Department Update
–Head & Neck Surgery
SUMMER 2025


































Warmsummer greetings to all! This summer brings exciting developments for the Department of Otolaryngology –Head and Neck Surgery. We are proud to announce that U.S. News & World Report has once again recognized us as one of the nation’s top programs for ear, nose, and throat care for 2025-2026.
Additionally, I am delighted to share that several of our distinguished faculty members have received well-deserved academic rank promotions for the upcoming year: Dr. Jessyka Lighthall, Dr. J.P. Gniady, and Tiffany Heikel, PA-C. These promotions reflect their ongoing success and significant contributions to Penn State.
We are also thrilled to welcome Dr. Michael Kupferman as the new CEO of Penn State Health. Dr. Kupferman joins us as a member of our department in the Division of Head and Neck Oncology and Surgery, bringing a wealth of experience and leadership to our team.
Furthermore, as of July 1, we have officially established the Division of Pediatric Otolaryngology. Dr. Allison Keane has been appointed as Division Chief, effective July 1, 2025. Dr. Keane joins our outstanding leadership team, overseeing the department’s four subspecialty divisions.

Together, we continue to advance in innovative clinical care and ambitious research initiatives. This newsletter highlights the many achievements of our talented team, and I encourage you to stay engaged and share your thoughts with us.
Enjoy this summer edition of our newsletter!
Dr. David Goldenberg Department Chair


PennState Health now offers a 12-month fellowship program for Advanced Practice Providers (APP) in the field of otolaryngology, led by Tiffany Heikel, PA-C, and Meghan Schmidt, PA-C, with Dr. John McGinn serving as the program’s medical director.
This unique training opportunity in otolaryngology is one of only four programs of its kind in the nation, underscoring the strength of our APP program. This distinction highlights our commitment to providing exceptional education and training, equipping students with the skills and knowledge necessary to excel in the field of otolaryngology. Our program continues to set a high standard for excellence and innovation in medical education.
The fellowship program will provide an environment and clinical experience that

fosters professional growth, procedural skills and clinical care through didactic training and direct patient care. Clinical curriculum will include rotations with subspecialized surgeons and the APP team, providing exposure to inpatient care, outpatient clinics, and the operating room.
The inaugural fellow of the APP fellowship program is scheduled to start in December.
Several distinguished faculty members have earned promotions for the upcoming academic year, effective July 1, 2025. These advancements are a testament to their dedication to teaching and learning, research and creative achievements, and service to the University, the community, and our profession. Their accomplishments highlight their successes and promise of future contributions at Penn State.
• Jessyka Lighthall, MD, FACS has been promoted to rank of Professor.
• J.P. Gniady, MD, FACS has been promoted to Associate Professor.
• Tiffany Heikel, PA-C has been promoted to Assistant Professor.


The
Children’s Miracle Network (CMN) Research Review Committee, announced selection of “Development of a Pediatric Multidisciplinary Airway Program” proposal to receive research funding under leadership of Dr. Allison Keane through the CMN fundraising campaign. This award reflects the mission of CMN to improve the quality of life for children in need of medical care at Penn State Health Children’s Hospital.
Pediatric multidisciplinary aerodigestive programs provide high-quality, coordinated care to a complex patient population. Such programs have been proven to enhance patient outcomes and patient satisfaction while also reducing the financial burden on patients and healthcare institutions.
A Pediatric Multidisciplinary Airway Program is crucial because it offers comprehensive and coordinated care for children with complex airway disorders through a team of specialists. This collaborative approach
ensures accurate diagnosis and tailored treatment plans, leveraging the expertise of otolaryngologists, pulmonologists, and other specialists.
The program improves outcomes by providing expert, holistic care, enhancing recovery times, and supporting families with education and resources. Additionally, it contributes to research and innovation in pediatric airway treatments.
Division Chief of Pediatric Otolaryngology, Dr. Allison Keane is the project principal investigator and responsible for providing overall leadership and strategic direction for the Pediatric Multidisciplinary Airway Program.
Dr. Gil Zoizner-Agar, Co-Investigator, will be responsible for assisting with strategic direction and Dr. Gavin Graff, Co-Investigator, will contribute expertise in pediatric pulmonology to the multidisciplinary airway program.

Anearache can turn a happy, energetic child into a cranky, uncomfortable one in no time. It’s a common struggle – five out of six kids will have an ear infection by age 3, according to the National Institutes of Health.
Ear infections and other ear, nose and throat (ENT) problems are among the top reasons children see doctors. During Kids ENT Health Month in February, pediatric otolaryngologist Dr. Gil Zoizner-Agar shares how to help children with ENT conditions.
Middle ear infections: Viruses or bacteria infect the space behind your child’s eardrum, causing ear pain and fullness, fever or muffled hearing. Middle ear infections usually affect kids under 7, especially after colds, Dr. Zoizner-Agar said. Fluid gathers in their middle ears due to underdeveloped eustachian tubes, which connect the middle ear to the back of the nose. Then, harmful bacteria multiply.
External ear infections: The outer ear canal gets infected, causing pain or drainage, Dr. Zoizner-Agar said. These infections are common in older kids. They’re often caused by excess water exposure (swimmer’s ear) or scratches from a fingernail or cotton swab.
HOW CAN I REDUCE MY CHILD’S RISK FOR EAR INFECTIONS?
• Use saline. When your child is congested, gently rinse their nose with saline two to three times per day. “The natural drainage of the middle ear is to the back of the nose, so if the nose is clear, in theory the ear should drain out better and hopefully not get an infection,” Dr. Zoizner-Agar explained.
• Avoid secondhand smoke. Smoke can irritate the lining of the nose, eustachian tube, and middle ear and make infections more likely.
• Sit your child up to feed. Bottle-fed children should sit or be held partially upright while drinking so milk does not enter their eustachian tubes.

