

Research Report 2025

Acknowledgement
Peninsula Health acknowledges the Traditional Custodians of the lands where our Health Services are located. We acknowledge the Bunurong and Boon Wurrung people of the Kulin Nation. We pay our respects to Elders past, present and emerging.
Welcome from the Board Chair
Welcome to the 2025 Research Report. We are proud to be sharing the research that is happening at Peninsula Health – research that will ultimately improve the lives and health outcomes of people across the Frankston and Mornington Peninsula communities.

Our mission is healthy lives for everyone, through sustainable, innovative, compassionate care. Under the direction of several research leaders, our research informs how we deliver effective, person-centred and efficient care, and is a key driver for future innovations. Research is an integral part of ensuring we provide the best healthcare now, and into the coming years.
This report showcases some of the many research projects underway at Peninsula Health. Our engagement in novel clinical trials of lifesaving drugs is rapidly increasing, promising access to such treatments to our community.
Cutting-edge technology is at the forefront of much of our work. For example, the Frankston Emergency Department is incorporating AI and sensing technologies within an in-situ resuscitation simulation to improve debriefing with real-time objective insights. We also support a study on how virtual reality can improve dental care and experiences for people of all ages and abilities.
The National Centre for Healthy Ageing (NCHA), a partnership between Peninsula Health and Monash University, is leading the way with data-driven ground-breaking research that will improve clinical care locally and across the sector. The NCHA is on the verge of delivering six unique technology-supported research simulation facilities, including a Smart Ward at The Mornington Centre – which will support transformative and innovative research towards healthy ageing.
The upcoming opening of Peninsula University Hospital in early 2026 – and the merger of our health service with Alfred Health, Bass Coast Health, Gippsland Southern Health Service and Kooweerup Regional Health Service to become Bayside Health – will provide exciting opportunities for collaborative major research projects and initiatives into the future.
With technology evolving rapidly across the world, this report captures a pivotal time in research at Peninsula Health, but is also a celebration of our people, across a range of healthcare settings, whose expertise and passion for their projects help make our mission - healthy lives for everyone – a reality.
Please enjoy reading this report.
Karen Corry, Board Chair
Message from the Director of Research
As Director of Research, I am pleased to present this year’s achievements within the framework of our newly co-designed Research Strategy (2025-2029).
In this report, we outline the research already underway in four key pillars:
› a skilled and supported workforce
› consumer and community involvement
› innovation and collaboration
› sustainability through strong systems and infrastructure.
We have a strong platform to enact this strategy building on our steady progress embedding research into everyday practice, strengthening capability across our teams, and ensuring that our work delivers meaningful benefits for patients, staff, and the wider community.
A skilled and supported workforce remains at the heart of our progress. Leaders such as Associate Professor Mahesh Iddawela and Associate Professor Cathleen Aspinall are shaping new models of clinical–academic leadership, embedding research into oncology, nursing, and midwifery practice.
Just as importantly, we are developing the next generation of researchers through structured pathways, mentoring, and postgraduate support.
This year, 20 PhD candidates were supported across diverse disciplines including oncology, surgery, speech pathology, mental health, and aged care, reflecting both the breadth and depth of our research culture. As you will read in this research report, early-career researchers are also making valuable contributions, tackling important questions in areas such as organ donation, stroke rehabilitation, and communication in care. These efforts demonstrate our commitment to nurturing a workforce that is research-active, well supported, and confident in turning clinical challenges into opportunities for discovery and improvement.

We have deepened our commitment to consumer partnership through Standard 2 implementation, the roll-out of a Consumer Clinical Trial Experience Survey, and the development of accessible information resources for consumers, including for our First Nations community. These initiatives ensure that our research is co-designed with those with lived experience of health conditions that are relevant and of high priority to our community.
Systems and infrastructure are critical. Apart from the exciting and imminent opening of the new Peninsula University Hospital, increased engagement with our Monash University partners, and near completion of the build of the various components of the National Centre for Healthy Ageing, we are working hard towards enabling improved working environments for our clinical research staff, particularly those involved in clinical trials.
Finally, our research maturity and sustainability continue to strengthen, with 101 new projects approved, 97 active clinical trials, and 159 peerreviewed publications in 2024–2025. Major grants and data-driven tools, such as the development of an Electronic Frailty Index, are helping us build sustainable systems to support future research.
I hope you enjoy reading this year’s report.
Professor Velandai Srikanth, Professor of Medicine, Director of Research, Peninsula Health and Director, National Centre for Healthy Ageing
Image: Professor Velandai Srikanth
Our vision is to create a culture where research is integral to care. To achieve our vision, there are four overarching goals guiding our research.
Goal 1: A skilled and supported workforce
We will grow and support our workforce to be research active.
A new leader of oncology care and research
Peninsula Health’s Head of Oncology, Associate Professor Mahesh Iddawela, says it was the rapid evolution of cancer research and treatments that sparked his interest in the field.
“Oncology has changed dramatically – patients are living longer and having more and more treatments, and it’s obviously a great success story in that way,” explains A/Prof Iddawela, who joined Peninsula Health earlier this year. “For example, a large number of patients with advanced melanoma are now cured; ten years ago when I first started as a consultant, they would only live for about six months.”
A/Prof Iddawela completed medical school in London before moving on to oncology training in Cambridge, where he spent 10 years as a consultant and completed his PhD on breast cancer biomarkers. Despite the gains he has seen in his field, A/Prof Iddawela is driven by the belief that there is still work to be done.
A/Prof Iddawela was attracted to working with Peninsula Health due to the strong cohort of services, co-location with Monash University, and what he described as a “shared vision” to embed academic structures and research within the organisation. He also observed that the region has a wide catchment of common cancers, presenting an opportunity to develop a comprehensive service that improves care for patients closer to home.
“We want to develop a comprehensive cancer program where we can really make both the services and outcomes better for the patients in the local area, so that they don’t have to go out of the region to get the best care,” explains A/Prof Iddawela.
With the upcoming Peninsula University Hospital, A/Prof Iddawela is looking forward to the Oncology Department having its own floor with combined services, and envisages “a centre of excellence for cancer care with integrated patient care, clinical trials, and research.”
“That’s one of the things I’m very keen on - to try and improve the service delivery to make things better for the patients in the short term, and also in the long term, to improve outcomes for patients by undertaking clinical trials and new research.”

