










The PHA UK is your charity, and we welcome your feedback on everything that we do, to ensure we are the best we can be. We’d love to hear your thoughts- good or bad - about any of our services, or about any aspect of our website, publications, or resources. In fact, we’d like your feedback about anything at all!
Scan this code to leave your feedback via our online form (where you can remain anonymous if you wish). You can also email feedback@phauk.org

Welcome to your new issue of emPHAsis. I hope the summer is treating you
Thisis another packed edition and there is something for everyone within these pages – whether you are looking for advice, inspiration, information, or simply a little lift.
I wanted to use this introduction page to update you on the new PAH therapy sotatercept, as I know many of our members are interested in its progress.
The drug was licenced for use in the UK around six months ago, but it is not yet available for prescribing. It is currently going through a National Institute for Clinical Excellence (NICE) review, to decide whether the benefit of the drug is worth the cost to society.
Here at the PHA UK we are playing an important role in the process, and as I write this, we are preparing to attend a NICE committee meeting in Augustwhere we will be representing the patient community in important discussions around the drug.
This meeting will have a significant impact on the commissioning decision, and the process will continue in its wake. There is no deadline for when a decision must be made but it is hoped an outcome will be reached before next year.
We know that where sotatercept is available in other countries, it is extremely costly. Whilst we’re unsure of how it will be priced in the UK, we know it won’t be easy to secure commissioning. If we need to challenge the price of the drug with those who produce it, we will do this on your behalf.
We have had to fight for every drug that’s available to treat PH, and we are aware that the NHS is under massive financial strain. However, I promise that as an organisation we will do all we can in this process, and as people with lived experiences of PH, your voices will play a vital part.
We’ll keep you updated as things progress. In the meantime, enjoy the rest of the summer – and don’t forget the sunscreen!
Sotatercept is a totally new type of drug for pulmonary arterial hypertension. There are already a number of existing drugs that are known as ‘vasodilators’ – which work by opening up some of the arteries that have narrowed or closed down. But these drugs are treating the symptoms of PH, rather than what’s causing the disease.
Rather than just opening up vessels, sotatercept works more directly on the underlying ‘problem proteins’ that are causing the disease in the first place. It’s the first time a PAH drug is getting to the root cause of the problem, rather than treating the consequences of it. It must be remembered though that this is not a cure, so it is not a life-saving drug.
Iain Armstrong Chair of the PHA UK media@phauk.org
Sotatercept isn’t suitable for everyone. It is designed to be taken by some people alongside other medications, via an injection under the skin administered every three weeks.









Member Neil Gambrell shares how he manages his mental
Dr Chris Chew on how this type of supportive care can help strike a balance

This time, meet Clinical Nurse Specialist Andy
Bringing
Photos from our latest ‘Together’ event

Understanding guilt and shame in chronic illness
Advice from psychotherapist Sophie Papageorgis
Disabled Student’s Allowance
Support if you’re studying with PH
Help to shape children’s PH services and research
Could you join our young person’s advisory group?
PHA UK members have helped secure funding for an innovative new patient toolkit that aims to help people manage their PH via a convenient app. Researchers from across the UK’s specialist centres submitted a bid to the British Heart Foundation (BHF) for a grant to develop the technology – and they used responses to our PHA UK surveys from the last few years as important evidence of its need.
Survey data from 1,653 people living with PH, who completed our surveys between 2021-24, was used as part of the funding bid. The £266,000 secured will be used to develop a mobile application for use by patients to track and manage their symptoms, learn more about the disease, and participate in research.
PHA UK members have already been involved in the early plans for the app, and there will be further opportunities to contribute when full development begins in the autumn.
Dr Frances Varian of the Sheffield Pulmonary Vascular Disease Unit is managing the project. She said: “PHA UK surveys were absolutely key to our funding success. Patient contribution through the PHA UK is so valuable for research, and it has a real impact on improving patient care for the future. It also helps us to really understand what is most important to those living with PH.”
It is hoped the app will be fully developed by 2026, when it will then be used to support the NHS to deliver even better care.
Dr Iain Armstrong, Chair of the PHA UK, said: “If you have completed any of our surveys over the last few years, you have directly contributed to the success of this funding bid and the development of this toolkit. Never underestimate the impact of sharing your lived experiences in these ways, as this is further proof of the difference it makes.”


The sun shone for our first Tea & Talk gathering, bringing a small group of PHA UK members together at our office in Sheffield.
The free informal event was a chance to meet others affected by PH in a relaxed setting, and it was a valuable get-together for us all. Lots was discussed, friendships were formed, and a delicious lunch kept everyone fuelled.
We hope to hold more of these intimate office gatherings, which sit separately from our larger and more formal ‘Together’ events, over the coming months. Please ensure you receive our monthly e-newsletter to be among the first to know when dates are announced – visit phauk.org/MonthlyMatters to subscribe.

A PHA UK study is aiming to increase understanding of the lived experiences of PH with lung disease.
The research is taking place throughout 2025, taking a mixed-method approach of interviews, surveys, and patient-reported outcome measures (which are used in clinical practice) to paint a clearer picture of how the two conditions affect people.
We’ve already conducted in-depth interviews with 20 PHA UK members living with both diseases, and the insights shared have been invaluable. The study is continuing, and we’ll share more updates in the next issue of this magazine.
A reminder of the patient perspective
In June, PHA UK members Bisma Hussain and Josh Howey (pictured below) helped a gathering of pharmaceutical company employees understand more about what it really means to live with pulmonary hypertension.
The pair, who were diagnosed with the condition in 2019 and 2024 respectively, joined the PHA UK’s Iain and Mary for a live Q&A in London. They candidly discussed the implications of dealing with the disease at a young age and shared their experiences of adapting to life with a chronic illness. It was a powerful reminder of what (and who) really matters when it comes to drug development, and we’re grateful to both Bisma and Josh for their time and insights.

International Nurses Day on 12th May was a chance for patients around the world to share their words of thanks for those who play such a key role in their care. Here’s a small snapshot of what you told us on Facebook about your very special PH nurses…
Clare Moore The nurses at my centre are so kind, knowledgeable and understanding. You can tell they really do remember who you are, actually care, and are interested. I’m newly diagnosed and they have felt like an absolute lifeline.
Anita Manson My nurses are amazing and have so much knowledge and understanding. Nothing is ever a problem and they are always on the end of the phone to answer any questions I have ��
Fiona Thompson A shout out to the amazing nurses who have been with us every step of the way since my husband was diagnosed with IPAH almost 18 months ago…We feel supported and cared for.
Julie Royle Our nurses are specialists in their field and always put our needs first at all times. They’re the most caring group of people we could meet ����
Molly Hart I can always rely on my nurses to sort out any problem and give me support. I can’t thank them enough xx
Shona Davis Our daughter was under PH nurses until she received her transplant last year… Their knowledge, expertise and communication with us has been first class. We will always remember with gratitude the role they have played in our daughter’s care.

PHA UK Chair Dr Iain Armstrong took to the stage at a major health and care conference in June, as part of a panel discussing the NHS England Breathlessness Pathway.
He represented people affected by PH in the influential discussion designed to raise the profile of the pathway – which aims to help speed up the diagnosis of diseases like pulmonary hypertension. The panel session took place at the NHS ConfedExpo in Manchester, a two-day event to drive innovation and improve care for patients and the public.
Published in 2023, the NHS England Adult Breathlessness Pathway is a pre-diagnosis support tool for healthcare professionals, designed to improve the early and accurate diagnosis of breathlessness. It involves the use of Community Diagnostic Centres (CDCs) – NHS facilities in accessible places such as town centres that give patients access to diagnostic tests without having to visit a hospital. The pathway aims to align clinical practice in primary care with guidelines, ensuring high-quality care and minimising variations across England. You can find out more about it at phauk.org/pathway.
Research conducted here at the PHA UK shows people are still waiting far too long to be diagnosed with PH, with delays remaining unchanged for the last 15 years. We are committed to playing our part in helping to change this.
Iain is pictured above with fellow panel members Sarah Sleet, CEO of Asthma + Lung UK; James Ramsay, Chief Medical Officer at NHS Sussex; and session Chair Alex Pinches, the National Lead for Community Diagnostic Centres with NHS England.
PH Day UK is back for 2025!
Pop Friday 7th November into your diary and look out for details of how you can get involved… Our annual awareness campaign takes place on the first Friday in November each year and aims to raise the profile of PH. Please support the initiative and help us turn up the volume.
2025 7th NOV UK DAY PH
My wife, mother-in-law, and aunt are all receiving treatment for pulmonary hypertension and my wife is currently utilising a Hickman line. This personal experience has provided considerable insight into the challenges posed by this disease.
I am a coach for my son Oliver’s rugby league team, the Farnley Falcons Under 10s in Leeds, and to raise awareness of pulmonary hypertension within the community we have sponsored my son's kit with the PHA UK logo for the next two years.
As we know this disease affects the lungs and heart, there’s nothing better than to spread awareness throughout sports week in week out. Our weekly team sheet, which also includes the PHA UK logo, is shared across all social media platforms.
This sponsorship raises awareness to other rugby clubs, but also Oliver feels proud wearing it and showing his support for PH.
We are really grateful to Lee and his family for this thoughtful support.


Thank you for the recent issue of emPHAsis. The article about self-image and identity felt really relevant to myself. I was diagnosed with PH in September 2024. I am 75.
I eventually got sorted with my medication and although l still have bouts of anaemia everything is under control. I also have a minimum of 17 hours oxygen. I’m a lot less mobile than l was and simple tasks have to be carried out slowly and be paced.
I was interested to note that some of your real-life contributors have holidays abroad. My husband and

My wife Leigh had PAH for most of her life and reading the dating feature in the last issue of emPHAsis took me back to 1998 when we started dating.
She was totally upfront about her condition and that it was life-limiting. To be honest I knew nothing about her PAH and Eisenmenger’s syndrome, but I was smitten with her and completely undeterred.
We married on the 5th June 2000 and lived a very happily married life until her passing in October 2019. She had been diagnosed earlier that year with adrenal cancer and the symptoms ultimately proved too much for her heart and lungs to cope with.
There’s not a day goes by that I don’t think of our love for each other.
I would hope that anyone that may read this would not let pulmonary hypertension stand in the way of a deep and loving relationship. Yes it takes commitment, but it is so worth it, and I speak from experience. Thank you for the opportunity to relay my story.
l can get away in the UK thanks to the NHS system that can supply oxygen to UK destinations and we are very grateful. Oxygen makes such a difference to my wellbeing. It would be great to hear other people’s experiences.
Thank you and I look forward to the next issue.
If you would like to share your experiences with Gill of going abroad with oxygen, please email media@phauk.org and we will pass them on.
We love to hear from you! Email your letters to media@phauk.org or write to PHA UK (emPHAsis), Unit 1, Newton Business Centre, Newton Chambers Road, Thorncliffe Park, Sheffield S35 2PH
If you need to talk, we’re here to listen...
Our free supportive call service gives you dedicated time with a PHA UK team member to talk through any worries or concerns you have relating to your emotional or mental wellbeing.
The Listening Line is for all PHA UK members and their family and friends too. It can help with:
• Adapting to a diagnosis of PH
• How to talk about it with others
• Coping with changes
• Concerns about the future
• Worries about loved ones
• How to access supportive palliative care
• Loss due to PH
….and much more! Please note we are unable to offer personalised medical advice or make or expedite NHS referrals.
Find out more or book a call at phauk.org/ListeningLine
Recent feedback from Listening Line users...
“This really helped me
when
I was diagnosed and scared”
“The
support lifted me”


Our Listening Line is operated by retired NHS nurses Paul Sephton and Sian Richardson, who have many years of experience in PH.
If you prefer support by email…
You can now choose and book your call online, at a date and time to suit you. Scan this code to find the next available appointment.
Our e-support service provides advice and signposting, or ongoing emails to help you through a difficult time. Contact us at support@phauk.org - at any time of day or night - and we’ll get back to you within two working days. You’re not on your own.





