Intercultural and Global Health Issues Spring 2024


Created by the students enrolled in PHRM 48500
Compiled by C. Koh-Knox Sharp, PharmD, RPh; Clinical Associate Professor Teaching assistants: Jordan Keuneke, BSPS and Matthew Wolter, BSPS Purdue University College of Pharmacy
Powered by Bing
This Photo by Unknown Author is licensed under CC BY-NC
Table of contents Topic (author) Page Infectious diseases ........................................................................................................................................ 4 Public response to disease (Mary Ayer) 5 Protecting vulnerable populations (Ryan Lee) ..................................................................................................... 6 Escherichia coli (E. coli) infection (Athena Phuong) 7 Malaria (Dayanarah Gonzalez) ............................................................................................................................ 8 Tuberculosis (Kate Veltri) 9 Geriatric health 10 Assisted living (Sydney Gregory) ....................................................................................................................... 11 Cognitive diseases (Owen Blundall) 12 Health literacy (Vuving Long) ............................................................................................................................ 13 Chronic diseases (Maddy Ping) .......................................................................................................................... 14 Polypharmacy (Thomas Lee) ............................................................................................................................. 15 Women’s health .......................................................................................................................................... 16 Contraception (Vienna Place) 18 Menstrual health (Annie Liu) ............................................................................................................................. 19 Breast cancer (Owen Booth) ............................................................................................................................. 20 Rare diseases falsely attributed to mental health (Bailey Walker) .................................................................... 21 Women’s sexual wellness (Emily Gu) ................................................................................................................ 22 The impact of culture and traditions on global healthcare ........................................................................... 22 Healthcare systems (Stella Hart) ....................................................................................................................... 24 Medication adherence (Emily Randall) .............................................................................................................. 25 Trust in healthcare professionals (Eli Walker) ................................................................................................... 26 Customs affect dietary and healthcare habits (Chieh-Hsun Chou) .................................................................... 27 Mental health in different cultures (Sofia Lombardi) ........................................................................................ 28 Healthcare in a resource-limited environment ............................................................................................ 29 Educational (Tushar Sardesai) ........................................................................................................................... 30 Geographical (Anna McCoy) .............................................................................................................................. 31 Post-disaster (Allison Cilke) ............................................................................................................................... 32 Correctional facilities (Journey Johnson) ........................................................................................................... 33 Tourism and travel (Brynlee Walters) ................................................................................................................ 34 Health in the media ......................................................................................................................................... 36 Supplement industry (Youssef Morad) .............................................................................................................. 37 Drug marketing (Stuart James) .......................................................................................................................... 38 Medical misinformation (Beiyan Wang) ............................................................................................................ 39 Body image (Emily Cmarik) ................................................................................................................................ 40 Debate and discussion (Emma Simmons) .......................................................................................................... 41
Table of contents, continued Topic (author) Page Pediatrics: Issues and successes .................................................................................................................. 42 Genetic diseases and disorders (Riley Smith) 43 Drug development: limitations and challenges (Sriya Nagubandi) .................................................................... 44 Resilience in pediatrics (Thomas Joo) 45 Influence of family support on health (Kennist Williams) .................................................................................. 46 Terminal illnesses: Quality of care (Emily Davidson) 47 Underserved populations ............................................................................................................................ 48 Immigrant access to healthcare (Carter Smith) ................................................................................................. 49 Developing countries and access to medicine (Frehiwot Kebede) 48 Rural healthcare (Emmett Niemeyer) ................................................................................................................ 50 Implicit bias in the healthcare system (Anabela Djurovic-Topalovic) ................................................................ 51 Women’s healthcare (Emily Wood) ................................................................................................................... 52 Epidemiology .............................................................................................................................................. 53 Antimicrobial resistance (Maverick Tebbe) 54 Pandemic response (Carolina Kim) .................................................................................................................... 55 Climate change (Terrence Duckworth) .............................................................................................................. 56 Respiratory vaccines (Benny Yang) .................................................................................................................... 57 Hospital acquired infection (Jacob Paulaskas) ................................................................................................... 58 Health disparities ........................................................................................................................................ 59 Health literacy (James Kim) ............................................................................................................................... 60 Education (Annie Frazier) .................................................................................................................................. 61 Accessibility (Joseph Pham) ............................................................................................................................... 62 Affordability (Evelyn Zhang) .............................................................................................................................. 63 Demographics (Sammy Thomas) ....................................................................................................................... 64 Organ transplants ........................................................................................................................................ 65 Black market organ harvesting (Camryn Fulton) ............................................................................................... 66 Xenotransplantation (Sam King) ........................................................................................................................ 67 Transplant backlog (Benjamin Tseng) ................................................................................................................ 68 Cultures and religions (Cindy Phan) ................................................................................................................... 69 Legal versus illegal (Annie Zhao)........................................................................................................................ 70
Infectious Disease GROUP 1
Mary Ayer, Ryan Lee, Athena Phong, Dayanarah Gonzalez, & Kate Veltri
https://d2jx2rerrg6sh3.cloudfront.net/images/news/ImageForNews_704632_16450045989739523.jpg
In 2019 alone, 13.7 million people around the world have died from infectious diseases. Infectious diseases are transmitted through environmental factors but also through human to human transmission. From person to person, water and food sources, and other organisms, infectious diseases can put anyone at risk. This infection occurs when these germs enter the body and cause a reaction. Some infectious diseases are treatable, where others aren’t. Through this monograph, we explore various facets of infectious disease and howitimpactsourcommunitiesandsocietyasawhole.
References
1.GrayA,ShararaF.Globalandregionalsepsisandinfectioussyndromemortalityin...TheLancet.March2022.Accessed March28,2024.https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(22)00131-0/fulltext.
[InfectiousDisease,Spring2024]
1
Public Response to Disease
Background
Mary Ayer, BSPS Student
Public perception and response to disease widely shapes access to treatment, stigma around certain diseases,andoveralldiseasespread.Thepublicfigures,in conjunction with experts in the field, must know how to deliver education around relevant diseases to the public. This is just as important as immunologists knowing the diseasestateitself.
Global Issue
As seen both in the COVID-19 pandemic and the 1918 influenza epidemic, these diseases are highly transmissible across borders in our interconnected world. The major distinctions are made when it comes to public response or non-response to disease. With the 1918 epidemic, the disease started on US military bases, quickly spreading to civilians and across borders. The disease took the lives of millions, but some harm in this was mitigated by having strong initial messaging from local health boards, instructing the public to stay indoors, limitingthatspread.
Who is Effected?
The relationship between the public and health experts is most at play here. Their connectedness, or how rapidly the public can receive accurate health information they can trust, plays a vital role in how public attitudes towards the dangers of disease adapt over time.This trust is built and fostered over time, and relies on the public’s belief that health professionals they interact with have their best interests in mind. Within the COVID-19 pandemic, misinformation was spread rapidly due to changing messaging. This lead to a further breakdown of trust and the public not being able to react appropriately in many circumstances when itcametomakingandvaccines.

https://www.google.com/url?sa=i&url=https%3A%2F%2Fnews.usc.edu%2F1918-flu-pandemic-covid-1 9-future-david-sloane-usc%2F&psig=AOvVaw1ABR1it9vRyG9H_1Ei9P0R&ust=1712717215536000& source=images&cd=vfe&opi=89978449&ved=0CBIQjRxqFwoTCJCtz4OPtIUDFQAAAAAdAAAAAB AE
Solutions
IN just 2023, the US Government Accountability office released recommendations to be implemented to provide clearer information to the public, and increase preparedness for subsequent pandemics. It explicitly suggests having a strong public infrastructure and experts in medicine to monitor public health concerns as the arise or in the case of emerging disease. It also highlighted need for sustained funding for these programs and infrastructures, rather than short-term funding as was utilizedinCOVID-19responsefromtheUSgovernment.
Personal Opinion
I believe this breakdown of trust can be restored, by having increased transparency, especially duringnovelpandemicssuchasin1918with influenza and 2020 with covid. Providing that insight to the public and voicing that guidelines and policies can changeasweaspublichealthofficialslearnmoreabout the disease state and how to best respond as a collective.-M. Ayer References
USGovernmentAccountabilityOffice.Publichealthpreparedness:BuildingandmaintaininginfrastructurebeyondtheCOVID-19pandemic.PublicHealthPreparedness:BuildingandMaintainingInfrastructure beyondtheCOVID-19Pandemic|U.S.GAO.November7,2023.AccessedFebruary19,2024.https://www.gao.gov/products/gao-24-105891
SternAM,CetronMS,MarkelH.The1918-1919influenzapandemicintheUnitedStates:lessonslearnedandchallengesexposed.PublicHealthRep.2010;125Suppl3(Suppl3):6-8. doi:10.1177/00333549101250S303
Disease,Spring2024]
Navarro
eds.Influenzaencyclopedia.TheAmericanInfluenzaEpidemicof1918:ADigitalEncyclopedia.2012.AccessedFebruary19,2024.https://www.influenzaarchive.org/
JA,MarkelH,
[Infectious
2
Protecting Vulnerable Populations
Background
Ryan Lee, BSBP Student
Variations in environment, age, genetics, behavior, and many other factors result in certain groups of people beingmoresusceptibletodiseasesthanothers.Inaddition to these variations, people may also increase their risk of disease by how they choose to respond to public health emergencies. People who increase their risk of infection willthenputotherswhomaybemorecautiousatrisk.All inall,vulnerablepopulationsrepresentasmall,yetcrucial portionofthelargerissueofinfectiousdiseases.
Global Issue
Specific peoples may be more susceptible to disease than others.Forexample,immunocompromisedpeoplemaybe more susceptible to severe complications from relatively benign diseases. Smokers may be more at risk for cardiovascularandlungdiseases. In the case of a public health emergency, such as in the case of a pandemic, people who ignore safety precautions put others at risk by being a source of infection themselves.
Who is Effected?
Although it seems as if only certain people are classified as “vulnerable populations,” the groups may be much larger. For example, people who carry a disease may bring them from population to population. This then causes another group of people to be “vulnerable”tothedisease.

Source: Progress In Mind. Alzheimer’s Disease. Psychiatry and Neurology Research Center. 2019. https://progress.im/en/content/which-populations-are-most-vulnerable-alzheimer%E2% 80%99s-disease-and-why
Solutions
The main solution in protecting vulnerable individuals is increased awareness. This may include increased health literacy taught by schools and a streamlined method to access to information and procedures during health emergency events. This in turn, helps to keep the public informed and allows people to make better educated decisionsinordertominimizeriskofinfection.
Personal Opinion
Methods to minimize risk of infection are well known and in place during times of public health emergencies. However, some sources of information do not put out reliable information to the public. Many of these sources spread misinformation to push a specific agenda; typically political. Such sources should be held accountableforincreasingtheriskofinfectionforthose who listen to them, as well as to the people who they wouldcomeintocontactwith.
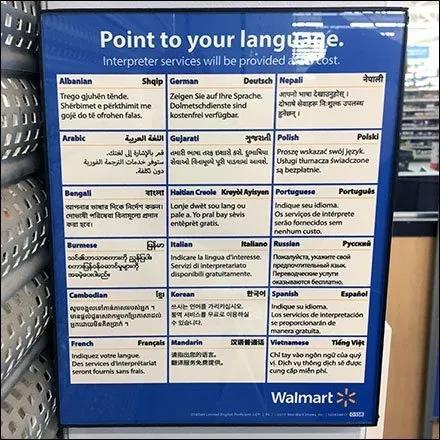
References
WangY,McKeeM,TorbicaAetal.SystematicLiteratureReviewontheSpreadofHealth-relatedMisinformationon Social Media.Soc.Sci.Med.2019;240:112552https://doi.org/10.1016/j.socscimed.2019.112552
OfficeoftheSurgeonGeneral(OSG).ConfrontingHealthMisinformation:TheU.S.SurgeonGeneral’sAdvisoryon BuildingaHealthyInformationEnvironment[Internet].Washington(DC):USDepartmentofHealthandHumanServices; 2021.https://www.ncbi.nlm.nih.gov/books/NBK572166/
[InfectiousDisease,Spring2024]
3
Escherichia Coli (E. Coli) Infection
Background
Athena Phuong, BSPS Student
Escherichiacoli,suchasE.coliO157:H7,isa typeofbacteriumresponsibleforinfectionstransmitted throughvariousmeansincludingcontaminatedfoodor drink,directcontactwithinfectedanimals, person-to-personinteractions,andexposuretountreated water.Indevelopingcountries,theprevalenceofE.coli infectionsisnotablyhigh,primarilyduetoinsufficient sanitation,lackofcleanwater,andinadequatefoodsafety measures.Theseconditionsexacerbatethebacterium's negativeimpacts,significantlyaffectingcommunity healthoutcomesandcontributingtoacycleofpoverty anddisease.
Global Issue
AccordingtotheFDA,annuallyintheU.S.,E. coliresultsinaround265,000illnessesand100deaths, with40%duetotheE.coliO157:H7strainandthe remaining60%fromothernon-O157:H7STECstrains andthatisjusttheU.S.afirstworldcountry..Regions withsignificantE.ColioutbreaksbesidestheU.S.are EuropeandAsia.AccordingtotheWHO,newglobal estimatesrevealthatnearlyoneintenindividualsbecome illannuallyduetoconsumingcontaminatedfood,leading toapproximately420,000deaths,withE.coliinfections contributingsignificantlytothistoll.Imagine3rdworld countrieswhodonothavetheeducation/awarenessofthis bacteriathatcouldcausethedeathofthemasseswhennot treatedproperly.Especiallywhenthesecountriesare often havingafoodshortagewithnowaystorefrigerateor simplynotwantingtowastefoodthathasbeenspoiled.
Who is Effected?
Individuals across all age groups can contract E. Coli infections, but children and the elderly may experience more severe effects due to weather immune systems. Annually, this disease claims the lives of millionsofchildrenandelderlyindividuals.
References
EscherichiaColibacterium
https://www.independent.co.uk/life-style/health-and-families/e-coli-bacteriasymptoms-infection-egypt-outbreak-treatment-explained-a8525486.html
Solutions
To combat E. Coli infections, solutions include enhancing surveillance of infection sources, educating on proper handling of raw salads and vegetables, improving traceability and labeling of cheeses, salads, and vegetables, advising on safety during educational farm visits, and implementing measures to safeguard private water supplies from contamination. While also spreading awareness for example, the CDC is sharing awareness to the subject and ways to prevent an outbreak to the masses through free and easy to access reliable internet sources i.e.www.cdc.gov.
Personal Opinion
E.coliinfectionscanbequitealarmingdueto theirpotentialseverityandtheeasewithwhichtheycan spread,particularlythroughcontaminatedfoodand water.Thefactthattheycanrangefrommild gastrointestinaldiscomforttolife-threatening conditionslikehemolyticuremicsyndromeunderscores theimportanceofrigoroushygieneandfoodsafety practices.However,withpropereducationon preventionandtimelyaccesstohealthcare, Ibelieve thattherisksassociatedwithE.coliinfectionscanbe significantlymitigated.~APhuong
NCDPH:E.coli.epi.dph.ncdhhs.gov.PublishedDecember16,2019.https://epi.dph.ncdhhs.gov/cd/diseases/ecoli.html https://www.independent.co.uk/life-style/health-and-families/e-coli-bacteria-symptoms-infection-egypt-outbreak-treatment-explained-a8525486.html.PublishedSeptember6,2018. ChristieB.Visitstothecountryposebiggestriskof E coli infection. BMJ : British Medical Journal.2001;323(7304):70.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1172660/ WHO.WHO’sfirsteverglobalestimatesoffoodbornediseasesfindchildrenunder5accountforalmostonethirdofdeaths.www.who.int.PublishedDecember3,2015. https://www.who.int/news/item/03-12-2015-who-s-first-ever-global-estimates-of-foodborne-diseases-find-children-under-5-account-for-almost-one-third-of-deaths BarrS.Ecoli:Whatisthebacteriaandwhatarethesymptomsofinfection? The Independent
[InfectiousDisease,Spring2024]
4
Background
Malaria
Dayanarah Gonzalez, BSPS Student
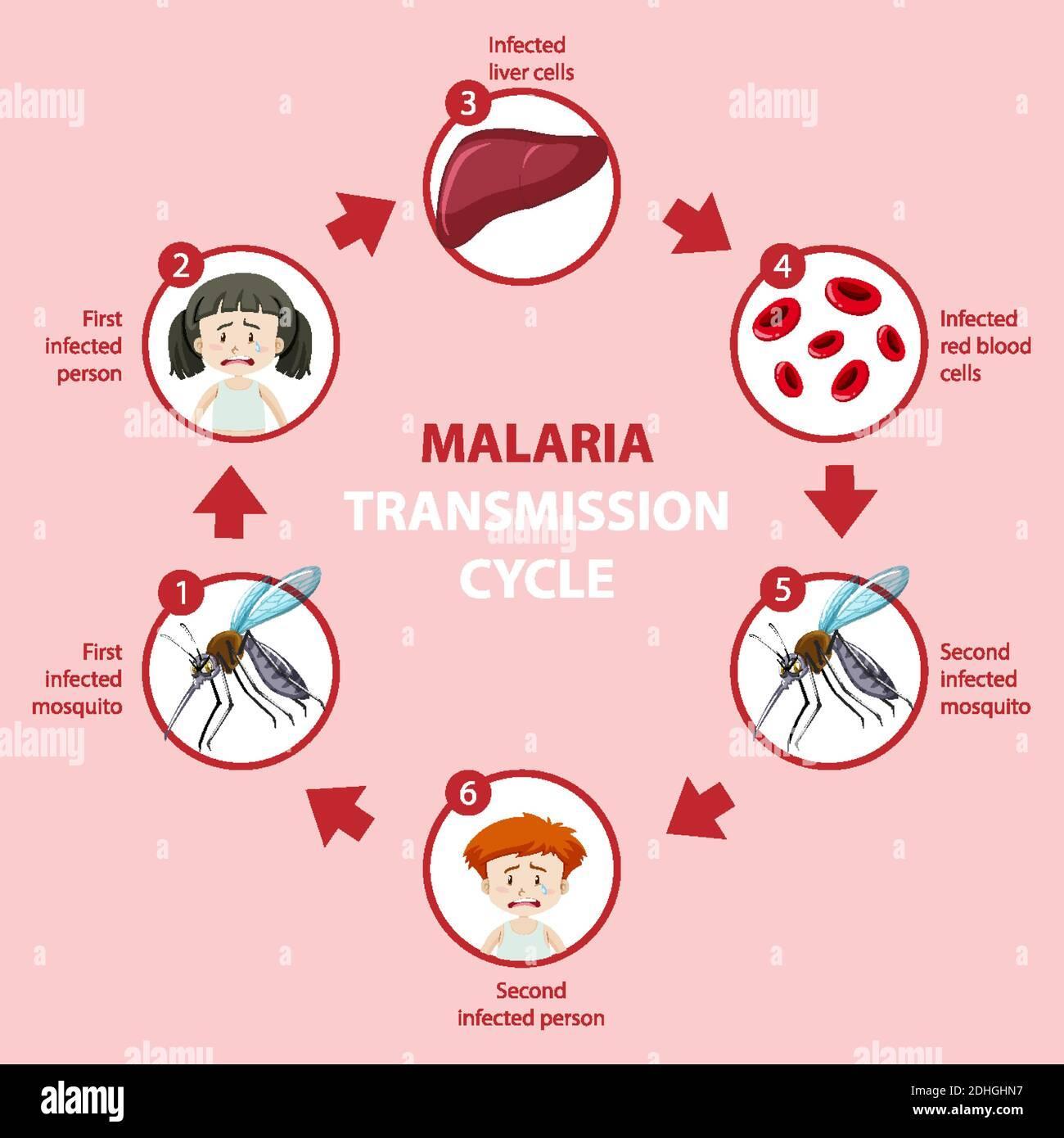
Malariaisaseriousdiseasethatiscausedbya parasitethatinfectsacertaintypeofmosquitocalled Anopheles.Peoplecontractmalariafrombitesofinfected mosquitoes.Malariacanonlybecontractedfrom mosquitoes,andnotfromotherinfectedhumans.Malaria canbeadeadlydiseaseifnotdiagnosedortreated. Seekingtreatmentformalariacanpreventsevereillness andevendeath.Thereareabout20,000casesofmalaria peryear.
Global Issue
MalariaiscurrentlyaprobleminAfrica,Asia,and CentralandSouthAfrica.Thereareabout2,000casesa yearintheUS.Mostofthesecasesareofpeoplewho traveledtoareaswheremalariaisprevalent.Therearea fewcasesthathavebeenreportedinFloridaandTexas. Malariaisanurgentpublichealthpriority. Between2021 and2022malariacasesincreasedfrom244millionto249 million.In2022Africawashometoabout94%ofthe malariacases.Thecostoftreatmentsandpreventionfor malariaarequiteexpensivewhichreducestheaccessto help.AccordingtoUnicef, “Today,nearlyhalfofthe world'spopulation,mostofwhomliveinsub-Saharan Africa,areatriskfordevelopingmalariaandfacingits economicchallenges.”
Who is Effected?
Thepeoplethatareaffectedbymalariaare infants,childrenunder5years,pregnantwomen, travelersandpeoplewithHIVandAIDS.Thechildren inAfricaarethemostsusceptibletogettingmalariadue tonothavingdevelopedimmunitytomalaria.In2022 78%ofmalariadeathswerereportedtobechildren undertheageof5.
References
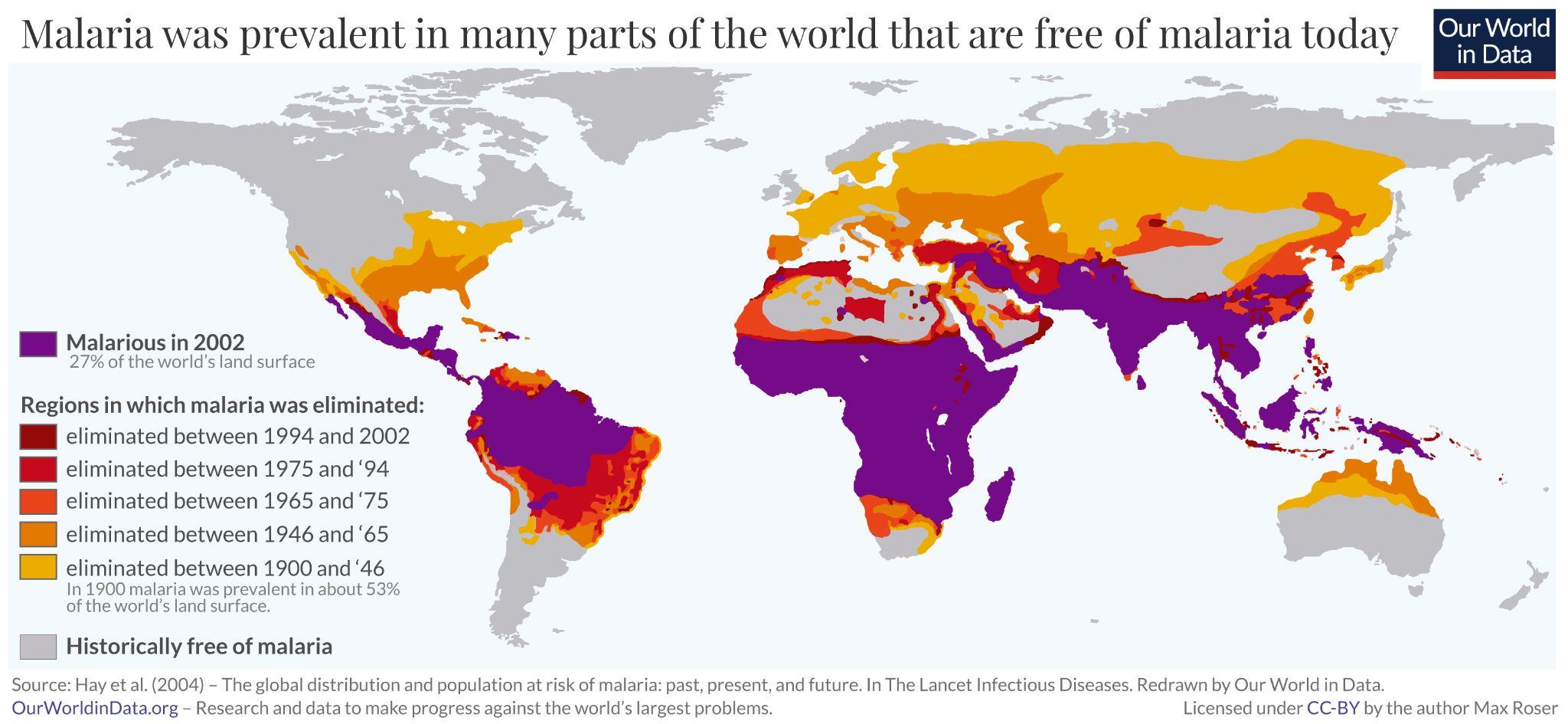
https://ourworldindata.org/malaria
Solutions
Therearetwodifferentmalariamedicationsthat arecurrentlyusedtotreatandpreventmalaria.These medicationstendtobequitecostlyandarenoteasily accessible.TherearealsovaccinesforMalariabutitis typicallyrecommendedforyoungerchildren.Thereare alsotwodifferenttypesofinterventionsthatareused calledinsecticide-treatednets(ITNs)andindoorresidual spraying(IRS).
Personal Opinion
Africancountriesarethemostaffecteddueto theirlackofsocioeconomics.Theydonothaveaccess totheresourcesneededtotreatmalaria,sotheyneedto maketheseresourcesmoreaccessibletohelpprevent andtreatmalaria.Thereareenoughresourcesthatcanbe providedtounder privilegedcountries. Ibelievethatwecan lowermalariaratesif weprovidetheresources ~DG.
https://www.alamy.com/m alaria-transmission-cycleand-symptom-information -infographic-illustration-i mage389442403.html
PreventionCCforDCand.CDC-Malaria-AboutMalaria.www.cdc.gov.PublishedFebruary14,2024.AccessedMarch27, 2024.https://www.cdc.gov/malaria/about/index.html#:~:text=The%20U.S.%20reports%20about%202%2C000 Malaria.WorldHealthOrganization.PublishedDecember4,2023.https://www.who.int/news-room/fact-sheets/detail/malaria
MalariainAfrica.UNICEFDATA. https://data.unicef.org/topic/child-health/malaria/#:~:text=Malaria%20is%20an%20urgent%20public
[InfectiousDisease,Spring2024]
5
TUBERCULOSIS
Kate Veltri, BSBP Student
Background
Tuberculosis, or TB, is caused by a bacterium called mycobacterium found in airborne droplets. Transmitted from person to person, TB persists as one ofthemostwidespreadanddeadlyinfectiousdiseasesto date. This disease is prevalent in many developing countries around the world. Due to its detrimental effects,thehighlycontagiousdiseasenegatively impacts many.
Global Issue
In 1993, the World Health Organization declared TB as a public health emergency to prepare countries for the disease. In 2010, 7% of all deaths were due to TB in developing countries. In 2022, tuberculosis was the second most deadly infectious disease, killing a total of 1.3 million people. From 1993 to 2022, almost 30 years since the emergency was declared, numbers are still high in the transmission rates of TB. Projected for 2023, over 10 million people will contact TB, while only 6 million will receive treatment. In 1981, the BCG vaccine approvedbytheFDA.Thisvaccinehasshownprotective effects after being administers. However, these effects canonlyoccurifthereisaccesstothedrug.
Who is Effected?
Anyone can be affected, especially those with weak immune systems and chronic conditions. When someone with active TB sneezes, speaks or coughs, then others nearby breathe in the mycobacterium. MostTBdeathsareduetolackofproperhealthcareor treatment options. If not treated, there are long lasting damaging effects on the lung that can occur. TB can begin to cause infections to other parts of the body. Including the bones, spine and lymph glands. Research has shown those who leave TB untreated, 7 years are takenoffoftheirlifeexpectancy.
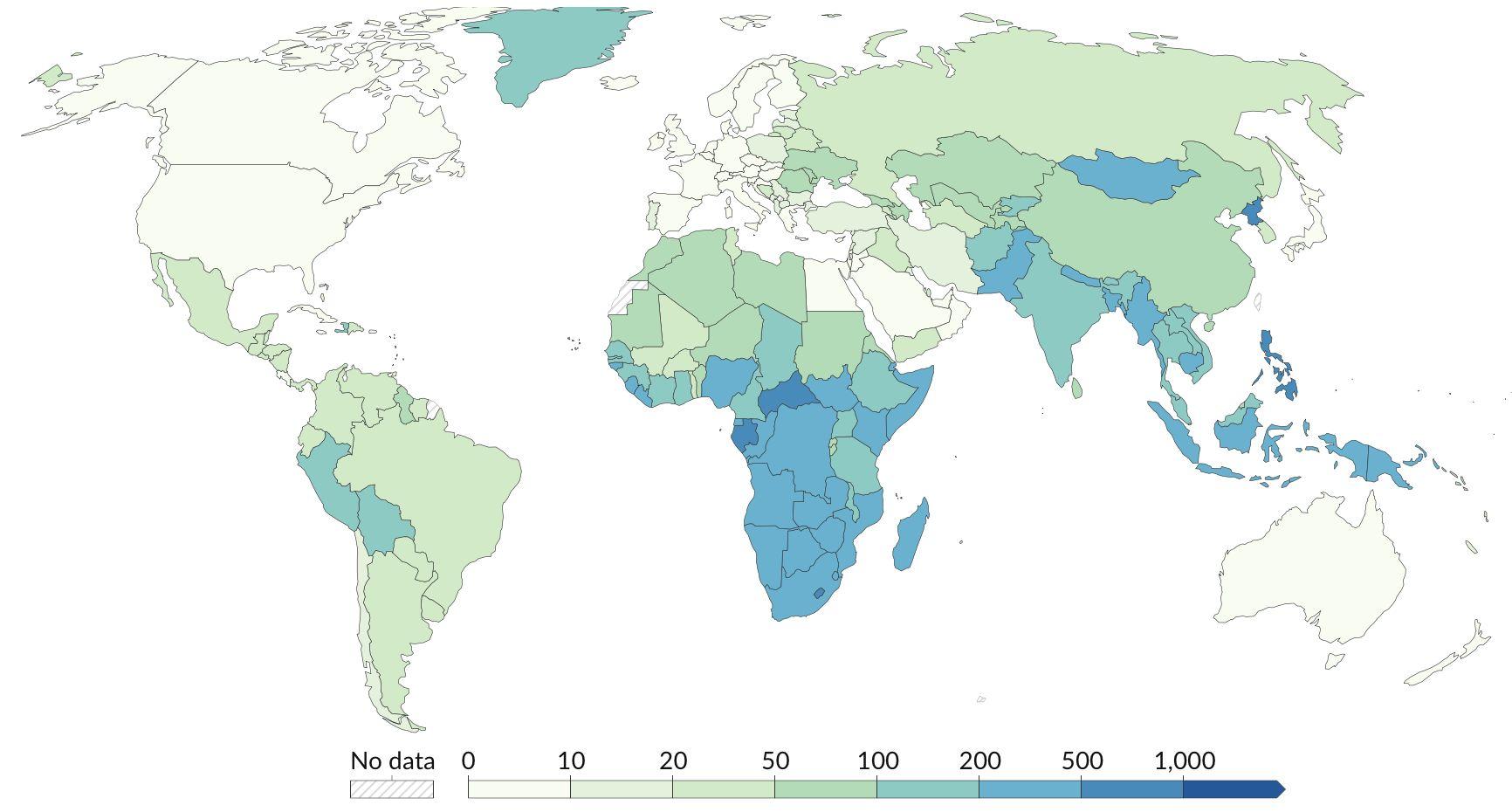
MapofTuberculosisCasesin2022per100,000People OurWorldInData.org/tuberculosis
Solutions
Preventionofthediseasethroughvaccination andlimitingspreadofoutbreaksmustoccur.More specifically,preventioncanbedonethroughgood ventilation,hygieneandeducation.TBishighly treatablewhengivenaccesstomedicationand adequatehealthcaretreatment.Patientscanbecured throughmedicationssuchasrifampin,isoniazid, pyrazinamideandethambutol.Ifthesemedicationsare abletobeprovidedandthecorrectregimeistaken, thenTBishighlycurable.
Personal Opinion References
Tuberculosiscanbeeffectivelytreatedwithmedical intervention. The majority of the reason for why transmission rates are so high, especially in developing countries, is due to the access and cost of drugs. Drugs to treat TB range from a 30%-400% markup cost from production. Drug companies need to lower the cost of their drugs for the treatment of this infectious disease. Lowering the cost of the drug, by even a couple of dollars, would save thousands of lives around the world. This infectious disease still being prevalent today is not from lack of scientific evidence. Instead, it is driven by drug companies priorizating money instead of the lives of patients. ~ K Veltri
CentersforDiseaseControlandPrevention.Tuberculosis(TB).CentersforDiseaseControlandPrevention.PublishedAugust29, 2023.https://www.cdc.gov/tb/default.htm
Opinion|Thedeadliestinfectiousdiseaseisn’tascienceproblem.It’samoneyproblem. Washington Post. https://www.washingtonpost.com/opinions/2024/03/21/tuberculosis-deadliest-curable-disease-tests-john-green/.PublishedMarch23, 2024.
WorldHealthOrganization.Tuberculosis.www.who.int.Published2020.https://www.who.int/health-topics/tuberculosis#tab=tab
[InfectiousDisease,Spring2024] 6
Geriatric Health
Spring2024
Background
Geriatric healthcare pertains to the care of elderly patients, an ever growing issue with the growth of the elderly(65+) population in developed nations. In the United States there are 58 million people in this population(17%) which is predicted to grow to 22% by 2040. These patients have special needs as they are more affected by chronic illnesses, certain diseases, and their unique living conditions.
Polypharmacy
A common problem for seniors is the usage of multiple drugs to treat various health issues that often come with old age. Having to manage a variety of drugs fordifferentdiseasescanintroduceanew set of problems, like dealing with side effects from medications, remembering when and how to take them, or knowing how one may interact with the others whenbeingtakensimultaneously.
Health Literacy
Health literacy has been documented to vary betweendifferentdemographicgroupsinthe UnitedStates,atleast.Theredoesn’tseemto be precise information on health literacy differences between specific cultural groups. However health outcomes, especially for geriatric patients, appear to be affected by thepatient’shealthliteracy.
Assisted Living
Assisted living has become an increasinglypopularwaytoprovidecare forelderlypatientswhomaynolonger be able to completely care for themselves or don’t have anyone to completelycareforthem.Assistedliving playsalargepartingeriatrichealth,as it is a very important decision that affects the elderly’s health in many ways.
Chronic Diseases
Geriatric patients have more difficulties completing daily activities because of factors such as cognitive decline, frailness, living alone, and more. Managing chronic diseases in elderly patients can be difficult because of these factors. This issue can be managed, but it also can become a problem for elderly patients who don'thavethesupporttheyneedtosuccessfully adheretoallmedicationandtreatments.
Cognitive diseases
Alzheimer’s disease is one of the most prevalent cognitive diseases in geriatric patients, accounting for 60-70% of dementia cases. However, the beliefs surrounding Alzheimer’s disease vary between cultures, with some viewing it as a normal part of the aging process. Sometimes these differences in cultural beliefs can lead to differences in the quality of care received by patients with Alzheimer’s, or could lead to differences in how family members or caregivers treat them. Additionally, the relationship between ethnicity and biomarkers in Alzheimer’s needs further exploration for better characterization.
Geriatric Health, Spring 2024 7
ASSISTEDLIVING
Sydney Gregory - BSPS Student
WHATISASSISTEDLIVING?
Assisted living is defined as “Housing for elderly or disabled people that provides nursing care, housekeeping, and prepared meals as needed.”
WHOISATAFFECTED?
The people who are affected by assisted living are typically the geriatric population (65+). This population is one that is usually in need of extra care or assistance in day to day activities
STATISTICS
The US has 30,600 assisted living communities providing space for almost 1.2 million people
China has 4x the population of the US and only has 10,000 more assisted living facilities
ASSISTEDLIVINGISSUES
Issue: Mental Health
Isolation in assisted living can lead to anxiety, depression, and memory impairment
GLOBAL ISSUES
In Asian countries, such as Taiwan, Thailand, and Singapore, it is more widely accepted that the elderly are the responsibility of their children and younger generations. Due to this, intergenerational living is common in these countries, meaning the elderly live with their children and are primarily cared for by their family. Often though, it can be a burden on families to constantly take care of their elderly, so other alternatives are becoming increasingly popular.
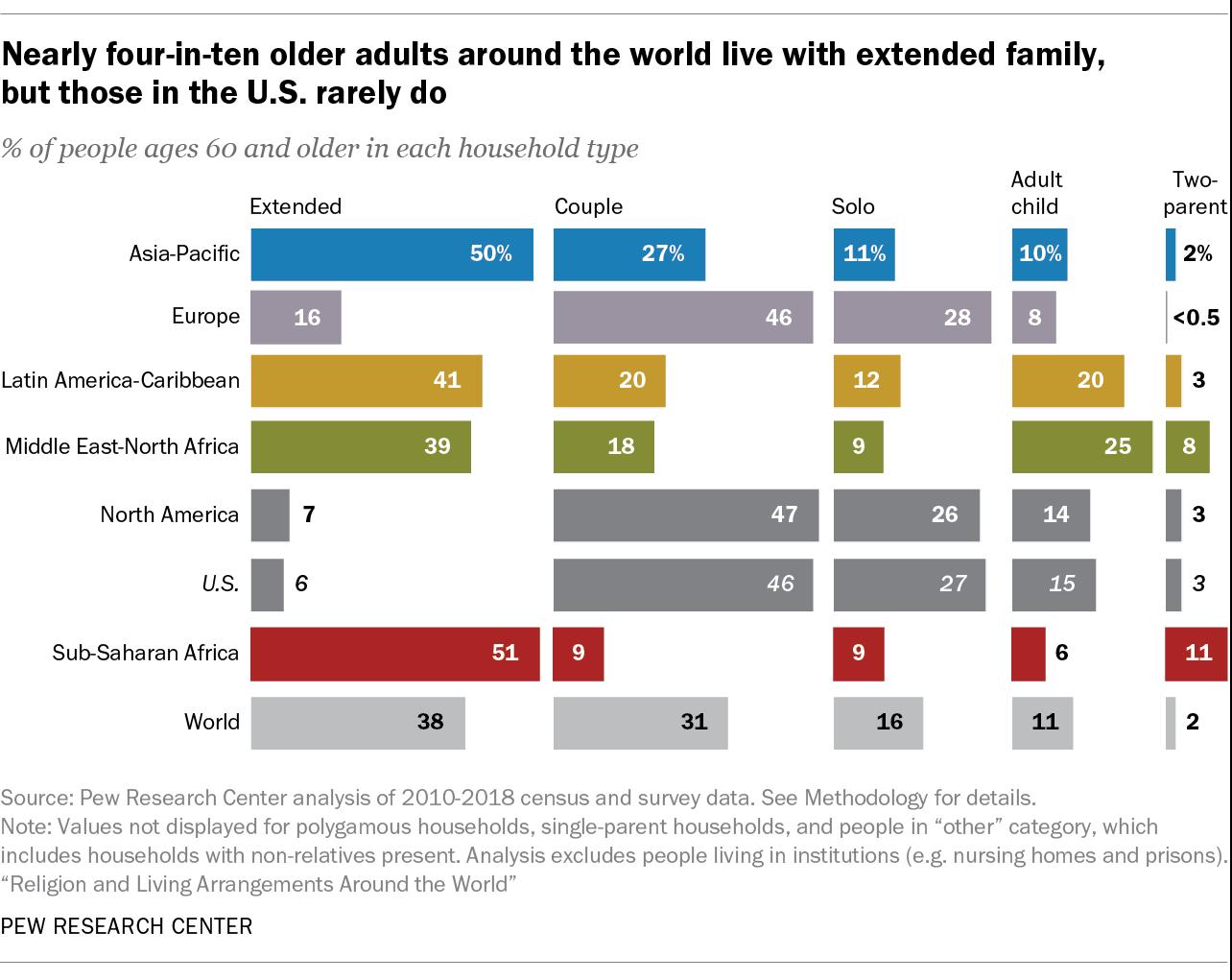
www.pewresearch.org/short-reads/2020/03/10/older-people-are-
Assisted living can worsen dementia, Alzeheimer’s, and generally cause cognitive decline
Solution:
Nursing homes combat cognitive decline by planning regular physical and social activites
The cost of assisted living continues to rise and can be unaffordable for geriatric patients who need it Issue: Cost
PERSONAL OPINION

