






A Message from the President: Haves and Have-nots in a Lucky Land
A Message from the CEO: Looking Forward to Seeing You All in Person
8 13
10
5 22 24
Passion is Infectious: An Interview with A/ Prof David Kok
RANZCR Trailblazers: Remarkable Careers
Photon-Counting CT: A Leap from Black & White TV to Colour HDTV
Volunteers in the Spotlight: Dr Xavier Yu
Impact of RANZCR Radiation Oncology Research Grants
27 28
29 33
Professor Sandeep Bhuta Wins Second Prestigious American Award
Dr Sanjay Hettige wins AMA’s Doctor in Training of the Year Award
Targeting Cancer Fun Run Returns
Vale Dr Jann Medlicott
Chief Censor for the Faculty of Clinical Radiology: Developments in Training
Accreditation: What Does this Mean to Us?: A Message from the FRO Dean
Chief Censor in Radiation Oncology: Training, Accreditation and Examinations
What are your thoughts?
Our ASM through the Archives
RANZCR Workshops, Courses and Events 2022
Cultural Safety and Cultural Competency Resources
Digital Health: A Message from the FCR Dean
If you have thoughts or comments about one of the stories you have read in this issue, we want to hear from you. The submission of letters to the editor, articles and news items is encouraged. Please email any submissions to editor@ranzcr.edu.au
Radiation Oncology Trainee Committee: Unlearning Helplessness
35 61 18 38 37
43 49 51 41
53 56 63
55
Chief of Professional Practice for the Faculty of Radiation Oncology
Quality Corner Standards of Practice for Interventional Radiology and Interventional Neuroradiology New Zealand Branch News
Have you moved recently?
Log into the MyRANZCR portal and ensure your contact details are up to date at www.myranzcr.com

In this edition, I want to canvass several issues to do with our place in society and the moral obligations that attach to us and our colleagues across medical practice. The thread which runs through each issue is generally one of community service, that is, how we perceive ourselves in relation to the various communities we choose to serve.

The media recently ran a story on the average incomes of the Australian workforce, notably concerning our most well-off, by occupation and location, and, predictably, the tax that a few avoid.1 As slanted as some of the coverage has been, the underlying statistics to this story are worth a few minutes of reflection.
According to the ATO's analysis of the nation's annual tax returns, the highestearning job in Australia in 2019–2020, in terms of average total income, was that of the neurosurgeon ($576,342) followed by the ophthalmologist ($541,916), otorhinolaryngologist ($443,360) and plastic surgeon ($359,654).2
Of the 1,154 occupations listed by the ATO, diagnostic and interventional radiologists ($380,162) sit ninth on the list and radiation oncologists ($265,799) are 16th. What is most striking about this list is that medical specialists comprise 18 of the top 20 occupations, by average income, with judges (11th) and financial investment managers (19th) the only non-medical jobs among the 20.
It's a similar picture with median incomes, with judges, magistrates and MPs the only non-medical occupations
in the top 30.3 In short, doctors as a group, especially medical specialists, are the best-paid workers in Australia; they earn on average, in the case of the radiologist, almost six times the average income of the workforce as a whole. (By the way, the highest earners don't live in Sydney or Melbourne, but in Perth, where I live and work.)
So, if you saw or heard these news reports, how did you react? Did you feel a little defensive or indignant? After all, we have worked hard over many years to get to where we are, and like (almost) everyone else, we pay taxes. Why shouldn't we be well paid for the essential services we provide to society? Well, I agree with you.
Yet, if your reaction was ‘How lucky am I?’, I agree with you too. In the main we live in the best suburbs, send our children to the best schools, and often head overseas for our summer holidays (at least when COVID permits us). Not for us is worrying about how to pay the mortgage if the spouse loses their job. But money worries are a common concern for many of our patients, who
might also have to deal with some bad news about a tumour.
This is the world we live in, a world in which almost everyone else is not so comfortable, and for some it's very uncomfortable. We are, for want of a better term, the lucky ones—lucky to be born with the innate abilities to do the exacting work we do and lucky to be given the opportunities and guidance at the right moments in our lives to fulfil our potential.
For me and other volunteer members, that's a strong incentive to invest some of our good luck in public goods—for example, doing unpaid College work to help make our part of the healthcare system as good as it can be for patients. Believe me, there's plenty to do, and we could well use your input within your College in addressing critical challenges facing our way of life, and those of the people we serve.
“This is the world we live in, a world in which almost everyone else is not so comfortable, and for some it's very uncomfortable. We are, for want of a better term, the lucky ones—lucky to be born with the innate abilities to do the exacting work we do and lucky to be given the opportunities and guidance at the right moments in our lives to fulfil our potential.”

Everlight Radiology offers a smarter way to address your work-life balance. A career in teleradiology allows you to work anywhere in the world. It’s your opportunity to spread your wings, explore life overseas and continue reporting on the most interesting emergency and trauma cases. All at a time that suits you, with no overnight shifts.






















As part of an organisation that puts clinical excellence first, you will also benefit from mentoring, continuous professional development and a dedicated support team.
Join Everlight’s growing team of Consultant Radiologists and you too could be to enjoying this rewarding way to further your career and follow your dreams.

For more information come and find us on
stand 44 at RANZCR ASM 2022, Adelaide
“ Sometimes we get our nose to the grindstone and we lose sight of the bigger picture. I’ve been very keen to improve my work-life balance. So I would recommend Everlight to anybody.”
–Consultant Radiologist at Everlight
Among the most serious—indeed existential—challenges to our way of life (I think we can give the pandemic a time-out for this quarter) is the likely impact of worldwide climate change due to greenhouse warming of the atmosphere and oceans.
The healthcare sector generates 4.4 per cent of net greenhouse gas emissions globally; if the health sector were a country, it would be the fifth largest emitter on the planet. Its contribution to greenhouse gas emissions comes from health-related energy use and transport, product manufacturing, use and disposal of waste.4 The climate crisis is indeed a health crisis
To address the concerns of our members and the medical profession over the health sector's environmental impact, the College has joined a campaign involving various Australian and New Zealand medical colleges. Led by the Royal Australasian College of Physicians (RACP), the campaign is a policy, advocacy and social media initiative to implement a national strategy on climate change and health and commit to net zero emissions in the healthcare sector by 2040.5
Among the recommendations of the RACP report is an undertaking to embed Aboriginal and Torres Strait Islander knowledge and leadership in climate health policy and implementation.
The argument made by the report's authors—and one with which I concur— is that an effective policy response to climate-related impacts on the health system needs to draw on the unique wisdom of Indigenous peoples and to adopt an approach which involves and connects in a culturally-sensitive way with this community.
We cannot begin to address meaningfully these societal challenges if, at the outset, we exclude from our planning those communities upon whom the health impacts may fall most heavily.
References
A similar argument applies to another community—the LGBTQIA+ community, which will be celebrating the World Pride parade in Sydney next year. This community is a minority that suffers disparities in health outcomes due to stigma, discrimination and denial of civil and human rights. As patients, people may not feel safe accessing health care due to a lack of trust in the medical profession and/or fear of discrimination or stigma. LGBTQIA+ physicians are likely to be under-represented in the medical workforce, which can only serve to reinforce the stigma felt by patients and worsen their health outcomes.
to advocate for the health of LGBTQIA+ people and indicate to medical students and junior doctors that the College not only welcomes but encourages aspiring radiation oncologists and radiologists in the LGBTQIA+ community to be a part of our profession.
As health professionals we we will serve serve society well and with fairness if we reflect its wide diversity and give support to all its cultural constituents. In my thinking, which I know many of you share, that's part of our job as health carers.
The World Pride parade is more than a street celebration with colourful floats and flag-waving marchers. It's an opportunity for associations such as ours to publicly demonstrate our willingness
I accept there will be members who may view this as a minority issue and others may not support the Board’s view, but as a member-based organisation our public standing is dependent on how we treat all members and recognise their views. The College has a commitment to workforce diversity, which is a key part of the Strategic Plan 2022–2024, in line with our leadership value of inclusivity. In recent times the College has come out in public support of marriage equality and has made progress in overcoming bullying, discrimination and sexual harassment towards trainees. RANZCR support for World Pride—and through the College, your support—is another important step in the march the College is making towards a better future for all our medical colleagues and the people we are sworn to comfort, treat and heal. The call I make to my fellow members to lend a hand, I make particularly to the critics of the decisions the College has taken of late. The organisation is not perfect by any means, but our volunteers and staff are doing their level best. If you count yourself among the critics, that's OK, criticism is fine, but you also need to invest a little of your time and energy into helping to make our organisation better for all, the haves and the have-nots. Think about that as you enjoy your luck.
1 For example, Nassim Khadem and Michael Janda, “The 60 millionaires who paid no tax and the richest and poorest postcodes revealed,” ABC News, August 9, 2022, https://www.abc.net.au/news/2022-08-09/millionaires-paid-no-tax-and-richest-and-poorest-postcodes-ato/101312118
2 Australian Tax Office, Taxation statistics 2019–20, https://www.ato.gov.au/About-ATO/Research-and-statistics/In-detail/Taxation-statistics/Taxation-statistics-2019-20/
3 In terms of median total income, radiologists are also ninth on the list and radiation oncologists are 27th.
4 Josh Karliner, Scott Slotterback, Richard Boyd, Ben Ashby and Kristian Steele, Health Care's Climate Footprint: How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action (Health Care Without Harm & ARUP, 2019), Climate-smart health care series, green paper no. 1, https://noharm-global. org/documents/health-care-climate-footprint-report
5 Peter Bragge, Fiona Armstrong, Kathryn Bowen, Milly Burgess, Sue Cooke, Alyse Lennox, Danny Liew, Loyal Pattuwage, Corey Watts and Tony Capon. Climate Change and Australia’s Health Systems: A Review of Literature, Policy and Practice (Melbourne: Monash University, 2021), https://www.racp.edu.au/advocacy/policyand-advocacy-priorities/climate-change-and-health
“Among the most serious—indeed existential—challenges to our way of life... is the likely impact of worldwide climate change due to greenhouse warming of the atmosphere and oceans.”
One of the best things about being CEO of the College is getting out and meeting our members at their workplaces and their regional meetings. COVID restrictions have impacted my ability to do this during my early days with the College, but with the easing of restrictions, I’ve been able to connect with members just like the ‘before-time’.
Video conferences are an excellent time- and cost-effective way to stay connected and they will remain as part of our communication landscape, but sometimes, nothing compares with faceto-face contact.
Recently I’ve been fortunate enough to attend the New Zealand ASM and Branch AGM; and visit a number of Perth hospitals and private clinics and attend the WA Branch AGM.
Thank you to all of our members who have taken the time to host me at their place of work or have taken the time to ask me questions about the College, raise concerns, or to offer a point of view on a broad range of topics. Two issues that were raised multiple times were CPD and our work with iRefer.
The Medical Board of Australia (MBA) and Medical Council of New Zealand (MCNZ) have announced changes to their CPD registration standards, to be adhered to by all colleges.

As a result of these imposed changes, the College, through the work of the FCR and FRO Professional Practice Committees have aligned the College CPD program requirements to ensure our members can meet the requirements of their medical registration.
The 2022 year has been a transition year for the College CPD program, with the introduction of a number of the new requirements for CPD as well as the new CPD ePortfolio.
This is to allow members to familiarise themselves with the new program requirements and CPD ePortfolio functionality in preparation for all regulatory requirements being mandatory from 1 January 2023. Please also be reminded that your 2022 CPD activities are due by 31 December. As the College has moved to an annual
CPD program, everyone should be recording their CPD in the ePortfolio to remain compliant. If you need assistance with your CPD, please contact cpd@ranzcr.edu.au
The CPD section of the website also has a number of resources to assist, including ‘how to’ guides and video recordings, handbooks, FAQs and general program information.
College staff are available to attend meetings with members either in person or virtually to assist. Please contact the College’s Standards team to arrange a time.
Clinical Decision Support (CDS) has been shown globally to improve patient care/safety by recommending the most appropriate imaging for a particular clinical need. It also reduces clinical variation in ordering and helps to increase the confidence for ordering and education of junior trainees. This in turn provides increased accessibility to imaging in a more timely manner for all. There are a number of guidelines developed globally that have been
“Video conferences are an excellent time- and costeffective way to stay connected and they will remain as part of our communication landscape, but sometimes, nothing compares with face-to-face contact.”
in use for over a decade, including the American College of Radiology’s Appropriateness Criteria, the European Society of Radiology’s iGuide and the Royal College of Radiologists’ iRefer
The iRefer guidelines are now in use in Canada, Poland, Middle East, Ireland, NHS Scotland and Wales; and are rapidly becoming the standard across many areas of the globe.
The College has recently reached an agreement with the Royal College of Radiologists (RCR) for the use and licensing of iRefer in Australia. It provides guidance on selecting the most appropriate imaging investigation for a range of clinical problems. Embedding iRefer into the Australian health landscape will provide the foundation for optimal patient health outcomes.
The iRefer Imaging Guidelines are based on best clinical evidence from a diverse range of sources, are validated through
an extensive network of clinical experts and subject to rigorous governance. The guidelines methodology has been accredited by the National Institute for Health and Care Excellence (NICE). This ensures that guidelines are best practice and not influenced by political or commercial factors.
With Government encouragement, the College is presently undertaking a pilot of iRefer in conjunction with the Royal Australian College of General Practitioners (RACGP), to demonstrate the benefits that imaging guidelines can bring to our healthcare system. GP feedback on this pilot will be used to inform how iRefer can support GPs to refer for the right test at the right time while still maintaining clinician autonomy for decision-making and allowing faster vetting or authorisation of orders through less order changes, cancellations or call-backs between radiology and referrers.
We are holding the 2022 Australian ASM in Adelaide South Australia, from 27–30 October. If you haven’t booked your tickets yet, time is running out.
With a thought-provoking program and strong support from industry partners, the ASM will be a showcase event for our profession to reconnect after our enforced time apart.
We will be welcoming a record number of graduates at our graduation ceremony in Adelaide, including many whose graduation ceremony was postponed due to COVID restrictions. I look forward to seeing all of you there.

“I’m extremely pleased that this video has received a Gold Award. It’s made for everyone to understand what’s the latest in technology advancement in radiation oncology space. It is a fascinating area where you can see a lot of technological enhancement happening and new enhancements for cancer treatment to improve cancer patient outcome.” A/Prof Kok
An educational video about stereotactic radiation therapy recently won a gold medal in The Telly Awards. Produced for the University of Melbourne, the video features A/Prof David Kok, radiation oncologist, who explains stereotactic radiation therapy, in an engaging and insightful way. Stereotactic radiation therapy is a highly advanced form of radiation therapy to treat cancer.
Easy to understand with ample animations and visuals, the video is a part of the development project of a cancer science degree at the University of Melbourne which aims to educate university students about the basics of radiation therapy. Driven by their huge passion, A/Prof Kok and Dr Sathana
Dushyanthen co-developed the script for the video, ensuring that it captures what’s important about stereotactic radiation therapy compared to the conventional approach.
“I’m extremely pleased that this video has received a Gold Award. It’s made for everyone to understand what’s the latest in technology advancement in radiation oncology space. It is a fascinating area where you can see a lot of technological enhancement happening and new enhancements for cancer treatment to improve cancer patient outcome.”
A/Prof Kok
The video stood out as one of the Gold Medallists in the General Training and Education Category of The Telly Awards
2022, followed by big-name runners-up including Microsoft.
We speak exclusively with A/Prof David Kok, a radiation oncologist who shares his passion for radiation oncology and cancer treatment and his behind-thescenes stories.