Our latest ‘Together’ event saw patients cared for by the Scottish Pulmonary Vascular Disease Unit (SPVU) gather with loved ones and their PH team in Glasgow.
Held at the Golden Jubilee Conference Hotel in May, this valuable day included educational talks and discussions, and many new connections and friendships were formed. Attendees enjoyed Q&A sessions with SPVU healthcare professionals, information sessions about clinical trials, and a presentation about our charity.
A special ‘patient panel’ segment allowed four PHA UK members to share their stories and experiences with attendees, and a raffle organised by supporters Nicki Ross and Jamie Beglin raised almost £300.
A delicious lunch was served halfway through the day, and regular break sessions provided lots of opportunities to get to know each other.
It was a pleasure to join forces with the Scottish Pulmonary Vascular Unit for this hugely beneficial gathering - which was completely free for patients - and we’re looking forward to organising more around the UK soon.
Keep an eye out for updates!



There
are many emotions to navigate when you have a condition like PH, and here psychotherapist Sophie Papagerogis - who has her own lived experience of pulmonary hypertension - explains more about two very common feelings…
Guilt and shame have been cropping up quite a lot recently within my therapy practice (and let’s face it, personally too). It’s quite fascinating (and sad) to see the impact this has on our lives.
Guilt and shame are often interlinked but have several differences. Guilt is the feeling of “I have done something bad and I am ashamed by it”, leading to feeling regret, remorse, fearing what the outcome might be, and wanting to do something to repair or fix the situation.
Shame can be even heavier than guilt. Shame is more like the feeling of “I am bad and my very existence is shameful”. If you have an inner critic who consistently tells you that you’re not good enough, and you find yourself feeling inferior to others, this can seep in and make us believe that it’s true.
Guilt and chronic illness (sadly) go
hand-in-hand for a variety of reasons. We may find ourselves feeling like a burden to loved ones, and feeling horrible about having to rest or say “no” to others. There’s often a stigma attached to aspects like maybe living at home with parents longer, needing to claim health benefits, and not working at 500mph all day every day. PH puts restrictions on our lives, whether this be in terms of exercise, having children, stamina/fatigue, symptom management…all these can add up and become difficult to manage, making us feel guilty about our impact on others, and perhaps even shame about ourselves. Shame is a weighty emotion, leading to a variety of tricky issues. We might have very low self-esteem, compare ourselves to others and negatively self-talk ourselves down. We may feel our emotions aren’t valid, and therefore shouldn’t be shared. We might feel we have to ‘prove’ ourselves in some way, which may be exhausting and unachievable. The worst thing about living with a sense of shame, is the desperate need to keep it hidden. Because if people see it, it’s shameful, right?!
Weirdly though, the best way to get rid of shame (or at least minimise it a bit), is to shine a big bright light on it. Shame likes to fester in the dark, and it wants to keep you there to eat away at you. Facing and sharing your perceived shame always lightens the load. I feel slightly awkward writing “always” because surely there will be exceptions to the rule. But from what I’ve seen in my work, it has never not helped to share the ‘shameful’ load. And most of the time, what we think is hideously shameful, really isn’t at all!
And frankly, it’s understandable to feel a bit crap about ourselves at times. The body can be a huge source of shame, feeling different to others can create shame, feeling that we need to rest more can create guilt, and changing our lives to manage symptoms and exhaustion can feel uncomfortable. These are all normal things that we deal with, day to day. And I would bet, if your friend or family member was dealing with what
we deal with, you wouldn’t think they need to feel guilty at all! So why are you so different? Self-care is not selfish. Having needs is normal. Having PH sucks at times. Managing it in the best way you can is courageous and worth celebrating. I think we’re all awesome! .
COMING SOON! We are currently working with Sophie to produce a resource to help people manage their mental wellbeing with PH. This will be made freely available via our charity, so please keep an eye out for details.
Keeping you informed and helping you to live well with PH
Our wide range of titles cover topics from medication to menopause, palliative care to pregnancy – and much more.




Scan to see the full library and order your copies, or visit phauk.org/publications


With a new academic year around the corner, some of you may be preparing to start a degree or considering applying for a course in the future. And with finances squeezed for many, this UK government grant could make all the difference…
Disabled Student’s Allowance (DSA) is a government grant, not a loan you have to pay back, and it’s designed to level the playing field and make sure you have everything you need to succeed in your studies. It’s available for those living with disabilities or long-term health conditions like PH, mental health conditions, or a specific learning difficulty like dyslexia.
You can apply if you live in the UK and you are studying any type of course (full-time, part-time, or even distance learning). It doesn't matter what your or your family's income is – DSA is all about what you need, not what you earn.
DSA is pretty flexible and can help with all sorts of things. For the 2025-26 academic year, you could receive up to £27,783 to help with the costs of:
• Technology that makes studying easier (like specialised computer equipment or software)
• Non-medical helpers (such as note-takers or mentors)
• Extra travel costs to attend your course or placement because of your health condition
• Other disability-related study support, for example having to print additional copies of documents for proof-reading
If you need a computer, you'll need to contribute the first £200 but DSA covers the rest.
DSA does not cover disability-related costs you’d have if you were not attending a course, or costs that any student might have. It is specifically for costs associated to your health condition.
• Apply as early as you can, ideally before your course starts
• Keep copies of all your documents
• Don't be shy about asking for help – that's what DSA is there for!
• Remember, this support is your right
1. Take the first step: Apply through your regional student finance body. If you're studying full-time, you can usually do this online.
2. Show your evidence: You'll need to provide some proof of your condition, which could be a letter from your doctor or an assessment report. Don't worry, the process is designed to be straightforward!
3. Have a friendly chat: Once you're approved, you'll have what's called a ‘needs assessment’. This isn't a test - it's just a relaxed conversation about what would help you most. You can even do this remotely from home!
4. Get your support in place: After your assessment, you'll receive a detailed plan of all the support you're entitled to. Most of the time, payments go directly to the people or companies providing your support, so you don't have to worry about handling the money.
Remember, DSA exists to help you make the most of university. It's not just about providing equipment or support – it's about making sure you have everything you need to reach your full potential.
Find more details about DSA at phauk.org/DSA If you need extra support or guidance when applying, you can get in touch with disabilityrightsuk.org or scope.org.uk


“Singing has proven to be a huge outlet for my emotional wellbeing when dealing with my illness”
When Jen Bardsley-Taylor was diagnosed with PH last year, it came as a total shock. She was working hard as a singer, actor, business coach, and presenter – and thankfully a positive response to treatment has allowed her to continue her career. We all have a story to tell, and here the 26-year-old from Gloucestershire, now living in Merseyside, shares hers…
At the age of 11, I started getting out of breath when exerting myself and very occasionally fainting. This was a big concern, but following a variety of extensive hospital tests, I felt reassured by the conclusion that my issues were as a result of low blood pressure, and that I would likely grow out of it.
Life went on, and as the medics suggested, my symptoms even appeared to improve. I went through school and my degree, graduating from one of the top drama schools in the country. Performing is my passion. Looking back, I’m so grateful to have been part of every stage or screen production at drama school, even performing in dance shows. In hindsight, I wonder if I’d just learned to listen to my body and adapt my behaviour, following my low blood pressure diagnosis. At the time, if I was ever getting dizzy or out of breath, I would briefly remove myself from the activity until things normalised. I never passed out while at drama school.
I still didn’t take my health lightly, but medical advice continued to indicate that my symptoms were simply a result of me having low blood pressure, so I took everyone at their word.
Five years after I graduated, I surprisingly fainted again during exercise. Shortly afterwards, my sister was diagnosed with cardiomyopathy, a heart muscle disorder. This prompted me to see my GP to get checked over again, and because of my sister’s condition, it was agreed to refer me for wider tests at my local hospital.

was devastating for them too. They insisted on returning straight home to be on-hand, driving over 3,000 miles in just a few days to be with me in those very challenging early days. My close family and boyfriend, Ryan, have been amazing. We have had numerous heartfelt, challenging, and often tearful conversations. Their support has
“The initial conversation with my consultant regarding the severity of the disease hit me hard”
Following these investigations, I received a call from the cardiologist to say I was being referred to the Sheffield Pulmonary Vascular Disease Unit, a specialist PH treatment centre. Given that I’d already had a firm diagnosis of low blood pressure for the majority of my life, I assumed my visit was just for further exploratory testing. Unfortunately, this was not the case and I was confirmed as having severe pulmonary arterial hypertension (PAH). The initial conversation with my consultant regarding the severity of the disease hit me hard.
My right heart catheter investigation showed very high pulmonary pressure readings, and it was a real shock, as previously I’d been leading a busy life and doing so much – despite having this disease.
My parents were on a driving holiday in Portugal at the time, and my diagnosis
been invaluable and has helped me to navigate and begin to come to terms with my diagnosis.
I encouraged them to read lots of leaflets and PHA UK publications, and then ask me questions, which they were very happy to do. I have also found the PH community to be incredibly helpful and humbling too; stories, articles and webinars, including within emPHAsis magazine and various support groups, have proved highly informative and valuable.
My discussions with loved ones have formed the basis for how I broach my diagnosis with friends and colleagues; something I still find very difficult and am figuring out how to do better on a daily basis.
As a self-employed professional, I don’t see or work with the same people every day so it’s tough to know how and what
You can listen to Jen sing by following the links on her website: www.jenniferbardsley.co.uk
to tell others, especially as I don’t want to have difficult conversations just before socialising or performing. I’ve always been proud of my professional reputation too and am eager to continue to lead as normal a life as possible.
Thankfully, the staff at the Sheffield Pulmonary Vascular Disease Unit have been incredible; they’re so dedicated and well-informed. I love the way that I’m never rushed during consultations and that they are willing to explore all issues, medical and more broadly, particularly when they are often so personal to me.
I’ll always be grateful for the care and attention they’ve given me, even though some of the subjects have been tough to talk about.
So far I’ve been lucky and have responded well to the treatments offered. My symptoms have reduced dramatically. I never take this for granted, and am always mindful of others less fortunate than me. My diagnosis has given me an explanation and greater understanding of things I’ve known about myself for years.

