psychosisaustralia.com.au

psychosisaustralia.com.au
29th - 30th of July 2025 | Brisbane
Tuesday 29th July to Wednesday 30th July
Rydges South Bank Brisbane
Welcome to the Australian Psychosis Conference 2025
On behalf of the Local and Scientific Organising Committee, we warmly welcome you to the Australian Psychosis Conference (APC) 2025.
Formerly known as the Australasian Schizophrenia Conference, APC has evolved into a space that brings together people with lived experience of psychosis, their families, carers, researchers, frontline workers, policymakers, and advocates. Our goal is to create a respectful and safe environment where all voices are heard and valued.
This conference is the result of collaboration across stakeholder groups, each committed to improving care, outcomes, and rights for people living with psychosis. We recognise the current system is failing many and urgently needs reform and investment at all levels of government.
As we come together with a shared purpose, we invite you to take up the challenge: share what you learn, speak up, and help drive the change we need. Everyone deserves access to high-quality care, recovery and rehabilitation services, psychosocial support, and their fundamental human rights.
Let’s work together to make a meaningful difference.
Local Organising Committee
Chair: Rob Ramjan, AM
Committee: Tony Stevenson
Committee: Ilyse Elphick
Scientific Committee
Chair: Professor Dan Siskind
Committee: Dr Justin Chapman
Committee: Kerry Hawkins
Committee:DrMegDoohan

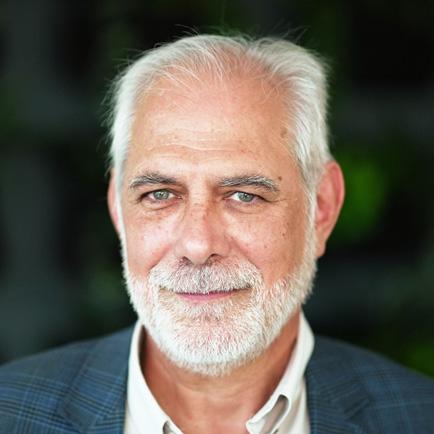
Chairperson
Robert Ramjan AM
Experienced Chief Executive Officer with a demonstrated history of working in the mental health care industry.

Trustee
Zoe Black
Co-Founder and Exec Director of Happy Paws Happy Hearts.

Trustee
Prof Dan Siskind
Professor of Psychiatry - NHMRC Emerging Lead Fellow (Second), University of Queensland.

Trustee
Dr Justin Chapman
Research Fellow with Griffith University and a Lived Experience Research Officer with Metro South Addictions and Mental Health Service.

Trustee
Dr James McLure
Research Fellow at IMPACT, Deakin University.

Secretary of Trust
Tony Stevenson
CEO of Mental Illness Fellowship Australia

Trustee
Kerry Hawkins CEO, Community Mental Health Australia

Trustee
Stuart Englund
Translating private sector insights to government, and public policy goals to industry.
Thank you to the following partners for their advertising support of the APC2025.














Town Hall Event Monday 28th July 2025
5.30pm- 8.30pm
5.306.00 Arrival & Networking
6.006.05 Welcome – Rob Ramjan & Introduce Cameron Thayer
6.056.10 Acknowledgement of Country & House Keeping – Cameron Thayer
6.106.15 Recognition of Lived Experience – Amanda Carpenter
6.156.25 Mental Health Address – Qld Mental Health Commissioner, Ivan Frkovic
6.256.35
Local Spotlight CoRTA – Co-design and Research Translation Alliance in Mental Health –Dr Justin Chapman
Human Rights & Social Determinants
6.356.45
The need to address social injustice in reforming mental health service delivery –Prof Lisa Brophy
Clinical Research & Treatments
6.456.55
Considering the whole person in psychosis, the body and mind – Prof Dan Siskind
6.557.25
Karakan Helping people with mental health needs to build resilience and live life better, together.
Perspectives & Narratives
7.257.35
Chemical Imbalance or Power Imbalance: UN Special Rapporteur 8 years on, and why narrative control matters for scientific progress – Kerry Hawkins & Amanda Habermann
Policy & Systems
7.357.45
Rebuilding community-based support for serious mental illness in Australia –Prof Jennifer Smith-Merry
7.457.55
Policy without evidence is a human rights issue – Prof Alison Yung
7.558.00 Final Words
8.008.30 Networking


Amanda Carpenter is a dedicated mental health professional with over 14 years of experience in the sector, underpinned by her own lived experience of mental health challenges. Her personal journey has provided her with a profound understanding of the systemic barriers individuals often encounter when seeking support, and this insight has been instrumental in shaping her compassionate, person-centred approach. She has been actively involved in both individual and systemic advocacy, working to ensure the voices of those with lived experience are recognised, respected, and embedded in service delivery.
Amanda currently serves as a Team Facilitator with Karakan, where she continues to promote recovery-focused care and lead from a foundation of authenticity, empathy, and experience. Her work remains grounded in the belief that recovery is not only possible but deeply personal—and best supported when services are informed by those who have walked the path

Cameron has worked in human services for 18 years with over 14 years in key leadership roles. His educational background includes a Bachelors in Behavioural Science (Psychology) and a Masters in Business Administration. His mantra and mission as a community-focused leader is to Empower people, Change lives and Give back to community

Commissioner Frkovic has worked in the Queensland mental health system for more than 30 years and oversees the delivery and implementation of Queensland’s strategic plan for mental health, alcohol and drugs and suicide prevention. Commissioner Frkovic is experienced across government and nongovernment organisations, bringing all sectors together to focus on delivering better mental health outcomes for Queenslanders.

The Co-design and Research Translation Alliance in Mental Health (CoRTA-MH) consortium aims to enable co-production and foster collaboration in translational research for innovation and reform. CoRTA-MH focuses on generating evidence to identify priorities and unmet needs, translating this evidence to influence policies and practices, and continuously adapting to changing circumstances. By leveraging cross-sectoral partnerships and strategic advocacy, the consortium seeks to improve community wellbeing through implementation research and action. The vision is a connected, inclusive community that drives mental health innovation and reform, and the mission is to implement evidenceinformed changes that meet community health and wellbeing needs.

Day 1 Tuesday 29th July 2025
2.003.00 Clinical Research & Treatments Considering the whole person in psychosis, the body and mind. – Professor Dan Siskind & Associate Professor Julia Lappin
3.003.30
3.304.30
Sundowner Tuesday July 29th
8.258.25

Day 2 Wednesday 30th July 2025
8.009.00
Policy & Systems
9.009.45
Rebuilding community-based support for serious mental illness in Australia –Professor Jennifer Smith-Merry
9.4510.45
Policy & Systems Policy without evidence is a human rights issue –Professor Alison Yung, Dr Carl Moller & Research Associate Professor Anna Waterreus
10.4510.55 Environment Check In – Jan Archer 10.5511.30 Morning Tea


Before leaving the Public Service Jan Archer was the Deputy Commissioner for Fair Trading in Queensland. She had previously completed significant reform agendas within the criminal justice system, including the Office of the Director of Public Prosecutions, Department of Corrective Services and the Queensland Police Service. During her membership of the senior executive service in Queensland, Jan acted as DirectorGeneral, Deputy Director-General and chaired several ministerial reference committees.
Much of Jan’s work in the university, public and community sectors has focused on innovation, reform and how leaders of public, private and community organisations can engage in adding value to their enterprises. Upon leaving the public service, Jan established Archersfield Consulting and Management, which has delivered change leadership support across sectors in QLD, NSW, NT and the ACT since 2005.
In 2010, Jan founded the Executive Challenge Academy,(ECA), an academy offering cross-sectoral leadership programs from foundations to masterclass levels, both nationally and internationally. In 2020, Jan was instrumental in founding The Alliance for Leadership Learning (ALL), a cross-sectoral Social Enterprise created to deliver placebased leadership development nationally, including all ECA programs. Reserve funds from the programs delivered by The ALL are re-invested to communities, sectors and organisations to provide further leadership development opportunities for leaders in their fields.



Lisa Brophy is Professor in Social Work and Social Policy at La Trobe University. Lisa has developed experience in mental health practice, research and knowledge of this complex sector. Lisa’s work has focused on human rights, social inclusion and reducing restrictive practice and compulsory treatment. She has also undertaken evaluations of recoveryoriented practice and innovations in service delivery. Lisa is committed to supporting consumer researchers and participation and codesign in mental health research.
Julia is a Psychiatrist with expertise in psychosis spectrum illness and bipolar disorder, focusing on early intervention, improving outcomes in severe mental illness, physical health promotion, comorbid substance misuse, and treatment resistance.
Having joined UNSW Australia from King’s College London, A/Prof Lappin collaborates locally and internationally on mental health outcomes and supervises research in these areas. She maintains strong ties to the AESOP-10 study, which tracked long-term outcomes for individuals with first-episode psychosis, exploring recovery pathways and improving clinical services. Her work includes developing integrated care models for comorbid substance use and mental illness, with a particular interest in the effects of crystal methamphetamine and other substances on cognitive and mental health outcomes.


Professor Siskind trained as a psychiatrist in Australia and the United States. He works clinically as a psychiatrist in Brisbane, Australia with people with treatment refractory schizophrenia. His research interests include treatment refractory schizophrenia, clozapine and the physical health comorbidities associated with schizophrenia. He has over 250 publications and over AU$50million in competitive research grants, with over AU$6.5 million as CIA.
Kerry works from a lived experience perspective as a family member. Her interests lie in systems transformation. She is Chair of the national Family, Carer and Kin mental health peak, Mental Health Carers Australia. She has worked in senior roles for the NDIA, the WA Mental Health Commission and as a carer consultant in both NGO and public mental health services. An alumni of Harvard Kennedy School’s Implementing Public Policy program, she is a graduate of Boston University’s Global Leadership Institute’s Recovery Class of 2013 and in 2024 undertook a Churchill Scholarship investigating international rights-based contemporary approaches to mental health that recognise the integral role of families in mental health. She served 3 terms as a National Mental Health Commissioner from 2018-2024.


Amanda Habermann
Amanda is an experienced independent Lived Experience Educator and consultant who has worked for the last twenty years from a consumer perspective in the mental health sector. Amanda provides realistic and real-world experience in the International Hearing Voices Network to groups and individuals who want to understand the Hearing Voices Approach, and is the Former Chairperson of ISPS (International Society of Psychological and Social Approaches to Psychosis) Australia. Amanda has been an active leader in the development of the Lived Experience Workforce both in Queensland, Western Australia and nationally.

Jennifer Smith-Merry is Professor of Health and Social Policy and Australian Research Council Industry Laureate Fellow (2023-2028) in the Sydney School of Health Sciences within the Faculty of Medicine and Health at the University of Sydney. Jen was Director of the Centre for Disability Research and Policy (CDRP) from 2018-2024 and remains an active member of the centre. CDRP is a multi-disciplinary centre whose mission is to make life better for people with disability in Australia and our region by translating research to policy and practice. Over the past decade her research work has focused on disability and mental health policy, particularly in relation to the implementation of the National Disability Insurance Scheme, and policy interventions for people with complex needs. Jen is chief investigator on multiple grants in partnership with government and non-government organisations. She works closely with people with lived experience of disability and has a strong interest in lived experience-informed policy and service design.

Professor Alison Yung
Professor Alison Yung is a renowned psychiatrist and international leader in early psychosis research. Based at Deakin University’s IMPACT Institute and an Emeritus Professor at the University of Manchester, she has been investigating the early stages of psychotic disorders since 1994. That same year, she established the world’s first clinical service for people at high risk of developing psychosis and developed the CAARMS tool, now used worldwide in both clinical and research settings.
Alison has received numerous prestigious awards, including the Lilly Oration Award, the Richard J Wyatt Award, and the Society for Mental Health Founders Medal. She was also named one of the “world’s most influential scientific minds” by Thomson Reuters and has been recognised as a “Highly Cited Researcher” every year since 2016. With over 400 publications, she continues to shape global understanding and early intervention approaches in psychosis.

Anna Waterreus is a researcher who trained as general and psychiatric nurse. She currently leads the Neuropsychiatric Epidemiology Research Unit at the University of Western Australia (UWA). Her work has including coordinating the first and second Australian Psychosis Surveys (1997 and 2010). She has an interest in ensuring research is conducted in an ethical manner and is a UWA Research Integrity Advisor and was Chair of the North Metropolitan Health Service Mental Health Ethics Committee. Underpinning her research has been the aim to improve the lives and care of people with mental illness, with a focus on addressing poor physical health.

Dr Carl Moller is a psychologist and Research Fellow in Psychosis Research at Deakin University’s School of Medicine. He holds a Master of Psychology in Clinical Neuropsychology and a Master of Public Health, and completed his PhD at the University of Melbourne’s Centre for Youth Mental Health and Orygen, focusing on suicidality in young people with depressive disorders. His research spans mood disorders, substance use, self-harm, suicide, and infectious diseases affecting the brain, such as HIV, with a strong interest in addressing health inequities, particularly among asylum seekers. Alongside his research and clinical work, Dr Moller is committed to supporting the next generation of mental health researchers. He co-chairs the Early and Mid-Career Researchers sub-committee of the Australasian Society for Bipolar and Depressive Disorders (ASBDD), where he helps create opportunities for collaboration and professional development in the field of mood disorders.

Stephen is a renowned English author, actor, screenwriter, playwright, journalist, poet, comedian, television presenter, broadcaster, podcaster, and film director.
A proud advocate for LGBTQ+ rights, Stephen has been championing the community for over 30 years, including his award-winning documentary Out There, which explores the lives of lesbian, gay, bisexual, and transgender people worldwide.
Since 2011, Stephen has served as President of Mind, the UK’s largest mental health charity, and has been an honorary fellow of the Royal College of Psychiatrists for over a decade.
In a specially pre recorded presentation, Stephen speaks candidly about the darkness that can accompany mental health challenges — but also the profound hope that exists. He reminds us that throughout history, individuals living with mental health conditions have made extraordinary contributions to art, science, culture, and society.

ORAL PRESENTATION
Co-design in health educator curriculum: From intent to action
11.15 AM Co-design in health educator curriculum: From intent to action – Victoria Stewart
11.25 AM Corollary discharges and inner speech as an explanation for auditory hallucinations in schizophrenia – Anthony Harris
11.35 AM Wounded Healer: Lived Experience of Postpartum Psychosis – Ariane Beeston
11.45 AM Dysfunctional Parent Modes and Auditory Hallucinations: Does Activation of the Inner Critic Increase Hallucination-Proneness? – June Engeland
11.55 AM Lived Experience engagement in mental health research – Victoria Stewart
12.05 PM Systematic review and meta-analysis of the relationship between repetitive negative thinking (worry and rumination) and positive symptoms of psychosis –Sharla Cartner
12.15 PM Unveiling New Insights into the Variation of Community Treatment Orders: The FACTOR Study – Lisa Brophy
12.25 PM Quality of life of people with mental health challenges and problematic substance use while engaged with an exercise physiology service –Justin J Chapman
12.35 PM Understanding the Family/Carer Lived Experience Workforce in Queensland – Victoria Stewart
12.45 PM Close
Victoria Stewart1,2*, Melanie Roberts1, Kim Walder1, Michelle Bissett3, Hannah Simmonds1, Maddy Slattery1
1School of Health Sciences and Social Work, Griffith University, Brisbane, Australia;
2Centre for Mental Health, Griffith University, Brisbane, Australia;
3Faculty of Health, Southern Cross University, Gold Coast, Australia.
Background:
Co-designing and partnering with people with lived experience expertise within higher education curriculum planning, development, and delivery in the health professions are increasingly embedded in policy and required by professional bodies. Experts-by-experience provide knowledge and perspectives that health educators do not necessarily possess, promoting an understanding of the experience of living with mental distress, and how professionals can best support positive outcomes. There is a growing expectation that health professional education programs broaden their expertsby-experience involvement beyond guest lectures to a partnership that spans curriculum design, development, implementation, and evaluation. While research in this area is growing, there is a lack of guidance in supporting experts-by-experience and health educators to partner in curriculum design, development and delivery. This presentation reports on the findings from a scoping review and qualitative study exploring principles of best practice, enablers and barriers to successful curriculum co-design and the experiences of those involved in co-designed education.
Method:
Six Australian experts-by-experience and six health educators were interviewed to share their experiences of codesigning and/or co-teaching health professional curricula. A qualitative descriptive approach underpinned a thematic analysis of the interviews. The scoping review examined key concepts, topics and issues within 141 studies. Study characteristics were extracted, and a thematic analysis of the data was undertaken.
Results:
Findings from both studies identified overlapping concepts. Five themes were developed from the scoping review that encapsulated the key concepts and issues: i) what’s in a name? navigating changing language and practices; ii)outcomes, perspectives and insights; iii) making it happen; iv) feeling supported and prepared; and v) balancing expertise and power. Four themes were generated from the qualitative data: i) Navigating co-teaching: From theory to practice, ii) Navigating the institutional labyrinth: Breaking down barriers, iii) Authentic partnerships, and iv) Beyond the blackboard: Real world connections.
Conclusions:
Co-design introduces social accountability to education, moving away from academics and academic institutions as the arbiters of knowledge, therefore shaping education in a less hierarchical manner. The findings identified a range of practical aspects, important considerations regarding ethical practice, and the complex conceptualisations of power that underpin co-designed education in higher education. In particular, the complexity of co-design, overcoming various institutional barriers, the importance of relationships and ensuring ethical and authentic partnerships were highlighted. The importance of how knowledge is understood and prioritised in higher education requires further consideration. There also needs to be robust research to develop our understanding of the theory and pedagogies underpinning co-designed education for health students and the longer-term outcomes from its inclusion in higher education settings.