• Do not insert cotton swabs (or anything else) in your child’s ears. Soften excess wax with peroxide-based earwax removal drops or a few drops of mineral oil.
HOW
Initial treatment with Tylenol or ibuprofen is reasonable as long as pain and fever are controlled.
Seek medical attention if your child’s symptoms have worsened within 24 hours or have not improved within 48 hours. The physician will
check your child’s eardrum for redness, swelling, bulging or pus. If they see an infection, they will prescribe antibiotics to kill the bacteria. If not, antibiotics are not needed and will not help.
“A thorough examination and diagnosis are crucial,” Dr. Zoizner-Agar said. “It’s important to determine whether the symptoms are caused by an ear infection or something else before prescribing antibiotics.”
Tell your doctor if your child is not improving within 48 to 72 hours. Sometimes, your child may need a different antibiotic. Nausea, vomiting and diarrhea are common antibiotic side effects. Your doctor might also recommend ibuprofen or acetaminophen for pain relief, especially until the antibiotic “kicks in,” which can take up to 48-72 hours.
External ear infections are different and are often treated with antibiotic, antifungal or steroid ear drops.
For kids with multiple, recurrent middle ear infections, ear tubes can bring relief. A surgeon places these tiny tubes in your child’s eardrum to help fluid drain from the middle ear.
Alert your doctor about other symptoms, too. “It’s important to see if a child also has issues of nasal congestion, a lot of secretions from the nose or snoring because many times an enlarged or infected adenoid is causing those symptoms,” Dr. Zoizner-Agar explained. Located at the back of the nasal passage, adenoids may trap bacteria and viruses. Your doctor might recommend surgery to remove them if they are causing persistent problems.
The Medical Minute is a weekly health news feature produced by Penn State Health. Articles feature the expertise physicians and staff, and are designed to offer timely, relevant health information of interest.
“Dr. Woo Yul Byun (PGY-1) is an amazing resident who from the very first minute of my ENT rotation showed me the ropes on how to be successful. He incorporated me into discussions on treatment plans for patients, making sure I always understood why we did things. He gave me opportunities to demonstrate my knowledge. He is friendly, wise, and overall an awesome person.”
“Nicole Fisher, SLP, has gone above and beyond for Penn State Health and our department in caring for complex multidisciplinary patients in the head and neck and facial paralysis realms. She has really been a remarkable collaborator, is a skilled facial nerve therapist, and continues to go above and beyond.”
“Kudos to Caia Hypatia (Research Project Manager) and Michah Grien, the IRB Analysts from the Full Board team wanted both of these individuals to be acknowledged for their collegial attitude, attention to detail and follow through on their submissions. We appreciate their efforts.”
“Dr. Jeff Lorenz (PGY-2) will make a superb doctor and you should be proud to have him on your team. He listens and then responds with a very pointed diagnosis and game plan. He’s excellent.”
“Bailey’s approach to the clinical trials at the Clinical Research Center has truly impressed us. Her attention to detail, strong handle of each study, and ability to manage even our busiest clinical trial days have stood out in the best way. Thank you for the great job you’re doing within our research program.”
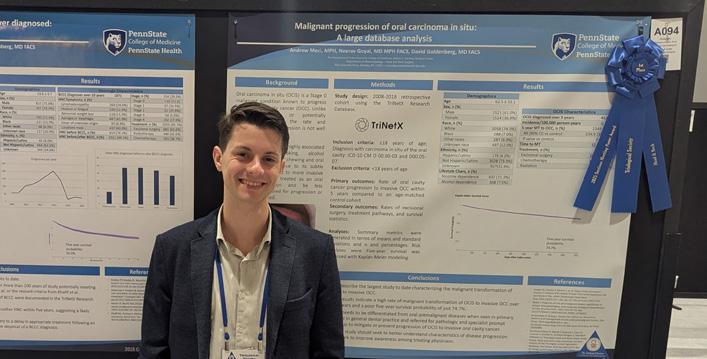
JANUARY 2025 – Research fellow Andy Meci, MPH, was awarded first place in the poster session at the Triological Society Meeting for his work on the malignant progression of oral carcinoma in situ.
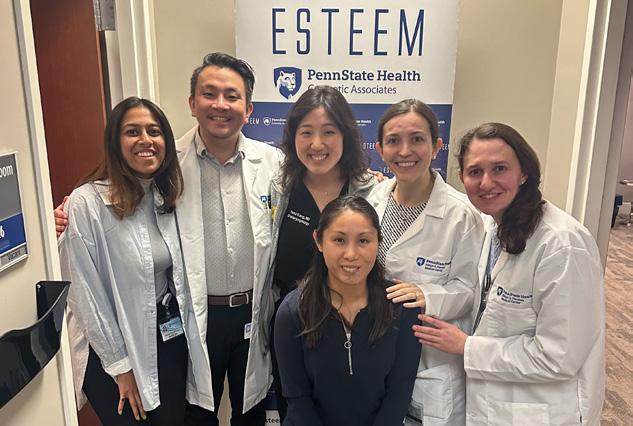
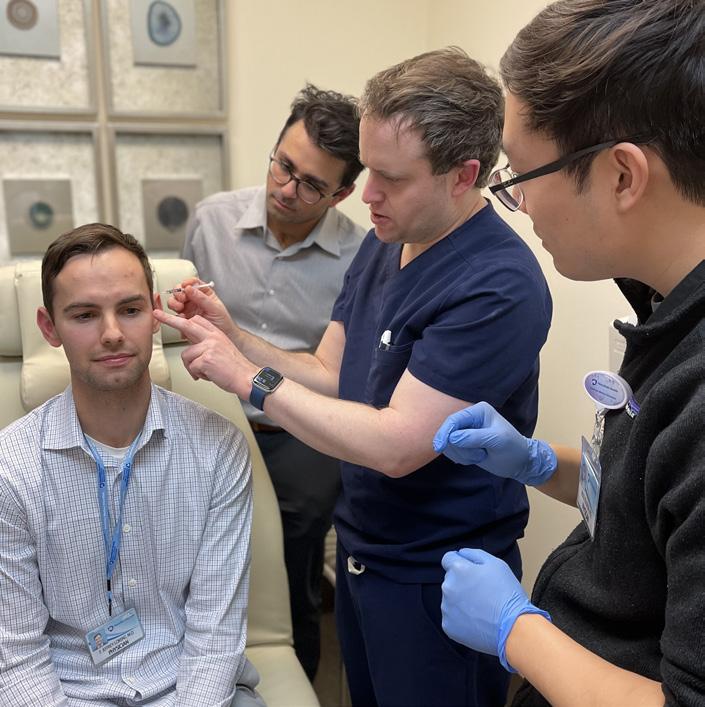
JANUARY 2025 – The Division of Facial Plastic and Reconstructive Surgery, in partnership with Esteem Cosmetic Associates, hosted a handson injectable training clinic to enhance resident education in Botox and filler techniques.
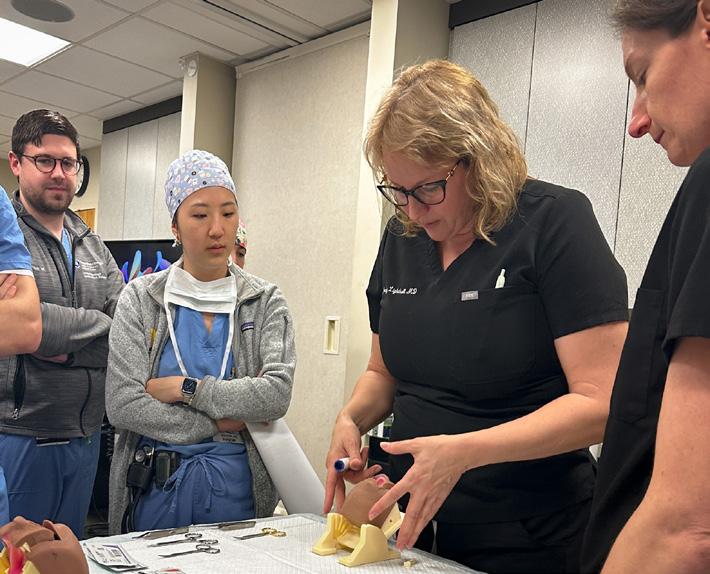
FEBRUARY 2025 – Residents participated in a cleft palate simulation session, honing their skills in cleft repair under the guidance of pediatric otolaryngologists and facial plastic and reconstructive surgeons.
ULTRASOUND TRAINING COURSE
MARCH 2025 – Residents attended the biennial head and neck ultrasound course, featuring expert-led instruction in ultrasound, fine needle aspiration, and radiofrequency ablation of thyroid nodules.