Image: Associate Professor Mahesh Iddawela

Building a strong culture of research in nursing and midwifery
A cultural shift in how nurses and midwives engage with research at Peninsula Health is underway, driven by Dr Cathleen Aspinall, Associate Professor of Nursing and Midwifery Research at Peninsula Health.
With a strong background in nursing and research, including a PhD focused on nursing leadership and empowerment, A/Prof Aspinall has a thorough understanding of the importance of creating clear pathways for nurses and midwives to become research leaders in their fields.
Associate Professor Aspinall’s goal is to make research exciting, engaging, and everyone’s business at every level, all while working towards improving patient outcomes.
“In my role, I’m involved in several areas of research. Currently, I’m focused on developing clinical academic roles for nurses and midwives, as well as exploring the importance of the fundamentals of care and how they can be embedded into policy, practice, education, and research,” says A/Prof Aspinall.
“Alongside this, I’m also deeply engaged in research projects at Peninsula Health, collaborating with individuals interested in conducting studies.
I support the development of research proposals and assist with grant applications, acting as a key link between universities and our health service.”
As of 2025, A/Prof Aspinall is supervising two PhD students, along with a small cohort of nurses and midwives completing their honours degrees, supported by Peninsula Health’s postgraduate scholarship program.
“It’s a privilege to serve as the connection – continuing the relationship from first meeting them at Peninsula Health to later supervising their academic work from a university perspective. Serving as a bridge between clinical practice and academic research is vital to ensuring these individuals feel truly supported,” reflects A/Prof Aspinall.
“Research is integral to improving patient outcomes and the quality of healthcare,” explains A/Prof Aspinall.
“Health services with a strong research culture report lower mortality rates, higher patient and staff satisfaction, and better organisational performance.”
“By supporting, advising, coaching, and mentoring nurses and midwives as they begin, continue, and excel in their research journeys, we can provide the evidence that underpins clinical practice and care at Peninsula Health,” concludes A/Prof Aspinall.
In working closely with department leaders, clinical staff, and students, A/Prof Aspinall is strengthening research across the organisation – driving better health outcomes and empowering nurses and midwives to deliver exceptional care through evidence-based practice.
Image: Associate Professor Cathleen Aspinall
Creating meaningful change through research
Anthony Cignarella is a critical care nurse, clinical educator, volunteer lifeguard, dad, and PhD candidate. His past experience as a clinical nurse specialist in the ICU at The Alfred led to an interest in organ donation.
“It takes a particular kind of person to be in that space,” Mr Cignarella explains. “It’s highly emotive, highly sensitive.”
Mr Cignarella ‘s PhD focuses on identity disclosure between the family members of deceased organ donors and transplant recipients.
From his clinical experience, Mr Cignarella is aware of the multifaceted nature of organ donation for families of lost loved ones – who are often young people. There is also the complexity of balancing one family’s loss with the joy of a recipient’s family.

“I’ve had to learn over the years to be mindful of worklife balance, self-care, and protective factors,” Mr Cignarella says. “I try to keep fit where possible – running, swimming, yoga, playing the piano.”
Mr Cignarella was born with congenital deafness and wears a hearing aid and a bionic ear. During COVID, working in a masked environment presented new challenges, forcing Anthony to decide whether face-toface nursing was going to be sustainable for him. Fortunately, it became the ideal time to pursue his passion for research.
“I’m passionate about helping others recognise their potential,” he says. “Nurses and midwives can create meaningful change – not just at the bedside, but also through research that contributes to the greater good.”
Image: Anthony Cignarella
A passion to improve experiences of people with communication impairment
PhD candidate and speech pathologist Vicky Aston had an unexpected ‘aha’ moment one day in Frankston’s Emergency Department, when a colleague commented that texture-modified food is “awful and nobody likes it”.
“I went – oh! – how do I know if that’s what patients actually think?” says Mrs Aston. “I looked at the research and, to my surprise, there was no research available exploring patients’ perspectives on mealtimes for those with both swallowing impairment and communication impairment following a stroke.”
Mrs Aston’s PhD research aims to understand the mealtime experiences of adult hospital patients who have dysphagia and communication disabilities (such as aphasia, dysarthria and dyspraxia of speech) and patients who have had a stroke.
As well as identifying the aspects of mealtimes that affect health, safety, and wellbeing, Mrs Aston hopes to better understand the barriers and enablers to accessing safe, enjoyable meals – from the perspectives of patients, family members, and hospital staff.
Historically, people with communication impairment are often excluded from research, but Mrs Aston plans to use strategies from her speech pathology
background to support and engage with these patients to get their perspectives.
After beginning her career as a British Army medic and earning the Iraq Medal, Mrs Aston transitioned to working as an anaesthetic technologist in operating theatres.
Later, inspired by her speech pathologist sister-in-law and memories of her grandmother’s severe expressive aphasia, she found a meaningful path in speech pathology and says, “I saw how my past could help make a real difference.”

Image: Vicky Aston
Goal 2: Consumer and community involvement
We will actively partner with consumers to co-design and deliver research programs important to our community.
Consumers guiding clinical trials
Consumers are working hand in hand with researchers to improve community participation and understanding of clinical trials, through a new working group.
“The Partnering with Consumers in Research Working Group is an important initiative that ensures our consumers are involved in everything we do,” explains Professor Nadine Andrew, Chair of the working group.
“Research is critical and it leads to better outcomes for everyone.”
As part of Peninsula Health’s commitment to upholding the accreditation of clinical trials and delivering safe, high-quality clinical trial services for patients and consumers, the working group has been established to support the implementation of Standard 2, under the Australian Commission on Safety and Quality in Health Care’s National Clinical Trials Governance Framework (NCTGF).
Established in May 2024, the working group is facilitated by Dr Kim Naude, Peninsula Health’s Clinical Trials Support Coordinator – Consumer Engagement, who is responsible for leading the implementation of Standard 2 of the NCTGF across the health service.
“Within Standard 2 of the NCTGF, there are nine key actions. The working group’s aim is to implement these actions across the health service,” explains Dr Naude.
It brings together clinical trial and consumer engagement staff from across the health service, along with a clinical trial consumer advisor who has firsthand experience as a trial participant.
“This includes initiatives such as improving health literacy, creating clear and accessible information for consumers about clinical trials, providing training for staff on consumer and community involvement (CCI) in research, and exploring ways to partner with consumers throughout the entire clinical trial research cycle,” explains Dr Naude.
Strong partnerships at every level of the organisation are essential to achieving the best outcomes for all involved. When clinical trials are delivered through these partnerships, they bring wide-ranging benefits for patients, consumers, clinicians, health service organisations, and the broader health system.
Over the past 12 months, the working group has undertaken a range of projects.
Standard 2 focuses on partnering with consumers, requiring health service organisations to work collaboratively with patients, carers, families, and consumers in the design and evaluation of all clinical services, including clinical trial services.

