Volume 18 No 1 | December 2021 Quarterly publication of The Royal Australian and New Zealand College of Radiologists Countering Uncertainty with Awe 2021 Research Grant and Award Recipients The IRTP: the Gippsland Experience Also Featured in this edition ‘De-cohorting' Post-Pandemic: Are We There? A 2021 TRIBUTE TO ALL MEMBERS
STAFF
AND
Radiologists, are you ready to be part of our team?
Beyond Radiology is growing.
We are recruiting Radiologists for new practices throughout New Zealand, with sub-specialist interests in Musculoskeletal, Spine and Neuro imaging. If you are the right candidate for one of these roles, you will receive a generous sign on bonus, the ability to own shares in Beyond Radiology and will be amply remunerated.
Please contact: Dr Philip Clark, Medical Director, Beyond Radiology phil@beyondradiology.co.nz
Beyond Radiology is a New Zealand owned, clinician led Radiology practice. Our team of healthcare providers are driven to provide excellence in patient care using state of the art imaging technology – including a NZ first EOS machine.
beyondradiology.co.nz

CT EOS ULTRASOUND NUCLEAR MEDICINE INTERVENTION X-RAY MRI
5 20
A Message from the President A Message from the CEO: Baton Changes
8 23
‘De-cohorting PostPandemic: Are We There?
What You Need to Know about
Medicare Compliance
The IRTP: the Gippsland Experience
CPD Program Changes Commencing January 2022
Meaningful Feedback in Medical Education
2021 Research Grant and Award Recipients
InsideRadiology: The Incalculable Value of Knowledge
RANZCR2021 ASM Wrap Up
Raising Our Gaze: Countering Uncertainty with Awe
From the Faculty of Clinical Radiology
Write First Time: Minimising Text Errors in Reports
Chief Censor in Clinical Radiology
Chief of Professional Practice Clinical Radiology Trainee Committee
The Transformative Potential of the IR Specialties for RANZCR
What are your thoughts?
If you have thoughts or comments about one of the stories you have read in this issue, we want to hear from you. The submission of letters to the editor, articles and news items is encouraged. Please email any submissions to editor@ranzcr.edu.au
Are You Ready for the RANZCR 2022 Training Program?
From the Faculty of Radiation Oncology
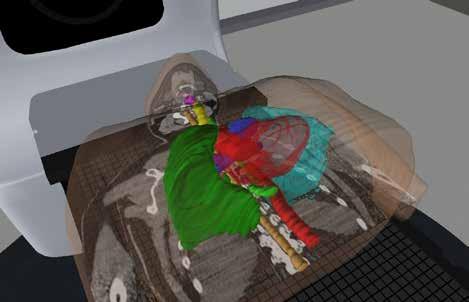
AI and the Quality of Radiation Oncology Practices
Chief Censor in Radiation Oncology
Radiation Oncology Trainee Committee News from New Zealand Varian brings Intelligent Cancer Care to Dubbo Targeting Cancer Fun@Home 2021
Have you moved recently?
Log into the MyRANZCR portal and ensure your contact details are up to date at www.myranzcr.com
Editor’s Pick Editorial Staff Editor-In-Chief Dr Allan Wycherley College In-House Editor Lindy Baker All rights reserved. No part of this publication may be reproduced or copied in any form or by any means without the written permission of the publisher. Publication of advertisements and articles submitted by external parties does not constitute any endorsement by The Royal Australian and New Zealand College of Radiologists of the products or views expressed. Inside News © 2021 The Royal Australian and New Zealand College of Radiologists® (RANZCR®) Inside News is printed on Sovereign Silk. Sovereign Silk is produced in an ISO 14001 accredited facility ensuring all processes involved in production are of the highest environmental standards. FSC mixed Sources Chain
Custody (CoC) certification
fibre
sourced from certified and well managed
of
ensures
is
forests.
51 34 52
17 39 14 41 37 45 43 46 48 30 32 7 13
News from the Branches
55 56 57 59 58 63
4D
Improving imaging confidence and patient experience




With 4D FreeBreathing, you can now offer free-breathing MRI liver to a broader population, while improving imaging confidence and the patient experience. This allows you to address patients who have difficulty holding their breath or find it difficult to follow breathing instructions.

4D FreeBreathing – Dynamic 3D T1w TFE Resolution: 1.6 X 1.6 X 5.0 mm Scan time: 3:16min Magnet ic Resonance
FreeBreathing
This is my final newsletter. After four years as President and nine on the Board it is time to hand the baton on. I have enjoyed my time, for the most part, it has been a privilege to hold this position and represent our profession. Four years ago, I listed what I thought were the biggest threats to our profession. It seems appropriate to revisit these.

Only a few years ago everyone was predicting the demise of radiology as a 'human' specialty, AI was coming and was so much better. We even saw a drop in applications for training positions (now reversed). However, from being the bogey man AI is now an exciting powerful tool that is going to make us super doctors. Yes, we have a long way to go, we expect difficult regulatory challenges, but the work we have done in AI—our committee, conference, ethical standards (a world first), the large AGM AI presence—has established the College at the forefront of Australian and New Zealand medical colleges in this field. We must work hard to stay there.
Increasing scope of practice of nurses, radiographers and sonographers into radiologist and radiation oncologist areas worried me for a long time, especially the work coming out of the NHS where it seemed anybody could do a course and report medical images. It's not that operating at the upper level of your training is bad, but it's hard to understand the impact this will have on our own work days, and the quality of work. My perspective has evolved. While I still have an issue with anyone reporting a medical image without
A Message from the President The Last Four Years
proper training (and will continue to fight for this), there are some things that can be done perfectly well by non-radiologists. Nurses have been placing PICC lines for many years, very successfully. I know I may be burned at the stake for saying this, but some radiographers and sonographers are very capable of learning procedures and safely performing them in a team. The powers-that-be know we cannot train enough future specialists and if we refuse to engage in this space we will simply be bypassed: a very bad outcome.
Other specialists entering the imaging field is another headache, not because they cannot do it, but because they tend to think they are better at it. Our experience in training and certifying imaging and oncology specialists has been hard won. The College is known for producing world-class, highly sought-after specialists. Why then, when cardiac CT became prime time, were we sucked into believing that radiologists and cardiologists needed the same new training and logbooks. I defy anyone to explain to me why a radiologist has to report 150 supervised cardiac CT cases to do one on their own, but you can jump into any other CT angiogram study without a hesitation. That's what we are trained for. When CT PET scanning arrived, somehow nuclear medicine physicians could pick up CT reporting after a weekend course, but radiologists need to do a two-year fellowship to report the PET component. We were caught off guard. My view is that the College is quite capable of deciding
what, if any, extra training our specialists need to pick up any skill, and we need to assert ourselves a lot more. Let’s learn from our mistakes, and maybe we will be able to redress them.
Radiologists and radiation oncologists are easily overlooked, sometimes on purpose. The 'doctor's doctor' or the 'hidden specialty', we have traditionally been an easy target—everyone knows how to do our job better than us and are only too willing to advise policy writers and funders. The College has two main areas of responsibility: training and assessment (pre and post Fellowship) and standards of practice. We have delegated powers for the former, basically what we say goes (as long as we follow the rules), for the latter we can only provide advice. This advice space can be very crowded.
Introduction Volume 18 No 1 | December 2021 5
Dr Lance Lawler
continued over...
“The powers-thatbe know we cannot train enough future specialists and if we refuse to engage in this space we will simply be bypassed: a very bad outcome.”
Four years ago, we decided that we needed to beef up our advocacy capabilities, so that we could make ourselves heard more clearly and more often, to become the trusted advisors in both medical imaging and our therapeutic specialties (IR, INR, radiation oncology, theranostics).
I believe we have made good progress. We are able to access decision-makers more regularly, and they seem inclined to listen to us more (not enough though unfortunately). A word of warning, it is imperative that we are not seen as a trade organisation, as any whiff of selfinterest rather than what is right for our patients sets us back. If we manage our conflicts of interest openly and properly, we will end up as an influential ally for future healthcare leaders.
Ironically, despite these external challenges, the hardest part of this role is managing internal conflicts. Our organisation runs on the freely given energy, enthusiasm and expertise of our members. I have regularly been in awe of how hard some of you have worked to advance our professions. On the flip side, we can be an opinionated bunch, so differences of opinion are inevitable, leading to all sorts of conflicts and headaches. Ultimately it seems it is always the 'College's' fault—as that dark overlord ruled by no name henchmen, at least that is what is often implied. I know members really want to call out the President and the Board but they are usually too polite (and almost always have the wrong end of the stick). For the record, in my experience, the presidents and the Board only have the professions’ best interests at heart. If you disagree with some calls, that's ok. If you want to influence things, run for a director's position. However, be very clear on your motivations—as long as our goals are to better serve our communities, referrers and patients we will do well.
My time as President has overall been a pleasure. I have immensely enjoyed getting to know so many of you and sharing your stories and views. I have gained many friends, here and internationally, and look forward to catching up with everyone when we are finally allowed to travel again. We have some great success stories to be proud of, some took a bit longer than expected (I am talking about the training and assessment reforms, a graveyard for well-meaning souls but also a triumph of perseverance for those who stuck it out). We are on the cusp of a major step change in our training and exam processes and systems. We are very well placed for the future.
members, but we are now on the right path. This is a significant step for our interventional colleagues who are falling behind the other procedural specialties in their ability to deliver end-to-end care.
There are many other good news stories, including collaboration with the The Royal College of Radiologists over clinical guidelines (work in progress), working with the Department on e-referrals, addressing inequitable MRI funding/access, cementing the College’s role in redeveloping the Cancer Australia Plan and the new health reforms in New Zealand. Too many more to list.....
I want to pay special tribute to my Board and the CEOs I have had the pleasure to work with. Natalia, Mark, and now Duane have all been effective leaders and made a difficult job easier. I wish Duane all the best, everything I have seen so far reassures me we have made an excellent choice. To the Board members, who see the best and the worst of the College, your considered thoughts have made us a better organisation. I will miss our regular meetings (or will I...?).
From a complete vacuum on Indigenous issues, we have now a well-formed and functional Māori, Aboriginal and Torres Strait Islander Executive Committee, ably chaired by our Board's independent director, Prof Vin Massaro. This is a strong platform for us to address the institutional flaws preventing us from achieving much better healthcare outcomes for Indigenous populations. I have high hopes for MATEC.
We have made good first steps in defining our interventional specialties This has been hampered over the years by strong differences of opinion by
A special mention to our College staff, without whom nothing gets done (you do not get enough credit); and of course to you, our members, without whom there is no College. I look forward to a beer or two with you.
All that remains is to wish Sanjay luck— my advice is not to sweat the small stuff (there is too much of it).
6 Inside News
Introduction
“I have immensely enjoyed getting to know so many of you and sharing your stories and views. I have gained many friends, here and internationally, and look forward to catching up with everyone when we are finally allowed to travel again.”
“To the Board members, who see the best and the worst of the College, your considered thoughts have made us a better organisation.”
As our President offers his farewells in his last Inside News column, I am at the opposite end of my College journey and typing my first column as your CEO. As someone with a long career in leading membership associations (including as interim CEO of the RACP following their online exam failure) and an experienced governance professional, I am thrilled to be given the opportunity to lead the College. My first weeks here have been a whirlwind of new acronyms, new people, new issues, new processes, and a new history to learn. I look forward to meeting more of you in the New Year as the borders across Australia and New Zealand open.
Farewell to our departing President and Treasurer
Lance Lawler has been President of the College for a remarkable four years and during that time, the College has undergone an incredible transformation. The role of president in a medical college is often time-consuming and thankless. It requires the patience of a saint, the negotiating skills of a senior diplomat, and the ability to guide Directors and members through multiple options in often uncertain environments.
The role also requires a leader who can work positively with the CEO to deliver long-term benefits to the College, encouraging the CEO and the management team to achieve, while ensuring Board oversight so that management delivers to the agreed strategic plan.
Lance has delivered extremely well against all these measures and after two terms as President, I am sure he will welcome the opportunity to take a
A Message from the CEO Baton Changes
breath and regain some of his valuable time. On a personal note, I will long carry Lance’s sage advice to his new CEO at our last Board meeting. The Board is also saying goodbye to our Treasurer, Brigid Hickey. Brigid has established a strong Board financial governance framework with the College’s Finance Manager, Jennifer Maher, during their time together. She also made an enormous contribution as Chair of the ASM Management Committee for the last four years. Brigid leaves the Treasurer position knowing that the College is in a solid financial position and that the Board is receiving the financial information it needs to make good decisions.
On behalf of members and staff, thank you Lance and Brigid.
Farewell to our interim CEO Mark Nevin

Along with our Board changes, the College also bids farewell to our interim CEO and long-standing staff member, Mark Nevin. Over an extensive career with the College, Mark had transformed our Policy and Advocacy capabilities, before announcing his intention to leave for a career change. Mark graciously accepted the interim CEO role twelve months ago and has guided the College through some uncertain times, while delivering a raft of key initiatives for the College. After handing over to me and catching his breath, Mark has now resumed his intention to change his career. We all wish Mark the best for this change, knowing he will succeed in any endeavour he chooses to pursue.
RANZCR 2022−2024 Strategic Plan
College members would have recently received an email with a link to the RANZCR 2022−2024 Strategic Plan. This plan builds upon the 2019 Strategic Plan and focuses on six Strategic Priorities:
• Member Experience
• Advocacy
• Education
• Workforce
• Clinical Excellence
• Organisational Resilience.
The plan provides goals and key initiatives under each of these strategic priorities. The College engaged in extensive member consultation during the creation of our strategic plan and we received considerable member feedback, which was then used to refine the plan to its current format. Thank you to everyone who contributed their thoughts during this process; your insights are much appreciated. We now have a College roadmap for the next three years, thanks to your efforts.
Our College team met in early December to build a series of action plans under each of these strategic priorities, that will operationalise the strategy and allow us to deliver the objectives of the plan.
Introduction Volume 18 No 1 | December 2021 7
Duane Findley
“On behalf of members and staff, thank you Lance and Brigid.”
'De-cohorting' Post Pandemic: Are We There?
Despite general acceptance (and relief) that the health systems in Australia and New Zealand have weathered the COVID crisis reasonably well over two hard years, hopes for a rapid return to normality in the third have dimmed markedly.
‘Highly doubtful, maybe in 2023,’ says incoming College President, Sanjay Jeganathan, when asked about prospects for normalisation.
As medical experts grapple with the implications of waning vaccine efficacy in 2022 and the potential for new variants and novel viral threats in the longer term, the future looks uncertain, and calls for new and urgent investment in health care are growing.
So, what can we reasonably expect the new year to hold, and what remains to be done?
Internationally, the COVID-19 pandemic—the fifth pandemic in a century—has to date killed in excess of five million people (second only in number of deaths to the Spanish flu pandemic of 1918–19) and devastated the lives of tens of millions more, economically, educationally and socially.1
The global impacts are likely to be felt for many years, especially among the poor and middle-income nations.
The World Health Assembly, the decision-making body of the World Health Organization (WHO), is currently seeking to develop a treaty on pandemic preparedness and response and, in May 2022, it is expected to examine proposals to give the WHO greater powers and resources to deal with future pandemics.2
Overworked, under-resourced
Australia and New Zealand have fared far better than most countries in coping with COVID-19, especially in health care, vaccinating their populations efficiently and maintaining vital hospital capacity throughout the pandemic's acute phase. However, the extra workload on medical and other health staff has taken a toll. A recent survey in NSW hospitals found that 38 per cent of junior doctors admitted to making medical errors due to working excessive hours, while 47 per cent felt their personal safety was at risk from fatigue.3
they're doing long days and some are doing additional College work because our normal processes have been disrupted. . . they have just been slammed,’ he told Inside News
One thing is clear: ‘COVID-normal’ is the catchphrase of the new decade. Health authorities do not expect a snap-back to pre-pandemic life any time soon, but rather an adaptation to a more or less permanent shift in healthcare delivery, including changes in the work of radiologists and radiation oncologists.
Some challenges facing medical practice are the result of general disruption across the health sector—for example, deferred elective surgery—while others are more specific to radiological practice, such as later-than-normal presentation by cancer patients due to lockdowns and postponed check-ups. The head of interventional radiology (IR) at The Alfred and incoming Dean of the Faculty of Clinical Radiology, Gerard Goh, says IR is again ‘very busy’ as deferred procedures have lengthened waiting lists and pushed many category 2 and 3 patients into category 1 and 2, respectively, requiring more urgent treatment. In addition, ‘the number of COVID and suspected COVID patients here has been significant, which increases pressure on our waitlist because these patients typically take much longer’ to process, he said.
Dr Grabau says a lack of relevant data is hampering efforts to interpret for medical administrators the impact of workload increases in clinical radiology which predate the pandemic but may have accelerated since its arrival.
The impact on senior clinicians and specialists may have been similar. The head of the College's Workforce Unit, Brendan Grabau, says many of the clinicians he speaks to are currently at risk of burnout. ‘They're really tired,
The College is currently undertaking analysis to better measure the workload generated by not just the number of radiological studies performed, but also the complexity of each study and the detail within each image assessed.
8 Inside News
Features
“Australia and New Zealand have fared far better than most countries in coping with COVID-19, especially in health care, vaccinating their populations efficiently and maintaining vital hospital capacity throughout the pandemic's acute phase. However, the extra workload on medical and other health staff has taken a toll.”
Clin A/Prof Jeganathan does not expect a normalisation of care in clinical radiology and radiation oncology practice in 2022 and he has highlighted both supply and demand issues facing the College and the specialties.
‘We have had few overseas doctors coming to Australia and this has helped create a shortage of medical specialists’. And he feels the issue may get worse before it gets better. ‘Our newly-trained specialists usually go overseas for a year or two to gain further experience. This has not been possible for two years, and now, with the reopening of the border, an exodus will begin,’ he said.
Dr Grabau notes that, due to the moratorium on inbound overseas travel, the College now has a backlog of applications from international medical graduates waiting for face-to-face interview and assessment, which will be difficult to process quickly.
In addition, the general public is seeking greater access to doctors because they have become more concerned about their health care. Among nondoctor medical staff, including nurses, radiographers and medical physicists, as well as non-medical staff, the shortages are ‘dire,’ A/Prof Jeganathan says. ‘This will be a huge problem for at least a few years. The existing workforce is working longer hours, with no leave or holidays, which is causing burnout’.
A/Prof Jeganathan expects many of the public health responses to the pandemic to remain for years to come, if not permanently. ‘Mask wearing, proper cleaning between patients, more PPE— these are measures that will stay with us for a long time, and that will add time and costs to carrying out our services,’ he said.
Medical waste
While the wearing of face masks has attracted a deluge of public attention and commentary, the general public is mostly unaware of the impacts of an explosion in the use of personal protection equipment (PPE) in health settings. Not least among these is the environmental impact of a muchincreased volume of medical waste, especially PPE made from treated latex or polypropylene. As the pandemic continues, so rises the risk of environmental contamination of marine and terrestrial habitats by plastics with limited or no biodegradability.
Medical waste is created in ‘phenomenal’ quantities worldwide, presenting serious challenges to the healthcare system during a pandemic, says A/Prof Goh. A recent media report mentioned that the Sunshine Hospital in Melbourne had experienced a 40 per cent rise in its clinical waste since the beginning of the pandemic, while estimates at other hospitals have ranged from 25 to 130 per cent, depending on the number of COVID patients admitted.4
A/Prof Goh says ‘there needs to be more research into safe and effective ways of recycling potentially contaminated PPE,’ while noting that radiologists can be smarter with PPE ‘at the patient-facing level’ and minimise unnecessary waste without compromising patient and staff safety.

Volume 18 No 1 | December 2021 9
Features
continued over...
“Dr Grabau says a lack of relevant data is hampering efforts to interpret for medical administrators the impact of workload increases in clinical radiology which predate the pandemic but may have accelerated since its arrival.”
What’s in Issue 6?