APRIL 2025 – Tiffany Heikel, PA-C and Chatur Patel, PA-C, led multiple in-person workshops in Salt Lake City, training clinicians in otolaryngology techniques during a conference attended by over 500 participants.

MAY 2025 – The 3rd Annual Penn State Health Thyroid Radiofrequency Ablation Course brought together trainees and faculty from around the world for this premier hands-on learning experience.

JUNE 2025 – Our team joined colleagues at the Pennsylvania Academy of Otolaryngology – Head and Neck Surgery Annual Meeting at the beautiful Hershey Hotel, contributing to the advancement of patient care and scientific discovery.

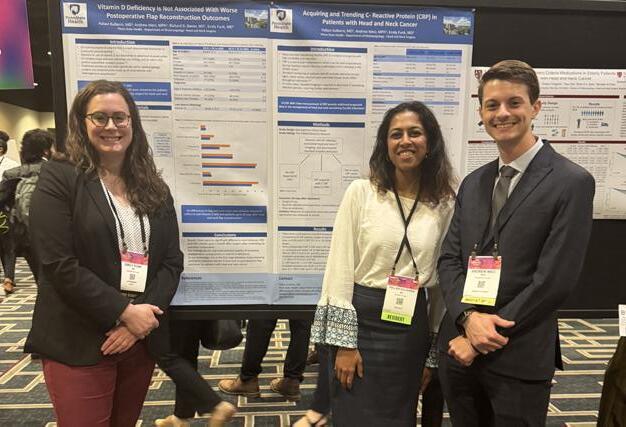
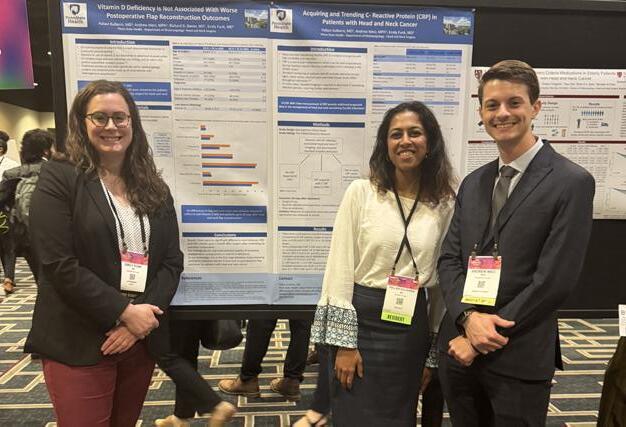
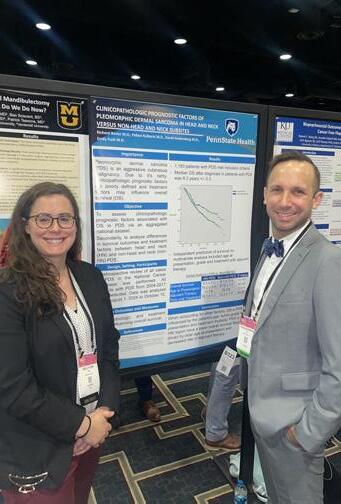
MAY 2025 – Residents, faculty, and research medical students represented our program at the Combined Otolaryngology Spring Meeting in New Orleans, presenting cutting-edge research, networking with peers, and exploring innovations across the field.


The Division of Head and Neck Oncology and Surgery, under the leadership of chief Dr. Neerav Goyal, continues to experience growth and expansion. We are pleased to welcome Dr. Shawn Li as the Department’s newest full-time faculty member.
In broader leadership news, Penn State Health recently announced Dr. Michael Kupferman as its new CEO. Dr. Kupferman brings extensive experience as a head and neck surgeon and a strong commitment to advancing care for patients throughout the health system.
WELCOME, DR. SHAWN LI
Dr. Shawn Li is a fellowship-trained head and neck oncologic surgeon and microvascular reconstructive surgeon. He most recently served as an attending surgeon at University Hospitals in Cleveland. He completed his fellowship at Indiana University and his residency at Case Western Reserve University
and University Hospitals Cleveland Medical Center.
Dr. Li has clinical interests in cutaneous malignancies, thyroid disorders, skull base diseases, and head and neck cancers. His expertise and dedication will further strengthen our mission of delivering comprehensive and compassionate cancer care to our patients.
The team has recently expanded to include two cancer nurse coordinators, Michele Spencer and Jill Gray, who work closely with head and neck cancer patients. Under the direction of the physicians, they play a vital role in coordinating treatment schedules and ensuring continuity of clinical care.
Their work is essential in managing the complex, multidisciplinary care that our

patients receive at Penn State Health. Michele and Jill serve as consistent points of contact for patients and families, helping to navigate each step of the treatment journey with compassion and expertise.
Michele Spencer selected as a recipient of the Penn State Health Positive Impact Award. Michele is one of just four winners chosen from over 830 employee nominations. A true testament to her exceptional teamwork and dedication to patients.
ACCOMPLISHED PHYSICIAN EXECUTIVE, CLINICIAN AND RESEARCHER TO LEAD UNIVERSITY’S HEALTH SYSTEM; COLLABORATE WITH COLLEGE OF MEDICINE TO ADVANCE TRAINING, RESEARCH AND CARE MISSIONS
From Penn State Health News
PennState President Neeli Bendapudi and the Penn State Health Board of Directors have appointed Michael Kupferman, MD, MBA, FACS as the next chief executive officer of Penn State Health. A seasoned physician executive, he brings more than a decade of experience leading transformation in academic medical centers and integrated health systems.
Dr. Kupferman joins Penn State Health from Phoenix-based Banner Health, where he served as president of the Banner – University Medicine Division and senior vice president of the physician enterprise. His portfolio includes academic medicine, service line strategy, hospital operations and payer partnerships.
He is a fellowship-trained head and neck cancer surgeon and professor, previously funded by the National Institutes of Health. He holds a Master of Business Administration

