
Editor’s Pick Editorial Staff Editor-In-Chief Dr Allan Wycherley Sub Editor Lindy Baker All rights reserved. No part of this publication may be reproduced or copied in any form or by any means without the written permission of the publisher. Publication of advertisements and articles submitted by external parties does not constitute any endorsement by The Royal Australian and New Zealand College of Radiologists of the products or views expressed. Inside News © 2020 The Royal Australian and New Zealand College of Radiologists® (RANZCR®) Inside News is printed on Sovereign Silk. Sovereign Silk is produced in an ISO 14001 accredited facility ensuring all processes involved in production are of the highest environmental standards. FSC mixed Sources Chain
Custody (CoC) certification ensures fibre is sourced from certified and well managed forests.
of
Quality
Audit
Prostate Cancer Outcomes Registry New Zealand Branch News Abdominal News: ARGANZ Radiology and the Confidence Question 47 41 43 45 48 49 55 57 30 15 12 50 26 28 33 35 38 39 25 23 53
Corner The Revised Peer Review
Tool (PRAT)
ESCAPE THE ordinary
WITH TRG IMAGING NEW ZEALAND
TRG Imaging is the second largest private radiology provider in NZ, delivering high quality patient care through a network of North Island clinics.


We offer: AUCKLAND NORTHLAND


• An opportunity to work with a progressive radiology provider;
• Work/life balance (evenings and weekends are yours);
• The choice of where you live... anything from city chic to rural tranquility;

• An MSK Fellowship programme;
• Access to develop your MRI sub-specialty skills on our fleet of modern high tech equipment;
• Further training opportunities and attendance at international conferences;
• Career progression;
• Shareholding opportunities;


• Locum opportunities so you can experience what it’s like here before you make the decision to move.




NZ owned
KEEN TO JOIN US?
We are seeking Radiologists with:
• the right capabilities;
• the right attitude; and
• the right workplace cultural fit.
You will join our unique team of professionals dedicated to exemplary patient care and positive working environments where everyone is valued and recognised for their contribution.
We measure our successes and learnings through IANZ accreditation and Net Promoter Score process.
We are well respected in the marketplace and are known for our brand and what it represents.
We place culture at the heart of our success and work continuously to build and maintain the right workforce.
Trusted – we have a direct relationship with seven different District Health Boards, plus are entrusted with contracts from all private medical insurers and Government healthcare agencies.
Sustainability is a responsibility TRG Imaging is passionate about.

Our Vision is to be the recognised leader in the delivery of medical imaging services through quality imaging, patient experience; referrer relationships; and engaged employees.

Email us careers@trgimaging.co.nz
www.trgimaging.co.nz
HAWKES BAY Rotorua/Taupo Gisborne
2020 has delivered a complex set of challenges to us all and an equally complex public health response is beginning to catalyse, with both strengths and weaknesses emerging. Our connected responses in New Zealand and Australia have been fundamentally robust however the intricacy of the challenges which remain before us requires thoughtful attention and careful navigation.
A considered return to normal service provision

The College strongly recommends a cautious, gradual and safety-first return to normal service provision. We have seen relative success in New Zealand and Australia in flattening the COVID-19 incidence curve, and this success only underscores the need for sensible, evidence-based decisions as the yardstick with which to proceed.
COVID-19 will continue to impact on delivery of health care in both countries for some time, likely until the availability of a vaccine. It is prudent as we continue to move from containment efforts to short-term recovery that plans to scaleup operations are carefully balanced.
Clinical radiology and radiation oncology departments and practices have responded to the pandemic with a range of necessary measures to prepare and reconfigure their operations. Care was prioritised according to clinical need, service availability and allocation of resources to protect patients and staff.
A Joint Message from the President and CEO
The way forward in New Zealand and Australia
New Zealand and Australia are currently well-placed, among comparable Western nations, to continue to deliver high quality health care to our populations due to our relative success to date in containing the spread of COVID-19. However, considerable uncertainties remain.
While our testing rates are among the highest in the world, the numbers of asymptomatic carriers are not known and may pose a risk to resumption of normal health care delivery. Now more than ever, we cannot afford to be complacent and risk losing the significant gains that have been made.
The College supports a carefully considered return to usual patterns of health care, which has begun in both countries with the resumption of elective surgeries. The College believes radiology and radiation oncology practices and departments should take a balanced approach to service delivery, taking into account the risks of a resurgence. Many of the safety changes introduced during the initial pandemic response will continue to be needed. We have an opportunity to embrace and build on innovations and pragmatic solutions so that we do not simply return to pre-pandemic business-as-usual.
Adaptive measures and 360 safety


Many factors ought to be considered when resuming services including: continuing to limit the risk of infection
by retaining infection control measures, including working from home and separation into teams; ensuring services are delivered according to clinical priority and in consultation with referrers; managing any risk of patients deteriorating while waiting for services; active monitoring of waiting lists and regular re-evaluation of patient needs; appropriate and ongoing communication with patients and referrers; and continuing appropriate use of personal protective equipment (PPE).
The College supports resumption of service delivery with the positive adaptations that have been made to limit patient contact, maximise the use of multi-disciplinary teams and provide alternate methods of accessing specialist advice and treatment, including the use of telehealth where appropriate.

Personal protective equipment
It is vital for clinical radiology and radiation oncology staff to have access to appropriate PPE in accordance with jurisdictional guidelines as well as comprehensive training in correct use of PPE. Lack of PPE increases the risk of transmission of COVID-19 to vital staff within radiology and radiation oncology practices and departments, potentially leading to self-quarantine, illness and temporary reduction in availability of services to communities.
Introduction Volume 16 No 3 I June 2020 5
Dr Lance Lawler
continued over...
Ms Natalia Vukolova
SUPPORT



*



Helping to meet the needs of patients with prostate cancer and healthcare professionals through initiatives such as patient support materials and supporting educational activities. Zoladex is indicated for:1 Palliative treatment of metastatic ( M+ ) or locally advanced prostate cancer where suitable for hormonal manipulation. Adjuvant and neoadjuvant therapy in combination with radiotherapy for the management of locally advanced prostate cancer in men suitable for hormonal manipulation.
Before prescribing please review full Product Information available on request from AstraZeneca on 1800 805 342 or at www.astrazeneca.com.au/PI
PBS Information: Zoladex 10.8mg. Restricted benefit for locally advanced ( equivalent to stage C ) or metastatic ( equivalent to stage D ) carcinoma of the prostate.






































Zoladex® 10.8 mg Implant ( goserelin acetate ) Minimum Product Information. Indications: Metastatic ( M+ ) or locally advanced prostate cancer; adjuvant and neoadjuvant therapy in combination with radiotherapy for locally advanced prostate cancer. Contraindications: Hypersensitivity to LHRH, LHRH agonist analogues or any components of ZOLADEX. Precautions: Not indicated for use in females or in children; patients with metastatic cancer at risk of developing ureteric obstruction or spinal cord compression - use of ZOLADEX should be carefully considered and monitored closely in the first month; injection site injury, including pain, haematoma, haemorrhage and vascular injury, care with patients of low BMI and/or receiving full anticoagulation medications; bone pain; serum testosterone concentrations may rise if implant is omitted or delayed; loss of bone mineral density; hyperglycaemia and increased risk of developing diabetes – periodically monitor blood glucose and/or glycosylated haemoglobin ( HbA1c ). Androgen deprivation therapy may result in prolongation of QT/QTc interval-consider benefits versus risks in patients with congenital long QT syndrome, congestive heart failure, frequent electrolyte abnormalities or taking drugs known to prolong the QT interval. Correct electrolyte abnormalities. Monitor for symptoms and signs of development of cardiovascular disease and manage appropriately. Effects on fertility – see full PI. Adverse reactions: Very common ( ≥10% ): decreased libido, hot flush, abnormal blood pressure, hyperhidrosis, erectile dysfunction, gynaecomastia, breast tenderness, paraesthesia, decreased bone mineral density; Common ( ≥1% to <10% ): impaired glucose tolerance, spinal cord compression, incontinence/urinary frequency ( post-radiotherapy ), rash, bone pain, arthralgia, injection site reaction, cardiac failure, myocardial infarction, increased weight, mood swings; For less common adverse reactions, see full PI. Dosage: One implant ( 10.8 mg ) injected subcutaneously into anterior abdominal wall every 3 months. Caution should be taken while inserting ZOLADEX into the anterior abdominal wall due to the proximity of underlying inferior epigastric artery and its branches. Use extra care when administering ZOLADEX to patients with a low BMI and/or who are receiving full anticoagulation medication. Date of first inclusion in the ARTG: 22 May 1996. Date of most recent amendment: 16 May 2017.
1. Zoladex 10.8 mg Approved Product Information. Zoladex® is a registered trademark of the AstraZeneca group of companies. Registered user AstraZeneca Pty. Ltd. ABN 54 009 682 311. 66 Talavera Road, Macquarie Park, NSW 2113. www.astrazeneca.com.au. For Medical Information enquiries: 1800 805 342 or medinfo.australia@astrazeneca.com. To report an adverse event: 1800 805 342 or via https://aereporting.astrazeneca.com. AU-5913, WL302306, April 2019
References:
THAT’S AS INDIVIDUAL AS THEY ARE *
A Joint Message from the President and CEO cont.
Disruption to trainees’ schedule
We recognise that the disruption to the trainees’ examination schedule has created uncertainty and concern. We are considering all potential risks and looking for the best possible solutions. The College Board released guiding principles regarding to faceto-face meetings for College activities during the pandemic, explicitly stating that we understand that different jurisdictions will have different requirements and restrictions, and that these may diverge further over time. This means that the Australian and New Zealand situations are de-coupled in the College’s eyes, unless the particular activity is bi-national and examinations are a bi-national activity.
We are making every effort to deliver examinations before the end of 2020 and reaffirm our commitment to give candidates at least three months' notice of any new dates. No examination dates are confirmed at the time of writing. Timelines to release examination results may also change to ensure that appropriate marking and reviewing processes take place. Comprehensive detail for trainees is provided in this edition.
If you believe that you may be significantly impacted by the deferment of examinations, the altered format of the examinations, or would like to defer sitting the examinations, you are advised to submit an application for Consideration of Special Circumstances, allowing the College to account for your unique circumstances. If you are unsure how the changes relate to your circumstances, you are advised to contact the College on radtaa@ranzcr.edu.au
The healthcare ecosystem
Diagnostic and interventional radiology are essential for delivery of health care. The College’s role is to ensure that patients all have timely and appropriate access to clinical radiology services. The viability of individual businesses is neither the concern nor mandate for the College. However, the sustainability of private radiology practices and overall access to public clinical radiology services are inextricably linked.
In these unique times the biggest threat to ongoing patient access is availability
of radiology services. The COVID-19 pandemic rapidly and severely affected private and community-based services, many diagnostic and interventional practices face formidable challenges.
It is crucial these services are resourced, supported and fully utilised to maintain service provision in the short term and to ensure the radiology sector continues to provide these essential services now, and in the years ahead. High equipment and facility costs make radiology practices highly vulnerable relative to other medical services. As restrictions are relaxed there will be a marked increase in demand to address delayed and deferred workload.
Following government directives for social distancing and the cancellation of elective surgery and non-essential medical services, patient referrals to clinical radiology services fell dramatically, as analysed further on pages 15 to 18.
Loss of continuity of care in hospitals
Hospital-based clinical radiology practices care for COVID-19 and non-COVID patients, including those suffering acute emergency conditions and all non-elective presentations to hospital. Without radiology services the provision of care in our hospitals is impossible—radiology is integral to clinical management in 2020. If hospitalbased radiology practices close it will leave many metropolitan acute hospitals and most regional communities without radiological services, endangering the lives of seriously ill patients.
Deferrals and backlogs in community-based practices
Our populations are being encouraged to consult with their doctors, and the College applauds government initiatives in this regard. However, encouragement alone will not be enough.
Patients who defer a visit to the GP or specialist and any subsequent referral for diagnostic imaging may delay critical diagnosis and the start of treatment by months. In this eventuality, patient outcomes are often compromised. Imaging is a key determinant of the urgency of a patient’s care.
As social distancing measures are lifted, the healthcare system will face a huge
backlog of patients requiring medical treatment. Community-based clinical radiology practices will need to be open to provide the imaging patients require, to clear the backlog and ensure the excellent long-term health outcomes we achieve in both jurisdictions are maintained.
Where community-based private practices fail to survive the downturn, despite the support already announced by federal, state and territory governments, numerous communities will be left without access to adequate clinical radiology services.
Call for urgent action
The viability of private radiology practices in hospitals and the community during the pandemic must be actively monitored and interpreted. The College is reviewing Medicare data monthly to analyse the impact on our sector and any implications for patient care. Federal and state governments must be ready to step in to provide additional support if private radiology practices become insolvent to ensure access to clinical radiology services during and after the pandemic.
The College has engaged with the Australian and New Zealand Governments to discuss the risks to patient access to clinical radiology services due to the pandemic, as well as the potential solutions to the many and complex issues affecting current service provision.
A confronting year
The complexity can feel like a marathon and we encourage all members to take the time to reflect, and revitalise, as we find our pace in the ‘new normal’ between the first (largely contained) wave and managing the possibility of a second wave of infection.
As we move forward, we need to understand the changes we keep, and those we move on from. Our basic goal remains the same: optimal patient care. Delivering that care has got a whole lot harder in 2020, there is no doubt, however the pandemic has made salient the value of working and thinking together to come up with crisis-driven solutions and adaptations. We will continue to do just that in the second half of this difficult year.
Introduction Volume 16 No 3 I June 2020 7
Maintaining Your Wellbeing in Public Health Crises An Examination of the Demands on the Professions
With each passing day, as the pandemic progresses beyond the acute phase of a major public health emergency to the persistent symptoms of an uncertain aftermath, the focus of medical attention shifts gradually from the physical to the mental.
Many health workers spearheading the community pandemic response—such as doctors and nurses who have borne the risks of treating infected patients in less-than-ideal circumstances, as well as disruption to their workloads, practices and home lives—have now entered an indefinite, uneasy period of recovery and reflection, combined with a raised level of alertness in anticipation of a resurgence in activity. Some are exhausted by the experience, most feel stressed, and it seems a few may be feeling much worse than that.
The impact of the coronavirus pandemic on the mental health of medical and allied health professionals has attracted
anecdotal attention in the mainstream media and serious research in medical and scientific circles.
Doctors participating in Facebook and radio discussions have spoken of their and colleagues' fears and emotional responses to the pandemic. In an ABC Radio National program aired in April, a group of GPs, specialists and nurses noted a sudden rise in burnout, heightened anxiety, inability to relax or sleep, excessive drinking and depression among medical practitioners dealing with the pandemic.1
Among them, Dr Caroline West, an East Sydney GP and health broadcaster, said that doctors who felt energised in the short term as they coped with the crisis, would have difficulty in sustaining this level of intensity, and she warned it would be unwise to do so. 'When you remove all the things in your life which have kept a sense of balance, including decent sleep, nutritious meals on time,
connecting with friends, and exercise, it's easy to become quite emotionally depleted.' Without 'recharge time', healthcare workers would eventually struggle to concentrate and bring their best to the job each day, she said.

Dr Emma Adams, a Canberra psychiatrist, felt that, while a few doctors had spoken to her of resigning their jobs or even experiencing suicidal thoughts, their tendency was to keep going.
'Doctors aren't going to collapse and put patient care at risk—they are more likely to put their own health at risk,' she told the ABC. 'There are a lot of barriers for doctors seeking help, and one is being seen as not coping. They are worried about being reported to the medical boards and the Australian Health Practitioner Regulation Agency if they admit they have depression or anxiety,' she said.
Features 8 Inside News
Adams's observations are supported by the findings of Beyond Blue’s national mental health survey of doctors and medical students in 2013. This study found that 40 per cent of Australian doctors felt that medical professionals with a mental health history were perceived as less competent than their peers. The survey also revealed that,

consequences were 'likely to be present for longer and peak later than the actual epidemic,' and that suicide prevention needed 'urgent consideration.'3
In these warnings, researchers have drawn on a body of compelling evidence gathered in the aftermath of the SARS and MERS epidemics in 2003 and 2015. For example, a study of 550 doctors, nurses and other hospital staff at a Beijing hospital in 2006 found that 10 per cent of respondents had experienced symptoms of posttraumatic stress (PTS) at 'high levels' since the SARS epidemic in 2003. Those who had been quarantined, had worked in SARS wards, or had relatives or friends with the disease were two to three times more likely to have PTS symptoms than those who did not have these experiences.4 Similar findings were obtained in Taiwan, Hong Kong and Singapore. At three hospitals in Hong Kong, over two-thirds of health workers reported high stress levels within months of the outbreak, and over half reported feeling 'psychological distress.'5
In Taiwan during the SARS epidemic, five per cent of staff in a teaching hospital suffered an 'acute stress disorder,' with experience of quarantine the most strongly correlated factor. The study also found that 20 per cent of staff felt stigmatised in their neighbourhoods for their hospital work, and nine per cent had considered resigning or had experienced a reluctance to go to work.6
With the MERS outbreak in 2015, a study of 1,800 hospital practitioners in South Korea found that those who undertook MERS-related tasks recorded the highest risk of PTS symptoms among staff in the aftermath of the outbreak, and this risk was even higher if they had been quarantined.7
What is most evident from these and similar studies is that pandemic and epidemic events have significant mental health implications, and in this, our healthcare workers, including doctors and nurses, are vulnerable.
continued over...
while rates of 'very high psychological distress' among doctors were similar to those in the general population (but higher than other professionals), doctors were less likely to seek treatment because of a preference to self-rely or due to embarrassment and/or concerns over loss of privacy, impact on the right to practise and career prospects.2
In the medical literature, academics and clinicians at home and overseas began to warn as early as February of the mental health risks that COVID-19 poses for health professionals. A research team at the University of Bristol described the mental health impact of the pandemic as potentially 'profound,' especially among healthcare workers operating at the leading edge of a response. The UK team argued that mental health
Features Volume 16 No 3 I June 2020 9
Image courtesy of the Pandemic Kindness Movement
“When you remove all the things in your life which have kept a sense of balance, including decent sleep, nutritious meals on time, connecting with friends, and exercise, it's easy to become quite emotionally depleted.”
In late March, the Australian government launched a national health plan and a website (www.headtohealth.gov.au) to address concerns about the mental health and wellbeing of Australians during the pandemic. At the end of April, the Pandemic Kindness Movement was created by clinicians across Australia to support and enhance the health and wellbeing of all health workers during the pandemic. The Pandemic Kindness Movement website by the NSW Agency for Clinical Innovation (ACI), directs users to helpful resources that are respected and evidence-informed, curated by teams of clinicians and wellbeing experts. Adapting Maslow’s hierarchy of needs to reflect potential challenges on the health workforce, resources are organised under six key areas; leadership actions and behaviours, contribution, esteem, love and belonging, safety and basic needs. The multi-state initiative is supported by the ACI, the Commission on Excellence and Innovation in Health South Australia, Safer Care Victoria, and Queensland Government.