Why did you want to make a video about stereotactic radiation therapy? How did the idea of making this video come into being?
This video comes out of a larger project that I’m in charge of to develop a cancer science degree at the University of Melbourne. As far back as 2014, the
university had identified that there was a surprising lack of knowledge about cancer treatment and wanted to devise an education program that could address that. I was brought on to lead the project in 2017, shortly after they agreed to partner with the Victorian Comprehensive Cancer Centre to produce the degree. While the degree covers all cancer treatments, I think having a radiation oncologist in this lead role has helped to emphasise the key role we play in cancer treatment and allowed us to really highlight some of the key advances in radiation therapy that have been made in recent years. In developing material for the degree, we were mindful throughout that we’re dealing with a professional clinical audience with a lot of experience in medical education, generally speaking. This type of audience is time poor, with 100 things on their to-do lists both in their business and personal lives. As such, we had to rethink how we made and delivered all of our content!
We decided it was really important to make short, sharp educational content that could be delivered flexibly, when and where people wanted it. After all, people rarely have time for one-hour lectures anymore! In addition, we wanted to make it really engaging to compete with all of the other distractors that are present these days. There are so many options—email, Netflix, family! That’s why we ended up focusing on short, simple, and engaging videos— like this one!
Who was this video made for when you had the idea of creating such a video? Was it for medical students at the university or general public?
Well, it’s essentially made for university students and also people from a health professional background. However, I’d like to say it’s for everyone because we make sure that any educational material produced is generalisable and jargon free so that anyone can understand it easily.
This video focuses on stereotactic radiation therapy, which is a relatively new, highly advanced technology in cancer treatment. It is a fascinating

area where you can see a lot of new technological enhancement happening for cancer treatment to improve cancer patient outcomes.
What’s the purpose of this video? Would you like to inspire the university students to be interested in this profession or just build understanding of radiation therapy in general?
I think it’s both. I’m a radiation oncologist and I genuinely love the subject and the material. I personally find the delivery of radiation therapy really fascinating. There are all the technological advancements happening around in our field as well as all of their new different indications for cancer treatment. So, it’s about communicating that passion to an, as yet,
undifferentiated group of professionals. And who knows, you may find people who share the same passion with you! All of a sudden, they realise radiation oncology is really interesting and want to learn more.
In addition, there’s also a big role for building knowledge of radiation therapy and literacy in the wider health professional community. We need to raise awareness of radiation therapy because a lot of people don’t even understand the basics of it. For instance, they don’t know when’s the right time to refer to radiation oncologists or to discuss their patients with us. And ultimately that lack of knowledge impacts patient care.
continued over...“In developing material for the degree, we were mindful throughout that we’re dealing with a professional clinical audience with a lot of experience in medical education, generally speaking. This type of audience is time poor, with 100 things on their to-do lists both in their business and personal lives. As such, we had to rethink how we made and delivered all of our content!”
How long did it take you to produce this video?
It took roughly about a month. I did the initial script and then consulted others for feedback and inputs. I wanted to make sure that it included a range of opinions about what’s important about stereotactic radiation therapy. Once the script was finalised, I went to talk to the animators. Luckily, we have a very strong team for digital technology in the cancer science team who brought the idea into vision.
The Telly Awards are prestigious, and some of the winners are from big name companies. What made this video stand out to win the Gold Medal in your opinion?
I believe ultimately there are two things you really need in a good video: the first is the information presented is clear so people can understand it easily without paying too much effort.
The second is the passion behind it. You need to convey the passion. I personally love this subject, and you know passion is infectious. A part of it is that I’m just showing the fact that I love this material and here are the reasons why you should love it as well. When you’re passionate about something then people around you will feel it, and when these two things come together, you have the ingredients to make a video worth watching.
You’re a natural speaker in front of the camera. You communicate with your audience very well on the video. Can you explain why that is?
Thank you. In the past I did a teaching degree as well as medicine, so I have a little bit of theory about learning styles of students and how to get them engaged on screen. I suppose that bringing that lens to it gives you some insight into what’s the appropriate way of wording things so you can better present your information, and how to move between different types of aspects of the screen. Little things like whether the camera should be focused on the presenter or the content at a specific time.
All of those things have a subtle effect that is hard to measure but will make a difference to the ways your audience understands the information you’re presenting. But I won’t pretend I’m perfect either—every professional speaker I’ve met is constantly trying to watch how others do it and improve their technique, and I’m no different!
Do you have a behind-the-scenes story to share with us from the video shooting process?
I do have one that you might like! We actually wrote a full script for the video and had a teleprompter, so you know what you’re going to say in advance. But on the shooting day the teleprompter wasn’t working, so I actually had to just go on the fly. During the recording process, a few parts took a couple of takes, but now looking at the final video, I think it actually made it a better video, a more natural one.
At the end of the video, you encourage your audience to go for a Nobel Prize. Can you elaborate your message here?
I think it’s always important for students to understand that we’re not at the limits of knowledge. There are a lot of things to learn and in the next decade there will probably be further huge steps forward that are going to revolutionise what we do.
The section you’re referring to is where I showed some PET scans that demonstrate the interaction between radiation therapy and immunotherapy. From time to time, this results in a phenomenon where the radiation triggers a widespread tumour response outside of the radiation field. This is called the “Abscopal Effect”, and in my opinion is a huge frontier for cancer care. A better understanding and leveraging these types of biological interactions between radiation and cancer will really move us forwards as a specialty. I was hoping to explain this, and at the same time try and stimulate the viewers’ sense of excitement about where the field is going.
Do you have any words to students, radiation oncology trainees, and health professionals in general?
Radiation oncology is an amazing field which has so many different possibilities lying ahead of us. I think that they're only limited by firstly imagination and secondarily the drive and passion to do so.
I suppose I hope that my own passion within education will remind people of that and to look to the horizon. There are really big opportunities for our radiation oncology profession.
“I think it’s always important for students to understand that we’re not at the limits of knowledge. There are a lot of things to learn and in the next decade there will probably be further huge steps forward that are going to revolutionise what we do.”
“Radiation oncology is an amazing field which has so many different possibilities lying ahead of us. I think that they're only limited by firstly imagination and secondarily the drive and passion to do so.
I suppose I hope that my own passion within education will remind people of that and to look to the horizon. There are really big opportunities for our radiation oncology profession.”
We continue our RANZCR Trailblazers series with more excerpts from the oral history interviews made in 2016 by the then College archivist, Ms Eva StokesBlake.

In this edition, read on for more insights and recollections from Professor Lesley Cala and past presidents Dr George Klempfner.
In these excerpts we see where a career in radiology or radiation oncology can take you and the breadth of life experience and practice opportunities offered. Many and varied interactions with colleagues, fellow researchers, patients are recounted as particularly life-enhancing.
We see where these trailblazers have seized opportunities, dealt with setbacks including the experience of being both doctor and patient, and sometimes made their own luck.
We see also the sheer range of clinical advancements over the years and the advances in teaching and examining.
As Dr George Klempfner puts it, “To my non-medical friends who play golf, I say, I don’t need to play golf, I can stick needles in things and enjoy the accuracy with which I can do that. I think that’s far more useful than and just as enjoyable as playing golf.”
We thank Eva Stokes-Blake for her invaluable work in amassing oral histories for future generations of radiologists and radiation oncologists. We would also like to invite your expressions of interest to actively participate in clinician-to-clinician interviews of RANZCR Trailblazers (of your nomination), more details are available via editor@ranzcr.edu.au. Interviews can be made face-to-face at RANZCR2022 ASM or now in your home city or via an online meeting.
Access the full recordings from the three interviewees for much more detailed history of the professions and the College here: www.webcast.ranzcr.com/ Mediasite/Showcase
We hear first from Professor Lesley Cala on a few of the clinical advancements that benefited patients and clinicians.
She was later put in charge of radiography at St John of God in Bunbury. I taught other radiologists the technique, including the late John Kennedy at Princess Margaret Hospital for Children and Trevor Apsimon at RPH, during 1971.
You have the honour of being the first radiologist in Australia to perform spinal angiograms and orbital venograms. Could you please share your memories from these days?
The first orbital venogram was performed in 1971 at St John of God Hospital (STGH), in Belmont, which is a suburb of Perth, and published with additional cases in Australasian Radiology March 1972. My radiographer was a very enthusiastic nun who was thrilled to be involved with the case.
”Spinal angiograms were learned in Paris from René Djindjian at the Hôpital Lariboisière and performed by me at Sir Charles Gairdner Hospital in 1973. The patient had a vascular malformation around the spinal cord which was causing backache and he was troubled
also with infertility. Safe corrective surgery to the malformation was then possible because the surgeon could identify the feeding arteries and draining veins pre-op and plan accordingly.”
It was very useful to show a surgeon pre-op the full extent of venous malformations in order to decide if the operation had anything to offer, without damaging the optic nerve.
Spinal angiograms were learned in Paris from René Djindjian at the Hôpital Lariboisière and performed by me at Sir Charles Gairdner Hospital in 1973. The patient had a vascular malformation around the spinal cord which was causing backache and he was troubled also with infertility. Safe corrective surgery to the malformation was then possible because the surgeon could identify the feeding arteries and draining veins pre-op and plan accordingly.
Would you like to share any other memories specifically regarding the development of radiology equipment and technologies?

My initial carotid angiograms in 1966 were by direct puncture of the artery in the neck and the films were handpulled through a cassette holder. It was essential to have good co-operation between the radiographer and myself because only four films could be taken. The radiologist had to call ‘shoot’ which coincided with the injection of 10 mls of contrast and the first film of four being taken. After that the radiologist had to call ‘pull” three times for the radiographer to first take an exposure and then remove the cassette to leave the next one ready to be exposed.
If both carotid arteries had to be examined, one pressed on the first one to achieve haemostasis and then went ahead and punctured the other side. One was always on the look out for the first side starting to bleed while the needle was still in the second side, or after an anaesthetist had removed the endotracheal tube!
With the development of image intensifiers and the Elema Schönander automatic film changer in 1962, it meant that more than four films could be taken and the machine took over “calling” the orders. Also at that time, RPH commenced to use the Seldinger method (started in Sweden in 1956) which consisted of introducing an arterial catheter in the groin, instead of puncturing the neck, and following it up to the aortic arch to catheterize carotid and vertebral arteries.
Air encephalograms and myodil ventriculography had been accomplished with difficulty prior to the use of image intensifiers in 1964. However, the major advance for both procedures was when STGH purchased a MIMER 3 ensemble in 1973. This had a chair attachment to the table, with an open back to allow the lumbar puncture with the patient sitting upright and then it was possible to rotate the patient, still strapped safely into the chair, forward and back to fill selective parts of the ventricular system.
It was a horrible procedure giving the patient a severe headache and they might vomit for a few days. Within one week of seeing what the CT scanner could show in 1975, this procedure was not ever done again by me.
“It was a horrible procedure giving the patient a severe headache and they might vomit for a few days. Within one week of seeing what the CT scanner could show in 1975, this procedure was not ever done again by me.”
I don’t know if you have a lot on Professor Hare in your archives but there is this story about him that he, I think, topped his year in medicine. He then developed tuberculosis and he was close to death and one of the first people treated with streptomycin which had just come in as a treatment for TB. So his life was saved but he had a lot of problems from, for instance, a fused shoulder, because he had tuberculosis of the shoulder, and when he recovered his doctor said ‘look, you’ll have to lead an easy life, you can’t become a physician as you wanted to or a surgeon, you can either become a dermatologist, a pathologist or a radiologist’ at that time, a radiologist was a rather boring profession, and in his words, he thought ‘I may as well shoot myself’. Anyway, it was not so at all and he started in a profession which has really blossomed and became one of the most interesting parts of medicine.
I regard him as one of the most important mentors in my life and I admired him very much.
In this life you have to be lucky and I’d just like to say I feel that in my life I have been lucky but also you have to take the chance to make your luck.

I realised that as a wealthy country we had resources here which we should try and make available to the people in the South Pacific; places like Fiji, Western Samoa, Tonga and even smaller places like Niue and so on, so we set this committee up and we arranged that people from radiology and radiography, cause some of these islands are so small they don’t have a radiologist, would come to our College meeting, we also arranged for radiologist to come to departments to further their education, we also brought education resources to the island. That was something I felt we really helped people and I really enjoyed the interaction between us and them. I was sent (to Samoa) as a result of my involvement with the ISR because it was a project I was sent on with World Health, so I did a report for World Health on Western Samoan radiology. My wife came with me and we were housed at a hotel called Aggie Greys, Aggie Greys is the only hotel virtually on the island and it’s quite famous in fact it features in a book by Somerset Maugham in a very famous short story called Rain, which I had read. When I arrived there, I realised there was only one radiologist on the island, Veni Siva, and when he was away no radiology got performed, there was nobody else to take over from him. He did all the reporting, he didn’t have a dictaphone, he handwrote his reports. And there was another strange system there where an X-ray cost very little, just a few dollars, but the system was, you could have as many X-rays as you wanted. So when a patient was referred for an X-ray of the chest, the referring doctor would say, ‘oh and X-ray his skull, he’s had some headaches as well’ and things like that. I think the companionship one gets as a councillor was great, you know, I have been on a lot of committees before and since and there is a sought of comradery and unity of purpose that I found amongst most of the councillors and I can’t really remember really very many angry words at any stage and I was on council a long time and I really enjoyed the companionship, the comradery, the unity of purpose. With the presidency I felt very privileged to be the president and feel very lucky as I was president in the year of the Rontgen centenary and
so not only was it being the president and having the annual meeting it was also part of the centenary which made it a very exciting year, so I enjoyed that. I also enjoyed all the friendships I made as a result of being part for just going to the meetings and part because of my position in the College. I have a lot of very good overseas and Australian friends who I have made as part of having had that position.
Initially I was an examiner in physics, and then I moved on to became an examiner for the second part. I found being an examiner was in fact incredibly invaluable because you give something to the College in all of this but you learn an awful lot, when you have to examine in something, you do your research and that you know that subject well so I found that it was educational to me.
As well as nuclear medicine, I was the director of a few places, I took great interest in mammography. I was the director of mammography at Cabrini hospital where I spent most of my time. In an effort to really excel in this, I had to join BreastScreen for a while and found that really valuable too. Because when you report to BreastScreen you get an assessment of your performance. Each case you see is recorded and any false positives or false negative you make is recorded against your name so you can quantitatively assess your performance, I found that interesting and very valuable. So really my career in radiology, like everything else, I must be a really positive person, I have really enjoyed it but it was continual learning. So one graduates, one does nuclear medicine, one does ultrasound, one learns CT. I decided MRI was one thing too many, you can cast yourself too far so while I understand the principals in MRI, I never tried to become an expert in MRI but then I performed and enjoyed mammography and also some of the more simple interventional work. I had done a bit of angiography when I worked as a register, but thought this was too specialised, you either did it full on or you didn’t. But there are other interventional procedures that the general radiologist can do safely with skill and I think I enjoyed those as much as anything else I did in radiology.
R ANZCR2022.com
2022 NISBET ORATOR
72nd Annual Scientific Meeting
27 - 30 October 2022

We’re offering a discounted kids creche service Thursday to Saturday of the ASM. Engage in a dynamic CPD program while your kids are looked after during the day!
The College’s Board establishes Special Interest Groups in areas of specific interest to the membership within clinical radiology and radiation oncology
Contact us to find out more and join a Special Interest Group www.ranzcr.com/contact
Australian and New Zealand Society of Thoracic Radiology (ANZSTR)
ANZSTR has been established to provide a networking platform for members with an interest in advancing knowledge, learning or clinical expertise in the area of thoracic radiology to communicate, meet and/or organise conferences to further this interest.
Australian and New Zealand Society for Paediatric Radiology (ANZSPR)
ANZSPR is a professional society for doctors with an interest in the medical imaging of children in Australia, New Zealand and neighbouring countries.
Abdominal Radiology Group
Australia and New Zealand (ARGANZ)
ARGANZ is a not-for-profit group uniting radiologists from Australia and New Zealand who have a special interest in imaging and image guided treatment of patients with the diseases of abdominal organs.
Australian and New Zealand Emergency Radiology Group (ANZERG)
ANZERG is a network of members interested in emergency and trauma radiology.
Australian and New Zealand Rural Radiology Special Interest Group (ANZRRSIG)
ANZRRSIG is a network of members interested in rural and remote radiology across Australia and New Zealand.
Obstetrics and Gynaecology
Special Interest Group (OGSIG)
OGSIG is a network of RANZCR members who are interested in O&G imaging. It aims to promote best practice for the performance and reporting of O&G imaging in Australia and New Zealand.
for practice in this area; and to raise the profile of brachytherapy for gynaecological cancers.
Faculty of Radiation Oncology
Lung Interest Cooperative (FROLIC)

Oncology Special Interest Groups
Australian and New Zealand Palliative Radiation Oncology Group (ANZPROG)

ANZPROG is a group of radiation oncologists who advocate and promote the role of radiation therapy in palliative care. It allows members to share the clinical experience of radiation therapy provision in the palliative oncology setting.
Breast Interest Group Faculty of Radiation Oncology (BIG-FRO)
The aims of the BIG-FRO are to promote best clinical practice for the management of breast cancer, and to enhance the profile of radiation oncology in the setting of breast cancer.
Faculty of Radiation Oncology
Genito-Urinary Group (FROGG)
FROGG aims to promote good radiotherapeutic and oncological practice as part of multidisciplinary patient management.
Gynaecological Oncology
Radiation Oncology Collaboration (GOROC)
GOROC aims to facilitate and promote best-practice radiation therapy in gynaecological cancers through establishment of clinical guidelines
FROLIC aims to facilitate best-practice radiation therapy treatment of patients with lung cancers and other thoracic malignancies (including thymic tumours and mesothelioma) with a particular emphasis on educational and quality assurance activities.
Faculty of Radiation Oncology
Paediatric Group
The Paediatric Group aims to maintain a network of radiation oncologists who manage paediatric patients in Australia and New Zealand to ensure the best quality of care by radiation therapy for children.
Asia-Pacific Radiation Oncology
Special Interest Group (APROSIG)
APROSIG aims to develop interaction with and support for radiation oncologists and their staff in Lowincome and Middle-income Countries (LMCs) in the Asia-Pacific region.
Faculty of Radiation Oncology
Particle Therapy Special Interest Group (PTSIG)
PTSIG aims to bring together radiation oncologists to investigate and promote the role of particle therapy in the treatment of cancer, to ensure particle therapy is introduced in a coordinated way through a collaborative approach –to ultimately benefit patients.
Photon-counting computed tomography (PCCT) promises to revolutionise CT imaging by substantially increasing spatial resolution and iodine contrast conspicuity, reducing radiation dose and beam hardening artifacts, and allowing spectral imaging with multiple energy bins.