www.aplaceformom.com/caregiver-resources/articles/cost-of-
In my personal/professional opinion, I think assisted living facilities can be a good thing, if family stays involved with those living there, but I would personally prefer at-home and familial care ( S Gregory). I have experienced this within my own family, where we had one family member be the primary caretaker of our grandparent. Later on, when it became too much for one person to care for them, they were moved to an assisted living facility Between the two, I think that their health was better when they were taken care of at home, just because of the familiarity, freedom, and routine.
References:
Geriatric Health, Spring 2024
more-likely-to-live-alone-in-the-u-s-than-elsewhere-in-the-world/
assisted-living Best Practices for Promoting Emotional Well-Being in Nursing Home Residents https://www ahrq gov/sites/default/files/wysiwyg/nursing-home/promoting-emotional-wellbeing pdf The Not-so-Novel Concept of Elderly Homes in Asia GLOBAL HEALTH AGING Published February 23, 2016 Accessed April 9, 2024. https://globalhealthaging.org/2016/02/23/the-not-so-novel-concept-of-elderly-homes-inasia/#:
:text=Elderly%20residential%20facilities%2C%20such%20as
COGNITIVE DISEASES
Owen Blundall - BSPS Student
What are cognitive diseases?
Cognitive diseases are among some of the most common health issues people face as they get older, with dementia being the most common cognitive disease among the geriatric population. About 10 million new cases of dementia are diagnosed each year, which amounts to a new diagnosis nearly every 3 seconds. Cognitive diseases cause a large strain on both the individual and their families and friends, as these people are likely to become caregivers if the disease progresses far enough in the individual. Cognitive diseases also cause a large strain on the healthcare system, with an estimated spending of over $300 billion each year in treating Alzheimer’s and other dementia cases in the United States Alone.
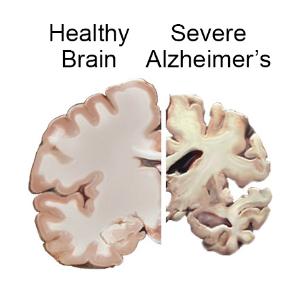
Alzheimer’s Disease
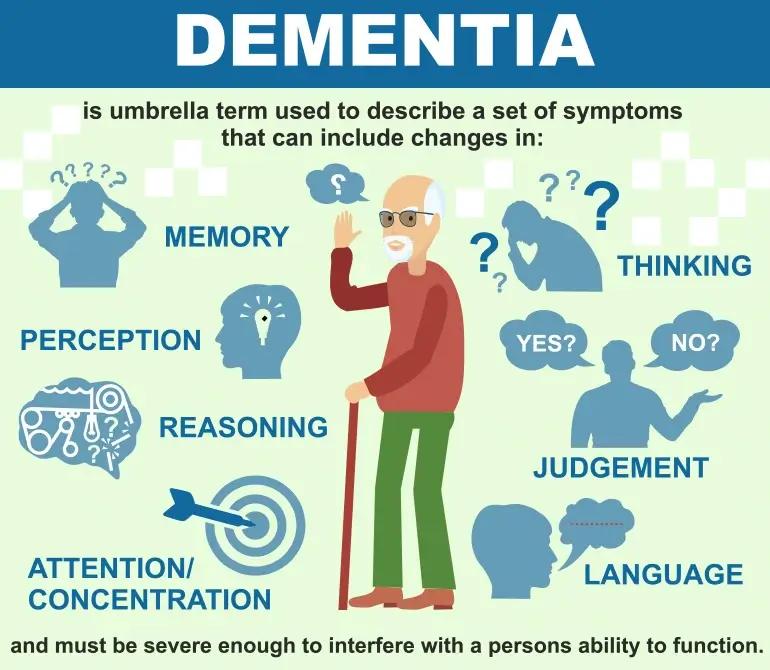
https://www.careinsurance.com/blog/health-insurance-articles/what-is-dementia-know-its-types-warning-signs-and-treatment
Alzheimer’s disease is the most common cause of dementia in older people, accounting for 60-70% of all dementia cases. Alzheimer’s disease is a progressive, neurodegenerative disease which causes memory problems, mood issues, disorientation, and behavioral issues. These symptoms are currently believed to arise due to the buildup of of amyloid and tau proteins in the brain, leading to plaque deposits and eventually shrinking the brain. Our current understanding of Alzheimer’s disease is somewhat limited. However, there appears to be some link between a person’s genetics and Alzheimer’s, with different ethnicities being diagnosed with Alzheimer’s at drastically different rates. This would suggest some kind of genetic component to the disease, despite many cases of Alzheimer’s not being inherited.
Issues with Alzheimer’s Genetics
There is growing evidence to support the idea of variation in the progression of Alzheimer’s disease and how badly a person’s cognition is affected based on their ethnicity. There is also evidence supporting a higher incidence rate of Alzheimer’s disease among certain populations. For example, African Americans have a twofold greater overall presence of the disease compared to other groups. Some of the biomarkers related to Alzheimer’s are mutations in apolipoprotein E and the presence of amyloid and tau plaques. When it comes to these biomarkers, Caucasians generally have a higher severity of amyloid and tau plaques, while African Americans have a higher prevalence of apolipoprotein E4, a variant associated with development of Alzheimer’s. However, there is conflicting data on these biomarkers in different populations, as well as conflicting data on how they impact the progression and prevalence of Alzheimer’s. More research needs to be conducted so that the genetic basis of Alzheimer’s disease can be further elucidated, and so that populations who may potentially be more at risk can get better access to care before the disease progresses too far.
References
https://www.nia.nih.gov/health/alzheimers-and-
Personal Opinion
My personal opinion on this topic is that it needs to be studied much more so that a consensus can be met (~O. Blundall). While I was researching this topic, the most useful paper I found summarized the results from many different studies on Alzheimer’s in different populations, and the results of these different studies were inconsistent. Some studies seemed to show strong evidence of differences between disease outcome, prevalence, and biomarkers in different ethnicities, while some studies showed no difference in biomarkers. I think more studies need to be conducted in this area, especially in regards to underrepresented populations in this field of research, such as African Americans and Hispanics.
Rosselli M, Uribe IV, Ahne E, Shihadeh L. Culture, Ethnicity, and Level of Education in Alzheimer's Disease. Neurotherapeutics. 2022;19(1):26-54. doi:10.1007/s13311-022-01193-z Gray HL, Jimenez DE, Cucciare MA, Tong HQ, Gallagher-Thompson D. Ethnic differences in beliefs regarding Alzheimer disease among dementia family caregivers. Am J Geriatr Psychiatry. 2009;17(11):925-933. doi:10.1097/JGP.0b013e3181ad4f3c 9
Geriatric Health, Spring 2024
dementia/alzheimers-disease-fact-sheet
Health Literacy Long Vuving - PharmD Student
What is Health Literacy?
The Centers for Disease Control and Prevention define personal health literacy as “the degree to which individuals have the ability to find, understand, and use information and services to inform healthrelated decisions and actions for themselves and others.”
Why does it matter?
In a study by Berkman and colleagues, lower health literacy is strongly associated with a number of negative health factors which include but are not limited to more hospitalizations, higher health care costs, and higher mortality.
Health Literacy and Geriatrics
Health literacy is of particular importance to the geriatric population, 65 and older, as this population is at greater risk of health issues such as chronic diseases. In addition, table D27 in the report by Kutner and colleagues states that adults above the age of 65 are the population with the lowest health literacy. Furthermore, the average for adults above 65 is significantly farther from the other age groups relative to one another.
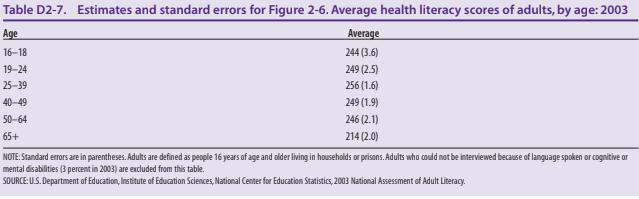
Health Literacy and Ethnicity in the U.S
Although there are no particular categories for culture, race and ethnicity can be used as a sort of general proxy in this regard. Particularly noteworthy results in table D2-5 are that black and hispanic subjects have lower health literacy levels compared to whites. Interestingly, Asians/Pacific Islanders have a higher percentage of people in the below basic level as well as the proficient level compared to whites. While these disparities can reflect culture, they can also be affected by other complex factors such as socioeconomic status and language barriers. The report does state that on average, people that have English as a first language have higher health literacy rates. So although these disparities have complex causes, it is very much an issue that should be addressed.
Global Considerations
The study by Sántha found that marital status had a strong correlation with health literacy by data from Poland and Ghana. Additionally, the study found that Hungarian mothers consumed more health related media as they got older. While this does not necessarily indicate an increase in health literacy, it might reflect a cultural difference that affects health literacy. Health literacy was confirmed to have a positive relationship with quality of life by a study in Tehran by Aryankhesal and colleagues.

References
Personal Opinion
After doing this research, I believe that something important to address is that health literacy often focuses on personal health literacy. Another aspect of health literacy is organization health literacy. This is critical because organizations can play a big role in dispensing information and organizational health literacy does factor into how an organization presents data. As such, increased organization health literacy can greatly improve overall health literacy. Examples of this include changing complex medical terms such as hypertension to simpler patient friendly terms such as high blood pressure. Other important methods to incorporate more cultures is to not only provide a translation but also provide proper cultural context. So although it is important to improve individual health literacy, improving organizational health literacy can provide effective and quick results. (~Long Vuving, PharmD)
Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. (2011) Ann Intern Med 155(2): 97–107.
Chesser AK, Keene Woods N, Smothers K, Rogers N. Health Literacy and Older Adults: A Systematic Review. Gerontol Geriatr Med. 2016;2:2333721416630492. Published 2016 Mar 15. doi:10.1177/2333721416630492
Kutner, M., Greenberg, E., Jin, Y., and Paulsen, C. (2006). The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006–483). U.S. Department of Education. Washington, DC: National Center for Education Statistics
What is health literacy? Centers for Disease Control and Prevention. July 11, 2023. Accessed March 15, 2024. https://www.cdc.gov/healthliteracy/learn/index.html.
Geriatric Health, Spring
10
2024
Chronic Diseases Maddy Ping - PharmD Student
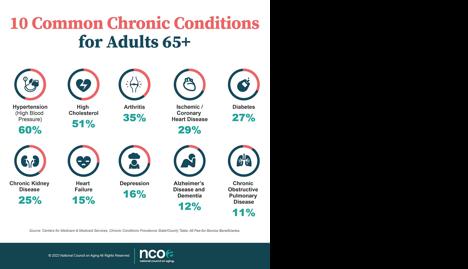
ChronicDiseasesinGeriatricPatients
Chronic disease is broadly defined as a condition that lasts 1 year or more, and/or requires medical attention or limits activities of daily living. According to studies, it is estimated that about 80%-90% of the geriatric population have at least one chronic condition or illness (chances increasing with age).
ManagementofChronicDiseasesin GeriatricPatients
Cultural Impact in Care of Elderly
“Western cultures have traditionally been labeled as ageist societies that undervalue their older adult populations. Eastern cultures are recognized for their more accepting view of older adults, placing them on a pedestal of wisdom and respect” according to a study from Colorado University. This has been shown to have an impact on the management of chronic disease in geriatric patients. In more Eastern cultures, it is more typical that a family member will become a caregiver but in Western cultures, it is more likely that a geriatric family member will be provided a primary caregiver. Factors such as a cultural diet can also heavily influence the overall health of a person over time and can be a contributing factor to chronic diseases in older age. These different cultures need to be respected to provide the best care possible for geriatric patients. Cultural understanding between physicians and patients will improve adherence, patient care, and clinical outcomes.
With age, the likelihood of having to manage a chronic disease increases significantly. Medication management, therapies, doctor appointments, patient caregivers, money, and more are examples of responsibilities that may come with a geriatric patient who has to manage a chronic disease. There are resources available to provide assistance and guidance for how to successfully manage chronic disease in geriatric patients. CDC National Center for Chronic Disease Prevention and Health Promotion is an organization that aims to improve the health of older adults.
unlimitedcarecottages.com/blog/helpful-information-for-family-members/elderlyforgetting-medication-5-tips-for-helping-elderly-patients-take-medications/
Personal Opinion
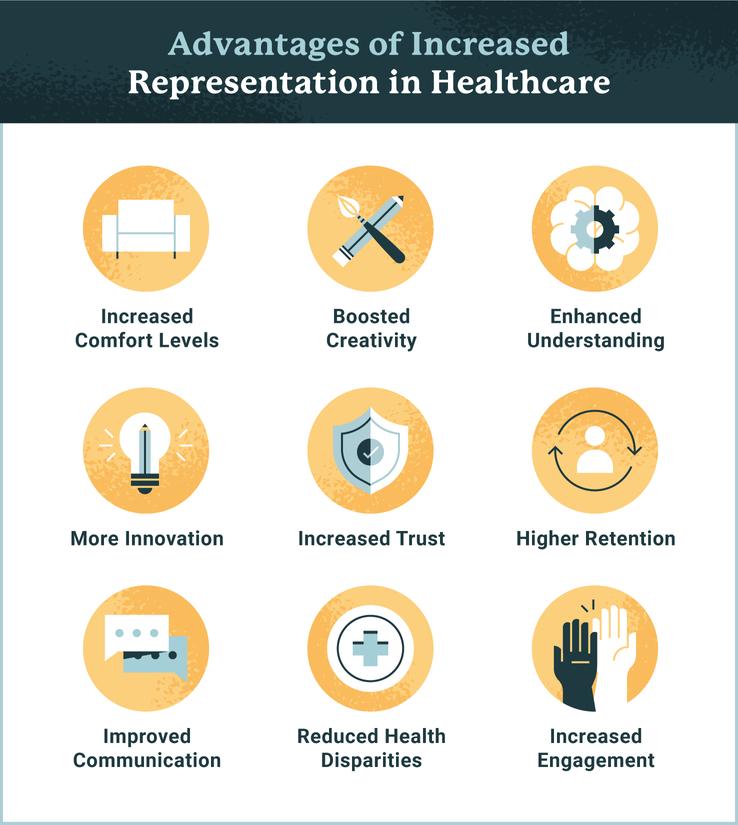
My personal opinion on Chronic conditions in geriatric patients is that, although there has been a significant increase in the percentage of geriatric patients with a chronic condition, I believe that overall there is adequate care and resources available to make proper and successful management possible (~M. Ping). There is a link between culture and health outcomes, I believe that as long as that this difference should always be respected. I believe diversity is important in a healthcare team and having diversity can lead to better overall treatment for not just geriatric patients but all patients.
Geriatric Health, Spring 2024 www.ncoa.org/article/the-top-10-most-common-chronicconditions-in-older-adults
www.usa.edu/blog/diversity-in-healthcare/ References Lambert S, Loban E, Li J, et al. Chronic Illness Management in Culturally and Linguistically Diverse Patients: Exploring the Needs, Access, and Understanding of Information. Qual Health Res. 2021;31(13):2426-2439. doi:10.1177/10497323211040769 Healthy Aging Team. The National Council on Aging. www.ncoa.org. Published August 31, 2023. https://www.ncoa.org/article/the-top10-most-common-chronic-conditions-in-older-adults 11
Polypharmacy
Thomas Lee - BSPS Student
What is Polypharmacy?
The definition of polypharmacy may vary but it most commonly refers to the concurrent usage of multiple medications, and is often associated with negative effects for those practicing it. Some people that practice polypharmacy may have to take multiple medications to treat a condition, or have multiple conditions that they take medications for.
Who’s at Risk?
Polypharmacy is most prevalent amongst people over the age of 65 who have a higher rate of chronic illnesses that often results in the prescription of multiple medications. Some younger people may also practice polypharmacy too, if they have multiple chronic conditions that each require medication to treat.
Global Issues with Polypharmacy
Problems with polypharmacy for elderly people occur around the world in countries with developed healthcare systems. Studies done in countries in the regions of Europe, North America, Asia, Oceania, and South America indicate problems related to polypharmacy amongst elderly patients to varying degrees but most prominently in Oceania and in developed countries.
References
Problems with Polypharmacy
Polypharmacy is considered undesirable due to the additional layer of risk that comes with heavy usage of different prescription drugs, with side effects and unintentional drug interactions compounded by multiple prescriptions being a main concern. Due to the nature of the main population affected by polypharmacy, polypharmacy may also increase the difficulty of managing medications, as having to regularly refill multiple prescriptions and remembering when and how to take them can be troublesome, possibly leading to problems with treating illnesses.
Possible Solutions?
Polypharmacy is often caused by issues related to getting regular access to medical consultation and health education about what drugs are being taken. Some potential solutions to lessen the effects of polypharmacy include increasing communication between health professionals for a patient as well as overall reduction of prescribed medication where possible. Additionally, consultation of a list called Beers’ Criteria by pharmacists and doctors, which contains medications potentially harmful for people older than 65, can help.
Geriatrics Society. 2014;62(12):2261-2272. doi:https://doi.org/10.1111/jgs.13153 Polypharmacy in Adults 60 and Older. www.hopkinsmedicine.org. Published December 14, 2023. https://www.hopkinsmedicine.org/health/wellness-and-prevention/polypharmacy-in-adults-60-andolder#:~:text=People%20over%2060%2C%20who%20may www.istockphoto.com/vector/pill-organizer-filled-with-tablets-and-capsules-for-each-day-of-the-week-weeklygm1497094507-519569786
Personal Opinion
Polypharmacy is a unique issue in pharmacy as it occurs because of an overabundance of medication rather than a lack of it, unlike some other issues. It is also a complex problem, as reducing the medications someone needs to take without diminishing their treatment is not always a possibility. Stronger diligence from healthcare professionals when it comes to elderly patients, however, can still have a large impact on reducing effects from polypharmacy. By cutting out unnecessary medications and ensuring education about them to patients, negative effects can be mitigated. - (T. Lee)
Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK. Health Outcomes Associated with
Geriatric Health, Spring 2024
in Community-Dwelling Older Adults: A Systematic Review. Journal of the American
12
Polypharmacy