Medical Imaging
Original Article: Development of a risk prediction model of pneumothorax in percutaneous computed tomography guided transthoracic needle lung biopsy
Corresponding author: Jang Ho Weon, The University of Melbourne, Faculty of Medicine Dentistry and Health Sciences, Melbourne, Victoria, Australia.
Introduction: To retrospectively evaluate the incidence of and the risk factors for pneumothorax and intercostal catheter insertion (ICC) after CT-guided lung biopsy and to generate a risk prediction model for developing a pneumothorax and requiring an ICC.
Methods: 255 CT-guided lung biopsies performed for 249 lesions in 249 patients from August 2014 to August 2019 were retrospectively analysed using multivariate logistic regression analysis. Risk prediction models were established using backward stepwise variable selection and likelihood ratio tests and were internally validated using split-sample methods.
Results: The overall incidence of pneumothorax was 30.2% (77/255). ICC insertion was required for 8.32% (21/255) of all procedures. The significant independent risk factors for pneumothorax were lesions not in contact with pleura (P < 0.001), a shorter skin-to-pleura distance (P = 0.01), the needle crossing a fissure (P = 0.004) and emphysema (P = 0.01); those for ICC insertion for pneumothorax were a needle through emphysema (P < 0.001) and lesions in the upper lobe (P = 0.017). AUC of the predictive models for pneumothorax and ICC insertion were 0.800 (95% CI: 0.745–0.856) and 0.859 (95% CI: 0.779–0.939) respectively. Upon internal validation, AUC of the testing sets of pneumothorax and ICC insertion were 0.769 and 0.822 on average respectively.
Conclusions: The complication rates of pneumothorax and ICC insertion after CT-guided lung biopsy at our institution are comparable to results from previously reported studies. This study provides highly accurate risk prediction models of pneumothorax and ICC insertion for patients undergoing CT-guided lung biopsies.
Medical Imaging
Original Article: Gelfoam slurry tract occlusion after computed tomography-guided percutaneous lung biopsy: Does it prevent major pneumothorax?
Corresponding author: Reuben Sum , Diagnostic Imaging, 246 Clayton Road, Clayton, Melbourne, Victoria, Australia.
Introduction: Computed tomography (CT)-guided lung biopsy is a frequently performed procedure in the diagnostic workup for suspicious lung nodules that can be complicated by pneumothorax. This retrospective study assessed the efficacy of biopsy tract occlusion with a gelatin sponge slurry for preventing post-biopsy pneumothorax.
Methods: Retrospective analysis was conducted on consecutive adult patients who underwent CT-guided lung biopsy over a 10-year period. Age, gender, existing chronic obstructive pulmonary disease (COPD), evidence of emphysema on CT, location of the lesion and the presence of pneumothorax on post-procedure CT and 4-h chest radiograph were recorded. Results: Two hundred and ninety-six patients were included (126 patients in the non-gelfoam group and 170 in the gelfoam group). When gelfoam was used, risk of developing an immediate pneumothorax was lower (P = 0.032). Patients with emphysema were 2.4 times more likely to develop a delayed pneumothorax without gelfoam (P = 0.034). There was a significantly higher risk of both immediate and delayed pneumothorax in non-peripheral lesions without gelfoam (P = 0.001 and P = 0.002, respectively). The frequency of requiring a chest tube to treat a pneumothorax was 86% lower when gelfoam was used (P = 0.012).
Conclusions: Gelfoam is effective in preventing immediate pneumothorax. In patients with emphysema, there was a significantly higher risk of delayed pneumothorax without gelfoam. Additionally, non-peripheral lesions were more likely to develop pneumothorax when gelfoam was not used. The use of gelfoam was especially important in preventing the development of major pneumothoraces that would require drainage with a chest tube.
Medical Imaging
Technical Article: Computed tomography guided lung biopsy under general anaesthesia with apnoea: Preliminary experience
Corresponding author: Smita Deb , Monash Health Diagnostic Imaging, Clayton, Victoria, Australia.
Summary: Certain pulmonary lesions may be challenging to biopsy with conventional computed tomography percutaneous lung biopsy (CTPLB) under local anaesthesia (LA) which requires consistent patient breath holding to minimise complications. We aim to describe and evaluate the feasibility of CTPLB under general anaesthesia (GA) with apnoea, comparing results to patients undergoing biopsy under LA. This was a retrospective analysis of CTPLB with 18 GA and 137 LA patients. All biopsies were performed using a coaxial needle system in the radiology department on a multi-detector CT scanner with patient positioning determined by assessing shortest distance to target lesion. GA cases were performed under relaxant anaesthesia with intermittent positive pressure ventilation. Lower lobar lesion location and a combination of size and location (including proximity to critical structures) were indications for GA biopsy in >90% of patients. Mean lesion size for GA biopsies was 18 mm and control group 30 mm (P < 0.006) and mean pleura to lesion distance 29 and 11 mm, respectively (P < 0.0009). Pneumothorax rates were lower in our GA biopsy group (11%) compared to control group (42%) (P < 0.05). No anaesthetic complications were encountered. All GA samples were diagnostic. Based on a small number of patients, CTPLB under GA with apnoea seems a safe, feasible alternative to conventional CTPLB under LA for technically challenging lesions. This technique is routinely employed at our centre allowing access to lesions previously deemed unsafe to biopsy.
Radiation Oncology
Original Article: Functional and patient-reported changes in swallowing and voice after combined chemotherapy and radiotherapy for limited-stage small-cell lung cancer
Corresponding author: Jacqui Frowen, Peter MacCallum Cancer Centre, Nutrition and Speech Pathology, Melbourne, Victoria, Australia.
Introduction: The purpose of this study was to describe the nature and impact of dysphagia and dysphonia in patients with limited-stage small-cell lung cancer (SCLC) before and after chemoradiation.
Methods: A prospective cohort study was conducted on patients receiving chemoradiotherapy for limited-stage SCLC. Patients received either 40, 45 or 50 Gy, commencing the second cycle of chemotherapy. Outcomes included: videofluoroscopy (VFSS) to investigate aspiration, swallowing function and oesophageal motility; oral intake limitations; patient-reported dysphagia; and patient-reported dysphonia. Data were collected before treatment and one, three and six months post-treatment.
Results: Twelve patients were enrolled. Oropharyngeal swallowing was safe and functional at all times. Three patients exhibited oesophageal motility disorders before treatment, and a further three post-treatment. Oral intake was most compromised one month post-treatment with five patients either tube dependent or eating very limited diets. At all other times patients were eating normal or near-normal diets. Despite normal oropharyngeal swallowing on VFSS, three patients reported moderate or severe dysphagia one month post-treatment. Three additional patients reported moderate or severe difficulties three and six months post-treatment. Patients who reported dysphagia one month post-treatment all received a mean and maximum oesophageal dose of ≥15.7 Gy and ≥42 Gy, respectively. Dose–response relationships were not apparent three and six months post-treatment. Voice problems varied, with worst scores reported one month post-treatment.
Conclusions:This study identified discordance between observed swallowing function and patient-reported problems, which has clinical implications for patient management, and highlights future research needs. Ongoing efforts to reduce mucosal toxicity in patients with lung cancer are essential.
Radiation Oncology
Original Article: A prospective evaluation of treatment recommendations compared to outcomes for a lung cancer multidisciplinary team and legal implications
Corresponding author: Daniel Klemm, 199 Ipswich Road, Woolloongabba, Queensland, Australia.
Introduction: This cross-sectional study compared treatment recommendations made by a respiratory multix-disciplinary team with the treatment received by those patients in practice. The aim was to evaluate the rate at which patients were treated in keeping with MDT recommendations. It was hypothesised that most patients would be treated in accordance with these recommendations. These data were then used to provide a practical basis to consider the potential legal liability of multi-disciplinary teams.
Methods: All patients discussed in the Princess Alexandra Hospital Lung MDT over a three-month period were included. The recommendations made by the MDT were compared with the treatment received. Where available, the reason for any change in management plan was recorded.
Results: 74/109 evaluable patients were treated in accordance with the MDT recommendation. A further 7 patients had commenced treatment prior to MDT discussion. The most common reasons for change in management were patient choice (n = 6) or deterioration in clinical condition prior to treatment (n = 6).
Conclusions: As hypothesised, there was a high rate of treatment in accordance with recommendations made by the MDT. Changes in management are mostly related to patient preference or change in condition after MDT discussion. In practice, there are only limited opportunities for an MDT to be liable for patient outcomes. It is suggested however that careful documentation and representation of cases where appropriate could further mitigate this risk.
If you are a member of the Royal Australian and New Zealand College of Radiologists, access JMIRO free online. - Go to www.ranzcr.edu.au -
1957!
your College journal online
Access
Log in using
= FREE
your College username and password
access to all JMIRO current and digitised backfile content from volume 1,
Disrupted supplies
With the acute phase of the pandemic beginning to recede (at least for those countries fortunate enough to achieve high levels of vaccination), so emerges a raft—or perhaps ‘container ship’ is the better term—of chronic after-effects as the world reacts in myriad ways to the impact of the pandemic.
Not least among the after-effects is a serious disruption to global supply chains, including supplies of vital medicines and medical equipment.
Radiologists claim they are experiencing shortages or delayed deliveries of various consumables, steroid injections, catheters, wires, embolisation devices and certain types of vacuum-assisted biopsy needles, to name just a few.
Lead times for replacing scanning equipment have stretched beyond six months in some instances, possibly due to a COVID-induced worldwide shortage of computer components.
Telehealth and tele-training
A public health measure that has enjoyed a mostly positive reception (and possibly a bright future) is telehealth, although it is unclear as yet if the Australian government will permanently list telehealth as a Medicare item in specialist care.

The College issued its radiation oncology telehealth principles in late August 2021, arguing that telehealth in radiological practice was a vital innovation for extending multidisciplinary care to rural and regional patients and lowering associated costs.
Meanwhile, Dr Grabau says the College has now largely shifted training and assessment online. ‘In our clinical exam, which is normally face-to-face, we used a digital version of that this year, with examiners in different states, putting images up on a screen and asking candidates to talk about the images.’
The College is also looking at other technology which would enable remote proctoring and improve exam security.
‘It's a huge shift in the way we do exams,’ he said. The College can now run its annual scientific meeting entirely online and will deliver CPD workshops in a similar fashion. However, despite achieving good progress in the transition to online assessment, applications from trainees for special consideration have risen in the wake of the changes, a reminder that all change comes at a cost.
Nevertheless, most agree that the move online for consultations, multidisciplinary meetings, training and assessment will continue. ‘This is a big game changer for us,’ says A/Prof Jeganathan.
Volume 18 No 1 | December 2021 11
Features continued
over...
“In our clinical exam, which is normally face-to-face, we used a digital version of that this year, with examiners in different states, putting images up on a screen and asking candidates to talk about the images.”
Recovery
Finally, as we contemplate a COVIDnormal world, health experts have sounded the call for a recovery phase at the end of the ‘final post-vaccination phase’ in which Australia moves away from major lockdowns and border closures.
Victoria's chief public health officer Brett Sutton and the health economist Stephen Duckett are among those critical of the national COVID roadmap for assuming the nation can ‘soon heave a sigh of relief and simply move on.’ Instead, we need time and money for recovery, by which the authors mean (i) ‘time out’ for health workers to recover from the increased workload and stress; and (ii) investment and reform to address the inequalities exposed in the health system by the pandemic.
‘The real lesson of the pandemic,’ they write, derives from the assumption that respiratory viruses spread randomly through the population—they do not. Instead, they spread differentially in line with the social drivers of health, including job security, income, homelessness, overcrowding, low literacy and cultural marginalisation.
‘In 2022, public health practitioners and organisations must seek to better understand these social drivers of health . . . and receive the resources to redress disparities exacerbated by the crisis’.5
It is a view reiterated in New Zealand by senior radiologists such as Helen

Moore at Auckland Hospital. Dr Moore says the pandemic has compounded the problems created by years of neglect in infrastructure investment and chronic understaffing among medical officers. ‘I don't have all the answers but obviously [addressing] inequality and investing in health care and education are key to fixing our problems,’ she said.
These issues go well beyond the ambit of the radiologists but, given the pivotal role played by radiological medicine in diagnosis and treatment, and the considerable investments required in public and private practice to maintain their services, the time may have arrived for these specialists to step up and have their say about which resources are needed and where.
References
1 The World Bank, “World Bank/IMF Annual Meetings 2021: Development Committee Communiqué,” October 15, 2021, https://www.worldbank.org/en/news/pressrelease/2021/10/15/world-bank-imf-annual-meetings-2021-development-committee-communiqu
2 H.E. Ellen Johnson Sirleaf and Rt Hon. Helen Clark, “Losing time: End this pandemic and secure the future,” Independent Panel for Pandemic Preparedness and Response, WHO, November 21, 2021, https://theindependentpanel.org/mainreport/
3 Lucy Carroll, “Junior doctors report increased bullying in NSW hospitals, stress leading to mistakes,” The Sydney Morning Herald, November 17, 2021, https://www. theage.com.au/national/junior-doctors-report-increased-bullying-in-nsw-hospitals-stress-leading-to-mistakes-20211116-p599bx.html#comments
4 Emilia Terzon, “Australia's healthcare system is generating tonnes of COVID waste,” The Business, October 13, 2021, https://www.abc.net.au/news/2021-10-13/ healthcare-waste-COVID-plastic-recycling-reusing-hospitals/100533552
5 Stephen J. Duckett and Brett Sutton, “On entering Australia's third year with COVID-19,” MJA, October 27, 2021, http://doi.org/10.5694/mja2.51328
12 Inside News Features
“Lead times for replacing scanning equipment have stretched beyond six months in some instances, possibly due to a COVID-induced worldwide shortage of computer components.”
What You Need to Know about Medicare Compliance
An overview of the FCR Faculty Forum from the 2021 ASM
At the recent Annual Scientific Meeting, the FCR Faculty Forum focused on what a radiologist needs to know about complying with Medicare. Presentations were provided from three different perspectives. The session was extremely informative and provided valuable insights for members. Here is an overview of the session for those who missed it.
Presenter One: Dr Lincoln Gillam
Dr Lincoln Gillam, Chair of the RANZCR Diagnostics Economics Committee (DEC), provided the College’s perspective and encouraged members to reflect on the structure of the radiologist/employer relationship and Medicare billing.
• The DEC is the College committee which provides advice to the Faculty of Clinical Radiology Council on economics and policy matters, particularly related to Medicare and government policy.
• The radiologist is solely responsible for the use of their provider number. It can be considered in the same light as a passport or citizenship.
• Radiologists have a responsibility to know what is being billed under their provider number. It is recommended that you check what is being billed by your employer under your provider number each month.
• A list of billings under your provider number can be requested from Medicare.
• Compliance activities are conducted against the holder of the provider number, the radiologist, not the radiology practice.
• It is important to review your employment contact carefully and consider if indemnity against repayment of funds to Medicare,
References
if non-compliance is identified, is covered in the contract. It is worthwhile to have a legal review of any contract before signing.
• You can request that your employer does not use your provider number to bill particular services or particular item combinations.
Presenter Two: Mr Alex Taylor
Mr Alex Taylor, Director of Risk Treatment from the Benefit Integrity and Digital Health Division of the Federal Department of Health, provided insights into the government’s approach to Medicare Compliance.
The purpose of Medicare compliance activities is to protect the healthcare payment system to ensure sustainability of the health system. The Department of Health responds to non-compliance with a range of treatment approaches which are proportion to the level of concern around non-compliance. The treatment levels escalate as follows:
• Targeted letter campaign
• Audit
• Practice review program
• Professional service review
• Fraud investigation.
Priority areas for investigation this year include:
• Telehealth and COVID-19 items
• Practice incentive programs
• Potentially invalid referrals
• Patterns which may indicate opportunistic claiming that may not be clinically necessary.
The Department of Health has recently published the Health Provider Compliance Strategy1 which details the priorities for 2021−22. Department of Health resources to assist practitioners
in understanding Medicare billing include:
• Ask MSB email advice services at AskMBS@health.gov.au
• MBS Online at www.mbs.gov.au
• PBS Online at www.pbs.gov.au
• Services Australia MBS information at www.medicareaust.com/index
• Doctorportal Medicare Billing eLearning Module www.doctorportal. com.au
Presenter Three: Ms Gae Nutall
Ms Gae Nutall, Risk Advisor at MDA National, provided advice on what your Medical Defence Organisation (MDO) can do for you.
• If you receive any kind of notification from Medicare, the first thing you should always do is contact your MDO.
• Even if your employer pays for your medical indemnity insurance, the policy is an insurance policy directly between the MDO and the individual radiologist. The employer has no involvement in this relationship.
• All MDOs work together with the Department of Health and are aware of compliance activities to support their policy holders when required.
• ‘My colleagues bill this way’ is not an acceptable defence, so it is important to have a clear understanding of the items you are billing.
• Ensure all referrals and services you provided can be justified as clinically appropriate.
• You can check all provider numbers registered under your name and delete those no longer used via the PRODA2 website.
• Recommendation to visit the Department of Health resource on Provider Compliance Education.3
1 Department of Health. Health Provider Compliance Strategy. Available at www.health.gov.au/sites/default/files/documents/2021/09/health-provider-compliancestrategy-2021-22.pdf
2 Services Australia Provider Digital Access (PRODA) www.servicesaustralia.gov.au/organisations/business/services/proda-provider-digital-access
3 Department of Health. Health Provider Compliance Education. Available at www1.health.gov.au/internet/main/publishing.nsf/Content/For+Health+Professionals-1
Volume 18 No 1 | December 2021 13
Features
The College’s Connection with the Integrated Rural Training Pipeline
and Operations Manager at The Alfred to see if they could and/or would partner with us. Also to talk about how the program might be structured and to find out how they go about recruitment. Once we finalised how the program would look, we utilised the I-MED recruitment team as well as The Alfred and the Department of Health to advertise our position on the platforms they use.
We had a great response of up to 80 applicants. All applications were reviewed and those who best met the requirements for rural practising and prior training were shortlisted. Eight shortlisted applicants were asked to attend an interview, from which a candidate would be chosen.
The Integrated Rural Training Pipeline (IRTP) was established in 2015 as part of the Specialist Training Program (STP) in an effort by the Department of Health to extend vocational training for specialist registrars into settings outside traditional metropolitan teaching hospitals, including regional, rural and remote and private facilities.
The aim in creating the IRTP is to help build a sustainable Australia-trained future workforce for regional, rural and remote communities.

The College now fills four IRTP training posts within Victoria and Queensland, Australia, with a fifth position expected to commence in Queensland in 2022. Training sites need to meet different eligibility requirements to the traditional STP model to participate in the IRTP. Namely enabling a trainee to complete the majority of their training—two thirds—within a rural or regional location and making sure that the trainee selected has shown a real commitment to working rurally or regionally post Fellowship.
In the second of a series of articles about the rural training pipeline, we hear from trainee Dr Andrew Van and Kade Joske, previous Regional Manager I-MED Regional Pty Ltd (Gippsland, Latrobe Regional Hospital Traralgon). Dr Van commenced his training at the site in 2018, as one of the College's first IRTP trainees, and will undertake his final year in the program in 2022.
The training site perspective
At the time I'm fairly certain we were the first in Australia to establish an IRTP radiology training position, so we had to design it from scratch.
To get the program up and going, the first step was to look at the training requirements to ensure these could be met. It became clear on review that we would have to partner with The Alfred if our program was going to succeed.
As such, Mark Simpson, now General Manager Government Relations and External Partnerships, Dr Mohit Gupta and I met with the Director of Training
To select the final candidate, each applicant was ranked on who was best qualified to begin a radiology training position based on their experience, and most importantly, on their commitment to regional practice (ideally working and living in Gippsland long term). As a requirement of the appointment, as well as a main purpose of the program, this was to ensure medical specialists, in our case a radiologist, would stay living and working in the rural community post Fellowship.
As a result, Dr Andrew Van was offered the position and I'd like to think it has been a positive experience for I-MED and for Andrew.
14 Inside News
Features
The trainee perspective
Are there any advantages in your opinion of training at a large regional hospital compared to a metropolitan hospital?
The biggest advantage is the breadth of cases you come across; the rural patient population is diverse with many presenting to radiology without any prior imaging. As a registrar you can therefore provide great value to the referring doctors and have a direct impact on patient health. There are plenty of feelgood moments as patients are especially thankful for being able to access high quality specialist services without having to travel to Melbourne.
Are there any disadvantages in your opinion of training at a large regional hospital compared to a metropolitan hospital?
Regional work is especially busy, and with fewer specialist staff on site there are fewer opportunities for ad-hoc learning. Self-directed learning is crucial to the IRTP training success, and as a solo registrar you miss out on the rivalry that pushes you through the grind of textbook reading and exam practice.
Is there anything you think that the site is doing in the IRTP training post that is of particular help to you in your training?
I-MED is very receptive and approachable, happy to re-work rosters and worklists so that you can have the best training experience possible. Whether it's for Melbourne based lectures/classes, conference/ examination leave, or roster changes for metro rotations, there have been no logistical issues. The subspecialised radiologists, both on and off site, are very helpful; some will share both interesting and/or examination cases to you (shout out to Dr Andrew Kong over in Wodonga).
What advice would you give to a trainee commencing training in an IRTP position?
Keep in touch with your metro or other IRTP colleagues; the camaraderie and rivalry will push you through the sometimes very gruelling training. Trust the process and you'll make it through to the other side!
What would you recommend to get the most out of this type of training experience?
Set yourself short and medium term goals for both learning and College requirements. Being out in the country on your own it's easy to lose track of the hurdles along the way but you'll be able to chunk through it all if you keep organised and plan ahead.
What advice would you give a hospital/practice looking to start an IRTP position?
In return for an enriching specialist training experience, the IRTP registrar can provide direct and indirect benefits by assisting with workloads; from procedural work to being the first point of contact with hospital staff.
That said, the registrar education and training as well as the staff work environment will directly contribute to the likelihood of a candidate wanting to work with the organisation in the future. If well addressed however I think an IRTP position will be a fantastic opportunity for all involved.
A few facts about Gippsland Stretching from outer Melbourne to the eastern-most point of Victoria, Gippsland has a population of just under 300,000 with health care and social assistance, retail trade and construction constituting its three largest employing industries.

The area’s natural features are many and broad-ranging from mountains to coast and it is home to the rich diversity to be found within no fewer than 14 national parks.
As of January 2022, students at Federation University Australia’s Gippsland campus will have a direct pathway to study medicine locally at Monash University’s School of Rural Health, following the launch of a new degree. The universities are partnering in an effort to improve health outcomes for the region and strengthen the future of the local health workforce by developing the three-year Federation University Bachelor of Biomedical Science (Gippsland Partnership Program).
The degree will be offered from semester one 2022 and enable Gippsland students, subject to entry requirements, to be eligible to apply for graduate entry into Monash University’s Bachelor of Medical Science and Doctor of Medicine program at its School of Rural Health, which is co-located with Federation University at Churchill.
Volume 18 No 1 | December 2021 15
Features continued over...
More Information on the Australian Government Department of Health Specialist Training Program
The STP aims to positively influence future workforce distribution and quality. In 2010, the STP became the single Commonwealth grants support program for specialist training in Australia. The program now encompasses three complementary streams:
Specialist Training Placements and Support
Integrated Rural Training Pipeline - STP Training More Specialist Doctors in Tasmania (Tasmanian Project)
The College administers funding on behalf of the Department for training posts across all three initiatives in clinical radiology and radiation oncology. Colleges receive a set allocation of training posts under individual agreements. Training sites must apply for the program through an Expression of Interest process, which is managed by the Department in conjunction with each state jurisdiction and colleges. Successful posts are placed on the College’s reserve list and must be accredited to fill vacant positions. The College currently has 27 clinical radiology regional training sites (15 posts filled 1 FTE and 5 posts shared with public metropolitan sites are STP funded) and 14 radiation oncology regional training sites (10 posts are STP funded).
To find out more about the program and funding opportunities, please contact the STP team at STP@ranzcr.edu.au.
Reference 1. Australian Government | Department of Health | Specialist Training Program: https://www1.health. gov.au/internet/main/publishing.nsf/Content/workspec
Memorandum of Understanding with the Australian Indigenous Doctors’ Association
The College is delighted to announce that we have formalised our relationship with the Australian Indigenous Doctors’ Association (AIDA) via a Memorandum of Understanding (MOU).
As set out in the College’s ‘Statement of Intent for Māori, Aboriginal and Torres Strait Islander Health’ we are committed to supporting the professions of clinical radiology and radiation oncology to contribute to equitable health outcomes for Māori, Aboriginal and Torres Strait Islander Peoples. This work is central to the strategic objectives of the College and is reflected in the next College Strategic Plan 2022−2024.
The College will honour our commitment to Indigenous health by:
• increasing the number of Māori, Aboriginal and Torres Strait Islander Peoples in the clinical radiology and radiation oncology workforce;
• ensuring cultural safety is an essential component of clinical safety, and aligns with best practice and the accreditation standards of the Australian Medical Council (AMC)
and Medical Council of New Zealand (MCNZ);
• building and maintaining sustainable relationships with the Indigenous health sector;
• ensuring College governance and strategic plans address Māori, Aboriginal and Torres Strait Islander Peoples’ health priorities.
AIDA is the peak body representing Aboriginal and Torres Strait Islander medical students and doctors in Australia and is one of our key stakeholders. AIDA membership includes doctors across a wide and growing range of medical specialties. We share a common purpose—to contribute to equitable health and life outcomes, and the cultural wellbeing of Aboriginal and Torres Strait Islander Peoples, by striving to reach population parity of Indigenous medical students and doctors and supporting a culturally safe healthcare system.
The MOU outlines a range of activities in which the College and AIDA will collaborate, such as the sharing of
advice and perspective on policy and advocacy matters and ensuring effective support is in place as we work to encourage more Aboriginal and Torres Strait Islander trainees into our training programs.
We are also working to encourage more Māori trainees into our training programs and will be seeking similar arrangements with Te Ohu Rata ō Aotearoa (Te ORA) to solidify our efforts to strengthen our relationships with the Indigenous health sector.
If you have any questions please get in touch with Madeleine d‘Avigdor, Senior Projects Officer at madeleine.davigdor@ranzcr.edu.au
www.ranzcr.com/our-work/
16 Inside News
Features
links Statement of Intent for Māori, Aboriginal and Torres Strait Islander Health
Useful
indigenous-health-andengagement
CPD CHANGES FROM 2022
Different categories
Reminder: CPD Program Changes
Commencing January 2022
The College will be transitioning to new CPD requirements in January 2022, with additional requirements to be implemented from 2023.
2022 RANZCR CPD requirements
Members are required to:
• Complete a minimum of 50 hours of CPD per year
• Complete a Professional Development Plan (PDP) annually
• All CPD must be relevant to the doctor’s scope of practice and based on the Professional Development Plan (PDP) completed each year
Clinical Radiology (Australian-based members) Only

• If reporting MRI, eight CPD hours are required annually
• If reporting Mammography, four CPD hours are required annually.

