
In-Home Recovery Services (IHRS)
A novel, cost saving, life - saving model






A novel, cost saving, life - saving model






“A Safe Space To Share Your Story” “Create Healing From Within”



A substance use disorder (SUD) is a chronic condition and acute reactive treatment is not effective.

McLellan, A. T., Lewis, D. C., O'Brien, C. P., & Kleber, H. D. (2000). Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA, 284(13), 1689-1695 Dennis, M., & Scott, C. K. (2007). Managing addiction as a chronic condition. Addiction Science & Clinical Practice, 4(1), 45-55 McKay, J. R. (2009). Treating substance use disorders with adaptive continuing care. American Psychological Association. Bodenheimer, T., Chen, E., & Bennett, H. D. (2009). Confronting the growing burden of chronic disease: Can the U.S. health care workforce do the job? Health Affairs, 28(1), 64-74. Yach, D., Hawkes, C., Gould, C. L., & Hofman, K. J. (2004). The global burden of chronic diseases: Overcoming impediments to prevention and control. JAMA, 291(21), 2616-2622. Anderson, G. (2010). Chronic care: Making the case for ongoing care. Robert Wood Johnson Foundation. Gerteis J., Izrael, D., Deitz, D., LeRoy, L., Ricciardi, R., Miller, T., & Basu, J. (2014). Multiple chronic conditions chartbook. AHRQ Publications No, Q14-0038.


• Conservatively, 50% relapse within six months
• 60% leave treatment early, typically within 33 days. Achieving stability often requires 3-5 treatment cycles, with many requiring hospitalization due to untreated and exacerbating comorbid conditions.
Individuals with comorbid medical and SUD conditions are responsible for at least 50% of national healthcare costs.
1. STATISTICAL BRIEF #540: Concentration of Healthcare Expenditures and Selected Characteristics of Persons with High Expenses, U.S. Civilian Noninstitutionalized Population, 2019 (ahrq.gov) 2. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. Treatment Episode Data Set (TEDS): 2020 3. NIDA. 2023, March 9. Treatment and Recovery. Retrieved from https://nida.nih.gov/publications /drugs-brains-behavior-science-addiction/treatment-recovery on 2023, May 4 4. Ramo DE, Prince MA, Roesch SC, Brown SA. Variation in substance use relapse episodes among adolescents: a longitudinal investigation. J Subst Abuse Treat. 2012 Jul;43(1):44-52. doi 10.1016/j.jsat.2011.10.003. Epub 2011 Nov 22. PMID: 22112505; PMCID: PMC3408390. 5. McLellan, A. T., Lewis, D. C., O'Brien, C. P., & Kleber, H. D. (2000). Drug dependence, a chronic medical illness implications for treatment, insurance, and outcomes evaluation. JAMA, 284(13), 1689-1695 6. Chung, T., Maisto S. A., Cornelius, J. R., & Martin, C. S. (2017). Adolescents and Emerging Adults With Substance Use Disorders: Treatment Needs and Treatment Settings. In T. Chung, S. A. Maisto J. R. Cornelius, & C. S. Martin (Eds.), Treatment of Adolescent Substance Use Disorders: Translating Research into Clinical Practice (pp. 3-30). 7.Dennis, M. L., Scott, C. K., & Funk, R. (2005). The duration and correlates of addiction and treatment careers. Journal of Substance Abuse Treatment, 28(2), S51-S62. 8. Kelly JF, Greene MC, Bergman BG, White WL, Hoeppner BB. How Many
Does it Take

A holistic and cost-effective solution for SUD patients, providing comprehensive care from nursing to personal training.


The IHRS difference
• Five-year proven track record
• Full-service bundled monthly rate of only $3,200.
• Addresses the shortcomings of traditional SUD treatments
• presents a promising model for sustained recovery with integrated support.