Disclosures:
A grant from the Australian & New Zealand Association for Health Professional Educators supported the qualitative study. Funding from Griffith University in the form of a summer scholarship supported the initial search and article inclusion and exclusion of the scoping review.
Acknowledgements:
We thank the experts-by-experience and health educators who participated in the qualitative study. We would also like to acknowledge our student, Tullia Blackburn who supported the searching and screening of articles for the scoping review.
LIGHTNING PRESENTATION
Corollary discharges and inner speech as an explanation for auditory hallucinations in schizophrenia
Thomas Whitford1, Lawrence Kin-hei Chung2, Anthony Harris3,4*, Suzanne Ho-wai2
1School of Psychology, University of New South Wales (UNSW Sydney), Sydney, Australia
2Department of Psychology, The Chinese University of Hong Kong, Hong Kong SAR, China
3Discipline of Psychiatry, University of Sydney, Sydney, Australia
4Brain Dynamics Centre, Westmead Institute for Medical Research, Sydney, Australia
Background
Auditory-verbal hallucinations (AVH) – the experience of hearing voices in the absence of auditory stimulation – are a key feature of schizophrenia-spectrum disorders. It has long been suggested that some AVH may reflect the misperception of inner speech as external voices due to a failure of corollary-discharge related mechanisms. We aimed to test this hypothesis with an electrophysiological marker of inner speech.
Methods
Participants produced an inner syllable at a precisely specified time, when an audible syllable was concurrently presented. The inner syllable either matched or mismatched the content of the audible syllable. In the passive condition, participants did not produce an inner syllable. We compared the amplitude of the N1-component of the auditory-evoked potential between: (1) schizophrenia-spectrum patients with current AVH (SZAVH+, n = 55), (2) schizophrenia-spectrum patients without current AVH (SZAVH-, n = 44), (3) community controls (CC, n = 43).
Results
The community control group showed reduced N1-amplitude in the Match condition (relative to Passive and Mismatch), replicating our previous results. In contrast, the SZAVH+ group showed the opposite effect: enhanced N1-amplitude in the Match condition. The SZAVH- group showed no difference between the Passive and Match conditions, but reductions in the Mismatch condition.
Conclusions
This study supports the theory that some AVH are caused by abnormalities in the suppressive mechanisms associated with inner speech. This phenomenon of ‘inner speaking-induced suppression’ may have utility as a biomarker for AVH specifically and/or schizophrenia-spectrum disorders more generally.

Dr Stewart is a mental health practitioner, educator and researcher. She is passionate about promoting the voice of lived experience and using co-design to improve research and education outcomes. She currently co-leads the Lived Experience Network within the Griffith Centre for Mental Health.

Anthony Harris is a Professor of Psychiatry and the head of the specialty of Psychiatry at the University of Sydney. He is based at Westmead Hospital and the Westmead Institute for Medical Research. He is the consultant psychiatrist for a youth mental health service in the surrounding area.

Ariane Beeston – Centre of Perinatal Excellence (COPE)
“I’m on my way home from work when my baby turns into a dragon.”
Ariane Beeston is a child protection worker and newly registered psychologist when she gives birth to her first child – and very quickly begins to experience scary breaks with reality. Out of fear and shame, she keeps her delusions and hallucinations secret, but as the months pass Ariane gets worse. Much worse. Finally admitted to a mother and baby psychiatric unit, the psychologist is forced to learn how to be the patient.
With medication, the support of her husband, psychotherapy and, ultimately, time, Ariane rebuilds herself. And she also begins a new chapter working in perinatal mental health, developing resources to support other new mothers.
This presentation blends Ariane’s lived experience of postpartum psychosis, which affects 1-2 in 1000 mothers, as well as clinical and research updates for health professionals, drawn from her critically acclaimed memoir: Because I’m Not Myself, You See and her work at Centre of Perinatal Excellence (COPE)
It will include an overview of Ariane’s experience: symptoms (visual hallucinations, delusions of persecution and death) medication, treatment in a mother and baby unit and general psychiatric unit, a summary of “sliding-doors” moments for clinicians and health professionals to reflect on their own practice and biases.
It also includes discussion of why and how women can fall through the gaps when it comes to perinatal psychosis, how to detect it and what supports and treatments are available in Australia (including the importance of new public mother/ baby units).
The presentation will also cover the challenge of being a wounded healer and why those working in helping professions often miss out on vital treatment due to shame and stigma.
LIGHTNING PRESENTATION
Dysfunctional Parent
June Engeland1, Andrew Allen1, Rachel Brand1,*
1University of the Sunshine Coast, Australia
Background:
Research consistently reports an association between auditory hallucinations and traumatic experiences, yet the psychological mechanisms underpinning this relationship remain unclear. Empirical evidence suggests that enduring factors, such as early maladaptive schemas, interact with immediate stressors to elicit auditory hallucinations. Furthermore, personal beliefs and emotions are theorised to influence the interpretation of auditory hallucinations as realistic and malevolent. While auditory hallucinations are characterised by high phenomenological heterogeneity, common presentations include voices resembling a salient inner critic. Schema therapy’s dysfunctional parent modes represent one conceptualisation of the inner critic that encompasses the immediate activation of early maladaptive schemas and concurs with the episodic nature of auditory hallucinations. This study aimed to examine the role of dysfunctional parent modes in auditory verbal hallucinations by investigating whether activation of the inner critic increases hallucination-proneness and the negative emotional valence of speech illusions.
Method:
In a quasi-experimental design, forty-three participants from the general population completed the ‘Babble Task’, an experimental auditory perception task assessing hallucination-proneness, before and after an imagery exercise activating the inner critic. Participants also completed self-report questionnaires measuring hallucination-proneness, self-criticism, and demanding and punitive parent schema modes.
Results:
A mixed factorial analysis of variance found significant effects of the inner critic imagery exercise on speech illusions, with participants reporting more speech illusions following activation of their inner critic. Additionally, participants high on the demanding parent mode reported more speech illusions overall. Linguistic analysis of speech illusions demonstrated increased negative tone following activation of the inner critic.
Conclusion:
These findings suggest that an activated inner critic increases proneness to hallucinatory experiences and contributes to these experiences being negatively valanced. Schema therapy may be a useful theoretical model to understand the aetiology and phenomenology of auditory hallucinations, with the inner critic as a potential target for treatment using well-established schema therapy techniques.
Disclosures:
Funding was received from the School of Health Honours and Masters Funding Support at the University of the Sunshine Coast.
Acknowledgements:
We would like to thank the participants who volunteered their time to participate in this study.

Ariane Beeston is a former child protection worker and psychologist with the NSW Department of Communities and Justice (DCJ). After experiencing postpartum psychosis following the birth of her first baby, Ariane joined Centre of Perinatal Excellence (COPE). Her memoir Because I’m Not Myself, You See: was published in May 2024.

June Engeland is a research assistant and Master of Psychology (Clinical) student with an interest in the treatment of posttraumatic mental illness. June has collaborated on projects investigating the role of schema modes in auditory hallucinations, ketamine treatment in PTSD, and scalable trauma interventions in low-resource settings.

SYMPOSIUM
Victoria Stewart1*, Helena Roennfeldt1, Amanda Wheeler1, Caroline Robertson1, Rosie Hinson1, Liz Asser1
1Griffith Centre for Mental Health
Background:
Co-design and the meaningful involvement of people with lived experience of mental health challenges in research is strongly encouraged by prominent funding bodies in Australia (e.g., NHMRC, MRFF) and emphasised in the Australian Code for the Responsible Conduct of Research. In co-design research approaches, researchers and people with lived experience work together to identify research questions, design methodology and conduct the analysis. The approach relies on the capacity to share power and decision-making responsibility. It is therefore important to build both researcher and lived experience capacity to engage in new ways of thinking about research, including respect for different forms of expertise and an openness for working differently.
Method:
The symposium will feature three presentations:
1. Lived experience at the heart of research. Sharing perspectives from members of the Lived Experience Network: A network of people with a Lived Experience interested in research
2. Essential elements and practical recommendations for co-design in mental health research – a scoping review
3. Learnings and recommendations from developing a research-focused Lived Experience Network
Results:
1. The Lived Experience Network (LEN) is an initiative embedded within the Griffith Centre for Mental Health (GCMH) aiming to strengthen lived experience perspectives in research activities. This presentation explores what motivates Lived Experience members to build a network and their vision for the future of mental health research.
2. Essential elements and practical recommendations for co-design in mental health research – a scoping review: Despite growing advocacy and recognised benefits for adopting co-design methods in mental health research, embedding these approaches into standard research practices remains challenging. This scoping review examined co-design methodologies, pinpointing crucial elements and practices that facilitate co-design in mental health research. Traditional academic research frameworks, including inflexible funding structures and top-down decisionmaking, remain major obstacles to genuine co-design. However, the review also identified potential for innovative research methods and outcomes. This study offers examples of strategies to overcome barriers and provides actionable recommendations for implementing co-design in mental health research.
3. Learnings and recommendations in developing a lived experience network: This study used qualitative data from the LEN advisory group to explore the supports and barriers to developing a network within a university-based research centre. Supports included the strength of a co-model of leadership, the need for a shared vision and a strong lived experience representation. Several barriers were noted in achieving authentic co-design, including structures within the university setting. Strategies for the network’s sustainability are also considered within a broader understanding of the tensions in achieving lasting change.
Conclusions:
While many health researchers engage with people with lived experience and end users, there is a need to build openness to recognise lived expertise and shared decision-making within co-design approaches to research. People with lived experience have often been excluded from meaningful involvement in research processes. There is a need to build trust and mutual respect to ensure that both researchers and people with lived experience are open to engaging in research processes that do not lead to further trauma and experiences of discrimination.
Disclosures:
Funding was received from the Griffith Centre for Mental Health for studies 1 & 3 and study 2 was supported by a cofunded Collaboration Grant between MSH SERTA and UQ Faculty of Medicine and Griffith University.
Acknowledgements:
We would like to acknowledge the Lived Experience Network members and advisory group for their time and expertise in informing these presentations.

Dr Stewart is a mental health practitioner, educator and researcher. She is passionate about promoting the voice of lived experience and using co-design to improve research and education outcomes. She currently co-leads the Lived Experience Network within the Griffith Centre for Mental Health.

Systematic review and meta-analysis of the relationship between repetitive negative thinking (worry and rumination) and positive symptoms of psychosis
Sharla Cartner1*, Imogen H Bell2,3, Kayan Skinner1, Wolfgang Viechtbauer5, Neil Thomas1
1Centre for Mental Health, Swinburne University of Technology, Melbourne, Australia
2Orygen
3Centre for Youth Mental Health, The University of Melbourne
4Maastricht University
Background:
This study aims to consolidate findings on repetitive negative thinking (RNT), including worry, rumination, and general RNT, and group them within psychosis indices (positive symptoms, hallucinations, and delusions) to better understand their relationships. Specifically, this review addresses: (a) Do people with positive psychotic symptoms exhibit greater levels of RNT than healthy controls? (b) Among people with positive psychotic symptoms, is RNT associated with symptom severity?
Method:
Forty-two peer-reviewed studies were identified across five databases reported either (1) a correlation between RNT measures and positive psychotic symptom indices or (2) a mean difference between a clinical group (with formal psychosis diagnoses or positive psychotic symptoms above a clinical threshold) and healthy controls.
Results:
The findings indicate that people with positive psychotic symptoms exhibit significantly higher levels of RNT compared to healthy controls (Hedge’s g = 0.86, p < .001; 95% prediction intervals (PIs): 0.69–1.03).
Large effects were observed for delusions (Hedge’s g = 1.31, 95% PIs: 0.92–1.70) and hallucinations (Hedge’s g = 0.91, 95% PIs: 0.13–1.69), while positive symptoms showed a medium effect size (Hedge’s g = 0.70, 95% PIs: -0.10–1.50). Across studies, all measures of RNT were significantly associated with all positive psychotic symptom indices (r = .33, p < .001; 95% PIs: .03–.58). Medium effects were observed for delusions (r = .41, 95% PIs: .12–.63) and hallucinations (r = .34, 95% PIs: -0.08–.66), and a small effect size for positive symptoms (r = .18, 95% PIs: -0.19–.48).
Conclusion:
The results suggest, RNT plays a significant role in positive psychotic symptoms, despite what RNT measure were used. These results suggests clinical interventions targeting RNT may mitigate these symptoms. A key limitation is the lack of studies investigating rumination and general RNT.

Sharla Cartner is a PhD student at Swinburne University of Technology investigating attentional processes and activity engagement in auditory verbal hallucinations. Her research seeks to advance understanding of attentional processes underlying hallucinations, with a focus on self-management in mental health.
LIGHTNING PRESENTATION
Unveiling New Insights into the Variation of Community Treatment Orders: The FACTOR Study
Lisa Brophy1,2, Tessa Zirnsak1, Chris Maylea3, Penelope Weller4, Sharon Lawn5,6, Vrinda Edan7, Christopher James Ryan8,9,10, Edwina Light11, Giles Newton-Howes12, Morgan Gould1, Claudia Bull2,13,14, Puneet Sansanwal7, Steve Kisely a,b,c,d,2,13,14,15,16
1Social Work and Social Policy, Department of Community and Clinical Health, School of Allied Health, Human Services and Sport, La Trobe University, Victoria, Australia
2The ALIVE National Centre for Mental Health Research Translation, The University of Queensland, QLD, Australia
3Law School, La Trobe University, Melbourne, Victoria, Australia
4Graduate School of Business and Law, RMIT University, Melbourne, Victoria, Australia
5Lived Experience Australia, Adelaide, South Australia, Australia
6College of Medicine and Public Health, Flinders University, Adelaide, South Australia
7Medicine, Dentistry and Health Sciences, University of Melbourne
8Discipline of Psychiatry and Mental Health, University of New South Wales, Sydney, NSW, Australia.
9School of Medicine, University of Notre Dame Sydney, Sydney, Australia.
10Department of Psychiatry, St Vincent’s Hospital, Darlinghurst NSW, Australia.
11University of Sydney, Sydney, NSW, Australia.
12University of Otago, Wellington, New Zealand
13The University of Queensland School of Medicine, Qld, Australia
14Metro South Health Service, Woolloongabba, Qld, Australia
15Griffith Criminology Institute (GCI), Griffith University, Qld, Australia
16Dalhousie University, Departments of Psychiatry, Community Health and Epidemiology, Halifax, Nova Scotia, Canada
Background:
There is emerging evidence that forced community treatment in the form of community treatment orders (CTOs) is applied arbitrarily and disproportionally affects marginalised groups such as Aboriginal and Torres Strait Islander peoples and those from culturally and linguistically diverse (CALD) backgrounds. However, this has never been systematically studied. The Australian Factors Affecting Community Treatment Orders Research Study (FACTORS) aims to explain, for the first time across Australia, the drivers underpinning variations in the use of forced community treatment, including who is most likely to be subjected to forced treatment and in what context.
Method:
The study has several arms with different foci. These include: a law and policy arm, interrogating the relationship between doctrine and practice, an administrative health data arm, investigating the variables associated with CTO placement and the impact of CTOs on health service use, a qualitative study, investigating clinician, service user and supporter experiences of CTOs, and a lived experience advisory panel, who provide feedback on the conduct of the study along with our First Nations consultant. All arms work together to investigate the variation in rates of CTOs.
Results:
Overall project findings so far suggest that there is considerable variation in implementation of CTOs between and within Australian states. In Queensland, we found that CTO use was more likely in people from First Nations (ORadj 1.14; 95% CI= 1.06-1.23), culturally diverse backgrounds (ORadj 1.45; 95% CI = 1.33–1.59), or those with a preferred language other than English (ORadj 1.21; 95% CI= 1.02-1.44). There is also a lack of consistent and comprehensive policy to guide practice Australia-wide. It appears that service-level factors are influencing the rates of CTOs. More research is required to understand what these influences are, and how they are interacting with CTO rates.

