

Understanding Ovarian Cancer Surgery: Comparing your options
Mario M. Leitao, Jr., MD
Member & Attending Surgeon, Gynecology Service
Director, Gynecologic Oncology Fellowship Program
Director, Minimal Access and Robotic Surgery (MARS) Program
Department of Surgery
Professor,Weill Cornell Medical College


Disclosure
Ad hoc consulting, lab proctoring for Intuitive Surgical
Ad hoc consulting, Medtronic & Ethicon

Anatomy


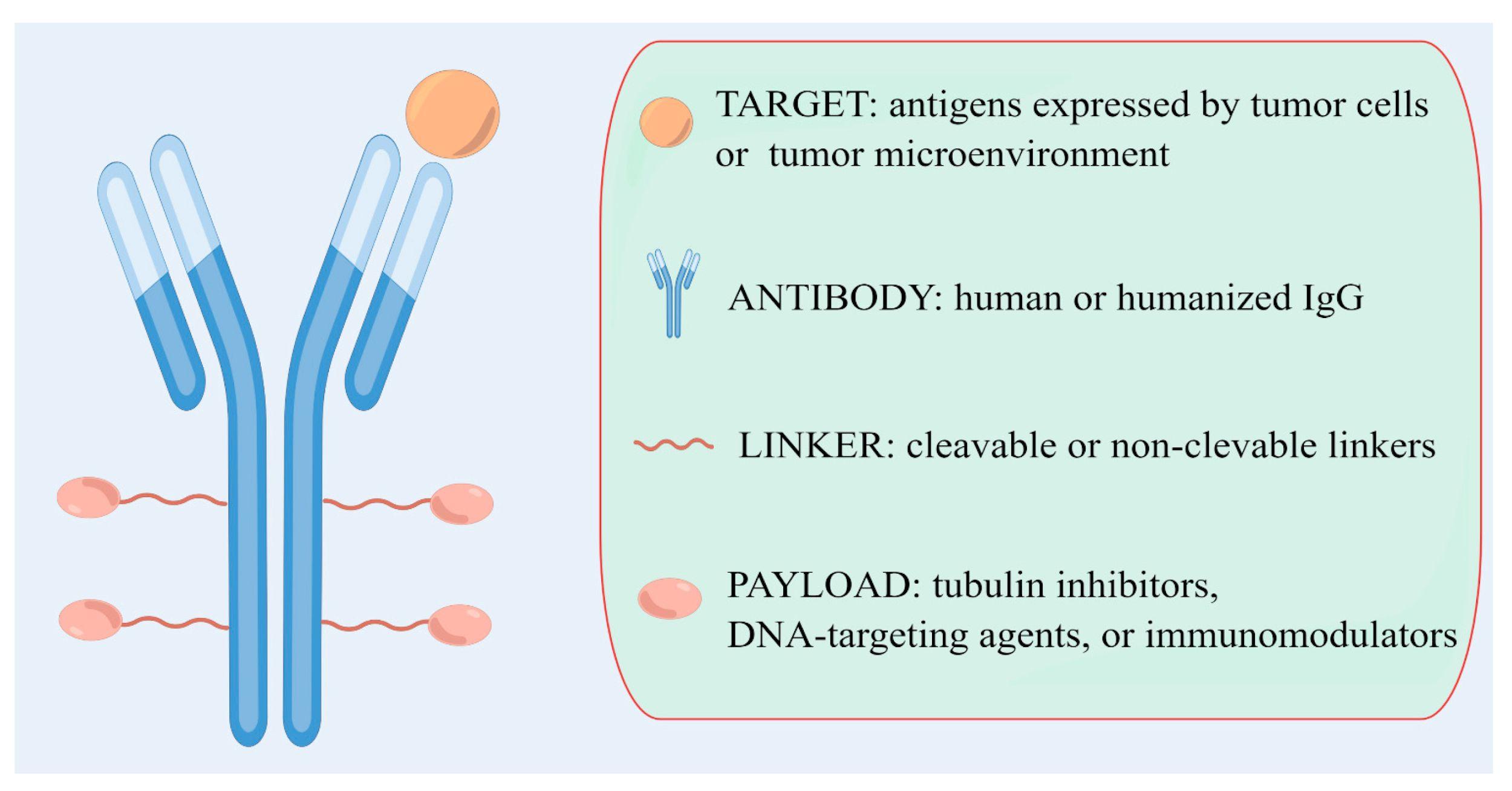
Different Diseases
• High grade serous
• Low grade serous
• Germ cell tumors
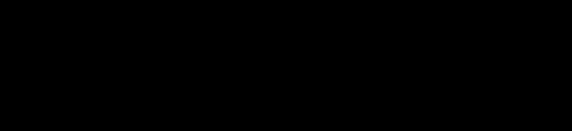
• Sex-cord stromal tumors
• Borderline tumors




https://ovarian.org/about-ovarian-cancer/types-and-stages/

LAPAROTOMY
“OPEN surgery”

LAPAROSCOPY
“Minimally Invasive Surgery”



LAPAROSCOPY – ROBOT ASSISTED
“Minimally
Invasive Surgery”





Most important to have a great surgeon!
Bonus if they know how and can do it minimally invasive
(less complications, less pain, home same day)
Every patient and situation is unique and individual
No ”ALL-OR NONE” approach

Ovarian Cancer At First Diagnosis Surgery is KEY!
• No obvious spread outside of ovary (clinical stage I)
• Establishes diagnosis
• Make sure no microscopic spread of cancer
– Accurate stage and prognosis
– Make sure if truly stage I
• Stage III if spread to lymph nodes and treatments are different
– Pick best treatments

“Suspicious” masses
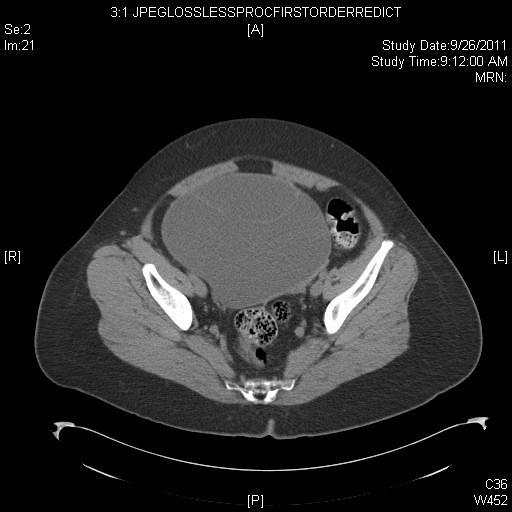
54yo (CA125=21)
Serous cystadenoma

48yo (CA125=104)
Endometriosis
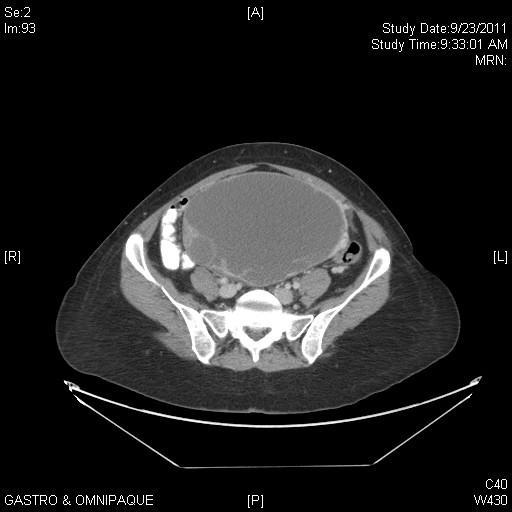
47yo (CA125=47) Serous adenoca
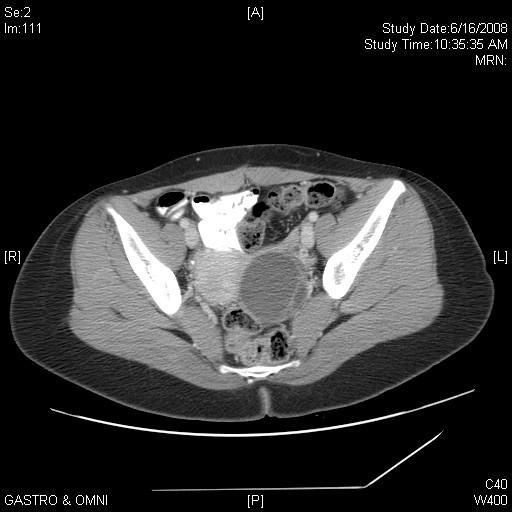

32yo (CA125=20) Mucinous BT
21yo (CA125=21)
Serous BT

Ovarian mass – possible cancer
Surgery - premenopausal
Remove affected ovary and tube
Remove other tube if completed family Send for frozen section (“quick look”) by pathologist during surgery
MIS or OPEN
Depends on surgeon and size of mass in relation to patient size

If cancer, then remove lymph nodes, omentum and do biopsies in abdomen

Can save other ovary and tube and uterus if wishes to have children
Ovarian mass – possible cancer
Surgery – post-menopausal
Remove affected ovary and tube and at least other tube
Consider removing both ovaries
MIS or OPEN
Depends on surgeon and size of mass in relation to patient size

Send for frozen section (“quick look”) by pathologist during surgery
If cancer, then remove uterus, cervix, lymph nodes, omentum and do biopsies in abdomen