from Northwestern University’s Kellogg School of Management and is board-certified in otolaryngology – head and neck surgery.
“I look forward to working shoulder to shoulder with my talented and dedicated colleagues at Penn State Health and the College of Medicine to deliver on our promise to provide unparalleled and innovative care to the people of central Pennsylvania and the commonwealth. Together we will foster an environment that enables us to train the best physicians and health care providers, advance research and expand our role as the region’s only locally based academic health system.”
In addition to his administrative duties as CEO, Dr. Kupferman intends to continue caring for head and neck cancer patients, as well as teaching medical students, residents and fellows.
Written by Jacqueline Price, Au.D.
Tinnitus – the perception of sound without an external source – is a condition that affects roughly 1 in 10 adults. Patients often describe it as ringing, buzzing, hissing, or whooshing in the ears. For most, it’s a mild annoyance. But for a small population, it can significantly impact sleep, concentration, and overall quality of life.
Tinnitus is not a disease itself but a symptom, often linked to hearing loss, noise exposure or ear injury. While there is no universal cure, many evidence-based management strategies can help reduce its impact on the perception. An established effective method is Tinnitus Retraining Therapy (TRT).
Hyperacusis is a disorder of decreased sound tolerance. This condition is managed with the help and use of Tinnitus Retraining Therapy (TRT). Hyperacusis is a negative reaction

to sounds dependent upon its physical characteristics, your brain’s sound system is being set to over amplify making every day sounds feel too intense.
Misophonia is an affliction where specific everyday sounds trigger a strong emotional reaction like anger, anxiety and/or disgust. Common sounds reported are chewing, breathing, or tapping. It is an intense involuntary reaction. This also can be managed with implementation of TRT.
TRT combines directive counseling using a Neurophysiological Model in conjunction with sound therapy. The counseling component helps individuals reframe the way they perceive and emotionally respond to the tinnitus and/or decreased sound tolerance, hence, reducing the brain’s negative association with sound. At the same time, low-level sound therapy is used to gently desensitize the auditory system and promote habituation. Over time, the brain learns to not focus on the tinnitus or helps with the desensitization of the individual’s decreased sound tolerance by making it far less noticeable or bothersome.

If you or someone you know is struggling with tinnitus, hyperacusis or misophonia, Dr. Jackie Price, level II audiologist and lead for the Tinnitus subspecialty and the audiology team at Penn State Health can help. With proper support and tools like TRT, habituation is possible.
Bhatt JM, Lin HW, Bhattacharyya N. Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol Head Neck Surg. 2016;142(10):959-965. doi:10.1001/ jamaoto.2016.1700
Henry JA, Dennis KC, Schechter MA. General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. 2005;48(5):1204-1235. doi:10.1044/1092-4388(2005/084)
Jastreboff PJ. Tinnitus Retraining Therapy. New York, NY: Cambridge University Press; 2007.
Jastreboff PJ. Tinnitus retraining therapy. Lecture presented at: Jastreboff Hearing Disorders Foundation; January 15, 2025; Maryland, USA.

MARCH 2025

APRIL 2025

MAY 2025

Robert Saadi, MD, and Carissa Saadi welcomed a baby girl, Evangeline Rose Saadi, on December 20, 2024.
2025

Natasha Garcia and Pedro Garcia welcomed a baby boy, Kaiden Xavier Garcia, on May 15, 2025.
Michael Vogt, PA-C, and Camry Vogt welcomed a baby boy, Karl Daniel Vogt, on March 30, 2025.
2025
Elaine Tierney, SLPD, and Linden Moot welcomed a baby girl, Troup Elizabeth Tierney, on April 19, 2025.

2025
Erin Groft, PA-C, and Brian Groft welcomed a baby girl, Lilian Josephine Groft, on June 20, 2025.
Brandon LaBarge, MD, and Lindsey LaBarge welcomed a baby girl, Margaret Ann LaBarge, on May 7, 2025.

Cheng Ma, MD, and Sharon Chu welcomed a baby girl, Juniper Grace Ma, on July 20, 2025.