Unlike traditional energy integrating detectors which use solid-state scintillators to first convert X-ray photons to light, photon-counting detectors use a semiconductor material to directly convert incoming X-rays to an electric signal in a single step. Each photon gives rise to a voltage that is proportional to its energy, allowing energy discrimination on the basis of voltage comparison. A count can therefore be assigned to the bin that matches the photon’s energy range, hence the name “photon counting”. With enough bins, one can therefore perform spectral analysis of the incoming photon flux, and extract spectral information for quantitation or material decomposition. Since lower energy photons, which produce more contrast information, get equal weighting to higher energy ones, the images have improved contrast resolution.
Prof Roland Bammer, Head of Monash University’s Department of Imaging*, describes this transition. “Remember the times when you were watching sports on a low-res black and white TV with the “bunny ears” on top? Now you can watch events in colour on your 4K TV. This is the paradigm shift in CT that’s currently happening with photoncounting. The ‘colour’ depth isn’t OLED quality yet, and more like on the old CGA or VGA monitors, but it’s there. You can do all the interesting things energy integrators can’t do without dual kV source or kV switching. PCCT does the energy discrimination on the
detector side, and opens up a new field in radiology.”
Although it has long been known that photon counting is the most efficient approach to X-ray detection for CT, developing a direct conversion material which can handle the high X-ray photon flux of CT has been the major challenge. Prof Bammer says “Whether the future of photon-counting CT will lie in cadmium telluride (CdTe), cadmium zinc telluride (CZT), or silicon (Si) semiconductors is still unclear. The jury is still out. The individual vendors seem to have made bets on different semis. Each material has its strengths and weaknesses, and the vendors have learned to leverage the strengths of their material and minimise the impact of its weaknesses. The upcoming RSNA will therefore be very interesting. We might see more vendors entering this space. I believe independent research— outside the corporate labs—is warranted to get to the bottom of it. Once more systems are installed, it will help us to provide the evidence base on real-world performance in clinical settings. Whether it’s the more difficult to manufacture but highly efficient CdTe semis, or the more broadly available, cheaper silicon substrate, is superior, of one thing I am confident: we will see a lot of innovation and new clinical applications in that space in the near future. It’s another big fork in the road for CT, similar to when spiral or multi-detector row CT were introduced. I am therefore very excited about this technology.”
Physicist Dr Christian Schroeter, PhD, who led the effort to develop the direct conversion detector material for Siemens Healthineers, talks to Associate Professor Shalini Amukotuwa, PhD, MB BS, FRANZCR (Head of Diagnostic Neuroradiology and MSK at Monash Health) about the detector and his experience in developing it.
Photon-counting detectors have brought about a paradigm shift in CT imaging. Can you tell us what the main advantages of this technology are, compared to the conventional CT scanners which we are currently using?
There are several technical advantages: higher spatial resolution, elimination of electronic noise, radiation dose efficiency and, last but not least, spectral information, not only in every image, but also everywhere in the image. Improvement in these crucial technical parameters translates to clinical benefits, which we have been working on since the prototype phase. We have already seen that there are certain things that you can only do with a photoncounting CT. For example, a really hot topic is imaging stented coronary arteries. The metallic stents cause a lot of artifacts, due to beam hardening and photon starvation, which obscure the vessel lumen. These patients are therefore often sent to cathlab instead
of CT coronary angiography. Now, with photon-counting CT, we can get really good images of the vessel lumen, to see in-stent details. This is because of the far superior spatial resolution, reduced blooming and beam hardening, and lack of electronic noise, which we can filter out. The spectral information also allows us to obtain material (iodine) images of the vessel lumen, and we can use material decomposition to subtract out any calcified plaques. We are currently exploring whether these images are now accurate enough for catheter angio to be avoided, which will be a big game changer for patients. Another important example is imaging obese patients, and low-dose imaging, where photon counting provides better image quality with less noise because electronic noise is eliminated. The journey has only just begun, and we will continue to see what these technical advantages really mean in clinical practice, since that’s what’s important.
which made cadmium telluride (CdTe) detectors. But the detector still wasn’t good enough for CT, to be able to deal with the high X-ray photon flux. We had to work on the properties of the material to make it CT ready. It was a tremendous challenge around 2008/9 to overcome this basic hurdle of the detector response to the X-ray photons.

up on photon counting using cadmium zinc telluride (CZT) at this time.
Are you are referring to polarisation, which is a property of the material whereby very high X-ray photon flux rates paralyse the detector and reduce its response? What was the solution?
The direct conversion material for the detector was the main barrier, and we had a long development phase. The project started 20 years ago. We seriously engaged in screening the market of available detector materials around 15 years ago. The first phase was to look at what was already available, then select the best vendor. We identified a company in Japan
The main challenge at that time, 15 years ago, was that most manufacturers used the detector material for gamma cameras, for SPECT, or just spectrometers. The company that we selected already used CdTe detector material for X-ray imaging, although this has a much lower X-ray photon flux than CT. Of all imaging applications, CT has by far the highest X-ray photon flux applied to the detector. The materials which were available then just couldn’t cope with this high flux. There were even scientific papers claiming, based on models, that it may not be possible for CdTe detectors to convert X-rays to photons directly at the typical flux-rates of CT. In the initial prototypes, we could slow down the flux to address this. However, for a clinical full body scanner, you need to be able to work at high flux rates, to be able to deal with any clinical scenario. We were lucky that we came to a point, around 2011, where we could overcome this apparent fundamental hurdle and major impediment which otherwise would have put an end to the project. Another group did actually give
Yes. The solution was based in the CdTe crystal growth itself. You have to go very deep into the very start of the process chain, to the crystal itself, to address the problem of polarisation. You need to understand the whole chain, from crystal growth to image generation, and we saw that many aspects of the crystal growth, for example doping (where tiny amounts of impurities are introduced to alter the crystal structure), the temperature treatment, and the electrodes that we applied, needed to match the bulk material. We had to bring all these pieces together, and understand the signal that comes out of the detector material to design the electronics, the application specific integrated circuit, accordingly. But the trick was really in the first steps, and it was quite a basic one.
“There are several technical advantages: higher spatial resolution, elimination of electronic noise, radiation dose efficiency and, last but not least, spectral information, not only in every image, but also everywhere in the image.”Finished cadmium telluride crystal: image courtesy of Dr Christian Schroeter
So those steps reduced the amount of charge (hole) trapping in the detector material, which is the cause of depolarisation?
Yes. The assumptions, which were made in the models which showed that building a CT detector from CdTe would not be possible, were not as simple as initially thought. The models that we now have, based on our empiric observations and better understanding of the detector material, are quite different. It turns out that hole trapping is not such an issue after all! In fact, it never was a fundamental issue for CdTe, but back then, we didn’t have the knowledge and understanding to have this insight and confidence. Now, the fact that there is a clinical whole-body photon-counting CT shows that the argument that CdTe can’t be used as a detector just doesn’t hold true. We have also seen that there is another company in Canada which is stepping into prototyping at a clinical level using a detector with similar material, CZT. I’m therefore confident that they have also overcome this basic hurdle.

Spatial resolution is the major weakness of silicon-based detectors, and also radiation dose efficiency because of lower absorption which is due to the lower atomic number. With any detector material, you can, with the right system design, bring out one specific parameter and excel at it. For example, extremely high spatial resolution, energy resolution, or dose efficiency. That is nice for a scientific paper or a prototype, but not for a clinical product. You need to have a holistic approach, and bring together and harmonise these parameters for a clinical scanner. You also need scan speed, which is underestimated, and not just for cardiac applications. Dose efficiency and spatial resolution maybe the most important, but then speed, and then energy information. We worked on this integration and harmonisation for 10 years, starting with prototypes scanners and ending with the final product. In my understanding and firm opinion, silicon just can’t do this.




We will see. It felt like the end of the journey when we launched the clinical scanner, now it seems like it’s just the beginning. We will see what the clinicians and researchers will find out. But right now, in my opinion, even if you have one threshold, you already have most of the advantages of photon counting, like dose efficiency, high spatial resolution, and absence of electronic noise. If you have two energy bins, you can do iodine separation. With a third bin, then you can do crazy stuff, with new contrast agents such as gadolinium and gold particles, which have a k-edge. It is possible then to make an additional energy separation, but this is a very early, pre-development research topic. The scanner has a fourth bin, so you are future proof in case somebody invents something where you need it. More bins than that are superfluous.
continued on page
It is our great pleasure to invite our radiation oncology community to the RANZCR ASM 2022 Adelaide, to be held on the traditional lands of the First Nations Kaurna People, from 27– 30 October.

This year, embracing the ASM theme of “Reflect, Revive, Reimagine”, we have assembled a spectacular program covering a wide range of topics, with distinguished international keynote speakers presenting on many interesting topics. Among the many highlights of this ASM, we are especially pleased to present the proton therapy session with keynote talks by Dr Anita Mahajan, Dr Nancy Lee and Dr Langendijk, the lung cancer session showcasing the keynote presentation by Dr Drew
Moghanaki and the head and neck session with Dr Nancy Lee and other eminent speakers. We are also excited to have Dr Umberto Ricardi, who will be speaking on lymphoma and stereotactic ablative radiotherapy. This year’s attractions will also include a head and neck cancer masterclass session on target delineation and an interdisciplinary radiology and radiation oncology combined session devoted to rectal cancer. A session dedicated to patient-reported outcomes and quality of life, with presentations by Dr Geoff Delaney and Prof Afaf Girgis, will bring the opportunity to learn about PROMs in cancer care.
As we emerge from the arduous few years crippled by the pandemic, we look
forward to this ASM as a great platform to come together as a community, revive ourselves and create partnerships for a better future. To this end, we have created many opportunities to meet and connect with industry leaders and many social events to interact. And let’s get together to run in the event we all missed in the past few ASMs—the Targeting Cancer Fun Run is back. And this year we are introducing the kids’ creche, so bring your family along to enjoy the delights of Adelaide as you reimagine your future at the ASM. We look forward to seeing you all in Adelaide.
Dr Ramkumar Govindarajand
Dr Laurence Kim Radiation Oncology Co-Convenors“To infinity and beyond” is not only our theme for this year’s ASM gala dinner as the clinical radiology program for the presents a brand new session on space radiology as we look to reimagine our discipline. The session is the first of its kind crossing over radiology and space science. It brings together prominent figures in both radiology and space science to explore the critical role of clinical radiology, medical imaging and aerospace medicine in supporting astronauts’ health and tackling challenges to human physiology in spaceflights, with world first research findings to be demonstrated. Presenters include Dr Vienna Tran (The role of radiology in human space flight); A/Prof Gordon Cable (Medicine for exploration class missions) and Prof Meng Law (MRI of perivascular spaces in
neurodegenerative diseases and space flight associated neuro-ocular syndrome: how to save and make humanity multiplanetary).
Complementing the space radiology session, we continue to address Artificial Intelligence with Dr Lauren Oakden Raynor presenting 'AI is coming to clinics, but is it safe?' and Chief Medical Officer at AGFA Healthcare Dr Anjum Ahmed 'AI in radiology, the next phase' alongside proffered papers that are further leading this path of how clinical radiologists must reimagine.
The need to revive and reconnect with each other is testament in our strong delegate numbers alongside a sold-out exhibition. The planned social events including the casual radiology quiz night
at our local The Strathmore on Thursday evening which will allow us to relax and unwind among friends. We continue the following evening applauding our new Fellows at the largest Annual Ceremony followed by the Dean’s Reception on the banks of the Adelaide River. Saturday evening, we see delegates think outside the box or shall we say the universe as we consider our costumes for “To infinity and beyond” and dance the night away. There has never been a need now more than ever for us to connect and Reflect Revive Reimagine who we are and where we are going. Registrations are still open for both face-to-face and virtual options at www.ranzcr2022.com
A/Prof Christen Barras Clinical Radiology Convenor
The College relies on extensive volunteer contributions which represent a substantial time commitment by members, sometimes made more problematic with increased workloads in general during the pandemic. We would like to affirm our appreciation of all the volunteer work contributed by many dedicated individuals to the College and the professions. We thank you!
Inside News is asking members to relate their experience in volunteer roles and share tips for others considering taking up a volunteer role. For this edition we spoke to Dr Xavier Yu whose current volunteer roles include RANZCR Victorian Branch Committee Chair and Australian Medical Association Federal Council Radiologist representative. Dr Yu’s previous volunteer roles include Australian Medical Association (Victoria)| Board of Directors 2012–2015, Vice President (2016–2018), RANZCR Trainee Committee Secretary 2015, Victorian Branch Committee 2015–2022, Media Profile Working Group 2015–2018, Diagnostics Economics Committee 2018–2020.
Dr Yu graduated MBBS/BA (University of Melbourne 2000), entered radiology training in 2011 (with previous training in general surgery and orthopaedics) and gained Fellowship in 2016. He performs his volunteer work in addition to a number of non-volunteer clinical roles, as clinical radiologist for Monash BreastScreen, North Western BreastScreen, St Vincent's Hospital Melbourne, Barwon Medical Imaging (Geelong), Western Hospital, Everlight Radiology and Capital Radiology. He also holds the following nonvolunteer non-clinical roles: designated radiologist and Director of Training for Monash BreastScreen, Capital Radiology (Capitol Health) Victorian Clinical Leadership Committee.
It’s clear that you have made a huge contribution by volunteering with the College. What motivates you to volunteer? How does volunteering contribute to patient care, to colleagues, to the professions?

My career in volunteering for the College has arisen from my extensive previous experiences and roles within the Australian Medical Association, including previously as the AMA Victorian branch Board of Directors and as Vice President. In particular, there was overlap between my role in the Clinical Radiology Training Committee as Secretary in 2015 and my previous role within the AMA on the Council of Doctors in Training.

“Volunteering allows us as radiologists to engage with others in different ways to the traditional radiologist-referrer relationship (or the doctorpatient relationship), and encourages us to be self-critical and analytical about our existing practices and how can we make them better. Also, volunteering permits us to engage with fellow radiologists to foster new ideas and challenge existing mindsets on ‘how the way things are done.”
I think my concern for the welfare of my colleagues, including but not exclusively radiologists, has provided the motivation to spare my time for involvement in College activities. Also, my perception of radiologists versus other doctors, reinforced by my involvement in the College’s Media Profile Working Group, is that we are generally more quietly spoken and need encouragement to air valuable opinions to our colleagues and other diagnostic imaging industry stakeholders.
Volunteering allows us as radiologists to engage with others in different ways to the traditional radiologist-referrer relationship (or the doctor-patient relationship), and encourages us to be self-critical and analytical about our existing practices and how can we make them better. Also, volunteering permits us to engage with fellow radiologists to foster new ideas and challenge existing mindsets on ‘how the way things are done.’
Has volunteering given you skills and experience you could not otherwise have gained?
Volunteering for College and AMA activities has definitely enhanced and reinforced my communication skills with colleagues and stakeholders outside our own diagnostic imaging industry
What achievements are you most satisfied with/proud of as a volunteer?
I think that my involvement particularly with the Diagnostic Economics Committee (DEC), which only met once every few months, nevertheless fostered ideas for the College to ensure the Commonwealth Government was held to account for its funding of Medicarerebatable diagnostic imaging services. Of course, government funding for radiology remains inadequate, but the activities of those in College committees such as the DEC ensure radiology remains at the forefront of the attention of the Department of Health.
aren’t yet in a committee—please put your hand up to help out! Every little contribution helps the College collectively advance your cause and that of your colleagues. We need greater diversity of opinions and representation—including more participants from all genders!”
What has the pandemic meant for the volunteer experience? What are the risks of burnout? How best are these managed, in your view?
I think there are pros and cons with how COVID-19 has changed volunteer activities. On the one hand, the need to move to online activities has increased the availability of radiologists to participant in meetings and therefore broadened the quality of inputs across our various committees. However, on the downside, the number of online meetings for both clinical work (for example, attending and participating in multidisciplinary meetings) and volunteer roles has escalated to the point that some radiologists who regularly undertake volunteer work may now feel they are taking on too much but also feel obligated to continue.
An additional consideration is that online meetings, particularly our Scientific Meetings, can only do so much. I’m pretty sure that we all value in-person interactions to share ideas, such as at upcoming ASMs.
I think that many hands make light work, and if there are more radiologists available to volunteer in College activities that would be fantastic. For example, the Victorian Branch Committee would definitely welcome even ‘ad hoc’ volunteers if they wished to assist in organising educational activities and events.
Do you have any advice on volunteering in general? Are there efficiencies to be gained in sharing the volunteer experience?
I would definitely say to my colleagues who aren’t yet in a committee—please put your hand up to help out! Every little contribution helps the College collectively advance your cause and that of your colleagues. We need greater diversity of opinions and representation—including more participants from all genders!
What more can the College do to support volunteers? How can the College best support collaboration and knowledge transfer?
Perhaps there needs to be a rethink on when meetings are run: typically, they are in the evenings after work, but perhaps during the day would be better. Therefore, the College could do more to support volunteers by better engaging with industry to spare us ‘non-clinical’ support time.
Do you have a question for the next ‘volunteer in the spotlight’?
My question would be: what are the perceived barriers to (particularly younger) Fellows taking on College volunteering activities?
To find out more about volunteering at the College, visit:
www.ranzcr.com/college/volunteering
“I would definitely say to my colleagues who