Conclusions:
The variation in rates of CTOs is concerning, particularly in light of our findings that this variation comes from service level influences, rather than service user needs.
The data collected across the multiple arms of this study create a narrative of how CTOs are being used, and suggest areas for reform that will generate social and cultural benefits for those directly affected and the broader community. This has clear implications for both clinical practice and policy.
Disclosures:
The authors have no conflicts of interest to declare
Acknowledgments:
We would like to thank the lived experience advisory team for their partnership throughout this study.

Lisa Brophy is a leading researcher on recovery, social inclusion, and human rights for people with psychosocial disabilities. She serves on Victoria’s Mental Health and Wellbeing Act Expert Advisory Group, the board of the Victorian Collaborative Centre, and is a Fellow of the Academy of Social Sciences in Australia.
LIGHTNING PRESENTATION
Qualityoflifeofpeoplewithmentalhealthchallengesandproblematic substanceusewhileengagedwithanexercisephysiologyservice
Jane Kugelmana, Meg A Doohanb, Brett Dyerc (Jake O’Briend, Mridula Kayale, Justin J Chapmanb,f,g,h*
a School of Public Health, The University of Queensland, Brisbane, Queensland, Australia
b Centre for Mental Health, School of Pharmacy and Medical Sciences, Griffith University, Brisbane, Queensland, Australia
c Griffith Biostatistics Unit, Griffith Health, Griffith University, Brisbane, Queensland, Australia
d Department of Gastroenterology and Hepatology, Metro South Health, Brisbane, Queensland, Australia
e Cairns and Hinterland Hospital and Health Service, Cairns, Queensland, Australia
f Addictions and Mental Health Service, Metro South Health, Brisbane, Queensland, Australia
g QIMR Berghofer Medical Research Institute, Brisbane, Queensland, Australia
h Equally Well Australia, School of Business, Charles Sturt University, Bathurst, New South Wales, Australia
Background:
People with mental health challenges and problematic substance use can experience low quality of life (QoL). Regular exercise can improve QoL, and Accredited Exercise Physiologists (AEPs) can provide evidence-based exercise interventions for people with a range of health conditions. The aim of this study was to evaluate QoL for people with mental health challenges and problematic substance use while engaged in a community-based AEP-led exercise and healthy lifestyle service.
Method:
The service was implemented over three years and involved weekly group exercise sessions and health education. Assessments were conducted every three months. Outcomes included the Assessment of Quality of Life (AQoL-6D) scale, social support, sense of belonging, self-reported exercise, and anthropometric measures. Linear mixed-effects models were used to evaluate trajectories of QoL total score and each dimension (independent living, pain, senses, relationships, mental health, coping).
Results:
A total of 295 participants were inducted, with 161 completing at least two assessments. QoL improved by 0.058 per year (95%CI: 0.018-0.098), predominantly in mental health and coping dimensions (0.075 (95%CI:0.014-0.136) and 0.073 (95%CI:0.012-0.135) per year, respectively). Higher social support and sense of belonging at baseline were associated with positive QoL trajectories. Women, participants with multimorbidity, and those with non-psychotic mental illnesses had less favourable QoL trajectories.
Conclusions:
AEP-led exercise and healthy lifestyle programs can improve QoL in people with mental health challenges and problematic substance use. Social support and sense of belonging are important for positive outcomes. Targeted interventions are needed for specific groups, such as women and those with multimorbidity.


Justin Chapman completed his doctorate in measuring and positively influencing physical activity behaviour in adults with mental illness (2016). Dr Chapman is a Research Fellow at Griffith University and Metro South Addictions and Mental Health Service. He takes a national approach to translational research in health service models to improve the physical health and wellbeing of people with mental illnesses. Through extensive industry partnerships with non-government organisations, hospital and health services, and sports and recreation organisations, Dr Chapman has successfully scaled up exercise programs evaluated in clinical trial designs to social impact for over 600 participants with mental illness. Dr Chapman’s work has been acknowledged with an Open Minds Mental Health Week Achievement awards (2018), and the Australian Rotary Health award for Mental Health Impact (2020). He is a Board member of the national advocacy organisation Psychosis Australia, and on the Editorial Board of the journal Mental Health and Physical Activity.
Victoria Stewart1,2*, Lorna Downes3, Cindy Heddle, Marianne Wyder4, Kath Sellick3, Amanda Wheeler1,2,5, Katherine Reid1,2
1School of Health Sciences and Social Work, Griffith University, Brisbane, Australia;
2Centre for Mental Health, Griffith University, Brisbane, Australia;
3University of Melbourne, Melbourne, Australia.
4Metro South Addiction and Mental Health Services, Queensland, Australia
5Faculty of Medical and Health Sciences, Auckland University, Auckland, New Zealand
Background:
Family/carers are important partners in the support and recovery of people experiencing mental distress. Several enquiries into Australia’s mental health system have found that families and carers can feel excluded from the mental health system, undermining their role in their family member’s recovery. The Family/Carer Lived Experience (F/CLE) workforce plays an essential role in supporting families and carers, ensuring service development, provision, and evaluation are responsive to the needs of families and carers. The growth in the Lived Experience workforce has largely focused on Consumer or Personal Lived Experience (Peer) workers, those who have a personal experience of mental health concerns and engaging with mental health services. F/CLE roles are still evolving in Queensland and much of Australia and little is known or understood about the types of roles that F/CLE workers are undertaking, the supports available for this workforce and how the Consumer and Carer workforce work together.
Method:
This study partially replicated the Victorian ‘Rising Together’ study. An initial mapping of the Queensland F/CLE workforce was undertaken to better understand where F/CLE workers are employed. Based on feedback from our Advisory Group, minor changes to the co-designed survey from the Victorian study were made to better fit the Queensland context. The survey was distributed through contacts made during the mapping process and the research teams’ networks. Survey results were discussed during two focus groups to allow a richer understanding of the reasons, motivations and attitudes behind participants’ responses to the survey.
Results:
44 F/CLE workers and advisor survey responses were received. Responses provide an overview of the scope and roles of the Queensland F/CLE workforce, their motivations to work in these roles, their experiences in the workplace and what supports could improve job satisfaction and safety. Insights into the differences between the Queensland and Victorian workforces will also be presented.
Conclusions:
The F/CLE workforce is an important emerging workforce that has received limited attention in service development and policy. The F/CLE role can be a complex, isolated experience that was not always valued by leaders or multidisciplinary teams. This was often due to the mental health system focusing on individuals rather than family networks. Our study identified a need to improve role clarity and workplace conditions for the existing workforce, increase the number of F/CLE workers and educate the broader mental health workforce about the benefits and scope of F/CLE worker roles. Supervision, professional development, and career opportunities are underdeveloped, and further attention needs to be paid to reduce the negative impacts of the roles and ensure the workforce’s safety and sustainability.
Disclosures:
A seed grant from the ALIVE National Centre for Mental Health Research Translation supported this study.

Acknowledgements:
We thank all Family/Carer Lived Experience workers and representatives who contributed to this Project by engaging in the survey or focus group. We also thank The Alive National Centre for Mental Health Research Translation for supporting this project through their Next Generation Capacity Building Funding Scheme.
11.15 AM Cannabidiol (CBD) for Clozapine Refractory Schizophrenia (CanCloz): A randomised controlled trial – Mike Trott
11.25 AM Evaluating the feasibility and acceptability of two dietary interventions for individuals with schizophrenia: The SNaCK study – Donni Johnston
11.35 AM Schizophrenia and Diabetes Mobile-Assisted Remote Trainer (S.M.A.R.T.): A codesigned digital intervention to improve diabetes self-management in people with schizophrenia – Urska Arnautovska
11.45 AM A Risk Prediction Model for Metabolic Syndrome in Psychosis – Dulari Hakamuwa Lekamlage
11.55 AM STEPS: Designing a digital Intervention to reduce Sedentary Behaviour via Physical Activity Snacks in Severe Mental Illness – Mike Trott
12.05 PM Increasing access to psychological therapies for psychosis in Australia: The need to upskill the private practice psychology workforce. – Rachel M. Brand
12.15 PM The utility of six-minute walk test and maximal fitness test in people with psychotic disorders– Meg Doohan
12.25 PM The Benefits of Belly Dance and Somatic Movement to Improve Mental and Physical Health and Wellbeing - A Pilot Study – Giulietta Valuri
12.35 PM Simplifying consent: A user-centered approach for people with schizophrenia –Rebecca Soole (Presented by Urska Arnautovska)
12.45 PM Close

Dr Stewart is a mental health practitioner, educator and researcher. She is passionate about promoting the voice of lived experience and using co-design to improve research and education outcomes. She currently co-leads the Lived Experience Network within the Griffith Centre for Mental Health.

Cannabidiol (CBD) for Clozapine Refractory Schizophrenia (CanCloz): A randomised controlled trial.
Mike Trott *1,2,3; Urska Arnautovska1,2,3; Steve Kisely1,2,3 Andrea Baker2,3; Dan Siskind 1,2,3
1Faculty of Medicine, University of Queensland, Princess Alexandra Hospital, Brisbane
2Queensland Centre for Mental Health Research, Wacol
3Metro South Addiction and Mental Health Services, Brisbane
Background:
Approximately 3% of the population are affected by psychosis, characterised by disturbance in cognition, affect, perception and behaviours. These psychotic conditions, such as schizophrenia, can be difficult to treat, even with optimal therapy. Approximately one third of people with schizophrenia have treatment resistant schizophrenia (TRS). TRS is defined as ongoing symptoms and functional impairment despite two adequate and adherent trials of different antipsychotics. Currently, the most effective antipsychotic for TRS is clozapine, which leads to reductions in positive symptoms and hospitalisations. Even so, only 40% of people with TRS trialled on clozapine meet clinical response criteria. For people with clozapine resistant schizophrenia, there are few agents available to augment treatment, and they have limited effectiveness.16
Despite encouraging results of cannabidiol (CBD) on psychosis symptoms, to date, there have been no trials of CBD among people with clozapine resistant schizophrenia.
Method:
This is a two-arm, double-blind randomised controlled trial to determine the efficacy of 1000mg daily CBD on positive symptoms in people with clozapine resistance schizophrenia, against non-active placebo. Positive symptoms were assessed using the Positive and Negative Syndrome Scale (PANSS positive subscale). Data was analysed using mixed measures repeated measures.
Results:
These results are from the pre-planned interim analysis. A total of 20 participants completed the study before the 1st interim analysis. Regarding the primary outcome, PANSS positive score decreased by 2.89 (SD 3.02) in the control group, and decreased by 3.82 (SD 2.82), a difference of 0.93 in favour of the intervention group (p=0.5; Cohen’s d=0.32).
Conclusions: The evidence from this in-progress trial supports the hypothesis that CBD augmentation in people with clozapine resistant schizophrenia helps alleviate positive symptoms.
Disclosures:
Funding was received from the Princess Alexandra Hospital Foundation

Mike completed his PhD in Sport and Exercise Sciences in 2022, and working with the Cambridge Centre for Sport and Exercise Sciences, and the Cambridge Vision and Eye Research Institute. Mike’s research interests include physical activity promotion in severe mental health, child maltreatment, and statistical considerations in complex clinical trials.
LIGHTNING PRESENTATION
Evaluating the feasibility and acceptability of two dietary interventions for individuals with schizophrenia: The SNaCK study
Donni Johnston1,2, Urska Arnautovska1,2,3, Andrea Baker3, Ingrid Hickman1, Hannah Mayr1,2, Nicole Korman1,2, Wolfgang Marx4, Nicola Warren1,2, Scott Teasdale5, Dan Siskind1,2,3
1Faculty of Medicine, The University of Queensland, Brisbane, QLD, Australia
2Metro South Addiction and Mental Health Service, Brisbane, QLD, Australia
3Queensland Centre for Mental Health Research, Wacol, QLD, Australia
4Faculty of Health, School of Medicine, Deakin University
5Faculty of Medicine and Health, The University of Sydney, Sydney, NSW, Australia
Background:
Individuals with schizophrenia face a significantly higher prevalence of chronic physical health conditions, especially cardiovascular diseases, leading to a 20-year reduction in life expectancy. Poor diet, compounded by side effects of antipsychotic medications and cognitive impairments, is a key modifiable risk factor. The Schizophrenia, Nutrition and Choices in Kilojoules (SNaCK) study aims to evaluate the feasibility, acceptability, and preliminary effectiveness of two dietary interventions—pre-prepared meals and meal kits—for individuals with schizophrenia.
Methods:
The SNaCK study employs a 12-week, three-arm randomized controlled trial (RCT) crossover design. Eighteen participants aged 18-64 years diagnosed with schizophrenia or schizoaffective disorder were recruited from a public community mental health service in inner urban Brisbane. Participants were randomized to receive either prepared meals, meal kits, or a supermarket voucher as a control, each for four weeks. Primary outcomes included feasibility and acceptability assessed through self-reported checklists and qualitative interviews. Other variables of interest included physical health measures, dietary intake, quality of life and food security measures.
Results:
Overall data on meal adherence, food wastage, and preparation difficulty indicated both interventions were generally acceptable and feasible for participants. Qualitative feedback provided insights into participants’ experiences and preferences.
Conclusion:
The SNaCK study addresses critical dietary needs of individuals with schizophrenia, a group at high risk for dietrelated health issues. Findings will inform future larger RCTs and could lead to improved dietary intervention strategies, leveraging resources like the National Disability Insurance Scheme (NDIS) to enhance health outcomes for this vulnerable population.
Disclosures:
Funding was received from Metro South Health Research Support Scheme (MSH RSS) Project Grant (RSS_2023_015) “’Improving metabolic health in patients with schizophrenia: feasibility, acceptability, and preliminary effectiveness of two dietary interventions”.

Donni Johnston is a Senior Community Nutritionist at Metro South Addiction and Mental Health Services. Currently pursuing a Higher Degree in Research on food use skills in people with severe mental illness (SMI). Donni has contributed to legislation mandating access to healthy food for adults with SMI in Queensland residential care.