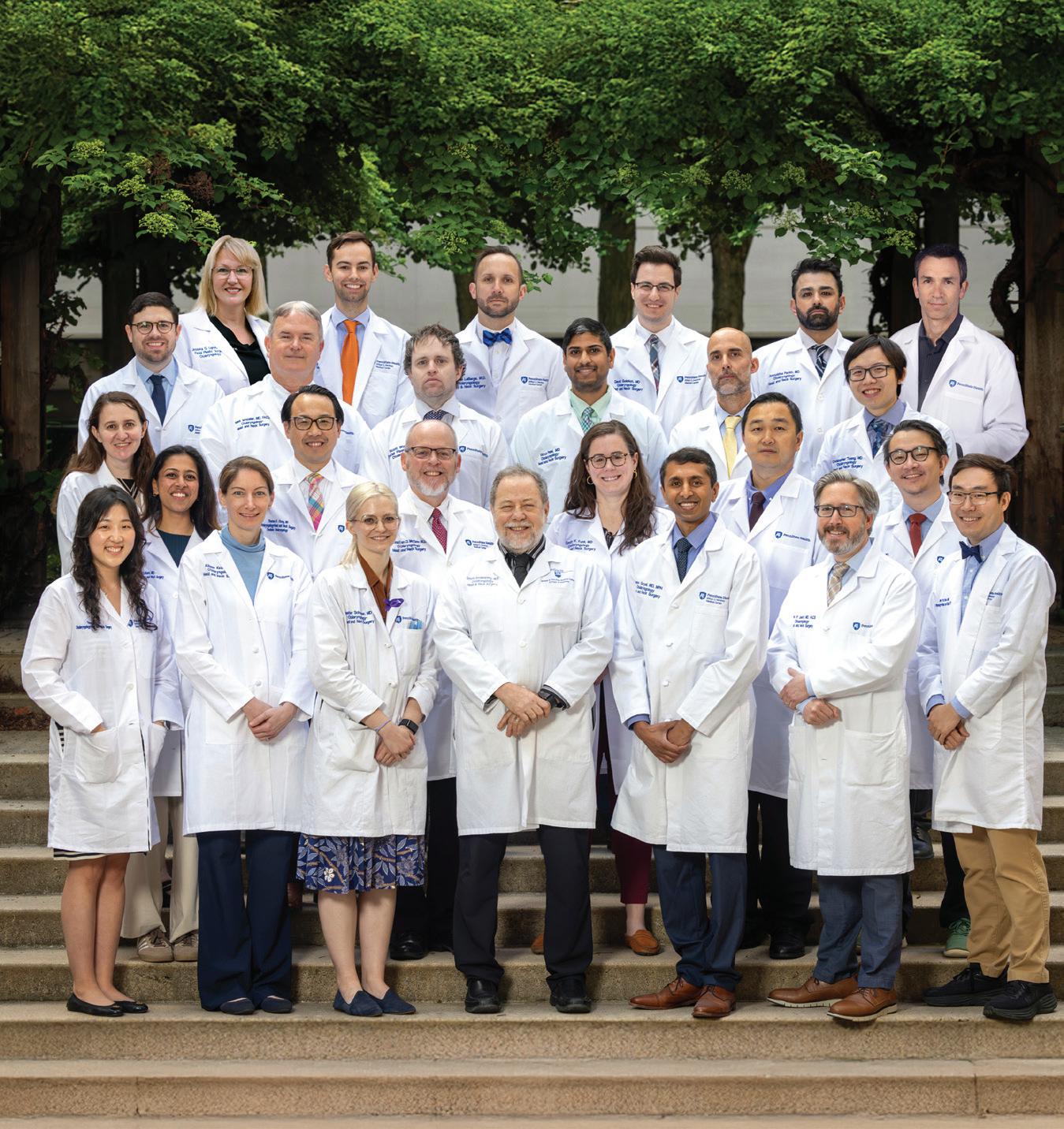
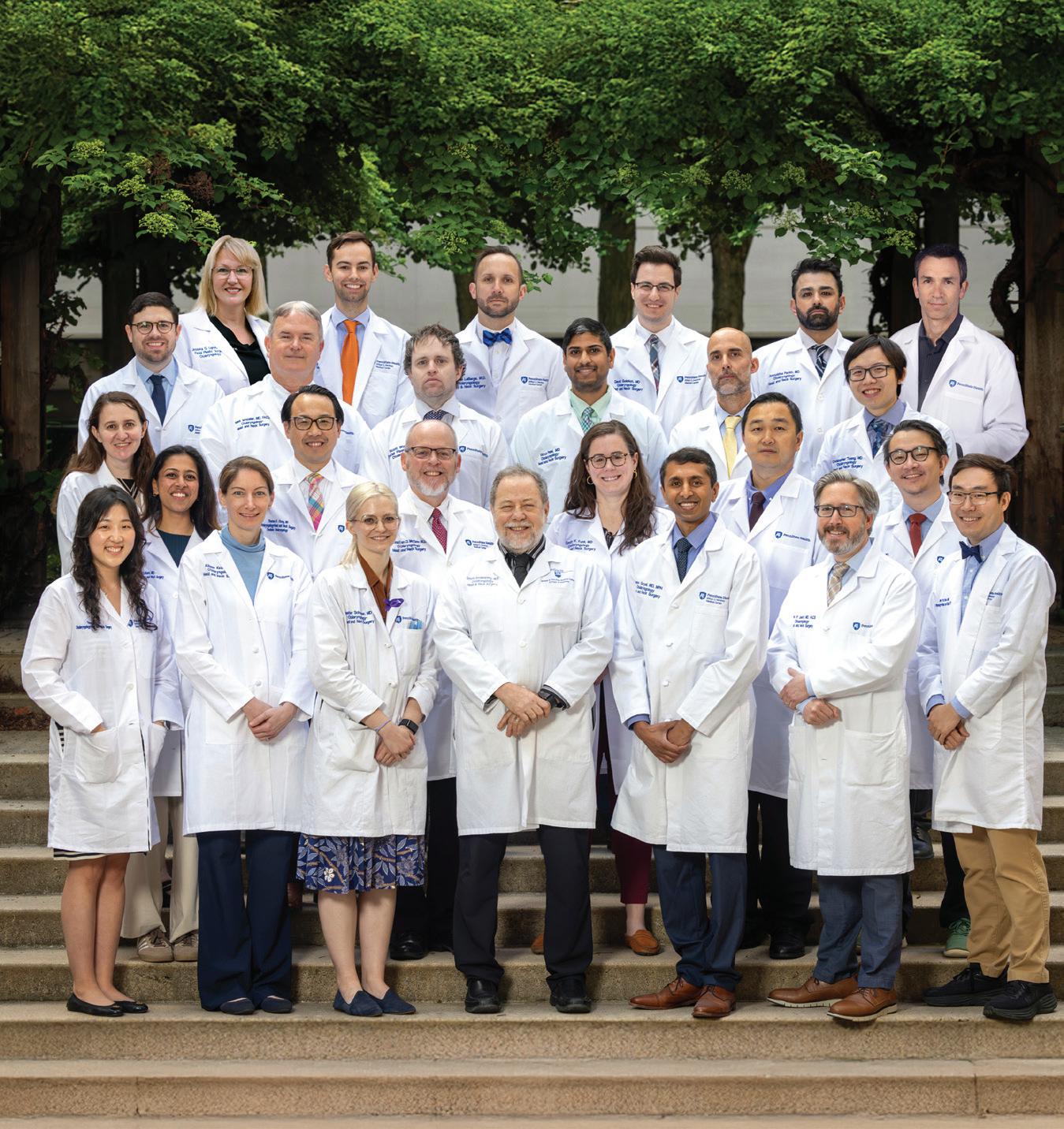
Faculty and staff from the Department of Otolaryngology – Head and Neck Surgery proudly celebrated the graduating residency and fellowship class of 2025.
Two chief residents graduated from the program: Dr. Richard Bavier is headed to the University of Utah to pursue fellowship training in head and neck oncology. Dr. Brandon LaBarge will be going to Vanderbilt University Medical Center for a laryngology fellowship.
Facial plastic and reconstructive surgery fellow, Dr. Aniruddha Parikh, will join the University of Nevada Las Vegas as a full-time faculty member.
The evening ended with departmental awards. Dr. Marc Polanik received the Extraordinary Otolaryngology Resident Award for exemplifying clinical excellence, teamwork, research, and dedication to patient care. Dr. Scott Walen earned the Faculty Teaching and
Mentorship Award for his ongoing commitment to resident education.
We wish our graduates the best as they begin the next chapter of their medical careers. Their dedication to care, education, and surgical excellence has left a lasting impact on our program and community




The Ferraro Resident Symposium in Otolaryngology, held in June at the end of the academic year, highlights research projects conducted by residents, selected medical students, and our fellow.
KEYNOTE SPEAKER
We were honored to host Dr. James Rocco, Professor and Chair of the Department of Otolaryngology – Head and Neck Surgery at The Ohio State University, as the keynote speaker. His lecture, titled “Solving the Puzzle of Disparate Outcomes in Head and Neck Squamous Cell Carcinoma: Charting Progress Across Decades,” offered valuable insights into decades of advancement in the field.
Dr. Jeffrey Lorenz, PGY-2 resident, was awarded winner for his presentation titled “Chemodenervation is Associated With Reduced Mental Health Disorders in Patients With Synkinesis.”
We extend our sincere thanks to Dr. Richard Ferraro, resident alumnus, for his generous support in making this exceptional event possible.



WELCOME NEW TRAINEES
Incoming PGY-1 residents Drs. Pallavi Kulkarni, Millind Vasudev, and Julio de Leon; 2025-2026 facial plastics fellow Dr. Edgar De Toro; and head and neck oncology fellow Dr. Christian Gluck.