A recent survey by four College members, focused on research seeding grants awarded to Australian radiation oncologists, reveals a 6.8-fold funding investment return, significant academic output and substantial broader patient benefits.
The various grants awarded to members have evolved over the years, but are mainly targeted at early career researchers, trainees or Fellows within five to ten years post-Fellowship (with or without a preexisting research higher degree).
Prof Daniel Roos, Dr Ben Ramsay,Dr Lisa Sullivan and A/Prof Puma Sundaresan developed the hypothesis that the grants result in significant impact well beyond the purely academic.
Between 2010 and 2020, 58 RANZCR grants, ranging from $5,000 to $26,000, were awarded to 41 researchers. Five recipients of failed projects were excluded.
The remaining 36 recipients of 51 grants totaling $940,000 undertook a Collegeapproved, voluntary online survey, which assessed grant outcomes, the factors promoting project success and perceptions of the grant process.
The survey response rate was 100 per cent. Objective academic outcomes attributable, at least in part, to the grants included 103 conference presentations (52 posters, 51 oral), 59 publications, 21 awards or prizes, 18 higher degrees, and 27 consequential grants totaling $6.4M (a 6.8-fold return on investment) (see Table on facing page).
Broader impacts included perceived contributions to changes in clinical decision-making (72 per cent of recipients) or radiotherapy techniques (61 per cent), enabling of subsequent research (56 per cent), development of clinical guidelines (53 per cent) or novel research tools (19 per cent), and recruitment of research assistants (19 per cent).
The three most important factors reported to contribute to project success were the grant itself (83 per cent of recipients), networking (81 per cent) and local infrastructure (81 per cent). The grant program was rated very positively.
The College survey has confirmed very good value for money from its radiation oncology research grants. In addition to an almost seven-fold funding investment return and continuing significant academic output, it has also revealed substantial broader impact.
It provides a great incentive for radiation researchers to submit grant applications in 2023—the benefits are strong, as you can see from these survey results. FRANZCRs, Educational Affiliates and student members in clinical radiology and radiation oncology are welcome to apply. New Zealand members are especially encouraged to participate. For more information visit Grants and Awards | RANZCR or email gaps@ranzcr.edu.au
* Int J Radiat Oncol Biol Phys 2022; 114 (2):198–202
“A recent survey by four College members, focused on research seeding grants awarded to Australian radiation oncologists, reveals a 6.8-fold funding investment return, significant academic output and substantial broader patient benefits.”
“The College survey has confirmed very good value for money from its radiation oncology research grants. In addition to an almost seven-fold funding investment return and continuing significant academic output, it has also revealed substantial broader impact.”

Medical Imaging
Original Article: Optimising CT-chest protocols and the added value of venous-phase contrast timing; Observational case-control
Corresponding author: Michael Croft, Royal Adelaide Hospital, 1 Port Rd, Adelaide, South Australia, 5000, Australia
Introduction: To optimize CT chest protocol by comparing venous contrast timing with arterial timing for contrast opacification in vessels, qualitative image quality and radiologists’ satisfaction and diagnostic confidence in assessing for potential nodal, pleural and pulmonary disease in general oncology outpatients.
Method: Matched case−control study performed following CT protocol update. 92 patients with a range of primary malignancies with 2 CT chests in a 2-year period, one with an arterial phase protocol and the second in the 60 second venous phase, were included. Contrast attenuation in aorta, pulmonary artery and liver were measured. Subjective measurements assessed perivenous artefact, confidence in nodal pleural and pulmonary assessment and presence of pulmonary emboli. Statistical analysis was performed using paired and unpaired t-tests.
Results: Venous-phase CT demonstrated more consistent enhancement of the vessels, with higher attenuation of the nodes, pulmonary and pleural lesions. There was a significant reduction in perivenous beam hardening artefact on venous-phase CT (P < 0.001). Diagnostic confidence was significantly higher for nodal assessment and pleural abnormality visibility (P < 0.001) and pleural assessment (P < 0.05). There was no significant difference in pulmonary mass visibility. There was adequate enhancement to diagnose significant pulmonary emboli (PE) with 4 incidental PEs detected on the venous phase, extending to segmental vessels.
Conclusion: Venous-phase CT chest performs better than arterial-phase on all fronts, without compromising assessment of incidental pulmonary emboli. When intravenous contrast is indicated in a routine chest CT (excluding a CT-angiogram), the default timing should be a venous or 60s phase.
Medical Imaging
Guidelines: Quality care guidelines for uterine artery embolisation in women with symptomatic uterine fibroids in Australia and New Zealand: According to the AGREE-II checklist and endorsed by the Interventional Radiology Society of Australasia
Corresponding author: Warren Clements, Department of Nuclear Medicine & PET, Alfred Hospital, 55 Commercial Road, Melbourne, Victoria, 3004, Australia
Radiation Oncology
Original Article: Disparities in radiation therapy utilization for cancer patients in Victoria
Corresponding author: Wee Loon Ong, Alfred Health Radiation Oncology, 55 Commercial Road, Melbourne, Victoria,3004, Australia
Introduction: To evaluate the proportion of cancer patients who received radiation therapy (RT) within 12 months of cancer diagnosis (RTU12) and identify factors associated with RTU12.
Methods: This is a population-based cohort of individuals with incident cancer, diagnosed between 2013 and 2017 in Victoria. Data linkages were performed between the Victorian Cancer Registry and Victorian Radiotherapy Minimum Dataset. The primary outcome was the proportion of patients who had RTU12. For the three most common cancers (i.e., prostate, breast and lung cancer), the time trend in RTU12 and factors associated with RTU12 were evaluated.
Results: The overall RTU12 in our study cohort was 26–20% radical RT and 6% palliative RT. Of the 21,735 men with prostate cancer, RTU12 was 17%, with no significant change over time (P-trend = 0.53). In multivariate analyses, increasing age and lower socioeconomic status were independently associated with higher RTU12 for prostate cancer. Of the 20,883 women with breast cancer, RTU12 was 64%, which increased from 62% in 2013 to 65% in 2017 (P-trend < 0.05). In multivariate analyses, age, socioeconomic status and area of residency were independently associated with RTU12 for breast cancer. Of the 13,093 patients with lung cancer, RTU12 was 42%, with no significant change over time (P-trend = 0.16). In multivariate analyses, younger age, male and lower socioeconomic status were independently associated with higher RTU12.
Conclusion: In this large population-based state-wide cohort of cancer patients, only 1 in 4 had RT within 12 months of diagnosis. There were marked sociodemographic disparities in RTU12 for prostate, breast and lung cancer patients.
Original Article: Randomised controlled trial on the effect of simethicone bowel preparation on rectal variability during image-guided radiation therapy for prostate cancer (SPoRT study)
Corresponding author: Jennifer Ward, Department of Radiation Oncology Sir Charles Gairdner Hospital Cancer Centre, Hospital Avenue, Nedlands, WA 6009, Australia
Introduction: The purpose of this study was to assess whether simethicone reduces the rectal volume (RV) and gas volume (GV), to increase treatment accuracy and to decrease toxicity of prostate radiation therapy.
Methods: 30 patients were randomised to simethicone or no intervention. Cone-beam computed tomography (CBCT) scans were performed on Days 1–3 and weekly until completion of radiation. RV and GV were measured using volume delineation. Toxicity data were collected.
Results: 264 CBCTs were analysed. RV and GV were not significantly different in the simethicone group compared with the control group at each time point (P >0.05) after adjusting for Week 0 values as a covariate. The simethicone group showed an average reduction in RV and GV of 10% and 21%, respectively, compared with the control group (P >0.05). Standard deviations were calculated over 10 time points, which were grouped to represent the first 2–3 weeks of radiation therapy versus subsequent weeks. These were not significantly different between the simethicone and control group. However, there was a statistically significant decrease in the variability of RV at time points 6–10 compared with time points 1–5 within the simethicone group (P = 0.012), but no significant difference was found between these grouped time points in the control group (P = 0.581). The toxicity questionnaires showed no significant difference between the groups.
Conclusions: Simethicone did not decrease the RV or GV overall. However, simethicone appeared to significantly decrease the RV variability from Week three onwards. This suggests that taking simethicone two to three weeks before starting radiation therapy may reduce RV variability, although a larger study is needed to confirm this.
If you are a member of the Royal Australian and New Zealand College of Radiologists, access JMIRO free online. - Go to www.ranzcr.edu.au
1957!
The College congratulates neuroradiologist Professor Sandeep Bhuta on being awarded an International Recognition Award from Symposium Neuroradiologicum (SNR) 2022, in recognition of his collaboration with other clinicians to conduct research and promote education to advance clinical care of head and neck cancers.

Prof Bhuta recently returned from New York from Symposium Neuroradiologicum (SNR) 2022 which was combined with the American Society of Neuroradiology’s (ASNR) annual conference.

More than 2,000 delegates from 56 countries attended the conference, where three academic papers by Prof Bhuta were displayed alongside researchers from John Hopkins University, Mayo Clinic, Stanford University, and other leading research institutions. Prof Bhuta also gave a faculty lecture on 'Trends in Head and Neck Oncology over a Decade in Australasia'.
The educational and research paper awarded in New York was entitled Sinonasal and Anterior Skull Base Tumours: Multidisciplinary Approach to Treatment.
“We see a lot of these cancers with anterior skull base involvement, and this was the motivation to work in this area so that our imaging and surgical approaches can be streamlined to have good surgical outcomes and help the patients,” he said.
The scientific paper had valuable contributions from co-author Karen Huang, radiology registrar (now at Townsville Hospital and Health Service), Emily Guazzo, head and neck surgeon, Gold Coast University Hospital (GCUH).
“Getting an award on the world stage and getting recognised for the work we do here at Gold Coast University Hospital and through an affiliation with Griffith University made this trip worth it,” Prof Bhuta said.
Throughout the pandemic, Prof Bhuta who sits on two ASNR committees, attended symposiums virtually, often getting up at 3 am to present papers to a northern hemisphere audience, like many clinicians. This was the first international event he has attended since the pandemic.
“This has definitely put our institute on the world map, and I had a lot of enquires from junior doctors for training opportunities and sabbaticals here.”
Prof Bhuta, who is from GCUH’s Department of Medical Imaging, is also Director of Research and MRI Supervisor and holds academic titles with Griffith University’s School of Medicine and the Menzies Health Institute.
“We see a lot of these cancers with anterior skull base involvement, and this was the motivation to work in this area so that our imaging and surgical approaches can be streamlined to have good surgical outcomes and help the patients,” he said.
“This has definitely put our institute on the world map, and I had a lot of enquires from junior doctors for training opportunities and sabbaticals here.”Prof Sandeep Bhuta Prof Sandeep Bhuta with Prof Christine Glastonbury (neuroradiologist, UCSF, USA), from ASNR 2022

“He served as the NSW representative of the AMA Council of Doctors in Training from 2016–2018 and played a key role in establishing the annual Hospital Health Check survey.
“Currently a radiology registrar at Nepean Hospital, Dr Hettige is committed to improving working conditions for all doctors-in-training. Through the AMA (NSW) Hospital Health Check survey, he played a significant role in helping doctors-intraining claim for un-rostered overtime.
The other nominees for the award were Dr Tahnee Bridson, Dr Ashna Basu and Dr Brad Macdonald.
Dr Khorshid said each nominee should take with them a sense of achievement and personal pride that stems from their excellent work as an advocate for doctors-in-training and improved healthcare outcomes.
The College also congratulates Dr Sanjay Hettige, who won the Australian Medical Association’s Doctor in Training of the Year Award in July this year. Dr Hettige has played a key role in establishing the annual Hospital Health Check survey and introducing an online claiming system for un-rostered overtime in NSW,
Dr Hettige was presented the award by AMA President, Dr Omar Khorshid at the association’s gala dinner in Sydney. Dr Khorshid told the dinner the AMA is committed to fostering the next generation of Australia’s medical leaders with the award recognising the outstanding achievements of doctorsin-training in leadership and advocacy and encouraging the development of leadership skills.
Dr Hettige, who received the award for his outstanding contribution to leadership and advocacy, has been an advocate for doctors-in-training in NSW throughout his medical career, Dr Khorshid said.
“And as a direct result of his meetings with the Health Minister, NSW Health introduced an online claiming system in NSW. In 2017, 11 per per cent of doctors training reported they were paid for all of the un-rostered overtime they worked. By 2021, that figure had risen to 74 per cent.
“With levels of burn out and bullying increasing during the pandemic, Dr Hettige is now focused on introducing measures such as setting fatigue standards and establishing a Bullying Forum.”
Dr Hettige said, “I am really honoured to win the AMA National Doctor in Training of the year award. It’s a testament to what passionate doctors-in-training in NSW and the great staff at Australian Medical Association (NSW) have been able to do to improve working conditions for doctors-in-training in NSW.”
“I am really honoured to win the AMA National Doctor in Training of the year award. It’s a testament to what passionate doctors-in-training in NSW and the great staff at Australian Medical Association (NSW) have been able to do to improve working conditions for doctors-in-training in NSW.”
The College is pleased to announce that the Targeting Cancer Fun Run will return this year at the 72nd Annual Scientific Meeting in Adelaide on the morning of 29 October after two years’ absence due to the pandemic.


Since its inception in 2015 in Adelaide, the Targeting Cancer Fun Run has become one of the most iconic events of the College’s Annual Scientific Meetings with a worldwide footprint. It all started along the scenic River Torrens in South Australia, and travelled to the Viaduct Harbour in New Zealand, lakeside in Canberra, and a Targeting Cancer supporting fun run at the ESTRO meeting in downtown Milan in Italy.

The fun run attracts and brings together hundreds of Targeting Cancer supporters including radiation oncologists, clinical radiologists, trainees, sponsors, exhibitors, health workers, health care consumers and College staff to raise awareness of radiation therapy.
Julie McCrossin AM, Targeting Cancer Campaign Ambassador, head and neck cancer survivor, and broadcaster, said: "I’m extremely excited about the return of the Fun Run. I was part of the inaugural run back in 2015 in Adelaide. It was truly impressive to see so many fit and lively radiation oncologists and colleagues showing their commitment to physical exercise, which helps prevent everything, and raising awareness about the importance of radiation therapy in cancer care. It is the treatment that saved my life!"
continued over...
“Julie McCrossin AM, Targeting Cancer Campaign Ambassador, head and neck cancer survivor, and broadcaster, said: "I’m extremely excited about the return of the Fun Run. I was part of the inaugural run back in 2015 in Adelaide. It was truly impressive to see so many fit and lively radiation oncologists and colleagues showing their commitment to physical exercise, which helps prevent everything, and raising awareness about the importance of radiation therapy in cancer care. It is the treatment that saved my life!"”
Targeting Cancer is an initiative of the College’s Faculty of Radiation Oncology, the peak body for radiation oncology in Australia and New Zealand. Targeting Cancer promotes radiation therapy as an effective treatment option for cancer. There will be prizes for the fastest female and male runners respectively at the fun run. Check out our website www.targetingcancer.com.au or follow us on Facebook and Twitter to find out more and stay updated.
Registration is open now! Join the Targeting Cancer Fun Run 2022 to help us raise awareness of radiation therapy. See you soon in Adelaide!