What is needed in addition to these sites and other general mental health resources such as Beyond Blue is first an acceptance in our ranks that medical staff and other health workers bear
the brunt of the response to the virus. Further, we need to accept that this burden—which may result in overwork, disrupted routines, fear of contagion for themselves and their families—is likely to increase the risk of psychological stress, burnout, anxiety, depression and suicidal ideation.
The Royal Australian and New Zealand College of Psychiatrists which attract CPD points.
Given that doctors have a tendency to prefer self-help over asking others for assistance, it is worth considering what they might do for themselves to release psychological stress caused by work and improve their mental health. In a year-long study of work engagement and wellbeing in Germany and Switzerland in 2010, researchers found that psychological detachment, informally known as 'switching-off,' outside of work buffered social workers and allied healthcare employees against emotional exhaustion and burnout. The study concluded that 'job demands . . . are less harmful when employees mentally disengage from their job during off-job time.'8
The College also recognises these needs and the role we have in protecting the mental health of our members and recognising the promotion of mental health as an important aspect of our mission. A College webpage on your wellbeing offers resources for Fellows, Educational Affiliates and trainees, including online self-care learning modules developed by
Of course, switching-off and sharply demarcating work life from home life has added difficulty during a public health crisis, as many workers have opted to work remotely, usually from home, to help minimise the spread of the virus. How is one to psychologically detach from work in the evening when the day's efforts surround you and the phone continues to buzz with emails and texts?
Features 10 Inside News
“Job demands . . . are less harmful when employees mentally disengage from their job during off-job time.”
The Pandemic Kindness Movement website: a clinician-led initiative for health workers
In examining the factors which helped cancer workers avoid burnout and recover from work stress, a Queensland team emphasised the value of psychological detachment outside of work and the risk factors which degrade mental health.9 These included hours worked each week, age (35 to 45 being the worst decade), children, marital status and frequency of strenuous exercise. Of these factors, only one is readily modifiable—that of exercise. The researchers noted a strong positive influence on psychological detachment and its benefits among those who exercise four or more times a week, and
even a statistically significant effect for those who exercise once a week.
The evidence clearly indicates that, in addition to seeking help from others, when your stress levels get too high, members can use exercise to improve not just your physical health but also boost your own ability to safeguard your mental health.
Scaffolding our wellbeing with mindfulness, meditation and good sleep hygiene also boosts our physical and mental staying power. All of these can sound like small measures in the face of a large challenge. They can also prove
surprisingly difficult to actually maintain, even if seemingly small. But the sum total of developing self-preservation habits of seeking help; accessing available resources; exercising regularly; practising mindfulness and meditation; and just simply getting enough sleep can make the crucial difference to our ability to pull through.
To access useful resources visit: www.ranzcr.com/fellows/general/ your-wellbeing
www.aci.health.nsw.gov.au/ covid-19/kindness
Reflecting Maslow’s hierarchy of needs, resources are organised under six key areas

Reference
1 ABC Radio National, "Mental health on the Covid frontline," All in the Mind, [radio program] 19 April 2020, https://www.abc.net.au/radionational/programs/ allinthemind/covid-frontline/12147598
2 Fei Wu, Michael Ireland, Katherine Hafekost, and David Lawrence, The National Mental Health Survey of Doctors and Medical Students [report] (Melbourne: beyondblue, Oct. 2013), https://tinyurl.com/ra85vxd
3 Yu-Tao Xiang et al., "Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed," The Lancet, vol. 7, March 2020, 228–229; David Gunnell et al., "Suicide risk and prevention during the COVID-19 pandemic," The Lancet, [online] 21 April 2020, https://doi.org/10.1016/S2215-0366(20)30171-1
4 Ping Wu et al., "The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk," The Canadian Journal of Psychiatry, vol. 54, no. 5, May 2009, 302–311.
5 Cindy W. C. Tam et al. " Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers," Psychological Medicine, vol. 34, 2004, 1197–1204.
6 YaMei Bai et al., "Survey of stress reactions among health care workers involved with the SARS outbreak," Psychiatric Services, vol. 55, no. 9, September 2004, 1055–1057.
7 Sang Min Lee et al., "Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients," Comprehensive Psychiatry, vol. 87, 2018, 123–127.
8 Sabine Sonnentag and Carmen Binnewies, "Staying well and engaged when demands are high: The role of psychological detachment," Journal of Applied Psychology, vol. 95, no. 5, 2010, 965–976.
9 Michael G. Poulsen et al., "Recovery experience and burnout in cancer workers in Queensland," European Journal of Oncology Nursing," vol. 19, 2015, 23–28. The study's authors contributed a feature article to Inside News in September 2018.
Features Volume 16 No 3 I June 2020 11
Trainees Rise to the Challenge
The
New Zealand Interisland Coronoschool
2020 has been an unprecedented and challenging year so far with catastrophic Australian bushfires and the COVID-19 pandemic. The difficult decision to cancel Series 1 examinations has been devastating to many of us, especially the exam candidates who were ripe and at their peak. However, that devastation did not last long as we rise to stand shoulder to shoulder with our frontline colleagues in the war against COVID-19.
It is overwhelming to many and there has been discussion that trainee teaching may be taking a backseat for a while. With anxiety and uncertainty surrounding this pandemic, which is accompanied by many deaths across the globe, it is easy to overlook the

little positive things that came out of COVID-19. As the quote goes, the phoenix rises from the ashes, the New Zealand Interisland Coronoschool was born on the eve of New Zealand Alert Level 4 lockdown through collaboration between Dunedin and Wellington trainees.
It is an initiative to bring trainees and consultants together through the implementation of virtual teaching sessions across both islands as well as across the public and private sectors in Dunedin and lower North Island cities of Wellington and Palmerston North. These sessions have run over five weeks, the total number of weeks when the whole of New Zealand was
in Alert Level 4 lockdown. The result has been amazing and beyond our expectation. We are overwhelmed by the response from multiple consultants who donated their time and effort to make the virtual teaching sessions successful and enjoyable.
We applaud the trainees for not giving up under the pressure of COVID-19 and the consultants for their never-ending commitment to our training.
We would like to acknowledge the contribution of the consultants who have supported this initiative to provide the education:
Features 12 Inside News
Online with radiology and childcare: the new normal
Prof Terry Doyle, Dunedin
Dr Amy Fong, Dunedin
Dr Michael Reddy, Dunedin
Dr Sue Craw, Dunedin
Dr Jacquie Copland, Dunedin
Dr Sally Charters, Pacific Radiology, Dunedin
Dr Greg Harkness, Dunedin
Dr Ben Wilson, Dunedin
Dr Rodney Wu, Pacific Radiology, Wellington
Dr Mulvey Kelly, Pacific Radiology, Wellington
Dr Jonathan Graham, Graham Radiology Ltd, Palmerston North
Mrs Katherine Graham, Graham Radiology Ltd, Palmerston North
Dr Pierre Struwig, Wellington
Dr Hannah Kim, Wellington
Dr David Healey, Wellington
Dr Matthew MacKay, Wellington
Dr Sook Yee Yong, Hutt
Many more consultants have expressed their interest in contributing to the ongoing NZ Interisland Coronoschool sessions.
This is the new normal where supporting peers and providing teaching goes beyond geographical constraints.
We do believe that the COVID-19 pandemic brings out the best in humanity.
Kia kaha and stay safe.
Missa Amin and Malcolm Gill
Wellington and Dunedin

4th Year Trainees
Interisland Coronoschool Coordinators
Please
Features Volume 16 No 3 I June 2020 13
The New Zealand Interisland Coronoschool links the two islands of NZ
feel free to email missa.amin@gmail.com or malcolmmrgill@gmail.com with your thoughts, questions or feedback.


ELYSIUM: DIAGNOSTICS AND THERAPEUTICS (NOW AND THE FUTURE) WITH AI ranzcr2021 .com Official Presenting Partner of RANZCR2021
The COVID-19 Impact on Services and Practices in Clinical Radiology and Radiation Oncology
The take-up of telehealth consultations and a corresponding downturn in test referrals raised concerns that patients were putting off seeing their doctor or not having diagnostic tests due to fears of contracting COVID-19.
Radiation oncologists have also become concerned that cancer patients are either not attending their required consultations or discontinuing their treatment after making incorrect assumptions about the safety, availability or capacity of clinical services.
Concerns about the spread of COVID-19 in Australia escalated rapidly from mid-March following the establishment of the National Cabinet on 13 March and the introduction of a raft of preventative and containment measures across the country.
Social distancing directives, the cancellation of elective surgery and non-essential medical services, the expansion of telehealth consultations for GPs and arrangements with private hospitals to ensure capacity to respond to the possible surge in infected patients were evidence of the calm before the expected storm.
In New Zealand, a four-level alert level system was introduced on 21 March to manage the outbreak within the country. The alert level, initially set at level two, was quickly raised to level four, putting the

country into a nationwide lockdown for at least four weeks from 11:59 pm on 25 March. All imaging services deemed non-urgent were deferred.
Severe disruption to clinical radiology and radiation oncology services
Clinical radiologists have reported significant drops in patient presentations in Australia and New Zealand. In Australia, while GP consultations remained steady throughout March, the proportion of teleconsultations increased dramatically.
Telehealth consultations were introduced in mid-March initially for patients or GPs required to selfisolate or for patients considered vulnerable and were expanded in stages to all patients from the end of March.
Statements from the government and the Australian Medical Association (AMA) in April urging people to continue to see their GP or specialist for chronic conditions, including cancer, are reported to have resulted in an upturn in the volume of radiology referrals.
The Medicare services data showed a downturn of 14 per cent in radiology service volumes in March 2020 over the same period of the previous year after adjustment for working days.
The decline in services suggests a downturn of some 30 per cent in volume in the second half of March when social distancing and other preventive measures were introduced. The downturn of 30 per cent decline has continued throughout April 2020. In May 2020, service volumes have shown signs of improvement compared to a corresponding decline in the previous month.
continued over...
Features Volume 16 No 3 I June 2020 15
DEVELOP YOUR PROFESSION WITH THE QSCAN GROUP
The Qscan Group’s growing national network offers Dual-trained Radiologists and Nuclear Physicians the opportunity for career development and earning potential. By partnering with our doctors, we encourage individual professional aspirations and provide market competitive, flexible avenues to join our team.
Why join the Qscan Group?
• Career opportunity customised in line with your skillsets and ambitions;
• The ability to be part of a supportive and strong collegiate doctor network;
• The very latest in cutting-edge technology;
• Assured access to a broad clinical case mix including tele-reporting which can provide flexibility or additional hours to expand your earning potential.
We are currently recruiting for our NEW up and coming PET-CT clinics in WA, SA, NSW & ACT.

Significant referral bonuses availableenquire today.
Fellowships are currently available
Qscan offers advanced training in Nuclear Medicine through the Royal Australasian College of Physicians. We support 2 (two) accredited sites for Advanced Training in Nuclear Medicine/PET in our Southport and Redcliffe clinics. Qscan is at the forefront of growth in this specialist area and we actively partner with doctors to develop their specialist careers within our industryleading facilities.
Your employment offer with Qscan can include:
• Above market-rate remuneration package;
• Significant sign-on bonus;
• Equity opportunities;
• Relocation assistance.
For more information or a confidential discussion please call our Qscan General Manager, Matthew Bellairs on 0412 939 200 or email matthew.bellairs@qscan.com.au
Trusted Analysis | Excellence | Compassionate Care qscan.com.au
Radiation oncology services have been slightly lower than expected, especially treatment services which were down 0.4 per cent, but overall up by one per cent in March 2020 over March 2019 (working day adjusted). Major treatment services which account for 98 per cent of the total radiation oncology services, have shown signs of improvement, up by around 10 per cent in early May 2020 over the same period in the previous year.
Surviving the crisis
The ability of private radiology practices to survive the COVID-19 pandemic downturn in the long term is unclear. Regulatory frameworks, together with high equipment and facility costs and a specialised workforce, place it at higher risk than other areas of health care. Any loss of community-based practices is likely to disrupt and diminish the quality and availability of health care: this would be magnified in rural and remote areas where there may be only one practice.
In Australia, as with all businesses affected by the pandemic, radiology practices have access to a range of financial support packages provided by the Federal and State/Territory Governments and other relevant entities, and it is assumed they have also been making commercial decisions based on their individual circumstances.
The AMA has put together a comprehensive summary of some of the financial support packages available. This list also includes a link
to a quick reference of Government business assistance measures provided by RSM Australia that has a summary of the key measures in one place, with detail of eligibility criteria, how each stimulus package works, and action needed to be taken to access these packages.
Most clinical radiology and radiation oncology services have remained open, although some have reduced operating hours, required staff to take leave, etc.
These additional necessary precautions have added to the service delivery costs due to greater use of more expensive PPE, increased time to prepare for scans and time required to clean and disinfect equipment.
Preparing for the ‘new normal’
It is expected that service volumes will gradually improve now that social distancing and lockdown restrictions are being eased, providing greater reassurance to patients about the risks to their health from the virus. However, more COVID-19 cases are expected, and it is likely there will be continued uncertainty for many months to come. It is impossible at this time to predict how long it will take before some semblance of ‘normality’ returns to imaging practices. The longer it takes, the larger the backlog of imaging studies. In New Zealand, the deferral of non-urgent imaging services has added to the extensive pre-pandemic waiting lists for radiology services.
Clinics have had to employ stricter infection control measures and patient management protocols, including social distancing, to ensure the safety of patients and staff and to minimise the risk of transmission of the COVID-19 virus.
There is no one single prescriptive strategy for managing both the return to normal activity and the expected backlogs. Imaging providers will need to weigh the costs and benefits of resuming full services in the new ‘normal’ and there will be different considerations in different locations.
For more information visit: www.ama.com.au/financialimplications www.rsm.global/australia/ coronavirus-resources#business
Features Volume 16 No 3 I June 2020 17
“There is no one single prescriptive strategy for managing both the return to normal activity and the expected backlogs. Imaging providers will need to weigh the costs and benefits of resuming full services in the new ‘normal’ and there will be different considerations in different locations.”
continued over...
Some of the more stringent COVID-19 related measures will need to stay in place for some time with practices expected to continue to be financially impacted as a result. Some practices may not have the capacity to return to full operation for many months and managing this will require a balance of clinical assessment, ethical judgement and logistical planning.
Impact on radiology services
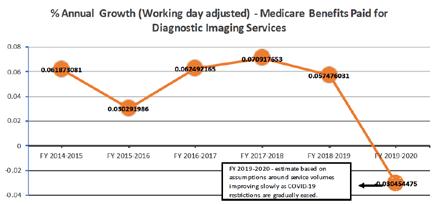
The accompanying charts show the estimated impact of the COVID-19 crisis on trends in radiology services and outlays in Australia. Comparable data for New Zealand are not available.
The 2019/2020 financial year impact on radiology service volume is estimated to be a decline of six per cent with a corresponding decline in Medicare outlays of three per cent. When expected growth in 2019/2020 is factored into these trends, it is estimated there will be some 2.5 million fewer imaging services than were anticipated in 2019/2020 and an estimated corresponding decline of some $350 million in Medicare outlays for imaging services.