$52,864
Penn State Health’s Department of Otolaryngology – Head and Neck Surgery raised $52,864 through its first annual “Let’s Get Ahead” campaign, held during Head and Neck Cancer Awareness Month in April. The campaign brought together Penn State Health staff, community partners, and members of the public to raise awareness and funds in support of head and neck cancer care and research.
Throughout the month, the Department of Otolaryngology – Head and Neck Surgery led a series of impactful initiatives, including free cancer screenings, participation in a community educational health fair, t-shirt sales, and a televised segment on WHTMTV (ABC27). The campaign culminated in the Department’s 5th Annual Sporting Clay Shoot on Saturday, May 3, which drew strong community participation and support.
A key driver of the campaign’s success was the enthusiastic participation in peer-to-peer







fundraising, where individuals and teams created personalized fundraising pages to rally support from friends, family, and colleagues. Teams from across Penn State Health competed in a friendly challenge to raise the most funds, fostering a spirit of collaboration and shared purpose.
“Our initial goal was $35,000, and we exceeded that thanks to the efforts of everyone involved,” said Dr. David Goldenberg, chair of the Department of Otolaryngology – Head and Neck Surgery “We thank our local businesses, event sponsors, volunteers and patients and their families for their outstanding support throughout the campaign. The funds raised will go a long way toward helping our patients at Penn State
“We thank our local businesses, event sponsors, volunteers and patients and their families for their outstanding support throughout the campaign. The funds raised will go a long way toward helping our patients at Penn State Health and many others in the communities we serve.”
– Dr. David Goldenberg
Health and many others in the communities we serve.”
The funds will directly support leading-edge care and research in head and neck oncology at Penn State Health, helping to improve patient outcomes and expand access to innovative treatments. The team is eager to carry this year’s momentum into a larger 2026 campaign.

MILTON S. HERSHEY MEDICAL CENTER EARNS NATIONAL ACCREDITATION FOR EXCELLENCE IN SURGICAL ONCOLOGY CARE
From Penn State Health News
Penn State Health Milton S. Hershey Medical Center has been recognized by the American College of Surgeons (ACS) as a Surgical Quality Partner through participation in the organization’s Commission on Cancer.
The ACS Commission on Cancer is a group of professional organizations dedicated to improving survival and quality of life for patients with cancer by setting high standards of care standards.
“We are proud to have earned this distinction as an ACS Surgical Quality Partner,” said
Dr. Michael Reed, chief of the Division of Thoracic Surgery and Cancer Committee chair at Milton S. Hershey Medical Center and professor of surgery at Penn State College of Medicine. “It reflects the highest level of comprehensive and multidisciplinary cancer care we provide to all our patients. This accreditation is also an endorsement of the dedication and expertise of our health professionals at Milton S. Hershey Medical Center.”
Hospitals recognized as Surgical Quality Partners have effectively demonstrated
their dedication to providing the tools and resources necessary to make quality a top priority. This designation assures patients that they can expect top-tier care driven by data, expert input and proven processes.
“Our designation as an American College of Surgeons Surgical Quality Partner reflects our continuous efforts to minimize complications, improve outcomes and ultimately save lives through exceptional surgical care,”
-Dr. Neerav Goyal, Cancer Liaison Physician for the Cancer Committee.

The Commission on Cancer awards accreditation to programs that meet its high standards for cancer care. Accredited programs undergo a thorough review every three years to ensure continued compliance.

Fellowship alumnus, Dr. Ciarán Lane, and invited visiting professor, Dr. Neerav Goyal, at the University of Manitoba Resident Research Day. Dr. Goyal delivered the Grand Rounds lecture, “Beyond Cancer: Quality of Life in Survivorship.”
These standards ensure that patients receive a full range of diagnostic, treatment and supportive services, either on-site or through referrals, including access to community resources.
“ACS quality programs are grounded in more than a century of experience, and participation is an important measure of a hospital’s surgical quality,” said Dr. Patricia Turner, ACS executive director and CEO.
“As an ACS Surgical Quality Partner, Milton S. Hershey Medical Center has shown a commitment to providing the best possible patient care, evaluating that care in a rigorous fashion and dedicating themselves to continuous self-improvement.”
The ACS is dedicated to improving surgical care by focusing on three critical components: care, evaluation and improvement. Its accreditation and verification programs, guidelines and tools improve quality in trauma, cancer, breast disease, bariatrics, children’s, geriatrics and overall surgical care.
Resident alumni, Drs. Nicole Ruszkay, Allison Keane, and Darrin Bann, at the American Society of Pediatric Otolaryngology Annual Meeting.