Additional requirements from 2023
In 2023, there will be a minimum requirement of activity needed to be met across the three broad categories:
• 12.5 hours (25 per cent) of hours recorded under Educational Activities
• 25 hours (50 per cent) of hours recorded across Reviewing Performance and Reflecting on Practice and Measuring and Improving Outcomes (with a minimum of five hours for each category)
• 12.5 hours (the remaining 25 per cent) distributed across any of the three types of CPD.
An example of CPD activity types and where they fit under the three categories:
Most of the activities that fall under the three categories above will be similar to what you are presently allocating your CPD to.
Medical Council of New Zealand (MCNZ) Requirements (New Zealand members)
The Medical Council of New Zealand (MCNZ) requires that all New Zealand Fellows, Educational Affiliates and CPD Participants meet the requirements of an approved CPD program, which includes recertification, to receive an annual practicing certificate.
The requirements of the MCNZ include:
•
structured annual conversation with a peer, colleague or employer and;
• Cultural safety and a focus on health equity must be reflected in CPD activities.
For more information regarding the upcoming CPD changes, please contact cpd@ranzcr.edu.au
Volume 18 No 1 | December 2021 17
Same activities Hours not points Visit the new user friendly CPD portal All information www.ranzcr.com/fellows/ general/cpd-overview General Interest
Educational Activities Self-Directed Learning Conferences and Meetings Professional and Clinical Governance Teaching, Training and Supervision Publications and Presentations Research Miscellaneous Activities for example Mentoring Guideline Development Preparing Patient Education Materials Reviewing Performance and Reflecting on Practice Participation in Clinical Governance Activities International Governance Reflective Diary Peer Review Meetings Professional Development Plan Multi-source Feedback Accrediting/Auditing Practices, Hospitals, Training Sites Multidisciplinary Team Meetings Cultural Safety Measuring and Improving Outcomes Audit Database Logbook Multidisciplinary Team Meetings Patient Experience Survey
A
MEETING 2022 | ICC SYDNEY
HYBRID MEETING
The ARGANZ Executive are delighted to announce they are planning a hybrid meeting in 2022, with on-site attendance at the ICC, Sydney and the opportunity to attend the meeting virtually. The program will include virtual presentations from our international experts with live Q&A, and planned on-site presentations by our impressive Australian and New Zealand faculty. We invite you to join us at ARGANZ 2022.

INTERNATIONAL GUEST SPEAKERS
ARGANZ Workshop
Friday 25 March 2022
Planned on-site only
Scientific Posters
All radiologists are invited to submit a poster relating to abdominal imaging.
Share your research or present a review topic.
Mendelson Research Prize



All RANZCR radiology registrars and fellows in training are invited to submit an abstract for the Mendelson Research Prize 2022. Oral presentations will fulfill the requirement for sign off of the RANZCR Project 2.
KEY DATES
9 November 2021:
Registration and Submissions Open
23 January 2022:
Abstract Submissions Close


14 February 2022:
Standard Registration Fee Applies
CONNECT WITH ARGANZ Search for arganz radiology

@arganz_online
arganz_online

 IMAGE CREDIT: DESTINATION NSW
Alberto Vargas Chief, Body Imaging Service Memorial Sloan Kettering Cancer Center New York
Ania Kielar Associate Professor Toronto General Hospital Department of Medical Imaging
Michael P Hartung Assistant Professor of Radiology Abdominal Imaging and Intervention University of Wisconsin School of Medicine and Public Health
Perry Pickhardt Professor of Radiology Chief of Gastrointestinal Imaging University of Wisconsin School of Medicine & Public Health
IMAGE CREDIT: DESTINATION NSW
Alberto Vargas Chief, Body Imaging Service Memorial Sloan Kettering Cancer Center New York
Ania Kielar Associate Professor Toronto General Hospital Department of Medical Imaging
Michael P Hartung Assistant Professor of Radiology Abdominal Imaging and Intervention University of Wisconsin School of Medicine and Public Health
Perry Pickhardt Professor of Radiology Chief of Gastrointestinal Imaging University of Wisconsin School of Medicine & Public Health
- 27 MARCH
26
THE NEW E-PORTFOLIO SYSTEM
Introducing the New e-Portfolio System
Key features and functionality of the Kaizen e-Portfolio System
Mobile compatible? Tick. Greater automation? Tick. The Kaizen e-Portfolio System will offer College members greater onthe-go access and the ability to monitor and control their professional goals more than ever before.
Training Programs
• Sign-in via My RANZCR portal
• Mobile compatible
• Dashboard view—everything available on that main page for example, links to resources, websites, templates, reports etc.
• Overview of progress of each requirement in the current phase of training
• Ability to complete electronic templates built into the system
• Electronic templates embedded to deliver and track trainee assessments
• Assessments can be completed and signed off on the same device
• Robust reporting and graphs tracking entrustability over time
In 2022, the Kaizen e-Portfolio System will replace the current Learning Portal (TIMS, LMS and CPD). The system records data on trainee progression for clinical radiology and radiation oncology and is used to record CPD activities for members.
The new e-Portfolio System will be made available to members by 21 January 2022, to coincide with the launch of the 2022 Training Programs and CPD Program for clinical radiology and radiation oncology.
On logging-in to the system, the user-friendly dashboard view will allow members to see their progress against goals at-a-glance, in addition to accessing links to resources, websites, templates and reports from one centralised area.
Members who are involved in both the training programs and personal CPD activities such as Directors of Training or Clinical Supervisors, will have the ability to toggle between Training Program and CPD tabs under the one sign-in feature.
CPD
• Mobile compatible
• Sign-in via My RANZCR portal
• Dashboard view—everything available on that main page for example, links to resources, websites, templates, reports etc.
• Ability to complete electronic templates built into the system
• At a glance view of your progress against RANZCR CPD requirements
• Ability to monitor and evaluate trainee progression
How do I sign into the Kaizen e-Portfolio System?
The e-Portfolio System will be accessed similarly to the previous TIMS and current CPD platforms—using the MyRANZCR portal. Members can choose to use a desktop or mobile device to log in with the option to bookmark the portal to shortcut the signing in process.

Ongoing updates and further information
Updated information pertaining to the launch of the e-Portfolio System will be made available on the TAR section of the College website. The QR code allows for quick access to the TAR section on the website, or you can visit the site at www.ranzcr.com/tar
For further information regarding the RANZCR CPD requirements, please visit the CPD overview section of the website www.ranzcr.com/fellows/general/cpdoverview

Volume 18 No 1 | December 2021 19 General Interest
The Royal Australian and New Zealand College of Radiologists
Meaningful Feedback in Medical Education
Best Practice and Implications for Clinical Radiology Examinations
It is commonplace to hear differing views on feedback in medical education. Trainees argue that they don’t get enough and what they do get is not useful. Trainers argue that they give large volumes of feedback but trainees do not necessarily engage with it in the right way. A 2019 article in Medical Education suggests this disconnect arises due to differing conceptions of feedback itself by learners and educators (1)
Recent developments in the feedback literature
The academic literature on assessment and feedback in higher education has shifted in recent times away from conceptualising feedback as a justification or explanation of marks, to a focus on feedback primarily being about the ability to impact and enhance future learning (2). Thus, current thinking is that feedback should be understood as a relational process that is enacted over time. Key aspects of good feedback are: encouraging dialogue between the giver and receiver of feedback; involving peers; explicitly encouraging self-assessment and reflection; and encouraging learners to be proactive in working with feedback (3)
“Feedback is a process whereby learners obtain information about their work in order to appreciate the similarities and differences between the appropriate standards for any given work, and the qualities of the work itself, in order to generate improved work” (4)
Two major components of feedback are the quality of the information or data that is presented to the trainee, and the requirement for active engagement by the trainee. One without the other
results in a mismatch, and an inability for meaningful feedback to occur. For this reason, it is suggested that the term ‘feedback’ itself should be reserved for a process that is dynamic and coconstructive. ‘Dynamic’ simply means that the feedback is not a static object, report or piece of data. ‘Co-constructive’ means that the process of feedback should be collaborative, mutually respectful and negotiated in a shared social space.
Thus, the most effective place that a good quality and meaningful feedback process can occur is day-to-day in the workplace. The nature of these collaborative conversations may be influenced by many factors, such as the trainer-trainee relationship, the organisational culture and the context in which they occur. Good quality feedback therefore relies on having an ‘educational alliance’: a shared sense of purpose and goals, working together on shared activities, and a strong mentorlike bond (5)
In another recent paper, it is argued that “involving the learner in feedback processes is the best way to navigate the emotional responses that are reported in teacher-led feedback rituals characterised by one-way information transmission” (6). A safe and mutually respective culture is essential to this. Of course, praise and reassurance are a crucial part of the act of feedback, but the supervisor must also be prepared to challenge the trainee in ways that will help the trainee strive to become the best practitioner they can be. Difficult conversations (that are truly a dialogue, rather than a ‘telling off’) are an essential part of feedback.
Implications for high-stakes examinations
The above conception of feedback is in tension with many of the elements of feedback that typically arise from higherstakes assessments like examinations. Information that is necessarily ‘static’, such as results, grades, ratings and even comments from examiners, cannot in and of itself engage the learner dynamically. The trainee can choose to interpret the information from their own viewpoint and, if they wish, ignore information that challenges them.
This does not, however, imply that static feedback provides no value. With a point-in-time assessment, meaningful information can still be collected and fed back to the learner. But it is important to recognise the role of this type of feedback and ensure that it is used in a meaningful and effective way. The quality of the assessment data is therefore key.
In consultation with the Australian Council for Educational Research (ACER), the College is committed to providing feedback to trainees that is ‘diagnostic’ and reported in a way that is meaningful and useful.
Taking the new 2022 Phase 1 Anatomy examination as an example, several options for candidate results letters are currently being explored. The first option on page 21 provides candidates with their score in relation to the passing standard based on the standard setting process.

20 Inside News
Features
Option 1: Simple Pass/Fail reporting scores
Anatomy Exam
Your score: 52.3%
Passing standard: 58.6% Outcome: Fail
Options for Candidate Results Letters
Option 2: Pass/Fail overall and by format
Anatomy Exam
Your total score: 52.3%
Passing standard: 58.6% Outcome: Fail
Your scores by format:
Labelling: 84%
MCQs: 75%
VSAs: 40%
SAQs: 20%
Option 3: Performance in relation to the standards by curriculum topic area
Anatomy Exam
Your total score: 52.3%
Passing standard: 58.6% Outcome: Fail
Your scores by format:
Labelling: 84%
MCQs: 75%
VSAs: 40%
SAQs: 20%
Performance by topic area:
Brain – at standard
Head & Neck – well below standard
Spine – below standard
Thorax – at standard
Abdomen & Pelvis – well above standard
Limbs – above standard
Our view is that there are more meaningful ways of reporting to candidates, such as identifying areas of strength and weakness in an examination report—even if they pass the examination. Option 2 does this by breaking the candidate’s scores down by item format.
This shows that the candidate did well in the Labelling and Multiple Choice Question (MCQ) items, but struggled with Very Short Answer (VSA) questions and Short Answer Question (SAQ) items requiring them to draw upon their deeper understanding of anatomy.
Option 3 above is, in our view, better still, as more diagnostic information is provided across item types and mapped to the curriculum itself. The trainee clearly has a deficiency in their knowledge of anatomy of the head
References
and neck and the spine, but has a strong command of their knowledge of abdominal and limb anatomy. This trainee now has more nuanced information with which to target their learning going forward. They should be proactive in seeking out more opportunities for exposure to head and neck and spinal anatomy in their training.
The College welcomes feedback from trainees and trainers alike on these presented options. If you would like to provide feedback, please email the team at CRtraining@ranzcr.edu.au.
Finally, remember it is a two-part equation
It is important to remember that the diagnostic information provided in examination letters and examiners’
1 Ajjawi R & Regehr G. (2019). When I say… feedback. Medical Education. 53(7):652-654.
reports is only one side of the feedback equation. Examination reports can provide detailed and meaningful information to the trainee, but it is how the trainee actively engages with this information that is crucial to the process of feedback. This means trainees entering into a dialogue with supervisors and directors of training in the spirit of co-construction, and reflecting on their own learning progress in light of the information received from the College.
Dr Jacob Pearce Principal Research Fellow Specialist &
Professional
Assessment
Australian Council for Educational Research (ACER)
2 Jackel B, Pearce J, Radloff, A & Edwards D (2017). Assessment and Feedback in Higher Education: Higher Education Academy, York UK.
3 Orsmond P, Maw S, Park J, Gomez S & Crook A. (2013). Moving feedback forward: Theory to practice. Assessment and Evaluation in Higher Education. 38 (2):240–52.
4 Boud D & Molloy E. (2013). What is the Problem With Feedback? In Feedback in Higher and Professional Education: Understanding It and Doing It Well. London: Routledge:1-10.
5 Telio S, Ajjawi R, Regehr G. (2015). The 'educational alliance' as a framework for reconceptualizing feedback in medical education. Academic Medicine. 90(5):609-614.
6 Molloy E, Ajjawi R, Bearman M, Noble C, Rudland J & Ryan A. (2020). Challenging feedback myths: values, learner involvement and promoting effects beyond the immediate task, Medical education 54(1):33-39.
Features Volume 18 No 1 | December 2021 21

2021 RESEARCH GRANT AND AWARD RECIPIENTS
awards.
Clinical Radiology Early Career Researchers Prize
Dr Michael Vinchill Chan
“Non-contrast MRI for Hepatocellular Carcinoma Detection: A Systematic Review and Meta-analysis – A Potential Surveillance Tool?”
Faculty of Radiation Oncology
Bourne and Langlands Prize
Dr Wee Loon Ong
“A Standard Set of ValueBased Patient-Centred Outcomes for Breast CancerThe International Consortium for Health Outcomes Measurement (ICHOM) Initiative.”
Faculty of Radiation Oncology Quality Research Prize
Dr Wee Loon Ong
“Are We Choosing Wisely in Radiation Oncology Practice - Findings from an Australian Population-Based Study.”
Withers and Peters Grant
Dr Nicholas Wentworth Bucknell
“Biologically adapted radiotherapy using 4D 68Ga Ventilation and Perfusion PET to avoid functional lung in patients with non-small cell lung cancer (NSCLC) - the High Intensity Functional Image guided Vmat lung Evasion trial (HI-FIVE).”
RANZCR Research Grants
RANZCR research grants provide financial support for Fellows, Educational Affiliates and student members in clinical radiology and radiation oncology to conduct research. Grants are awarded for sums between AU$5,000 and AU$30,000.
Withers and Peters Grant
This AU$25,000 grant supports Fellows up to five years post-Fellowship and trainees post-Phase 2 exams to carry out significant research projects.
Clinical Radiology Early Career Researchers Prize
This AU$1,500 prize recognises a clinical radiology trainee or junior Fellow who is the first author of a paper accepted for publication by JMIRO or another Medline Indexed peer-reviewed journal.
Faculty of Radiation Oncology Bourne and Langlands Prize


This AU$1,500 prize is awarded to a trainee who has written an exceptional trainee research requirement manuscript.
Faculty of Radiation Oncology Indigenous Health Prize
This AU$2,000 prize is awarded in the case of high-quality research in Indigenous health being published in a peer-reviewed journal.
Faculty of Radiation Oncology Quality Research Prize

This AU$2,000 is awarded in the case of high-quality research in Quality Improvement in radiation oncology being published in a peer-reviewed journal.
For more information visit www.ranzcr.com/college/awards-and-prizes/research-awards-and-grants or email gaps@ranzcr.edu.au
Education Volume 18 No 1 | December 2021 23
Congratulations to the recipients of the 2021 research grants and
If you would like to apply for a research award or grant, the College is now inviting applications for 2021. A variety of opportunities are available to support research projects and foster a culture of research at the College.
2021 COLLEGE HONOUR RECIPIENTS
Christopher Hugh Atkinson, CNZM BSc, MBChB, Dip Ob, FRANZCR, FAChPM
The Gold Medal honours a Fellow who has rendered outstanding service or benefactions to the development, teaching or practice of clinical radiology or radiation oncology in Australia, New Zealand or Singapore.
A/Prof Atkinson graduated MBChB from Otago University in 1975 and began radiation oncology training at Christchurch Hospital in October 1977, obtaining his FRANZCR in 1982. After two years overseas as a postgraduate fellow he returned to New Zealand and was Head of Radiation Oncology at Christchurch Hospital for 20 years. He was inaugural Dean of the Faculty of Radiation Oncology in 1994, a member of Council, a member of the Faculty Board, and awarded the Rouse Travelling Fellowship in 1994 and the Roentgen Medal in 2004. Since 2005, the prize for the best radiation oncology paper at each annual scientific meeting of the College is awarded in his name annually.
He is Associate Professor in Medicine, University of Otago since 2000 and co-author of more than 75 published papers on cancer care. He helped establish the Trans-Tasman Radiation Oncology Group in 1989 and was the inaugural President. He has been National President and former Medical Director of the Cancer Society of NZ and was either Chair or Deputy Chair of all incarnations of Cancer Control in NZ from 1993−2012. He helped establish Psycho-Oncology NZ and was the inaugural President from 2005−2009. After 32 years as a radiation oncologist at Christchurch Hospital, he helped
establish St Georges Cancer Care in 2010, where he still works. In 2015, he was made a Companion of the New Zealand Order of Merit for services to cancer care.
“His career has exemplified the radiation oncologist, not only as highly skilled clinician and technician, but also as patient advocate, passionate activist for better care and quality of life of people with cancer, and dedicated administrator who ensures that health care and social systems can provide durable benefit to all patients.”
Roentgen Medal
The Roentgen Medal is awarded to Fellows who have made a very valuable contribution to the College over a significant period of time.
Dr Robert George Bourne graduated MB BS from the University of Queensland in 1955, training in radiotherapy at the Queensland Radium Institute, qualifying MCRA/FRANZCR in 1959 and FFR in 1963. He has worked at the QRI throughout his career as HOD, Mater Centre, Brisbane. He was Director of Education and WHO consultant to PNG reporting on radiotherapy to the PNG Government. From 1970 to 1985, he was College Examiner in Radiotherapy/Radiation Oncology and Senior Examiner 1985 to 1990. In 1972, he was appointed College Co-examiner (RO) for the FFR Exam. In 1963, he was the first to report in the literature (MJA) his discovery of 13 cases of what he called paradoxical fibrosarcoma of skin/ pseudo sarcoma and which was named atypical fibroxanthoma by Helwig (AFIP, Bethesda). He wrote many other single or first authored papers, such as the Costello Memorial Oration (NZ) on a large series of perineural involvement
of facial SCC, and treatment policy of Merkel cell carcinoma. He wrote the chapter on radiotherapy for the first and second editions of Emmett and O’Rourke Malignant Skin Tumours.
Dr Bourne was on the College Council in the late 1960s, Branch Chairman in 1972 and became President for the usual 12-month period in 1992. He found the Fort Street Headquarters inadequate for future expansion and oversaw the purchase of space in 51 Druitt Street. With the assistance of a committee of three, he wrote a constitution for the newly formed Faculty of Radiation Oncology. As immediate past President, he moved that a committee be formed to extend the presidential term and review the structure of College. He retired from practice in 1994 and in later life worked on the Trainor Trust.
“He has given lifelong service to and interest in College matters and continues a genuine interest in the profession of radiation oncology. Thanks to his vision, we have seen the preservation of valuable archival material which helps preserve the College’s rich history.”
Dr David Brazier graduated in 1979 from the University of New South Wales. He accepted a position as a radiology trainee at St George Hospital in 1980, moving to the Royal North Shore Hospital Sydney in 1982. On completing his fellowship, he remained at RNSH and saw the arrival of the first public MRI system in NSW, sparking his interest in MRI and neuroradiology. He has been actively involved in teaching at both the RNSH and Sydney teaching programs, and an examiner for the College for the last 25 years.
Education 24 Inside News
Gold Medal – Associate Professor
College Honours celebrate the important contribution clinical radiologists and radiation oncologists make to the health of patients across Australia, New Zealand and Singapore. It gives the College great pleasure to announce the recipients of the 2021 College Honours.
He was responsible for the College's Continuing Professional Development program and was awarded the Rouse Travelling Fellowship in 1991. He served on the Federal Department of Health Review of MRI which led to the introduction and setting of the Medicare fee for MRI. He was involved in Government negotiations including the relativity of CT items in the Medicare schedule, redrawing the MRI relativity and the abolition of the original threetiered MRI schedule, and had a position on the AMSAC sub-committee on assessment of MRCP and pelvic cancer. He served on the Diagnostic Medicine Clinical Committee and Diagnostic Imaging Clinical Committee, including a time as the Chairperson in the Medicare schedule review.
“David has had an incredibly farreaching influence on raising the calibre of innumerable Australian radiology trainees over his 35-year career as a radiologist to date. With kindness and patience, he has fostered the careers and mentored countless radiologists, many of whom, including myself, will forever hold him in such high regard.”
Life Membership
Life Membership is awarded to Fellows over the age of 65 who have made an unusually significant contribution to their field or the College.
Dr Michael Keith Alcock graduated with a Bachelor of Medicine, Bachelor of Surgery from the University of Tasmania in 1976. He commenced his training in radiology at the Royal Hobart Hospital 1980–1982, and later at the Queen Elizabeth Hospital in Adelaide 1982–1984, where he participated in a project on Dialysis Related Arthropathy. In 1984, he helped establish and validate a new protocol for imaging of neuroblastoma at the Adelaide Children's Hospital.
From 1999–2005 he was examiner in neuro/head-and-neck with an emphasis on more ear, nose and throat exam content and served as a College Councillor from 1999–2004. In 2000, he was appointed as the President of Australasian Musculoskeletal Imaging Group and was co-convenor of the AMSIG 2000 meeting which was a conjoint meeting for the first time with the Australasian Society for Ultrasound in Medicine. He worked for 13 years at Breast Screen Tasmania and working with two other colleagues, he introduced the first MRI service to Hobart in the1990s.
He joined colleagues to establish an MRI fellowship at Calvary Hospital Hobart. For 25 years, he ran an ENT Clinical-Radiological Meeting in the private sector with surgeons, providing invaluable feedback. Dr Alcock retired from I-MED Hobart in March 2021.
Dr (William) John Childs graduated MB ChB from the University Auckland Medical School in 1977. He completed specialist joint training in medical and radiation oncology training in the Oncology Department, Auckland Hospital with FRANZCR (FRACR) in radiation oncology awarded 1987 and FRACP in medical oncology in 1989. He completed specialist postgraduate training at Addenbrooke’s Hospital Cambridge UK followed by a Commonwealth fellowship position at the Royal Marsden Hospital UK. He works as a consultant radiation oncologist at the Regional Cancer Centre Auckland District Health Board since 1992, and has been Interim Clinical Lead for Radiation Oncology since 2020. He has held leadership roles with the Auckland District Health Board including as Clinical Director Radiation Oncology 1995 to 2001 and clinical leader for medical services 2001 to 2004.
Dr Childs was member and secretary of the NZ Radiation Advisory Committee 1998 to 2005 and principal drafter of the report used as a component of a report on improving non-surgical cancer services in NZ, as well as Chairperson NZ Cancer Treatment Working Party 2001 to 2008. He was National Clinical Director of the Ministry of Health Cancer Programme from 2005 to 2012 as advisor to the minister of health, responsible for implementation of the National Cancer Control action plan.
He was awarded the New Zealand Order of Merit in 2013 for contribution to health services. He has held a number of College roles from Clinical Examiner Part 2 1998 to 2007 to Chair of the of NZ Branch Advisory Body for Radiation Oncology for assessment of overseas trained specialists 2004 to 2019. At a national level, he remains the chair of the National Bowel Cancer Screening Advisory Group, member of the Bowel Screening Governance group and member of the National Radiation Oncology Work Group.
Associate Professor Lee Torine Coleman is a Clinical Associate Professor Radiology and Paediatrics at the Medical and Dental School, University of Melbourne. She is concurrently a paediatric radiologist at
the Department of Medical Imaging Royal Children’s Hospital Melbourne and has been for 27 years. She has also been a paediatric radiologist at I-MED Victoria since 2001. A/Prof Coleman has been part of FRANZCR since 1991. This has included training at Hamilton, Auckland NZ and Royal Melbourne hospital. She has completed a post graduate fellowship in paediatric radiology with an interest in paediatric neuroradiology at the Children’s Hospital of Philadelphia, USA in 1992–1994 under Professors Ken Fellows and Robert Zimmerman. She has a Bachelor of Medicine and Bachelor of Surgery from the University of Otago NZ and a BSc major chemistry/biochemistry. She has 76 co-authored publications and is part of the paediatric team involved in undergraduate radiology training at the University of Melbourne. She is involved in the Part 2 RANZCR Viva exams in paediatric radiology and for 20 years has provided three sessions per week of paediatric radiology services in Victoria to I-MED.
If you would like to nominate someone in one of the categories above in 2022, or the honours below, nominations will open in January.
The Clinical Radiology Educational Service Award recognises members who have demonstrated outstanding longterm commitment, participation and leadership in training and education in clinical radiology.
The Denise Lonergan Educational Service Award recognises members who have demonstrated outstanding longterm commitment, participation and leadership in training and education in radiation oncology.
An Honorary Fellowship recognises individuals who have contributed to the advancement of clinical radiology or radiation oncology and allied sciences, either through original research or by special services to the College.
The Sally Crossing Award for Consumer Advocacy acknowledges outstanding commitment of consumers involved in health care advocacy. The award honours the memory of the late Sally Crossing AM, in recognition of her exceptional contributions to advocating for cancer patients.
To find out more, or to nominate someone you know, visit www. ranzcr.com/college/grants-andawards/college-honours or email gaps@ranzcr.edu.au
Education Volume 18 No 1 | December 2021 25

