




“






“
Life should be one big adventure but not at the expense of an exciting career.

Everlight Radiology offers a smarter way to address your work-life balance. A career in teleradiology allows you to work anywhere in the world. It’s your opportunity to spread your wings, explore life overseas and continue reporting on the most interesting emergency and trauma cases. All at a time that suits you, with no overnight shifts.
As part of an organisation that puts clinical excellence first, you will also benefit from mentoring, continuous professional development and a dedicated support team.
Join Everlight’s growing team of Consultant Radiologists and you too could be to enjoying this rewarding way to further your career and follow your dreams.

Sometimes we get our nose to the grindstone and we lose sight of the bigger picture. I’ve been very keen to improve my work-life balance. So I would recommend Everlight to anybody.”
– Consultant Radiologist at Everlight





















Fellowship opportunity
If you are a radiologist on a fellowship this is also your chance to keep your ANZ diagnostic experience current and earn extra remuneration.
For more information visit everlightradiology.com/careers
Live
the
of both worlds.
A Message from the President: Our Challenges in 2022
A Message from the CEO: A Respectful Conversation
Kid Gloves in the West
An Interview with Dr Chaturica Athukorala, Winner of an AIIA 2022 iAward
RANZCR Trailblazers: Professors Gillian Duchesne and John Earwaker
Volunteers in the Spotlight December Dr Jennifer Chang
ASM Sponsor Grant Recipients Enjoy RANZCR2022
Workforce Gender Disparity in Clinical Radiology
2022 Research Grant and Award Recipients, College Honours, Educational Fellowships
To Infinity and Beyond…a Wrap Up of Our Biggest Annual Scientific Meeting to Date
Targeting Cancer: Are We Winning?
The “Quiet Achiever” and the Road to the RANZCR Board: A/Prof Brigid Hickey
RANZCR Workshops, Courses and Events 2023
Celebrating the Life of Dr Gwen Pinner
My Farewell Dean’s Message: Faculty of Clinical Radiology
Chief Censor for the Faculty of Clinical Radiology: Training and Examinations in 2022
Changes: Where Are We and Where Do We Want to Be? A Message from the FRO Dean Radiation Oncology Trainee Committee
Quality Corner: How Well Do We Look After Men with Prostate Cancer?
New Zealand Branch News
What are your thoughts?
If you have thoughts or comments about one of the stories you have read in this issue, we want to hear from you. The submission of letters to the editor, articles and news items is encouraged. Please email any submissions to editor@ranzcr.edu.au
Have you moved recently?
Log into the MyRANZCR portal and ensure your contact details are up to date at www.myranzcr.com
Inside News is printed on Sovereign Silk. Sovereign Silk is produced in an ISO 14001 accredited facility ensuring all processes involved in production are of the highest environmental standards. FSC mixed Sources Chain of Custody (CoC) certification ensures fibre is sourced from certified and well managed forests.
Editor-In-Chief
Dr Allan Wycherley College In-House Editor
Lindy Baker
All rights reserved. No part of this publication may be reproduced or copied in any form or by any means without the written permission of the publisher.
Publication of advertisements and articles submitted by external parties does not constitute any endorsement by The Royal Australian and New Zealand College of Radiologists of the products or views expressed.
Inside News © 2022 The Royal Australian and New Zealand College of Radiologists® (RANZCR®)

The year that was, 2022, has conjured many challenges for the College, but it has also gifted us important achievements which demonstrate the capacity of our members and College staff to make progress in difficult times.

There's nothing like a pandemic to pressure-test a health system. And what a test it has been these last two years— it made organising a family gathering at Christmas look easy for a change. We continue to deal with the aftershocks of COVID-19, especially the deadly backlog of delayed investigations and procedures, but the silver lining in that dark cloud has been the revealing of serious weaknesses in our healthcare, aged care and disability insurance systems.
Thanks to the wake-up call from the pandemic, politicians of all persuasions are now falling over themselves to recognise the impact of chronic underfunding in public hospitals and offer big budget solutions. In the recent Victorian state election, Christmas came early for some as the major parties competed with each other to offer the most generous plan for new hospitals, hospital upgrades and scholarships for trainee nurses. The bidding war became so aggressive that it drew the ire of the Victorian Healthcare Association, which is rightly seeking a more transparent and orderly process to health funding.1
In a climate like this, if it is to last beyond the election cycles of our various governments, our political leaders need our help. Health commands a large slice of the available tax dollars and we can ill-afford to waste
them. Our College is among a number of respected voices advocating sensible, affordable policies in health care, each aimed at achieving high quality care with positive cost-benefits for patients and providers.
Not all solutions require big budgets. This year, at our ASM, the College collaborated with the National Imaging Facility to showcase research into new tools in artificial intelligence to
of this one condition.2 Underpinning the application of this research is the policy work done by the College to help guide the regulation of AI in medicine and manage risks and opportunities presented by the new technology.3
Earlier, we ran a successful campaign for the deregulation of Medicare-funded MRI services in rural, regional and remote Australia, lowering out-of-pocket costs and improving outcomes for patients in these areas.4 This coincided with the formalisation of our relationship with the Australian Indigenous Doctors' Association and the launch of a program jointly led by the College to increase numbers of non-GP specialist trainees among Aboriginal and Torres Strait Islander doctors.5 We issued an action plan to help improve Māori, Aboriginal and Torres Strait Islander health over the next three years6 and launched a video campaign aimed at increasing access to radiation therapy for patients subject to inequities in cancer care due to race, ethnicity, sexual orientation, gender, age and disability.
enhance point-of-care medical imaging. A beneficiary of this research is the Australian Epilepsy Project, which is working to bring gold-standard diagnosis, advanced imaging and precision treatment options for epilepsy to the broad community. Even a small improvement in freedom from seizure would save or extend thousands of lives and save billions in lifetime healthcare costs and lost productivity for sufferers
Our plan for formal specialty recognition for interventional radiology (IR) and interventional neuroradiology (INR) progressed another important step this year, with the issue in March of a position paper on the IR and INR range of practice, and then in October the first comprehensive set of standards for the preparation, delivery and follow-up of IR and INR services. These standards will help to reduce variability in service delivery in Australia and New Zealand and safeguard patient safety.
Clin A/Prof Sanjay Jeganathan
“In a climate like this, if it is to last beyond the election cycles of our various governments, our political leaders need our help. Health commands a large slice of the available tax dollars and we can ill-afford to waste them.”
Alpenglow Australia are seeking expressions of interest from radiologists to join two clinics located in beautiful Tamworth. Both clinics encompass a wide range of modalities, with platforms to support strong collaboration with subspecialist peers across the Qscan Group and on-site radiologists. Be part of a tight-knit community and join an organisation with a vision and reputation of uncompromising quality radiology.
Work and live in the rolling countryside, yet take advantage of being only an hours flight away from Sydney
Backing of the Qscan Group Executive and a collegiate doctor network across Australia

Members, we need to have a conversation. A respectful conversation.
There are numerous studies revealing that since the start of the COVID-19 pandemic, there has been a rise in bad or aggressive behaviour towards service providers. Some companies are including new messages on their automated telephone service warning callers not to be rude or aggressive to their staff and other companies are placing similar signage in their clientfacing outlets.
Sadly, this trend has been seen at the College, with staff reporting a rising number of negative email, telephone, and interpersonal interactions between Fellows, trainees, and staff. Some of these interactions have been so egregious that I’ve contacted the member to discuss their communication.
College staff are morally and legally entitled to a physically and psychologically safe workplace. There are substantial penalties in place for companies that do not ensure a safe workplace, and for those that transgress in this area. The College will be taking a robust approach to this issue and I make no apologies for that. The College will not tolerate behaviour that mocks, belittles, insults, abuses or unfairly criticises staff, members or stakeholders. It doesn’t matter if the person communicating the message did not mean the message to cross a line, or if they thought they were making a joke, or even if they thought their message was acceptable because they were upset that the recipient had not acted in the way they wanted them to.

It’s worthwhile thinking about our interactions with other people from their perspective and to really consider how your communication might be viewed by an independent third party.
• It is good practice that, if you must write a long and impassioned email, that you do so without any email address and you leave the email overnight and read it again the next day, removing contentious parts of the email so that it is concise, factual and free from mocking, insulting or belittling comments about staff, members, suppliers or other stakeholders.
• Carefully consider who actually needs to read the email—keep the distribution list to those who absolutely have to know
• Sometimes it is just better to simply pick up a phone and call the other person.
Telephone calls:
• Don’t make any telephone call in anger. College staff are instructed to terminate angry, mocking, hostile or abusive telephone calls and to report these to their manager.
Some tips for better and more professional communications are listed below.
Emails:
• Emails are a permanent record. The Australian Institute of Company Directors suggests that each email you write, should start with the words “Dear Judge”, because it could end up as physical evidence one day. And intemperate comments, read in a cold light, could come back to haunt an author.
• If writing an email, remember that this is a “cold” medium and that written messages are received without the surrounding verbal and non-verbal cues that an in-person meeting provides.
• Write down the points you need to get across, or the questions you want to ask, before you make that call and stick to those points during the call.
• If the call starts to get heated, call a halt to the conversation without blaming the other person and suggest reconnecting at another time when everyone has had the time to refocus, perhaps with a third party involved to keep the conversation on track.
“College staff are morally and legally entitled to a physically and psychologically safe workplace. There are substantial penalties in place for companies that do not ensure a safe workplace, and for those that transgress in this area.”
The College has been busy with housekeeping too, amending our articles of association to better represent our New Zealand members at Board and Faculty level and clarifying issues related to the ethical use of referrals in radiology, especially in regard to NZ practice models. This last topic generated much feedback from members with frankly divergent points of view and some dissatisfaction over the College's role. It is a challenge we will continue to address next year.
The other challenges of 2022 include issues both outside and within our control. In the former category, the critical shortage of iodinated contrast media agents. The College lead the way in managing this shortage, providing advice to government, members and the wider health community. I was very impressed to see other suppliers such as Guerbet swooping in to assist by seeking urgent TGA approvals to bring stock to Australia. As the situation normalised, Guerbet has been left with excess stock which cannot be used after February when their TGA approvals expire. Guerbet will be left with no
continued from page 5... continued from page 7...
• It is good practice to summarise the conversation and any agreed actions at the end of the conversation, then confirm these in an email.
• Be conscious of your body language and your tone and level of voice. Refrain from generalising comments or comments that belittle or insult the recipient(s).
• Try not to shout or talk over others and make space for everyone to have a say.
• If you feel things are getting heated, suggest a five-minute break away from the meeting room so that everyone can collect their thoughts and consider alternative ways to get to a shared outcome, or disengage and suggest that the issue needs to be escalated for consideration.
Staff don’t always get things right. They are human and they make mistakes. At other times, they may be bound by rules or processes that have been put in
choice but to destroy the contrast. They supported us in our hour of need, and I encourage members to reciprocate now by utilising Guerbet’s stock before the TGA deadline.
Among the challenges within our control is our financial management and the absolute need to increase College revenue to meet the higher costs of a new examination system. The changes brought by the Board, which have stung some members and trainees, were entirely necessary to ensure the College actually has a few more new years to look forward to.
Finally, on a personal level, 2022 has challenged me as your President in ways I had not fully anticipated as a former Dean of Faculty. The President has a demanding role, not just because she or he is the usual target of members' emails, but because the job requires a focus on both specialties, an awareness that their actions affect all members and, as a key member of the Board, a strong sense of responsibility for decisions that determine the College's strategic direction and long-term sustainability.
It has been a challenging job for me this year on top of my other challenging job as a clinician, but immensely satisfying. I try to do both in much the same way: listen and learn and do the best you can for those you serve.
If the festive season has special significance for you, have a joyous Christmas and Happy New Year; if it doesn't, have one anyway, because you probably deserve it.
1 https://www.theage.com.au/national/victoria/ call-for-transparency-on-merits-of-victorianelection-hospital-cash-splash-20220926p5bkyp.html
2 https://n.neurology.org/content/95/24/e3221
3 https://www.ranzcr.com/whats-on/newsmedia/570-ranzcr-position-paper-on-theregulation-of-artificial-intelligence-in-medicine
4 https://www.ranzcr.com/whats-on/newsmedia/551-ranzcr-applauds-the-deregulation-ofmri-services
5 https://aida.org.au/app/uploads/2022/03/ AIDA-RANZCR-STSP-FATES-funding-mediarelease-FINAL1.pdf
6 https://www.ranzcr.com/whats-on/newsmedia/550-action-plan-maori-aboriginal-torresstrait-islander-health
place by members at Board or Faculty Council level, or by senior management. But when things are not going the way you would like, it’s your choice how to respond. A good approach is to contact the staff member about the issue directly and respectfully and if the issue cannot be resolved, then escalate to their manager or to the relevant committee.
Our College staff are here because they want you and the College to be successful. They understand the incredible difference our members make every day, often under difficult circumstances, and they want to support each of you. The College staff care. When we get it wrong, we will accept responsibility and do our best to rectify the situation, keeping our members informed as to what they are doing to resolve things. Your respectful communications with our people can help us to give you all the support you deserve.
“Staff don’t always get things right. They are human and they make mistakes. At other times, they may be bound by rules or processes that have been put in place by members at Board or Faculty Council level, or by senior management. But when things are not going the way you would like, it’s your choice how to respond.”
The work of women in radiology has often been hidden from history. An early pioneer was Anna Hammann, who studied under Wilhelm Roentgen and went on to make outstanding contributions to radiation therapy. Hamman was the first female radiation oncologist in the US, where she developed a habit of always wearing pearl-buttoned kid gloves, to the amusement of her male colleagues.
Half the way around the world, the first use of radiology in Western Australia was in 1896, when innovator radiologist William Hancock demonstrated the new technology at the Perth Public Hospital. He took ‘a beautiful negative of a lady's hand through her kid glove’.
It’s not known who the first female radiologist in WA was, but we do know that the radiology profession in that state has come a long way, with 408 College members currently based in WA. Of these, 130 are women, and they are succeeding in their continuing commitment and focus on providing the highest quality service to the community of Western Australia.
Meet four of these Western Australian radiologists: three are College Life Members, and one an emerging star.
At the 2022 ASM, the College was proud to award Life Membership to Dr Fiona Bettenay, ClinA/Prof Anita Bourke and Clin A/Prof Elizabeth Wylie. All three have made outstanding contributions to Western Australian breast imaging over the past few decades, as well as to the College and the broader profession.
Dr Fiona Bettenay has worked tirelessly for the betterment of radiology in Western Australia for forty years, in particular with her contributions to improving the standard of paediatric radiology in Western Australia.
Dr Bettenay was awarded the Beazley Medal and the AMA prize on graduation, and her subspecialist interests were paediatrics, women’s imaging and medico-legal. She was appointed to Princess Margaret Hospital (PMH) in 1989, and was Head of Department at PMH from 2010 to 2016.

In 2015, she was appointed the Branch Education Officer for WA and Network Training Director for WA Radiology Training Program. She has also held various council and board positions with Medical Defence Australia since 1996. In 2019 she was awarded the Professor Turab Chakera Award for excellence in radiology teaching.
Dr Bettenay retired from clinical practice in paediatrics in 2019, and continues to work in mammography, providing screen reading and assessment services and paediatric post-mortem imaging at PathWest.
Dr Bettenay has been an examiner in paediatrics for the College since 1996 and is remembered by many for coaching a generation of trainees through their paediatric Vivas. With contributions to public radiology service, outstanding teaching and mentoring, she has devoted herself by way of afterhours tutorials and the mentoring of exam candidates. In turn, she is loved and highly respected by her trainees for her exceptional teaching and generosity.
She couldn’t be happier with her important role in her profession: ‘I consider myself fortunate in my choice of career. My proudest achievement is to have been a teacher and mentor to a generation of trainee radiologists.’
“She couldn’t be happier with her important role in her profession: ‘I consider myself fortunate in my choice of career. My proudest achievement is to have been a teacher and mentor to a generation of trainee radiologists.”
Clinical Associate Professor Anita Bourke belongs to the Faculty of Health and Medical Sciences at the University of Western Australia (UWA). She was the first dual-trained nuclear physician and senior breast radiologist in Western Australia.
Clin A/Prof Bourke worked as a consultant radiologist at Sir Charles
Gairdner Hospital and at BreastScreen WA for more than thirty years, introducing multiple new imaging and interventional breast techniques, including the introduction of the breast MRI service, breast tomosynthesis and ROLLIS seed localisations.
During her career she has mentored many trainees, running breast imaging
tutorials and preparing them for their clinical radiology examinations. She has also served as a College Examiner and as a member of the College’s Breast Imaging Group for many years.
Clin A/Prof Bourke is also a member of the WACOG Breast Collaborative, MR Breast Interest Group and was involved in WA Cancer Workforce Planning. She is an accreditor for BreastScreen Australia and her research is very well known.
Clin A/Prof Bourke also successfully undertook a Bachelor of Arts at UWA, in French and Italian, winning the Nisbett Prize in 2009. She is a member of Dalkeith Rotary Club and helped to set up the Nokor Tep Women’s Hospital in Cambodia, developing their programs and co-ordinating donations from Sir Charles Gairdner Hospital. She retired from BreastScreen WA in 2021, and has been a tireless teacher, and is beloved by innumerable radiology trainees for her support and teaching.
Clinical Associate Professor Liz Wylie is highly regarded in Australia and New Zealand for her contribution to breast imaging and clinical radiology. She belongs to the elite club of HR Sear Prize recipients for the most successful candidate in the Part 2 Clinical Radiology examinations.

Clin A/Prof Wylie has taught generations of radiologists in Western Australia, and she remembers the start of her journey in the medical profession. ”Doing radiology made me realise how an inspiring teacher can have such an influence on you as a student. I remember one of the radiology registrars doing a tutorial for medical students when I was in fifth year at
Princess Margaret Hospital. He made it fun, and I thought ‘I can do this!’”
In 1980, she graduated from the University of Western Australia. She completed her residency at Royal Perth Hospital in 1982, and trained in diagnostic radiology before completing overseas fellowships in 1988–89. She continues her work as Clinical Associate Professor at Royal Perth Hospital, and is also consultant radiologist there, and Medical Director of BreastScreen WA. Her work in many WA and Australian breast cancer groups is well known.
Clin A/Prof Wylie pioneered the use of ultrasound and stereotactic fine needle aspiration, core biopsy and vacuum assisted breast biopsy.