Dulari Hakamuwa Lekamlage1,*, Asier Corrales2,3, Manuel J Cuesta2,3, Carl Moller1 , Mohammadreza Mohebbi1, Mojtaba Lotfaliany1, Alison R Yung1, PEPsNa groupd
1The Institute for Mental and Physical Health and Clinical Translation (IMPACT), Deakin University, Geelong, Victoria, Australia
2Department of Psychiatry, Navarra University Hospital, Pamplona, Spain
3Mental Health Department, Navarra Health Service – Osasunbidea, Pamplona, Spain
Background:
Individuals with psychotic disorders, such as schizophrenia, have a significantly reduced life expectancy, often by 10–15 years, compared to the general population. This reduction is largely due to a higher incidence of physical health issues like type 2 diabetes and cardiovascular disease (CVD). These conditions reduce quality of life, increase mortality, and impose a substantial economic burden on healthcare systems.
An early marker of cardiometabolic disease risk is the metabolic syndrome (MetS), which is a clustering of metabolic abnormalities such as disrupted glucose-insulin homeostasis, adiposity, hypertension, and dyslipidaemia. Early detection of high-risk individuals in MetS is essential for preventing progression to chronic cardiometabolic disease.
Method:
We analysed data from an early intervention for psychosis service in Navarra, Spain, which consists of both inpatient and outpatient individuals aged 15-55 years with first episode of psychosis. We aimed to identify risk and protective factors for MetS . We used logistic regression with a time-clustered variance-covariance structure, incorporating negative and positive symptoms, duration of untreated psychosis, duration of untreated illness, premorbid and current functioning, socioeconomic status, childhood stress, substance use, age, sex, immigration status, and using antipsychotic as potential predictors of MetS status.
Results:
Risk factors for MetS comprised childhood sexual abuse (OR= 4.30, 95% CI=1.64-10.37, p=0.002), severe tobacco use (>20 cigarettes/day) (OR= 2.81, 95% CI= 1.45-5.29, p<0.001), immigrant status (OR= 1.89, 95% CI= 1.19-2.98, p<0.001), medium socioeconomic status (OR= 1.79, 95% CI= 1.11-2.88, p=0.011), negative symptoms (OR= 1.62, 95% CI= 1.04-2.56, p<0.001), and age (OR= 1.05, 95% CI= 1.03-1.07, p<0.001). Protective factors included and being female (OR= 0.33, 95% CI= 0.20-0.54, p<0.001), moderate/high cannabis use (OR= 0.34, 95% CI= 0.14-0.73, p=0.023), higher socioeconomic status (OR= 0.57, 95% CI= 0.33-0.96, p=0.024), and current functioning (OR= 0.97, 95% CI= 0.96-0.99, p<0.001).
Conclusions:
These findings highlight having negative symptoms, medium socioeconomic status, childhood sexual abuse, high tobacco consumption, older age, and being an immigrant as risk factors. Protective factors include being female, moderate or high cannabis use, higher socioeconomic status, and global functioning. Individuals with these risk factors warrant close metabolic monitoring and consideration for early use of specific interventions to reduce risk. These could include dietician and exercise physiologist referral, anti-smoking interventions, and use of pharmacological agents such as metformin, GLP1 receptor agonists such as semaglutide (Ozempic), anti-hypertensives and/or statins. These measures may reduce MetS and potentially fatal CVD outcomes.
Disclosures:
The authors declare that they have no conflicts of interest.
Acknowledgements:
The authors would like to thank all participants and their parents for their participation.

Dulari Hakamuwa Lekamlage is a Research Fellow in Biostatistics at the Institute for Mental and Physical Health and Clinical Translation, Deakin University. She completed her PhD in Applied Statistics at Queensland University of Technology. She has expertise in longitudinal data analysis, predictive modeling, and machine learning techniques for healthcare applications.

Mike Trott *1,2,3; Nicole Korman1,2,3; Justin Chapman1,4; Urska Arnautovska1,2,3; Dan Siskind 1,2,3
1Metro South Addiction and Mental Health Service, Metro South Health, Brisbane, Australia
2Queensland Centre for Mental Health Research, Wacol, Australia
3School of Medicine, The University of Queensland, Brisbane, Australia
4School of Pharmacy and Medical Sciences, Centre for Mental Health, Griffith University, Brisbane, Queensland, Australia
Background:
People with severe mental illness (SMI), including schizophrenia, bipolar disorder, and major depression, have high levels of sedentary behaviour, a major risk factor for cardiovascular disease and premature mortality. Current physical activity (PA) interventions in SMI have primarily focused on structured exercise programs, which are resource-intensive, challenging to scale, and exclude those unwilling or unable to engage in structured activity.
Methods:
This project aims to develop a novel, scalable intervention based on PA snacks (<10 minutes in duration) that can be performed without special equipment, using digital solutions. We will explain two Work Packages: 1) Design phase of a digital app with associated wrist wearable; and 2) Pilot study to determine feasibility and acceptability.
Results:
We will discuss consumer involvement in Work Package 1, and study design in Work Package 2. It is expected that the STEPS app may increase PA and decrease sedentary behaviour in people with severe mental illness, with associated metabolic outcomes.
Conclusion:
The STEPS app may increase physical activity and decrease sedentary behaviour in people with SMI, with associated metabolic outcomes.
Disclosures:
Funding was received from the MSH Research Support Scheme (RSS) Project Grant (ID RSS_2024_095), awarded to MT.
Increasing access to psychological therapies for psychosis in Australia: The need to upskill the private practice psychology workforce.
Brand, R.M.1 Wilson, T.1, and Rune, K.1
1 School of Health, University of the Sunshine Coast, QLD, Australia.
Background:
Cognitive behavioural therapy for psychosis (CBTp) is an effective psychological intervention and is recommended by Australian guidelines. Unfortunately, access remains limited in Australia, with only 10% of people receiving evidencebased CBTp. People with persistent, but stable, psychotic experiences are increasingly discharged from secondary care for management within primary care and are thus moving toward private practice for their additional support needs (including for psychological interventions through Medicare or the National Disability Insurance Scheme). This shifting landscape of service provision provides an opportunity for a much-needed increase in access to CBTp, through the private practice psychology workforce. In order to harness the potential capacity of the private practice psychology sector it is important to understand the willingness of private practice psychologists to treat psychotic symptoms and any potential barriers to the implementation of CBTp in this setting.
Method:
An online survey was completed by 261 Australian private practice psychologists. Participants were asked whether they would accept a referral to treat someone with active psychotic symptoms. In addition, data was gathered on variables that previous research has found to be relevant in the implementation of CBTp, including: hours of training, hours of experience, access to supervision, stigma, causal beliefs about psychosis, and therapeutic optimism. To assess which variables predicted acceptance of the referral, a binomial logistic regression was conducted.
Results:
Only 38% of private practice psychologists indicated that they would accept the referral. Psychologists also reported low levels of training and practical experience in psychological therapy for psychosis. Experience, stigma, causal beliefs about psychosis, and therapeutic optimism were significant predictors of accepting the referral.
Conclusions:
These findings suggest that if private practice psychologists are to be part of the solution to increasing access to psychological therapies for psychosis, there is a need to upskill our private practice psychology work force.

Mike completed his PhD in Sport and Exercise Sciences in 2022, and working with the Cambridge Centre for Sport and Exercise Sciences, and the Cambridge Vision and Eye Research Institute. Mike’s research interests include physical activity promotion in severe mental health, child maltreatment, and statistical considerations in complex clinical trials.

Rachel is a Clinical Psychologist and Senior Lecturer in Clinical Psychology at the University of the Sunshine Coast. Rachel has provided psychological therapies for people experiencing psychosis for over 15 years and conducts research into developing and disseminating psychological interventions for people experiencing distressing psychosis.

Meg Doohana*, Justin Chapmana,b,c, Justin Hollandd, Nicole Kormanb,d,e, Robert Mullinsd, Steve Kohd, Rob Robergsd
aSchool of Pharmacy and Medical Science, Centre for Mental Health, Griffith University, Queensland, Australia
bAddictions and Mental Health Service, Metro South Health, Queensland, Australia
cQIMR Berghofer Medical Research Institute, Queensland, Australia
dSchool of Exercise and Nutrition Sciences, Queensland University of Technology, Queensland, Australia
eSchool of Medicine, University of Queensland
Objectives:
People with psychotic disorders have low cardiorespiratory fitness (CRF), contributing to low physical functioning and heightened risk of cardiometabolic diseases. CRF can be directly measured using a cardiopulmonary exercise test (CPET) in which peak oxygen consumption (VO2peak) is measured during maximal exercise, or estimated using submaximal fitness tests, such as the six-minute walk test (6MWT). The aim of this study was to evaluate the utility of the CPET and 6MWT in people with psychotic disorders to inform physical health screening practices in mental health services.
Methods:
37 people with psychotic disorders were recruited from tertiary mental health services. Participants completed two 6MWTs, a CPET, and self-report questionnaires about negative symptoms and perceptions of the CPET. Regression analyses were used to investigate the validity of 6MWTs for predicting VO2peak measured using the CPET. Feasibility and acceptability of the CPET was evaluated using adherence, completion rates, and test perceptions.
Results:
Most participants did not adhere to CPET preparation instructions, and VO2peak was unable to be measured for eight participants because of early termination. The first 6MWT trial did not significantly predict VO2peak; however, the second 6MWT trial combined with age explained 60.1% of the variance in VO2peak. Despite reporting discomfort with the CPET, participants reported generally positive experiences.
Conclusions:
While the CPET was acceptable for participants, feasibility is limited by low adherence and completion rates. The 6MWT may be a suitable alternative; however, only the second attempt provided a reasonable estimate of VO2peak

Meg is a postdoctoral research fellow in the Centre for Mental Health at Griffith University; her work focusses on the influence of physical health interventions on individuals with severe mental illness. Meg earned her PhD from QUT in 2024, where her research explored the influence of dehydration and thermal strain on cognitive and physical performance in females.
LIGHTNING PRESENTATION
Giulietta Valuri1,*, Anna Waterreus1, Susie Hincks2
1Neuropsychiatric Epidemiology Research Unit, School of Population and Global Health, University of Western Australia. 2Meeting for Minds, Perth, Western Australia and lived experience research partner
Background:
People with severe mental illness often experience low self-esteem, loneliness, social disconnection, impaired cognitive function and a reduction in overall health and wellbeing. Evidence shows the use of dance movement therapy is associated with improvements in physical, emotional and cognitive areas. Belly dancing, also known as Arabic or Middle Eastern dance, is a form of dance that has been practiced by both men and women, for many years. Those who participate in this activity have reported experiencing a healing effect, a sense of community, belonging and support, and feeling more empowered, specifically improved self-confidence. To date, few studies have explored Belly Dance as a tool to improve mental and physical health and wellbeing.
The aim of this pilot study was to examine the short-term impacts of participating in Belly Dance classes on mental and physical health and wellbeing.
Method:
Adult participants, from the general community, were recruited into one of two dance groups and took part in four, one hour, dance classes over 4 weeks. The classes were run by a professional teacher and consisted of a maximum of 12 people. Each participant completed questionnaires at baseline (before the first class), after each class and after the 4 weeks of classes. A short group discussion was conducted after each class and comments and feedback were collected from each participant. Participants were reimbursed for their time. The study involved analysing both quantitative and qualitative data.
Results:
A total of 21 people participated, ranging in age from 19 to 87 years and all were women. Classes were well attended with 85.7% of participants attending all 4 classes. At baseline 52.4% rated their current mental health and wellbeing to be very good or excellent and 38.1% fair. Eight of the participants (38.1%) were currently receiving treatment (medication/therapy) for a mental illness. At end of study the proportion rating their current mental health and wellbeing as very good or excellent rose to 66.7%. Also, 81% reported an improvement in their overall physical health, 76% reported social improvements and 100% indicated that the classes had had a positive impact on their overall mental health and wellbeing. Participants’ commenting that they felt more connected, less anxious, less self-conscious, happy and relaxed.
Conclusions:
Belly Dancing can provide a flexible and comfortable environment in which everyone can participate regardless of their age, gender, size, background or ability. This pilot study suggests that participating in a brief series of Belly dance classes may be associated with an increase in self-confidence, social connectedness, and overall mental and physical health and wellbeing. Therefore, it could be a novel approach to address some of the challenges people with psychotic disorders experience including social isolation, self-stigma and low levels of physical activity.
Disclosures:
Funding was received from The School of Population & Global Health 2023 Staff Incentive Scheme.
Acknowledgements:
We would like to acknowledge those who participated in the dance classes and group discussions, and Keti Sharif, professional Belly Dance and Somatic Movement teacher, who conducted the dance classes.


Dr Giulietta Valuri is an epidemiologist and data analyst with expertise in database design, data management and analysis. She has worked extensively with linked population databases in both criminology and mental health. Giulietta is also a Belly Dancer and has recently incorporated her passion for Belly Dancing into her research.
LIGHTNING PRESENTATION
Simplifying consent: A user-centered approach for people with schizophrenia
Rebecca Soole1,2,3*, Urska Arnautovska1,2,3, Nicole Korman1,2, Andrea Baker3, Dan Siskind1,2,3
1Faculty of Medicine, University of Queensland, Brisbane, Australia
2Metro South Addiction and Mental Health Services, Brisbane, Australia
3Queensland Centre for Mental Health Research, Brisbane, Australia
Background:
Individuals with schizophrenia face unique cognitive challenges, including difficulties with attention and memory, which can hinder their ability to fully understand and engage with traditional, typically paper-based Patient Information and Consent Forms (PICFs). These often lengthy, jargon-heavy documents can act as barriers rather than facilitators of informed consent, potentially limiting an individual’s participation in research and excluding a marginalised population from studies that could benefit them. This study aimed to redesign our a traditional, paper-based PICF to improve accessibility, comprehension, and engagement in clinical trials for individuals with schizophrenia while maintaining ethical and regulatory integrity.
Methods:
Using a participatory co-design approach, we conducted two collaborative sessions with individuals with lived experience of schizophrenia, recruited from community-based rehabilitation facility in Brisbane. Participants provided feedback on our traditional PICFs utilised in current practice and contributed to the development of revised materials tailored to their needs and preferences. Key considerations included simplifying language, incorporating visual elements, and structuring information to enhance comprehension and engagement.
Results:
The co-design process resulted in a two-tiered PICF system: (1) a short, user-friendly version featuring icons, a question-and-answer format, and simplified language to facilitate initial discussions, and (2) a detailed, text-based version maintaining essential study details while incorporating consistent visual elements for ease of navigation. Additional design enhancements included increased white space, thoughtful use of colour, and a focus on autonomysupportive language.
Conclusions:
By involving individuals with lived experience, we developed a PICF format that is more accessible, inclusive, and empowering. These redesigned forms have been integrated into ongoing research and approved for use in a national multi-site clinical trial. This work underscores the importance of tailoring consent materials to diverse populations and provides a framework for improving informed consent processes across research involving individuals with cognitive or communicative challenges.
Disclosures:
Funding was received from UQ Faculty of Medicine EMCR and HDR Consumer and Community Involvement (CCI) Kickstart Internal Funding Scheme.
Acknowledgements:
We would like to acknowledge consumers who participated in the codesign consultation groups that informed the redesign of the PICF.

Dr. Rebecca Soole is a Postdoctoral Research Fellow at UQ Medical School and a Psychologist. She received the Chancellor's Award for Excellence (2016) for her PhD. Passionate about lived experience-driven research, she focuses on improving mental health of people with severe mental illness.

11.15 AM Reducing stigma and discrimination: A Lived Experience & current research perspective – Amanda Aiyana
11.25 AM Post traumatic growth following psychosis – a lived experience perspective – Tracey Watson
11.35 AM How the Power, Threat, and Meaning Framework Aligns with Recovery from Psychosis – Justin McDermott
11.45 AM Unshared Realities: A co-designed interactive learning experience with discovery college – Joseph Muro & Lucy Mahony
11.55 AM Hearing Voices and the Quest for Autonomy: An Interpretative Phenomenological Analysis – Sepinood Noroozi
12.05 PM STEPS Transitional Recovery and Support Service: A Contemporary, Holistic Service Model for Sustainable Recovery – Cameron Thayer, Martin Staines and Kimberley Lloyd-Jones
12.35 PM Close
LIGHTNING PRESENTATION
Reducing stigma and discrimination; a Lived Experience & current research Perspective
Amanda Aiyana1*
1Curtin University, Perth Australia, School of Allied Health
It is time to end all forms of stigma and discrimination against people with mental health conditions, for whom there is a double jeopardy: the impact of the primary condition itself and the severe consequences of stigma. Many people describe stigma as ‘worse than the condition itself. Stigma and discrimination in mental health infringe basic human rights and have serious consequences that compound marginalisation and social exclusion. PWLE of mental health conditions are often denied access to life opportunities, such as employment, education, health care, and active participation in the community (Thornicroft et al, 2022)
Australian national mental health policy outlines the need for a nationally coordinated strategy to address stigma and discrimination, particularly towards people with complex mental ‘illness’ that is poorly understood in the community. A recent review of existing Australian stigma and discrimination reduction initiatives and programs identified that bestpractice programs are not widely implemented; programs designed and delivered by people with Lived Experience and ‘carers’/family and significant others involving education/training and Face to face. (Morgan et al., 2021; WHO, 2024)
Language is seen as the starting point of stigma and discrimination reduction. There is a pressing need to transform the language used in talking about mental health issues and psychosocial wellbeing. In fact, how mental health is spoken about has profound implications on public perception, policy formulation, help-seeking behaviour and the quality of support extended to those in need. (UNICEF, 2024)
Amanda is a Lived experience Educator/Researcher (with 2 accepted papers for publishing) with Curtin University and has her own personal experience of hearing voices and altered states. Amanda will deliver research supported Lived Experience understanding of the paradigm shift needed to reduce and eliminate stigma and discrimination of people with the experience of voice hearing and altered states.