Features 18 Inside News
“Some practices may not have the capacity to return to full operation for many months and managing this will require a balance of clinical assessment, ethical judgement and logistical planning.”
Training and Assessment Reform (TAR) – What’s the Plan?
The one question our trainees keep asking is “will the enhanced training programs still be introduced in December 2020/February 2021?”
While we are keen to introduce the enhanced training programs as planned, it has been agreed that the roll-out should be postponed until 2022. We know this may be disappointing to some members, but this is a difficult decision made in an effort to minimise stress and concern among our trainees over the coming months. Many trainees have expressed frustration over the uncertainty they have endured since the beginning of the COVID-19 crisis, and we comprehend the need to dispel this sense of uncertainty as far as is practicable.
The existing training programs will continue throughout 2021, notwithstanding the temporary arrangements related to the pandemic and its aftermath. Trainees are required to complete all the assessments and training requirements under the current training programs. All clinical radiology trainees must complete both Project 1 and Project 2.
The new format of examinations will be introduced in 2022 and beyond. The timeline for each examination is being reviewed to ensure they are introduced at the right time in the right way, so the benefit to trainees is maximised.
Lots of work has been put into the development of the enhanced training programs in the last few years by many clinicians from both
Faculties, particularly those sitting on the Steering Committees and Implementation Working Groups. We are confident that the enhanced programs, which are more up to date and aligned with current and contemporary practice, will continue to produce highly-skilled practitioners that provide optimal patient care in the fields of clinical radiology and radiation oncology.
Since late last year, the TAR project has moved to the implementation phase, with many educational educational and training activities being planned and undertaken. Earlier this year, key clinicians and College staff started visiting training networks and sites to provide trainees, clinical supervisors and Directors of Training with details of all the changes. The roadshows run in Auckland and NSW in February were well received with lots of positive feedback and useful suggestions gathered from both trainees and trainers.
However, with the declaration of a pandemic and escalation of COVID-19 cases in Australia and New Zealand, our TAR engagement and communication plan has been disrupted, just like many aspects of clinical practice and training. Other implementation activities have also understandably been slowed down or postponed due to travel restrictions, social distancing measures, limited clinician engagement due to increased clinical workload and competing priorities, as well as lack of stakeholder engagement in a broader sense.
The Implementation Working Groups and project team are in the process of reviewing the implementation timeline, taking into consideration all of the dependencies of the program implementation, that is, IT infrastructure development, stakeholder engagement and so on. The detailed plan will be communicated to our members once it becomes available.
In the meantime, the implementation activities are continuing to progress to ensure we are well prepared when the enhanced training programs are introduced in December 2021 for New Zealand trainees, and in February 2022 for Australian and Singaporean trainees.
Stakeholder consultation
A wide stakeholder consultation for the enhanced training programs and learning outcomes was scheduled for March/April 2020 but is currently on hold amid the pandemic. During the last two months, both Implementation Working Groups continued to review and fine tune the enhanced training programs remotely. We now expect the stakeholder consultation to take place in June/July this year to ensure our members and external stakeholders have the opportunity to provide feedback and suggestions for improvement to the enhanced training programs.
Education Volume 16 No 3 I June 2020 19
continued
over...
Pioneering Radiation Oncology


Bringing Viewray MRI dian to Australia & New Zealand.


Device Technologies has proudly supported the Healthcare Industry for over 25 years with over 850 employees, 60 factory trained technicians, offices in every state of Australia + New Zealand.
33 global installations
35 mri dian systems deployed
10,000 adaptive treatments 1
Reduction in
~50% PTV volume by MRI based Targeting 2
~6,500 patients treated 1
~50 disease sites treated on mri dian system 1
18m patients diagnosed with cancer globally 3
~130,000 hours mri dian touching a patient 1
from 10.8 months
20.8
Improving Overall Survival pancreatic cancer patients 4


1. ViewRay internal data on file (as of 1 May 2019)
2. Zoberi et al. First Ever Magnetic Resonance Image Guided Radiation Therapy for Accelerated Partial Breast Irradiation: Early Results of a Single Institution’s Prospective Experience. ASTRO 2016 (Wash U) Results from this case study are not predictive of future results.
3. International Agency for Research on Cancer. World Health Organization (2018). GLOBOCAN (2018), http://gco.iarc.fr
4. Rudrah et al. Using adaptive magnetic resonance image-guided radiotherapy for treatment of inoperable pancreatic cancer. Cancer Medicine, 2019; 1-10.

For further information please contact:
Glenn Whittaker
Senior Business Manager
E: gwhittaker@device.com.au
M: +61 411 896 970
Merna Moushi Business Development Manager
E: moushi@device.com.au
M: +61 437 899 407
Development of IT infrastructure
A new fit-for-purpose Training ePortfolio System is currently being developed to replace the current Trainee Information Management System (TIMS) in late 2021. The new system will provide better support in managing the enhanced training programs, to measure identified outcomes and allow tracking of trainee progression.
The College is planning to undertake extensive testing and piloting before the system goes live, which will be followed by training for trainees and trainers on how to use the new system before it is launched.
Communication and training
Most likely the face-to-face roadshows will be limited during and after the pandemic, but we will continue with communication and training activities, using a viable and effective alternative plan. The plan is to develop online resources such as video lectures, instructional videos, educational videos and FAQs and make them available on the College TAR webpage during the course of the implementation of the enhanced training programs.
The aim of these online resources is to inform members of the key changes and allow the provision of feedback to ensure that all members are kept up-to-date with regards to the enhanced training programs. The timeline for the development and release of these resources
will be communicated separately once the COVID-19 impact on the health system becomes clearer. In the meantime, communication regarding any significant development in this area will be provided through the College website.
Trainee transition
As communicated previously, the College has decided that all current trainees will transition to the enhanced programs when they are implemented. This will allow all trainees to benefit from the new programs and avoid the need to operate two IT systems at the same time and reduce potential confusion. The transition plan is continuing to be developed, endeavouring to minimise disadvantaging trainees, and to allow some flexibility during the transition. Disruption of trainees’ progression caused by COVID-19 will also be factored into the transition plan.
All trainees are asked to complete the training requirements under the current training programs, and are encouraged to keep their relevant information and records up-to-date in TIMS, including details of training status, rotation, experiential training requirements, logbooks and workbased assessments. This will ensure that the data being transferred to the Training e-Portfolio system are as accurate as possible.
The College will make sure all trainees are well-informed of the transition plan and properly supported throughout the transition process.
We would like to thank all members who have contributed their time and expertise to this important project.
It is important that you read the information and keep abreast of changes shared with you through College communication channels, including the College website, enewsletters, printed newsletters and direct correspondence.
If you would like more information or have any questions regarding the project, please visit the TAR webpage www.ranzcr.edu.au/tar or contact Faeha Tashkeel, Project Officer, Training and Assessment Reform on:
faeha.tashkeel@ranzcr.edu.au
Education Volume 16 No 3 I June 2020 21
As you may know, the Medical Board of Australia (MBA) are changing their registration requirements for doctors. While exact details of the implementation are yet to be announced, the College is mindful that 2022 is not as far away as it seems, and we are actively preparing to assist members transition to the new requirements which include the need to review performance and measure outcomes.

How the College is working with the MBA
In February 2020, the College responded to a second, public consultation released by the Medical Board of Australia.
Members of the Faculty of Clinical Radiology Professional Practice Committee and the Faculty of Radiation Oncology Post Fellowship Education Committee provided content for the College response. The response requested clarification in relation to the requirements for measuring outcomes and reviewing performance, as the College has members practising in rural and regional communities or in isolated practice and those working in non-clinical roles, who may be unsure of how they will be able to meet these new requirements.
The College is optimistic the concerns will be addressed by the MBA in any future iterations of the Registration Standard: Continuing Professional Development.
Types of CPD
Undertaking educational activities
• Lectures
• Conferences
• Courses
• Reading
• Supervision
• Workshops
• Grant rounds
• Online learning
Reviewing performance
• Peer review of performance
• Performance appraisal
• Peer review of medical records
• Peer discussion of cases, critical incidents, safety and quality reviews
• Multi-source feedback
• Peer review of journal articles
• Peer review of educational activities
The 2019–2021 CPD Handbooks for both clinical radiology and radiation oncology provide examples of how CPD points can be accrued under the new categories, the lists are not extensive.
We encourage members to find out more by visiting: www.ranzcr.com
We will continue to provide up-to-date information as it comes to hand.
If you have any questions or concerns about the upcoming changes to your Australian medical registration requirements, please send them to cpd@ranzcr.edu.au
Measuring outcomes
• Clinical audit
• Review of medical records
• Mortality and morbidity reviews
• Review of clinical indicators/standards etc
• Comparison of comparative data sets
• Audit of medico-legal reports
• Reflection on professional outcomes
• Clinicopathological correlation meetings
Education 22 Inside News
Cardiac MRI Certification Update
The cardiac MRI initial certification pathway has recently been approved for implementation, following two years of discussions between the College and the Cardiac Society of Australia and New Zealand (CSANZ).
Representatives of the College and CSANZ met earlier this year to finalise the position statement for initial certification and maintenance of recognition in cardiac MRI.
The position statement is intended to support and foster the provision of quality, safe cardiac MRI services in Australia and New Zealand. It was commissioned after consultation between the CSANZ Imaging Council and the College with members appointed by both bodies.
The document was developed with consideration of international standards as well as the training and workforce requirements particular to Australia and New Zealand.
The position statement underwent external review by way of membership consultation with College members in 2018 and was approved by the Faculty Council of Radiology and the CSANZ Board in February 2020.
Cardiac MRI is an increasingly utilised technology, offering unparalleled image quality and diagnostic performance with the ability to obtain functional and multiparametric information.
The acquisition, analysis, and interpretation of cardiac MRI examinations require substantial training and expertise for both the medical imaging provider and for other staff within the cardiac MRI service (including radiographers / technologists, nursing staff, allied health and associated professionals).
The position statement outlines the training requirements for providing adult cardiac MRI services in Australia
and New Zealand, including initial certification as well as maintenance of recognition. Key components of both processes are: involvement in continuing medical education and maintenance of professional standards, with a strong emphasis placed on collaboration with specialists who use cardiac MRI for clinical decision-making; and engagement in cardiac MRI-specific education. The position statement pertains specifically to cardiac MRI in adults, as distinct from general vascular MRI or paediatric imaging.
Gaining accreditation in cardiac MRI
The Conjoint Committee for Certification in Cardiac MRI (Conjoint Committee) is comprised of members from both the College and CSANZ with an active interest in reporting cardiac MRI and has been assessing and credentialing existing providers. Established provider certification began in April 2018 and closed in December 2019.
The initial pathway and maintenance of recognition pathway is outlined in the position statement and the Conjoint Committee is now able to start taking applications.
The Conjoint Committee would like to invite those who report cardiac MRI to submit their applications. Application forms and the position statement can be found on the College website: www.ranzcr.com/fellows/clinicalradiology/quality-assurance-andaccreditation/certification-in-cardiac-mri
If you have any questions regarding the application process, please send them to cardiacmri@ranzcr.edu.au
In 2014, the European Association of Cardiovascular Imaging (EACVI) published the Core Syllabus in CMR, which is a jointly produced radiologycardiology position statement by leaders in the field developed for candidates seeking to sit the EuroCMR examination. This syllabus is a recommended structured learning framework for those training to perform cardiac MRI in Australia and New Zealand. The present document provides a rationale for single level training across both groups and incorporation into general radiology and cardiology training.
Volume 16 No 3 I June 2020 23
General Interest
“Cardiac MRI is an increasingly utilised technology, offering unparalleled image quality and diagnostic performance with the ability to obtain functional and multiparametric information. ”















The Faculty of Radiation Oncology
The Royal Australian and New Zealand College of Radiologists
RANZCR Workshops, Courses and Events 2020–2021
As you are aware, the COVID-19 pandemic has had a significant impact on public health, social wellbeing and the economy. There has been widespread cancellation of conferences and meetings in line with government guidelines. The College’s COVID-19 Taskforce and the Board of Directors have been monitoring the situation closely to foresee and mitigate any risks to members, staff and general community. Unfortunately, this has meant we have had to postpone some of our upcoming events. This has been done bearing in mind that social distancing restrictions may continue well into the end of this year with strict restrictions on international travel as well as mass gatherings.
Phase 2 Course
Radiation Oncology Phase 2 Exam Preparation Course. Postponed to 2021.
Phase 1 Course
Radiation Oncology Phase 1 Foundation and Exam Preparation Course. Postponed to 2021.
RANZCR/ACR Education Center Courses
Scheduled to be held in Melbourne from 7–16 August 2020. These courses have been postponed as we must support our faculty members who will be travelling from the United States.
The new dates for these courses are Friday 8 January–Sunday 17 January 2021 at the Pan Pacific, Melbourne.
Paediatrics: 8–10 January
Emergency Radiology: 8–10 January
HRCT: 11–13 January
MSK: 15–17 January
Registered delegates who cannot attend the new dates will be issued a full refund. Seats for the January 2021 dates have been reduced and are limited so reserve your seat today!
Register here!
www.bit.ly/ACREducation
NZ Branch Annual Scientific Meeting
Postponed to 6–8 August 2021, to be held at the InterContinental Hotel, Wellington.
RANZCR Annual Scientific Meeting (ASM) – New Dates

Announced
Scheduled to be held from 15–18 October 2020 at the Melbourne Convention and Exhibition Centre, the ASM has been postponed till 2021.
The Board and ASM Committee are excited to announce the new dates are Thursday 16 September–Sunday 19 September 2021. The theme of the meeting remains ‘Elysium: Diganostics and Therapeutics (Now and in the Future) with AI’.
We would also like to welcome our 2021 ASM presenting partner Intelerad. We thank you for your support and are looking forward to another successful meeting.
The ASM Committee will review all abstracts already submitted to the College, with a view to potentially use some for the 2021 ASM or for future events held by the College. Our Convenors and the ASM Committee are working through all available options and we will communicate them to you in the coming weeks.
RANZCR trainees who have submitted abstracts as part of their training program requirements and are immediately affected are asked to submit a Consideration of Special Circumstances request as outlined in the relevant policy:
www.ranzcr.com/college/documentlibrary/consideration-of-specialcircumstances-policy
ESTRO Basic Clinical Radiobiology Course
An introduction to radiation biology as applied to radiotherapy, focusing on technology, biology and molecular oncology. Postponed to 15–18 April 2021. Trainees who have already registered and cannot attend the new dates will be issued a full refund.
Register here!
www.bit.ly/ESTROBasic
If you have any questions relating to any College events, please don’t hesitate to contact the Conferences and Events team at events@ranzcr.edu.au
Education Volume 16 No 3 I June 2020 25
College Honours 2020
Every year the College invites nominations for a range of College Honours. These are awarded to members to acknowledge and publicly celebrate outstanding contributions to the College and, importantly, to the professions of clinical radiology and radiation oncology.

We encourage you to take time out to reflect on the achievements and efforts of your peers in day-to-day work and in the advancement of shared knowledge and expertise.
Nominations are open until 13 July 2020. In 2019, Dr Gerard Goh nominated A/Prof Dinesh Varma for the Roentgen Medal.
Question: What motivated you to nominate A/Prof Varma for the award?
Answer: A/Prof Varma has had a long history of service with the College having been President, Chief Censor and now Chief of Professional Practice, just to name a few of his contributions!

During his time as President he led the transition of the College governance structure to its current form. Few fellows have contributed to the College as much as Dinesh has and continues to.
I wanted to formally recognise Dinesh for his voluntary work towards the leadership of the College. Many people who volunteer for the College, in particular Dinesh, contribute so much of their own time on top of already busy clinical commitments to help better the College.
College President
Dr
Question: Why did you choose the Roentgen Medal in particular?
Answer: The Roentgen Medal was the most appropriate award to acknowledge Dinesh’s contributions. Dinesh has had a very long history of service with the College at multiple levels and he has helped institute many changes within the College. I couldn’t think of a more appropriate recipient for the medal.
Question: Do you think the Medal is a good way to recognise Fellows of the College who have made an unusually significant contribution to their field or the College?
Answer: Absolutely. This is a competitive award and is considered very carefully by the College. Having this awarded at the RANZCR ASM in front of the membership is a very special occasion.
Question: Was the process of submitting a nomination simple?
Answer: Yes. All the details about the award and regarding eligibility were available on the website, and the application process was straightforward. I decided I wanted to make it a semisurprise, so the hardest part was getting an up-to-date CV without giving away too much information!
Education 26 Inside News
Get Involved YOUR MEMBERSHIP MATTERS FELLOWS www.ranzcr.com/fellows/general/get-involved TRAINEES www.ranzcr.com/trainees/general/get-involved
Lance Lawler awards A/Prof Dinesh Varma with the 2019 Roentgen Medal
Dr Colette Kennedy nominated Dr Turi Mark Osborne for Life Membership in 2019.
Question: What motivated you to nominate Dr Osborne?
Answer: I nominated Dr Osborne for this award for several reasons. He had given considerable time and his expertise to assist the College over the years and he was the NZ chairman for a number of years. Dr Osborne was also a longstanding executive member of the College, was on the South Pacific liaison committee and a member of the New Zealand education trust.
In Auckland he is a highly regarded radiologist among his peers and has taught and mentored innumerable radiologists throughout his career.
To me personally he has been a fantastic colleague, a huge support, and always willing to share his knowledge and expertise. I had noticed that several of his senior colleagues had been given College awards and I felt that it was only fitting that Mark should also be recognised in this manner.
The College is currently inviting nominations for a variety of College Honours, including the Roentgen Medal and Life Membership:
Gold Medal
The Gold Medal is the highest accolade to be given by the College. It honours a Fellow who has rendered outstanding service or benefactions to the development, teaching or practice of clinical radiology or radiation oncology in Australia, New Zealand or Singapore. This most prestigious honour is only awarded on rare occasions for exceptional circumstances, and no more than one medal is awarded in a single year.
Roentgen Medal
The Roentgen Medal is awarded to Fellows who have made a very valuable contribution to the College over a significant period of time.
Life Membership
Life Membership is awarded to Fellows over the age of 65 who have made an unusually significant contribution to their field or the College.
College President
Question: Do you think Life Membership is a good way to recognise Fellows of the College who have made an unusually significant contribution to their field or the College?
Answer: I do think that Life Membership is a good way to recognise outstanding Fellows.
Honorary Fellowship
An Honorary Fellowship recognises individuals who have contributed to the advancement of clinical radiology or radiation oncology and allied sciences, either through original research or by special services to the College.