Changes observed over the course of a year
IHRS's approach boasts a 78% completion rate over 8 months, aligning with evidence-based treatment durations favored by insurers. This means the substance use disorder and comorbid chronic conditions are managed by our team while the client learns the skill of self-care in preparation of transitioning out of the program.
Advocating for 12-month treatment, IHRS maximizes outcomes with insurers in mind.
Note on Andy’s document - still needs to be developed


Average Treatment Costs
Chronic Condition Substance Use Disorder + Other Chronic Condition
$6,032
$12,064 - $24,128

Disproportionate Healthcare Costs for the most
Prevalent High-Cost Conditions:
• Hypertension
• Osteoarthritis/Non-traumatic joint disorders
• Nervous system disorders
• Mental Disorders
• Hyperlipidemia
• Heart Disease
• Chronic Respiratory
• Diabetes


The typical patient in our IHRS program presents as follows:
DEMOGRAPHIC
• 40 years old
• Male
121 patients were admitted in 2021 ranging from 13-69 years old

PRESENTING WITH FOLLOWING CHRONIC CONDITIONS
• At least one SUD
• At least one form of diagnosed mental illness
• *40% had at least one comorbid medical condition
• 9% (or 11 of 121) struggled with somewhere between 6-11 co-occurring chronic medical conditions.
THE 5 MOST COMMON MEDICAL CONDITIONS:
• Kidney problems
• Hypertension *
• Hyperlipidemia*
• Chronic pain Diabetes* and obesity were tied
* These are conditions cited in the previous slide that are very costly to treat. Thus, many of our clients are diagnosed with conditions that are included as some of the most expensive to the nation’s healthcare costs

Individual diagnosed with opioid use disorder (OUD), anxiety disorder, and diabetes type 2, who relapses twice over a year and needs to be hospitalized on one occasion.


There were 10.7 million such Emergency Room visits for “mental and substance use disorders”
Hospitalized patients with SUDs are more likely to require resource and cost-intensive healthcare interventions and leave without completing treatment, against medical advice…Medical and surgical inpatients with substance use disorders are also more likely to return to the emergency department or be readmitted to the hospital within 30 days of discharge.
A similar study found that 63% of patients with a SUD were readmitted within 30 days of discharge and were at an increased risk of readmission for any reason/condition.