Amanda Aiyana is a Lived Experience Educator and Researcher at Curtin University, Western Australia. Amanda has direct experience of hearing voices and altered states, non-suicidal self-injury, mental distress and recovery, as well as over 30 years’ experience of the mental health system.

Tracey Watson1*
1The Institute for Mental and Physical Health and Clinical Translation (IMPACT), Deakin University, Geelong, Australia
Objective:
To reflect on my own lived experience of personal growth post psychosis as inspiration for undertaking a PhD with IMPACT to further understanding of this construct. The aim is to investigate the experience of post traumatic growth in individuals after psychosis and identify interventions which both services and families can adopt to support people on their healing journey.
Conclusion:
Recovery involves not only managing clinical symptoms of the illness but also rebuilding your life in the aftermath of experienced trauma. The concept of post traumatic growth provides a framework to study positive change, to identify how to best support people following trauma and to establish a more hopeful lens for recovery.
Post traumatic growth (PTG) is defined as the “positive psychological changes as a result of the struggle with traumatic or highly challenging life circumstances”. Theoretically, it is not the event itself that produces the change but the effect it has on an individual’s core beliefs about themselves and the world. PTG has been found to occur in five major domains: i) increased appreciation for life, ii) more meaningful relationships, iii) increased sense of personal strength, iv) new possibilities, and v) a richer existential and spiritual life.
Psychosis can be a frightening and overwhelming experience for both an individual and their family. Psychosis is significantly associated with higher rates of trauma, and PTSD than the general population. Additionally, high rates of psychosis-related PTSD, due to the trauma of symptoms and/or hospitalisation, have been reported. Despite these higher rates of trauma, both lived experience testimony and recent research reveals that people can experience positive change following psychosis. Further knowledge about what contributes to fostering positive growth following psychosis will assist in promoting a hopeful outlook that, while psychosis is challenging, it is possible to grow from the experience.
Disclosures:
Tracey Watson is funded by an Australian Government Research Training Program Scholarship
Acknowledgements:
I would like to thank Professor Alison Yung, Dr Carl Moller and Dr James McLure for their support and encouragement as I undertake this research.

Tracey Watson has a Bachelor of Psychology (Honours) from Deakin University and is currently undertaking a PhD with the Institute for Mental and Physical Health and Clinical Translation (IMPACT), focusing on the area of post traumatic growth following psychosis. This topic is inspired by her own lived experience.
LIGHTNING PRESENTATION
Justin McDermott1*
1Alfred Health Victoria
Background:
Recovery from psychosis is shaped not only by clinical interventions but also by power imbalances that influence distress and healing. The Power, Threat, and Meaning Framework (PTMF) offers an alternative to traditional psychiatric models by examining how power dynamics contribute to psychosis experiences. This presentation explores how PTMF aligns with lived experience, particularly in understanding the roles of coercive, interpersonal, and systemic power in recovery.
Method:
This presentation is based on lived experience reflections framed within PTMF’s conceptual model. It will discuss how different types of power shaped my distress and psychosis and how recognising these influences helped shift my perspective during recovery. Each type of power will be examined through personal experiences and the framework’s emphasis on meaning-making and agency.
Results:
Coercive Power and the Impact of Fear
Coercive power—through force, threats, or aggression—played a significant role in my psychotic experiences. Bullying, victimisation, and fear-inducing interactions left me feeling powerless, and my voice often echoed these past threats, reinforcing a sense of danger and helplessness. PTMF helped me see these experiences not as random or meaningless symptoms but as responses to real threats, allowing me to approach my distress with greater self-compassion.
Interpersonal Power and Relational Isolation
Another key factor was interpersonal power—providing or withholding security, love, and validation. Feeling dismissed, neglected, or unseen in my relationships contributed to a deep sense of isolation mirrored in the voices I heard. My distress was not solely internal but relational, shaped by my interactions with others. PTMF reinforced what I had already discovered in recovery: rebuilding relational security was essential. Finding supportive people and spaces helped me heal from these wounds and shift how I experienced psychosis.
Social, Cultural, and Systemic Power
Beyond personal and relational factors, systemic power imbalances—such as stigma, poverty, and discrimination— exacerbated my distress. The way society devalues those of us with psychosis creates additional barriers to recovery, reinforcing feelings of exclusion and limiting access to opportunities. PTMF validated these struggles and emphasised that psychosis cannot be separated from the broader social and cultural contexts in which we live. Understanding these dynamics helped me reclaim a sense of agency in advocating for myself and others.
Conclusions:
This presentation is based on lived experience reflections framed within PTMF’s conceptual model. It will discuss how different types of power shaped my distress and psychosis and how recognising these influences helped shift my perspective during recovery. Each type of power will be examined through personal experiences and the framework’s emphasis on meaning-making and agency.
Disclosures:
No funding was received for this presentation.
Acknowledgements:
We would like to acknowledge consumers who participated in the focus groups that inspired this grant proposal and subsequent project.

Unshared Realities: A co-designed interactive learning experience with discovery college
Joseph Muro, Lucy Mahonyn
discovery college is a space for learning about mental health and well-being in ways that feel safe, inclusive, and meaningful. From courses and panels to podcasts and digital content, we create free and engaging spaces for people to explore mental health in their own way. We are a federally funded recovery college and part of headspace and Alfred Health based out of Melbourne, Australia. We have a youth focus, but we’re for everyone.
“Do You Hear What I Hear?” is a five hour, in-person and online (3hrs) course exploring the ways we think about psychosis including different cultural and societal perspectives. This course was developed in response to desire from community and staff from the headspace Early Psychosis program. Through a process of co-design spanning over two years, we brought together individuals with lived and living experience of psychosis, carers, clinical, educational, and community perspectives to create a thoughtful, and meaningful learning space which challenges how we think about psychosis.
The result is a unique, and innovative learning experience, incorporating lived and living experience stories of psychosis, interactive activities helping understand what the experience of psychosis can look and feel like, and rich and thoughtful discussion that acknowledges the complexity of psychosis. Since this course was developed, it has run seven times in locations throughout Melbourne reaching over 130 total participants.
Feedback has been overwhelmingly positive, with one participant noting, “I loved yesterday’s workshop. It was brave and innovative and turned my thinking inside out and upside down.” Several participants have highlighted the course’s unique exploration of psychosis as an “unshared reality.” This response highlights the course’s ability to challenge assumptions and create meaningful dialogue around psychosis.
In this presentation for the 2025 Australian Psychosis Conference, we will introduce discovery college and share the story of how this course was developed. We will touch on the co-design process while providing an overview of key takeaways from the course. We will also give attendees an interactive experience of an activity from the course and allow space for questions. Our hope is to inspire people to discover and engage in learning while reducing stigma and opening a space for more compassionate conversations around psychosis.

Lucy is a Lived Experience Specialist who co-facilitates and co-produces creative, authentic learning spaces. She co-hosts the Extremely Human podcast and champions storytelling as a path to compassion. She’s passionate about fun, meditation, and discovering new ice cream flavours.

Justin McDermott is a dedicated Senior Peer Support Worker at Alfred Health, bringing lived experience to the forefront of mental health care. Passionate about fostering hope, connection, and recovery, they empower individuals through peer support, group facilitation, and advocacy—bridging the gap between clinical insight and real-life experience.

As Clinical Lead at discovery college, Joey combines his mental health expertise and creative background to develop co-produced, evidence-based learning content. With over 8 years as an Occupational Therapist in youth psychosis and education, he brings a fresh, inclusive approach to his practice.

Sepinood Noroozi1*, Nastaran Doroud2, and Neil Thomas3, 1
1Centre for Mental Health, Swinburne University of Technology, Melbourne, Australia
2Nursing and Allied Health, Swinburne University of Technology, Melbourne, Australia
3The Alfred Hospital, Melbourne, Australia
Background:
Hearing voices occur outside of one’s voluntary control and are often experienced as controlling, powerful, threatening and critical. This study aimed to examine how autonomy is experienced among people who hear voices. Employing a qualitative design, this study sought to examine the lived experiences, personal narratives, and meaning-making processes of voice hearers to gain deeper insights into nuanced ways autonomy is experienced, diminished, attempted, reestablished and constructed by those who hear voices.
Method:
In-depth semi-structured phenomenological interviews with voice hearers were analysed using Interpretative Phenomenological Analysis to capture the ways participants interpret and respond to their experiences.
Results:
Three superordinate themes were identified in the data. First, participants reflected how hearing voices challenged their sense of self, individuality, and the space available for self-authorship. Developing a personally meaningful narrative became crucial for re-establishing autonomy. Second, they portrayed a coexisting dynamic where autonomy and power were shared and negotiated with the voices. Third, participants described how hearing voices interfered with their perceived efficacy, competence, and decision-making, introducing limitations in their ability to navigate life on their own terms. Participants’ capacity for integration, perceptions of their ability to influence and cause change affected the extent to which they felt self-determined.
Conclusions:
The study suggests the importance of supporting voice hearers in constructing self-oriented, meaningful narratives to strengthen their sense of autonomy. Future research may further investigate strategies that empower voice hearers to integrate their experiences constructively, facilitating resilience and autonomy.
Disclosures:
This study was conducted as part of Sepinood Noroozi’s PhD research at Swinburne University of Technology.
Acknowledgements:
We would like to extend our sincere gratitude to the participants who generously shared their experiences and perspectives, without whom this research would not have been possible.

Sepinood is a PhD candidate in Psychology at Swinburne University. Employing multi-method research, she explores how autonomy relates to voice-hearing. She applies Interpretative Phenomenological Analysis to develop lived account of ways voice-hearing and autonomy relate to each other. Her work further investigates these relationships within the framework of Self-Determination Theory.
LIGHTNING PRESENTATION
Cameron Thayer1*, Martin Staines2, Kimberley Lloyd-Jones3
1Karakan Ltd
2Addiction & Mental Health Service | Metro South Health
3Queensland Health
Background:
The STEPS Transitional Recovery and Support Service is a collaborative program developed by Karakan in partnership with Metro South Addictions and Mental Health Services and funded by Queensland Health. The program emerged from a journey of collaboration with key community partners and government stakeholders after identifying the need to address a critical service gap in the Logan region, where Karakan clients and loved ones were missing out on life saving services. This process involved exploring how Karakan and Metro South Addictions and Mental Health Services could work together to provide a holistic, innovative solution to support the mental health recovery goals and housing goals of adults experiencing severe and persistent mental illness who are at risk of homelessness.
The program’s design draws on evaluation research, contemporary recovery principles, and evidence-based practices from successful models across diverse settings. Building on key learnings and positive outcomes from other programs, we developed a place-based approach for the Logan region. A key innovation of the STEPS program is its holistic and integrated approach, where non-clinical and clinical supports are seamlessly delivered under a person-centred, recovery-oriented framework that incorporates lived experience perspectives.
Method:
The STEPS model is underpinned by a four-stage framework – Support and Sustain, Step In, Step Down and Step Forward – which combines focused case management, transitional supported accommodation, and mobile support. Through an integrated model, the program aims to reduce hospitalisations and lengths of hospital stays, improve mental and physical health, stabilise housing, strengthen engagement with support networks, and sustain community participation.
This presentation will feature insights from three speakers representing the key partners involved in the program:
1. Karakan – understanding the need and critical service gaps, developing a local, place-based service model, service model design and implementation, and the integration of holistic and lived experience approaches, with key insights on how to build strong partnerships to support a holistic model.
2. Metro South Addictions and Mental Health Services – highlighting the integration of clinical supports and collaborative service delivery, and perspectives on a partnership approach in new service design and delivery.
3. Queensland Health – sharing the importance of strategic funding in enabling innovative service models to address critical local needs, and Queensland Health’s commitment to evidence-based service design incorporating lived experience.
Results:
The STEPS program demonstrates how partnerships, evaluation research, lived experience perspectives and contemporary service design principles can be leveraged to deliver innovative, localised solutions for individuals with complex mental health needs. By addressing systemic gaps and working to prevent the revolving door of hospitalisation through enhanced community mental health supports, the STEPS program fosters sustainable recovery and enhanced quality of life outcomes.
Conclusions:
This presentation will provide a comprehensive understanding of how holistic, partnership-driven approaches, grounded in community collaboration and lived experience, can transform mental health service delivery, improve outcomes, and generate positive returns on investment for communities and government.




Kimberley has over 20 years of experience in the human services field, working in both government and non-government roles, primarily focusing on mental health and disability services. Kimberley’s expertise spans a broad range of client-centred services, with expertise in client advocacy, strategic program development, and community-based initiatives.
11.30 AM The Patterns of Hearing-Voices Coming and Going: A Reflexive Thematic Analysis – Sharla Cartner 11.50 AM Let’s talk about voices: Supporting mental health workers to support voice hearers – Anne Honey 12.10 PM Integrating virtual reality into psychological therapies for psychosis – Leila Jameel 12.30 PM AMETHYST: The Australia-wide telehealth superiority trial of Avatar vs CBT therapies for people who hear voices – Neil Thomas
Marty is an Occupational Therapist with over 20 years experience of working in mental Health and Learning Disability services in the UK and Australia. He has lived in Queensland since 2009 and has been working for Metro South Mental Health Services since that time. He has a strong occupational focus in his interventions and also uses a strengths based approach.
Cameron has worked in human services for 18 years and through his own lived experience, Cameron has a strong focus and passion for driving and leading social innovations and program development to support marginalised people who fall through the gaps of social systems and service infrastructure. He has led the development of both national and localised service innovations and programs


Sharla Cartner1, Imogen H Bell2,3, Melanie Hawkins4, Neil Thomas1
1Centre for Mental Health, Swinburne University of Technology, Melbourne, Australia
2Orygen ; 3Centre for Youth Mental Health, The University of Melbourne
4Global Health and Equity Unit
Background:
Research indicates that the experience of hearing voices fluctuates with various factors such as negative affect, stress, social interactions, paranoia, sleep patterns, worry, rumination, and daily activities. Experimental studies have found voices are more likely in noisy or very quiet environments and less likely when speaking out loud, engaging in physical activity, or performing cognitively demanding tasks. Ecological momentary assessment studies also suggests that voices are more intense during passive activities and less likely during engaging activities, like creating art or working. However, there is a lack of direct evidence from people who hear voices about the patterns they notice in the coming and going of voices. This study explores these patterns from the perspective of those who experience them.
Method:
Fifteen participants who heard voices at least four times a week for more than six months completed daily diary entries for one week, tracking the patterns of their voices. They used prompts related to activities, location, time of day, social interactions, and their emotions and thoughts when the voices were coming and going. Participants then took part in semi-structured interviews, lasting about an hour, to discuss these patterns. Reflective thematic analysis, guided by critical realism, was used, applying inductive, deductive, abductive, and retroductive coding to extract meaningful insights. The deductive coding applied a hypothesis from previous research suggesting that greater engagement in activities results in quieter voices compared to unengaging activities.
Results:
Participants, primarily diagnosed with schizophrenia, had been hearing voices for 8 to 54 years. Four themes were established. The first, externally immersed, aligned with previous research, where voices were minimal or absent during engaging activities that also provided benefits like positive affect, self-efficacy, or a sense of purpose. The second, internally entrenched, described the voices coming, as attention shifted inward toward thoughts, emotions, fears, and reactions to stress or unpredictability. Two pathways were identified from here. The first, switch attention focus to external, involved being deeply engaged in activities, using learned therapeutic skills, or changing environments, which led to the voices going. The second pathway, voices have captured attention, described immersion in the voices. This theme varied in severity, with some participants becoming overwhelmed by the voices and reacting emotionally as the voices persisted.
Conclusion:
The findings of this study suggest that engaging in personally immersive activities may facilitate a reduced focus on voice hearing experiences, reducing their severity and distress. This suggests that interventions to support engagement in these activities may be beneficial, particularly with individualised activity plans developed in collaboration with the client to account for variation between people in what may be more engaging.

