




Plastic Surgery The Meeting 2025 returns to New Orleans for an unforgettable four-day summit.
Page 17



New ASPS, PSF presidents tackle questions facing the specialty
Page 7
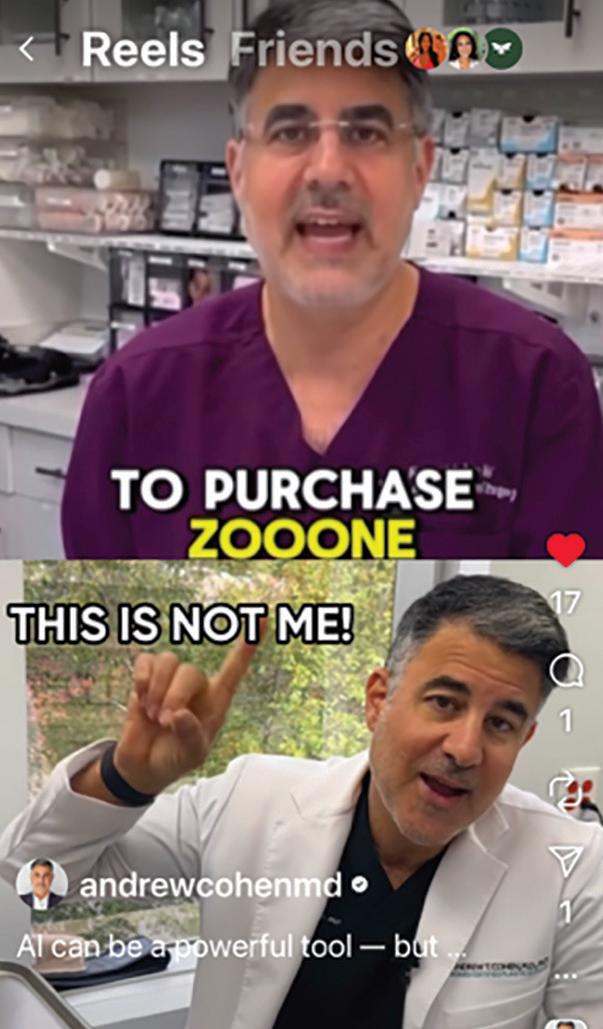
Members surprised by social media imposters
Page 8
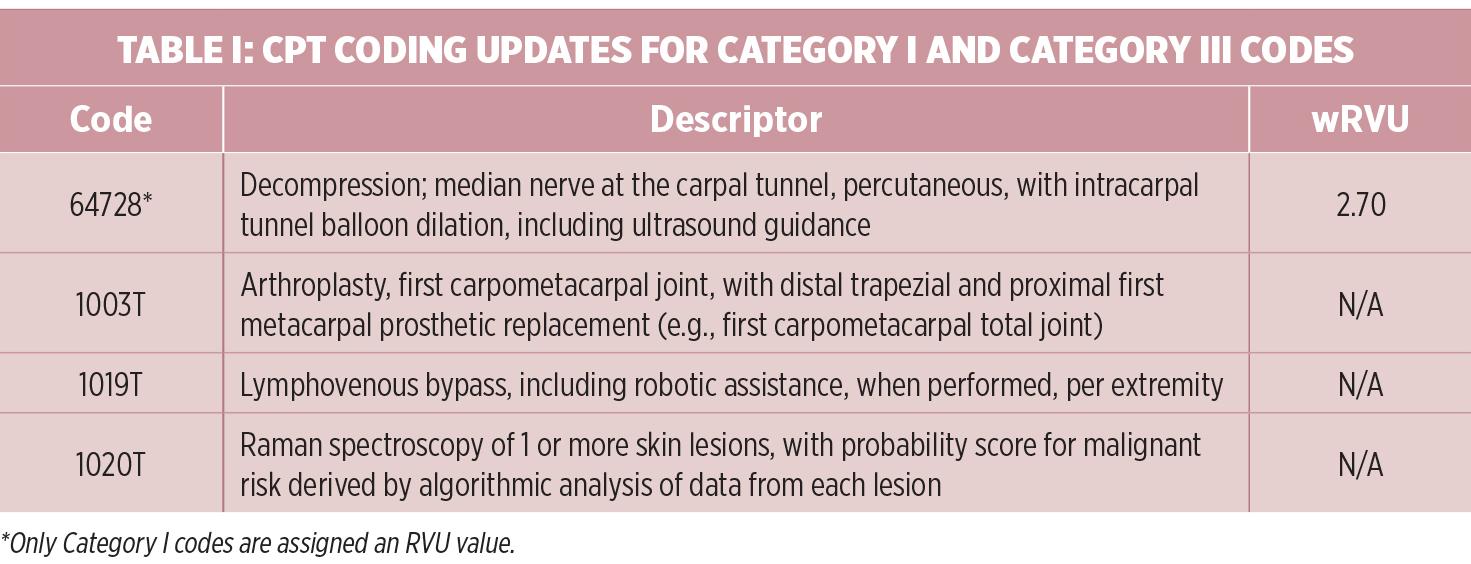
Impact of Medicare Physician Fee Schedule changes
Page 12
The ASPS Plastic Surgery Coding Workshop provides attendees with the most up-to-date coding information and specialty-specific instruction. This comprehensive learning program is a live, online interactive meeting that allows new coding professionals and those with more experience to learn accurate coding and implementation strategies from experts in the field.
This is the only ASPS Coding Workshop in 2026 and it will not be recorded. Don’t miss out! Make plans to join us virtually on March 13-14!

When
Help Address Concerns About Cost & Financing
If the patient is unsure about financing, your response could help make a difference.
“I really want this procedure, but I just don’t have room in my budget right now.”

“We want to help you look and feel your best, which is why we accept CareCredit. It’s a health, wellness and beauty credit card that includes promotional financing to help you fit the treatments and procedures you want or need into your budget. I have a QR code you can scan to see if you prequalify.”

“With the CareCredit credit card, promotional financing is available on purchases of $200 or more. If you’re approved, you can use it again and again to pay over time for additional treatments and procedures to help you maintain your look. Would you like to learn more about CareCredit or see if you prequalify?”






Handling Patients Not Yet Ready to Schedule



If the patient says they need to think about the procedure, be empathetic and have a strong follow-up plan.
Practice:
“We understand this is a big investment and you need time to think about it. Here’s the full recommendation from the doctor and more information about post-care. If cost is a concern, we have a link to the CareCredit credit card application on our site so you can apply from home. Would you mind if we followed up in a few days to address any additional questions?“
Make sure patients know CareCredit offers a way to help pay for the care they want or need. Display a window cling at your front door, stock brochures at the front desk, and place counter displays in waiting areas to highlight the CareCredit health, wellness and beauty credit card. Feature your custom QR code in your office reception area and add your custom link to your website so patients can see if they prequalify and apply easily from their mobile device.
New ASPS, PSF presidents tackle a variety of topics in annual Presidents Forum
C. Bob Basu, MD, MBA, MPH, and Babak Mehrara, MD, give their takes on issues facing plastic surgeons.
videos steal plastic surgeons’ likenesses to advertise products
ASPS member Andrew Cohen, MD, shares his surprise at finding an AI version of himself selling supplements.
Sam Hamra, MD,
Plastic surgeons pay tribute to Dr. Hamra, a pioneer in aesthetic surgery, who passed away on Oct. 1 at age 88.
WPS members reflect on the networking, education and relaxation highlights on offer at PSTM25.
for improvements in breast reconstruction
Abigail Peoples, MD, explains her research on the breast microbiome in implant-based breast reconstruction.
Big fun in the Big Easy at PSTM25
Marking several of the high points of another successful annual meeting in New Orleans.




2025 Vol. 36 No. 8
The mission of the American Society of Plastic Surgeons is to support its members in their efforts to provide the highest quality patient care and maintain professional and ethical standards through education, research and advocacy of socioeconomic and other professional activities.
ASPS PRESIDENT
C. Bob Basu, MD, MBA, MPH drbasu@basuplasticsurgery.com
CHIEF MEDICAL EDITOR
Richard Baynosa, MD richard.baynosa@unlv.edu
ASSOCIATE MEDICAL EDITORS
Paige Myers, MD, MPH paigelm@med.umich.edu
Andrew Rosenthal, MD drdrew@rosenthal-md.com
ADVERTISING EDITOR
Anu Bajaj, MD anukbajaj.mac@mac.com
EXECUTIVE VICE PRESIDENT
Michael Costelloe mcostelloe@plasticsurgery.org
STAFF VP OF COMMUNICATIONS
Mike Stokes mstokes@plasticsurgery.org
MANAGING EDITOR
Paul Snyder psnyder@plasticsurgery.org
SENIOR NEWS EDITOR
Jim Leonardo jleonardo@plasticsurgery.org
CONTRIBUTING EDITORS
Jeff Kozlow, MD, MS; Alan Matarasso, MD; Eric Payne, MD; David Schnur, MD
CONTRIBUTING WRITERS
Erika Adler; Niccole Caan; Elizabeth Gibbons; Samara Reigh; Alex Walton
COVER DESIGN
Paul Snyder
DISPLAY ADVERTISING SALES
Michelle Smith, (646) 674-6537 michelle.smith@wolterskluwer.com, Wolters Kluwer Health
CLASSIFIED ADVERTISING
Jeanne Embrey, jembrey@plasticsurgery.org
Plastic Surgery News (ISSN 1043-4119) is published eight times per year: March, June, September, December single issues – and combined January/February, April/May, July/August and October/November issues – by ASPS. Phone: (847) 228-9900; Fax: (847) 228-9131
POSTMASTER, send address changes to: ASPS Membership Department Plastic Surgery News 444 E. Algonquin Road Arlington Heights, IL 60005
Periodicals postage paid at Arlington Heights, IL, and at additional mailing offices. USPS# 508-890.
The views expressed in articles, editorials, letters and other publications published by PSN are those of the authors and do not necessarily reflect the opinions of ASPS. Acceptance of advertisements for PSN is at the sole discretion of ASPS. ASPS does not guarantee, warrant or endorse any product, program or service advertised.
2025 Subscription Rates:
Basic subscription rate: $90; for foreign subscriptions add $90 for first class service. The subscription price for PSN is included in annual membership dues. Letters, questions or comments should be addressed to: Editor, Plastic Surgery News, 444 E. Algonquin Road, Arlington Heights, IL 60005. plasticsurgery.org
By Richard Baynosa, MD PSN Chief Medical Editor
It’s an honor and a pleasure to be writing this editorial for the first time as the PSN chief medical editor. It has been a tremendous privilege to have a forum to share my thoughts with the plastic surgery community over the last four years through this periodical, which remains the specialty’s No. 1 news source and is accessible to plastic surgeons around the world.
I’d also like to extend my thanks and congratulations to B. Aviva Preminger, MD, MPH, my predecessor as PSN chief medical editor – and to our incoming associate medical editor, Andrew Rosenthal, MD. Working with Dr. Preminger over the past four years has been a tremendous experience, and I’m excited to see the amazing contributions that I know Dr. Rosenthal will bring to this publication alongside our other fantastic associate editor, Paige Myers, MD, MPH.
It’s a little-known fact that becoming a PSN medical editor (or “meditor” as we call ourselves in house) is a six-year time commitment, with four years as an associate medical editor followed by two years as the chief medical editor. For the next two years, I will be charged with writing editorials for every other issue of PSN, and as I was briefly sweating the increased deadlines, it occurred to me that few – if any – plastic surgeons reading this column (other than PSN alumni) really know what’s required during our time of service other than these editorials.
In addition to brainstorming stories for the year, reviewing stories to be included in the weekly PSN Media Update email blast and evaluating ASPS member article submissions, one of the greatest privileges we have is moderating the yearly PSN Presidents Forum,
which is featured in this month’s issue starting on page 7. The forum, held every year during Plastic Surgery The Meeting, involves four ASPS members from across the country representing academic and private practices engaging in an intimate question-and-answer session with the incoming ASPS and PSF presidents. I’ve had the honor of moderating this session three times now, and each time it has been the highlight of my year of ASPS service. Not only does this session provide a great introduction to our incoming Society and Foundation presidents, it provides a glimpse of the concerns and issues that our member surgeons have in their practices and the potential roles they see ASPS and The PSF playing in addressing these matters.
Through the years, many similar themes sprang up in these sessions, including scope-ofpractice and encroachment issues, the impact of social media and AI on the specialty, diversity and inclusion issues – as well as ever-declining insurance reimbursements and research funding. Although priorities can change from year to year, the commitment to ensuring that membership’s voice is heard by leadership continues to ring true. In fact, the one theme that remains constant for both those participating in the Presidents Forum and our readership is that we often must be reminded of just how much ASPS and The PSF does for members and the specialty at large. This is not surprising, given the sheer size of both organizations and multiple layers of structure that are inherent in their makeup. Although I’ve not served on the ASPS/PSF Board or Directors, I have nevertheless had multiple friends and mentors who’ve not only encouraged me to become more involved but also helped me to understand the structure – as well as understand the need for such a large umbrella organization for plastic surgeons.
By Paul Snyder
For the second consecutive year, ASPS bestowed Social Media Awards to members during the Annual Business Meeting held in conjunction with Plastic Surgery The Meeting 2025 in New Orleans.
“The primary goal of ASPS social media is to educate the public about the safety and efficacy of plastic surgery – and do so in a way that appeals to a broad audience,” said 2025 ASPS President Scott Hollenbeck, MD, Charlottesville, Va. “Both the Society and our members are using social media to provide engaging – and most importantly, accurate –information to help patients make informed decisions about procedures and the surgeons they consult.”
Dr. Hollenbeck and 2025 PSF President Alan Matarasso, MD, New York, honored the awardees, who were nominated by ASPS members. This year’s winners were:
• Best Use of Social Media: Educational –Elizabeth Malphrus, MD
• Best Use of Social Media: Inspirational –Rukmini Rednam, MD
• Best Use of Social Media: Representation – Rukmini Rednam, MD
A successful year recapped
Dr. Hollenbeck also highlighted the meeting’s success in returning to New Orleans and thanked the Annual Meeting Council Chair for building another a robust event for membership. This year’s annual meeting counted

3,286 total registrants and more than 200 exhibitors. Plastic Surgery The Meeting 2025 also boasted more than 100 live sessions, 92 live abstract sessions, 34 resident on-demand presentations and 74 Global Partner e-Posters on-demand, with up to 75 AMA PRA Category 1 CreditsTM provided – 25 of which were applicable to patient safety.
ASPS/PSF Vice President of Health Policy and Advocacy Lynn Damitz, MD, Chapel Hill, N.C., highlighted the Society’s efforts at the state and federal levels over the past year –looking at the work done on the AMA’s RUC and CPT processes and its continued efforts on improved coverage for breast reconstruction patients and toward the Ensuring Lasting Smiles Act.
Dr. Matarasso highlighted The Foundation’s efforts over the past year to continue pushing plastic surgery further through research grants and data collection aided by a robust registry network.
At the conclusion of the meeting, C. Bob Basu, MD, MBA, MPH, and Babak Mehrara, MD, were introduced as 2026 ASPS president and The PSF president, respectively. PSN
With increasing transparency and awareness of the structure and functions of the organizations and continuing to learn “how the sausage is made,” I’ve developed a deep appreciation and loyalty to ASPS and The PSF. I hope to share some of this with our readers over the next couple years by focusing some of my editorials on the recurrent questions that not only come up in Presidents Forums but also in many members’ minds: What is ASPS/PSF doing for me now to make my membership worthwhile, and how can I become more involved in shaping the direction of the Society?
One viewpoint that I often hear is that ASPS/ PSF is so big that the organization doesn’t have as much value as the smaller, more subspecialty-specific organizations that are more closely tailored to what each plastic surgeon does. I would counter that only focusing on subspecialty endeavors overall weakens the potential strength-in-numbers approach needed to effectively deal with so many of the recurring concerns plastic surgeons face. The fact of the matter is that when we look at issues such as scope of practice and encroachment, plastic surgery’s sheer numbers pale in comparison to nearly every other specialty that we compete with.
According to the ABMS Board Certification Report (ABMS BCR) for 2024-25, there are 9,119 board-certified plastic surgeons currently active in the United States. Compare this to the number of active board-certified diplomates in competing specialties such as dermatology (16,090), otolaryngology-head and neck surgery (16,160), ophthalmology (25,888), general surgery (45,760) and OB-GYN (52,809) –whose members not only often practice similar aesthetic and reconstructive procedures, but are also often the referring physicians.1 This doesn’t even include practitioners who are non-board certified or even non-surgical specialists who compete in the lucrative aesthetics and medical-spa spaces. Although we have, perhaps, lost too much ground in areas such as head and neck reconstruction and complex abdominal wall reconstruction to be considered the preeminent players we once were in these fields, the battle for aesthetic surgery is ongoing – and the war for breast reconstruction and non-cancer related breast surgery still looms.
The point that underscores the need to bring the consolidated unity of all plastic surgeons to bear is the market forces involved in the adoption of robotic surgery in our specialty. The global market for robotic surgery in 2025 was estimated at $80.5 billion.2 The innovation in this field is advancing rapidly, with nearly every specialty adopting new applications for this burgeoning technology. However, plastic surgeons interested in incorporating this advancement into their practice face increasing difficulty with obtaining privileges for the dominant robotic platform on the market in Intuitive’s DaVinci robotic system. Currently, the use of the DaVinci surgical robot is considered an off-label use by plastic surgeons, and there’s currently no interest by the parent company to pursue an FDA-approved on-label indication for plastic surgeons – presumably not because of a lack of interest by plastic surgeons, but likely the seemingly minor impact on the company’s market share and business growth.
This might not seem like a tremendous issue for plastic surgeons, given that we have advanced patient care through adoption of new devices and biomaterials – sometimes ahead of formal labeling. Nevertheless, the unique control that manufacturers exert over robotic surgery certification, and therefore the credentialing and privileging process, creates an unusual barrier to surgical innovation.
As individual plastic surgeons at our hospitals, this is a nearly insurmountable obstacle to adoption and innovation for our practices – but the ASPS Robotic Steering Committee under the Society’s Technology, Innovation, Disruption and Entrepreneurship Committee is actively working on a certificate of robotic training pathway for both active practitioners and trainees, similar to how urologists first developed robotic training pathways through the American Urological Association (AUA) in 2012.3 Urologists are now perhaps the dominant specialty in the utilization of robotic techniques due not only to their innovation and progressive thinking, but also to the advocacy and unity provided by their society in the AUA. Indeed, the number of active board-certified urologists per the ABMS BCR is only slightly more than plastic surgeons at 12,102, but still well below all the previously cited surgical specialties.
Given the increasing competition and innovative robotic platforms that have or will be coming to market – including the Symani and MUSA for microsurgery, Versius and Hugo for minimally invasive surgery and plastic surgery-specific robots such as the craniofacial robot and the Artas robot for hair restoration – it’s only a matter of time before the technology has touched and potentially disrupted every subspecialty of plastic surgery. With the inherently innovative nature of plastic surgeons combined with the overwhelming support, resources and advocacy of ASPS and The PSF, I have no doubt that plastic surgeons can rise to similar heights that urologists have in the realm of robotic surgery and beyond.
With those resources and our continued advocacy, I can see many potential strengths of our Society and Foundation – and I hope that I am able to convince you of many others in the next two years. I also want to encourage all plastic surgeons to become more involved in ASPS and The PSF in order to actively help address the issues and concerns that we all see as challenges affecting not only ourselves but our colleagues.
I believe the reason to be active members of our organization was best said by President Teddy Roosevelt in his inspirational “The Man (Woman) in the Arena” speech:
“It is not the critic who counts, not the man who points out how the strong man stumbles or where the doer of deeds could have done them better,” he said. “The credit belongs to the man who is actually in the arena, whose face is marred by dust and sweat and blood; who strives valiantly; who errs, who comes short again and again, because there is no effort without error and shortcoming; but who does actually strive to do the deeds; who knows the great enthusiasms, the great devotions; who spends himself in a worthy cause; who at the best knows in the end the triumph of high achievement, and who at the worst, if he fails, at least fails while daring greatly, so that his place shall never be with those cold and timid souls who neither know victory nor defeat.” PSN
References
1. American Board of Medical Specialties (2025). ABMS Board Certification Report 2024-2025. abms.org/abms-board-certificationreport/
2. Trishita Deb. Market.us Media (Jan. 13, 2025). Robotic Surgery Statistics 2025 By – Procedures, Safety, Complications. media.market.us/ robotic-surgery-statistics
3. Urology Times (Jan. 1, 2012). American Urological Association Outlines Framework for Robotic Surgery Credentialing. urologytimes.com/view/american-urologicalassociation-outlines-framework-roboticsurgery-credentialing
By Paul Snyder
In their final hours before taking office, ASPS
President C. Bob Basu, MD, MBA, MPH, Houston, and PSF President Babak Mehrara, MD, New York, shared their positions on an array of topics ranging from the Society’s work on scope-of-practice battles and member engagement to research funding and the transformative power of AI during the 35th annual PSN Presidents Forum held at Plastic Surgery The Meeting in New Orleans
The forum provides the Society’s incoming leaders an opportunity to field a broad range of questions from a diverse group of plastic surgeons. PSN Chief Medical Editor Richard Baynosa, MD, Las Vegas, served as moderator.
The ASPS members invited to participate in the forum were Alison Snyder-Warwick, MD, Ann Arbor, Mich.; Neil Tanna, MD, Great Neck, N.Y.; Raj Vyas, MD, Orange, Calif.; and Diana Yoon-Schwartz, MD, PhD, Huntington, N.Y. The following is an edited transcript of the discussion.
Dr. Snyder-Warwick: What inspired you to pursue these leadership roles and what do you want to accomplish this year?
Dr. Basu: One of my mentors taught me that “academic plastic surgery is a state of mind, it’s much more than just a job title.” As a private practitioner, I found my academic home in ASPS through service on different committees and task forces. These experiences allowed me to meaningfully impact our specialty far beyond the walls of my own practice, and organized plastic surgery has become a cornerstone of my professional life.
I want our members to see that this is no longer your parents’ ASPS. We are entering a new era. I look forward to leading efforts to modernize the way ASPS communicates, engages and delivers information to both our members and external stakeholders – including patients, consumers, policymakers and the public. We are laser-focused on optimizing membership value. A key part of this strategy is judiciously embracing innovation and AI. ASPS is actively developing a new, externally facing website for the more than 10 million unique public visitors we receive each year. Our goal is to more effectively channel this traffic to our members’ practices using CRM tools, analytics and, eventually, AI-powered systems that help members meaningfully engage with potential patient inquiries.
really good feedback, learn some hard lessons and get the seed funding that I needed to then go on to get NIH grants – which are becoming increasingly hard to get. I think The PSF is the area where I can make the most difference.
My goals are to modernize the way we review grants and the way applicants write them. The review process hasn’t changed in the last 25 years. Grants are sent to two or three reviewers – some reviewers have a lot of experience, others don’t – and then you get mixed feedback from that. We have almost 20 years’ worth of grants that have been annotated and graded by PSF reviewers. Having that in an AI format would be helpful to providing feedback and, essentially, screen grants and make the review

and The PSF ensure that membership in the Society is relevant and delivers value for private and academic members?
Dr. Basu: Membership value is absolutely essential, and I believe ASPS can do a much better job communicating our value proposition. Simply put: What is ASPS doing for you? We’re fortunate that ASPS has a strong financial foundation, and that strength allows us to do many things other organizations simply don’t have the resources, staff or infrastructure to support. Given our size, ASPS also has critical touchpoints across nearly every facet of our specialty. That reach and positioning matter. At both the state and federal levels, ASPS is a recognized and respected voice. As our position grows stronger, our voice grows louder

end of the day, we’re the last true general surgeons. We operate from head to toe, we operate on patients of all ages – and that’s why we see creep enter into the specialty. Other societies and specialties have seen their bases shrink. General surgeons now primarily do gallbladders, hernia repairs and appendectomies – and they’re looking for a way to expand. How do you prevent that? You need advocacy at a big level – not at the level that a small subspecialty society can provide, but as a united voice from all plastic surgeons. We need to be able to make it clear that plastic surgeons do these operations and that we have the requisite training to do them correctly. .
Dr. Yoon-Schwartz: We’re a small group of professionals with shared goals and interests. How do we protect our specialty without alienating some of the key providers or specialties with which we share some of the same goals and initiatives?
Dr. Basu: We protect our specialty by staying true to who we are and to our core values. ASPS always speaks to the vital importance and value of a board-certified plastic surgeon in patient care, whether reconstructive or cosmetic. That principle is non-negotiable, and it provides a foundation for collaboration with other medical professionals who share our commitment to patient safety and high standards. Over more than two decades representing plastic surgery at the AMA, I’ve learned that building productive, respectful relationships with other specialties is critical. When we focus on areas of alignment – ethical practice, quality of care, patient safety – we can work together while still clearly defining the unique training and capabilities that distinguish our specialty.