Register now: www.ranzcr2022.com/ targeting-cancer-fun-run/

We’d love to hear from you if you have any feedback and suggestions, via email at info@targetingcancer.com.au

Neuroradiology A

A/Prof Michael Bynevelt and Dr Kate Mahady
Neuroradiology B
Prof Alan Coulthard and Dr Paul O’Connell
Head and Neck
Dr Grace Aw and Dr Jennifer Gillespie
Spine
Dr David Lisle and Dr Scott Davies
Musculoskeletal Systems A
Dr Catherine Hayter and Dr Clinton Pinto
Musculoskeletal Systems B
Dr Aziz Osman and A/Prof Bruno Giuffre
Chest A
Dr James Bewes and Dr Sally Ayesa
Chest B
Prof Catherine Jones and A/Prof Karin Steinke
Forge
a unique and exciting career with South East Radiology
South East Radiology is seeking expressions of interest from radiologists to join a growing network of clinics in the beautiful Southern Highlands and South Coast regions of NSW.
Work and live in the rolling countryside and beautiful seaside locations of South East NSW

Backing of the Qscan Group Executive and a collegiate doctor network across Australia
Market competitive remuneration and eligibility for equity
for more information or a confidential discussion
Qscan Group members
“Medlicott, Jann (Dr) MNZM, radiologist, philanthropist, art supporter, literary champion, true friend and cat lover, Jann died at her home 12 August 2022, surrounded by whanau.”
Jann worked in Tauranga as a hospitalbased radiologist, and co-founded two private radiology practices, Bay Radiology and Medex Radiology, retiring from Medex in 2011.
Included in her long involvement and contribution to radiology and the College, Jann was NZ Branch Chairperson 1995–1997, RANZCR Councillor 1995–1998, and was involved in the RANZCR Quality & Accreditation programs (including for mammography and DEXA scanning). She established and edited the NZ Branch newsletter. She was awarded Life membership of the College in 2006.
Jann’s love of teaching was well known—she shared her knowledge widely, from radiography students to registrars in many disciplines, with a particular love of orthopaedics.
As one Tauranga GP messaged me on hearing of her death: “I first met Jann as a junior house surgeon—she was passionate about teaching and would hold regular, often lunchtime teaching sessions, invaluable, always with great wit —and entertaining”.
Many would say Jann mellowed in later years. She continued to pursue her love of the Arts. Jann had been closely involved with the Acorn Foundation since 2008, sponsoring many awards in the Arts. Since 2016 she had been the anonymous donor of the annual $50,000 Acorn Foundation Fiction Prize (Ockham NZ Fiction Book Award) but ‘came out’ as the donor in 2020. It was then renamed “The Jann Medlicott Acorn Prize for Fiction”.

Becky Manawatu, winner of the 2020 prize, wrote about a lunch Jann hosted: “not only were flutes of champagne … thrust into our hands when we walked into the Tauranga Club, but Jann’s charm and spirit filled the room. She had on these incredible pink Doc Martin boots, and a jacket with pink flowers and sequins”.
Jann’s death at age 79 years does not mean the end of this annual book prize—she has arranged for it to be given in perpetuity, annually adjusted for wage inflation, with a current value of $63,000. Her legacy also continues in other awards. Many people can truly say “Jann Medlicott changed my life”. She was honoured in late 2020 when named as a Member of the NZ Order of Merit.
Jann had been fighting cancer for several years, “collaborating” with her oncologist, other medical colleagues and a supportive GP. A truly erudite woman, she remained keen to discuss her options for treatment but accepted
her very rapid deterioration over the final two weeks of her life, once options were exhausted.
At her private cremation, a host of fantails attended it is told.
The College notes with regret the death of the following members:
Dr Robert Hugo MacKay, Fellow, QLD
Dr Jann Medlicott, Life member, NZ
Dr Thomas Shailer Weston, Life member, NZ





The College will once again be heading to the city of Adelaide this year for the much anticipated Annual Scientific Meeting (ASM), which will be held between 27–30 October 2022. Adelaide hosted the first ASM, which was held on 1 November 1950, and has hosted it many times since then.
On 6 October 1949, the College of Radiologists (Australia and New Zealand) was formed. The formation of a medical college for the field of radiology was regarded as formal recognition of the field at the time; and placed it on par with the longstanding medical colleges of surgeons and physicians.

The College began with only 193 foundation members. The inaugural scientific meeting was held at the University of Sydney in December 1949.
At the first ASM, on 1 November 1950, various combined scientific sessions were held in conjunction with several social gatherings, much like the ASMs which have taken place more recently. The Roentgen Oration was delivered by Dr S W Pennycuick at the Bonython Hall at Adelaide University.

Much, of course, has changed in the past 72 years since the first ASM was held in Adelaide. For example, the College in those days was heavily male-oriented, with only seven female members at the time.

“The College began with only 193 foundation members. The inaugural scientific meeting was held at the University of Sydney in December 1949.”
The South Australian Premier at the time of the first ASM, Sir Thomas Playford, focused on South Australia’s agricultural industry and power production in his welcoming address to the Fellows who attended. South Australia’s colonial history, water supply, and its meat and wheat exports were also mentioned. With a population of only 680,000 at the time, the Premier portrayed a far more quaint picture of Adelaide than what we see today.
‘Growth following the war’ was a major theme of the first ASM in 1950, with a focus upon the positive contribution made by returned servicemen towards agricultural growth in South Australia.
One important South Australian attraction which has not changed since the 1950s is the beautiful wine country, including the Barossa Valley. Fellows are encouraged to pay a visit, and to sample some of the local produce, when you visit Adelaide this October.
Some things have definitely changed since the 1950s. For example, the College will no longer be supplying cigars. The current ASM planning committee is no doubt thankful for the cost saving in that respect, not to mention the added health benefits!


For the first time in a little while the Archives will be presenting at the ASM. Please come along and check out the various displays which will be on offer.
If you have any queries in the meantime, please do not hesitate to reach out at archives@ranzcr.edu.au
Natasha Ramrakha College ArchivistThe RANZCR events team are planning a busy annual calendar of events in 2022.
All new events are loaded to the Events page on the RANZCR website, follow this link to stay up-to-date www.ranzcr.com/whats-on/events .
Clinical Radiology Centralised Learning Program
New lecture released by the last Sunday of each month, check www.ranzcr.com/clp for more information and see page 31 for full details of the current schedule.
RANZCR ASM, Adelaide, SA
27–30 October 2022
For more information and to register, please visit the website: www.ranzcr2022.com
RANZCR Annual Ceremony, Adelaide, SA
28 October 2022
FROGG Webinar with Dr Amar Kishan
SAVE THE DATE | 18 November 2022, 8 am AEDT
Webinar | Post-mortem imaging after stillbirth & neonatal death: what is the evidence?
17 November 2022 8 pm AEDT
Live lecture delivered through GoTo Webinar to attendees with Q&A at the end of the presentation.
Presented by Prof Owen Arthurs, United Kingdom. Prof Arthurs is an academic consultant paediatric radiologist, funded by an NIHR Fellowship. He holds a PhD in brain imaging and trained in both paediatrics and academic radiology in Cambridge, London and Paris.
This webinar is part of an ongoing series of five webinars to be delivered across late 2022 and early 2023.
This webinar is one part of the broader Stillbirth Project for which the College has obtained funding from the Australian Government through the Department of Health and Aged Care. The project will increase clinicians’ capacity (particularly radiologists and pathologists) to undertake stillbirth investigations and autopsies and ensure these services are available to the bereaved parents who choose to access them.
The Stillbirth Investigations Project will develop tailored strategies, educational programs and resources to improve the uptake, acceptability, range and quality of stillbirth investigations in Australia. The program of work will produce a training package, best practice standards/guidelines, practice support resources and decision support tools.
To find details and register for these events, visit the RANZCR What’s On page by scanning the QR code here:

For regular updates, in addition to the website listings, simply like and follow our RANZCR social media accounts:
If you have any questions relating to any College events, please contact the Conference & Events team at events@ranzcr.edu.au
Events are a great way to gain CPD hours!

The College is committed to supporting the professions of clinical radiology and radiation oncology to contribute to equitable health outcomes for Māori, Aboriginal and Torres Strait Islander Peoples. This work is central to the strategic objectives of the College and is reflected in the College’s Strategic Plan. To support clinical radiologists and radiation oncologists in enhancing their cultural competency and promote cultural safety, a large number of general resources have been collated for members to use as part of their professional development.
Cultural safety is defined by the Australian Health Practitioner Regulation Agency and National Health Leadership Forum of Aboriginal and Torres Strait Islander health peak organisations (in consultation with the MBA and AMC) as follows:
‘Cultural safety is determined by Aboriginal and Torres Strait Islander individuals, families and communities. Culturally safe practice is the ongoing critical reflection of health practitioner knowledge, skills, attitudes, practicing behaviours and power differentials in delivering safe, accessible and responsive healthcare free of racism.’

‘Patient safety for Aboriginal and Torres Strait Islander Peoples is the norm. We recognise that patient safety includes the inextricably linked elements of
clinical and cultural safety, and that this link must be defined by Aboriginal and Torres Strait Islander Peoples.’ (AHPRA, 2020)
Cultural safety is defined in the New Zealand context as:
'The need for doctors to examine themselves and the potential impact of their own culture on clinical interactions and healthcare service delivery.
The commitment by individual doctors to acknowledge and address any of their own biases, attitudes, assumptions, stereotypes, prejudices, structures and characteristics that may affect the quality of care provided.
The awareness that cultural safety encompasses a critical consciousness where healthcare professionals and healthcare organisations engage in ongoing self-reflection and selfawareness and hold themselves
accountable for providing culturally safe care, as defined by the patient and their communities'. (MCNZ, 2019)
See opposite page for a selection of resources available on www.ranzcr.com
To suggest further resources, contact Madeleine d’Avigdor | Senior Projects Officer - Indigenous Workforce | Policy, Advocacy and Workforce Unit at madeleine.davigdor@ranzcr.edu.au
To access the full range of resources, including online learning modules, articles and books, scan the QR code

“The need for doctors to examine themselves and the potential impact of their own culture on clinical interactions and healthcare service delivery.
The commitment by individual doctors to acknowledge and address any of their own biases, attitudes, assumptions, stereotypes, prejudices, structures and characteristics that may affect the quality of care provided.”
The links to all of these resources and more can be found on our website: www.ranzcr.com
Websites
Health Promotion Forum of New Zealand | Maori Health
The Healing Foundation
Australian Institute of Health and Welfare (AIHW) | Snapshots on Indigenous health
Common Ground
Death and Sorry Business and protocols of bereavement.
Lowitja Institute
Australian Indigenous HealthInfoNet | Cultural Safety for Health Professionals
The LIME Network
Stop Institutional Racism
Podcasts/Audio
Getting Better | A year in the Life of a Maori Medical Student Katherine Hospital: Back from the brink Indigenous Health MeDTalk
Ask the Specialist
Videos
The Journey of Health and Wellbeing
Health Navigator | Maori health videos
Understanding Conscious Bias
Guidelines and Frameworks
Communicating Effectively with Aboriginal and Torres Strait Islander people
Aboriginal and Torres Strait Islander Patient Care Guideline Sad News, Sorry Business
Aboriginal and Torres Strait Islander | Cultural Safety Framework and Continuum of Cultural Safety Reflective Tool
Guidelines for Research
Health Research Council of New Zealand | Māori Health Research
National Health and Medical Research Council
Reports
Baseline Data Capture: Cultural Safety, Partnership and Health Equity Initiatives. Final Report. Medical Council of New Zealand | Statement on Cultural Safety
Medical Council of New Zealand | He Ara Hauora Māori: A Pathway to Māori Health Equity
Partnership for Justice in Health: Scoping paper on Race, Racism and the Australian Health System
Radiation Oncology Specific Resources
National Indigenous Cancer Network (NiCAN)
Key Documents
Review of cancer among Aboriginal and Torres Strait Islander people (2020)
Guide to Implementing the Optimal Care Pathway for Aboriginal and Torres Strait Islander People with Cancer
Patient Information
Cancer Information for Patients
Cancer Information for Aboriginal and Torres Strait Islander Peoples
Websites
Cancer Australia | For Aboriginal and Torres Strait Islander People
Culturally safe communication skills for non-Indigenous health professionals
It was a typically chaotic day. Two admin staff and one of the radiographers were away with Covid, and the practice was running late. Staff resuscitation training had been put on the backburner for the third time in six months, and the drug trolley was accumulating dust. The remaining radiographer came charging in …. “The lady in CT two, something’s not right. I think it might be a contrast reaction” …..
Use of iodinated contrast agents dates back to the 1920s. Since then, contrast media have evolved and the risk of reactions has decreased over time, however serious and life-threatening reactions can still occur.
It is vital to understand the risks and to be prepared for early recognition and prompt, appropriate management in the event of an adverse reaction.
Hypersensitivity reactions to iodinated contrast media may be immediate anaphylactic reactions or delayed reactions.
Mild contrast media reactions include flushing, limited nausea/ vomiting, pruritus, headache and mild urticaria. They are usually self-limited and resolve without specific treatment. Mild reactions can be seen in up to 1% of patients after non-ionic low-osmolality contrast media administration.
Moderate contrast media reactions include severe vomiting, marked urticaria, bronchospasm or other respiratory symptoms, facial/laryngeal oedema, and vasovagal attacks.
Severe contrast media reactions include hypovolaemic shock, respiratory arrest, cardiac arrest, and convulsions. Severe anaphylactic reactions are uncommon, occurring in less than 1 in 100,000 patients.
This risk was highlighted by the coroner in a recent report into the death of a patient following intravenous administration of contrast medium in a suburban radiology centre.
One of the issues opined on by experts at the inquest was whether the recognition, treatment, and management of the patient’s contrast reaction by the radiologist was appropriate.
It was found that even if the radiologist was unsure whether the patient was experiencing anaphylaxis, he should have administered adrenaline as soon as possible and continued to administer it.
The coroner found that the radiologist’s training and experience did not adequately prepare him to respond appropriately to the patient’s contrast reaction. The coroner found that any symptoms immediately following the administration of contrast medium should alert a health practitioner to consider a diagnosis of anaphylaxis.
This case was particularly tragic as it was found that the process that led to the patient undergoing the CT coronary angiogram was not appropriate, and the patient had not been adequately assessed.
The coroner made a large number of recommendations in his report. Many relate to the referral process itself, but there were important recommendations relating to contrast reactions. Coroner’s recommendations to RANZCR with regards to the recognition and management of contrast reactions:
‘1. That RANZCR implement a mandatory requirement that radiologists working in settings where contrast is administered without other expert medical support undertake specific training in the recognition and management of severe contrast reactions and anaphylaxis every 3 years.
2. That RANZCR, the Australasian Society of Clinical Immunology and Allergy (ASCIA) and the Australian Resuscitation Council (ARC) develop and implement a comprehensive training and certification programme for radiologists in the recognition and management of severe contrast reactions and anaphylaxis and the provision of CPR and basic life support including airway management with equipment available in radiology practices.
The coroner also commented specifically on private diagnostic imaging practices, recommending that:
adrenaline auto-injectors (in addition to vials of adrenaline) are accessible in every room where contrast medium is injected;
radiographers are trained in the recognition and management of anaphylaxis and severe contrast reactions; practice staff are trained to play an active role in emergency situation; and orientation of new radiologists includes location of emergency equipment.
Although the likelihood of a patient suffering a severe anaphylactic reaction to contrast is fairly low, implementing the coroner’s recommendations may result in other patients avoiding such a catastrophic outcome.
Further reading - RANZCR Iodinated Contrast Guidelines https://www.ranzcr.com/college/document-library/ranzcr-iodinatedcontrast-guidelines
Dr Jane Deacon Manager, Medico-legal Advisory Services
I am very excited that we will be returning to a face-to-face ASM. The convenors have put together a very interesting scientific program and I think we will all enjoy being able to network and socialise together at last!
A feature of each ASM is the Faculty Forum, an opportunity for us to explore and discuss issues that are impacting our profession or will do so in the future. In past years, we have featured artificial intelligence and digital health, to name a few. This year the overarching theme is diversity in our profession with a focus on how we can encourage more Indigenous doctors into our professions. This year we are changing it up a bit with the forum split into two sections. In the first half we will have a panel discussion among radiologists on how to attract a more diverse group of medical students into our profession. Then, for the first time, we will join with the Faculty of Radiation Oncology to focus on how we can work towards more equitable health and workforce outcomes for Māori, Aboriginal and Torres Strait Islander Peoples. This is an important goal of our Action Plan for Māori, Aboriginal and Torres Strait Islander Health.
In this second half of the forum, a panel of members of the College will engage in a conversation on how we can encourage more Indigenous doctors into our professions as well as share strategies for improving the provision of culturally appropriate clinical radiology
and radiation oncology health care for Indigenous communities. This session will address the rationale for this work, discuss real life examples and provide a networking opportunity for interested members.
I look forward to seeing your all there.
Our College has long recognised the significant potential that AI has in transforming radiology. We made a deliberate decision to become a ‘leader’ rather than ‘bystander’ in understanding and harnessing the potential of AI. We want to guide the implementation of AI in radiology and radiation oncology to ensure that patient safety and highquality standards are at the centre of decision-making.
This role has been articulated through the work of our Artificial Intelligence Committee (AIC). The AIC first developed Ethical Principles for AI in Medicine, to set out an ethical framework for AI. Following this, the AIC developed Standards of Practice for AI, which sets out how these ethical principles should be deployed in the practice setting.
Most recently we have published our Position Paper on the Regulation of Artificial Intelligence in Medicine. The introduction of AI into clinical practice has created opportunities to enhance patient care but has also created a range of new risks and responsibilities. In our position paper, the College is
advocating for effective regulation that provides clarity for AI developers and the rest of the healthcare system while safeguarding patient care. This paper set out principles and recommendations to guide the development of a robust regulatory framework for AI technology in medicine and will be used to guide government conversations around AI regulation.