Sharla Cartner is a PhD student at Swinburne University of Technology investigating attentional processes and activity engagement in auditory verbal hallucinations. Her research seeks to advance understanding of attentional processes underlying hallucinations, with a focus on self-management in mental health.
Let’s talk about voices: Supporting mental health workers to support voice hearers
Nicola Hancock1
1The University of Sydney, Sydney, Australia
2Northern Sydney Local Health District, Sydney, Australia
Background:
Voice-hearing is an experience that affects many people and can be a distressing and debilitating. However, the ways people approach, engage with and cope with voices are a critical determinant of distress and functioning and evidence suggests that understanding one’s voices can facilitate recovery. Yet many mental health workers lack knowledge of and confidence with using evidence-based, non-medical approaches to working with voice hearers. Let’s Talk About Voices was co-designed by clinicians and voice-hearers. It is a freely accessible website that provides mental health workers with resources they can use to start optimistic conversations about voice-hearing (https://www.nslhd.health. nsw.gov.au/hearingvoices). The aim of this study was to evaluate the impact of Let’s Talk About Voices on mental health workers’ capacity to support voice hearers.
Method:
We used a randomised controlled crossover trial design to assess the impact of engaging with Let’s Talk About Voices on the beliefs, attitudes and confidence of mental health workers about working with voice hearers. We also gathered data on participants’ subjective perspectives of the usefulness of the resources. A total of 256 mental health workers commenced the study, with 120 completing assessments at all three timepoints.
Results:
The findings demonstrate the effectiveness of Let’s Talk About Voices, with participants showing significant improvements after the intervention, which were sustained at follow-up. The difference between intervention and control conditions was significant with a large effect size (F=40.2, p<.001, ηp2=0.19), and significance remained on intention-to-treat analysis with a medium effect size. Participants reported finding the resources useful for their practice.
Conclusions:
Let’s Talk About Voices provides mental health workers who work with voice hearers with useful information and resources to help them support voice hearers in an evidence based, non-medical way.
Disclosures:
This research was funded through the Moyira Elizabeth Vine Fund for Research into Schizophrenia, administered by The University of Sydney.
Acknowledgements:
The authors would like to thank the stakeholder group of clinicians, peer workers and voice-hearers for their contributions to this study.

Anne Honey is an occupational therapist and Associate Professor at the University of Sydney. She has been involved with a wide variety of mental health research including service evaluations; parenting; and recovery-oriented practice, with an emphasis on consumer-led and collaborative research.

Leila Jameel a,b,c*, Mar Rus-Calafell b,d, Matteo Cella a,b, Jonathan Bradley e, Lucia Valmaggia b,f,g
a South London and Maudsley NHS Foundation Trust, London, United Kingdom, b King’s College London, Department of Psychology, Institute of Psychiatry, Psychology & Neuroscience, London, United Kingdom, c Centre for Mental Health, Swinburne University of Technology, Australia, d Mental Health Research and Treatment Centre, Faculty of Psychology, RuhrUniversitat Bochum, Bochum, Germany, e South West London and St George’s Mental Health NHS Trust, United Kingdom, f KU Leuven, Department of Psychiatry, Leuven, Belgium, g Orygen, Centre for Youth Mental Health, The University of Melbourne, Australia
Background:
Virtual reality (VR) presents a unique opportunity to enhance psychological therapies by bringing real-world experiences to life in the clinic. VR can be used to recreate (e.g. voice hearing) or represent challenging aspects of people’s experiences and daily life (e.g. using public transport). VR environments can offer a safe space to experiment with new ways of coping with, responding to and overcoming daily challenges. It can serve as a stepping stone to the ‘real world’. This talk will focus on an exemplar study from the UK led by the author: a case-series of virtual-reality assisted cognitive behavioural therapy (VR-CBTp) for people with first episode psychosis (FEP) experiencing social difficulties. It will then broaden out to consider other applications of VR to enhancing psychological therapies for people with psychosis. The talk will be supplemented by video examples of VR technology in action.
Methods:
People with psychosis often experience social difficulties associated with psychological processes, such as fear of harm or negative evaluation from others. The case series presented aimed to evaluate the feasibility and acceptability a novel VR-CBTp in real-world clinical settings. Eight eligible participants were recruited and received a course of 10 sessions of individual formulation-driven VR-CBTp with a focus on improving social functioning. A novel VR environment and therapy package were piloted for the use of the assessment, formulation and treatment of social difficulties. Psychometric assessments were conducted pre- and post-therapy, and participants provided qualitative feedback about their experiences.
Results:
The results provided preliminary information to suggest that the therapy was feasible and acceptable, recruiting to target and with good participant retention. Pre-post comparison of treatment outcomes revealed a reliable change on some of the assessed domains, indicating participants experienced clinical benefits from the therapy.
Conclusions:
The inclusion of VR into a course of CBTp for people with psychosis who experience social difficulties was found to be feasible and acceptable with potential therapeutic benefits. This is in line with the broader literature in this area, suggesting that VR can enhance psychological therapies for people with psychosis. The talk will end by reflecting on several other streams ongoing VR research in Australia, including the AMETHYST trial on Avatar therapy for people who hear voices.
Disclosures:
No funding was received for this work.
Acknowledgments:
We would like to acknowledge all the consumers and clinicians who have supported the studies mentioned in this talk.

Dr Leila Jameel is a Trial Co-ordinator and Research Therapist on the AMETHYST trial, investigating psychological therapies for people who hear voices. She is a member of the Swinburne University Voices Clinic team. Leila holds a research PhD in Clinical Neuropsychology and trained as a Clinical Psychologist in the UK.
AMETHYST: The Australia-wide telehealth superiority trial of Avatar vs CBT therapies for people who hear voices
Neil Thomasa, Rachel Brandb, Leila Jameela,c*, Imogen Belld, David Castlee, Louise Glenthøjf, Eleanor Londgeng, Denny Meyera, Cathrine Mihalopoulosh, Georgie Paulik , Susan Rossella, Andrew Thompsond and Greg Wadleya
aCentre for Mental Health, Swinburne University of Technology, Australia
b School of Health and Behavioural Sciences, University of the Sunshine Coast, Australia
c South London and Maudsley NHS Foundation Trust, London, United Kingdom
dOrygen Youth Health, Australia
eTasmania Centre for Mental Health Service Innovation, Australia
fCopenhagen Research Centre for Mental Health, Denmark
g University of Manchester, United Kingdom
hMONASH University, Australia
Perth Voices Clinic, Australia
Background:
Psychological therapies can support people to cope with and make sense of distressing experiences of hearing voices. Current best practice psychological therapy for hearing voices (CBT) can help experiences of hearing voices to be less distressing and have a less negative impact on daily life. However, therapy effectiveness could yet be improved, and specialist therapies may be hard to access in Australia. The AMETHYST trial seeks to bridge these gaps by harnessing digital technology to improve the access to and effectiveness of specialist psychological therapies. First, by using telehealth to increase reach of delivery. Second, by creating a digital avatar to simulate voice-like experiences within a therapy session, which can be used by the therapist and client to practice different ways of responding and relating to voices.
Methods:
AMETHYST is an Australian Government-funded randomised controlled trial examining whether technology can improve the outcome of psychological therapy for hearing voices. 212 participants from across Australia will receive sessions delivered by videoconferencing from a specialist telehealth-based voices clinic. Participants will receive either standard best-practice therapy (CBT), or a new therapy using a digital avatar and voice modulation software to support therapy (Avatar). The main outcome is to compare the day-to-day impact of hearing voices on a battery of measures following either therapy. Qualitative interviews will also seek to better understand patient and therapist experiences of receiving and delivering these therapies.
Results:
The trial is recruiting until March 2026, and the main outcomes will be disseminated in 2027. In this talk we will present an update on recruitment and retention. We will also draw on our trial experience to date, to discuss feasibility and acceptability and will share insights into the experiences of delivering both therapies using technology.
Conclusions:
This trial will help to add to a body of emerging work on Avatar therapy. It is the first study in the world to compare the effectiveness of Avatar therapy to standard best-practice therapy (CBT) and to deliver all therapy via telehealth. Our trial will provide important information on how it compares with current best practice therapy: Is it more effective? What are people's experiences of avatar therapy relative to usual therapy? What characteristics inform who will benefit more from which treatment? How to choose which therapy to use in practice? It will also provide data on tolerability of this novel therapy, the health economics, costs of delivery and telehealth considerations.
Disclosures:
The AMETHYST trial is funded by the Australian Government National Health and Medical Research Council.



Dr Rachel Brand is a Senior Lecturer in Clinical Psychology at the University of the Sunshine Coast. Rachel is a chief investigator and therapy lead on the AMETHYST trial. Rachel’s research focuses on developing psychological interventions for people experiencing psychosis, and improving access to these.
11.30 AM Embedding tobacco treatment in psychiatry settings using a system change intervention. – Sally Plever
11.50 AM The association of evoked gamma power and clinical outcome in first episode psychosis – Stephen Wood
12.10 PM The Australian Early Psychosis Collaborative Consortium (AEPCC) – building and implementing Australia’s first mental health clinical quality registry – Andrew Thompson
12.30 PM My Early Psychosis journey – Djidda Manning, Amit Banerjee
Dr Leila Jameel is a Trial Co-ordinator and Research Therapist on the AMETHYST trial, investigating psychological therapies for people who hear voices. She is a member of the Swinburne University Voices Clinic team. Leila holds a research PhD in Clinical Neuropsychology and trained as a Clinical Psychologist in the UK.


Embedding tobacco treatment in psychiatry settings using a system change intervention.
S Plever1,2,3, S Kisely4,5, B Bonevski3,6, I McCarthy1, E Ballard7, M Anzolin1, B Emmerson1, D Siskind4,5, J Allan8, C Gartner2,3
1The Queensland Mental Health Clinical Collaborative, Metro North Hospital and Health Service, Brisbane, Australia, 2The University of Queensland, School of Public Health, Brisbane, Australia, 3NHMRC Centre of Research Excellence on Achieving the Tobacco Endgame (Tobacco Endgame CRE), The University of Queensland, Brisbane, Australia, 4The University of Queensland, School of Clinical Medicine, Brisbane, Australia, 5Metro South Addiction and Mental Health Service, Metro South Hospital and Health Service, Brisbane, Australia, 6Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University, Adelaide, Australia, 7 QIMR Berghofer Medical Research Institute, Brisbane, Australia, 8Mental Health Alcohol and Other Drugs Branch, Clinical Excellence Queensland Health, Brisbane, Australia
Background:
Tobacco-related disease is a leading cause of premature mortality for people experiencing mental illness (Dickerson et al., 2018). Tobacco treatment is not routinely provided in psychiatric settings with systemic barriers preventing access to treatment. To overcome these barriers, a system change intervention was used in publicly funded adult psychiatric and alcohol and other drug (AOD) services across Queensland. The aim of this study was to evaluate the effectiveness and sustainability of this approach for, at-scale, implementation of routine smoking care in public adult acute inpatient, community mental health and AOD services.
Method:
Secondary analyses of two independent statewide mental health administrative datasets was conducted for adult inpatients (Oct 2015 to Dec 2020) and community mental health consumers (July 2017 to June 2023). Changes in documentation of smoking status and delivery of a brief Smoking Cessation Clinical Pathway (Pathway) were evaluated using interrupted time series analysis. Preliminary trends in implementation across AOD services are also reported.
Results:
Smoking in mental health inpatient (56%), community (53%) and AOD (>70%) settings was high. Statewide documentation of smoking status increased in inpatient and community settings. sustaining high reporting rates (>90%) despite small significant declines following implementation (inpatient -1.3% [95% CI -1.7, -0.9]; community -2.1% [95% CI -3.4, 0.8]). Pathway documentation also showed sustained significant increases post-implementation. Preliminary trends in AOD services suggest increases in documentation.
Conclusions:
Smoking rates across psychiatry and AOD settings are high. This research is the first, that we are aware, to demonstrate potential for a system change intervention to sustainably embed tobacco treatment, at scale, in diverse psychiatry settings. Preliminary results also suggest potential for this approach in AOD services. The delivery of routine tobacco treatment in psychiatry and AOD settings is vital for addressing treatment inequity in this population and has the potential to impact disproportionately high mortality rates.
Disclosures:
No funding was received for this research. The authors declare no conflicts of interest.
Acknowledgements:
We would like to acknowledge the Queensland public mental health services and staff whose work in smoking cessation provided the information for this research.

Sally is a Psychologist (MClinPsych) who has worked in mental health services for 20+ years. She is co-manager of the Queensland Mental Health Clinical Collaborative and is undertaking a PhD in smoking cessation and mental illness at the University of Queensland.
ORAL PRESENTATION
The association of evoked gamma power and clinical outcome in first episode psychosis
Stephen J Wood1,2,3*, Magdelene de Rozario1,2, James Reeves1,2, Andrew Thompson1,2, Elise Rowe4, Tahnee Bridson1,2, Marta Garrido4, Moritz Haaf5, Julia Adams1,2, Christos Pantelis6, Gregor Leicht5
1Orygen, Parkville, Australia
2Centre for Youth Mental Health, University of Melbourne, Parkville, Australia
3School of Psychology, University of Birmingham, Edgbaston, UK
4Melbourne School of Psychological Sciences, University of Melbourne, Parkville, Australia
5University of Hamburg, Hamburg, Germany
6Department of Psychiatry, University of Melbourne, Parkville, Australia
Background:
Traditional dopaminergic antipsychotics fail for 30-40% of people with psychotic illness. This treatment-resistance is hypothesised to be due to glutamatergic dysfunction, which results in excitation/inhibition (E/I) imbalances. Evidence from electroencephalographic (EEG) measures relating to E/I imbalance in patients with schizophrenia, specifically, gamma power (30-90 Hz) evoked during different cognitive tasks, have been varied across the literature. Thus, we aimed to determine how gamma power at-task differs in those with a first episode of psychosis (FEP) compared to healthy controls (HC) and whether these are related to the severity of psychotic symptoms and psychosocial functioning.
Method:
We recorded EEG data from people experiencing FEP (N=23) and HC (N=21) during an ‘easy’ and ‘hard’ auditory task. We examined mean evoked gamma power (split into total: 30-90 Hz, low: 30-45 Hz and high: 55-90 Hz) at central locations (Cz), and correlated it with symptom severity and psychosocial functioning.
Results:
We found no significant differences at the group-level comparing: (1) the easy and difficult evoked gamma power for FEP individuals or (2) the FEP and HC groups between the tasks, however, there were a number of significant correlations. Specifically, in the easy auditory evoked task, higher evoked total and high gamma power at baseline was correlated with worse total, negative and positive psychotic symptoms at follow-up. Furthermore, higher evoked high gamma power at baseline was correlated with poorer functioning at follow-up.
Conclusions:
Overall, our results suggest that elevated gamma power during easy cognitive tasks may predictor worse long-term symptom and functioning outcomes.
Disclosures:
Funding was received from NHMRC (Grant ID: APP2003392) and the Brain & Behavior Research Foundation.

Professor Stephen Wood is Deputy Chief of Research and also leads the Clinical Neuroscience research area at Orygen. He holds honorary positions at the School of Psychological Sciences, University of Melbourne and the School of Psychology, University of Birmingham (UK).