WOMEN’S HEALTH
Women’s health not only includes health subjects that are unique to or different for women, but also non-gender-based healthcare. Women’s health is generally under-recognized, under-studied, and under-funded despite encompassing half of the world’s population’s needs.
PRESENTED BY:
Annie Liu, Vienna Place, Bailey Walker, Emily Gu, Owen Booth
GROUP 3
SPRING 2024
13
WOMEN’S HEALTH
Contraceptives are difficult to access in much of the world, exacerbated in cases of minority race/culture/background. Education regarding contraceptives also leaves much to be desired and while some progress has been made, much more must be done.
MENSTRUAL HEALTH
Women on average get their period around the age range of 10-15 years old. Due to period poverty, lack of education, misdiagnosis, and stigmas or taboos around menstruation, it has become more and more difficult for women to properly understand and care for their menstrual health which is related to their overall mental and physical health.
Breast cancer is the most diagnosed cancer worldwide and women in transitioning countries are dying at a disproportionate rate. Potential solutions exist, but their efficacy needs to be further tested.
There are too many cases all around the globe where women are given a false diagnosis to rare diseases
CONTRACEPTION
2
3 BREAST CANCER
4 RARE DISEASES FALSELY ATTRIBUTED TO MENTAL DISEASES
can
in the
becoming more severe or death. 5 WOMEN’S SEXUAL WELLNESS There is much medical and social stigma surrounding women’s sexual well-being that is causing an opaque scarcity in knowledge and cultural dismissal of its importance. 6
that
result
diseases
2024 Annie
Bailey Walker, Emily Gu, Owen Booth PRESENTED BY: 14
SPRING
Liu, Vienna Place,
Contraception
Vienna Place, BSPS Student
Population and Effects
The issues arising from lack of contraceptive access and education often affect women of minority races, as well as cultures, politics, and religions that differ from the presiding laws and regulations. Regarding insurance, 41% of women don’t know their insurance coverage is required to include contraception and 20% of uninsured women report having to stop contraception when they can no longer afford it. As shown below, only 12% of Asian/Pacific Islander women felt that they received all the information they needed before starting contraception, compared to 34% of white women. However, contraception remains an essential option. As of 2022, shown below, 49% of pregnancies were reported to be unintended
UnintendedPregnancies
IntendedPregnancies
References
1. Frederiksen B, Ranji U, Long M, Diep K, Salganicoff A. Contraception in the United States: a closer look at experiences, preferences, and coverage. Kaiser Family Foundation. Published November 3, 2022. Accessed February 26, 2024.
https://www.kff.org/womens-health-policy/report/contraception-in-theunited-states-a-closer-look-at-experiences-preferences-and-coverage/
Background and Relevance
Widespread problems beyond reproductive health are exacerbated by the global problem of women's health being negatively impacted by restricted access to and education about contraception. Limiting women's access to contraception makes it more difficult for them to make informed decisions about their reproductive health, pursue an education, and engage fully in society, which feeds the cycle of economic inequality. In the past, women's health issues—including reproductive health—have gotten less financing and research focus than those pertaining to men's health. This has left women with knowledge gaps and insufficient access to healthcare. Existing health inequities are made worse by this discrepancy in funding and research, especially for women from marginalized communities who already face obstacles to getting access to contraception. To confront these issues, all-encompassing strategies that put women's health first and address the underlying social, cultural, and economic issues that impede women's access to healthcare services around the world and sustain gender inequality are needed.
Solutions and Progress
Globally, there is a broad range of projects aimed at increasing access to and teaching contraceptives, including public health campaigns, family planning programs, and school-based education initiatives. Particularly in underprivileged areas, community health professionals are essential in providing reproductive health care, and mobile health technology provides easy ways to get information and assistance from a distance. Public-private partnerships use resources and knowledge to increase the accessibility and cost of contraceptives. These collaborations are supported by advocacy activities for access-block removal and legislative reform. Countries may strive toward achieving universal access to contraceptives by putting these methods into practice cooperatively, enabling people to make educated decisions regarding their sexual and reproductive health. Continued emphasis on these efforts across the globe will show remarkable increases in access and education, lowering unwanted pregnancies and other associated risks.
2. Access to contraception. American College of Obstetrics and Gynecology. Published January 2015. Updated 2022. Accessed February 26, 2024.
https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2015/01/access-to-contraception
Personal Statement
While many advancements have been made globally to increase access to and education about contraception, a lot of work still remains to be done. Because the consequences of such issues are so drastic (unwanted pregnancies, the spread of STDs, and other complications), they need to become an even higher priority. Unfortunately, despite its innovation in other areas such as technology, the US remains one of the countries with much improvement to be made. While recent political developments can prove to be an obstacle, they should not deter individual organizations and providers from doing everything they can to provide contraception for their clients/patients. Additionally, a lot of work can be done by the individual to push for legal changes. One area I believe deserves more focus in particular is increasing birth control options for men as well (besides condoms) to distribute the responsibility more evenly. An example of this is ADAM, or the “male IUD.“ While progress such as this is encouraging, it‘s important to push for equal priority in the comfort and side effects for women‘s birth control as in new men‘s birth control. - V Place
WOMEN’S HEALTH, SPRING 2024
EnoughInformation NotEnough
1 2 15
Menstrual health
Annie Liu, BSPS student College of Pharmacy
COMPLICATIONS; PERIOD HEALTH
Menstrual health is linked to physical and mental health issues in those that have periods. Depression, stress, and anxiety taking a big toll on women who are feeling lack of support. An abnormal period or lack of a period can relate to the reproductive and urinary tract health in a woman. Serious health complications can also be misdiagnosed as menstruation related. For example, if a woman has severe cramping and pain during the month of their period, it could actually be endometriosis which is commonly mistaken as PMS. Endometriosis takes place when tissue grows outside of the uterus or near other organs causing severe pain, bleeding, painful intercourse, nausea, and cramps prior to their period. Other misdiagnosis include but are not limited to fibroids, polycystic ovarian syndrome, and much more.
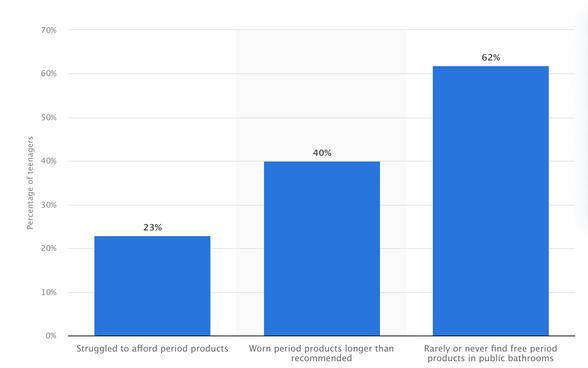
% of teenagers in the US who struggled to afford feminine hygiene products as of 2023
REFERENCES
PERIOD POVERTY
In a 2019 study, K. Krumperman noted that about 64% of menstruators had struggled to afford or get access to proper menstrual products within the last year. The lack of resources for those that menstruate can cause complications in their overall physical and mental health. Period poverty, the lack of access to period products and period education, can stem from costs, education issues, stigma or stereotypes. In terms of proper education for all to understand the menstruation process, a study looking at the health education standards in schools was done in all 50 states of the USA. It was found that only 3 of the states in the USA completely cover personal hygiene product education while 3 other states covered period management, which is not nearly enough literacy.
STIGMA
Discussion and understanding surrounding menstruation and period health can be difficult for menstruators as many negative, false, and unfair beliefs are made upon women on their periods. Thinx, a period product company, found that 58% of the 1,500 women studied in the USA said they were embarrassed and 42% felt shame while menstruating. In Nepal, there are some individuals/families that have a taboo in their culture where menstruation is seen as a dirty concept, resulting in isolation from the family member going through their menstruation, sleeping and living separately to avoid them during that time period. it is also not uncommon for menstruation discussion to be seen as improper, making it even more difficult for women to feel comfortable in understanding their health properly.
Krumperman, K. (2023) Period Poverty in the United States, Ballard Brief. Available at: https://ballardbrief.byu.edu/issue-briefs/period-poverty-in-the-united-states. 1. Elflein, J. (2023) Teens experiencing Period Poverty U.S. 2023, Statista. Available at: https://www.statista.com/statistics/1242985/us-period-poverty-teenagestudents/. 2.
3.
Hudson, Nicky. “The Missed Disease? Endometriosis as an Example of “Undone Science.”” Reproductive Biomedicine & Society Online, vol. 14, no. 14, Mar. 2022, pp. 20–27, www.ncbi.nlm.nih.gov/pmc/articles/PMC8517707/, https://doi.org/10.1016/j.rbms.2021.07.003.
Personal
statement:
Menstruation is a normal bodily function in women that can be easily misunderstood, causing women all around the world to be affected. Efforts have been made by the Period Project organization in attempt to solve period poverty, but further assistance in promoting menstrual health literacy and greater access to period products needs to be developed and advanced. A wider understanding on proper care during menstruation and normal menstruation symptoms/activity without the stigma underlying it can help women take better care of their mental, physical, social, and productive/urinary health; All which is related to a woman’s well being. (-Annie Liu)
Women’s health, Spring 2024
16
Breast Cancer
Owen Booth, BSPS Student
Global Problem
In 2020, 2.3 million women were diagnosed with breast cancer worldwide. Transitioning countries account for only 18% of cases, but account for 30% of breast cancer deaths. Both percentages are projected to rise by 2040 due to the aging population. These countries have a 20% higher mortality rate compared to transitioned countries and this can be attributed to the lack of access to quality, affordable diagnostic and treatment options. Lower-resource countries do not have properly funded breast cancer programs despite being the most commonly diagnosed cancer in the world. With the aging population and projected increase in incidence, these countries must develop a strategy to better control breast cancer outcomes.

Potential Solution
A collection of evidence-based publications called the Knowledge Summaries for Comprehensive Breast Cancer outlines a potential solution. A group of researchers set out to develop an integrated toolkit to help guide policy and breast health program interventions based on existing data to provide recommendations for countries with limited resources. These researchers surveyed primary literature and combined it into 14 concise publications called the Knowledge Summaries for Breast Cancer. There are seven different categories of publication: Planning, Prevention, Early Detection, Diagnosis, Treatment, Palliative Care, and Survivorship Care. These publications focus on providing recommendations tailored to four different resource levels including basic, limited, enhanced, and maximal.
Implementation and Efficacy
The implementation of this solution was tested in Kenya. There, it was distributed to a group of policymakers and healthcare professionals. They concluded that KSBC is useful as a learning tool and was even incorporated into a pathology resident training curriculum. It was also deemed useful as a planning tool with one policymaker saying that it helped them understand how to design and link breast cancer programs, including how to adapt the information according to cultural variations within the country. However, this study was quite limited, as it was a small sample size and the follow-up survey had a low response rate. Therefore, the long-term efficacy of this solution is still unknown, making wider distribution and better outcome tracking critical to further test the efficacy of this toolkit.
Personal Statement
References
1. Arnold M, Morgan E, Rumgay H, et al. Current and future burden of breast cancer: Global statistics for 2020 and 2040. The Breast. 2022;66:15-23. doi:10.1016/j.breast.2022.08.010
2. Zujewski JA, Dvaladze AL, Ilbawi A, et al. Knowledge Summaries for Comprehensive Breast Cancer Control. J Glob Oncol. 2018;(4):1-7. doi:10.1200/JGO.17.00141
3. Cira MK, Zujewski JA, Dvaladze A, Brand NR, Vogel AL. Knowledge Summaries for Comprehensive Breast Cancer Control: Feedback From Target Audiences in Kenya. J Glob Oncol. 2019;(5):1-6. doi:10.1200/JGO.18.00119
One of the major issues in breast cancer control in transitioning countries is that women present with more advanced malignancies compared to those in transitioned countries. This is likely due to a lack of access to proper screening and detection methods. This then contributes to the higher mortality rates seen in these countries. Therefore, while treatment efforts are important, I believe that dedicating what resources these countries have to prevention, early detection, and diagnosis should be the priority. Catching this cancer in an earlier stage will more often than not lead to less extensive treatment requirements and better outcomes. ~ O Booth
WOMEN’S HEALTH, SPRING 2024
1 1 1 2 2 3 3
Estimated number of breast cancer cases from 2020 to 2040. 1
1 17
 (BAILEY WALKER, BSPS STUDENT)
(BAILEY WALKER, BSPS STUDENT)
IVI. What is Hyperemesis Gravidarum? Symptoms, causes and treatment. IVI Fertility. Published January 3, 2022. Accessed March 26, 2024. https://ivifertility.com/blog/hyperemesis-gravidarum/
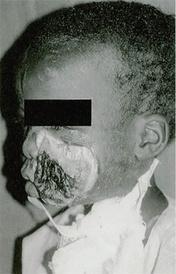
False Diagnosis
There are times when pregnant women are being told they just have normal symptoms when they have hyperemesis gravidarum (severe vomiting and dehydration) or being told it’s all in their heads, which leads to severe consequences. Rebecca Rommen reported that a woman named Stephanie Aston in New Zealand was told that she had a factitious disorder, symptoms produced by the belief of the patient that they are ill. Stephanie died from this false diagnosis from a disease called Ehlers-Danlos Syndrome, a disorder affecting the connective tissue of the skin, bones, and other organs, that was brushed off since they didn’t evaluate her properly.
Funding
Too often, women all around the globe are given diagnosis errors that can lead to death. Maya Dusenbery found that 40-80K deaths in the US are from women given a false diagnosis and women also have a longer wait time for a diagnosis than men . Women are told that it is all in their heads and have to wait longer, even though they have to make more doctor’s visits than men. Sometimes the doctors label the women as hysterical or having a diagnosis of hysteria, a mythical disorder since ancient Greece with a belief that the movement of the uterus causes women to act hysterical. It has become too prevalent of a stigma that must be removed since this is a false diagnosis that even the doctors (especially male doctors) are unsure of. There should be education seminars to educate people about this stigma, it could potentially help reduce the stigma and even diagnosis errors.
There has been very minimal effort to put a lot of funding and research into women’s rare diseases. A 2021 study by Martha Nolan found that funding of men’s rare diseases is three times that of the funding of women’s rare diseases. What should be done is to put more funding into the medical research and studies for women’s rare diseases. Organizations like WHO and the National Institute of Health need to use more of their budget towards women’s health and diseases instead of a small fraction of it (around 11 percent of their budget)
References
DusenberyM.'Everybodywastellingmetherewasnothingwrong' BBC.https://www.bbc.com/future/article/20180523-howgender-bias-affects-your-healthcare2022.AccessedFebruary13, 2024.
2.Rommen, R. A 33-year-old woman with a rare illness died aged 33 after a doctor said it was a mental-health problem instead, Business Insider 2023. Available at: https://www.businessinsider.com/woman-33-with-rare-disease-dies-doctor-diagnosedmental-health-problem-2023-9 (Accessed: 13 February 2024).
3.Martha Nolan opinion contributor. The NIH must address disparities in women’s health research funding. The Hill. Published May 22, 2023. https://thehill.com/opinion/healthcare/4015424-the-nih-must-address-disparities-inwomens-health-research-funding/
Personal Statement
I believe that more effort should be put into the funding (research and studies) of women’s rare diseases. I feel like if there was more funding, women’s rare diseases could actually be known, and we could possibly be made aware of them from symptoms/tests, instead of giving diagnosis errors. Removing the stigma around women and hysteria needs to happen as well since they help contribute to these diagnosis errors (like implementing education semiars). Women are seen as being hysterical or “it’s all in their heads” when doctors (more so male doctors) have no idea what the actual problem is. (~BWalker).
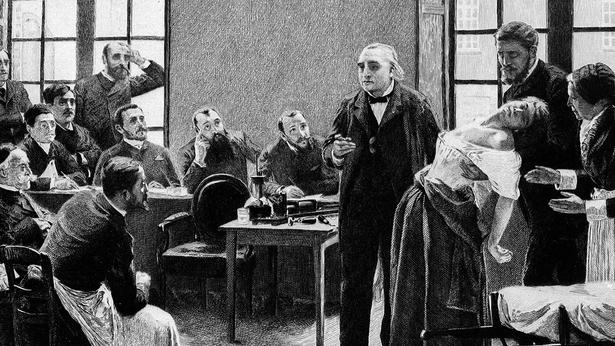
RARE DISEASES FALSELY ATTRIBUTED TO MENTAL DISEASE
Women’s Health, Spring 2024
Jaffray S. What is hysteria? Wellcome Collection. Published August 13, 2015. https://wellcomecollection.org/articles/W89GZBIAAN4yz1hQ
1. 3 2 1 18
Women’sSexualWellness
EmilyGu,BSPSStudent
Invasive Procedures
Invisible to Medicine
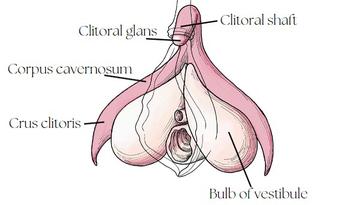
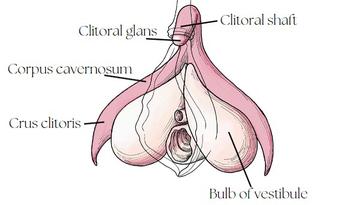
There is limited medical knowledge on women’s sexual anatomy due to past and current neglect for the subject. A study found that most anatomy textbooks that today’s medical practitioners studied from only briefly references the vulva, often describing it as weak and secondary to the penis, while covering the penis extensively . Gray’s Anatomy, still considered the “doctor’s bible” today, gave a detailed description of the dorsal penile nerve and comparison stated that the corresponding dorsal nerve of the clitoris is very small, which is incorrect. The same study found that only 11 articles on the anatomy of the clitoris have been published from 1947-2020 worldwide. This is resulting in disastrous consequences. While surgeons would make sure to avoid the penile nerves during prostate removal surgeries, “there have been documented injuries to the clitoris in procedures including pelvic mesh surgeries, episiotomies during childbirth and even hip surgeries”, resulting in women losing their ability to orgasm.
Outside of the standard medical procedures, many procedures unnecessarily alter female genitalia without consent across the world. This includes genital cutting and the husband's stitch. In some countries in Sub-Saharan Africa and the Arab States, female gentital cutting is routinely performed without informed consent . These procedures are much more invasive than the male circumcision performed in the U.S.. Even in Western countries, accounts of the husband stitch, or a stitch in the vagina to make sex more pleasurable for the male partner, persist across message boards and online forums, undocumented by the doctors who secretly performed them when the woman was under anesthesia after childbirth.
References
1.
3.
5
O’Connell H, Haller B, Hoe V. Moving from Critical Clitoridectomy. Australian & New Zealand Journal of Obstetrics & Gynaecology. 2020;60(5):637-639. doi:https://doi.org/10.1111/ajo.13243
2. Amphis. A Labeled Digram of the Human Clitoris. (Campbell M, ed.).; 2022. Accessed March 27, 2024. https://cdn.technologynetworks.com/tn/images/body/clitorisdiagram1667477328749.jpg
Gross RE. Half the World Has a Clitoris. Why Don’t Doctors Study It? The New York Times. https://www.nytimes.com/2022/10/17/health/clitoris-sex-doctors-surgery.html. Published October 17, 2022.
United Nations Population Fund. Female Genital Mutilation (FGM) Frequently Asked Questions. Unfpa.org. Published March 2024. Accessed March 25, 2024. https://www.unfpa.org/resources/female-genitalmutilation-fgm-frequently-asked-questions
4. Murphy C. The Husband Stitch Isn’t Just a Horrifying Childbirth Myth. Healthline. Published January 24, 2018. Accessed March 26, 2024. https://www.healthline.com/health-news/husband-stitch-is-not-just-myth
8.
5. Wade L, Ferree MM. Gender: Ideas, Interactions, Institutions. 3rd ed. W.W. Norton & Company, Inc; 2022. 6. Orenstein P. Girls & Sex. HarperCollins; 2017. 7. Wetzel GM, Cultice RA, Sanchez DT. Orgasm Frequency Predicts Desire and Expectation for Orgasm: Assessing the Orgasm Gap within Mixed-Sex Couples. Sex Roles. 2022;86(5-6). doi:https://doi.org/10.1007/s11199-022-01280-7
Personal Statement- Emily Gu
“The fact that there is even a practice called the husband stitch is a perfect example of the intersection of the objectification of women’s bodies and healthcare.”
-Stephanie Tillman, a certified nurse midwife5
The Lesser Need
Women’s sexual wellness is inextricably tied to the social construct of sex. In cultures where rape is rare, the strength of women’s genitalia is emphasized and the vulnerability of the penis and tested highlighted in cultural representations such as folklore . In the U.S. sexual health education, female pleasure is rarely brought up, if sexual health is taught at all . It is no surprise then that there is a significant orgasm gap between men and women, as reported by numerous studies . In typical American heterosexual hook-ups, both men and women put the man’s pleasure first and believe that the men are more entitled to orgasms . On the other hand, the Dutch teachers, doctors, and parents have open conversations with the youth on sexual wellness that includes pleasure. As a result of this effort, 86% percent of Dutch girls and 93% of boys surveyed report that they were equally eager for their first sexual experience.
When anatomical drawings of the human bodies were first being studied and produced, Leonardo Da Vinci dissected 30 male human cadavers and crafted his famous human (male) anatomy drawing. He produced his female anatomy drawing based on his dissection of a female cow. What parts might have been omitted when the invisible first became visible? What did the future medical field dismiss when they studied the visible structures? Today, research for women’s health is still grossly underfunded, despite serving half the world’s population. Women’s sexual wellness, especially outside of reproductive needs, is often dismissed. I think most people would agree that even if a man’s sperm is non-viable, if he wants to enjoy sex (and the shared experience with his partner) then that need should be met. Yet, women’s sexual needs are invisible in the doctor’s offices, in the surgery rooms, and in the bedrooms, because they have been missing from the dissection tables, the research laboratories, the textbooks, and the classrooms.
2
WOMEN’S HEALTH, SPRING 2024
CompleteAnatomyoftheClitoris
2
1
3
4
7 8 6 6 7 19
TheImpactof Cultureand Traditionson Global Healthcare

AComprehensiveAnalysis onhowCulturalNorms
AffectHealthcareDelivery andOutcomesWorldwide Global Health Institute 20
The intercultural and global health issue that we evaluated was how culture and traditions affect global healthcare systems.
We started our project by finding a definition of culture that we could use to spot differences. We chose UNESCO’s definition: “the set of distinctive spiritual, material, intellectual and emotional features of society or a social group, that encompasses, not only art and literature but lifestyles, ways of living together, value systems, traditions and beliefs.” Location is not completely representative of culture, but it can provide some overlap and insight into how culture and traditions influence and support healthcare systems. With this information, we chose subtopics and different regions of the world to analyze.
Subtopics:
Healthcare Systems by Stella Hart, BSPS student
Medication Adherence by Emily Randall, BSPS student
Trust in Healthcare Professionals by Elias Walker, BSPS student
Customs affect Dietary and Healthcare Habits by Chieh-Hsun Chou (Scott), BSPS student
Mental Health in Different Cultures by Sofia Lombardi, BSPS student
21
Background: The type of healthcare coverage someone has can truly be the difference between life and death. All around the world, each country, region, or certain cultures have different ways of treating patients, and whether if they can afford the proper treatment can determine if the patient can receive access to it. Altogether we are discussing how cultures and traditions affect healthcare or the lack of healthcare. In this section, I will be discussing how different types of healthcare coverage varies throughout the world and how some cultures use alternate routes of treatment.
The Americas:
United States-The United States provides the most variety of healthcare coverage. These include private insurance, federal insurance, and publicly funded healthcare. The US healthcare system allows providers to fluctuate price and other expensive services. Brazil- Brazil provides a government-run universal public health system. This is funded by taxes at federal, state, and municipality level. Though this system covers for all types of healthcare, it leads to long wait times and out of pocket spending for treatment.
European Union:
Each country has its own healthcare system, but all aim to follow the National Health System (NHS) and follow and three model system: single payer, socialized, and privatized regulated. In the UK, an NHS is provided. 80% is funded by taxes and 20% by national insurance. France has a private healthcare system where Germany has privatized but regulated; meaning citizens earning below a threshold must take insurance
Personal Thoughts: Personally, I think socialized medicine is a good solution for everyone to have coverage, but i do think it would be very difficult to have an entire country’s population to obtain. From the information gathered, I think a reasonable solution for nations would be a universal healthcare system, so that everyone has some access. -Stella Hart, BSPS
Healthcare Systems
Stella Hart, BSPS student
Asia: In China, universal publicly funded insurance is provided, with urban employees enrolled in the employment-based programs. Others may enroll if they choose, but many residents are satisfied with the coverage that is received. In India, the states oversee organizing services, though nationwide, universal free inpatient and outpatient care is provided.

Africa: Very few can afford highquality private care, so many resort to public health systems or traditional healers. Many countries rely on healthcare that is provided by donor money and many times international loans are provided, but that ultimately increases the cost of drugs and primary care. Many who can’t afford proper treatment turn to spiritual healers that have been taught through passed down traditions.
pogonici/Shutterstock.com
Solution: With different types of coverage throughout different cultures, many citizens seem satisfied with their treatment options, but the ones who can’t afford certain care, they turn to an alternate way. Recently, socialized medicine has been a thought of a way to provide for all. Socialized medicine is healthcare system in which the government owns and operates healthcare facilities and employs the healthcare professionals, thus also paying for all healthcare services. This can be helpful for everyone to have access to coverage and affordable treatment.
References: healthinsurance.org. socialized medicine definition. healthinsurance.org. Published September 23, 2017. https://www.healthinsurance.org/glossary/socialized-medicine/ Thomas L. Healthcare Systems Around the World. News-Medical.net. Published April 6, 2021. https://www.news-medical.net/health/HealthcareSystems-Around-the-World.aspx
[CulturalDifferences,Spring2024] 22
Background: Medications are taken to control chronic conditions as well as temporary conditions. Adhering to medication regimens recommended by your doctor and pharmacist is important for the well-being of the patient. Medication nonadherence could lead to substantial worsening of the disease, more frequent visits to the doctor/ER, leading to, more healthcare costs, and in worst cases, death. We are looking at this topic to determine if this varies from culture to culture/country to country. For the sake of this monograph, we are going to be focusing on prescription medications. 3
Medication Adherence
Emily Randall, BSPS student
Europe: In Europe, a team looked at three different chronic disease medications including, antihyperlipidemic, antiosteoporosis, and oral antidiabetic medications. This was assessed in Italy, Spain, and Ireland. First, they looked at suboptimal implementation of medication, Antihyperlipidemic medications averaging the three countries was around 53.45%, Antiosteoporosis medications averaging the three countries was around 61.35%, and Oral antidiabetic medications averaging the three countries was around 30.33%.
Next, they looked at the discontinuation of the medication in those three countries. Antihyperlipidemic medications were 55.63%, Antiosteoporosis medications were 60.24%, Oral antidiabetic medications were 46.80% . 1
Personal/professionalopinion: In my opinion, this topic is a very challenging one. This is a global health issue and I do feel like this varies from culture to culture/country to country. There are a lot of solutions that I consider to be surface level such as educating patients more. In my opinion, a lot of medication adherence relates to the section mentioned above labeled, health systems. Drug costs and limited health care access is a huge issue when relating to medication adherence and I feel that could be a big factor in some of the patients who do not adhere to their regimens. - E
Randall
1.Menditto E, Cahir C, Aza-Pascual-Salcedo M, et al. Adherence to chronic medication in older populations: application of a common protocol among three European cohorts. Patient Preference and Adherence. 2018;Volume 12:1975-1987. doi:https://doi.org/10.2147/ppa.s164819
2.Mahmood S, Jalal Z, Hadi MA, Khan TM, Haque MS, Shah KU. Prevalence of nonadherence to antihypertensive medication in Asia: a systematic review and metaanalysis. International Journal of Clinical Pharmacy. 2021;43(3):486-501. doi:https://doi.org/10.1007/s11096-021-01236-z
3.Jimmy B, Jose J. Patient Medication Adherence: Measures in Daily Practice. Oman Medical Journal. 2011;26(3):155-159. doi:https://doi.org/10.5001/omj.2011.38

Asia: In Asia, patients with hypertension were looked at with a mean age of 58. Overall nonadherence was 48%, Highest prevalence of non-adherence was in South Asia at 48%, followed by East Asia at 45%, and then Middle East Asia at 41%. Higher rate of non-adherence was observed in Low/lower-middle income countries at 50%, Upper-middle income: 37%, High-income: 44%. 2
Solution: Some fixable solutions include the level of prescribing from doctors, better communication with the patient, and addressing the concerns of nonadherence. Health systems in different countries can be a big factor when talking about medication adherence. For example, drug costs and limited health care access in different countries is a problem that is harder to be fixed. 3
[CulturalDifferences,Spring2024] 23
TrustinHealthcare Professionals
Elias Walker [BSPS Student]
Introduction
What defines a healthcare professional varies between cultures. In Western Medicine, it covers roles like doctors, pharmacists, nurses, dentists, etc. In other cultures, it may refer to individuals in rural areas treating injuries without formal education. The medicine and professionals you trust often depend on your cultural background and your culture’s healthcare system.
What is being done?
One of the main issues that we were able to identify is that not having a free healthcare system can cause a distrust of healthcare professionals among the citizens. So far, there are only 43 countries in the world that do not have free or almost free healthcare. This is a great step in the right direction, as it also shows that the healthcare systems are focused on serving the patients, not making money. As general knowledge has expanded, many countries have been focused on improving their education systems, which include medical schools. Growth in this aspect has changed for the better what it means to be a healthcare professional in individual cultures.
Personal Opinion
Who is affected by this issue?
The issue of trust in healthcare systems and professionals affects individuals globally, demanding high standards for healthcare delivery. Low trust levels signal a need for improvement within systems to better meet patient needs. This becomes an intercultural issue as different cultural approaches to healthcare and professional pathways offer valuable lessons for improvement across countries. Enhancing trust is crucial for healthcare professionals to effectively serve their patients, as distrust can lead to patient reluctance in following recommended treatment plans, regardless of their validity.
Western Medicine
In Western nations like the United States, trust in healthcare professionals lags behind some African regions, despite stringent education standards. This distrust is linked to the profit-driven nature of the US healthcare system, which ranks among its top industries. Conversely, countries like Mexico and Canada, offering free healthcare, report higher trust levels despite differing educational criteria for healthcare professionals. This underscores the impact of healthcare system structures on trust, rather than solely professional education.
I believe that bringing free general healthcare to every culture would be beneficial for the citizens. While most countries already have this, too many people are forced to pay large amounts for their health. We can see that this harms their trust in the professionals, as well as the obvious negative effects that come with paying large amounts for healthcare. In a culture that has accepted paying higher taxes to the government for free healthcare, it would make sense that the culture as a whole cares about the healthcare industry. This would cause a larger focus on the education of healthcare professionals which could also improve the trust in their professionals.
-E Walker
References: IBISWorldReporters.(2024).BiggestIndustriesbyRevenueintheUSin2024.IBISWorldIndustryReports. AccessedMarch27,2024.https://www.ibisworld.com/united-states/industry-trends/biggest-industries-byrevenue/ 1. Farrar,J.(2019,August26).Whythemostimportanttoolinhealthcareistrust.WorldEconomicForum. AccessedMarch27,2024.https://www.weforum.org/agenda/2019/08/important-tool-in-healthcare-is-trustvaccines-africa/#:~:text=Close%20to%20one%2Dthird%20of,have%20low%20trust%20in%20scientists
4.
2. Vankar,P.(2023,November30).Trustinhealthcarebycountry2022.Statista.AccessedMarch27,2024. https://www.statista.com/statistics/1071027/trust-levels-towards-healthcare-in-select-countries/ 3 Wang,C.(2022,October25).AnoverviewofcountriesthatofferFreeHealthcare.Skuad.AccessedMarch27, 2024.https://www.skuad.io/blog/an-overview-of-countries-that-offer-freehealthcare#:~:text=visitors%20and%20foreigners.-,How%20many%20countries%20have%20free%20health care%3F,healthcare%20for%20all%20its%20citizens


African Regions
A global survey on trust in healthcare professionals, vaccinations, and scientists revealed lower trust levels in African regions towards healthcare professionals and scientists. Surprisingly, these regions exhibited significantly higher trust in vaccinations compared to the rest of the world. This trust likely stems from firsthand experiences witnessing the effectiveness of vaccinations in combating diseases such as malaria and Ebola.
24 [Cultural Differences, Spring 2024]
Background:
Modern dietary patterns are shifting globally, with an increased consumption of processed foods high in sugars and saturated fats. This shift is occurring while traditional diets, generally rich in fibers, whole grains, and minimally processed foods, are being abandoned. The implications of these changes are far-reaching, affecting healthcare outcomes and the prevalence of non-communicable diseases across different cultures.
Custom affect dietary and healthcare habits
Scott Chou (BSPS student)
Asia:
In Asia, the transition from traditional diets to more Westernized eating habits has contributed to an upsurge in diet-related health issues such as obesity, diabetes, and cardiovascular diseases. Notably, in urban areas, there's a marked increase in fast-food consumption, which correlates with rising obesity rates. These changes have significant implications for healthcare systems, which now have to manage an increasing burden of chronic non-communicable diseases.
Who or what is affected?
The global shift in dietary customs affects a broad spectrum of the population, with children and adolescents being particularly vulnerable to adopting poor eating habits. The healthcare systems, policy-makers, and economies of nations are all impacted, as they must adapt to the changing health profiles of their populations.
Efforts or Solutions:
Efforts to counteract the negative health impacts of modern diets include public health campaigns promoting traditional, nutrient-rich foods, reformulating processed foods to be healthier, and improving the labeling of food products. Healthcare systems are also focusing on preventive measures, nutrition education, and improving the affordability and accessibility of healthy foods.
Europe:
Europe presents a mixed picture, with Mediterranean countries still adhering to diets high in vegetables, fruits, and healthy fats, while Northern European countries are seeing a rise in processed food intake. The diverse dietary customs across Europe result in varied healthcare challenges, necessitating tailored public health strategies to encourage healthy eating habits and manage chronic diseases.
North America:
North America is witnessing a continuous battle with obesity and its associated health conditions. Dietary habits high in calories and poor in nutritional value are exacerbating the incidence of type 2 diabetes, heart diseases, and certain types of cancer. Healthcare systems are stressed by the increasing need for chronic disease management and the high cost of medical care related to poor diets.
Russia:
Russia's dietary customs, influenced by both European and Asian patterns, have seen an increase in processed food consumption. This has led to a growing prevalence of noncommunicable diseases, posing challenges for a healthcare system that is working to improve access and quality of care in both urban and rural areas.
Personal Opinion:
I think eating more processed food and less healthy stuff is a big problem that affects our health. We need to remember the good parts of traditional eating but also fit them into our busy lives today. To fix this, we need to teach people about eating right, make good food policies, and make sure they fit with how different people live and what they can afford. Getting this right is important not just for staying healthy, but it also helps everyone save money and trouble in the long run. ~ S Chou
South America:
Similar to North America, South American countries are facing challenges with the rise of noncommunicable diseases driven by poor dietary habits. Fast food chains have proliferated, contributing to the obesity epidemic and related health concerns such as hypertension. The healthcare infrastructure is being tested by the need to provide widespread education on nutrition and manage the growing healthcare demands.
Africa:
Africa's unique dietary challenges are influenced by a dichotomy of undernutrition and a rise in processed food consumption among the urban population. Traditional diets, rich in grains and legumes, are giving way to more calorie-dense, nutrient-poor foods, contributing to a rise in lifestyle diseases. The healthcare systems, often underresourced, are facing the double burden of combating infectious diseases and emerging non-communicable diseases.
Reference:
Whatweeatmatters:Healthandenvironmentalimpactsofdiets worldwide.Healthandenvironmentalimpactsofdietsworldwide-Global NutritionReport.AccessedMarch27,2024.
https://globalnutritionreport.org/reports/2021-global-nutritionreport/health-and-environmental-impacts-of-diets-worldwide/ WriterAACC.11globalhealthissuestowatchin2023,accordingtoIHME experts.InstituteforHealthMetricsandEvaluation.AccessedMarch27, 2024.https://www.healthdata.org/news-events/insights-blog/actingdata/11-global-health-issues-watch-2023-according-ihme-experts. MitchellC,Karl-WaithakaZ,UnnikrishnanS,OyekanT.Transforming Africa’sfoodsystemsfromthedemandside.BCGGlobal.January31,2022. AccessedMarch27,2024.
https://www.bcg.com/publications/2021/transforming-africa-foodsystems-from-demand-side JackaF.Foodandmood:howdodietandnutritionaffectmentalwellbeing? https://www.bmj.com/
[CulturalDifferences,Spring2024]
25
Mental Health in Different Cultures
Sofia Lombardi (BSPS Student)
Introduction