Early Stage Ovarian Cancer Recommended
AdjuvantTherapy in U.S.
Low Risk
Stage IA/IB, Grade 1
Intermediate Risk
Stage IA/IB, Grade 2
High Risk
Stage IA/IB, Grade 3
Stage IC, any Grade
Stage II

Observation with no further therapy
Observation with no further therapy OR
Consider platinum based therapy
Combination chemotherapy with platinum and paclitaxel for 3-6 cycles OR Consider participation in research protocols
Hensley, Leitao, Brown. Atlas of Cancer 2003.
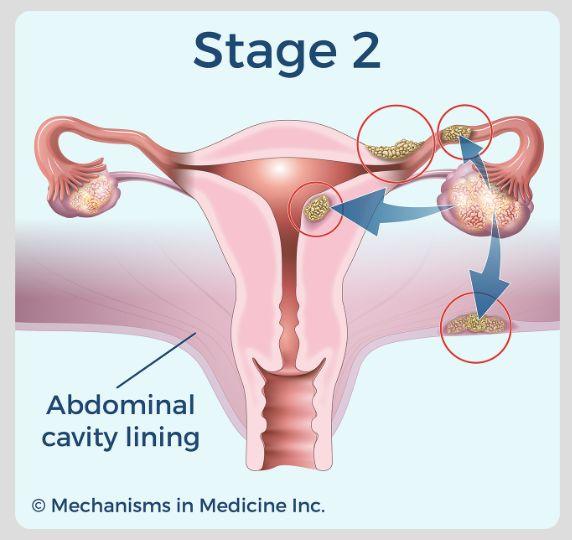
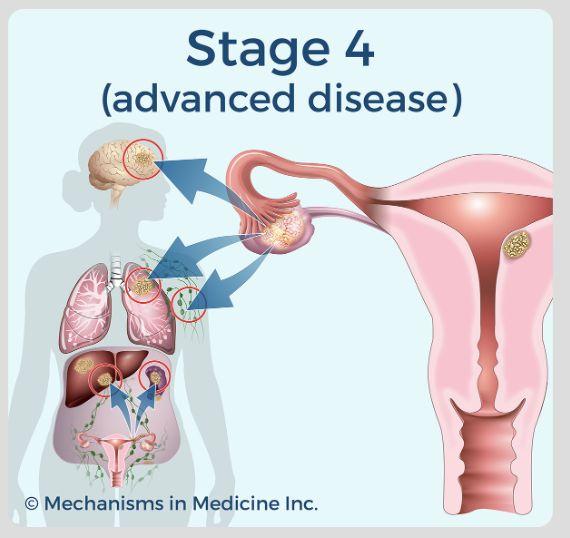
Ovarian Cancer At First Diagnosis Surgery is KEY!
• Obvious spread of cancer (stages II-IV)
– Goal is to surgically remove all visible tumor
– Chemotherapy is also key
– Questions:
• Surgery or chemo first?
• Can be done with laparoscopy (with or without robot)?






Optimal Cytoreduction
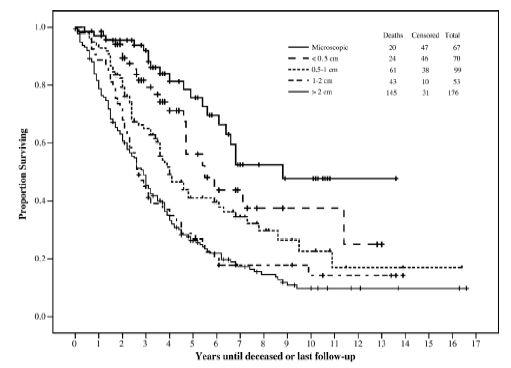
Women living 10 years and more with their cancer!!



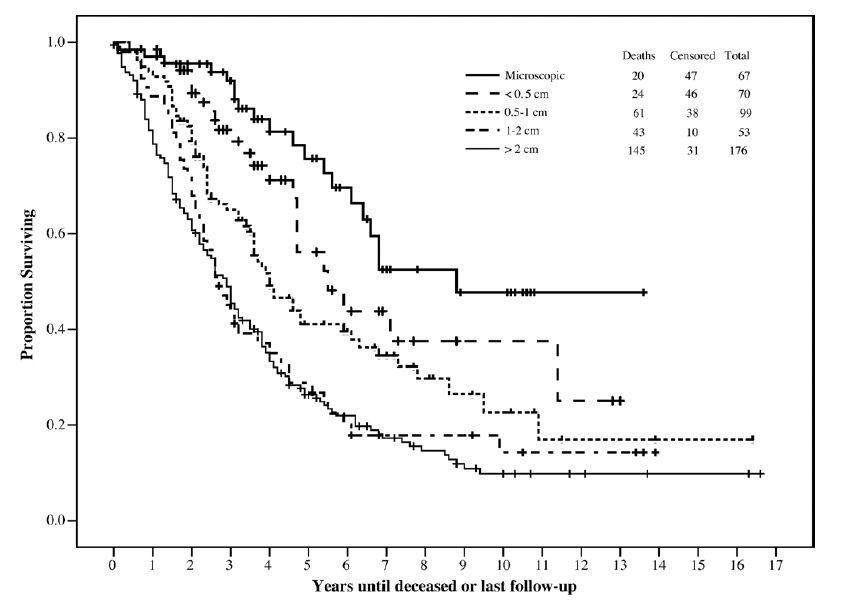
Chi DS, et al. Gynecol Oncol 2006;103:559-564.
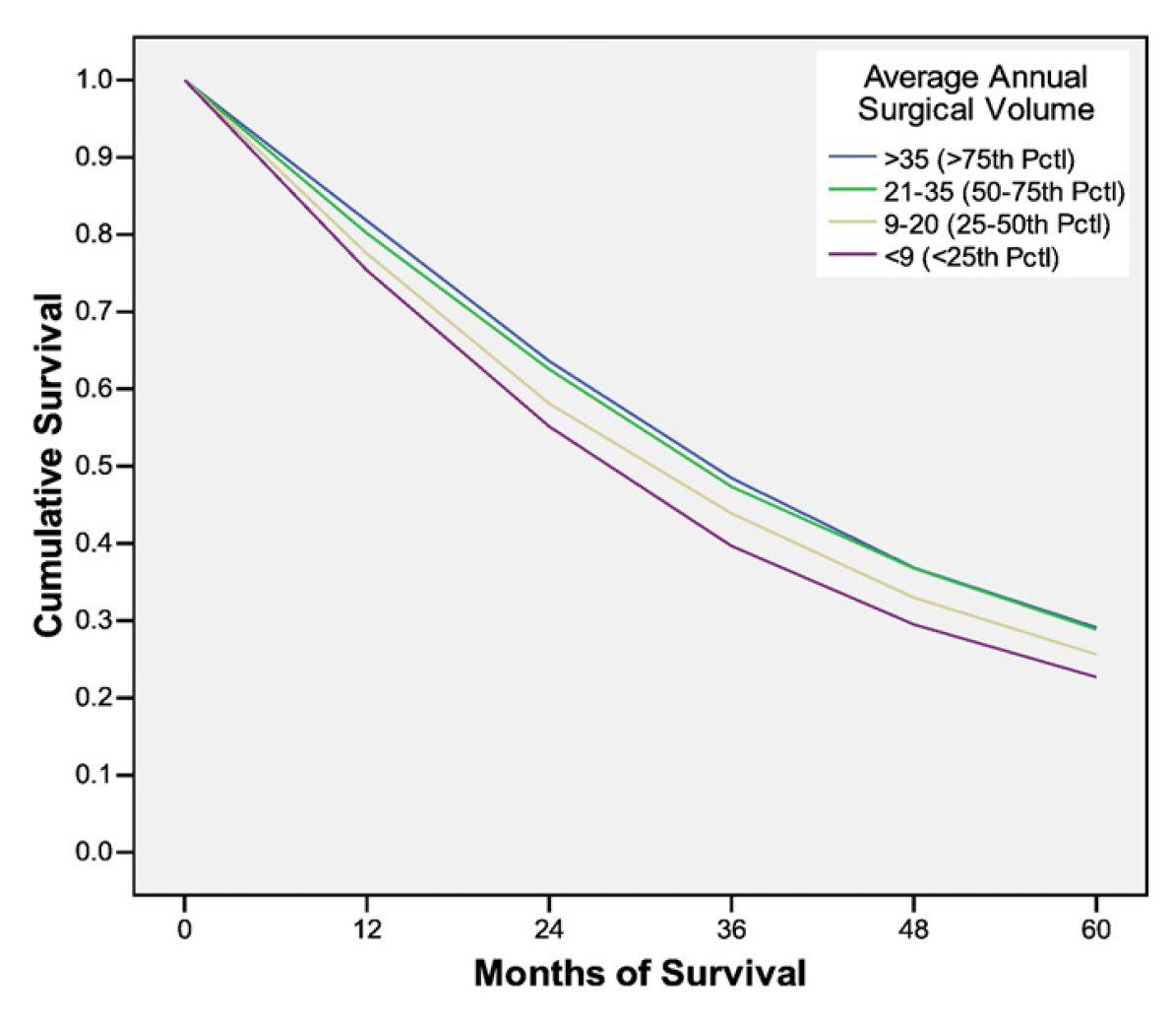
It MattersWhoYou See First