“The Australian Federal Government has allocated $750,000 over four years to the College to increase the profession’s capacity to undertake stillbirth investigations and ensure that these services are available to bereaved parents who choose to access them. This is a great win for the College.”
The Australian Federal Government has developed a National Stillbirth Action and Implementation Plan to deliver its goal to reduce the rate of stillbirths by 20 per cent by 2025. The government has identified education and research as key areas of focus for this plan.

Radiologists have an important role to play in achieving this goal. In our submissions we have highlighted the role of radiology in supporting better pregnancy screening to identify pregnancies at risk and the underfunding of these services which has led to poor access for patients who are unable to self-fund.
We also highlighted the important role of radiology in investigating the cause of a stillbirth. While full autopsy, including imaging is the ideal, more than 50 per cent of parents do not consent to the procedure. Particularly for these parents, an MRI investigation can assist in identifying the cause of the stillbirth.
The Australian Federal Government has allocated $750,000 over four years to the College to increase the profession’s capacity to undertake stillbirth investigations and ensure that these services are available to bereaved parents who choose to access them. This is a great win for the College.
We have established a Stillbirth Steering Group to lead the delivery of this project. Over the coming months you will see and hear about educational courses to develop additional skills in stillbirth investigation and I encourage those with an interest in this area to engage in these opportunities.
We have reiterated to the Government that increasing the profession’s capacity to undertake stillbirth investigations is positive, however, without increasing the capacity of the health system to fund these investigations, patient access to these services will still be compromised.
Our advocacy continues, both to have better funding for pregnancy screening and better funding for stillbirth investigations.
“We have reiterated to the Government that increasing the profession’s capacity to undertake stillbirth investigations is positive, however, without increasing the capacity of the health system to fund these investigations, patient access to these services will still be compromised. Our advocacy continues, both to have better funding for pregnancy screening and better funding for stillbirth investigations.”Australasian International Breast Congress (AIBC)
The clinical year seems to be flying by, and much has been happening in the education and training space to keep us all busy. Series 1 Vivas were completed successfully in May with a transitioning of the examiners back to a central location in Melbourne.
As I mentioned in the previous June edition, an issue had been identified with the Reporting Work-Based Assessment (WBA). A review was undertaken and a new fit-for-purpose Reporting Work-Based Assessment was released in the ePortfolio system in mid July 2022. Trainees are now able to record multiple cases in a single reporting session, as originally intended.
The first evaluation of the newly launched Clinical Radiology Training Program will take place in October 2022, with a focus on the WBAs. WBAs were selected as the first evaluation area due to emphasis towards programmatic assessment and the changes to how work-based situations are assessed— the range, frequency and variety of supervisor feedback.
The evaluation will provide insight on the functionality of WBAs within the ePortfolio system including reviewing entrustability scaling, as well as identify whether the ideal number and types of assessments are built within the training program. If you are a trainee or have a supervising role, I encourage you to provide your feedback.

A comprehensive review of the Clinical Radiology Training Site and Network Accreditation standards has commenced and significant progress has been made towards completing the project plan within the anticipated timeline. The Accreditation Review Working Group (ARWG) has considered the results from an accreditation survey distributed to Network Training Directors, Heads of Department and Directors of Training and a best practice review completed on accreditation of specialist training in Australia and overseas.
The draft standards have been further refined and are nearing completion for presentation to the relevant committees and the focus will soon shift to the process of accreditation.
The College is undertaking a comprehensive review of selection into training processes and a five-phase framework which will meet the AMC re-accreditation requirements ensuring that the College’s selection policy is consistent, transparent, rigorous and fair. A Selection Review Working Group (SRWG) has been established and work has already commenced. At their first meeting in May, the SRWG approved the recommendations of the College’s cross-faculty selection review working group.
These recommendations include that the College take a more centralised and active role in the initial application process, while recruitment and selection decisions will continue to be made by the training networks. Consideration is also needed as to how the College can introduce mechanism/s to increase Aboriginal, Torres Strait Islander and Māori applicants as well as those from rural and regional backgrounds.
“A comprehensive review of the Clinical Radiology Training Site and Network Accreditation standards has commenced and significant progress has been made towards completing the project plan within the anticipated timeline.”
continued over...

From 2023, the examination timeline will change to better reflect the requirements of the new training program. The Phase 1 and Phase 2 written examinations have been separated to ease the potential burden on the hospital rosters. Examinations will continue to be held over two sittings during the year. For updated dates for 2023 please visit the examination section of the RANZCR website.
Work is underway for developing the new Phase 2 exams and multiple exam panels have met recently to progress. While the Clinical Radiology MCQ exam remains unchanged, the new Pathology exam will have 10 short-answer questions (SAQs) besides the 100 MCQs and extend to three hours.
The new case reporting exam will have a mixture of short, medium and long cases. The OSCER examinations will have seven stations across seven different topic areas, but questions within stations will also be explicitly mapped to other domains, such as observation, interpretation, management, pathology, anatomy, AIT/ patient safety and intrinsic roles. Sample questions for the new formats have been developed and will be released very soon.
These exams will be robust, more defensible and align with the new curriculum learning outcomes.
We go beyond simply meeting training requirements:
l Participants eligible to claim 117.5 RANZCR CPD points for the 5 day course and 67 RANZCR CPD points for the recertification course.
l Maximum allowable course based live and library cases for ANZ credentialing.
l Clinician led teaching by high volume operators.
l State of the art low dose, High Definition imaging.

l Unrivalled venue and catering.
2022 COURSE DATES:
5 Day Level A Course
12th - 16th May and 20th - 24th October
3 Day Recertification Course 14th - 16th May and 22nd - 24th October
For more information and online registration log on to: www.aicct.com.au or contact us at: info@aicct.com.au
Lung disease is an alarmingly common phenomenon in Australia. It can be difficult to detect early on and often progresses without symptoms until it reaches the incurable late stage where treatments are almost impossible.
Our objective at Lungscreen is to provide much-needed diagnosis and follow up services for individuals who may develop lungrelated illnesses such as Pneumoconiosis, Silicosis, or Lung Cancer. We aim to save lives by early detection and robust diagnostic follow up, preventing further lung damage before it’s too late.
To be part of Lungscreen and help save the lives of all Australians at risk of lung disease, contact us. info@lungscreen.com
Hi everyone,
What an eventful quarter! The introduction of the Transition to Fellowship Fee sure did throw the cat among the pigeons. We have grave concerns regarding the psychological and financial stress this fee will place on all trainees, but particularly final year trainees given the short turnaround between fee announcement and implementation. On behalf of trainees, the CRTC has engaged and will continue to engage with the College, the AMC, and the AMA regarding this fee. Disappointingly, these decisions which directly impact on trainees and our training were made by the Board without any consultation with trainees. Additionally, our interests on the Board were not, and are not, advocated for due to a lack of a trainee Board member and the inability of trainees to influence Board member composition as we are not afforded voting rights. For these reasons, the CRTC are petitioning for a
Board trainee representative in addition to trainees being able to vote in Board member elections.
Other focuses of the CRTC have been the new curriculum and ePortfolio, planning the trainee day for the 2022 ASM, how to incorporate artificial intelligence into training, cultural competency, and much more. The nominations have now closed for the 2023 CRTC positions and next quarter I will be able to update you with the new and shiny committee members.
RANZCR2022 is just around the corner, and it promises to be a great conference in the beautiful city of Adelaide. I am looking forward to a moderate amount of learning in addition to generous quantities of eating, drinking and socialising.
Hopefully I’ll see you there!
Dr Sarah Robertson Chair, Clinical Radiology Trainee Committee

The Professional Practice Committee (PPC) now has three meetings completed for this year and is planning to enter the last quarter of 2022 with a face-to-face meeting during the ASM this October. We anticipate this will be an energising gathering with a robust discussion on wrapping up the year and what’s coming up for 2023.
Some of the key pieces of work worth mentioning at this time include the following.
The College website now has a series of new CPD ePortfolio “how to” video guides available to assist you in navigating through some of the main processes required for submitting CPD activities. Each of the clips are only a few minutes long and a great go-to for additional instructions. You can access these clips now via the QR code or on the website.

It concerns me that many members are yet to start entering their CPD activity on the ePortfolio. I would like to emphasise that it is an annual activity and the requirements for 2022 need to be completed by 31 December. I earnestly request members do not to leave it until the last minute.
If you have any questions or require support regarding the CPD Program or ePortfolio, please contact the College team at CPD@ranzcr.edu.au
During June, representatives from the three CTCA parent bodies; RANZCR, CSANZ and AANMS attended a full-day workshop to troubleshoot the training guidelines for CTCA. Items that were discussed included:
• Pathways into and exiting CTCA
• Standardisation of quality of Fellowships
• Definitions
• Supervision roles and responsibilities.
The agreed next steps to progress the guidelines have been presented to the CTCA conjoint Committee for further work with plans to have the approved changes in place by 1 July 2023.
The ASM in Adelaide is a live/virtual hybrid event this year and it’s just around the corner! I am looking forward to seeing many of you there. A combined CR and RO CPD session will be held at the ASM, I hope you can attend. We’ll be talking all things CPD including:
• Looking back at 2022
• Plans for 2023 plus a first look at the updated CPD resources,
• Best practice guidelines for CPD participation.
This is a great opportunity for us to engage on this topic in a face-to-face format where we can look to what’s coming up next with the ePortfolio in 2023 and open the floor to questions which can be answered in real time.
The NZ ASM in Queenstown in August had a large in-person attendance and was a huge success. A combined CR and RO CPD session was conducted by Dr Carol Johnson my RO counterpart, Amy Young and myself. Dr Ken Clark, a member of MCNZ gave a very informative presentation virtually.
If you have any questions or comments regarding the work of the FCR Professional Practice Committee, please feel free to reach out by emailing the College team at professionalpractice@ranzcr.edu.au
Yours sincerely Dinesh
Associate Professor Dinesh Varma Chief of Professional Practice
One of the most powerful tools you rely on to help you treat cancer just got a lot more power. New capabilities for your TrueBeam® platform include soft tissue visualisation, high-precision SRS, and enhancements to motion management techniques—giving you the confidence to know you can deliver your treatments as planned. Take advantage of high-precision, highaccuracy cancer care for the most challenging cases you face today, and well into the future.
See the new capabilities of TrueBeam at varian.com/truebeam
Safety information: Radiation may cause side effects and may not be appropriate for all cancers. © 2022 Varian Medical Systems, Inc. Varian, Varian Medical Systems and TrueBeam are registered trademarks of Varian Medical Systems, Inc. Refer enquiries to Varian Medical Systems Australasia on 1800.657.036 or customerservice-anz@varian.com

As members of our College, we are proud to be awarded Fellowship to allow us to carry out our profession. The College provides education and training to our trainee members, sets the curriculum and standards for such training to be undertaken in the training centres and ensure that training outcomes are achieved with competence.
Indeed, the College spends considerable time and monetary resources to ensure these standards are met and to enable our trainees to graduate as Fellows who are internationally recognised.
Our volunteers (the many Clinical Supervisors, Directors of Training and examiners) are a vital part of this education and training processes. This is overseen by our Radiation Oncology Education and Training Committee (ROETC) led by the Chief Censor, Dr Yaw Chin; Deputy Chief Censors, Dr Lisa Sullivan and Associate Professor John Leung; Chief Accreditation Officer, Dr Vanessa Estall and Deputy Chief Accreditation Officer, Dr Anne Capp. The Radiation Oncology Phase 1 and Phase 2 Examinations is overseen by Associate Professor John Leung who is also currently leading the Phase 2 Examination Panel. Dr Apsara Windsor currently leads the Phase 1 Examination Panel.
There is a strong secretariat that supports our office bearers and the many volunteers of the Committees as well as undertaking the business of ensuring proper standards and processes are maintained.
In the Faculty of Radiation Oncology, I am very aware of the Fellows who spend a lot of time (voluntarily) to ensure that we ‘pass on’ the necessary knowledge and skills required to make a competent and highly valued radiation oncologist. On behalf of the Faculty and College, we acknowledge and thank you for your many unselfish contributions.

The College ensures that our training and education accreditation standards are met throughout the training networks and training sites: with separate standards for each of these. The College has the authority to remove a training site should these sites fail to meet and maintain these accreditation standards.
These standards change and as the practice of radiation oncology evolves, so too must the College review its accreditation standards. Over the next two years the Faculty of Radiation Oncology will undertake to review these accreditation training standards. The Accreditation Team lead by our Chief
Accreditation Officer provides this very important oversight function of these standards and processes.
However, the College itself has to meet certain standards to be authorised to deliver such an education and training program. These standards are set by the Australian Medical Council (AMC) and the Medical Council of New Zealand (MCNZ). These bodies also set assessments over cycles of every few years to assess and ensure that the College is continuously able to meet these standards.
In 2019, our College was accredited to deliver our education and training program with a set of conditions; with the need to self-report on work we must undertake to satisfy these conditions while maintaining the standards already achieved. This is not a task taken lightly as the implications of failure to do so would be enormous.
“In the Faculty of Radiation Oncology, I am very aware of the Fellows who spend a lot of time (voluntarily) to ensure that we ‘pass on’ the necessary knowledge and skills required to make a competent and highly valued radiation oncologist. On behalf of the Faculty and College, we acknowledge and thank you for your many unselfish contributions.”
While work has been affected by the pandemic, much has been achieved over the past two to three years as the College has satisfied more than half of the 30 conditions set in 2019 and is progressing well in the remainder of time until the next accreditation cycle. The work has been undertaken by the Specialist Training Unit of the College. There is much involvement of our Fellows, particularly in the ROETC and its sub-committees, who volunteer their time continuously and generously. The resources invested are substantial given the detail of reports required and the necessary resultant person-hours
required. The Faculty of Radiation Oncology Council and the Board are well aware of this and recently received an update on the report to the AMC. These external accreditation standards do not remain constant as the AMC and MCNZ standards are updated from time to time. For example, cultural safety especially from Indigenous health perspectives; transparency of trainee selection processes which are to be centralised; and management of conflicts of interest of examiners are items that have to be met as they are introduced over time.
Indeed, these accreditation standards evolve as both Australia and New Zealand develop progressive views on such education and training programs applicable to specialist colleges. This is also influenced by community expectations and regulatory imposts that change over the years.

As such, accreditation standards are applied to our College processes as much as we as a college and faculty apply our own standards to our education, training and professional practice.
As always, we need to have a “whole of College” approach (members and secretariat) to ensure our trainees and indeed Fellows continuously receive the best education and training program we can afford; and continue to make our College as highly respected as it is. There are certain “must-dos” and this is where much of our resources, whether fiduciary or voluntary, are directed to.
“As always, we need to have a “whole of College” approach (members and secretariat) to ensure our trainees and indeed Fellows continuously receive the best education and training program we can afford; and continue to make our College as highly respected as it is. There are certain “must-dos” and this is where much of our resources, whether fiduciary or voluntary, are directed to.”
With the new Radiation Oncology Training Program well underway now and the new Phase 1 examinations looming, we have encountered many queries from trainees, Directors of Training and Training Network Directors with regards to the unique situation that transitioning trainees find themselves in.
Despite the Radiation Oncology Training Program Handbook and the College’s Trainee Transition arrangement documents being available online, it was evident that explicit information regarding this subgroup of trainees is required.
A Frequently Asked Questions (FAQ) document resource was therefore developed and disseminated to provide additional clarity on specific Phase 1 examination scenarios pertaining to both new and transitioning trainees.
Following the approval of the RACP Australian Aboriginal, Torres Strait Islander and Māori Cultural Competency and Cultural Safety eLearning module as a mandatory component of training for Phase 2 trainees commencing in 2022, the Radiation Oncology Education and Training Committee (ROETC) also approved the updated the College’s Cultural Safety Online Trainee Resource. The updated website consists of a comprehensive list of online resources consisting of articles, podcasts, guidelines/frameworks, online modules, videos, eBooks and websites.

