
Julie Larson, LCSW - www.julielarsonlcsw.com


Julie Larson, LCSW - www.julielarsonlcsw.com
When we experience distress, we can initially perceive ourselves as incapable of coping
Distress depletes energy, cognitive problem-solving skills and emotionally and physically feels unpleasant





•How hard is this going to be?
•Do I have the skills?
•Do I have the emotional strength and courage?
•Is there anyone who can help me?

• Studies have shown that 4-22% of cancer survivors have a risk of developing PTSD.
• Those with more pain, advanced cancer or who have suffered other types of trauma are more at risk.
• PTSD includes intrusive thoughts, irritability, sleeplessness which interfere with quality of life, daily functioning or work.
• Symptoms can cause patients to avoid places or things that remind them of the event and cause delays in follow up care.
Julie Larson, LCSW - www.julielarsonlcsw.com
ALL attention focuses on avoiding, fighting, escaping the pain
Help patients bring attention to how their body is experiencing stress and how that influences behavior. (reduce shame)
Educate on the involuntary nature of the response to hardship (Fight, Flight, Freeze)

Julie Larson, LCSW - www.julielarsonlcsw.com
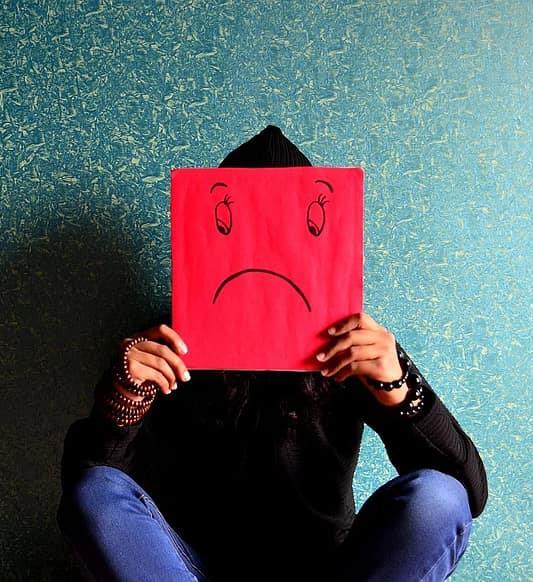
• Shock/disbelief
• Fear
• Sadness/grief
• Helplessness
• Guilt
• Anger
• Shame Physical Symptoms
• Dizziness, faintness, shakiness
• Rapid breathing and/or heart rate
• Racing thoughts
• Changes in sleeping patterns
• Physical pain (especially stomach and headaches)
• Loss or increase in appetite
• Increased substance use/dependence to numb
Julie Larson, LCSW - www.julielarsonlcsw.com
Respect the body’s reaction to trauma and how this may have changed someone’s neurophysiology.
Because breath changes during acute stress, we can help bring attention to the change and build awareness and skill to breathe through.
Reframe the personal narrative to body’s response. Understanding leads to more self-compassion.

Validated and forgiving of self.
Normalized within peer-to-peer support. Julie Larson, LCSW - www.julielarsonlcsw.com
Make decisions more easily
Engage with others
Take positive risks
Open to new ideas

“I HAVE TO DO THIS ON MY OWN. “
When people have trusted relationships available to them they can begin trusting themselves and the world around them.
“I CAN NOT DO THIS BY MYSELF.”
Attachment and connection to someone who can tolerate the ups/downs and doesn’t judge helps begin the process of PTG.
Julie Larson, LCSW - www.julielarsonlcsw.com

Will cancer come back? Will it progress?
Will I get a secondary cancer related to my treatments?
Will I recognize symptoms?
What do I pay attention to? What do I dismiss?
Am I doing enough?
Am I overdoing it?
Julie Larson, LCSW - www.julielarsonlcsw.com
Many Factors influence a person’s response during their cancer experience:
•Interactions with their care team
•Social support network
•Personal coping style
•Personality
•Past experiences

• When a traumatic event happens, most people experience a stress response – fight, flight or freeze.
• Traumatic stress and PTSD look similar initially, but PTSD progresses differently over time.
• With PTSD your mind stays in a state of shock or hypervigilance instead of feeling better over time.
• The symptoms interfere with normal functioning
1. Re-experiencing the trauma through intrusive flashbacks and/or nightmares
2. Emotional numbness and avoidance of places, people and activities that remind you of the traumatic event
3. Trauma heightened arousal: difficulty sleeping, trouble concentrating, feeling jumpy or irritable
1. Share your story and your feelings with others you trust
2. Find the facts you know to be true
3. Find more facts from others or with reflection
4. Connect with others who have a similar story and listen to their response and the way they have walked through hardship
1. Visualize your body as safe, calm, secure – I am safe. I am ok in this exact now.
Stretch
Meditation, prayer, stillness
Nature
Music
Mindless activities: knitting, gardening, cooking, crafting…
1. Connect with your five sense: 5-4-3-2-1
2. Quiet and elongate your breathing – inhale/exhale
3. Take off your shoes, wiggle your toes, connect to the gound
4. Touch your own body
5. Prolonged hug with someone else – match your breathing
6. Put your hands in water – splash your face
7. Drink ice cold water – notice the sensation as you swallow
Julie Larson, LCSW - www.julielarsonlcsw.com
Avoid Negative Coping 1. Quick fixes may make things worse in the long run 2. Substance abuse 3. Escape (flight) sleeping
Withdraw and isolation
Irritation and outburst of anger directed at others/circumstances
1. Processing with a therapist might help you identify thoughts/feelings that you are less aware of today
2. A outside perspective might notice your strengths and helpful coping which strengthens your ability to care for yourself
3. Sharpen self awareness – thinking, feeling and being
4. Develop new or more nuanced thoughts to help facilitate healing
Julie Larson, LCSW - www.julielarsonlcsw.com
• Remember your feelings will likely change day to day.
• Try not to ignore your need to share your worries, fears and questions.
• Often talking with others helps you work through concerns or uncertainties in a natural way.
• Try not to put on a “happy face” if you are not feeling that way. Your true feelings are more helpful to everyone.
• Talking about cancer can be complicated. Most conversations are not a one-shot deal, they are an ongoing dialogue.