The Australian Early Psychosis Collaborative Consortium (AEPCC) – building and implementing Australia’s first mental health clinical quality registry
Andrew Thompson1,2, Jo Fitzsimons1,2, Yehudi Saling1, Carolyn Sanderson1
1Orygen, Parkville, Australia
2University of Melbourne
Background:
Over the last few decades research into early psychosis has increased dramatically. Early Intervention services have been established in an increasing number of countries internationally including clinical services for those at high risk of developing a psychotic disorder. However, the quality of service delivery is often not adequately monitored, data collection not systematized and the understanding of long term outcomes outside of research settings is lacking. Clinical Quality Registries (CQR’s) are tools for monitoring the quality of care delivered to a specific diagnostic group or procedure. They are widespread in Australian healthcare outside of mental health. They involve the collection of minimum clinical and service data on a wide number of individuals in real-world clinical settings with opportunities for wider linkage to other routinely collected health care data such as mortality and prescribing. In this sense they fulfill the criteria of a learning health care tool. As part of the recently established Australian Early Psychosis Collaborative Consortium initiative we are establishing a CQR for early and emerging psychosis (FEP and UHR) Australia wide.
Methods:
We describe the process of designing and establishing the minimum dataset (MDS) and the CQR infrastructure. A series of panel discussions with an establishment committee of clinicians, research and lived experience experts has guided the development of the MDS and implementation of the CQR in diverse services across the country.
Results:
The current state of the national CQR infrastructure and the challenges in implementing this in the 5 demonstrator sites (New South Wales, Northern Territory, South Australia, Victoria) will be discussed.
Discussion:
The establishment of a national CQR for early psychosis is the first of its kind for mental health in Australia. The CQR will lead to an improved collection of minimum data on outcomes, establish and improve risk profiling in practice, allow services benchmarking and improve quality and also understand long term outcomes in early psychosis.
Disclosures:
Funding was received from the Wellcome Trust

Professor Andrew Thompson is a Professor of Youth Mental Health at Orygen and the Centre for Youth Mental Health, University of Melbourne. Andy leads AEPCC and the early psychosis clinical service at Orygen Specialist Program. Andy’s research interests include risk factors for development of psychosis, predictors of outcome and novel approaches to treatments.
Djidda Manning1, Amit Banerjee2*
1Student, Kiara College, WA
2Consultant Psychiatrist, headspace Early Psychosis, Midland WA 6056
Introduction:
Galang Nguruindhau. My name is Djidda Manning, and I am a 14-year-old boy from Perth Western Australia and today I want to talk about some of the difficulties faced in my year long journey with psychosis so far.
Summary:
Through this first-person account, I would like to highlight the long hours I have spent in the Emergency Department of the Children’s Hospital on several occasions. My mother and I had to wait, away from the family and my young sisters, not knowing whether we were going to get the help I needed. There was uncertainty about what I was experiencing, the most the doctors knew was that it could have potentially a case of bipolar or schizophrenia, and some were doubtful if it was even psychosis at all, which was very confusing and upsetting.
During the multiple long stays in hospital, I was tried on a seemingly endless cocktail of medications, having to give each one a trial for several weeks. The differing opinions on what I am experiencing and what could be the best path of action, both from professionals and from those who am close to, caused me to be very confused. The worrying and bizarre nature of some of my thoughts caused my family to be frightened, concerned and bewildered. It caused temporary but dramatic rifts between them and affected all.
Symptoms:
I have experienced very unusual symptoms even recently, which my doctors say could be early symptoms of schizophrenia. I will provide a longitudinal account of my psychosis journey through this presentation.
Discussion:
My current psychiatrist who is co-presenting with me, encouraged me to write this first-person account. Despite the severe and concerning nature of my current symptoms, I am articulate and was able to write the first draft of this abstract. I have completed my tests and am going to start a trial of Clozapine very soon.
I hope that I have a good response on Clozapine and that the medication won’t have to be stopped due to sideeffects. My psychiatrist has explained to me that Clozapine is the only medication that clearly is superior to all other medications used to treat schizophrenia.
I might be much better in my mental state in the coming months having responded to the Clozapine and I might not have any symptoms when the Conference comes along in late July 2025. I hope I will handle the stress of talking about my deep, unpleasant personal experiences, which by then will be a thing of the past, in front of an audience without too many problems.
Conclusions:
Experiencing symptoms of psychosis for the first time can be very distressing and scary. It is important for doctors and mental health staff to be calm and reassuring, explain the options of treatment for psychosis in simple language. I wish Emergency Departments of hospitals were better able to look after the needs of mental health patients like me.
Disclosures:
Nil
Acknowledgements:
Nil



Djidda is a 14-year-old aboriginal Noongar boy and student attending Kiara college in Perth, WA. He lives between his grandparents' house and parents' house and spends most of his free time with his family, reading, listening to music, going for walks and learning.
11.30 AM A lived experience transformation of psychosis to mental health: Inspiring a movement of hope – James McLure
11.50 AM Mental Health Consumers and Participation in Occupational Therapy Education (MHCAPOTE); Improving student readiness to support people healing from psychosis via coproduction – Julia Bocking
12.10 PM Expectations VS Reality: The lived experiences of Australians seeking support for psychosocial disability under the NDIS – Joel Hollier, Jen Smith-Merry
12.30 PM Making Sense of Psychosis Through Open Dialogue: A Personal Journey of Transformation – Deborah Warner
Amit is a recovery-oriented psychiatrist with primary interests in social and critical psychiatry, cross-cultural psychiatry and addictions. With his sub-continental background and his interest in sociology and mental illness, he believes he might have some unique insights about psychosis, not very recognisable by the mainstream.


James McLure
Deakin University, Geelong, Australia
Objective:
To reflect on my own lived experience to affirm the importance of hope in fuelling personal growth after an experience of psychosis. My personal testimony describes the experience of psychosis ultimately as a blessing as it precludes an humbling an exquisite transformation and healing process. Secondly, to review one of the ways hope spreads through mental health systems, identifying peer support as the example.
Conclusions:
A narrative of lived experience testimony of psychosis and subsequent transformation can inspire hope and sustained growth in individuals and communities. One of the most important drivers of profound healing comes in the form of hope. Currently, peer support workers employed in mental health systems embrace companionship with the people accessing services while simultaneously growing to sounder mental health together through hopeful, healing relationships.
Keywords:
transformation, hope, lived experience, personal testimony, mental health systems
In the World Mental Health Report: Transforming Mental health for all, the World Health Organization encourages nations to invest in mental health. Over 980 million people were reported to experience a diagnosable mental disorder globally. This statistic highlights an urgent need for investment into, and propagation of hope toward, global mental health. Reflecting on my own lived experience, psychosis was the catalyst which ultimately led to a hope-filled lifechanging experience, a sustained new cycle of personal growth and transformation into a truer and improved version of myself. Such experiences are also reported in the literature.
While offering peer support in an acute mental health facility I have learnt that individuals accessing acute mental healthcare often experience deep personal challenge while simultaneously finding themselves primed for personal change. Mental health systems need not miss the opportunity to support transformation in the individuals they support. Transformation can be facilitated, for a start, by expressing genuine empathy and compassion for an individual’s or community’s struggles, holding hope for, and retaining the dignity of, people impacted by mental illness, using person-centred growth-oriented language and care, and essentially by loving people back to health. One of the most recent revolutionary service delivery offerings in public mental health services, is that of peer support. This movement is spreading rapidly around the world, for it is companionship, empathy, shared growth toward mental health, lived experience leadership, and living hope for people traversing incredibly challenging transformations. The origins of peer support in mental health services date back over two hundred and thirty years. A French physician, Philippe Pinel, identified that ex-patients of the mental health system were gentle, humane and disposed to kindness and were highly effective in playing a part in the healing of mentally unwell individuals. Profoundly, these attributes hold true for peer workers today who courageously meet and connect with people who’ve extreme mental health challenges, where they are at. Peer workers see and relate to the person, not the illness.
Acknowledgements:
I’d sincerely like to thank Dr Tari Forrester-Bowling, Stephanie L Bennetts, Dr James J Lucas, Associate Professor Debbie Scott, Professor Anna Peeters, Professor Steve Moylan, Renae Carolin, Dr Amelia McGuinness, and Professor Michael Berk for the fruitful work we’ve shared, your belief in me, and for the most excellent support each of you have extended.

Dr James McLure, Research Fellow, IMPACT, Deakin University. James leads a team of peer workers at Barwon Health, Geelong, and reconnected to a passion in research to play a greater part in the healing of others, in 2021. He leads culture change and creates communities of lived experience in research.

Mental Health Consumers and Participation in Occupational Therapy Education (MH-CAPOTE); Improving student readiness to support people healing from psychosis via coproduction
Julia Bocking1, Professor Douglas Boer, Dr Claire Pearce, Dr Kate Holland, Associate Professor Aine O’Donovan, Professor Holly Northam3
1University of Canberra, Canberra, Australia
2University College Cork, Cork, Ireland
3University of Western Sydney, Sydney, Australia
Background:
Clinical curricula has not kept pace with changes to Australian mental health policy and consumer needs. New graduates can be ill-equipped to offer recovery-orientated support. Furthermore, like the rest of the population, clinical students often hold negative attitudes about a mental health career. Stigma is a major issue. Involving consumers in mental health teaching has shown to promote more positive attitudes and ability to practice according to policy. There is substantial support for coproduced curricula in the nursing literature. Consumer involvement is relatively new in Occupational Therapy teaching. MH-CAPOTE was an innovative teaching intervention to reduce stigma and enhance Occupational Therapy student clinical readiness. A key feature was new unit content which was coproduced and cotaught by a consumer educator.
Method:
The teaching intervention took place at the University of Canberra. MH-CAPOTE had a mixed method design. First, unit content and support systems were established (for students, the consumer educator and academic staff). Next, Occupational Therapy students enrolled in ‘Mental Health Practice’ were invited to participate. A pre and post-test of student attitudes towards consumers was collected. Students were also invited to take part in a focus group to share their experiences (n = 41). Occupational Therapy academics also shared their perspectives separately (n=7). Three data sets were produced: pre/post student data, student focus groups, staff interviews. A student resource was also created via coproduction and distributed for enhanced support. A key contribution was a conceptual teaching framework created by the consumer educator to guide her narrative selection with students.
Results:
Overall, the findings were very encouraging. The pre/post test showed a statistically significant drop in student stigma. Students reported finding the unit engaging. The narratives shared by the consumer educator assisted their selfreflection. Occupational Therapy staff retained much of the new unit content after the intervention was complete. The coproduced student resource was also continued. An unexpected finding was the huge demand for mental health clinical placements after the unit.
Conclusions:
Coproduction of university curricula is worthy of further exploration. The findings suggests that it improves student skills and attitudes; meaning they are better equipped to provide recovery-orientated support. The findings of MHCAPOTE also indicate that coproduced university teaching may improve service quality faster than policy reform (and other strategies). Students were more motivated to pursue a career in mental health and felt more confident in their practice. The consumer educator found the conceptual framework provided helpful guidance for her role.
Disclosures:
This research was supported by the Australian Government Research Training Program. MH-CAPOTE forms part of a larger body of work on coproduced mental health curricula (Modus Liberi) led by the consumer educator for her doctoral research.
Acknowledgements:
We would like to acknowledge the Occupational Therapy students and staff at the University of Canberra who generously gave their time and perspectives for this research.

Julia Bocking is a mental health activist. She has used her lived experience to advocate for consumers for over 20 years. She is currently a PhD candidate at the University of Canberra. Julia’s research aims to advance co-produced university curricula to improve service quality for people healing from psychosis.

Joel Hollier, Jen Smith-Merry
The University of Sydney
Background:
Currently over 62 000 people receive support from the NDIS for severe and persistent mental illness (referred to as “psychosocial disabilities”), with a significant portion of these experiencing long-term psychosis. Despite an investment of approximately 4.25 billion dollars/year. outcomes for participants continue to lag behind other groups.
Concurrently, Australia’s mental health systems remain fractured, siloed, and ill-equipped the handle complexity. As reforms are considered, and governments prepare to negotiate the scope and shape of “foundational supports” it is vital that the voices of those poised to receive said support are amplified. To date, scant research has sought to explicitly investigate what expectations NDIS participants with psychosocial disabilities have of the scheme, and how these expectations are being met/not being met. As part of a broader research body, this project aimed to do just that.
Method:
Semi-structured interviews were carried out with NDIS participants with psychosocial disability (n=20) and carers/ informal supports (n=9). Interviews were transcribed and data was analysed following Clarke and Braun’s thematic analysis. The protocol for this research was reviewed by an advisory group containing people with lived experience of psychosocial disabilities, and the project received ethics approval from the University of Sydney’s Human Research Ethics Committee.
Results:
For some there remain sharp discrepancies between participants’ expectations prior to joining the scheme, and their experiences once on the NDIS. This was reflected in participants’ 1) frustrations with how their plans were developed, 2) ongoing lack of choice and control regarding their plan expenditure, 3) lack of clarity regarding appropriate support, and 4) ongoing experiences with unscrupulous and/or inept providers.
Concurrently, some participants entered the scheme with little-to-no expectations, reflecting a lack of awareness about what the NDIS could potentially offer. This was caused by 1) a lack of accessible information to help them navigate the planning process, 2) confusion regarding what supports are NDIS funded, and what are supposed to be covered by other systems, and 3) the reality of being unwell at the time of application and thereby lacking motivation or awareness.
For most participants, the NDIS has brought a net positive good, while for a small number, their experience has left them worse off on their recovery journey.
Conclusions:
The vital reforms that are being considered must continue to take into account the lived realities of people with psychosocial disability. Clear, accessible, and timely information during application and planning phases is required. Further, any reforms should factor in the episode and fluctuating nature of severe and persistent mental illness, while upholding an incontrovertible emphasis on choice and control.
Disclosures:
The author has no disclosures to report.
Acknowledgements:
This project is a team effort, alongside Jade Change, Ivy Yen, Firew Bobo, and a range of advisors and participants who are living out their commitment to a better country for those experiencing severe and persistent mental illness.

Jen is Australian Research Council (ARC) Laureate Fellow and Professor Health and Social Policy in the Sydney School of Health Sciences (the University of Sydney). Her work focuses on creating practical, research-informed policy and practice development in partnership with government and non-government organisations.

Joel is a postdoctoral research fellow at the University of Sydney’s Centre for Disability Research and Policy. His current research explores Australia’s mental health policy landscape, with an ongoing emphasis on person-centred, holistic framing of severe and persistent mental illness.

Deborah Warner
Alfred Health's Early Psychosis
Background:
Traditional approaches to psychosis often focus on symptom reduction and medication, potentially overlooking meaningful experiences and narratives. As a family peer specialist currently working in an Early Psychosis team that uses Open Dialogue and network meetings, I bring both professional and personal insights to this approach. This presentation will explore the seven core principles of Open Dialogue and how they transform our understanding and response to psychosis.
Method:
Drawing from my dual roles as a family peer specialist and as a mother, I will share my son's journey through three different mental health teams, including his transformative experience with an Early Psychosis service. I will outline how Open Dialogue's seven principles - immediate response, social network perspective, flexibility, responsibility, psychological continuity, tolerance of uncertainty, and dialogism - create a framework for meaningful engagement. Through these experiences, I will demonstrate how network meetings create opportunities for shared understanding and healing.
Results:
The contrast between approaches was stark. The first team's traditional approach left us feeling isolated and fearful, with limited understanding of my son's experiences. In contrast, the Open Dialogue approach used by the Early Psychosis team was transformative for our entire family. Network meetings enabled my son to articulate his experiences without fear of judgment, while helping our family develop a deeper understanding of psychotic experiences as meaningful responses to life events rather than just symptoms to eliminate.
Conclusions:
Our family's journey demonstrates how Open Dialogue's approach to psychosis as a meaningful experience worthy of exploration represents a powerful alternative to traditional treatment models. This reframing helps reduce stigma, build stronger family connections, and create more effective pathways to recovery through shared understanding rather than symptom suppression alone.
Disclosures:
No conflicts of interest to declare.
Acknowledgements:
Special acknowledgment to the Early Psychosis team whose Open Dialogue approach transformed our family's journey

Deborah Warner is a Senior Family Peer Worker with Alfred Health's Early Psychosis program and an Open Dialogue Peer Facilitator/Trainer, bringing eight years of handson experience supporting families. As co-director of APOD Family Support and a passionate advocate for accessible mental health and AOD services, she combines lived experience with professional expertise to promote transformative care.
No mental health without oral health: why is it important and what can we do to close the gap?
– Amanda Wheeler, Steve Kisely, Bonnie Clough & Caroline Robertson
Managing Cardiometabolic Health in People Taking Psychotropic Medications: Implementing solutions
– Andrew Watkins, Hamish Fibbins & Rachel Morell
Implementing Recovery Principles in the management of schizophrenia –Examining Theory and Practice through Case studies
– Amit Banerjee, Begonya Grasa-Ward, David Ward