The World Health Organization defines mental health as, “…a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community”. Cultures relate to a group of people that may share location, religion, and ideologies that can influence their view on mental health, and whether or not it should be part of healthcare systems. Often times, tradition and generational beliefs can create stigmas about an individual with poor mental health; conversely, they can also emphasize individuality and prioritize strong mental health. The word stigma, while it can have multiple definitions, is usually used to communicate a concept of stereotyping and a general idea of shame.
Global Mental Health
Mental health is an important intercultural global issue, as it impacts a person’s ability to function in society and support oneself, as well as puts this person at risk for distress and harm against oneself or others. When investigating the stigma behind mental health, it is essential to look at how different cultures and regions of the world view mental health, and how time has further strengthened or changed ideas and stereotypes associated with poor mental health. In China, several surveys show a long prevailing high public stigma and limited knowledge about depression and schizophrenia. It is also possible that mental health is not a priority for a country’s healthcare funding for several other reasons. In many countries located in Southeast Asia, most money and resources are focused on infectious and tropical diseases, which is a prevalent and dominating issue. In Nigeria, most patients with mental health conditions seek help outside of a healthcare setting, often wanting spiritual interventions, as mental health related illnesses are often associated with cultural and ancestral routes.
References StuartH.ReducingtheStigmaofMentalIllness.GlobalMentalHealth.2016;3(17). doi:https://doi.org/10.1017/gmh.2016.11
1. TanKA,KengSL,TalibMA.Editorial:MentalhealthissuesinSoutheastAsiaregions:lookingbackandmoving forward.Frontiers.PublishedMay3,2023. https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2023.1229079/full
2. WadaYH,RajwaniL,AnyamE,etal.MentalhealthinNigeria:ANeglectedissueinPublicHealth.PublicHealth inPractice.2021;2(100166):100166.doi:https://doi.org/10.1016/j.puhip.2021.100166
3. WorldHealthOrganization.MentalHealth.WorldHealthOrganization.PublishedJune17,2022. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response 4. YinH,WardenaarKJ,XuG,TianH,SchoeversRA.Mentalhealthstigmaandmentalhealthknowledgein Chinesepopulation:across-sectionalstudy.BMCPsychiatry.2020;20(1).doi:https://doi.org/10.1186/s12888020-02705-x 5.

https://www.istockphoto.com/illustrations/mental-health
Who is affected?
People can be affected by mental health at varying degrees and is best understood as a complex spectrum that can result in many different clinical, social, and personal outcomes. Globally, mental health resources and their availability are very different. Mental health resources can be defined as any public health service that advances and improves the behavioral health of an individual and society. Services can include access to a psychiatrist and mental health professional team, outpatient treatments, and prescription medications.
What are possible solutions?
The simplest effort that works toward ending the stigma around mental health is to normalize conversations about mental health, open conversation helps to facilitate an environment in which a person suffering from mental health issues could seek help from a trusted individual or healthcare professional. Negative societal responses toward mentally ill people is perhaps the leading barrier in the forming of worldwide mental health programs. Additionally, integrating education and information about how to promote good mental health, as well as providing knowledge on what constitutes poor mental health, is an important aspect in improving negative attitudes and stigma of individuals who face mental health issues. Education can be provided in the form of seminars in the workplace, coursework in the public school systems, and addressed in healthcare professional trainings.
Personal Opinion
I think the influence of culture and tradition on mental health is an important issue that has the potential to change negative attitudes directed toward individuals with poor mental health. Educating oneself and others is the important first step to clear up any spread misinformation and false stereotypes about those with poor mental health and mental illness. Additionally, I believe governments should consider prioritizing mental health resources by citizen demand and prevalence in the region.
~ S Lombardi
[CulturalDifferences,Spring2024]
26
Healthcare in a RESOURCE-LIMITED ENVIRONMENT
Addressing the healthcare needs of resourcelimited environments requires a multifaceted approach that considers various determinants of health, along with sustainable investment in healthcare infrastructure, workforce development, and health education. To evaluate the situation, we have broken down the main topic into five subtopics: post-disaster, educational, correctional facilities, geographical, and travel & tourism.
While the effects of healthcare in a limitedresource environment are seen most clearly in patients, the medical education of children, adolescents, and adults is affected as well, and can perpetuate a cycle of poor quality healthcare or a general lack of understanding of medical topics.
GEOGRAPHICAL
It is estimated that one in every five Americans lives in a rural area. Location can often limit the amount and quality of care a patient receives. Geographically isolated communities often have difficulties with access to providers, facilities, and specialized care. In particular, remote areas such as the American Samoa are at greatest risk for healthcare disparities.
Areas that go through a major disaster often result in major disruptions in their healthcare systems making it difficult to receive access crucial medical services According to a study done by the NIH, “There have been more than 11,000 disasters documented since 1960 as evidenced by the 510,837 deaths and 3.9 billion people”.
CORRECTIONALFACILITIES
Correctional facilities, integral to the justice system, are mandated to provide healthcare to inmates, yet they face challenges in meeting adequate standards due to limited resources and systemic issues. This results in disparities in healthcare access, particularly concerning noncommunicable diseases, communicable diseases, and mental health conditions.
TOURISM&TRAVEL
In China and India, there are less than 1/10 of the plastic surgeons per million people as in North America, but yet many Americans travel to these countries for procedures. When individuals arrive back in their home countries following an operation, they typically do not receive adequate care, posing additional risks to their health.
BACKGROUNDINFORMATION POST-DISASTER
EDUCATIONAL
SPRING 2024 [HEALTHCARE IN A RESOURCE-LIMITED ENVIRONMENT, SPRING 2024] 27
EDUCATIONAL
BACKGROUND INFORMATION
When examining healthcare in a limited-resource environment through the lens of education, some key topics include basic medical education in school systems, disconnect between healthcare providers and residents of limited-resource communities, and limited access to specialized medical tools used for diagnosis and treatment of diseases.
AS A GLOBAL HEALTH ISSUE
Asaglobalhealthissue,theunderlyingissue islackofeducationconcerningrelational skills.Simplyput,doctorsandmedical professionalstodayarenoteducatedon howtocommunicateandempathetically relatetoindividualswhohavegrownupin impoverishedenvironments(Hudonetal. 2016).Improvingtheawareness,abilityto self-reflect,andcapacitytoadjusttoeach patients’realityisnecessasryformedical studenteducation(Hudonetal.,2016).
WHO IS AFFECTED?
Individuals of all backgrounds are affected by this gap in medical education. Whether it is the patients in these limited resource communities that do not receive adequate care, or it is the potential medical professionals that are forced away from desired career paths, the effects on healthcareandeducationarenotlocalized.

CURRENT EFFORTS
In China’s Yunan province, health literacy studies are being conducted within impoverished communities. Findings support the implementation of visual and media tools as critical parts of health literacy and medical education (Li et al., 2023). A combination of provincial (local) and national programs proved to be most effective in improving education (Li et al., 2023).
FUTURE EFFORTS
Specific efforts are being put into place by medical schools and accreditation boards like the ACGME to matriculate and train medical students that have come from disadvantaged backgrounds and can relate to the problems that residents of limited resource communities are going through. Following the steps of medical programs like UCLA’s Drew Medical Education program, training with disadvantaged populations can expose future physicians to communities they need to form strong bonds within (Ko et al., 2007).
PROFESSIONAL OPINION
Currently, medical education of medical professionals and other individuals is clearly lacking in communities that don’t have the healthcareinfrastructureorresourcestosupport them. More emphasis needs to be placed on a local level within these communities to promote medical education initiatives that produce a cycleofqualityhealthcare.
-T. SARDESAI, BSPS SENIOR [HEALTHCARE IN A RESOURCE-LIMITED ENVIRONMENT, SPRING 2024] 28
GEOGRAPHICAL
BACKGROUNDINFORMATION
Rural areas in the United States are often at higher risk for poor health outcomes. This is evidenced by higher rates of obesity and lower life expectancies.
In the US, metropolitan areas have a life expectancy of 79.1 years compared to 76.7 years in rural areas
In the American Samoa, 85% of the adult population is overweight or obese, compared to the national average of 69%
A major cause for concern in these rural areas is the provider shortage
Rural areas have just 39.8 primary care physicians per 100,000 people, compared to 53.5 in urban areas
These numbers decrease as the provider becomes more specialized
ASAGLOBALHEALTHISSUE
Rural healthcare disparities are not limited to the United States. 90% of the world’s rural population lives in Africa and Asia. Similar to the United States, citizens of these rural areas are often socioeconomically disadvantaged and have poor access to quality care.
WHOISAFFECTED?
Both patients and providers are affected by location limitations. Patients who are older, have chronic conditions, and are socioeconomically limited are most at risk for worse health outcomes. Providers in these areas are often overworked, so they are also affected by this global health issue.
CURRENTEFFORTS

home
Many medical schools in the United States have incentives for those who practice rural healthcare out of medical school
Japan
To help serve patient populations on Pacific Islands, Japan uses a ship containing a portable x-ray machine, dental unit, and surgical theater that can travel to small islands
FUTUREEFFORTS
Create more mobile healthcare options for patients in geographically limited areas
Add walking paths and more healthy food options to rural areas
Encourage small hospitals in rural areas to partner with larger health systems
Create more incentives for specialized providers to live and work in rural areas
PROFESSIONALOPINION
“The global health issue of healthcare disparities in geographically isolated areas will not get fixed over night. In the meantime, individuals in these areas should take advantage of the resources available. Commit to a proper exercise routine, and try to schedule telemedicine appointments when needed.”
-A. MCCOY, BSPS SENIOR
[HEALTHCARE IN A RESOURCE-LIMITED ENVIRONMENT, SPRING 2024]
ANNA MCCOY - BSPS SENIOR (“ADDRESSING HEALTH INEQUITIES”) 29
POST-DISASTER
Author: Allison Cilke, BSPS Senior
BACKGROUNDINFORMATION
In post disaster or post war situations, healthcare systems and access to health resources become limited. Disasters tend to overwhelm healthcare facilities along with its staff which results in limitations when giving proper care along with creating medicine shortages. Lack of resources force staff to focus on more critical cases which leaves the rest of the population to fall to contaminated water and sanitation problems. Due to the unstable infrastructure, it is likely that many people can become displaced.
ASAGLOBALHEALTHISSUE
Disaster, either caused by war or natural disasters creates a more drastic effect to regions that have weaker health systems to begin with. Disaster can create a strain on the medical supply chain since nations would want to divert resources to these regions that have been negatively affected the most.
Natural disasters and war can displace citizens creating crowded living conditions, poor sanitation, and contaminated water resources which can make people more susceptible to infectious diseases. According to UNICEF, “people in conflict-affected areas are eight times as likely to lack basic sanitation.” If conditions like this continue these diseases can quickly spread across neighboring regions causing outbreaks.
Since disaster and war have the capacity of creating detrimental damage, recovery can take years requiring tremendous amounts of resources. Rebuilding healthcare facilities is an incredible financial burden along with training new staff. Addressing the resulting health risks also requires many resources to maintain and reverse the negative effects.
Everyone can somewhat be affected, but more specifically low resource communities (those with weak healthcare systems), displaced populations since they are forced to leave their homes and healthcare workers because disasters can displace and cause distress on them which then limits their ability to give quality care.
CURRENTEFFORTS
Department of Homeland Security
Has principles that guide recovery support activities
Facilitates communication for post-disaster recovery planning
Other organizations (Red Cross, FEMA, etc.)
Provide financial assistance, hot meals, clean water, and emergency supplies, these usually last about 18 months
FUTUREEFFORTS
Using improved techniques
To develop accurate assessments on how to give relief
Post disaster assessments being followed by a recovery framework (includes policies, financial techniques etc.)
Specific analysis of damages and losses of the needs of the at risk groups

Allen.K“TheChallengesofPost-disasterdesign”PublishedMay2013.AccessedMarch2024.
In order for a region to effectively carry out post disaster relief, governments should be able to perform accurate damage reports in order to effectively pinpoint areas that need the most attention.
WHOISAFFECTED? PROFESSIONALOPINION
~A.
CILKE, BSPS SENIOR
[HEALTHCARE IN A RESOURCE-LIMITED ENVIRONMENT, SPRING 2024]
30
CORRECTIONAL FACILITIES
BACKGROUNDINFORMATION
Correctional facilities, including state and federal prisons and juvenile facilities, detain individuals convicted of crimes. Despite legal obligations under the 8th Amendment, healthcare provision in these facilities often falls below adequate standards due to limited resources, understaffing, and systemic issues. This has led to three main challenges within prison healthcare systems:
Non-Communicable Diseases (ex. increased rates of hypertension and asthma, limited availability).
Communicable Diseases (ex. HIV/AIDS, sexually transmitted infections (STIs).
Mental Health
ASAGLOBALHEALTHISSUE

Healthcare in correctional facilities is a global health concern, impacting incarcerated populations worldwide. Both Europe and the United States struggle with high rates of chronic conditions, mental illness, and substance dependence among inmates. In Eastern European and Central Asian countries, resource constraints and policy gaps result in suboptimal health outcomes for prisoners.
WHOISAFFECTED?
Limited healthcare in correctional facilities exacerbates health disparities for marginalized communities, including ethnic minorities, socioeconomically disadvantaged individuals, and those with pre-existing conditions, leading to disproportionate rates of untreated illnesses and preventable deaths.
CURRENTEFFORTS

Current efforts to address healthcare in correctional facilities emphasize the implementation of comprehensive health promotion strategies and the adoption of a whole-prison approach. Such efforts have resulted in reduced recidivism rates; with Norway having a recidivism rate of 20% compared to the United States’ rate of 76.6%.
Examples:
Inclusion of art programs and smoking cessation programs.
Enrolling inmates in medicare programs to ensure healthcare once released.
FUTUREEFFORTS
Healthier Dietary Options: Tailoring menus to inmates' nutritional needs can alleviate chronic conditions and contribute to overall well-being.
Cost Containment: Partnering with third-party administrators (TPAs) allows institutions to leverage existing provider networks, reducing healthcare expenses while maintaining quality.
Increasing Use of Technology: Utilizing telehealth services for healthcare delivery in prisons eliminates security risks by allowing prisoners to receive treatment within their cells, reducing the need for transportation and escorting, which can also expedite medical attention.
PROFESSIONALOPINION
Limited healthcare in prisons is not just a matter of policy or legal obligation; it's a profound moral failing of our society. We must prioritize the health and well-being of all individuals, regardless of their circumstances, and work towards systemic reforms to ensure equitable access to healthcare for those within correctional facilities.
-J. JOHNSON, BSPS SENIOR
[HEALTHCARE IN A RESOURCE-LIMITED ENVIRONMENT, SPRING 2024]
31
TOURISM & TRAVEL
Author: Brynnlee Walters, BSPS Senior
BACKGROUND INFORMATION
Medical tourism is defined as “travel primarily for the purpose of receiving healthcare” and carries many risks such as infectious disease transmission, difficulties obtaining follow-up care, and communication gaps.
Plastic surgical expertise is concentrated in urban areas where surgeons may use their skills for cosmetic purposes or other more lucrative interventions, rather than to decrease the burden of disease in the far more populous rural regions.
AS A GLOBAL HEALTH ISSUE
There are a number of global diseases that lead to problems requiring plastic and reconstructive intervention such as Noma, which has a 90% mortality rate, and cleft lip and palate (CLP).
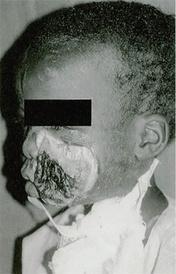
MimiRBorrelli.Figure4,African childwithnomaoftheleftcheek. doi:10.29252/wjps.7.3.275. PublishedNovember2018. AccessedMarch2024.
Currently, there are 4,000,000 untreated CLP patients worldwide. CLP increases perinatal mortality and risk of malnutrition, infection, and speech and feeding problems. There is a lack of knowledge relating to surgical intervention and access to treatment is severely limited in the developing world.
WHO IS AFFECTED?
Everyone! Whether you are on a cruise ship, an airplane, or receiving treatment abroad, you are affected. Additionally, things like war and natural disasters contribute to the greatest surgical burden, but low and middle income countries lack the funding and healthcare infrastructure to meet the need.
Global Disease
Over 100 plastic surgery non-profit associations have been founded, aiming to increase plastic surgical services for people in the developing world.
Development of healthcare infrastructure by empowering medical staff, improving education, and training of in-country personnel, and construction of new units.
Education of patients following their procedure; this had led to a decrease in lip wound infections after a CLP repair.
Medical Tourism
Some physicians choose to not proceed with a procedure if there are not proper post-treatment arrangements for when the patient arrives back in their home country.
FUTURE EFFORTS
Transparency about the risks and challenges patients may face when receiving treatement abroad.
Development of technology required for proper post-operative care. This includes telemedicine integration. Development of a globally recognized accreditation system that evaluates facilities based on factors such as infrastructure, medical expertise, safety protocols, and patient satisfaction.
PROFESSIONAL OPINION
Before opting for medical treatment aboard, individuals should thoroughly research and consider factors such as the reputation of the healthcare facility, qualifications of medical professionals, accreditation standards, travel logistics, potential risks, and post-treatment care arrangements.
-B. WALTERS, BSPS SENIOR
CURRENT EFFORTS
[HEALTHCARE IN A RESOURCE-LIMITED ENVIRONMENT, SPRING 2024]
32
REFERENCES
EDUCATIONAL
Hudon C, Loignon C, Grabovschi C, et al. Medical education for equity in health: a participatory action research involving persons living in poverty and healthcare professionals. BMC Med Educ. 2016;16:106. Published 2016 Apr 12.doi:10.1186/s12909-016-0630-4
Ko M, Heslin KC, Edelstein RA, Grumbach K. The role of medical education in reducing health care disparities: the first ten years of the UCLA/Drew Medical Education Program. J Gen Intern Med. 2007;22(5):625-631. doi:10.1007/s11606-007-0154-z
Li B, Huang Y, Ling C, Jiao F, Fu H, Deng R. The effect of community-based health education programs on health literacy in severely impoverished counties in Southwestern China: Results from a quasi-experimental design. Front Public Health. 2023;10:1088934. Published 2023 Jan 10. doi:10.3389/fpubh.2022.1088934
GEOGRAPHICAL
Neuendorf S, Neuendorf J, Yakub M. Origin, Impact, and Solutions for Lifestyle-Related Chronic Diseases in Samoa and American Samoa. Cureus. 13(9):e17749. doi:10.7759/cureus.17749
Avenue 677 Huntington, Boston, Ma 02115. Adult Obesity. Obesity Prevention Source. Published October 21, 2012. Accessed March 27, 2024.
Healthcare Access Disparities among Rural Populations in the United States. Ballard Brief. Accessed March 27, 2024.
Chronic Disease & Rural Health Disparities | RTI Health Advance. Published January 17, 2023. Accessed March 27, 2024.
Singh GK, Siahpush M. Widening Rural–Urban Disparities in Life Expectancy, U.S., 1969–2009. American Journal of Preventive Medicine. 2014;46(2):e19-e29. doi:10.1016/j.amepre.2013.10.017
Addressing health inequities among people living in rural and remote areas. Accessed April 8, 2024. https://www.who.int/activities/addressing-health-inequities-among-people-living-in-rural-and-remote-areas
POST-DISASTER
FEMA. “National Disaster Recovery Framework.” Www.fema.gov, 7 Sept. 2022, www.fema.gov/emergencymanagers/national-preparedness/frameworks/recovery.
Gharib, Sarah El . “5 Ways War Impacts Global Health.” Global Citizen, 7 Apr. 2022, https://www.globalcitizen.org/en/content/how-war-impacts-global-health/.
Leitmann, Joe. “Five Ways to Do Better Post-Disaster Assessments.” World Bank Blogs, 24 Aug. 2018, blogs.worldbank.org/en/sustainablecities/five-ways-do-better-post-disaster-assessments. Accessed 27 Mar. 2024.
“Reconstructing Health Medical Services after Natural Disasters.” Utilities One, utilitiesone.com/reconstructing-health-medical-services-after-natural-disasters.
Salam, Abdus, et al. “The Impact of Natural Disasters on Healthcare and Surgical Services in Low- and Middle-Income Countries.” Annals of Medicine and Surgery, vol. 85, no. 8, 6 July 2023, pp. 3774–3777, https://doi.org/10.1097/MS9.0000000000001041.
CORRECTIONAL FACILITIES
Udesen, Caroline. Edited by Lars Møller et al., Prisons and Health, www.unodc.org/lpomex/uploads/documents/Publicaciones/Prevencion-del-delito-y-justiciapenal/2014_WHO_UNODC_Prisons_and_Health_eng.pdf. Accessed 25 Mar. 2024.
McLeod, Katherine E, et al. “Global Prison Health Care Governance and Health Equity: A Critical Lack of Evidence.” American Journal of Public Health, U.S. National Library of Medicine, Mar. 2020, www.ncbi.nlm.nih.gov/pmc/articles/PMC7002953/.
TOURISM & TRAVEL
Borrelli MR. What Is the Role of Plastic Surgery in Global Health? A Review. World J Plast Surg. 2018;7(3):275-282. doi:10.29252/wjps.7.3.275
Moghavvemi S, Mogan K, Ghazali EM. The issue, challenges and risk of post- surgery treatment abroad among medical tourists from doctors’ perspective. Journal of Quality Assurance in Hospitality & Tourism. Published online September 27, 2023:1-32. doi:10.1080/1528008x.2023.2262142
[HEALTHCARE IN A RESOURCE-LIMITED ENVIRONMENT, SPRING 2024] 33
HealthIntheMedia
Health in the media is a broad area encompassing various topics including but not limited to medical misinformation, the portrayal of the “ideal body image” by various celebrities and public figures, the marketing of drugs (unique to the United States), the often controversial supplement industry, and giving the public the opportunity to constructively debate various health topics and issues.
By understanding and researching the aforementioned topics, one is able to build a comprehensive idea of the role that the media plays in healthcare (both positive and negative) which allows people to make more informed decisions about their health to lead healthier and more fulfilled lives.
This includes a deeper dive into the supplement industry and how the media has led to the of this unregulated industry, drug marketing and the negative effect this has on patient-physician relationships, medical misinformation, body image, and finally how the media can be valuable to encourage debate and discussion to debunk medical misinformation and discuss ambiguous topics.
Issue,Spring2024
HEALTHINMEDIA 34

TheSupplementIndustry
While the FDA tightly regulates the manufacturing, sale and R&D of drugs and other products, it seems to have taken a much more relaxed approach with regards to supplements. In recent years, there has been a rise in so called “cure all supplements” which oftentimes make unsubstantiated and unverified claims about the benefits of their products. Additionally, these companies have been known to shell out exorbitant amounts of money on marketing, recruiting A-list celebrities to convince the masses to take products that are not only unproven, but also expensive and potentially dangerous. This relates to Health in the Media overall as the majority of sales are made online on social media platforms when large celebrities endorse them.
ExtentoftheProblem
Firstly, it is important to create a distinction between these “trend” supplements and those that can be beneficial to people. The latter include dietary supplements that are often prescribed by physicians to mitigate deficiencies or help prepare for physical events such as pregnancy or puberty. However, this does not make up for the unregulated nature of the industry. The number of dietary supplements on the market has increased from 4,000 in 1990 to over 90,000 in 2014 with a whopping 55 million Americans using them instead of drugs and OTC medication which can be attributed to the claims that they make.
NegativeEffects:
UnvalidatedClaims:
The claims that Supplement companies have been making over the past few years have lead to the FDA sending out over 5 warning letters (enforceable) to help reign in the situation. Unvalidated claims about disease prevention and quality of life improvement have led to 55 million Americans completely replacing medications with supplements.
NoBarrierstoEntry:
One of the most dangerous aspects of the supplement industry pertains to its lack of barriers to entry. In theory, anyone could create a concoction in their garage, slap a label on it and sell it as a dietary supplement with little to no effort. This is incredibly dangerous as it opens the door for anyone, educated or not to create and sell potentially harmful substances.
StigmatizesPotentiallyBeneficialSupplements:
While much of the industry can be scrutinized due to the lack of regulatory oversight, it is important to note that the existence of dietary supplements is essential to many. Almost 30% of Americans report using supplements regularly for deficiencies that necessitate them. Many doctors are also known to prescribe supplements to their patients (70%).
RulesandChanges
CurrentRegulations
FDA does not actively regulate dietary supplements hence the meteoric rise since 1990. The FDA only ensures that labels explicitly state that the claims are not verified by the FDA.
Whatisneeded?
The federal government needs to mandate the FDA to regulate multi-ingredient supplements that make claims about their potential benefit.
Personalopinion-YoussefMorad
While supplements are beneficial to some, it is essential that we educate people about their potential risks. The fact that such a large percentage of the American population uses them on a regular basis, as well as a large proportion of people uses them instead of drugs is risky and scary. Part of this should include regulation on the production and marketing of these drugs to ensure that people are receiving accurate information and safe to consume supplements.
References
1. StarrRR.TooLittle,TooLate:IneffectiveRegulationofDietary SupplementsintheUnitedStates.AmericanJournalofPublicHealth. 2015;105(3):478-485.doi:https://doi.org/10.2105/ajph.2014.302348
3.
WehlanderB.“Unregulatedsupplementindustry”needsmore transparency,warnsEthicalIncfounder.nutritioninsight.com/. PublishedJune22,2022.AccessedMarch28,2024. https://www.nutritioninsight.com/news/slap-a-label-on-and-sell-as-aneffective-supplement-industry-stresses-fda-regulations.html
2. AMA.Dietarysupplements:Underregulated,unknownandmaybe unsafe.AmericanMedicalAssociation.PublishedMay11,2022. https://www.ama-assn.org/delivering-care/public-health/dietarysupplements-underregulated-unknown-and-maybe-unsafe
Youssef Morad, BSPS student Issue,Spring2024
HEALTHINMEDIA
35
DrugMarketing
Drug advertisements are one of the most widely viewed forms of health media. Drug advertising and marketing occurs globally, however there are different rules and regulations between countries and regions. Virtually all countries required drug advertisements to present the risk information, not have false or misleading claims, and not promote off-label uses. Most countries also only allow drug advertisements to be marketed to providers or pharmacists. The only two countries that allow this direct-toconsumer marketing are New Zealand and the United States.

unique to only two countries, New Zealand and the United States. Because US pharmaceutical ads could be viewed close to the border in Canada, the country has partial DTC marketing which allows the advertiser to only state the indication or the drug name, not both.
EffectsofDTCM
CostofPrescription Drugs
Consumers bear the cost of drugs. From 1997 to 2007, spending on drugs in the US tripled. In 2015, US consumers spent $1000 per person on prescription drugs, with the next closest nation being Switzerland with $783 per person.
Morepeopleseeking care
In a 2004 FDA survey 88% of patients that had seen a drug ad and asked their provider about the drug had a condition for which the drug was indicated. In fact, DCTM increases sales for the entire drug class, not just the brand products. This can increase treatment rates for chronic diseases.
Patient-Provider Relationship
Many providers believe DTCM causes the patient to ask for specific medications that they might not need and change the prescribing practices. Providers said DTCM leads to them spending more time with patients, however, patients find more time with their provider to be a positive effect.
FDA regulations
Bans violate US 1st Amendment
AU, South America, Asian Countries, and EU ban DTCMTechnical System Support
FurtherEfforts
Increase FDA funding
In 2004, 32% of ads were reviewed before they aired
In 2006, the FDA had less than 6 employees to review 15,000 ads
Providers should be discuss generic treatment options with patients Requiring cost information and decreasing restrictions on DTCM in banned areas could increase treatment rates for chronic diseases by informing patients ~SJones
References
DonohueJM,CevascoM,RosenthalMB.ADecadeofDirect-toConsumerAdvertisingofPrescriptionDrugs.NewEngland JournalofMedicine.2007;357(7):673-681.
doi:https://doi.org/10.1056/nejmsa070502
RobinsonAR,HohmannKB,RifkinJI,etal.Direct-to-consumer pharmaceuticaladvertising:physicianandpublicopinionand potentialeffectsonthephysician-patientrelationship.Archives ofInternalMedicine.2004;164(4):427-432.
doi:https://doi.org/10.1001/archinte.164.4.427
VentolaCL.Direct-to-ConsumerPharmaceuticalAdvertising: TherapeuticorToxic?.PT.2011;36(10):669-684.
Stuart Jones, BSPS student HealthinMedia, Spring2024
HEALTHINMEDIA
36
MedicalMisinformation
BeiyunWang|BSPS student
Medical misinformation is a pervasive problem. The widespread availability of information on the internet and social media platforms continually exposes individuals to health-related content, much of which can be inaccurate and misleading.

This subtopic will focus on how the ease of publishing and sharing information online contributes to the proliferation of misinformation, and the negative effects of misinformation in media can have on public health.
Howmisinformation appear?
CommercialInfluence
Some people or organizations purchased paid promotion services on social media platforms. These platforms use algorithms to promote content that is likely to appeal to users, often content that aligns with their existing beliefs and interests.
Anonymityoftheinternet
Anyone with an internet connection can create and share content online, regardless of their expertise or credibility. The anonymity of the internet can embolden individuals to share misinformation without fear of repercussions.
ConfirmationBias
People may be more likely to accept and share information that aligns with their existing beliefs or biases, even if it lacks scientific validity. This confirmation bias can perpetuate the spread of medical misinformation.
Negativeeffects
Misinformation can be produced and widely spread, allow it to have a large audience before facts are verified or disproved. As a result, people may make uninformed decisions about their health, engage in risky behaviors.
ErosionofTrustin HealthcareProviders
Immunizationcoverage decrease
According to official data published by WHO, The percentage of children receiving three doses of the vaccine against diphtheria, tetanus, and pertussis (DTP3) dropped by 5 percentage points between 2019 and 2021. This decline translates to 25 million children missing out on one or more doses of DTP.
PersonalOpinion
Addressing medical misinformation on the internet requires a multi-faceted approach.As individuals, we can learn how to identify and avoid sharing health misinformation. Engage with our friends and family on the problem of health misinformation. ~ B. Wang
References WangY,McKeeM,TorbicaA,StucklerD.SystematicLiteratureReviewontheSpreadofHealth-relatedMisinformationonSocialMedia.SocSciMed. 2019;240:112552.doi:10.1016/j.socscimed.2019.112552 Suarez-LledoV,Alvarez-GalvezJ.PrevalenceofHealthMisinformationonSocialMedia:SystematicReview.JMedInternetRes.2021;23(1):e17187.Published2021 Jan20.doi:10.2196/17187
HEALTHINMEDIA
Individuals may question the credibility and reliability of medical advice provided by experts.
Issue, Spring 2024
37
HEALTHINMEDIA BodyImage
EmilyCmarik|BSPS student
With almost constant exposure to some form of media, billions of people around the world every day are faced with ad campaigns, celebrities, and influencers that represent the “ideal” body standard of how a healthy person should look. The pressure caused by this constant bombardment can weigh heavily on the minds of teenagers and adults alike, resulting in unhealthy habits and decreased mental health for people all across the world.