(Clockwise from top) ASPS President C. Bob Basu, MD, MBA, MPH, shares his thoughts during the 2025 PSN Presidents Forum; The PSF President Babak Mehrara, MD, answers a question; and (left to right) Neil Tanna, MD, Alison Snyder-Warwick, MD, Diana Yoon-Schwartz, MD, PhD, Raj Vyas, MD, PSN Chief Medical Editor Richard Baynosa, MD, Dr. Basu and Dr. Mehrara trade insights during the 35th annual forum.
At the same time, we are transforming our member-facing digital infrastructure. As we hear more about personalized medicine, ASPS is moving toward personalized membership. Our members represent the full breadth of plastic surgery, with diverse interests and professional priorities. Through thoughtful digital design, we can tailor the member website and app to deliver a more customized experience, giving each member the content, tools and resources most relevant to their practice and passion.
Finally, I know our members remain deeply concerned about scope-of-practice challenges. ASPS must continue to be proactive in defending patient safety and our specialty. I firmly believe that a strong offense is the best defense, and I look forward to working with our ASPS team to take a more assertive and strategic posture in protecting the integrity of plastic surgery.
Dr. Mehrara: My decision to pursue this leadership role was based largely around my experience with ASPS. The PSF has been an area where I was able to secure grants, initially, get
process easier. We’d be able to help people overcome a lot of early mistakes – overlapping aims, overly ambitious projects, rationale is not well stated, etc. Another big goal is to operationalize some of our registry data. We now have almost 100,000 procedures in GRAFT, and large datasets in NBIR and TOPS. I want to utilize the power of those datasets to their full extent.
I also want to try to identify new funding sources for The PSF. Historically, we’ve relied on member contributions, but as our membership ages and financial constraints become more problematic, it would be nice to find additional sources. Perhaps we can collaborate with device or drug companies to have an RFA for a particular project that they’re interested in. That way, grant money would come through The PSF, the researchers get the funding – and they don’t have to get the funding directly from the company. It answers the clinical questions that companies are interested in, it helps our researchers do work that’s clinically relevant and important – and it also removes the sort of “blemish” of it being industry-sponsored research.
Dr. Tanna: A lot of subspecialty societies are competing for our attention. How will ASPS
– and our ability to deliver meaningful impact for our members and patients grows with it. I encourage our members to join other plastic surgery organizations in addition to ASPS. When our sister organizations thrive, it raises the bar for the entire speciality. Supporting the whole specialty is central to the ASPS mission. I often remind colleagues that we share a common heritage: We are all plastic surgeons first. Our specialty is uniquely interconnected. As an aesthetic surgeon, why do I go to Washington to advocate for the Ensuring Lasting Smiles Act, which focuses on congenital and pediatric care? Because it reflects our shared foundation. Even in my deep-plane facelift work, I’m drawing on principles I learned during craniofacial training. That heritage sets plastic surgery apart.
At a time when non-plastic surgeons and “wannabes” continue to expand into aesthetic and reconstructive spaces, standing together is more important than ever. ASPS is committed to fostering collaboration across subspecialties so that we speak with one strong, unified voice – for our patients, our practices and the future of plastic surgery.
Dr. Mehrara: ASPS is your advocate. At the
I am increasingly concerned with scope-of-practice expansion from non-plastic surgeons and unqualified providers. It feels like a “whack-a-mole” landscape: As soon as one scope challenge is resolved, two more emerge. I wish I had the cure-all solution, but I don’t. We must remain continuously engaged with the public, policymakers and regulatory bodies at both the state and federal levels. Unfortunately, given decreasing reimbursements, I believe scope creep will continue to intensify. That’s why it is essential that we speak louder, more often and more directly – not only to legislators and stakeholders, but to the public itself. When patients understand the difference in training and experience, they make safer choices.
Dr. Mehrara: The most important thing is to listen to members, understand what they need then do as much as we can. You can’t please everyone as a leader. You need to make tough choices. Hopefully we can provide a little space between us and general surgery. As a Society, it’s important for us to think about how we’ve always been part of general surgery – and how that prevents us from being at a table when the chairs are sitting and discussing privileges. We’re not there. There are some plastic surgery departments in this country, but most are still divisions. I think bringing ourselves together as plastic surgeons – uniting and becoming an actual department that can stand up for our values and what we think is important – will play an important role in our efforts to fight creep. Credentialing in hospitals is still regulated at the departmental level. If we’re considered to be under the department of general surgery, we don’t have a voice in that. If breast surgeons want to start doing breast reconstruction, they’ll get breast reconstruction, and we won’t
By Paul Snyder
As AI technology advances, plastic surgeons are finding myriad benefits for streamlined processes and increasingly expedited ways to gather and process information. Unfortunately, some plastic surgeons are also learning – through no fault of their own – some of the downsides of the technology.
ASPS member Andrew Cohen, MD, Encino, Calif., says he was surprised in late October to find a Facebook message on his phone from a nurse he worked with several years ago.
“The message just said, ‘Do you really promote this company?’ and it had a link attached,” Dr. Cohen recalls. “My first thought is not to click because I’m careful about opening suspicious links, but it came from someone I trusted.”
When he opened the link, Dr. Cohen watched a video of himself – or someone who looked vaguely similar (“I mean, come on – I think I’m better looking than this guy,” he notes) claiming to be Dr. Cohen and selling supplements.
“I said, ‘That’s not me – you know me, I would never do this,’ and she replied, ‘Well it’s a good hack because it even sounds like your voice,’ ” Dr. Cohen says. “But if you look closely, it’s not my name on the scrubs. It’s an AI-generated fake.”
TDr. Cohen says he tried to uncover information on the company that posted the video, which he found to be based in Greece. He went to the company’s Yelp page and left a bad review, saying they’d stolen his identity to make a fake video. He also posted a video on his own social media channels (with a split screen of the fake video) and explained how it was not him – encouraging patients to schedule Zoom and in-person consults with him to ensure they know who they’re working with.
“I’m a board-certified plastic surgeon who’s interested in the best patient care and education – I’m not and would not ever be selling supplements,” he tells PSN. “But it’s the Wild West out there and other plastic surgeons got in touch with me to say similar things had happened to them.”
With AI software able to capture both visual and audio representations of doctors who’ve posted videos online, the possibilities not only exist for nefarious players to create fake videos of doctors “advertising” any number of questionable products – they’re beginning to spread online. Although some might be more convincing than others, the ethical and reputational hits these videos can cause are not lost on the victims.
Richard Cahill, JD, vice president and general counsel for The Doctors Company, says plastic surgeons might have some recourse in re-
sponding to these imposter accounts and videos, but the international origins of some accounts and AI-generated videos can muddy the waters.

“Ordinarily we’d recommend that the physician have corporate counsel send a letter to the account holder who posted the fraudulent ad demanding that it be taken down immediately or that the physician will consider pursuing all available legal remedies,” Dr. Cahill tells PSN. “However, if the posting individual is in another country, that threat probably won’t do much. Another suggestion might be to have an office manager post on the same site that the physician’s name, image and likeness have not been authorized, and that the physician does not in any way endorse the product identified.”
In addition to contacting the company and account that posted the fake videos, ASPS past President Steven Williams, MD, says that plastic surgeons who find themselves victims of these scams should also notify the social media channels hosting the content.
“These companies are using your likeness to validate a product because you’re a physician and occupy some part of the public space,” he notes. “If a patient uses the product based on what they think is your endorsement and is hurt, that’s very harmful – and very serious. Social media tends to be sensitive to matters of identity theft – particularly if it involves a physician – because there is a liability issue there. So members should always try to contact Facebook, TikTok, Instagram or whatever platform is being used to share these videos.”
he ASPS/PSF Board of Directors in October finalized the election of the 2026 Nominating Committee. The committee’s roster for 2026 is as follows:







Scott Hollenbeck, MD
Co-Chair, ASPS Immediate-Past President University of Virginia Charlottesville, Va.
Alan Matarasso, MD Co-Chair, The PSF Immediate-Past President Private Practice New York
J. Brian Boyd, MD West Regional Representative Private Practice Rolling Hills Estates, Calif.
Jared Davis, MD Southwest Regional Representative University of Mississippi Medical Center Jackson, Miss.
Daniel Freet, MD Member Sections Representative University of Iowa Iowa City, Iowa
Caroline Glicksman, MD, MSJ Northeast Regional Representative Solo Practice Sea Girt, N.J.
Matthew Greives, MD, MS State and Regional Societies Representative University of Texas Health Houston
Daniel Krochmal, MD Midwest Regional Representative Solo Practice Hinsdale, Ill.
Delora Mount, MD Southeast Regional Representative University of North Carolina Chapel Hill, N.C.


Gary Smotrich, MD Trustees Representative Lawrenceville Plastic Surgery Lawrenceville, N.J.

Gregory Swank, MD Presidential Line Representative Multi-Specialty Group Practice Hickory, N.C.

Victoria Vastine, MD Member Sections Representative Employed Physician Charlottesville, Va.

Steven Williams, MD Carryover Member (ASPS) Tri Valley Plastic Surgery Dublin, Calif.

Prospective candidates interested in applying for a position under the Nominating Committee’s purview should know that the Candidate Conduct Policy strictly prohibits candidates from contacting any member of the Nominating Committee throughout the nominating process. Questions or concerns about the process should be directed to Louise Pereyra, the Nominating Committee staff liaison, at lpereyra@plasticsurgery.org PSN
Dr. Cohen says that, as of press time, he’s unaware of any other videos that use his likeness floating around social media – and that he hopes his quick response put an end to it. However, with not only the proliferation of AI technology, but how quickly it’s evolving to make video appear more realistic, he says it’s likely other plastic surgeons will need to keep an eye on their own likeness in the near future.
“It’s just another thing we’re going to have to deal with, unfortunately,” he says. “I know we don’t know how to fight back against this yet –but at least having the knowledge that this kind of thing can and does happen is a start.” PSN
ASPS is calling on its members and their patients to share stories of breast reconstruction insurance denials. The recently introduced Advancing Women’s Health Coverage Act, led by Rep. Kat Cammack (R-Fla.) and bipartisan cosponsors, would strengthen the Women’s Health and Cancer Rights Act of 1998 to close insurance gaps and expand access to modern reconstructive care. Surgeons and patients can support this legislation by sharing their stories. Learn more about the Society’s progress on this effort – and submit your stories at plasticsurgery.org/awhca. PSN

By Joseph McCarthy, MD
Our friend and colleague, Sam Hamra, MD, died in his home in Dallas on Oct. 1. He was 88.
Sam was born and raised in Oklahoma, the son of Lebanese immigrants. He grew up in a tight-knit family surrounded by many relatives. He especially admired his father, a caring patriarch who imparted his values of hard work and integrity to Sam and his sister. His background fostered a lifelong affection for Lebanon and resulted in many trips to his ancestral home.
Sam received his undergraduate degree from the University of Oklahoma in 1959, where he also served as class president. He continued at the same institution for his medical degree and also later completed a five-year general surgery residency. Not unexpectedly, he was a lifelong Sooner and nothing made his weekend more wonderful than a Saturday football victory.
A fellowship at the University of Lausanne, Switzerland, introduced him not only to the excitement of international travel but, more importantly, to the rewards that come from interchange with surgeons from other countries. With his perspective expanded, Sam developed his lifelong interest in facial anatomy and recognized the great possibilities of plastic surgery. Fluent in French, he enjoyed his European travels to the fullest.
He satisfied his military obligation as a U.S.
Air Force medical officer in California and in Libya, where he witnessed the coup led by Muammar Gaddafi in 1969. One of his favorite stories was the sudden disappearance of the Mercedes limousines, which was the first visible clue of the coup. After a few weeks, they returned to the streets, the only occupants, the military victors.
Sam’s next stop was a three-year residency at the NYU Institute of Reconstructive Plastic Surgery. The chief of plastic surgery there, John Marquis Converse, MD, and Sam got along famously. Both were unabashed Francophiles and enjoyed an international lifestyle. It was an historic experience to be in training in the 1970s, as it was a period of incredible innovation and growth in plastic surgery. I was honored to be part of the 1973 graduating class with Sam, along with Henry Kawamoto, MD, DDS, and Brunno Ristow, MD.
Sam’s New York experience also ended his years as a bachelor enjoying the social life of Manhattan. He met the love of his life, Sonia Amal Younis, a talented jewelry designer at Tiffany & Co. They married in 1973 in Jamaica. In their 52 years of marriage, they traveled extensively and had two sons, Andrew and Taylor, and two grandsons, Wyatt and Quinn. It was rare to see a presentation by Sam without the ever-gracious Sonia in the audience.
Following residency, Sam moved to Dallas to join the practice of Mark Lemmon, MD.
Sam’s legacy transcends plastic surgery, extending to his family and heritage in Dallas, the art world, international travel organizations, the University of Oklahoma and the countless other spheres he touched.
He trained in plastic surgery at NYU during a remarkable era – one in which its residents and Fellows routinely went onto distinguished careers across every dimension of the specialty. The program’s graduates went on to establish themselves in cities across the United States and around the world, forming a generation-spanning network of NYU-trained leaders whose careers shaped the specialty. Sam emerged from this environment just as aesthetic surgery was gaining legitimacy as a serious academic discipline and integral component of our specialty.
Sam became synonymous with the development and refinement of the composite and deep-plane approaches to facial rejuvenation. His contributions extended beyond the face, making advances in eyelid surgery, rhinoplasty and body contouring – always marked by a willingness to challenge prevailing assumptions and refine established concepts.
Above all, Sam was a teacher, mentor, colleague and friend to generations of plastic surgeons. His influence endures through the surgeons he trained, the advancements he made and the countless patient lives he enhanced through his integrity and vision.
– Alan Matarasso, MD ASPS Past President and The PSF Immediate-Past President New York
Many of us who trained in Dallas had the honor and privilege of learning from Dr. Hamra – both in the operating room and in the conference room. He was an extraordinary fountain of knowledge, gifted with the rare ability to make even the most complex concepts clear, logical and accessible. His surgical results spoke volumes, setting a standard that inspired all who witnessed his work.
Dr. Hamra’s contributions to plastic surgery are profound and enduring. His influence extends far beyond those fortunate enough to have trained directly under him, reaching countless others who studied his landmark publications and his seminal book. His wisdom, innovation and artistry left an indelible mark on our field – and, fittingly, his influence (and his patients) remain truly ageless.
– Jeffrey Janis, MD
ASPS
Past President Columbus, Ohio
We grieve the passing of an extraordinary plastic surgeon whose limitless energy and enthusiasm touched and uplifted colleagues, trainees and patients across the globe for decades. He gave his knowledge freely and with great passion, leaving a legacy on our specialty and on all who were fortunate to learn from him.
– Jeffrey Kenkel, MD
The Aesthetic Society Past President Dallas

As a resident, Sam developed a keen interest in the complexities of facial anatomy. He also had become dissatisfied with the results of the subcutaneous facelift as practiced at the time. He first adopted many of the principles of the facelift procedure advocated by Tord Skoog, MD, of Sweden, and with Dr. Lemmon he reported a series of facelifts using the Skoog technique.
However, he continued to be disappointed with his results – and with his inability to restore what he called “facial harmony.” He not

only focused on the deeper layers of the facial soft tissues but also recognized their changes with aging. In rapid succession he published classic papers: “Deep Plane Rhytidectomy” (1990), “Composite Facelift” (1992) and “Lower Eyelid Repositioning” (1995). These papers, among the most cited in the plastic surgery literature, jolted the world of aesthetic plastic surgery. They represented a paradigm shift in surgical technique but also generated considerable controversy.
Sam presented his work in the United States and abroad. A force of nature, he was ever eager to express his opinion and engage with those who did not embrace his techniques. Panel discussions with Sam and his critics often took an air of high drama. He was direct and honest – and had little tolerance for colleagues who clung to dogma. He was an indefatigable teacher and maintained an extensive international lecture schedule. For more than 40 years, he also generously welcomed visitors who had made a pilgrimage to his O.R.s in Dallas.
To his friends, Sam was always good company. His sense of friendship was boundless. He especially enjoyed sitting down to dinner and regaling friends with tales of his family, his travels and his political views. He often expressed his gratitude that he was a plastic surgeon and felt strongly about teaching and advancing the techniques of his chosen profession.
Sam Hamra will be remembered as a surgeon who worked tirelessly to improve patient outcomes and whose commitment to education knew no bounds. He was an innovative surgeon who made a lasting imprint on the standards of plastic surgery care. He will be sorely missed by his family, friends and colleagues. PSN

“CPT Corner” provides general information, available at the time of publication, regarding various coding, billing and claims issues of interest to plastic surgeons. ASPS is not responsible for any action taken in reliance on the information contained in this column.
By Jeff Kozlow, MD, MS; David Schnur, MD; Eric Payne, MD; & Erika Adler
The CPT code set is reviewed and updated each year in an effort to remain aligned with the latest medical practices and technologies. These annual revisions – which include introducing new codes, revising existing ones and retiring outdated codes – ensure accurate reporting, appropriate reimbursement and alignment with modern healthcare delivery.
Staying up to date with these changes is crucial for plastic surgeons to ensure compliance and accuracy in medical coding. For 2026, there are 418 notable updates to the CPT codes set, including 288 new codes added, 84 deletions and 46 revisions. The updated CPT 2026 code set was released Sept. 9, with new Category I codes scheduled to take effect on Jan. 1, 2026.
Percutaneous Release of Carpal Tunnel – A new Category I code, 64728, has been established to report decompression of the median nerve at the carpal tunnel percutaneously.
Percutaneous carpal tunnel release is an alternative to and distinct from traditional endoscopic or open surgical approaches. Real-time ultrasound guidance allows preoperative visualization to assess the critical anatomy, and it provides intraoperative visualization of all critical anatomy – as well as precise navigation and placement of a single-use device with integrated inflatable balloons. Intracarpal tunnel balloon dilation is included in this procedure; this allows the physician to create additional space to protect all critical anatomy and visually confirm proper device placement prior to transecting the transverse carpal ligament to decompress the median nerve.
An exclusionary parenthetical note has been
added to restrict the reporting of code 64728 in conjunction with codes 29848, 64721, 76942 and 76998. In addition, the current exclusionary parenthetical note in this code family has been revised to restrict the reporting of code 64728 with code 11960
Unlike the other codes used to report other carpal tunnel procedures, code 64728 has a 0-day global period and is valued only for the day of service. Subsequent post-procedure visits would be reported with the standard established patient E&M codes (99211-99215) since this care would be outside of the 0-day global period.
Surgery Guidelines – A new subsection has been added to the surgery guidelines to alleviate confusion about the work of harvesting a graft in codes that include obtaining the graft. Within this section, a guideline has been added to clarify that the codes include procuring the graft from the patient during the same operative session. For example, code 21154 Reconstruction midface, LeFort III extracranial), any type, requiring bone grafts (includes obtaining autografts); without LeFort I states it includes obtaining autografts. To clarify, this means that the autografts are obtained from the patient during the same operative session.
Category III CPT
It’s important to note that Category III codes are intended for data collection on emerging technology or services and they may not yet be widely covered by payers and do not have

On Oct. 15, the Monmouth Society of Plastic Surgeons celebrated its 21st annual educational meeting. It was held at Buona Serra in Red Bank, N.J., and sponsored by Revance. Steve Sanabria, representing Revance, presented updates on new injectables. In attendance were Alan Zaccaria, MD, the society’s founding president, and A.K. Bhattacharya, MD, the society’s acting president. The society is open to all ASPS members and plastic surgery residents in the New Jersey, New York and Pennsylvania regions. It sponsors eight educational dinner programs per year. In addition to the evening’s educational presentation, updates are presented concerning any issues in plastic surgery from the regional medical centers, along with the New Jersey Society of Plastic Surgeons. Any surgeons interested in obtaining additional information should email Dr. Bhattacharya at mosum@aol.com or immediate-past President Stephen Chidyllo, MD, DDS, at sachidyllomd@gmail.com. PSN
assigned RVUs (work value units) in the same way Category I codes do, meaning reimbursement and payer recognition can vary widely. Even though a code is listed, coverage is not guaranteed. It’s strongly advisable to verify with individual payers ahead of time (especially Medicare/Medicaid and private insurers) whether they will accept the code and what documentation may be required.
Carpometacarpal Joint Prosthetic Arthroplasty – CPT code 1003T is a new Category III code for 2026. This code is designated for reporting placement of a distal trapezial and proximal first metacarpal prosthetic replacement (e.g., first carpometacarpal total joint), a surgical intervention aimed at treating arthritis or other degenerative conditions affecting the first carpometacarpal (CMC) joint, commonly known as the basilar joint. Table I outlines the new Category I and III codes.
Lymphovenous Bypass – A new Category III code, 1019T for lymphovenous bypass, has been established. This code is designated for reporting lymphovenous bypass procedures, which are advanced microsurgical techniques aimed at treating lymphedema and other lymphatic disorders. These procedures involve lymphovenous anastomosis, facilitating the rerouting of lymphatic fluid from obstructed or damaged lymphatic vessels to nearby veins. An exclusionary parenthetical was added to indicate that 1019T should not be reported in conjunction with 38308, 38790, 38900 or 69990. Category III code 1019T will be active only in 2026 as better-defined Category I codes for microvascular lymphovenous bypass surgery have been created through the CPT process for 2027, with concurrent deletion of the above-mentioned Category III code.
Raman Spectroscopy of Skin Lesion – CPT code 1020T is a new Category III code designated for the Raman spectroscopy of one or more skin lesions. Specifically, it’s intended to report the use of Raman spectroscopy technology, which utilizes laser-induced light scattering to analyze the molecular composition of skin tissue – aiding in the assessment and diagnosis of skin lesions. This technology is a tool for distinguishing between malignant and benign skin lesions without the need for invasive procedures.
For the fiscal year that began Oct.1, a total of 487 new ICD-10-CM codes have been added. In addition, 38 existing codes were revised and 28 codes were deleted, reflecting updates to improve specificity and accuracy in medical documentation. These codes are effective for patient encounters and discharges from Oct. 1, 2025, through Sept. 30, 2026, ensuring compliance with the latest ICD-10-CM coding standards.
Chapter 12 – Diseases of the Skin and Subcutaneous Tissue includes new codes for cutaneous abscess of flank, as well as new codes for non-pressure chronic ulcers based on anatomic area.
Chapter 19 – Injury, Poisoning and Certain Other Consequences of External Causes introduces more than 200 new codes that provide greater anatomic and clinical detail for injuries – such as specifying depth and laterality, and whether penetration occurred in areas such as the abdominal wall, flank and groin. These refinements improve the accuracy of documenting trauma, wound complexity and complications. For plastic surgeons, the expanded specificity is especially important for linking reconstructive and repair procedures to the underlying injury or condition, ensuring proper reimbursement, reducing claim denials and enhancing data quality for outcomes reporting and research. The updates also strengthen the ability to capture postoperative complications and external causes, supporting more precise clinical documentation and quality metrics in reconstructive and trauma care.
For calendar year 2026, CMS will now have two distinct Physician Fee Schedule (PFS) conversion factors. For clinicians participating in qualifying advanced alternative payment models (APMs), the conversion factor will increase to $33.57 – an increase of approximately 3.77 percent (or +$1.22 per RVU) from the current factor of $32.35.
For clinicians not participating in qualifying APMs, the conversion factor will increase to $33.40 – a projected increase of about 3.26 percent (or +$1.05 per RVU) over the current factor of $32.35.
These increases are driven by three components: a statutory update under Medicare Access and CHIP Reauthorization Act of +0.75 percent for APM participants / +0.25 percent for others; a one-year +2.5 percent adjustment included in recent legislation; and an estimated +0.55 percent offset tied to work RVU changes. However, there are also two very notable changes from CMS that will result in decreased payment for many plastic and reconstructive surgery services.
First, CMS has finalized an “efficiency adjustment” (-2.5 percent applied to the work RVU component of non–time-based services) starting in CY 2026. The efficiency adjustment is being applied to essentially all surgical, procedural and radiology services. This adjustment is based on the assumption that there have been efficiencies in time and intensity for most procedures that lead to persistent over-valuation of these services. This adjustment was not applied to time-based services including E&M, behavioral health or global maternal-care services. There was significant opposition from many societies – including ASPS – to this faulty efficiency adjustment; however, CMS opted to enact this change. The Society will continue to fight against these changes, but implementation is still set by CMS for Jan. 1.
Second, CMS finalized changes to the allocation of indirect practice expense physician costs (e.g., clinic staff time) moving physician reimbursement dollars from when services are provided in a facility (e.g., hospital, ASC) to when the services are provided in a non-facility (e.g., clinic). This change is intended to address concerns about overpayment of practice expense for duplicated services. Although this will, in part, better support a private practice model, it will significantly decrease physician payment for when services are provided in a facility, with estimates between 7-10 percent when combined with other elements of the final rule.
Although we’re still analyzing the final rule at this article’s press time, an upcoming follow-up article will explain these changes in more detail and assess their impact on our specialty. PSN
A Curriculum for Plastic Surgery: A Cognitive and Care-Based Approach, Vols. I
By Edward Luce, MD Springer, 2025
Many years ago, my father gave me a mantra for success: “Fill a void.” It seems ASPS and The PSF past President Edward Luce, MD, must have received the same advice, as his upcoming publication, A Curriculum for Plastic Surgery: A Cognitive and Case-Based Approach, does just that.
As plastic surgeons, we all received an educational experience based on learning how to provide the very best patient care. Although this allowed each of us to practice as plastic surgeons, it fell far short for those of us who decided to play a role in the education of medical students, residents and Fellows. Simply put, we were trained as plastic surgeons – not as plastic surgery educators. Additionally, with few among our ranks trained as educators, there were limited opportunities to raise our game and learn how to properly teach our trainees. Dr. Luce, in contradistinction to many of us, distinguished himself as a surgeon intent on learning all he could about the education of others. In this 1,300-page textbook, he gives readers the opportunity to appreciate what he learned during a career spanning more than four decades.
In the book’s introduction, Dr. Luce contrasts the current system of surgical resident education (“Where Are We Now”) with his concept of ideal surgical education (“Where Should We Be”). This section of the book alone is worth the price of admission with the author’s treatise on adult learning principles – many of which are generally not taught at plastic surgery meetings. A surgeon interested in learning these principles would likely have to attend either the ACGME meeting or the Canadian International Congress of Resident Education meeting. Dr. Luce saves the reader a trip and then some.
After covering adult learning principles, Dr. Luce focuses on several educational innovations, particularly endorsing the the “flipped classroom” technique, which has the student come to lecture fully prepared with questions rather than the time-honored pedagogy of the teacher lecturing to a largely ill-prepared group of students.
Dr. Luce cites several of his own publications in this chapter, which underscores his familiarity with these concepts. He then reviews the nuts and bolts of a plastic surgery residency and concludes with a provocative question: If a plastic surgery residency program director was to start a program from the ground up, what elements would he or she need to implement in the formal education portion of their program? The curriculum provided in his book covers all the bases –and would allow a new program director to adopt it as a turnkey design for resident education.
The curriculum is organized into 12 general categories, which are then divided into modules – with the number of modules per category ranging from two to 15. The modules cover a