“She is a member of Dalkeith Rotary Club and helped to set up the Nokor Tep Women’s Hospital in Cambodia, developing their programs and co-ordinating donations from Sir Charles Gairdner Hospital. She retired from BreastScreen WA in 2021, and has been a tireless teacher, and is beloved by innumerable radiology trainees for her support and teaching.”Clin A/Prof Anita Bourke
Clin A/Prof Wylie is very happy about the rise in awareness of breast screening, “I love the work,” she says. “I love the interaction with women— being in a clinic and making small talk and doing procedures as painlessly as possible. It’s also surprising—but heartening—at the level of joy there is amongst the staff and participants in the clinics. It all gives me and the multidisciplinary team a strong sense of purpose.”
Sir Charles Gairdner Hospital. In 2019, Dr Lee was honoured as Australasian Sonologist of the Year by the Australasian Society of Ultrasound in Medicine.
reminded her audience to reimagine gender disparity in radiology. ‘We know the College supports women, but the College can’t do it alone … women need to step up too”.
These three professionals are paving the way for emerging leaders in WA. They have worked with many other women in their professional journeys, including our final highlighted member.
She is an enthusiastic teacher of radiology trainees and sonographers, and was the recipient of the Prof Chakera Award for Radiology Teaching in 2014. Her favourite time of the week is making tea for the radiology trainees on Thursdays. Dr Lee is the lead examiner in Obstetrics and Gynaecological Imaging for the College’s Part 2 examinations, and she started the WA Women’s Radiologist group.
She is the inaugural and current Chair of the College’s Obstetrics and Gynaecology Special Interest Group. Her research interests have led her to be on the Editorial Panel of Diagnostic Imaging Pathways, a suite of imaging guidelines that has been developed over twenty years and is endorsed by the College. She is the Expert Advisor for Obstetric Imaging in the popular website, Radiopaedia, and is co-lead in obstetrics and gynaecology for Radiology Across Borders. Through these and other avenues, Dr Lee volunteers her time regularly to share her expertise with radiologists and other doctors in the developing world, including in Samoa and Vietnam.
Women like these four members have been, and continue to be, vital for bringing improved care for the people of Western Australia. They train their junior colleagues, and handle their patients, with kid gloves.
Dr Emmeline Lee trained in Western Australia, graduating in 1994, and then undertook sub-specialist training in women's imaging and in breast imaging, and since then worked as an obstetrics and gynaecology ultrasound and breast imaging sub-specialist radiologist. She is the Director of Western Ultrasound for Women, and radiologist at Perth’s
The topics of women in the radiology profession, and women in medical leadership, are dear to Dr Lee’s heart, and one of her roles at the recent ASM was to moderate the panel on Women in Medical Leadership. The panel, of six leading women radiologists, tackled some important and vital issues, including the unacknowledged barriers to advancement in the profession, gender diversity in medical student cohorts, gender equity strategies, and

“She is an enthusiastic teacher of radiology trainees and sonographers, and was the recipient of the Prof Chakera Award for Radiology Teaching in 2014. Her favourite time of the week is making tea for the radiology trainees on Thursdays.”
“I love the work,” she says. “I love the interaction with women—being in a clinic and making small talk and doing procedures as painlessly as possible. It’s also surprising— but heartening—at the level of joy there is amongst the staff and participants in the clinics. It all gives me and the multidisciplinary team a strong sense of purpose.”
 Dr Chaturica Athukorala
Dr Chaturica Athukorala
cases, the accuracy and relevance of our reports is affected and in some cases we have no choice but to recommend potentially unnecessary repeat or followup imaging, which can be detrimental to the patient and does not necessarily improve their outcomes.
that we surveyed indicated that the inability to efficiently access patient imaging caused delays in their day-today practice.
Congratulations, you recently won Start-Up of the Year at the Australian Information Industry Association (AIIA) 2022 National iAwards for the development of Aurabox, a cloud-based, medical imaging storage, viewing and collaboration platform for doctors and patients.
Can you tell us more about the benefits Aurabox offers to clinical radiologists and radiation oncologists and other clinicians?
Thank you so much!
I developed Aurabox with my team to solve a problem that radiologists face multiple times a day—the inability to access a patient’s complete imaging history in one place. I spend a considerable amount of time attempting to locate and view previous imaging to accurately interpret the imaging that I am reporting, and generate a clinically meaningful report. We have all received requests to “assess progress” of abnormalities for which we have no previous imaging or found an abnormality that we are 99 per cent sure is benign but have no previous imaging to confirm stability. In these

Colleagues in other specialties including radiation oncology experience the same frustration when attempting to access patient imaging, particularly when caring for complex patients who require multi-modality and serial imaging for diagnosis and monitoring.
We conducted a survey of these specialists and found that the majority were unable to access necessary patient imaging for at least one patient every day. One hundred per cent of specialists
Aurabox solves this problem by allowing a patient’s complete imaging history to be accessed in one place, regardless of how many medical imaging practices they visit. Because it is cloud-based and aggregates imaging from providers, Aurabox allows doctors to share patient profiles containing complete imaging histories with their colleagues quickly and easily. The Aurabox multidisciplinary team (MDT) function allows an MDT meeting to be run from a single platform, negating the need for the MDT radiologist to access multiple, disparate imaging platforms during the meeting which is time consuming and can make comparison of imaging performed at different practices difficult and inaccurate. Aurabox is also beneficial for doctors conducting research involving imaging protocols across multiple sites as it facilitates collaborative collation and a single point of access for all researchers without geographic constraint.
And to patients? How can patients be involved in management of their care? How does it improve their care journey? What is the ideal— clinician input into Aurabox or patient input?
We conducted a quality improvement pilot study at the Canberra Region Cancer Centre earlier this year and received positive feedback from several of the enrolled patients on how Aurabox improved their care journey.
One patient had a newly diagnosed brain tumour and had imaging performed at four different medical imaging practices outside of Canberra for his work up. Prior to trial enrolment, several of his imaging studies had
“Following his initial surgery and radiation, he decided to undergo chemotherapy in Sweden and his Aurabox profile containing his complete imaging history was able to be shared with his Swedish oncologist within minutes. This allowed her to review his imaging and formulate a treatment plan prior to his arrival without placing any unnecessary burden on the patient.”
to be copied to USB and posted to Canberra for his specialist to access them. This delayed his treatment planning and caused him considerable stress. Following his initial surgery and radiation, he decided to undergo chemotherapy in Sweden and his Aurabox profile containing his complete imaging history was able to be shared with his Swedish oncologist within minutes. This allowed her to review his imaging and formulate a treatment plan prior to his arrival without placing any unnecessary burden on the patient.
He was able to compare his experience pre- and post-Aurabox and credited Aurabox for making the process of sharing his imaging with his overseas specialist seamless and stress free.
Another patient with metastatic melanoma found it useful to be able to view her complete medical imaging history and reports within her Aurabox profile so she could better understand the chronology of her condition. She developed adrenal metastases during the trial period and found Aurabox to be of “immense value” at that time as she was able to provide access to her complete medical imaging history to her radiation oncologist at Canberra Hospital, radiation oncologist at Prince of Wales Hospital in Sydney and her surgeon at Canberra Hospital who performed her adrenalectomy.
How widely might it be used in the future? Are there any constraints for uptake? How scalable is the innovation?
Currently, Aurabox is targeted at patients with complex medical imaging requirements such as oncology patients. However, we know that there is benefit for almost every patient, so the potential reach is very wide. If you look at the kinds of organisations which are currently using or considering Aurabox, there is a very diverse range, including healthcare providers, cancer hospitals, research organisations, as well as individual specialists.
We can scale Aurabox as far as required to make it work for users across the healthcare system. Modern software development makes it relatively easy to build systems that can scale without the overheads of traditional software. Aurabox has been designed and built from the beginning as a flexible system that can be scaled to meet demand elastically. For example, the service we built to power our viewer uses technology known as “serverless” to deliver imaging at the maximum speed available to the user, regardless of how many users we have. We can deliver a complete PET scan to the viewer in less than two minutes, for every user. Images in our viewer are displayed in full quality DICOM as opposed to the lossy, non-diagnostic JPEG format, which is displayed by other cloud-based viewers on the market.
Currently our focus is medical imaging however we plan to add other patient assets to patient profiles including pathology and correspondence between doctors in their care team.

Both! Both patients and doctors can upload, store and share medical imaging within patient profiles on the Aurabox platform. This caters for patients who want to be more involved in their care as well as those with limited digital literacy. Aurabox also offers a concierge service to both doctors and patients to assist them to use the platform.
Australia is the perfect place to kickstart the platform. We have issues with accessing imaging across jurisdictions and health systems, between public and private providers, and in remote and regional areas. Aurabox can help to solve all these challenges, by providing a central place to aggregate and view imaging from private and public imaging practices and crossing state and territory borders.
But no matter where you go in the world, most countries have similar issues, and because DICOM has been
standardised since the 1980s Aurabox can effectively drop in anywhere and be compatible with local systems from day one. So, we do see ourselves expanding to other countries in the future. The challenge for us will be scaling it in a way that does not reduce the quality of the service that we provide and continue to deliver on our mission of helping doctors deliver better care for patients.
Can you identify any other areas that could benefit from innovation to improve communication and efficiencies in sharing information between clinicians, between different specialties, in health care in Australia and New Zealand? And beyond our jurisdictions?
The status quo for accessing patient data means that a considerable amount of time is wasted performing unnecessary administrative tasks. I am sure we all agree that we can improve efficiency across the board, whether that be accessing clinical notes, medical imaging, pathology, referral letters or making referrals to our colleagues. The sub-specialty nature of medicine means that most patients have more than one doctor in their care team. The inefficiencies that we face become exponentially worse as each member of the care team attempts to access the patient data they require and collaborate with colleagues in other specialties.
I believe the cause of the problem is the organisation-centred approach that we currently have for storing healthcare data for patients. This results in multiple, siloed storage systems which do not communicate with each other. This is highly problematic because each silo contains critical patient information that needs to be evaluated concurrently with other information held in a disparate silo to optimise patient care.
A collective approach is key to solving this problem. Existing databases need to be integrated in a patient-centric manner in addition to the development of new, innovative solutions like Aurabox. A further critical ingredient for success is the involvement of us, the end-users, when developing solutions. We all have fantastic ideas for how our day-to-day workflow can be optimised and I would strongly encourage you to become involved in the development of solutions where you can.
More from our RANZCR Trailblazers series with excerpts from the oral history interviews made in 2016 by the then College archivist, Ms Eva Stokes-Blake.
In this edition, read on for insights and recollections from Professor Gillian Duchesne and past president Professor John Earwaker.
In these excerpts we see how both recognised the opportunities to follow their interests and curiosity, demonstrating the importance of taking a decision and sticking with it. We see also their dedication to clinically and educationally advancing the professions and importantly, their dedication to care and to patients.
We thank Eva Stokes-Blake for her invaluable work in amassing oral histories for future generations of radiologists and radiation oncologists. We would also like to invite your expressions of interest to actively participate in clinician-to-clinician interviews of RANZCR Trailblazers (of your nomination), more details are available via editor@ranzcr.edu.au.

Access the full recordings from the two interviewees for much more detailed history of the professions and the College here: www.webcast.ranzcr.com/ Mediasite/Showcase
We hear first from Professor Gillian Duchesne on her dedication to putting patients at the centre of their care. Prof Duchesne’s most fundamental advice is “whatever you’re going to do, you can’t be faulted if you look at it from the point of view of how it’s going to affect your patients.”
You know it’s funny, I don’t know how many people plan from day one how their careers are going to pan out. You have to be prepared to be flexible, to take the opportunities as they appear. I already mentioned that my mentor in Bristol said, “Did I really what to do academia or did I want to be a jobbing physician?” When I got to the Marsden the academic environment there was just fantastic, so I did three and a half years registrar training and got my fellowship. Then I disappeared off into the labs for two years to do a doctorate in cell biology which …was absolutely fascinating, superb; people said ‘you’ll miss the clinic’, but you actually don’t because you get so much more out of that. Understanding the scientific method then allows you, when you to come back into the clinic, to look at things from a different perspective.
So I did two years of doctorate and then returned to the clinical world as a senior registrar again at the Marsden and I was attached to the academic unit which specialised basically in neurological tumours. I had two years doing that.
I started writing papers myself, which is something you really have to learn to do, someone has to guide you through it to start off with but I was hooked on the academic world then. At the beginning of 1989, I was fortunate to be appointed senior lecture at University College London with a consultant appointment at Middlesex Hospital. I was there for seven years and I don’t think I have ever worked quite so hard in my life. But it was an extraordinarily interesting time, I had a full clinical load but I was very well supported by a good
clinical team. I continued to run a small lab program although at that stage it was quite difficult to balance everything out. I set up and ran a master’s course in the science of oncology, so cancer science masters, which was fantastic. In fact, it was one of the things that contributed to us receiving the Queens Award for higher and further education. Which was great. We all tripped off to Buckingham Palace and met Her Majesty and Her Majesty’s husband and got a nice award for that. So that was good.
However in late 1995–96, Prof Lester Peters took over as Director of Radiation Oncology at Peter Mac and he was looking for academic radiation oncologists and I was offered the chance to come out here and have a look at Peter Mac and see whether I wanted to join in. The moment I landed, it sounds trite but it’s not, the moment I landed in Australia, I loved the country and the environment of Peter Mac was just buzzing and thriving, Lester had just come in and was re-vamping things and it was such a superb opportunity. So I made the great decision to jump with both feet first. But you do that if given an opportunity like that. I was then in my early 40s. If I wasn’t going to do it then, I never would and so we came out here
in September 1996, so I’ve just done the 20 years here and I have to say, I haven’t looked back.
The opportunities have been superb; clinically, academically but also in terms of developing my leadership profile which was almost serendipitous. Not something I necessarily planned to, I was always interested in finding out a little bit more, getting a new perspective on something, giving something back and I was somebody who just couldn’t say no. The opportunities, as I say, were superb.
I think it’s really pertinent to say for the archives, that patients are now part of the partnership and it’s one thing I’ve always wanted to strive for, is to make a patient feel that you are actually working together to get an outcome and get rid of the patriarchal view that we make decisions for you but rather we will discuss it together and sort it out.
We should/ I should mention, give tribute to a wonderful person called Ian Ruth, I don’t know if you have ever come across him, he was an academic at Peter Mac in the labs at one stage and went into education and worked at the University of Melbourne. He got prostate cancer about 15 years ago— aggressive. I was fortunate enough to be his physician and treated him and he became the most wonderful patient advocate for men with prostate cancer but more than that for patients with cancer in general, ensuring good access and so on. He’s done a lot of work, did a lot of work with the College and with both state and federal government to ensure that people had equitable access to radiation therapy and so on. He unfortunately died from his disease about 18 months ago, but he was a model of how the patient as the consumer and the professionals as the care providers can work together to improve how care is delivered. He was an inspiration to a lot of people.

I think the fundamental bit of advice I’ll give is whatever you’re going to do, you can’t be faulted if you look at it from the point of view of how it’s going to affect your patients. The patients come first—are their outcomes going to be better, how might they be effected by anything I do? If you take that tenet and you work through even if you come away with something that isn’t popular or it’s political—not a happy choice—you can’t be shot down. You are doing it for the patient not yourself and I think that’s an incredibly strong tenet.
I graduated in medicine in 1962 in Brisbane. My ambition was to be an orthopaedic surgeon Sadly,18 months later I was diagnosed with ankylosing spondylitis. It was then that I realised that going forward there was the prospect of a physical impediment to any career which involved procedural work.
So after showing some initial interest in radiotherapy, I ultimately opted for a career in diagnostic radiology, which I began in 1965 a as a registrar at the Royal Brisbane.
I was the registrar at the Royal Brisbane, which was then called the Brisbane General Hospital. The staff consisted of a director, a deputy director, one staff radiologist and three registrars. The total throughput in that department at that time was something like 70,000 examinations a year, so it was grossly understaffed. There was virtually no formal teaching of the trainees. You learnt on the job, and it was vastly different from what it is today. So, in 1967 with the help of John Masel we introduced the first Queensland Branch Registrar lecture series.
You've held a lot of different positions of office at the College, from a committee member; a councillor, a member of the education board and finally holding the position of president. Which position would you find most memorable?
It all depends what you mean by memorable. Looking back at my involvement in the College, I think my involvement in the educational activities of the College was by far and away the most significant and rewarding. I chaired the Continuing Education Committee for 15 years and was responsible for the first realistic College continuing medical education (CME) program to be launched in this country.
”Then I disappeared off into the labs for two years to do a doctorate in cell biology which …was absolutely fascinating, superb; people said ‘you’ll miss the clinic’, but you actually don’t because you get so much more out of that. Understanding the scientific method then allows you, when you to come back into the clinic, to look at things from a different perspective”


The CME activities of the College for years centred around the Annual Scientific Meeting and in fact the Annual Scientific Meeting did really not have much of a continuing medical education element within it. It really consisted of the wisdom of visiting luminaries from overseas, most often from Britain and latterly, from the United States. And there wasn't really much in the way of continuing refresher type courses.
In the late 1980s, the College through the efforts of Professor Geoff Benness established a liaison with the American College of Radiology (ACR). The ACR was in fact the benchmark of continuing medical education in America; in that they provided a lot of postgraduate programs for radiologists. At that time, they had devised a series of programs called Viewbox Seminars. Professor Benness and Peter Duffy and several of the radiologists from Sydney then combined to bring one of those courses to Sydney.
It was an outstanding success, and was soon followed by two more similar courses. At that time, I was the chairman of the College Continuing Education Committee and decided that we had sufficient home-grown talent to mount one of these courses ourselves. We then successfully staged a similar course in Sydney in 1981 and that was followed by a Body CT Seminar in 1983. I think that this was probably the turning point for continuing education within the College. Subsequently the continuing education segments at the annual meeting became more and more prominent. I was involved at various times in the organisation of five annual meetings of the College, including one in Singapore which I organised in 1986 with Angus Robertson.
The first annual meeting in 1977, I did by myself, with the help of my wife and the state committee. We had no conference organisers. I virtually organised it with my wife from the kitchen table at our house. I guess it was quite a controversial meeting because it was held at the Gold Coast and a College meeting had never been held outside a capital city before that time. The outcome proved to be a great success.
In the 1980s, the ACR introduced a system of credits for CME participation The College was among the first in Australia to follow down this pathway, so that in 1998 when I attended the inaugural meeting of College CME chairs at the RACS in Melbourne, we were well ahead of the field with the CME program that we already had in place.
Do have any memories you'd like to share of advancements in the development of radiology?
At the outset we virtually lived in the dark. We were like mushrooms, and that's the way that radiologists were regarded. Historically hospital X-ray departments were in remote locations.
I have personal experience of one located in the basement in London and another located within the ceiling in Oslo! There was not a lot of interaction between clinicians and radiologists. Radiologists were treated as not much more than technicians. In the teaching hospitals clinicians would come to the department for clinical meetings and that was about it. …
Then we saw, particularly in the United States, the development of radiology departments, which were teaching and academic departments, and they blossomed in the 1960s and 1970s.
At that time in Australia that type of department just did not exist. So Australian radiologists like myself tended to go overseas to gain further experience in that environment. But gradually it happened here, both with the return of specialty trained radiologists, and the emergence of the new technologies. The dynamics changed with increased consultation with us, by the clinicians. We had subspecialised, so we knew just as much as the urologists or the neurosurgeons. The standing of departments was raised with the influence of respected figures such as Bill Hare, John Hunt, Hal Luke, Peter Breidahl, Colin Alexander and Jim Hood. Not only did the new technologies bring with them exciting imaging vistas, but there were also more informed opinions. Furthermore, the 1990s witnessed the advent of the various subspecialty groups within the College, which have since flourished. For those of us raised in the era of barium and the air encephalogram, we had emerged from the shadows and had finally arrived.
”The first annual meeting in 1977, I did by myself, with the help of my wife and the state committee. We had no conference organisers. I virtually organised it with my wife from the kitchen table at our house. I guess it was quite a controversial meeting because it was held at the Gold Coast and a College meeting had never been held outside a capital city before that time. The outcome proved to be a great success.”