NegativeEffects
TeenSelf-Esteem
With as much exposure to ads and social media as pre-teens and young adults get in the modern age, they have a strong grasp on what physical characteristics are viewed as attractive. At this young age, they are particularly susceptible to feeling insecure about physical appearance, resulting in low self-esteem and body dysmorphia.
CosmeticsCraze
With the now common practice of using filters and photoshop to touch up pictures on social media, the cosmetic industry has been steadily on the rise. Aging is out of fashion, leading to 15-step skin care routines that can sometimes do more harm than good and unnecessary cosmetic surgeries that can be dangerous and even fatal.
DangerousDiets
Countless unsustainable and unsafe fad diets and exercise routines have been promoted across media platforms for as long as media has existed, marketed as sure-fire ways to reach a person’s ideal body goals.
Solutions
Limit screentime for children and teens.
Encourage positive self-talk with young people.
Discourage the use of filters and photo editing.
Normalize having an average body type.
Broaden body type representation in the media. Research the safety of a particular diet before attempting it, and don’t set unrealistic expectations.
TheMedia’s InfluenceonBody Image
Body image includes the thoughts, feelings, and perceptions related to one’s body, perceived attractiveness, and self-worth. This sense of self develops within the context of what societal norms consider to be attractive and desirable. The body types that are commonly represented in the media have a huge role in influencing what this standard of health and beauty is across the world, often showing body types that are rare and difficult to attain.
RelatedStudies
A 2019 study in the UK showed that 64% of the 14-year-old female participants who spent more than 5 hours a day on social media have low selfesteem vs. the 39% of girls who used it for less than an hour per day.
The global cosmetics market has increased at an annual rate of about 3.9% from 2000-2022, which includes the 8% decrease in 2020, without which would raise the rate to ~4.4% annual growth.
The #WhatIEatInADay trend, though unassuming, can be dangerous. There are no one-size-fits-all diets, so when people show that they are eating at a calorie deficit, this could lead to an eating disorder for someone who tries to replicate the diet for themselves.
PersonalOpinion
The impact that the media (both social and nonsocial) has on body image is a world-wide issue that needs to be addressed, especially at a young age. Health is not defined by how a person looks. Representing the ideal body throughout media as a nearly impossible standard for people to reach only leads to people taking up unhealthy practices in hopes of achieving this. ~E. Cmarik
2.
doi:https://doi.org/10.1016/j.eclinm.2018.12.005
1. Mills JS, Minister C, Samson L. Enriching sociocultural perspectives on the effects of idealized body norms: Integrating shame, positive body image, and self-compassion. Frontiers in Psychology. 2022;13. doi:https://doi.org/10.3389/fpsyg.2022.983534
Kelly Y, Zilanawala A, Booker C, Sacker A. Social Media Use and Adolescent Mental Health: Findings from the UK Millennium Cohort Study. EClinicalMedicine. 2019;6(2589-5370):59-68.
Issue, Spring 2024
38

DEBATEANDDISCUSSION
Emma Simmons | BSPS student
Debate and discussion in health media can take on a variety of forms. Whether it is through news outlets like TV channels and online articles or through popular social media platforms such as TikTok or X (Twitter), these conversations bring about a myriad of perspectives, influenced and shaped by many factors. It is important to identify these factors so that these debates and discussions can be conducted in a constructive manner in which all sides can be heard.
ALOOKINTODEBATESONLINE
Debates and discussions can look very different between healthcare professionals and the average person. Even then, factors like cultural background and education can affect the way information is presented and interpreted. However, as pointed out earlier, some debates can be skewed due to circulating media sources such as misinformation and disinformation.
SOURCESAND FACILITATION
Popular Themes
Kington et. al. (2021) conducted several discussions with the National Academy of Medicine (NAM) and noted several themes when it comes to validating sources: a need for a concrete system to evaluate, a need to consider the constant evolution and improvements in the healthcare field, and a need to emphasize cultural compentence.
Online Platforms
Various platforms facilitate the way people can express their opinions, however it is often times limited. Information becomes easier to digest if presented correctly, however. Misinterpretations and misrepresentation becomes more common due to the limited space individuals have to express and share information with others.
Existing Solutions?
Solutions can vary given the actual topic an online debate may be surrounding. Usually, we can look towards dedicated forums to facilitate and to keep more focus on a particular topic compared to general social media apps. Information and education backing up these debates can also come from continuing education programs that help better the understanding of other factors (listed on the right).
Media versus Professional INFLUENCESON DEBATE
Disagreement can come about when it comes to intentions of sharing information. News stations have focused more so on sensationalism rather than informative; something in which scientists and experts have issues with as some important health topics may go unnoticed simply because it is not “popular.”
Cultural Influence
Cultural competence refers to the awareness and acknowledgement of the differences that many have in values, beliefs, and viewpoints that are influenced by their cultural experiences and upbringings . A lack of this can negatively influence many debates and discussions, especially in health media.
Variable Quality
It is easier for professionals to validate certain sources due to educational background and familiarity with terminology. For the layman, this becomes more difficult as many may not know where to look exactly, as in they are not aware of which search engines and sites are reliable.
source(s): Warde F, Papadakos J, Papadakos T, Rodin D, Salhia M, Giuliani M. Plain language communication as a priority competency for medical professionals in a globalized world. Can Med Educ J. 2018;9(2):e52-e59. Published 2018 May 31. AMA J Ethics. 2018;20(11):E1059-1066. doi: 10.1001/amajethics.2018.1059.
ISSUE,SPRING2024
IN
HEALTH
MEDIA
39
PEDIATRICS: ISSUES & SUCCESSES
INTRODUCTION
The pediatric population in healthcare consists of infants, children, adolescents, and young adults from birth up until the age of 21. A large portion of the worldwide population falls within this category and are therefore affected by the topics discussed below. They represent a vulnerable population due to age, mental capacity, and dependence on caregivers so there are numerous restrictions and regulations that are in place to protect these age groups, which in itself creates some challenges, However, their age may also provide some benefits since their bodies are quickly growing and regenerating itself thus setting them up for better success against diseases and illnesses that could be potentially fatal in adults.
One growing concern that has become increasingly debated about is the use of gene editing technology in the treatment of genetic disease and disorders within fetuses. With the growth and improvement of modern technology, physicians and parents are able to determine whether a child will be born with a specific genetic disease.
Another issue is that there is currently a lack of drug development for treatments targeted against specifically pediatric illnesses or diseases because of the numerous restrictions and ethical issues that come into play.
However, an interesting trait of pediatric patients is the resilience they display throughout their treatment of disease that often give them better outlooks on prognosis and chances of recovery.
While some form of a support system is important for any patient trying to recover, family support plays a critical role in the successful recovery and treatment of pediatric patients since they are in critical periods of development and growth.
Finally, deciding whether to pursue quality or quantity of care for terminal pediatric patients remains a highly debated topic with little guidelines to aid parents and physicians in the decision-making process. Figuring out what course of action is in the best interest of the patient is where the challenge arises, especially since there are so manybarriers to overcome. While the physician maymake recommendations, this ultimately leaves the decision-making process completely in the hands of the parent or guardian. To ensure that the child receives the highest quality of life possible, it is vital that parents/guardians and physicians work together so that they can make the best choices for the child.
SPRING 2024
40
Riley Smith, BSPS student
GENETIC DISEASES & DISORDERS

Background
With increases in the sophistication of technology, genetic engineeringhas become apossible treatment for many hereditary diseases. Parents are now able to find the chances of their unborn child having a genetic disorder. However, this technology raises ethical questions on whether gene editing should be legally allowed for use in these instances to prevent the child from ending up with such a disease. This ethical dilemma has left many scientists unsure of the future of gene editing, and whether it should be further honed.
Intercultural/Global Issue
Manycountries arebeginningto discuss thepossible implications of genetic engineering and how its use could affect society in both positive and negative ways. While its use for the treatment of hereditary diseases is regarded as groundbreaking, many countries and legislators are wondering how to prevent its use from transitioning to eugenics.
Those Affected
Those affected are mainly unborn children who are likely to develop hereditary diseases. Parents of the children are also affected, as theyare the ones taking responsibility for the decision of whether to treat or not.
Possible Solutions
A possible solution to prevent the use of genetic engineeringforreasons otherthanhereditarydisease would be establishing laws and/or guidelines to distinguish whengeneeditingwould benecessaryor not.
Opinion
I believe genetic engineering could become a very widespread and effective technology to cure hereditary diseases, but it is a very slippery slope. We must make sure gene editing does not become a technique used to enhance the aesthetics or physical qualities of one’s child. ~ R. Smith
References:
Genetic Engineering-Genetic Engineering – National 5 Biology Revision - BBC Bitesize.“ BBC News, BBC, 2 Mar. 2023 www.bbc.co.uk/bitesize/guides/zqqs2nb/revision/1.
Joseph, Andrew M, et al. “Ethical Perspectives of Therapeutic Human Genome Editing from Multiple and Diverse Viewpoints: A Scoping Review.” Cureus, U.S. National Library of Medicine, 27 Nov. 2022
www.ncbi.nlm.nih.gov/pmc/articles/PMC9793437/.
41
DRUG DEVELOPMENT: LIMITATIONS & CHALLENGES
Sriya Nagubandi, BSPS student
Background:
Pediatric children and neonates are often still largely neglected in terms of new drug development and because of this don’t have drugs created specifically for them, but rather take drugs created for adults that have been scaled down for their age and demographic. This issue occurs because pediatric populations represent an extremely broad maturational range both physiologically and psychologically and that causes conditions that affect this population and the factors that influence drug pharmacokinetics and pharmacodynamics to be highly varied. There are also ethical issues surrounding pediatric children's consent for clinical trials, and these factors lead to wasted opportunities for children with diseases.
Intercultural/Global Issue:
A global issue related to drug development designed for the pediatric population is the number of off-label prescriptions. Currently, up to 60% of treatments that are prescribed for children are not approved for pediatric use but are rather off-label prescriptions and this number reaches 90% when it comes to neonates. While off-label medicine may provide the best available intervention for a patient, as well as the standard of care for a particular disease, it has many challenges associated with it. Challenges arise because drug solubility and absorption in children is impacted by smaller gastric fluid volumes compared to adults, and organ maturation in young patients changes rapidly over time. These differences make it difficult to make dosing recommendations and this could lead to higher risk of dosing errors, adverse events, or allergic reactions in pediatric patients
Those Affected:
Pediatric patients, more specifically neonates. All pediatric patients are affected regardless of gender and nationality.
Possible Solutions:
A possible solution would be to create regulatory frameworks that encourage and incentivize drug sponsors to develop new pediatric medicines and increase the financial opportunities associated with developing pediatric medications.
Opinion:
Creating regulatory frameworks will help solve the issue of pediatric drug development. I think that is a good starting step and that coupled with other regulations regarding consent for children in clinical trials will increase pediatric drug development and can help to provide solutions to pediatric patients battling diseases. I believe that including children in clinical trials is alright if there is proper consent and a wellresearched plan of action if anything was to come up.
~S.Nagubandi
References:
Spadoni C. Pediatric Drug Development: Challenges and Opportunities. Current Therapeutic Research. Published online December 2018. doi:https://doi.org/10.1016/j.curtheres.2018.12.001
McCune S, Portman RJ. Accelerating Pediatric Drug Development: A 2022 Special Issue of Therapeutic Innovation & Regulatory Science. Therapeutic Innovation & Regulatory Science. 2022;56(6):869872.doi:https://doi.org/10.1007/s43441-022-00398-w

Pediatric Drug Development: Challenges and Opportunities
42
Background:
RESILIENCE IN PEDIATRICS
Thomas Joo, PharmD student
Patient resilience is a big factor that is often overlooked when considering the prognosis of the patients. It is especially important in pediatric patients as it can positively affect their condition and result in recovery. Resilience is defined as the ability to overcome adversity of trauma, surgery, and serious health problems. Lack of resilience can result in poor adjustment, slow recovery, disruptive behavior, and psychiatric disorder. Factors that can affect resilience include parental distress, few social contacts, poor family functioning, and low cohesion among family members. Resilience is characterized by equanimity, perseverance, selfreliance,meaningfulness, andexistentialaloneness. Since children have inadequate cognitive skills to process traumatic events, there is good social support to help them. Although patient resilience will not completely cure a disease, it can still help patients in a very unlikely or hopeless scenario.
Intercultural/Global Issue:
Factors out of the patient's control can affect their resilienceaswell.Someofthesefactorscaninclude natural disasters, lack of cohesion among family members, and poverty. Citizens of 3rd world countries with less access to basic healthcare supplies and emotional stability within their families.
Those Affected:
Pediatric patients who are estranged from their families or have no strong emotional support system.
Possible Solutions:
A possible solution to this could be to develop a system to see how close patients are to their family, and if no such figure is present provide ways for the pediatric patients to take stress off from their current condition.
Opinion:
I think this could be a good solution to the problem, but it could be a problem for underdeveloped countries where they are understaffed and do not have the resources to carry this out for the pediatric patients. ~T.Joo
References
Global Perspectives on Resilience in children and. youth - masten - 2014 - child development - Wiley online library. (n.d.).
https://srcd.onlinelibrary.wiley.com/doi/10.1111/cdev. 12205
Masten, A. S., & Barnes, A. J. (2018, July 17). Resilience in children: Developmental perspectives. Children. (Basel, Switzerland).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC60694 21/
van der Laan, S. E. I., Berkelbach van der Sprenkel, E. E., Lenters, V. C., Finkenauer, C., van der Ent, C. K., & Nijhof, S. L. (2023). Defining and measuring resilience in children with a chronic disease: A scoping review. Adversity and resilience science.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10088 629/
43
INFLUENCE OF FAMILY SUPPORT ON HEALTH
Kennist Williams, BSPS student
Background
Family support plays a crucial role in aiding pediatric patients on their journey towards recovery and well-being. The influence of family support is profound, providingnot onlyemotional comfort but also practical assistance in managing medical routines and navigating healthcare systems. Families act as pillars of strength, offering unwavering encouragement and fostering a positive outlook in pediatric patients facing challenging health circumstances. Their presence during medical procedures and treatments offers a sense of security and reassurance, alleviating fears and anxiety.Familysupport extendsbeyondthe hospital, as caregivers play a important role in implementing treatment plans, administering medications, and promoting healthy lifestyle habits at home.
Intercultural/Global Issue
Aglobalissuerelated to familysupportforpediatric patients is the lack of access to healthcare services and resources, particularly in low-income and developing countries. In many parts of the world, families may struggle to access essential medical care due to factors such as poverty, inadequate healthcare infrastructure, and geographical barriers. Socioeconomic disparities can exacerbate the impact of health issues on families, leading to increased financial strain, emotional stress, and decreased quality of life for both pediatric patients and their caregivers
Those Affected
Those affected include pediatric patients and their support systems.
Possible Solutions
A possible solution would be to invest in lowerincome countries to build better and more available healthcare systems. Another great investment would be to help families understand how to help their children during their hospital visits.
Opinion
My personal opinion is children need adult figures theyarecomfortablewith at thehospitals with them. Not only does this improve their mental health but also leads to faster recovery times and shorter hospital stays. I also think that we should find ways to help lower-income countries, so no child is left behind.
~ K. Williams
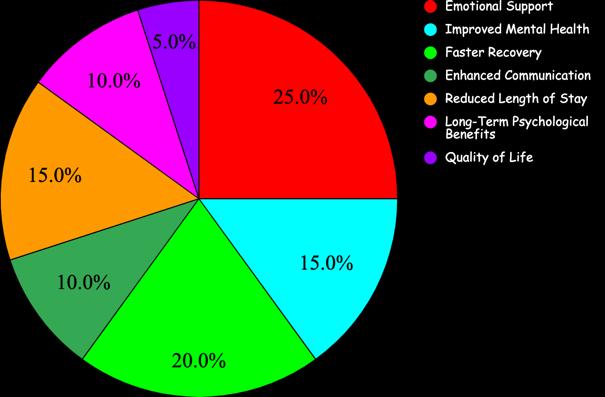

Sources
• Garcia, A. M., & Martinez, B. R. (2019). Family support and pediatric hospital length of stay: A longitudinal study. Pediatric Health Care Management, 14(1), 23-35.
• Clark, S. P., & Adams, R. D. (2017). The long-term psychological effects of family support during pediatric hospitalization. Journal of Pediatric Psychology, 42(5), 678-689.
• Johnson, M. E., & Davis, L. F. (2021). Improving communication between families and healthcare providers: The impact on pediatric hospitalization outcomes. Pediatric Nursing, 40(4), 189-198.
• Brown, L. M., & Garcia, R. S. (2020). Family presence and pediatric mental health during hospitalization. Pediatric Psychiatry, 25(2)
44
TERMINAL ILLNESSES: QUALITY OF CARE
Emily Davidson, BSPS student
Background
There are thousands of children who are diagnosed with terminal illnesses or diseases globally each year. Despite this number, there currentlyremains no set of guidelines, globally or nationally, regarding decisions that need to be made by parents and providers regarding care of pediatric patients. While there is no set age for when children or adolescents are allowed to make suggestions or contributions to the decisions being made regarding their care, whether these decisions are taken into consideration often depends on the cognitive capacity of the patient to understand their prognosis and treatment options. Furthermore, even if the patient fully understands their circumstances, their wishes may become second place compared to those of the parent/guardian since children are legally unable to make medical decisions.
Therefore, a complex issue arises in determining what medical decisions will provide pediatric patients with the highest quality of care during the end of their life.
Intercultural/Global Issue

Reference: https://www.shutterstock.com/search/d octor-checkingchild?image_type=vector

Reference: Spotlight on Pediatric Palliative Care: National Landscape of Hospital-Based Programs, 2015-16
Possible Solutions
Establishing a set of guidelines for which to guide the decision-making process for physicians regarding pediatric patients with terminal issues would help improve consistency across hospitals and cultures. Likewise, having a set structure in place may also ease the decision-making process for parents because they would be able to devote more time towards making decision regarding the child’s comfort rather than medical decisions.
Opinion
As of 2023, about 30% of the world’s population was under the age of 18 In the US, about 73 million Americans are under the age of 18. Of this number, about 5.3 million hospitalizations occur per year involving pediatric patients, and of this number, approximately 500,000 children are dealing with life-threatening illnesses with 27,000 being diagnosed each year. Hospitalizations of pediatric patients in other countries varies wildly based on a variety of factors including quality of healthcare, cultural beliefs, and access to healthcare. For example, a study found that in Spain there were 9 pediatric hospital admission for every 100 people per year while Germany had about 20 pediatric hospital admission for every 100 people per year. Furthermore, about 2000 pediatric patients die in Spain each year while only about 205 pediatric die each year.
Those Affected
An estimated 16 to 18 percent of children and/or adolescents will be diagnosed with a terminal illness of disease each, which totals to about 500,000 children in the US alone. Terminal diseases or illnesses are incurable and are predicted to lead to death. Terminal childhood illnesses not only affect the child, but also their parents and other family members. The mental and emotional toll experienced by the patient’s loved ones can be heavy and burdensome possibly leading to effects on their own health in severe cases.
Facing situations in which young children or adolescents are diagnosed with terminal illnesses and are given only a few months to live will always be difficult due to the emotions and ethics involved. However, while I know that this issue can never truly be solved due to its complexity, I think that healthcare providers should take the time to establish a general set of guidelines for physicians to follow in these situations in order to ensure that the child is able to receive the highest quality of life possible. I that these guidelines should be global so that all children would be able to access the same quality of care, but that is a big task that I don’t see being achieved in the near future. ~Emily Davidson
References
•Huang IC, Shenkman EA, Madden VL, Vadaparampil S, Quinn G, Knapp CA. Measuring quality of life in pediatric palliative care: challenges and potential solutions. Palliat Med. 2010;24(2):175-182. doi:10.1177/0269216309352418
•Santoro JD, Bennett M. Ethics of End of Life Decisions in Pediatrics: A Narrative Review of the Roles of Caregivers, Shared Decision-Making, and Patient Centered Values. Behav Sci (Basel). 2018;8(5):42. Published 2018 Apr 26. doi:10.3390/bs8050042
45

Underserved Communities
Spring 2024
Underserved communities are groups of people that have inadequate access to parts of society and healthcare. The focus of this educational document will be on the realms of underserved populations’ health care access and research representation. We will discuss the immigrant experience with US healthcare, rural populations and their access to care, the disparities women face in medical research and healthcare, implicit bias, and the effects of government corruption in the drug industry on the population.

https://www.saldru.uct.ac.za/2018/10/31/underestimating-thehealth-inequality-gap/


Immigrants face a variety of challenges in their new homes, one of which is navigating the healthcare system leading to unequal access to care. Ensuring proper access such as language services can reduce the heath disparities for immigrants.
Citizens of developing countries face unequal access to care due to the high cost of healthcare. Regulating importation and pharmaceutical industry prices as well as providing aid could prevent widespread infection and save millions of lives worldwide.
Due to geographical isolation, lower health literacy, and lower socioeconomic status, and employee shortages, residents of rural areas can find it difficult to access healthcare. Through educational programs and better funding, we can decrease the health disparities of the rural population.
While we all have them, implicit biases can be problematic in the healthcare setting and lead to negative patient health outcomes. Proper education of medical professionals on bias training can ensure better treatment for underserved communities in the healthcare setting.
Women's healthcare has a long history of disparities spanning all the way back to ancient civilizations to modern times. Sexism exists in cultures worldwide causing women to face underrepresentation in medical research and inequities in medical care. With more resources and better education on these issues there is hope for continued improvement in the future.
…
https://allea.org/health-inequalities/
46

ImmigrantAccess to Healthcare
Carter Smith (BSPS student)
Immigration can be challenging for any individual. Depending on one’s immigration status, obtaining access to proper healthcare can be a complicated process. This section will discuss reasons that immigrants might not get the same quality of care, causing them to be underrepresented in the US health care system.
Differences in Immigration Populations
There are an estimated 110 million refugees who were displaced from their country of origin due to persecution, violence or human rights violations1. These people tend to be in a more vulnerable state as they might come from areas of conflict or poverty where their access to healthcare might have been insufficient in the first place, and therefore have a higher incidence of infection or disease. Those who choose to move to another country willingly might fare better than those who are removed due to their planning and access to resources.
Literacy and Language Barriers
These are among the top reasons for an individual’s hardship for access to healthcare2. Language barriers can be common in Immigrant populations, especially those who have migrated from lower income families or refugee populations. Often, these families might not know their destination and have little autonomy because of their situation, making obtaining healthcare one of the lower priorities. Efforts to reduce the barrier might include language identifiers or use of translation applications to reduce the language barrier for those who are not native English speakers.
Navigating New Systems and Solutions
Universal healthcare systems would eliminate the issue of non-insured or under-insured immigrants, so everyone in the country is covered. Government assistance in the U.S. does exist but can be complicated to obtain and limited to who is eligible. Even without health coverage for all, resources to these populations that would inform immigrants of their healthcare coverage would help them be more confident and informed in getting the necessary healthcare. (~C. Smith)
References:
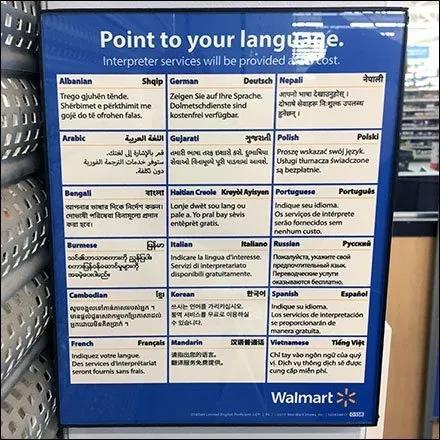
https://www.fixturescloseup.com/2022/ 09/29/retail-choose-your-languageposter/
1.World Migration Report 2022. Iom.int. Published 2022. https://worldmigrationreport.iom.int/wmr-2022interactive/#:~:text=The%20current%20global%20estimate%20is
2. Al Shamsi, H.,Almutairi,A. G.,Al Mashrafi, S., &Al Kalbani, T. (2020). Implications of Language Barriers for Healthcare:A Systematic Review. Oman medical journal, 35(2), e122. https://doi.org/10.5001/omj.2020.40
https://www.nbcnews.com/news/latino/california-considers-health-care-undocumented-immigrants-n1008201 47
https://economictimes.indiatimes.com/industry/healthcare/biotech/pharmaceuticals/cost-of-651-essential-medicines-down-7-pc-from-april-as-govtcaps-ceiling-prices/articleshow/99211856.cms?from=mdr

Developing Countries andAccess to Medicine
Frehiwot Kebede (BSPS student)
Underserved communities are populations that face challenges due to their limited access to certain resources. This makes the citizens of developing countries a prime example of underserved communities. Developing countries do not have the same access to medication or health care compared to developed countries due to the high cost of medication, private pharmacies, corruption, contraband, and the absence of medical insurance. Developing countries, like many underserved communities, suffer from the double burden of having to deal with higher rates of chronic diseases and limited resources4
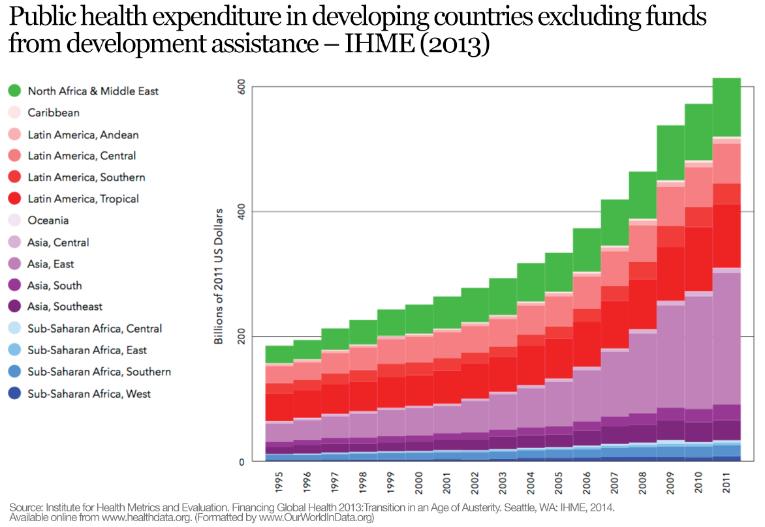
https://ourworldindata.org/financing-healthcare
Measures to Achieve Fair Access to Medication
The impact of this issue can be minimized by implementing solutions. Global health initiatives can increase funds for aid and invest money to build manufacturing facilities to avoid the costs of medication importation. Governments can enforce stricter laws to control medication and implement entry-point inspections to prevent contraband drugs from entering. Pharmaceutical companies can also offer lower prices for medication and invest in developing countries to offer employment while utilizing the natural resources to minimize costs3 Governments could also regulate pharmaceutical prices and inquire about pricing transparency.
Ripple Effect of High Cost of Medication
High medication cost is a global health concern. When certain countries cannot afford medication for infectious diseases, it can spread throughout the world and threaten the lives of millions. Because these populations are not able to treat infectious diseases effectively, bacterial and viral diseases can develop resistance that could spread worldwide, thus making it harder to treat them. Eventually, it will have detrimental effects on the funds of even developed countries to treat global health issues since national budgets need to be stretched to treat these diseases instead of other major health issues like cancer.
Affordable Medication for All
This matter is complex in nature, and no single strategy can solve the issue. My opinion on this matter is that all human beings deserve fair access to medication no matter their status or location.As someone who is from a developing country, I have seen the impact of the high cost of medication firsthand. People die every day from a simple disease because they could not afford to buy the medication. People should not be forced to choose whether to buy food or medication. I know drug discovery and development is a lengthy and expensive process, however the pharmaceutical industry is a lucrative business. Therefore, they should find a fair way to make drugs available at lower prices for underserved communities. (~F. Kebede)
3 Sykes AO. TRIPS, Pharmaceuticals, Developing Countries, and the Doha Solution. Chicago Journal of International Law. 2002;3:47. https://heinonline.org/HOL/LandingPage?handle=hein.journals/cjil3&div=9&id=&page=
4. Fazal F, Saleem T, Ur Rehman ME, et al. The rising cost of healthcare and its contribution to the worsening disease burden in developing countries. Annals of Medicine and Surgery. 2022;82:104683. doi:https://doi.org/10.1016/j.amsu.2022.104683
48
https://sdaho.org/2024/01/18/arpa-h-launches-paradigm-program-to-improve-rural-health-outcomes/

Rural Healthcare
Emmett Niemeyer (BSPS student)
Rural healthcare in America is currently facing challenges stemming from geographic isolation, socioeconomic factors, and healthcare workforce shortages. These obstacles contribute to disparities in both healthcare access and outcomes in rural areas. This intercultural issue highlights the challenges rural residents face in obtaining quality and equitable healthcare5. In this section, we will delve into the issues facing rural healthcare in the United States and efforts directed at alleviating these health disparities.
Geographic Isolation
A primary issue facing healthcare access in rural areas is a logistical one. Remote locations seldom have healthcare facilities nearby, forcing rural residents to travel long distances to receive medical care. In extreme cases, rural residents may need to travel hours to receive specialized medical care or may not have access to emergency services. Barriers such as these lead to delayed care, missed medical treatments, and worse health outcomes for rural patients6 .
Healthcare Workforce Shortages
Another factor contributing to health inequities in rural areas is the lack of healthcare workers. Rural areas encompass 20% of the US population but account for less than 10% of physicians. Rural areas may struggle to attract physicians, nurses, and other healthcare professionals due to a less desirable location, leading to understaffing. Rural residents may not receive adequate care from understaffed hospitals and may have difficulty seeing a specialist, increasing healthcare disparities in rural areas. Current efforts to alleviate this issue focus on recruiting and training residents local to rural areas to establish more healthcare professionals in these areas and government funded loan forgiveness programs7 .
I believe that addressing the rural health disparities is a challenge of both resource allocation and biases in our medical system. Rural areas deserve equitable care, and it is important we work to improve access and quality of care in these areas. Achieving these objectives will require a collaborative effort involving government, healthcare providers, and the rural communities themselves (~E. Niemeyer).
Socioeconomic Factors
Socioeconomic factors play another key role in rural healthcare disparities. Rural areas have higher poverty rates, lower educational attainment, and a higher proportion of elderly individuals. These factors impede rural residents' abilities to afford medical services and they lower health literacy.Additionally, geriatric patients may be more susceptible to certain conditions. The increase of internet access in rural areas may assist in increasing overall health literacy6 .