The current Radiation Oncology Accreditation Standards and Criteria for Training Networks and Sites hark back to 2016. A major review is therefore essential to align the standards, governance processes and internal processes and procedures to not only current best practice requirements, but also to the new training program.
In March of this year, the terms of reference for the Accreditation Review Working Group (ARWG) were approved, along with a project plan. Following this, the members to the group were appointed with an inaugural meeting held on 25 May.
In addition to analysing the results from the recent accreditation survey, the group conducted a best practice review on accreditation standards of specialist training in Australia and internationally.
Following this, a draft revised standards and requirements document for training sites has been generated and approved by the ROETC. The standards and requirements document for training networks is pending. I would like to thank Dr Vanessa Estall, Chief Accreditation Officer, in leading the ARWG in this crucially important work.
Over the past few years, the number of training sites has increased but the number of accreditation assessors has unfortunately been limited and assessors are often also involved in multiple other facets of College activities. Due to the COVID pandemic and the inability to conduct site assessments adequately, there is currently a significant backlog of overdue assessments which need to be conducted.
continued over...
“However, with an overwhelming number of assessments still to be completed, the ROETC made the difficult decision to temporarily cease the accreditation of all new sites until the current schedule of sites requiring accreditation is completed. I ask for your patience, as well as careful consideration to be involved in the Accreditation team, as it continues to struggle to function effectively with very limited resources.”
This prompted a College-wide expression of interest being sent earlier on in the year, with a number of volunteers coming forward to assist in this role. The new assessors are now being trained and mentored.
However, with an overwhelming number of assessments still to be completed, the ROETC made the difficult decision to temporarily cease the accreditation of all new sites until the current schedule of sites requiring accreditation is completed. I ask for your patience, as well as careful consideration to be involved in the Accreditation team, as it continues to struggle to function effectively with very limited resources.
I am happy to report that both the written and Viva Voce components of the Series 2 Phase 2 written examinations were delivered without any issues on 4–5 July and 22–24 August 2022 respectively. The Phase 1 examinations are scheduled to be delivered on Friday 9 September 2022.
A Phase 1 Examination Course was held online recently and was very well received by all trainees in attendance. Many thanks to Dr Apsara Windsor, Chair of the Phase 1 Examination Panel and Dr Bomi Kim, a current third year trainee who presented at the course.
The Phase 1 Examination in 2023 will, for the first time, allow trainees who commenced on the new Training Program from February 2022 to sit the three oncology sciences subjects individually.
New question items such as multiple choice and very short answer questions will also be utilised at that examination to allow for a greater breadth and depth to be examined across the Learning Outcomes.
At the request of the Radiation Oncology Trainee Committee and foreshadowing the formal Phase 2 Examination Course to be held later on in the year, Chief of Examinations, Professor John Leung conducted a Q&A session with candidates who are enrolled in the forthcoming series of the Phase 2 Examinations.
The session was held virtually, providing information to candidates on both the written and Viva examinations. Once again, this session was very well received by attendees.
On the forefront of the work being undertaken by examiners is ensuring the delivery of the examinations on the digital platform.
Examiners will soon start to use the Practique system with meetings set in place for both Phase 1 and Phase 2 examiners to familiarise themselves with the system and question platform. Following this, candidates enrolled in the 2023 examinations will also have ample opportunities to habituate themselves to the new system.


We go beyond simply meeting training requirements:
l Maximum allowable course based live and library cases for ANZ credentialing.
l 117.5/67 RANZCR CPD points available for the course.
l Officially sponsored and endorsed by GE Healthcare for more than 10 years.
l Live scanning at second highest global recruiting site in SCOT-HEART study.
2022 COURSE DATES:
5 Day Level A Courses:
12th - 16th May and 20th - 24th October
3 Day Recertification Course: 14th - 16th May 2022 and 22nd - 24th October

WATCH THIS SPACE: www.aicct.com.au
For Face to Face and online courses: info@aicct.com.au


With a crisis of such behaviour occurring in healthcare environments, surely we are reporting these events to encourage needed change? Unfortunately, the results indicated that only a third of people who personally experienced bullying reported it. And even less (a quarter) of people who witnessed a colleague facing bullying reported it. What is worse, is that over the last three years—the data has not improved.
the small hurdle. However, this group of dogs failed to learn the task—most of them did not even attempt it. They just laid down and passively accepted their fate. They had learned to become helpless. The sequelae of learned helplessness in humans reflect many of the symptoms of burnout: having low self-esteem, decreased motivation, lack of persistence, apathy, feelings of frustration and giving up.
After renewing my AHPRA registration, I completed this year’s medical training survey. I was interested to know what the results from last year’s survey were—so I looked it up (www.medicaltrainingsurvey.gov. au). In particular, I looked up the section from last year’s report on Workplace Environment and Culture— the information was shocking. The worst statistic was that of the 21,000 trainees surveyed in 2021: 35 per cent of them reported that they had either personally experienced or witnessed bullying, harassment or discrimination in the workplace over the last 12 months! Most of them had experienced it themselves (22 per cent). Even more concerning was that 51 per cent of those who personally experienced bullying reported that the person responsible was a senior doctor. In a large proportion of cases this person was their direct supervisor. The report did also highlight that another 30 per cent of cases of bullying were reportedly instigated by a fellow doctor-in-training. Arguably, we are modelling our behaviour at least in part on the behaviours of the senior colleagues we rely on to mentor and train us.
This phenomenon of experiencing bullying and not speaking up, has been attributed by some leaders in this field to a concept known as ‘learned helplessness’. This term was coined by Professors Martin Siegelman and Stephen Maier. They performed a number of experiments where dogs quickly learned to jump over small hurdles to dodge ‘avoidable’ electric shocks to their legs. In a subgroup of these dogs, they administered a series of ‘unavoidable’ shocks. They then administered the previous test to see whether the animals would escape ‘avoidable’ shocks by jumping over
The AMA position statement on bullying, discrimination and harassment from 2021 highlighted the adverse effects of these behaviours towards junior doctors—including absenteeism, turnover, increase risk to patient safety, quality of care and adverse outcomes. The framework provided by the AMA to change bullying culture highlights the need for structural changes at an organisational level. But ultimately it also requires a cultural shift among medical staff at all levels—that they do not have to accept being bullied, and that they should not allow bullying to occur to those around them either. Perhaps this will enable those around us who already feel helpless as a result of bullying, discrimination or harassment to speak up too.
It is one thing for doctors to champion anti-bullying sentiment in surveys and in the media. But as individuals, we must also be directly engaged with changing workplace culture to improve the health of our colleagues, our patients and ourselves. As former US president Barack Obama so eloquently said: “If we aren't willing to pay a price for our values, if we aren't willing to make some sacrifices in order to realise them, then we should ask ourselves whether we truly believe in them at all.”
Dr Hari Kirupananther
“As former US president Barack Obama so eloquently said: “If we aren't willing to pay a price for our values, if we aren't willing to make some sacrifices in order to realise them, then we should ask ourselves whether we truly believe in them at all.”
Global oncology company Varian, now part of Siemens Healthineers, is dedicated to creating a ‘world without fear of cancer’.
Patients are more engaged in their healthcare today. Access to large amounts of healthcare information means they can take a more active role.
“We’re ensuring that patient feedback is central to decisions around care,” explains Rebecca Cortiula, Senior Managing Director for Varian Australasia. “There is a multidisciplinary component to that, where physicians with different areas of expertise have to come in. They make decisions on the best treatment options for a patient, taking patient preferences into account along the way.”
By 2050, some experts think it will be possible to make cancer a manageable disease, similar to diabetes. “A cancer diagnosis will no longer hold the fear it does today - both for the patient and for their families. There’s a lot of emerging treatments that have the potential to deliver better treatment outcomes and improve both the convenience and the quality of life for cancer patients.
“It requires a multidisciplinary approach: radiation therapy, surgery, pharmaceuticals, in-hospital care, outside of hospital care. That continuation of care is really important for the patients and relies on the whole healthcare ecosystem working together and understanding where we fit into that continuum of care for the patient.”
Ensuring radiation therapy is part of this care continuum is central to Rebecca’s role, both from a financial and moral point of view.
“Ultimately the responsibility is to ensure
that we have a health care system that's sustainable and can continue to provide some of the best healthcare outcomes in the world for every dollar spent in Australia and New Zealand.”
“As a business, while we have a responsibility to deliver on financial metrics, we also have to deliver on customer satisfaction and employee engagement.”
Rebecca says this dedication to customer satisfaction stood out to her during the pandemic. “For me, I’ve learned just how far we are willing to go to ensure there is continuity of care,” says Rebecca.
“Many of the ANZ team have gone over and above during this pandemic - some of our team endured hotel quarantine to ensure there was no disruption to supporting our customers and patients. That was amazing!
“A lot of innovative ideas came through the team during this time. We’ve worked with the Australian Society of Medical Imaging and Radiation Therapy to create a registry of licensed radiation therapists, including Varian employees, to support departments. There was concern that teams would have to go into lockdown if there was a major outbreak in a hospital. To avoid a human resource crunch, this database was created to see if another radiation therapist would be needed to step in.”
In April 2021, Siemens Healthineers completed their acquisition of Varian. Cortiula believes the two companies can drive faster progress in cancer care together. “It means we can fast-track our vision for a world without fear of cancer,” said Cortiula. “It allows us to ensure the best outcomes can be
reached by combining people, technology and data. Siemens has some of the best imaging technology available. I see this as an opportunity to really accelerate our product development.”
So, what does the future hold for the combined businesses? “Varian’s approach is still centred around intelligent cancer care and driving progress for cancer care for the next 30 years and beyond,” says Rebecca. “I see us accelerating our use of software automated processes and helping oncology professionals collaborate and develop more precise and holistic cancer treatments. We’ll see greater cooperation between research institutions oncology practices. Multidisciplinary teams working together with a whole of care approach, so that no matter where the patient is located, they can get access to the best possible quality care.
Further information can be obtained at www.varian.com
All enquiries, please direct to Varian Medical Systems Australasia on 1800 657 036 or customerservice-anz@varian.com

A version on this article previously appeared in Global Healthcare, https:// healthcareglobal.com/brochure/variansrebecca-cortiula-world-without-cancer

Greetings. The FRO Professional Practice Committee (PPC) recently held its third meeting since commencing operations in January this year and our current focus is on the FRO CPD program, getting ready for the ASM in October and preparations for a new and improved Mentoring Program.
After a successful 2021 pilot, the College is relaunching its FRO Mentoring Program. This is an exciting opportunity for members who are interested in enhancing the trainee experience with a focus on goal setting and working with a diverse group of stakeholders to ensure the Mentoring Program is a continued success. With the support of the FRO PPC and the Mentoring Program Working Group, the College is in the process of redesigning the program ready to kick-off in the first quarter of 2023. Expressions of interest to join the Working Group are still open, if you want to participate or have any questions about this program, please email mentoring@ranzcr.edu.au
This year’s ASM in Adelaide is merely weeks away and I am delighted to be attending in person and sharing a presentation space with my CR counterpart, A/Prof Dinesh Varma, Chief of Professional Practice FCR. We’ll be talking all things CPD including:
• Looking back at 2022
• Plans for 2023 plus a first look at the updated CPD resources,
• Best practice guidelines for CPD participation.
I look forward to seeing you there!
The College’s website now has a series of new CPD ePortfolio “how to” video guides available to assist you in navigating through some of the main processes required for submitting CPD activities. Each of the clips are only a few minutes long and a great go-to for additional instructions. Use the QR code now to access these clips or you can access them via the website.

Please do not wait until the end of the year to try out the new CPD ePortfolio. We are entering the final quarter of this year. How are you doing? Have you recorded more than half the required activities? Do you have any queries? Let us know if you have concerns. If you have any questions about the CPD program, please contact the team at cpd@ranzcr.edu.au
The Professional Development Plan (PDP) is a new requirement of the College’s CPD program commencing this year. Members have the option to complete the template in the CPD ePortfolio or use a PDP that they may
have already done, for example, with their employer. Members can also enter this as a CPD activity and claim a maximum of two (2) hours toward their CPD. If you haven’t yet completed your PDP, I encourage you to do so as soon as possible. You’ll find an instructional video on this topic using the QR code above. If you have any questions or suggestions regarding the work of the FRO Professional Practice Committee, please get in touch at professionalpractice@ranzcr.edu.au.
I look forward to bringing you further updates on the work of the FRO PPC in coming editions.
Best regards,
Carol Dr Carol Johnson Chief of Professional Practice Faculty of Radiation Oncology

The Australian Council on Healthcare Standards (ACHS) Clinical Indicator Program is the world’s largest dedicated clinical indicator data collection and reporting service. The program was established more than 30 years ago, and today the clinical indicators cover 22 specialty medical disciplines, including radiation oncology and radiology, and more than 600 healthcare organisations regularly submit data to the program.
The aim of the Clinical Indicator Program is to assist organisations to identify areas for improvement, by detecting variations within or between health services. Participating organisations submit data six-monthly through an online performance indicator reporting tool. Comparative reports are provided to submitters and The Australasian Clinical Indicator Report is a publicly available summary report which is published annually.
The reporting of clinical indicators to the ACHS is optional and is not a mandatory component of the accreditation process. However, subscription to the Clinical Indicator Program is free for ACHS accreditation members, and members are encouraged to submit indicator data to demonstrate continuous quality improvement.
To ensure that the indicators remain relevant to current practice, the indicator sets are regularly reviewed and updated as necessary. Recently, a multidisciplinary working group met to review the radiation oncology clinical indicator set.
The working party consisted of members with expertise in radiation oncology practice, management and administration, as well as a statistician and a consumer. We assessed each clinical indicator against its relevance for clinicians, whether it was practical and worthwhile to measure, and if there was consensus on how the data would be collected and reported.
The sixth iteration of the radiation oncology set now has eight indicators, covering issues such as waiting times, unscheduled treatment prolongation, treatment plan peer review and use of motion management.
Monitoring and measuring quality should be a focus for all radiation oncology departments. These clinical quality indicators provide a standardised measurement tool to allow comparisons both within a department over time and between departments. The Radiation Oncology Working Party encourage more departments to contribute data to this program.
Dr Rachel Effeney Quality Improvement CommitteeProtect your health, access our wellbeing resources
www.ranzcr.com/fellows/general/your-wellbeing
“Monitoring and measuring quality should be a focus for all radiation oncology departments. These clinical quality indicators provide a standardised measurement tool to allow comparisons both within a department over time and between departments. The Radiation Oncology Working Party encourage more departments to contribute data to this program.”
continued from page 20...
You had a pivotal role in the development of this new technology as the project lead for direct conversion materials (the CdTe detector material). Can you describe your work and that of your team?
I’ve worked through different roles. I initially started out as a detector physicist, straight out of my PhD in 2007, with a focus on the CdTe material itself. My job was to measure and model the material, determine why we didn’t have the signal from the detector that was needed for CT, find out what signal was needed for CT, and then identify what property it was inside the crystal that prevented us from getting the response that we needed. Then, I had to discuss these findings with my colleagues in Japan to determine what we could change to get the properties that we needed for photon-counting CT. That was the first phase, at the end of which (in 2014) we had proof with a pre-clinical whole-body prototype CT scanner. These were assessed at three clinical sites, and we proved that clinical CT image quality was achievable for any body part. We then turned our attention to industrialising the processes. In a prototype, you can hand-build, handtune, exchange and refine components until it works. For serious commercial production, on the other hand, you need reproducibility and quality in your process, as well as scalability. In this second phase, the German and Japanese teams joined forces, to bring our German process engineering and quality skills, and combine them with the fundamental knowledge of crystal growth that our Japanese partners had. Bringing this together wasn’t easy, but we did a really good job of building a highly effective inter-cultural team. It allowed us to ramp up production. Now, in phase 3, we have a fully developed clinical scanner. The task at hand is to see what makes clinicians happy. To ask: what does the PCCT allow them to do that can’t be done with classical CT technology? And what are the differentiators? This brings us back to the first question that you asked.
So how many years of research and development went into this, from the start of phase 1 to when you went live with the first commercially available clinical, whole-body PCCT?
15 years. Even after the detector material is sorted, there is a long journey from a lab prototype to a preclinical prototype, then clinical prototypes, preproduction and finally serious production. You need to walk through each of these stages. This road takes longer for the pioneers than for those who follow, but they still need to go through these stages. Therefore, if we consider the question of silicon which you mentioned earlier, it is a new technology, and you still need to go through these stages. If you are only starting to scan humans, you can easily estimate from the timelines that we had how long it takes to have a product.
Was there a eureka moment for you and your team?
Overcoming the scientific barrier was a pivotal moment. You have such a huge parameters space to play with, with the crystal growth, the electrodes, and what you do with the detector response, with your readout electronics. Most of the things that we tried out in crystal growth had either no effect or a negative one. But once we found the parameter that really improved things, then we dug deeper, and it helped us to understand. Even the failures did help us to understand and model crystal growth. I remember this moment when we had the right parameter to crack the polarisation challenge in our hands, and then it got clearer and clearer that photon-counting CT will be feasible. I also remember standing there and saying: “this is too good to be true, there will come a setback”. But it never came. That was a little over 10 years, when, within one year, we made the transition from “maybe not feasible” to “will be feasible”. This was a really exciting time.
How long does it actually take to grow the CdTe crystals, it sounds like a very complex process with well-orchestrated steps?
It takes three months for the actual crystal growth step in our method, the travelling heater method (THM). But it actually takes longer, because THM is a two-step approach, with two kinds of crystal growth consecutively. First, we react the cadmium telluride to form a polycrystal that we then use as the feed stock in the second step THM. It’s very complicated. From filling the starting materials, cadmium and telluride, into an ampoule until we get to the finished crystal takes 6–8 months. Then there are further processing steps: slicing, polishing, photolithography to apply the electronics, making the module, and making the detector. The entire chain to make the detector takes more than a year! (see schematic on page 20).
So, what’s next in PCCT? Will there be other scanners using this detector?
We have to distinguish between the first clinical photon-counting CT product, and our photon-counting detector. The basic technology is an element inside the detectors. This will not change anytime soon, since there is very small potential to improve it in a way that radiologists would even notice. What we are working on now are applications. What do we do with the large amount of data coming out of the scanner? How do we bring this data to the user, so that they can make the best use of what the machine produces for clinical impact? We will focus on that, and provide applications and training to really harvest all the advantages that the technology offers.
“The entire chain to make the detector takes more than a year!”
“I also remember standing there and saying: “this is too good to be true, there will come a setback”. But it never came. ”
Do you participate in College activities, such as committees, examining, training, teaching and supervision?
Did you know you can claim these activities as part of your annual CPD requirements?
The College is currently transitioning the CPD program to meet the requirements of the Medical Board of Australia (MBA) and Medical Council of New Zealand (MCNZ). At the start of 2022, the College commenced the first annual cycle of CPD, with all members required to undertake the following:
• 50 hours of CPD
• Completion of a Professional Development Plan (PDP)
• MRI and Mammography CPD hours if applicable
• Annual conversation (New Zealand members, MCNZ requirement)
• CPD with a focus on cultural safety and health equity (New Zealand members, MCNZ requirement).
There are several CPD activities that can be recorded by members who volunteer their time at the College, whether that is as a committee member/chair, examiner, or those involved in teaching and supervision. Examples of these are detailed in the table below.
Please note, from 2023 onwards, you will need to meet a minimum requirement of CPD activity in each of the overarching MBA/MCNZ categories:
• Educational activities
• Reviewing performance and reflecting on practice
• Measuring and improving outcomes.
This may mean some changes to the way you currently record your CPD and the types of activities you are recording. You may not be aware that you are doing a number of different activities in your daily work that can be claimed as part of your CPD, particularly in the reviewing performance and reflecting on practice and measuring and improving outcomes.
In the meantime, if you have any questions regarding your CPD, please don’t hesitate to contact the College via CPD@ranzcr.edu.au. In addition, the CPD section of the College website has all the information regarding the CPD program requirements, ‘how to’ guides and video recordings to assist in using the CPD ePortfolio and other information resources such as Frequently Asked Questions, CPD handbooks and templates.
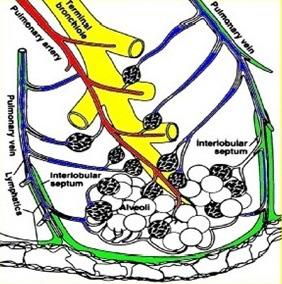
OGSIG’s AGM has been scheduled for Saturday 29 October at the College’s ASM at 7 am. Come along to meet the Executive, and to participate in voting and other matters. Virtual attendance is likely to be possible. Please contact myself or OGSIG@ranzcr.edu.au to become a member of OGSIG.
Membership is free and open to all members of the College.
OGSIG will be running a session at the ASM in Adelaide on Saturday 29 October at 1.30 pm where there will be fantastic lectures on Soft Signs, O-RADS MRI, Communication and Tubal Patency Assessment.
It is with great excitement that we announce that Dr Rachael McEwing will be convening a face-to-face meeting in 2023 in Adelaide on Thursday 23 March Prof Jon Hyett will be the keynote speaker.
Please diarise—we are looking forward to seeing lots of people there. There will be no virtual component, but lectures will be available on demand.
This will be OGSIG’s 3rd ASM, but the first time it will be face-to-face; it will be an excellent opportunity to network with both O&G subspecialists as well as general radiologists.