No mental health without oral health: why is it important and what can we do to close the gap?
SR Kisely1,2, AJ Wheeler3,4, C Bull1, C Robertson3, B Clough3
Session Chairs: SR Kisely1,2, AJ Wheeler3,4
1School of Medicine, The University of Queensland, Princess Alexandra Hospital, Ipswich Road, Woolloongabba, Brisbane, Australia.
2Departments of Psychiatry, Community Health and Epidemiology, Dalhousie University, Halifax, Canada
3Centre for Mental Health, Griffith University, Brisbane, Queensland, Australia
4Faculty of Medical and Health Sciences, Auckland University, Auckland, New Zealand
5Monash University Health Economics Group (MUHEG), School of Public Health & Preventive Medicine, Faculty of Medicine, Nursing and Health Sciences, Monash University, Australia
6Deakin Health Economics, Institute for Health Transformation, School of Health and Social Development, Deakin University, Australia
Background:
There has been little focus on the impact of mental ill-health (MIH) on oral health, despite oral health being an important aspect of overall well-being that is linked to many other chronic conditions incl. diabetes, cardiovascular disease, and cancer. This is partly attributable to common risk factors incl. tobacco/alcohol but also because poor oral health leads to intermittent bacteraemia and secondary immune complexes resulting in inflammatory responses in arteries and distal organs. The most common dental diseases are erosion, caries (tooth decay), and periodontal (gum) diseases. People with MIH are at greater risk due to difficulties with self-care or access to dental care, lifestyle, or as a side effect of psychotropic medications (mainly dry mouth). Given the bidirectional relationship between oral health and mental health, neglecting dental disease may compromise recovery from MIH.
Method:
This symposium presents: (i) research on physical impacts of oral health inequalities in people with MIH; (ii) multilevel enablers & barriers to dental care in this population; (iii) advice on improving oral health in this population.
1. What is the epidemiology of dental disorders among people with MIH?
2. Avoidable emergency department presentations for dental comorbidities of psychiatric disorders: Queenslandwide record-linkage analysis;
3. Overcoming oral health obstacles for youth with MIH;
4. Healthy smiles: an investigation of brief online interventions to improve oral health among young people experiencing psychological distress.
Results:
1. The strongest association is between dental decay and severe MIH or substance use, and erosion and eating disorders. People with severe MIH have nearly three times the odds of losing all their teeth than the general community (OR=2.81, 95%CI=1.73-4.57). Findings for periodontal disease are more equivocal, but still strongest for schizophrenia.
2. There were 1,381,428 individuals in the linked database; 13% had a history of contact for MIH and 1.5% at least one avoidable dental presentation. Psychiatric patients were 72% more likely to experience an avoidable dental presentation (95%= 1.65-1.79; p<0.0001). Within inpatients, those with substance use or personality disorders had highest risk of avoidable presentations. Most common dental presentations were toothache (n=9619), dental abscesses (n=8449), caries (n=1826), stomatitis (n=1213) and gum disease (n=939).
3. Key promoters of good oral hygiene included: delivery of appropriate educational resources around attending dental appointments and undertaking preventative oral self-care; support from mental health staff in providing
supportive strategies to enable access to oral healthcare services; and the building of trusted relationships for those involved in both oral and mental healthcare.
4. Participants in the education intervention reported significantly greater oral health knowledge at post-intervention than pre-intervention, with gains maintained at follow-up. Some benefits also observed for attitudes and oral health values post-intervention, across conditions. The addition of motivational interviewing components did not result in improved intervention effects.
Conclusions:
Evidence-based mental health policy research and analysis is essential to improve oral health in people with MIH. Mental health practitioners should screen for oral diseases when treating those with MIH and facilitate referral to affordable treatment when indicated. Prevention should be a priority, including promotion of oral healthcare.

Amanda Wheeler, Professor of Mental Health, and Deputy Head of School (Research) at Griffith University (GU) and a registered pharmacist (BSc [Biochem] 1984-1986; BPharm 1987-1989; DipPsychiatrPharm 1996-1998; CertPubHealth [Effective Practice] 1999-2002). I have worked as a practitioner, educator and researcher in mental health and pharmacy practice for over 25 years.


Dr Caroline Robertson is a lived experience Research Fellow at the Griffith Centre for Mental Health and the ALIVE National Mental Health Research Translation Centre. Her areas of interests include the physical health of those experiencing mental illness and developing and implementing innovative integrated healthcare interventions to reduce barriers to care and improve wellbeing.
Professor Steve Kisely is a psychiatrist and public health physician with health services research experience in the UK, Australia and Canada. He currently works as a Professor at The University of Queensland.

Dr Bonnie Clough is a clinical psychologist, based at Griffith University. She was awarded her PhD (clinical) in 2016. Her research focuses on ways to improve consumer access and engagement with mental health services, particularly through the use of digital technologies. She is passionate about the training of health professionals and is currently Program Director of postgraduate clinical psychology at Griffith University.

Andrew Watkins1,2*, Eliza Draper1, Scott Teasdale3, Patrick Gould2, Philip B. Ward3,4, Liam Conlon1,2, Rachel Morell1,3*, Oscar Lederman5, Michael Hodgins1,3, Jackie Curtis1,2,3, Hamish Fibbins1,2,3*
1Mindgardens Neuroscience Network, Sydney Australia
2South Eastern Sydney Local Health District, Sydney Australia
3Discipline of Mental Health and Psychiatry, UNSW, Sydney Australia
4Schizophrenia Research Unit, Ingham Institute for Applied Medical Research, Liverpool, Australia
5School of Sport, Exercise and Rehabilitation, University of Technology, Sydney Australia
Background:
Extensive research has highlighted a significant disparity in health outcomes and mortality between people that experience a severe mental illness and the general population. Most of this disparity is driven by cardiometabolic diseases and as such are considered preventable. Lifestyle interventions along with identifying and treating earlystage signs of cardiometabolic dysregulation are considered best practice early intervention management but are poorly implemented in people that experience a severe mental illness.
Method:
The symposium will feature three presentations:
1. Cardiometabolic Resources Development: An overview of resources to upskill mental health professionals and general practice on cardiometabolic health management
2. Implementation in public mental health settings: Implementation of a group multidisciplinary physical health intervention across three community mental health centres in Sydney.
3. Keeping the Body in Mind-Primary Care: Evaluation of a primary care physical health service for people with severe mental illness.
Results:
1. Cardiometabolic Resources Development: Studies have shown clinicians lack confidence and knowledge in the early management of cardiometabolic dysregulation in people that experience a severe mental illness. Providing easy to use resource guides on this topic allows clinicians to increase their confidence and knowledge which can lead to improved service provision for cardiometabolic health protection in this population. This presentation will outline frameworks for cardiometabolic health management (both adult and adolescent) and tobacco treatment that have been developed.
2. Implementation in public mental health settings: A group physical health program was feasible and acceptable for preventing deterioration in cardiometabolic health. Ensuring successful implementation required service culture change for managers, clinicians and consumers of services. Peer work was considered fundamental for engagement, though the role itself lacked clarity and guidance. The group program promoted strong social connection which facilitated engagement.
3. Keeping the Body in Mind-Primary Care: Interviews with KBIM-Primary clinicians, participants and referrers revealed four themes that facilitate engagement with physical health services in this setting: accessibility (i.e. a hybrid approach, free cost), a mental health-informed service, multidisciplinary support, and impact on quality of life. Participation in this program was associated with clinically significant improvements in exercise and dietary measures.
Conclusions:
Improving clinicians’ knowledge in early lifestyle and pharmacological intervention can improve physical health outcomes for people living with a severe mental illness. Further implementation science research is needed to better understand the elements of successful delivery of such interventions into varying health care settings and geographical locations. This symposium will contribute to ongoing discussions for planning and implementing early intervention cardiometabolic health management for people that experience a severe mental illness by providing best practice guidance and real-world exemplars of implementation.
Disclosures:
Funding was received from the Mental Health Commission of NSW, South Eastern Sydney Local Health District and Central and Eastern Sydney Primary Health Network.
Acknowledgements:
We would like to acknowledge consumers and clinicians who participated in the evaluation of these projects.

Andrew is a Nurse Practitioner and has completed a PhD on physical health care in people experiencing severe mental illness. He is the Director of Programs and Innovation with Mindgardens Neuroscience Network. He was the co-developer and lead of the internationally acclaimed Keeping the Body in Mind (KBIM) across South Eastern Sydney Local Health District (SESLHD). Andrew has a longstanding interest in the physical health of people with severe mental illness.
Andrew has published over 40 peer-reviewed articles, book chapters and evidence guides. His clinical research has had strong practical translation implications, influencing clinical practice, health service delivery, policy and guidelines in mental health services locally, nationally and internationally.

Hamish is the Director Translational Research for Mindgardens Neuroscience Network, working implement research into practice at the system and service levels. In addition to completing a PhD with the UNSW Discipline of Psychiatry and Mental Health, Hamish has worked clinically as a mental health exercise physiologist and in health services management as a quality improvement advisor. He currently holds a Conjoint Senior Lecturer position with UNSW, Sydney.

Rachel Morell is Director of Operations for Mindgardens Neuroscience Network. Mindgardens brings together the strengths of four founding member organisations –UNSW, Black Dog Institute, Neuroscience Research Australia and South Eastern Sydney Local Health District, to improve the lives of people living with mental illness, drug and alcohol and neurological disorders by integrating research, healthcare and education.

SYMPOSIUM
Implementing Recovery Principles in the management of schizophrenia –Examining Theory and Practice through Case studies
Amit Banerjee1*, Begonya Grasa-Ward2, David Ward3
1 Consultant Psychiatrist, Headspace Early Psychosis, Youth Focus, Midland WA, Board Member ISPS Australia
2 Lived Experience as family member, Rockingham WA, Board Member ISPS Australia
3 Consultant Psychiatrist, Child and Youth Mental Health Services, Metro Health South, Logan, QLD, Ex-Board Member ISPS Australia
Background:
Recovery principles are enshrined in the National Standards for Mental Health Services. Recovery language is powerful and uplifting. All mainstream mental health services are supposed to be following them. Yet, their implementation in clinical service delivery in public mental health services across Australia leaves a lot to be desired. Outcomes are often poor, therapeutic nihilism is rife, dreams are routinely shattered, and lives are ruined. How have we got it so wrong? Are we doing anything right at all?
Method:
For this symposium, two consultants and a family member for a loved one diagnosed with schizophrenia, all members of the International Society for the Psychosocial Treatment of Psychosis, Australian branch (ISPS Au), come together to discuss a couple of case studies exploring controversies around the diagnosis of psychosis (David) and then the mother of a young adult diagnosed with schizophrenia (Begonya).
The symposium will start with a quick overview of Recovery principles to be mindful of when treating someone with schizophrenia (Amit), salient among them being least restrictive treatment, not reinforcing the power hierarchy, consulting with family, assertively addressing psychosocial factors and substance use, taking positive risks, avoiding polypharmacy and minimising side-effects.
David will then give a brief outline of a couple of young people where a standardised approach to diagnosis and management stalled progress, but a more nuanced individualised approach was more helpful. Begonya will then trace the treatment journey of her son, the onset of his illness at age nineteen, his long admissions to inpatient units in between, and aberrations such as being put on two depot injections as part of his routine treatment. A bright young man of twenty-nine who continues to suffer ongoing symptoms has been labelled ‘treatment resistant’ and whose family suffers with him. She will end by giving her perspective on what she thinks was done right for him over the years, what gives her hope now and what she thinks could have been done differently in the past.
Results:
The presenters will first discuss controversies around the nature of psychosis, citing concepts espoused by ISPS International, and highlight the dangers of jumping to hasty conclusions and subsequent inappropriate medication management. The presenters will then use an established scale measuring the application of recovery principles to the care of our main case study and try to reach a consensus score for each domain, with the help of the audience. Our hypothesis is that his care has fallen well short of expected standards.
Conclusions:
The aim of this symposium is to hold up a mirror to all who are doing routine clinical work in adult mental health services. Our hypothesis is that we are paying lip service to Recovery across the board in mental health services and falling way short of what is ideal. The presenters want to use the platform of this conference to appeal to professionals, lived experience champions, carers, policymakers, and everyone working in the sector. Give Recovery a chance. You won’t regret it.
Disclosures:
None
Acknowledgements:
To Begonya’s son, who has kindly provided consent for his case study to be presented


Amit is a recovery oriented general adult psychiatrist with primary interests in social and critical psychiatry, cross-cultural psychiatry and addictions. He considers his forte to be least restrictive treatment, critically appraising mental health systems and understanding the sociology of mental health and illness.
Begonya a culturally diverse advocate based in Western Australia, brings lived experience in mental health as a family member. As a lived experience educator at Curtin University, Yale LETS LEAD fellow and an ISPS board member, she is dedicated to inclusion, equity, and amplifying marginalised voices to drive meaningful change in mental health.

David is a senior child and adolescent psychiatrist working in a multi-stakeholder recovery-oriented adolescent day program in Queensland. He was involved in the development of early intervention services in the UK and was one of the co-authors of the NICE guidelines for child and adolescent psychosis.

Real-world antipsychotic prescription patterns among patients with schizophrenia in Australia: Results from the ARIEL study – Zainab Alttahir
Feasibility and effectiveness of digital health interventions in people with schizophrenia: A systematic review and meta-analysis – Urska Arnautovska
The Australian Early Psychosis Collaborative Consortium (AEPCC) PriorityTrials – development and implementation of research priorities into practice – Jo Fitzsimons
Newly Graduated Australian Psychologists’ Interest and Confidence in Psychological Approaches for Psychosis: What Role Can Psychology Training Providers Play in Increasing Access to Psychological Interventions for Psychosis? – Rachel M Brand
The Co-design and Research Translation Alliance in Mental Health: Developing architecture for streamlining implementation hybrid studies – Justin Chapman
Evaluating a referral-based exercise physiology service for people with mental and substance use issues – Meg Doohan
Supporting staff to address the physical health of consumers in mental healthcare settings: A modified Nominal Group Technique – Di HU
From Conversation to Commitment: Advocating priorities and driving change in psychosis research – Hamish Fibbins


Zainab Alttahir is an Australian registered pharmacist with a broad experience in clinical practice and in the pharmaceutical industry. In her professional career she has worked across a broad range of therapeutic areas and acquired regulatory and medical expertise in prescription and OTC medicines.
Dr Arnautovska is a psychologist, Senior Research Fellow at the UQ Medical School and Senior Mental Health Clinician at Queensland Health. Her research interests include digital interventions targeting physical comorbidity among people with schizophrenia and innovative clinical trial designs. She has over 50 publications and $13.5 in competitive research funding.



Jo Fitzsimons is the Executive Officer for the Australian Early Psychosis Collaborative Consortium (AEPCC). Jo has worked at in the mental health sector for over 20 years across many areas of including research, stakeholder engagement, network and partnership management and youth engagement both nationally and globally.
Dr Rachel M. Brand is a Clinical Psychologist and Senior Lecturer in Clinical Psychology at the University of the Sunshine Coast. Rachel has provided psychological therapies for people experiencing psychosis for over 15 years and conducts research into developing and disseminating psychological interventions for people experiencing distressing psychosis.
Justin Chapman completed his doctorate in measuring and positively influencing physical activity behaviour in adults with mental illness (2016). Dr Chapman is a Research Fellow at Griffith University and Metro South Addictions and Mental Health Service. He takes a national approach to translational research in health service models to improve the physical health and wellbeing of people with mental illnesses. Through extensive industry partnerships with non-government organisations, hospital and health services, and sports and recreation organisations, Dr Chapman has successfully scaled up exercise programs evaluated in clinical trial designs to social impact for over 600 participants with mental illness. Dr Chapman’s work has been acknowledged with an Open Minds Mental Health Week Achievement awards (2018), and the Australian Rotary Health award for Mental Health Impact (2020). He is a Board member of the national advocacy organisation Psychosis Australia, and on the Editorial Board of the journal Mental Health and Physical Activity.



Meg Doohan is a postdoctoral research fellow in the Centre for Mental Health at Griffith University; her work focusses on the influence of physical health interventions on individuals with severe mental illness. Meg earned her PhD from QUT in 2024, where her research explored the influence of dehydration and thermal strain on cognitive and physical performance in females.
Di Hu is a PhD candidate at Griffith University. Her doctoral research focuses on measuring and positively influencing staff practices in addressing the physical health of people with severe mental illness within mental healthcare. Her research applies frameworks such as COM-B and the Theoretical Domains Framework, and uses Nominal Group Technique and Delphi methods to engage mental health professionals in enhancing physical healthcare in mental health settings. She is also involved in a multimorbidity physical health project within mental health services. During her Master of Public Health at UQ, Di contributed to suicide prevention research.and physical performance in females.

Hamish Fibbins is the Director Translational Research for Mindgardens Neuroscience Network, working implement research into practice at the system and service levels. In addition to completing a PhD with the UNSW Discipline of Psychiatry and Mental Health, Hamish has worked clinically as a mental health exercise physiologist and in health services management as a quality improvement advisor. He currently holds a Conjoint Senior Lecturer position with UNSW, Sydney.