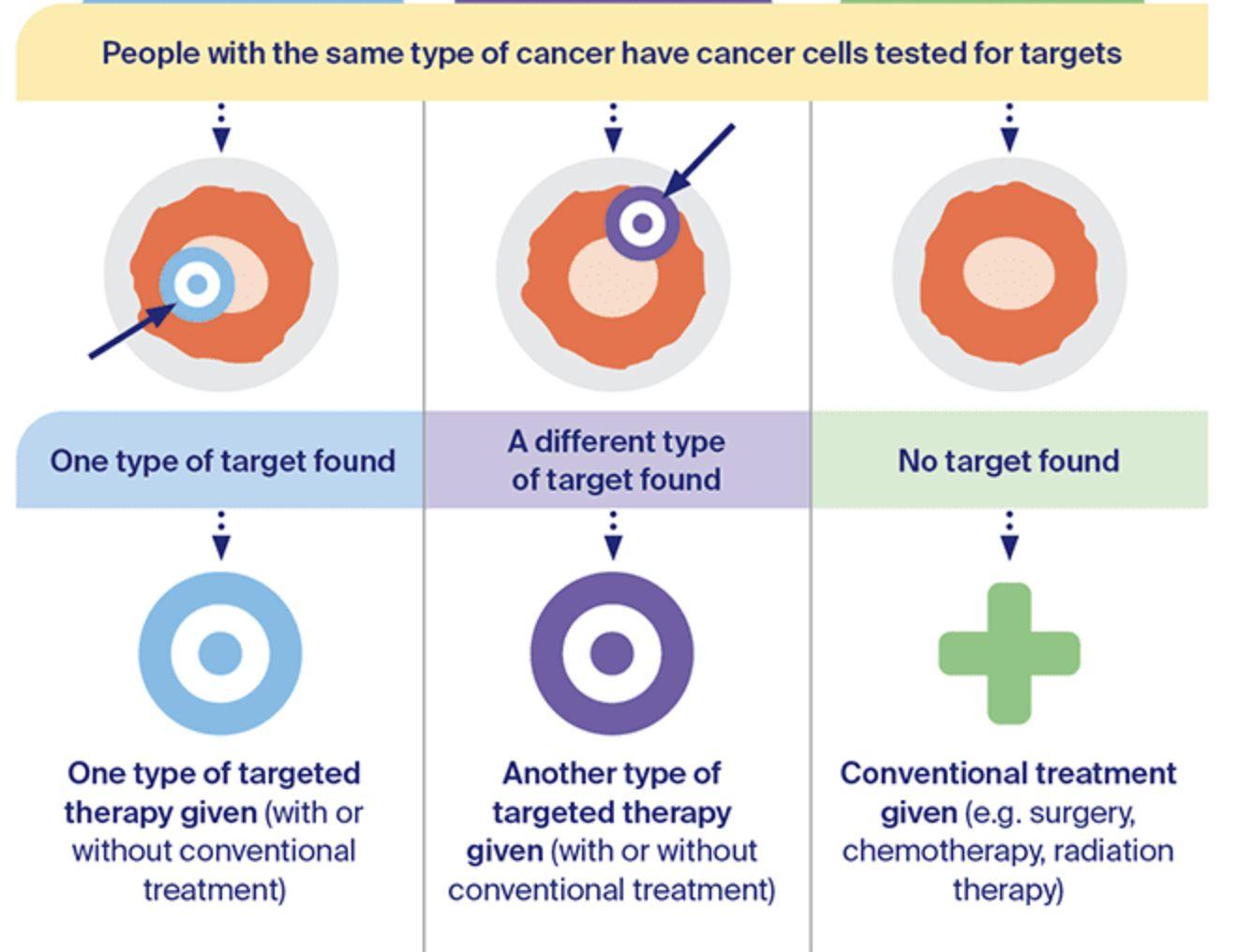
Clinical randomized trials (PDS v NACT)



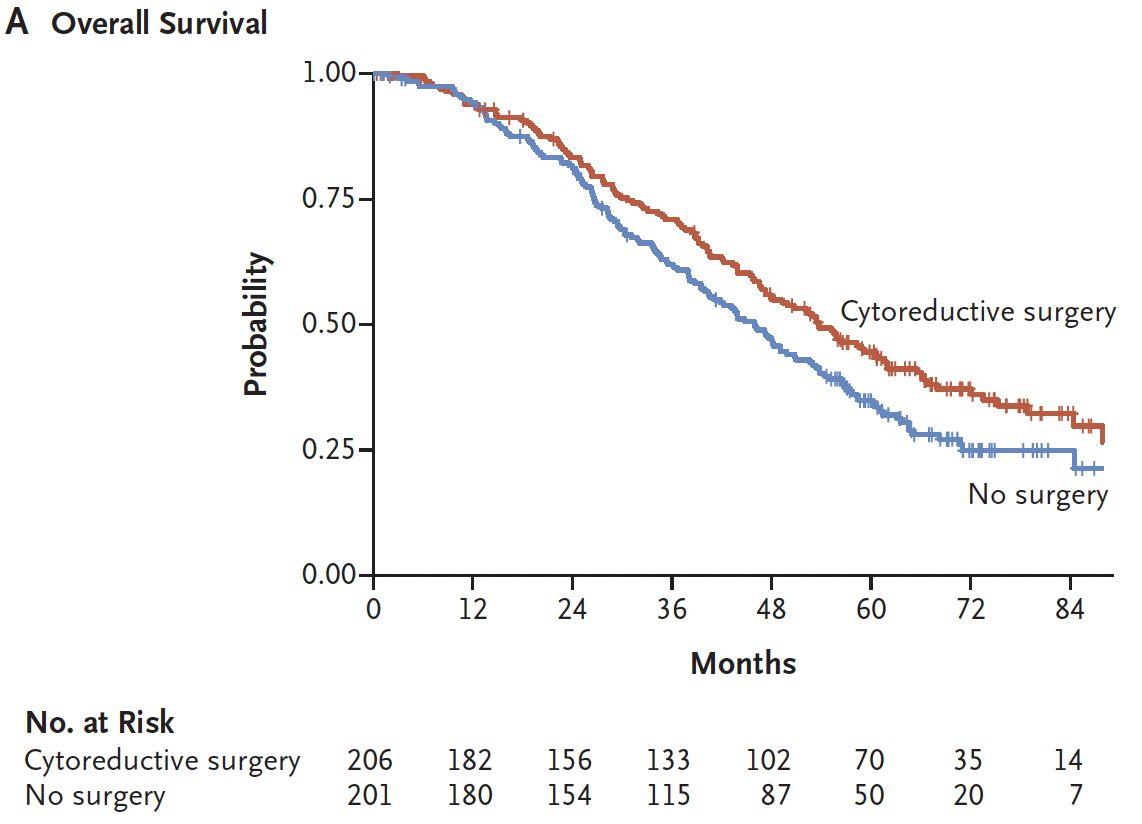
TRUST Study Design
Primary endpoint
Main Inclusion Criteria
• Epithelial ovarian, fallopian tube or peritoneal cancer
• FIGO stage IIIB/C, IVA/B
• Considered resectable
• Fit enough to tolerate radical surgery
RBiopsy
Stratification factors
•Center
•Age-ECOG-combination
ECOG0 and age ≤65y vs.
ECOG>0 or age >65y
Qualification process for participating centers to ensure surgical quality
Primary Cytoreductive Surgery

• Overall survival Key secondary endpoints
• Progression-free survival
• Complete resection rate
• Surgical procedures
• Surgical morbidity
• Quality of life
Neoadjuvant Chemotherapy +
Interval Cytoreductive Surgery
Recommended systemic treatment:
• Carboplatin AUC5, Paclitaxel 175mg/m2 q3w
• Bevacizumab 15mg/kg q3w as indicated
• PARPi as indicated
• Study participation or any other treatment as long as applicable for both study arms