Has volunteering given you skills and experience you could not otherwise have gained?
Becoming a DoT as a junior consultant required rapid upskilling in people management and leadership skills which I learnt from my experienced co-DoT, the late great Dr Eric Sclavos, on-the-job through trial and error (sorry, former trainees!) and by participating in multiple courses and workshops.
What achievements are you most satisfied with/proud of as a volunteer?
Do you have any advice on volunteering in general? Are there efficiencies to be gained in sharing the volunteer experience?
Volunteering is an activity that fits around the rest of life, so it helps to be organised, to know why you are doing it and to celebrate the wins.
The College relies heavily on volunteers. There are more than 60 different volunteering roles through the organisation and right now around 1,200 members offer their time as volunteers to support the College. We look at the experiences, insights and motivations of key volunteers.
You have made a huge contribution by volunteering with the College. What motivates you to volunteer? How does volunteering contribute to patient care, to colleagues, to the professions?
I started as a Director of Training (DoT) because I care about maintaining high quality training at my site and in my network. Junior doctors are incredibly powerless, and I wanted my trainees to always have someone in their corner. After nine years as DoT, the evolution to Queensland Branch Education Officer (BEO) and now Trainee Wellbeing Officer feels like I am working for the same outcomes but on a larger scale.
The biggest win has always been the satisfaction gained from watching my trainees pass the exam. That is especially sweet when I feel have helped a trainee to overcome specific challenges to achieve that conquest. Being a part of the team that successfully facilitated the Queensland Vivas during COVID comes a close second.
What has the pandemic meant for the volunteer experience? What are the risks of burnout? How best are these managed, in your view?
I believe that the spontaneity, creativity and collegiality that occur in the process of shared decision-making on working groups, committees and other College activities is something that is difficult to capture virtually (and I stand by that opinion despite having caught COVID in Sydney while there on College business!).
In health care, demands on the time, goodwill and empathy of staff are high even in times of relative plenty, so burnout is a constant risk even without lockdowns and high levels of absenteeism. Most doctors are very high functioning individuals and can happily live their lives using 99 per cent (or 120 per cent) of capacity. Just pushing through has seen many of us overcome big challenges but, as a profession, we need to learn that self-care is not selfish and admitting weakness is a strength.
I think it’s helpful for members to remember that those of us who are fulfilling these roles are doing them around the same unrelenting clinical load, teaching, kid wrangling etc that fill everyone else’s week. I believe the College punches above its weight given our relatively small size thanks to the indefatigable College staff and volunteers. However, with limited resources, there is always a need (and requests) to do more. If more people volunteered, imagine what we could achieve together!
Dr Chang responds to the question posed by our previous Volunteer in the Spotlight Dr Xavier Yu.
What are the perceived barriers to (particularly younger) fellows taking on College volunteering activities?
It can be difficult to find the time to fit College work around everything else. I think it is helpful when there are others in the network who volunteer so it is easy for interested Fellows to get a realistic idea of what is required and to know that there is local support for advice when needed.
Do you have a question for the next “volunteer in the spotlight”?
We need to train more radiologists to overcome current and future workforce shortages, but our training capacity is limited by our workforce shortages. How do we break this deadlock without limiting access to learning opportunities and compromising the quality of training?
It’s her first conference; and for her, “one of the best things has been the personalisation of the support from the College … to simplify the process [of becoming a radiologist].”
One of her favourite sessions was on proton therapy, with Dr Anita Majahan from Mayo Clinic. Ashleigh said, “It’s inspiring to see the level of professionalism here—it’s amazing. And I never dreamt I would have access to see that in person, so I was really keen to come, and I was delighted to get the opportunity.”
More than 1,400 delegates attended the 2022 Annual Scientific Meeting in Adelaide. Among the crowds were six ASM Sponsor Grant recipients.
This year, Kaitlyn Calvert-Shandley, Dr Jessica Del Bianco, Patricia Harris, Dr Kate Idiens, Ashleigh Morrison and Jordyn Tomba attended the conference thanks to their College grants, which assist with covering the costs associated with their registration, travel and accommodation.
This initiative is part of our long-term commitment to achieve equitable health outcomes of Māori, Aboriginal and Torres Strait Islander people and increase representation in our future workforce.
One of the recipients is Dr Jessica Del Bianco from Newcastle. Jessica, a member of the Australian Indigenous
Doctors’ Association, has enjoyed learning more about the advances in technology. She particularly found the session on gender diversity in radiology helpful and inspiring. She also enjoyed the session on research in radiology, and learning techniques to incorporate more research into a clinical radiology career.

“Coming to the conference has been very good for networking. Everyone has been so friendly and approachable,” she said. “I’ve been given a lot of contact details here, and a lot of cards, from people who I hope to keep in contact with.”
Ashleigh Morrison, another recipient, is a first year postgraduate medical student at Flinders University. In her work there, she said, “I have had very little exposure to clinical radiology or radiation oncology.”

The ASM Grant has been a great incentive for First Nations people at the start of their professional journey. Madeleine d’Avigdor, the College’s Senior Project Officer for Indigenous Workforce, said, “The College’s vision is for equitable health and workforce outcomes for Māori and Aboriginal and Torres Strait Islander Peoples. To encourage more First Nations doctors to consider a career in radiation oncology or clinical radiology, the ASM Grant was established in order to provide an immersive experience to learn more about our professions and provide insight into recent advances and the latest research. It also provides an invaluable networking opportunity to connect with College Fellows. I am delighted that these are now an annual offering.”
“It was impressive to see how engaged the recipients were, attending many of the scientific sessions and using their time to speak with specialists about their areas of expertise. The grants are clearly a success at giving potential trainees valuable exposure to our professions,” said Prof Vin Massaro, Chair of the College’s Māori, Aboriginal and Torres Strait Islander Executive Committee.
For enquiries about the ASM Sponsor Grant, email gaps@ranzcr.edu.au
”It was impressive to see how engaged the recipients were, attending many of the scientific sessions and using their time to speak with specialists about their areas of expertise. The grants are clearly a success at giving potential trainees valuable exposure to our professions.”
The MRI prostate sessions will be delivered by local faculty and Dr Richenberg, the MRI rectum sessions will be delivered by local faculty. Friday 24 March - Full Day


ARGANZ brings you a one day ESGAR liver imaging workshop with ESGAR faculty members Prof Valérie Vilgrain and Prof Giuseppe Brancatelli. The workshop will be in lecture and case-based discussion format. Friday 24 March – Full Day



Prof Valérie Vilgrain University of Paris and The University Beaujon Hospital, Clichy, France
A/Prof Giuseppe Brancatelli University of Palermo, Sicily, Italy
Dr Jonathan Richenberg Brighton and Sussex University Hospital Trust, United Kingdom
It was entirely fitting that the recent Women in Leadership breakfast at the College’s 72nd Annual Scientific Meeting to recognise and celebrate outstanding female leaders in clinical radiology, was also the platform for a lively and illuminating panel discussion on gender disparity in the clinical radiology workforce.

The College saw this as a valuable opportunity to highlight and explore the gender gap in the clinical radiology workforce and the under-representation of female radiologists in leadership roles. With the theme Reflect | Revive | Reimagine, participants were treated to thought-provoking presentations and insights from a cross-section of highly accomplished women in clinical radiology and radiation oncology, facilitated by clinical radiologist, Dr Emmeline Lee.
Drawing upon the latest gender-specific data from the College’s clinical radiology workforce census and international research, clinical radiologists and researchers, Dr Sally Ayesa1 and Dr Wanyin Lim2, shared the results of their recently published research which explored the challenges of achieving gender diversity within the College’s own governance and within the Australian and New Zealand clinical radiology workforce. Their findings are compelling.
While the College’s membership data (2012–2022) indicate an increase of female clinical radiologists from 25 per cent to 31 per cent and that of radiation oncologists from 39 per cent to 44 per cent in Australia and New Zealand, it is still an under-representation of female clinical radiologists when compared with gender distribution of medical students and junior doctors.
These numbers are exacerbated in clinical radiology where women are significantly under-represented at higher leadership levels.
The Australian data are comparable to international trends which confirm that gender inequity among representative leadership in clinical radiology is a global issue, with the lack of gender diversity in leadership even more marked when compared to workforce representation.
Internationally, academic radiology has a “leaky pipeline”, where the proportion of women incrementally decreases as they progress further along the career path towards leadership and senior faculty positions.
Women leaders face a disproportionate magnitude of seen and unseen challenges to leadership engagement and progression when compared to men, described by Dr Ayesa as a ‘glass labyrinth’ which is likely contributing to this discrepancy.
”While the College’s membership data (2012–2022) indicate an increase of female clinical radiologists from 25 per cent to 31 per cent and that of radiation oncologists from 39 per cent to 44 per cent in Australia and New Zealand, it is still an under-representation of female radiologists when compared with gender distribution of medical students and junior doctors.”
Research confirms that the causes are complex, with this disparity likely resulting from the interplay of multiple, intersecting factors including unconscious bias at an organisational, institutional and personal level, compounded by social constructs around gender roles and the challenges of balancing work and home responsibilities.
Unconscious bias refers to ways that humans unknowingly draw upon assumptions about individuals and groups to make decisions about them. These biases can lead to differential treatment on the basis of negative or positive stereotypes about social identity groups.
In clinical radiology, these include assumptions of inferior capability, capacity and credibility among women radiologist leaders, creating unique challenges at organisational, institutional and personal levels, as do perceptions of what constitutes a leader, where ‘male’ traits of assertiveness, charisma, confidence are valued over ‘female’ traits of empathy, sensitivity and collaboration.
In sharing her personal experience, Dr Ayesa illustrated many of the barriers to gender parity that emerged in her research and the fact that female clinical radiologists have gender-specific work patterns which need to be considered in workforce planning.
“I had a child in training and took time off, then had to work part-time. I fell behind my other colleagues in terms of my career progression and certainly didn’t engage with leadership opportunities. Because I was working part-time, I was unable to take senior registrar roles at my hospital,” she said.
“Did it hinder me and my progression and did it stop me from doing things I would have liked to have done? Yes, probably.”
According to Dr Wanyin Lim, in Australia and New Zealand clinical radiology is widely perceived to be a specialty where it is easy to work part-time yet its popularity among female medical graduates is declining, reflected in a steady decrease in the proportion of female trainees since 2012.
While there is a good gender balance in most medical schools, the current under-representation of women in clinical radiology training programs suggests that there is a need to expose medical students and junior doctors to the speciality of clinical radiology early in their careers to stimulate their interest and dispel common misconceptions about the profession.
Improving gender equality requires a systemic, multi-dimensional and inclusive approach informed by members, research and international experience, one that tackles unconscious bias; understands and responds to the gender-specific differences in workforce participation; upskills people of all genders; and encourages them to engage or reengage with representation at all levels of their career.
In the USA, the American College of Radiology (ACR) established a Commission for Women and Diversity to give a voice to women and minority clinical radiologists. Formal recommendations from the group included initiatives that offer greater flexibility in work options to respond to gender-specific work patterns; remove the stigma associated with balancing work and home; and provide greater flexibility to enable women to develop leadership skills at a later stage in their career.
The College is committed to working with members to consider potential knowledge gaps and solutions in this area, with the ultimate goal of improving gender diversity both in the clinical radiology workforce and in governance structures.
“It is of great importance that we recognise the gender gap, which is the first step towards achieving gender diversity and equality in our workforce. I firmly believe that improving gender diversity in the radiology workforce will ultimately deliver patient-centred care and better health outcomes. I pledge that the College will embark on this journey through enabling innovations and collaborations that can achieve gender equality,” said Clin A/Prof Sanjay Jeganathan, College President.
In our jurisdictions, the College is working on other ACR recommendations to offer professional opportunities to increase women’s visibility by recognising success and achievement; and to offer targeted member services including networking and mentoring opportunities which are known to positively impact gender diversity.
Dr Wanyin Lim notes however, that while working towards a diverse and inclusive workforce that is reflective of the community it serves, this needs to be done with full recognition that aspirations and goals are those of the individual and not inherently tied to gender or other characteristics used to define individuals.
In her closing remarks, Dr Emmeline Lee affirmed that achieving diversity is the responsibility of every member of the profession, regardless of gender or role, and that it is time to re-imagine what is possible.
Clinical radiology as a specialty stands to gain much in the way of progress and innovation as we move towards improved diversity within our workforce and our leadership.
References
1 Ayesa, S.L., McEniery, J.C., Hill, L.S., McCloskey, C.E. and Lee, E.H. (2022), Navigating the glass labyrinth: Addressing gender diversity in Australian and New Zealand representative radiology leadership. J Med Imaging Radiat Oncol.
2 Lim, W., Gupta, N. and Mandel, C. (2022), Analysis of gender in radiology in Australia and its importance to the profession and workforce planning. J Med Imaging Radiat Oncol.
”In her closing remarks, Dr Emmeline Lee affirmed that achieving diversity is the responsibility of every member of the profession, regardless of gender or role, and that it is time to re-imagine what is possible.”
Early Career Researchers Prize
Dr Heather Kate Moriarty Leonard
“PiVET – ED. Pelvic VeinEmbolisation for Treatment of Erectile Dysfunction: Study Protocol for a Prospective, Randomized, Single-Blinded, ShamControlled Study.”
Dr Anna Kathleen Lawless

“Dosimetric Comparison of Volumetric Modulated Arc Therapy and Intensity Modulated Radiation Therapy for Soft Tissue Sarcoma of the Extremities.”
Associate Professor Wee Loon Ong

“TROG-TD-21.11: Androgen suppression combined with elective nodal and dose escalation with stereotactic body.”
If you would like to apply for a research award or grant, applications for 2023 will open in January. A variety of opportunities are available to support research projects and foster a culture of research at the College.

RANZCR research grants provide financial support for Fellows, Educational Affiliates and student members in clinical radiology and radiation oncology to conduct research. Grants are awarded for sums between AU$5,000 and AU$30,000.
This AU$20,000 grant will support a trainee or Fellow to undertake a TROG Category D project and can be used to supplement an existing salary from an institution or for additional research project support.
This AU$25,000 grant supports Fellows up to five years post-Fellowship and trainees post-Phase 2 exams to carry out significant research projects.
This AU$1,500 prize recognises a clinical radiology trainee or junior Fellow who is the first author of a paper accepted for publication by JMIRO or another Medline Indexed peer-reviewed journal.
This AU$1,500 prize is awarded to a trainee who has written an exceptional trainee research requirement manuscript.
This AU$2,000 prize is awarded in the case of high-quality research in Indigenous health being published in a peer-reviewed journal.
This AU$2,000 is awarded in the case of high-quality research in Quality Improvement in radiation oncology being published in a peer-reviewed journal.
For more information visit www.ranzcr.com/college/awards-and-prizes/research-awards-and-grants or email gaps@ranzcr.edu.au
The Gold Medal honours a Fellow who has rendered outstanding service or benefactions to the development, teaching or practice of clinical radiology or radiation oncology in Australia, New Zealand or Singapore.
Associate Professor Dinesh Varma completed his medical training in India and migrated to Melbourne in 1989. He trained at The Alfred Hospital, Melbourne and was awarded FRANZCR in 2000. He has been at The Alfred since as Head of Trauma and Emergency Radiology. In 2003, he was appointed Deputy Director of Radiology and in 2009 appointed Clinical Associate Professor, Department of Surgery, Monash Medical School, Melbourne.
His contributions to the College span more than 20 years starting as the Junior Radiologist Representative on the Council in 2000 then elected President in 2011. He was appointed Clinical Radiology Chief Censor (2016−2018) and the inaugural Clinical Radiology Chief of Professional Practice (2019 to date).
In 2009 he became the College’s representative on the Executive Council of Asia Oceanian Society of Radiology (AOSR) and elected President of AOSR in 2018. His major contributions include education and raising standards of practice in many underdeveloped countries. He was also a key member on the project that built and developed a trauma centre and services in Galle, Sri Lanka.
He is the founder and Chair of the Australian and New Zealand Emergency Radiology Group (ANZERG), established in 2016 and President Elect, Australian and New Zealand Trauma Society. In 2019 he was appointed Deputy Chair, Traumatic Brain Injury (TBI) Mission, MRFF, Commonwealth Government that granted AU$50 million for research in traumatic brain injury.
His academic work includes more than 60 peer-reviewed publications, supervisor of BMed at Monash University, invited speaker at numerous national and international conferences. He was an Associate Editor of JMIRO and is a reviewer of many journals. He is the recipient of the Rouse Travelling Fellowship (2009), Rohan Williams Travelling Professor (2011), awarded Honorary Fellow of Singapore Academy of Medicine (2013), the Roentgen Medal in 2019 and the recipient of the 2022 AOSR Gold Medal.
A/Prof Varma was described by his nominators as someone with “indefatigable dedication to improving standards of the radiology profession in Australia and its recognition abroad” and who is “a worthy recipient of the Gold Medal, not only through his sustained, deep commitment to the College but also to his international involvement in other radiology societies.”
The Roentgen Medal is awarded to Fellows who have made a very valuable contribution to the College over a significant period.
Associate Professor Brigid Hickey attended the University of Queensland, graduated in 1986 and completed postgraduate training in Brisbane, Queensland. She became a FRANZCR in 1997. She is currently employed as Acting Director, Radiation Oncology, Raymond Terrace, Princess Alexandra Hospital. She has been involved with the College since 2003 and has been a Committee Member, or Chair, Faculty of Radiation Oncology Councillor or RANZCR Director continuously since then. Nominators described A/Prof Hickey’s “commitment, hard work, wisdom and generosity”, and someone who is “a perfect ambassador for our College, a
positive force promoting the value of radiation oncology and radiology.”
Life Membership is awarded to Fellows over the age of 65 who have made an unusually significant contribution to their field or the College.
Dr Michael James Baker qualified in medicine at the University of Rhodesia and obtained the Scottish Triple Qualification, before coming to New Zealand for his pre-registration years. He qualified as a physician in the UK and joined the radiology registrar training scheme in Auckland in 1983. Dr Baker worked at North Shore Hospital for more than 25 years and in private practice for TRG Imaging. He is currently working as a specialist breast radiologist at TRG and BreastScreen Aotearoa. He has been involved in the College since 1988, holding several committee and other roles. Dr Baker is currently a Councillor on the Faculty of Clinical Radiology Council and member of the NZ Branch Committee. Highlights of Dr Baker’s career include establishing the NZ Radiology Education Trust in 1994; registrar education; celebrating the Roentgen Centenary by developing educational material for schools; and his service as Chair of the Radiologist Professional Advisory Committee for IANZ, NZ’s accreditation authority.
Clin A/Prof Anita Geraldine Mary Bourke qualified with honours in medicine and surgery from the Royal College of Surgeons in Ireland (RCSI) in 1980. She moved to Perth in 1982 for her radiology training. She holds RANZCR and RCSI Fellowships. She was the first dual qualified radiologist and nuclear physician in WA and the first female in Australia to have dual specialisation. A dedicated clinician and teacher, breast imaging is her specialty and research interest.
College Honours celebrate the important contribution clinical radiologists and radiation oncologists make to the health of patients across Australia, New Zealand and Singapore. It gives the College great pleasure to announce the recipients of the 2022 College Honours.
Clinical positions she has held include Senior Consultant Breast Radiologist at Sir Charles Gairdner Hospital, Perth, Western Australia, where she received the Clinical Association’s Excellence in Service Award for 2021; BreastScreen WA Radiologist; and Clinical Associate Professor, School of Medicine at The University of Western Australia. Clin A/Prof Bourke is a Fellow of RANZCR and the Australasian Association of Nuclear Medicine Specialists, a member of the WACOG Breast Collaborative, Breast Interest Group (RANZCR) and MR Breast Interest Group. She is an examiner for the Royal College of Radiologists and an Accreditor for BreastScreen, Australia.
Dr Lynne Maree Brothers studied medicine at the University of Tasmania and completed her fellowship at the Royal Hobart hospital. Throughout her career, she has pursued her interests in breast, obstetric and gynaecological imaging as a VMO at the Royal Hobart Hospital, BreastScreen Tasmania and Women’s Imaging in Hobart. Dr Brothers has been actively involved in teaching Radiology and Obstetric registrars and Diploma of Medical Ultrasonography candidates.
Dr Brothers has been involved in College activities including as a member of BRIG and holding roles in OGSIG and RANZCR at a branch level. She represented the College on the RANZCOG Nuchal Translucency and Monitoring Program Steering Committee and has been a reviewer for the ASM and JMIRO. In 2019 Dr Brothers was a recipient of the RANZCOG Excellence in Women’s Health Award.
Dr Charles Weetman Lott graduated from the University of Adelaide in 1978 and pursued a surgical career in Australia and the UK, obtaining his fellowship of the Royal College of Surgeons in 1983. Seduced by advances in diagnostic radiology, he trained in Oxford, gaining his fellowship of the Royal College of Radiologists in 1988 and his FRANZCR in 2008. In 2009 his focus shifted to teleradiology, and he worked in both Australia and UK, becoming the Global Medical Director of Everlight Radiology. He is currently Emeritus Clinical Director of Everlight.
He has worked in both public and private settings. He was Convenor, RANZCR ASM 2008, Convenor, Cardiovascular SIG 2004−08, President AMSIG 1998−99. He was active in
the development of the College’s Teleradiology Standards. The pursuit of excellence in reporting, and creating the pathway to best achieve it, remains a prime focus for Dr Lott. His imaging interests include interventional, cardiovascular, emergency, MSK and prostate. He holds AHPRA, MCNZ and GMC registration.
Dr John Howard Lawrence Matthews graduated with his MBCHB (University of Auckland) in 1977 and trained in radiation oncology at Auckland Hospital (FRANZCR 1985). From 1985−1987 he worked at Cross Cancer Institute, Alberta, Canada, as Consultant Radiation Oncologist and Experimental Radiobiologist, investigating inherent radiosensitivity of cultured human tumour cells. In 1987 Dr Matthews was appointed as Consultant Radiation Oncologist Auckland Hospital, working across many tumour streams later focusing on genitourinary and skin tumours. He also worked in private oncology practice and introduced LDR prostate brachytherapy into New Zealand in 1999.
Dr Matthews is a founding member of TROG with particular involvement in genitourinary trials. He was awarded as the Rouse Travelling Fellow in 1998. He has enjoyed teaching trainees and his service as a Part 2 RANZCR Examiner. He has served as a member of the NZ Branch Radiation Oncology Executive Committee and the NZ Ministry of Health Genitourinary working groups.
A/Prof Ross Alan O'Neil graduated from the University of Sydney with a Bachelor of Medicine, Bachelor of Surgery in January 1980 (FRANZCR 1986). He is currently a Senior Specialist at Canberra Hospital and an Associate Professor at the Australian National University Medical School. Dr O’Neil served RANZCR as a Part 2 Examiner for 25 years, as the ACT Branch Education Officer for 22 years, as the Canberra Hospital Director of Training for 28 years, as a Faculty Councillor for eight years, as the ACT Branch Chairperson for five years, and as the ACT Branch Treasurer for 24 years.
Clin A/Prof Elizabeth Jane Wylie is a graduate of the University of Western Australia. Dr Wylie worked as junior doctor at Royal Perth Hospital (RPH) and undertook her Radiology Training at RPH under the tutorage of Prof Turab Chakera, who was a lifelong friend and mentor.
Following a two-year stint in the UK, Dr Wylie returned to WA, to take up a consultant position at RPH, and to work at BreastScreen WA (BSWA). Dr Wylie was appointed Medical Director of BSWA in 2000 and was Head of the Department of Radiology at Royal Perth Hospital from 2007 to 2019. Dr Wylie was appointed an Associate Professor at the University of Western Australia in 2007. Dr Wylie’s contributions to the College include her role as Convenor of the Breast Imaging Reference Group from 1989−2016, College elected Councillor 2005−2007, and Associate Editor of JMIRO for more than 20 years. Dr Wylie has been an active teacher, researcher, public speaker and stalwart of the College’s WA branch activities.
If you would like to nominate someone in one of the categories above in 2023, or the honours below, nominations will open in January.
The Clinical Radiology Educational Service Award recognises members who have demonstrated outstanding longterm commitment, participation and leadership in training and education in clinical radiology.
The Denise Lonergan Educational Service Award recognises members who have demonstrated outstanding longterm commitment, participation and leadership in training and education in radiation oncology.
An Honorary Fellowship recognises individuals who have contributed to the advancement of clinical radiology or radiation oncology and allied sciences, either through original research or by special services to the College.
The Sally Crossing Award for Consumer Advocacy acknowledges outstanding commitment of consumers involved in health care advocacy. The award honours the memory of the late Sally Crossing AM, in recognition of her exceptional contributions to advocating for cancer patients.
To find out more, or to nominate someone you know, visit www. ranzcr.com/college/grants-andawards/college-honours or email gaps@ranzcr.edu.au
Dr Samantha Stott for Clinical Radiology