Trusted Analysis | Excellence | Compassionate Care qscan.com.au Various engagement opportunities available. Significant sign on bonus available for the right candidate. Please email careers@qscan.com.au for more information about opportunities available in our incredible clinics in Hobart and North Queensland, or for a confidential discussion about any opportunities you may be seeking, phone Matthew Bellairs on 0412 939 200. 1 4 5 6 Ability to be part of a collegiate doctor network 2 Access to a broad range of clinical case mix 3 Enjoy quality work life balance whilst exploring some of Australia’s most beautiful locations Benefits of working with a high quality radiology practice State-of-the-art equipment Highly skilled staff What we have to offer: ARE YOU LOOKING FOR YOUR NEXT ADVENTURE? Opportunities in Hobart and Mackay
EDUCATIONAL FELLOWSHIPS
Fellowships for 2021.
Thomas Baker Fellowship
Dr Michelle Pui-Ming Li for Radiation Oncology
Dr Li has been appointed as the Clinical Proton Fellow at The Christie Hospital in Manchester, UK.


Windeyer Fellowship
Dr Shilpa Narula
Bill Hare Fellowship
Dr Liesl Marie Celliers
Rouse Travelling Fellowship
Not awarded in 2021
The College offers a variety of Fellowships each year, to support members in their continuing education and to further their knowledge and expertise. If you would like to apply for any of these opportunities, visit www.ranzcr. com/college/grants-and-awards/ educational-fellowships or email gaps@ranzcr.edu.au
Thomas Baker Fellowship
This Fellowship enables a clinical radiology or radiation oncology member up to six years post-Fellowship to further their knowledge by studying abroad for between three and 12 months. It is supported by a grant of AU$20,000.
Bill Hare Fellowship
This Fellowship supports a Fellow more than five years post-Fellowship for a period of intensive or overseas study (three to 12 months) or for attendance at an international short course (two weeks to one month) with a grant of AU$30,000.
Rouse Travelling Fellowship
In 2022, this Fellowship is available for a clinical radiology Fellow from Australia to attend the 2022 New Zealand Annual Scientific Meeting and to visit and present in their field of interest in three training centres in New Zealand. This is supported with a grant of AU$8,000.
Windeyer Fellowship
This is a 12-month position for Fellows up to two years post-Fellowship or trainees post-Phase 2 exams that provides clinical research opportunities at the Mount Vernon Cancer Centre in the United Kingdom. The position is under the broad supervision of Professor Peter Hoskin. There may also be an opportunity for the Windeyer Fellow to spend time at other UK centres including the Christie Hospital, Manchester, and University College London Hospitals (UCLH), where experience in subspecialty interests such as proton therapy, MR linac treatment and paediatric oncology can be provided.
Spotlight on Awardees
Dr Michael Chan, Thomas Baker Fellow, 2020

“I am grateful for the award and thankful to the collaborating co-authors. This research provides a basis for more advanced approaches for hepatocellular carcinoma screening.”
Ms Kate Idiens, ASM Indigenous Grant Winner 2021


“Kia ora. I want to thank RANZCR and express my gratitude for being the first Māori recipient of the ASM Grant, which allowed me to attend the 2021 event. As a medical student, there is limited exposure to radiology and therefore it was eye-opening to hear about the wide range of AI technology and IR procedures that are changing the landscape of this specialty. It was exciting to hear about how technology is working alongside radiologists to improve the efficiency and quality of care provided. The wide variety within the radiological field makes it an attractive training program for me to apply for in a few years’ time.”
Mr Jordan Glover, ASM Indigenous Grant Winner 2021
“Being given the opportunity to attend the ASM virtual event was extremely exciting and exceeded expectations. I was keen to attend the event as I wanted to learn more about radiation oncology, but left blown away at the diversity that’s associated with a career in radiology in general. I can’t wait to hopefully attend the next ASM in Adelaide next year!”
Education Volume 18 No 1 | December 2021 27
Congratulations to the recipients of the following Educational
25th AMSIG ANNUAL SCIENTIFIC MEETING Imaging in Sport
25th ANNUAL SCIENTIFIC MEETING
25th ANNUAL SCIENTIFIC MEETING
MAY 14 & 15 2022
MAY 14 & 15 2022
melbourne2022.amsig.org
MELBOURNE CENTREPIECE FUNCTION CENTRE
MELBOURNE CENTREPIECE FUNCTION CENTRE
The 25th Annual Scientific Meeting will focus on Imaging in Sport.

We plan to run sessions with shorter presentations covering interesting and challenging subtopics on traumatic and overload-related musculoskeletal injuries. Musculoskeletal radiologist, orthopaedic and sports physician speakers will be included in the program.
Virtual and in-person registration available.
25th ANNUAL
MEETING
SCIENTIFIC
A 2021 Tribute to All Members and Staff
the difficulties encountered and managed to provide an excellent service to all our membership. They are to be congratulated on a superb effort. They are the backbone of our College. As the Editor in Chief of Inside News, I was amazed at the work done in the College office by Lindy Baker and her colleagues. On top of that our readership increased by 90 per cent in 2021.
Dear Readers,
The beginning of 2020 seemed very much like the year before. Overseas and interstate travel was at a high level and large gatherings were a way of life. In the big cities people crowded on to public transport or jumped into cars heading for the city centre or other work sites accepting the time taken to travel to work.
Then it all changed! And these changes have altered life as we know it! Life will never be completely the same. The College staff were suddenly spending most of their time working from home. Daily interaction was via a computer screen. No chit chat over the morning coffee. Limited to the confines of their homes and for some the additional task of home schooling and additional care for others.
College members—Fellows and trainees—both in radiology and radiation oncology along with the very broad spectrum of allied staff both in private and public found their practice and home lifestyle completely altered. So did all their families and friends. For some the isolation was a massive hurdle to overcome. Not to mention the added toll of sickness and death of this wild pandemic.
So much uncertainty which still continues worldwide.
We all take pride in the way our dedicated College staff have absorbed
We should not forget also the large number of hardworking members who give of their time in the College management from the President down. They also had personal difficulties to address.
"We all take pride in the way our dedicated College staff have absorbed the difficulties encountered and managed to provide an excellent service to all our membership. They are to be congratulated on a superb effort. They are the backbone of our College.”
There was also the terrible disruption of training and examination timetables. The trainees I worked with battled on regardless.
Looking forward in 2022 we will continue to collaborate with colleagues from the committees, sub-committees, Special Interest Groups, and new Associate Members.
Keep the contributions coming it. The Newsletter is a fundamental communication avenue.
Hopefully 2022 will be a brighter year, despite the continuing challenges and everyone deserves to have a relaxing and pleasurable Christmas and New Year.
Best wishes to all of you and your families.
Dr Allan Wycherley Editor in Chief

As we head into our second end-ofyear break among the constraints of the pandemic, it is worth taking a moment in our day-to-day lives to reflect on the last two years: specifically on the immense contribution of all members of the College as clinicians to the management of our populations’ health care in this continued crisis, together with your colleagues in other medical and allied health professions.
When American anthropologist Margaret Mead was asked what she considered to be the first evidence of civilisation she answered: ‘a human thigh bone with a healed fracture found in an archaeological site 15,000 years old... in ancient times, if someone broke their thigh bones, they cannot hunt, fish or escape from the wild animals unless they are helped by others, who must have provided shelter, protection, food and drink over an extended period of time for this kind of healing to be possible.’
The sustained and civilised care necessitated by the global public health crisis has been delivered by the medical professions. We pay tribute to your efforts and recognise the toll this represents for members. We hope, as we approach the time of the year traditionally spent with family and friends, that you can find time to revive with your loved ones. We wish all members the very best for the season.
Dr Munish Verma Head of Member Engagement and Services Unit

Volume 18 No 1 | December 2021 29
Dr Munish Verma
Dr Allan Wycherley
The Incalculable Value of Knowledge …or the ongoing quest for access to the right healthcare information at the right time
Diagnostic Imaging (QUDI) program, and the College was quick to make way for the new, ‘health consumer’ movement that was starting to gain traction.
So, what is a health consumer?
was someone with a grudge to settle. In a few cases, this was correct and consumer representatives with their own agendas didn’t always make for a smooth transition into this brave new world.
The College is the peak body representing radiologists, specialist doctors at the forefront of the technological revolution in health care. It may not be so well known the College is also at the forefront of providing credible, professional information on its comprehensive and easy-to-access InsideRadiology website for health consumers and health professionals.
Radiologists are the only ones who have the background and understanding to ensure health consumers can access the right clinical radiology information at the right time. Health consumers need radiologists to engage directly with them through InsideRadiology and take their place in a multidisciplinary health environment. This way the College can remain in the vanguard of not only technological innovation but also information innovation.
It may be even less well known that the College was at the forefront of engaging a health consumer in its quality and standards programs.
In 2005, I was the first health consumer on the College’s Quality Use of
To try to understand what a health consumer is, we need to back up a few years before 2005. A definite change emerged as the general public became more informed and more vocal about health issues and had greater expectations of the health system. Experts would be able to better unpack the reasons for this trend but from a lay perspective, contributing factors might be the rising influence of the internet where people could access copious amounts of health information; the exponential curve in new and innovative health technologies that manufacturers proudly advertised, health professionals welcomed, and patients wanted to access; the impact of a greater number of private facilities offering an alternative to public health care, and perhaps the influence of the baby boomer generation who were of an age where they were accessing the health system in increasing numbers.
Whatever the individual factors that led to the change, they resulted in patients, ex-patients and other interested parties forming health consumer groups and organisations to advocate for better treatment and care, greater transparency and accountability, and for consumer groups to be included in healthcare policy and decision-making.
In the early days of health consumer representation, health professionals did not always embrace non-professionals being on boards and committees, and often genuinely could not see any benefit would derive from it. It was also believed a health consumer

My own journey and experiences with breast cancer gave me valuable insights into the system. I morphed from a consumer of health services into a health consumer representative serving on professional medical groups and committees to contribute my perspective into the mix of different perspectives working together to improve health care.
While there is still a way to go for health consumer representation, over the years the health sector and government have, I believe, come to see the benefit of the consumer perspective applied at all levels of the health sector, or at least have learned to live with it. Articles in professional medical journals always depict health consumers and health professional as two distinctly diverse groups of people, so it follows they will have two distinctly different perspectives to contribute to the big picture.
In health there is not a straightforward way to define a consumer as it is for consumers of other services and products. In both an individual and collective sense, it is fluid because everyone at some stage in their life will be a consumer of health services. As a health consumer representative my role is clear and that is to draw on my own experiences and the experiences of others to add my viewpoint. Sometimes the ultimate decision-makers accept my perspective and sometimes they don’t. The important thing for me is to ensure I give my view from a consumer perspective honestly and with conviction.
30 Inside News
Advocacy
Ann Revell
The knowledge gaps
One of the areas I have focused on is improving consumer information. While I was able to navigate the information maze on my journey there were gaps, and it was clear to me a lot of people would have difficulty finding the right information at the right time. Knowledge helped me get through the various tests and procedures, take an active part in managing treatment side effects and inspiring me to have a positive attitude. It gave me some control at a time when I felt like I was on a fast-moving conveyor belt.
Joining the College QUDI program was a match made in heaven for me because of the commitment of the College to embracing projects such as promoting the valuable role of radiologists in multidisciplinary team care, and its Australia-wide survey of what consumers wanted to know about radiology tests and procedures and how they wanted it presented. This latter project led to and informed several other projects, including InsideRadiology
The knowledge revolution
The number of people accessing InsideRadiology is increasing within Australia and New Zealand and from overseas. Importantly, InsideRadiology is reaching not only major centres but regional and remote locations where patients and their families find information difficult to access and treatment outcomes are known to be less effective.
InsideRadiology has a robust process to ensure accuracy and readability for consumers and health professionals. The InsideRadiology Secretariat tracks new items and items being reviewed and updated. Radiologists write the items in collaboration with members of the editorial team comprising a sub-editor, clinical adviser, general practitioner and consumer.
Yes, a radiologist often has limited direct contact with patients but as radiology tests, procedures and treatments becomes more sophisticated and specialised, this is changing. Information about radiology tests and procedures is a vital part of a patient journey and has a direct impact on a patient’s ability to access trusted information and reduce anxiety.
InsideRadiology can only remain at the forefront of the knowledge revolution if College Fellows are willing to support it by writing new content and reviewing existing content to ensure the website
is comprehensive and up-to-date. If there are barriers to this, please let the InsideRadiology team know how the process could be adapted to suit you.
A recent comment left on the website says it all:
Just a quick note from a reasonably informed, but not medically trained, patient to congratulate you on your excellent informative website. I just chanced on it while looking for a reputable source to explain what the acronym 'CTCA' stood for.
I found your site easy & quick to use, as it is reasonably well structured and gets straight to the point without users having to wade through unnecessary graphics. In particular, I found the content really informative; uses intelligent but plain English language (without appalling modern management speak); and being the site of a peak organisation, it is blessedly absent from the self-promotion/advertising that seems inevitable on the sites of providers who are competing with each other.
Please convey my congratulations and thanks to all responsible and also to the RANZCR for your contribution to quality science communication. I will certainly recommend your site to friends who are having different types of scans.
Name given
Ann Revell Consumer Advisor and Consumer Editor to InsideRadiology
InsideRadiology is an Australasian resource on clinical radiology tests, procedures, and interventions, providing up-to-date information to health consumers and health professionals and improving doctor-patient communication. www.insideradiology.com.au

Volume 18 No 1 | December 2021 31
Advocacy
“While I was able to navigate the information maze on my journey there were gaps, and it was clear to me a lot of people would have difficulty finding the right information at the right time. Knowledge helped me get through the various tests and procedures, take an active part in managing treatment side effects and inspiring me to have a positive attitude. It gave me some control at a time when I felt like I was on a fast-moving conveyor belt. ”
That’s a Wrap RANZCR 2021 Virtual ASM
More than two years in planning the RANZCR 71st Annual Scientific Meeting originally scheduled for October 2020, was successfully pivoted and delivered as a virtual experience from 16–19 September 2021. With the postponement of the 2020 ASM in Melbourne due to COVID-19, there was hope and optimism that Melbourne could pull off a great event in September 2021, with the local organising committee working tirelessly to showcase their city and introduce new program features.
The outbreaks in June and July 2021 across the east coast of Australia had all stakeholders closely monitoring the situation and playing out various scenarios. However, in early August the uncertainty of borders and venue restrictions led the College and stakeholders to acknowledge that we needed to move to a completely virtual experience, ensuring the safety of our participants as our number one priority. COVID-19 did bring new opportunities for the ASM program, with more than 40 internationals experts in clinical radiology and radiation oncology sharing their knowledge and insights in their various specialty areas. While the networking opportunities were missed, the organising committee delivered one of the largest programs seen in recent years at the ASM, and more than 1000 unique pairs of eyeballs viewing the program content over the three-and-ahalf-day program.
Acknowledgement must be given to College members who assisted in reviewing of the abstracts both in 2020 and 2021 for inclusion in the program, as well as the many others that participated as invited speakers and session chairs. Our trainees shone in the program in the strongly contested Varian Prize for Radiation Oncology and the Clinical Radiology Branch of Origin Prize. The commitment of our trainee representatives on the local organising committee that delivered a standout
Trainee Day program with hints and tips that will assist trainees moving forward as they prepare for their examinations was also notable.
The College has received strong feedback and suggestions to further enhance our ASM in the future and we thank our participants for their valuable feedback. We had many positive comments on the program through our survey including standout presentations on Clinical Radiology AI from Dr George Shih, USA, the Mock MDM on Breast Cases chaired by Dr Jill Evans, Thoracic Imaging also received extremely positive feedback with committee representative A/Prof Sam Ellis coordinating a strong
Dr Stephanie de Boer. Special interest group sessions delivered by APROSIG and FROLIC received strong interest and buy-in from the radiation oncology cohort.
All program content is available to registered delegates until January 2022 to access as part of your registration fee. Profound congratulations to Prof Meng Law, Chair Clinical Radiology and Prof Farshad Foroudi, Chair Radiation Oncology for delivering an outstanding 2021 ASM program. Your commitment and dedication over two and half years, a year more than originally planned ensured the success of our first ever
Education 32 Inside News
ELYSIUM: DIAGNOSTICS AND THERAPEUTICS (NOW AND THE FUTURE) WITH AI Official Presenting Partner of RANZCR2021
The College would like to acknowledge the contributions made by the Organising Committee over 2020 and 2021 to deliver the Virtual Annual Scientific Meeting (RANZCR2021 ASM), along with the reviewers over the two-year period of submitted abstracts