“We have achieved a lot in our first year,” says Dr Naude. “One highlight has been developing a Clinical Trial Consumer Experience Survey, which is now being progressively implemented across all clinical trial units in the health service.”
Designed as an ongoing quality improvement measure, this survey aims to continually assess participant satisfaction, identify opportunities for improvement, and strengthen person-centred care in clinical trials. It builds on a survey piloted by The Alfred Hospital, which has since been refined locally.
Image: Consumers and staff in the Standard 2 Working Group

“We piloted the survey from April to June in Peninsula Health’s Oncology, Cardiology and Respiratory units, and received feedback from 13 participants about their experiences,” says Dr Naude.
“Participants rated their overall experience of care as ‘very good’, reporting that they felt well-supported during the consent process and found trial information clear and accessible. Overall, they were very happy with the care they received.”
Alongside the survey, the team has also designed and implemented a Consumer and Community Involvement in
The Partnering with Consumers in Research Working Group continues to play a pivotal role in embedding consumer voices at the heart of Peninsula Health’s clinical trial services. By fostering strong partnerships, implementing practical initiatives, and driving continuous improvement, it is not only meeting the requirements of the NCTGF but also shaping a more collaborative, transparent, and responsive approach to research.
“One key objective is to increase consumer participation in the working group, and we anticipate the newsletter will play an important role in achieving this,” says Dr Naude.
Research Framework, delivered a training session on consumer involvement in research for clinical trials staff, developed a “Thinking about Joining a Clinical Trial?” flyer for trial participants, and produced participant information reviewed by the Consumer Information Committee.
Looking ahead, the working group is preparing a community newsletter, which will include highlights on current Peninsula Health clinical trials, stories from participants and clinical trial staff, updates of consumer engagement activities and opportunities, and resources and information to support inclusive research.
Through this commitment, Peninsula Health is strengthening its reputation as a leader in high-quality, consumer-focused clinical trials. By ensuring patients and the community are actively involved in shaping research, the organisation is building a future where clinical trials are more accessible, better understood, and ultimately deliver greater benefits for the entire community.
The influence of emotions on confronting death in end stage renal disease
The attitudes, beliefs, and decision-making process of elderly patients in their management of end stage renal disease (ESRD) have been examined in a new study by Dr Vinod Venkataraman, a nephrologist at Peninsula Health.
Dr Venkataraman’s study found that emotions on confronting death are varied and they have a significant but subtle influence on decision-making for patients. Better understanding these emotions is considered essential for clinicians to deliver patientcentred care. Decision-making for elderly patients with ESRD about treatment options is a complex process.
“We identified a knowledge gap in the literature about the influence of emotions on confronting death,” explains Dr Venkataraman.
“Our research objective was to explore the attitudes, beliefs, and decision-making process of elderly patients in their management of ESRD.”
“We focused on two main research questions: How does death anxiety differ in elderly patients with ESRD between the dialysis treatment and the conservative kidney management groups? And what is the role of death anxiety in the decision-making process?” adds Dr Venkataraman.
The research methodology chosen was interpretive phenomenology, using semistructured interviews based on seven pre-determined questions.
The interviews were conducted with 12 patients receiving dialysis and eight patients receiving conservative kidney management, who were over 65 years of age and diagnosed with ESRD in the last five years. All had an English-speaking background.
The interviews identified six themes:
1. ‘Illusion of choice’: The concept of decision-making is based on choice, and that itself can be dubious
2. ‘Myriads of emotions on facing the inevitable: Participants faced various emotions on approaching death, both positive and negative. Death anxiety is not the only emotion faced by people in this situation

3. ‘Death denial and acceptance’: The thoughts involved in processing the news of death are variable too. Death anxiety, a manifestation of an inability to process the news of death, was fairly distributed in both the dialysis and conservative kidney management participants
4. ‘Coping with news of death’: Multiple strategies were employed to overcome these emotions when confronting death. Some were self-reliant and others from external support
5. ‘Process of decision-making’: Participants were influenced subtly by their emotions in various ways
6. ‘Receptivity to education and information on facing news of death’: The clinicians’ knowledge and education were not able to help participants when these emotions surrounded them

Dr Venkataraman found that a lack of insight into these emotions can lead to frustration of clinicians and patients in the decision-making process.
“Further quantitative research into death anxiety needs to be conducted to appreciate its full impact in the Australian environment,” explains Dr Venkataraman.
“The emotional preparedness of clinicians also needs to be studied for establishing the best possible patient-centred care.”
ESRD is the last stage among the five stages of chronic kidney disease. Patients experience many symptoms due to uremic toxin build-up – such as tiredness, fatigue, loss of appetite, and weight loss. The symptoms can be due to electrolyte disturbances like high potassium, high phosphate, and low bicarbonate levels. They can also be due to fluid buildup and associated shortness of breath. If these complications are not treated in time and adequately, the patient’s life can be compromised.
The treatment options for ESRD consist of transplantation, dialysis and conservative kidney management. Transplantation involves a major surgical procedure and significant suppression of immunity to implant another’s kidney into the patient’s body, to remove the toxins that are not cleared by the patient’s own kidneys.
Dialysis involves an invasive and intense treatment procedure for the patient, where an external machine clears the toxins and fluid built up in the patient’s body. Conservative kidney management is a gentler treatment option, where symptoms and complications are managed by medicines and non-invasive measures only. This disease and its treatment have a big impact on our population.
“Clinicians need to be educated on the various emotions patients could face, which will pave the way for better shared decision-making,” explains Dr Venkataraman.
“By knowing and understanding these emotions, clinicians can connect, empathise, address, support and acknowledge them in their ongoing interactions with patients with ESRD.”
Image: Dr Vinod Venkataraman with consumer Carol in the Dialysis Unit
Bridging the gap: how clinical trial staff and consumers define partnership in clinical trials
Clinical trials give patients access to new and developing treatments. What can we learn from better understanding the lived experience of participants? How can their active involvement in the research cycle enhance the planning, design, delivery, and evaluation of clinical trials?
Dr Kim Naude works in the Office for Research, leading the implementation of Standard 2 of the National Clinical Trials Governance Framework –Partnering with Consumers. This Standard aims to ensure that consumers are not just participants, but partners in their own care and in the overall clinical trial process.
“There’s quite a gap between policy and practice and this term ‘partnering with consumers’,” says Dr Naude. “What does it actually mean for clinical trial staff and consumers?”