https://www.ers.usda.gov/data-products/chart-gallery/gallery/chartdetail/?chartId=106208
5. Coughlin SS, Clary C, Johnson JA, et al. Continuing Challenges in Rural Health in the United States. J Environ Health Sci. 2019;5(2):90-92.
6. Nielsen M, D'Agostino D, Gregory P. Addressing Rural Health Challenges Head On. Mo Med. 2017;114(5):363-366.
7. Russell D, Mathew S, Fitts M, et al. Interventions for health workforce retention in rural and remote areas: a systematic review. Hum Resour Health. 2021;19(1):103. Published 2021 Aug 26. doi:10.1186/s12960-021-00643-7.
49

Implicit Bias in the Healthcare System
Anabela Djurovic-Topalovic (BSPS student)
Implicit bias is defined as the unconscious thoughts and beliefs towards a certain group of people that influence the way we interact with said group. It is an inevitable natural product of our environments and upbringings. In a healthcare setting, such unconscious beliefs of a healthcare provider can be damaging to patients of underserved populations and result in unequal treatment or access to healthcare.
Why Should You Care?
The patient-provider interaction significantly influences a patient’s health outcomes as it impacts diagnosis, treatment, and prognosis. Yet, the quality of the patient-provider interaction is dependent on factors including the patient’s race, migration status, SES, and gender8. Unconscious bias of the provider can affect the patient’s diagnosis and treatment decisions even when controlling for symptoms and healthcare access, leading to health inequalities and disparities in the underserved populations. Underserved populations who face health inequalities and/or discrimination are less likely to trust healthcare professionals and get regular checkups, therefore exacerbating this issue8,9 .
Who is Affected?
Certain demographics that are disproportionately affected by implicit biases include females, lower SES individuals, racial minorities, and patients with opioid addiction9 Studies have shown that implicit bias in healthcare professional can lead to bias-based misdiagnoses, not disclosing information to patient, or stigmatization8 .
What Can be Done?
While implicit biases are here to stay, they are malleable. Efforts to educate future and present healthcare providers of their personal implicit biases and how to detect and navigate them have been shown to increase the quality of patient-provider interactions10 . Furthermore, increasing the diversity of healthcare staff has been shown to lower incidences of issues resulting from implicit bias.
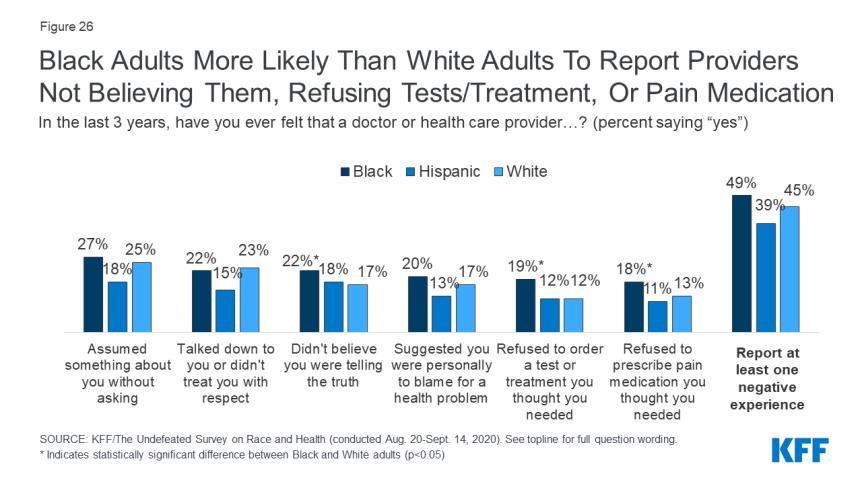
Opinion
US healthcare providers are extensively educated on scientific facts and patientcare. However, their education provides little experience with understanding and navigating diverse populations or understanding social institutions that affects our daily lives. Implicit biases are impossible to remove within healthcare. However, education and awareness of it can bring about more understanding and trust between the provider and their patient, leading to better healthcare outcomes. (~A.
Djurovic-Topalovic)
8. Timmermans S. The Engaged Patient: The Relevance of PatientPhysician Communication for Twenty-First-Century Health. J Health Soc Behav. 2020;61(3):259-273. doi:10.1177/0022146520943514
9. Williams DR, Lawrence JA, Davis BA. Racism and Health: Evidence and Needed Research. Annu Rev Public Health. 2019;40:105125.doi:10.1146/annurev-publhealth-040218-043750
10 Reddy S, Starr S, Hayes S, et al. Implicit Bias Curricula In Medical School: Student And Faculty Perspectives. HealthAffairs. Published January 15, 2020. https://www.healthaffairs.org/content/forefront/implicit-biascurricula-medical-school-student-and-faculty-perspectives https://www.kff.org/report-section/kff-the-undefeated-survey-on-raceand-health-main-findings/
50
https://easterniowahealthcenter.com/obgyn/title-x-services/attachment/diagnostic-and-cure-of-gynaecological-disease-with-stethoscope-andfemale-symbol-on-pink-background-top-view-mock-up-2/

Women’s Healthcare
Emily Wood (BSPS student)
Women across the globe struggle with disparities and inequalities, especially when it comes to healthcare In the 17th to 19th centuries, male doctors started to use the word hysteria to describe women’s health issues.11 It came from the Greek root hysteria, meaning uterus. This word was an umbrella term for female health concerns. Its negative connotation is evidenced by the present-day definition, “behavior exhibiting overwhelming or unmanageable fear or emotional excess.”12
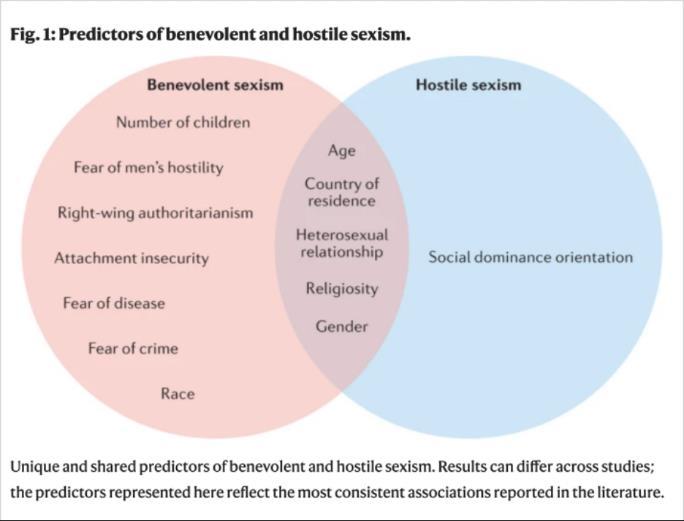
Barreto M, Doyle DM. Benevolent and hostile sexism in a shifting global context.
Nature Reviews Psychology. 2022;2(2). doi:https://doi.org/10.1038/s44159-022-00136-x
Professional Opinion
In my opinion, women need to be taken more seriously by medical professionals and more resources need to be made available to improve the quantity and quality of healthcare worldwide. These inequalities are not just a problem, they constitute a health crisis, and women everywhere are falling victim to it every single day. Without a change, the number of women who suffer potentially fatal consequences will just keep rising. (~E. Wood)
Sexism and Different Cultures
Gender-based violence encompasses everything from sexual assault to female genital mutilation, and societal norms and stigmas discourage people from seeking out care for it. In many cultures, sexist ideology is rooted in traditional beliefs and ideals.11 Cultures evolve and change over time, and advances in gender equality come along with that change. Social constructs change with time, and the more we can break down those barriers, the more progress we will make towards gender equality.
Underrepresentation in Medical Research
There is a significant research gap due to the lack of women in medical studies. Many studies especially older were primarily or exclusively done on male subjects.11 It is unreasonable to assume that the only difference between men and women is their reproductive organs our bodies behave differently, and the presentation of different health issues can vary 13 This leads to misdiagnosis or lack of needed care. Better outreach efforts, reimbursement for their time, and increased sample diversity are among the many ways that this issue can be addressed.13
Inequity in Medical Care
Access to healthcare is a major issue across the globe. Every day, 810 women globally lose their lives from preventable complications related to pregnancy and childbirth 11 Pain is also undermined and treated differently; sexist stereotypes associate women with being overdramatic. Women report pain more frequently and with higher intensity, yet do not receive equal treatment to men.11 Women also consistently wait longer for diagnoses, receive less treatment for cardiovascular diseases, and are less likely to receive life-saving CPR compared to male patients 11
11. The Deadly Inequities of Gender Bias in Healthcare | Concern Worldwide. concernusa.org. Published September 16, 2022. https://concernusa.org/news/gender-bias-in-healthcare/
12. Merriam-Webster. Definition of HYSTERIA. Merriam-webster.com. Published 2019. https://www.merriamwebster.com/dictionary/hysteria
13. Tobb K, Kocher M, Bullock-Palmer RP. Underrepresentation of women in cardiovascular trials- it is time to shatter this glass ceiling. American Heart Journal Plus: Cardiology Research and Practice. 2022;13:100109. doi:https://doi.org/10.1016/j.ahjo.2022.100109
51
Epidemiology
Maverick Tebbe, Carolina Kim, Benny Yang, Terrence Ducksworth, Jacob Paulaskas
Spring 2024
Our group's main topic is epidemiology and how diseases spread in different cultures. Different countries have different customs that affect the way diseases spread. By analyzing the determinants and outcomes of disease within populations, we can make informed decisions for future global health policies that will lead to eradication or mitigation of these diseases. Through a variety of subtopics, we can break down the facets of epidemiology of global health issues and solutions. Due to the recent COVID-19 pandemic, the world of epidemiology and its importance in society has never been illustrated more worldwide. By collaborating worldwide, we can prevent future pandemics and super viruses from occurring.
One example is the rise in antimicrobial resistance in several bacterial strains that poses a threat due to its projected mortality in the future. With little to no development of new antimicrobial therapies recently, a new therapy option, such as bacteriophage therapy, needs to be explored and possibly implemented to prevent the rising severity of this issue. Another pressing issue due to the recency of the pandemic is the pandemic response in different countries. With various strategies used, it was interesting to notice the differences in these responses and what outcomes these strategies produced. There have also been some disparities in respiratory vaccine distribution which can be highlighted by looking at the recent distribution of the COVID vaccines. Developing countries often had a harder time obtaining the vaccine which led to various issues. Furthermore, climate change has shown to be linked to increased disease spread. With these rising temperatures, mosquitoes and ticks have become commonplace in unseen areas of the spread often in a hospital setting due to lack of sterile practices or other varying factors. We wanted to look into different countries’ practices for sterilization in hospitals to prevent hospital acquired infections. All of these subtopics help paint a piece of the picture for the current landscape of epidemiology in the world.


[Epidemiology,Spring2024]
52
Antimicrobial Resistance -
Maverick Tebbe (BSPS student)
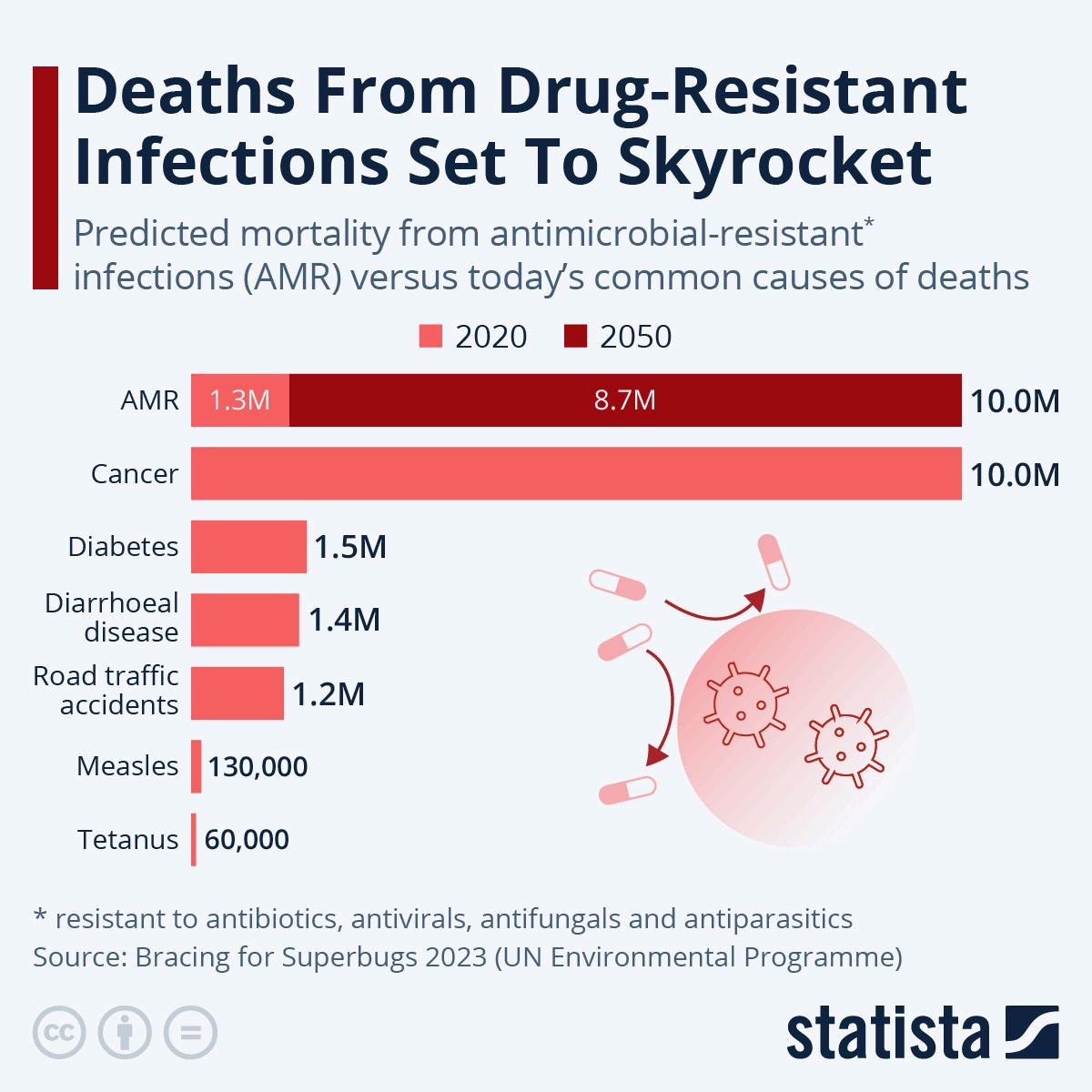
As can be seen in the graphic, antimicrobial resistance infections are projected to increase rapidly over the next 30 years. Some of the reasons that antimicrobial resistance is increasing are overuse/misuse of drugs and poor sanitation practices. The overuse of antibiotics across the world whether it be for non-bacterial infections or use in agriculture, this leads to developing more resistant strains that make these bacterial infections harder to treat. Poor sanitation in developing countries leads to non-access to clean water which increases the risk for infections and overuse of these antibiotics. On contrary many nations such as the United States, many Southeastern Asian countries allow for over-the-counter purchase of antibiotics. This OTC availability contributes to the misuse of these drugs and therefore contributes to bacterial resistance. In this case study, many doctors were interviewed about antibiotic use and mentioned how availability of these drugs heavily influenced their prescription preferences. Since antibiotics are over-the-counter, education programs need to be put in place for their countries to help stop misuse and overuse.

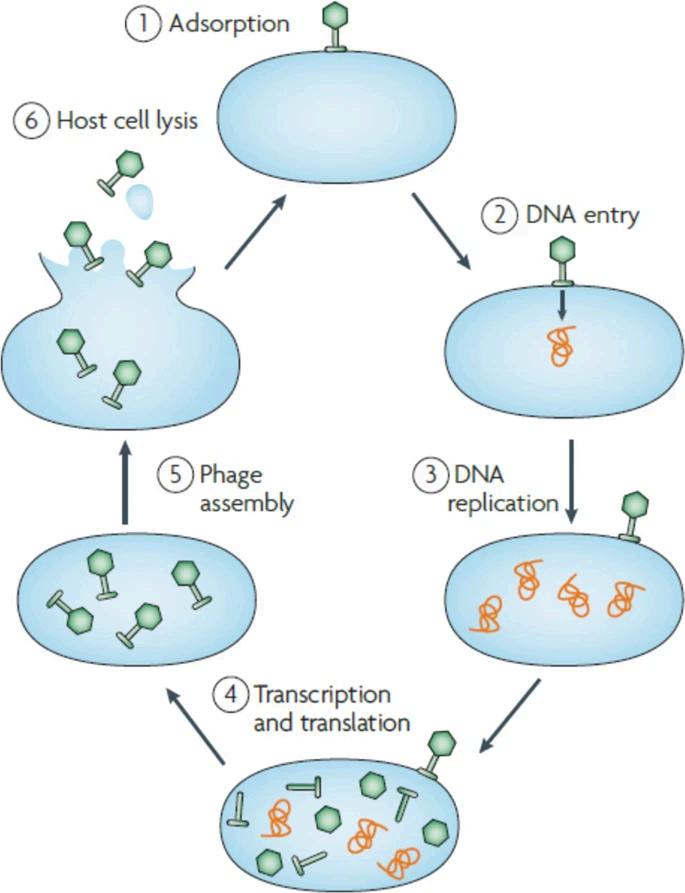
Onepotentialtherapyoptiontotreatresistantbacterialinfectionsis bacteriophagetherapy.Bacteriophagesaresmallnaturallyoccurringvirus moleculesthatareabletoinfectandreplicatewithinspecificstrainsof bacteria.Oncetheyinjecttheirgeneticmaterialtohijackthebacterial machinery,theyareabletoreplicatethemselvesandeventuallylysethe bacterialcellbyproducingenzymesthatweakenthebacterialcellwall. Afterthebacterialcellislysed,multiplecopiesofthenewlyformed phagesarereleasedandattacknearbybacterialcells.Sincetheyareso specific,bacteriophagescanbemodifiedandtailoredtowardspecific bacterialstrainstohelptreattheseinfections.Therearecurrentlynodrugs onthemarkettotreatbacterialinfectionsbutbacteriophagesare commonlyusedinfoodsafetyandagriculturalpestcontrol.
PersonalOpinion: Duetothelowprofitabilityofdevelopingnewantibiotics,Ibelievethereneedsto begovernmentinterventionsuchassubsidiesmaybeneededtopromotethisdevelopmentfornew therapyoptions.Therehasnotbeenlittletonodevelopmentofanyantibiotictherapiesinthelast50 years,andthatdemonstrateshowproblematicthisissuecanbecomeifnostepsaretakennow. ~M. Tebbe
References: Brives,C.,Pourraz,J.PhagetherapyasapotentialsolutioninthefightagainstAMR:obstaclesandpossiblefutures. PalgraveCommun 6,100 (2020).https://doi.org/10.1057/s41599-020-0478-4
HitchcockNM,DevequiGomesNunesD,ShiachJ,etal.CurrentClinicalLandscapeandGlobalPotentialofBacteriophageTherapy.Viruses. 2023;15(4):1020.Published2023Apr21.doi:10.3390/v1504102
[Epidemiology,Spring2024] 53
ThesuddenglobalriseofCOVIDhasledtourgentconcernsforhealth,economy,andgovernmentinvolvement. Inearly2020,inexperiencedcontainmenteffortsresultedinasignificantnumberofdeaths,highlightingthe importanceofepidemiologicalunderstanding. Variouscountriesresponded differentlytothepandemic,with varyingstrategiesandresources, particularlyaffectingdeveloping countrieswithlimitedresourcesand stability.Approximately186 countriesimposedrestrictions, includinglockdowns,resultingin decreasedcasesanddeaths. Developedcountriesprimarily adoptedtwomainstrategies: containment,prioritizingtestingand distancing,andmitigation,focusing onmanagingcases.AstudycomparingChina,SouthKorea,andSingapore(containment)withtheUS,UK, andFrance(mitigation)foundstrictercontainmentmoreeffective.

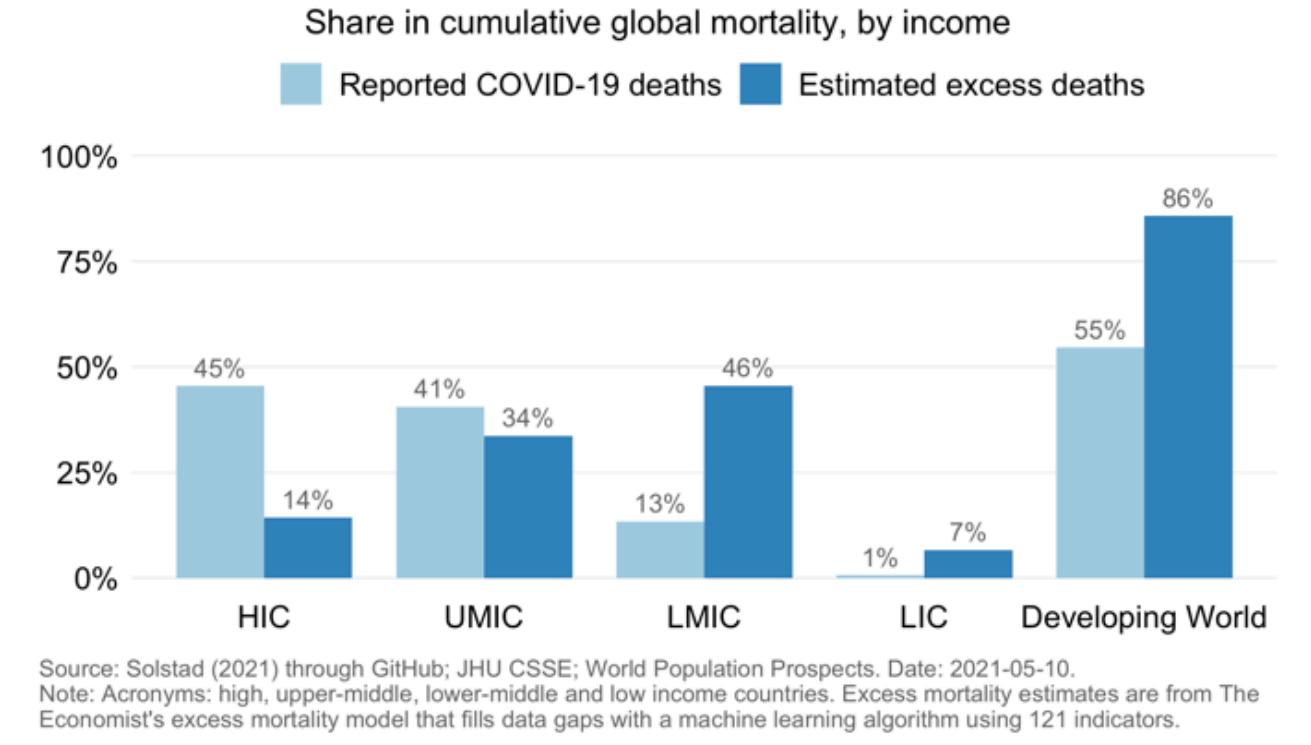
Conversely,developingcountriesfaced uniquechallengessuchasincomeloss, especiallyforvulnerablepopulations.Recent dataindicateashiftinthepandemic'simpact towardsdevelopingcountries,whichnow accountforover50%ofglobalmortality, despitehigherpercapitamortalityin high-incomenations.BrazilandPerustand outasseverelyaffectedcountriesinLatin AmericabyCOVID-19.Brazil'schallenges includePresidentBolsonaro'srefusalto acknowledgeandimplementpreventive requirements,leadingtoprotestsandconflicts withstategovernors,Congress,andthe SupremeCourt.Incontrast,Peru'sstrugglesmainlyrelatetoinadequatesupportmeasuresratherthanleadership denial.
PersonalOpinion:Inmyview,thecontainmentofthepandemicdependedsignificantlyonavailableresources, butthegovernment'sauthorityanditsinfluenceonthepopulationalsohadaconsiderableimpact.Analyzing COVIDdeathsandlearningfromsuccessfulpreventionmeasuresduringthepandemiccanenhanceour readinessforfutureoutbreaks. ~CKim
References:
ChenH,ShiL,ZhangY,etal.Responsetothecovid-19pandemic:comparisonofstrategiesinsixcountries. FrontPublicHealth.2021;9:708496. doi:10.3389/fpubh.2021.708496
ChowdhuryAZ,JomoKS.Respondingtothecovid-19pandemicindevelopingcountries:lessonsfromselectedcountriesoftheglobalsouth. Development(Rome) 2020;63(2-4):162-171.doi:10.1057/s41301-020-00256-y IndermitGillandPhilipSchellekens COVID-19isadevelopingcountrypandemic.2021. Brookings https://www.brookings.edu/articles/covid-19-is-a-developing-country-pandemic [Epidemiology,Spring2024]
Pandemic
– Carolina
Response
Kim (BSPS student)
54
Climate Change
- Terrence Omar Ducksworth (BSPS student)
For disease prediction, the direction which seems the most interesting would be how climate change will impact the occurrence of diseases across the globe. Studies have shown that increasing temperatures have already raised the rates of certain fungal infections; furthermore, there are many other pathogens which could also become more rampant with the changing global climate. There is a great interest in how changes in global climate will affect the presence of disease in populations.
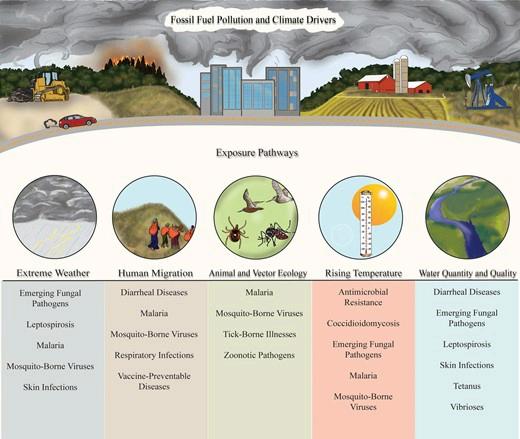
Currentlyglobalincreasesintemperaturehavebeen correlatedwithincreasesinmosquitoandtick populations.Thesetwoinsectsareprimarydisease vectorsformultipledifferentdiseases.Mosquitoes areresponsibleforspreadingmultiplediseases includingMalaria,WestNilevirus,YellowFever,and Zikavirus.Withticks,theyareresponsibleforother dangerousdiseaseslikeanaplasmosisandLyme disease.Withgloballyincreasingtemperatures coupledwithmilderwintersandlongerwarm seasons,thelengthoftheyearwhereticksand mosquitoesareactiveandthreateningpopulations withdiseasesteadilyincreaseovertime.Inaddition, highertemperatureshavebeencorrelatedtohigher bitingrateformultiplespeciesofmosquitoes,further increasingthethreatofclimatechangetowards humanpopulations.Inthepastfewdecades,the southeasternUnitedStatesexperiencedthereintroductionofseveralmosquito-bornediseasesfromsustained localizedtransmission,possiblyresultingfromanincreaseinregionaltemperatures.A speciesofinterestisthe Aedesalbopictus mosquito,whichisavectorforchikungunya,dengue,andZikavirus.Thisspeciesalready hasabroadgeographicrangethatcoversthemajorityoftheAmericansoutheastthroughtheMidwest,but globalheatingmayevenextendthisrangeasnorthasHudsonBayinCanadaandevenSouthernGreenland.
Solutions
Thechangesinbehaviorandactivityofdiseasevectorscausedbyclimatechangewillpresentrapidlyevolving challengesforhealthcaresystemsacrosstheworld.Researchershavebegundevelopingmathematicaland computationalmodelsthatwillhelppredicthowclimatechangesinregionswillinfluencediseaseincidence. Thiswillgivelocalhealthcaresystemsmoretimetoprepareandmaximizeeffectivenessofresponse.
PersonalOpinion
Whetherclimatechangeisman-madeornotisnolongerarelevantdiscussioninthecaseofepidemiology.The mainfocusinthisfieldshouldbedirectedtowardstargetinganddevelopingpredictionmodelstomitigatethe effectsofclimatechangeandhowitwillbeaffectinghumanpopulations.Inaddition,thereshouldbeamajor pushforhealthcaresystemstobeequippedtohandleanydiseasesthatmaybemoreprevalentinthefuturefar beforeitbecomesaconcern.Whiletheprocessbynaturewouldnotbeperfect,itisimportanttobepreparedfor theoncomingriseinvector-bornediseases.~TerrenceD.
References CentersforDiseaseControlandPrevention.(2022,August2). Climateandinfectiousdiseases.CentersforDiseaseControlandPrevention. https://www.cdc.gov/ncezid/what-we-do/climate-change-and-infectious-diseases/index.html
EdelsonPJ,HaroldR,AckelsbergJ,etal.ClimatechangeandtheepidemiologyofinfectiousdiseasesintheUnitedStates.OUPAcademic.September 1,2022.AccessedFebruary13,2024.https://academic.oup.com/cid/article/76/5/950/6681128.
[Epidemiology,Spring2024]
55
Respiratory Vaccines - Benny Yang (BSPS student)
Respiratory diseases, such as influenza, COVID-19, and pneumonia, represent a significant global health burden, affecting millions worldwide. However, disparities in vaccine access between higher-income countries (HICs) and lower-income countries (LICs) highlight global inequality, with HICs often benefiting from earlier and broader vaccine coverage.

LICsoftenfacebarriersduetoinadequate infrastructureandresourcescriticalforeffective vaccinedeployment.Thesechallengesinclude unstablevaccinationmanagementandinformation systems,insufficientcoldchainfacilities,limited transportoptions,underdevelopedpublichealth infrastructure,adequateserviceproviders,anda lackoffinancialsupport.Furthermore,vaccine acceptancewithinthesecommunitiesisoften lower,partlyduetoalackofaccurateknowledge aboutCOVID-19risksandvaccineeffectiveness. Misinformationandlackofaccesstoreliable healthinformationcontributetothisissue,making ithardertoachievehighcoveragerates.
WhentheCOVID-19vaccinewasreleased,HICplaced advancedordersfor4.6billiondosesoutof7.1billion doseswhichis65%ofthetotaldoseseventhoughHIC onlymakesup16%oftheworldpopulation.Onaverage, LICexperienceda90-daydelayinaccessingthefirst COVID-19vaccinescomparedtoHIC.Thesedelays causedanincreaseincasesandmortalityinLIC.Among LIC,therewasa1.92%increaseincumulativecasesfor eachday'sdelayinHIC.