Adjunct Associate Professor Helen MacDonald Lovat Frazer
Dr Mei Ling Yap

The College offers a variety of fellowships each year, to support members in their continuing education and to further their knowledge and expertise. If you would like to apply for any of these opportunities, visit www.ranzcr. com/college/grants-and-awards/ educational-fellowships or email gaps@ranzcr.edu.au
This Fellowship enables a clinical radiology or radiation oncology member up to six years post-Fellowship to further their knowledge by studying abroad for between three and 12 months. It is supported by a grant of AU$20,000.
This Fellowship supports a Fellow more than five years post-Fellowship for a period of intensive or overseas study (three to 12 months) or for attendance at an international short course (two weeks to one month) with a grant of AU$30,000.
In 2023, this fellowship is available for a clinical radiology Fellow from Australia to attend the 2024 New Zealand Annual Scientific Meeting and to visit and present in their field of interest in three training centres in New Zealand. This is supported with a grant of AU$8,000.
This is a 12-month position for Fellows up to two years post-Fellowship or trainees post-Phase 2 exams that provides clinical research opportunities at the Mount Vernon Cancer Centre in the United Kingdom. The position is under the broad supervision of Professor Peter Hoskin.
There may also be an opportunity for the Windeyer Fellow to spend time at other UK centres including the Christie Hospital, Manchester, and University College London Hospitals (UCLH), where experience in subspecialty interests such as proton therapy, MR linac treatment and paediatric oncology can be provided.
Associate Professor Dinesh Varma, Gold Medal 2022
A selection of A/Prof Varma’s recent publications:

• Dwivedi S, Kimmel LA, Kirk A, Varma D.Radiological features of pulmonary fat embolism in trauma patients: a case series. Emergency Radiology 2022 Feb; 29(1): 41–7.
• Clements W, Varma D, Koukounaras J. Consent, consultation and outpatient clinics in radiology: Are we moving with the times? Journal of Medical Imaging and Radiation Oncology 2020 Apr; 64(2): 257–9.
• Thompson C, Karunadasa H, Varma D, Schoenwaelder M, Clements W. Impact of COVID vaccination rollout on the use of computed tomography venography for the assessment of cerebral venous sinus thrombosis. Journal of Medical Imaging and Radiation Oncology. 2021 Dec; 65(7): 883–7.
• W ijetunga C, O'Donnell C, So TY, Varma D, Cameron P, Burke M, Bassed R, Smith K, Beck B. Injury detection in traumatic death: postmortem computed tomography vs. open autopsy. Forensic Imaging. 2020 Mar 1; 20: 100349.
“This is indeed a big honour and I am very humbled and privileged to be the recipient of the 2022 Gold Medal.”

Last month saw a record turnout for our 72nd Annual Scientific Meeting (ASM) in Adelaide, with more than 1,400 delegates coming together for our first face-to-face ASM in three years. There was a real buzz around the Adelaide Convention Centre during the 3.5-day program, packed with rigorous scientific content and lots of opportunities to connect with each other in person.
The ASM kicked off with the Women in Medical Leadership Breakfast. More than 110 attendees heard from a panel of impressive female leaders, who presented their research on the lack of gender parity in the professions of clinical radiology and radiation oncology and shared their own inspiring leadership journeys. The thoughtprovoking discussion about barriers and opportunities for women in leadership gave us a lot to interrogate as we strive to improve gender diversity in the professions. See page 20 for more on this topic.
The program was then opened with a Welcome to Country from First Nations Kaurna People Elder, Cliffy Wilson. This was followed by an official welcome from President, Clin A/ Prof Sanjay Jeganathan and the ASM Organising Committee, together with Sarah Andrews MP representing the South Australian Minister for Health and Wellbeing, and Dr Richard Harris SOC OAM as the Nisbet Orator. Dr Harris shared his story as a doctor and expert cave diver in the Thai cave rescue operation that captured the world’s attention and imagination. A stirring way to begin the conference.
All-star keynote speakers from home and abroad gathered to present more than 250 presentations across 70-plus sessions and workshops, showcasing the latest in medical technology advancements, leading multi-disciplinary collaborations, and exciting milestones in cancer treatments.

Highlights of the clinical radiology program included the Space Radiology Session, a unique exploration of the critical role of clinical radiology, medical imaging and aerospace medicine in a multi-planetary future for humankind. The National Imaging Facility (NIF) Showcase delved into opportunities for NIF and the College to collaborate on cutting-edge research and innovate at a strategic level to deliver benefits to Australian health care. In a session
on Advances in CT we heard an indepth expert review of Australia’s first application of the latest revolutionary photon-counting CT scans in South Australia.

The radiation oncology program was equally impressive, with highlights including the Proton Therapy Session, in which keynote speakers addressed current controversies and further developments in proton therapy, model-based approaches for patient selection and proton therapy in headand-neck cancers. The Particle Therapy Session delivered exciting updates about national progress towards treating the first patients with proton beam therapy at the Australian Bragg Centre in Adelaide in 2025. Masterclasses and workshops in head and neck contouring and lung cancer were also highlights.
Alongside our keynote sessions, there were many opportunities for early career researchers to present their work, with the Varian Prize session for radiation oncology trainees and the Branch of Origin session for clinical radiology trainees. We also offered a series of non-clinical workshops for the first time, with sessions on health and wellbeing, financial management and medico-legal issues.
Another first for the 2022 ASM was the introduction of the Everlight Kids Club, a free children’s creche service that allowed delegates to engage in the scientific program while their little ones enjoyed their own program of exciting activities.


The conference program was complemented by a series of social events, in which delegates had the opportunity to relax and connect while sampling the best that the South Australian culinary scene has to offer. Highlights of the social program included the Clinical Radiology Quiz and Faculty of Radiation Oncology Dinner, the Trainee and Junior Consultants Reception, and of course the Gala Dinner, where the theme of “To Infinity and Beyond” inspired many a sparkly outfit, light sabres and a special rendition of “A Whole New World” performed by our 2022 ASM Convenors, as a love song to their hometown of Adelaide.
Special mention must be given to the more than 180 new Fellows (graduates from 2020–2022), who were welcomed into the College in front of a standingroom only audience of family, friends and colleagues at the Annual Ceremony. It was a much-anticipated, long-awaited joyful occasion.




The 2022 ASM was an energising and collegial event which reminded all of us of the importance of coming together to reflect, revive and reimagine. We hope that you left feeling inspired and reinvigorated. Don’t forget, you can claim up to 24.5 points for your ASM attendance via the College’s ePortfolio system.
The College would like to thank all who attended—both in person and online— particularly our speakers, exhibitors and sponsors, including our Presenting Partner, Intelerad, for their support of the meeting. And, of course, a special thanks to the 2022 ASM Organising Committee, whose dedication, commitment and personal warmth were key in making RANZCR2022 the stellar event we all hoped for.
Clinical Radiology Convenor – A/Prof Christen Barras
Radiation Oncology Co-Convenor – Dr Ramkumar Govindaraj
Radiation Oncology Co-Convenor – Dr Laurence Kim
Clinical Radiology Trainee Representative – Dr Upuli Pahalawatta
Radiation Oncology Trainee Representative – Dr Peter Nguyen
Professor Sujal R Desai, UK
Professor Elizabeth Dick, Imperial College NHS Trust, UK
Professor Mark Jenkinson, AUS and USA
Dr Melissa McCradden, Canada
Professor Elizabeth Morris, USA
Professor Perry Pickhardt, USA Dr Asif Saifuddin, UK
Professor Tarek Yousry, UK
Professor Hans Langendijk, the Netherlands Dr Nancy Lee, USA
Dr Anita Mahajan, USA
Dr Umberto Ricardi, Italy
American College of Radiology
American Roentgen Ray Society
Asian Oceanian Society of Radiology (virtual)
College of Radiology, Academy of Medicine, Malaysia (virtual)
European Society for Radiotherapy and Oncology (ESTRO) (virtual)
European Society of Radiology
Faculty of Radiologists, Ireland
Hong Kong College of Radiologists (virtual)
Indian Radiological & Imaging Association
Japan Radiological Society (virtual)
The recent RANZCR ASM 2022 provided us with a pertinent opportunity to perform a health check for the Targeting Cancer campaign, a highly acclaimed College campaign that aims to increase awareness of radiation therapy as an effective, safe and sophisticated treatment for cancer.
- Are the core objectives of the Targeting Cancer campaign being met?
- Is access to radiation therapy really improving?
- Are health professionals and the wider public aware of the benefits of radiation therapy?
At the Radiation Oncology Faculty Forum on 29 October, the Targeting Cancer Management Committee Co-Chair Dr Lucinda Morris led a panel discussion to look for answers to these questions and explore solutions with the following leaders in radiation oncology from home and abroad:
Dr Tuan Ha, Radiation Oncologist, RANZCR Faculty of Radiation Oncology Council Member and Co-Chair of the RANZCR Targeting Cancer Management Committee, Dr Melissa James, Radiation Oncologist, RANZCR Faculty of Radiation Oncology New Zealand Executive Committee Member, Radiation Oncology Research Committee Member, RANZCR Post Fellowship Education Committee Member, and
Dr Drew Moghanaki, Chief of Thoracic Oncology, Professor, Stanley Iezman and Nancy Stark Endowed Chair in Thoracic Radiation Oncology Research, UCLA Department of Radiation Oncology.
Radiation oncology is desperately under-utilised and under-valued and lacks the profile of other cancer treatments. This is due to widespread lack of understanding of radiation therapy. There are many myths and misconceptions that radiation therapy is a dangerous and difficult treatment. Many referral pathways to radiations oncologists are broken and there is a lack of funding for resources, workforce and research into the radiation oncology sector.
The Targeting Cancer campaign aims to raise awareness of radiation therapy in the community, including patients and their carers and health professionals, especially GPs and medical students. For the past few years, we have achieved a lot. However, COVID hit the campaign hard, and many domains of campaign work became stagnant. As Dr Lucinda Morris pointed out: “Targeting Cancer Campaign: Are we winning? The answer is no. We’re struggling.”
What are the key challenges observed by radiation oncologists working on the ground from Australia, New Zealand and around the world?
Dr Tuan Ha provided his perspective as a Rockhampton-based radiation oncologist and stressed that the
Indigenous population faced more barriers in accessing radiation therapy despite the fact that more and more cancer centres opened up across Australia. Watch Tuan’s video about closing the care gap: bit.ly/TuanHaCloseTheGap
Dr Melissa James talked in-depth about the severe radiation oncology workforce shortage issue in New Zealand. That has direct impact on the health of New Zealanders because within 8–10 years we may no longer have radiation oncologists in New Zealand and patients with cancer won’t be able to get radiation therapy when they need it. Watch Melissa’s video: bit.ly/MelissaJames
Dr Drew Moghanaki shared his stories and views as an international guest. He commented that the Targeting Cancer campaign had good global reach and relevance within the radiation oncology community, but he’s uncertain about its reach in the general public. He highlighted surprisingly low awareness of radiation therapy among patients and even among medical and healthcare professionals and he suggested that radiation oncologists should proactively reach out to the leadership team within the hospital and colleagues from other hospital departments to engage them in a dialogue about radiation therapy.
Watch the session: 2022 RANZCR ASM – Targeting Cancer: Are We Winning?



➜
One hundred runners gathered to join the Targeting Cancer Fun Run 2022 at the Torrens riverbank in the early morning of 29 October to run for closing the care gap and raising awareness of radiation therapy.




We were pleased to see the record number of runners who showed their support for the campaign, including those from both the clinical radiology and radiation oncology communities and our sponsor, Icon Cancer Care.

Congratulations to our winners: Justin and Alexandra for winning the race as the first male runner and female runner, respectively.
Thanks to everyone for your participation, with a special mention to Susan who is the winner of our mystery prize. In celebration of the return of the Targeting Cancer Fun Run as the seventh running event, we decided to give a mystery prize to the seventh registration for the Fun Run.
We’d love to hear from you if you have any feedback and suggestions via email: info@targetingcancer.com.au

The 3Dimensions™ system provides high quality 3D™ images for radiologists, a more comfortable mammogram for patients and enhanced workflow for radiographers. Discover how sharper images and smarter technologies continue to help find invasive cancers, increase clinical confidence, and allow for greater operational e ciencies regardless of age, breast size, or density.2-8

Hologic Clarity HD™ imaging captures 70-micron high resolution 3D™ data that provides sharper 1mm tomosynthesis images, revealing more detail. It enables upgrades to more natural looking Intelligent 2D™ synthesised images and workfl ow advantages with 3DQuorum™ technology – reducing patient dose, time under compression and a radiologist’s interpretation time by 2/3. 9-12
The SmartCurve™ system’s curved compression surface mirrors the shape of the breast for more even compression and greater patient comfort. 12,13 Shown to improve comfort in 93% of patients who reported moderate to severe discomfort with standard compression methods. 13
Thoughtful design includes ergonomic advantages to assist the radiographer with positioning, accelerate workfl ow, save time, reduce physical strain, and optimise viewing. The system improves the patient experience through reduced compression and the industry’s fastest 3D™ scan time at 3.7 seconds. 1,3,8,14,15


The College’s Roentgen Medal honours Fellows who have made a very valuable contribution to the affairs of the College over a significant period. In 2022, A/Prof Brigid Hickey, nominated by her peers, is the deserving recipient of this prestigious award.
Brigid Hickey attended the University of Queensland, graduated in 1986 and completed postgraduate training in Brisbane. She became a RANZCR Fellow in 1997 and today is Acting Director, Radiation Oncology at Princess Alexandra Hospital. Brigid’s volunteering journey with the College began nearly two decades ago in 2003, and she has been a committee member, Chair, Faculty of Radiation Oncology Councillor or Board Director continuously since. Some of Brigid’s most notable achievements during this time include:
• developing the first Tripartite Plan as Chair of the Tripartite Committee (now the Radiation Oncology Alliance), which is the formal radiation oncology alliance of RANZCR, ASMIRT and ACPSEM
• fostering her passion for postFellowship education to lead the
Brigid often described herself
all she was doing was
humility, and humanity,
FRO’s Post Fellowship Education Committee and Annual Scientific Meeting Management Committee
• playing an important role in reorganising the JP Trainor Trust Archives Committee to ensure this important link to the College’s past is in very good standing
• helping to steer the College through the unprecedented disruption of the COVID-19 pandemic as Board member, Treasurer and Chair of the Audit and Risk Committee.
Although she has been described as a “quiet achiever” by her peers, Brigid’s contributions have not gone unnoticed. Past President Dr Lance Lawler says, “Brigid is one of those rare 'think before you speak' individuals who always deeply considers the issues before weighing in, and as a result frequently ends up making the most significant contribution to any decision. Never one to blow her own trumpet, Brigid often described herself as 'an imposter'; in reality all she was doing was defining her innate humility, and humanity, and underlining her suitability to serve.”
Dr Tanya Holt, who has known Brigid as a training supervisor, colleague and mentor commented, “Through
mentorship and altruism, she has inspired me to follow her lead and be heavily involved in the College…. It is only with such positive role models that the College is able to function and have so many Fellows volunteering their time”.
This is a sentiment that Brigid herself echoed when we caught up with her at our recent Annual Scientific Meeting (in between answering questions at the AGM and officially receiving her Roentgen Medal at the College’s Annual Ceremony). “I would never have stepped forward had I not been encouraged by colleagues. You always think you are not ready but it is in the doing that you learn most.”
View a full list of our 2022 Award and Prize recipients in our special 2022 Awards and Honours Keepsake
Do you have a colleague or mentor who deserves recognition? Nominate them for a College Honour in 2023. See page 25 for more information
“Brigid is one of those rare 'think before you speak' individuals who always deeply considers the issues before weighing in, and as a result frequently ends up making the most significant contribution to any decision. Never one to blow her own trumpet,
as 'an imposter'; in reality
defining her innate
and underlining her suitability to serve.”
A/Prof Brigid Hickey