Previous research suggests that researchers may often approach partnerships as a procedural or compliance-driven task, whereas the consumers seek genuine opportunities to influence research priorities and processes.
“Research tends to focus on the investigation side and not on finding out from the people with lived experience … about how we can help them and make trials better for our community,” explains Dr Naude.
“There’s a lot that can be done in this space to ensure our trials meet our consumers’ needs.”
The research will be undertaken by conducting semi-structured interviews with clinical trial staff, and a focus group with consumers – either someone who has been involved in a clinical trial at Peninsula Health as a participant or someone who has cared for or supported someone in a clinical trial.
“It’s a qualitative research project, which by its nature is exploratory,” Dr Naude says.
“That’s the beauty of qualitative research because you don’t actually know what people are going to say.”
It’s hoped that the findings will generate practical insights and recommendations for health services in the early stages of consumer and community involvement implementation under the National Clinical Trials Governance Framework. This will identify training needs, assist in developing tools to support partnership clarity, and provide guidance to researchers to avoid tokenism. By clarifying what “partnership” means to those expected to practice it – and those most impacted by it – this research can help services engage consumers more meaningfully, improving the relevance, trust, and quality of clinical trials.
“We’re just at the start of implementation, and hopefully this research will help other health services and guide them in how to do this,” says Dr Naude.
Image: Dr Kim Naude
Goal 3: Innovation and collaboration
We will foster a culture of innovation and collaboration, strengthening research quality through strategic partnerships.

Using AI to enhance learning
Artificial Intelligence (AI) and sensing technologies are being incorporated into in-situ resuscitation simulations in the Emergency Department (ED) to explore whether these technologies can enhance the learning experience for medical and nursing staff, and augment the debriefing process with real-time, objective insights.
“AI in simulation-based learning has been explored within the university setting, and now in a partnership between Monash University and Frankston Hospital Emergency Department, it is being trialled for real-world application,” explains Joy Davis, Associate Investigator and Education Stream LeadSimulation and Learning Design, Peninsula Health.
Simulations replicate real-world clinical scenarios for training. Interprofessional in-situ simulations bring staff together – as they would work in their natural environment, with locally contextualised challenges and resources.
The pilot scenarios in August saw ED staff care for a critically unwell patient and provided the research team with further refinements to the analytics and case in preparation for the rollout of six scenarios in October.
“As part of the study, microphones and cameras are set up in the room, and participants wear positioning tags that track movement and spatial interaction, wristbands (like a smartwatch) that detect physiological data such as heart rate spikes, and microphones to capture verbal communication,” explains Ms Davis.
Multiple sources of data are analysed by the software designed by Monash University and presented in a visual display to discuss with participants during the analysis phase of the debrief.
“Audio is analysed by AI to identify key communication interactions between the team, such as sharing information and allocating of tasks.”
Image: Emergency Department staff during the simulation
This includes visual representations, such as each person’s location and movement within the room, or the strength and directional flow of communication.
“Normal practice is to facilitate a simulation scenario with the debriefer observing, noting key actions, decisions, or communications to discuss in the debrief,” explains Ms Davis.
Following the simulation activity, participants enter the debrief phase, which is a collaborative discussion on the events of the scenario, and the learning that can be applied in future clinical situations.
“The facilitator has a significant cognitive load trying to remember specifics of the simulation to talk about, plus actively listening to what the participants say because it’s not like leading a lecture; you’re facilitating a learner-centred discussion,” explains Ms Davis.
“The intent is to explore if the data produced from the AI and sensing technologies can support the debriefer, providing objective data to enhance the debrief and provide greater insights into teamwork, team performance, and communication.”
Following the August pilot, the Peninsula Health and Monash University research teams are working together to script the code book that supports the AI to identify statements around leadership, task management, communication, teamwork, and situational awareness.
“We know the way people communicate is really important,” adds Ms Davis.
“So we’re programming the AI to look at different communication patterns: Was there task allocation? Was the instruction received and acknowledged? Was there a handover?”

“It’s about augmenting the debriefing to enhance the learning.”
As well as examining the effectiveness of having AI as part of the debriefing process, the study will also look at barriers and feasibility.
“We will examine whether the benefits outweigh the disadvantages – there are ongoing costs in using this technology,” adds Ms Davis.
“Following participation in the scenario, both participants and debriefers will be contacted seeking their feedback in postscenario interviews, considering what it was like having to wear wearables and a microphone during a simulation and whether it was distracting.”
The study received funding from the Laerdal Foundation, and is being led by principal investigators Associate Professor Samantha Sevenhuysen, Director Education and Training, Peninsula Health and Associate Professor Roberto Martinez-Maldonado, Faculty of Information Technology, Monash University.
There are many possibilities for how AI and sensing technologies could be used in healthcare settings in the future to enhance learning, teamwork, and communication in critical situations, such as peer-to-peer training, and is applicable to other clinical areas.
Image: Joy Davis
The Smart Ward – the future of healthcare for older adults