single topic and are linked to the ACGME milestones of patient care and medical knowledge. Leaving nothing to chance, Dr. Luce recommends a program using the curriculum to have two weekly conferences. These would be a one-hour cognitive conference, and an hour-and-ahalf or two-hour case conference, both powered by the curriculum.
Each module is a chapter and begins with a bibliography of selected relevant – and comprehensive – readings. Using the flipped classroom technique, residents receive the reading assignment seven to 10 days prior to the conference, allowing them to come to the conference fully prepared to ask questions about the readings rather than have a faculty member lecturing to the residents. What follows in the module are the faculty discussion points and study guide. Regardless of the module, both are excellent and structured so that a question is posed and answers are provided. I found these answers to be not only thoughtful, but thorough. Faculty members can easily review this information and apply it, and each module ends with a written examination, consisting of three or four multiple choice questions, based on the topics of the cognitive conference.
The intuitive or case conferences are linked to the modules covered in the cognitive conferences. Material provided for the case conferences includes representative photos, a lengthy discussion using the case-conference questions as prompts and several broad-based questions to frame the discussion. Dr. Luce points out that the weakness in most residencies is that what’s presented at case conferences is driven by the clinical practices of the faculty (i.e., what the residents have been exposed to in the O.R.). This can lead to large gaps in both the residents’ surgical experience and knowledge base, as it can place an inappropriate emphasis on the program’s strengths while ignoring the program’s weaknesses. As such, Dr. Luce makes several recommendations for a case conference around the curriculum, adherence to principles and making it both interactive and duplicative of clinical scenarios. For those of us who have served as ABPS oral board examiners, these intuitive conferences should serve as excellent preparation for the oral exams – as well as a guide for young practitioners.
From this reviewer’s perspective, this book should find its place onto the shelves of every program director, faculty member and resident or Fellow intent on a career in academic plastic surgery. This is Dr. Luce’s magnum opus and should be a perennial seller for decades to come.
–AnthonyA.Smith,MD ProfessorofPlasticSurgery,MayoClinicArizona PastPresident,ACEPS PSN
Program Chair
Albert Losken, MD
Program Co-Chairs
Amy Alderman, MD
Michael Mirzabeigi, MD
James D. Namnoum, MD
Symposium Faculty
Rachel A. Anolik, MD
Yoav Barnavon, MD
Yoav Barnea, MD
M. Bradley Calobrace, MD
Mark W. Clemens, MD
Onelio Garcia, Jr., MD
Gabriela Garcia-Nores, MD
Caroline A. Glicksman, MD, MSJ
Nicholas Haddock, MD
Dennis C. Hammond, MD
Lynn Jeffers, MD, MBA
Sean Kelishadi, MD
Danielle M. LeBlanc, MD
David Mathes, MD
Babak J. Mehrara, MD
Christopher J. Pannucci, MD
Marcelas Sanchez, MD
Filip Stillaert, MD
Louis L. Strock, MD
Steven Teitelbaum, MD
Bruce W. Van Natta, MD
Kamakshi R. Zeidler, MD
Michael R. Zenn, MD, MBA
By Samara Reigh
The Centers for Medicare & Medicaid Services (CMS) on Oct. 31 issued the Calendar Year 2026 Medicare Physician Fee Schedule (PFS) Final Rule (CMS-1832-F), with policies taking effect Jan. 1. Although the rule includes modest rate increases, it also introduces major structural changes that will shape physician reimbursement for years to come. For plastic surgeons, the 2026 rule delivers both opportunities and challenges – most notably, the introduction of an “efficiency adjustment” to work relative value units (RVUs), revisions to practice expense methodology, continued telehealth flexibilities and a fundamental overhaul of reimbursement for skin substitute products.
Consistent with the Medicare Access and CHIP Reauthorization Act of 2015, CMS established two separate conversion factors beginning in 2026. Physicians who are qualifying participants (QPs) in an Advanced Alternative Payment Model – those who meet specific thresholds for quality and cost accountability – will use a conversion factor of $33.57, an increase of 3.77 percent from 2025. Physicians who are not QPs will use a conversion factor of $33.40, a 3.26 percent increase from last year’s rate of $32.35. Both conversion factors include a 2.5 percent one-year increase to the physician fee schedule conversion factor – included in the budget reconciliation bill – as well as a .49 percent positive budget neutrality adjustment. Although these are technically positive updates, the overall financial effect is likely to be

muted because of broader structural changes elsewhere in the rule. In practical terms, plastic surgeons will see a nominal improvement in payment rates – but many procedural services could simultaneously lose value due to new adjustments in the underlying RVUs.
The efficiency adjustment
By far the most problematic policy in the 2026 rule is CMS’s new “efficiency adjustment,” which reduces work RVUs and corresponding intra-service time by 2.5 percent for all nontime-based services. The agency’s stated goal is to account for assumed gains in efficiency that occur as procedures become more routine, practitioners gain experience and technology advances. CMS argues that over-reliance on survey data from the AMA’s Relative Value Scale Update Committee led to inflated time assumptions and distorted payment values –particularly for procedural services.
A quick look at some of the work ASPS did in September and October to advocate on behalf of the specialty at the state level.

In principle, the efficiency adjustment is a thinly veiled end-run of the established system for valuing physician services. In practice, CMS created a recurring automatic cut to physician reimbursement. The uniform 2.5 percent cut in 2026 applies broadly and indiscriminately – including to many surgical procedures that have recently been re-valued; are currently under review; or are newly proposed for 2026. For plastic surgeons, this means that a wide range of commonly performed operations – nearly all of which are coded as non-time-based – will be subject to a reduction in work RVU value, even when there’s no evidence of decreased complexity or duration. The adjustment does not apply to time-based services such as evaluation and management (E/M) visits, care management, behavioral health, telehealth services or maternity global codes, but nearly all operative plastic surgery codes fall outside those exemptions.
The surgical community has reacted strongly against this policy. The ACS on Nov. 2 sent a letter to congressional leadership urging legislative intervention to block the efficiency adjustment before it takes effect. ASPS joined 33 other organizations in signing this letter. The coalition’s argument is straightforward: CMS’s assumption of increasing procedural efficiency is not supported by evidence. A peer-reviewed study published in the Journal of the American College of Surgeons in 2025 examined more than





In support of the ASPS-backed Advancing Women’s Health Coverage Act (AWHCA) by Rep. Kat Cammack (R-Fla.), staff contacted every local, state and regional plastic surgery society (LSR), and each state medical association (SMA), with the opportunity to sign onto letters thanking the current AWHCA sponsors for their efforts and encouraging congressional leadership to support the measure. So far, 25 LSRs and 4 SMAs have signed on.


ASPS led efforts alongside the South Carolina Society of Plastic Surgeons and the Southeastern Society of Plastic and Reconstructive Surgeons to support legislation that would require advanced practice registered nurses (APRNs), physician assistants (PA) and anesthesiologists assistants to practice as part of a patient-care team, while opposing two separate bills that would allow APRNs and PAs to practice independently after just 2,000 hours of clinical practice. Through testimony cosigned by the Massachusetts Society of Plastic Surgeons, New England Society of Plastic and Reconstructive Surgeons and Northeastern Society of Plastic Surgeons, ASPS requested amendments to a bill requiring plans to cover medically necessary functional repair or restoration of craniofacial disorders. As introduced, the legislation excludes downstream cosmetic and dental or orthodontic treatments that may be needed.


ASPS signed onto two letters drafted by the American Society for Dermatologic Surgery Association, opposing legislation in Oregon and Massachusetts that would allow dental hygienists to administer Botox and dermal fillers.
In a joint letter of opposition, ASPS and the Ohio Valley Society of Plastic Surgeons pushed back on legislation that would change the title of PAs to “physician associates” in Ohio.
1.7 million operations across 249 CPT codes and 11 specialties. It found that 90 percent of codes had unchanged or longer operative times in 2023 compared with 2019, with an overall 3.1 percent increase in operative duration. The data suggest that, if anything, surgical complexity has increased rather than decreased.
The ACS letter also warns that repeated efficiency adjustments – CMS has indicated these could recur every three years – would compound reimbursement erosion, especially for surgical fields reliant on non-time-based codes. As many physician employment contracts link compensation directly to work RVU production, this policy will not only cut Medicare reimbursement but also reduce physician income even for work that has not changed in scope or intensity. The resulting uncertainty could accelerate consolidation and threaten the viability of smaller independent practices. For plastic surgery, where case complexity and operative variability are high, the CMS assumption of universal time savings is particularly ill-founded.
The 2026 rule also finalizes major revisions to the practice expense (PE) methodology that determines how indirect and direct practice costs are allocated between facility and non-facility settings. CMS declined to adopt the new Physician Practice Information and Clinician Practice Information survey data collected by the AMA in 2024, citing methodological concerns such as small sample sizes and inconsistent reporting. Instead, the agency implemented its own updates to better reflect the shift in contemporary medical practice away from independent private practice toward hospital or system employment.
CMS will now recognize greater indirect costs for practitioners in office-based (non-facility) settings compared to those practicing in facilities, adjusting the relative value allocation accordingly. This change acknowledges that maintaining office infrastructure entails higher
Continued on page 30
PlastyPAC, the bipartisan political action committee of ASPS, works to educate and influence Congress on issues that directly affect plastic surgery. As the largest voice for reconstructive and cosmetic surgery, PlastyPAC is grateful for the support of the following people whose contributions during September and October help play a key part in the specialty’s success on Capitol Hill.
Arizona
Zoe MacIssac, MDu
California
Cagri Cakmakoglu, MD
Jennifer Cheesborough, MDs Debra Johnson, MDI Kelly Killeen, MDs Gabriel Kind, MDs Steven Williams, MDH Nance Yuan, MDs
Florida
Alicia Billington, MD, PhDI Nicole Cabbad, MD
Illinois
Daniel Krochmal, MDu Allison Shore, MDI
Indiana
Christiane Ueno, MDI
Maryland
Michele Manahan, MD, MBAI
Michigan
Jeffrey Kozlow, MD, MSu
New York
Jeffrey Ascherman, MDH Scot Glasberg, MDI
B. Aviva Preminger, MD, MPHu Raymond Schultz, MDn
North Carolina
Jessica Biagiotti, MDn
Pennsylvania
Gunnar Bergqvist, MDH Gayle Gordillo, MDu Sean Li, MDs
Tennessee
Dennis Hatef, MDu Ellis Tavin, MDI

David Halpern, MDI
Lauren Kuykendall, MDs Sabrina Pavri, MDu Andrew Rosenthal, MDI Rajendra Sawh-Martinez, MD, MHSI Devinder Singh, MDL
Georgia
Olumayowa Abiodun, MDu Chelsea Venditto, MD
Minnesota Sagar Deshpande, MD
Mississippi Marc Walker, MD, MBAs
Missouri
Paul Mills, MDs Justin Sacks, MD, MBAI
Nevada
Richard Baynosa, MDu
Mary Ann Contogiannis, MDI Lynn Damitz, MDH William DeBrock, MDn Eric Halverson, MDH Kristen Rezak, MDn Christopher Runyan, MD, PhD
Sonja Samant, MDn Pragna Shetty, MDn Shruti Tannan, MDs Paul Tenzel, MDs Cindy Wu, MDs
Ohio
R. Michael Johnson, MDI Ann Schwentker, MDu Anne Taylor, MDH
Texas
Steven Albright, MDs Olga Bachilo, MDs Jessica Goodwin, MDs Danielle LeBlanc, MDu
Utah
Christopher Shale, MD
Wisconsin Karri Adamson, MDs
Compiled by Paige Myers, MD, MPH
The phrase “huge success” certainly could be applied to the multitude of events held by the Women Plastic Surgeons Forum during Plastic Surgery The Meeting 2025. The lively city of New Orleans offered an ideal setting for a series of inspiring and energetic events – where attendees from across the globe gathered to celebrate the specialty and enjoy the vibrant atmosphere.
WPS members gathered Friday morning for the Close the Loop 5K to support breast reconstruction awareness. The mood was great as everyone put on their running jerseys and numbers, took photos and laughed. The crowd –made up of plastic surgeons, residents, students, staff, survivors and well-wishers – cheered us on with the sun rising over the Mississippi River in a beautiful display of light along the running path. Some people ran in large groups, others in duos and trios, and some solo – but all showed up to support this important cause. We later learned that we had donated our largest amount for this event to date – a total we now look forward to beating every year.
This WPS networking event, like every year, provided a vibrant mix of residents, students, surgeons new to practice and seasoned professionals. For many, the event served as a reunion, allowing members to reconnect with old friends and catch up on past experiences. For others, it served as an introduction to the WPS community – and an opportunity to meet new colleagues and friends. The reception fostered a sense of camaraderie and shared passion that truly made it a memorable occasion.
The WPS Luncheon drew a standing-room-only crowd of more than 200 people as Diana Yoon-Swartz, MD, PhD; ASPS President-elect Lynn Damitz, MD; and ASPS past President Lynn Jeffers, MD, MBA; took the stage to discuss advocacy, advancement and the power of collective action. Moderated by Carolyn De La Cruz, MD, the discussion inspired attendees with a call to engage in advocacy – from updating the Women’s Health Care and Reconstruction Act to fighting the cosmetic tax and scope of practice. It was an invitation to be part of meaningful impact in our specialty and to help patients through examples of how to educate, collaborate and create change in our practices and communities. The audience listened to powerful stories, such as a young Dr. Jeffers writing to Hillary Clinton with an invitation to speak at her high school. The message was clear: Together with one voice, we can make a difference. The event concluded on a high note, raising more than $4,500 for PlastyPAC to continue supporting advocacy efforts for the specialty.
The WPS Pilates session drew record attendance and provided a lively start to Saturday’s schedule. Participants enjoyed an energetic and empowering group workout, moving together to great music in a supportive environment. Thanks to Evergen, everyone left with fantastic swag – including mats, socks and other Pilates essentials. We look forward to moving together again next year.
The charm of New Orleans was abundant at this year’s WPS Exhibit Hall Lounge, which transformed into a French Quarter-esque set-

ting, complete with a pink exterior, shutters and streetlamps. Visitors were invited to create ornate

masks with all the glitz and glamour of a masquerade ball. Guests stopped by to enjoy a bev-



erage, catch up with friends and colleagues, and add a picture to the wall. The WPS Lounge has become a signature spot to debrief after meeting panels, review the latest surgical techniques and share practice ideas. The lounge was also a great place to catch a glimpse of the new WPS swag – including hats, bags and cropped sweatshirts. Year after year, annual meeting attendees enjoy the WPS Lounge as a peaceful spot to recharge during the meeting – and this year provided that point of connection once again.
It was a truly memorable conference, and we can’t wait to see everyone in Palm Springs on Jan. 30-Feb. 1 for the 2026 WPS Symposium. PSN
WPS members Patricia Mars, MD; Vinaya Rednam, MD; Carolyn De La Cruz, MD; Jennie Cheesborough, MD; and Meredith Collins, MD; each contributed to this piece.
Ideal Exposure For:
• Caudal aspect of platysmal plication.
• Low transverse platysmal division.
• Anterior cervical defatting and hemostasis.
• Submandibular gland resection
• Medial SMAS dissection and fixation.
Retractor Features:
• Curved side wings expand visualization
• Fiberoptic endpoint elongates the optical cavity
• Polished Surfaces enhance illumination
ASSI.ABR90626 WITH Fiber Optics & Universal Adapter
ASSI.ABR90426 WITHOUT Fiber Optics & Universal Adapter


Compiled by Elizabeth Gibbons
Nine plastic surgery residents were given the chance to attend Plastic Surgery
The Meeting 2025 in New Orleans, thanks to the generous support of KLS Martin Group. The residents, who traveled from around the world, share their reflections for PSN
Opportunities over obstacles

My attendance at PSTM25 greatly piqued my interest in participating in ASPS and The PSF. In particular, while attending committee meetings, I spoke with committee coordinators regarding how I could continue to contribute throughout the year. I received emails regarding the opportunity to attend further committee meetings, and I look forward to learning and growing by attending these meetings in the future. All the committee meetings I attended were fascinating in their own way, but the area that I became most interested in is the robotics subcommittee and the entrepreneurship events meeting. I was fascinated to learn about the future robotics education events, as well as the future investment vehicles the Society is creating – in particular, the innovation accelerator and future efforts toward the creation of an investment fund for early-stage ventures.
Two things stand out in my mind as my biggest successes of this experience. The first is simply the opportunity to get involved in the subcommittees. The second is getting three separate opportunities to have one-on-one conversations with plastic surgery department and division chairs. I used these opportunities to discuss how I can best position myself to achieve my goals in the future – a position in academic medicine, a productive research career and being a physician entrepreneur.
I felt incredibly supported during my time in New Orleans and the experience was filled with a sense of opportunity rather than obstacles.
– Hilliard Brydges, MD University of Washington Seattle
The bigger picture

Being able to come to the annual meetings while in residency reinforces the “bigger picture.” This is important to me, as in residency we sometimes lose the forest for the trees, and it’s easy to get stuck in the dayto-day and forget what our long-term goals are. Being able to connect with people from across the country and globe – and share ideas, successes and challenges – is a great part of our jobs as plastic surgeons and a highlight of PSTM. I found the information learned at the Senior Residents Conference to be timely and incredibly helpful. As a fourth-year resident, I’m starting to think more about my preferred practice setting and long-term career goals. Hearing from
those who’ve been through the process and landed in various positions was a great way for me to contextualize those preferences and start making concrete plans for the next several years. Thinking about these things earlier helps demystify the otherwise enigmatic transition period from residency to attending.
My favorite talk at PSTM this year was on drainless abdominoplasty. I found the structure of the panel to be well-done, with an initial review by practiced surgeons followed by a discussion by a surgeon who only recently adopted the technique. The talk was a great example of how coming together at PSTM can fuel advances in practice and support a collaborative approach to providing the best care to our patients. It’s fun to see newer techniques and ideas shared across our specialty, and I look forward to contributing while in practice myself soon.
that go into every exam question – each undergoing multiple rounds of review and discussion by subspecialty experts to ensure accuracy and educational value.
Overall, attending these committee meetings was an incredibly enriching experience that deepened my appreciation for the leadership, collaboration and advocacy efforts that shape our field. It inspired me to become more actively involved in ASPS committees and to pursue future leadership roles within the organization.
– Elizabeth Cox, MD Stanford Plastic & Reconstructive
Surgery Stanford, Calif.
– Christina Chopra, MD Stony Brook University Hospital New

York
Thanks to the generous support of the KLS Martin Resident Travel Scholarship, I had the opportunity to attend PSTM25 in New Orleans. This experience provided invaluable exposure to the inner workings of several ASPS committees – including the Plastic Surgery Robotics Subcommittee, the Legislative Advocacy Committee and the In-Service Exam Committee. Each offered unique insights into the challenges and successes shaping the future of our specialty.
At the Plastic Surgery Robotics Subcommittee, we discussed the growing interest in robotic-assisted procedures – a rapidly emerging “hot topic” within plastic surgery. One of the key challenges identified was the limited access to robotic systems for surgical training. However, a training site equipped with 10 robots was identified, allowing for the development of a large-scale educational workshop to train other surgeons. The committee’s discussions highlighted the momentum behind integrating robotics into plastic surgery and the need for structured, equitable access to this technology.
The Legislative Advocacy Committee addressed ongoing efforts to influence policy for the benefit of both patients and plastic surgeons. A major challenge discussed was the current government shutdown and its ripple effects on healthcare initiatives. Despite these obstacles, the committee celebrated several recent successes driven by effective lobbying for patient-centered legislation. A key takeaway was the strategic importance of selecting legislative issues that have a realistic chance of passing in the current political climate, ensuring that advocacy efforts yield tangible results.
The In-Service Exam Committee provided fascinating insight into the structure and philosophy behind the In-Service Exam. One of the ongoing challenges is encouraging residency programs to eliminate punitive measures tied to lower in-service scores, given that the exam is intended as a formative assessment tool. I was impressed by the rigor and collaboration

My attendance in New Orleans piqued my interest in further participating in ASPS and The PSF. I attended committee meetings anticipating that I would have a passive observer-style role. In several instances, however, I found that I had insights and opinions that I wanted to share with the group. For that reason, I’d like to join the Annual Meeting Educational Program Committee to contribute unique resident perspectives on educational topics and to learn more about the decision-making process in meeting programming. I would also like to join the Young Plastic Surgeons Forum with the aim to receive mentorship from surgeons early in their careers who can provide mentorship to budding trainees, thus providing a greater sense of belonging within the plastic surgery community. I also applied to become a reviewer for PRS Global Open – an opportunity that I was not made aware of until the meeting. With my prior experience as a research Fellow and a recent abstract reviewer for the Association of Women Surgeons Starr Research Forum, it would be a privilege to further contribute to research through manuscript peer review. This would also enhance my skills of assessing and interpreting academic literature, thus furthering my own ability to write quality papers. Finally, the Women Plastic Surgeons luncheon was an excellent opportunity to learn about policies affecting plastic surgery – and this led me to participate in a virtual briefing on Oct. 20 to discuss new legislation to modernize the Women’s Health and Cancer Rights Act and strengthen coverage requirements for women undergoing breast cancer treatment.
As someone aiming to pursue fellowship in microsurgery, I also recognize my particular interest in a few other areas that I might like to incorporate into my future practice. For example, I enjoy some aspects of general reconstructive plastic surgery, as well as the delicate structure of the nose and ear. One goal of my attendance at PSTM was to learn more about rhinoplasty – a subject to which I’ve had limited exposure as an early third-year resident. The Rhinoplasty Symposium offered a comprehensive review of lectures, starting with the basics of anatomy and aesthetics, and finishing with a debate of best techniques to address common concerns seen among experts in the field. It was insightful to hear how preferences vary in the setting
of new innovations (e.g., using a rasp versus a piezotome for bony work), however the fundamentals remain the same. It was a sincere privilege to hear from big names in rhinoplasty firsthand. I even had the opportunity to discuss my interest with one of the speakers. This opportunity reinforced my interest in rhinoplasty while additionally offering valuable insight into management of facial trauma. This scholarship enabled me to not only absorb the wisdom of plastic surgery experts, but to listen to their musings and recommendations during committee meetings. I had the chance to discuss future career plans and identify opportunities for academic growth with mentors in plastic surgery during breaks in schedule programming. The connections I made will be maintained long after my time at the conference. It’s a privilege to be able to meet surgeons from programs of interest at a single conference such as ASPS, and the opportunity to meet and speak to them in person is invaluable. I look forward to working with them in the future through research and regular meetings aimed at shaping the practice I want after graduation. I also was able to meet medical students who expressed interest in my own program and to act as a mentor and contact person for future research and networking opportunities. Finally, exposure to a wide-ranging breadth of topics and presentations has sparked interest in new research topics, and I was able to discuss the design of a new project with a resident from another program. I certainly found my place within a supportive community of hardworking and talented individuals who not only share my proclivities but feel impassioned to facilitate my own professional development. – Alisa Girard, MD Cooper Medical School of Rowan University Camden, N.J.