Predefined exploratory and translational endpoints
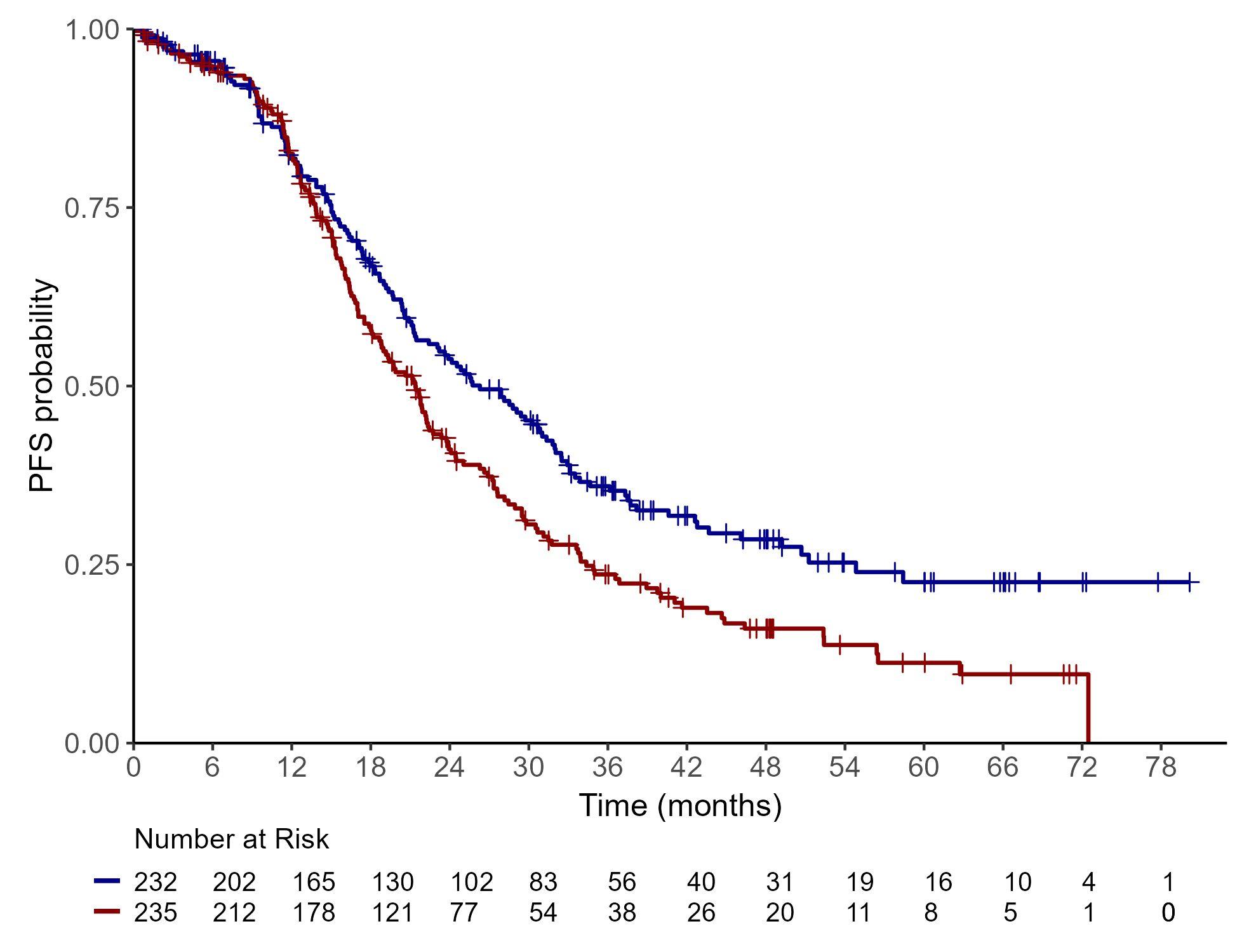
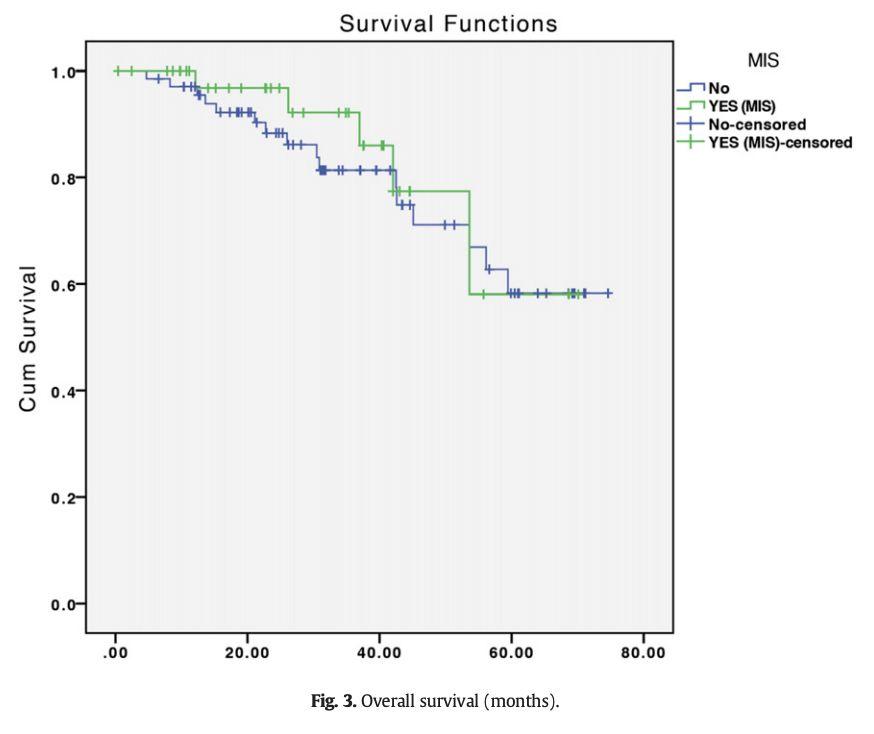
TRUST Results: Progression-free Survival (ITT)
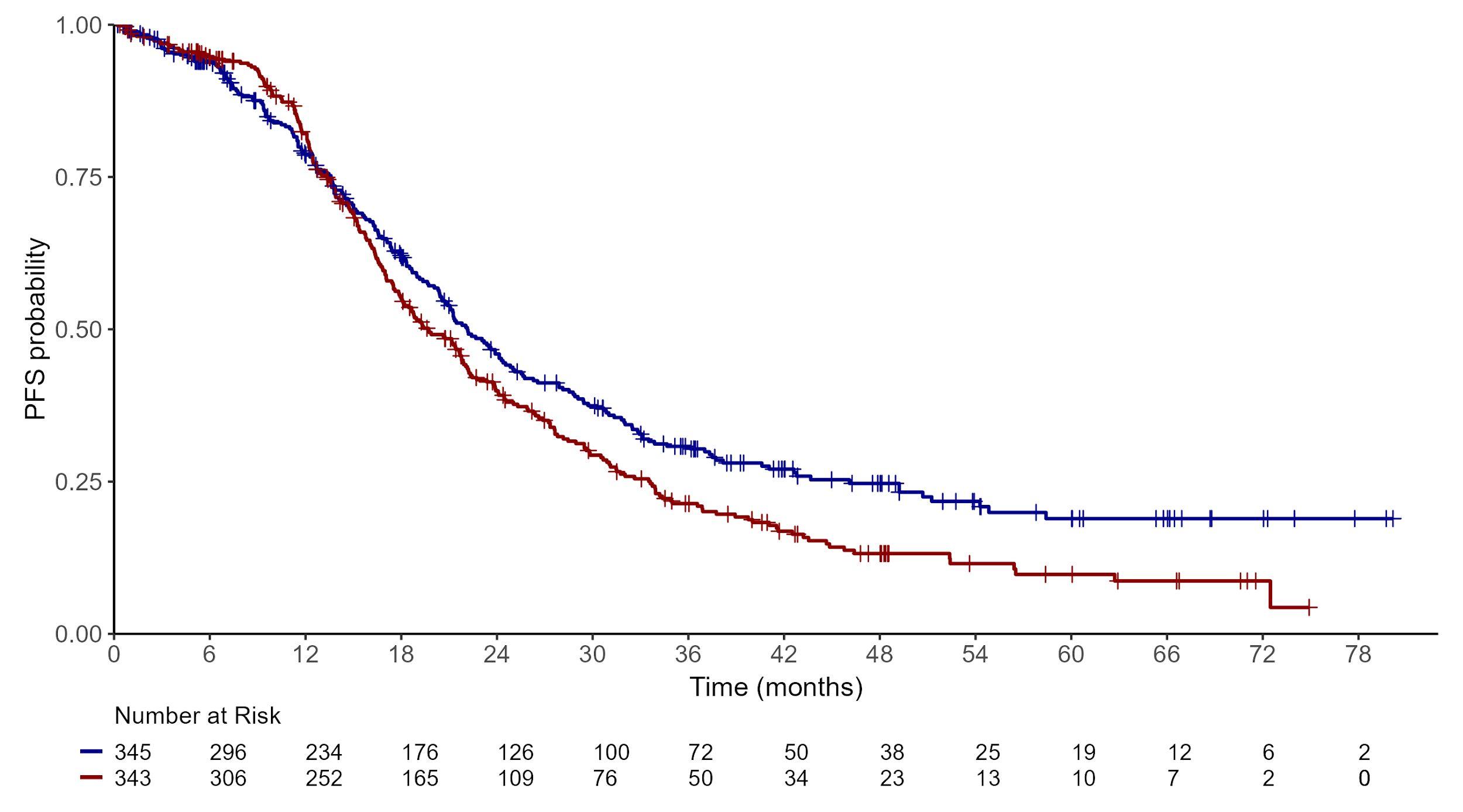
Median follow-up for PFS: 46.8 mos, IQR: 30.7-60.5 mos (69% maturity) patients were censored at their last regular date before experiencing a follow-up gap of more than 210 days (7 months) without a PFS assessment.