Your time, dedication and expertise are greatly appreciated
Clinical Radiology
Prof Meng Law Clinical Radiology Convenor
Dr Paul Beech Clinical Radiology Social Committee
Dr Shalini Bigwood Clinical Radiology Social Committee
A/Prof Warren Clements Clinical Radiology Representative, IR
Dr Andrew Dixon Clinical Radiology Representative, Education
A/Prof Sam Ellis Clinical Radiology Representative, Body
A/Prof Gerard Goh Clinical Radiology Representative, IR
Dr George Harisis Trainee program
Dr Alex Jarema Trainee program
Dr Anthony Kam Clinical Radiology Representative, Neuro
Dr Phil Lew Clinical Radiology Representative, Cardiac
Dr Matt Lukies Trainee program
Dr Daniel Macmanus Clinical Radiology, Trainee Representative 2021
Dr Paul Marovic Clinical Radiology Social Committee
Dr Ben McDonald Clincial Radiology Representative, MSK
Dr Maddy Scicchitano Trainee program,
Dr Jarrel Seah Trainee program and AI
Dr Miranda Siemienowicz Clinical Radiology Representative, Body
Dr Anoushka Rajaratnam Clinical Radiology Representative, Body/Mammography
A/Prof Dinesh Varma Clinical Radiology Representative, Emergency/Trauma
Radiation Oncology
Professor Farshad Foroudi Radiation Oncology Convenor
Associate Professor Michael Chao Radiation Oncology Representative
Associate Professor Hany Elsaleh Radiation Oncology Representative
Professor Gerry Hanna Radiation Oncology Representative
Dr Carminia Lapuz Radiation Oncology Social Committee
Dr Lachlan McDowell Radiation Oncology Social Committee
Dr Wee Long Ong Radiation Oncology Trainee Representative 2020
Dr Nikki Plumridge Radiation Oncology Social Committee
Dr Cristian Udovicich Radiation Oncology Trainee Representative 2021
RANZCR 2021 ASM Reviewers
Clinical Radiology
Dr Brendan Adler
Dr Aadil Ahmed
Dr Aparna Baruah
A/Prof Colleen Bergin
Dr Lynne Brothers
Dr Fraser Brown
Dr William Bugg
Dr Timothy Cain
A/Prof Joga Chaganti
Dr Michael Chan
Dr Virgil Chan
A/Prof Ronil Chandra
Dr Murthy Chennapragada
Dr Warren Clements
Dr Gregory Compton
Dr Elizabeth Dillon
Dr James Drummond
Dr Greg Filewood
Dr Gregory Fitt
A/Prof Gerard Goh
A/Prof Mary-louise Greer
Dr Deepika Gunawardena
A/Prof Craig Hacking
Dr Anthony Kam
Dr Colette Kennedy
Dr Gabes Lau
Prof Meng Law
Dr Glen Lo
Dr Charles Lott
Dr Tracey Muir
Dr Dee Nandurkar
Dr Nick Pang
Dr Frank Parrish
Dr Kumar Ramavathu
A/Prof Lloyd Ridley
Dr Bann Saffar
Dr Mahomed Seedat
Dr Rupinder Sekhon
Dr Teck Siew
Dr Lisa Sorger
Dr Stephanie Tan
Dr Mark Teh
Dr Roy Thomas
Dr Bei-Tyan Toh
Dr John Troupis
Dr Ross Vander Wal
A/Prof Dinesh Varma
Dr Yuranga Weerakkody
Dr Chris Welman
Dr Merle Wigeson
A/Prof Liz Wylie
Dr Natalie Yang
Dr Jiajia Zhang
Radiation Oncology
A/Prof Verity Ahern
Prof David Ball
Dr Guy Bryant
Prof Geoff Delaney
Dr Hany Elsaleh
Prof Farshad Foroudi
Dr Suki Gill
A/Prof N Kumar Gogna
Dr Brigid Hickey
Dr Benjamin Hindson
Prof Angela Hong
A/Prof Michael Jackson
Dr Melanie Jackson
Dr Melissa James
Prof Michael Macmanus
Dr Roya Merie
Dr Wee Loon Ong
A/Prof Sasha Senthi
Dr Lisa Sullivan
Dr Neetu Tejani
Prof Michael Veness
Raising Our Gaze Countering Uncertainty with Awe
I earned my doctorate in Human Development and Education from HGSE, where my dissertation research focused on the emotion of awe and its role in scientific learning and discovery. More broadly, I tend to conduct research that focuses on the relationship between learners and the social and emotional contexts in which their learning takes place.
Why is awe important?
Evidence suggests that there are many benefits to experiencing awe, including stimulating our curiosity and motivating us to act in ways that support the wellbeing of the collective. And though it's still speculative, some early research indicates that awe may even have a positive impact on our immune systems.
As humans, we do not like uncertainty. It is hard for our brains to deal with, and can make stressful situations even harder by causing anxietyi. This, in turn, narrows our ‘window of tolerance’ii and can make it more difficult to deal with everyday stressors and major events. We are nearly two years into the pandemic and we are still not certain what our new normal looks like—when we think we might have reached that point, something changes which throws us back into those feelings of uncertainty. In many ways this has not only narrowed our windows of tolerance but our worlds too. From hard lockdowns with limited reasons to leave the house to not being able to travel to see loved ones, the pandemic has made the circles in which we move smaller.
A growing body of research suggests that one way to mitigate the impacts of uncertainty and the anxiety it produces is to look beyond our immediate environment and focus on the things that bring us wonder and aweiii. While
this body of research is relatively new, it has shown that getting outside and looking up from our devices and out into the natural world can result in less distress.iv
As we continue to discover what our new normal will be, the end of the year is a good time to recognise how awe and wonder can help us not only navigate through continuing uncertainty but also improve our experience of work and research. To this end, I interviewed Dr Megan Cuzzolino at the Harvard Graduate School of Education (HGSE) about her research on awev
Could you tell me a little bit about yourself and your work?
I am the Senior Project Manager for the Next Level Lab, a research group at the HGSE that draws on research from the learning sciences and innovative instructional design to address emerging and urgent issues in K-12 education and workforce development.
What role does awe play in our lives?
Awe falls into a category of emotions called the ‘epistemic emotions’. These are the ‘finding out’ emotions like curiosity, surprise, and wonder that make us aware of gaps in our understanding and motivate us to learn more. Researchers also classify awe as a ‘collective emotion’, because it draws our attention to our role within phenomena, systems, or communities that are larger than ourselves.
Are there benefits to taking time to notice moments that inspire awe?
Many of my study participants remarked that the interview process itself heightened their awareness of the impact that awe has had on their personal and professional lives. In the moment, I think that taking time to notice awe-inspiring events can be a nice chance to pause, take a deep

Feature 34 Inside News
breath, and gain some perspective. More long-term, a regular reflection practice that involves documenting moments of awe and considering their impact can help translate those feelings into action. For instance, you might ask yourself, "How did that experience make me think about myself and my relationship to something larger?"
What does your research tell us about awe in science?
I don't think we talk enough about the human side of science, how much emotions play a role in the research process, and how challenging and isolating the work can be. The interview quote that sticks with me more than any other is, "There's so much drudgery, that if you don't hang on to those moments [of awe], I don't know what else you hang on to."
Unfortunately, institutional pressures to publish, get funding, and so on don't always support the kind of work that can lead to awe or allow researchers the time and space to reflect on their awe experiences. I also think there are concerns that expressing emotions can be seen as overly vulnerable or even ‘unscientific’.
I'd love to see institutional norms shift such that we all feel more comfortable acknowledging that scientific research is conducted by real people who have real emotional reactions to their work.
How can awe improve our research or work?
In my research on the awe experiences of professional scientists, I found that feelings of awe were often elicited by moments of discovery—that experience of unlocking some new secret of the universe, no matter how small or insignificant the finding might seem. Critically, participants told me that this feeling of awe served as a powerful antidote to the daily grind of research work. Scientists were willing to persist through long hours, low pay, and failure after failure in part because of the promise, or hope, that they would eventually achieve their next aweinspiring ‘a-ha moment’.
What surprises you or your research subjects the most about awe?
In addition to the awe that came from individual moments of discovery, participants in my research identified a sense of awe that came from perceiving themselves as members of the larger scientific community.
Personally, as someone who has spent years involved in research on outer space and politics, awe has played in important role in my ability to stay excited about the work and its importance. Policy can sometimes seem far removed from the application of it, but moments like seeing the first picture of Pluto’s heart from New Horizonsvi or the way the sound of a rocket launch physically washes over you as you watch a spacecraft human hands made leave Earth forevervii stay with you and allow you to see the bigger picture of your work. Clinicians in both our professions have faced unprecedented times over the pandemic and, like other members of the healthcare workforce, are facing many personal and professional challenges. However, taking time to recognise the moments in our work or our research that produce wonder and awe may help us persist and deal with the challenges of living in uncertain times.
Dr Kat Robison
References
I. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective | Nature Reviews Neuroscience, https://www.nature.com/articles/ nrn3524
II. GoodTherapy | Window of Tolerance, https://www.goodtherapy.org/blog/psychpedia/window-of-tolerance
III. Eight Reasons Why Awe Makes Your Life Better (berkeley.edu) https://greatergood.berkeley.edu/article/item/eight_reasons_why_awe_makes_your_life_better

IV. Big smile, small self: Awe walks promote prosocial positive emotions in older adults. - PsycNET (apa.org) https://psycnet.apa.org/record/2020-69974-001?doi=1
V. “The Awe is In the Process”: The nature and impact of professional scientists' experiences of awe - Cuzzolino - 2021 - Science Education - Wiley Online Library https:// onlinelibrary.wiley.com/doi/epdf/10.1002/sce.21625
VI. pluto-planet-heart-color-image.png (1042×1042) (nasa.gov) https://mars.nasa.gov/imgs/2015/07/pluto-planet-heart-color-image.png
VII. #207: Rocket Lovesong “We stood, heads raised to... | Consider This Thought (tumblr.com) https://considerthisthought.tumblr.com/post/81535729303/207-rocketlovesong-we-stood-heads-raised-to
Feature Volume 18 No 1 | December 2021 35
Abstract Submissions Open 17 Jan 2022

Abstract Submissions Close 8 Apr 2022










Registrations Open 11 Apr 2022
PRESENTING PARTNER
36 Inside News NEW ZEALAND ASM AUGUST 5-7 2022 QUEENSTOWN MILLENNIUM HOTEL www.ranzcr2022.co.nz Revive. Reflect. Reimagine.
RANZCR2022.com
Nick Rains, Bethany Wines, Barossa
Sebastian Aviles-Cardenas, SAHMRI, Adelaide
Ivyanna Roselyn, Rundle Mall, Adelaide
A Thank You to Colleagues
All good things must come to an end, and sadly my role as Dean of the Faculty of Clinical Radiology comes to end on 31 December 2021. I have served in this role for the past three years and consider myself very fortunate and privileged to have held this esteemed position in our College. It was a dream run, but not without major challenges, far more than I had anticipated when I signed up. 2018 was really a good year. COVID hit our shores in March 2019, and everything changed. No one in their worst nightmare would have imagined the 21st century world would come to a grinding halt!
I call it a dream run, because I had enormous support from my fellow Councillors on whom I could always rely to work hard with multiple meetings, especially during the past two years when state borders were closed. I could not have asked for more. This was ably and admirably supported by FCR staff, especially Melissa Doyle, Executive Officer, FCR, to whom I am indebted. Melissa worked tirelessly keeping business on track during difficult times. I would also like to acknowledge Kirsten Fitzpatrick. She is an excellent Senior Project Officer. Kirsten’s ability to take Council minutes is unparalleled.
At FCR we have a team of highly dedicated office bearers, namely A/ Prof Dinesh Varma (Chief of Professional Practice), Dr Meredith Thomas (Chief Censor), incoming Chief Censor Dr Barry Soans, and A/Prof Mike Bynevelt (Chief Accreditation Officer). These talented people made my job easy. I

The End of One Era, the Beginning of Another A Message from the Dean
am also grateful to our President Dr Lance Lawler as he was always available for advice and would make things look simple and easy to conquer when I called him to discuss difficult issues. My predecessor Professor John Slavotinek was always there for me, eager to help with wise consul when I needed it most.
Our Senior Management Team are very capable, highly committed individuals who have worked long hours each day and many times on weekends to make things happen. All our College staff working from home with no holiday escapes and with no work-home boundaries have had a tough two years, but they have done an excellent job under extremely difficult, unpredictable circumstances. The work they do is not visible to members and mostly goes unacknowledged.
Without the support of all these hardworking people and our Chairs of the committees and volunteer members of various committees, my journey as Dean of the Faculty would have been quite different. I am very grateful for all their support and look forward to working with them in my role as President next year.
I feel very privileged and humbled to have been elected to the role of President from 2022 and am cognisant of both the honour and the responsibility of leading our great College. To fill the very big shoes of our President Dr Lance Lawler is not an easy task. Next year my focus will naturally change to the strategic direction of the organisation for both clinical radiology and radiation oncology. I move on
confident of the immense skill and ability of the Councillors around the Faculty of Clinical Radiology table.
A/Prof Gerard Goh has been elected to the role of Dean and I am confident that Gerard will ably lead FCR Council to continue with the great work and ensure that clinical radiology continues to be at the forefront of patient care.
With the old cliché about how quickly time flies in mind, reflecting on the past three years, I am still astonished by all that has been achieved in what seems like the blink of an eye. There are many achievements, but I would like to highlight some of the standouts.
• Our Ethical Principles for Artificial Intelligence in Medicine and Standards of Practice for AI have been very received by the wider medical community and are leading the way to establish appropriate frameworks to ensure that these technologies are incorporated into clinical practice safely and in the best interests of patients.
• After almost 20 years of freeze on indexation, we have seen the staged re-introduction of indexation to almost all of the clinical radiology items listed in Medicare.
Clinical Radiology Volume 18 No 1 | December 2021 37
Clin A/Prof Sanjay Jeganathan
continued over...
Following College advocacy and the hard work of members several new items have been listed on the Medicare Benefits Schedule including: Obstetric MRI, Liver MRI, Breast MRI, Prostate MRI and Digital Breast Tomosynthesis to name a few. This offers our patients much greater access to the vital services we provide.
There has been a significant expansion of the number of MRI licenses—this advocacy work is continuing with our policy of full deregulation of the licensing system. Our work and positive attitude with the Government has positioned us as a trusted stakeholder which allows our voice to be heard whenever an issue related to clinical radiology is debated.
• The College has made a major contribution to the New Zealand Health and Disability Review. This review will reshape how health care is delivered to New Zealand patients. We continue to advocate to ensure our key recommendation around investing in capacity building, particularly around workforce and technology are realised.
• A few years ago, we established an Interventional Radiology Committee (IRC) to support members who are practising in this increasingly subspecialised area. The hard work of the IRC has reached an exciting milestone with the recent announcement that the College will propose formal recognition of Interventional Radiology (IR) and Interventional Neuroradiology (INR) specialties. with the Medical Board of Australia and the Medical Council of New Zealand.
• Our response to the COVID-19 pandemic ensured that members were provided with advice to navigate the impacts of the pandemic on our practice and training. Training was able to continue and exams were successfully completed allowing our trainees to progress their careers and be welcomed into the clinical radiology workforce.
• Our Training and Assessment Reform has been a monumental endeavour and is a credit to all involved. Next year will see the implementation of the enhanced training program ensuring that our training program remains world class into the future.
• The College has been at the forefront of advising governments on the appropriate use of imaging for lung dust disease with the emergence of the silicosis and re-emergence of coal workers’ pneumoconiosis impacting so many Australian. This has resulted in enhanced standards and a recognition of the role of clinical radiology in detecting these serious diseases.
• The technological advance of mechanical thrombectomy is a game changer for stroke patients. We have developed the Framework for the Recognition of Training in Percutaneous Stroke Intervention to establish standards for the delivery of this life saving treatment balancing high-quality training and access for patients.
I wish I could continue sharing the many achievements with you but there is just not enough room on the page. I would however, like to take this opportunity to extend my thanks and appreciation to each person who has served on FCR Council over the past three years. Beyond FCR Council, there are many members who make a very valuable contribution by serving on committees and joining the many activities right across the spectrum of College initiatives. I would like to thank each one of you for the very significant time and effort you so generously give—it is only through members volunteering that the College can operate effectively and achieve so much.
Clinical Radiology 38 Inside News
“I wish I could continue sharing the many achievements with you but there is just not enough room on the page. I would however, like to take this opportunity to extend my thanks and appreciation to each person who has served on FCR Council over the past three years. Beyond FCR Council, there are many members who make a very valuable contribution by serving on committees and joining the many activities right across the spectrum of College initiatives. I would like to thank each one of you for the very significant time and effort you so generously give—it is only through members volunteering that the College can operate effectively and achieve so much. ”
Write First Time
Minimising text errors in reports
glitches or complete nonsense phrases that are obviously wrong to the reader. More serious issues may arise when words are omitted (particularly the word ‘no’), added or replaced resulting in a missense error—a plausible word or phrase with a different meaning from what was intended.
How we report also affects the risk of these types of errors. Historically, all reports were dictated by radiologists, typed by another staff member, then reviewed by the radiologist before release. Experienced transcriptionists frequently queried incorrect or unclear phrases. The main drawbacks of this system were longer report turnaround times and higher costs.
may not detect missense errors) and software that transfers image data such as measurements directly into the report, but this is not yet widely available. Report audit and feedback may also be beneficial.
Report bloopers like these can be quite entertaining—unless you are the patient, clinician or radiologist involved. Radiology communication errors occur after we have already examined the images carefully and interpreted findings correctly. They can lead to adverse outcomes for the patient and medicolegal strife for the radiologist, especially when reports are delayed or misdirected.
Textual mistakes like the cases above are usually less significant, but confusion about the meaning of the report can also derail timely treatment or subject patients to unnecessary procedures, including additional imaging. Resolving these issues generates extra work for radiologists, technologists and the department or practice as a whole. Reputations can be damaged, particularly with greater patient access to records and the rise of social media.
Studies find textual errors, variously defined, in anything from 5 to 60 per cent of reports, with an average of 1.6 to 1.7 errors per report. Most of these (around 80 per cent) do not cause major problems—they are typos, grammatical
Voice recognition (VR) systems started to come into everyday practice in the early 2000s. Studies showed that while spelling mistakes and typos decreased, rates of certain errors, particularly soundalike word replacements like ‘brain’ for ‘drain’ and other missense errors, increased by factors of two or more; there has possibly been some improvement since then as the technology has matured.
When physicians type notes themselves, there may be even more mistakes. Many of these, however, are obvious typos. More recently, there has been a move toward templated or structured reporting, with largely or completely prepopulated text fields. Errors unique to template use include the inadvertent retention of prepopulated text or fields that contradict case-specific information entered by the radiologist.
Research evidence is still sparse, but suggests some improvement in error rate with template use, particularly in the frequency of missense errors. Some other interventions have been explored to reduce textual errors, including spelling and grammar checkers (which
Regardless of the report creation method—voice recognition, selftyping or templated, radiologists are now largely their own transcriptionists and editors, without the valuable proofreading step that expert typists once provided. Advice from the British Medical Journal in 2005 seems rather quaint now: ‘Good dictating skills are largely good manners. Stay polite and don't forget to say thank you from time to time’. In 2021, expressing thanks may not help radiologists improve reports as much as it once did, but we still have a number of other ways to reduce textual errors:
• Dictate and edit reports in a quiet space with minimal interruptions whenever possible; enunciate clearly.
• Use VR hardware and software with high-quality noise-cancelling technology.
• Take the time to train the VR software—and yourself. Most software defaults to American English spelling and pronunciation but this can be changed with training.
• Take the time to retrain words the VR software has trouble recognising.
• Train phrases rather than individual words: ‘No tumour’ rather than ‘no’ and ‘tumour’ separately.
• Use the auto-correct function (if available) for words that sound particularly similar when spoken quickly such as calcification and cavitation.
Clinical Radiology Volume 18 No 1 | December 2021 39
‘A brain was inserted into the abscess’
‘The left right finger’
‘Cyst measuring 17m’
‘Fatty change in the lover’
continued over...
‘High-grade tear of the musculotendinous junction of the kidney’
• Some software can be programmed to automatically generate predefined phrases when a keyword is dictated, for example, ‘PIRADS 2’ will appear as ‘PI-RADS 2 (clinically significant tumour is unlikely to be present)’.
• Plan your report outline, even when you are not using a template.
• Use wording that avoids ambiguity and problem areas for omissions, additions and replacement. Pertinent negatives are important in many clinical and imaging scenarios but findings can often be described positively: ‘normal diameter’ instead of ‘not dilated’.
• Consider using templates where available, but take care to select appropriately for the context, and to delete or edit any prepopulated
sections that conflict with your findings and interpretation elsewhere in the report.
• Monitor your own reports to identify recurring problem words or phrases and consider alternatives.
• Proofreading is crucial—try not to skim read. Research shows that errors are reduced when there is a delay between text creation and editing/ review so the reader comes back to the text with fresh eyes. This is unfortunately not always practical, but may be particularly important for complex reports.
• Just as when you review images, pay attention to ‘check areas’ in the report text—laterality, measurements, units, negatives and wording highlighted by your past experience.
• A practice-wide report audit may be a worthwhile quality improvement project.

Structured Report Writing Group
Dr Felicity Pool | Chair
Dr Chian Chang
Dr Miranda Siemienowicz
Clinical Radiology 40 Inside News
Greater
Now Open * Past performance is not an indicator of future performance. Consider the PDS and TMD on our website and your situation before making decisions, because we haven’t. UniSuper Limited ABN 54 006 027 121 ATF UniSuper ABN 91 385 943 850.
our low fees and proven long-term investment performance*
to everyone. Join now and look forward to greater super.
331 685 unisuper.com.au/open
Super
After more than 40 years shaping greater futures for Australia’s brightest minds,
are now open
1800
Training Program 2022
I’m very excited that our years of work on the Training and Assessment Reforms are finally culminating in Training Program (TP) 2022, implemented from February next year. The name reflects that there will be continual evaluation and refinement of the program with anticipated annual updates.
Radiology practice is continually evolving, as are educational theories and practices, and we need to remain contemporary in our approach to the delivery of training. This will allow expansion of training in areas of practice such as advanced imaging techniques and artificial intelligence, as well as ensuring that our training meets the needs of the profession and the referrers and consumers we serve.
Training Program 2022 assessments
I have previously spoken about changes to work-based assessments and examinations. We are now very close to implementation, and it is pleasing that so many Directors of Training and Clinical Supervisors have attended or viewed the Training and Assessment Reform webinars, particularly those discussing the use of the new Kaizen e-Portfolio system. Kaizen will be used, not only to monitor trainee progression and host trainee workbased assessments, but also to host and manage CPD for Fellows, so it is important that all Fellows are upskilled in its use.
The Vital Link Between Robust Training and Maintaining Radiology Standards

Chief Censor in Clinical Radiology
Programmatic assessment of trainees relies on low stakes work-based assessments, with multiple assessments, by multiple assessors, across multiple learning experiences, and all Clinical Supervisors in training departments will need to be familiar with the system. The e-Portfolio will be easily accessible on mobile devices for both trainees and clinical supervisor assessors.
Programmatic assessment also facilitates increased feedback to trainees, both in the workplace, and also at higher stakes examinations. In recent years we have improved examination feedback to candidates, and this will be further expanded and streamlined as part of TP 2022.
I would refer to the excellent article on meaningful feedback in medical education on page 20 by Dr Jacob Pearce, who is a Senior Research Fellow at the Australian Council for Educational Research. Many of you would be familiar with Jacob due to his ongoing work with the examination team to improve our examination processes.
COVID-19 challenges
I’m not sure that any of us anticipated the long term and ongoing repercussions of COVID-19 when the impacts were first felt in March last year. Among so many health, societal and economic impacts, the impact on the delivery of education, at all levels, has been profound. As a provider of specialty medical education we have navigated this to the best of our ability, as we are acutely aware of the need to
ensure progression through training, both to ensure maintenance of an adequate medical workforce, and to ensure continual recruitment into our training program.
My enormous gratitude goes to the College staff, particularly the examination team. With the exception of Series 1 last year, we have been able to run all of our examinations, but this has required nimbleness: continual innovation, lateral and forward thinking, open mindedness and an ability to swerve and pivot. Unpredictable and unanticipated jurisdictional conditions have meant that no exam sitting has been the same—we have had to continually change and evolve.
As I write this, the team are making final preparations for the Part 2 Viva examinations. In addition to addressing COVID challenges, we also have an obligation to address AMC training conditions and recommendations, and we are therefore running the Vivas online, with standardised digital cases. The associated challenges are significant but I am reassured that the team has the skills to negotiate challenges as they arise. We are also incorporating changes to the examinations in association with TP 2022, with Part 1 examination format changing in 2022, and Part 2 in 2023.
Thanks to the many Fellows who have volunteered for our new Examination Review Panels, particularly the new OSCER Panel who have put in many hours of work submitting and reviewing cases for the upcoming digital Viva.
Clinical Radiology Volume 18 No 1 | December 2021 41
continued over...
Dr Meredith Thomas
Specialty Training Unit and Workforce Unit
All aspects of training have traditionally been overseen by the Specialty Training Unit (STU), however the workload of STU has significantly increased in recent years, particularly in relation to ensuring AMC compliance and the Training and Assessment Reforms, all compounded by the challenges of COVID-19. A new Workforce Unit has been created, with responsibilities including Accreditation, the management of International Medical Graduates, and Specialist Training Program (STP) funding.
I welcome Brendan Grabau who has been appointed as head of the new unit, recognising his wealth of experience across various medical specialty colleges, including RANZCR.
Faculty
The governance processes of the College are very robust. While the Clinical Radiology Education and Training Committee oversees all training activities and multiple training committees (including review panels and working groups), CRETC is itself overseen by Clinical Radiology Faculty Council.