Following the highly successful RANZCR2022 ASM in Adelaide, the College’s events team is now planning a busy annual calendar of events in 2023. Mark the dates in your calendar for the events listed below and keep up-to-date with all new events on the Events page of www.ranzcr.com by following this link www.ranzcr.com/whats-on/events
2023 Events
Radiation Oncology Trainee SMART Workshop, Hilton Hotel, Adelaide, SA 19 June 2023
Save the Date! Further information coming soon.
RANZCR NZ ASM, Millennium Hotel, Queenstown, NZ 11–13 August 2023

Save the Date! Further information coming soon. www.ranzcr2023.co.nz
RANZCR ASM, Brisbane Convention and Exhibition Centre, Brisbane, QLD 19–22 October 2023
Save the Date! Further information coming soon.
As part of the six-part perinatal post-mortem webinar series, the College will be delivering two webinars in the month of February 2023. The series forms part of the broader Stillbirth Investigations Project for which the College has obtained funding from the Australian Government through the Department of Health and Aged Care. The project will increase clinicians’ capacity to undertake stillbirth investigations and autopsies and ensure these services are available to bereaved parents who choose to access them. The Stillbirth Investigations Project will develop tailored strategies, educational programs and resources to improve the uptake, acceptability, range and quality of stillbirth investigations in Australia.
Prof Michael Aertsen will present the topic ‘Fetal intrauterine vs post-mortem imaging: what have we learnt?’ from 8–9 pm AEDT on 2 February 2023 . Prof Aertsen is a subject matter expert in the field of fetal MRI with a research focus on fetal brain development with advanced MRI techniques.
Prof Susan Shelmerdine will present the topic ‘Post-mortem imaging for beginners: what, how & why’ from 8–9 pm AEDT on 23 February 2023. Prof Shelmerdine is a subject matter expert in the field of novel imaging relating to post-mortem investigation with sub specialty expertise in paediatric imaging.
Register here for any of the upcoming webinars: bit.ly/RANZCRSIPWebinars
Webinars will be delivered online using GoTo Webinar. Registration and attendance of the session is required in order to retain access to the recording of the webinar.
A reminder to members to ensure you have entered your 2022 CPD activities by 31 December. As the College CPD program has moved to an annual cycle, it is imperative that you are regularly entering your CPD activities in the ePortfolio to ensure you remain compliant and you are ready to commence the next annual cycle at the start of the calendar year. The 2022 CPD requirements are as follows:
• 50 hours of CPD activities, in any of the MBA/MCNZ categories
• Professional Development Plan (PDP)
• MRI and mammography CPD hours for members participating in these programs (8 hours for MRI, 4 hours for mammography)
• Structured annual conversation (New Zealand members, MCNZ requirement)
• CPD activities with a focus on cultural safety and health equity (New Zealand members, MCNZ requirement).
The CPD section of the College website has all the information regarding the CPD program requirements, ‘how to’ guides and video recordings to assist in using the CPD ePortfolio and other information resources such as Frequently Asked Questions, CPD handbooks and templates.
In addition to the 2022 CPD requirements, from 2023 onwards, members must meet minimum requirements across the three CPD Categories:
With the current changes to CPD requirements, there is one category that members may have missed out on—and here’s some news.
In the CPD category of Reviewing Performance and Reflecting on Practice, you may not be aware that formal peer review of a manuscript counts towards the mandatory minimum five hours per annum of “reviewing performance”.
CPD requirements and evidence have changed for 2023. Each year at least five hours of “Reviewing Performance” is required.
A formal peer review of a manuscript for JMIRO qualifies towards your annual College CPD requirement of at least five hours of “Reviewing Performance”.
As well as that, it would be very much appreciated by your colleagues. Just record the dates and hours spent in your calendar as evidence.
It’s not just your CPD record that benefits. Stephen B. Kritchevsky notes five top reasons for being a peer reviewer:1
• Reviewing makes you a better writer. Thinking about how others could express themselves more clearly is a mini-tutorial in composition every time you do it.
• Reviewing helps you think critically about your own research. The experience of identifying the strength and weaknesses in others’ research makes you more likely to adopt the strengths and avoid the weaknesses in your own.
• Being a reviewer is a sign of an emerging national reputation. It is an acknowledgment that you are a peer worthy of providing editorial guidance. Editors notice when you have done a thoughtful job, which can lead to unanticipated opportunities. My being asked initially to be an associate editor at JGMS was a result of the strength of my performance as a reviewer.
• at least 12.5 hours (25 per cent of the minimum) in educational activities
• at least 25 hours (50 per cent of the minimum) in activities focused on reviewing performance and measuring outcomes, with a minimum of five hours for each category, and
• the remaining 12.5 hours (25 per cent of the minimum), in any CPD category
• anaphylaxis training to be completed once every 3 years (Clinical Radiology members only).
Please refer to the newly published 2023 CPD Handbooks for further details regarding the 2023 CPD program and requirements, as well as a full listing of CPD activity types and which category they correspond to.
For more information regarding the College’s CPD program, please contact cpd@ranzcr.edu.au. Please note the College office will be closed from Friday 23 December 2022, reopening on Monday 9 January 2023.
• Reviewing is a professional service. This may be beneficial when coming up for academic promotion. At my university, the tenure and promotions committee views those participating in shaping their discipline through writing, editing, and reviewing favourably.
• Reviewing provides advanced access to emerging ideas and trends within your area of expertise. The lag from journal submission to publication is shortening but can be six months or more. Even articles that are rejected can provide important insights that can inform your own thinking on a topic.
Benefits of being a peer reviewer include contributing to the profession, developing critical analytic skills, learning about new content related to the profession, and helping authors to improve the clarity of their manuscripts. Serving as a peer reviewer can be a great introduction to becoming an author.
References 1 Kritchevsky, S.B., 2018. The benefits of reviewing. Journal of the American Geriatrics Society, 66(7), pp.1253-1253.
During my first year as the College Archivist, I felt duty bound to take a deep dive into the history of the College. One very important figure, who I feel that I must give voice to, is none other than the College's first female President, Dr Mancell Gwenneth Pinner (1922–1998).
She was one of just eight females to receive their Bachelor of Medicine and Bachelor of Surgery in 1945 from the University of Melbourne.
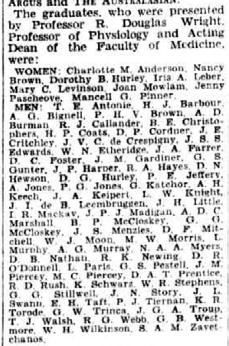
An unfortunate bout of tuberculosis took her out of the field for two years, but this ultimately proved to be an inspiration to Dr Pinner. She was appointed to head a survey team in 1949 to examine the incidences of tuberculosis infection in the ACT and in Queanbeyan for the Commonwealth Department of Health.
Not only did this campaign promote awareness of the disease, but it also resulted in Dr Pinner leading a similar survey on Norfolk Island.
Dr Pinner then began working as an assistant radiologist at the Royal Melbourne Hospital under Dr Barbara Wood, along with fellow future College Presidents such as Dr Schubert and Professor Hare. She received her Diploma of Diagnostic Radiology in 1952 from the University of Melbourne.
In 1954, Dr Pinner became the first woman to be awarded the Thomas Baker Memorial Fellowship. She then went on to spend 18 months abroad, in countries such as Great Britain, Sweden, America, Canada and Mexico.
She documents her travels, and her learnings from global radiologists, in the first edition of Australasian Radiology (1957, Vol 1, p 10–20). The knowledge gained, and the hospitality shown to her, were greatly appreciated, and proved to be another inspiration in her career.
Returning home, Dr Pinner worked as a consultant radiologist at the Royal Canberra Hospital. In 1965, she founded Canberra’s first private hospital, the John James Memorial Hospital.
She was elected to the fellowship of the UK Faculty of Radiologists in 1957, and became a Fellow of the College in 1964. Throughout this period, she continued to solidify her position as a leading figure in the field.
From 1984 to 1985, Dr Pinner became the first woman to fill the position of President at the College, which at the time was called the Royal Australasian College of Radiologists. There were approximately 800 qualified radiologists in Australia and New Zealand at the time. Despite the usual brevity of presidential tenure, she faced many challenges, and achieved a number of successful outcomes.

The fallout from the Pennington Inquiry Report, which focused on potential overcharging of medical services, resulted in radiologists being shown in a much more favourable light than had initially been portrayed by the media. The emergence of Nuclear Magnetic Resonance (NMR), and the funding of MRI, was a hotly contested debate, along with discussions around the Medicare rebate.
Dr Pinner retired in 1987, and sadly passed away in 1998.
One anecdote seemed to follow Dr Pinner for her whole life. At the age of four, she was selected to present a bouquet of roses to the Duchess of York at the Opening of Parliament House in 1927. Sixty-one years later, in 1988, Dr Pinner attended the opening of the New Parliament House, where she was presented to the late Queen, Elizabeth the Second. Some may say this was royalty meeting royalty.
Dr Pinner was a pioneer in her field and, I am sure, an inspiration to many.
The momentum around the work of the Interventional Radiology Committee (IRC) has continued to build over the last 12 months as the College progresses its work towards advancing interventional radiology (IR) and interventional neuroradiology (INR) in Australia and New Zealand.
The IRC is a standing committee of the Faculty of Clinical Radiology and provides advice to Council on interventional related matters (see figure 1).
The Committee’s overarching aim is to elevate the practice of IR and INR within the College and throughout Australia/New Zealand, and the IRC has worked tirelessly since 2017 to develop the necessary foundations to improve clinical practice, develop formalised training programs and qualifications for IR and INR, and advocate for the
recognition of IR and INR as formal clinical specialties. (See figure 2)
A major milestone in 2022 has been the launch of the first-ever IR and INR Standards of Practice for Australia and New Zealand. This adds to the development and endorsement of the Range of Practice and Definition of specialty IR and INR completed last year.
The development of a formal IR and INR Training Program, expected to be endorsed in the future by both the College and the Australian Medical Council (AMC), leading to formal qualifications, has also been continued under the IRC by the IR and INR Training Pathway Working Group. These significant developments will add considerably to the platforms from which recognition of IR and INR as Fields of Specialty Practice are being launched. (See figure 3)
Interventional radiology and interventional neuroradiology save lives and restore health to patients right across the healthcare system. These existing clinical specialties have the potential to significantly boost clinical radiology, and already provide important, high-value health care to patients, hospitals and the healthcare system. (See figure 4).
The momentum around the work of the Interventional Radiology Committee (IRC) has continued to build over the last 12 months as the College progresses its work towards advancing interventional radiology (IR) and interventional neuroradiology (INR) in Australia and New Zealand
The IRC is a standing committee of the Faculty of Clinical Radiology and provides advice to Council on interventional related matters (see figure 1). The Committee’s overarching aim is to elevate the practise of IR and INR within the College and throughout Australia/New Zealand, and the IRC has worked tirelessly since 2017 to develop the necessary foundations to improve clinical practice, develop formalised training programs and qualifications for IR and INR, and advocate for the recognition of IR and INR as formal clinical specialties. (See figure 2)
A major milestone in 2022 has been the launch of the first-ever IR and INR Standards of Practice for Australia and New Zealand. This adds to the development and endorsement of the Range of Practice and Definition of specialty IR and INR completed last year. The development of a formal IR and INR Training Program, expected to be endorsed in the future by both the College and the Australian Medical Council (AMC), leading to formal qualifications, has also been continued under the IRC by the IR and INR Training Pathway Working Group. These significant developments will add considerably to the platforms from which recognition of IR and INR as Fields of Specialty Practice are being launched. (See figure 3)
Specialty Fields of Specialty Practice Specialist Titles
Diagnostic Radiology Specialist Radiologist
Diagnostic Ultrasound Specialist Radiologist
Radiology
Surgery
Nuclear Medicine Specialist in Nuclear Medicine







Interventional Radiology Specialist Interventional Radiologist
Interventional Neuroradiology Specialist Interventional Neuroradiologist
Vascular Surgery Specialist Vascular Surgeon
Urology Specialist Urologist Neurosurgery Specialist Neurosurgery
General surgery Specialist General surgeon
Physician
Cardiology Specialist Cardiologist General medicine Specialist General physician Neurology Specialist Neurologist
Figure 3: Snapshot of current Specialty and Fields of Specialty Practice, with proposed IR and INR specialties. Recognition of IR and INR as distinct Fields of Specialty Practice under radiology will elevate these specialties to the same level as other specialties such as vascular surgery, urology, neurosurgery and neurology.
Figure 3: Snapshot of current Specialty and Fields of Specialty Practice, with proposed IR and INR specialties. Recognition of IR and INR as distinct Fields of Specialty Practice under radiology will elevate these specialties to the same level as other specialties such as vascular surgery, urology, neurosurgery and neurology.
Interventional radiology and interventional neuroradiology save lives and restores health to patients right across the healthcare system in ways that no other specialty can These existing clinical specialties have the potential to significantly boost clinical radiology, and already provide important, high-value health care to patients, hospitals and the healthcare system. (See figure 4).
Figure 4: IR and INR add significant value and embody the characteristics desirable in modern, high-value healthcare services.
Figure 4: IR and INR add significant value and embody the characteristics desirable in modern, highvalue healthcare services.
“Interventional radiology and interventional neuroradiology save lives and restore health to patients right across the healthcare system.”
Laying a foundation for achieving specialty recognition is ongoing work and drives the IRC through all its activities. Some of the key highlights for 2022 are outlined below.
Expanded the IRC to include an additional two members
Published Specialist Interventional Radiology and Interventional Neuroradiology Range of Practice
Continue formal engagement with IRSA and ANZSNR on the RANZCR IR and INR Tripartite Committee and the Training Pathway Working Group
Engaging with College members through the work of the IRC and keeping members abreast of the inroads being made for interventional radiology and interventional neuroradiology is of utmost priority for the IRC. We are always seeking ways to improve our communication with members, and the need for accurate flow of information concerning our achievements, opportunities and challenges. It is equally important that there be a two-way flow of information and we strongly encourage members to provide us with any feedback, ideas or concerns. This will allow us to respond and pivot to issues that are important to College members.
Expanded the membership on the IR and INR Training Pathway Working Group to include trainees and early career Fellows
Published Standards of Practice for Interventional Radiology and Interventional Neuroradiology
Extensive member and stakeholder consultation on RANZCR’s proposal for specialty recognition
Conducted a workplace survey to better understand the extent and breadth of IR and INR services across Australia and its workforce
Developed briefing papers for Interventional Radiology and Interventional Neuroradiology, articulating the case for recognition
Advocacy for IR and INR, including in Stroke models of care, Cancer Australia Plan, MBS reform and with consumer organisations
I would like to take this opportunity to thank all the members of the IRC, who have worked tirelessly to advance the cause of IR and INR within Australia and New Zealand. I would like to thank all College members who have supported the work of the IRC and share the vision for a future where IRs and INRs can securely practise their craft as clinicians within a recognised specialty and for the benefit of patients. If we get this right, it will provide tremendous opportunities for the College to expand clinical radiology and promote the important and evolving role of radiologists in modern medicine. These successes will require effort and input from a broad range of members across the whole profession, and the IRC looks forward to continuing to work with all stakeholders in 2023.
Please get in touch at interventional@ranzcr.edu.au
A/Prof Nicholas Brown Chair, IRC
As 2022 comes to a close, now is the time to reflect on the great strides the College has made this last year. From continuous advocacy on important issues such as MRI and breast markers; to the great work done to keep members updated on the contrast media shortage issue, it certainly has not been a quiet one.
Looking back, we have progressed work in the areas of:

In May and June the world experienced an international shortage of contrast which affected radiology practice in Australia. The College showed leadership in a very proactive manner by providing advice to the Therapeutic Goods Association (TGA), liaising with contrast manufacturers, communicating to the membership and wider public, with many media appearances. Statements on our website were downloaded more than 6,000 times and the media reach where the College’s name was mentioned was more than 72 million times.
The Australian Federal Government has allocated $750,000 over four years to the College to increase the profession’s capacity to undertake stillbirth investigations and ensure that these services are available to bereaved parents who choose to access them. We have established a Stillbirth Steering Group to lead the delivery of this project.
The College has engaged in a number of meetings targeting members of parliament and assistant ministers to advance priority issues such as those related to breast markers, MRI and workforce distribution.
The College has published our Position Statement on the Regulation of Artificial Intelligence in Medicine, which was developed by the Artificial Intelligence Committee. This paper set out principles and recommendations to guide the development of a robust regulatory framework for AI technology in medicine.
The Interventional Radiology Committee has worked to develop applications for specialty recognition and advance development of the training pathways for IR and INR. We are hoping the applications are fit to be submitted to the AMC within the next couple of months.
The implementation of the new CPD system has required knowledge, foresight and persistence (particularly for those who leave completion of their CPD requirements until the last minute). A range of videos have been prepared and is available on the College website to assist members with the ePortfolio system.
The launch of the 2022 Training Program like the CPD program is the culmination of years of work. From new work-based assessments, examination structures, a new ePortfolio system to a vision for transitioning trainees into the new training program and ‘moving’ trainees through phases of training, those who have worked in the education and training are to be commended on all their effort.
Personally, as my Deanship comes to an end, I look back on these advances with a sense of satisfaction that we are travelling in the right direction. Having chaired the Faculty of Clinical Radiology Council, I have observed the work we drive move up the governance chain from its infancy to final signoff. None of this work would be possible without the dedication of our members who tirelessly volunteer countless hours in collaboration with the College secretariat to advance the causes that affect our profession.
I would like to thank everyone involved in College work. From our special interest group members, working group members, examination panel members to our committee members, Councillors, office bearers and staff; all in all, 2022 has been a good year for clinical radiology thanks to your efforts.
Passing the reins along is not an easy task, but I trust that the profession is in capable hands with Dr Rajiv Rattan at the helm. With a fresh perspective, Rajiv will lead the Council in monitoring and progressing the work of the College in evolving spaces such as Artificial Intelligence, collaboration with our New Zealand counterparts (and Te Whatu Ora), our AMC reaccreditation process and governance.
Looking forward, 2023 will be a year of connecting and reconnecting. I have never under-estimated the importance of interacting with our peers and

the recently held ASM was a prime example of this. It was a great few days of witnessing our talented members presenting on their passions, chatting, networking, collaborating and enjoying themselves (especially at the Gala Dinner!). I hope you all got as much out of this year’s ASM as I did.
There is a still a tremendous amount of work to be advanced and the momentum must be kept up. In saying this, a time to rest, recharge and start fresh is valuable and needed. I wish you all a safe, happy and relaxing holiday season.
Interesting case load
Emergency and acute complex cases, routine and overflow reporting.
Flexible hours
Full time, part time or casual shifts available on weekdays, evenings or weekends.
This year has flown by and has seen the launch of the new Training Program and ePortfolio system. Thank you all for your feedback and patience during the implementation process. I encourage you all to continue providing feedback as we will continue to try and make the documentation process easier for you. The new Training Program saw a review of the existing policies as well as additional policies to support and guide all new and transitioning trainees.
The College and committees have had a big focus on the wellbeing of all trainees. The introduction of the Trainee Wellbeing Officer (Dr Jennifer Chang) has been an important initiative in this regard. The appointment to the role of Director of Training and Clinical Supervisor Support Officer allows all trainees and supervisors to engage directly and provide feedback.
The recent ASM in Adelaide was an excellent opportunity for the radiology community to reconnect and was very well attended. It was nice to meet up with some old friends and engage with trainees and junior doctors looking for a career in radiology. It was great to oversee a record number of our trainees graduating at the Annual Ceremony after the three-year hiatus. It has been quite satisfying to see that our College has managed to facilitate trainee progression during the challenges of the past couple of years.
The Series 2 Clinical Radiology Written Examinations were hosted electronically including successful utilisation of the ProctorExam platform for the efilm