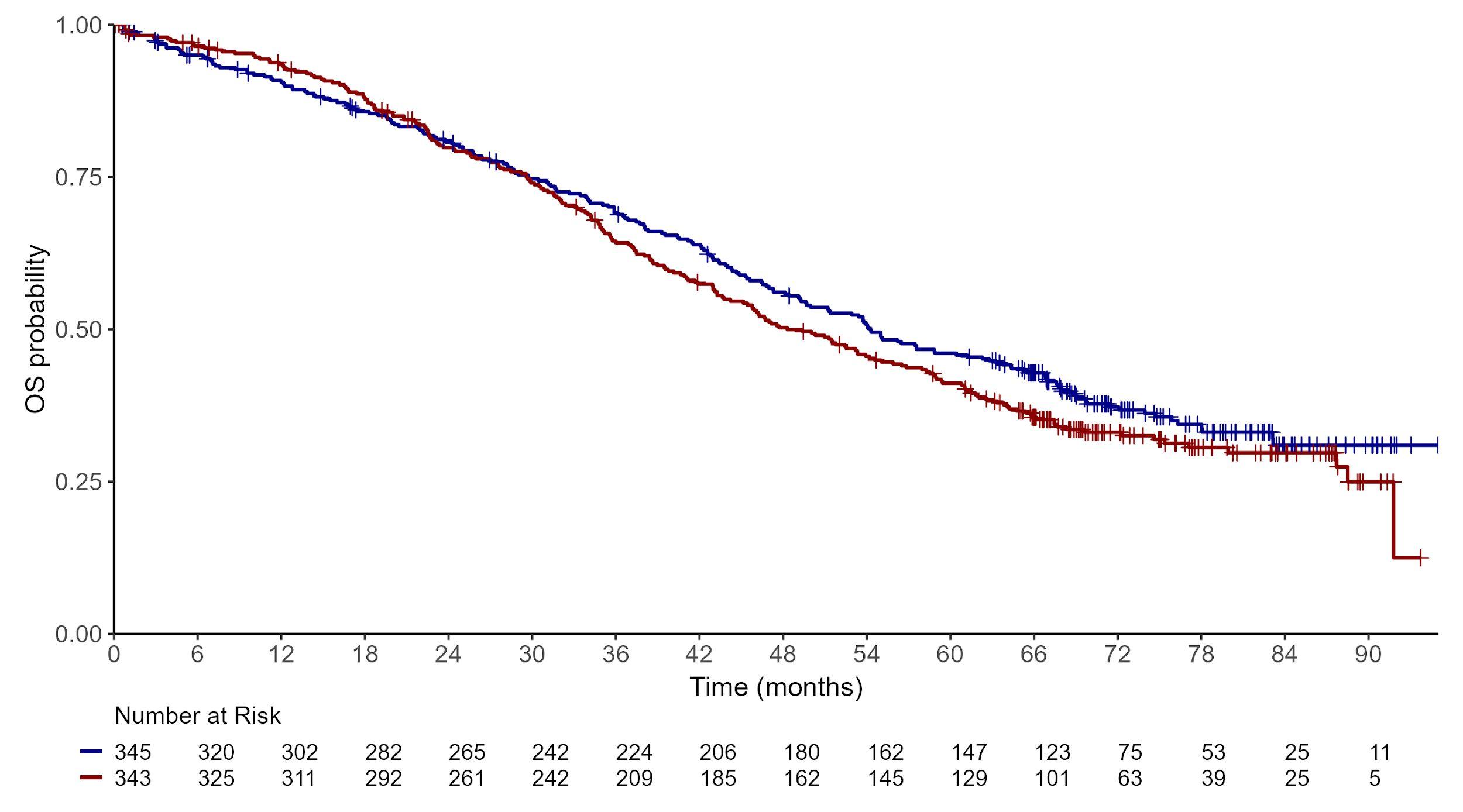
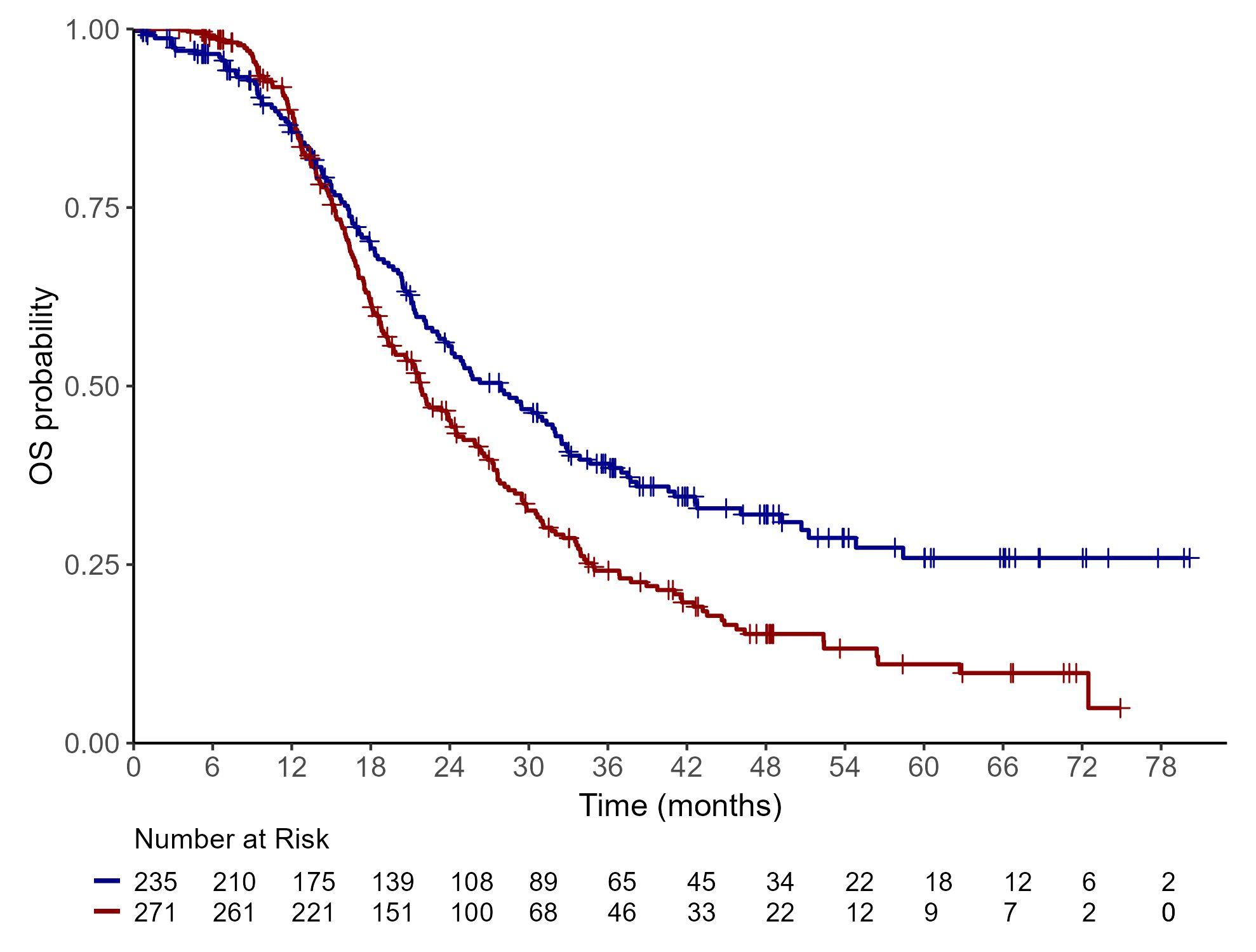
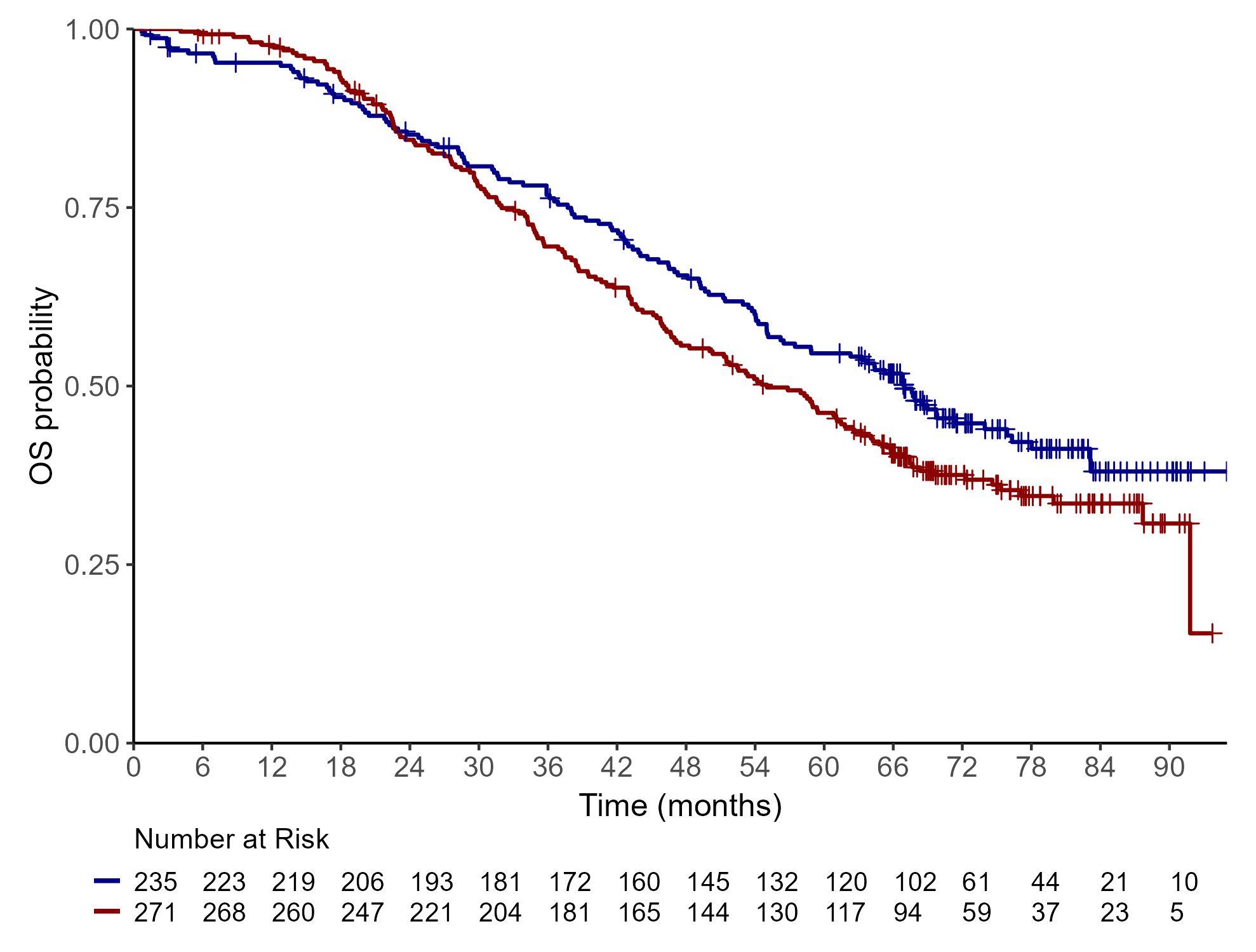
TRUST Results: Overall Survival (ITT)