Now, I just try and do everything I can to be as healthy as I can be. I always take my medications, routinely monitor my blood pressure and pulse, and report anything unusual to my specialist centre. I continue to be as active as possible and am careful about what I eat. I’ve started learning more about nutrition and have stopped drinking alcohol completely.
My mental health too has always benefitted from keeping as active as possible, and by me performing. Singing has proven to be a huge outlet for my emotional wellbeing when dealing with my illness.
I know it’s different for everyone, but when I commenced my treatment, I initially experienced nausea, indigestion and headaches, but over time these have improved. The main thing I continue to suffer with is fatigue, but I still love running my own business and having an active social life – which I’m so grateful for.
Jen will be performing at Together25, our special event in August to mark the 25th anniversary of the PHA UK.

“I have found the PH community to be incredibly helpful and humbling”
2025 marks 25 years since the PHA UK was formed, so could you help us mark our milestone by gathering sponsorship for something related to the number 25?
Here are just a few ideas:
• Walk 25 laps of your garden over the course of a week
• Give up coffee, alcohol, swearing or chocolate for 25 days
• Read 25 books (or chapters!)
• Make 25 cupcakes or cookies for a coffee morning …the possibilities are endless! Why not encourage little ones to complete 25 household chores in return for donations?


Acts of kindness…
• Pick up 25 pieces of rubbish during a walk
• Spend 25 hours volunteering through the year
• Send 25 cards to residents of local care homes
For the sporty ones…
• 25 press ups a day for 25 days
• Cycle 25 miles
• Run 25km
• Swim 25 lengths
Whatever you choose to do, we’ll be with you all the way. Please scan the code to complete our registration form and we’ll send you some goodies to help you with your fundraising and raise awareness of PH.


If you have any questions, get in touch with us by emailing fundraising@phauk.org We’ll always be happy to help!
Gifts in Wills help us continue our work to support people affected by PH – making a huge difference to those dealing with this challenging disease. Could you or your family consider thinking of the PHA UK in this very special way?
Legacies, however small, play a critical role in supporting our work and securing the future of our charity.

“I updated my Will recently and decided to include the PHA UK as a way of giving something back for all the support I’ve received. It feels like a thank you from me and my family and it will help them to continue their work to help others.”
Julie, PHA UK member since 2012
Thanks for chatting with us, Victora!
What’s the biggest thing you’ve learned about PH, or about yourself, since being diagnosed?
That I am capable of whatever I put my mind to, and that PH isn't holding me back (I try not to let it, anyway). Travelling is my passion, and PH makes it a bit trickier, but I don't let it stop me.
Whereabouts do you receive your PH treatment?
The amazing Royal Brompton Hospital in London. I enjoy the familiarity with the team after so many years. I'm one of many patients but they still take an interest in my life when they see me, and I couldn't ask for better care. Oh, and I do appreciate the amount of airline health forms I have asked them to sign over the years ��
What’s the best thing about being a PHA UK member?
I’ve been a member since my diagnosis; I signed up when I was still in hospital. The best thing is the community and knowing I'm not alone in having the disease (sadly). The PH community is amazing and so supportive and encouraging.
What does ‘living well’ mean to you?
Having a good balance. Spending time with friends and family and doing what I enjoy but also taking time to heal. As I've gotten older I've learnt that sometimes I need a day in bed to feel better the next day. Every year is a blessing since my diagnosis.
What advice would you give someone newly diagnosed with PH?
Don't be scared. I remember when I was diagnosed I thought my life was over, but the treatment has evolved so much. And don't Google! I was so afraid of the worst-case scenarios, but everyone is different. Listen to your healthcare team (they are experts!) and don’t let PH define you.
And finally, what makes you smile?
Spending time with my family (this is so precious when you have as many health conditions as me) and travelling. Exploring a new country is one of my favourite things to do!
Travel fan Victoria Sant recently turned 40 and when she’s not exploring the world, she lives in Surrey. She was diagnosed with pulmonary arterial hypertension in October 2016 and has other conditions including autoimmune hepatitis and connective tissue disease.



"Me on some of my travel adventures…"



Help our community get to know each other!
If you would like to introduce yourself to other PHA UK members in this feature, scan the code or visit phauk.org/MeetTheMember to complete our short form. You could see yourself on our website or in a future issue of this magazine…


Summertime means holidays, garden gatherings, weddings, and barbeques – and if you’re newly-diagnosed with pulmonary hypertension, you might be wondering whether you can still enjoy a drink.

We hear many questions in our community around this topic, so this feature aims to shed some light and help you make informed decisions.

Carl Harries, Lead Clinical Nurse in the Royal Brompton Hospital’s PH service, has 22 years’ experience of caring for people with pulmonary hypertension.
Having PH does not exclude you from having a good time, whether that includes alcohol or not. For some people, alcohol simply isn’t part of their lives, but for some people it is. We need to be realistic about that, and to give patients credit – it’s not for us to lecture on safe limits.
A lot of people newly diagnosed with PH will ask if they are ‘allowed’ to drink and we need to normalise this question. They ask if they are able to have the odd drink at a party, or if they drink a fair bit, whether they can continue with that. My answer is always the same…

There are only two reasons you would need to be a bit careful with alcohol if you have PH – one is if you are
on warfarin and the other is if you are on diuretics (see the question and answers opposite). However, these are issues which are easily managed most of the time. You simply need to be aware of them.
The answer to whether you can continue to enjoy a drink, is simply ‘yes’. It’s important to continue to enjoy social engagements, and to live a life beyond your illness.
Drinking alcohol is personal choice, and you don’t need to have a diagnosis of pulmonary hypertension to drink sensibly. I take a real-world view on this!



In 2023 we conducted a survey of the eating and drinking habits in our PH community, to help us tailor effective support.
Over 600 people with PH responded, and the findings showed that:
35% never drink alcohol
22% drink once a month or less
16% drink 2-4 times a month
18% drink 2-3 times a week
9% drink 4 or more times a week
How does this compare to the general population? A 2021 NHS Digital survey showed that 21% of adults has not drunk alcohol in the last year, and 49% drink alcohol at least once a week.










The most important thing to mention here is that there are no known interactions between alcohol and PH-specific therapies. That means the tablets, or the nebulised or intravenous medicine you take to treat your PH, won’t be affected by consuming alcohol. Drinking won’t make it less effective or cause unwanted side effects.

Dr Neil Hamilton, Consultant Pharmacist at the Sheffield Pulmonary Vascular Disease Unit, explains more about medication and alcohol….
“My aim here is to try and dispel some myths and bring some reality to discussions that I frequently overhear, and address questions we pharmacists get asked around drinking and medicine. Much of this advice is not unique to patients with pulmonary hypertension and consists of general tips and considerations applicable to all.”
Patients prescribed warfarin can safely consume alcohol, provided it is in moderation. A steady, regular intake of two units per day is preferable to 14 units* in one night. Binge drinking close to an INR (international normalised ratio) blood test check may well affect the result, so be aware, and if you have drunk more than usual near to a blood test, just let the clinic know so they can interpret the result in context.




This depends on which type of antibotics. There is no blanket advice across antibiotics. As you may be aware there are many different medicines we treat
infections with, so make sure you check with your doctor and / or pharmacist to be certain. The ones to definitely avoid alcohol with are metronidazole and tinidazole. Others that can be problematic are co-trimoxazole, linezolid, doxycycline, nitrofurantoin and erythromycin. The NHS website (www.nhs.uk) has more helpful advice on this subject.
My advice here is to take care. Alcohol does have a ‘diuretic’ effect, causing you to pass more water. Patients with any tendency towards fluid retention should take care when drinking beer, cider or anything ordered in larger volumes (such as pints). I would also urge some caution if taking diuretics when consuming significant amounts of Continued...






alcohol as the added diuretic, and therefore dehydration, effects would be potentially damaging to the kidneys and blood salt levels if repeated regularly. If you know you will be drinking in the evening, I suggest taking your diuretic medication in the morning, to lessen the chances of you needing lots of visits to the loo.
This depends on which ones. Strong painkillers such as ‘opioids’ - which includes morphine, tramadol and codeine - all have the potential to cause drowsiness and nausea. This will be enhanced by alcohol. Sensible advice here is to avoid alcohol altogether when starting a new painkiller and also immediately after a dose increase. This way you can assess how the change is affecting your body.

“If you take your medication via an IV line or a nebuliser, my advice is that you avoid making up your pump or nebuliser after drinking alcohol. These tasks require concentration and a sterile environment, both of which can be impaired by drinking. If you know you will be having a few drinks, it’s best to plan to do all this beforehand. If you are on oral medications, you may wish to take these earlier in the day too, to lessen the risk of forgetting.
Coping with a condition such as PH can be stressful and cause anxiety, depression and other mental challenges. There are some interactions between some of the older anti-depressants, but these are far less frequently prescribed nowadays. Newer treatments are likely to be preferable but it is always worth checking if in any doubt.
For many of us, drinking alcohol socially is a pleasure, and as with lots of things in life, enjoying a drink in moderation is unlikely to interact too much with commonly prescribed medication.
Sticking to the government’s safe alcohol limits of 14 units per week is applicable to us all, as the evidence suggests this reduces health risks. Your pharmacist, either locally or at your specialist centre, will be happy to advise on alcohol in relation to your specific treatments.”
*See opposite for more information on units





If you choose not to drink at social gatherings, gone are the days of Diet Coke being your only option. The alcohol-free drinks industry is booming, and supermarkets, pubs and restaurants now stock a wide range of low-or-no-alcohol beers, wines, and spirits. Most establishments also have an impressive menu of mocktails too.
Found an alcohol-free drink you want to shout about? Email media@phauk.org and we’ll share your recommendations…




The NHS recommends that to keep health risks from alcohol to a low level, if you drink most weeks, you should stick to no more 14 units a week. This is now the same recommendation for both men and women. But what does that look like in reality?
A pint of average-strength (ABV* 5%)
lager, beer, or cider
A single (25ml) measure of vodka, gin, rum, or whisky
3 UNITS
1 UNIT
A medium 175ml glass of wine (ABV 12%)
2.1 UNITS

A large 250ml glass of wine (ABV 12%)
3 UNITS

*ABV stands for Alcohol By Volume, and is a standard measure of how strong a drink is.
Unsure how many units are in your drink of choice? Try the handy online calculator by Drinkaware at bit.ly/UnitsCalculator to work it out.