Denise Lonergan Educational Service Award
This award recognises members who have demonstrated outstanding longterm commitment, participation and leadership in training and education in radiation oncology.
Clinical Radiology Educational Service Award
This award recognises members who have demonstrated outstanding longterm commitment, participation and leadership in training and education in clinical radiology.
Question: Was the process of submitting a nomination simple?
Answer: Selecting colleagues to write submissions was no trouble. Overall the process was clear and easy.
Sally Crossing Award for Consumer Advocacy
The Sally Crossing Award for Consumer Advocacy acknowledges outstanding commitment of consumers involved in health care advocacy. The award honours the memory of the late Sally Crossing AM, in recognition of her exceptional contributions to advocating for cancer patients. The College recognises that due to the COVID-19 pandemic, submitting a nomination for a College Honour may not have been a top priority for our members. As a result, the deadline for 2020 nominations has been extended until 13 July.
For more information, or to nominate someone, visit www.ranzcr.com/college/grantsand-awards/college-honours or email gaps@ranzcr.edu.au
Education Volume 16 No 3 I June 2020 27
Dr Lance Lawler awards Dr Turi Mark Osborne with Life Membership in 2019
Reassuring Cancer Patients During COVID-19
Radiation therapy services are essential and have remained accessible throughout the pandemic. Radiation oncologists had been concerned that cancer patients may have been either not attending their required consultations or discontinuing their treatment after making incorrect assumptions about the safety, availability or capacity of clinical services.
In April, Targeting Cancer launched a media campaign to address these concerns, and more importantly to reassure patients that it was safe and essential for them to continue treatment. This followed statements from the Australian Government and the Australian Medical Association (AMA) that urged people to continue to see their GP or specialists for chronic conditions including cancer.
Dr Madhavi Chilkuri, Dean of the Faculty of Radiation Oncology said it was crucial for patients to be reassured about the availability of radiation oncology services.
“Radiation therapy services are essential and still accessible. Radiation oncology teams have made special provisions for patients to ensure any risks presented by COVID-19 are minimised. Every precaution has been taken to ensure infection control and the safety of patients and staff,” said Dr Chilkuri.
To support the campaign, Targeting Cancer also produced a range of resources including videos, FAQs and social media content.
The FAQs cover a range of topics including cancer screening, infection prevention measures, and telehealth. They also include a range of useful resources from governments and other agencies in Australia and New Zealand. Visit the Targeting Cancer website at www.targetingcancer.com.au to read the FAQs.
Thanks must go to all of you for the great effort put into ensuring treatment could continue for everyone who needs it, including practice preparations,
implementation of telehealth services, and adjustments to treatment plans.
Explaining the costs of radiation therapy in Australia
There are several cost factors that patients and their families need to think about when choosing the best treatment provider for them. These include direct costs which are those associated with treatment, and other indirect costs like travel, parking, accommodation and any allied health care that may be required.
a handy list of questions that patients can take with them to their radiation therapy centre to talk through these considerations.
Targeting Cancer has shared this important resource with a wide range of stakeholders including other medical colleges, consumer groups, and healthcare providers. Since February 2020, the document has been viewed more than 1,500 times. Feedback has been extremely positive, with many colleagues and stakeholders saying the document has provided an easy to understand overview of cost considerations for patients undergoing radiation therapy and their families.
We will continue to promote this important resource to patients and referrers through social media and by collaborating with external stakeholders. The factsheet can be downloaded from the Targeting Cancer website at www.targetingcancer.com.au/faqs/whatyou-need-to-know-about-the-costs-ofradiation-therapy-in-australia/
Help us share your patients’ stories
To help answer some frequently asked questions, the College earlier this year developed a helpful factsheet that includes a list of questions patients should ask their radiation therapy provider about the costs of treatment.
In addition to covering the range of costs that patients should consider, the factsheet also explains the Medicare Safety Net, Medicare contributions and arrangements for concession card holders. The factsheet includes
We are always looking for patients and clinicians to support our efforts to raise awareness of radiation therapy by sharing their stories and experiences. Reading and hearing their stories helps other cancer patients and their families and friends to understand the experience of radiation therapy treatment. They are a powerful tool and offer valuable insight into the patient experience. Personal stories also create a shared sense of community and connection, lessening the isolation many patients may feel when faced with decisions about the best treatment options for them.
If you or your colleagues have any patients who may be willing to share their experiences with Targeting Cancer, please let us know by emailing us at faculty@ranzcr.edu.au

Advocacy 28 Inside News
“Radiation therapy services are essential and still accessible. Radiation oncology teams have made special provisions for patients to ensure any risks presented by COVID-19 are minimised. Every precaution has been taken to ensure infection control and the safety of patients and staff.”
RADIATION THERAPY: WHAT YOU NEED TO KNOW ABOUT THE COST OF TREATMENT IN AUSTRALIA
There are several cost factors you and your family need to think about when choosing the best treatment provider for you. These include direct costs such as those covered by Medicare, and other costs such as travel, parking, accommodation and any allied health care that may be required. Many radiation therapy centres have staff who can talk you through these considerations.
For more information about radiation therapy and how it helps patients visit https://www.targetingcancer.com.au/what-is-radiation-therapy/
WHAT ARE THE COSTS ASSOCIATED WITH RADIATION THERAPY?
Radiation therapy treatment at public or partnership radiation therapy centres (where public services are provided at a public centre by a private provider) is generally provided without a cost to the patient.
Radiation therapy at a private centre may incur out of pocket costs, also known as a gap or gap payment. This is the difference between the cost of treatment and Medicare rebate. You are required to pay the full cost yourself before you can claim a rebate from Medicare.
Any direct costs charged by a radiation therapy centre, Medicare rebates applicable to you and any out of pocket costs (gap) that you will need to pay must be made clear to you before treatment begins.
You will also need to confirm with the radiation therapy centre what other costs you are likely to need to pay as part of your overall treatment and recovery. Allied health care providers may be free of charge in the public system or may incur a cost if they are private providers. Your doctor or the radiation therapy centre may be able to advise you about your eligibility for government assistance for travel and accommodation.
You have the right to choose the radiation therapy centre who will provide your treatment based on your needs and considering all the costs involved Many radiation therapy centres have accounts staff to talk you through these considerations.
MORE THAN 1,500 VIEWS SINCE FEBRUARY 2020
The College’s radiation therapy factsheet has been viewed more than 1,500 times since February 2020.
Feedback has been extremely positive; the factsheet provides an easy to understand overview of cost considerations for patients undergoing radiation therapy and their families.
Referrers can direct patients to download the factsheet from the Targeting Cancer website at www.targetingcancer.com.au/faqs/what-you-need-to-know-about-the-costs-of-radiationtherapy-in-australia/

The State of Neurointervention Practice in Western Australia
Interventional neuroradiology (INR) has developed as a specialty rapidly over the last 20 years but its status varies in different continents and states. Neuroradiology was the first recognised subspecialty in radiology in the early seventies and, from this beginning, early interventions were restricted to palliation of arteriovenous malformation and congestive cardiac failure. The proliferation of endovascular techniques in the late 1990s/early 2000s, specifically for aneurysm treatment, gave baseload numbers for INR to practise. This combined with a simultaneous explosion of accurate non-invasive vascular imaging (MRA and CTA) increased the numbers of patients requiring treatment.
The opportunity to practice as a fulltime interventionist has been a reality in WA since 2000. In some cities this is hampered by a lack of infrastructure and understanding of the requirements to do so when viewed through the prism of a traditional general radiology department. Diagnostic radiology has a myriad of players, modalities and interest groups. The potential for INR can also be hamstrung by a lack of understanding or support from administration/allied craft groups and further compounded by the invisibility of the interventionist to the public.
Neurological Intervention and Imaging Services of Western Australia (NIISwa) was formed in 2007, as a holistic allembracing approach to patient care. We focused on the following elements:
• Admission rights
We had enjoyed these for many years, but they require suitable junior staff to manage the patient’s hospital admission.
• Ward junior staff
A single Fellow is inadequate, and we required, as does any clinical team, a medical registrar and two RMOs attached to our service, enabling a consultant-led practice. An offshoot of this practice is that we now have 10 years of junior staff (more than 200) who intimately know what benefits
INR provides and act to make the department more visible to the medical community. NIISwa furthered our exposure by having a medical student attached to the unit and affording nursing staff and students study days to attend our unit.
•
Clinical governance of patients’ admission
This is essential, especially if there is a complication. The appropriate therapy or advice is given by the expert practitioner rather than being filtered through related parties. Liaising and counselling family is best directed by the expert practitioner rather than under the bedcard of a third party. Follow-up and discharge planning are more efficient and accurate for GP liaison.
• Ward support
Provision of beds with patients under our bedcard and daily ward rounds have normalised INR activity, with nursing and allied staff welcoming the input and interest of the team. Equal access to paramedical staff (physiotherapy, occupational therapy and speech) makes treating patients easy and routine, even with complications, as we are part of the furniture not ’the X-ray guys who want something’.
• Anaesthetic support
75 per cent of INR procedures are category 1 emergencies. It was and is inappropriate that INR units are given one to two days of general anaesthetic support when other disciplines were given daily access to anaesthetic support. The provision of 14 sessions of support per week at one site and seven sessions at other sites, enables appropriate and rational treatment of patients and allows new procedures to flourish. A separate anaesthetist is on call specifically for our service including an anaesthetic technician.
• Expert MIT and nursing staff
NIISwa nurses and MIT staff are full-time which has a logarithmic effect on room
turnover, appropriate device stocking, procedure time and calm advice from the right of the operator late at night. It engenders team spirit and a great working environment, good for staff, anaesthesia, related craft groups and the patient.
• Administrative support
This is essential to enabling all outpatient visits, whether new or followup, to be logged and a letter to the referring doctor, with a copy to the GP, to be produced. This closes the loop and clearly demonstrates to the medical fraternity who is performing the procedure and prescribing the therapy so any questions or complications can be directed to the right person.
• Standardised imaging follow-up
Arranged by the INR and organised by the administrative team, this allows the INR who performed the procedure to follow up and use the imaging report to triage the patient back to out-patients, plan therapy, additional follow-up and send a copy to the GP with a clinical plan. No case is reported by another radiologist therefore none are lost to the system. It is a closed, efficient loop and medico-legally sound.
• Expansion of outpatient clinics
We now have 14 clinics per week including a 3-month modified Rankin Scale (mRS) stroke clinic that allows us to independently assess suitability for treatment and follow-up of patients from statewide specialty and non-specialty referrals.
• Position at the table
Involvement in decision-making with administration is essential. A highvolume dedicated specialty has more chance of cutting through than occasional operators working in a large multi-interest radiology group. Positions such as the Neuroscience Divisional Director, membership to the State Stroke Advisory Committee and hospital executives give INR a voice.
30 Inside News Interventional Radiology
• New procedures
We can introduce new procedures more easily as the infrastructure and human support makes the environment favourable to do so, both with new devices (pipeline, web, thrombectomy) and revolutionary procedures (venous stenting for intracranial hypertension and middle meningeal artery embolisation for chronic subdural haematoma). These are added to the routine epistaxis, tumor embolisation, DAVF/AVM/peripheral vascular anomaly treatment, carotid and vertebral artery stenting, vasospasm and other ancillary procedures.
• Data collection and research
This is centralised and benefits from the set-up of the department with contemporaneous statistics on stroke outcome available 24/7.
• CCINR accredited high-volume INR practitioners
CCINR accredited INRs are the linchpin of the service resulting in a uniform approach to pathology and treatment with regular morbidity and mortality meetings. Weekly INR case conferences regarding upcoming cases and weekend phone calls to a friend for extra support are routine. A collegiate atmosphere allows discussion of complications and a practice-wide minimum standard of care is demanded.
The establishment of a stand-alone interventional neuroradiology specialty group cross campus state service (NIISwa), supported by diagnostic neuroradiologists, was welcomed by neurosurgery, neurology, ICU and anesthesia, who saw the patient benefits as they worked closely with INR. Interestingly, at its commencement, the sole resistance encountered was from other radiologists. It has been seen however to be a highly beneficial exercise and made rolling out a 24/7 stroke service seamless and amazingly cost-effective with few new resources available to the department. Length of stay for aneurysm cases is less than 36 hours and the endovascular treatment of SAH and stroke treatment have revolutionised patient outcome, quality of life and cost to the state.
Figure 1 shows that procedures have exponentially increased over the last six years with no additional INR consultants. The benefits of a high-volume service have been demonstrated innumerable times in many fields of surgery and INR is no different.

INR can be practised in many ways but leveraging expertise in a unit with high volumes results in a great working environment, recognition by patients and related craft groups and excellent patient outcomes with associated large cost savings.
Australasian radiology would benefit from similar models being employed in other areas, as performing the procedure is a small part of the service. For general IR to flourish, its value needs to be acknowledged and embraced by both the medical community and diagnostic radiologists, recognising its clinical requirements and infrastructure in a meaningful way.
This will enable interventional radiologists to practice as fully-fledged clinicians, warts and all, rather than merely developing novel techniques that pass to other craft groups that possess the infrastructure as a given.
Clinical A/Prof Will McAuliffe FRANZCR CCINR Consultant Interventional Neuro Radiologist Neurological
Intervention and Imaging Service WA
Do you have any IR or INR articles you would like to contribute to future editions?
Please email your interest to interventional@ranzcr.edu.au
Volume 16 No 3 I June 2020 31 Interventional Radiology
What’s in Issue 3?
Medical Imaging
Original Article: Omental apoplexy: Unravelling the mystery
Corresponding author: Dr Warren Clements, Department of Radiology, Alfred Health, 55 Commercial Road, Melbourne, Vic, 3004, Australia.
Introduction To describe cases omental haemorrhage and to review the literature on this topic.
Methods We describe three cases of spontaneous omental haemorrhage and discuss various management strategies, in an attempt to provide direction for similar cases in the future.
Results A number of case reports of spontaneous or idiopathic omental haemorrhage exist in the literature. These cases are often attributed to an underlying vasculopathy, such as segmental arterial mediolysis (SAM). Appropriate resuscitation is paramount for best outcome. Severe bleeding may require surgery or transcatheter arterial embolisation, which is best performed early if required. Endovascular management using selective catheterisation of the bleeding vessel and embolisation is a minimally invasive alternative to emergent operative intervention. In the three cases we present, endovascular embolisation was performed in two patients, and surgical ligation in a third. Segmental arterial mediolysis is considered the likely aetiology in at least 2 of the 3 cases, based on imaging findings. No further episodes of haemorrhage occurred at follow‐up (ranging from 6 months to 2 years).
Conclusions Acute omental haemorrhage is a rare condition; however, it may be associated with significant morbidity and mortality. CT angiography is the imaging of choice. Management strategies include both endovascular and surgical intervention.