PREFERRED
Medically fit for surgery
A complete resection of all tumor possible
Surgeon/team skills critical
Majority needs to be done with OPEN surgery
Very select situations in which MIS is possible
Do not do NACT to try to get to MIS
Sometimes use laparoscopy to assess “resectability”

MSKCC RESECTABILITY SCORE
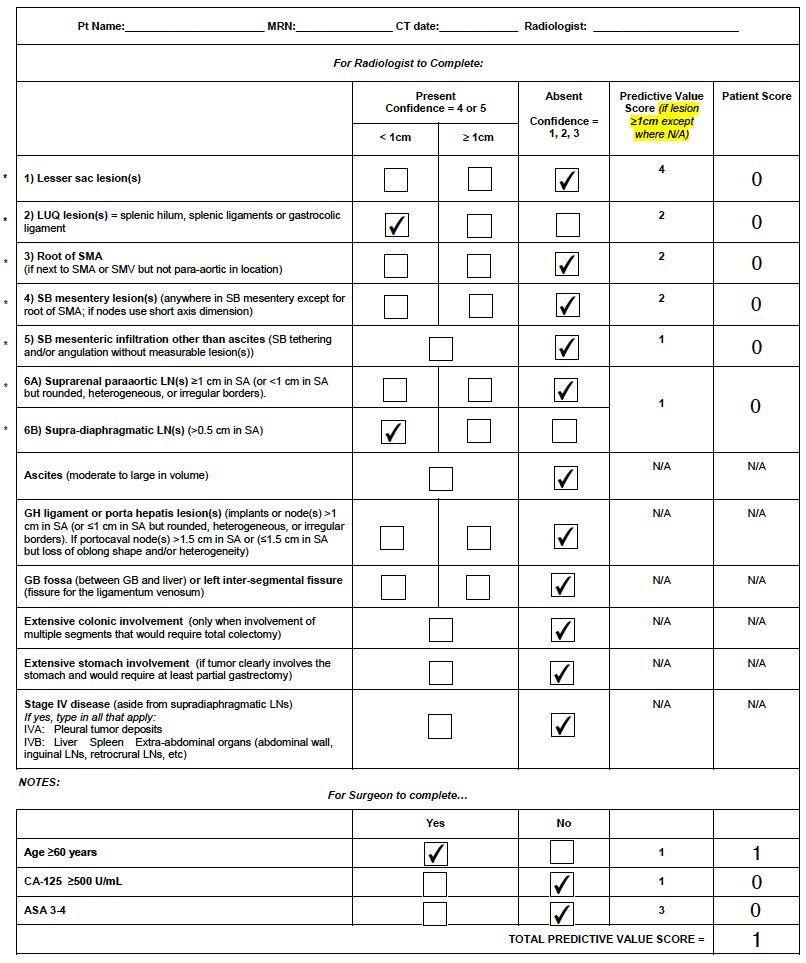

MSKCC RESECTABILITY SCORE
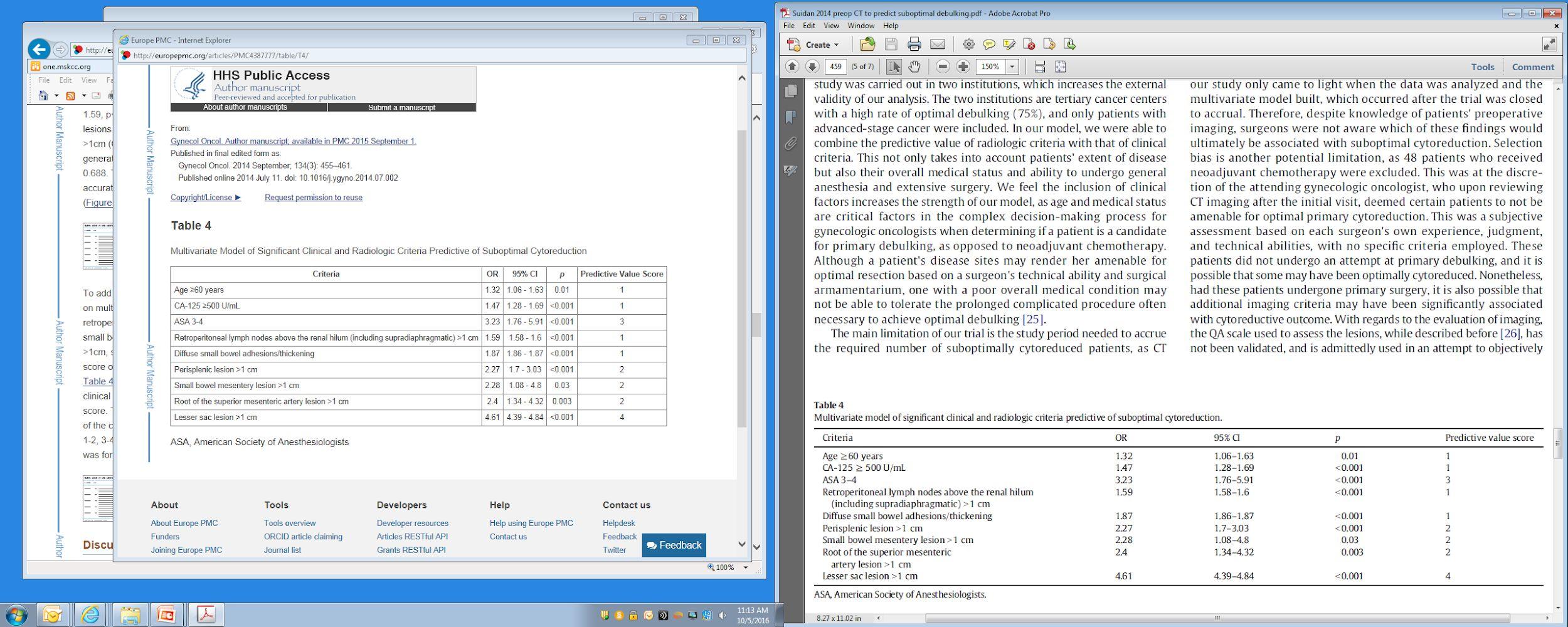
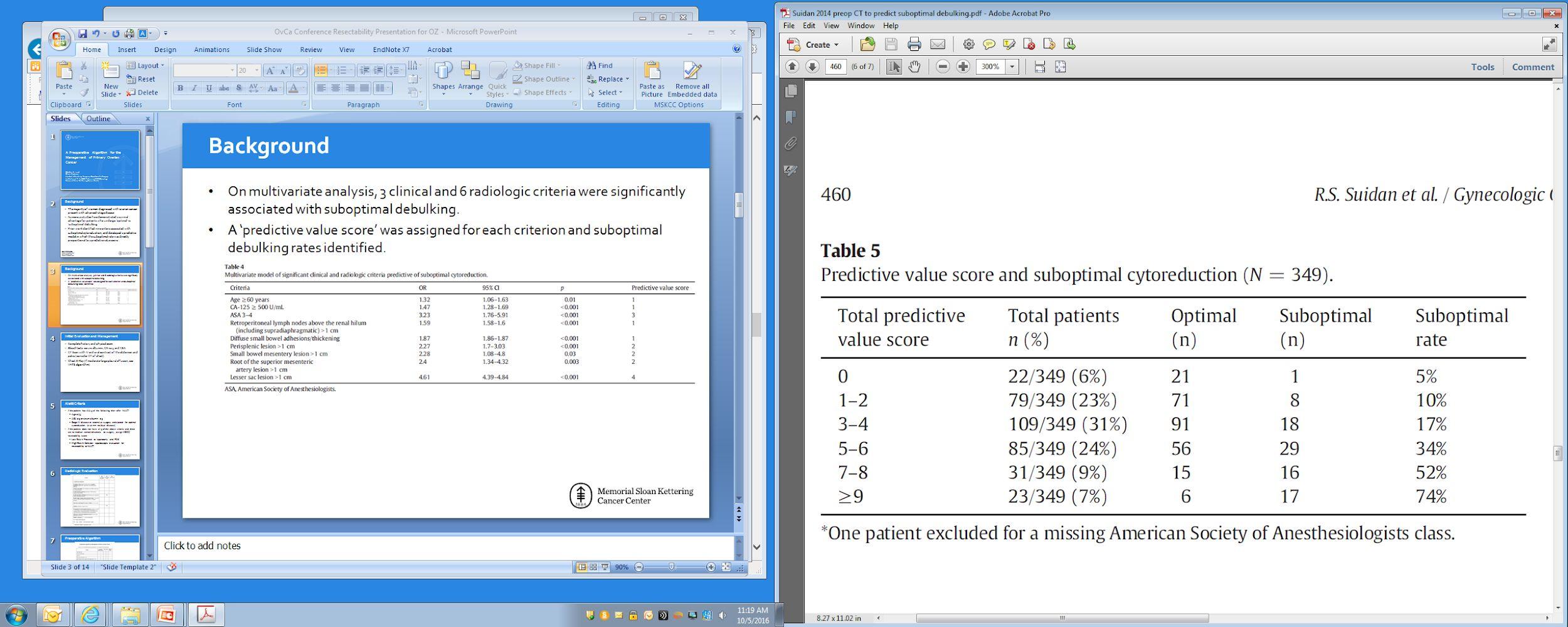

Suidan RS, et al. Gynecol Oncol 2014;134:455-461.