Fancy tracking your drinks?
If you think you’d find it helpful, there are now lots of free apps around that allow you to track what you’re drinking and calculate your units, calories, and even what you’re spending on alcohol. Try My Drinkaware (which also allows you to track your sleep), DrinkControl, or Drink Free Days (which is produced by the NHS).

If you would like help to reduce your drinking, contact your GP who can provide you with advice or refer you for extra support in your area. You’ll also find advice, support, and resources via the UK-based charities Alcoholchange.org.uk and Drinkaware.co.uk
From Consultant Pharmacist Dr Neil Hamilton
All medication for pulmonary hypertension must be prescribed by your specialist centre and delivered to you.
Summer holidays may have an impact on these services but there are several ways that you can help in making sure your deliveries run smoothly. All of the following highlight the need for a good relationship and communication:
• Make sure you are in at the agreed time slot to receive a delivery. The NHS has to pay for each delivery slot, so it is crucial these are not wasted.
• They may use a number which shows on your phone as “unknown/withheld number”. This is also true of the hospital. Please do not ignore these calls if possible.
• If you miss a call from homecare, please return their voicemail message.
• The NHS contract requires homecare companies to ask you for a regular stock check. If this is not possible when they call, please do this as soon as you can and call them back.
• If you get into your last two weeks of supply and you have not heard from your company, please call them. Last-minute or emergency delivery runs are difficult for everyone and costly to the NHS. These can and should be avoided.
If you have any queries regarding your stock levels or delivery dates, your PH centre is unlikely to have the information you need, so the best people to contact are the delivery companies directly.
(formerly known as Healthcare at Home)
Deliveries 0333 103 9499
Emergency line for IV Pump replacements 0333 207 6343
0800 783 3178 (+ option 3)
Deliveries 0800 083 3060
Emergency line for IV Pump replacements 0113 340 1833
Deliveries 0345 263 6123 (option 9)
Emergency line for IV Pump replacements 0345 263 6122

With summer in full swing, do you have plans for time away?
Having pulmonary hypertension doesn’t mean you have to stop enjoying UK breaks or seeing the world — but it does require a bit of extra preparation. Our dedicated web area aims to answer common travel questions around topics including
Can’t find what you’re looking for online?
Email support@phauk.org and we’ll do our best to help…

An easy and affordable way to support our charity from just £1 a week… with the chance of winning up to £25,000!
✓ Regular cash prizes from £5-£25k
✓ Automatic payouts (no need to claim)
✓ Just £1 per entry
✓ Enter as many times as you like each week

“It’s
Last year, Bethany Boyden entered hospital to have a baby and left with a PAH diagnosis and a Hickman line. Her story is unique, and she is sharing it here to help others feel less alone…

"I think the enormity of the whole situation hit me all at once"
Iwas healthy before conceiving, working long and active shifts as a healthcare assistant and going to the gym, and until the last stages of my pregnancy I had no symptoms to suggest anything might be wrong.
From around 34 weeks, I started to feel light-headed. Three weeks before Elsie-Lucille was born I could just feel that something wasn’t right, but the GP told me everything was fine. I couldn’t make the ten-minute walk to the local shop without stopping, but I was told it was just part of pregnancy. This was my first, so I had nothing to compare things to.
I had a natural birth at my local hospital in Grimsby, a day before the due date. The labour was fine, and everything went well. I was preparing to take Elsie-Lucille home 24 hours later, and whilst my partner took my case to the car, the nurse took my blood pressure one last time. I remember her saying ‘I don’t like those numbers’ – and they decided to keep me in for a few more hours. I didn’t think anything of it.
My oxygen was checked, and that triggered a scan they couldn’t do whilst I was pregnant. I was told to call my partner back to look after Else-Lucille, and that’s when I knew something was really wrong. My mum died of a

pulmonary embolism, so we thought it might be a clot.
A group of doctors came into the room, and I was told I was being taken to the high dependency unit – without my baby. It was a whirlwind and as they took me away, I wondered if I would ever hold her again.
A day later, I was transferred to the specialist PH centre in Sheffield for further tests, so I was now two hours away from my three-day-old newborn. I’d have night terrors and rip my oxygen off, thinking she was crying and I couldn’t get to her (even though she wasn’t there) but the kindness of the nurses made such
My first photo with Elsie-Lucille, just after she was born

into her arms. I think the enormity of the whole situation hit me all at once. I’d gone into hospital to have a baby and within four days I was being diagnosed
"I knew I couldn’t give up, and I’ve adapted to this new way of life"
a difference. I was hooked up to all sorts of monitors and I was begging them to tell me if I would die, but it wasn’t something they could answer.
When I was told I had pulmonary arterial hypertension after the right heart catheter test, I had no idea what it was. It destroyed me to find out it was incurable. Elsie-Lucille was just four days old; a little doll.
I stayed in hospital and was put onto intravenous therapy when Elsie-Lucille was three weeks old. That was huge to deal with on top of everything else. When I came back from theatre after having my Hickman line fitted, the specialist came up to me. All she said was ‘are you alright?’ but it was said with such a soft tone that I just bellowed and crumbled
with an incurable condition – and then having a line put into my chest.
As well as having to stay in hospital to be trained on the medication, I also contracted COVID-19 – so I was in Sheffield for over a month, whilst Elsie-Lucille was at home. It was such a long time to be away from her.
Despite being so pleased to be back with her, the first night at home after being discharged was incredibly hard. Elsie-Lucille was five weeks old and I was sitting there with a newborn baby, my Hickman line, and all the medication, wondering how the hell I was going to cope. How was I going to be strong enough to be her mum as well as administer my own medication and do my own dressings? How was I
I keep my scan images framed in my living room
going to be able to do night feeds? Would I be enough for her? There was so much going through my head.
I was struggling with air bubbles in the medication, with the medication cassettes, and with the deliveries of the medication too. I’d barely had to take paracetamol for a headache before all of this.
But I knew I couldn’t give up, and I’ve adapted to this new way of life. Elsie-Lucille gives me my strength. If I had been diagnosed without a baby, perhaps my mindset would have been different. But she needed me, and I needed her.
The timings around my IV medication were really challenging at first because I had to stick to the ones I’d been on in hospital – where I had nothing else to juggle. Back home, I had to work around a newborn, a partner, baby groups, and everything else.

My partner is a truck driver, so when he was out working, there was no-one to look after Elsie-Lucille whilst I sorted my medication. For the first three months I tried to time it in-between her feeds, but because everything has to be so sterile, I couldn’t touch her if she cried whilst I was sorting it, or if she needed her nappy changing. It would take me up to 45 minutes, and on bad days I got through multiple gloves, dressings and cassettes.
Now though, I’ve managed to change the time I do it each day so that someone can be there with her. As a mum, that was a hard pill to swallow though because I wanted to do it all without having to have someone there. I’m quite a loner and I’ve always tried to cope with things on my own, but I had to accept I needed people around me if I was going to get through things.
Now Elsie-Lucille is a bit older, she touches and pulls on the Hickman line without realising. She wraps her hands or feet in it or pushes against the buttons on the pump. These are things no-one can prepare you for, and I worry that things will get harder as she gets older. Will she try and pull it out? Will I be able to keep up with her as she gets more mobile?
And of course, I worry about the disease progression. What if it gets to the point where the medication isn’t helping me anymore? Then what? But I've got a reason to stay alive. I’ll do whatever the consultants and doctors say because Elsie-Lucille is my world, and I need to stay around for her.
If it wasn’t for Elsie-Lucille, I would never have known I had PAH. In that sense, I was lucky. Giving birth saved my life. I’m lucky too that I have my daughter, as I can’t imagine how I would have dealt with the diagnosis without her. She has saved me in so many ways.
I'm so thankful to the team at the specialist centre in Sheffield too. They are remarkable people, and I put my trust wholeheartedly into their hands. During that awful time post-birth they treated me like a person, not just a patient. When I go back for appointments now, I love to see them, and to show them photos of Elsie-Lucille.
I wanted to share my experiences with others via the PHA UK because I was so lost when all of this was happening to me. I felt like such a unique case, and I was searching desperately for people to relate to – in the charity’s booklets and magazine, and on
online forums, but I never found someone that had experienced the diagnosis in the way I had. If telling my story can help just one woman who ends up in the same position I was, then it has been worth it.
It's not an easy story to tell, and I do feel proud of getting through it all, but mostly I just feel lucky. Lucky to be alive, and lucky to have Elsie-Lucille. She is my strength.

PAH almost killed me, and it took so much away from me, but it's not going to carry on doing that. I’m still me, and I’ve got a lot to be thankful for. I can’t look at it in any other way.
"I’ve got a lot to be thankful for"
In his
Neil Gambrell, 68, lives with PH alongside chronic obstructive pulmonary disease (COPD). He uses his experiences of working with people with mental health conditions to manage his own emotional wellbeing.
Before I had to take ill-health retirement, I spent many years as a support worker for people with serious mental health conditions living in supported housing. There were 17 residents with a whole range of issues including paranoid schizophrenia and personality disorders, and I learned a lot there that I can apply to my life today.
It certainly helped me a lot when I was initially diagnosed with PH last year, after living with COPD since 2022. Hearing it was a rare disease without a cure was difficult. But my training allowed me to take a step back and see that whilst the two conditions might be incurable, that didn’t mean they couldn’t be manageable.
I’m part of the PHA UK private Facebook group and I read a lot from people newly diagnosed talking about fear and trepidation. Some people worry their ‘life is over’ – but the bottom line is that it isn’t.
I try to give myself the advice that I would give to other people, and
particularly the advice I gave at work. During my career, some of the stories I would hear from residents would be very distressing – but it was my role to help them see they could still live a good life, and that they didn’t have to carry on feeling like a ‘victim’. I'd be naive if I said that worked with every single resident, but when it was successful, it was the best feeling in the world.
I encouraged the residents not to be defined by their illnesses, and that applies to me now. I am not defined by PH, and I am not defined by COPD. I’m still the same Neil I was before these health conditions – I just do things a little slower!
I try and concentrate on doing things which I know are good for both my body and my mind.
I know I won’t be running a marathon any time soon, but I have an exercise bike in my flat, which I use daily, and that makes me feel good because I know it’s good for my health. And it’s something I can do. From a mental standpoint, I try to focus on what I can still do, rather than what I can’t.
The exercise makes me feel better both mentally and physically. Clearly, PH and COPD affects energy levels and mobility, but the bike helps with my fatigue, and when I keep up with it regularly, I notice how much better I’m able to move around my flat.
Completing a session on the bike gives me a sense of achievement and exercise releases a feel-good hormone called dopamine.
Whilst it’s important for me to understand my body, I have recognised that with all the technology aroundsuch as smart watches that monitor your heart rate - it can be easy to become obsessed. Constantly tracking your ‘data’ means everything revolves around your illness and it becomes what defines you. Now, all I use on a regular basis is a pulse oximeter on my finger. I’ve still got a smart watch, but it’s basically just there to tell me the time.
I accept that I have PH and there is currently no cure – there’s nothing I can do to change that. But there are things I can do to change the way I approach my new life. I live on my own, and whilst I had a carer to come in and help when I was first diagnosed last year, I have learned to now do things
“I am not defined by PH, and I am not defined by COPD. I’m still the same Neil I was before these health conditions –I just do things a little slower!”

myself. I do all my own cooking and housework and simply accept that it takes a long time.
I try not to look back on my life pre-PH, because it risks getting fixed into negative thinking. Yes, I could walk uphill before, but it doesn’t matter how much I whinge that I can’t anymore – it’s not going to change. Like I said, focus on what you can do, not what you can't do.
I do try to talk about my health and how I feel with a select few people – namely my daughters, my brother, and my best friend. I need to do that, because it’s not good to keep everything inside your head. Last year, being diagnosed with PH, was scary. I was very ill, and it was a difficult conversation with my daughters, but they
are encouraged by how much better I am now. We are able to talk about the future again. I think sharing how you're feeling and being honest about how you're feeling, is very important. I was scared last year. I wasn’t strong enough mentally to do it all on my own, so I shared it with my daughters, and that made a big difference.
Do you feel you need support for your mental health? Turn to pages 44 and 58 for details our self-help programmes for people who live with PH and anxiety or depression.