I have had the privilege of sitting on Faculty Council for many years, initially as an elected representative, and more recently by virtue of my role as Chief Censor. I would argue that the most important roles of Faculty are to ensure our training program remains robust, and to ensure that radiology standards are maintained. The two are, of course, intrinsically linked. While
Faculty Councillors are our elected representatives, I am sure that they would join me in recognising the commitment and enormous volume of work done by so many volunteer Fellows on the committees they oversee, and acknowledging the particular skills and expertise these Fellows provide.
My thanks again to all College staff, some of whom I have worked with for many years. Their commitment, and the commitment of the Fellows I have worked with, has made my long College journey a tremendous one.
Dr Meredith Thomas Chief Censor in Radiology 2019 - 2020
42 Inside News Clinical Radiology
Welcome to the world of comprehensive AI for CXR Annalise CXR, a second pair of eyes for radiologists, detecting 124 findings. By clinicians, for clinicians. Demo now available at www.annalise.ai Only available for purchase by healthcare institutions. Always read and follow instructions for use. Annalise CXR is entered in the ARTG. No: 343577. 7 John Doe 73Y, M DOB Chest X-ray DATE OF EXAM 1 image Focal airspace opacity Multifocal airspace opacity Simple effusion Diffuse upper airspace opacity Segmental collapse Patient rotation Diaphragmatic elevation 6 PRIORITY 1 TECHNICAL Annalise ABSENT PRESENT
The end of 2021 marks the end of the first three-year term of the Professional Practice Committee (PPC). The PPC was established by the Faculty of Clinical Radiology in late 2018 to provide guidance and oversight for the development, implementation and review of post-fellowship learning. As we head toward the end of another year, the PPC has continued to progress a number of key College priorities.
Changes to the RANZCR CPD Program commencing 2022
A reminder to members that the College CPD program is transitioning in 2022 to align to the changes announced by the Medical Board of Australia (MBA) and Medical Council of New Zealand (MCNZ). Full compliance to these regulatory changes is required by medical colleges from 2023 onwards. To assist members with this process, 2022 will be a transition year, with some changes being introduced from 2022, these changes include:
• CPD will be operate on an annual cycle (by calendar year)
• 50 hours required each year
• Completion of a Professional Development Plan will be required annually
• Structured Annual Conversation activity will be required annually (New Zealand members only).
As a result of program changes, the College has updated CPD resources that support members. I am pleased to announce the new 2022 Clinical Radiology CPD Handbook was recently approved by the Faculty of Clinical
Looking Forward to 2022
Chief of Professional Practice
Radiology Council. The 2022 handbook contains all the information you need to know about the changes to the CPD program, the new CPD e-Portfolio system and how to record your CPD activities. You can view and download a copy of the new CPD Handbook from the College website.
To complement the changes to the CPD program commencing in January 2022, the College is also rolling out a new CPD e-Portfolio. The new CPD e-Portfolio is mobile friendly and has a dashboard layout, allowing members to view their CPD progress and access all functions from the dashboard page. More in-depth information about the e-Portfolio and its functions for both the College training and CPD programs can be found in the article on page 19.
2019−2021 Triennium—are you compliant?
A reminder to members to ensure you have recorded your CPD activities for the 2019−2021 triennium. Please note, we are encouraging members to complete this as soon as possible due to the commencement of the new CPD program requirements and use of the new online portal from January 2022. The 2019−2021 triennium CPD compliance audit will commence in early 2022.
To be compliant for the triennium, you need to have recorded 125 points, with a minimum of 30 points in the 2019 calendar year only, this is due to the reduced point requirements due to the COVID-19 exemptions. For further information about the current CPD requirements please see the 2019-2021 CPD Handbook for Clinical Radiology.
If you have any questions regarding your CPD or the new program requirements, please contact the College at cpd@ ranzcr.edu.au
RANZCR Position Statement on Post Mortem Imaging – now open for member consultation
Post-mortem imaging is a niche area of radiology which is growing in significance. The Post Mortem Imaging Working Group have been working on a position statement detailing the ‘The role and value of radiologists in post mortem imaging’. This position statement is now open for member consultation and is accessible via the College website. I extend my thanks to the members of the Post Mortem Imaging Working Group for producing this document.
In closing, I would like to wish everyone a very, safe and happy holiday season and extend my best wishes for the New Year and thank members for their support in 2021. I look forward to bringing you further updates on the work of the PPC as we move into 2022.
Yours sincerely,
Dinesh
Associate Professor Dinesh Varma

Chief of Professional Practice
Faculty of Clinical Radiology
Useful links
2022 Clinical Radiology
CPD Handbook
https://www.ranzcr.com/college/ document-library/2022-ranzcrclinical-radiology-cpd-handbook
2019-2021 Clinical Radiology
CPD Handbook
www.ranzcr.com/college/documentlibrary/clinical-radiology-cpdhandbook-2019-2021
RANZCR Position Statement on Post Mortem Imaging
www.ranzcr.com/college/documentlibrary/2021-ranzcr-post-mortemimaging-position-statement-formember-consultation
Clinical Radiology Volume 18 No 1 | December 2021 43
A/Prof Dinesh Varma
The Clinical Radiology Training Program is Changing Along with the Examinations
In preparation for the launch of the training program in February 2022, there have been changes to the style and delivery of examinations. From 2023, there will also be changes to the timeline for sitting.

What are the changes to examinations?
The Part 1 Examinations have been reviewed and new Phase 1 Anatomy and Applied Imaging Technology (AIT) Examinations will commence from Series 1 in March 2022, aligned with Phase 1 of the 2022 Training Program.
For Part 2 Examinations there have been changes to the eligibility requirements for the Viva/OSCER examinations in that candidates must pass the written components before presenting for the Vivas/OSCERs. The Part 2 Examinations will continue in 2022 with the reviewed Phase 2 Examination commencing from Series 2 in 2023.
What are the timetable changes?
A new examination timetable plan developed, considering a trainee's introduction to training, examination components and the examination operational administrative requirements such as application, marking, results and so on.
Why the changes?
Feedback received from the training program stakeholder consultation indicated that there were a number of areas to improve examinations process, specifically:
• allow trainees to sit the written examinations and OSCERs in the same sitting or within reasonable timeframes (if they had met the written examination requirements)
• consider the impact to departments with having Part 1 and Part 2 candidates away on study leave at the same time
• delay the Part 1 Examination schedule at the beginning of Phase 1 training to allow trainees to settle into training departments.
Clinical Radiology 44 Inside News
Where to go for more information? Useful links Clinical Radiology Trainees’ Exams Page www.ranzcr.com/trainees/clinicalradiology/exams Contact CRtraining@ranzcr.edu.au
Sitting 1 Sitting 2 Phase 1 Examinations Applications Open/Close January / February July / August Examinations Held April October Release of Results End June End November Phase 2 Written Examinations Applications Open/Close October / November (the year prior) April / May Examinations Held February July Release of Results April September Phase 2 OSCER Examinations Applications Open/Close (intention to sit) February / March July / August Examinations Held Early June Early November Release of Results Late June Late November
Timetable
New
to be implemented from 2023
Clinical Radiology Trainee Matters
good work the committee has done in the trainee realm over this period:
• Auditing the after-hours workload of trainees across Australia and New Zealand including non-reporting tasks (discussions with clinicians, real-time reviewing of studies, etc.)
• Road-testing and providing feedback on the new curriculum, exam format and software
• Advising CRETC on ‘non-medical expert’ topics for the new centralised teaching series
• Advocating to change policy to allow trainees to sit exams while on parental leave (hopefully this will be ratified by the release of this update)
• Organising and running the Trainee Day at the RANZCR ASM
Hello everyone,
What a crazy year it’s been! At the time of writing this, most lockdowns are starting to ease and there seems to be a light at the end of the tunnel. Give yourselves a HUGE pat on the back for making it through another tough year and I hope the holiday season brings some rest and relaxation.
As this is the last CRTC update from me for the year (and maybe forever) I’d like to finish with a highlights reel of all the
• Providing input into the artificial intelligence modules for the new curriculum
• Successfully advocating for timing of the new Part 2 exam format so the Written exams and Vivas can be sat within the same exam series
• Liaising with the College/AMA regarding advocacy for the Westmead trainees affected by the deaccreditation
• Contributing to planning of the new trainee selection process
• And much more but you get the idea.
I’d like to thank Allister Howie (NSW), Amer Mitchelle (NSW), Dan MacManus (QLD), Danielle Coupland (SA), Joel Earley (WA), Laura Hill (NZ), and Tom Pearson (QLD) for their tireless work this past year. I couldn’t have dreamed of a better group of people to spend 2021 with and I hope you’re incredibly proud of all you’ve achieved for trainees across Australia and New Zealand. Hopefully one day we’ll all be able to meet in person.
I have a really good feeling about next year (touch wood) and I’m sure the next bunch of CRTC members will continue building on the great work done every year by the CRTC.
As always, if you have any questions, comments, or want to get involved please email clinicalradtc@gmail.com.
If you don’t hear from me next year, it’s because you’ve made a very sensible choice and voted me off the island. Goodbye and/or see you next year!
Dr Sarah Robertson Chair | Clinical Radiology Trainee Committee 2021 (CRTC)

RANZCR Workshops, Courses and Events 2022
Upcoming Events
The College’s events team are planning a busy annual calendar of events in 2022. To stay up-todate on all information for College events, visit the website and follow us on all our social media channels.
Useful links
RANZCR What’s On | Events www.ranzcr.com/whats-on/events
Useful Links
RANZCR Webcast Library www.webcast.ranzcr.com/Mediasite/Showcase
RANZCR WA Branch ASM
19–20 February 2022
Nedlands, Western Australia
ANZSNR ASM
10–13 March 2022
Sydney, New South Wales
TRoG - Radiation Oncology
Trainee SMART Workshop
14 March 2020, 8.30–5.00 pm
RACV Royal Pines Resort, Gold Coast Queensland
ARGANZ ASM
26–27 March 2022
Sydney, New South Wales
AMSIG ASM
14–15 May 2022
Melbourne, Victoria
RANZCR NZ ASM
5–7 August 2022
Queenstown, New Zealand
IRSA ASM
9–11 August 2022
Queenstown, New Zealand
RANZCR ASM
27–30 October 2022
Adelaide, South Australia
Clinical Radiology Volume 18 No 1 | December 2021 45
Dr Sarah Robertson
The Transformative Potential of the Interventional Radiology Specialties for RANZCR: the Importance of Recognising IR and INR as Clinical Specialties
Yesterday, at one of the hospitals where I work, a patient who was critically unstable had a life-saving procedure to stop major bleeding in their chest from a tiny artery just below their aorta.
At a hospital down the road, another patient who presented earlier that day suffering a stroke is now sitting up in bed conversing with her daughter.
In hospitals around the country, select groups of patients had their tumours cured without undergoing major surgery or unpleasant chemotherapy.
Similarly, women with symptomatic uterine fibroids, men suffering from prostate enlargement and elderly patients with debilitating vertebral fractures all had their problems successfully managed without the need for an operation.

These patients were all treated, not by surgeons or physicians, but by radiologists. The radiologists responsible were not sitting in dimlylit rooms reporting diagnostic scans, they were interventional radiologists and interventional neuroradiologists— clinical specialists who use imaging technology to deliver highly targeted treatments. While IRs and INRs are also specialist diagnostic radiologists, and many diagnostic radiologists expertly perform image-guided procedures, specialist qualified IRs and INRs possess technical capabilities and a clinical skillset additional to that of diagnostic radiology. Specialists in interventional radiology and interventional neuroradiology actively assess patients, evaluate potential treatment options, contribute to management decision, and perform image-guided procedures.
Like Artificial Intelligence, Digital Health and Tele-radiology, modern IR and INR practice presents many exciting opportunities for the College, with the potential to transform clinical radiology
and the role of the radiologist. The clinical utility and considerable value that IR and INR bring to patient care, hospitals and the broader healthcare system adds a whole new dimension to the evolving face of the radiology profession that should be celebrated. Supported by a growing evidence base, the capacity for minimally-invasive, image-guided procedures to save lives, cure disease or alleviate suffering better, faster and for less money than some other, traditional methods of treatment is only beginning to be realised by policy-makers and hospital administrators. In the era of Value-Based Healthcare, IR and INR are therefore well placed to capitalise on these strengths, presenting exciting opportunities for the College to embrace this expanding frontier, grow its brand and consolidate the importance and influence of clinical radiology within modern health care.
The College is well advanced with its planned application for formal specialty recognition of IR and INR by the Medical Board of Australia and the Medical Council of New Zealand, which will provide a tremendous boost for all of clinical radiology. This process has emphasised the need for dedicated governance structures and resources
within the College to support specialty training and practice in IR and INR, alongside existing procedural radiology. Far from dividing the profession, such a development will expand the foundations of the College and consolidate the important links between diagnostic and interventional radiology, allowing specialist IRs and INRs to train, qualify and practise alongside other procedural radiologists who perform expert image-guided procedures. Links to diagnostic radiology also remain crucial for the IR and INR specialist, with advanced image interpretation being a core component of radiological guided procedures and essential for making real-time treatment decisions. It is this that sets IRs and INRs apart from other endovascular specialties.
IR and INR also share DNA for clinical practice with the College’s other image-guided profession: radiation oncology. Knowing how to clinically assess and manage a patient, make treatment choices and perform high quality, targeted interventions (especially in oncology) are critical skills that IRs and radiation oncologists have in common. This adds a whole new dimension to the College, where the value of an interventional radiologist or interventional neuroradiologist is not
46 Inside News
just measured in the number of studies reported but in the number of consults performed, treatments delivered, benefits gained and problems solved.
These are specialties where radiologists don’t just get up from their workstations to perform the occasional injection or biopsy, but spend their days consulting and reviewing patients, receiving referrals and performing a growing range of minimally invasive, imageguided procedures. In this regard, IR and INR overlap with both radiation oncology and clinical radiology, and recognition of their specialty status would be an enduring credit to the College.
The attributes of IRs and INRs merely extend the already very long list of benefits that clinical radiology brings to the table. Just as AI has the potential to augment radiology and provide greater awareness of the role that radiologists play in patient care, so too does IR and INR afford an opportunity to pull radiologists out of the proverbial dark rooms and into the clinical and therapeutic consciousness of referrers and patients. Such an advent is in the best interests of all College members and simply an opportunity that we cannot afford to miss. The alternative is to repeat the mistakes of the past and acquiesce ground that should so obviously rest within the domain of clinical radiology.
It is the goal of the IRC that a current first year radiology registrar will have available to them, should they choose, a clear pathway from FRANZCR to advanced training in IR or INR that will lead to a formal qualification, a recognised specialist title and acknowledgement by their peers of the
important role they play in a modern health system. This will help the College, our colleagues, our patients and the hospitals and health services for which we work, value the importance of IRs and INRs providing essential care for patients yesterday, today and tomorrow.
Dr Nick Brown Chair, Interventional Radiology Committee
Cardiac CT Training 2022
We go beyond simply meeting training requirements:
l Maximum allowable course based live and library cases for ANZ credentialing.

l 117.5/67 RANZCR CPD points available for the course.
l Officially sponsored and endorsed by GE Healthcare for more than 10 years.



l Live scanning at second highest global recruiting site in SCOT-HEART study.
l Unrivalled venues - Now at ICC, Darling Harbour, Sydney.
2022 COURSE DATES:
5 Day Level A Course 24th - 28th February 2022
3 Day Refresher Course 26th - 28th February 2022
WATCH THIS SPACE: www.aicct.com.au
For 2022 Face to Face and online courses: info@aicct.com.au

Volume 17 No 5 | December 2021 47
Are You Ready for the RANZCR 2022 Training Programs?
The Training Programs for Clinical Radiology and Radiation Oncology for all Australian, New Zealand and Singapore trainees launch in February 2022.

Learning Outcomes and Training Program Handbooks
In preparation for the February 2022 launch, the two Faculties have released electronic versions of the Learning Outcomes and Training Program Handbooks. These documents have been compiled as resource guides for College trainees and members involved in new Training Program.
The Learning Outcomes are comprehensive guides to education and training for the specialty, designed to form the basis of the structured learning activities, formative workbased assessments, and assemble content for examinations within the Training Program. The Training Program Handbooks provides information and guidance for trainees, Fellows, and staff in relation to all aspects of the Training Program, from commencement to Fellowship.
Both Faculty Learning Outcomes (draft) and Training Program Handbooks are available under the TAR section of the College website.
Webinar Series: Training and Assessment Reform (TAR)
As we come towards the end of the year, the TAR webinar series for 2021 draws to close. The webinars provided critical information to trainees, Clinical Supervisors, Directors of Training, and Networks about the key changes to the Clinical Radiology and Radiation Oncology Training Programs ahead of the February launch.
More than 800 participants joined the live webinars, with many more viewers accessing the recordings via the webcast library. For those who missed previous webinars, recordings and presentations are available on the TAR webinar page. The College will continue with its webinar series in 2022 to provide trainees, Clinical Supervisors, Directors of Training, and Networks practical skills and details on completing the assessment tools within the Clinical Radiology and Radiation Oncology Training Programs. Details of the upcoming webinars will be made available on the TAR webinar page.
Training e-Portfolio System
During the months of October and November, the TAR team undertook the mammoth task of migrating data from TIMS into the new e-Portfolio system. The migration was a success,
with all trainee information having been migrated across to the new system in preparation for quality checks of the training profile data over the upcoming weeks for the launch in January 2022. For further information on the e-Portfolio System including key features, functionality and how to access, refer to the article on page 19.
Policy Review
The College policies relating the training program are currently being reviewed to align with the new Training Program. Please refer to the TAR webpage on the College website to view the latest updates on training policies.
Ongoing Updates and Information

Updated information pertaining to the 2022 Clinical Radiology and Radiation Oncology Training Programs will be made available on the TAR section of the College website. The QR code on page 49 will present all future updates and information relating to the programs to allow for quick access to the TAR section on the website.

General Interest 48 Inside News
Useful links TAR Webinars www.ranzcr.com/college/tar/ webinars
GET INVOLVED: SPECIAL INTEREST GROUPS The College’s Board establishes Special Interest Groups in areas of specific interest to the membership within clinical radiology and radiation oncology Contact us to find out more and join a Special Interest Group www.ranzcr.com/contact
The Royal Australian and New Zealand College of Radiologists®


Cancer touches us all in one way or another. That’s why every effort put into the fight must tear down the walls separating patient from progress with more intelligent ideas and answers. Intelligent Cancer Care™ is building shorter paths from research to remission. Bridging the distance between Dehli and Dubbo. Driving a direct link from high tech to high impact. And resolutely facing today’s unique challenges by connecting us all through more intelligent solutions, data, and insights to deliver advanced care—ultimately helping us realise our vision of a world without fear of cancer.


We’re all connected through Intelligent Cancer Care.
more at varian.com/intelligence ©2021 Varian Medical Systems, Inc. Varian and Varian Medical Systems are registered trademarks and Intelligent Cancer Care is a trademark of Varian Medical Systems, Inc. Refer enquiries to Varian Medical Systems Australasia on 1800.657.036 or customerservice-anz@varian.com
Learn
Indigenous Health Action Plan
This Action Plan will implement a change process. There are four pillars that are essential to this:
1. Education
2. Networking, Collaboration and Advocacy
3. Selection of Trainees
4. Mentorship
It is the work in these areas that will drive the College towards achieving equitable health and workforce outcomes for Māori, Aboriginal and Torres Strait Islander Peoples. The Action Plan has ambitious goals for 2022−2024 and even after that period, there will need to be a continuing renewal of goals to ensure we remain on that path. So much will depend on individual willingness to learn, reflect, share and grow; as well as organisational resilience to provide frameworks to allow us to overcome established barriers. So much of this will be the learning around cultural safety. Within the Faculty of Radiation Oncology (FRO), the initial work will be in the Education and Training and the Professional Practice domains where FRO has the ability to set the curriculum and influence the accredited training sites to build in cultural safety and to set goals in continuing professional development to ensure professional practice embraces cultural safety.
There are a number of approaches to developing cultural safety. From an organisational point of view, the College (staff and FRO Councillors) has
The Faculty in 2022 A Message from the Dean