Medical Imaging
Point of View: What is a modern Interventional Radiologist in Australia and New Zealand?
Corresponding author: Dr Warren Clements, Department of Radiology, Alfred Health, 55 Commercial Road, Melbourne, Vic, 3004, Australia. As specialists in the use of medical imaging, radiologists are in a unique position to offer a range of non‐invasive and minimally invasive tests and procedures for patients. Prior to the 1990s, many diagnostic tests were invasive, and the skill set to perform most of the image‐guided procedures fell within the role of all radiologists. This included common yet invasive therapeutic procedures such as cerebral angiography, gastrointestinal embolisation and nephrostomy. The role of the modern radiologist has evolved since the explosion of technological advances in cross‐sectional imaging and in interventional techniques leading to the subspecialty model within radiology. This is supported by the most recent Royal Australian and New Zealand College of Radiologists (RANZCR) workforce survey results from 2016.1 Of the 2237 radiologists who responded, 155 identified as an interventional radiologist (IR) with the definition of Tier B procedures (advanced or complex) and 24 identified as an interventional neuroradiologist (INR). The report describes a reduction in the number of general radiologists performing basic interventional procedures over the last 10–16 years based on the current and previous surveys.1 There is also a small group of determined IRs establishing a foothold as independent clinicians within the private health system, which is not captured within these statistics.
Radiation Oncology
Original Article: Adapting to a global pandemic through live virtual delivery of a cancer collaborative trial group conference: the TROG 2020 experience
Corresponding author: Dr Lachlan McDowell, Department of Radiation Oncology, Peter MacCallum Cancer Centre, 305 Grattan Street, Melbourne, Victoria, 3000, Australia.
Introduction The global COVID‐19 pandemic forced the cancellation of the TROG 2020 face to face Annual Scientific Meeting (ASM). It was instead delivered as a live virtual meeting with six days of planning. Here we report the participants’ experience of this live virtual meeting.
Method Participants were invited to complete custom developed, pre and post meeting surveys to assess their expectations of and satisfaction with the live virtual format. Speakers and moderators were also invited to complete a custom developed satisfaction survey. The working parties of TROG (head neck/skin, genitourinary, breast and lung) were also sampled.
Results In total, 188/273 (69%) registered participants logged in to the live virtual meeting. The online engagement for each of the oral sessions ranged from 53‐66%. There were 102 and 57 responders to the online pre and post meeting surveys, respectively. The majority of pre meeting responders indicated a significant level of employer support to attend the virtual meeting. Post meeting satisfaction exceeded pre meeting expectations (‘very much’ and ‘quite a bit’; 86% v 54%; p<0.0001). The majority indicated they would be ‘quite a bit’ or ‘very much’ interested in future live virtual meetings.
Conclusion The TROG 2020 ASM was conducted as a live virtual meeting. Participant satisfaction and future interest in a live virtual meeting was high, indicating this is a viable platform for other CCTG’s faced with the decision to deliver virtual content at times of global public health threats.
Radiation Oncology
Original Article: Quality and access – Early experience of implementing a virtual stereotactic chart round across a national network Corresponding author: Mr Rhys Fitzgerald, Icon Cancer Centre, Gold Coast University Hospital, Southport, Qld, 4215, Australia.
Introduct Stereotactic radiation therapy is a highly specialised technique which requires careful and structured implementation. As part of a national stereotactic programme implementation, protocols were developed and a national stereotactic chart round was formed, which strongly recommended attendance and presentation of all cases before treatment. Herein, we describe our experiences launching a national chart round and its importance in a stereotactic programme.
Method Stereotactic chart rounds were held via videoconference between July 2018 and July 2019. Data collected included attendances, patient‐related information including, diagnosis, clinical background, treatment intent, prescribed dose and fractionation and technical approach. Consensus recommendations regarding changes to treatment approaches were also recorded.
Results For the 12 months recorded, there were 1126 attendances, from 144 individual attendees, across 21 locations. In total, 285 cases (237 new cases, and 48 re‐presentations) were presented by 27 radiation oncologists (ROs) from 13 different locations. From the cases presented, 65 changes were recommended from 53 patients (22.3%), including 27 (11.4%) changes to contours, 18 (7.6%) changes to dose prescription/fractionation, 9 (3.8%) changes to plan dosimetry, 1 (0.4%) changes to treatment technique and 10 (4.2%) recommendations for which stereotactic radiation therapy was not advised. A significant inverse relationship was found between frequency of recommended changes and the individual RO’s stereotactic case load (P < 0.002).
Conclusion The implementation of a national stereotactic chart held via videoconference has ensured national protocol compliance across the network of locations. Furthermore, the chart rounds have allowed the entire multidisciplinary team to be provided with mentorship and guidance. Increasing number of cases presented was associated with lower rates of recommended changes highlighting the impact of experience and the need for continued mentorship.
If you are a member of the Royal Australian and New Zealand College of Radiologists, access JMIRO free online. - Go to www.ranzcr.edu.au -

your College username and password
to all JMIRO current and digitised backfile content from volume 1, 1957!

your College journal online
Access
Log in using
= FREE
access
The current human biosecurity emergency has rightfully seen our governments be agile and act very quickly to implement legislation and strategies to minimise the spread of the virus and provide economic support to the peoples of Australia and New Zealand.
The quick decision-making and speed of implementation by government is appropriate to the circumstances but very different from the regular process of progressing change in policy, which involves a great deal of work from a large number of people. Our experience of advocating change to governments is one of many meetings and a very long lead time in achieving change.
Advocacy is one of the strategic pillars of our College strategy and we work hard to improve safety, quality and access for our patients in both Australia and New Zealand.
Amid the turmoil of the pandemic it is easy to overlook the positive. I would like to share with you a good news story about the changes that have been achieved though the collective effort of many members advocating for better access to imaging for women with breast cancer symptoms.
In 2016, the International Day of Radiology’s theme was breast imaging. We used the opportunity to conduct a roundtable in Canberra with other stakeholders who are similarly committed to improving outcomes for patients with breast cancer. From the roundtable a Statement of Principles
Our Advocacy: A Good News Story for Breast Cancer Patients
A Message from the Dean

was developed and presented to the Federal Government. There were three cogent asks:
• Unfreeze and increase Medicare patient rebates
• Remove the multiple services rule for breast ultrasound and biopsy
• Expand access to breast MRI.
• From 1 July 2020, indexation will be introduced for CT, X-ray and ultrasound which includes mammography so patient rebates will be increased
• From 1 May 2020, a new item has been introduced to Medicare which allows for a diagnostic breast ultrasound and a biopsy to be done at the same time, removing the multiple services restriction that has caused such difficulty for patients
• From 1 November 2019, a new rebate for breast MRI was introduced into Medicare.
We were successful in achieving our goals due to a number of key factors. Firstly, we identified and documented the issues. Our message was clear, concise and easy to follow. We had very specific asks of what action we wanted the government to take. The actions we sought of the government were measured and showed a clear benefit to patients. We also had support of other stakeholders with similar interests including key consumer groups to carry the same messages to government.
It is very gratifying to see that our advocacy has borne fruit with each of these asks achieved, or set to be achieved, in the period from November 2019 through to July 2020.
This is a long overdue advance and recognises the critical role that diagnostic imaging plays in improving health outcomes for Australian women.
One meeting rarely brings results. These asks for breast imaging have been advocated for through many channels, in addition to the abovementioned roundtable, we have pressed for these changes via the Diagnostic Imaging Advisory Committee of the Medical Benefits Schedule Review Taskforce, through many meetings with several Health Ministers, politicians and Department of Health public servants.
continued over...
Clinical Radiology Volume 16 No 3 I June 2020 33
Clin A/Prof Sanjay Jeganathan
“I would like to share with you a good news story about the changes that have been achieved though the collective effort of many members advocating for better access to imaging for women with breast cancer symptoms.”
The College is bi-national and we are working just as hard in New Zealand to achieve improvements for patient care.
The College is a very actively participating in the New Zealand Health and Disability Review. Our submission highlights a number of key issues including:
• The critical workforce shortfall of clinical radiologists

• The need for investment in digital technology
• The pivotal role of clinical radiology and radiation oncology in all aspects of healthcare delivery: prevention, diagnosis, treatment and monitoring.
These issues will be a key focus for our election strategy for the upcoming New Zealand election. I look forward to providing an update about similar positive results from our advocacy activities in New Zealand in the future. Advocacy requires relentless determination from both members and staff at the College, but if we work hard and stay focused, we will reap the reward for our patients.
If you have any questions or comments about this article please contact Kirsten Fitzpatrick, Project Officer, on fcr@ranzcr.edu.au
Cardiac CT Training 2020
We go beyond simply meeting training requirements:
l Maximum allowable course based live and library cases for ANZ credentialing.
l RANZCR accredited for 117.5/67 CPD points (Level A/Recertification).
l Officially sponsored and endorsed by GE Healthcare for more than10 years.
l Live scanning at second highest global recruiting site in SCOT-HEART study.

l Unrivalled venues - Now at Zest, Point Piper, Sydney.
5 Day Level A Course: 8th - 12th October 2020
3 Day Level A Course: 10th -12th October 2020 For more information and online registration log on to: www.aicct.com.au or contact us at: info@aicct.com.au
lnsid eR0 diology
Clinical Radiology Information for HEALTH CONSUMERS & HEALTH PROFESSIONALS

Raises awareness of medical imaging and the role of the clinical radiologist. Written by RANZCR Fellows and other Australian and New Zealand health professionals, edited by consumer and GP contributors.

✓ Information about clinical radiology tests and procedures in plain English
✓ Additional technical information for health professionals
✓ Approximately 100 information items with new items added regularly
Clinical Radiology 34 Inside News
2020 COURSE DATES: UA T R ALIANINSTITUTE OF CARDIOVASCU A TC A I CCT
Like most aspects of society, our training departments, and the lives of our trainees and trainers, have been significantly disrupted by the global pandemic. The earliest and most significant of these changes was the cancellation of our Series 1 examinations, but all facets of training have been affected, from the day-today training environment, to formal and informal training activities, department accreditation, and assessment of IMGs.
We have been in close communication with other medical specialty Colleges during this period, and it has been reassuring to know that we are not unique in the challenges we have faced and the decisions we have needed to make.
The College COVID-19 Taskforce was created in early March, and includes the Chief Censors of both Faculties. It has been an honour to work with this group to navigate the issues that have affected our profession. The objectives of the group include keeping abreast of the current global and national status of the virus, government advice and restrictions and latest research, and ensuring continuing provision of a safe and operational working environment for members, including trainees.
One of the early outcomes of the Taskforce was the creation of Guidelines for education and training decisionmaking in relation to COVID-19. These guidelines set out the overarching priorities, principles and strategies to guide decision-making on training and accreditation, assessments,
Clinical Radiology Training During the COVID-19 Pandemic
Chief Censor in Clinical Radiology
examinations and other training activities, and can be found on the College website:
www.ranzcr.com/college/documentlibrary/education-and-trainingguidelines-for-decision-making-relatedto-covid-19
Our priorities include protecting the wellbeing of trainees and trainers, and while we recognise that there have been and will continue to be necessary changes to the training environment, we prioritise maintaining a balance between the provision of clinical services and the objectives of the training experience.
Our principles are many: we recognise that training and IMG placements will likely be disrupted for a period of at least 6 months, that while the experiences during this period will be different from normal they will nonetheless be professionally valuable, and most importantly we seek to ensure that, as far as is practicable, trainees progress through training at the usual pace.
Our strategies necessarily cover the main aspects of training, and in line with our priorities and principles seek to be flexible, to support and not penalise trainees during this period, to extend timelines where needed, and to consider alternative and innovative ways to deliver training and assessments.
It is reassuring that our guidelines are in line with the National principles for clinical education during the COVID-19 pandemic recently released by the Australian Government Department of

Health, AHPRA and National Boards, including safety, continuation, outcomefocus, collaboration, innovation, capacity, and risk management.
www.health.gov.au/sites/default/files/ documents/2020/04/national-principlesclinical-education-during-the-covid-19pandemic.pdf
To accompany the College guidelines we have developed FAQs which can also be found on our website:
www.ranzcr.com/our-work/coronavirus/ impact-on-college-activities#FAQs
I recognise that the cancellation of the Series 1 examinations created enormous stress and anxiety for those trainees and IMGs involved, but it was a necessary decision given the rapidly escalating government, jurisdictional and workplace requirements at that time around social distancing and border closures.
In line with our focus on facilitating trainee progression, the Specialty Training Unit (STU) is working toward the delivery of both Part 1 and Part 2 examinations later in the year.
It is very unlikely that we will be able to run the examinations in the usual manner, and while we will endeavour to minimise change to examination content, it is likely that there will be changes to the examination format to enable examinations to be taken locally. Also, in line with our guidelines, we will give a minimum of three months’ notice of examination sittings.
continued over...
Volume 16 No 3 I June 2020 35 Clinical Radiology
Dr Meredith Thomas





36 Inside News NEW ZEALAND ASM A UGUST 6 - 8 2021 NZ Annual Scientific Meeting 2021 Intercontinental Hotel, Wellington www.ranzcr2021.co.nz NEW DATES ANNOUNCED 6 - 8 AUGUST, 2021 MEETING UPDATE
There are clearly continuing uncertainties about the longer-term impact of the pandemic. We have been through a confusing period where, contrary to expectations, both our public and private training departments have experienced a significant reduction in workload.
Many departments have implemented measures to protect their radiologist workforce, with home reporting for both consultants and trainees, and division into teams. Clinical meetings and multidisciplinary meetings have largely moved online, as have tutorials and lectures.

There has been considerable stress for trainees relating to impact on training, progression and employment opportunities, as well as concerns regarding their own safety and the safety of their families, access to personal protective equipment, and the potential for deployment to more high-risk areas.
Please contact the Trainee Liaison Officer, Senice So, via senice.so@ranzcr.edu.au or 0437 893 913 if you would like to discuss any issues or concerns.
While case numbers in Australia and New Zealand are reducing and social distancing measures are being relaxed in some jurisdictions, it is likely that the novel coronavirus will continue to have an impact until a vaccine becomes available.
There is an increasing recognition of the impact there has been on usual healthcare provision with recent relaxation of the restrictions on provision of screening services and surgery, and radiology workload is gradually returning to pre-pandemic levels.
I would encourage departments and practices to continue their infection mitigation strategies, and carefully balance the up-scaling of operations with the risks associated with relaxation of containment strategies.
During this period there have been some positives; we have all become more familiar with online communication and meeting delivery, we have learnt to compromise and collaborate and be innovative in the way we do things, and have been more willing to reach out to others and share ideas and resources. For some working from home has enabled increased time with family. We have all become much more aware of our vulnerabilities and I would like to think that we have developed a heightened awareness of those around us and an increased willingness to reach out and support others.
If you have any further questions in relation to COVID-19 and training, please contact radtaa@ranzcr.edu.au
Volume 16 No 3 I June 2020 37
Clinical Radiology
Clinical Radiology Trainee Matters

• Completing the application form for consideration of special circumstances www.ranzcr.com/college/documentlibrary/consideration-of-specialcircumstances-policy
• Including your desired payment structure (for example: quarterly payment, monthly payment or deferred payment).
travel interstate or across the Tasman sea, and I am cautiously confident that there will be some examinations in the second half of this year. Please stay on track as best as possible with your preparation and keep an eye out for official updates if you plan to sit examinations at the next available attempt.
Dr Matthew Lukies Alfred Health

Fast forward to June 2020, and who would’ve predicted this year could be so unique and challenging? I hope that you are all keeping well, (re)discovering home hobbies, making the most of electronic learning resources and mastering the optimal angles and lighting for video meeting chats. Many of you will have been involved in the care of patients with novel coronavirus and others affected indirectly by changes to emergency and elective services. Australia and New Zealand have done a tremendous job in the early stages of this pandemic and I am confident that we can navigate the road ahead well as a community.
Over the past few months, I have been contacted by a number of trainees with concerns about the College training and exam fees given their personal financial situation. Everybody’s circumstances are different, and the College has a process by which individual circumstances can be considered and alternative arrangements made. If you would like to apply for consideration, I suggest:
Outlining your desired structure makes the process more efficient administratively and increases the chances of approval. The College has made alternative arrangements for many trainees in the past and I encourage anyone experiencing difficulty to get in contact.
Progression in training has also been on the minds of many trainees during this period. Please be assured that the priority of the College is to ensure that trainees are minimally impacted by the disruptions this year, and this sentiment is reinforced by the trainee representatives on the core committees including training and assessment, research and faculty council. A large body of work is going on behind the scenes to structure examinations that can be implemented without requiring
Regarding research, the cancellation of conferences this year has decreased the available opportunities for trainees to complete their research requirements in training. The College is understanding of this and I encourage anyone who has concerns about their project to speak to the Director of Training (DoT) about alternative options.
Finally, memes are great. I hope you enjoy this one.
Much like your parents, we would love to hear from you more often!
Please feel free to email the Clinical Radiology Trainee Committee (CRTC) at clinicalradtc@gmail.com with your thoughts, questions, and feedback.
Clinical Radiology 38 Inside News
Image credit: reddit.com/r/Radiology/
The Professional Practice Committee (PPC) has started the year off with a flying start. Although it’s not the start to the year that any of us were expecting with the current pandemic causing widespread disruption across the health system, the PPC are still progressing with planned work.
Fortunately, the committee held a face-to-face meeting just prior to travel restrictions coming into effect across both Australia and New Zealand. Some of the key pieces of work that are being undertaken include:
2020 CPD exemptions due to COVID-19
Just a reminder that due to the pandemic both the Medical Council of New Zealand (MCNZ) and the Medical Board of Australia (MBA) have acknowledged that COVID-19 work will impact on the ability of all doctors to maintain CPD requirements in the coming months.
As a result, the College has revised the CPD requirements for the 2019–2021 triennium with clinical radiology members only requiring a total of 125 points required for the triennium (usually 180 points).
In addition to this, there will be no annual compliance audit for the 2020 CPD calendar year.
Chief of Professional Practice Update
If you have any questions about the revised CPD requirements for 2020, please contact the team via cpd@ranzcr.edu.au
Silicosis: National Dust Disease Taskforce
In the March edition of Inside News, we detailed the five national actions which have come out of the Commonwealth Department of Health National Dust Disease Taskforce. From here, a stakeholder meeting was held in late March 2020 to workshop and develop nationally consistent guidelines for the health assessment of workers associated with the engineered stone industry. The College is continuing to remain at the forefront of this important health issue and is currently working with our clinical leads with expertise in dust lung disease imaging to provide feedback to the Department of Health. We will continue to provide updates on this rapidly evolving issue.
Lung cancer screening enquiry
Earlier in the year, the College was invited by Cancer Australia to provide feedback into their consultation on the design and development of a proposed national lung cancer screening program. The College welcomed the opportunity to be a part of this important piece
of work, which will ensure that the crucial role of radiology in screening is considered during the design and development phase of the project. The College will also be commencing the development of a position statement on lung screening to complement this and will again utilise the expertise of the Australian and New Zealand Society for Thoracic Radiology (ANZSTR) to help steer this process. If you are interested in being involved, please get in contact with the College via professionalpractice@ranzcr.edu.au In closing, if you have any questions regarding the work of the Professional Practice Committee please get in touch via professionalpractice@ranzcr.edu.au.
I would like to extend my best wishes to the Fellowship as we progress through these unprecedented and uncertain times. I hope to be able to catch up with you at upcoming events in the future.
I look forward to bringing you further updates on the work of the PPC as we move through 2020.
Yours sincerely,
Dinesh
A/Prof Dinesh Varma Chief of Professional Practice Faculty of Clinical Radiology