Attending PSTM25 in New Orleans definitely increased my interest in participating in ASPS and The PSF in the future. ASPS is the most comprehensive society in our specialty, and seeing all of the diverse ways that I could connect with other plastic surgeons was very encouraging. I’m definitely interested in getting more involved as I advance in my career and feel more comfortable and confident about doing this, having had this experience as an introduction. I attended the Residents Council meeting, which was held virtually prior to the onsite event in New Orleans, where I also attended the Hot Topics and Legislative Advocacy Committee meetings. Each of those meetings were different with different vibes and styles, so I felt encouraged that I should really pursue involvement in committees where I have true interest. I also felt that the committees were great ways to get to know other plastic surgeons. I felt like I was able to meet with residents of other programs and reconnect with faculty that I had met as a medical student. The meeting was a fantastic networking experience in a way that felt genuine. One of the biggest challenges I encountered
during the meeting was deciding which sessions to attend, as there were so many good events happening simultaneously. I sometimes skipped around to different concurrent sessions to be able to get a small sense of each one, but I also accepted that I would not be able to attend everything and reminded myself that there are many future meetings that I can attend to continue to learn about the amazing things happening in our specialty.
I felt inspired at the committee meetings because there were so many people from different backgrounds and practice models all coming together to participate in an aspect of plastic surgery that they were passionate about. This also gave me a new perspective on networking, as I felt that attending the various networking sessions and committee meetings fostered a more genuine networking experience, as everyone at each of the sessions was there because they were interested in that topic. I really look forward to future meetings where I can continue to meet other inspiring individuals.
– Alexandra Junn, MD Medstar Georgetown University Hospital Washington, D.C.

Attending this year’s annual meeting strengthened my interest in active involvement with ASPS and The PSF – particularly in light of being able to spend time with the global plastic surgery, robotics, social media and wellness committees. The network of plastic surgeons presenting groundbreaking research is unmatched, and I feel fortunate to be a part of such a large community dedicated to spreading academic efforts. My biggest success was meeting with plastic surgery mentors and sharing my own research efforts at our institution on plastic surgery match trends and ongoing projects in breast reconstruction. I feel proud to have been able to support my resident colleagues in their own research presentations as well. My main challenge was balancing multiple sessions while networking effectively; planning ahead and using the PSTM app helped me manage time efficiently.
My “wow” moments included hearing pioneering talks on regenerative biomaterials and AI-assisted surgical planning, which reframed
tees within ASPS/PSF to both learn from and contribute to this vibrant community.
My biggest successes during PSTM25 were rooted in both professional growth and meaningful connection. Presenting and discussing my work with international peers and faculty gave me valuable feedback and confidence in the global relevance of my research. It was immensely rewarding to see that the challenges and innovations emerging from resource-limited settings resonated with an international audience. Equally fulfilling was building relationships with mentors and fellow young surgeons who share similar aspirations in reconstructive and academic plastic surgery. These interactions expanded my perspective on collaborative research and future fellowship opportunities. Beyond academic engagement, a personal success was learning to articulate my ideas and experiences in a global forum – something that has strengthened my confidence as a communicator, researcher and future leader in plastic surgery.
Attending PSTM 2025 was an eye-opening experience that deepened my understanding of both the artistry and innovation driving modern plastic surgery. Witnessing the seamless integration of technology with reconstructive principles – particularly the sessions on AI-assisted surgical planning and patient management, and the evolving frontiers of microsurgery – was illuminating.
Equally impactful was the opportunity to network with global leaders and young innovators in plastic surgery. Engaging with them helped me appreciate how research, collaboration and mentorship fuel progress in our field. It reinforced my aspiration to contribute meaningfully to both academic and reconstructive surgery in India – bringing evidence-based, resource-conscious innovation to where it’s needed most.
Receiving this travel scholarship not only made my participation possible but also strengthened my sense of belonging within the international plastic surgery community. It has motivated me to pursue advanced training and collaborative research, with a renewed focus on global best practices adapted to local challenges. This experience has truly broadened my vision of what it means to be a plastic surgeon – an innovator, healer and lifelong learner.
– Anshu Saini, MBBS,
MS, DNB All India Institute of Medical Sciences New Delhi, India
Knowledge exchange

My primary areas of interest lie in fostering international collaboration and developing resources for residents. Based on my experience chairing the International Residents Forum, I’m keen to further contribute to developing international webinars and podcasts, creating a resident-focused newsletter and establishing structured exchange and fellowship programs to connect trainees across the globe.
My main takeaway from PSTM25 is the significant – and unmet – demand for international resident-focused programming. There’s a strong desire for sessions on fellowship opportunities across different continents and for direct interaction with program directors and heads of units. The enthusiasm from residents from countries such as Qatar, Australia, Romania and Kuwait highlighted the global need for mentorship and collaborative platforms within ASPS.
My biggest success was successfully launching and chairing the inaugural International Residents Forum session at the International Center. The session was well attended, and the positive feedback affirmed the value of the initiative. A key success was seeing the immediate impact of the forum, as a delegate from Qatar was inspired to conduct on-site interviews for mentorship opportunities at the international center directly following our session. Furthermore, successfully leading the committee selection meeting and outlining a clear plan for future projects (webinars, exchange programs, etc.) felt like a major accomplishment.
The connections I made with senior leadership and international peers are invaluable and will serve as a foundation for future collaborative projects and leadership roles. This scholarship provided me with the financial support necessary to attend PSTM25 and, more importantly, to take on a leadership role as the chair of the International Residents Forum. This experience has solidified my career goal of being actively involved with ASPS/PSF leadership – specifically to serve as a bridge for the international plastic surgery community. It has given me a clear direction and a platform to develop new and impactful programs for residents worldwide.
– Jing Qin Tay, MBBCh, PhD, MBA Thames Valley Deanery United Kingdom
I belong here

PSTM25 energized my involvement with ASPS and The PSF. Moving forward, I would like to engage more deeply with resident leadership groups such as the Residents Council and the YPS Steering Committee. I appreciated their ability to focus on resident-specific interests and challenges. Although I was unable to participate in the Global Plastic Surgery Congress Committee and the Diversity and Inclusion Committee this year, I’m very interested in joining their efforts in the future, as both align strongly with my professional interests and values.
My biggest success was networking with other residents and leaders in the field. I connected with peers who share similar interests and learned about ongoing initiatives and projects I hadn’t previously known about. These interactions broadened my understanding of the many ways residents can contribute to advancing plastic surgery beyond clinical training and through leadership and research.
As a new independent resident, my biggest challenge was attending committee meetings without knowing many people initially. However, I viewed this as an opportunity rather than a barrier. I made a point to introduce myself, ask questions and engage with attendees from various programs. This proactive approach allowed me to connect with new people and gain valuable insight.

I enjoyed the constant displays of innovation and collaboration throughout the meeting. I was inspired by the breadth of scientific presentations, many focused on refining or reimagining surgical techniques, which reminded me of the creativity and progress that initially drew me to plastic surgery. Receiving this scholarship made me feel truly included in the greater plastic surgery community. It reinforced that I belong here – not just as a learner, but as a potential contributor.
– Yadira Villalvazo, MD, MS University of Pittsburgh Pittsburgh |


with my aspirations as a young plastic surgeon. I’m particularly interested in contributing to global reconstructive initiatives, surgical education and outcomes-based research. The PSF’s focus on advancing evidence-driven care and supporting early-career surgeons resonates deeply with me. I would also like to engage in international collaborations, resident education programs and diversity initiatives that promote equitable access to reconstructive and aesthetic surgery worldwide. In the future, I hope to participate in research mentorship programs, clinical outcome registries and educational commit-

By Jim Leonardo
Editor’s note: The following is part of an ongoing series highlighting The PSF Research Grant Award winners, and research they’re conducting to improve patient safety and develop new technologies for plastic surgeons. These features examine research funding awarded prior to the current year, as projects to which grants were awarded this year may not yet have results ready to discuss.
Abigail Peoples, MD
Title: PGY-3, Wake Forest University School of Medicine
Award: The PSF Directed Research Grant – Breast Implant Safety Project: Characterization of the Breast Microbiome in Implant-based Breast Reconstruction (Under supervision of Adam Katz, MD)

PSN: What prompted you to study the breast microbiome in implant-based breast reconstruction?
Dr. Peoples: The reported rate of surgical site infection in implant-based breast reconstruction ranges broadly in the literature – anywhere from 1-30 percent. These procedures are classified as “clean contaminated” cases with an expected surgical-site infection rate around 3-11 percent. Our team wondered if the patient’s own microbiome could be the source of infectious organisms – or if dysbiosis from the mastectomy and reconstructive processes increases the risk of infection beyond what would be expected from a “clean contaminated” case. We collected swabs and tissue samples during patients’ operations and partnered with colleagues at Wake Forest to perform shotgun genomic sequencing on these samples. For our pilot analysis, we selected patients who had culture-confirmed infections. We then compared the bacterial, viral and fungal species that were identified on genomic sequencing to what grew in the patient’s cultures from the O.R.



PSN: How far along are you in this research?
Dr. Peoples: We’ve just completed a pilot analysis of a subset of patients who developed infection during their mastectomy and reconstruction. We confirmed that each patient had a unique microbiome at the start of their reconstruction, and that the microbiome changed at each operation. We were surprised to find that the infectious species identified by culture were not always found in the collected specimens, even when the samples were collected concurrently with the culture specimens. We’re continuing to work through how to interpret and understand this surprising finding.
PSN: What do you see as the project’s practical applicability?
Dr. Peoples: While we’re still in the early stages, I see meaningful potential for its applicability. For instance, a deeper understanding of how dysbiosis influences infection risk could open the door to creative strategies aimed at preserving eubiosis and, ultimately, improving patient outcomes. There’s ongoing work that’s
particularly interesting – examining the interplay between the gut microbiome and the breast microbiome, suggesting that systemic interventions may influence local microbial environments. Building on that concept, our team has discussed whether approaches such as oral probiotics, dietary modulation or even targeted microbiome therapies could play a role in mitigating breast dysbiosis. In the near term, this project can help clarify whether microbial imbalance is a significant and modifiable risk factor – and if that’s so, it may lay the groundwork for interventions that are low-cost, patient-friendly and scalable. While it’s too early to draw conclusions, I’m excited by the possibility these findings could eventually shift the way we think about infection prevention and antibiotic use, as well as pre- and postoperative care in breast surgery.
PSN: Has anything unexpected surfaced that might change your focus?
Dr. Peoples: Having species grow in culture and not be identified in the shotgun genomic sequence for samples taken at the same time
was surprising to us. It has led us to try to understand how the lab MALDI-TOF identification process could identify different organisms than the genomic sequence from these samples. Our study wasn’t well constructed to answer this question, but this is something we’re interested in understanding more.
PSN: Do you have any thoughts as to what’s behind that surprise?
Dr. Peoples: We wonder if this could be a sampling error; or if the genomically identified species we have didn’t survive through the culture process; or if genomic sequencing is more specific than the culture data.
PSN: Who helped out with this project?
Dr. Peoples: I must thank Adam Katz, MD, and Ramon Llull, MD, PhD, for their mentorship throughout this project. As a medical student with limited prior research experience, I’m especially grateful they gave me the opportunity to spend a dedicated year working with them between my third and fourth years of medical school. From the outset, they conceptualized the project and helped frame the key research questions, while also guiding me through the process of developing a rigorous and feasible protocol. They reviewed and strengthened our grant submission, provided constructive feedback on every abstract I submitted and consistently challenged me to think critically on how our findings could inform future work. What has been most impactful, however, is how they’ve modeled what it means to be a surgeon-scientist: combining clinical excellence with curiosity, innovation and a genuine commitment to advancing the field. They’ve made research approachable and exciting, while also creating an environment where I felt supported to take initiative and grow as an investigator. Their mentorship has not only shaped this project, but has also given me a framework for how research can be integrated into a surgical career.
PSN: What did you want to be growing up?
Dr. Peoples: In high school, I wanted to be a Spanish teacher. I’ve always loved teaching, and I anticipate that I’ll want to be involved in academic medicine or teaching in some way as I continue my career.
PSN: Apart from this project, what’s been your favorite research project to date?
Dr. Peoples: By virtue of the fact that I still remember it, I have to say my first-grade project on Mustang horses in the western United States. I made a very cool diorama that I was proud of at the time.
PSN: How do you spend time away from the lab?
Dr. Peoples: As a junior resident, my time outside the hospital is valuable. I spend a lot of time outdoors with my dog, Poppy, as well as reading and spending time with friends.
PSN: What sounds are most often heard in your O.R.?
Dr. Peoples: I’ve recently started building my own O.R. playlist – and it includes a lot of upbeat pop songs. The Spotify “Lady Gaga Radio” channel always seems to provide a good go-to medley.
For more information about the many research studies funded by The PSF or to support our current and future research initiatives, please go to ThePSF.org PSN





By ASPS Staff
Plastic Surgery The Meeting 2025 returned to the Crescent City in October, boasting its trademark wealth of educational programming over a four-day schedule and using the unique energy and flavor of New Orleans as the seasoning for the gumbo of networking events, fundraisers, the Close the Loop 5K and myriad opportunities for plastic surgeons from around the world to connect, collaborate and spend time together.
“New Orleans is such an energetic city and PSTM seemed to thrive off that energy this year,” says ASPS immediate-past President Scott Hollenbeck, MD. “The education was exceptional as always and the Convention Center was arranged to maximize networking and hitting multiple talks. There was also palpable thrill at the social events and dinners that we had hoped for while planning this year’s meeting. New Orleans more than lived up to – and, in many ways, exceeded – our expectations.”
In preclinical studies, AlloDerm™ RTM was shown to minimize inflammation, enable rapid revascularization and fibroblast repopulation, and transition into host tissue instead of forming scar tissue.1-4*

With over 4 million implantations and more than 1000 scientific* and clinical publications, AlloDerm™ RTM is the most-used, most-studied ADM by far.5-7 And our portfolio has blossomed into the industry’s most extensive, with 32 sizes, 5 thicknesses, and 3 shapes to fit your needs.8
*Correlation of these results, based on animal studies, to results in humans has not been established.

INDICATIONS
ALLODERM SELECT™ Regenerative Tissue Matrix (ALLODERM SELECT™ RTM refers to both ALLODERM SELECT™ RTM and ALLODERM SELECT RESTORE™ RTM products) is intended to be used for repair or replacement of damaged or inadequate integumental tissue or for other homologous uses of human integument. ALLODERM SELECT™ RTM is intended for use in post-mastectomy breast reconstruction surgical procedures where the use of the acellular dermal matrix (ADM) is considered homologous, such as managing a potential skin defect created from harvesting tissue for use in autologous tissue reconstruction. Examples of uses in post-mastectomy breast reconstruction not considered homologous include use of an ADM to form an extension of the submuscular pocket for placement of a breast implant or tissue expander, and use to prevent expander or implant extrusion, or to constrain the expander or implant in the correct position. This product is intended for use in one patient, on a single occasion. ALLODERM SELECT™ RTM is not indicated for use as a dural substitute or intended for use in veterinary applications.
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
ALLODERM SELECT™ RTM should not be used in patients with a known sensitivity to any of the antibiotics listed on the package and/or Polysorbate 20.
WARNINGS
Processing of the tissue, laboratory testing, and careful donor screening minimize the risk of the donor tissue transmitting disease to the recipient patient. As with any processed donor tissue, ALLODERM SELECT™ RTM is not guaranteed to be free of all pathogens. No long-term studies have been conducted to evaluate the carcinogenic or mutagenic potential or reproductive impact of the clinical application of ALLODERM SELECT™ RTM.
DO NOT re-sterilize ALLODERM SELECT™ RTM. DO NOT reuse once the tissue graft has been removed from the packaging and/or is in contact with a patient. Discard all open and unused portions of the product in accordance with standard medical practice and institutional protocols for disposal of human tissue. Once a package or container seal has been compromised, the tissue shall be either transplanted, if appropriate, or otherwise discarded. DO NOT use if the foil pouch is opened or damaged. DO NOT use if the seal is broken or compromised. DO NOT use if the temperature monitoring device does not display “OK”. DO NOT use after the expiration date noted on the label. Transfer ALLODERM SELECT™ RTM from the foil pouch aseptically. DO NOT place the foil pouch in the sterile field.
PRECAUTIONS
Poor general medical condition or any pathology that would limit the blood supply and compromise healing should be considered when selecting patients
for implanting ALLODERM SELECT™ RTM as such conditions may compromise successful clinical outcome. Whenever clinical circumstances require implantation in a site that is contaminated or infected, appropriate local and/or systemic antiinfective measures should be taken.
ALLODERM SELECT™ RTM has a distinct basement membrane (upper) and dermal surface (lower). When applied as an implant, it is recommended that the dermal side be placed against the most vascular tissue. Soak the tissue for a minimum of 2 minutes using a sterile basin and room temperature sterile saline or room temperature sterile lactated Ringer’s solution to cover the tissue. If any hair is visible, remove using aseptic technique before implantation.
ALLODERM SELECT™ RTM should be hydrated and moist when the package is opened. DO NOT use if this product is dry. Use of this product is limited to specific health professionals (eg, physicians, dentists, and/or podiatrists). Certain considerations should be made to reduce the risk of adverse events when performing surgical procedures using a tissue graft. Please see the Instructions for Use (IFU) for more information on patient/product selection and surgical procedures involving tissue implantation before using ALLODERM SELECT™ RTM.
ADVERSE EVENTS
Potential adverse events which may result from surgical procedures associated with the implant of a tissue graft include, but are not limited to, the following:

wound or systemic infection; seroma; dehiscence; hypersensitive, allergic or other immune response; and sloughing or failure of the graft.
ALLODERM SELECT™ RTM is available by prescription only.
For more information, please see the Instructions for Use (IFU) for ALLODERM SELECT™ RTM available at https://hcp.alloderm.com/ or call 1.800.678.1605.
To report an adverse reaction, please call Allergan Aesthetics at 1.800.433.8871.
References: 1. Xu H, Wan H, Sandor M, et al. Host response to human acellular dermal matrix transplantation in a primate model abdominal wall repair. Tissue Eng Part A. 2008;14(2):2009-2019. 2. Harper JR, McQuillan DJ. Extracellular wound matrices: a novel regenerative tissue matrix (RTM) technology for connective tissue reconstruction. Wounds. 2007;19(6):163-168. 3. Data on file, Allergan; Study Report LRD-2010-04-005. 4. Data on file, Allergan; Study Report LRD-2012-05-006.
5. Data on file, Allergan Aesthetics, AlloDerm Global Product Sales 2023. 6. Data on file, Allergan Aesthetics, LIS Publication Search performed May 2024. 7. Data on file, Allergan Aesthetics; iData MedSKU Hospital Purchasing Data. Q1’17–Q4’23. 8. Data on file, Allergan Aesthetics, 2022; Manual of competitive ADM sizes, shapes, thicknesses by brand, by company.