been participating in the Leaders in Indigenous Medical Education (LIME) workshops run by the LIME Network: a program of the Medical Deans of Australia and New Zealand and hosted by the Faculty of Medicine, Dentistry and Health Sciences at the University of Melbourne. The second workshop was held on 9−10 November 2021. The focus of this particular workshop will be for College staff and senior executives.
Continuing Professional Development (CPD)
As the CPD triennium 2019-2021 comes to an end, there will be a new CPD program from 2022. The new program was presented at the Faculty Forum on Thursday 16 September 2021 during the ASM with a demonstration of the CPD e-Portfolio that will house the program; and a Q&A discussion on how CPD and Professional Practice are integral to the quality practice of radiation oncology. See also www.ranzcr.com/fellows/ general/cpd-overview and see page 17 for details of changes.
As a requirement for specialist recognition, all members will be required to participate in CPD.
The College is working on a CPD Handbook to be published in December 2021 to allow some time for members to familiarise themselves with the new arrangements. There is much change to be implemented and during the first year of operation, amendments and adjustments will need to be made to parts of the system including the activities list as more is understood of individual experiences. Updates to the
CPD Handbook will be made known in the later part of 2022 for 2023 onwards. Integrating all these changes will be the work of the FRO Professional Practice Committee (PPC), a standing committee of FRO, which is the evolution of the Post-Fellowship Education Committee (PFEC). We thank the leadership of Dr Ziad Thotathil as chair of PFEC in the development of the new CPD program. During 2021, FRO Council appointed Dr Carol Johnson as chair of PPC, becoming the inaugural Chief of Professional Practice of the Faculty of Radiation Oncology. This is an office bearer position.
Renewal
As 2021 draws to its end, many of us will be thinking of the time we will have to refresh ourselves, review what we have achieved or not and renew our energies to do what we have set our sights on. These past two years have been challenging in many ways both in and outside the workplace.
As a profession, we must remain focused on doing what is best for our patients while also looking after ourselves. The localities most affected by COVID-19 infections have had to consider modification of practice norms to ensure intent of treatment is balanced against the risks of COVID-19 in a population that is immune-compromised and at the same time adhering to regulatory impediments and to protocols for personal protection against the virus. Nothing has been easy.
Radiation Oncology Volume 18 No 1 | December 2021 51
continued over...
Dr Keen Hun Tai
The flow-on effects have compromised our training and assessment program, delaying the introduction of our reforms for a year. The need to introduce a digital platform for examinations (and many educational events) have re-prioritised IT requisites but at the same time made us smarter in how we go about delivering business as usual expectations. The training and assessment reforms have been publicised and introduced by the Implementation Work Group (IWG) over many webinars. Please see www.ranzcr.com/college/tar
The renewal of the efforts throughout 2021 will take us to a better program from 2022 onwards.
There are many other aspects of renewal including usually a new FRO Council each year as Councillors are elected. For 2022, your FRO Councillors are:
Dr Keen-Hun Tai (Dean)
Dr Gerard Adams (Chair, FRO Economic and Workforce Committee)
Dr Angela Allen
Dr Yaw Chin (Chief Censor)
Dr Shaun Costello (Chair, New Zealand Radiation Oncology Executive)
Dr Tuan Ha (Co-Chair, FRO Targeting Cancer Management Committee)
Ms Lee Hunt (Consumer Member)
A/Prof Sanjay Jeganathan (RANZCR President, ex-officio)
Dr Carol Johnson (Chief of Professional Practice)
Prof Jeremy Millar (Chair, FRO Quality Improvement Committee)
Dr Lucinda Morris (Co-Chair, FRO Targeting Cancer Management Committee)
Prof Daniel Roos (Chair, FRO Research Committee)
Dr Ziad Thotathil (New Zealand member)
A/Prof Sandra Turner
Dr Hari Kirupanather (Chair, FRO Trainee Committee)
I encourage the membership to approach any one of your Councillors with your discussion points and questions.
With 2022 approaching, I wish you all season’s greetings and a safe holiday period.
The Emerging Role and Potential Effects of Artificial Intelligence (AI) on the Quality of Radiation Oncology Practices
Radiation therapy is one of the complex modalities of treatment for cancer patients with multiple time-consuming steps and well-established quality assurance activities integrated in current practices. The specialty has always been the forefront of technology adoption in health care and its role has evolved through embracing transformative and disruptive technologies. Artificial intelligence (AI) has been proposed as a tool to increase quality, standardisation and acceleration of these steps leading to more safe and accurate administration of treatment. (1, 2, 3)
An artificial intelligence system is a machine-based system that can, for a given set of human-defined objectives, make predictions, recommendations, or decisions influencing real or virtual environments. AI systems are designed to operate with varying levels of
autonomy. Within this definition there are various forms of AIs with limitations and evolving capabilities to solve more difficult problems. These include various algorithms, neural networks and deep learning which uses many layers of artificial neurons to solve more complex issues. (4, 5)
Given the recent technological advances in the field of artificial intelligence and the possibility of the rapid dissemination of this technology throughout the Australian and New Zealand healthcare systems, the development of an effective regulatory framework for intelligent medical software must be considered an urgent public health priority. (6, 7)
The new technology has the potential to enhance the quality of care for patients and improve the safety, efficiency and personalisation of treatments in a timely
fashion but also introduce new risks into our current established quality assured practices. AI doesn’t just analyse and act on big data at speed and at levels of accuracy unachievable by humans, machine learning can also be built into AI algorithms, enabling them to learn from their mistakes, evolve and improve their performance.
This requires high quality of the datasets feeding the systems with appropriate human oversight to reduce risks and discriminatory outcomes and ensure high level of robustness, security and accuracy. (8,9)
Considering the potential and profound effect of AI in radiation oncology, it is necessary that these programs have appropriate governance to ensure ethical, legal and moral compliance while aiming to improve the quality of care for patients and minimising
Radiation Oncology 52 Inside News
disruptions. Safe application of AI in radiation oncology requires wellestablished standards and evidencebased research in the deployment and utilisation of AI into practice. It also requires rigorous periodic monitoring of these intelligent systems and ongoing education and upskilling of our current and future generations of workforce involved in radiation oncology departments.
AI can potentially affect various steps of radiation oncology workflow from decision-making tools in initial consults to toxicity and outcome prediction empowering the radiation oncologist to offer a more precise and personalised treatment plan and patients to make a more informed decision. It can potentially facilitate and improve quality and consistency of contouring and automated treatment planning with potential quicker QA processes and enhanced treatment delivery monitoring. While these can be exciting and perceived as great potentials, it is important to acknowledge a mismatch between the perceived capabilities of AIs and actual capabilities and limitations. (1,8)
Machine learning algorithms predominantly search for correlations between myriad input and outcome
data, the quality and utility of even the best algorithms are constrained by the well-established limitations of any study relying upon observational data. Furthermore, available radiation oncology datasets have generally been smaller and more limited than the datasets other professions may use to tune their predictive algorithms. The complex interpersonal and interventional nature of the specialty also adds to the current limitations of AI. (8,9)
The pace of developments in the field of artificial intelligence and its potential effect on our specialty makes early safeguarding and implementing standards for practice and academic research in this field of paramount importance and will enable us to use this force safely to the benefit of our patients and reduce any disruptive effect.
Dr Reza Masoud Rahbari Quality Improvement Committee
References
1 Vandewinckele L, et al. Overview of artificial intelligence-based applications in radiotherapy: Recommendations for implementation and quality assurance. Radiother Oncol. 2020 Dec;153:55-66. doi: 10.1016/j.radonc.2020.09.008. Epub 2020 Sep 10. PMID: 32920005.
2 Hosny A, et al. Artificial intelligence in radiology. Nat Rev Cancer. 2018 Aug;18(8):500-510. doi: 10.1038/s41568-018-0016-5. PMID: 29777175; PMCID: PMC6268174.
3 Brouwer CL, et al. Machine learning applications in radiation oncology: Current use and needs to support clinical implementation. Phys Imaging Radiat Oncol. 2020 Nov 30;16:144-148. doi: 10.1016/j.phro.2020.11.002. PMID: 33458358; PMCID: PMC7807598.
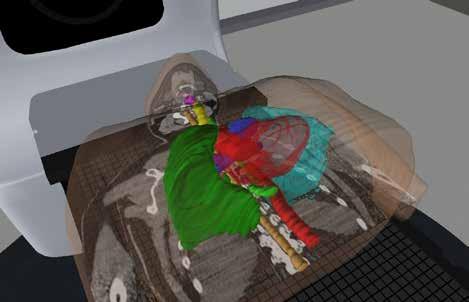
4 OECD Legal Instruments. Recommendation of the Council on Artificial Intelligence [cited 2020 29 July]. Available from: https://legalinstruments.oecd.org/en/ instruments/OECD-LEGAL-0449 3
5 OECD Legal Instruments. Recommendation of the Council on Artificial Intelligence [cited 2020 29 July]. Available from: https://legalinstruments.oecd.org/en/ instruments/OECD-LEGAL-0449
6 RANZCR Position Statement on the Regulation of Artificial Intelligence in Medicine (Only for consultation)
7 RANZCR Standards of Practice for Artificial Intelligence, Faculty of clinical Radiology
8 Thompson RF, et al. Artificial intelligence in radiation oncology: A specialty-wide disruptive transformation? Radiother Oncol. 2018 Dec;129(3):421-426. doi: 10.1016/j. radonc.2018.05.030. Epub 2018 Jun 12. PMID: 29907338.
9 Deig CR, Kanwar A, Thompson RF. Artificial Intelligence in Radiation Oncology. Hematol Oncol Clin North Am. 2019 Dec; 33(6):1095-1104. doi: 10.1016/j. hoc.2019.08.003. Epub 2019 Sep 11. PMID: 31668208.
Radiation Oncology Volume 18 No 1 | December 2021 53
Radiation Oncology Phase 1 Examination
The Radiation Oncology Phase 1 Examination are changing
In 2022, the delivery of the Radiation Oncology Phase 1 Examination will change and from 2023, the style and timeline for sitting will change.
What are the changes?
In 2022:
• The Radiation Oncology Phase 1 Examination will be transitioning from the written paper-based examination process to an electronic format.
In 2023:
• Examinations will be held twice a year
• Three 2-hour subject papers in the three oncology science subjects (Anatomy, Radiation Oncology Physics, Radiation and Cancer Biology) which can be sat independently
• A pass in each subject paper can be carried over to the next sitting.
Anatomy
One 2-hour paper, aligned to the new learning outcomes, comprised of:
• Diagram Labelling
• Multiple Choice Questions
• Short Answer Questions.
Radiation Oncology Physics
One 2-hour paper, aligned to the new learning outcomes, comprised of:
• Multiple Choice Questions
• Short Answer Questions.
Radiation and Cancer Biology
One 2-hour paper, aligned to the new learning outcomes, comprised of:
• Multiple Choice Questions
• Short Answer Questions.
Why the change?
As part of the TAR Project, improvements and enhancements to the Radiation Oncology Phase 1 Examination were considered. These included:
• amending the Phase 1 examinations to allow assessment of a greater breadth of knowledge that is relevant to clinical reasoning
• transforming to digital delivery of the examinations to align to modern practice
• increasing to two examination sittings per year
• providing flexible options to allow trainees to prepare for their exams at their own pace
• introducing new item types and multiple-choice questions (MCQs).
When are the changes happening?
The 2022 Phase 1 Examination will be delivered electronically and conducted as per the current policy and rules for eligibility requirements.
From 2023, the new Phase 1 Examination format will come into place and the examination eligibility requirements and timetable for the Phase 1 Examinations will be aligned to the 2022 Training Program.
What are the timetable changes?
From 2023, there will be two examination sittings (series) and each Phase 1 Examination series will offer all three subject papers.
Radiation Oncology Phase 2 Examination
The Radiation Oncology Phase 2 Examination will have some changes.
In 2022, the delivery of the Radiation Oncology Phase 1 Examination will change and from 2023, the changes to examination eligibility will take effect.
What are the changes?
• The Radiation Oncology Phase 2
Examination will be transitioning from the written paper-based examination process to an electronic format from Series 2
• Examination eligibility will progressively change throughout 2022 through to 2023 to align with the new training program. For information on 2022 examination eligibility, please refer to the Trainee Transition Exam Eligibility document.
Eligibility from 2023
To be eligible to apply for the Phase 2 Examination, trainees must be in an accredited radiation oncology training position, in Phase 2 of training and have completed:
• A minimum of 24 months full-time equivalent (FTE) of accredited training in Phase 2
• The SMART workshop
• Phase 2 Practical Oncology Experiences
• All Phase 2 Work-Based Assessments
• A Multisource Feedback within Phase 2.
All trainees must have rotated to another training site for a minimum of 12 months FTE prior to sitting.
For further information on examinations, please refer to the Radiation Oncology Training Program Handbook.
What is the timetable schedule for Phase 2 Examinations?
Detailed information on the upcoming examination series can be found on the College’s website
Radiation Oncology 54 Inside News
Phase 1 Examinations Series 1 Series 2 Applications Open / Close January July Examinations Held March September Release of Results May November
Phase 2 Examinations Series 1 Series 2 Applications Open / Close December (year prior) May Written Examinations Held February July Viva Examinations Held March August Release of Results April September
It is with a sense of relief and thankfulness that I write this as I am pleased to report that both phases of the Radiation Oncology examinations for 2021 have been successfully delivered. Despite the seemingly insurmountable challenges we faced, both logistically and emotionally, this milestone was achieved through the selfless efforts of many people working towards a common goal. A massive thanks and congratulations to all our volunteer examiners for their resilience and adaptability in the ever-shifting sands of the COVID restriction landscape.
The Phase 1 examination was held on Friday 10 September at a record 13 sites. All marks were finalised at the Board of Examiners meeting and released to the candidates on 5 November 2021. I would like to thank and acknowledge Drs Claire Hardie and Carminia Lapuz, who are both stepping down as co-leads of the Phase 1 examination program at the end of this year. Their years of contribution and hard work are greatly appreciated and valued.
To provide greater recognition and support to the Phase 1 examiners, the ROETC approved the terms of reference and the position descriptions for members and the chair of the Phase 1 Examination Panel (P1EP). This panel will be responsible for setting, reviewing, marking and developing the Phase 1 examinations, as well as organising the Phase 1 examination course. The formation of the P1EP is timely, as not only will it have to deliver the Phase 1 examination in its current format in 2022, but also start the necessary transitionary arrangements towards the new digital format for two sittings in 2023. This new format will include different styles of
Training in 2021 and 2022
Chief Censor in Radiation Oncology

questioning such as multiple choice and very short answer type questions.
The delayed Viva component of the Phase 2 examinations was held between 6−8 October at 10 sites. All marks have now been finalised and the formal results were released to the candidates on 29 October 2021. The 6-week delay has meant that our examiners will now need to start preparing for the Series 1 2022 examinations almost as soon as they have completed the current series. Again, next year will involve work towards the transition of a digital format in Series 2. Plans to gradually expand the current Phase 2 examiner pool are underway to reduce examining fatigue for our pool of dedicated examiners.
The threshold of the implementation of the new training program is well and truly here with Trainee Information Management System (TIMS) now having gone off-line. Data migration is proceeding smoothly as planned with data archiving into the College’s file servers (SharePoint) and data migration into the new e-Portfolio system. Trainees would now have received transcripts of their status and progress within the training program. Once these have been checked and signed off in terms of their veracity, this information will be uploaded into the e-Portfolio system and ready to go live by 21 January 2022 for transitioning trainees.
There is still a significant volume of work involved in tidying up loose ends before the new training program commences including finalising details in the Training Program Handbook, the Oncology Sciences Information Pack and Workshop Documents. Additionally, Terms of Reference for committees and formal position descriptions for roles within the training networks such as the Training Network Directors, Directors of Training, Clinical Supervisors, Research Mentors and Educational Support
Officers have been revised and brought up-to-date in alignment with the new training program.
The bi-faculty Selection Review Working Group (SRWG), which was formed in 2019 has now disbanded and has provided both Education and Training Committees (ETC) with seven recommendations to improve trainee selection and recruitment. These recommendations are made to ensure that the selection guidelines and processes are standardised and that they are consistent, transparent, robust and sustainable. A five-phase selection framework will be implemented, with the College taking a more active and central role in the initial stages of screening and selection, while still allowing individual training networks to shortlist candidates, conduct the interviews and make final decisions regarding recruitment.
Finally, the Māori, Aboriginal and Torres Strait Islander Committee (MATEC) which was formed by the Board in 2020, has developed the Indigenous Action Plan, which was launched at the 71st RANZCR Annual Scientific Meeting in September. The Action Plan consists of four foundational pillars. In line with the third pillar of Selection of Trainees, one of the SRWG’s key recommendations include a mandate for the ETCs to consider mechanism/s to increase the selection of Māori, Aboriginal and Torres Strait Islander applicants and applicants from rural and regional backgrounds. With the first foundational pillar being Education, cultural safety has been incorporated into the learning outcomes of the new training program. Accreditation standards for training sites are also being reviewed to ensure that they are culturally safe environments for Māori, Aboriginal and Torres Strait Islander trainees.
Radiation Oncology Volume 18 No 1 | December 2021 55
Dr Yaw Chin
Radiation Oncology Trainee Committee (ROTC)
trainees. I am proud of how much we’ve been able to do in the space of a year. We prioritised trainee engagement and communication, we actively sought out the trainee perspective and made a conscious change in the tone of our communication. We wanted an approachable and relatable ROTC (lame jokes and all) and to do away with formality which has a way of hindering frank and open conversations. Though it is difficult to quantify there was been more community and engagement with trainees and their representatives.
contingency planning and outlined what would be most important for the trainees moving forward. This formal communication was necessary, not for the sake of antagonism but for transparency and accountability. We would have been inadequate in our role as trainee advocates had we ignored the concerns from the trainee body. While we may not have received the response we had hoped for, we have started the conversation.
As the year draws to a close it is only right that we reflect on the year that was, and what a year it has been! For me, it has been an absolute privilege to be the chair of the Radiation Oncology Trainee Committee (ROTC) for 2021. I cannot give enough praise to this year’s committee, my energetic and engaged team of colleagues who I have come to count as friends. I must recognise them here for their significant contributions; Dr Tachi Zhong Hu (NSW – Southern Network), Dr Cristian Udovicich (Victoria and Tasmania), Dr James Gallo and Dr Kim Budgen (Queensland), Dr Adam Byrne (South Australia), Dr Caris Chong (Western Australia) and Dr Katherine Tse (New Zealand).

We started the year with a workplan that was something of a shift from previous years, we realigned the ROTC for what it should be at its heart—strong representation and advocacy for the

Of course, the bulk of our advocacy focuses on education, assessment and accreditation of training. The ROTC had the great experience of being involved in a pilot workshop to review and discuss the incoming changes in assessments and highlight where trainees may face difficulties. This year’s ROTC represented the breadth of the trainee experience, we come from such a wide range of backgrounds, and it was a lightbulb moment for how the ROTC could be used as a sounding board early in planning for these big-ticket items that have such a significant impact on our trainees. I suspect in future we will see more of a role for the ROTC in similar situations.
No discussion of trainee issues this year would be complete without mention of the examinations. I cannot imagine what it has been like for our examsitting trainees this year. The ROTC advocated for our trainees and sent formal communication to highlight how difficult postponements are for trainees, requested clarification of the
Finally, I would like to encourage trainees to get involved in the ROTC. Part of why I chose to get involved is that advocacy is important. We are beholden to the colleges from which we seek fellowship, this is simply the nature of medical training. Consequently, if there are issues with training the only way to fix them is to identify what the issues are and talk to those who have the power to create change. We may not be successful at every turn but we will definitely make inroads.
We have a seat at the table—it is important that we don’t waste it.
Radiation Oncology 56 Inside News
Protect your health, access our wellbeing resources
Dr Chamitha Weerasinghe
www.ranzcr.com/fellows/general/your-wellbeing
Kia Ora. The weather is finally warming up, the AB’s recent Northern Tour had some mixed results and the 90 per cent vaccination target set by the government seemed ambitious when first introduced. But as I write, NZ has achieved, or nearly achieved, a 90 per cent vaccination rate for most DHB regions. This is good news for NZ as the world surpasses 5 million COVID deaths according to the WHO.
I’ve been attending Radiology COVID Agile Response Team (RAD CART) meetings. These are Ministry of Health meetings held fortnightly. The primary purpose is to assess how the regions are coping. Unsurprisingly, ultrasound is an issue with a significant backlog in some regions and we are all increasingly concerned about the surge in demand that will occur once the lockdown is lifted. At the last meeting we were all reminded by one of the radiologists attending that our allied health professionals face a higher burden of risk with significant face-to-face time with patients. Our ability to maximise system capacity is linked to our ability to keep them safe.
A highly vaccinated population supports the whole system and allows all of us to provide care in a safe environment.
Doctors Stand Up for Vaccination (DSUV)
The College, along with all other colleges, endorsed the DSUV initiative. The open letter is ‘written on behalf of the undersigned doctors of Aotearoa New Zealand…who wish to present a united and evidence-based voice to the people of Aotearoa New Zealand in support of vaccination against COVID-19 for all eligible New Zealanders.’
New Zealand Branch News
It is better late than never, so feel free to join more than 6,500 of your colleagues and sign here. They are still accepting signatures.
www.doctors-stand-up-for-vaccination. com
Ethical Referrals
The College has now finalised its Ethical Referrals Discussion Paper. I, along with Dr Kate O’Connor (NZ representative on the Faculty of Clinical Radiology Council), have now also met with key stakeholders to advocate for arm’s-length referrals: ACC, Health and Disability Commissioner, Medical Council of New Zealand and the Ministry of Health.
We received support for the paper at all four meetings. The MCNZ will be reviewing Doctors and health related commercial organisations in 2022. The document will be widely distributed for consultation. Please be on the lookout for the communication from the MCNZ and respond to the consultation if you would like more strongly phrased guidance around medical entrepreneurship and conflicts of interest.
Those of you with an ACC contract will have also received recent correspondence from ACC about collecting referrer information. This is so ACC can start accurately and efficiently tracking referral patterns. ACC has also recently reminded service providers that they are obliged to declare conflicts of interest to ACC. The College has also suggested increasing the range of GP referrals in its discussions with ACC. I’d welcome hearing from those of you with a view on GP referrals: nzbranch@ranzcr.org.nz
Prior to finalisation of the paper, College representatives met with the Royal Australian College of Surgeons (RACS) to discuss the importance of
arm’s-length referrals. RACS already has a Code of Conduct and we hope to continue a conversation with RACS about how we might work together in 2022. An article about our Ethical Referrals document will be appearing in the RACS newsletter Cutting Edge
NZ Branch Committee
A number of members of the NZ Branch Committee will be finishing their current terms in December 2022. An EOI will go out in March 2022. I’d like to invite all NZ members to consider joining the Branch Committee. The discussions are interesting and meaningful to the NZ radiology community. Some examples of 2021’s activities included:

• Ethical referrals
• Consultations from stakeholders including MCNZ and Te Aho O Te Kahu (Cancer Control Agency)
• Scheduling the New Zealand ASM
• Advocacy for increasing the obstetric ultrasound fee
• Liaison with International Accreditation New Zealand (IANZ) regarding monitor display requirements.
Kia kaha. Stay safe, vigilant and strong.
Useful links
Ethical Referrals Discussion Paper
www.ranzcr.com/college/documentlibrary/ethical-referrals-in-clinicalradiology-discussion-paper
Doctors and health related commercial organisations
www.mcnz.org.nz/assets/standards/ e77cce6f24/Doctors-and-healthrelated-organisations.pdf
News Volume 18 No 1 | December 2021 57
Dr Gabes Lau
Varian brings Intelligent Cancer Care to Dubbo in regional-first