The future of healthcare has arrived in the form of the Smart Ward. The Flinders Ward at The Mornington Centre is a Geriatric Evaluation and Management ward, providing sub-acute care for older adults.
In September 2025, it became the first ward at Peninsula Health to become a Smart Ward. In the Smart Ward, there are electronic devices in the ceiling and on the walls to help keep track of patients’ health and wellbeing, improve patient care and safety, and improve the patient experience in hospital.
Image: Associate Professor Christina Ekegren
“Some of these devices are in place in other health and aged care settings. But it’s the integration of all of the technology, along with the integration of all of the data from the technology, that makes this project different,” explains Smart Ward Research Lead, Associate Professor Christina Ekegren from the Monash University Rehabilitation, Ageing and Independent Living Research Centre.
The Smart Ward is designed to capture information to improve patient care, safety, and experience through advanced technology. To address patient comfort, environmental sensors have been installed at every bedside to measure light, noise, temperature, and air quality.
A tag will be attached to patients’ identification wristbands, which will connect to Bluetooth low-energy sensors throughout the ward to monitor patient movement and location, which can improve safety and reduce complications. Radar sensors in patients’ rooms will detect patient events, location, and movements.
Data collected by the devices is stored securely and linked to patients’ medical records. This information may be used for research purposes, but only after all patient identifying information has been removed and appropriate ethics committee approval obtained.
As a physical activity researcher, A/Prof Ekegren says that her main interest is the localisationbased sensors. She explains that the use of traditional movement trackers is problematic in a hospital setting, as the devices need regular charging, downloading, and laborious input from staff to keep the devices working, and to provide access to the data.
“The most exciting thing for me is that it’s all going to be completely automated and passive,” A/Prof Ekegren says.
“So staff will still need to put the tag on upon admission. But that’s pretty much it.”
“It’s really hard to understand patient movement on a ward where everybody is so busy.
The nurses are very aware of what patients are doing most of the time, but not all of the time,” explains A/Prof Ekegren.
This unique combination of technologies is anticipated to help improve health outcomes by picking up data that indicates health conditions requiring healthcare interventions.
“We may be able to use that data to better predict who is at risk of functional decline, deconditioning, pressure injuries, and thrombosis,” explains A/Prof Ekegren.
“We’ll also be able to produce some clinical dashboards so that staff have a better understanding of how much, and where, patients are moving or not moving so they can intervene earlier.”
The Smart Ward also provides patients with entertainment and connectivity. Every patient has access to their own wallmounted touchscreen tablet, allowing them to make and receive video and phone calls, watch videos and slide shows, listen to the radio or music playlists, and play games.
There is also an electronic nurse call system, which will monitor patients’ use of the nurse call button.
The idea for the Smart Ward was led by Professor Terry Haines, Head of School, School of Primary and Allied Health Care, Monash University.

“The complexity of this project is like nothing I have ever experienced before, because we’ve had to involve so many different parts of the health service and university to make sure that what we’re doing is acceptable, feasible, legal, and ethical. And within budget.”
He assembled a group of clinical researchers – from many disciplines – who brainstormed which information would be interesting to capture in a hospital environment to improve outcomes for both patients and staff. With funding released by the Commonwealth Government for the project in early 2024, the Smart Ward has come into being incredibly quickly. “The project then went into overdrive, and has been in overdrive ever since,” A/Prof Ekegren says.
The Smart Ward is funded by the Commonwealth Government of Australia through the National Centre for Healthy Ageing, a collaboration between Peninsula Health and Monash University.
Image: Smart Ward technology in action at The Mornington Centre
Virtual reality application for adult dental treatment: a feasibility study
New research is testing how virtual reality (VR) can improve dental care and experiences for people of all ages and abilities.
Peninsula Health is proudly partnering with Monash University’s Rehabilitation, Ageing and Independent Living (RAIL) Research Centre, Opportunity Tech Lab, and the National Centre for Healthy Ageing (NCHA) to launch this pioneering initiative.
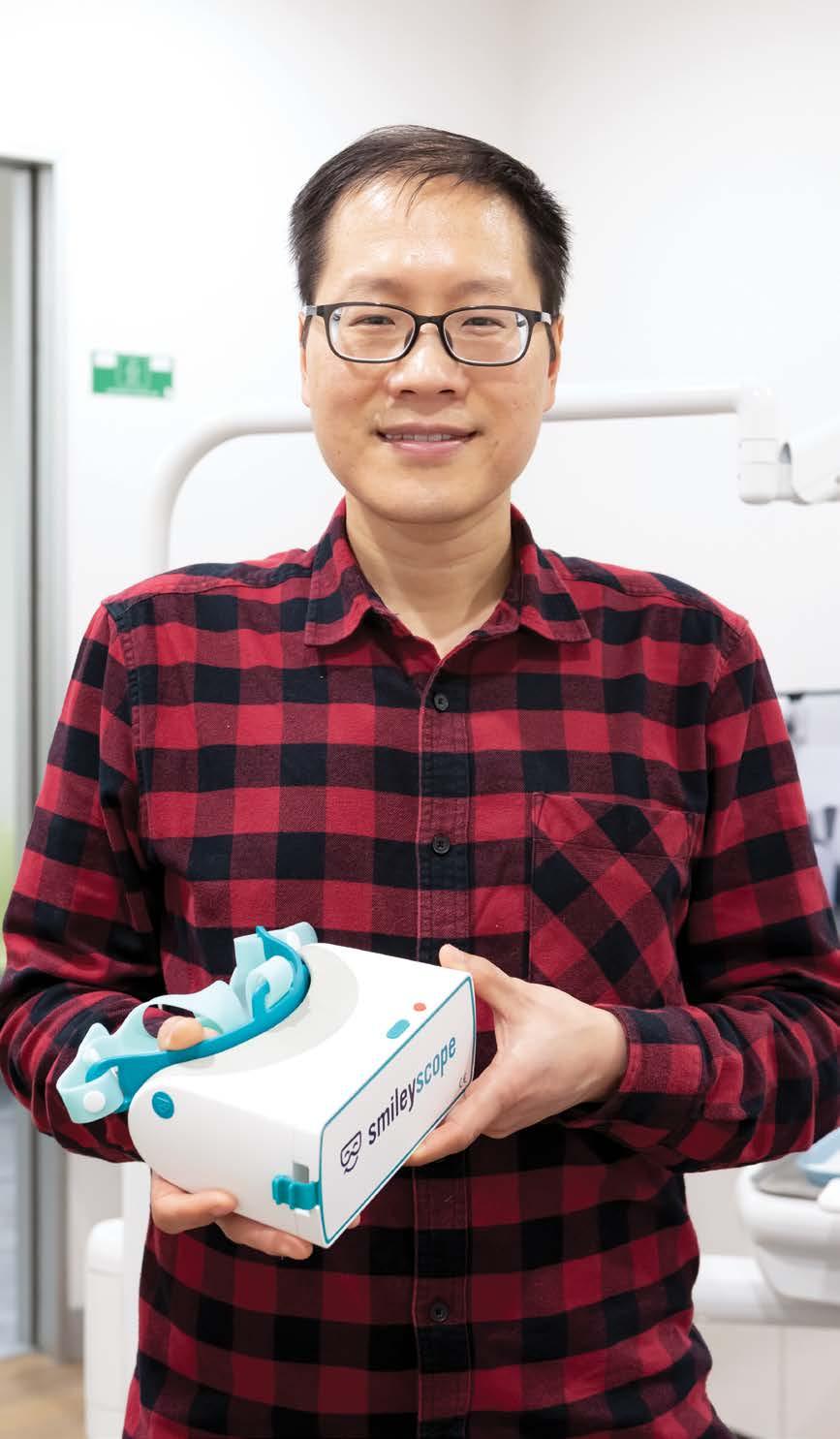
Supported by a research grant from the Monash Assistive Technology and Society Centre, the project is a bold step toward more inclusive, compassionate, and technologically advanced oral healthcare.
“By integrating VR, we’re not only aiming to reduce the anxiety some people experience in receiving general dental treatment, but to redefine what inclusive, person-centred, and technology-enabled healthcare can look like,” explains Associate Professor Libby Callaway, Independent Living Stream Lead, RAIL Research Centre and Associate Professor in Occupational Therapy, Monash University.
Common barriers to accessing dental services include heightened anxiety, sensory sensitivities, communication challenges, and limited availability of tailored care –often for children, older adults, and people who experience disability. These factors can lead to dental avoidance and poorer oral health outcomes.
Recognising this gap, an interdisciplinary research group from Monash University and the NCHA is partnering with Peninsula Health Dental Services to explore the use of SmileyScope™, a therapeutic VR headset, to reduce anxiety and enhance the dental experience for patients.