total registrants and more than 200 exhibitors. Plastic Surgery The Meeting 2025 also boasted more than 100 live sessions, 92 live abstract sessions, 34 resident on-demand presentations and 74 Global Partner e-Posters on-demand, with up to 75 AMA PRA Category 1 CreditsTM provided – 25 of which were applicable to patient safety.
The Sapphire Supporter for Plastic Surgery
The Meeting 2025 was Allergan Aesthetics, an AbbVie company; Platinum Supporters were Mentor and Solventum; and Gold Supporters were BD, Gore, Integra, Motiva by Establishment Labs®️, MTF Biologics, Organogenesis, Pacira Biosciences, Tiger Aesthetics and Vertex.
This year’s Opening Ceremonies employed AI techology in its introductory videos to place Dr. Hollenbeck, 2025 PSF President Alan Matarasso, MD, and 2025 ASMS President Francis Papay, MD, in outer space, an adventure movie and a haunted laboratory, respectively. As has become tradition at the annual meeting, the recipients of the 2025 Patients of Courage: Triumph Over Adversity Awards took the spotlight during Opening Ceremonies. The awards program – this year sponsored by CareCredit –celebrated the bravery and charitable actions of three patients whose lives were changed or saved through reconstructive surgery. Since 2003, the Society has honored more than 50 patients through the program.
Anna Crollman (nominated by Ron Israeli, MD) sacrificed her breasts to cancer, but she refused to let it take her sense of style. Instead, she turned her passion for beauty and fashion into MyCancerChic, a blog and social media community, chronicling her decade-long breast cancer journey from research through reconstruction. This vital resource now empowers young women to navigate their own cancer journeys with confidence.
Michael Goodman, MD (nominated by Jason Cacioppo, MD), was born with Treacher Collins syndrome, enduring countless surgeries and bullying because of his facial difference. After finally accepting himself, he shared his story in a social media post, which went viral reaching thousands of people. Today, he speaks to students and others around the world, encouraging compassion and inclusion through his lived experiences.
After giving birth in October 2022, Krystina Pacheco (nominated by Chandra Ellis, MD) faced a life-threatening infection that led to the amputation of all four of her limbs. Despite this unimaginable loss, she remained steadfast in her goals of being a devoted mother and dancing with her husband. Embracing physical therapy, mental health support and prosthetics, Krystina’s journey exemplifies how profound adversity can be transformed into a new beginning.
The Opening Ceremonies also welcomed
Chris Campbell, MD, (along with his wife, Kristin) and Narayanan Nair, MD. The Maliniac Circle is composed of plastic surgeons whose generosity helps guarantee success for the future of the specialty. Maliniac Fellows have made a minimum $100,000 deferred gift commitment or have provided $50,000 or more via an outright contribution of cash or appreciated securities to The PSF. An outright cash donation, yearly pledge, insurance policy or appreciated securities are all accepted forms of contribution.
In an annual meeting first, Dr. Hollenbeck and Dr. Matarasso presented a joint Presidents Panel, “What is Plastic Surgery?” Dr. Hollenbeck made the case that aesthetics and reconstruction are “inseparable; one in the same,” and aesthetics will be lost if reconstructive surgery isn’t practiced – although he noted that poor reimbursement has made that a challenge.
“Our strength in aesthetic surgery is based on our reconstructive principles,” Dr. Hollenbeck told the audience. “Recon is our strength and we could lose that to others if we don’t provide that.”
Dr. Matarasso noted that competitive practices can be created by following his “P’s of Practice,” which include passion, preceptors, practice, preparation, performance, product, planning, possibility, priorities, personnel, prices and prescience – among other factors.
“Success takes a lot longer to achieve than failure,” he said. “Take care of your health, it catches up very quickly, and don’t forget your family, because nothing works if it’s not good at home.”
Mark Constantian, MD, who undertook several years of research training, took part in the panel and detailed how that helped him become a better reconstructive surgeon. “I never considered myself an aesthetic surgeon; but the rules I learned in research became my criteria for reconstructive and aesthetic surgery,” he said.
ASPS past President and PRS Editor Emeritus Rod Rohrich, MD, addressed how to develop cosmetic surgery expertise.
“Reconstructive surgery helps make you who you are,” he told attendees. “It makes us the best aesthetic surgeons, by far. It gives us the caring, compassion and confidence to be the best we can be in aesthetic surgery.”
Mark Sultan, MD, described training under such luminous figures as ASPS past President Norman Hugo, MD; John Coleman III, MD, and Donald Wood-Smith, MD, who informed him that, “You build your reputation first, and your practice will follow.”
Quoting Sir Harold Gillies, MD, he referred to reconstructive surgery as a “return to normal” and aesthetic as surpassing the normal.
“My advice to younger surgeons is: Don’t narrow your focus to cosmetic surgery pre-
yourselves of a great deal of satisfaction and a great number of excellent cosmetic and reconstructive results.”
Oscar Ramirez, MD, invoked his paper “Components Separation Method for Closure of Abdominal-Wall Defects: An Anatomic and Clinical Study,” which has nearly 2,000 citations, as one of the most-cited PRS articles in the last 50 years and has gained several awards and widespread recognition. He wrote it after realizing the widespread occurrence of hernias and the costs involved, as well as a myriad of secondary problems. He noted his training at Facultad Medicina de San Fernando, Franklin Square Medical Center, Johns Hopkins Hospital, University of Pittsburgh – all of which “prepared me to become a complete plastic surgeon.” He also described his history with component separation involving the rectus muscle and how a procedure that he created is done more commonly if not exclusively by general surgeons.
Samuel Lin, MD, MBA – himself double-boarded in plastic surgery and ENT –asked whether the two specialties can coexist.
“I support anything related to plastic and re-
ing that competition between the two could rely on the $40 billion aesthetics industry. One study reveals that case volume for several procedures, including rhinoplasty and head and neck reconstruction declining significantly for plastic surgeons.
L. Scott Levin, MD, addressed whether plastic surgery “dropped the ball” with hand surgery. Videos of several American Hand Society past presidents were played with some noting that training together and maintaining close training relationships will keep the specialties together. Dr. Levin invoked such hand and plastic surgery luminaries as Sterling Bunnell, MD; Susan Mackinnon, MD; and Harry Buncke Jr., MD. Dr. Levin said hand and plastic surgery are intertwined but the latter must work to keep the two engaged and intertwined.
Meredith Collins, MD, who devoted her career to breast reconstruction, described her journey of having a benign breast cancer tumor removed and subsequent reconstruction, calling it the moment she understood what breast patients feel.
“The silver lining of this chapter in my life was a new understanding of empathy and com-
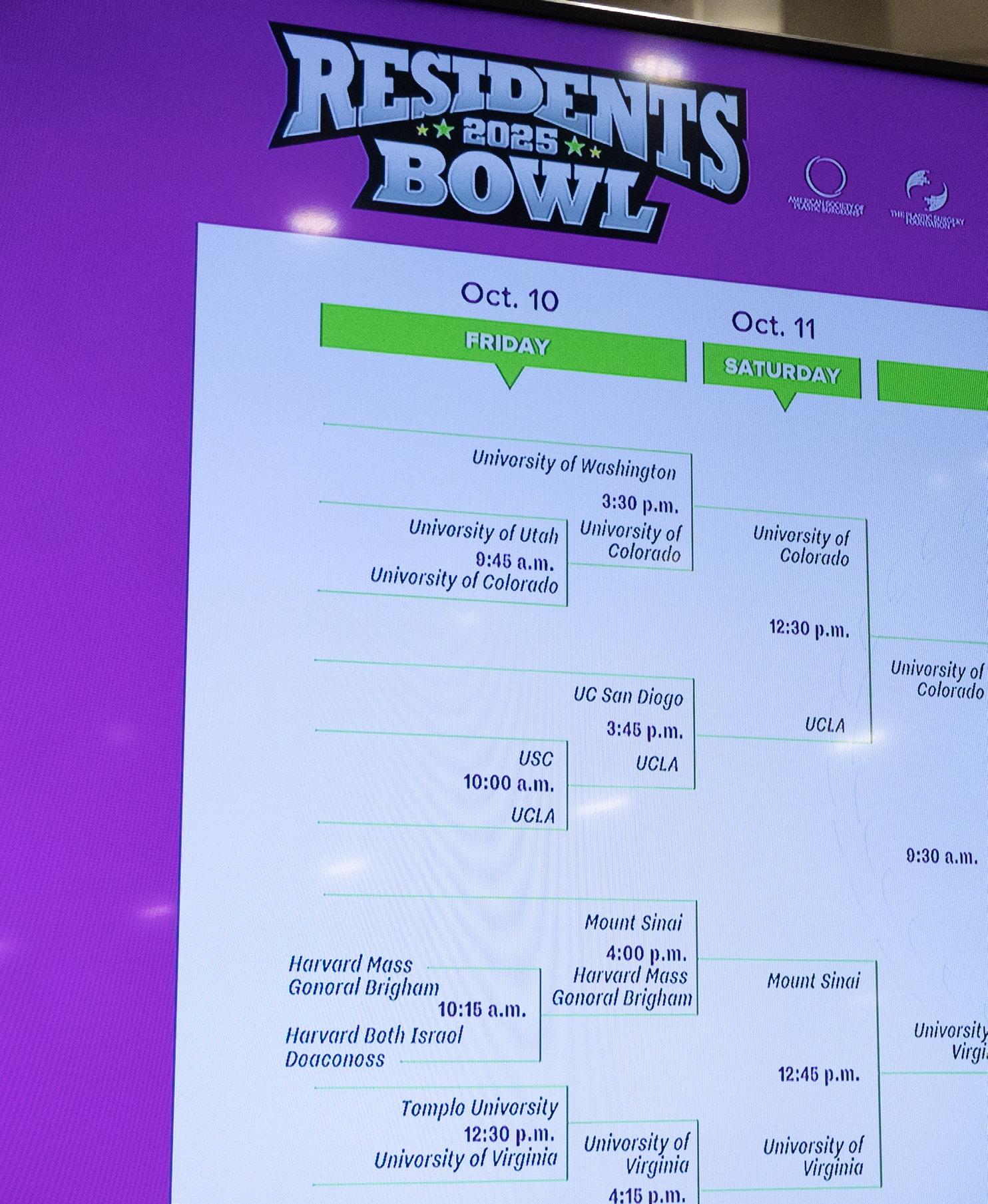
After falling short in the championship round last year, Baylor College of Medicine triumphed in a hard-fought battle against the University of Virginia (UVA) to be crowned Residents Bowl champion during Plastic Surgery The Meeting in New Orleans. Baylor’s route to the title included vanquishing Louisiana State University, University of Texas Health San Antonio, University of South Florida and Washington University.
UVA, meanwhile, dispatched Temple University, the University of Pittsburgh, Mount Sinai and the University of Colorado on its march to the championship round. The final score indicated a close contest that Baylor residents say came down to their perseverance.
UVA enjoyed a lead in scoring until the Skills Lab, a new Residents Bowl feature. The “microanastomosis” skills competition saw each team of four players execute a relay-style game – a revolving roster of three players who answered quiz questions, while the fourth moved to a microscope, with four minutes to perform suturing on a rubber-tube model. Baylor’s winner-take-all Skills Lab point total of 2,500 provided the final margin of victory.
Baylor Chief of Plastic Surgery William Pederson, MD, says the skills portion’s emphasis on microsurgery played into one of Baylor’s strengths.

“When we learned it involved a microanastomosis, I knew they’d won,” Dr. Pederson tells PSN. “I told our team, ‘You got this. You do this every day.’ They’ve had as good, if not better, exposure and experience with microsurgery as any other program. Speaking generally, Baylor has excellent residents and an amazing culture. This leads to great teamwork in challenging environments.”
The team, consisting of Amjed Abu-Ghname, MD, Samuel Cole, MD, Austin Jiang, MD, and Anna Skochdopole, MD, says the perseverance and trust the residents have developed throughout their training paid off in New Orleans.
“We had trust in each other’s knowledge and abilities, but also in how well we communicate under pressure,” Dr. Jiang says. “We kept our mind on the task at hand and tried not to worry about winning or losing.” PSN

superpower: The ability to help women with breast cancer and other deformities come out of the darkness.”
She moved to academic positions after realizing that pursuing breast procedures in Florida was neither professionally nor personally fulfilling for her, while other career goals led to another move from Vermont to Kansas, landing at MD Anderson in New Orleans, where she’s chief of plastic surgery. “A straight trajectory isn’t mandatory for a rewarding career – in fact, more personal growth happens when comfort zones are left and risks are taken,” she said.
Kelly Ledbetter, MD, said that plastic surgery leaders must understand today’s trainees have very different points of reference. Programs need to evolve to meet those differences, with today’s trainees valuing mentorship, flexibility, purpose, impact, innovation, technology, meaningful work and wellness. A big factor is the quality of training and curriculum.
“How we teach outside the O.R. really matters,” she said. “Today’s trainees don’t want traditional didactic lectures; they prefer videos and other media. YouTube and TikTok are important, and leaders must teach trainees how to properly utilize these. Be a good mentor, provide work/life balance, be open on your successes/failures, and give quality feedback. Programs must provide a wide-ranging palette
trainees engaged.”
In “Protecting the Future of Plastic Surgery,”
Peter Neligan, MD, 2009 PSF president, described plastic surgery-developed innovations that have been usurped – with the specialty then innovating new approaches and technologies again. He described one particular cranial-based procedure collaboration with three specialties that became safer and more successful than had they each tried alone.
“It was a huge lesson for me,” he told attendees, adding that money holds back more collaboration, as does availability. Ego can also get in the way, which is why he said there is no room for ego in collaboration – referencing the work of Joseph McCarthy, MD, Roger Khouri, MD, Gino Rigoti, MD, and Paul Tessier, MD – and how innovations in other specialties can spur innovation in plastic surgery.
“We need to be the best,” he said. “We need to collaborate. Be there, be nice and be good.”
David Fogarty, MD, DDS, delivered this year’s Noordhoff Lecture and spoke of his reconstruction mission trips to countries including
This year’s Close the Loop 5K, held during Plastic Surgery The Meeting 2025 in New Orleans, drew 191 participants and raised $68,416 to support breast reconstruction charitable care and research. Even if you missed the chance to run in-person in New Orleans, you can still participate in The PSF’s fundraising efforts and sign up or donate at runsignup.com/Race/LA/NewOrleans/BreastReconstructionAwarenessClosetheLoop5K
To date, The PSF’s Breast Reconstruction Awareness program has allocated 188 grants, totaling more than $2 million in awards.
Allergan Aesthetics, an AbbVie company, and Stryker and were this year’s Gold Sponsors; while Apyx Medical, MTF Biologics, Biocircuit Technologies and Integra Foundation were Silver Sponsors. PSN

Nepal, Indonesia, Vietnam, Honduras and the West Indies. Without the teams of volunteers, thousands of children would not have been treated, he said – highlighting the importance of using your gifts as plastic surgeons to care for others.
“If your life’s about you, you won’t be happy,” he told the audience. “It’s got to be about someone else… one of life’s greatest gifts is the opportunity to give, and everyone in here has that ability.”
Beyond self-satisfaction, the rewards culled from these experiences include personal and professional friendships, a widened knowledge base and better cultural understanding. He said everyone has the ability to give back – but it means nothing until that ability’s shared. He noted that he brought patients to the University of West Virgina, 29 have stayed for a period, some for a year – and added that whether in academic or private practice, it’s entirely manageable to donate your time for a few occasions throughout the year.
Maliniac Lecture
David Chwei-Chin Chuang, MD, Taipei, Taiwan, provided a biography of Jacques Maliniac, MD, the namesake of the lecture and renowned giant of plastic surgery – who created ASPS in 1931. Dr. Chaung, a past president of the World Society for Reconstructive Microsurgery, reflected upon previous Maliniac Lecturers, some of whom he personally knew, and regaled the audience with stories and anecdotes. He spoke of plastic surgeons who inspired him – and some of the early cases that helped Dr. Chaung’s career trajectory, including working with brachial plexus injury and reconstruction, about which he has published several books and chapters. He spoke of his “four periods” of brachial plexus reconstruction: Recognition, pessimism, improvement and improvement (part II). He discussed changes in brachial plexus terminology and treatment, successful nerve-related cases in which he was lead surgeon and the evolution of the treatment of several other related conditions.
Kazanjian Lecture
While delivering his “Road Less Traveled” address, this year’s Kazanjian Lecturer, James Zins, MD, revealed an illustrious roster of plastic surgeons who assisted him in his journey to excellence – revealing stories of how he was once told he was “just not college material,” to serving on Good Ship Hope in Masayo, Brazil, where he “really got sold on plastic surgery.”
author Malcolm Gladwell; to illustrate different paths to excellence and different methods through which to arrive there. He advised the use of coaches, to have a plan and set deadlines (they minimize procrastination), and to write solid papers that include valid data and well-written discussions.
Dr. Zins described learning from The PSF past President Peter Randall, MD, and Linton Whitaker, MD, and the difficulties and triumphs of building a plastic surgery training program at Cleveland Clinic. He imprinted upon the audience the importance of completing a postgraduate fellowship, of learning how to write and to present; and of knowing “a lot about a little,” with focused training.
“Don’t be afraid to fail,” he concluded. “Be willing to start over… with lessons learned.”
CranioCheck, a pediatric implant, won top honors in the ASPS Inventors Challenge, a competition that saw four products created by plastic surgeons in competition for a $10,000 top prize and “Top Innovator of 2025” title. Each inventor provided a five-minute presentation about their product, after which a judging panel asked questions and announced the winner. Vying for the prize along with CranioCheck, presented by Jasmine Craig, MD, Madison, Wis., were Doc Paper Scissors, presented by Tripti Burt, MD, Plainfield, Ill.; FitRhap, presented by Steven Bates, MD, San Jose, Calif.; and TissueTape, presented by Justin Sacks, MD, MBA, St. Louis.

He advised early trainees to “do a little each day and you’ll be amazed at what you accomplished in a few years.”
He invoked such figures as The PSF past President R. Barrett Noone, MD; Maria Siemionow, MD, PhD; his “coaches,” Ernest Rosato, MD, and Alden Harkin, MD; tennis great
The CranioCheck pediatric implant monitors cranial pressure without complex equipment or risky procedures. Sans batteries or electricity, it gently changes shape when pressure builds up, with data gathered via simple X-rays. Second place, and $5,000, was awarded to TissueTape which aids closure of tissue planes during abdominoplasty. Its double-sided surgical adhesive bonds to close wounds and eliminates the need for suture closure, later breaking down into biocompatible components.
The ASPS Inventors Challenge judges were Kyle Belek, MD, MBA; Nicole Cabbad, MD; ASPS past President Lynn Jeffers, MD, MBA; The PSF past President Howie Levinson, MD; entrepreneur Bill Perry; Aisha White, MD, MBA; and ASPS past President Steven Williams, MD.
During the Closing Ceremonies, Dr. Hollenbeck and Dr. Matarasso formally passed the gavels to 2026 ASPS President C. Bob Basu, MD, MBA, MPH, Houston, and 2026 PSF President Babak Mehrara, MD, New York. The new presidents immediately assumed their leadership roles and will seek to build on the momentum established this year in New Orleans. Plastic Surgery The Meeting 2026 is slated to take place Oct. 15-18 in Houston. PSN
The following is an edited version of the Opening Ceremonies address of 2025 ASPS President Scott Hollenbeck, MD.
As I stand before this room of remarkable surgeons, healthcare professionals, cherished office staff and guests from around the world, I’m reminded that – while we all come from different places and have different lives – the strength of our specialty lies in both our shared experiences and, more importantly, our shared purpose.
That’s why we are here, to share with one another – our friendships, our opinions, our experiences, our triumphs and our tribulations – all with the goal of becoming better plastic surgeons and providing exceptional and safe care for our patients. This is plastic surgery.
When people outside our specialty hear “plastic surgery,” many immediately think of the cosmetic work we do – along with images of red carpets, glamor and, of course, social media influencers. But we know the reality.
Plastic surgery is also craniofacial reconstruction for a child born with a cleft lip in Nairobi. It’s microsurgery for a breast cancer survivor in rural Missouri. It’s hand surgery for a construction worker in Houston. And, yes, it’s aesthetic artistry for patients seeking greater confidence and transformation whether in Beverly Hills, Manhattan, Toledo or Des Moines.
This is plastic surgery: The integration of form and function, of science and art, of reconstructive resilience and aesthetic precision. Whether we end up in reconstructive or aesthetic careers, there’s no shortcut, substitute or equivalence to the training we receive. In this way, we honor those who came before us – the trailblazers and the innovators who laid the foundation for all we do to help our patients.
We’re special because of the breadth of our training. Aesthetic surgery expertise doesn’t exist apart from reconstructive principles – it’s

built on them. Our understanding of tissue perfusion, flap design, bone modifications, wound healing and tissue remolding are not electives. They are foundational.
The complete plastic surgeon brings an unparalleled skillset to a head and neck procedure such as a facelift or a mandibular reconstruction; a breast procedure such as an oncoplastic reduction, implant augmentation or a microsurgical flap; a hand procedure such as a scaphoid non-union, flexor tendon injury or syndactyly repair; a trunk procedure such as body contouring, hernia repair or liposuction; and an extremity procedure such as an amputation, a rotational flap for osteomyelitis or a medial thigh lift.
Still, if we narrow our range of procedures and place extreme limits on our availability, our unique identity is at risk from others who will gladly step in to perform these procedures with less skill and less training. Likewise, if we only focus on the most lucrative procedures then we will become no different than those who abandon their chosen field to become “cosmetic surgeons.”
I propose that we encourage our students, residents and young surgeons to seek a career that includes both reconstructive and aesthetic surgery. I recall a time in our specialty when almost all the famous aesthetic surgeons had started their careers with a strong reconstructive experience. I fear that’s fading. We must seek individuals who value the full scope of plastic surgery and encourage them to dedicate a portion of their career to serving our hospitals and our communities with their reconstructive skills. Irrespective of their final career destiny, I truly believe they will find it rewarding.
Plastic surgeons are the ultimate problem-solvers. We were born to innovate, and I’m confident many of you in the audience will solve the present and future problems we face in healthcare and within our specialty. However, innovation isn’t just about new flaps or new lift techniques. It’s also about navigating the patient experience, maximizing resources and, now, incorporating artificial intelligence into our daily lives. AI is here, and at ASPS, we’re taking steps to harness this powerful tool in a way that will help our member surgeons achieve more than they ever could have imagined – responsibly.
All this being said, our specialty, our society, our country and the world at large seems to be at a perpetual crossroads. What can we do? I would propose we must remain grounded, collaborative, collegial, innovative, willing to help and optimistic. After all, those characteristics define the very best in plastic surgery. We should find that these behaviors and habits come quite naturally. We should seek opportunities for leadership within our hospitals and communities. This is what ASPS means to me – to step up and become a leader. Whether it’s protecting the specialty through endless advocacy efforts in Washington and across the United States, expanding global humanitarian
and education efforts through programs such as SHARE or building collaborations across the global plastic surgery community, ASPS is about engagement and leadership.
This is ASPS, and this is plastic surgery. It’s not one procedure or one setting or one perspective. Plastic surgery is a discipline, a way of thinking and a commitment to healing – inside and out.
So as your colleague and in my final days as ASPS president, I ask you to stay involved. Lead in your institutions and communities –and mentor the next generation. Celebrate aesthetics – and protect reconstruction. Share your voice and your talent with the world. Be visible and engaged.
When we stand together as plastic surgeons, our impact multiplies, our future strengthens and our patients benefit. Let’s make this meeting and the year ahead one of progress, global connection and pride in who we are and what we do. What is plastic surgery? This is plastic surgery.
On a personal note, I would like to thank my mentors and the people who’ve inspired me in my career, from New York City to Durham, N.C., and now in Charlottesville, Va. I’ve had great fortune and come across so many wonderful people. I want to thank the executive leadership team for their patience and kindness in supporting me, as well as our incredibly talented Board of Directors. I wish C. Bob Basu, MD, MBA, MPH, the best as he becomes your next ASPS president. I look forward to many more years of being engaged in the specialty and the healthcare field overall.
Finally, I want to thank my wife, Julie, who’s here tonight along with my sons, Zeph and Charles. They have put up with endless Zoom calls, scheduling changes and time away – all to allow me to serve you all and our specialty. Everything I have achieved is because of their support. Thank you. PSN
The following is an edited version of the Opening Ceremonies address of 2025 ASMS President Frank Papay, MD.
Each year, this gathering is more than just a meeting – it is a celebration of who we are as a specialty, of the transformative innovations we have introduced to medicine and of the patients whose lives we have forever changed.
From the earliest days of reconstructive surgery after World War I to the development of craniomaxillofacial surgery, microsurgery, composite tissue allotransplantation and the integration of computer-assisted planning –in addition to virtual surgical navigation and simulation – our specialty has not only kept pace with medicine, it has defined it.
Think for a moment about the defining innovations of our field contributed by surgeons and scientists in this room:
• Microsurgery, which gave us the ability to restore form and function with precision unimaginable 50 years ago.
• Craniomaxillofacial distraction osteogenesis, which transformed craniofacial reconstruction and gave new possibilities to children once destined to live with deformity.
• Vascularized composite allotransplan-
tation, which brought face and hand transplantation from science fiction into reality.
• And now 3D surgical planning, simulation and intraoperative navigation, which allow us to achieve the accuracy that once required multiple operations and years of compromise.
These advances are not only technical triumphs – they are stories of vision, courage and collaboration. They remind us that we’re at our best when we look forward, not backward. But here’s my challenge and the theme of this year’s ASMS program: We cannot live on yesterday’s successes. We must become even more innovative so as to increase our scope of practice and compete in an ever-changing, fastpaced technical world.
Scientific discovery, advancing technological adoption – combined with invention and an entrepreneurial spirit – is the fuel that firesup our innovation engine. If we allow ourselves to grow complacent and not feed this fire, others will take the torch and run with it. Some already are.
In addition, patients today have more choices than ever. They do not simply ask, “What surgeon should I see?” They Google. They watch YouTube and TikTok. They look for patient stories, outcomes, brand identity and what the latest technologies are. If they

don’t find us there – if we don’t define who we are and what we offer – others will.
So, what must we do?
First, we must recommit to surgical inno vation. Advances in regenerative medicine, artificial intelligence, robotics and digital twinning are not abstractions – they are tools waiting to be integrated into our specialty.
Second, we must expand our definition of innovation to include communication and ad vocacy. We need to harness digital platforms, patient outreach and strategic marketing to
ensure the public knows the life-changing procedures we can provide. If patients aren’t aware of our capabilities, then our innovations remain hidden.
Third, we must embrace collaboration across specialties without losing our identity. This competitive, collaborative innovation often arises at the intersections of disciplines – but we must lead those conversations rather than watch from the sidelines.
Colleagues, our history is glorious – but it must remain a prologue, not an epilogue. The true measure of our specialty will not be in

The following is an edited version of the Opening Ceremonies address of 2025 PSF President Alan Matarasso, MD.
The PSF was started 77 years ago by Jacques Maliniac, a European immigrant, with a $5,000 savings bond. Today, The PSF funds innovation, fuels research and connects knowledge across borders and generations. It’s more than a foundation – it’s the engine of innovation in our field. Yet, I’m still asked: How is The PSF different from ASPS?
ASPS runs the business of our Society, while The PSF drives the future of our specialty. Here’s an even more basic answer: ASPS is funded by your dues. The PSF is funded by your generosity.
Each year, we review dozens of grant applications. We fund close to $1 million in research and programs annually, but we receive applications asking for more than three times that amount. We can’t predict which new idea will change the specialty, but without donations from plastic surgeons, we may never find out.