Chan K, Patel S, Keane A, King TS, Lighthall JG. Evaluating Outcomes in Septorhinoplasty Procedures Using Serum Cotinine as a Measure for Tobacco Use. Otolaryngol Head Neck Surg. Mar 2025.
Chan K, Tseng C, Milarachi E, Goldrich D, Schneper L, Sheldon K, Aliaga C, Alam S, Chatterjee S, El-Bayoumy K, Meyers C, Goldenberg D, Broach JR. Genome Instability Precedes Viral Integration in Human Papillomavirus–Transformed Tonsillar Keratinocytes. Mol Cancer Res. Feb 2025.
Contrera KJ, Kansara S, Goyal N, et al. Neoadjuvant Therapy for Mucosal Head and Neck Squamous Cell Carcinoma: A Review From the American Head and Neck Society. JAMA Otolaryngol Head Neck Surg. Apr 2025.
Eberly HW, Pradhan S, Tucker J, Sciscent BY, King TS, Lighthall JG. Fibrin Sealants in Facial Plastic Surgery: A National Database Analysis of Complication Risk. OTO Open. Mar 2025.
Goldrich DY, Patel S, Sciscent BY, Eberly HW, Goyal N. Ultrasound-On-Chip With Semiconductor Silicon Chip Array for Transcutaneous Salivary Gland Injections: A Pilot Cadaver Study. Laryngoscope Investig Otolaryngol. Feb 2025.
Heikel T, Goldenberg D. In-Office Management of Thyroid Nodules. Otolaryngol Clin North Am. May 2025.
Higgins RC, Hennessy M, Aynardi JT, Goldenberg D, Goyal N. An invasive tracheal paraganglioma: A rare cause of a thyroid mass. Ear Nose Throat J. May 2025.
LaBarge B, Lorenz FJ, Gniady JP. Association of Laryngeal Dystonia With Common Neurologic Disorders. The Laryngoscope. July 2025.
Congrats to Dr. David Goldenberg and Dr. Bradley Goldstein on the publication of the Handbook of Otolaryngology – Head and Neck Surgery, 3rd Edition. This essential guide provides detailed, practical guidance across the full continuum of patient care. Highly regarded in the field, it serves as a comprehensive, quick-reference resource for otolaryngology residents and practicing physicians. Praised for its concise yet thorough coverage of key topics, it remains an invaluable tool for board review, clinical practice, and rapid information retrieval.
Lighthall JG. Simplifying a Complex Puzzle: Optimizing Outcomes in Face and Neck Trauma. Facial Plast Surg Clin North Am. May 2025.
Lorenz FJ, Kharouta M, Mahase SS, Goyal N, Rezaee R, Lavertu P, Machtay M, Yao M. Hospital-Based Registry Analysis of Staging Efficacy and Proposed Staging Subclassification for Stage I HPV-Associated Oropharyngeal Squamous Cell Carcinoma. Oral Oncol. Mar 2025.
Lorenz FJ, Ma C, Givens AK, Walen SG. Borderline Personality Disorder Diagnoses in Facial Plastic Surgery: A Large Database Analysis. OTO Open. May 2025.
Lorenz FJ, Ma C, Parikh AC, Lighthall JG. Cleft Lip and/or Palate Is Associated with an Increased Prevalence of Mental Health and Behavioral Disorders. Cleft Palate Craniofac J. Apr 2025.
Lorenz FJ, Ma C, Walen SG. The Impact of Bioabsorbable Nasal Implants, Nasal Radiofrequency Remodeling, and Anesthesia Type on Patient Selection for Nasal Valve Surgery. OTO Open. May 2025.
Lorenz FJ, Schopper HK, Walen SG. The Role of Toxins and Fillers in Optimizing Perioral Rejuvenation. Facial Plast Surg. Jun 2025.
Ma C, Parikh A, Lighthall JG. Evaluation and Treatment Planning to Maximize Perioral, Submental, and Neck Aesthetics. Facial Plast Surg. May 2025.
Meci A, Bollig C, Tseng C, Goyal N. Evaluating YouTube Videos for Resident Education in Free Flap Surgery. Laryngoscope Investig Otolaryngol. Feb 2025.
Meci A, Goyal N, Goldenberg D. Malignant Transformation Rate of Oral Premalignant Disorders: A Large Database Analysis. Laryngoscope. May 2025.
Meci A, Lorenz FJ, Goyal N, Goldenberg D. Elevated Risk of Thyroid Malignancy in Biological Males Taking Estrogen Hormone Therapy. Otolaryngol Head Neck Surg. Jan 2025.
Meci A, Tseng C, Jensen Z, Goyal N. Online Discourse and Trends Surrounding HPV Vaccination for Head and Neck Cancer Prevention. Otolaryngol Head Neck Surg. Mar 2025.
Oxford M, Tucker J, Goldenberg D, King TS, Ziai K, Henry C, Lighthall JG. Comparison of Pediatric and Adult Mandibular Fractures: Identifying Differences in Presentation and Management Using a National Trauma Database. J Craniofac Surg. Mar 2025.
Parikh A, Harvey A, Walen S. Comprehensive Review on the Management of Subcondylar and Condylar Mandibular Fractures. Facial Plast Surg Clin North Am. May 2025.
Parikh A, Lighthall JG. Repairing the Nasal Valve in Revision Surgery. Otolaryngol Clin North Am. Jan 2025.
Rossip M, Lorenz FJ, Goyal N, Goldenberg D. Hypocalcemia After Thyroidectomy in Patients Taking Proton Pump Inhibitors. Laryngoscope Investig Otolaryngol. May 2025.
Rossip M, Lorenz FJ, Sciscent B, Truong N, Nimmagadda C, Goyal N, Goldenberg D. Effect of Histamine-2 Receptor Antagonists on Hypocalcemia after Thyroidectomy: A Retrospective Cohort Study and Sensitivity Analysis. Otolaryngol Head Neck Surg. Feb 2025.
Schopper HK, Strohl-Bryan AM, Lighthall JG. Technological Advances and Adjuncts to Optimize Outcomes in Craniomaxillofacial Trauma. Facial Plast Surg Clin North Am. May 2025.
Sciscent BY, Polanik M, Lorenz FJ, Eberly HW, Whitaker ME. Anxiety and Depression in Patients With Vestibular Disorders. OTO Open. Jun 2025.
Tucker J, Patel S, Benyo S, Wilson MN, Goyal N, McGinn J. Descriptive Analysis of Otolaryngology Program Directors with a Focus on Gender Disparity. Ear Nose Throat J. Apr 2025.
Bavier R, Kulkarni P, Goldenberg D, Funk E. Clinicopathologic Prognostic Factors of Pleomorphic Dermal Sarcoma in Head and Neck Versus Non-Head and Neck Subsites. COSM. New Orleans, LA. May 2025. Poster Presentation.
Chan K, Ma C, Sciscent BY, Urso A, Goyal N, Lighthall JG. Emerging Medications in Facial Nerve Recovery: A Systematic Review and Meta-Analysis. COSM. New Orleans, LA. May 2025. Poster Presentation.
Cinnamo M. The Effects of Chemotherapy on Hearing (Ototoxicity) and General Tips on Hearing Health for Cancer Patients. Support for People With Oral, Head and Neck Cancer. Virtual. Mar 2025. Oral Presentation.
Delp E. Hearing Loss. Hearing Loss Association of Cornwall Manor. Lebanon, PA. May 2025. Oral Presentation.
Eisenhart C. Hearing Aids. Hearing Loss Association of Cornwall Manor. Lebanon, PA. Apr 2025. Oral Presentation.
Gniady JP, Purnell P. VYLO™ 455nm Blue Light Laser System Clinical Event. COSM. New Orleans, LA. May 2025. Oral Presentation.
Goldenberg D. Thyroid Nodule Ablation: When, Why, How. Mount Sinai Beth Israel Division of Endocrinology, Diabetes and Bone Diseases. Virtual. Mar 2025. Oral Presentation.
Goldenberg D. History of Antisemitism. Penn State Health and Penn State College of Medicine. Hershey, PA. Apr 2025. Oral Presentation.
Goyal N. Grand Rounds: Beyond Cancer – Quality of Life in Survivorship. University of Manitoba Resident Research Day. Winnipeg, Manitoba. Apr 2025. Oral Presentation.
Goyal N. The Impact of Big Data: Shaping Health Policy and Clinical Decisions. University of Manitoba Resident Research Day. Winnipeg, Manitoba. Apr 2025. Oral Presentation.


Dr. Pallavi Kulkarni, PGY-1, earned second place for her oral presentation, and Dr. Christopher Tseng, PGY2, placed second for his poster.
Goyal N (Moderator), Hutchenson K, Mohebbi A, Manduchi B, Hullfish H, Cleer EF, Owoc MS. Scientific Session 2: Quality of Life & Health Behaviors. COSM. New Orleans, LA. May 2025. Panel Presentation.
Hadlock T, Bhama P, Lighthall J. Management of Chronic Facial Paralysis. Facial Nerve Symposium Pacific Neuroscience Institute. Santa Monica, CA. Feb 2025. Panel Presentation.
Keane A. Pediatric Airway Emergencies. Division of Pediatric Emergency Medicine Educational Series. Hershey, PA. Mar 2025. Oral Presentation.
Kulkarni P, Goyal N. Timing of Tracheoesophageal Puncture Placement and an Association with Mental Health Disorders. COSM. New Orleans, LA. May 2025. Poster Presentation.
Kulkarni, P, Chan K, Tseng C, Walter V, Broach J, Goldenberg D. Genomic Structural Variation of Anaplastic Thyroid Cancer Using Optical Genome Mapping. COSM. New Orleans, LA. May 2025. Poster Presentation.
Kulkarni, P, Meci A, Funk E. Acquiring and Trending C- Reactive Protein in Patients with Head and Neck Necrotizing Fasciitis. COSM. New Orleans, LA. May 2025. Poster Presentation.
Kulkarni, P, Meci A, Bavier R, Funk E. Vitamin D Deficiency Is Not Associated With Worse Postoperative Flap Reconstruction Outcomes. COSM. New Orleans, LA. May 2025. Poster Presentation.
LaBarge B, Lorenz FJ, Gniady JP. Analysis of the Surgical Etiology of Vocal Fold Paralysis and need for Medialization. COSM. New Orleans, LA. May 2025. Poster Presentation.
LaBarge B, Lorenz FJ, Gniady JP. Association of Laryngeal Dystonia with Common Neurologic Disorders. COSM. New Orleans, LA. May 2025. Poster Presentation.
Lighthall J. What is Facial Synkinesis? Surgical and Nonsurgical Options. Facial Nerve Symposium Pacific Neuroscience Institute. Santa Monica, CA. Feb 2025. Oral Presentation.
Lighthall J. Allograft use in Facial Reanimation Surgery Pros & Cons. Facial Nerve Symposium Pacific Neuroscience Institute. Santa Monica, CA. Feb 2025. Oral Presentation.
Lighthall J. Advances in Facial Reanimation. Thomas Jefferson University Herbert Kean, MD Lectureship. Philadelphia, PA. Apr 2025. Oral Presentation.
Lighthall J (Moderator), Bhama P, Hadlock T, Seruya M, Kochar A. Management of Synkinesis. Facial Nerve Symposium Pacific Neuroscience Institute. Santa Monica, CA. Feb 2025. Panel Presentation.
Dr. Jeffrey Lorenz, PGY-2 resident, was awarded winner for his presentation titled “Chemodenervation is Associated With Reduced Mental Health Disorders in Patients With Synkinesis” at the Ferraro Resident Symposium in Otolaryngology.