SmileyScope™ is a TGA-approved device that delivers calming, nature-based VR content designed to soothe patients during medical procedures. While it has been successfully used in hospital settings to reduce pain and distress, this study marks its first known application in public dental care.
“Emerging technologies have the real potential to change the way services are delivered to people of all ages and abilities,” says A/Prof Callaway.
“This trial of VR technology in general dental services is a unique opportunity to learn from dental patients and staff how VR-enabled treatment may be safely and effectively embedded in usual care.”
The pilot study involves 50 participants – including adults with disabilities and individuals ageing into disability – receiving dental care across Peninsula
Image: Dental Therapist Sarah Johnston with a consumer using the SmileyScope™ VR headset
Image: Dr Trung Dung Bui

Health’s Community Dental Service. Using a combination of quantitative and qualitative methods, the research team is assessing changes in patient anxiety levels, and the usability and acceptability of the VR technology in general dental care by both patients and dental staff. The goal is to evaluate whether VR can be safely and effectively integrated into routine dental care, improving patient comfort, and service delivery.
A key strength of the project is its commitment to co-design and lived experience. Disability advocate Mr Jonathan Bredin – an adult with cerebral palsy and extensive experience using assistive technology in everyday life – will offer important lived experience expertise as part of the project team.
Expected outcomes of the study include:
› a peer-reviewed publication presenting foundational evidence on the feasibility of VR in dental care for people with disabilities and individuals ageing into disability
› an implementation toolkit with costed solutions to common barriers, such as staff training and accessibility modifications
› evidence-based recommendations for implementing VR use in public dental services, with a focus on improving patient experiences.
His contributions include early feedback on approaches to engage people with disability in the VR pilot, consideration of graded approaches to the technology engagement, and advice on inclusive evaluation methods.
This will ensure the voices of people of all abilities are embedded throughout the research process.
“The project also aligns with national priorities in digital health and disability-inclusive service design, contributing to broader efforts to improve oral health outcomes,” explains Dr Trung Dung Bui, Research Fellow at the National Centre for Healthy Ageing.
“It exemplifies how targeted investment and collaboration can lead to meaningful change –not only for individuals but for the health system as a whole.”
The project also supports the development of future leaders in inclusive healthcare. Four Early Career Researchers from Monash University are actively involved, bringing expertise in medicine, health technology, economics, and information systems.
They are mentored by senior academics and Peninsula Health professionals, fostering interdisciplinary collaboration and building capacity in digital health innovation.
This initiative reflects Peninsula Health’s ongoing commitment to innovation in care and equity in service delivery. By embracing emerging technologies, driving new evidence to inform practice, and partnering with community voices, we are working to create a more inclusive health system, which is one that recognises and responds to the diverse needs of our population.

Image: Dr Rosie Dwyer
Better psychosocial care for older people in the Emergency Department
When a patient presents to the Emergency Department (ED), it’s vital to identify and treat their immediate needs. However, Emergency Physician and researcher Dr Rosie Dwyer has a hunch that there might be a different way to approach things – especially for older patients.
“ED traditionally has been a lot about rapidly treating a physical complaint, an injury or illness, resuscitation, procedures – things like that. And for a lot of these older people, that’s not necessarily what they need,” Dr Dwyer explains. “They need more comprehensive assessment, perhaps less invasive management, and more focus on their holistic care.”
Dr Dwyer’s research, Informed Psychosocial Care for Older People in an Emergency Setting, is one of the projects
spearheaded by the National Centre for Healthy Ageing (NCHA) through its Living Labs program. It’s an Australianfirst study exploring the relationship between symptoms of depression and subsequent emergency healthcare attendance in a population of older Australians.
“Older people are making up an increasing proportion of the patients who we see,” says Dr Dwyer. “They’re quite complex, they can be quite vulnerable, and often the care that we provide in the ED is not very well suited to them. A lot of the care can cause them more harm than good in some ways, and so that’s where I’ve tended to focus most of my research.”
Dr Dwyer also explains that older people can typically be more difficult to examine than their younger counterparts – they may be more stoic, more selfcontained, and less comfortable with speaking about their mental health. This can be difficult for staff to navigate in a busy emergency setting.
In order to find out more about older patients’ experiences in ED, Dr Dwyer and the research team began with an existing dataset from a national cohort of older people to identify the associations between common mental disorders and frequency of emergency care, and found that people who had higher symptoms of depression and anxiety were more likely to present to ED.
The research was further informed by health and administrative data from Peninsula Health to determine the local prevalence of common mental health disorders among ED patients.
The team then conducted qualitative interviews with patients and staff to explore how a person’s mental health may influence their presentation to the ED, how their experience of emergency care may affect their psychological and emotional wellbeing, and to find ways to better support people during their emergency care.
While Dr Dwyer has spent many years in the ED and had a strong sense that older patients could benefit from more psychosocial understanding, she was slightly surprised by some of the staff responses.
“I found the staff interviews quite interesting, in that [staff] really didn’t have a great understanding of a broad range of mental health concerns,” explains Dr Dwyer.
“In older people, some of the staff tended to fixate on conditions like delirium and dementia, but not really thinking about other conditions like anxiety or depression, which may actually be more prevalent and more of a concern.”
“That was eye opening for me, that there is a lot of work that needs to be done in terms of educating and upskilling staff so that we can provide better, more holistic care for people,”
Dr Dwyer adds.
The next step in the project involved Dr Dwyer and the research team partnering with Action Lab at Monash University to develop a digital solution.
The digital tool is designed to facilitate a more comprehensive psychosocial assessment of older people, involving some screening tools and questions about their social circumstances, as well as questions about what they’re experiencing currently while they’re waiting for care.
The suggestion is that the patient could complete the assessment while waiting in ED.
Dr Dwyer’s research team is now getting ready to launch a pilot program to test and implement the digital prototype.
“Given the time pressures on staff, a digital self-report tool may be a way that we can improve our assessment of these concerns, identify any highrisk features, and then also have it presented to clinicians so that they can include that in their management plans and discussions with the patient,” says Dr Dwyer.