BEST OPTION FOR SOME
Not fit for surgery and CGR not possible “Interval Debulking Surgery (IDS)”
Many still require OPEN surgery Greater chance of being able to use MIS (+/- robot)
HIPEC is a consideration

HIPEC Only “standard” at IDS


“All-or-none” approaches are not


Thoracic disease
Parenchyma
1% (2/178)
Supradiaphragmatic
63% (112/178)
Location of Resection

Multiple intrathoracic areas
17% (30/178)
Mediastinum
12% (22/178)
Pleura
7% (12/178)
ProceduresTo ConsiderTo Obtain CGR
Cytoreduction – PDS or IDS
• Bowel resection (small and large)
• Retroperitoneal lymphadenectomy
• (Modified) posterior exenteration
• Ureteral/bladder resection
• Hepatectomy
• Splenectomy
• Diaphragmatic stripping and/or resection
• Supradiaphragmatic nodal dissection
• VATS/pleurectomy (THO)
• Mediastinal nodal dissection (THO)

CANCER CAME BACK “Recurrence”


MANY OPTIONS





An option again based on patient, tumor and surgeon factors
Goal is complete resection
OPEN or MIS possible
Secondary cytoreduction MSKCC
Recommendations

Secondary cytoreduction GOG 213
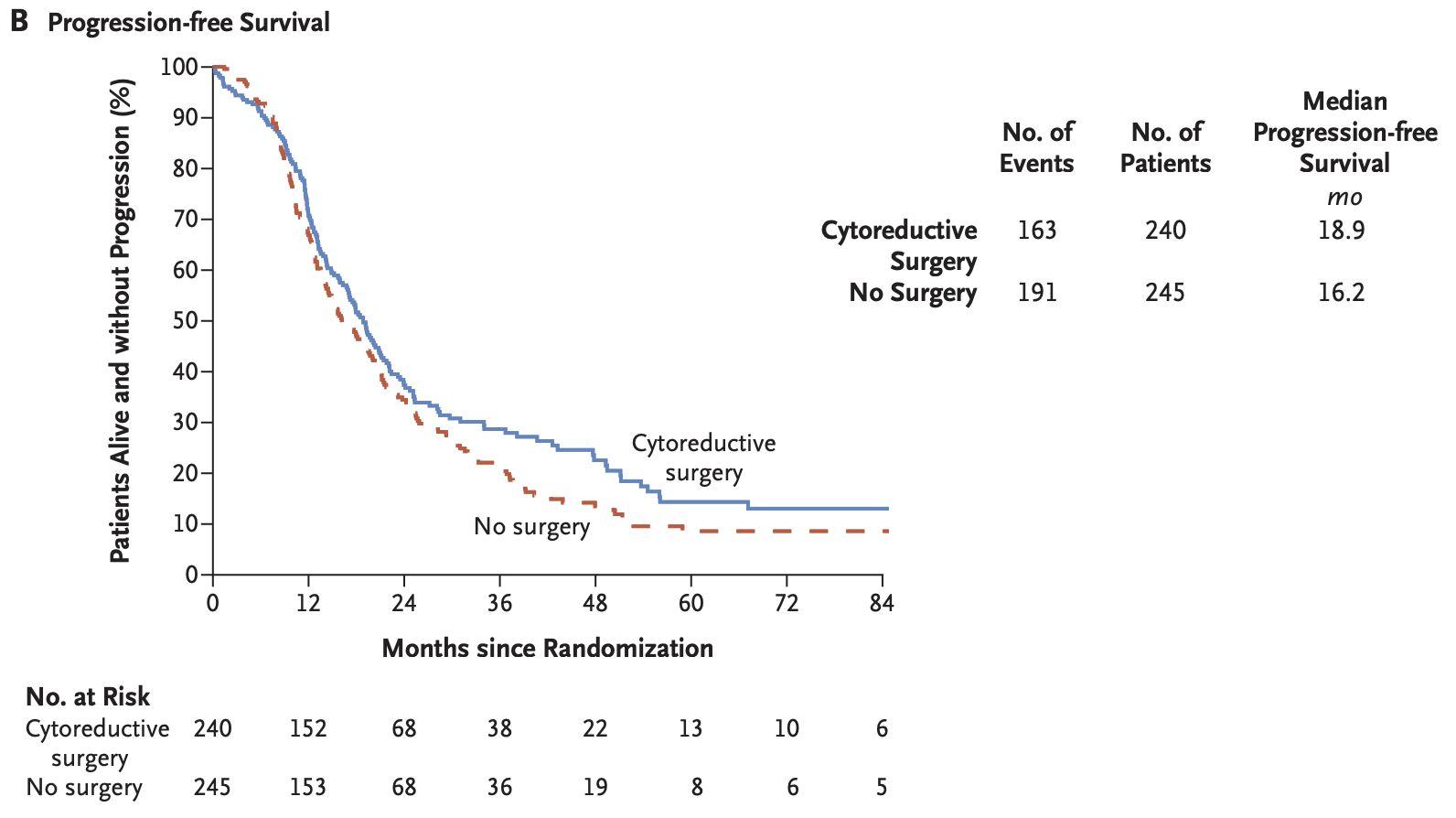
HR 0.82 (95%CI: 0.66-1.01)