Our regular space for children with PH

My favourite out-of-school activity is… Jujitsu
My favourite flavour of crisps is… Teddy faces (salted)
My favourite film is… Harry Potter
My favourite place is… Fuerteventura - a family holiday last year. I played in the pool every day with my cousin Jessica and bought lots of Pokémon cards.
Dominik Pavlik is 9 years old and lives in Preston, Lancashire. He was diagnosed with PH 2 years ago.
My favourite thing to watch on TV is… Traitors
My favourite animal is… Snake

My favourite book to read is… The Tom Gates series
Dominik as his favourite film character, Harry Potter
My favourite thing to do at school is… Art
My favourite meal to eat is… Fish and chips


Do you know a young person with PH who would like to share their favourite things in this magazine? Email media@phauk.org and they could see themselves on these pages!

Coco is 11 years old and has been treated for PH since she was a baby. She has a twin sister, Aika, and they live with their parents in London.
Given that I love reading, my mum has taken me to many author events to see the people who have written some of my favourite books. So far I have met: Liz Pichon, Alex T. Smith, Rob Biddulph, Jacqueline Wilson, Maggie Aderin- Pocock and Andy Griffiths.
Budding journalist Coco Praest is our Kids Corner columnist and for this issue, she interviewed the comic artist and author Jamie Smart – well-known for his children’s cartoon series.
Since I was little, I have always loved books. One of my ideas of a fun day out is to go to a bookshop or library. Every year, I dress up for World Book Day. It is a day celebrating reading and books all around the world and you get to dress up as any character from a book or comic. It's really fun! This year, my sister and I dressed up as Pig and Weenie, two characters from Bunny vs Monkey (or BvM for short).







One of my favourite (award winning) authors is Jamie Smart, who writes BvM. I like his comic books because they are really funny and jam-packed full of action! To find out more about Jamie Smart and his books, I decided to interview him.
Jamie Smart was encouraged by his parents to do art because they weren’t allowed to become artists themselves. His mum and dad loved what he was drawing from a very young age and really wanted him to become an artist. They are very happy he’s a cartoonist now. His sister is also a fine artist and makes 3D art.
Coco and her sister dressing up as characters from Jamie's cartoon series for World Book Day

Keep reading over the page..!

When he was at school, his favourite subjects were English and Art. As a child, he was interested in becoming an archaeologist, but also knew that he wanted to be a cartoonist.
his first ever job which was a newspaper round. He didn’t enjoy it though, so he only did it twice because the newspapers were really heavy.
He is best known for his funny, laugh out loud comics like: BvM, Megalomaniacs and Looshkin. He also writes comic strips for The Phoenix. Jamie Smart has been writing BvM for 11 years and has 10 books so far and another three already drawn. Book 11 comes out in October. He also has enough Megalomaniacs comic strips to make three books which will come out over the next few years.
He is most proud of the first panel of every comic strip and often makes them look big and dramatic. is favourite character to draw is Bunny, he has drawn him thousands of times and he is very easy for him to draw. Action Beaver is the trickiest character to draw because of the big helmet.
He also writes spin-off BvM books like joke books and puzzle books. He hopes to make BvM for a very, very long time because he really enjoys making comics. I asked him if there would be a BvM movie, but he said there’s a lot involved and
Growing up, he read Calvin and Hobbes by Bill Watterson. It's a funny little comic about a boy and his teddy tiger from the 80s and 90s. It was his favourite when he was a kid. My mum bought some Calvin and Hobbes books for Aika and I to read. They were enjoyable and we liked them.
His top movie when he was a child was Back to the Future. He watched it about ten times and he loved it. His favourite video game was Dizzy (about an egg with boxing gloves) which was played on an Amiga computer. At 14, he started

Interviewing Jamie via Zoom

if it did happen it wouldn’t be for quite a long time. Jamie thinks that the character he is most like is Bunny because he just wants a peaceful life but there’s all this chaos happening around him. His favourite character ever is Bin Bag Sam (who is a bit unusual) because he’s a wombat sitting on a load of bin bags and he was rude to Monkey and Bunny equally.
His BvM books have how-to-draw guides of one or two characters. He said: “I’m very keen to show people that everything I draw is made out of very, very simple shapes and it's a case of putting those shapes together.”
He creates his comics at home with his pet dog Rocky (who is a labrador and lurcher cross) in a room dedicated to writing and drawing. To create his comics, he uses an A3 sketchbook (from an art shop) and 2B pencils. After he has drawn a page of artwork, he goes over it with ink. He uses a very thin paintbrush. It can be messy, but he is very
careful as he’s been doing it for many years. His tips for becoming a comic book artist is to love drawing and the more you draw the better you get. You need to enjoy it and want to tell stories you’ve always wanted to tell. His advice for when you’re stuck when writing a comic is to just plow on and get it done and if you still don’t like it, give it a rest for a few days and look at it later.
His favourite snack when writing is biscuits like chocolate digestives. I like them too. His favourite chocolate bars are Aero (the minty one), Cadbury’s Big Taste triple chocolate and Reese’s bars. One of his favourite foods is Chicken Katsu curry.
I sometimes make comics at home. My twin sister Aika makes her own comics too and has a comic club which my parents and I attend. She gives us starter activities, shows us how to draw things and gives badges for good drawing. Aika’s comic club is the best! Recently, I joined an after-school comic club. We get to read Beanos and The Phoenix (which BvM is in) and do drawing. For fun, I do online drawing workshops like the Magical Students Workshop with Sam Davies and a Donut Squad Workshop with Neill Cameron.
I’m very fortunate that I interviewed Jamie Smart. I think he is an inspiration to children who want to make comic books when they grow up. I can’t wait for his next BvM book to come out!
We have 5 copies of Bunny vs Monkey: The Whopping World of Puzzles to give away to lucky Kids Corner readers. These books have very kindly been purchased and donated as prizes by Coco’s family. To be in with a chance of winning, simply answer the following question (the answer can be found in Coco’s interview!)
What is the name of author Jamie’s pet dog?
Ask an adult to email your answer to media@phauk.org with your name and address, before the closing date of Friday 12th September 2025. We’ll select 5 winners at random, who will each receive a copy of the book. Good luck!
Dr Chris Chew, a
Lung

and PH, is passionate about helping his patients understand palliative care and the support it can provide. In his own words, this is why it matters…
In my experience, it’s perfectly normal to get a jolt of anxiety or even fear when your doctors bring up the topic of palliative care or suggest that you should meet your local palliative care team. After all, a lot of people (including some doctors) still think that you only get palliative care if you’re imminently dying and don’t have long left for the world. But that’s not the whole picture anymore – palliative care is actually quite a young specialty, and a lot has changed since it was founded!
In fact, palliative care got its start right here in the UK, when Dame Cicely Saunders founded St. Christopher’s Hospice in London in 1967. Dame Saunders wanted to make sure that dying and terminally ill patients weren’t simply left alone, as they were often neglected by the medical establishment at the time. However, she also advocated for a more holistic approach to relieving discomfort in all its forms, coining the term “total pain”. This described not just physical symptoms, but also mental distress, social, and spiritual issues too. Nowadays, as the specialty of palliative care has grown and expanded, there is an increasing focus on relieving symptoms and discomfort rather than just caring for those in their final days.
A lot of patients receive palliative care successfully in the community for many years. In fact, some studies even suggest that those receiving palliative care can live longer than those who don’t!
So, how do I usually explain palliative care to my patients? I tell them that getting palliative care professionals involved is about helping us find the right balance in their care, in all the ways that matter most. After all, our palliative care colleagues bring both common sense and specialised experience to the table!
The first ‘balance’ is making sure we remember that symptoms and discomfort are important in themselves and should be treated. We always do everything we can to cure or stop disease. But even if we can’t yet alter a disease’s natural trajectory, it’s still vital to ease the impact of symptoms.
For example, a lot of really common diseases - such as asthma and diabetes - aren’t actually curable, yet. But we can get a lot of mileage by treating the symptoms, like with inhalers or insulin injections. Similarly, palliative care teams are experts in palliating symptoms like breathlessness, pain or fatigue, even when the underlying disease itself isn’t curable.

Palliative care isn’t a one-way trip to some sort of strange parallel medical universe.
Instead, it works hand-in-hand with your usual medical care – making sure we are getting the balance right, together with you.
Visiting from Australia, Dr Chew has spent the last year working as part of the pulmonary hypertension team at the Royal Brompton Hospital in London. He is also part of the PHA UK research team studying the lived experiences of PH and lung disease.