TheCOVAXFacility,establishedbyWHO,GAVI,andCEPI,aimstoensureaccesstoCOVID-19vaccinesfor LMICs,collectingresourcesfromover145countries.ByDecember2020,COVAXsecured2billionvaccine doseswith$2.4billionraised,startingitsrolloutinMarch2021tocovervulnerablepopulationsinitially.The initiativeplanstoexpandtoprotectupto20%ofthepopulationsinparticipatingcountries,focusingon healthcareworkers,theelderly,andthosewithunderlyingconditions.
PersonalOpinion:LMICsmakeupalargepopulationoftheworld.Ibelievethatbyprovidingthesecountrieswithquick accesstonecessaryvaccines,spreadofdiseasecanbelimited.Also,ratherthandependonvaccinedonationsfromHICs, LMICscouldreceiveadditionalfundingfromHICstodeveloptheirownrespiratoryvaccines.~B.Yang
References: ChoiEM.COVID-19vaccinesforlow-andmiddle-incomecountries. TransactionsofTheRoyalSocietyofTropicalMedicineandHygiene.PublishedonlineMarch18,2021.doi:https://doi.org/10.1093/trstmh/trab045
DuanY,ShiJ,WangZ,ZhouS,JinY,ZhengZJ.DisparitiesinCOVID-19VaccinationamongLow-,Middle-,andHigh-IncomeCountries:TheMediatingRoleofVaccinationPolicy. Vaccines.2021;9(8):905. doi:https://doi.org/10.3390/vaccines9080905
DuroseauB,KipshidzeN,LimayeRJ.TheimpactofdelayedaccesstoCOVID-19vaccinesinlow-andlower-middle-incomecountries. FrontiersinPublicHealth.2023;10.doi:https://doi.org/10.3389/fpubh.2022.1087138 [Epidemiology,Spring2024]
56
Hospital Acquired Infections –
Jacob Paulaskas (PharmD student)
The COVID-19 pandemic put the concept of transmissible infections into the global spotlight and for over 3 years dictated how people around the world lived. Personal protective equipment (PPE) once only seen in healthcare facilities such as surgical masks, face shields, and hand sanitizer were now taken with every person just as one brought their keys and wallet everywhere. Protocols for high-level disinfection, infection screening checkpoints, and quarantine/isolation became common practice. While new to the public, these infection prevention measures have been around long before COVID-19.
Around the world, healthcare facilities of any/all kinds serve as a place of healing and hope for the sick. In a place where people of all illnesses come together, without the proper PPE and protocols these facilities can quickly allow infections to spread faster with more devastating consequences through those insides. From the top medical institutes in the USA to third-world countries struggling to vaccinate and provide basic hand hygiene supplies to their citizens, all battle to prevent infection within their facilities.
With a lack of standard record keeping and recording of HAIs between institutions and countries, it is extremely difficult for a collective study to be done on HAIs on a global scale. In May 2022, the World Health Organization (WHO) released an article entitled, “WHO launches first-ever global report on infection control”. The findings of the results include notable statistics such as 70% of HAIs can be eliminated with the implication of (what will be discussed later) infection prevention and control (IPC) protocols. These include hand hygiene and PPE, along with the safe and responsible use of antibiotics to prevent microbial resistance.

According to the analysis “Global prevalence of nosocomial infections: A systematic review and meta-analysis”, the topics of HAI prevention barriers (eg. financial, cultural, political) are discussed. The practicality of complete HAI prevention is also called into question as the nature of a healthcare facility will always include closer proximity of immunocompromised individuals with opportunistic infections.
Professional/Personal opinion: Ideas such as hand hygiene and pathogen transmission continue to dramatically underlie HAI prevention, just as they did when first introduced hypothesized, proven, and shared with the world. I believe this issue is now finding the resources to produce, distribute, provide, and educate people of all countries on HAI prevention. Until all countries can provide the best and most cutting-edge healthcare to citizens, then we cannot effectively analyze HAI prevention. (~J. Paulaskas)
Raoofi S, Pashazadeh Kan F, Rafiei S, et al. Global prevalence of nosocomial infection: A systematic review and meta-analysis. PLoS One. 2023;18(1):e0274248. Published 2023 Jan 27. doi:10.1371/journal.pone.0274248
WHO. WHO launches first ever global report on infection prevention and control. www.who.int. Published May 6, 2022. https://www.who.int/news/item/06-05-2022-who-launches-first-ever-global-report-on-infection-prevention-and-control
57
HEALTH DISPARITIES
Joseph Pham, Annie Frazier, Evelyn Zhang, Sammy Thomas, James Kim
Spring 2024
What are disparities?

Disparities are the gaps and differences that result in reduced quality of care that is typically preventable. Causes of this include socioeconomic differences, educational levels, race, ethnicity, income levels, etc.
Focus
Health Literacy:
Ability to obtain and process health information to make an appropriate decision for oneself. Inadequate health literacy create difficulties in medication adherence and communication with health professional, which could result in health disparity, increase in mortality, and increased costs.
Education:
Noting how low literacy levels in the patient population, in combination with inadequate physician connection and empathy, leads to a devastating disconnect that can inevitably harm the patient and lessen the quality of care
Accessibility:
Ensuring that patient populations globally are able to get care and treatment is vital to ensuring the growth and sustainability of communities
Affordability:
Notifying the inequalities between the rural-urban areas, China implemented a healthcare reform and introduced policies to ensure patient’s affordability for essential and innovative drugs.
Demographics:
The different demographics people identify and present with have a significant impact on healthcare outcomes both in the US and globally. This can include race, gender, socioeconomic class, age, disability, and more.
*All clipart taken from canva 59
HEALTH LITERACY
James Kim -BSPS student
Background
Health literacy is defined as the capacity to obtain, process, and understand basic health information and services to make appropriate decisions about health. Health literacy problem has arose in the early 2000s.
What issues are we facing?
Elderly population is experiencing challenges with low health literacy due to decline in physical abilities, and they are the most vulnerable population as almost 80% of age over 65 experience chronic illness.
Cultural/Language difference in the United States especially Hispanics showed lowest average level of health literacy. This specifically happens predominantly in the U.S with larger diversity.
Health literacy in global scene
Australia and U.S showed consistent policy efforts directly addressing health literacy. India, Mexico, and South Africa has no dedicated policy regarding health literacy, instead has indirect health promotion program.
Malaysia, Philippines, and New Zealand showed limited health literacy level.
South Korea and China has showed most increasing policy development.
Personal Opinion on health literacy
The key issue with health literacy mainly comes from the awareness of the problem itself. As I was also not aware of much problem associated with health literacy on health risks of the public, and the significance of the problem. To be able to solve the health disparity caused by low health literacy, governmental efforts is the most important. From the examples I have read through research, constant policy and regulation efforts are essential. More programs should be created to also focus on lifelong adult education with health literacy.
Health literacy induced economic inefficiency loss in the U.S health care 106B $~ 238B $
Hispanic in the U.S with below intermediate level of health literacy 65%
references: 1.Shahid R, Shoker M, Chu LM, Frehlick R, Ward H, Pahwa P. Impact of low health literacy on patients’ health outcomes: a multicenter cohort study. BMC Health Services Research. 2022;22(1). doi:https://doi.org/10.1186/s12913-022-08527-9 2.HEALTH LITERACY in ASIA-PACIFIC 2023 NATIONAL HEALTH LITERACY POLICIES & STRATEGIES in the REGION. https://lymphomacoalition.org/wp-content/uploads/2023_Report_Health_Literacy_In_Asia_Pacific_VF_A4_Digital.pdf 3.The Economist. Health literacy around the world: policy approaches to wellbeing through knowledge and empowerment. Economist. Published 2021. https://impact.economist.com/perspectives/sites/default/files/lon_-_es_-_health_literacy_paper_v8_0.pdf 4.America’s Health Literacy: Why We Need Accessible Health Information. Agency for Healthcare Research and Quality. Published 2008. https://www.ahrq.gov/sites/default/files/wysiwyg/health-literacy/dhhs-2008-issue-brief.pdf [Health Disparities, Spring 2024]
60
EDUCATION
Annie Frazier, BSPS Student
BACKGROUND AND SCOPE: Limited
education of both patients and physicians minimizes the overall care accessible to patients across the world, causing an extensive international health disparity
Physician Education
Emotional Training Clincal training
“[Physcians have a] moral obligation to maintain a continued awareness of patient’s beliefs, background, and values.”
Carmen G del. The patient-physician disconnect: Understanding patient values. UTHealth. 2008. Accessed March 22, 2024..
“Although the number of osteopathic and allopathic medical students requiring clerkship spots has increased, there has not been a commensurate increase in the number of clerkship spots nor has there been an increase in clinical preceptors.”
Cox WJ, Desai GJ. The crisis of clinical education for physicians in training. Missouri medicine. 2019. Accessed March 22, 2024.
SOLUTIONS
By building a reputation of understanding the patient, patients are more likely to seek and follow through on treatments, thus improving overall patient health
Required regular emotional awareness and empathy training
Restructure healthcare systems to have an empathetic, patient forward, focus to allow this mindset to continue down the chain of command
Offer reward systems for the healthcare professionals who behave empathetically
James TA. Building empathy into the structure of Health Care. Building Empathy into the Structure of Health Care | HMS Postgraduate Education. January 12, 2023. Accessed March 22, 2024.
By implementing programs that would promote more widespread, specialized clinical training, that would allow physicians to stay up to date on new techniques, treatments, and skills
Subscribe to and continually read new and credible medical journals and publications
Regularly attend medical conferences
Get physical practice with hands-on training programs
Reward self-directed education that will promote increased specialization
1HHMGlobal CT. Content team HHMGlobal. HHM Global B2B Online Platform Magazine. March 13, 2023. Accessed March 22, 2024.
Patient Education
42.3% of patients did not understand their disease condition at time of discharge 97.1% of patients did not understand common side effects of their prescribed drugs at time of discharge A study on emergency care showed:
Yadav AK, Budathoki SS, Paudel M, Chaudhary R, Shrivastav VK, Malla GB. Patients Understanding of their Diagnosis and Treatment Plans During Discharge in Emergency Ward in a Tertiary Care Centre: A Qualitative Study. JNMA J Nepal Med Assoc. 2019;57(219):357-360. doi:10.31729/jnma.4639
Personal Opinion
I believe that the major educational issue in the healthcare realm is the disconnect between patient comprehension and physician explanation. Continuing, I believe it is absolutely necessary that physicians take the time to ensure that the patients adequately understand their condition, healthcare plan, and treatment regimen before leaving the clinic/hospital. Further, providing patients with an understandable explanation at their level and additional materials that can be individually accessed and referred back to, then the patients can have the resources that will allow them to make the best decisions for their health both in the clinic and at home. ~A. Frazier
“Illiteracy in the health domain leads to problems such as insufficient use of prevention services, excessive delay in diagnosis, insufficient adherence to medical guidelines, increased risk of hospitalization, increased risk of death, and much more health-care costs”
Bayati T, Dehghan A, Bonyadi F, Bazrafkan L. Investigating the effect of education on health literacy and its relation to health-promoting behaviors in health center. J Educ Health Promot. 2018;7:127. Published 2018 Oct 29. doi:10.4103/jehp.jehp_65_18
SOLUTIONS
Direct patients to online resouces such as AMA (American Medical Association), Medlineplus, etc. to do individual research as needed
Provide patients with information packets at the time of discharge; clearly listing medications, duration/regimen, and condition summary
Speak at a level at which the patient can comprehend the information and build up understanding from there
Know the educational background and literacy level of the patients
[Health Disparities, Spring 2024]
61
ACCESSIBILITY
Joseph Pham - BSPS student
Access to Care & Medicines
Domestic (United States)
1/10 are rural physicians compared to 1/5 of US population in rural communities *1 Mississippi, Arkansas, Louisana, New Mexico, West Virginia, and Alabama have largest healthcare deserts *2
Southeast Asia (ASEAN members)
1 pharmacist per 10,000 people *3
1.1 physician per 1,000 people *4
58% of hypertensive population in Cambodia are untreated
Only 27.5% of generic/brand name drugs are available within the Philipines
DRUG SHORTAGES DUE TO LOW QUALITY
Cause of US Drug Shortage
60%
US drugs shortages were due to quality *5
“Facilities with a great number of manufacturing violations had a stastically signficiant higher likelihood of a shortage event”
-Vizient (medical and pharmaceutical supplier)
Vulnerable Supply Chain
95%
Sterile injectables rely on materials and drug substance from India and China
Incorporation of data for end-end pharmaceutical supply chain i.e Valletta Declaration May 2017 to find bottlenecks that are most at risk to prevent drug shortages
Harmonization of international pharmacuetical regulation to create a standard of quality as well as industry veterans trained with FDA and EU regulations to implement these standards
References Finster LJ, Salvy SJ, Haile RW. A cancer care desert: living in between the urban and rural and the case for defining semirural regions. Front Oncol. 2023;13:1204821. Published 2023 May 22. doi:10.3389/fonc.2023.1204821 1. Loccoh EC, Nguyen A, Kim G, Warraich HJ. Geospatial Analysis of Access to Health Care and Internet Services in the US. JAMA Netw Open. 2022;5(11):e2243792. Published 2022 Nov 1. doi:10.1001/jamanetworkopen.2022.43792 2. Singh PK. Access Medical Products in the south-East Asia Region 2023. World Health Organization. 2023. Accessed February 15, 2024. 3. Physicians (per 1,000 people) - east asia & pacific. World Bank Open Data. Accessed March 7, 2024. https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?end=2007&locations=Z4&start=2007&view=map. 4. The health and national security risks of drug shortages. March 2023. Accessed March 7, 2024. https://www.hsgac.senate.gov/wp-content/uploads/2023-06-06-HSGAC-Majority-Draft-Drug-Shortages-Report.-FINAL-CORRECTED.pdf. 5.
Opinion/Solutions
[Health Disparities, Spring 2024] 62
AFFORDABILITY
Evelyn Zhang - BSPS student
Inequalities in Affordability - Background
There are increasing rural-urban inequalities in the equity of affordability of medical care and pharmaceuticals in China. The average medical expense consistently increased in all societal layers, especially for the employees in the state-owned enterprises.
Principle of Chinese Health Care Reform
“Relaxing policies, streamlining administration and delegating powers, raising funds from various sources, broadening the horizon in developing health undertakings and doing a good job”
Solutions
Essential Medicine Policy
Propsed by National Health Ministry
Public hospitals and primary care facilities cannot charge patients above the procurement price
Regular assessments are carried out
Drug affordability ensured
Impoverishment caused by inaccesible medications are avoided
Drug Reimbursement Policy
Improve affordability of innovative drugs
Further lower the price of generic drugs
Drug list is continuously updated
Negotiations and bidding processes are conducted
Professional Opinion
The change in China’s pharmaceutical system may pose challenge on its sustainability. Innovative drug discovery and entry of innovative drug from foreign pharmaceutical companies will be impacted due to the stringent price limitation policies.
M Jakovljevic
80-90% Generic Drug Price Reduction
References Jakovljevic, Mihajlo, Hanyu Chang, Jay Pan, Chao Guo, Jin Hui, Hao Hu, Danko Grujic, Zhong Li, and Lizheng Shi. “Successes and Challenges of China’s Health Care Reform: A Four-Decade Perspective Spanning 1985—2023.” Cost Effectiveness and Resource Allocation 21, no. 1 (August 30, 2023): 59. https://doi.org/10.1186/s12962-023-00461-9. 1. Zheng L, Zhang L, Chen K, He Q. Unmasking unexpected health care inequalities in China using urban big data: Service-rich and service-poor communities. PloS One. 2022;17(2):e0263577. doi:10.1371/journal.pone.026357 2.
40-50% Innovative Drug Price Reduction
[Health Disparities, Spring 2024] 63
DEMOGRAPHICS
SAMMY THOMAS - BSPS student
Race, Gender, Income, and Geographic Location
Differences in these areas cause disparities that play a role in the health outcomes of different groups. Underserved demographic groups worldwide suffer from worse health outcomes, lower life expectancy, and higher disease burden. This can be preventable with better treatment and changes to healthcare systems.
What is gender bias in healthcare?
There is an
18 year
difference in life expectancy between high and low income countries
In the United States:
3.4x
Worldwide, women experience worse healthcare treatment than men due to gender bias. In 72% of instances it takes women a longer time to receive the same diagnosis as men. Women’s physical pain is more likely to be treated as a symptom of mental illness than a physical health problem.
2.3x
112%
higher prostate cancer mortality rate in black men than white men higher infant mortality rate in black babies than white babies higher maternal mortality rate in black women than white women
39%
higher breast cancer mortality rate in black women than white women
33% of women will experience reproductive health problems in their lifetime
Higher income is directly correlated to longer life expectancy due to access to medication, doctors, better housing, athletics, and higher quality food.
Solutions Opinion
Diversify clinical research
Further research on diseases that disproportionately affect different demographics
Recognize differences between different demographic groups in order to address them
Educate HCPs and patients
Increases accessbility to healthcare
I believe implicit bias plays a large role in the health outcomes of different demographics. The way doctors perceive patients can tremendously change the level of care they provide. Additionally, clinical research needs to include more diverse participants. Recognizing heterogeneity between different groups will lead to better outcomes for everyone. - S. Thomas
References Burrowes K. newsGP - Gender bias in medicine and medical research is still putting women’s health at risk. NewsGP. Published 2021. https://www1.racgp.org.au/newsgp/clinical/gender-bias-in-medicine-and-medical-research-is-st 1. Villines Z. Gender Bias in healthcare: Examples and Consequences. Medical News Today. Published October 25, 2021. https://www.medicalnewstoday.com/articles/gender-bias-in-healthcare#examples 2. World Health Organization. Social Determinants of Health. www.who.int. Published 2021. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_3 3. Racial Disparities in Healthcare: A Call to Action. HealthScape Advisors. https://www.healthscape.com/insights/racial-disparities-in-healthcare-a-call-to-action/ 4.
[Health Disparities, Spring 2024] 64
ORGAN TRANSPLANTS
SPRING 2024
CAMRYN FULTON, ANNIE ZHAO, CINDY PHAN, SAM KING, AND BENJAMIN TSENG
BACKGROUND
Organ transplantation is a critical global health issue. Over the past 50 years, it has become a successful worldwide practice, saving and improving the lives of millions of patients suffering from organ failure. However, the organ demand significantly exceeds the supply, resulting in several challenges. These cover problems related to organ transplantation practices' ethics, safety, quality, and efficiency. Specific subtopics will cover black market organ harvesting, xenograph transplantation, transplant backlog, cultural and religious beliefs, and what is considered legal vs illegal.
BLACK MARKET ORGAN HARVESTING
XENOGRAPH TRANSPLANTATION
TRANSPLANT BACKLOG
CULTURAL AND RELIGIOUS BELIEFS
LEGAL VS ILLEGAL
https://www.google.com/imgres? q=organ%20transplant&imgurl=https%3A%2F%2Fletstalkscience.ca%2Fsites%2Fd efault%2Ffiles%2F202006%2Fhuman_organs_for_transplant.jpg&imgrefurl=https%3A%2F%2Fletstalkscien ce.ca%2Feducational-resources%2Fbackgrounders%2Forgantransplantation&docid=ULyRCJHE6FMkM&tbnid=L_pJgML34MRFSM&vet=12ahUKEwiNi5fSp6-FAxVQC3kGHX_A5kQM3oECBMQAA..i&w=600&h=600&hcb=2&ved=2ahUKEwiNi5fSp6FAxVQC3kGHX-_A5kQM3oECBMQAA
https://www.google.com/url?sa=i&url=https%3A%2F%2Fwww.brit-med.com%2Fblog%2Fan-introduction-to-organ-transplantation-why-to-consider-going-abroad-fortreatment%2F&psig=AOvVaw1yVDqRqjqmIZSLEYP37iG&ust=1712552043320000&source=images&cd=vfe&opi=89978449&ved=0CBIQjRxqFwoTCIDxq8Kor4UDFQAAAAAdAAAAABAE%20poop

ORGAN TRANSPLANTS, SPRING 2024
65

WHO IS AFFECTED?
Human trafficking is closely associated with organ trafficking, and many victims are involved in both. Others that can be involved are refugees and migrants, who may sometimes voluntarily sell their organs in order to provide for themselves and their families. Other victims may be scammed into thinking that they are getting a certain surgery, but will have an organ involuntarily harvested instead. Finally, some victims will unfortunately be killed for their organs.
EFFORTS + SOLUTIONS
Because there is a low level of reporting and research conducted regarding organ trafficking, it is critical that more information is gained in order to combat these actions. Law enforcement must have more detailed training on identifying perpetrators and victims of organ trafficking to help mitigate these crimes. Additionally, since many of the victims are involved in human trafficking, any efforts to help and support these victims will also combat organ trafficking.
REFERENCES
BLACK MARKET ORGAN HARVESTING
CAMRYN FULTON BSPS STUDENT
BACKGROUND
Illegal organ harvesting and transplants is a substantial global issue, posing several ethical and health-related risks. It is estimated that about 10 percent of organ transplants are performed with trafficked organs, with the most commonly transplanted organ being kidneys. The existence of organ trafficking stems from the high demand for organs met with a low supply. The desperation of organs to patients and desire to make high profits from selling are two of the main motivations that drive the organ trafficking market. The trade makes an annual profit that is estimated to be between $840 million and $1.7 billion.
GLOBAL ISSUE
Organ trafficking is an issue that affects people around the world. The trade is most commonly seen in South and South-East Asia, Central America and Europe. Specific organ ‘hotspots’ that have been characterized by the World Health Organization are China, Pakistan, Egypt, Colombia, and the Philippines. The organ trade is considered illegal globally, with exception to Iran, which allows its citizens to buy and sell organs. Organ trafficking is often underground and difficult to track. This is partially because many of the crimes are associated with licensed medical facilities and practices, and most go unreported.
PERSONAL OPINION
I personally believe that much more research needs to be done on illegal organ trafficking in order for action to be taken properly. More resources need to be provided for victims to be able to report these crimes and lead investigators to prosecute the criminals involved. - C.
Fulton
ACAMS today. Organ Trafficking: The Unseen Form of Human Trafficking – ACAMS Today. Acamstoday.org. Published June 26, 2018. https://www.acamstoday.org/organ-trafficking-the-unseen-form-of-human-trafficking/ Whitney C. Organ Trafficking Facts. The Exodus Road. Published January 16, 2023. https://theexodusroad.com/organtrafficking-facts/#:~:text=How%20prevalent%20is%20organ%20trafficking Prevention of Trafficking in Persons.; 2008. https://www.unodc.org/documents/human-trafficking/Toolkit-files/0858296_tool_9-19.pdf
Reuters. FACTBOX-Five Organ Trafficking Hotspots. reuters.com. Published August 9, 2007. Accessed March 27, 2024. https://www.reuters.com/article/idUSL01426288/
ORGAN TRANSPLANTS, SPRING 2024
ptth
m/ e d u
veda
b3ac 5 1 1 9 1 3 02%3c 66
s : /
m .com/@
.bhattaram/organ-trafficking-causes-and-potential-solutions
XENOTRANSPLANTATION
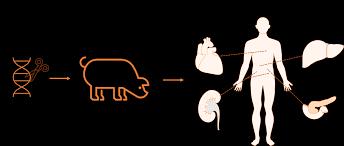
From “Recent progress in xenotransplantation – a new way to fight donor organ shortage” by Biopharma Excellence
WHO IS AFFECTED?
A significant issue that ideas about xenografts affect is equitable access. Thus far, xenotransplants have only been given to those at death's door with no other treatment options. In the US, porcine transplants are still technically currently banned due to the risks of zoonotic viruses identified decades ago. As the technology improves, it could greatly help patients with organ failure who face long waitlists for human organs. However, access may primarily benefit the wealthy and wellconnected unless regulations ensure equitable distribution.
There are also concerns specific to testing and developing xenotransplants. Conducting trials requires finding participants willing to undergo high-risk, unproven procedures with limited potential personal benefit. This raises ethical questions about taking advantage of vulnerable populations for medical experimentation. Traditionally, prisoners are unable to participate in clinical trials. However, a prisoner was recently subject to a xenotransplantation. The genetic engineering of pigs also causes animal welfare concerns. Genetic engineering comes with concerns from the public, as seen in genetically modified foods or GMOs.
REFERENCES
1.
BACKGROUND
Xenotransplantation is the practice of using a different species for organ donation. Pig organs have been the most prominent due to their similar size, structure, and immune-related traits. Xenotransplantation has generated much ethical debate as surgeons have begun transplanting genetically engineered pig organs into humans. In 2023, a team at NYU Langone Health made a breakthrough by transplanting a pig kidney into a brain-dead man and achieving function for over 30 days.
GLOBAL ISSUE
Health risks like cross-species disease transmission further complicate the issue. Scientists have used gene editing to remove potentially hazardous viruses from donor pigs. However, preventing all viral exposures or the possibility of new zoonotic diseases is challenging. This public health concern has led countries like Canada and Australia to ban xenotransplantation. Meanwhile, China is poised to become a world leader in this area, given its extensive work on genetically modified pigs.
Additionally, some religions prohibit the use of porcine products, causing moral objections. Focus groups show acceptance from Islamic, Catholic, and Protestant leaders, but opposition remains in specific communities and countries. Hence, cultural sensitivity is applicable as this technology expands worldwide.
EFFORTS + SOLUTIONS
EFFORTS AND SOLUTIONS
While Xenotransplantation has many ethical and health issues, it is a solution to organ shortages. Therefore, pilot programs currently being implemented should continue running. Pilot programs should also work with a wide variety of populations.
PERSONAL OPINION
I think more time and resources should be dedicated to xenotransplantation. Since animal “parts” are already used for various other medical purpose, animal organs seems like a natural extension of the technology. However, much more work needs to be done in order to start using xenotransplantation in patients who can recover.
Ref1. de Jongh D, Massey EK, Cronin AJ, Schermer MHN, Bunnik EM. Early-Phase Clinical Trials of Bio-Artificial Organ Technology: A Systematic Review of Ethical Issues. Transpl Int. 2022;35:10751. doi:10.3389/ti.2022.10751
The attitudes of religious group leaders towards xenotransplantation: A focus group study - PubMed. Accessed March 27, 2024. https://pubmed.ncbi.nlm.nih.gov/36069244/ 2.
SAM
BSPS STUDENT
KING
ORGAN TRANSPLANTS, SPRING 2024
67
TRANSPLANT BACKLOG
BACKGROUND
THE GLOBAL ISSUE
103,443 people in the U.S alone as of Feburary 2024, up from 103,650 people in November 2023.
10,000+ people waiting in Taiwan as of November 2023, with 8,684 people waiting for kidney transplants alone.
Around 7,000 people waiting in the U.K between 2023 and 2024 with 430 people dying before a donor can be found according to the NHS.
In 2013, 60,000 patients in the European Union were waiting for an organ transplant.
In 2023, 13,498 patients were waiting for a transplant in Eurotransplant member countries with an additional 10,466 patients on the list that year.*
WHO IS AFFECTED?
Patients on the waitlist: There is a risk that you do not survive before a suitable donor is found. Even with a successful transplant, the need to take immunosupressant medication to avoid organ rejection creates vulnerability to infections.
Organ donors: While some donors can donate some organs while they are still alive, they run the risk of complications while their organ is taken out. Even if the extraction is successful, there is the need for extra care to be taken should the remainder of the organ get damaged or fail during recovery.
Organ transplants have provided a critical lifeline for people who suffer from organ failure. While there has historically never been enough organs available for transplant, in recent years, this problem has only continued to worsen. This is because you cannot just transplant any available organ from one person to another due to the risk of the recipient’s immune system rejecting the transplant. As a result, the recipient must be matched to a suitable donor first before an organ can be transplanted. The result is the creation an organ wait list where people are forced to wait for a suitable donor followed by being forced to take immunosuppressant drugs for the rest of their life. Even then, there are many that do not survive long enough for a suitable donor to be found.
EFFORTS AND SOLUTIONS
There are currently many solutions being discussed for the problem ranging from artificial organs and stem cell organs to xenografts. Artificial organs can be made from biomaterials and always be available for transplant, eliminating the need for waiting for a donor. Alternatively, in a stem cell organ, the individual’s stem cells can be taken out of the patient, cultured, and then made into the required organ and then transplanted back into the patient. More recently, there has been success in transplanting pig heart valves into a patient, indicating potential to use animal organs as a stopgap solution while longer term solutions are developed.
PERSONAL OPINION
The long backlog in organ transplants does not surprise me as organs aren’t always on demand on top of the need for a near perfect match in order to avoid transplant rejections. Given the circumstances, while I do believe that xenografts are a good temporary solution, I believe that looking into artificial organs or growing organs from one’s own cells will help to eliminate the backlog all together. Artificial organs can serve as a temporary organ and allow a patient to have some normal semblance of life while a new organ made from one’s own cells. Once the new organ is ready, the patient can comes back in and get the artificial organ replaced with the newly made organ, eliminating the need to be on a waitlist, the need to be in intensive care for some tranplants, and chances of organ rejection. - B. Tseng
*: Eurotransplant Members include: Austria, Belgium, Croatia, Germany, Hungary, Luxembourg, Netherlands, and Slovenia
REFERENCES
U.SDepartmentofHealthandHumanServices.(n.d.).OPTN:OrganProcurementandTransplantationNetwork-OPTN.OrganProcurementandTransplantationNetwork.AcessedFeburary2, 2024.https://optn.transplant.hrsa.gov/ Statistics.(n.d.).Eurotransplant.AcessedFeburary2,2024.https://statistics.eurotransplant.org/index.php? search_type=waiting+list&search_organ=&search_region=&search_period=by+year+chart&search_characteristic=&search_text= NHS.(2022).OrganDonationandTransplantation.NHSBloodandTransplant.AcessedFeburary2,2024.https://www.nhsbt.nhs.uk/what-we-do/transplantation-services/organ-donation-andtransplantation/ Fazekas,E.(2013,January).Klinikum[ReviewofKlinikum].Morethan60000PatientsintheEUWaitingforaNewOrgan,1–5.AcessedFeburary2,2024. https://health.ec.europa.eu/system/files/2016-11/art_hungary_2012_en_0.pdf Ruzicka,A.J.(2023,October12).Organdonorwaitlist—here’swhohasthelongest,shortestwaittimes|NorthwellHealth.Www.northwell.edu.AcessedFeburary2,2024. https://www.northwell.edu/news/the-latest/organ-donor-wait-list-longest-shortest-wait-times 6.Scanlan,S.(2023,November15).Taiwanconsideringallowingfriends,consentingadultstobeorgandonars|TaiwanNews|2023-11-1511:05:00.TaiwanNews.AcessedFeburary2,2024. https://www.taiwannews.com.tw/en/news/5040217
BENJAMIN
TSENG BSPS STUDENT
ORGAN TRANSPLANTS, SPRING 2024
68
CULTURES& RELIGIONS
CINDY PHAN
PHARMD/BSPS STUDENT
THE GLOBAL ISSUE
Organ donation rate of different religious groups in the US
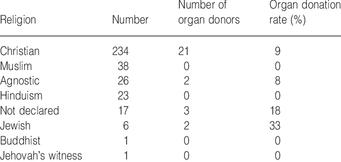
Organ donation rate of different countries
BACKGROUND
Cultural, religious, and traditional beliefs play a significant role in shaping individuals' attitudes towards organ donation. In the United States, the diverse array of cultural backgrounds often influences perceptions and behaviors related to organ transplantation. People's attitudes towards xenotransplantation vary according to time, culture, and social groups. According to the article by Ö Şahin Akboğa and others, it has been reported that young and highly educated women have positive attitudes towards xenotransplantation. Muslims, on the other hand, religiously emphasize that no part of the pig should be used for medical purposes.
EFFORTS AND SOLUTIONS
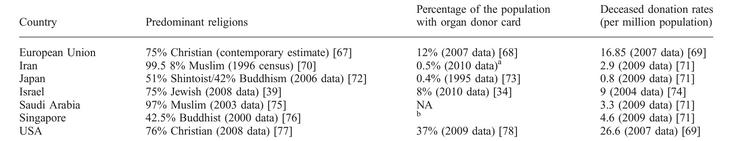
WHO IS AFFECTED
Black, Asian and minority ethnic groups have a high need for organ transplantation but a low donation rate, reducing chances for an organ match
However, according to Donate Life Organ, in regards to religious views on organ donation, nearly all religious groups support organ and tissue donation and transplantation as long as it does not impede the life or hasten the death of the donor.
REFERENCES
In the USA, it is uncertain whether and how centers that are considering a clinical trial of xenotransplantation are planning to engage the public. Aside from one single-center study, no empirical data have been published detailing how persons of different racial and/or ethnic backgrounds view xenotransplantation.
PERSONAL OPINION
Understanding the complex interplay between cultural, religious, and traditional beliefs is crucial for addressing disparities in organ donation acceptance. As we navigate this field and approach clinical trials, it is evident that the public's perspective on xenotransplantation is a crucial factor that merits further consideration. Efforts to promote organ donation should consider cultural sensitivity and engage with diverse communities to foster awareness and overcome barriers. By respecting individuals' cultural and religious perspectives, healthcare professionals can work towards enhancing organ donation rates and ultimately saving more lives.
-C. PHAN
Sobnach S, Borkum M, Millar AJW, Hoffman R, Muller E, McCurdie F, Kahn D. Attitudes and beliefs of South African medical students toward organ transplantation. Clin Transplant 2011 DOI: 10.1111/j.1399-0012.2011.01449. Ali, A., Ahmed, T., Ayub, A., Dano, S., Khalid, M., El‐Dassouki, N., ... & Mucsi, I. (2020). Organ donation and transplant: the Islamic perspective. Clinical transplantation, 34(4), e13832.
Şahin Akboğa, Ö., & Rukiye Hobek, A. (2023). Acceptance of xenotransplantation by patients waiting for organ donation: a qualitative study. Xenotransplantation, 30(5), e12813.
Siminoff, L. A., Bolt, S., Gardiner, H. M., & Alolod, G. P. (2020). Family first: Asian Americans’ attitudes and behaviors toward deceased organ donation. Journal of racial and ethnic health disparities, 7(1), 72-83. Cultural Challenges of Organ Donation. (2023). https://www.cedars-sinai.org/blog/cultural-challenges-of-organ-donation.html Hurst, D. J., & Cooper, D. K. (2024). The importance of public engagement in clinical xenotransplantation. Health Care Science.
ORGAN TRANSPLANTS, SPRING 2024
69
LEGAL VS ILLEGAL
ANNIE ZHAO BSPS STUDENT
WHO IS AFFECTED?
Patients
Legal: save lives
Illegal: pose serious health risks.
Health System
Legal: manage allocation
Illegal: challenge due to shortage Society
Raises societal questions about ethics, law and economic disparties
Donors
Legal: voluntarily give organs, often to relatives
Illegal: from vulnerable populations, may be exploited
Medical Professionals
Legal: perform surgeries under monitor
Illegal: face ethical dilemmas
EFFORTS + SOLUTIONS
The WHO and international bodies have set guidelines to fight organ trafficking. Countries have laws supporting transparent waiting lists and donor registries.
Public awareness programs educate on donation importance.
Measures in well-resourced countries can deter transplant tourism.
Regulated Compensation Schemes ensure donor safety.
Developing countries could establish ethical organ procurement systems.
Strict law enforcement against illegal organ trade is crucial.
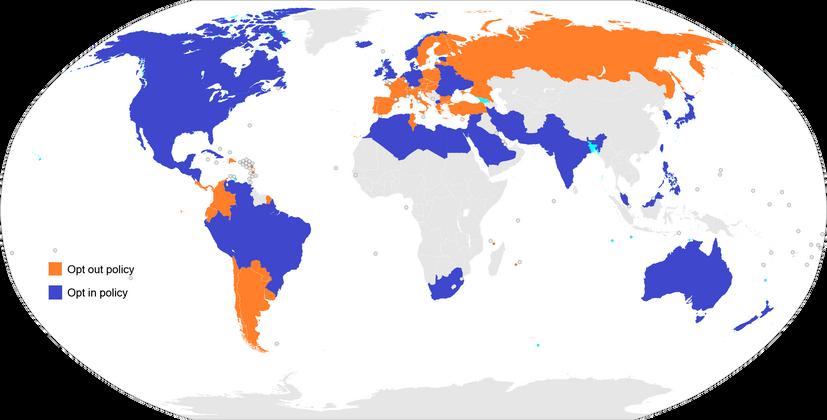
https://i.redd.it/g0vasave2zg51.png
BACKGROUND
In legal organ transplantation, organs are donated voluntarily. In many countries, there are two main systems for organ donation: “opt-in” (where explicit consent is required) and “opt-out” (where everyone is considered a donor unless they explicitly opt-out), for example, Austria, Belgium, and Spain. The U.S. organ transplant system is inequitable with significant nonuse of donated organs Illegal organ trade occurs when organs are removed from the body for commercial transactions. Despite laws against organ sales, this practice persists, with studies estimating that anywhere from 5% to 42% of transplanted organs are illicitly purchased. This illegal trade often exploits vulnerable individuals from impoverished backgrounds, who may sell their organs out of desperation. The subtopic relates to the main issue by addressing the ethical and societal challenges associated with obtaining organs.
GLOBAL ISSUE
Legal transplantation involves voluntary organ donation, while illegal transplantation involves organ trade, often exploiting socioeconomic disparities. Cultural beliefs influence organ donation rates, and laws vary by country. The global organ shortage has led to illegal organ trade, raising ethical and legal challenges. This issue underscores the need for international cooperation, legal reform, and innovative solutions to ensure ethical practices in organ transplantation.
PERSONAL OPINION
Legal transplantation ensures that organs are properly screened for diseases, which is crucial for the recipient’s health. Illegal transplantation, on the other hand, lacks these safeguards, potentially leading to adverse health outcomes. Furthermore, posttransplant care involves complex medication regimens to prevent organ rejection. In illegal settings, the necessary follow-up care and counseling may be inadequate or non-existent, posing significant health risks. Therefore, it’s imperative to advocate for legal and ethical organ transplantation practices. - A. Zhao
REFERENCES
Jafar TH. Organ trafficking: Global solutions for a global problem. American Journal of Kidney Diseases. 2009;54(6):1145-1157. doi:10.1053/j.ajkd.2009.08.014
The Lancet. Legal and illegal organ donation. The Lancet. 2007;369(9577):1901. doi:10.1016/s0140-6736(07)60889-7
ORGAN TRANSPLANTS, SPRING 2024
70