Clinical Radiology Volume 16 No 3 I June 2020 39
A/Prof Dinesh Varma

It’s been said that the next wave of progress in oncology will come from an increased ability to harness the power of technology—collecting and analysing data to enable better, faster decision-making in clinical care and business processes. That next wave is here. We call it Intelligent Cancer Care™ . Learn more at varian.com/intelligent Welcome to a new era in oncology © 2019 Varian Medical Systems, Inc. Varian and Varian Medical Systems are registered trademarks, and Intelligent Cancer Care is a trademark of Varian Medical Systems, Inc. Refer enquiries to Varian Medical Systems Australasia on 1800.657.036 or customerservice-anz@varian.com
These are interesting times we are living in. Only three months ago I welcomed members to a new year and new decade. At that time, many of us were struggling with the effects of the Australian bushfires. No one could have imagined being engulfed in a pandemic so soon afterwards.
COVID-19 has been a challenge, but I am proud at the way our profession has stood up to it. Departments have responded nicely to the crisis making necessary changes to the way they run their business.
Safety of patients and staff remained central to these changes even while ensuring continuity of services. Most departments have taken appropriate steps to keep their vulnerable staff safe and I encourage other departments to do the same.
I am pleased to see that staff that tested positive for COVID-19 have recovered well and the affected departments continued their services with strict risk mitigation strategies keeping the rest of their staff and patients safe.
These are indeed tough times and there may still be more to come; however, as restrictions are eased, we should move forward with caution.
The College’s decision to put together a COVID-19 Taskforce proved to be the key strategy that allowed us to respond quickly to multiple challenges.
The Taskforce included busy clinicians who worked very hard developing guidance for our members and
Caring for Each Other: COVID-19 and Beyond A Message from the Dean
departments, taking learnings from other countries, reviewing emerging evidence for patient treatments, recommending risk mitigation strategies, providing useful resources developed nationally and internationally, assessing trainee-related matters, and making appropriate recommendations to the Board.
Prof Liz Kenny, a member of the task force, will be participating in the International Atomic Energy Agency’s webinar on ‘COVID-19 Related Changes in RT Practice’, sharing our experiences with our international partners and learning from theirs. As is evident by now, despite closed borders, we are more unified than ever before as we support each other across geographical boundaries.

New Zealand’s pandemic response has also included guidance posted on the Ministry of Health website about appropriate care for patients with cancer. The protocols have including telehealth appointments where possible, deferment of care and adjustments to planning.
At the time of writing, New Zealand looks set to drop to Level 2—it is hoped that care can return to a more ‘normal’ state, with sensible social distancing and hygiene protocols.
Trainee wellbeing
The current situation warranted some tough decisions to be made relating to our trainees and examinations. The interruptions in training activities,
varying work arrangements and uncertainty around examinations no doubt are causing significant anxiety among our trainees. I would like to reassure all trainees that our education, training and examinations teams are busy developing workable solutions. In the meanwhile, I urge trainees with any concerns to reach out to their clinical supervisors, Director of Training or the College’s Trainee Liaison Officer.
While this is an especially challenging time for the trainees, the Faculty Council and the Board have long been concerned with the wellbeing of our trainees. The recent survey by the Medical Board of Australia (www.medicaltrainingsurvey.gov.au/ Results/Reports-and-results) showed that almost a third of radiation oncology trainee respondents have experienced workplace bullying and harassment at some time during their training.
This is appalling and unacceptable. We must have zero tolerance to bullying and harassment and must be neither silent spectators nor perpetrators.
The mentoring working group was set up with an aim to develop strategies to support our trainees. The College also has a policy document on bullying and harassment and trainees are encouraged to refer to this. However, I am well aware that more needs to be done.
Volume 16 No 3 I June 2020 41 Radiation Oncology
Dr Madhavi Chilkuri
continued over...
New Zealand workforce
Before the pandemic sent New Zealand into lockdown, the Cancer Control Agency and Health Workforce had been working on demand and workforce modelling in New Zealand. The modelling supports the College’s longstanding argument that New Zealand must train more radiation oncologists.
Encouragingly, the government seems interested in discussing real solutions to the workforce crisis, which includes radiation oncologists, radiation therapists and physicists.
Regional services
Over the past months a significant amount of work has been put into the review and update of the 2016 Establishing and Sustaining Regional, Rural and Remote Radiation Therapy Centres position paper. Published by the College, this document has been developed under the auspices of the Radiation Oncology Alliance (Australasian College of Physical
Scientists and Engineers in Medicine, Australian Society of Medical Imaging and Radiation Therapy, Cancer Nurses Society of Australia, and the Faculty of Radiation Oncology) and serves to provide guidance to new and existing regional facilities.

More detail is provided on page 47 of this issue. I extend my thanks to all the members and stakeholders who took time to review and provide feedback on the document during the consultation phase.
This is a key guidance document for establishing regional services and I am hopeful that this will help both new and existing regional centres in fulfilling their purpose of providing safe and highquality care to patients irrespective of their geographical location.
Targeting Cancer
The Targeting Cancer Management Committee has made a strong start since being formed in March. Before their first meeting, the Committee was charged with developing a set of
questions that our cancer patients may have in relation to COVID-19 and providing the answers.
'Radiation therapy during COVID-19: frequently asked questions' has been published on the Targeting Cancer website:
www.targetingcancer.com.au/radiationtherapy-during-covid-19-frequentlyasked-questions/
The College will develop further resources for consumers as part of the Targeting Cancer campaign.
If you have any questions or comments about this article, please contact the Dean via faculty@ranzcr.edu.au
42 Inside News Radiation Oncology
As I write my second report as Chief Censor, it seems that aeons have passed since I wrote my first. It is probably due to the fact that we have felt that we have been living in limbo, uncertain of what is to come in the days or weeks ahead.
Yet, I am proud to say that I work alongside friends and colleagues who have courageously stepped up in response to the enormously disruptive effects of the pandemic. They have made significant changes to their operations, plans and policies, as well as communicating them in a timely fashion to the relevant stakeholders.
In early March 2020, the Board decided to establish a COVID-19 Taskforce, comprising of key members of the College, to coordinate a whole-ofCollege response to the evolving outbreak in a thorough, responsive and targeted manner.
It is indeed a privileged experience to have collaborated with this experienced and well-informed group of individuals. One of the first tasks of the Taskforce was to establish a guideline articulating the overarching priorities, principles and strategies to guide decisionmaking on all matters related to training and assessment, accreditation and examinations during the pandemic and beyond.
In line with this document and in order to mitigate the risks of disease spread, as well as prioritising the health of all Fellows, trainees and College staff during the escalating period of the COVID-19 outbreak, the Taskforce made a series of difficult but pragmatic decisions.
Agility, Resilience and Lasting Change
Chief Censor
in Radiation Oncology
The recommendation was for the suspension of most activities related to the education and training sphere. These included the viva voce component of the Series 1 Phase 2 examinations, the Phase 1 and Phase 2 teaching courses, the ESTRO Basic Clinical Radiobiology Course and the Directors of Training workshop.
and ensuring that the administrative workload for departments is not overly onerous during this time, a basic framework outlining trainees’ working arrangements during this time has been requested and implemented.
The impact on any individual trainee is, however, very diverse and unevenly distributed across different countries, states and territories and even among the various local health jurisdictions within any given state.

As different trainees are affected differently and cope differently under these circumstances, it was important that the principle of flexibility be maintained and therefore a universal pause in the training trajectory was not enforced for every trainee. Instead, individuals who felt that they require consideration of special circumstances were encouraged to apply for this under the stated College policy:
www.ranzcr.com/college/documentlibrary/consideration-of-specialcircumstances-policy
In particular, extended time in training, if required, would be supported.
These resolutions have undoubtedly caused stress and anxiety on our trainees. The additional strain of a reduction in both clinical supervision and clinical exposure to training program requirements has been recognised.
In order to achieve a practical balance between protecting trainees, fulfilling accreditation requirements
The resumption of the safe delivery of the examinations is a priority currently but it is likely that a change in format would occur to comply with principles of social distancing.
Alternative methods of educational delivery and training are already in place in many training networks and I want to take this opportunity to express my thanks and gratitude to the invaluable contribution of those who have worked tirelessly to make this operational.
Radiation Oncology Volume 16 No 3 I June 2020 43
Dr Yaw Chin
continued over...
“Alternative methods of educational delivery and training are already in place in many training networks and I want to take this opportunity to express my thanks and gratitude to the invaluable contribution of those who have worked tirelessly to make this operational.”
The resilience and innovation demonstrated by all those involved has been exemplary and is a testament to the commitment of Examiners, Training Network Directors, Directors of Training and Clinical Supervisors, for ongoing trainee education and their welfare.
The other significant area of disruption from the pandemic is that of the Training and Assessment Reform (TAR) implementation. As a result of cancellation of the roadshows and other activities, the commencement of the new training program is now scheduled for late 2021 for New Zealand trainees and early 2022 for the Australian and Singaporean cohort.
Nevertheless, work is ongoing in this arena with development of online resources such as video modules to replace the face-to-face roadshows, educational videos and podcasts/ vodcasts.
The additional time afforded to the Implementation Working Group will be spent refining the training materials and communication tools to convey key messages and bite-sized information regarding the new training program. Despite the unpredictable nature of the road to recovery, I feel confident that together, we are able to adapt and adjust to the changing environment that we have been subjected to.
The transformative impact of this pandemic on the way we educate, train, assess and examine will be felt for many years to come but the changes implemented as a result of this will hopefully be changes that are for the better.
If you have any questions or comments about this article please contact Legend Lee, Manager, Training Programs, on rotraining@ranzcr.edu.au

Radiation Oncology 44 Inside News
Radiation Oncology Trainee Matters
the resumption of these activities will be guided by the COVID-19 College Taskforce. Education and training opportunities at each individual training site are also affected to varying degrees, with working-from-home arrangements in place at some centres, and reduced face-to-face clinical exposure with the use of telehealth or phone reviews at others. This is a challenging period for various reasons for us all. Nonetheless, it is most important for all trainees to continue to stay safe and well.
ROTC members are assigned to a College sub-committee. Throughout this year, we will be providing trainees with insights into ROTC members’ involvement in these sub-committees— starting with an update from Dr Mollie Kain (NZ) from the Radiation Oncology Research Committee (RORC) in this edition of Trainee Matters. We hope that this will encourage more trainees to be involved in the ROTC and continue to contribute to College activities in the coming years!
With a rather disrupted start to the clinical year with the COVID-19 pandemic, there is no doubt that many of the College-related activities for the year—including educational courses, Training and Assessment Reform (TAR) implementation roadshows, examinations, and the Annual Scientific Meeting (ASM) among others—have been impacted, and any decisions on
During this period of uncertainty, some of the priorities for the Radiation Oncology Trainee Committee (ROTC) for 2020 will continue to progress, including collating and developing an updated radiation oncology fellowship database that will be accessible to all trainees, and conducting a survey in collaboration with the Australasian Brachytherapy Group (ABG) to better understand trainees’ experience in brachytherapy and ways to enhance the learning experience and opportunities in this respect.
Apart from being a conduit between trainees and the College, most of the
Lastly, the ROTC will continue to communicate with all trainees through the ROTC representatives in your respective networks, as well as the monthly eNewsletter. Please feel free to reach out to us. The College also welcomes Senice So as the new Trainee Liaison Officer, please do not hesitate to contact Senice (senice.so@ranzcr.edu.au) to discuss any trainee-related issues or concerns in a confidential manner.
Dr Wee Loon Ong Chair, ROTC 2020

Radiation Oncology Research Committee (RORC)
The Radiation Oncology Research Committee has the role of promoting research within the field of radiation oncology. There are currently a lot of exciting initiatives and I have found being the trainee representative is a great way to get involved.
There are two new research prizes to be aware of: the Indigenous health research prize which has been set up to encourage awareness of and research into Indigenous cancer care, and the Quality research prize which recognises research on quality improvement.
I am looking forward to reading the manuscripts provided by this year’s applicants and to consider further ways of stimulating research and awareness in Indigenous cancer care.
The ASM is always inspiring for budding and experienced researchers alike and the Radiation Oncology Research Committee is continuing to explore options with the ASM organisers to promote the work of previous grant recipients as there is significant potential to learn from their experiences in the research arena.
I would like to remind trainees about The Clinical Scientist Pathway as it is an
excellent opportunity for those with a keen interest in research and I hope all new trainees consider it.
I also encourage trainees, Fellows and Educational Affiliates to check out the grants, prizes and awards available now to give yourself plenty of time to consider applying early next year.
To find out more more about The Clinical Scientist Pathway visit: www.aacb.asn.au/ professionaldevelopment/careers/ career-pathway
Radiation Oncology Volume 16 No 3 I June 2020 45
Dr Mollie Kain Trainee Representative, RORC 2020
Dr Wee Loon Ong
Simple* and Convenient †1,2
*Reconstitution and intramuscular administration vs leuprolide SC
†Available in 1, 3 and 6 month dosage forms
ADT for the treatment of hormone-dependent locally advanced or metastatic prostate cancer.1

ADT: Androgen Deprivation Therapy
SC: subcutaneous
These
not actual patients and are used for illustrative purposes only.
Before prescribing please refer to full Product Information which is available from Ipsen Medical Information. Ph: 1800 317 033 or from www.guildlink.com.au/gc/ws/ipsen/pi.cfm?product=ispdiphi.
PBS Information: Restricted Benefit. Locally advanced (stage C) or metastatic (stage D) carcinoma of the prostate.
Diphereline®: Triptorelin embonate 3.75 mg (1 month formulation) and 11.25 mg (3 month formulation) and 22.5 mg (6 month formulation). Indications: Hormonedependent locally advanced or metastatic prostate cancer. Contraindications: Known hypersensitivity to triptorelin or product excipients, GnRH or other GnRH agonist analogues; spinal cord compression secondary to prostate cancer metastases. Precautions: Androgen deprivation therapy may prolong the QT interval; potential bone mineral density loss; increased risk of mood changes and incident depression; adjustment of antihypertensive therapy may be required; initial transient increase in serum testosterone levels with potential transient worsening of symptoms of prostate cancer (tumour flare) and cancer related pain (metastatic pain) – consider administration of anti-androgen to counteract initial rise in serum testosterone levels and worsening of clinical symptoms; isolated cases of spinal cord compression or urethral obstruction; haematoma risk in patients treated with anticoagulants; suppression of the pituitary gonadal system; unmasking of previously unknown gonadotroph cell pituitary adenoma; hyperglycaemia and increased risk of diabetes mellitus; increased risk of cardiovascular events. Drug Interactions: Use with caution when administered with medicines known to prolong the QT interval or induce torsade de pointes; or with other medicines affecting pituitary secretion of gonadotrophins; hyperprolactinaemic agents should not be prescribed concomitantly. Adverse Events: Very common (≥10%): asthenia, back pain, paraesthesia lower limbs, libido decreased, erectile dysfunction, hyperhydrosis, hot flush. Common (≥1%, <10%): nausea, dry mouth, injection site reactions, oedema, hypersensitivity, weight increased, musculoskeletal pain, pain in extremity, headache, dizziness, loss of libido, depression, mood changes, pelvic pain, hypertension. Dose: Diphereline 3.75 mg once a month or 11.25 mg once every three months or 22.5 mg once every six months. Administration: Intramuscular injection; injection site should be varied periodically; inadvertent intravascular injection must be strictly avoided. Storage: Store below 25°C.
References: 1. Diphereline Approved Product Information. 2. Shore ND et al. Urologic Nursing 2013; 33:236-44 Diphereline® is a registered trade mark of Ipsen Pharma S.A.S. For further information about Diphereline®, contact Ipsen Pty Ltd: T (03) 8544 8100 F (03) 9562 5152 E info@ipsen.com.au www.ipsen.com.au. Ipsen Pty Ltd, ABN 47 095 036 909. Level 2, Building 4, Brandon Office Park, 540 Springvale Road, Glen Waverley, Victoria 3150, Australia. Date of preparation January 2020. TRI-AU-000446.
are
Supporting Quality Radiation Therapy in Regional Areas
The Radiation Oncology Alliance has recently updated guidance for provision of radiation therapy in regional or rural centres.
The Alliance consists of the four peak bodies representing radiation oncology professionals—the College’s Faculty of Radiation Oncology, the Australasian College of Physical Scientists and Engineers in Medicine, the Australian Society of Medical Imaging and Radiation Therapy, and Cancer Nurses Society of Australia.
The issues paper, Establishing and Sustaining Regional and Rural Radiation Therapy Centres, was first published in 2016 to give practical guidance to new and established radiation therapy centres providing services to regional areas.