The second ‘balance’ is making sure that we have our priorities right between the future and the here-and-now. In medicine, we often ask people to put up with a lot of things that are tough or unpleasant in the here-and-now (like surgery or chemotherapy), in the hopes of better days in the future. But if it becomes clear that time is short or limited, figuring out how to make the most of right here and right now might be more sensible than suffering for an unclear future.
The third ‘balance’ is remembering that psychosocial support is just as important as medical care for quality of life. Many palliative care teams work predominantly in the community and have staff who can come and visit you at home and in the early stages this is now often taken on by a district nurse.
They might also have access to allied health practitioners like social workers or occupational therapists who can help get you the support you need to stay at home, or pastoral care staff to lend a listening ear when you need it the most.
I think it’s essential to say that palliative care isn’t a one-way trip to some sort of strange parallel medical universe. Instead, it works hand-in-hand with your usual medical care – making sure we are getting the balance right, together with you.
So don’t be afraid to ask your team about palliative care, or to engage in a conversation if they bring it up themselves.
Our free publication aims to help you understand more about the role of palliative care in PH. With advice from experts and real experiences, this resource is designed to educate, inform, and spark important conversations.
It also includes a separate Anticipatory Care Plan booklet, tucked inside the back cover, to help you plan for the future. Scan the code to order your copy, or visit phauk.org/PalliativeCare&PH




DEADLINE EXTENDED UNTIL FRIDAY 5TH SEPTEMBER!
could your photo make the cover of this magazine?
Snap a nature-themed photo whilst you’re out and about this summer and share it with our PH community.
Gardens, seascapes, wildlife, flowers, animals… the possibilities are endless! And you don’t need a fancy camera to take part in this fun competition – mobile phone snaps are fine.
1st PRIZE A £50 Love2shop voucher (redeemable with over 50 retailers) and your entry on the cover of emPHAsis

2nd PRIZE £20voucherLove2shop
The top 10 photos will also be published on our website and as part of a special feature in the next issue of this magazine. ENTRIES ARE STILL OPEN
Get the kids involved over the summer holidays! We have an additional prize of a £20 Love2shop voucher for the best photo taken by a child under 13…
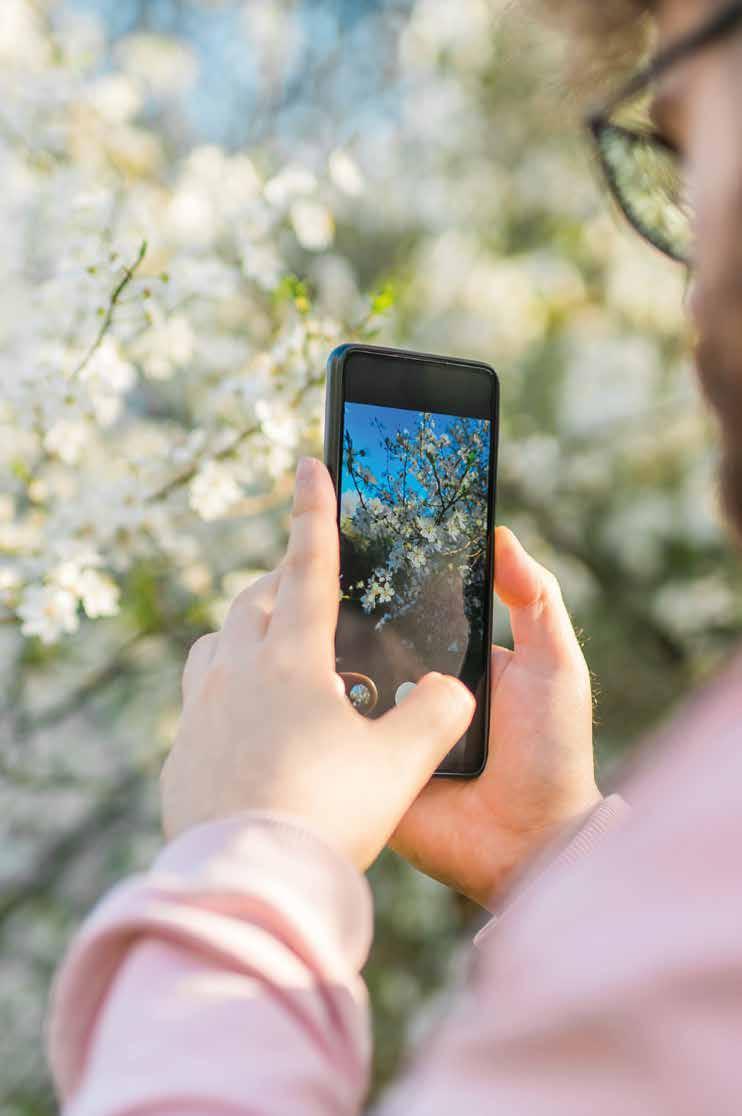
READY TO ENTER?
Head to phauk.org/competition to upload your photo or scan the code below. There is an OPTIONAL entry fee of £5 per photo, which is a charitable donation to help cover the prize costs and support us to continue our work.
Animal lover and emPHAsis columist Raya Mynot has found a way to enjoy feline friendship whilst giving something back…


As many of us know, having PH can really limit what you can do in life. I’ve been wanting to work with animals for a really long time but unfortunately due to my PH this has been almost impossible.
This has been because of many factors such as distance, travelling, accessibility, the jobs involved, and work hours involved. Not many places have the means to accommodate all my needs and I have found volunteering difficult for the same reasons.
However, a year ago I came across a lovely cat rescue called 'Stepping Stones Rescue and Haven'. They rescue cats all over my local area, and this could be because they have been abandoned, they have lost their owner, or are unwanted… the list goes on and it breaks my heart. I adore cats and as some of you know I have my own cat called Mateo. So when the rescue advertised that they were looking for people to foster, I immediately applied.
Becoming a foster for them has been the best thing I have ever done. When a cat comes into the rescue they are placed with a foster to be cared for until they are adopted. I have a spare room set up for potential fosters, and this means I don’t have to travel anywhere or be out in the cold/hot weather. I can help so many cats from the comfort of my own home. If I’m feeling unwell I know the cats are safe in their room with everything they need, and my mum or my fiancée Jade are always on hand to take care of them if I can’t. This is very rare though as when I do feel unwell I actually love going in and seeing the cats, as they give the best cuddles and it really is such an escape for me.
Our first foster cat was a pregnant female (Sylvie) who was abandoned and ended up having two kittens (Pumpkin ad Peach) in our care. Being able to experience this was beautiful. Being able to be there for Sylvie and watch the kittens grow was amazing! They went on to the best forever homes and really are being spoilt. Next up was Ozzy, a beautiful white



male cat with the bluest eyes ever! He was only young and had been a stray for most of his life. His founder called the rescue because he was worried about Ozzy being out over winter and fireworks night. I was a free foster so he came straight to me. It took a while to gain his trust but in the end he became the most beautifully loving cat ever. He was almost a foster fail! But he ended up finding a lovely home with an owner who needed him, like he needed her.
Whilst fostering Ozzy I had the opportunity to take a course on hand -rearing kittens, organised by the rescue centre. I loved every minute of this! I passed every module with 100%, and qualified with flying colours. I have a certificate of completion. It was such a privilege to be able to do this.
Not long ago we took in Evie-Mae, who was abandoned by her owners when they moved house. She’s only young and wasn’t neutered or microchipped (which is now

a law), so became pregnant. The person who found her contacted the rescue immediately and she was brought to me.
Unfortunately, Evie had a very traumatic experience. She birthed two kittens but then needed to be rushed for an emergency c-section and unfortunately lost the two remaining kittens. This was incredibly heartbreaking. Evie and her surviving kittens (KitKat and Rolo) have had so many ups and downs. Rolo needed supplement feeding, so I’ve been doing feeds throughout the night and during the day. This helped him massively! Evie is incredibly lucky and has the most amazing family waiting for her. Her and her kittens truly deserve the world.
Stepping Stones Rescue and Haven is incredible. I’ve met the most beautiful people, fostered the most amazing cats, and become part of a incredible team. This rescue runs solely on donations from the public. We could not do any of this without our amazing followers and donators.
Please go and give them a follow on Facebook to keep up with all the beautiful animals and visit their website at steppingstonesrescue.org to see all the cats they have up for adoption.
Our free self-help programme has been developed with psychologists specifically for people with pulmonary hypertension – and 100% of those who tested it said it helped with their anxiety. Based on Cognitive Behavioural Therapy (CBT)
Complete the workbooks at home
Work through them in your own time




Benefits Calculator
Find out what you might be able to apply for by answering questions about your personal circumstances. phauk.org/BenefitsCalculator
Grant Search
Discover what supportive grants may be available to you and your family. phauk.org/GrantsSearch
Personal Independence Payment (PIP) Helper
Walk through the PIP application process step by step, access tips and checklists, and more. bit.ly/PIPhelper




When
Lindsey Greenwood decided to take on a fundraiser for our charity, she set her sights high. Earlier this year, she trekked to the top of Kilimanjaro – the tallest mountain in Africa –and the memories will stay with her forever…
After watching her partner’s uncle struggle with PH, adventurous Lindsey booked the February climb to raise both sponsorship and awareness – and she did an amazing job in both respects.
At 5,895 metres, Kilimanjaro is not only the highest mountain in Africa, but also the highest free-standing mountain above sea level in the world. Knowing what lay ahead, Lindsey trained hard for months and raised almost £1,500 along the way.


She thought of everyone impacted by PH whilst she climbed, and flew a flag at the top to celebrate their bravery.

Whilst it was difficult, Lindsey told us she has no regrets about taking on such an ambitious adventure. She said: “It was tough, and it really pushed me mentally and physically, but I made it to the top and back down successfully. The people I met and the scenes I saw were incredible. It was a life-changing experience.”



Have

By Shaun Clayton, Certified Nutritionist and Operations and Finance Director at the PHA UK
iving with PH is challenging enough without the added pressure of trying to follow government healthy eating guidelines that are increasingly out of reach for many families. Recent findings from the "Broken Plate 2025" report by the Food Foundation have revealed a stark reality: the most deprived fifth of the UK population would need to allocate 45% of their disposable income to meet these guidelines, and for families with children, this figure rises to an alarming 70%
options have seen their prices rise at twice the rate of less nutritious choices over the past two years.
As both a Certified Nutritionist and the Operations and Finance Director of PHA UK, I want to address this issue directly. I want to assure you that it is possible to make appropriate, affordable, and nutritious food choices without feeling guilty or like you’re falling short. Perfection isn’t the goal— progress is.



This raises an important question — how practical are these guidelines for people living with PH, especially amidst a cost-of-living crisis? The report highlights a growing disparity: healthier foods, based on their nutrient profile, now cost more than double per calorie compared to ultra-processed alternatives. Moreover, these healthier
For individuals with PH, maintaining a heart-healthy diet is essential. Yet, the evidence presented in the "Broken Plate 2025" report underscores the urgent need to address health inequality in the UK. While some segments of society can afford to follow the idealised versions of a healthy diet—complete with organic avocados, sourdough



toast, and pasture-raised eggs—many families must make do with far more modest options.
Take, for instance, beans on toast
This simple meal, costing less than £2, is often dismissed by those who promote more expensive dietary choices. However, it offers a nutrient-dense, affordable source of fibre and protein — a practical and valuable option for those on a tight budget. For someone managing PH, ensuring adequate fibre intake and avoiding excessive sodium is far more valuable than striving to match dietary ideals that are financially out of reach.
Advising families to replace such meals with costlier alternatives not only disregards the financial realities faced by many but also risks exacerbating feelings of failure and inadequacy. The focus should, instead, be on promoting realistic and accessible improvements that align with both nutritional needs and budgetary constraints Cont...
The truth is that eating well does not have to mean spending excessively. There are numerous nutritious and budget-friendly options available that can support health for those living with PH:
Legumes
Beans and lentils are not only inexpensive but also rich in protein and fibre, helping to manage cholesterol and maintain energy levels.
Frozen vegetables
Often more affordable than fresh produce, they retain most of their nutritional value and are easy to incorporate into meals.
EMBRACING SMALL CHANGES WITHOUT GUILT
It’s essential to recognise that even modest dietary adjustments can significantly benefit your health. Adding an extra portion of vegetables, choosing whole grains, or incorporating fibre-rich foods like beans and lentils can all contribute to better health outcomes. Perfection isn’t the goal—progress is Every small improvement is a step forward, and it’s important to focus on what’s achievable given your financial circumstances. Making practical, budget-friendly choices is not something to feel guilty about —it’s something to be proud of
Got a question about nutrition?
Find more advice on nutrition and PH by scanning below. In this dedicated area of our website, you’ll find information on:
Eating to manage the side effects of PH medication...Ultra-processed food...Managing a reduced appetite...Making one-pan meals with PH...Understanding calories... and much more!