Supporting inclusive clinical trial participation
Peninsula Health is one of six Victorian health services supported by TrialHub, an Australian-first pilot program launched by the Federal Government in 2020. TrialHub partners with outer metro, regional, and rural hospitals to establish independent and sustainable clinical trial units, improving access to potentially life-saving treatments for communities outside major cities.

TrialHub uses a ‘hub-and-spoke’ approach, with Alfred Health acting as the central ‘hub’ and partners like Peninsula Health as the ‘spokes’. This model provides support and networked expertise to build local capabilities and reduce barriers such as long-distance travel and time off work, which have historically limited access to clinical trials in regional and remote areas. TrialHub has recently shared two key resources with partner sites to support inclusive trial participation.
The Gift of Healing is a bespoke brochure designed to help Aboriginal and Torres Strait Islander communities better understand clinical trials. Developed over 18 months of consultation with First Nations researchers, medical students, and community members, the brochure features vibrant artwork by Dixon Patten, a proud Gunnai, Yorta Yorta, Gunditjmara, and Dhudhuroa man. The artwork reflects strength, resilience, and the power of community-led healing, and is now displayed across TrialHub partner sites.
TrialHub has also developed a clinical trial explainer video in partnership with members of culturally and linguistically diverse (CALD) communities. The video shows that clinical trials are open to everyone and helps to demystify the process for people from diverse backgrounds.
Peninsula Health’s Director of Research, Professor Velandai Srikanth says clinical trials are vital to patient care.
“We’ve been conducting clinical trials here for almost 40 years because they are the only way to find the next best treatment for our patients. All current medicines and treatments were once a clinical trial, but we’re always looking for the next best treatment for our patients.”
“Our goal at Peninsula Health is to ensure that every patient, regardless of their background, has equal access to the opportunities and benefits that clinical trials offer our community,” adds Professor Srikanth.
These resources are available to Peninsula Health through its partnership with TrialHub, reinforcing a shared commitment to improving access, understanding, and equity in clinical trials across Victoria.
Image: Artwork by Dixon Patten
Goal 4: Sustainability, through strong systems and infrastructure
We will grow our research maturity and sustainability through financial certainty, centralised systems and integrated use of health data.
New research to inform government policy related to healthy ageing
Australia’s aged care sector is facing a critical shortage of services and qualified health professionals. With Australia’s ageing population growing faster than ever, this shortage is set to intensify – posing serious risks to the quality and accessibility of care.
In response, a new federal Aged Care Act will take effect in November 2025, introducing major reforms aimed at helping older Australians maintain independence, with a stronger focus on in-home care and enhanced primary healthcare services. However, policymakers do not currently have access to robust evidence of the effectiveness of past and current in-home care policies, making it impossible to reliably forecast the impact of future policies.
To address this gap, Professor Nadine Andrew is set to lead a $1.5 million research project funded by the National Health and Medical Research Council (NHMRC) through its Ideas Grant scheme. In partnership with Peninsula Health and Monash University under the National Centre for Healthy Ageing, the four-year study will develop a comprehensive population
dataset to support rapid, reliable evaluation of past and present aged care policy and simulation of the effectiveness of future policies.
“Essentially, our aim is to provide evidence on the effectiveness of current and future federally funded policies related to ageing. We’re particularly focused on services delivered through general practitioners, such as chronic disease management
plans and medication management plans, as well as in-home care models like home care supports,” explains Professor Andrew.
The project will be rolled out in three phases.
Phase One will focus on developing a comprehensive population dataset for the entire Frankston-Mornington Peninsula region. This dataset will establish linkages between Electronic Health Record (EHR) data and relevant state, Commonwealth, and administrative datasets, enabling a more integrated and accurate view of population health.
“Importantly, the dataset will also be shaped by consumer lived experience,” adds Professor Andrew.

Image: Professor Nadine Andrew
“We’ll engage with consumers to understand factors that help them live well in the community. Important factors such as social supports, which are not readily available in the linked EHR and government datasets, will be generated through the application of artificial intelligence to clinical notes.”
Phase Two will focus on developing a new framework for the emulation of target trials involving complex interventions. This framework will then be applied to the linked population dataset.
“Target trial emulation is a relatively new and cutting-edge approach to data analysis,” explains Professor Andrew.

“It allows us to use all of our data within a structured framework to replicate the conditions of a clinical trial as closely as possible. This method has been shown to produce more robust and reliable evidence compared to many traditional approaches typically applied to observational data.”
As part of this process, Professor Andrew and her team will also develop a suite of tools and frameworks for application to observational data, similar to those used to uphold the level of rigour typically required in clinical trials.
Phase Three will culminate in the creation of a regularly updated, linked data asset. This resource will be used to evaluate emerging policies and simulate future Commonwealthfunded initiatives aimed at helping people remain living independently in the community.
“Our ultimate goal is to build a simulation platform that government agencies can use to test ideas and policies in a virtual environment,” says Professor Andrew.
“This would allow for evidenceinformed decision making before real-world implementation.”
“They’d be able to simulate a new policy, or a change to an existing one, using the dataset and see what impact it might have on the number of people transitioning to aged care as a result.”
Creating this platform will not only influence practice and policy, but it will also help align them with consumer preferences.
“We know that most older people want to stay in their own homes for as long as possible, with the right supports in place, and we’re working to make that achievable,” concludes Professor Andrew.
By understanding how to help people stay healthier for longer and remain living in the community, this project will advance multiple fields, including target trial emulation, data linkage, biostatistics, and policy evaluation, while delivering critical knowledge and realworld evidence to inform policy development for healthy ageing.
“For example, you could test what happens if the number of home care packages available across Australia is increased, and examine how that affects the proportion of people entering aged care. With the simulation platform, you’d be able to produce those insights before the policy is actually implemented.”
Identifying frailty earlier to improve outcomes for older people in hospital
The early identification and management of frailty is essential to prevent further decline and enhance the quality of life for older individuals in hospital settings –where the challenges and implications of frailty present unique complexities.
Frailty in these environments is often exacerbated by acute illnesses, surgical interventions, or other stressors that can precipitate rapid declines in health. Hospitalised patients who are frail are more likely to experience complications such as prolonged hospital stays, readmissions, or adverse outcomes like delirium and functional decline.
Frailty is a clinical syndrome characterised by a decline in physiological reserves and increased vulnerability to adverse health outcomes. Those experiencing frailty are at heightened risk for negative outcomes, such as falls, hospitalisation, disability, and mortality. Frailty and other negative outcomes are typically associated with ageing and are influenced by a combination of biological, psychological, and social factors. Frailty continues to be strongly related to functional impairment, institutionalisation, and increased healthcare utilisation.
To help address this, a study of the Electronic Frailty Index (eFI) – that uses routinely collected data from hospital Electronic Health Records (EHR) – is offering a promising solution.