Although focused on non-metropolitan centres, some of the content is relevant to any service. The 2020 update considers new and emerging techniques and technologies, changing models of care, and provides what are considered the minimum requirements for creating and continuing management of safe and quality service in regional areas. There was considerable stakeholder feedback during consultation, which was gratefully received by the Alliance.
The Alliance chose to update the guidance following government announcements in both New Zealand and Australia that will have positive impacts on access to services in regional areas.
In announcing funding for replacements of half the linear accelerators in New Zealand, the Ardern government noted that radiation therapy would be able to be delivered in Northland, Taranaki and Hawkes Bay, reducing travel for patients in these areas.
In the lead up to the May 2019 Australian federal election, the Morrison Government committed to establishing an additional 13 regional radiation therapy centres across the country. In the media release by the Nationals, it was acknowledged that neither the cost of radiation therapy nor the effectiveness as a treatment were barriers for patients; access is the key issue. Providers will tender to extend access to radiation therapy in the 13 identified areas, with the tender process managed by the Federal Department of Health.
The Radiation Oncology Alliance’s draft regional issues paper was shared with the Department of Health to help inform determinations around the upcoming tender and support quality service provision.
Members and stakeholders are encouraged to download and read the document, available on the College website:
www.ranzcr.com/college/documentlibrary/consultation-establishing-andsustaining-regional-rural-and-remoteradiation-therapy-centres
Volume 16 No 3 I June 2020 47 Radiation Oncology
Quality Corner Making Sure That 50Gy is 50Gy
Delivering quality care to our cancer patients is a multi-disciplinary approach. As radiation oncologists, we are fortunate to be able to work with highly trained and qualified radiation professionals. While we conduct our day-to-day work in front of patients, there are a group of professionals who work tirelessly in the background to ensure that treatment is delivered with the accuracy and precision required. Among these professionals are those of the Australian Clinical Dosimetry Service (ACDS).
The ACDS is an independent dosimetry auditing program, providing quality assurance for radiation oncology facilities and patients. The ACDS covers 100 per cent of Australian radiotherapy facilities and selected New Zealand facilities. Facilities undergo yearly audits, ranging from machine output checks, through to end-to-end tests of the patient treatment pathway. The core component of the audits cover 3DCRT, IMRT, VMAT and SABR deliveries. Additionally, the ACDS is continually developing audits to meet advancing radiotherapy technologies.
The latest development by the ACDS has been audits to test both the MRand CBCT-based adaptive workflows, which have recently been clinically released in Australia.

After a year-long development, the team completed a Level Ib (output check) and a Level III (end-to-end test) audit on the Elekta Unity MR-Linac. Dosimetric accuracy in the adaptive workflows was tested using MR-visible plastic ‘tumours’, which changed shape and size between CT and treatment. The process was subsequently applied to the Varian Ethos adaptive CBCT solution.

The ACDS has also begun field trial audits for stereotactic radiosurgery (SRS). The cranial head phantom, ‘Max’,
was custom designed by the ACDS for audits of complex SRS deliveries, in particular concurrent treatment of multiple metastases. Audit design was in consultation with TROG, to assist in credentialing for the OUTRUN and Local HER-O brain metastases clinical trials. The audit can be applied to SRS treatment on Conventional Linacs, Gamma Knife, Cyberknife, Tomotherapy and Halcyon systems, and has been completed at 5 facilities to date.
For more information on the ACDS you can visit their website: www.arpansa.gov.au/our-services/ testing-and-calibration/calibration/ australian-clinical-dosimetry-service
Dr Jessica Lye Director ACDS, Medical Physicist, ACDS
Ms Maddison Shaw
Clinical Operations Lead, Radiation Therapist, ACDS
Dr Albert Tiong RANZCR representative on the Clinical Advisory Group of the ACDS
Radiation Oncology 48 Inside News
ACDS' Rhonda Brown and Jessica Lye perform the Level III audit on the Elekta Unity MR-Linac.
'Max', the new ACDS cranial SRS phantom
The Revised Peer Review Audit Tool (PRAT)
Faculty of Radiation Oncology
Peer review is considered a valuable and important part of medical practice. The Peer Review Audit Tool was initially developed in 1999 to support peer review. To gauge peer review practice a survey of departments across Australia and New Zealand was conducted in 2018.

The PRAT is part of the quality framework delineated by the Radiation Oncology Practice Standards for systematically maintaining and improving the quality of the department.
It is not about ‘ticking boxes' or functioning as a tool for individual performance review: it is designed to enable organisations to understand processes, maintain quality control and learn to enable improvement.
It provides a template scoring sheet and can be modified to suit department practices, such as site-specific peer review involving a subgroup of radiation oncologists.
This revised peer review audit tool has been created using a combination of the last version of the PRAT, 2018 survey feedback, the ASTRO 2013 white paper on peer review 1, the RCR 2017 document on target volume delineation and peer review 2 and a number of other peer review tools used in practice and described in the literature 3–8
The Peer Review Audit Tool can be found on the College website: www.ranzcr.com/college/documentlibrary/radiation-oncology-peer-reviewaudit-tool
The College’s Recommendations
1. The PRAT should be combined with feedback to the treating radiation oncologist. This feedback is ideally provided in a peer review meeting where peers give educational and enabling feedback in order to improve radiation oncologist practice. In addition, where changes to patient management are discussed, the Faculty of Radiation Oncology recommends the patient be re-audited later to determine whether changes to patient care were implemented.
2. The PRAT should ideally be applied to every new patient simulated rather than selected ‘unusual’ or ‘difficult’ cases, as types of cases at high risk for suboptimal care have not been reliably identified. However, if it is not feasible to audit every patient, selection as per the ‘patient selection’ section of this document is strongly recommended.
3. Departments should provide regular teaching to auditors and peer reviewers in order to ensure consistency of scoring.
4. Departments should consider reviewing their audit results annually and consider publishing their results to improve the evidence base.
5. Peer review should be a component of a department’s written quality improvement policy.
Reference
1. Marks, L. B. et al. Enhancing the role of case-oriented peer review to improve quality and safety in radiation oncology: Executive summary. Pract. Radiat. Oncol. 3, 149–156 (2013).
2. Royal College of Radiologists. Radiotherapy target volume definition and peer review – RCR guidance. (2017).
3. Thaker, N. G. et al. Assessing the Quality of a Radiation Oncology Case-Based, Peer-Review Program in an Integrated Academic and Community Cancer Center Network. J. Oncol. Pract. 12, e476–86 (2016).
4. Matuszak, M. M. et al. Enhancing safety and quality through preplanning peer review for patients undergoing stereotactic body radiation therapy. Pract. Radiat. Oncol. 6, e39–46 (2016).
5. Gabriel, P. E. et al. An automated electronic system for managing radiation treatment plan peer review reduces missed reviews at a large, high-volume academic center. Pract. Radiat. Oncol. 6, e307–e314 (2016).
6. Mitchell, J. D., Chesnut, T. J., Eastham, D. V., Demandante, C. N. & Hoopes, D. J. Detailed prospective peer review in a community radiation oncology clinic. Pract. Radiat. Oncol. 7, 50– 56 (2017).
7. Harris, E., Hearne, R. & Shelton, C. A Prospective Peer Review Model for Radiation Therapy. Oncology Issues 32, 24–34 (2017).
8. Atwell, D. B. et al. Radiation Oncology Quality Assessment Tool: A proposal for a new audit tool in modern radiation oncology. J. Med. Imaging Radiat. Oncol. (2019). doi:10.1111/1754- 9485.12928
Volume 16 No 3 I June 2020 49 Radiation Oncology
Prostate Cancer Outcomes Registry
The Prostate Cancer Outcomes Registry-Australia and New Zealand (PCOR-ANZ) collects information on the patients, the care provided, and the patient-reported outcomes for men diagnosed with prostate cancer in Australia and New Zealand.
The registry is endorsed by the College alongside the Royal College of Pathologists of Australasia (RCPA), the Urological Society of Australia and New Zealand (USANZ), Cancer Council Australia, the Medical Oncology Group of Australia (MOGA) and the Société Internationale d'Urologie (SIU).
Clinicians, researchers and men affected by the disease are working together to improve the wellbeing of those diagnosed and living with prostate cancer.
So far, tens of thousands of men have contributed to PCOR-ANZ and this number is continually growing with coverage of prostate cancer patients on the registry now over 50 per cent bi-nationally.
PCOR-ANZ Impacts
1. REDUCE VARIATION: Reduce the current variation in treatment and outcomes, by benchmarking outcomes that matter to men
2. PROVIDE INFORMATION: Provide helpful information to men about the risks and benefits of different treatment options available
3. SUPPORT RESEARCH: Support research to advance the treatment options for men diagnosed with prostate cancer
PCOR-ANZ annual report 2019
The report is now available online: www.prostatecancerregistry.org/ publications/newsletters-annual-reports/ This will be of interest not only to Fellows who look after men with prostate cancer, but also other members
INFOGRAPHIC: HOW PCOR-ANZ WORKS
PCOR-NT 2016
PCOR-ANZ
Monash University Hosted at
more broadly as an example of how population-based registries can act as rapid review of patterns of care and outcome for patients we treat, benchmarking this across comparable units or clinicians.
We are currently in the first year of the registry’s plans to develop reports for specifically radiation oncologists. In the past, if radiation oncologists received reports from the registry, any modalityspecific clinical indications were on surgical management, and not so much on radiation.
This year PCOR-ANZ aims to produce bi-annual reports more specifically for radiation oncologists. This should allow radiation oncologists to gain an impression of their treatments in comparison to peers, and perhaps stimulate reflection and qualityimprovement efforts.
Professor Jeremy Millar Governance Group and FRO Representative PCOR-ANZ
The map shows the jurisdictional registries that contribute to PCOR-ANZ and the year they were first established. Each jurisdictional registry runs its own database and is responsible for its own governance, data collection and data integrity.
SA-PCCOC
APPROVED BY JURISDICTIONAL ETHICS COMMITEES
PCOR-ANZ has been approved by an overall ethics commitee, as well as one from each jurisdiction and by the Aboriginal Health and Medical Research Council Ethics Commitee. Each ethics committee has approved an opt-out recruitment approach.
DATA SECURITY AND DATA QUALITY
PCOR-NZ 2016
GOVERNANCE BY STEERING COMMITEE
PCOR-ANZ is overseen by a Steering Commitee that is responsible for how data is collected, stored and used for quality improvement at a bi-national level. They meet four times a year.
Data security: Data are collected in each jurisdiction
records
Established with funding from Movember in 2012, PCOR-ANZ is a federated, bi-national registry. Previously existing clinical registries and newly established registries all periodically send their data through to PCOR-ANZ.
RUNS WITH HIGH-LEVEL SECURITY AND A STANDARDISED DATA DICTIONARY
Stored on Monash University managed secure and resilient infrastructure located in Australia that compiles will all applicable data protection standards and privacy obligations.
across all jurisdictions. To ensure this occurs, PCOR-ANZ has a ‘data dictionary’ which describes and clearly defines each data element, including when it is to be collected; and how it is to be recorded.
Radiation Oncology 50 Inside News
APPENDIX
APPENDIX
TABLE A2: TOTAL NUMBER OF PARTICIPATING SITES WITHIN EACH JURISDICTION BY NUMBER OF PUBLIC AND PRIVATE SITES Jurisdiction Total no. recruiting sites PUBLIC sites recruited PUBLIC % of total PRIVATE sites recruited PRIVATE % of total ACT 7 2 29% 5 71% NSW 42 35 83% 7 17% NT 3 2 67% 1 33% NZ 30 18 60% 12 40% QLD 49 12 24% 37 76% SA 18 8 44% 10 56% TAS 8 2 25% 6 75% VIC 87 53 61% 34 39% WA 0 0 0% 0 0% Total 244 132 54% 112 46%
2
3
from medical
pathology
and directly
records,
1998 PCOR-QLD 2016 NSW-PCCR 2015 PCOR-VIC 2008 PCOR-ACT 2016 PCOR-TAS 2016
Release of Treatment Planning System: Eclipse™ v16
Driven by its Intelligent Cancer Care approach in developing new solutions that use advanced technologies like machine learning, Varian has announced the newest release of its treatment planning system, Eclipse™ v16. This new release includes intelligent features such as RapidPlan® PT, the first clinical application of machine learning in proton treatment planning, and RT Peer Review, which is a collaborative workspace designed to streamline and accelerate the peer review process for radiotherapy treatment plans.
Previously only available for photonbased radiotherapy treatment planning, RapidPlan is knowledgebased treatment planning software that enables clinicians to leverage knowledge and data from similar prior treatment plans to quickly develop highquality personalized plans for patients. This knowledge-based planning software is now available for proton treatment planning with RapidPlan PT. The software also allows dose prediction
with machine learning models that can be used as a decision support tool to determine which patients would be appropriate for proton or photon therapy. Varian is the first vendor in the industry to offer machine learning capability in both proton and photon treatment planning.


"With the number of operational proton treatment rooms continuing to increase, there is a need for experienced proton therapy clinicians," said Kolleen Kennedy, chief growth officer, president, Proton Solutions, Varian. "RapidPlan PT helps bridge the learning curve, allowing established centers to share their models and clinical experience. The machine learning in RapidPlan PT has the potential to reduce proton treatment plan optimization from a one to eight-hour process, as reported by
clinical proton centers, to less than 10 minutes, while also potentially improving plan quality."
In many radiotherapy departments, radiation therapy peer review meetings have been routinely integrated into the clinical QA process for safer health care delivery for the patient. Although the relevant patient information is manually retrievable from the clinical database, there is currently no efficient and effective platform to support these peer reviews. The RT Peer Review feature in Eclipse v16 is designed for the oncology community to seamlessly integrate this review process into their normal clinical workflow by automatically presenting the necessary information that is required for peer review.
"With the number of operational proton treatment rooms continuing to increase, there is a need for experienced proton therapy clinicians."
Advertorial
2020 CPD Changes Reminder
As the pandemic continues to evolve, both the Medical Council of New Zealand (MCNZ) and the Medical Board of Australia (MBA) have acknowledged that COVID-19 work will impact on the ability of all doctors to maintain CPD requirements in the coming months.
The College has made changes to the 2019–2021 CPD requirements to align with the MBA and MCNZ decisions.

Radiation Oncology
• Radiation oncology members will be exempt for 11 months (or equivalent to 50 points)
• Radiation oncology members need to accrue 130 CPD points by the end of 2021
• There are no annual requirements for a minimum number of CPD points to be met in 2020 or 2021
Clinical Radiology
• Clinical radiology members will be exempt for 11 months (or equivalent to 55 points)
• Clinical radiology members need to accrue 125 CPD points by the end of 2021
• There are no annual requirements for a minimum number of CPD points to be met in 2020 or 2021
The College will not be conducting its annual compliance audit on CPD for 2020.
While we recognise there is disruption or cancellation of many educational events scheduled in 2020, we encourage members to bear in mind that if you are undertaking any type of CPD activities, you are still able to log these in the learning portal and they will still count toward your triennium total.
The Royal Australian and New Zealand College of Radiologists®
CHANGES TO YOUR MEDICAL REGISTRATION REQUIREMENTS
ARE YOU PREPARED?
The MBA are changing their registration requirements for doctors.
The changes will transform the way you maintain your medical registration by shifting the focus to tailored professional development activities, that aim to enhance patient safety.
Find out more: www.ranzcr.com
Some examples include web-based learning, participation in clinical meetings, teaching, journal reading and research, to name a few.
If you have any questions about the revised CPD requirements for 2020, please contact the team via cpd@ranzcr.edu.au
52 Inside News Education
Professional Development Remediation Wellbeing
Kia Ora. In the usual course of things, I would be starting this article with a bit rugby banter or sharing my enthusiasm for Liverpool FC. It’s been a disappointing year for sports fans. But it certainly isn’t disappointing that New Zealand has been so successful at minimising the rate of infection for COVID-19.
I hope this article finds you, your family (especially those overseas), and your colleagues safe and well.
COVID-19: impact on practice
It was quickly apparent once New Zealand entered Level 4 Lockdown that patients were staying home, referrals were not happening and hospitals were using all resources to prepare for a wave of patients (which, thankfully, never came). As non-urgent radiology services were deferred, NZ’s radiologists twiddled their thumbs.
In response, the College prepared a position statement: Patient Access to Imaging Services in New Zealand— During and After COVID-19 Social Distancing. The Statement was shared widely with stakeholders, the media and is on the College website.
The responses were positive but did not result in a rapid reconsideration of the volume of patient care that was being deferred.
I remain concerned about the preCOVID-19 burgeoning waitlists that have further escalated and the patients whose delayed diagnosis and treatment may result in less than optimal outcomes.
New Zealand Branch News
It is now hoped that all radiology resources can be used to clear the backlog as efficiently as possible.
As I write this, Level 2 has only just begun. The guidelines for Level 2 suggest that business-as-usual patient care can resume as long as patients are screened for COVID-19 and appropriate safety protocols are used. I encourage my colleagues to follow these protocols—radiology services should remain vigilant to avoid a new outbreak, however unlikely that may seem.
The training year
There have been significant challenges for RMOs this year. I have heard plenty of feedback about how well the trainees are doing and am grateful for the efforts of DoTs and supervisors who have worked hard to make sure training is not compromised more than necessary.
The DHBs have cancelled the current round of rotations and have deferred recruitment of registrars and house officers. It is understood the medical schools may not be able to graduate their students in time for the usual start of the PGY1 year in December.