Lorenz FJ. Cleft lip and/or palate is associated with an increased prevalence of mental health and behavioral disorders. Penn State Resident and Fellow Research Day. Hershey, PA. May 2025. Poster Presentation.
Ma C, Chan K, Eberly E, Newland M, Lighthall JG. Hair Preservation and Restoration in Chemotherapy-Induced Alopecia. COSM. New Orleans, LA. May 2025. Oral Presentation.
McClelland J. Advocacy in Audiology: The Invested Audiologist. Lehigh Valley Health Network. Mar 2025. Oral Presentation.
McClelland J. Hearing Loss and Inpatient Amplifiers. Penn State Health Geriatrics Scholars Program. Hershey, PA. Mar 2025. Oral Presentation.
McClelland J. Audiology and Geriatrics: Hearing Loss and Cognition. Penn State Health Internal Medicine Residency Program. Hershey, PA. Feb 2025. Oral Presentation.
McClelland J, Shafer J, Brown J, Lemme K, Mowatt T, Czuhajewski S. Lobbying 101: AuDvocating for Public Policies that Advance Patient Care. Pennsylvania Academy of Audiology and the Academy of Doctors of Audiology. Virtual. Feb 2025. Panel Presentation.
Meci A, Goldenberg D. The risk of hypoparathyroidism following head and neck radiation therapy. COSM. New Orleans, LA. May 2025. Poster Presentation.
Meci A, Goyal N, Goldenberg D. Branchial cleft cyst carcinoma is grossly over diagnosed: A large database analysis. Triological Combined Sections Meeting. Orlando, FL. Jan 2025. Poster Presentation.
Meci A, Goyal N, Goldenberg D. Malignant progression of oral carcinoma in situ: A large database analysis. Triological Combined Sections Meeting. Orlando, FL. Jan 2025. Poster Presentation.
Meci A, Goyal N, Goldenberg D. Malignant transformation rate of oral premalignant conditions: A large database analysis. Triological Combined Sections Meeting. Orlando, FL. Jan 2025. Oral Presentation.
Meci A, Rothka A, Hearn M, Lorenz FJ, Goyal N, Gniady JP, Goyal N. Utilizing Artificial Intelligence to Reduce the Reading Grade Levels of Patient Education Materials in Laryngology. COSM. New Orleans, LA. May 2025. Oral Presentation.
Meci A, Ji Q, Goyal N, Goldenberg D, Pandian V. Impact of Early Versus Late Planned Tracheostomy on Survival and Complications in Critically Ill Patients: A Retrospective Analysis Using TriNetX. Translating Research into Innovations in Practice Symposium. Camp Hill, PA. May 2025. Oral Presentation.
Meci A, Pradhan S, Lorenz FJ, Goyal N, Goldenberg D. Trends in the features of male thyroid cancer in the United States. COSM. New Orleans, LA. May 2025. Poster Presentation.
Mukhtar H, Meci A, Goyal N, Goldenberg D. Role of Exogenous Estrogen Use on the Development of Thyroid Cancer. COSM. New Orleans, LA. May 2025. Poster Presentation.

Speech-language pathologists Kali Anderson and McKenzie Troutman earned their neonatal therapy certification after completing specialized training and passing the exam, allowing them to deliver neuroprotective, developmentally appropriate care to the tiniest of patients.
Purinton R. Tinnitus. Hearing Loss Association of Cornwall Manor. Lebanon, PA. Mar 2025. Oral Presentation.
Purinton R. Tinnitus and Hyperacusis. Calvin G. and Janet C. High Learning & Wellness Center. Lancaster, PA. Mar 2025. Oral Presentation.
Tseng C. Exploring the impact of obesity on thyroid pathology in the DUOX271200H murine model of thyroid cancer. Penn State Resident and Fellow Research Day. Hershey, PA. May 2025. Poster Presentation.
Shannon Welch, SLP, and Erin Edwards, BCBA, were honored as Employees of the Month in December 2024 for their outstanding dedication to empowering patients through communication support.

Brown T. Outstanding Staff Departmental Award. Penn State Health Department of Otolaryngology – Head and Neck Surgery. May 2025.
Goyal N. Physician of the Month. Penn State Health Milton S. Hershey Medical Center. May 2025.
Lighthall JG. Helen Krause, MD Distinguished Service Award. Pennsylvania Academy of Otolaryngology – Head and Neck Surgery Annual Scientific Meeting. Jun 2025.
Patel C. Excellence in Clinical Care Departmental Award. Penn State Health Department of Otolaryngology – Head and Neck Surgery. Hershey, PA. May 2025.
Polanik M. Extraordinary Otolaryngology Resident Award. Penn State Health Department of Otolaryngology – Head and Neck Surgery. Hershey, PA. Jun 2025.
Rodriguez D. Excellence in Nursing Departmental Award. Penn State Health Department of Otolaryngology – Head and Neck Surgery. Hershey, PA. May 2025.
Spencer M. Positive Impact Award. Penn State Health. Hershey, PA. Jun 2025.
Walen S. Faculty Teaching and Mentorship Award. Penn State Health Department of Otolaryngology – Head and Neck Surgery. Hershey, PA. Jun 2025.
Welch S, Edwards E. Employees of the Month. Penn State Health Milton S. Hershey Medical Center. Hershey, PA. Jan 2025.















Department of Otolaryngology – Head and Neck Surgery
Penn State Health Milton S. Hershey Medical Center
Penn State College of Medicine
500 University Drive, MC H091
Hershey, PA 17033-0850
med.psu.edu/otolaryngology


@PSH_OTO