Whole grains
Foods like brown rice, oats, and wholegrain bread provide necessary fibre and energy, which are crucial for managing PH symptoms.
Tinned fish
Affordable options such as sardines and mackerel offer heart-healthy omega-3 fatty acids without breaking the bank.
Here are some practical strategies to help manage your diet without overspending:
Plan your meals
Creating a meal plan not only helps manage your budget but also ensures you can include heart-healthy foods regularly.
Limit processed foods
While convenient, processed foods often contain high levels of sodium and unhealthy fats that may exacerbate PH symptoms. Focusing on whole foods is both healthier and more economical in the long run.
Utilise community resources
Food banks and community kitchens can provide access to nutritious foods at little to no cost. These resources exist to support you—there is no shame in using them. Cook in batches
Preparing meals in bulk saves both time and money and ensures you have nutritious options readily available.
You can email Shaun at nutrition@phauk.org
PHA UK chairman Dr Iain Armstrong is well-known for his love of Indian restaurants, but he’s equally happy rustling up a curry at home (and it’s much kinder to his waistline too!)
Here he shares his favourite chicken balti – which provides a balanced, nutritious and tasty meal that can be batch-cooked on good days and frozen for those times you’re not feeling so great.
I like to take leftovers of this in for my colleagues at the Sheffield Pulmonary Vascular Disease Unit. Neil Hamilton, our consultant pharmacist, is allergic to dairy so he loves this recipe and always takes some home with him! I cook this curry at least a day in advance and keep it in the fridge before eating as I feel this really intensifies the flavours.

• Spice may be nice, but if you need to temper the heat a little, drizzle some natural yogurt over when you serve (use a dairy-free version if needed).
• If you’re keen to reduce your carbohydrate intake, try serving with cauliflower ‘rice’ instead. This can be bought ready-prepared for both cupboards and freezers.
• All sorts of vegetables work with this curry, so don’t feel you need to stick with what’s in the recipe. Chuck in whatever you fancy – the more, the better!
Vegetarian or vegan?
Swap the chicken for paneer (Indian cheese), tofu, or a meat substitute such as Quorn.
On a budget?
Bulking this dish out with more chickpeas can help you use less chicken. These versatile little legumes provide a powerful hit of plantbased protein and fibre!

Real photos of Iain's balti, bursting with goodness. You can serve this balti with rice, potatoes, bread or poppadoms
• 450g skinless, boneless chicken thighs (cut into bite-sized pieces)
• 1 tin of chickpeas
• 1 tbsp lime juice
• 1 tsp paprika
• ¼ tsp hot chilli powder
• 1½ tbsp sunflower or groundnut oil
• 1 cinnamon stick
• 3 cardamom pods (split)
• 1 small to medium green chilli
• ½ tsp cumin seed
• 1 medium onion (coarsely grated)
• 2 garlic cloves (very finely chopped)
• 2cm-piece ginger (grated)
• ½ tsp turmeric
• 1 tsp ground cumin
• 1 tsp ground coriander
• 1 tsp garam masala
• 250ml organic passata
• 1 red pepper (deseeded and cut into small chunks)
• 1-2 medium sized ripe tomatoes
• 85g spinach leaves
• 150ml water
1 Heat 1 tbsp of the oil in a large non-stick wok or pan and then throw in the cinnamon stick, cardamom pods, whole chilli and cumin seeds, and stir-fry briefly just to colour.
2 Stir in the onion, garlic and ginger and fry for 3-4 mins until the onion starts to turn brown.
3 Add the remaining oil, then drop in the chicken and stir-fry for around 2-3 mins.
4 Mix the turmeric, cumin, ground coriander and garam masala together and pop into the pan, lower the heat to medium and cook for about 2 mins.
5 Pour in the passata and 150ml water, then drop in the chunks of pepper. When starting to bubble, adds the spinach and lower the heat and simmer for 15-20 mins or until the chicken is tender.
Would you like to share your favourite recipe? Email details to media@phauk.org and you could see it in the next issue!

It's been more than 16 years since Connecticut-based Colleen Brunetti was told she had PH, and she continues to make the most of life. We had the pleasure of meeting Colleen at last year's World Symposium on Pulmonary Hypertension, where she spoke to us about adopting her daughter, navigating the American healthcare system, and how she keeps positive through the challenges of her condition...

“I had to learn to stop fearing dying and focus more on living”
The diagnosis came as a total shock. A lot of patients go doctor to doctor, year by year, looking for answers, but I presented at hospital with shortness of breath - because of an unrelated lung condition - and I was diagnosed with pulmonary hypertension within six weeks.
At this time my son was 18 months old. He was just a toddler, and I was very sick. I would look at him and wonder if I was going to live to see him reach kindergarten.
But fast forward to today, 16-and-a-half years and incredible care and treatments later, and this month he graduated from high school – with me there to see it. That is such an incredible gift.
I was 28 when I was diagnosed and the recommendation was immediately to make sure that I never got pregnant again. That was devastating. I mourned the family that I had dreamed of, that I wasn't going to be able to have, and exploring other options was scary because I didn't know if I'd be alive to raise my first child – never mind another one.
But as I stabilised, we decided to look into other ways of adding to our family. We explored all the different options, including private adoption, going through the foster system, and surrogacy. We ultimately decided that we had been through quite a bit, and there were a lot of kids already out there who needed love, and so we chose the foster system.
We were placed with a little tiny 4lb baby girl whose parents were not well enough to care for her, and we were able to actually adopt her nine months later. She is now nine years old and doing beautifully.
I can't do anything about the fact that I got pulmonary hypertension, but I can do everything in my power to be as healthy as possible - in mind, body and soul - so that I am as strong as possible to fight the disease.
I can't fix my lungs, but I can choose my nutrition, I can choose to move my body, and I can choose to take a deep breath. I can choose a spiritual practice and I can choose to follow hobbies that make me happy. And when I do all of those things, I'm in a better place to fight the PH that I didn’t choose.
When you're critically ill, how you learn to accept the disease matters. I had to learn to stop fearing dying and focus more on living. And when I was able to make that paradigm shift in my head and choose to do what I could, when I could – that's when I found my hope. And that's when things turned around.
The biggest difference in pulmonary hypertension care between the UK and the United States is our healthcare systems. We do not have universal healthcare [like the NHS] in the US.


We are either under private insurance or insurance that's meant to be assistance for people with disabilities. That’s a very, very challenging situation because it also varies company by company and state by state.
Even if you're very well insured, it's still very, very expensive. You can have co-payments [mandatory contributions set by the insurers] up to thousands of dollars. You might owe $7,000 before your insurance kicks in. There is help available through charitable assistance, but those funds open and close based on what money is available. So it can be very, very challenging.
Healthcare is a human right, and I think that patients in the UK are very lucky not to have those battles.
Colleen is a certified health coach and educator and ten years ago, she used her experiences of PH to produce a book that aims to help others adapt to life with the disease. Defining the new normal: A guide to becoming more than your diagnosis is available from Amazon now.
Whether it’s a booklet, poster, video, or web page, we need to be sure that it meets the needs of the PH community.
That’s why we’re building a mix of people affected by PH - patients, and their loved ones too - to give us feedback on new materials before they are launched. Your opinions are really important, and they help us make sure we’re getting things right.
As part of our Feedback Forum, we’ll ask you to spend a little time reviewing our materials before they are launched. This may be in the form of reading a leaflet, watching a short video, or having a look at a web page.
You will then be asked to fill in an online form with your thoughts. Sometimes, we may ask your thoughts on an idea for a campaign or project during the planning stages, to ensure we are taking things in the right direction.
Join at www.bit.ly/PHAUKfeedbackforum
There’s never been a more important time to lend your voice and experiences to PH research. As well as conducting our own studies to help people affected by PH live better lives, we are regularly approached by researchers from healthcare and academia, who recognise the importance of the patient voice.
Our Research Forum is for patients and loved ones or carers who would be willing to help with these studies when possible.
They often involve completing surveys or questionnaires, and sometimes they may involve online or telephone chats, or focus groups. Occasionally, you may receive an invitation to be involved in a different type of study, but it is unlikely you will be asked to take part in a clinical trial in this way.
Join at www.bit.ly/ResearchForum_PHAUK
Members of our Feedback Forum and Research Forum panels play a key role in helping to guide PHA UK activities and contribute to important research work. We contact all forum members with opportunities via email, and it is up to you whether you respond. We appreciate that PH comes with bad days so we understand if you need to give some of our invitations a miss!

Family and friends of PHA UK member Alex Charlesworth raised thousands for our charity in a touching show of support earlier this year.
They joined forces to take on a team run event in March, covering between 30 and 50 miles each. The ‘Fortitude Ultra’ required them to start a three, four, or five-mile loop on the hour, every hour, for a full ten hours – a true



Celebrating just some of our fundraiserswonderful & supporters

test of fitness, stamina, and mental strength too. The crew completed 176 miles between them, dedicating each one to Alex.
Ella Soady went more than the extra mile for her best friend Annie – she walked 150 of them!
Ella covered the mileage throughout the month of May, gathering sponsorship in support of Luciana (Annie) Pettit, who lives with PH and is waiting for a double lung and heart transplant. With one of the sunniest spring’s on record the weather was definitely on her side, but the challenge wasn’t without its rainy moments too. Ella was joined on some of her stomps by her loyal golden retriever, and after the final day of walking, she met up with Annie and her family and dogs for a celebratory picnic. Friendship at its finest!
David Whittington and Conor Keeling took on separate challenges for similar reasons in the spring – covering thousands of miles to raise funds and awareness.
Both David and Conor underwent life-saving pulmonary endarterectomy surgery for their chronic thromboembolic pulmonary hypertension, in 2020 and 2024 respectively.
Keen to give something back and celebrate their second chances, they completed challenges that fulfilled their ambitions as well as their fundraising goals.
At the end of April, former pilot Conor cycled from Royal Papworth Hospital in Cambridge to his home in Malahide near Dublin – pedalling an incredible 520km. Conor’s fundraising was split between the PHA UK and Pulmonary Hypertension Ireland.
Following hot on his heels, 81-year-old David and his wife Thelma set off on their own journey at the beginning of May. The pair drove their 57-year-old classic car the length of the UK from John O’Groats to Land’s End, completing a lifelong dream as well as generating funds for the PHA UK and the Royal Papworth Hospital Charity.
David and Conor didn’t know each other prior to these challenges but were introduced to each other via the PHA UK and have now struck up a friendship. The power of community and connection is strong!
Thank you to everyone involved in these challenges for their commitment, their kindness, and for spreading such positivity along the way.