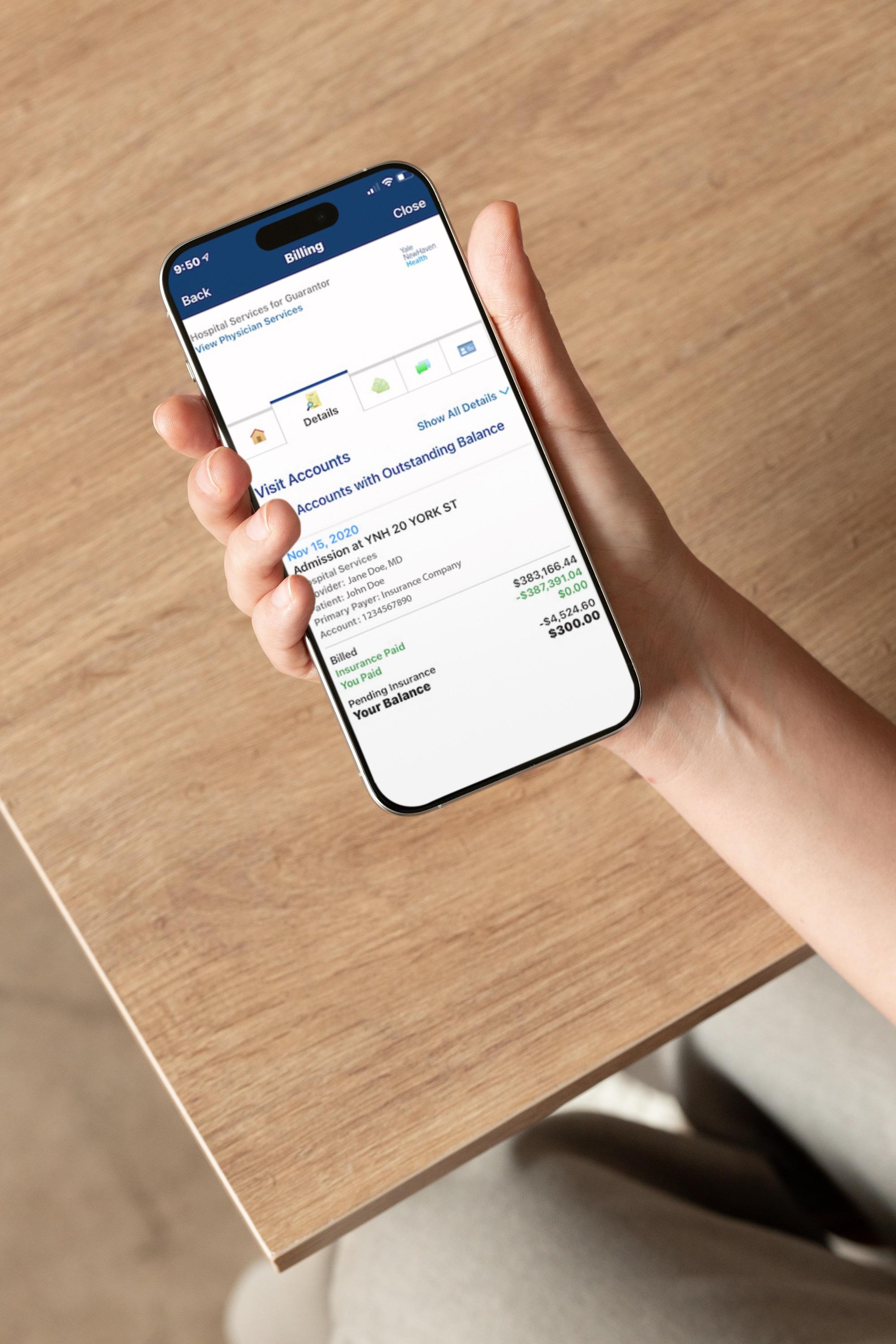

Savings: $44,992
The Cost Savings of Our Comprehensive In-Home Recovery Services
$70,592 VS $25,600
Residential Treatment, mental health counseling, medication assisted treatment, relapse, diabetes management & hospitalization: $70,592
$3,200/mo (Over the average 8 month timeline, that’s $25,600)


• Sustained reduction in substance use
• Sustained period of abstinence; decreased relapse rates
• No referrals to a higher level of care, or readmissions
• Reduction in mental illness symptoms
• Management of medical conditions
• Improved motivation to change
• Engaged in pro-recovery behaviors
(e.g. attendance at support group meetings, attending therapy, adopted regular exercise routine, etc.)


• Toxicology results
• Adherence and Retention (individuals and family)
• URICA: The University of Rhode Island Change Assessment scale.
• The McMaster Family Assessment Device (FAD)
• Quality of Life (QOL) measure
• Client Satisfaction
• Utilization Data



Toxicology Results: Breakdown of positive tests by specific substance
Between baseline and post 1-year assessment, marijuana users had an 75% reduction in positive urinalysis tests. During the same timeline, alcohol users had a 79% reduction, and opioid users had an 87% reduction in positive urinalysis tests.
These results are based on verified laboratory results provided by QUEST medical laboratories, not on in-house point-of-care results





• Hospitalizations
• Emergency room visits
• Residential programs
• Stays in Intensive Care
• Duplicative services
• Multiple relapses
• The synergistic effect that the aggravation of one chronic conditions can have on the others





• Family Therapy
• Family Support Groups
• Family Coaching
• Psychoeducational Groups for families



SUD: 303.90 (F10.20), Alcohol use disorder, Severe Psychiatric: 300.00 (F41.9), Unspecified anxiety disorder; 311 (F32.9) Unspecified depressive disorder occurring medical conditions:
Hypertension, Chronic Pain, Obesity
AT DISCHARGE
• Completed 12 months of IHRS programming.
• SUD disorder in complete remission, and abstinence from all substances
• UTOX negative for 13 panel POC urine screen with laboratory confirmation.
• 74 pound weight loss, Change in Blood pressure 134/80 to 110/68