reporting examinations for the first time. This will be the preferred technique for delivering our written exams moving forwards. As I write this, the Series 2 Vivas are underway with the return of both examiners and candidates to Melbourne. Two different exam venues are hosting the candidates and examiners, enabling more centralised oversight of the process. The digital Viva examinations will be last series in its current format. Series 1 of 2023 will see the rollout of the new Phase 2 examinations including the new Objective Structured Examination in Clinical Radiology (OSCER).
A heartfelt thanks to the Clinical Radiology Trainee Committee (CRTC) which has had a busy and productive year. The 2023 CRTC has recently been appointed and I look forward to working with them over the next year. While some jurisdictions had multiple applicants, several had none and I encourage all trainees to consider volunteering for this very important committee. It is an opportunity to have a voice as there is broad representation across the many educational and training committees of the College, and to be involved in the decision-making processes.
The Clinical Radiology Paediatric Working Group (CRPWG) was established earlier in the year to identify new and innovative ways of providing additional training, exposure and supporting trainee learning outcomes within paediatric training. As you will be aware, some jurisdictions are finding it
hard to deliver the requisite training and experiential requirements to all trainees, and this has been a limiting factor in increasing the number of training positions. The CRPWG have been a very dynamic and hardworking group and have developed recommendations for appropriate paediatric training (pending approval) which will be included in the Training Program Handbook.
The Clinical Radiology Training Site and Network Accreditation draft standards will soon progress to broad external stakeholder consultation. The working group will now focus on the processes related to accreditation and review stakeholder feedback over the coming months.
I wish you all a restful summer break, a chance to relax and recharge for next year. Keep safe and enjoy the holidays with your loved ones.
Original Article: Pseudoendoleak: A post-endovascular aortic repair ultrasound surveillance pitfall – Single institution case series
Corresponding author: Timothy Buckenham, Department of Diagnostic Imaging, Christchurch Hospital, 2 Riccarton Ave, Christchurch Central City, Christchurch 8011, New Zealand
Introduction: In the context of increasingly common endovascular treatment for abdominal aortic aneurysms, endoleak is a relatively common complication of (abdominal) EVAR, and ongoing multimodality surveillance programs are recommended by expert bodies including the Society for Vascular Surgery (SVS). We describe the colour doppler ultrasound (CDUS) finding defined as pseudoendoleak that may be misinterpreted as significant endoleak and may be resolved through the use of contrast-enhanced ultrasound (CEUS).
Methods: Retrospective review of cases at our institution identified five cases where apparent endoleak on CDUS was not evident on CEUS, performed immediately following CDUS. Results: Each of these five cases demonstrated interval increase in sac size at varying intervals post-EVAR, and in 4 out of 5 cases, no endoleak was demonstrated on multiple other modalities, at multiple time points. One case demonstrated an isolated type 2 endoleak at one time point, a finding that could not be reproduced. In each case, index-positive CDUS is thought to represent agitated fluid within the excluded sac that is not in continuity with the arterial blood pool as evidenced by the absence of CEUS enhancement.
Conclusions: In cases of positive post-EVAR CDUS, CEUS is an effective tool to exclude the presence of pseudoendoleak and thus avoid further and potentially invasive diagnostic modalities in an elderly and comorbid cohort.
Pictorial Essay: Granulomatosis with polyangiitis: Common and uncommon presentations
Corresponding author: Qiao Xin Tee, Monash Imaging, Monash Health, 246 Clayton Road, Clayton, Victoria, 3168, Australia
Summary: Granulomatosis with polyangiitis (GPA) is a multisystemic autoimmune small vessel vasculitis predominantly affecting the respiratory and renal systems. Other systems such as the central nervous system, orbital, cardiac and gastrointestinal systems may also be involved to a lesser degree. Although there are no imaging features that are pathognomonic for GPA, there are known radiological patterns suggestive of the disease and imaging plays an important role in diagnosis, assessment and monitoring of disease activity. This is more evident when combined with clinical features, biochemical values and histopathology results. This pictorial review aims to present both common and uncommon radiological features of GPA.
Original Article: Development of binational radiation therapy quality indicator reports for prostate cancer treatment using registry data
Corresponding author: Edward Chmiel, Alfred Health, 99 Walpole Street, Kew, Melbourne, Victoria, 3101, Australia
Introduction: Quality indicators (QIs) are metrics which seek to allow comparison of clinicians’ and institutes’ practice to best evidence-based practice. The Australia and New Zealand Prostate Cancer Outcomes Registry (PCOR–ANZ) is a bi-national clinical quality registry with coverage estimated to be over 60% of the men newly diagnosed with prostate cancer. We outline the production and ambition of institute-level QI reports to benchmark performance for radiation therapy in the treatment of prostate cancer.
Methods: An expert clinician panel was assembled to create a list of candidate QIs based on a comprehensive literature review, and on modified Delphi-method and expertconsensus voting. A separate implementation group—including, clinicians, epidemiologists, data managers and data scientists—employed an evidence- and consensus- based approach to generate an effective QI report designed for automated production and regular distribution to participating institutes. Feedback from the recipient clinicians was sought to enable refinement of these reports.
Results: Seven QIs, including three related to post-treatment symptoms, were deemed feasible to analyse with the currently available data. Utilising an existing report template employed for benchmarking of surgical indicators, a novel radiation therapy report was generated using registry data in a secure analytical environment. The first, beta version of these reports have been produced and confidentially distributed. It is planned to automatically generate these reports biannually and iteratively refine them based on the clinician input.
Conclusion: QI reports for the treatment of prostate cancer by radiation oncologists have been produced using data from Australia and New Zealand patients. These are being disseminated to institutes on a six-monthly basis allowing comparisons to de-identified peers. The reports aim to facilitate improving patient outcomes, deepen engagement with the radiation oncology community and increase the breadth of PCOR–ANZ coverage. Additional QIs will be included in future iterations of these reports as data matures.
Original Article: Variations in whole brain radiation therapy fractionation for brain metastases in Victoria
Corresponding author: Wee Loon Ong, Alfred Health Radiation Oncology, 55 Commercial Road, Melbourne, Victoria, 3000, Australia
Introduction: We aim to evaluate the use of different whole brain radiation therapy (WBRT) fractionation schedules for brain metastases (BM) in Victoria, and the factors associated with it.
Methods: This is a population-based cohort of patients who received radiation therapy for BM between 2012 and 2017, as captured in the Victorian Radiotherapy Minimum Dataset. We excluded patients with primary brain tumour and those who had ‘prophylactic’ intent treatment. The Cochran–Armitage test was used to evaluate changing trend in WBRT fractionation. Multivariate multinomial logistic regressions were used to evaluate factors associated with WBRT fractionation.
Results: Of the 3111 patients who had WBRT, 1048 (45%), 1291 (42%) and 312 (13%) had ≤5, 6–10 and >10 fractions WBRT respectively. There was progressive increase in ≤5 fractions WBRT use over time, from 37% in 2012 to 50% in 2017 (P-trend < 0.001). In multivariate analyses, increasing age, patients with gastrointestinal cancer, patients living in remote/regional areas and more recent treatment were associated with the use of shorter WBRT fractionation (≤5 fractions), while patients who had WBRT plus stereotactic radiosurgery, and those treated in private institutions were associated with the use of prolonged WBRT fractionation (≥6 fractions). Three hundred eighty-nine (13%) patients died within 30 days of WBRT, of which 241 (64%), 119 (32%) and 17 (5%) had ≤5, 6–10 and > 10 fractions WBRT respectively.
Conclusion: We observed large variations in WBRT fractionation that are associated with patient, tumour, treatment and institutional factors. It is important to continuously monitor and benchmark our practice in order to reduce potentially unwarranted variations.

If you are a member of the Royal Australian and New Zealand College of Radiologists, access JMIRO free online. - Go to www.ranzcr.edu.au
- Log in using your College username and password = FREE access to all JMIRO current and digitised backfile content from volume 1, 1957!
The Professional Practice Committee (PPC) has had its fourth and final meeting for 2022. It was a robust agenda and a successful face-to-face gathering in Adelaide during the ASM. Some of the key pieces of work relating to the PPC worth mentioning at this time include:
CPD, ePortfolio, resources and the ASM
If you haven’t completed your CPD activities on the ePortfolio for this year, please start entering your activities now. I would like to emphasise that it is an annual process and the requirements for 2022 need to be completed by 31 December—that is only 2 weeks away!
2022 has been a milestone year of transition for CPD and there has been a big focus around how to use the new online ePortfolio. I’d like to remind you that the College website has a series of CPD ePortfolio “how to” video guides available to assist you in navigating through some of the main processes required for submitting CPD activities. Each of the clips is only a few minutes long and a great go-to for additional instructions. You can access these clips via the website. Also, keep your eye out for the 2023 CPD Handbook on the website.
The combined CR and RO CPD session at this year’s ASM was a great success. We had a packed house and it provided members the opportunity to see a live demonstration of how to navigate the ePortfolio. We appreciated the lively engagement and the many questions we could answer in real time. My only
disappointment was that our session ran out of time, and we couldn’t continue the discussion.
I extend my thanks to the CPD team and College staff for providing support to members in the CPD space, I know the support will be ongoing into 2023.
If you have any questions or require support regarding the CPD Program or ePortfolio, please contact the College team at: CPD@ranzcr.edu.au
An exciting piece of work to watch for in 2023 is the development of a new College Learning Management System (LMS). As of August 2022, an urgent and growing need to offer members learning opportunities through structured content and educational modules has been identified across several business units. Benefits from an LMS will be delivered by providing direct access to:
• Resources and learning content from projects across the College
• Training modules on topics such as governance, confidentiality, and conflict of interest
• Orientation sessions demonstrating how to use the CPD ePortfolio
• And much more…
A centralised content delivery platform presents an opportunity to enhance the offerings to members and non-members in turn increasing the value of College membership. The PPC looks forward to watching this exciting project come to fruition.
Drs Marc Agzarian, Kwang Chin and Joe Feltham finish their final term on the PPC in the first quarter of 2023 and, I would like to thank them sincerely for their enormous contributions. They guided the PPC, and previously the CPD committee, through the new CPD requirements and their assistance in revising the CPD handbook along with other PPC members is to be commended. Their corporate knowledge and skills were of immense value. Thank you.
If you have any questions or comments regarding the work of the FCR Professional Practice Committee, please feel free to reach out by emailing the College team at: professionalpractice@ranzcr.edu.au
I’ll take this opportunity to wish you and your loved ones a happy and safe holiday season, enjoy the new year festivities. I look forward to a busy and exciting 2023.
Yours sincerely Dinesh
Associate Professor Dinesh Varma Chief of Professional Practice


• Providing feedback and advice on the implementation of the ePortfolio including the “how-to” guides and videos and work-based assessments
• Involved in developing the cultural competency component of the new curriculum
• Recommending and providing content for the centralised learning program
• Organising and running the Trainee Day at the RANZCR ASM
• Advocating for a reduction in the new “Transition to Fellowship fee”
• Auditing the after-hours workload of trainees across Australia and New Zealand including non-reporting tasks (discussions with clinicians, real-time reviewing of studies, etc.)
But out with the old, in with the new! Your fresh and shiny 2023 CRTC members are Annika Cruickshank (QLD), Son Do (QLD), Denver Khoo (QLD), Sian Chin (WA), Charles Robertson (NZ), Max Howcroft (TAS), and Rachele Quested (QLD). Sanjay Hettige (NSW) is not new but still fresh and shiny as he returns for his second bite of the CRTC cherry.
Although a part of me does love seeing Queensland dominating the competition like our State of Origin team from 2006–2013, it would be great if all states could be represented. If you’re from Victoria, South Australia, or the ACT and want to be involved in any capacity please let us know at clinicalradtc@gmail.com.
Hello Everyone,
And just like that another year draws to a close. It has been a huge year for trainees with the implementation of the new curriculum, ePortfolio, and Part 1 exams. I’d like to congratulate all trainees on making it through another tough year as we dealt with the lingering effects of COVID-19 both on our health system at large and the amount of sick leave we had to cover for. I hope the holiday season brings some rest, relaxation and a reprieve from infectious respiratory illnesses.
The CRTC has also had a massive year and I’d like to use this opportunity to spruik all the good work the committee has done in the trainee realm over the last 12 months:
• Providing input into the artificial intelligence modules for the new curriculum

• Involved in planning of the new trainee selection process
• And much more but you get the idea!
None of this would’ve been possible without this year’s stellar CRTC membership of Philip Ruppeldt (NZ), Hayley Wong (NZ), Sanjay Hettige (NSW), Upuli Pahalawatta (NSW), James Harvey (QLD), and Thilina Jayaratne (WA). I’d also like to give an extra special thank you to Tom Pearson (QLD) who has suffered through the underappreciated job of CRTC secretary for the past 2 years—you are truly invaluable.
The end of this year marks the end of my three-year tenure (reign of terror) on the CRTC with the last two years serving as Chair (fearless leader). I’d like the thank all the CRTC members, College members, and especially the College staff for their tireless work in keeping this ship afloat. Looking back on all the messages I’ve written during my term; I’ve become more and more unhinged as time has gone by. I hope you’ve enjoyed it as much as I have.
Signing off, Dr Sarah Robertson Chair, Clinical Radiology Trainee Committee

The College launched the Clinical Radiology Centralised Learning Program in early 2022, providing online educational lectures for all trainees, international medical graduates and FRANZCRs. Each lecture session is delivered by subject matter experts designed to support trainees in the Clinical Radiology Training Program.
The last Sunday of each month a new session is published to the College’s webcast library to view on demand. The response for this resource has been overwhelming, since launch there have been more than 3,500 views across the first seven topics. The College would like to take the opportunity to thank the following lecturers that contributed to the 2022 program.
A/Prof Michael Bynevelt
Dr Kate Mahady
Prof Alan Coulthard Dr Paul O’Connell
Head and Neck
Dr Grace Aw Dr Jennifer Gillespie
Spine Dr David Lisle Dr Scott Davies
Musculoskeletal Systems
Dr Catherine Hayter
Dr Clinton Pinto Dr Aziz Osman
A/Prof Bruno Giuffre
Chest
Dr James Bewes
Dr Sally Ayesa
Prof Catherine Jones
A/Prof Karin Steinke
Cardiac and Vascular Imaging
Prof Ken lau
Dr Stephen Merrilees
A special mention to Co-Convenors
Dr Sally Ayesa and Dr Jane McEniery who work tirelessly to coordinate and produce each monthly session.
The 2023 session will commence again in February, topics planned for 2023 include Procedural Radiology, Interventional Radiology and Interventional Neuroradiology, Breast, Obstetrics and Gynaecology, Abdominal and Paediatrics.
Members interested in presenting in upcoming CLP sessions are encouraged to email centralisedlearning@ranzcr.edu.au.
Non-Clinical
Dr Amy Imms
Dr Aden McLaughlin
Dr Nicholas Karsz
“A special mention to Co-Convenors Dr Sally Ayesa and Dr Jane McEniery who work tirelessly to coordinate and produce each monthly session.”

Gold Coast Convention & Exhibition Centre, QLD March 3 - 4, 2023 Scan for further details and to register.
At Varian, a Siemens Healthineers company, we envisage a world without fear of cancer. For more than 70 years, we have developed, built, and delivered innovative cancer care technologies and solutions for our clinical partners around the globe to help them treat millions of patients each year. With an Intelligent Cancer Care approach, we are accelerating the fight against cancer by harnessing advanced technologies such as artificial intelligence, machine learning, and data analytics to enhance cancer treatment and expand access to care. Join us on the beautiful Gold Coast as we explore hot topics like Access to Care, Health Equity, Multi-disciplinary Approaches, Workflow Challenges and Technology Innovation in the Radiation Oncology Environment. Immerse yourself in the Varian Experience. © 2022 Varian Medical Systems, Inc. Varian and Varian Medical Systems are registered trademarks of Varian Medical Systems, Inc. Refer enquiries to Varian Medical Systems Australasia on 1800.657.036 or customerservice-anz@varian.com

Even as 2022 ends, the work of the Faculty does not diminish. The scope and intensity of work of the many committees and working groups continue to be driven by work plans and necessity as internal and external imperatives impact the timelines of ongoing projects.
One of the most exciting pieces of work this year was the Annual Scientific Meeting that concluded on Sunday 30 October. Planning and work for the meeting began months, even years ago. It demonstrates the value of planning for the future. So too must the Faculty Council look ahead at all times while ensuring that current projects and operational pieces of work continue. It is also important to evaluate and review at the appropriate times.
This inevitably leads to change. Indeed, it is only with change that we can work towards improvements and addressing our priorities that have been set via our Strategic Plan and Action Plan for Māori, Aboriginal and Torres Strait Islander Health. These strategic priorities are delivered through much of the daily operations undertaken by our supportive secretariat and the volunteer members who provide such a strong unpaid workforce for our profession within our College.
It is this workforce that helps to train and educate our future radiation oncologists and sets the standards that our community expects of us. While we recognise these substantial efforts, we perhaps do not reward them as well as we could and should. As already highlighted in the October issue of
Faculty of Radiation Oncology eNews, on behalf of our Faculty we extend a heartfelt thanks to everyone. As a college we will continue to work on how else we can acknowledge your efforts.

Change is also what drives our understanding of our targets in radiation therapy and the ever-increasing precision in the delivery of radiation dose. The means to do so are much more sophisticated compared to even just a short few years ago. The adoption and integration of ever advancing software, perhaps almost to the extent of a degree of artificial intelligence and commissioning of clever and complex technology, allows us to deliver treatments we used to dream of.
At the same time, these advances allow us to continue our research into the radiation effects on normal and tumorous tissues to enhance our global understanding of molecular oncology which is where radiation therapy has its most fundamental therapeutic effects.
As a Faculty, all of us contribute to this every day, ultimately in the care of our patients in their best interests. In so doing, we must always review and evaluate the successes and understand “why” when the outcomes are not as desired.
Change requires many drivers. Some of these are external to our Faculty and College. There is a wide range of stakeholders that demand our attention to regulatory imperatives and standards that apply to a specialist college as well as the expectations and responsibilities we have to our patients and community. These drivers change as our place in
society evolves as society itself evolves and paradigms of cancer management evolve. We must be mindful of where we have been, where we are at any present time to try to understand where would want to be. Consider the College’s Strategic Plan already mentioned. The internal drivers therein are those we have set for ourselves as a college. As part of this, we must always review and assess what we set out to do while we undertake such change.
At the beginning of each year, the Faculty Council has a planning day as its first meeting to look at the work that has been done the previous year(s) and what must be done in the year(s) ahead to ensure we continue to deliver all aspects of our Strategic Plan and priorities. The planning day sets priorities and goals for the standing committees of the Faculty (Education and Training, Quality Improvement, Economic and Workforce, Research, Targeting Cancer, and Professional Practice with the Chairs of these committees appointed from the Councillors) and its working groups (a number of which are jointly constituted with the Faculty of Clinical Radiology). All these are well supported by a strong secretariat. We must work as a team to deliver these goals to meet internal and external drivers.
Overarching all of this is governance, the Faculty Council must responsibly oversee the work described. There are by-laws, policies and guidelines that determine how we do so. Ultimately, the Dean of the Faculty of Radiation Oncology has the responsibility for all aspects of the business of the Faculty. The Dean must always act in the best interests of the Faculty and our profession. The Dean also sits on the Board of the College and in so doing has an additional range of responsibilities of caring for all members of the College and in particular has a fiduciary responsibility. I acknowledge thanks to my fellow Board members in this work.