Dubbo’s newest cancer centre is now home to a state-of-the-art Varian TrueBeam radiotherapy system, bringing radiation treatment to the region for the first time. With Australia’s regional and remote areas still falling short of the cancer survival rates in major citiesi, the new installation is a welcome addition for patients wanting to undertake radiation treatment closer to home.
The installation provides hundreds of thousands of residents in Dubbo and surrounding Central West areas with the confidence and quality care of a radiation system which is currently being used in top cancer clinics around the world. Currently, residents considering radiation therapy in the area either need to decide between travelling to surrounding major hubs, potentially requiring weeks away from family and work, or choose to forego the treatment option.
The new Varian TrueBeam linear accelerator system combines advanced imaging, flexible treatment options and high precision radiation doses, with submillimetre accuracy, to enable clinicians to treat a wide array of cancer cases. The system empowers clinicians to flexibility tailor treatment options to each patient, unlocking the potential to make a significant impact to patient outcomes.
The installation is another step in Varian realising its vision for a world without the fear of cancer.
“Varian’s Intelligent Cancer Care approach is driving the progress of cancer care for the next 30 years and beyond, both in Australia and globally. We are using software and automated processes to help oncology
professionals collaborate and develop more precise and holistic cancer treatments, making cancer care easier to manage and deliver,’ said Rebecca Cortiula, Snr Managing Director Varian Australasia.
“With Varian part of Siemens Healthineers, we have brought together two leaders in imaging and radiation therapy, combining the sharpest minds in healthcare to transform the future of oncology and achieve new victories against cancer. The new centre in Dubbo is just one example of how we can tangibly transform cancer outcomes for Australians through our innovations,” said Rebecca.
The $35 million-dollar Western Cancer Centre was funded by both State and Federal government and started taking patients in September. With a range of advanced imaging and treatment technology, like the Varian TrueBeam system, the centre will provide lifesaving cancer care to the thousands of people living in regional and remote areas of western NSW. The advanced offering also has the potential to attract more healthcare professionals, including medical oncologists and radiation oncologists, to practice in the region, further improving quality of care for residents.
The Western Cancer Centre was approved after Local Government fought for its development with the backing of a petition with more than 45,000 signatures. In conjunction with the Dubbo Hospital redevelopment, the centre includes a chemotherapy suite, consultation rooms and a wellness space for patients and families.
Varian software systems enable leading cancer treatment centers, like the Western Cancer Centre, to provide integrated, multidisciplinary care to residents in regional areas. Multidisciplinary care means physicians with different expertise, who may be geographically disbursed, can come together to provide a comprehensive roadmap of treatment options.
As a global leader in radiation therapy, Varian is committed to delivering more comprehensive, multi-disciplinary and fully integrated cancer care solutions. By bringing teams closer together to build multi-modal treatment plans in more effective ways, Varian can democratise access to cancer treatment for all Australians.
In Australia, Varian is the leading provider of radiation accelerators with over 150 linear accelerators installed, treating more than 70,000 patients a year.
References
i Cancer in Australia 2019, Australian Institute of Health and Welfare. Access November 2021. https://www.aihw.gov.au/getmedia/8c9fcf520055-41a0-96d9-f81b0feb98cf/aihw-can-123.pdf. aspx?inline=true
Radiation Oncology 58 Inside News
Advertorial
Targeting Cancer Fun@Home 2021










To bring back memories of all the annual Targeting Cancer Fun Runs in years past, this year we ran Fun@Home 2021, an online photo and video competition on social media to connect to and engage with the wider Targeting Cancer community and raise awareness of the Targeting Cancer Campaign.
From 1 to 31 October 2021, we encouraged our staff, members and the Targeting Cancer community to share a short video or photo on Facebook and Twitter or via email. The video or photo needed to contain a Targeting Cancer Fun@Home logo to qualify for the final prizes.
The event attracted great entries including videos and photos, covering a wide range of fun activities including outdoor and indoor exercises, gardening, home cooking, Halloween, crochet, and many others. It activated the online community with increased engagement in the month of October, extending the reach of the campaign and increasing brand visibility.
In October, the Targeting Cancer Facebook post reach exceeded 4,000, the total post impressions exceeded 10,000, with more than 1,000 engagements generated while Targeting Cancer Twitter generated 14,700 impressions.
The two winners of Targeting Cancer Fun@Home 2021 were announced in November. The video or photo which received the most likes, comments, and shares on social media and won the Most Popular Category was from Emily Potts-Humphrey, and our judging panel comprised of the Targeting Cancer Management Committee Members selected Yvette Cabello’s collage as the winner of the Most Creative and Fun Category. Congratulations to both winners and thank you all for your support.
You can support our Targeting Cancer Campaign at any time of the year, help us raise awareness of radiation therapy as an effective treatment for cancer. We’d love to hear from you if you have any feedback and suggestions via email: info@targetingcancer.com.au


Volume 18 No 1 | December 2021 59 Advocacy
Vertebroplasty: a New MBS Item
Interventional Radiology Society of Australasia (IRSA)
IRSA are pleased to report that ten years after we first commenced the VAPOUR trial, the Government has supported the public listing of an item for vertebroplasty on the Medicare Benefits Schedule (MBS).
From 1 November 2021, there will be a new MBS item 35401 for vertebroplasty for the treatment of a painful thoracolumbar vertebral compression fracture of the thoracolumbar spinal segment (T11, T12, L1 or L2) in patients where pain is severe and has had a duration of three weeks or less, symptoms are poorly controlled by opiate therapy and there is MRI (or SPECT-CT if MRI is unavailable) evidence of acute vertebral fracture.
What does this mean for providers?
This service is to be performed by interventional radiologists. Practitioners should be registered with and provide relevant service data to the Vertebroplasty MBS Service Monitor (the Monitor) managed by IRSA. If you perform these services and have not advised IRSA please contact us as soon as possible via secretariat@irsa.com.au
The Monitor has been established by agreement of the Department of Health and IRSA, on the advice of the Medical Services Advisory Committee. The objective of the Monitor is to capture data relating to services of item 35401 including patient age, patient sex, provider name and state of practice, duration of fracture before the procedure, in-patient or out-patient status at the time the decision was made
to perform the procedure, and adverse events related to the procedure that require additional hospitalisation or medical treatment.
IRSA will share this data with the Department of Health in six-month intervals for the lifetime of the Monitor.
How will these changes affect patients?
Patients will receive Medicare rebates for clinically relevant vertebroplasty services.
IRSA ASM 2022: SAVE THE DATE
The IRSA ASM will take place in Queenstown, New Zealand on 9−11 August 2022 at The QT Hotel, Queenstown. Please save the date as we look forward to welcoming you in Queenstown next year.
Australian and New Zealand Society of Neuroradiology (ANZSNR)
ANZSNR ASM 2022 SAVE THE DATE
Hilton Hotel, Sydney 10–13 March 2022
On behalf of the Australian and New Zealand Society of Neuroradiology and the ASM Scientific Committee we would like to invite you to the 2022 Annual Scientific Meeting to be held 10−13 March 2022 at the Hilton Hotel, Sydney. After a yearlong hiatus we are planning an ambitious ASM. The last one to two years have presented many challenges. The medical community, like others, has been fractured and separated. Our vision is to reunite with our colleagues in a way that continues to push the science and patient outcomes forward.

We are excited to be introducing several novel initiatives to the 2022 ASM:
• Selected abstracts will be published in the Journal of Medical Imaging and Radiation Oncology, the official journal of the College—start preparing your research and abstracts now—check the website for the call for abstracts
• Interventional Neuroradiology Course on the opening Thursday
• Diagnostic Neuroradiology Course on the closing Sunday
• Interventional and Diagnostic Neuroradiology/Head and Neck Radiology parallel program. For further information, please visit the ASM website www.anzsnrasm.com
We look forward to welcoming you to Sydney in March 2022. For those delegates who are unable to attend the ASM in Sydney due to COVIDmandated travel restrictions or quarantining requirements on return, a local hub, joined in real time to the main ASM will be provided. Hub attendees will have a local social program and small exhibition at the Hub venue. The Organising Committee will continue to monitor the COVID situation and will provide further details on Hub locations over the coming months.
To register your interest for the ASM, please email the Events Manager, Natacha Costa at ncosta@ncevents.com.au
News 60 Inside News
Faculty of Radiation Oncology
Genito-Urinary Group (FROGG)
In spite of long lockdowns and COVID fatigue, the FROGG executive committee has continued its regular, two-monthly, virtual meetings and is currently busy finalising the program for the next FROGG meeting which is to be held in Hobart in September 2022. With double vaccinations rates looking very healthy and booster shots looming, we have our fingers crossed that this meeting will be a face-toface meeting and colleagues from all states and territories and New Zealand will be free to travel without fear of quarantine. The prostate cancer focused meeting is shaping up to be fabulous with three prominent international guest speakers: Professor Daniel Spratt
original, GU-focused research project. The successful applicants will present their project at an inaugural trainee poster session at the meeting.
In addition to organising the FROGG meeting, over the course of 2021, we have continued to provide advice and support on behalf of the College for a number of Medical Services Advisory Committee applications including the use of Lutetium PSMA for the treatment of metastatic castrate resistant prostate cancer. We have also worked with EViQ, Prostate Cancer Foundation of Australia (PCFA) and the Cancer Council to update patient information resources on prostate cancer and other genitourinary malignancies.
had such a high calibre of speakers including Professor Anthony D’Amico, Dr Alison Tree, Professor Vedang Murthy, Professor Andrew Loblaw, Dr Patrick Cheung and Dr Gerard Morton. These webinars will continue into the first half of 2022. We are also excited to be working closely with the College on another pharmaceutical-sponsored trainee educational event in 2022. Lastly, please watch out for our Expression of Interest advertisement in Inside News and in your email inbox. We are looking for two fellows to join the FROGG committee in 2022. As one of the longest standing Special Interest Groups in the College, being a FROGG executive committee member


The Faculty of Radiation Oncology


Genito-Urinary Group (FROGG)
2022 Prostate Cancer Workshop

News
Precision Medicine in Prostate Cancer: Genomics, Technology and Evidence Based Practice
PROF DANIEL SPRATT Professor of Radiation Oncology University of Michigan USA
DR ALISON TREE Consultant Clinical Oncologist The Royal Marsden Hospital London UK
Marsden Hospital
8-10 September 2022 | Crowne Plaza, Hobart, Tasmania | www.frogg.com.au
PROF
CHRIS PARKER
Clinical Oncologist The Institute of Cancer Research The Royal
London UK
Make Savings, Access Benefits in our Member Rewards Program
The College’s Member Rewards Program has been carefully tailored to meet your needs—automotive, advisory, finance, insurance, legal, travel and lifestyle products and services are all included.
BUSINESS ADVISORY SERVICES
KPMG Enterprise
KPMG Enterprise is a specialist division of KPMG Australia, dedicated to advising the emerging, private and midmarket. KPMG works with established and emerging entrepreneurs, family business, private clients, not-for-profit and fast-growing companies to build successful organisations.

RANZCR members can access the following benefits:

• An initial meeting with a Partner or Director free of charge
• A minimum 40 per cent discount on KPMG standard rates for the engagement period with all RANZCR members
• Access to a dedicated national KPMG Enterprise team to support your members, across all service areas.
This offer is available to the following services provided by KPMG Enterprise Australia, New Zealand and Asia:
* Audit and Assurance
* Tax, Transaction, and Accounting
* Advisory
* Accelerating Business Growth
To access the offer, please complete the online form. You will then be connected with the appropriate KPMG Enterprise contact.
FREEDOM IS IN THE AIR— BORDERS ARE OPENING AND TRAVEL MEMORIES ARE WAITING TO BE CREATED!
The Accommodation Brokers

If you are planning or thinking about booking a holiday don’t forget our partner The Accommodation Brokers. Members receive great discounts on over 1.6 million travel products both domestically and internationally.
Just this week one member saved more than $200 on accommodation and car rental for Hobart— they had booked via Booking.com, but contacted The Accommodation Brokers and obtained better pricing.

To get these savings you must register at The Accommodation Brokers website.
LIFE INSURANCE
NobleOak

NobleOak Life Insurance has partnered with Carbon Neutral who will plant 10 trees in Australia for each RANZCR member taking out cover from 1 October until 16 December.
RANZCR members also receive a 10 per cent lifetime discount on quality, awardwinning Life cover from NobleOak (T&Cs apply).
To get a quote visit www.nobleoak.com.au/ranzcr
The Member Rewards Program
Useful links
www.theaccommodationbrokers.com.au
Useful links
www.ranzcr.com/component/ rsform/form/20-contact-kpmg
Don’t forget to read more about our current Member Rewards offers. We also have unique Member Rewards offers from Mercedes, Home Loan Solutions, Tesla, Petals Network, BUPA, Europcar, Medical Wealth Advisory, and BMW/Mini. Visit
General Interest 62 Inside News
our full Member
Program www.ranzcr.com/college/memberrewards
Rewards
Branch News
Queensland Branch
The Queensland Branch held their Annual Scientific Meeting at the JW Marriott Gold Coast on 5 June 2021.This year’s program had a focus on MRI, with dedicated streams on women’s, body and neuro imaging. The eminent line-up of speakers included Professor Sandeep Bhuta, the Anne Osborne International Outreach Professor of 2019. It was a very successful event, with nearly 120 attendees plus sponsors and vendors.




We thank our event coordinator Rebecca Fielding for an incredible job at late notice.
Dr Charlie Hsu, Dr Candice Sagi and Dr Arj Somasundaram

Co-convenors, RANZCR QLD ASM 2021

Australian Capital Territory Branch
The ACT Branch Educational Evening held Wednesday 17 November 2021 at Hotel Realm was well attended and enjoyed by all.

Radiology registrar research presentations
• Dr James Bain - VIRADS for pre-treatment staging of bladder cancer in an Australian cohort.
• Dr Philip Hingley - The relationship between age, breast density and histological tumour grade: a 3-month retrospective audit of a national screening program.
• Dr Jade Lee - "Radiologists and surgeons, beware: rare presentation of the ureteral inguinal hernia."
Guest Speakers
• Dr Sean Robison - Keeping Abreast of Imaging.
• Dr Vipul Aggarwal - Update on evaluation and management of Pancreatic cystic lesions.
• Dr Kylie Jung - Radiation brain necrosis - challenges in diagnosis and management.
The

Volume 17 No 5 | December 2021 63 News
~ In Memoriam ~
College notes with regret the death of the following members:
Dr Laurence Alfred Lees, Fellow, NSW
Australian and New Zealand Emergency Radiology Group (ANZERG)

While COVID has kept us busy in a different way, unfortunately there has been rather little movement in our Special Interest Group.
We were able to appoint two members to the Executive Committee following an expression of interest. The new members are Dr Elizabeth Dillon and Dr John Vedelago. Liz is based in Perth and John in London and we are fortunate to have them join the Committee.
My second term as Chair expired some time ago but I was asked to continue till we could appoint a new Chair. We intend to do that once the new Committee convenes.
The ANZERG session at the recent virtual RANZCR ASM was well attended and I would like to thank Dr Ramdas Sanasi (England), Dr Ferco Berger (Canada), Dr John Vedelago (England) and Dr Tim Joseph (Melbourne) for their excellent presentation.
ANZERG is partnering with global Emergency Radiology Societies and Special Interest Groups in organising the first ever Joint International Congress on Emergency Radiology (JICER). The conference will be based on ‘follow the sun’ concept, a 24 hour non-stop virtual conference based on the philosophy that emergency radiologists provide a 24/7 service. The conference will run over 5 and 6 February 2022 starting in the Asia Pacific region and moving west finishing in The Americas.
We are bringing together American and Canadian Society of Emergency Radiology, European and British Society of Emergency Radiology, Society of Emergency Radiology - India, ANZERG, Japanese, Korean, Thai, Taiwanese and Asian Societies of Emergency Radiology and a host of other countries that do not yet have an emergency radiology SIG or society.
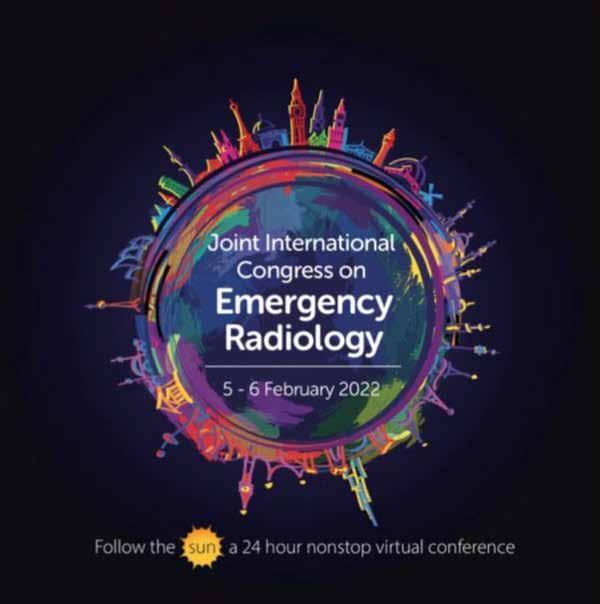
We have a fantastic panel of speakers from all corners of the world and the scientific program will be very comprehensive and exhaustive. Please visit the website and express your interest to attend. We would also appreciate if you could assist in promoting the conference within and outside your hospital or practice.
As this is the last 2021 edition I wish you all a very joyful festive season and hope you can unite with your family members wherever they are.
A/Prof Dinesh Varma Chair, ANZERG
64 Inside News News
links
International Congress on Emergency Radiology www.jicer22.com
Useful
Joint
Communication in Obstetric Ultrasound
In case you missed the RANZCR ASM, I would like to draw attention to the important topic of communication in obstetric ultrasound, presented by Dr Peter Duffy.
RESPONSIBILITY: Radiologists providing obstetric ultrasound services are responsible for the examination and communication of its report to the referring clinician. Usually, this involves the doctor being available to attend the patient to deal with significant or unexpected findings while the patient is on site.
DIAGNOSIS: Unlike most of radiology, ultrasound is ‘real time’. The most important diagnostic issue in obstetric imaging is the assessment of the presence (or absence) of fetal cardiac activity.
URGENCY: Protocols should exist to trigger urgent/significant findings being brought to the attention of the reporting doctor ASAP, and ensure that doctor uses all reasonable endeavours to communicate directly with the referrer who will be providing clinical follow-up,
PATIENT-CENTRED CARE: Patientcentred care is advocated by all authorities and requires a collaborative interdisciplinary approach with a focus on patient outcomes delivered with compassion and empathy.
COMMUNICATION:
Sonographer and patient: when there are no issues of concern, it is usual for the sonographer to be reassuring at the end of the examination. For the urgent finding of fetal demise, the sonographer either communicates such to the patient under delegated authority and/or calls in the radiologist.
Sonographer and the radiologist: have a verbal and worksheet communication system with urgent clinical trigger criteria.
Radiologist and patient: if the condition is urgent, the radiologist either communicates directly with the patient, or delegates this to the sonographer, communicates with the referrer and prepares the report, including documentation of the date, time, nature of what was conveyed or discussed.
Sonologist and the referring clinician: as above.
RECOMMENDATIONS:
1. Radiologists regard fetal demise as an urgent condition.
2. Expand ultrasound worksheets to include communication information, in addition to the ultrasound findings, of the date/time, nature of what was conveyed etc for inclusion in the final report.
3. Radiologists formalise sonographer communication through implementation of written protocols (including after hours), to ensure urgent patient triage if necessary, and document urgent communication with the referrer.
Thank you for highlighting this very important topic, Peter.
Also, a reminder that the OGSIG Meeting is planned for 25 March 2022.
Best wishes to all for a safe and happy holiday season.
Dr Emmeline Lee Chair of OGSIG
Australian and New Zealand Palliative Radiation Oncology Group (ANZPROG)
ANZPROG is a Faculty of Radiation Oncology Special Interest Group that seeks to build a community for the members to connect, share their experience and find opportunities to collaborate.
The ANZPROG Members Forum was launched at the RANZCR2021 Annual Scientific Meeting. The first of the series was a roundtable discussion highlighting the benefits and challenges of the Rapid Access Palliative Radiation Therapy Clinics in Australia and New Zealand. Also in 2021, ANZPROG conducted an Australian and New Zealand wide survey on this topic and Dr Daniel Roos presented the findings at the
ASM. This is now in press in the Red Journal, the first published project for ANZPROGi. ANZPROG will continue to create opportunities for members to engage in conversations around pertinent topics in palliative radiation therapy. The anticipated topics for the Members Forum in 2022 are: updates and perspectives on voluntary assisted dying in Australia and New Zealand and optimal utilisation of advanced techniques in palliative radiation therapy.
Join ANZPROG as a member. If you wish to read the Terms of Reference for ANZPROG you will find them on the College website.
Useful links
ANZPROG
The Australian and New Zealand Palliative Radiation Oncology Interest Group
www.ranzcr.com/college/specialinterest-groups
If you have any questions, please don’t hesitate to get in touch.
T: +61 2 9268 9777
E: FROSIG@ranzcr.edu.au
W: www.ranzcr.edu.au
Volume 18 No 1 | December 2021 65 News
References i Roos D, James M, Lah M, Pope K, Shorthouse A, Govindaraj R, Holt T. Rapid Access Palliative Radiotherapy clinics – the evidence is there, but where are the clinics? An Australian and New Zealand perspective. Int J Radiat Oncol Biol Phys 2021:111;959-64, and the related article: Roos D, Job M, Holt T. Establishing a palliative Advanced Practice Radiation Therapist role: the Brisbane experience. In press, J Med Imag Radiat Oncol.
Calling all International Fellowship FRANZCRs
Heading to Canada, the US or UK in the coming months? Why not take a little ANZ with you?
Everlight Radiology is ANZ’s largest teleradiology provider. Many of our reporters are just like you - FRANZCRs living in Canada, the UK, USA, Europe for a year or more and reporting for our ANZ clients in their down times.

Cardiac CT Training 2022

We go beyond simply meeting training requirements:
l Maximum allowable course based live and library cases for ANZ credentialing.

l 117.5/67 RANZCR CPD points available for the course.
l Officially sponsored and endorsed by GE Healthcare for more than 10 years.

l Live scanning at second highest global recruiting site in SCOT-HEART study.

l Unrivalled venues - Now at ICC, Darling Harbour, Sydney.
2022 COURSE DATES:
5 Day Level A Course: 24th - 28th February 2022
3 Day Level A Course: 26th - 28th February 2022
WATCH THIS SPACE: www.aicct.com.au
For Face to Face and online courses: info@aicct.com.au
Keep your ANZ diagnostic experience current Report on interesting cases including Urgent Emergency and Trauma
Work at a time that suits you
Highly competitive remuneration

General Interest 66 Inside News
out more: Contact Trish Hay today T: (+61) 432 084 415 E: phay@everlightradiology.com All communications are confidential.
Find
AstraZeneca Pty. Ltd. ABN 54 009 682 311. 66 Talavera Road, Macquarie Park, NSW 2113. www.astrazeneca.com.au. For Medical Information enquiries or to report an adverse event or product quality complaint: Telephone 1800 805 342 or via https://contactazmedical.astrazeneca.com Or email Medical Information enquiries to medinfo.australia@astrazeneca.com. AU-11158. July 2021.








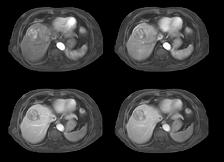
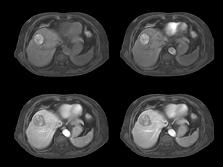





















 IMAGE CREDIT: DESTINATION NSW
Alberto Vargas Chief, Body Imaging Service Memorial Sloan Kettering Cancer Center New York
Ania Kielar Associate Professor Toronto General Hospital Department of Medical Imaging
Michael P Hartung Assistant Professor of Radiology Abdominal Imaging and Intervention University of Wisconsin School of Medicine and Public Health
Perry Pickhardt Professor of Radiology Chief of Gastrointestinal Imaging University of Wisconsin School of Medicine & Public Health
IMAGE CREDIT: DESTINATION NSW
Alberto Vargas Chief, Body Imaging Service Memorial Sloan Kettering Cancer Center New York
Ania Kielar Associate Professor Toronto General Hospital Department of Medical Imaging
Michael P Hartung Assistant Professor of Radiology Abdominal Imaging and Intervention University of Wisconsin School of Medicine and Public Health
Perry Pickhardt Professor of Radiology Chief of Gastrointestinal Imaging University of Wisconsin School of Medicine & Public Health