I encourage you to participate in The PSF by lending your time and experience by helping to guide young surgeons as they start their careers.
On that subject, I’d like to congratulate the University of Texas Health Science Center in Houston for winning our resident Match Day fundraising competition earlier this year. They raised more than $6,700 for The PSF. Thanks to the contributions of our mem bers and others across the United States and around the world, The PSF this year was able to award more than $600,000 to fund 21 grants to support investigator-initiated re search, fellowships and other initiatives. That’s a lot of money, but as I mentioned earlier, it’s not enough to fund the 112 grant requests that we received. If every ASPS/PSF member gave $375 a year – or about $1 per day – we could triple our grant-making capacity. Plastic surgery is an extraordinary specialty filled with extraordinary people. As surgeons, we operate on the entire body – and while we may not always extend life, we certainly en hance the quality of life. As we say in Spanish, “años buenos y muchos” – good years and many of them. I’d like everyone please take a moment to reflect on how extraordinary you are. Think
about what it took to get here, to get into medical school, into a plastic surgery residency and

The following ASPS/PSF awards were presented by ASPS President Scott Hollenbeck, MD, The PSF President Alan Matarasso, MD, and ASPS Trustee Kant Lin, MD, at the Board of Directors dinner during Plastic Surgery The Meeting 2025 in New Orleans.
Noordhoff Humanitarian Award
David Fogarty, MD, DDS

Dr. Fogarty: When I was told about this award, the floodgates opened beyond my eyes and tears fell on my cheeks – not because I was awarded this prestigious honor, but because 30 other qualified people were nominated. I accept this award for those people who are carrying on volunteerism for the less fortunate around the world. I accept this award for my family, and I accept this award for the late PSF past President Don Laub, MD, who was my mentor and took me on my first volunteer trip to Mexico 50 years ago.
Maliniac Lecturer Award
David Chwei-Chin Chuang, MD

Dr. Chuang: It is my greatest honor to receive this kind of award. I feel very lucky and honored to be part of the tradition that has included names like Dr. Noordhoff and Fu ChanWei, MD. They are fundamental names at Chang Gung and in Taiwan. I hope my lecture lives up to their example – and that you can understand why they chose me for this award.
The PSF Distinguished Career Researcher Award
Jay Austen, MD

Dr. Austen: When I started all this, there were two things I wanted to do: I wanted to be an innovator and I wanted to become a better teacher. Early on, I thought I was a terrible teacher, and until now, the most important award I’d ever received was the Harvard Teaching Award – because I had to really work at it. It meant something. This really means something too, and I thank you for it.
The PSF Distinguished Career Researcher Award
Bahman Guyuron, MD

ASPS Presidential Award
Jeffrey Janis, MD

Dr. Guyuron: As David said, it’s about the combination – the team – and not the individual. I’m delighted that I’ve had so many researchers over the years, some of whom are in this room. I could not have accomplished all of what I accomplished without you and everyone else. So I thank you.
The PSF Distinguished Service Award
James Zins, MD

Dr. Matarasso: Dr. Zins has written more than 250 peer-reviewed publications – predominantly in the areas of resident education, facial aesthetic and craniofacial surgery. He has edited five textbooks and oversaw 30 book chapters. He has served as president of AAPS, director of the ABPS, member and Vice Chair of the Resident Review Committee of Plastic Surgery of the ACGME.
The Maliniac Circle Award for Outstanding Support of The PSF
Scott Spear, MD (posthumous)

Dr. Matarasso: Scott Spear’s influence around the world as an educator and innovator was tremendous. He was invited to serve as faculty at virtually every breast conference around the world. To this day, it is almost impossible to attend a breast conference where he isn’t mentioned by name. He always made himself available to answer questions about relevant issues and thoroughly enjoyed his role as a teacher. His contributions to the development of breast implants and breast surgery are unparalleled.
ASPS Special Achivement Award
Robert X. Murphy Jr., MD

Dr. Murphy: Plastic surgery is a team sport – what we do for our patients, each other and the community is a team effort, and to receive recognition for being part of that is humbling. I accept this award on the basis of what we do every day, what we do for the specialty and why we are plastic surgeons. Thank you.

Dr. Janis: This room is filled with people – all of whom are known to plastic surgery and to our patients – and it’s an honor to have served with each and every one of you. I don’t feel that I deserve this honor, but I do want to acknowledge that I’m so grateful to be friends and colleagues with all of you. Plastic surgery is a journey and I learn so much from all of you. Thank you very much.
ASPS Honorary Citation
Lloyd Gayle, MD

Dr. Gayle: I’ve got to echo what Dr. Murphy said. I’m basically a utility player. I see problems, I try to fix problems and I try to honor my patients in providing the best care I can. At the same time, I enjoy the camaraderie of our specialty and the potential to educate the next generation. We all stand on the shoulders of giants – but we enjoy creating the new giants for the next generation as well. I’m honored – thank you.
ASPS/PSF Level 5 Leader Award
Arun Gosain, MD

Dr. Gosain: Speaking to a room of leaders, it’s hard to say anything that hasn’t been said about leadership. We all know leaders who get to a position because they walk over others to get there with a goal of just having the title or position. But a true leader is a servant leader – someone who realizes and serves the needs of the organization. That means the people around you are not trampled upon, but elevated. I’m hoping we can continue to work together to achieve a common cause. PSN





































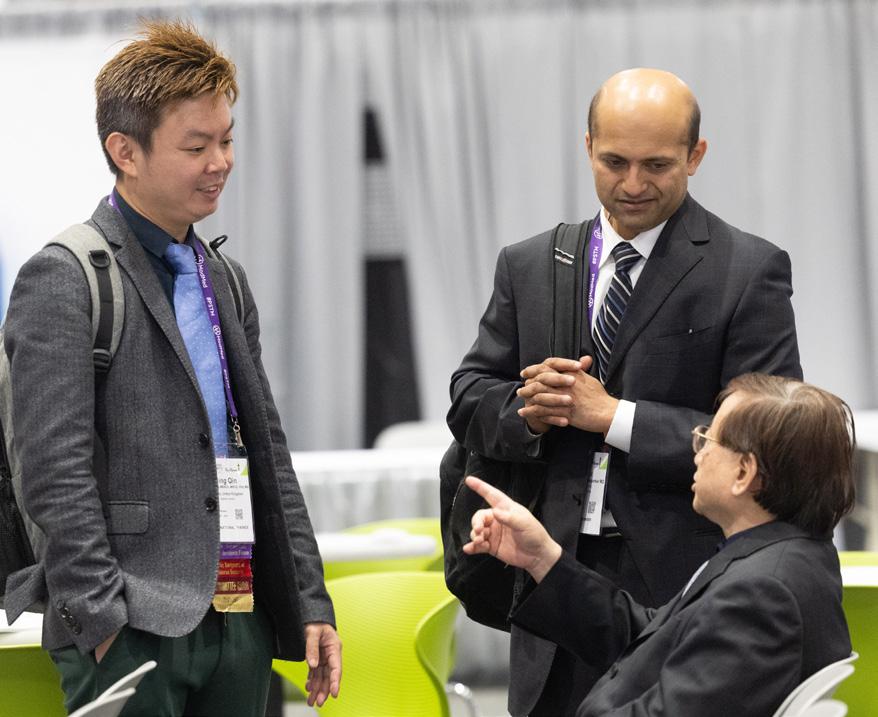








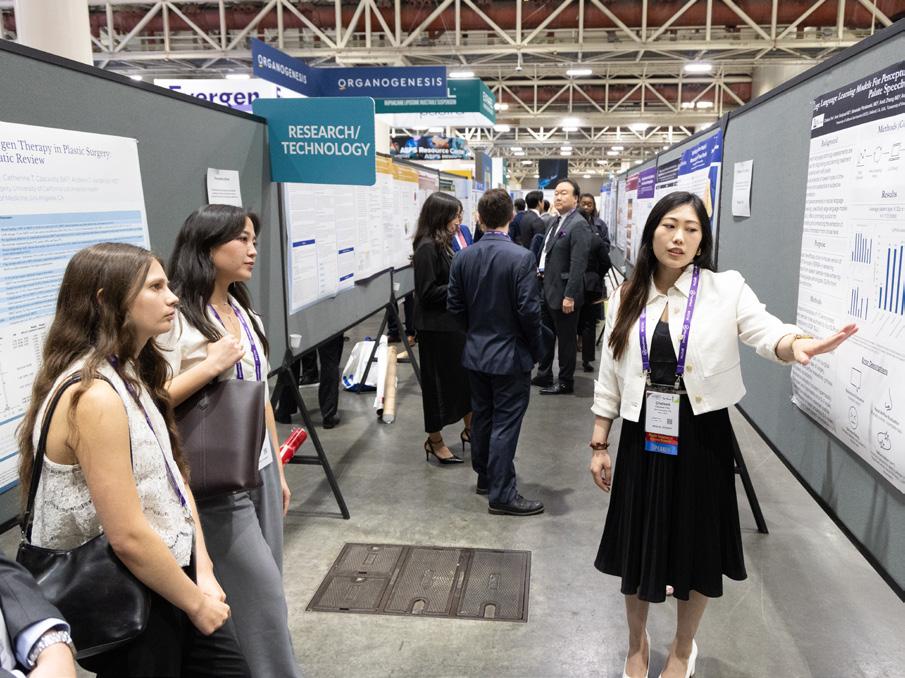




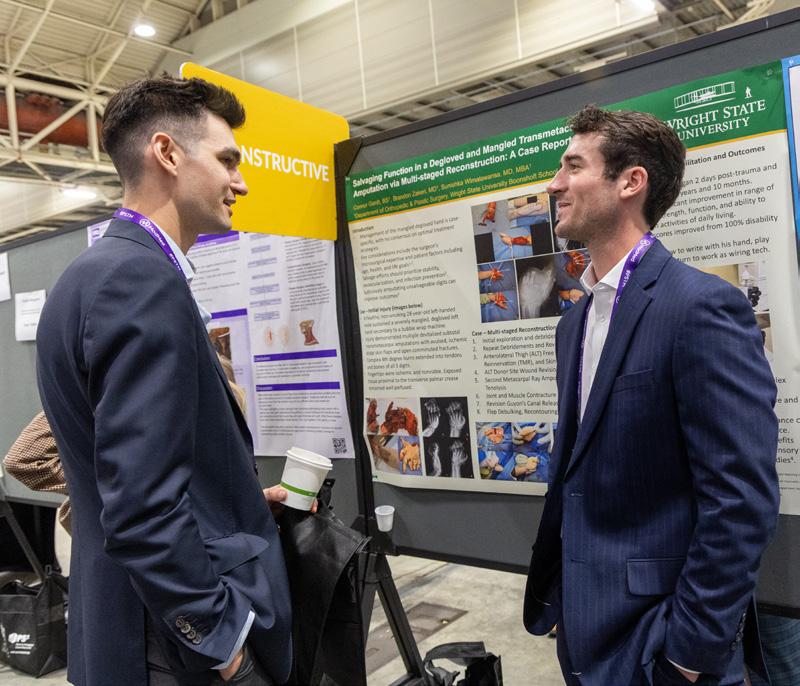









the value proposition of having a plastic surgeon’s support.
be able to fight that. Uniting on a common cause is really important.
Dr. Vyas: With increasing encroachment from various specialists who do aesthetic and reconstructive work – and some states considering expanding legislation around scope – what specific legislative and educational strategies will ASPS and The PSF pursue to protect plastic surgery’s domain and ensure patient safety remains paramount?
Dr. Basu: ASPS has a robust advocacy infrastructure made up of engaged members and an exceptional staff with deep policy expertise. Over the years, we’ve built meaningful, bipartisan relationships with legislators at both the state and federal levels. Our strategy begins with education. ASPS helps decision-makers understand the unique value that board-certified plastic surgeons bring to patient care, and why our training and standards directly translate to safer outcomes for their constituents. Legislatively, we will continue to oppose unsafe scope expansions, support state societies with coordinated advocacy efforts and mobilize our members – who are often the most influential voices at the state level. On the educational side, we will continue to strengthen public awareness about the differences in training between plastic surgeons and other providers. When patients understand those differences, they demand safer care, which reinforces our position with legislators. We won’t win every battle. But keeping our voice loud, consistent and credible – and tapping into our members on the frontlines – is key to protecting our specialty and ensuring patient safety.
Dr. Mehrara: For a long time, we’ve been on defense. We need to go on offense. Plastic surgeons need to take control of their patient flow. If you really love breast reconstruction, then maybe we should start building it into our curriculum. You can have breast reconstruction fellowships that come with a certificate recognized for the ACGME. At the end of the day, you’re not going to stop an MD from operating, but all of us have treated patients who’ve had surgery by unqualified practitioners and been horribly deformed, injured, etc. Those would make good social media posts and patient stories – documenting their journey and what happened, and then how a board-certified plastic surgeon helped them recover. People don’t always understand when you talk about complications. We must do a better job of telling the story of what can go wrong and
Dr. Vyas: AI still raises questions about liability, training requirements, data privacy and maintaining the human element of surgical care. What’s your vision for how ASPS should guide the specialty’s adoption of AI tools – and what policies or educational initiatives will you champion to ensure plastic surgeons remain at the forefront of technology innovation while addressing these concerns?
Dr. Basu: AI offers tremendous opportunities for our specialty – particularly in practice management, billing, appeals and other time-consuming tasks that burden both private practices and academic departments. ASPS is also evaluating AI for improving registry data, society workflows and initial patient engagement, while ensuring the human element of surgical care remains central. As we modernize our consumer-facing website, we’re working with partners who understand the rapid evolution of AI. Our goal is to better capture and route the millions of annual public visitors directly to our members’ practices in a safe, ethical and effective way.
However, we also have to address the risks, such as misinformation, AI-generated before-and-after images and misleading content that can distort patient expectations. ASPS should lead in establishing ethical guidelines, consumer education and clarity around what is real and safe, reinforcing the Society as the trusted authority for patients.
What’s promising is how AI search tools are reshaping how patients find physicians. Generative AI increasingly pulls from authoritative sources, and ASPS – and board certification through ABPS – consistently carry the highest authority in these platforms. Early data show that 60-70 percent of patients now use AI to find or validate their doctor. Those searches strongly emphasize the importance of choosing a board-certified plastic surgeon. Although some of our members might be frustrated, thinking board certification may not matter or patients may not care, I do think we’re going to start seeing the pendulum swing back. We must remain vigilant around privacy, liability and training requirements, but I’m optimistic. With thoughtful policy, strong ethics and continued education, ASPS can ensure plastic surgeons stay at the forefront of innovation while AI actually helps reinforce the value of our specialty and protects patients seeking safe, qualified care.
Dr. Mehrara: From an education standpoint, there’s a tremendous amount of information
and it’s hard for anyone to keep up-to-date with ongoing advancements. One of the things we’re working on is how AI can be used to help members get the most recent, as well as historical, clinical information. We’re hoping to prevent AI hallucinations as much as possible by limiting the source data. I think you can expand that to, for example, a breast module that provides data on treatment for breast cancer or other things that we need to be experts at.
Dr. Basu: Let’s say a resident is on call and they get a consult. They can type in “breast implant cellulitis” and quickly pull evidence-based recommendations with supporting publications with the current level of evidence. Rather than doing a query on PubMed, they could use this tool, find the articles, the level of evidence and go forward. ASPS is making bold, forward-thinking investments in new technologies. As I said before, this is not your parents’ physician organization. We are committed to being proactive, leading from the front and embracing innovation rather than waiting for someone else to do it for us. First movers have a real advantage, and ASPS intends to stay ahead of that curve.
Dr. Tanna: Short, high-quality videos are proven tools for education for surgeons and patients, trainees and consumers. They can help patients better understand procedures and help surgeons learn the latest techniques, ultimately improving outcomes. What strategies do ASPS and The PSF have around digital video education to maximize impact for both patients and member surgeons?
Dr. Mehrara: We have a wealth of information already available, involving both procedures and patient information. We need to take that to the next level. Virtual-reality videos would be tremendously helpful for surgical teaching. We haven’t really discussed it, but that would be the direction I would want to head because virtual reality glasses will become widely available within the next five years. That will provide a whole different level of experience for both patients and students.
Dr. Basu: The Society recently launched our new EdNet platform, and we’re seeing tremendous demand for high-quality on-demand video education. If a member misses a session at PSTM, they can now go back and access that content. We’re actively building this library, and with our upcoming customizable website, we plan to fully integrate EdNet’s content management system. The goal is a seamless, personalized learning portal where every member can easily access the education most relevant to their practice.
Dr. Yoon-Schwartz: What do you see as some of the financial challenges still existing for our Society? And do you have any plans that can help overcome those challenges?
Dr. Basu: ASPS not only weathered the COVID-19 pandemic but emerged from it in a remarkably strong financial position – something very few physician organizations can say. I still recall people joking, “You’re taking over as Board Vice President of Finance during COVID? Good luck!” I’m happy to report ASPS is in a strong financial position. That said, every organization faces ongoing financial pressures. We can’t pursue every idea or initiative as there will always be limitations in staff capacity and resources. To stay focused, ASPS relies on a formal strategic plan that helps us prioritize projects with the highest member value and the greatest long-term impact. At the same time, we’ve built the ability to remain nimble and opportunity-driven. We maintain a dedicated strategic investment fund – separate from our endowments – that allows us to move quickly on new programs, technologies or member services when the right opportunities arise. This balance of discipline and agility allows us to continue navigating financial challenges while still investing in initiatives that advance our specialty and support our members.
Dr. Snyder-Warwick: Surgeon scientists are minority members of our specialty, and there’s a lot of uncertainty currently surrounding federal funding – and a somewhat bleak outlook for a lot of people in an already small but important part of our membership. How can The PSF provide additional support for those engaged in research? How can we further work to inspire trainees to pursue research in their own careers and not look at us and think, “No way am I doing that?”
Dr. Mehrara: It’s hard. In my department, the funding process has become more difficult, progressively, almost every year. The process of federal funding is probably not a great option for most people, so I think we’d have to rely on pharmaceutical companies, device companies, societies and other sources – perhaps internal funding. Hopefully this will foster some innovation. Basic science research is difficult. My guess is the funding lines are going to go down below 10 percent and you’ll have to beat out, you know, 90 percent of all grants to get funded. And you’re competing against people who do this as a living. For us, it’s a part-time job. I think the educational ideas we have will hopefully help people write better grants. I don’t think our clinical research will change –and plastic surgeons are curious by nature – so
whether there’s funding or not, we’ll figure out a way to do it. It may spur us to do better.
Dr. Snyder-Warwick: Do you think that as a result of innovation by necessity, people will develop other areas of research in addition to clinical, basic and translational?
Dr. Mehrara: Plastic surgeons are smart, innovative and resourceful. It’s hard to keep us down. My guess is there’ll be a lot more interaction with device companies and pharmaceutical companies. They’re a good source of funding and our interests largely align because we want to take care of patients and do the right thing. These companies are good at doing the initial work, but clinical translation is something they’ll always need help with.
Dr. Tanna: With reimbursement pressures and increasing coding decisions impacting access to reconstructive surgery, what strategies will ASPS and The PSF take proactively to protect fair payment and access for patients for reconstructive surgery?
Dr. Basu: Reimbursement pressures are one of the toughest challenges we face, and there’s no single formula that can overcome the headwinds coming from CMS and private payers. Protecting access to reconstructive surgery will continue to rely heavily on strong, persistent advocacy within the house of medicine at the AMA and directly with federal policymakers. The good news is that, even as a relatively small specialty, ASPS consistently punches above its weight and we’ve earned credibility that allows our voice to be heard. At the same time, we need to support members with practical, creative strategies for improving private-payer reimbursement. This includes optimizing revenue cycle management, exploring carve-out arrangements and helping practices develop sustainable out-of-network strategies when appropriate. ASPS members can also leverage PS², our practice management consulting service, for individualized guidance to strengthen financial performance.
Dr. Mehrara: At the risk of sounding like a broken record, we need to move toward departments of plastic surgery. We’re paying a huge overhead tax to the department of surgery and literally carrying many other divisions, which is fine, but that impacts plastic surgery to a much larger degree than people know. If you look at most departments of surgery, you’ll see that plastic usually brings in somewhere between 25-35 percent of the revenue for the entire department. So when you’re under the dean and the department of surgery, a lot of your collections are simply going out of your hand. Hopefully, as a Society, we can figure out a way to do that – so that we aren’t forced to fight those battles individually. It’s kind of aspirational, but we need to head that way, because it’ll help us have a stronger voice and keep more of what’s ours.
Dr. Vyas: In learning at our institution about how we went from a division to a department –and all the benefits we get from that – it seems like that transition was luck, timing and politics all coming together. How does ASPS advocate for that to be across the board? Has there ever been an attempt to do that at a Society level?
Dr. Basu: These conversations have absolutely taken place within the Academic Affairs Council, and this remains on our radar. ASPS provides a powerful network for academic leaders to share best practices and learn from institutions that have successfully transitioned from division to department status. That said, there is no universal blueprint. Every academic environment has its own dynamics – finances, research portfolio, institutional politics, who the dean is, the relationship with the chair of surgery and many other factors. The key is for academic leaders to stay alert for the right moment and recognize when the alignment of opportunity, support and institutional priorities make that transition possible.
ASPS can facilitate the dialogue and provide the network, but the strategy must be tailored to each institution’s unique landscape.
Dr. Mehrara: Our position is getting better. Years ago, we were dependent on general surgery, because our residents rotated. They had to do general surgery before they came to us. Now we’re independent of that. We need to come up with a better centralized strategy to approach this – not on an individual basis, but rather as a collective.
Dr. Vyas: The SHARE program is one of the initiatives The PSF offers that is a wonderful game changer. I’m on the leadership team, and I direct the clinical research curriculum that we share with our Global Fellows. How do you envision expanding the program’s impact? And what role should ASPS members play in supporting sustainable surgical education infrastructure development internationally?
Dr. Basu: SHARE leadership has done a phenomenal job, and its success stems from its strong sense of purpose. We volunteer because we know we’re making a genuine impact, and that mission resonates deeply with our members. I absolutely want to see SHARE expand its reach. That includes increasing staff support, elevating its visibility at the Board level and giving it a stronger presence at PSTM – such as a dedicated SHARE booth in the Exhibit Hall or a high-profile event to showcase its work. I also want to amplify its global visibility so that more of our international members can engage, collaborate and help strengthen sustainable surgical education around the world. ASPS members play a critical role in that effort. Their expertise, mentorship and willingness to serve are the backbone of SHARE – and expanding that engagement will allow the program to touch even more communities and build lasting educational infrastructure internationally.
Dr. Mehrara: The best thing about plastic surgery: What we do, you see right away. If the general surgeon takes out an appendix, it’s great – but if you have a patient who has a burn contracture and can’t use their arm and you help them with that, it’s an immediate thing that you both see. The impact is tremendous, and that’s why it makes us feel so good about what we do. Making the world a better place appeals to our nature. Expanding SHARE to our glob
al partners will be amazing, because our reach will be bigger. Perhaps we can even extend it to things that are not so esoteric, or to areas that are not so underserved. Microsurgery, for example, is still not commonly performed in a lot of places. Being able to share some of those skills with people who have a good training in plastic surgery, but not necessarily microsurgery, would be great.
Dr. Yoon-Schwartz: What do you see as the most important current and future challenges for our specialty as a whole?
Dr. Basu: Scope-of-practice battles remain one of the most significant challenges – and they will only intensify as financial pressures and declining reimbursements push more providers into areas traditionally managed by plastic surgeons. I used to feel somewhat pessimistic about this trend, but recent shifts in consumer behavior give me optimism. As patients increasingly turn to AI-driven search tools for medical information, these platforms consistently highlight the importance of choosing a board-certified plastic surgeon. That presents a real opportunity for us to reshape the narrative and reinforce what sets our specialty apart. It won’t end scope battles, but it does strengthen our position. We must stay proactive. That includes exploring innovative approaches, such as accreditation strategies and clearer differentiation of training and qualifications, to help the public, policymakers and patients understand the unique value we bring.
Dr. Vyas: Craniofacial actually did that. Last year, they went toward the Fellows who just graduated and were the first class to sit for a CAQ in craniofacial.
Dr. Basu: The challenge with that, though –let’s take hand surgery. Does a consumer know about a CAQ in hand?
Dr. Vyas: No, but when you’re arguing to your hospital that you should be the one running the cleft program or a hand program – and not this other person because they don’t have this – it gives you something on paper.
Dr. Tanna: Or you’ll feel bad when someone from another specialty comes up with it.
Dr. Vyas: That’s what actually pushed the
with their own CAQ. There isn’t one for breast or microsurgery.
Dr. Basu: You’re right. There’s an absolute arms race for this. It’s a difficult balance. Do we need to pursue a CAQ, subspecialty accreditation or whatever else there might be – or are our members going to be unhappy with that? “I went through all this training, I do my MOC and now I have to do one more thing?”
Dr. Yoon-Schwartz: With regard to young surgeons coming through – whether in institutional employment or private practice – there’s a lot of new corporatization of medicine, and I think our specialty has become part of that whole world. Could you share your perspectives on that, and what advice you can give our members about optimizing their positions in this climate?
Dr. Basu: Every practice environment is different, and there’s no one-size-fits-all answer. ASPS has been striving to provide our members the tools to critically evaluate their individual opportunities – whether they’re entering institutional employment, joining a group or considering private equity.
In some situations, joining a larger entity can dramatically improve access to reconstructive work and reimbursement. For surgeons in their final 5-10 years of practice who have built significant value, a private equity partnership may make sense. However, for early-career or mid-career surgeons, the limitations and long-term trade-offs of working within a PE-owned structure might be far less favorable. The key is due diligence. ASPS will continue to support members through panels, webinars and educational resources that help them assess these decisions through a business, legal and professional lens.
Dr. Vyas: What’s your favorite song, band or type of music to play in the office or O.R.?
Dr. Basu: It depends on my mood. I listen to diverse genres from hip hop, pop, techno, international, country, etc. As a default, I tend to go back to ’80s music. It’s the music that I grew up with and puts me and most – though not all –of my O.R. team in a happy place.
Dr. Mehrara: Me, too – ’80s music is the go-to. But there are definitely days where I play heavy metal. It’s not very popular with the nurses. PSN