Registrar recruitment 2020
Regardless of when they will start, the College closed recruitment for registrars on 6 May. I’m pleased to report that we received a larger number of applications than we usually do for both radiology and radiation oncology.
The College is currently preparing for interviews in a COVID-19 environment. Once the plans are in place, they will
be formally communicated to the candidates and the training sites.
I understand the networks and the Wellington office have already been working through the options and drafting up the plans.
2020 election
COVID-19 has almost pushed the September election off the radar. We still intend to engage with the political parties about their election platforms and the issues that are important to the NZ members. Discussions so far have indicated a shared desire between radiation oncology and radiology to focus on issues of workforce, infrastructure and technology.
Once the formal documents are finalised, they will be posted on the College’s website.
If you do wish to discuss any particular issue with myself or College representatives, please email nzbranch@ranzcr.org.nz
News Volume 16 No 3 I June 2020 53
Dr Gabes Lau
Interventional Radiology Society of Australasia (IRSA) Update
IRSA ASM 2020
The IRSA Executive have been monitoring advice provided by Government officials regarding restrictions in light of the COVID-19 virus.
It is with the best interest of public health in mind that we have made the difficult decision to cancel the 2020 IRSA ASM and, in partnership with the Cardiovascular and Interventional Radiological Society of Europe (CIRSE), cancel the Australian and New Zealand sitting of the European Board of Interventional Radiology (EBIR) scheduled to take place in Queenstown in August.
We wish to acknowledge the time and effort put in by the 2020 ASM Convenors, Prof Tim Buckenham and Dr Gabes Lau.
Virtual AGM
IRSA will be holding the 2020 AGM virtually in August this year. Further details on this, including a date for the meeting will be available shortly, with members requiring 21 days’ notice of an AGM.
2021 ASM
Plans for the 2021 ASM are well underway. We are excited to announce that the meeting will be held on the Gold Coast in early July and the two appointed Convenors are Muddassir Rashid and John Grieve.
Junior Committee Member
The IRSA Executive are pleased to invite Expressions of Interest (EOIs) for the position of IRSA Junior Committee Member. This is a new position that has
been created to involve current junior members in contributing to the work of the society.
The position would suit a RANZCR Fellow who has not yet attained their EBIR but wishes to pursue Interventional Radiology as a specialisation. For more information on this role, please contact the IRSA secretariat at secretariat@irsa.com.au
IRSA Branch Education Dinners
Due to COVID-19, all IRSA Branch Education dinners are currently postponed. The dinners will be reinstated as soon as the ban on public gatherings is lifted. If you are interested in attending or holding an IRSA Education dinner in your state, we encourage you to contact the IRSA secretariat on secretariat@irsa.com.au
The Australian and New Zealand Society of Neuroradiology (ANZSNR)
In late 2019, RANZCR informed its affiliated societies that it was no longer able to provide financial and membership management services. Therefore, the ANZSNR Executive has appointed new service providers to support the society, including financial services support, new secretariat support (with a strong background in our profession).
We have developed a new system for subscription payments, which allows members to pay their subscriptions directly through the ANZSNR website. Our new contact details are:
Ph: +61 2 8074 1181
Email: Bianca Heggelund at secretariat@anzsnr.org.au
2020 ASM
The 2020 ASM was held at the Howard Smith Wharves in Brisbane from 12–15 March 2020. The ASM was very well attended and a huge success. The ANZSNR Executive and Council would like to extend a big thank you to the conveners—Dr Kate Mahady and Dr Jennifer Gillespie—for organising an excellent meeting.
2020 AGM
The ANZSNR AGM was held on Saturday 14 March. Thank you to everyone who attended.
Dr Christen Barras was ratified as the South Australian Council Member, we would like to formally welcome Christen to the Council.
A formal Head and Neck/ENT position on Council was ratified. This will be occupied by Dr Jennifer Gillespie who was previously co-opted to Council.
2021 ASM in Queenstown, NZ
The plans for the 2021 ASM are well underway. Dr Ben McGuiness, from Auckland, is the Convener and the Millennium Hotel in Queenstown is the chosen venue.
The ASM will run from Thursday 11 March till Saturday 13 March 2021. Three international speakers have been invited: Dr Adam Arthur (Memphis, USA, INR), Dr Wende Gibbs (Phoenix, USA, Neuroradiology) and Prof Larry Ginsberg (Houston, USA, Head and Neck).
Conjoint Committee for Recognition of Training in Interventional Neuroradiology (CCINR)
Prof Alan Coulthard has stepped down as the ANZSNR representative on the CCINR. He is replaced by Dr Tim Phillips. The ANZSNR Executive and Council would like to extend thanks to Alan for all his hard work and contribution to the CCINR over the years.
54 Inside News News
Abdominal News
Abdominal Radiology Group of Australia and New Zealand (ARGANZ)
The ARGANZ executive was disappointed to cancel the 2020 ARGANZ meeting scheduled for March this year. We had record registrations of over 360 delegates and were all excited by the program and chance to catch up with colleagues. We are delighted many of the scientific posters were delivered online and can still be viewed on our website: www.arganz.org
The 2021 meeting will now be held in Brisbane, with further details regarding international speakers to be confirmed in the post COVID-19 world. It will once again be a stimulating program.

During the past year ARGANZ has been busy focusing on our three pillars of Education & Research, Collaboration and Advocacy.
Past meeting lectures continue to be popular, including the time limited access to European Society of Gastrointestinal and Abdominal Radiology (ESGAR) e-learning.
We have added a wider range of scan protocols and published a list of abdomino-pelvic fellowships available
across the two countries. To further support our members, ARGANZ is pleased to announce education and research grants, which will be available from the second half of 2020. Follow us on Facebook and Instagram for updates.
Over the coming year we will be developing focus groups within ARGANZ to connect people who have interest in areas including research, particular diseases and techniques.
This will make it easier to share ideas and to assist in advocacy where ARGANZ provides feedback to RANZCR and other groups. A recent successful example was the bringing together of radiologists from within and outside ARGANZ to create an ARGANZ position statement on the use of CTC in Covid-19.
We are currently working with RANZCR, the Gastroenterological Society of Australia (GESA) and the Colorectal Surgical Society of Australia and New Zealand (CSSANZ) to push for broadening of CTC Medicare eligibility. Please contact us at admin@arganz.org if you are interested in becoming involved.
2020 has seen further discussion with the Society of Abdominal Radiology (SAR) on ways to collaborate. One opportunity is to involve ANZ radiologists in the SAR ‘Disease-Focused Panels’, which currently include representatives from other continents.
I would like to sincerely thank the executive; Joe Feltham, Sonja Gustafson, Gabes Lau, James Seow, Sarah Skinner and Tom Sutherland, for their tireless work in ARGANZ matters. It has been a great privilege to serve as Chair of ARGANZ for the last three years and see the group continue to grow. A/Prof Tom Sutherland will become the new Chair on 1 July 2020 and I wish him the very best.
Dr Kirsten Gormly, Chair ARGANZ
News Volume 16 No 3 I June 2020 55
Education & Research • Collaboration • Advocacy
New Rewards for Members
Unsworth Legal Free Duty Solicitor Service for Australian Members

The College is committed to supporting members both personally and professionally during this period of uncertainty.
We recognise that some of you may have questions or concerns relating to your employment and workplace arrangements as a result of the COVID-19 pandemic
We have therefore partnered with Unsworth Legal solicitors to provide you with access to free legal advice in this and other areas.
Unsworth Legal is a law firm based in Sydney with particular experience in providing legal services to medical practitioners.
This duty solicitor service, which will initially run as a pilot program until 31July 2020, entitles all Australian College members to a free 30 minute confidential telephone consultation with an Unsworth Legal solicitor in relation to any of the following legal issues:
• employment issues and workplace disputes
• enquiries from Medicare about billing
• complaints about professional practice.
To access the offer visit the Unsworth Legal web portal: www.unsworthlegal.leapweb.com.au/ and complete the enquiry form, providing a summary of your enquiry and identifying yourself as a College member. Unsworth Legal have committed to contacting you by email within one business day to schedule a time for your telephone consultation.
BUPA Corporate Health Insurance

Bupa’s goals align with our goals—they are committed to helping people live longer, healthier, happier lives, with a focus on preventative health.

Bupa Corporate offers considerable health cover savings on member's corporate private cover. Their aim is to give you better, smarter, and more flexible cover options from day one.
We have worked together to create an exclusive offer tailored specially for members.
Bupa Corporate are offering members:
• a discount of four per cent on Health Insurance
• the waiving of two and six month waiting periods on selected Extras when you combine Hospital and Extras cover—giving you immediate access to general dental, optical, physiotherapeutic, chiropractic services and more
• no waiting periods for services you were covered for with your previous health insurer
• a range of other discounts and benefits.
We encourage you to compare your health plan with Bupa Corporate’s offer for members. Note that terms and conditions apply.
Call 134 135 and quote RANZCR ID# 2133228
General Interest 56 Inside News
Radiology and the Confidence Question

Strictly
Anecdotal Evidence from the Sub Editor
Only three days into my new publications role at the College, I (very) unfortunately was hit by a car on a pedestrian crossing in a blink-of-an-eye accident which could just have easily not happened. I was collected from the kerbside by ambulance and whisked to St Vincent’s Hospital, Darlinghurst and… scanned. First by CT scan, then by X-ray. When I came to from the effects of ketamine and morphine administered at the scene, I very gradually and haphazardly pieced together my new and radically altered reality. But what really defined that reality for me was the results of the scans. I learnt that my injuries were confined to my leg, in essence.
could discern or what I was experiencing during that time I would have been considerably more scared and anxious. Which is not to say I wasn’t scared and anxious at all. I was, and this is precisely my point: it was the radiology which allowed me to both frame and manage that fear and anxiety, which gave me a measure of confidence.
The X-ray taken on admittance guided the surgeons while they performed what was, for them, a routine operation and anything but for me as it was my very first experience of a trifecta of a broken bone, surgery and a hospital stay. The follow-up X-rays initially showed non-union of the bone and then gradual union as well as a seemingly astounding amount of titanium and a worrying number of fragments which still looked distinctly out of place.
Once again, the anxiety induced by non-union—all the what ifs and if nots— was answered by the consequent X-ray where a small, slightly darker smudge indicated some healing. Or, at least, so I was informed. I myself would not have read it as anything particularly spectacular or noteworthy. But it was a smudge I came to appreciate.
My most recent X-ray (my last for at least three months) was easier to read for
me, as I was able to see it side by side with the previous one and compare the differences. I could see the changes and it only further assuaged any lingering doubts I had about using my leg as normally as possible.
All the scans in the course of my recovery functioned as touchstones of fact in a kind of sea of uncertainty, providing much-needed confidence in a new actuality where I could no longer have confidence in my leg to do what it had always done.
It may well have been excessive in terms of background research for joining the College (!) but I do now have very particular, first-hand experience of the fundamental role radiology can play in treatment and recovery.
It goes without saying that I give heartfelt thanks for the efforts of all the medical staff at St Vincent’s: ambulance officers, radiologists, orthopaedic surgeons and last, but most certainly not least, the heroic nurses who are often on the receiving end of the understandable anxiety experienced by patients and expressed in various ways.
I was shown exceptional care and support as an in-patient and outpatient within a healthcare system that delivered.
It was this knowledge—that I didn’t have spinal or brain damage, that I had sustained a broken femur which, while a major injury, was fixable—that calmed me down and brought me out of shock.
This knowledge, gleaned from the scans, delivered the basic confidence which allowed me to withstand the following six months of pain and discomfort, particularly at times when all external indicators seemed to point in a different direction. Had I relied solely on what I
General Interest Volume 16 No 3 I June 2020 57
“Which is not to say I wasn’t scared and anxious at all. I was, and this is precisely my point: it was the radiology which allowed me to both frame and manage that fear and anxiety, which gave me a measure of confidence.”
~ In Memoriam ~
The College notes with regret the death of the following member:
Dr James Moore, Fellow, QLD
Cardiac CT Training 2020
We go beyond simply meeting training requirements:
l Maximum allowable course based live and library cases for ANZ credentialing.
l RANZCR accredited for 117.5/67 CPD points (Level A/Recertification).
l Officially sponsored and endorsed by GE Healthcare for more than10 years.

l Live scanning at second highest global recruiting site in SCOT-HEART study.
Correction: In the March 2019 edition of Inside News, on the basis of information received, Dr Neville Myers, Fellow, SA was incorrectly noted as deceased. The College apologises unreservedly.
l Unrivalled venue - ICC, Darling Harbour, Sydney
2020 COURSE DATES:
5 Day Level A Course
8th - 12th October 2020
5th - 9th November 2020
3 Day Recertification Course

10th - 12th October 2020
7th - 9th November 2020
For more information and online registration log on to: www.aicct.com.au or contact us at: info@aicct.com.au
13 & 14 FEBRUARY 2021
The Division of Medical Imaging at Flinders Medical Centre will offer a two day Pathology Course, consisting of lectures and “pots” sessions to be held on Saturday 13 and Sunday 14 February 2021 at the Adelaide Convention Centre.
The course will be of particular value to registrars and candidates preparing for the Part II FRANZCR examination. It will also provide an overview of pathology for practising radiologists who are encouraged to attend.
Closing date for registrations is: Monday 30 November 2020
For registration form and further information please contact Helen Sainsbury: helen.sainsbury@sa.gov.au / (08) 8204 4405
58 Inside News
UA S T R ALIANINSTITUTE OF CARDIOVASCU L A R TC A I CCT
FLINDERS MEDICAL CENTRE PATHOLOGY COURSE
Intensive MRI Courses M ELBOURN E
All Intensive Pelvic and MRI Courses incorporate a comprehensive range of real patient MRI examinations with pathological correlation.
PELVIC MRI
An outstanding faculty of internationally recognised experts in Rectal / Prostate / GYN MRI will lead these intensive, hands-on interactive Pelvic MRI Courses.
BREAST MRI
Since 2010 the Intensive Breast MRI Course has been the leader in utilising the latest technology to provide an intensive hands-on course which also includes a large number of Abbreviated MRI
Course Director: CLAIR SHADBOLT
Director of Training, Imaging Department
The Royal Women's Hospital
Course Director: ALLISON ROSE
Head, The Royal Melbourne & The Women's Hospital
FURTHER DE TAILS & REGISTRATION

w w w.tniaustralia.com | Phone:
+61 418 51 5090
Harnessing the enormous computational power of a Deep Convolutional Neural Network (DCNN), Advanced intelligent Clear-IQ Engine (AiCE) is trained to differentiate signal from noise, so that the algorithm can suppress noise while enhancing signal. Because it is trained with advanced MBIR, it exhibits high spatial resolution and our best low-contrast resolution, ever1. But unlike MBIR, AiCE delivers natural image noise texture and fast image reconstruction for seamless clinical adoption.

AiCE is now available on the following systems



 0.5mm AiCE
CAP acquired at CTDIvol 2.9mGy.cm / DLP 195 mGy.cm
0.5mm AiCE
CAP acquired at CTDIvol 2.9mGy.cm / DLP 195 mGy.cm
Intelligence
Using Artificial Intelligence to set a new standard for CT image quality.
Artificial
11.5mm @ 0.3%, 22 mGy 160
World’s 1st Deep Learning Reconstruction for CT
0.5mm Hybrid IR









































































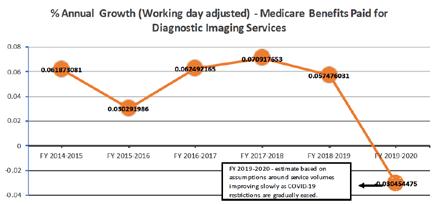





































































 0.5mm AiCE
CAP acquired at CTDIvol 2.9mGy.cm / DLP 195 mGy.cm
0.5mm AiCE
CAP acquired at CTDIvol 2.9mGy.cm / DLP 195 mGy.cm