DIAGNOSES
• SUD: 303.90 (F10.20) Alcohol use disorder, Severe, 304.30 (F12.20) Cannabis use disorder, Moderate
• Psychiatric: 300.00 (F41.9) Unspecified anxiety disorder
• Co-occurring medical conditions: Hypertension, Type 2 Diabetes,
• Chronic Pain, Obesity, Hyperlipidemia
• Prior to treatment in IHRS this patient’s insurance utilization report included 1 Hospitalization, 1 Residential treatment episode, 2 emergency rooms visits, and 70 pharmaceutical authorizations over 1 year.
AT DISCHARGE
• Completed 12 months of IHRS programming.
• All SUD disorders in complete remission, and abstinence from all substances
• UTOX negative for 13 panel POC urine screen with laboratory confirmation.
• 43-pound weight loss
• Change in Blood pressure 132/88 to 118/76, A1C 7.0 to 5.9, Chronic pain self report from 6 to 1


IHRS is a CARF Accredited Program

IHRS is a dually licensed psychiatric and substance use disorder treatment facility by the Connecticut Department of Public Health.


Andy Bucarro
Executive Director Ryan Hocking
Assistant Executive Director
Courtney Bushnell
Director of Clinical Services
Matt Gaffey Co-Director of IHRS
Antonio Piscitello Co-Director of IHRS
Maria Koslawy APRN
Kevin Coyne
Recovery Coach Diane Wright APRN



• Residential or inpatient nonhospital treatment costs can vary widely depending on factors such as the location, the specific treatment program, the duration of the treatment episode, and the services provided. There are some sources that provide cost information on residential or inpatient treatment for substance use disorders:
• According to Optum an out-of-network residential treatment episode costs $44,000, while an in-network residential program costs $13,000
• In 2017 SAMHSA’s Treatment Episode Data Set (TEDS) residential treatment costs ranged from $3,000-$12,000. 2
• According to Beetham et al. the price range for residential treatment is $5,712$17,434.3
• Finally, McCollister et al. determined that residential treatment costs for individuals with a criminal record costs $17,000. 4
• According to the National Center for Drug Abuse Statistics residential treatment (defined as existing outside the hospital system and lasting 3-6 weeks) can cost between $5,000-$80,000. 5
• Averaging these price points comes to figure of $21,414 with a range of $3,000-$80,000
1. Working to End the Opioid Epidemic (optum.com).
2. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. Treatment Episode Data Set (TEDS): 2020
23 Beetham T, Saloner B, Gaye M, Wakeman SE, Frank RG, Barnett ML. Admission Practices And Cost Of Care For Opioid Use Disorder At Residential Addiction Treatment Programs In The US. Health Aff (Millwood). 2021 Feb;40(2):317-325. doi
10.1377/hlthaff.2020.00378. PMID: 33523744; PMCID: PMC8638362.
4. McCollister, K. E., French, M. T., Prendergast, M., Wexler, H., Sacks, S., & Hall, E. (2004). Long-term cost-effectiveness of addiction treatment for criminal offenders. Justice Quarterly, 21(3), 659-679.
5. Average Cost of Drug Rehab [2023]: by Type, State & More (drugabusestatistics.org)

• According to NIDA1:
• Methadone treatment, including medication and integrated psychosocial and medical support services (assumes daily visits): $126.00 per week or $6,552.00 per year ]
• Buprenorphine for a stable patient provided in a certified OTP, including medication and twice weekly visits: $115.00 per week or $5,980.00 per year Naltrexone provided in an OTP, including drug, drug administration, and related services: $1,176.50 per month or $14,112.00 per year

• How much does the average hospitalization cost:
• According to the National Institute of Health’s Agency for Healthcare Research and Quality (AHRQ), the average cost for a hospitalization in 2017 was $12,055.1
• 2018 comparison of the costs for hospital stays AHRQ determined that individuals between the ages of 18-64 with no diabetes diagnosis stayed 4.9 days and cost $14,000. 2
• Also in 2018, AHRQ determined that the average cost for a hospital readmission was $15,200.3
• The average of these price points is $13,750
1. Hospitalizations in 2017 | Agency for Healthcare Research and Quality (ahrq.gov)
2. Diabetes-Related Inpatient Stays, 2018 #279 (ahrq.gov)
3. Overview of Clinical Conditions With Frequent and Costly Hospital Readmissions by Payer, 2018 #278 (ahrq.gov)