As with my predecessors, I have had the privilege to be an office bearer of the College in the position of Dean. It has been a learning experience that one can never be fully be prepared for. Indeed, if one does not “learn on the job” in this position, it would not be in the best interests of the Faculty, the College, our patients and society. As I complete my two-year term as Dean and eight years on the Faculty of Radiation Oncology Council, I welcome Dr Gerry Adams, the Dean-elect who takes over from 1 January 2023.

Over these past years, I hope I have been able to contribute to the Faculty and College. The secretariat has been very supportive and I do thank you. I especially thank all Councillors and our

leaders, past, present and emerging. Change is inevitable and necessary to ensure we have progress. To this end, we should consider ourselves as potential mentors and role models for all our members to understand and share where we are and get to where we would want to.
I acknowledge the Traditional Owners of Country throughout Australia. I recognise the continuing connection of Aboriginal and Torres Strait Islander people to the sky, lands, waters and culture and pay respect to their Elders past, present and emerging. I recognise Māori as tangata whenua and Treaty of Waitangi partners in Aotearoa New Zealand.


It is with mixed feelings that I pen my final report as Chief Censor. It has been both a rewarding and challenging three years, punctuated by instances of personal accomplishment and utter disappointment. Nevertheless, I would like to reflect on several milestones, including the successful delivery of both the 2020 and 2021 Phase 1 and 2 examinations, at the height of the global pandemic, and the launch of the new Training Program in February this year. Alongside the Training Program, two crucial and comprehensive accompanying documents were delivered—the Radiation Oncology Training Program handbook and the Radiation Oncology Learning Outcomes document. All these would have been impossible without the collaboration and determined efforts of my fellow colleagues, trainees and College staff.
The recent 72nd RANZCR Annual Scientific Meeting (ASM) was a resounding success and massive thanks and acknowledgement go to the organisers of Drs Laurence Kim, Ramkumar Govindraj and Christen Barras from Adelaide. Fellows and trainees have rebounded from their virtual prisons to attend in person, making this the most well-attended meeting ever.
It was a particularly heart-warming and poignant moment for me during the Annual Ceremony, when the names of trainees who have been admitted into Fellowship over the last three years were read out and the physical receipt of the Fellowship certificate was joyously celebrated together with their family and loved ones. This, I believe, is the vision of fulfilment and culmination of the years of
labour for all who volunteer to serve in the education and training arena, and it was an absolute honour and privilege to be a witness to this.
There is however still much work to be done moving forward. In September 2019, the Australian Medical Council (AMC) completed a full re-accreditation assessment of the College’s education, training and continuing professional development program, granting accreditation to the College for another four years. The AMC was reasonably satisfied that the College’s training and development programs substantially met accreditation standards. However, 30 conditions were stipulated to be met by 2022, with annual progress reports required.
A follow up assessment is required to be undertaken in 2023 before the current period of accreditation ends, focusing on the outstanding conditions from the 2020 report. The assessment will comprise of a mixture of training site visits, as well as interviews with College officers and key committee members between August and September 2023. This is a crucial event which requires significant input and work to meet all stipulated conditions.
With the launch of the new Training Program this year, there has been significant activity in the evaluation and review of the training program components including:
a) Iterative changes of the ePortfolio to improve useability of functions, modify access and dashboard views of users and revise access and process of completing work-based assessments
b) On-the-ground validity and useability of work-based assessments
c) On-the-ground validity of the entrustability scale.
The majority of these tasks has been performed under the operations banner of the Radiation Oncology Implementation Working Group (ROIWG), which was initially formed to implement changes delineated in the new training program and currently chaired by the Chief of Training and Assessment, Dr Lisa Sullivan. The initial terms of reference of this high-level working group sets out the end date of December 2021 but was extended for another 12 months in order to support the implementation of the new Training Program. With the anticipated dissolution of the ROIWG, and the recognition that continuing work is necessary to ensure that the Training Program is agile, responsive to feedback and continuously reviewed to maintain its fitness-for-purpose, plans are underway to form a new committee which will inform, advise and report to the Radiation Oncology Education and Training Committee (ROETC) in all matters related to training and assessment.
As stated in my previous report, there is major work that is currently underway with regards to accreditation. The Accreditation Review Working Group, chaired by the Chief Accreditation Officer, Dr Vanessa Estall, had its first meeting in May 2022 and continues its major review of accreditation standards. Draft accreditation standards and requirements have now been developed for individual training sites and these have been sent to key stakeholders for consultation. Guidelines for training networks will be developed separately. Major changes from the current accreditation standards include the re-focusing of standards on training sites and clear requirements for what constitutes adequate clinical supervision.
The Statistical Methods, Evidence Appraisal and Research for Trainees (SMART) workshop is a College event held annually in conjunction with the TROG Cancer Research Annual Scientific Meeting. It is designed to enhance trainee knowledge and skills in statistical methods, critical appraisal of the medical literature and research methodology. The workshop has biennial programs with each year rotating between one of two topics. After convening this event for many years, Dr Trang Pham has decided to pass the baton over to A/Prof Wee Loon Ong. I would like to offer my heartfelt thanks to Dr Pham for her many years of service and particularly for her efforts to ensure that this workshop continued to be delivered through the COVID-19 pandemic.
In line with the new Training Program, certain revisions for the SMART workshop were decided upon including:
a) Delivery of the workshop will continue as a face-to-face format in alignment with the requisite structure for the learning outcomes to be met
b) Changing the workshop as an eligibility requirement of the Phase 2 examinations to Progression to Completion of Training
c) Completion of the workshop can occur at any phase within the training program but is recommended that this occurs within 12 months of Phase 2 training to facilitate completion of the Research Project requirement.
Both the 2022 Phase 1 and Phase 2 Series 2 examinations were successfully delivered recently but finalised results are still pending, awaiting endorsement by the ROETC. Again, my sincere thanks go out to the many volunteer examiners who readily sacrifice their valuable time in ensuring that these examinations are delivered to the highest standards. There are still many goals that lie ahead in the examination space including final formation of both Phase 1 and Phase 2 examinations panels, increase in the number of and training of new examiners, change of format in the Phase 1 and 2 examination papers and finally, the launch of delivering the Phase 1 examinations and Phase 2 written examinations on a digital platform in 2023.
The Trainee Selection Working Group, chaired by Dr Catherine Bettington, continues its crucial work in implementing the proposed changes according to the five-phase selection framework recommended by the Selection Review Working Group in 2019. The group’s recent meeting considered strategies in which the College can:
1. take a more centralised and pro-active role in the initial selection of trainees
2. provide dedicated and streamlined resources to assist training networks to continue to manage recruitment and selection

3. consider practical ways to increase selection of Māori, Aboriginal and Torres Strait Islander applicants and applicants from rural and regional backgrounds.
Although much has been achieved in the last few years, it is evident that much remains to be done to develop and maintain our Radiation Oncology Training Program as a world-class training program. It is with much hope and optimism therefore, that with the dawning of a new era in 2023, with a new Chief Censor (Dr Lisa Sullivan), a new Chief of Examinations (A/Prof Alex Tan) and a new Chief of Training and Assessment (yet to be determined) as well as several new members on the ROETC, that I express my utmost confidence that our College will continue to shine and pave the way for education and training excellence.
All good things must come to an end. As 2022 comes to close, this is certainly true for our time as members of the ROTC. We’ve had the privilege of advocating on behalf of our peers with regards to education reform. We saw the implementation of two exam preparation sessions for the first time since the pandemic. We did our best to procure additional resources for trainees as a ‘quid-pro-quo’ to weather the impact of new fees. The “centralised learning platform” is an initiative we hope to see implemented over the coming year or so. And we look forward to seeing a new ‘roadshow’ being provided for soon-to-be-Fellows to help them procure employment opportunities. Thank you to all our peers for contacting us throughout the year to ask questions and give us feedback.
Our work would not have been possible without the support of our senior colleagues. Our Dean, Dr Keen-Hun Tai ensured that we always had an equal voice at the table. Particularly when discussing matters pertinent to trainees. He was always there when we needed him most. We can’t thank you enough Keen-Hun for all of your guidance and mentorship. Thank you. We’re very lucky that our Dean-elect, Dr Gerry Adams,
has shown the same commitment to supporting the success of trainees. Anyone who skips breakfast on a Sunday morning to attend a trainee meeting is clearly very passionate about our needs!
Thank you to Dr Yaw Chin, our Chief Censor, who had the Herculean task of implementing complex training and assessment reforms throughout a pandemic. He understood that trainees faced significant challenges attending to assessments (particularly exams) during the last few years. He was always open to discussing these concerns at Faculty Council meetings. And he also patiently fielded questions, together with Prof John Leung at our trainee forum. The incoming ROTC will continue to have this collaborative relationship with our new Chief Censor, Dr Lisa Sullivan.
There are innumerable College staff members who have been working tirelessly to help us. Thank you to Pamela Spoors for being the sounding board for our ideas. We really appreciate the time that you and Jenna Howell took to update us on new College initiatives. Despite our three-hour time-zone difference, it was always easy to contact you both as you always seemed to be at work! Thank you to Julia Snedic for enduring the approximately elevenbillion emails she would have received about exam prep courses. Julia, thank you so much for understanding how
important these courses were to us. And thank you so much for getting them across the line. We also wanted to thank Cheryl Jendrachowski for helping us understand the ePortfolio system—the videos are great. Apologies to the eNews and Inside News team for always being late with my messages (I never knew what to write). But thanks for always publishing them!
Finally, I would like to thank the 2022 ROTC—Tracy Lim, Therese Kang, Katherine Meng, Anna Lawless, Chris Williams, Peter Nguyen and Su Shan Chan. You are the reason our committee was a success. Thank you for giving up your weekends to attend meetings and time during the week to review countless documents. But most of all, thank you for your friendship.
Congratulations to Dr Tracy Lim on being elected chair of the 2023 ROTC. We know that you will take the best from what we did this year and continue to make it better. We wish you and your team endless success. We wish everyone a very Merry Christmas, and all the best for 2023 and beyond.
Warmest regards, Hari Kirupananther
2022 Chair | Radiation Oncology Trainee Committee

“Finally, I would like to thank the 2022 ROTC— Tracy Lim, Therese Kang, Katherine Meng, Anna Lawless, Chris Williams, Peter Nguyen and Su Shan Chan. You are the reason our committee was a success. Thank you for giving up your weekends to attend meetings and time during the week to review countless documents. But most of all, thank you for your friendship.”Dr Hari Kirupananther


Over the last decade there have been significant advances in the treatment of cancer. Advances include the development of targeted, immunomodulating medicines, such as monoclonal antibodies (mAbs), and radiation oncologic techniques which can deliver site-specific, high-dose Radiotherapy in short courses. These advances have led to improved patient outcomes, including quality of life, life expectancy and mortality rates.
Radiotherapy plays an important role in achieving these outcomes for patients and is integral to contemporary oncology practice. It is considered one of the four central pillars of cancer treatment; Radiotherapy, Surgery, Chemotherapy and Immunotherapy.
What follows a cancer diagnosis is a complex treatment algorithm that is highly dependent on the site of the cancer and the patient’s entry point into the healthcare system. Some, all, or none of the four pillars of cancer therapy, presented above, may be offered to patients as options for treatment or care. Navigating this can be daunting for many patients.
Radiotherapy is a commonly prescribed treatment pathway for patients diagnosed with cancer.
Despite this, the cost-effectiveness and advances in technology, radiotherapy is underutilised in Australia and eligible cancer patients are not always offered or receive access to this important intervention.
In Australia it is estimated that one out of every five cancer patients who should receive radiotherapy do not receive it. The difference is stark in some of our most common cancers, such as lung and prostate. An estimated 62% of eligible prostate cancer patients and 48% of eligible lung cancer patients do not receive radiotherapy.
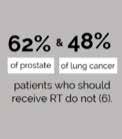
Varian, a Siemens Healthineers Company, commissioned an independent white paper to assess the barriers to accessing radiotherapy and how to overcome them. Through extensive research and interviews, this white paper provides three recommendations that improve access, raise awareness, and reduce the financial burden on cancer patients.
These recommendations have been designed to be simple and easily implemented within the existing policy frameworks of the Australian healthcare system, so that all Australians who are eligible to receive radiotherapy can do so.
Conservative estimates show that the underutilisation of Radiotherapy in NSW alone has resulted in the premature death of 1,162 people and the suboptimal management of local cancer containment for 5,062 people over a five year period. In the absence of other data on premature death, it is expected that these results can be extrapolated across Australia and may be worse in more remote locations where accessing radiotherapy has additional barriers.
Underutilisation of radiotherapy is having detrimental effects on patients’ health outcomes when it comes to cancer care. The full report independently written by Evo Health has identified opportunities within the Australian health system to improve uptake of radiotherapy.
These opportunities are:
• support multidisciplinary approaches to cancer care;
• improve awareness and understanding of radiotherapy; and
• improve equitable access to radiotherapy services
The full report, Shining a Light: Radiotherapy cancer treatment in Australia, was presented to Parliament House in November 2022
To view the complete article including a full list of references, please refer to https://evohealth.com.au/insights/
Further information can be obtained at www.varian.com
Please direct all enquiries to Varian Medical Systems Australiasia on 1800 657 036 or customerservice-anz@varian.com

Greetings. The FRO Professional Practice Committee (PPC) has had a busy 2022 and as we prepare for another productive year ahead, I’ll take this opportunity to mention a few key achievements in recent months:
ASM Session | Your CPD Home and an introduction to the 2023 CPD Program

At the ASM in Adelaide, I had the privilege of co-Chairing the CPD Program session with A/Prof Dinesh Varma, Chief of Professional Practice FCR. It was fantastic to see so many of you there, eager to attend this session to watch a live demonstration of the ePortfolio which then afforded us the opportunity to answer your questions on how to best navigate your CPD home. I offer my thanks to the CPD team and College staff for providing support to members in managing their CPD requirements, I know the support will be ongoing into 2023.
I’d like to remind you that your annual CPD activities for 2022 are due to be finalised on the ePortfolio by 31 December—a mere 2 weeks from now! If you’re seeking guidance, please visit the College website for a series of CPD ePortfolio “how to” videos which can assist you in navigating through some of the key processes required for submitting CPD activities. I am happy to advise that the revised 2023 version of the CPD Handbook is also now available on the website; another valuable resource to familiarise yourself with.
If you have questions or require support regarding the CPD Program or ePortfolio, please contact the College team at: CPD@ranzcr.edu.au
Gynaecological
The Gynaecological Oncology Radiation Oncology Collaboration (GOROC) SIG had a very successful meeting at the ASM this year. I’d like to make a special mention of the Gynaecological Brachytherapy Professional Development Guideline (GBPDG) which was finalised and endorsed by FRO Council at their recent meeting on 25 November.
This came about in response to the FRO Council’s recommendation in 2019, a survey was carried out on case numbers with all centres offering brachytherapy services in Australia and New Zealand invited to participate.
Pulling the data together from the survey, the Gynaecological Brachytherapy Professional Development Guideline was developed by a working group comprised of
the following members: Dr Carminia Lapuz, Dr Geetha Govindarajulu, Dr Stephen Thompson, Dr Robyn Cheuk and myself on behalf of GOROC. The GBPDG provides guidance on minimum caseload reflecting the need to balance required expertise, patient safety and access to treatment particularly in rural and remote areas of Australia and New Zealand.
If you have any questions or suggestions regarding the work of the FRO Professional Practice Committee, please get in touch at: professionalpractice@ranzcr.edu.au.
I look forward to bringing you further updates on the work of the FRO PPC in coming editions.
I’ll take this opportunity to sign off 2022 by offering you compliments of the season and best wishes for the new year! I look forward to continuing important work with the FRO PPC in 2023.
Best regards, Carol Dr Carol Johnson Chief of Professional Practice Faculty of Radiation Oncology

Fundamentally, we all want to provide the highest quality care for the patients we manage with radiation therapy (RT). How can we know we do this?

The new Australian and New Zealand Prostate Cancer Outcomes Registry (PCOR-ANZ) radiation oncology clinical quality indicator (CQI) reports are a good start for radiation oncologists and RT units looking after men with prostate cancer.
The initial two biannual PCOR reports have been released in a ‘slow roll-out’ fashion across Australia and NZ, and these twice-yearly reports will—in the fullness of time—go to all participating RT units and clinicians treating significant numbers of men with prostate cancer, to provide feedback on the patterns of presentation and care for the men they look after, and their outcomes; as well as providing comparison with deidentified peers from their jurisdiction.
Also, the reports for radiation oncologists and for RT units provide summary statistics on the origin and referral pathways for the patients managed with RT in the context of pathways for all the prostate cancer diagnoses in the states.
PCOR has been providing surgical quality reports on a biannual basis since 2016, and the RO reports were based on this experience. The QIs for prostate RO care were selected from the published literature and a survey, and then honed using a ‘Delphi process’ involving radiation oncologists David Pryor, Marketa Skala, Andrew Kneebone, Peppe Sasso, Hany Elsaleh, and Jeremy Millar. The reports were then developed in a co-design process working with data-scientists at Monash, to create the PDF reports generated by R Markdown from the data outputs from PCOR.
The RO clinical quality indicator reports are intended as individualised reports to ROs (indexed on the RO, irrespective of the facility site) and to RO sites (indexed on the facility site, irrespective of the RO). They thus provide two perspectives of the same large dataset. They are intended as part of a quality-improvement loop, and to be an ongoing ‘conversation’ between clinicians/facilities and PCOR to encourage improvements in the registry, the reports, and the care.
As well as the overall statistics, the secured and confidential reports also detail names of men who report back to PCOR that they have very poor qualityof-life symptom outcomes, so sites and clinicians can be made aware of these (if they don’t know).
PCOR hopes they will be interesting and informative to recipients and might provoke quality-improvement efforts similar to those seen by surgeons with the surgical reports. The reports are almost 30 pages long, and provide statistics and figures conveying descriptive statistics on the men looked after, and comparative and longitudinal information on the seven quality indicators based on process and outcome measures.
These bespoke, personalised quality reports are enabled by the RANZCRendorsed Movember-funded PCORANZ. PCOR is also endorsed by COSA, USANZ, MOGA, CCA, and Cancer Australia. The Australian Commission on Safety and Quality in Health Care (ACSQHC) has listed PCOR-ANZ as
How Well Do We Look After Men with Prostate Cancer?
“PCOR hopes they will be interesting and informative to recipients and might provoke quality-improvement efforts similar to those seen by surgeons with the surgical reports.”
a nationally prioritised clinical quality registry. The PCOR-ANZ is a federated quality registry, operating in accordance with the operational and governance principles incorporated in the ACSQHC ‘Framework for Australian clinical quality registries’ across all jurisdictions in Australia and New Zealand except (so far) West Australia, on a population-incidencediagnosis and opt-off consent basis.
Men are registered by a PCOR instance in each jurisdiction, and all combine and consolidate a common dataset in the PCOR-ANZ registry administered at Monash University in Melbourne with almost 75,000 men registered in PCOR-ANZ (from 2015) and in preexisting associated South Australian and Victorian registries. PCOR is particularly remarkable because it also collects, among other outcome datapoints, patient-reported outcomes measures (PROMs), directly from the patient, and using a standardised, validated, reliable, widely-employed prostate quality-oflife survey instrument. Two hundred and fifty sites participate, about evenly spread public and private; 382 clinicians participate (341 urologists, 23 radiation oncologists, and 18 medical oncologists); and PCOR distributes well over 1,000 individualised reports a year, on a biannual basis, via the jurisdictional PCORs.
Radiation oncologists make up a significant group of people in the PCORANZ leadership groups, for example Farhan Syed, Marketa Skala, Wee Loon Ong, Jeremy Millar, David Pryor, Saad Maqsood, and Doug Iupati. At a state level many more are involved. The leadership groups contain diverse group from many clinical, geographic and academic backgrounds; the Chair of the ANZ Governance Group is Professor Frank Frizzel, an academic colorectal
surgeon and Editor-in-Chief of the New Zealand Medical Journal.
PCOR has a wide range of activities apart from CQI reports, and collects and contains a wealth of data; PCOR encourages ROs with project and research ideas to partner with PCOR to make best use of the resource. The RO reports are a ‘first draft’ and PCOR expects and hopes to have feedback to allow improvements both in the data quality and in the report style and format. In turn PCOR hopes that these reports will stimulate and enable local quality improvement efforts in the RO management of men with prostate cancer.
In the broader radiation oncology quality effort, this type of clinical quality registry will become increasingly fundamental in cancer health care as part of the digital information framework promoted by the new Australian National Cancer plan. Already the College is in a process of endorsing another registry, the binational colorectal cancer registry,
and other cancer registries have been prioritised by the government: breast, lymphoma, and lung. We will start to see more of these, as well as reports for these, and ROs might be wise to get involved and become familiar with them to ensure that the registry and reports are fit-for-purpose as cancer care quality registries by recognising the important role RT plays in the care of patients with cancers. This is the mechanism by which we can get closest to knowing about the quality of care we provide.
 Prof Jeremy Millar Chair | Quality Improvement Committee
Prof Jeremy Millar Chair | Quality Improvement Committee
“PCOR is particularly remarkable because it also collects, among other outcome datapoints, patient-reported outcomes measures (PROMs), directly from the patient, and using a standardised, validated, reliable, widelyemployed prostate quality-of-life survey instrument.”