Plat-sensitive first recurrence
Deemed amenable to CGR by surgeon 63% CGR rate
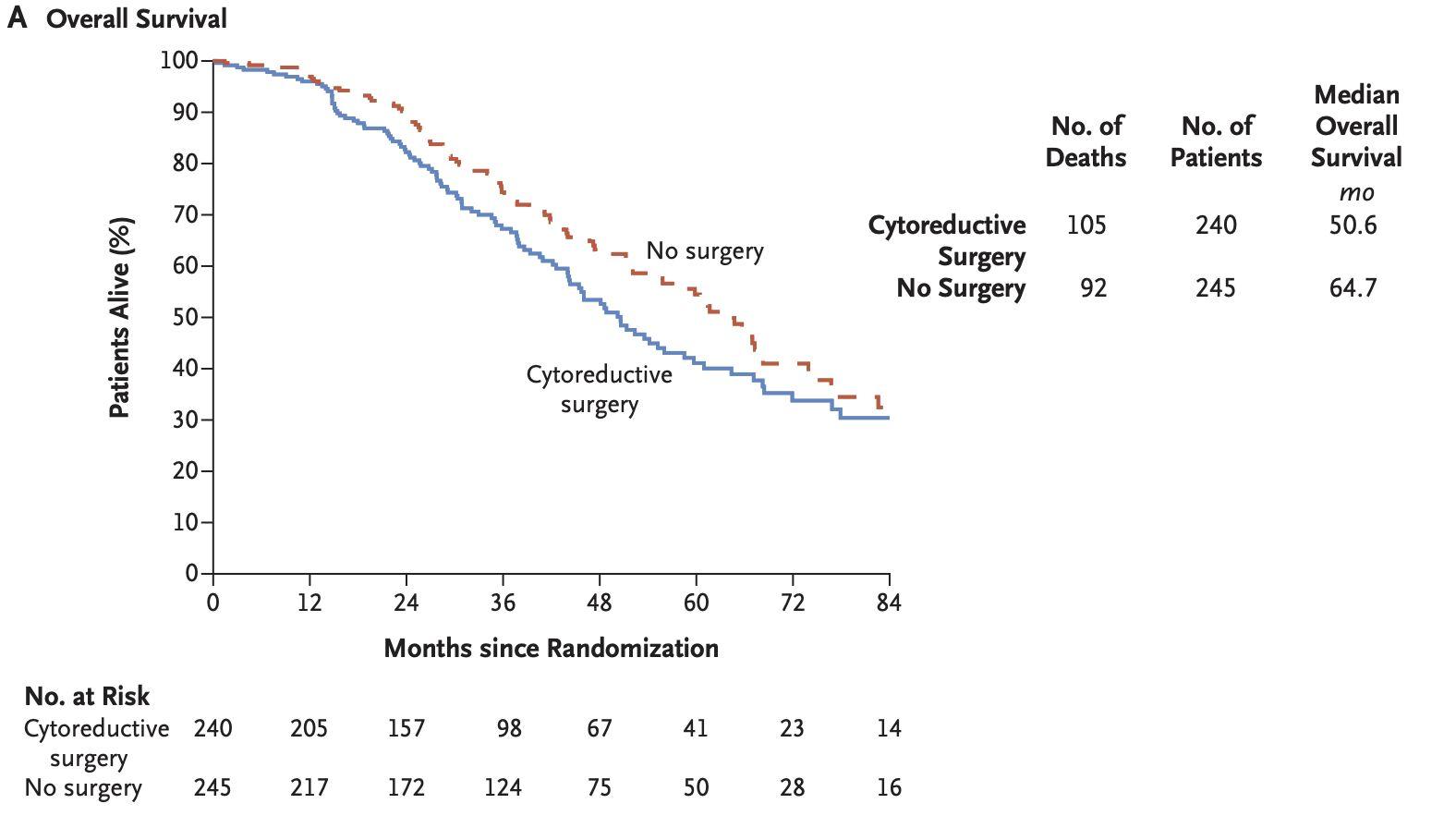
HR 1.29 (95%CI: 0.97-1.72)
Coleman RL, et al. N EnglJ Med 2019;381:1929-1939.
Secondary cytoreduction DESKTOP
III
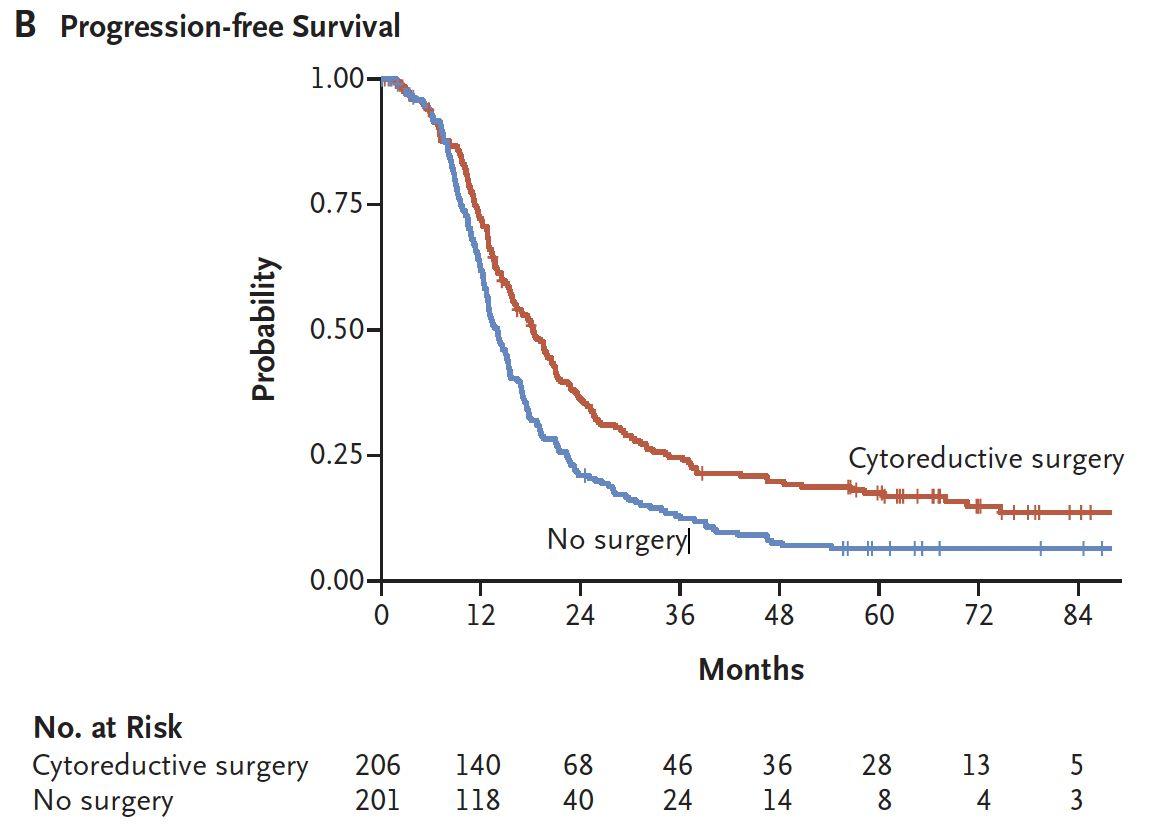
Plat-sensitive first recurrence
Positive AGO score:
ECOG=0 CGR after primary surgery
Ascites < 500ml 75% CGR rate HR 0.66 (95%CI: 0.54-0.82)

Harter P, et al. N EnglJ Med 2021;385:2123-2131.
Secondary cytoreduction
Plat-sensitive first recurrence
iModel score (<4.7) + PET/CT:
FIGO stage
Residual after primary surgery
Plat-free interval
ECOG, CA125, Ascites

OS HR 0.82 (95%CI: 0.57-1.19)

ShiT, et al. Lancet Oncol 2021;22:439-449.


Manning-Geist BL, et al. Gynecol Oncol 2021;162:345-352.
Quatenary+ cytoreduction MSKCC
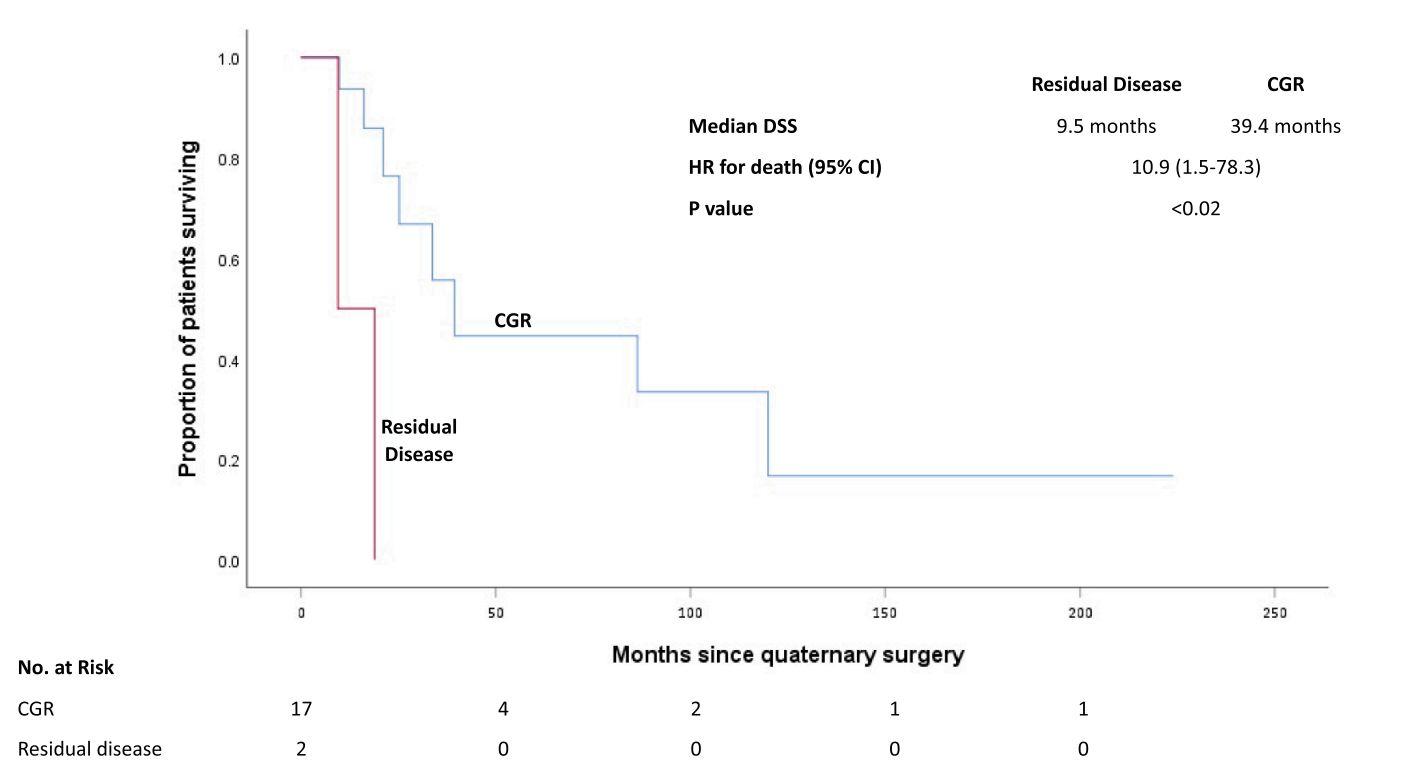

Manning-Geist BL, et al. Gynecol Oncol Rep 2021;37:345-100851.


Top 3 (+1) top takeaways…
• SURGERY is a key intervention in the care of women with ovarian cancer at first diagnosis and in recurrence
• Need to find experienced surgeon/center who know who to operate on, when to operate on, and which surgical approach is best
• Minimally invasive surgery is better but in properly selected cases and the robot is a tool to do MIS
Encourage participation in clinical trials!!







SpecialThanks to all the wonderful strong women that I have the privilege of being a part of their life