This meeting will be the day before the ARGANZ ASM/workshops—so why not make a long weekend of it and come to both!
Best wishes to all. I am always pleased to be contacted with anything O&G Imaging related.
Dr Emmeline Lee Chair of OGSIG emmeline@westernultrasound.com.auOn behalf of the ANZSNR ASM Organising Committee, we are pleased to announce our plans for the 2023 Annual Scientific Meeting (ASM).
Venue: RACV, Cape Schanck, Mornington Peninsula, Victoria

Dates: Thursday 30 March–Sunday 2 April 2023
We look forward welcoming delegates to the stunning Mornington Peninsula for our three-day ASM.
The meeting will commence at midday on Thursday 30 March and conclude at lunchtime on Sunday 2 April 2023.
A/Prof Ronil Chandra and Dr Elaine Lui are working with the scientific committee to develop a diverse program which will appeal to RANZCRaccredited trainees and radiologists with an interest in neuroradiology.
The concurrent three-day program will include a mix of interventional
neuroradiology, with presentations from our key industry partners, showcasing the latest technology and equipment, a diagnostic program and dedicated sessions for head-and-neck specialists.
We look forward to announcing our international and local teaching faculty when the provisional program is launched next month.
Early Bird Registrations will open from 1 November 2022. Delegates are reminded that ANZSNR members receive a discount. If you are not a member, we encourage you to join prior to registrations opening to take advantage of this great offer.
Join now
ANZSNR is open to all radiologists with an interest in neuroradiology, interventional neuroradiology or headand-neck radiology and welcomes new members to join.
ANZSNR has several categories of membership, including: Full members – RANZCR Fellow radiologists practising in Australia and/ or New Zealand
Student members – RANZCR trainees in accredited training positions, including those holding relevant fellowship training positions either in Australia and New Zealand or overseas.
Membership provides access to a range of members benefits and the opportunity to connect and collaborate with other radiologists with interests in neuroradiology, head-and-neck and interventional neuroradiology in both Australia and New Zealand. To join us, complete the short application form here: www.anzsnr.org.au/member-application

On behalf of the Interventional Radiology Society of Australasia Organising Committee, we wish to thank all delegates who attended our very successful 2022 Annual Scientific Meeting, held from 9–11 August in Queenstown, New Zealand on venous access, and intervention.
We’d like to take this opportunity to congratulate and thank the 2022 ASM Convenors, Prof Tim Buckenham and Dr Gabriel Lau, who successfully delivered an excellent scientific meeting, well attended, and appreciated by all.
Following a three-year hiatus on faceto-face meetings, it was a pleasure to see all colleagues together again and enjoying much needed opportunities to learn and network again.
Attendance at the three-day IRSA ASM equates to 20 hours of CPD and can be recorded under the ‘Educational activities’ category and by selecting ‘Conference attendance’. Certificates of attendance are being circulated via email and can be uploaded into the RANZCR CPD portal. For information, please visit RANZCR CPD.
Delegates are also reminded that the Scientific Program has been recorded and will be edited and made available on the IRSA website over the next month. Delegates will be notified when access to the recordings is granted as part of the IRSA webinar library.
continued on page 62...

This year saw the release of the first version of the Standards of Practice for Interventional Radiology (IR) and Interventional Neuroradiology (INR), representing the culmination of the first dedicated and comprehensive standards of practice for IR and INR in Australia and New Zealand.
These Standards offer a framework for a nationally consistent approach for interventional radiologists, interventional neuroradiologists, radiology leaders and hospital administrators to support the delivery of high-quality patient care and outcomes and are applicable to all IR and INR services across Australia and New Zealand.
We know that professional standards can establish minimum levels of performance, establish consistency and help reduce variation in care across multiple individuals and healthcare services.
These Standards set out what is expected across several domains, such as Governance and Coordinated Patient Care, with examples of what each healthcare service is accountable for and the evidence required to demonstrate that the Standard is met.
The Standards are based upon similar documents published by The Royal Australian and New Zealand College of Radiologists and the Cardiovascular and Interventional Radiological Society of Europe.
They include expectations that the patient safety must be central to system design and that the quality of care provided and patient outcomes are evaluated and compared to national and international benchmarks.
This approach demonstrates a renewed focus on improving patient safety by:
• Strengthening clinical governance arrangements to support safe clinical practice
• Promoting a culture of continuous quality improvement
• Providing guidance for the professional practice of IR and INR
• Detailing workplace health and staff safety.
The publication of the Standards marks a significant commitment by the College to improve the practice of IR and INR in Australia and New Zealand. Moving forward, radiology leaders will have to consider how they will consider
implementation of the Standards in their organisation.
At many leading institutions in Australia and New Zealand, we will not meet the Standards that have been set. The Standards provides us all with an opportunity to identify the system level gaps in IR and INR services, and work with radiology leaders, hospital administrators and funders to address them.
continued over...
“The Standards are based upon similar documents published by The Royal Australian and New Zealand College of Radiologists and the Cardiovascular and Interventional Radiological Society of Europe.”
“The Standards reflect what patients expect, and healthcare services now have a framework against which the standard of their IR and INR services will be evaluated.”
The Standards reflect what patients expect, and healthcare services now have a framework against which the standard of their IR and INR services will be evaluated.

This is a large step forward to safeguard patient safety, and I encourage all radiology leaders to step up and meet the challenge that has been set.
The development of the standards was undertaken by the College’s Interventional Radiology Standards Working Group and led by the Interventional Radiology Committee.
As always, the College welcomes your feedback on the Standards of Practice for Interventional Radiology and Interventional Neuroradiology. All feedback should be forwarded to standards@ranzcr.edu.au
Members of the Interventional Radiology Standards Working Group are: A/Prof Winston Chong (Chair), Dr Nick Brown (Chair, Interventional Radiology Committee), A/Prof Ronil V. Chandra, Dr Andrew Cheung, Dr Con Phatouros, A/Prof Gerard Goh, Dr Jim Koukounaras, Dr Matthew Lukies, Dr Colin Chong, Dr Martin Dobes and Mr Murray McLachlan (consumer representative).
Members of the Interventional Radiology Committee are: Dr Nick Brown (Chair), A/Prof Dinesh Varma (Chief of Professional Practice), A/ Prof Winston Chong, A/Prof Ronil V. Chandra, Dr Andrew Cheung, A/Prof Warren Clements, Dr Terry Kok, A/Prof Andrew Holden, A/Prof Will McAuliffe, Dr Craig Ferguson, Dr Wen Ter Kan, Mr Murray McLachlan (consumer representative).
continued from page 60...
Plans are already underway for our next ASM, planned for Sydney, NSW in mid-2023. The convenors are Dr Murthy Chennapragada, Dr Luke Baker and Dr Phil Chan. Venues are currently being sourced and interested IRs (this includes registrars, nurses, and radiographers) should keep an eye on the IRSA website for updates. We encourage everyone to take advantage of the early bird offering.
We would like to invite all College members (consultants, IR fellowship holders and accredited registrars) with an interest in IR to join IRSA. We have many member categories to suit all. For more information, including details of benefits offered and how to join, please visit:
www.irsa.com.au/join-us/
“As always, the College welcomes your feedback on the Standards of Practice for Interventional Radiology and Interventional Neuroradiology.”
Kia Ora Koutou. New Zealand’s 20 gold medal haul at the Commonwealth Games is well worth noting. Not sure we need to discuss the All Blacks though.
Thank you to all the candidates and the voters for the 2022 NZ Branch election. I’m pleased to welcome the following to the NZ Branch Committee:
• Dr Missa Amin
• Dr David Dow
• Dr Alana Heath
• Dr Verity Wood (re-elected)
• Dr Adam Worthington.
We look forward to having you on the Committee and helping to progress the College’s NZ activities and member concerns.
As always, the NZ ASM was a success— many thanks to Ben Wilson, Cameron Simmers and John North who convened. Thanks also to the Outshine Team and College staff who assisted with the planning and organising.
Highlights from the event include Dr Gary Ulaner’s PET/CT expertise, the in-depth gynae session on Saturday morning and the talk from the Health and Disability Commissioner, Morag McDowell.
I understand the radiation oncology sessions were equally interesting with a focus on SABR, led by A/Prof David Pryor.
Congratulations as well to the following registrars:
• Dr Hugh McHugh, winner of the Obex Medical Registrar Research Award
• Dr Harry Alexander, winner of the NZRET Poster Prize
• Dr Bomi Kim, winner of the FRONNZ Prize.

I’m certain many members are looking forward to next year’s NZ ASM which will be held in Queenstown 11–13 August 2023.
NZRET Pikimairawea Award
2022 was the first year of the NZRET Pikimairawea Award, which will be awarded each year at the NZ ASM. This year’s winners were Dr Melissa James (radiation oncology) and Dr Michael Hurrell (clinical radiology).

Dr James won for her contribution to teaching and education (notably her roles as DoT and examiner), College participation and advocacy (particularly around workforce issues) and her ongoing research.
Dr Hurrell won for his 45-year contribution to teaching, including postgraduate students, and his research.
It was a well-attended AGM held on 6 August at the NZ ASM in Queenstown. I appreciated all the members that came and shared their concerns. The concerns have been heard. Poor wording on EOIs, new admission to Fellowship fees and ethical referrals are issues of importance and I welcome ongoing discussion. It is important that our voices are heard across the Tasman, and it was good to have their presence at the AGM.
Additionally, feedback about the length of the AGM has been received. It is worth noting that most AGMs are finished in less than 20 minutes. Any lengthening of the meeting would come out of time currently reserved for scientific content. I am somewhat reluctant to make this change but am open to hearing views from members. Please email nzbranch@ranzcr.org.nz.
Kia kaha. Stay safe, vigilant and strong.











See why Australian College members are selecting Medical Wealth Advisory for all their lending needs.
Starting with a complimentary mortgage review service by a specialist adviser, Medical Wealth Advisory aims to identify ways for you to structure loans to reduce taxation, improve your interest rates, strengthen your equity position and fund new investments.
Through Member Rewards, you can look forward to:
• Complimentary Service: No fees or charges for using our mortgage lending service.
• Specialist Lending Solutions: Customised solution utilising products and services from a range of lenders.
• Extended Service Hours: After-hours services that allow you to book a day and time that suits you.
• Dedicated Relationship Manager: Single contact point to handle your entire lending needs.
• Cash Back Offer: In addition to any lender promotional offer.
To find out more:
• Call: 1300 41 81 61
• Visit: www.medicalwealthadvisory.com.au
• Email: ranzcr@medicalwealthadvisory.com.au

College members across Australia can choose Home Loan Solutions—a team of finance professionals to assist with all types of lending such as home loans, investment loans, commercial loans, SMSF loans, motor vehicle loans or personal loans.
When a College member establishes a residential home loan through Home Loan Solutions, either a purchase or refinance, the following rebates will occur:
• Home Loan Solutions will rebate the member up to 50 per cent of Home Loan Solutions’ Up-Front Commission*. College members will be paid 50 per cent of their rebate when Home Loan Solutions receive the commission (approximately two months after settlement) and the remaining 50 per cent 18 months after settlement if the loan is still in place.
• In addition, if a College member refers a successful application to Home Loan Solutions, that is someone who is not a College member, Home Loan Solutions will give the College member a referral fee of $500.
• Home Loan Solutions will rebate 10 per cent of Home Loan Solutions’ UpFront Commission* to the College.
*Note that the commission is calculated on the amount Home Loan Solutions receives less GST. Lenders pay different percentages in commission, but for an example on a $1.5M loan a College member could receive approximately $3,750 in rebated commission.
Home Loan Solutions can:
• Review your current lending and offer tailored advice to suit your circumstances.
• Filter through a huge range of products from multiple lenders with you, so you can choose a product that is right for you and not have to research alone. They are paid by the lender, so do not charge their clients for their services.
• Provide details of various grants or lender’s specials.
As Finance Brokers, Home Loan Solutions have an obligation to act in your best interest and will educate you to ensure you understand the loan you are applying for.
Contact Home Loan Solutions via the Member Rewards page.
Medical Financial Advisory Services Ltd (MFAS) provides specialised financial planning advice to health professionals across New Zealand and have been doing so for over 20 years. They have a comprehensive understanding of the opportunities and hurdles that RANZCR members may encounter throughout their career.
MFAS offers members a comprehensive range of services including:
• Investment advice and management
• Personal and business insurances
• Home loan lending and mortgages. MFAS know one size does not fit all, so they tailor strategies to specific goals, ensuring each strategy will work in a simple but effective manner. The MFAS team includes specialists in investment, insurance and mortgage finance to deliver a professional friendly approach to optimise efficiency.
There are three easy ways to access this offer:
• Simply send your details to MFAS and they will contact you
• Email your details to MFAS
• Call MFAS on 0800 379 325 Visit our full Member Rewards Program here.

Prof Valérie Vilgrain

University of Paris and The University Beaujon Hospital, Clichy, France
A/Prof Giuseppe Brancatelli


University of Palermo, Sicily, Italy
Dr Jonathan Richenberg
Brighton and Sussex University Hospital Trust, United Kingdom
ARGANZ WORKSHOP
Dr Richenberg and local faculty will deliver a workstation-based MRI rectum and prostate workshop.
Friday 24 March - Full Day
ESGAR LIVER IMAGING WORKSHOP

ARGANZ brings you a one day ESGAR liver imaging workshop with ESGAR faculty members Prof Valerie Vilgrain and Prof Giuseppe Brancatelli. The workshop will be in lecture and case-based discussion format.
Friday 24 March – Full Day