Getting an edge in the SEO game isn’t always easy, but with a Connect profile on the ASPS Find a Surgeon referral service, it can be.
Add a backlink to your practice website from PlasticSurgery.org to let search engines – and real people looking to become patients – know you’re not just any practitioner, you’re an ASPS Member Surgeon.
The Society welcomed the following surgeons into ASPS on the October 2025 ballot for Active and lnternational membership. ASPS has a formal membership process which requires an application, letter of sponsorship, board certification, adherence to ethical standards and more. The Society extends a warm welcome to its new members.
California
Daniel Chang, MD
Bryan Curtis, MD
Bao-Quynh Julian, MD
Emma Koesters, MD
Amie Miller, MD
Anita Mohan, MBBS, PhD, MBA, MRCS
Florida
Michael Keyes, MD
Jerette Shultz, MD
Eric Weiss, MD
Georgia
Spencer Anderson, MD
Thomas Hagopian, MD
Idaho
Louis Poppler, MD, MSc
Illinois
Courtney Cripps, MD

Kentucky Alisha Paranzino, MD, MS
Maryland
Neha Datta, MD
Jason Wink, MD
Massachusetts
Krystle Tuano, MD
Minnesota
James Drinane, DO
Montana Christopher Stewart, MD
New Jersey
Steven Ovadia, MD
Mark Yazid, MD
Argentina
Nicolás Vila, MD
Australia
Yezen Sheena, MBBS
Brazil
João Carlos Oliveira Lima, MD
Victor Lima, MD
Nelson De Paula Piccolo, MD
Rodrigo Gouvea Rosique, MD, PhD
Chile
Juan Pablo Camacho Martino, MD
Giovanni Vivas Rosales, MD
Colombia
Diego Arango Ardilla, MD
Nadia Patricia Betancourt Justinico, MD
Rodrigo Munera Velez, MD
Dominican Republic
César Augusto Peralta Fernández, MD
Ecuador
Armando Jose Serrano, MD
Egypt Yasser Helmy Ismali Ali, MD Sherihan Mohamed, MD
Germany Mirko Przybilski, MD
Guatemala Rigoberto Avila, MD
Iraq Paiwand Mahmood Ali, MD
Italy
Marco Marcasciano, MD, PhD
Massimo Massatani, MD
Japan Toshiro Imai, MD, PhD
Kenya Nang’Andu Amanda Malungo, BScHB, MBChB, MMed
New York
Elan Horesh, MD
Sergei Kalsow, MD
Alfredo Lloreda, MD
North Carolina
Vanessa Parada, MD
Ohio
Raymond Isakov, MD
Michelle Sieffert, MD, MBA
Brian Starr, MD
Ontario, Canada
Jerome Edelstein, MD
Oregon
Monica Llado-Farulla, MD
Pennsylvania
Sean Li, MD
Jason Jaein Yoo, MD
Tennessee Carey Campbell, MD
Lauren Connor, MD
Maelee Yang, MD
Texas
Natalie Barton, MD
Roger Cason, MD
Edward Salim Chamata, MD
Berry Fairchild, MD
Austin Ha, MD
Philip Hanwright, MD
Phuoc Thien Nguyen, MD
Christopher Parham, MD
Paymon Sanati-Mehrizy, MD
Hope Shin, MD
Washington
Grace Um, MD
Wisconsin
Suzanne Inchauste, MD
Mexico
Adda Sanchez Durazo, MD
Arturo Mendez Escudero, MD
Alejandro Lopez Gaxiola, MD
Raul Manuel Cedillo Lopez, MD
Luis Fernandez de Cordova Rio De La Loza, MD
Jose Guillermo Segura Medina, MD
Fabiola Rosano Soriano, MD
Peru
Percy Nunez Villar, MD
Portugal
Luis Ferreira Mata Ribeiro, MD
Romania
Dana Miricioiu, MD
Saudi Arabia
Amr Abdalla Ibrahim, MRCS, MS, MSc
Spain
Guillermo De Piero Belmonte, MD
Mike Dewever, MD
Taiwan Ching-En Chen, MD
Turkey
Isil Akgun Demir, MD
Safa Manav, MD
Süleyman Özer, MD
Yunus Saglam, MD
Baris Yigit, MD
United Arab Emirates
Vikesh Vij, MD
United Kingdom
Bejamin Baker, BMBS, BA
Venezuela
Jose Rosales, MD
Maribel Sanchez, MD
Aquiles Siverio, MD

For additional ASPS/PSF meeting information, visit the Meetings & Education page at www.plasticsurgery.org/meetings; e-mail registration@plasticsurgery.org; or call (800) 766-4955 / (847) 228-9900. Dates, locations and program information are subject to change without notice.
RENEW YOUR MEMBERSHIP FOR 2026!
Subscriptions:
• Plastic and Reconstructive Surgery Journal ® (PRS)
• Plastic Surgery News ® (PSN)
• ASPS Education Network (ASPS EdNet)
Members-only Access:
• Products and services to help grow your practice
• Inclusion on Find-A-Surgeon feature on PlasticSurgery.org
• Member discounts on educational meetings and symposia
• Advocacy that focuses on public and private sector issues, so you can focus on your practice
13-14
ASMS Pediatric Plastic Surgery Course
New York
Contact: (978) 927-8330
Web: maxface.org
13-17
American Association For Hand Surgery Annual Meeting
Chula Vista, Calif.
Contact: (978) 927-8330
Web: meeting.handsurgery.org
16-20
American Society for Reconstructive Microsurgery Annual Meeting
Chula Vista, Calif.
Contact: (312) 456-9579
Web: microsurg.org
16-18
American Society for Peripheral Nerve Annual Meeting
Chula Vista, Calif.
Contact: (978) 927-8330
Web: meeting.peripheralnerve.org
28-30
LIMITLESS Leaders Summit
Palm Springs, Calif.
Contact: (847) 228-9900
Web: plasticsurgery.org/limitless
Jointly provided by ASPS, The Aesthetic Society and the American Hernia Society
30-Feb. 1
WPS Symposium
Palm Springs, Calif.
Contact: (847) 228-9900
Web: plasticsurgery.org/wps
Directly provided by ASPS
30-Feb. 1
Southeastern Society of Plastic and Reconstructive Surgeons 41st Annual Atlanta Breast Surgery Symposium

Atlanta
Contact: (435) 901-2544
Web: sesprs.org
2026
12-15
American Council of Educators in Plastic Surgery 13th Annual Meeting
Nashville, Tenn.
Contact: (978) 299-4510
Web: aceplasticsurgeons.org
27-March 1
ASPS Spring Meeting
Online
Contact: (847) 228-9900
Web: plasticsurgery.org
Directly provided by ASPS
5
In-Service Self-Assessment Residents Exam
Online
Contact: (847) 228-9900
Web: plasticsurgery.org/exams
Directly provided by ASPS
5-8
Mountain West Society of Plastic Surgeons 11th Annual Meeting
Vail, Colo.
Contact: (847) 228-9900
Web: mwsps.org
Jointly provided by ASPS
13-14
ASPS Plastic Surgery Coding Workshop
Online
Contact: (847) 228-9900
Web: plasticsurgery.org
Directly provided by ASPS
21
Northeastern Society of Plastic Surgeons Spring Meeting
New York
Contact: (978) 927-8330
Web: nesps.org
8-June 3
In-Service Self-Assessment Surgeons Exam
Online
Contact: (847) 228-9900
Web: plasticsurgery.org/exams
Directly provided by ASPS
10-12
California Society of Plastic Surgeons 76th Annual Meeting
Huntington Beach, Calif.
Contact: (978) 927-8330
Web: californiaplasticsurgeons.org/meeting
1-3
International Aesthetic & Plastic Surgery Meeting Dubai
Dubai, United Arab Emirates
Contact: +97143116323
Web: iamplast.com
2-5
American Association of Plastic Surgeons 104th Annual Meeting Lihue, Hawaii
Contact: (978) 927-8330
Web: meeting.aaps1921.org
By Lawrence B. Keller, CFP, CLU, ChFC, RHU, LUTCF
Editor’s Note: From time to time, PSN provides space for ASPS Endorsed Partners to offer insight on market trends, new products and company offerings as a way to highlight collaboration between Society leadership and industry.
Although the disability insurance landscape has evolved gradually, recent innovations have made what was once old new again. Insurers have expanded guaranteed standard issue (GSI) offerings, creating new pathways for professionals to secure coverage even when traditional underwriting would pose challenges.
A GSI plan is an individual disability insurance policy that doesn’t require medical underwriting. It’s identical to a traditionally underwritten policy from the same carrier, except certain features – such as mental/nervous and/or substance abuse disorder limitations and maximum monthly benefits – are predetermined.
Guardian, Standard and Ameritas are the insurance companies leading the charge in making GSI coverage available to medical residents and Fellows.
Endorsed programs are formally supported by the institution or Graduate Medical Education (GME) office, which promotes the plan to residents and Fellows through official communications and benefit materials.
Non-endorsed programs, by contrast, are
Legislative Update
Continued from page 12
fixed overhead when care is delivered outside the hospital. Conversely, CMS will reduce the allocation of indirect costs to PE RVUs in facility settings, arguing that hospital-based physicians no longer bear those expenses directly.
Additionally, CMS will begin using data from the Hospital Outpatient Prospective Payment System to set relative rates for selected technical services, such as radiation treatment and remote monitoring. For plastic surgeons, the implications of these methodological changes depend on the practice model. Surgeons operating predominantly in office-based or ASC settings may see a modest improvement in relative reimbursement, while those working largely in hospital outpatient departments may experience small declines. The revisions reinforce CMS’s emphasis on “site-neutrality” and on tying payments more closely to measurable cost-data rather than historical surveys.
CMS continues to expand telehealth and supervision flexibilities that were introduced during the COVID-19 public health emergency. For 2026, the agency is streamlining the process for adding services to the Medicare Telehealth List by removing the distinction between “provisional” and “permanent” categories. CMS will now simply assess whether a service can be safely and effectively delivered via interactive, twoway audiovisual communication.
Another significant change is the permanent adoption of a definition of “direct supervision” that allows supervising physicians to be virtually present through real-time audiovisual technology for certain incident-to services and diagnostic tests. This option applies to most services except those with 10- or 90-day global periods, which encompass the majority of operative plastic surgery codes. Consequently, while major surgical procedures remain excluded, this change could fa-
independently offered by agents and may not be recognized or supported by the institution. Accordingly, inquiries to GME offices may not yield information on these opportunities.
One of the most significant challenges surrounding GSI availability involves the rules governing eligibility. Applicants who pursue medically underwritten coverage and are subsequently declined or modified may become ineligible for the GSI offer.
According to the Milliman 2024 Annual Survey of the U.S. Individual Disability Income Insurance Market, 53 percent of individual disability insurance policies are either modified (34 percent) or declined (19 percent).
• Recently had surgery or had surgery where hardware was placed
• Have seen a chiropractor for treatment or have been to physical therapy recently
• Are currently pregnant or have a history of infertility or complications of pregnancy
• Have been diagnosed with anxiety/depression, ADD/ADHD, or see a therapist
• Have been diagnosed with psoriasis or psoriatic arthritis
• Have a history of have been diagnosed with a sleep disorder

Therefore, if one is available at your institution, with few exceptions it should be your first choice – regardless of the insurance company offering it. GSI disability insurance isn’t a backup plan or something to be viewed as being “not as good” or as “cheap” compared to a fully underwritten policy.
Common conditions that often result in modified or declined offers include:
• Have been diagnosed with diabetes or pre-diabetes
• A history of cancer
• A history of self-prescribing
• A history of musculoskeletal issues such as back or neck pain
cilitate more flexible staffing and supervision for ancillary services within a plastic surgery practice – particularly those involving preoperative evaluations, imaging or postoperative wound care provided by physician extenders.
Finally, CMS again solicited public comment on strategies to improve the accuracy of payment for global surgical packages, including the potential revision of postoperative care valuation and transfer-of-care modifiers. Although no reforms were finalized, CMS signaled its intent to continue refining global package payment models – an area of ongoing interest and concern for surgical specialties.
For reconstructive surgeons, one of the most consequential changes in the 2026 rule is the overhaul of how Medicare pays for skin substitutes, also known as CAMPs (Cellular, Acellular, and Matrix-like Products) or CTPs (cellular and tissue-based products). Until now, most of these materials were paid separately under Part B using the average sales price (ASP) methodology, with each product assigned its own billing code and rate. Spending in this category ballooned in recent years – from about $250 million in 2019 to more than $10 billion in 2024 – prompting CMS to redesign the payment system.
Beginning in 2026, CMS will pay for covered skin-substitute products as incident-to supplies when they are used as part of a covered application procedure in both office and hospital outpatient settings. The agency will group products by their FDA regulatory category – PMA, 510(k) or section 361 HCT/P – and set a single payment rate across all three for the first year, based on hospital outpatient utilization data. In future years, CMS plans to differentiate rates across these regulatory categories. The initial rate is $127.28 per square centimeter before geographic adjustments. Products that are licensed as true biologics under section 351 of the Public Health Service Act will continue to be paid under the traditional ASP methodology, and non-sheet products such as gels or powders will be priced
Some GSI plans include a 3/12 pre-existing condition(s) limitation. This means there’s no coverage for a disability beginning in the 12 months after the policy issue date if it’s caused by a pre-existing condition (a condition for which the insured sought, or for which a prudent person would have sought, medical treatment during the three months prior to the issue date). After you have owned the policy for 12 months, even pre-existing conditions will be covered.
To run an instant, personalized quote, go to disabilityquotes.com/plastic
Guardian has introduced an Accept/Reject Disability Insurance Program available exclusively to ASPS members age 50 or younger.
The Accept/Reject Program allows ASPS members to secure an individual disability insur-
separately by the Medicare Administrative Contractors.
For plastic surgeons who perform wound care, grafting or burn reconstruction, this new policy represents a major change. The uniform rate will flatten reimbursement for many products, reducing payment for some higher-cost materials and compressing margins in office-based care. Practices should review their product mix, supplier contracts and billing processes ahead of January. Although CMS frames the move as an effort to curb fraud and excessive costs, surgeons worry that it could limit access to advanced biologic products that improve outcomes for reconstructive patients.
Taken together, the CY 2026 PFS final rule presents a complex financial landscape. The modest increase in the conversion factor provides limited relief from long-term payment erosion, while the efficiency adjustment introduces a new layer of uncertainty. For specialties such as plastic surgery, which rely heavily on non-time-based codes, the cumulative impact could be significant.
Practices should begin by modeling their revenue projections under the new RVUs, paying particular attention to high-volume CPT codes that are non-time-based and therefore subject to the efficiency adjustment. Employment contracts that tie compensation to work RVUs will need to be revisited to ensure fairness under the new valuation. The potential downward drift in work RVUs may also affect benchmark data used in physician productivity comparisons and could distort compensation models if not corrected.
From an operational standpoint, surgeons might benefit from examining their site-ofservice distribution. Because CMS now recognizes greater indirect costs for office-based care, performing more procedures in accredited office-based O.R.s or ambulatory surgical centers could yield relatively higher payments than similar cases performed in hospital outpatient departments. This trend aligns with broader policy efforts toward site-neutral re-
ance policy with a substantial monthly benefit of up to $15,000. This program allows members to apply for up to $15,000 in monthly benefits with simplified underwriting. Applications are evaluated on an accept/reject basis – approved policies are issued without medical exclusions, substandard ratings or benefit reductions. Non-citizen members may still receive travel exclusions under standard guidelines.
Members outside the program’s age or underwriting parameters may still qualify for Guardian’s fully underwritten coverage, which includes a 10 percent association discount.
To run an instant, personalized quote, go to disabilityquotes.com/asps
The disability insurance industry continues to evolve. Accelerated by the post-pandemic environment, insurers have embraced innovation, making it easier for residents, Fellows and physicians to obtain coverage through GSI and similar programs. As awareness grows, so does recognition of disability insurance as an essential component of income protection for medical professionals. PSN
Lawrence Keller, CLU, ChFC, CFP is the founder of Physician Financial Services, a firm specializing in disability insurance and term life insurance for physicians. He can be reached at (516) 677-6211 or by email to Lkeller@physicianfinancialservices.com with comments or questions.
imbursement and may create incentives for shifting appropriate cases out of the hospital.
Plastic surgeons should also pay attention to the evolving rules for telehealth and supervision. Although most operative codes remain excluded, the new allowance for virtual supervision of incident-to services could facilitate expansion of multidisciplinary practices and outreach clinics. Practices should ensure that compliance protocols, documentation and billing procedures are updated to reflect the new standards.
The CY 2026 Medicare Physician Fee Schedule underscores the ongoing tension between CMS’s cost-containment objectives and the need for fair valuation of surgical services. The efficiency adjustment represents a philosophical shift toward presumed productivity gains and periodic across-the-board reductions, a policy many in the surgical community view as unsupported by empirical evidence. The decision by ASPS to join the ACS-led coalition opposing this adjustment reflects the specialty’s recognition that the rule’s long-term trajectory threatens the financial stability of surgical practice and, ultimately, patient access to care.
Plastic surgeons should remain closely engaged in advocacy efforts and in the comment process for future rulemaking cycles. They should also monitor the detailed Addendum B to identify code-specific changes and quantify the precise impact on their practices. Early financial modeling, careful contract review and proactive communication with administrative and legislative stakeholders will be essential to navigating the year ahead.
Although the CY 2026 PFS final rule delivers incremental payment gains on paper, its deeper reforms will likely define the reimbursement environment for the remainder of the decade. For plastic surgeons, vigilance, adaptability and continued advocacy will be the key to maintaining the viability of both reconstructive and aesthetic practices within Medicare’s evolving framework. PSN
Assistant/Associate Professor Plastic Surgery Faculty Medical College of Wisconsin Milwaukee, Wis.
The Department of Plastic Surgery at the Medical College of Wisconsin is recruiting a board certified or board eligible plastic surgeon with a focus on breast reconstruction to join our group of fourteen faculty members in Milwaukee. Our breast care team sees 550 new breast cancer patients a year with over 300 primary reconstruction patients treated a year. A team of 4 surgeons offer the spectrum of options including microvascular and implant-based procedures. The position will allow ample opportunity to treat patients with a breadth of reconstructive and cosmetic needs.
Our MCW partner institutions including a major cancer center, a top ranked tertiary adult and children’s hospitals as well as community hospitals. We collaborate with all surgical specialties in our system. Our integrated plastic surgery residency is one of the oldest in the country and we support one microsurgery fellow a year.
Milwaukee and SE Wisconsin is a playground in all four seasons for those who enjoy the outdoors – whether it be on the lakefront, 1000’s of miles of trails or on the 15,000 inland lakes throughout the state. Milwaukee and its surrounding communities include 1.2 million residents who enjoy the benefits of a big city without its headaches.
Contact: John LoGiudice Professor and Program Director Microsurgery Fellowship Program - Medical College of Wisconsin Department of Plastic Surgery jlogiudice@mcw.edu
Palm Beach County, Fla.
Seeking BC/BE plastic surgeon to acquire boutique aesthetic practice with prestigious reputation. Opportunity to join and transition practice. Fully accredited AAAASF surgical suite with overnight facility. Excellent opportunity to assume an established practice. Located in a desirable area with beautiful beaches and excellent schools. Please send CV to plasticsurgery561@gmail.com.
Prestigious Beverly Hills Plastic Surgery Practice For Sale
Well-known plastic surgeon offering 35+ year practice for sale. The practice is highly regarded nationally and internationally with a balance of cosmetic and breast reconstruction. Prime upscale, welcoming Beverly Hills location. Seeking experienced, highly skilled, compassionate, board-certified plastic surgeon to take over this solo practice. Skill in all aspects of breast reconstruction desired. Transition is aimed to be completed by July 1, 2026, but the timing is flexible. Seriously interested and qualified parties please send CV and inquiries to: Bhplasticsurgery24@gmail.com.
Plastic Surgeon Partnership Opportunity
Boca Raton, Fla.
Prestigious boutique aesthetic practice in Boca Raton seeks BC/BE Plastic Surgeon for partnership, with a structured path to full ownership. Join an established practice known for excellence in cosmetic surgery, with mentorship from a highly regarded surgeon. The facility includes an accredited Quad A surgical suite in a premier location. This is an outstanding opportunity to advance your career in an upscale, thriving practice with a loyal patient base.
Send CV to: cosmeticjourney77@gmail.com

Join Our Thriving Plastic Surgery Practice In Oregon’s Stunning Willamette Valley!
Are you a passionate, ambitious plastic surgeon ready to make your mark? Neaman Plastic Surgery, located in the picturesque Willamette Valley of Oregon, is seeking a talented surgeon to join our dynamic team. With several surgeons retiring in our community, there’s an urgent demand for your expertise. Our outpatient elective referrals are surging, and we need skilled hands for facial trauma call coverage and complex hand trauma care. If you excel in aesthetic surgery, this is your chance to shine in one of the Northwest’s busiest cosmetic practices, specializing in breast and body contouring, with growing opportunities in facial aesthetics.
Why Choose Neaman Plastic Surgery?
• State-of-the-Art Facility: Operate in our onsite JCAHO-accredited surgery center with a consistent, highly efficient staff.
• Supportive Team: Our physician assistants handle consults, freeing you to focus on performing cases.
• Diverse Practice: Join a bustling Medi spa, active hand therapy program, and wellness center. Passionate about injectables? Tap into our large patient funnel.
• Robust Referral Network: Benefit from a strong dermatology referral base for Mohs reconstruction.
• Unrivaled Cosmetic Practice: We’re one of the busiest cosmetic practices in the Northwest—ask your Allergan rep!
• Hand Surgery Opportunities: Hand fellowship training is a major plus. Our weekly orthopedic hand sur geon needs support with our growing volume.
• Manageable Call Schedule: Enjoy a collegial Q5 call rotation, with opportunities for additional call if desired.
• Ideal Location: Live and work in vibrant Salem, Oregon—just minutes from Portland, the Oregon Coast, and world-class outdoor recreation. Love hiking, skiing, or beach getaways? This is your paradise.
Qualifications
• MD or DO with completion of an accredited plastic surgery residency.
• Board-Certified or Board-Eligible by the American Board of Plastic Surgery.
• Active Oregon medical license (or ability to obtain).
• Hand fellowship training preferred but not required.
Compensation & Benefits
Beverly Hills Practice And Private Surgery Center For Sale
A plastic surgery practice and Quad A Medicare certified surgery center in Beverly Hills’ Golden Triangle is for sale. This is a turn-key opportunity of 30+ years, featuring a spacious, bright office and an independent, free standing operatory. The practice caters to a sophisticated, discrete patient population. Physician/owner of both entities is looking for a masterful clinician to assume his 98% cosmetic practice. Surgeon availability is possible to facilitate the transfer of both entities. Transition date mid 2026.
Please email your inquiry along with resume to bhscplastic@gmail.com
West Coast Florida Plastic Surgeon
Well established 100% aesthetic surgery practice in Tampa Bay with accredited Office Surgery Facility seeks Board Certified / eligible Plastic Surgeon.
Submit CV and inquires to BPS500@aol.com.
Plastic Surgeon Career Opportunity Louisville, Ky.
Mays Plastic Surgery & MPS Surgical Suites, led by board-certified plastic surgeon Dr. Chet Mays, is seeking a talented Plastic Surgeon to join our premier cosmetic practice in Louisville. Our 13,000 sq. ft. facility includes a clinic, luxury med spa, and accredited ORs, offering an ideal setting for advanced care. With a trusted reputation, high patient demand, and exceptional support staff, this is a rare opportunity for professional growth. Louisville features affordable living, rich culture, and southern hospitality.
Transform Your Career: Own a Thriving Practice in a Growing Community! Greenville, S.C.
Imagine stepping into a thriving, well-established aesthetic practice where dozens of patients seek the expertise of a caring, experienced team every day. After 30 years of dedicated service, I’m ready to pass the torch. I’m seeking a compassionate, positive, and skilled surgeon(s) to carry forward this successful legacy of providing aesthetic surgery, injectables, laser treatments, non-surgical body contouring, and specialty skin care to thousands of loyal and future patients.
What Awaits You:
• A stellar business reputation, glowing reviews, consistent profitability and opportunities for growth
• Decades of AI-safe procedures
• Prosperous and growing community: Greenville, SC
• 16+ talented employees including 8 providers
• Spacious 6,500+ sq ft facility, including a QuadA certified OR
• Robust external and internal marketing
• Support with transition
This is your chance to own a valuable practice and shape your future. Visit AestheticCenterGreenville.com for practice profile, photos and testimonials.
Email us at femurs82409@mypacks.net for Practice Summary to learn more.