In 2014, the College commissioned a review of its training programs to evaluate the quality and sustainability of its training, assessment and examination activities, and to recommend strategies for improvement. Following this review, in 2015 the College initiated the Training and Assessment Reform (TAR) project to ensure the Clinical Radiology and Radiation Oncology Training Programs were revised in accordance with the recommendations of the review. A number of key milestones were achieved throughout this period resulting in changes to the curriculum learning outcomes, learning experiences, work-based assessments (WBAs) and examinations.
The two key concepts of the review centred on 1) the constructive alignment of the training programs to the learning outcomes, specifically, aligning the curriculum content, teaching strategies and assessment tasks, and 2) implementing programmatic assessment strategy by using multiple points and methods for assessing a trainee to provide a detailed picture of their competencies and development across the training program.
The outcome | What was achieved in 2022
The immense task of implementing the TAR project commenced early 2022, beginning in February with the launch of the enhanced training programs and the new ePortfolio platform for all new and transitioning trainees. To support the new training programs, the first Training Program Handbooks were published complementing the revised Learning Outcomes and updated training policies and providing detailed information on the various elements of the training program.
Additional learning guides, workshop resources, research templates and resource lists were developed and published as well as revamping the Trainee section of the College website
aligning the webpage content with the changes of the programs. The first evaluation of the training programs commenced in October focusing on the Work-Based Assessments and entrustability scales.
Future steps | What will happen in 2023?
The TAR project will conclude with the remaining milestones transitioning the various teams within the Specialty Training Unit. There are a number of targets scheduled for 2023 including:
• Announcing the results and recommendations from the first evaluation
• Publishing the second version of the Training Program Handbooks and Learning Outcomes
• Continuing to improve the functionality and user experience in the ePortfolio

• Implementing the changes to the Clinical Radiology and Radiation Oncology Examinations
• Commencing the second evaluation.
The College is grateful to all those who have contributed their time and their invaluable input to the TAR Project. Thank you to the members of the working groups, committees and Council who contributed to the TAR initiative. Finally, special mention to all the trainees, Fellows, staff and external experts for their professional expertise and involvement ensuring the successful launch of the Training Programs.
We are happy to report that OGSIG presented a session at the RANZCR2022 ASM in October. This was a mixture of invited speakers and proffered papers. Thanks to the convenors, especially A/Prof Christen Barras for the opportunity to present O&G Imaging content to a wider audience.
A reminder to diarise Thursday 23 March 2022 for the OGSIG's first faceto-face ASM in Adelaide. This is being convened by Dr Rachael McEwing who has put together a superb program. We are happy to announce superstar keynote speakers Prof Jon Hyett and Prof Rabih Chaoui. For the first time, we are calling for oral presentations from attendees with a $500 prize for the best paper. Please submit your abstracts by 29 January 2023. Go to ogsig.org for
more details. This meeting is aimed at the general radiologist who reports O&G imaging, with pro tips to make it more enjoyable and less stressful. If you can't make it the meeting in person, the lectures will be available on-demand.
 Dr Emmeline Lee Chair of OGSIG emmeline@westernultrasound.com.au
Dr Emmeline Lee Chair of OGSIG emmeline@westernultrasound.com.au
Under the guidance of our convenors, A/Prof Ronil Chandra and A/Prof Elaine Lui, planning for the 2023 ASM is making great progress.
On behalf the organising committee we are delighted to announce further details on this dynamic and interactive ASM which we have planned under the theme ‘New Horizons’; and we look
forward to welcoming all delegates back for a full face-to-face meeting in the coveted Mornington Peninsula.
The three-day ASM, commencing on Thursday 30 March at midday and concluding at lunchtime on Sunday 2 April, will bring together a mix of delegates, from RANZCRaccredited trainees, generalist radiologists, with an interest in head and neck and neuroradiology to interventional neuroradiologists, diagnostic neuroradiologists, nurses, radiographers, medical students, and JMOs.
With all borders fully opened, we will be joined, in person by two internationally renowned presenters in the fields of neuroradiology and interventional neuroradiology.
 Professor Alessandra Biondi (INR)
Professor Alessandra Biondi (INR)
Department of Neuroradiology and Vascular Radiology
Besançon University Hospital, France
Professor of Radiology, Neurology, and Neurosurgery
Joseph F. Sackett Professor of Radiology at the University of Wisconsin, Madison
The parallel program will include presentations from our key industry partners in INR, showcasing the latest technology and equipment, a diagnostic program, dedicated sessions for Head and Neck specialists and interactive cases with Radiopaedia’s Frank Gaillard.
Early Bird Registrations will be opening from Monday 21 November 2022 Delegates are reminded that ANZSNR
members receive a discount on registration. If you are not a member, we encourage you to join prior to registrations opening to take advantage of this great offer. To join the ANZSNR, please click this link: www.anzsnr.org.au/join-anzsnr
We look forward welcoming delegates to the RACV, Cape Schanck.

On behalf of the 2023 ASM convenors; Dr Murthy Chennapragada, Dr Luke Baker and Dr Phil Chan and the organising committee, we are pleased to announce plans for the 2023 ASM.
We are delighted that the ASM will be held from Tuesday 27 to Thursday 29 June 2023 at the newly refurbished and conveniently located Intercontinental, Sydney. The hotel is located on Macquarie Street in Sydney’s CBD, a short walk from the harbour foreshore and the beautiful Botanic Gardens.

Once again, IRSA is planning for a collaborative and vibrant meeting. The three-day scientific program will appeal to a diverse range of delegates, including RANZCR-accredited trainees and general radiologists with an interest in IR, and nurses and radiographers.
Arrangements are currently underway to bring out an excellent international teaching faculty. The three-day program will include a mix of didactic sessions, workshops, live cases, simulator sessions and more. Accredited trainees are encouraged to take up the opportunity as part of the Call for Abstracts offering for Oral Presentation opportunities where original pieces of research can be showcased. Next year we will again be partnering with CIRSE to offer the winning research presentation a trip to Europe for the 2023 CIRSE Congress.
To avoid missing out on the discounted early bird offer, please visit our ASM website to register and book your accommodation.
www.anzsnrasm.com
For queries or to find out more, please contact the secretariat at secretariat@anzsnr.org.au
Interested delegates are asked to please save the date. Further information regarding registration early bird opening dates, call for abstracts and announcements on the scientific program will be made shortly.
Reduced ASM registration is offered directly to current IRSA members. IRSA offers various categories of membership to suit all demographics and interested
delegates, who are not yet members, are encouraged to join IRSA prior to registrations opening to take advantage of this great offer.
For more information regarding the other benefits on offer and to join, visit: www.irsa.com.au/join-us/
For questions or queries, please contact the secretariat at secretariat@irsa.com.au
Kia Ora Koutou. New Zealand just finished hosting the Women’s Rugby World Cup with lots of exciting action. Go the mighty Black Ferns – great result!
The New Zealand Branch Committee and the New Zealand Radiation Oncology Executive have begun discussing the College’s advocacy priorities for the 2023 Election. We are open to hearing from the membership about the advocacy priorities so please email the Branch your thoughts. We plan to keep the wish list short and the messaging punchy and simple. Our current thinking can be summarised as follows:
• The workforce crisis for radiation oncology has only deepened over the last few years and is compromising existing services and making the prospect of staffing new services in Northland, Taranaki and Hawkes Bay unlikely. The need for more trainees and a staff retention scheme remain the top priorities.
• A national RIS/PACS would enable reporting efficiencies and accuracy, reduce redundancy of imaging and improve regional access to subspecialist expertise. The creation of Te Whatu Ora, particularly in these early days, has created a once-in-a-generation opportunity. Te Whatu Ora is actively promoting interoperability within a consistent nationwide health service—a national RIS/PACS should fit with that plan. We won’t be recommending a system but if anyone has a favourite, please share. The Branch Committee members are curious.
Te Whatu Ora and Te Aka Whai Ora
Nearly six months after the launch of Te Whatu Ora and Te Aka Whai Ora, New Zealand now has Te Pai Tata (the Interim Plan for the healthcare system).
Te Whatu Ora has also released some updates from the Planned Care Taskforce and the Workforce Taskforce. Many members will have also attended recent Te Whatu Ora presentations at work.
What is clear from these documents and presentations is that there is a focus on equity and the goals are ambitious. However, a plan without a pathway to achieving its stated goals feels incomplete and I am still uncertain about how these goals will be achieved. New Zealand’s radiation oncologists will be pleased about the commitment within Te Pai Tata to “establish the agreed radiotherapy satellite sites for linear accelerator services (LINAC rollout) to improve people’s access to treatment in their communities and ensure equity of access to radiotherapy.”
The College supports the expansion of new radiation therapy services in Aotearoa. However, there is no detail about how the bunkers will be built and no confirmation of funding to train the staff needed to operate the new LINACs. New Zealand’s radiation oncology services are already shortstaffed.
Increasing training numbers is not the only solution but given the lag time between deciding to fund more trainees and actually producing fully trained staff, making decisions to increase training numbers probably should have been the priority. Unfortunately, the Workforce Taskforce Webinar on 11 November seemed to confirm that plans to increase training numbers are not a priority. There was a lot of discussion about enabling flexible and modular training, not to mention working at top of scope.
Radiologists might feel more hopeful with the announced funding for 15 additional trainees (split over three years) and the Planned Care Taskforce which is considering radiology capacity, which suggests more trainees may eventuate. However, workforce issues for radiology services are also critical, particularly for our allied health. Some hospitals are now reporting 40 per cent MRT vacancies.

For members that have any research or education initiatives planned in 2023, please consider applying for funding from NZRET. Information is available on the NZ Branch page of the College’s website or you can email trust@ranzcr.org.nz.
If you have any thoughts, comments or suggestions, please email nzbranch@ranzcr.org.nz
Kia kaha. Stay safe, vigilant and strong.
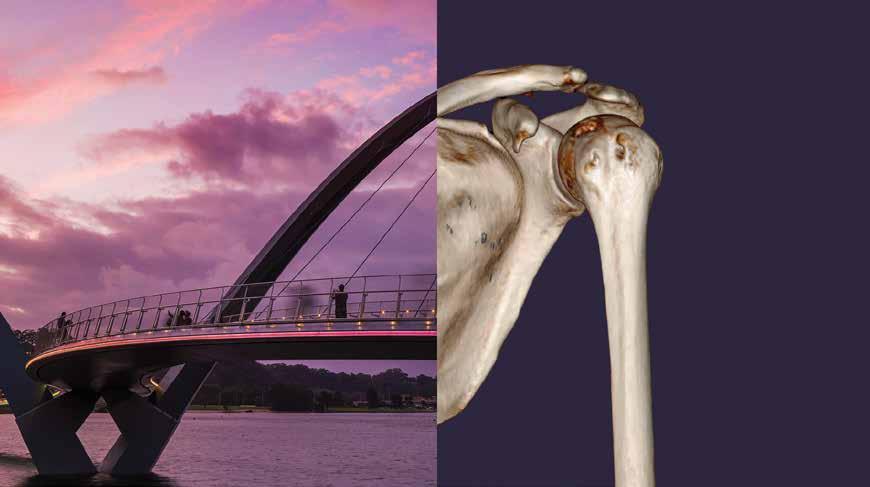
It has been a very busy six months for the FROGG executive committee culminating in our successful workshop in Hobart in September. We were very excited to have a record turnout of both attendees and sponsors. The FROGG executive would like to thank all of our sponsors as well as Leishmann & Associates, our conference convenors.
The theme of the meeting this year was ‘Precision Medicine in Prostate Cancer’ and the meeting also focused on revising the 2008 FROGG postprostatectomy guidelines. For many of the attendees it was their first face-toface meeting for several years and for some of our international speakers, their first trip to Australia. We had excellent input from our three invited overseas speakers, Professors Alison Tree and Chris Parker from The Royal Marsden Hospital and Daniel Spratt from Cleveland, as well as from numerous local colleagues who presented on topics for which they have recognised expertise, including urologist Dr Niall Corcoran.
Similar to previous FROGG workshops, there was a preceding survey of both the wider FROGG membership and our urology colleagues on postprostatectomy radiation, and Dr Anna Lawless presented these results. The program also included innovative planning sessions, case-based discussions and a lively debate. Of course, the social functions did not disappoint.
The meeting also brought to a close the chairmanship of Dr Tanya Holt to whom the executive is grateful for her inspirational leadership. Stepping into her place is David Christie. Following the meeting, Daniel Spratt kindly posted a positive message and photo on Twitter.

The FROGG executive is undergoing expansion and expressions of interest were requested from College members. We were overwhelmed with positive responses and after interviews we can announce the appointment of three new members, Drs Shreya Armstrong, Neetu Tejani and Michael Jones.
We also gratefully acknowledge the many years of outstanding service of A/Prof Andrew Kneebone who has recently stepped down from the committee and to Dr Matthew Knox who has completed his two years as the trainee representative on the FROGG committee. An EOI for the next trainee rep will also be advertised shortly.
With our next FROGG workshop not until 2025, the executive committee will continue to work supporting trainee education in all things GU and prepare the manuscript for the revised post-prostatectomy radiation therapy guidelines. FROGG will also be working on some exciting new educational ventures in 2023….for that you will have to watch this space!


ANZPROG seeks to build a community for the members to connect, share their experience and find opportunities to collaborate.
Join ANZPROG as a member. Please don’t hesitate to get in touch.
T: +61 2 9268 9777 | E: FROSIG@ranzcr.edu.au | W: www.ranzcr.edu.au
The Terms of Reference for ANZPROG are found on the RANZCR website.
In 2023, ANZPROG AGM will be held at the RANZCR ASM 2023 in Brisbane.
ANZPROG Members Forum meets twice a year and invites the members to engage in conversations around relevant and pertinent topics in palliative care and palliative radiation oncology. Past topics for the Forum include the Rapid Access Palliative Radiotherapy Clinics in Australia and New Zealand and the Voluntary Assisted Dying— an RO perspective. The next Members Forum is anticipated to be held in April 2023 and the details will be available soon.
In 2021, ANZPROG conducted an ANZ clinical practice survey on the Rapid Access Clinics. This study was published in the Red Journal (Roos D, James M, Lah M, Pope K, Shorthouse A, Govindaraj R, Holt T. Rapid Access Palliative Radiotherapy Clinics: The Evidence Is There, but Where Are the Clinics? An Australian and New Zealand Perspective. Int J Radiat Oncol Biol Phys 2021:111;959-64).
ANZPROG’s current project is on the Use of Advanced Techniques and Technologies for Palliative Radiotherapy. A questionnaire is created around 5 palliative case scenarios to assess the current utilisation of advanced techniques and all FRO Fellows are invited to participate in the survey. Everyone’s view will be valued. Please find the survey link below to complete the ANZPROG survey.
www.surveymonkey.com/r/Palliative-Radiotherapy-Utilisation-Survey

See why Australian College members are selecting Medical Wealth Advisory for all their lending needs.
Starting with a complimentary mortgage review service by a specialist adviser, Medical Wealth Advisory aims to identify ways for you to structure loans to reduce taxation, improve your interest rates, strengthen your equity position and fund new investments.
Through Member Rewards, you can look forward to:
• Complimentary Service: No fees or charges for using our mortgage lending service.
• Specialist Lending Solutions: Customised solution utilising products and services from a range of lenders.
• Extended Service Hours: After-hours services that allow you to book a day and time that suits you.
• Dedicated Relationship Manager: Single contact point to handle your entire lending needs.
• Cash Back Offer: In addition to any lender promotional offer.
To find out more:
• Call: 1300 41 81 61
• Visit: www.medicalwealthadvisory.com.au
• Email: ranzcr@medicalwealthadvisory.com.au
College members across Australia can choose Home Loan Solutions—a team of finance professionals to assist with all types of lending such as home loans, investment loans, commercial loans, SMSF loans, motor vehicle loans or personal loans.
When a College member establishes a residential home loan through Home Loan Solutions, either a purchase or refinance, the following rebates will occur:
• Home Loan Solutions will rebate the member up to 50 per cent of Home Loan Solutions’ Up-Front Commission*. College members will be paid 50 per cent of their rebate when Home Loan Solutions receive the commission (approximately two months after settlement) and the remaining 50 per cent 18 months after settlement if the loan is still in place.
• In addition, if a College member refers a successful application to Home Loan Solutions, that is someone who is not a College member, Home Loan Solutions will give the College member a referral fee of $500.
• Home Loan Solutions will rebate 10 per cent of Home Loan Solutions’ UpFront Commission* to the College.
*Note that the commission is calculated on the amount Home Loan Solutions receives less GST. Lenders pay different percentages in commission, but for an example on a $1.5M loan a College member could receive approximately $3,750 in rebated commission.
Home Loan Solutions can:
• Review your current lending and offer tailored advice to suit your circumstances.
• Filter through a huge range of products from multiple lenders with you, so you can choose a product that is right for you and not have to research alone. They are paid by the lender, so do not charge their clients for their services.
• Provide details of various grants or lender’s specials.
As Finance Brokers, Home Loan Solutions have an obligation to act in your best interest and will educate you to ensure you understand the loan you are applying for.
Contact Home Loan Solutions directly here: bit.ly/RANZCRHLS
Medical Financial Advisory Services Ltd (MFAS) provides specialised financial planning advice to health professionals across New Zealand and have been doing so for over 20 years. They have a comprehensive understanding of the opportunities and hurdles that RANZCR members may encounter throughout their career.
MFAS offers members a comprehensive range of services including:
• Investment advice and management
• Personal and business insurances

• Home loan lending and mortgages.
MFAS know one size does not fit all, so they tailor strategies to specific goals, ensuring each strategy will work in a simple but effective manner. The MFAS team includes specialists in investment, insurance and mortgage finance to deliver a professional friendly approach to optimise efficiency.
There are three easy ways to access this offer:
• Simply send your details to MFAS and they will contact you
• Email your details to MFAS
• Call MFAS on 0800 379 325
Visit our full Member Rewards Program here.