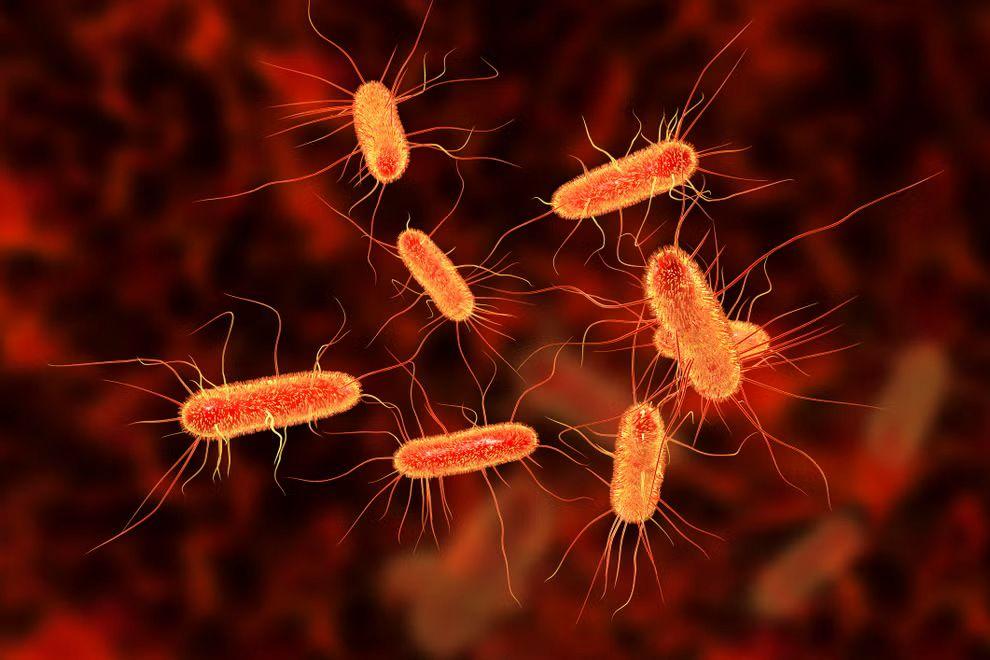
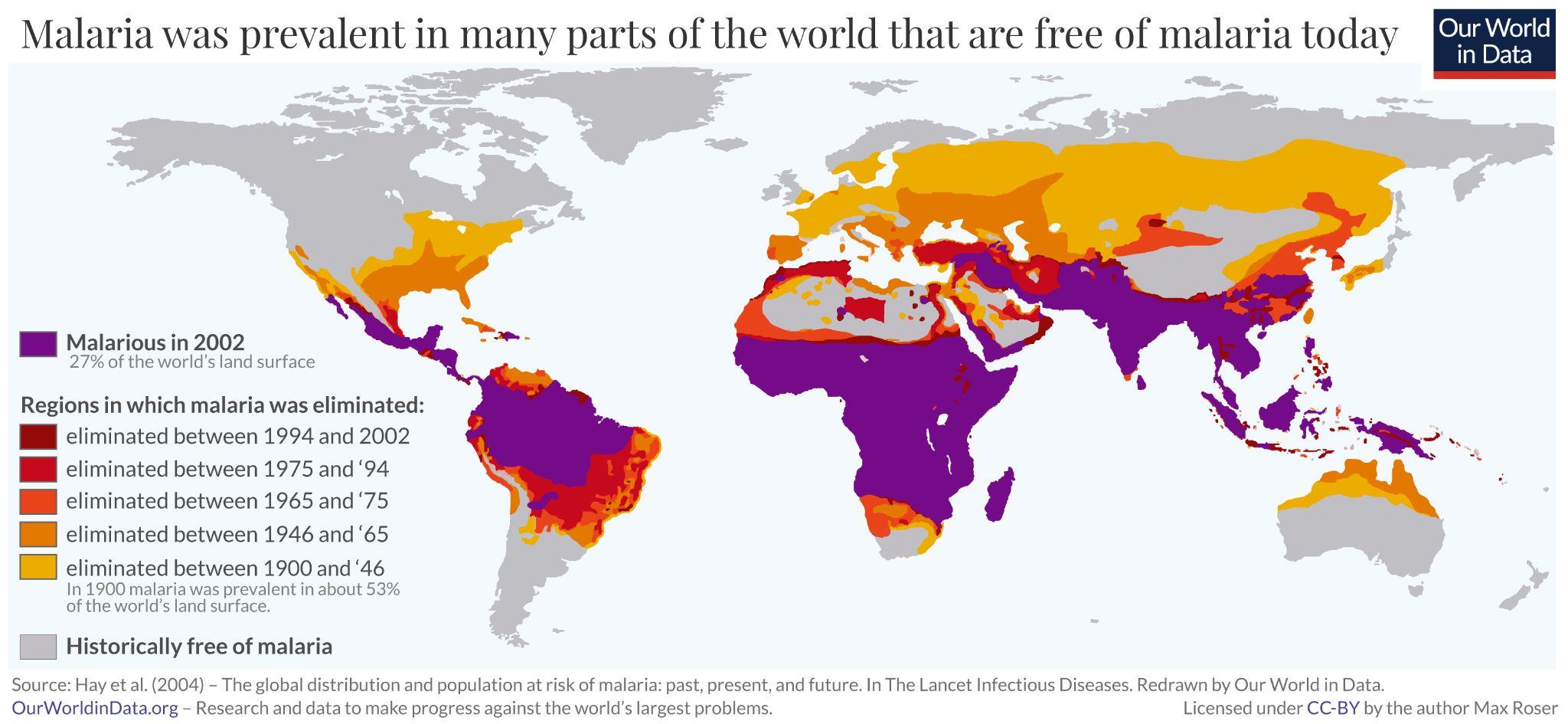
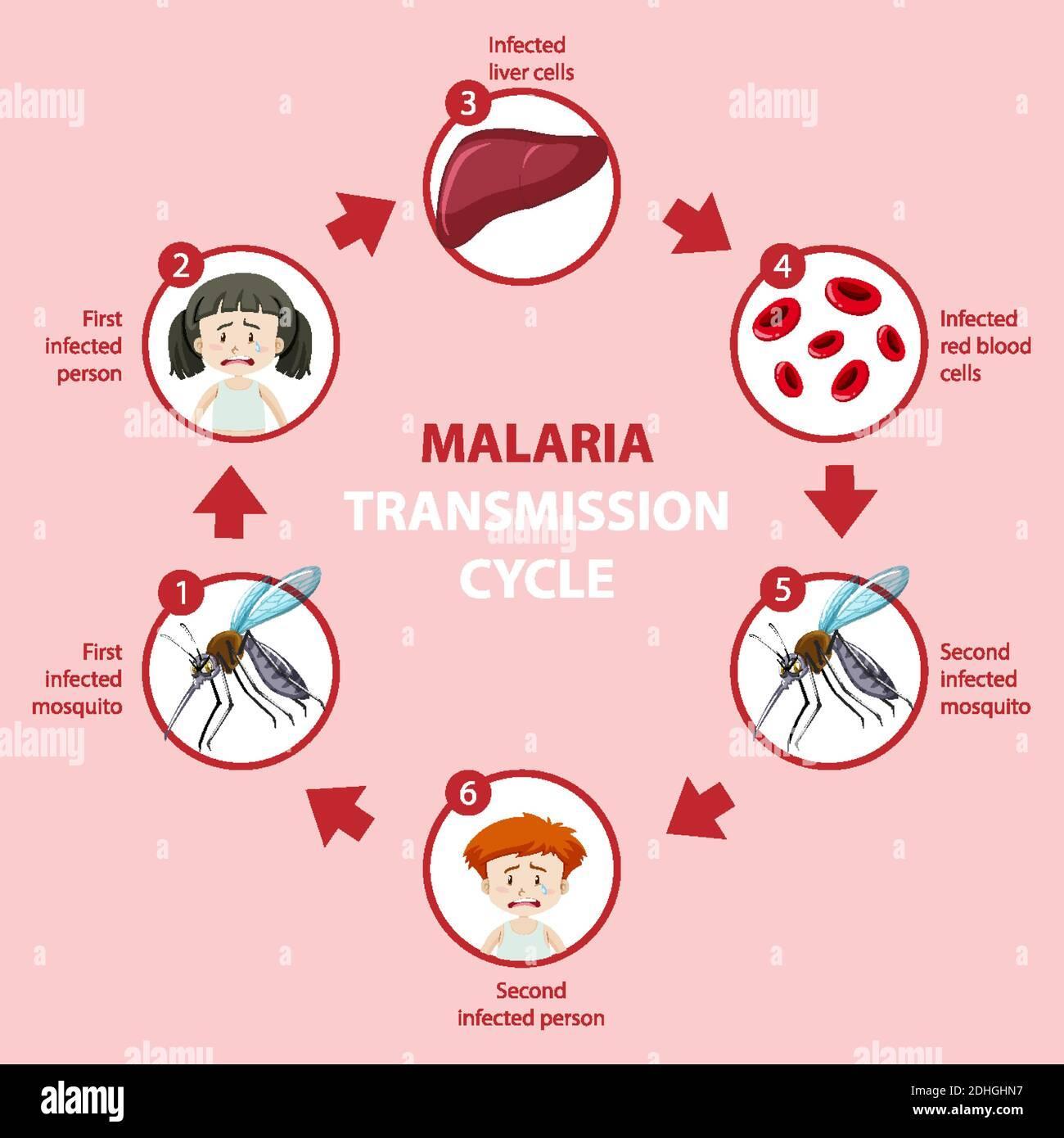
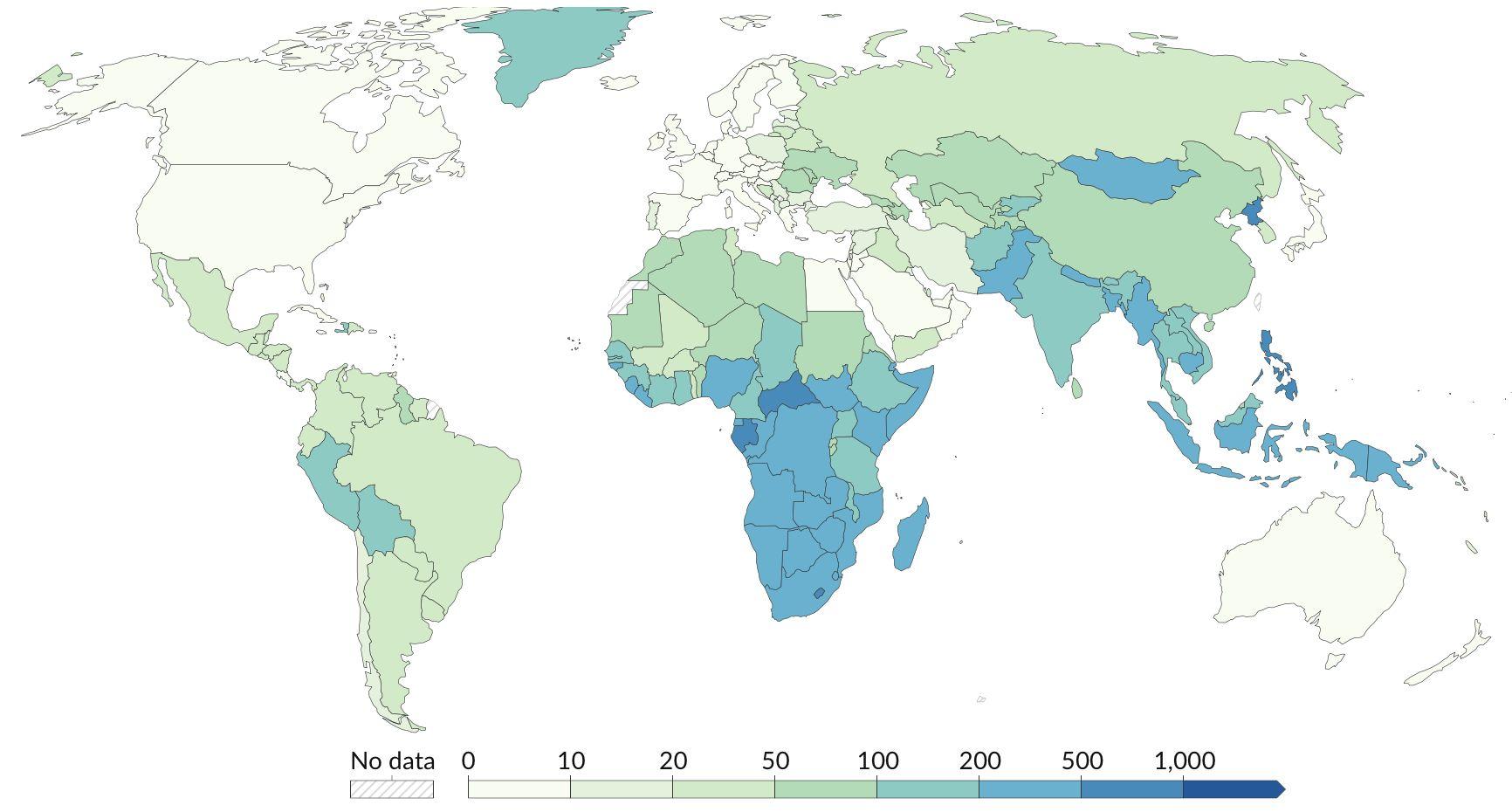
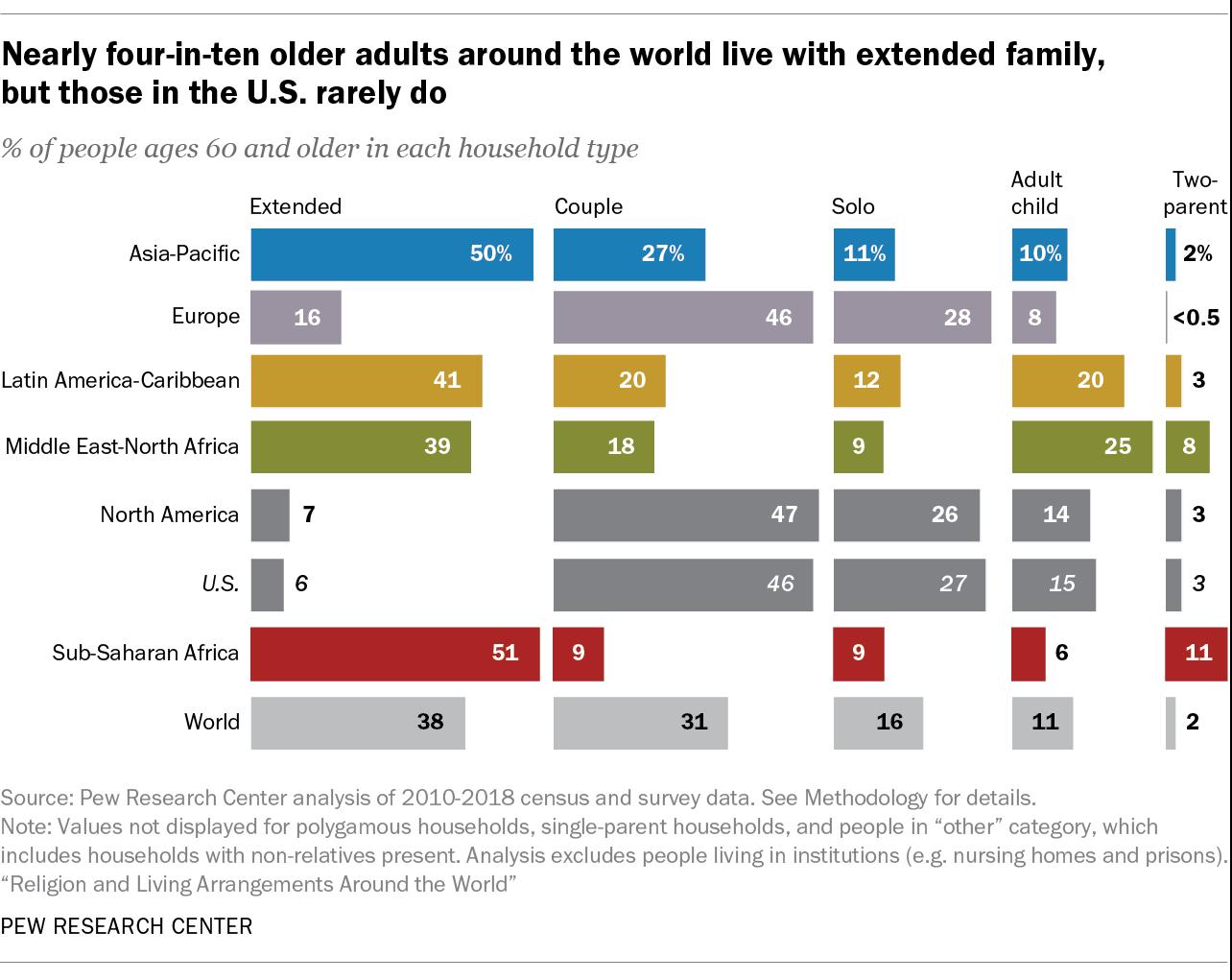

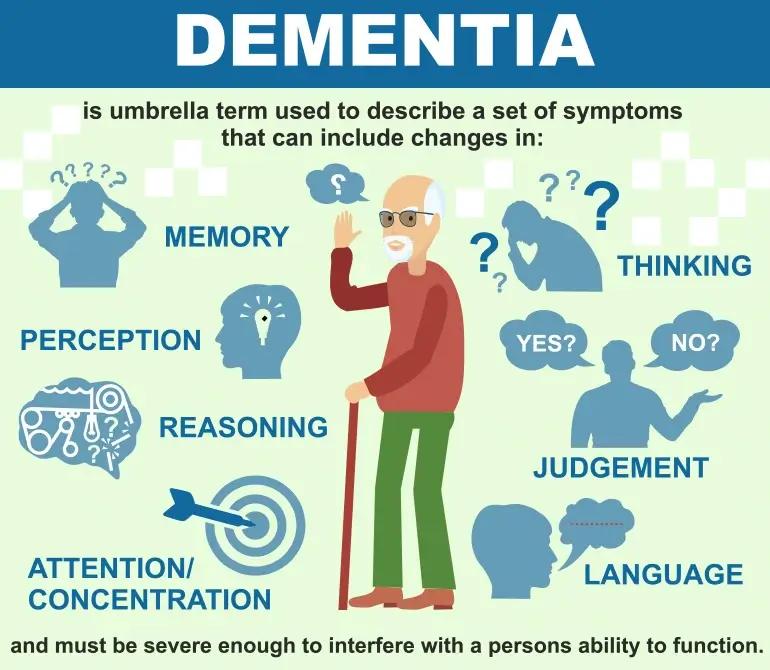
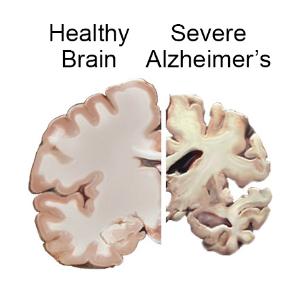
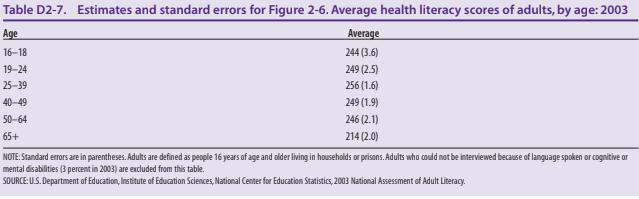

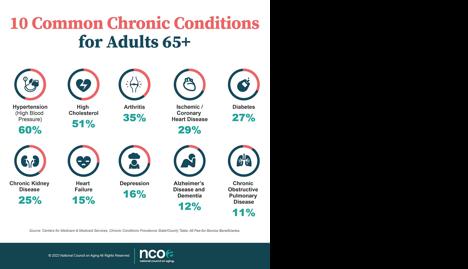
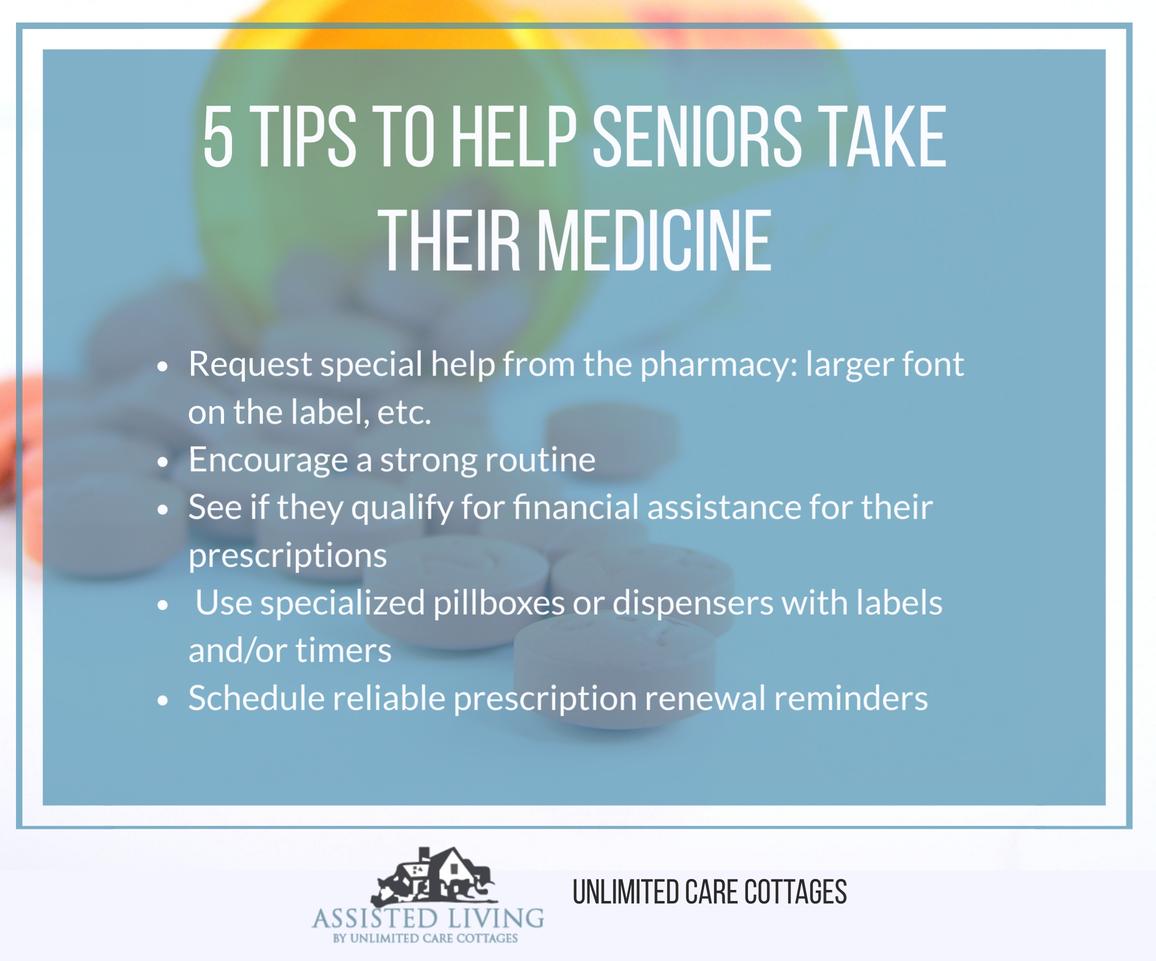
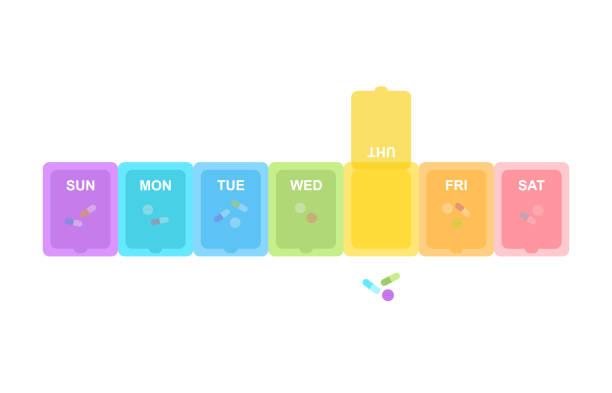

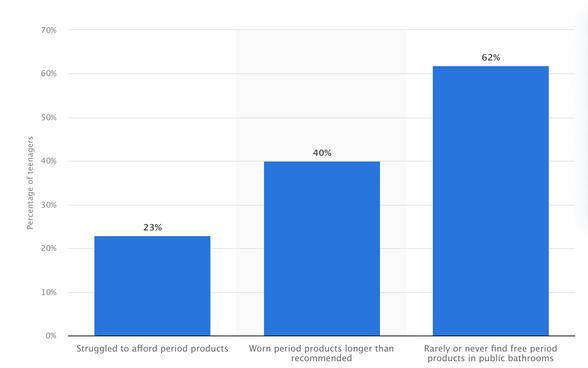

 (BAILEY WALKER, BSPS STUDENT)
(BAILEY WALKER, BSPS STUDENT)