“As it says on carved stones at John O'Groats: In every end, a new beginning, every mile a memory, and every step a story.” David Whittington

“Always remember that life is for living, whatever your ability.” Conor Keeling
We are an independent charity with no government funding, so we rely on the kindness of our fundraisers to help us support people affected by pulmonary hypertension. From bake sales to bike rides, marathons to motor racingand everything you’ve seen in this feature - we’re constantly amazed by the lengths our supporters go to in our name. We are so grateful for every penny raised, and with summer in full swing there couldn’t be a better time to support us. Find out more, get inspired, or request your free fundraising kit, by scanning this code >>>
The Sheffield Half Marathon is notoriously challenging, but Dr Thanos Charalampopoulos and Clinical Nurse Specialist Sammy Abraham were spurred on by thoughts of the people they care for with PH.
The pair work as part of the Sheffield Pulmonary Vascular Disease Unit team, and they were due to be joined by Ward Manager John Harington until a last-minute injury left him cheering on from the sidelines instead. He was with them in spirit on the hills though!
Thank you to Thanos, Sami, and John for supporting our charity with their sponsorship for this event.




Supporters Natasha Hinton and Mark Harris joined thousands of runners in West Yorkshire in May, taking on a sweaty Leeds Marathon for people very special to them. Natasha made her way round the hot and hilly course in memory of friend Yan, after losing him inspired her to get back into running as a celebration of his life.

They’re doing it…



Mark’s brother Paul was diagnosed with PH in 2015 and along with friends, he has been raising money for our charity ever since. We are grateful to both Natasha and Mark for their efforts.
PHA UK Chairman Dr Iain Armstrong will be joined by Javier Jimenez, Clinical Nurse Specialist in PH at The Royal Free Hospital, for a challenging sponsored swim event in September.
The pair will be taking to the open water in London’s Hyde Park as part of ‘Swim Serpentine’, aiming to complete a mile in the famous lake in support of their patients and PHA UK members.
Find out more and sponsor them at phauk.org/SwimSerpentine





We’re here to support people like you. Join the PHA UK today and benefit from:
• Support and advice
• Helpful printed information & resources
• emPHAsis magazine delivered to your door
• Free access to financial advice from qualified professionals via our partnership with Turn2Us
• Fundraising ideas and guidance
Being part of the PHA UK also enables you to participate in important research, and our friendly office staff are just one call away when you need advice. Join our PH family and you’ll be joining 4,500 members in a unique network of support and inspiration.


Here at the PHA UK we’ve teamed up with Great Ormond Street Children’s Hospital (GOSH) to build a young person’s advisory group to help shape the paediatric PH service and PH research.
This is your chance to make a real difference!
We’re looking for people living with PH who are aged around 10-16, and their parents or guardians, to take part in regular feedback sessions with the team from GOSH and the PHA UK. These meetings will take place either online or in-person, and they will be a chance to share your ideas and opinions, and your thoughts on what could be done better.
Your voice can:
✓ Influence future projects
✓ Keep research relevant to young people
✓ Help GOSH to receive funding to turn ideas into action
Being part of our advisory group will enable you to connect with other young people with PH – and it will also make a great addition to your CV! In some cases, you will reimbursed for your time in the form of gift vouchers and if events are in-person, then all travel and accommodation costs will be covered.

Please scan this code or visit phauk.org/GOSHgroup to complete the form and we will contact you with further details.

If you are under 16, please ensure you have the permission of a parent or guardian.

If you have any questions, please contact Annabelle Barnes from the PH research team at GOSH on annabelle.barnes@gosh.nhs.uk.
Our new self-help programme is available now
Developed by psychologists, and supported by the PHA UK, this is the world’s first self-help programme for people who live with pulmonary hypertension alongside depression or low mood. Complete the series of workbook over four weeks, in your own time and from your own home, and learn how to change your thinking habits and behaviours. The programme is based on cognitive behavioural therapy (CBT) and 87% of those who completed it as part of a controlled trial rated it as ‘good’ or ‘excellent’.

“It taught me how to change my negative thoughts and reactions to adverse situations”
“I was able to make this journey on my own in the privacy of my own home”


Andy Kerr is a man of many talents. A Clinical Nurse Specialist in PH by day, his spare time is spent writing and illustrating children’s books, singing in punk bands, designing card games, and even more besides. We caught up with the Glasgow-based Scottish Pulmonary Vascular Unit team member to discover how it all fits together, and what makes his nursing role so rewarding...
What led you to working in pulmonary hypertension, Andy?
I qualified as a nurse about 15 years ago and started off in medicine for the elderly at the Gartnavel Hospital in Glasgow. It was a really nice, well-rounded grounding in general medicine, and about five years later I moved to the respiratory ward there. As well as other diseases like cystic fibrosis, we also saw some patients with PH, so I was exposed to it very quickly in terms of my career.
I was on that ward for about six years, and in 2018, I had the opportunity to take a secondment with the Scottish Pulmonary Vascular Unit team, meaning I worked exclusively with PH patients. I loved working with such a specialist team, but the secondment ended after nine months, and I went on to become a respiratory nurse specialist.
I absolutely loved it, but when the permanent Clinical Nurse Specialist in PH job was advertised, I remembered my experiences during the secondment and went for it. I’m so glad I did. I’ve been in-post for over two years now and I’ve just qualified as a nurse prescriber, meaning I will be able to prescribe medications too. I’m excited about having this additional skill.



"Our PH patient community is a really special one"


What does a typical working day look like for you? (If there is such a thing!)
My time is split between two hospitals in Glasgow – The Golden Jubilee, and the Queen Elizabeth.
A ‘typical’ day involves different combinations of seeing inpatients during a ward round, seeing outpatients at a nurse-led clinic, catching up with calls and tasks, and working on specific projects. A lot of time is spent prepping for upcoming admissions and clinics too, as there is a lot of background work that goes into ensuring things run smoothly.
As nurses our first focus is the patients, and we try and develop our more junior staff too. We do also need to dedicate some time to things such as clinical audits, which can seem monotonous at times, but the end result is always to make sure that our clinical outcomes are the best they can be for patients.
Despite the odd boring bit (who doesn’t love an audit?!) it sounds like you enjoy the vast majority of what you do. What are the best parts of your job?
I love getting to know our patients. As PH is a chronic illness, you see them for a long time, whereas in some other areas of medicine people come in and out of your care and it can almost feel like a revolving door.
Our PH patient community is a really special one. I love our interactions, and they are truly grateful for the care they receive. As healthcare professionals we don’t do the job for thanks and praise, but it’s a lovely thing that is sometimes quite unexpected. It really gives us a boost and makes the challenging times feel worthwhile.
It might sound like a cliché but knowing I’ve helped someone is hugely rewarding, especially when they have struggled for a long time. For so many patients, they come to our service after seeing too many doctors without answers.


Without a doubt, becoming a permanent part of the Scottish Pulmonary Vascular Unit team. I feel like it was a long time coming, after the secondment in 2018. I’m proud of my progression from a newly qualified nurse to where I am now, and proud that I can make a difference to people – something which has always been my goal. It’s a lovely feeling to say ‘I’m one of the SPVU nurses’.
Family is really important to me. I have an utterly amazing five-year-old son who constantly keeps me on my toes and inspires a lot of what I do [more on that later!]. My wife is incredible too, and she keeps me grounded. We share our home with a ragdoll cat called Sasha, who is definitely a pampered princess.
One thing that most people say about me is that I don’t ever really stop. Work is busy, but I have a lot going on outside of nursing too.
Can you tell us about some of those things?
Firstly, I write, illustrate and self-publish humorous children’s books, and I’ve got four of them out via Amazon at the moment: Tips and Tools for Bashful Ghouls; The Sheep-Shifter; The Last Sausage, and Genie in a Bottom
It’s something I wanted to do from the age of about 19, but a lot of the inspiration for them came from having my son, Cameron. The books are aimed at children of pre-school age primarily and I’ve already started working on another two.
The first is called Why is that Turtle Purple? and it’s got a serious message about the importance of accepting



"One
most people say about me is that I don’t ever really stop."
differences. My last one was about a boy who couldn’t stop farting, so it’s a far cry from that! Book number six is based on my younger sister, and the hilarious mishaps she used to have as a child.
Switching between nursing, writing, and illustrating is quite a skill! Is there anything else you like to add to the mix?
I used to be a singer in a couple of bands, and I've always written my own songs, so I approach writing my books in the same way as it’s all based on verses and rhyming. I’ve been in rock bands and punk bands, but I’d say my voice is a little too ‘Disney’. I can’t play a musical instrument as I just don’t have the patience for it, but I’ve got a loud voice and a lot of confidence.
I’m also hoping to bring a children’s card game to market soon too. It’s something I’ve been working on with my son called Chaos the Cuddly Bear the classic game of Snap! both illustrated and real-life teddy bears.
I’m planning to pitch it to some companies, but even if it goes nowhere, it’s still been fun to work on.
Ultimately, all of these things I do are a great way of relaxing outside of work. They help me switch off from stress, and





Please email media@phauk.org if you’d like to contribute to your member magazine.
✓ Share your PH story
✓ Tell us your tips
✓ Submit a letter
✓ Send us your poems, pictures or photographs
✓ Pass on a feature idea
✓ Give your feedback on this issue
WOULD YOU LIKE TO CHANGE HOW YOU RECEIVE THIS MAGAZINE?
Scan below to receive your copy by email instead, change your address, or cancel your subscription. You can also email hello@phauk.org
Contact us here at emPHAsis by emailing media@phauk.org or writing to emPHAsis, PHA UK Resource Centre, Unit 1, Newton Chambers Road, Thorncliffe Park, Chapeltown, Sheffield S35 2PH

Tear off the page opposite and display on your front door or in your window to let delivery drivers know it may take some time for you to answer.
Thank you to PHA UK member Salina Issory for getting in touch with this idea, after struggling with missed parcels due to impatient delivery drivers.
www.phauk.org





Our private Facebook groups are a valuable source of support and advice from people who truly understand. They are safe spaces to talk to other people with lived experiences of pulmonary hypertension. You need to have a Facebook profile in order to join these groups. Sign up at www.facebook.com. It’s free and easy!
We have dedicated groups for patients, carers, and loved ones too. Scan the code to access the groups, or visit phauk.org/SafeSpaces