CHEMICAL & PETROLEUM ENGINEERING
Robert S. Parker, PhD
931 Benedum Hall |3700 O’Hara Street | Pittsburgh, PA 15261 P: 412-624-7364
Robert v.d. Luft Professor Vice Chair for Graduate Education
rparker@pitt.edu
Systems Engineering at the Medical Interface Advanced computation and analysis tools are sorely needed to help clinicians visualize, assimilate, and analyze the complex interplay of the measurements and data available to them. These tools provide a complement to the outstanding linear intuition of clinicians, as multiple variables of interest (actuations and/or measurements) are common and nonlinearities (such as saturation phenomena) are ubiquitous in biological systems. We take a model-based approach to characterizing medical disease and treatment problems, working to understand the dynamics and mechanism of disease progression as well as treatment. We closely collaborate with clinical practitioners to formulate and solve clinically-relevant problems for societal benefit. The overall goal is to improve the efficacy and efficiency of health care delivery and policy by developing patient-tailored treatment approaches in such problem areas as: • Cystic Fibrosis: Working with UPMC clinicians and scientists, we are characterizing the system (body) and cellular response to osmotic challenges and therapies. By focusing on easily
accessible cells (nasal epithelia), as a personalized model for bronchial epithelia, we target a patient-tailored understanding of disease dynamics in the individual and targeted treatment approaches and interventions. • Glucose Control in Critical Care: Intensive care unit patients often manifest stress-induced hyperglycemia even though they are not diabetic. In collaboration with Critical Care Medicine, we are developing artificial pancreas-like control systems and a clinician-friendly interface and alarm layer to improve patient outcomes in intensive care. • Inflammation and Sepsis: Pathogenic invasion excites the human inflammatory response system, and the role of these inflammatory mediator dynamics in survival is not well understood. We are working to model the dynamics of system response in order to characterize patient groups that are aided by existing or novel therapeutic interventions. • Solid Tumor Cancer Chemotherapy: see below.
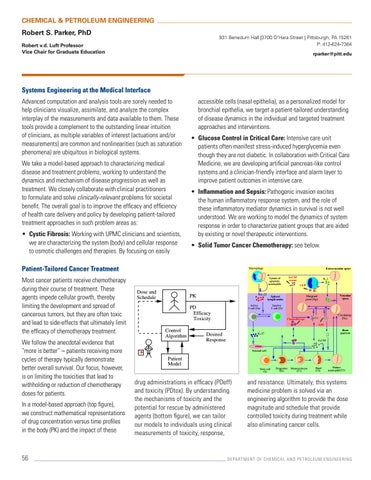
Patient-Tailored Cancer Treatment Most cancer patients receive chemotherapy during their course of treatment. These agents impede cellular growth, thereby limiting the development and spread of cancerous tumors, but they are often toxic and lead to side-effects that ultimately limit the efficacy of chemotherapy treatment. We follow the anecdotal evidence that “more is better” – patients receiving more cycles of therapy typically demonstrate better overall survival. Our focus, however, is on limiting the toxicities that lead to withholding or reduction of chemotherapy doses for patients. In a model-based approach (top figure), we construct mathematical representations of drug concentration versus time profiles in the body (PK) and the impact of these
56
Macrophage
Extravascular space G-CSF rescue
Uptake of apoptotic neutrophils
Dose and Schedule
IL-23
PK
Vascular space
Marginal pool (Np)
Spleen/ lymph nodes
Active T cell (Ta)
PD Efficacy Toxicity
IL-1
CLP
Inactive T cell (Ti)
Circulating (Nc)
Chemotherapy
LPS
Control Algorithm
Bone marrow
IL-17
Desired Response
G-CSF
Stromal cell
+ Patient Model
Stem cell (S)
drug administrations in efficacy (PDeff) and toxicity (PDtox). By understanding the mechanisms of toxicity and the potential for rescue by administered agents (bottom figure), we can tailor our models to individuals using clinical measurements of toxicity, response,
Progenitor (Pr)
Metamyelocyte (T1)
Band (T2)
Mature neutrophil(T3)
and resistance. Ultimately, this systems medicine problem is solved via an engineering algorithm to provide the dose magnitude and schedule that provide controlled toxicity during treatment while also eliminating cancer cells.
DEPARTMENT OF CHEMICAL AND PETROLEUM ENGINEERING