• Competitive Salary: $350,000–$500,000/year starting, with production-based bonuses that can push earnings beyond $750,000, depending on your drive.
• Relocation Support: Generous assistance to help you settle in.
• Comprehensive Benefits: Health, dental, vision, 401(k), malpractice coverage, CME stipend, and generous paid vacation.
• Full Support: Dedicated administrative, marketing, and clinical teams to ensure your success.
How to Apply
Ready to elevate your career in a thriving practice and vibrant community? Send your CV, cover letter, and references to: careers@neamanplasticsurgery.com (503) 364-5033
Join Neaman Plastic Surgery and build your legacy in one of the most beautiful regions of the Northwest!
New York Plastic Surgical Group (NYPS Group) is the largest & longest running private & academic plastic surgery group in the United States. Our 20+ plastic surgeons practice out of 10+ affiliated offices, ambulatory surgery centers, and 20+ hospitals.
We are looking for a fellowship trained, Board Certified/Board Eligible Plastic Surgeon to join our practice. The surgeon to fill this position will have the full support of NYPS Group to build a practice that suits their interests (cosmetic, reconstructive, hand, craniofacial, transgender, etc).
NYPS Group offers a full comprehensive benefit program and a competitive salary. NYPS Group is committed to an ACGME accredited plastic surgery residency program. Since 1954, the practice has directed and contributed to resident education.
If interested, please email resume/CV to Gary Blank, DPM, MBA at gblank@nyplasticsurgical.com.
Plastic Surgeon - Geisinger
Geisinger is seeking plastic surgeons to join our team in central or northeastern Pennsylvania. Our services include general plastic surgery, cosmetic surgery, microsurgical and/or implantbased breast reconstruction, maxillofacial trauma, and cancer/trauma reconstruction.
Our integrated plastic surgery residency provides opportunity for teaching, research, and program development. Geisinger has an established reconstructive and cosmetic referral base which is geared to building a thriving practice. We collaborate closely with multiple disciplines throughout the system, and we are supported by an excellent team of physician assistants, nurses, and staff.
We are looking for highly motivated, exceptional plastic surgeons who love the breadth of plastic surgery and want to build the plastic surgery program by being an integral part of this team, continuing Geisinger’s tradition of innovation and excellence. Salary and benefits are very competitive.
If you want to learn more about these opportunities, we would love to speak with you.
Please reach out to Christian Kauffman, MD, Chair c/o Sarah Lipka, Physician Recruiter, at slipka1@geisinger.edu
Bloomfield Hills, Mich.
We’re looking for Board-Certified Plastic Surgeons to join our state-of-the-art surgical facility in Bloomfield Hills, Michigan, with a team of Board-Certified Anesthesiologists, RNs, and CSTs. Please contact our DON or ED with all questions or to set up a tour of the center. Contact Information: Phone: 248-839-9440 or email: ssalam@platinum-center.com
Plastic Surgeon Opportunity – Upstate NY
Established, exclusively aesthetic Plastic Surgery Practice and MedSpa seeks a Board-Certified Plastic Surgeon with 2–3+ years of experience. The ideal candidate is a skilled, compassionate surgeon with long-term career goals. Partnership opportunity available. Our state-of-the-art facility features a QuadA-accredited operating suite and a collaborative, patient-focused team dedicated to excellence, innovation, and growth.
Enjoy life in New York’s beautiful Capital District—affordable living, excellent schools, four-season recreation, and easy access to NYC, Boston, and the Adirondacks.
Build your future with us while enjoying all that upstate New York has to offer.
Contact plasticsurgrecruiting@gmail.com.
Unique Fellowship Training: Craniofacial & Facial Gender-Affirming Surgery
Department of Plastic Surgery at Lenox Hill Hospital, Northwell Health (UES Manhattan): one-year post-Plastic Surgery fellowship with large volume gender-affirming facial reconstruction, craniofacial, cleft lip/palate, orthognathic, pediatric, & CF trauma. If interested, please reach out to Mallory McClure mmcclure1@northwell.edu for more information.
Office Sharing Opportunity
Newport Beach, Calif.
A beautifully appointed office adjacent to Fashion Island area of Newport Beach, with onsite AAAASF operating room. Ideal for a second location, or someone building their practice. The prospective candidate must have impeccable skills and affable personality, BC/ BE. Please submit a brief Cover Letter and CV to ackerman92660@gmail.com

100% Aesthetic Practice in Dallas/Fort Worth Metroplex
Signing bonus, large guaranteed salary and the ability to make huge bonuses with proven track record of success for young surgeons.
• 100% aesthetic practice
• Five locations in DFW Metroplex
• No insurance accepted
• No ER call, no nights, no weekends
• Dedicated 6 OR AAAASF accredited surgical facility
• 4 full-time anesthesia providers
• 5 medical spas
• Technology focused practice with 3-dimensional imaging, HIPPA compliant texting apps, state-of-the-art lasers and body contouring equipment
• Large dedicated social media team
• Personal patient care consultant for each surgeon
• 4 weeks paid vacation
• Additional paid time off for meetings
If you dream of being a successful aesthetic plastic surgeon, we can make it happen! Please email CV to sandy@northtexasps.com. To learn more about our practice, please check out our website www.northtexasplasticsurgery.com.
Aesthetic Plastic Surgeon
We are seeking a BC/BE Plastic Surgeon to join our beautiful and luxurious medical aesthetic practice in Springfield, IL to do breast, body and facial cases. This is an excellent opportunity to join an established practice in a community that needs these services. We seek an ambitious, driven self-starter with a strategy for becoming the best. We have an onsite ASC and a large procedure room.
Interested candidates should send cv and cover letter to prairieaesthetics@prairie-eye.com.
Cosmetic Surgery Practice For Sale
Delaware
Be Busy from Day One in this Well Established Solo Private Plastic / Cosmetic Surgery Practice for Sale.
Large patient base with over 30 years in the area.
Excellent Mix of mostly Cosmetic (80%) and some Insurance (20%) Cases.
Full Medspa Onsite with Injectables / Lasers / Aesthetician.
Large multi-state draw area in great community. Great place to live and work. Close to beaches / Delaware and Jersey Shore and lots of outdoor activities. Close to Philadelphia / Baltimore / Washington DC / NYC.
Owner willing to stay on if desired for smooth transition.
Very flexible purchase options with No Money Up front and No Buy-In.
Contact aestheticplasticinfo@gmail.com for more information.

Long Island & NYC
Excellent opportunity with partnership track.
Well-established cosmetic plastic surgery practice with locations in Long Island and Manhattan seeks a plastic/reconstructive board certified/board-eligible surgeon to join our thriving practice. Modern offices, professional team environment, state-of-the-art and accredited facilities, knowledgeable and professional staff, competitive compensation and benefits.
Greenbergcosmeticsurgery.com
To apply, forward CV to docstg@aol.com or call 516-364-4200
Opportunity for BC/BE Plastic Surgeon to Join Private Practice in Houston, TX Memorial Plastic Surgery (MPS) is a leading aesthetic and reconstructive plastic surgery practice, known to deliver unparalleled patient care and results.
Excellent opportunity for a Board-Certified / Board-Eligible Plastic Surgeon, with a strong interest in microsurgery to perform DIEP flap breast reconstruction and/or cosmetic breast and body procedures, to join a well-established practice.
MPS OFFERS:
• Mentorship and hands-on training with premier group of board-certified plastic surgeons
• Heavy volume of patient overflow for associate to build practice
• Team-oriented staff for administrative and clinical support, including marketing and social media needs
• Physician offices, spacious exam rooms, MedSpa area for non-surgical services
• Private AAAHC accredited ORs located on-site
• Multi-specialty ASC located one floor below with direct access to 4 additional ORs
COMPENSATION:
• Competitive compensation models
• Partnership track opportunity
• Medical/Vision/Dental Insurance & 401k Benefits Package
QUALIFICATIONS:
• Board Eligible or Board Certified in Plastic Surgery
• Active Texas Medical License
• Aesthetic fellowship/training a plus, but not required
• Must have a passion for delivering high-quality patient care and results
Qualified applicants are encouraged to apply by submitting an updated CV & headshot photo to:
APPLY@MEMORIALPLASTICSURGERY.COM
Pediatric Microsurgeon
Texas Children’s Hospital and Baylor College of Medicine in Houston, Texas are recruiting a pediatric microsurgeon. Texas Children’s Hospital is one of the top-ranked children’s hospital in the United States and has a busy plastic surgery service. TCH performs many complex procedures on children including cranioplasty, cleft lip and palate surgery, surgery for congenital defects, and tumor reconstruction. TCH is a Level I pediatric trauma hospital and therefore sees quite a bit of pediatric trauma as well. Pediatric microsurgery which is performed at TCH includes brachial plexus reconstruction, head and neck reconstruction, and extremity reconstruction. We also work closely with general surgery and perform a number of chest and abdominal wall reconstructions.
Applicants must have completed an accredited residency in Plastic and Reconstructive Surgery and must at least be eligible for board certification in Plastic Surgery. Having completed a fellowship in microsurgery is also considered essential for this position. Applicants must be eligible for licensure in the State of Texas and able to work in the United States.
For more information or questions, please contact Mary Kana, Practice Administrator for Plastic Surgery, at 832-822-3493 or mdkana@texaschildrens.org.
Akron/Canton, Ohio
Established mostly Aesthetic, facial rejuvenation
Plastic surgery solo practice by board certified plastic surgeon. Free standing office with OR room in the best location. 2 large hospitals in the area, local airport with access to all major airlines. Sale will include all equipment including Liposuction machine, surgical instruments and office furniture in move in ready condition. Price negotiable.
Please contact: tuscanblue4800@gmail.com
Ph. 330-493-3785
Looking for a motivated surgeon to thrive in our state-of-the-art facility!
Join a premier plastic surgery facility in North Texas, fully equipped practice with two operating rooms, offering patient comfort and privacy. Enjoy flexible terms, and comprehensive administrative support.
Email us at karina@drplano.com for more details.
Want your own solo 100% cosmetic surgery practice on the Northshore of Chicago? Want to make the next generation of gender affirming care your expertise? Over 60% gender affirming care practice (FFS/BAM/BBL), other 40% bread/butter cosmetic with strong Latina component. My 28 year turnkey International Center of Gender Excellence becomes available April 1, 2027. Easy buyout, self-referring base thru independent large volume electrology program that generates cash flow for buyout, rent, and gender referrals. Onsite surgical facility with 22 years of consecutive accreditation. Start work July 1, 2026, or later at no cost to you until 4/1/27. If Chicago is your goal, this is a once in a lifetime opportunity.
Respond to facesculptor@yahoo.com with a CV.
Upstate Plastic Surgery in Greenville, SC is seeking an additional partner to meet patient demand for our high-volume private practice. Greenville is a growing community in the Upstate region of South Carolina.
Our private practice is located in a practice owned building with 3 floors sitting on a beautiful golf course which hosts the BMW Charity Pro Am on an annual basis. Our AAAASF officebased surgery center is located inside our building along with our Medical Spa and Laser Center. There is close access to both local hospitals and the airport.
Our practice has an aesthetic focus. We currently perform both aesthetic and reconstructive surgery with an established referral base. We have received multiple community awarded honors. The office is essentially turnkey with a talented medical and administrative staff. We are committed to marketing a new surgeon and helping him or her succeed. We are offering an attractive package including salary with a bonus structure, moving expenses, and benefits. We are looking for a long-term relationship leading to a partnership/ownership track.
Our ideal candidate is BC/BE with an interest in performing both aesthetic and reconstructive surgery. An aesthetic fellowship or planning an aesthetic fellowship is preferred. We are looking for a surgeon who is well trained and has an entrepreneurial spirit. We offer a collaborative environment with a passion for excellence where a new surgeon can thrive.
Interested candidates please send your CV to dmccray@upstateplasticsurgery.com.
Manhattan Plastic Surgeon Office For Sale Plastic Surgeon is retiring and desirous to sell upper eastside office.
Fully furnished office with operating room; office approximately 1,250 sq ft.
Perfect office for bi-coastal practice or young surgeon desiring own space.
Please contact me for more information:
Charles K. Loving Jr., MD
17 E 84th St. Suite 1B
New York, NY 10028
cutrush7@aol.com 212-472-0900
Aesthetic Surgery Fellowship 2026-2027 Academic Year
This aesthetic fellowship will offer a comprehensive experience in both face and body surgery with an emphasis on facial rejuvenation and aesthetic breast surgery. Both surgeons are experienced educators and leaders in the field.
Somenek+PittmanMD is an established aesthetic surgery practice, located in the heart of Georgetown, offering a full menu of surgical and non-surgical services. The facility includes a large clinical space, a AAAASF-accredited operating suite - with 2 operating rooms, and a free-standing MedSpa.
There will be ample opportunity for the fellow to lead and curate their own clinic, with the operating room and MedSpa at their disposal to expand their experience. There will also be ample opportunity to learn the nuts and bolts of building and maintaining a profitable aesthetic practice.
In addition to the clinical experience, the practice has several FDA and industry-sponsored clinical research trials in process, providing the fellow with ample opportunity for clinical research, based on their individual interests.
Applicants must have completed an ACGMEapproved plastic surgery residency, be BC/ BE, and be eligible for medical licensure in the District of Columbia. Salary commensurate with PGY level, malpractice insurance covered, individual health insurance and financial assistance with meetings provided.
Interested candidates should send a cover letter of interest and CV to Dr. Troy Pittman (drpittman@spmeddc.com)
Application Deadline is December 31, 2025. www.somenekpittmanmd.com
PatientList.org: Electronic Health Record (EHR) for Plastic Surgeons
✓ Integrated Patient Charts
Note templates, Photos, Files, and much more
✓ Smart Calendar Management
Advanced Patient Scheduling System
✓ Advanced Billing Dashboard and Analytics
Intuitive insurance claims, Cash Payments, and IDR/arbitration. HIPAA-Compliant
→ All-inclusive: $100/month* (single-surgeon practice, limited time)
Specializing exclusively in Plastic Surgery billing with over 25 years’ experience. We check for correct coding for maximum reimbursement and review each claim before submission. Once the claims are submitted, we follow closely and appeal when necessary. We work remotely, off-site with excellent references. Call Ana at 239-297-3737.
Rates for printed classified ads are based on word count and must be paid prior to publication. Logos, boxes and color enhancements can be designed for additional fee. The editors do not investigate positions of employment and assume no responsibility for them. ASPS reserves the right to accept, reject or cancel any advertisements in its sole discretion.
■ 1 to 50 words: $165
■ 51 to 100 words: $305
■ 101 to 150 words: $440
■ 151 to 200 words: $555
■ 201 to 250 words: $763
■ More than 250 words: Contact jembrey@plasticsurgery.org for “designed” ad options
Designed Ad Rates
■ 1/8 page: $930
■ 1/4 page: $1,440
■ 1/2 page: $2,175
■ Full page: $3,195
To place a classified, contact: Jeanne Embrey Advertising Coordinator jembrey@plasticsurgery.org
Visit the Job Opportunity Board plasticsurgery.org/job

Patient Education e-Brochures
Quickly send trusted procedural information along with personalized messages directly to your patients’ inboxes.
What is the ASPS eNLIGHTEN Collection?
The ASPS eNLIGHTEN Collection features updated, digital Patient Education Brochures from the American Society of Plastic Surgeons. Available on both mobile and web platforms, these brochures can be directly emailed to patients, allowing surgeons to efficiently share detailed procedural information with personalized touches.
Key Features: Multi-platform compatibility | Instant delivery Customizable communication | Access via the ASPS Mobile App or the ASPS Member website
Sign up with a monthly or annual subscription at plasticsurgery.org/shop and access over 20 procedures instantly.
Jeffrey Darrow, MD, Brookline, Mass., expresses his creative side by using two materials that could hardly be less alike: human flesh and stone. Dr. Darrow has added to his “materials redesign” armamentarium to include stone masonry for the work he’s completed at the Eleanor Cabot Bradley Estate in Canton – one of Massachusetts’ most famous homesteads.
Dr. Darrow and his wife, Ellen, regularly walk around Canton, and these outings brought them to the Bradley estate – a historic, nonprofit country house and gardens constructed in the early 1900s by a wealthy, local physician. The property spans roughly 90 acres with about three miles of walking trails. During one outing in March 2020 – during the COVID-19 shutdown – Dr. Darrow encountered two stone walls measuring slightly longer than 100 yards in disrepair. The sight reminded him of his youth, when he helped his father build stone walls that, in one instance, protected against sloping land that threatened to slide down into their driveway.
“I asked the caretaker if the estate – which is operated by the Trustees of Reservations – if they would be interested in me repairing those,” he tells PSN. “To me, it was sort of a no-brainer. ‘Why wouldn’t they want something to look nice that’s a visible part of the property?’ But I still had to go through a process to get my work approved – even though I was going to do the work for free.”
Once approved, Dr. Darrow set out to rebuild two walls – each about 3 and 1/2 feet tall by 3 feet wide, with stones in disarray. “The principles involved have a lot in common with those that we learn in plastic surgery,” he says. “You need to have a solid foundation of everything that you’re doing. When working with stone, the foundation must be solid because it’s necessary to build upon itself. Then the upper stone layer is the ‘aesthetic’ layer.”
Dr. Darrow relied on other lessons learned while working with his father. “For the biggest stones, they need to be as flat-surfaced as possible, so that the smaller ones we put on top of those can be balanced and then built-up from there. Part of it’s trial and error: If you put a roundish stone on top of the wrong stone, it just rolls off. Also, the outside of the wall has the two biggest stones, and then you fill the space between that – giving your next stone a floor, so even if it doesn’t balance perfectly with the outside stone, it’s still supported internally by the inner part of the wall. If you’re going to err on positioning on either side as you move up the wall, you always err slightly by placing it to fall inward as opposed to outward – because it won’t fall inward, as the rest of the wall is there.”
Editor’s note: The bulk of PSN’s pages are devoted to specific elements of our mission statement – to keep members informed of the social, political and economic trends and educational opportunities that affect the specialty of plastic surgery.
PSN is pleased to take liberties with the “social” aspect of its mission statement by presenting a good-natured look at the lives of notable members who we believe are making significant contributions to the specialty.

In this issue, we present ASPS member Daniel Krochmal, MD, Hinsdale, Ill., founder of The Krochmal Center for Plastic Surgery. Dr. Krochmal is a member of the ASPS Health Policy, Legislative Advocacy and Nominating committees, and he’s served several terms for a long roster of additional panels and committees in the past. Dr. Krochmal, an avowed foodie, took a few minutes out of planning his next mission on all things gastronomic to answer the following questions for PSN:
If I had to start my career over, I would... Have done exactly the same thing, but also bought Bitcoin. I received fabulous mentorship during my residency and fellowship, and had a great job out of training that allowed me to flourish. Thanks to all who offered advice along the way. Except those that told me not to buy Bitcoin.
The best thing about being a plastic surgeon is... That life is never boring. I get to meet incredible people, hear their stories, develop creative ways to help them live the lives they want to lead, and be challenged intellectually, physically and emotionally. I couldn’t picture myself doing anything else and being genuinely fulfilled by it. Except possibly being a writer/ satirist for The Onion.
The worst thing about being a plastic surgeon is... The everincreasing patient expectation of achieving perfection.
The last book I read was... A Gentleman in Moscow. After a string of non-fiction business books such as Unreasonable Hospitality, I was looking to switch it up a bit. The dialogue and characters made me giddy every time I cracked it open.
The best thing I can make for dinner is... Reservations. I can cook, but I’m deeply ingrained in the Chicago hospitality industry (as a diner and investor) with loads of chef friends, so I’m often enjoying what they make that’s infinitely better than what I can make. (And there are way less dirty dishes.) My restaurant recommendations are so revered that my friends made me launch a “Dr. Dan Dining Awards” series on my Instagram page.
One perspective I didn’t have before COVID-19 is... How medically illiterate many people are (not their fault) and how much doctors are actually up against regarding where our patients get their “health information.”
I couldn’t operate without my... Bose SoundLink Revolve+ II Bluetooth speaker. And if you’re curious, SiriusXM Lithium.
Another time-consuming challenge involved finding the right stones. “The New England soil is filled with old stones from the glacier era – they’re not flat, they’re different shapes and aren’t easy to stack,” he says. “You have to spend a lot of time figuring that out.”
The entire project of rebuilding both walls took two years, Dr. Darrow says. One might think that a plastic surgeon working with stones that weigh up to 20 pounds each would be career threatening, but experience paid off for Dr. Darrow. “My only casualties were a few bruised fingers and a little poison ivy – and my wife calling me while I’m full of sweat and exhausted, saying: ‘Where are you?’ ” PSN
A surge in the number of plastic surgery divisions receiving department status garnered positivity from many in the specialty in 2010, when 15 plastic surgery departments had been established – doubling the amount seen just two years prior. Department heads shared their pointers and hopes for the future in the December 2010 issue of PSN:
“It appears now that the growing number of departments will continue, with the momentum that’s being created helping to push more divisions to consider department application. We seem to be nearing a self-perpetuating mode, which will benefit the specialty in general – and our patients significantly.”


The best vacation I ever took was... To Australia for six months. After graduating undergrad early (nerd alert), I deferred med school for a year to travel. Even after six months I felt like I barely scratched the surface of the country. The next summer, I spent five months exploring Europe. I had planned to go to Africa in-between, but 9/11 happened while in I was in Australia, so I spent those few months stateside working as a “Tuxedo Representative” for the Men’s Wearhouse while trying to process the abrupt world change. It was a formative time, for sure.
My all-time favorite movie is... You want the answers to my password challenge questions? Why not just ask about my first car or my great grandmother’s favorite color? My second favorite movie is The Hunt for Red October. RIP Sean Connery and James Earl Jones.
I seriously collect... Passport stamps. I love to travel. There’s simply so much in the world to experience. I just wish there were more time and money, and less geopolitical risk in certain regions, so I could do it even more.
The best part of next weekend will be... Relaxing by the pool, or snowshoeing (sometimes in the same day, because, you know, Chicago).
The single-greatest influence on my decision to become a plastic surgeon is... The spot-on career advice offered in The Graduate (I probably just dated myself). Seriously, that influential person is Edwin Wilkins, MD. Early in my first year of medical school, he gave a lecture at a plastic surgery interest group meeting on what plastic surgery actually was. The proverbial light bulb went off in my head. I’ve grown a lot since then.
The words I try to live by are... “Of course I’m not skipping dessert” – Anonymous. Also, “The only thing you take with you when you’re gone is what you leave behind” – John Allston. PSN
Grand Hyatt Indian Wells, Palm Springs, CA
Explore Cutting-Edge Insights at the 2026 WPS Symposium!
REGISTER TODAY Join us for an exceptional lineup of panels, redefining expertise and inspiring surgical practices. Don’t miss this opportunity to discover the latest advancements in plastic surgery!



Hear from the Experts. Reconnect with Women in Plastic Surgery.