This study aims to adapt, develop, and validate the eFI by utilising data from the National Centre for Healthy Ageing (NCHA) Data Platform, which includes hospital EHRs alongside other linked health datasets.
The study is using de-identified clinical and administrative data from older adults who attended Peninsula Health between 2015 and 2024. It will consist of more than 200,000 patients aged 60 years and over at the time of their hospital admission.
The exact sample size will be determined by data already available in the NCHA’s Healthy Ageing Data Platform, ensuring only those with sufficient information for frailty assessment are included.
Using routinely collected hospital admission data is an economical, systematic, and sustainable method for measuring frailty. The NCHA’s Healthy Ageing Data Platform contains a curated set of research-relevant data derived from multiple data sources within a large metropolitan health service. The primary purpose of the Platform is to support the development and evaluation of innovative research relevant to healthy ageing.
Professor Velandai Srikanth, Director of Research at Peninsula Health and Director of the National Centre for Healthy Ageing, is leading the study. He says that once developed,
the eFI will be specifically tailored for hospital use, ensuring practical applicability for frailty assessment in older inpatients.
“The eFI will provide evidencebased stratification of patients based on their frailty status, allowing for targeted interventions and improved management strategies to reduce adverse health outcomes such as readmissions, complications, and mortality,” explains Professor Srikanth.
“This tool is intended to be embedded within clinical workflows to support real-time decision-making and resource allocation in hospital settings.”
Dr Asmare Gelaw, the epidemiologist and data analyst on this project, says the team will follow 10 key steps to develop the eFI.
“These steps will help carefully select and refine the variables and health measures associated with frailty to ensure the index is both accurate and meaningful,” explains Dr Gelaw.
“Additionally, we are using natural language processing – a branch of artificial intelligence for automated analysis of narrative or unstructured text – to extract valuable information from unstructured data sources such as progress notes, discharge summaries, nursing notes, and allied health documentation.”
According to Dr Jessica Manzoni, Consultant Geriatrician and Orthogeriatric Clinical Lead at Peninsula Health, frailty is becoming an increasingly significant issue as our population ages.

Frailty is a clinical syndrome characterised by a decline in physiological reserves and increased vulnerability to adverse health outcomes, particulary among older adults.
“Frailty reduces a person’s ability to cope with illness or stress, and even minor injuries or illnesses can escalate when frailty is present, particularly in hospital settings,” says Dr Manzoni.
“We’re also seeing a rise in chronic disease, which compounds these challenges. Frail individuals are less able to manage daily activities, often leading to a reduced quality of life.”
From a hospital perspective, frailty contributes to longer stays, increased risk of complications, and greater reliance on institutional care.
“However, if we can identify frailty early, potentially through tools like the eFI, we can implement targeted strategies to mitigate risks, improve management, and enhance overall outcomes,” adds Dr Manzoni.
“This research lays the groundwork for a better understanding of frailty in hospitals and highlights the importance of early assessment to support preventative care.”
Image: Dr Asmare Gelaw

Using AI to diagnose dementia
Dementia is one of the most pressing public health challenges in Australia. The number of people living with the condition continues to increase due to our ageing population.
Dr Alicia Lu, geriatrician and PhD candidate, is investigating how artificial intelligence (AI) and data science methods can be applied to routinely collected electronic health record (EHR) data to support the identification of people who may be living with unrecognised dementia in an Australian hospital setting. Based at the National Centre for Healthy Ageing (NCHA), Dr Lu’s research draws on data from the Healthy Ageing Data Platform and focuses on Peninsula Health sites.
“If successful, this research could contribute to the development of decision-support tools that help hospital teams better identify people with dementia, especially those without a formal diagnosis,” explains Dr Lu.
“This may allow for more tailored hospital care pathways, such as prioritisation for geriatric medicine unit admission, appropriate room allocation, and targeted discharge planning.”
“The broader aim is to improve hospital care for people with dementia, reduce preventable harms, and facilitate timely referrals for further specialist assessment or communitybased supports,” says Dr Lu.
Although the prevalence of dementia is increasing, many individuals remain undiagnosed.
This may reflect the subtle nature of early cognitive changes, limited community awareness, or a lack of recognition in healthcare settings – especially where cognitive symptoms are not overt. People with dementia are at higher risk of adverse hospital outcomes (such as delirium), and without timely recognition, they may miss out on opportunities for appropriate care planning or specialist input.
Image: Dr Alicia Lu with a consumer Jean
A rapidly growing area of research looks at how we can improve detection of dementia using algorithms developed with routinely collected EHR data.
This approach recognises the practical challenges clinicians face in busy hospital environments, where dementia may not be easily detected due to limited time, competing priorities, or a lack of dementia-specific training.
This has been spurred by the growing amounts of EHR data available, as well as increasingly sophisticated data science and AI techniques that can unlock the potential of these large datasets. There are two key types of EHR data: structured data (e.g. vital signs, laboratory results) and unstructured data (e.g. admission notes, discharge summaries). While structured data has long been used in research, recent progress in natural language processing is enabling the extraction of meaningful insights from unstructured data, thus opening up new possibilities for dementia detection.
Through her research, Dr Lu aims to:
• systematically assess the quality and performance of existing models that use EHR data to detect dementia
• understand what matters to those who would use or be affected by these tools: clinicians, people with dementia and their carers, and the wider community
• develop and test new AI models that are specifically tailored to the Australian hospital context, with the ultimate goal of real-world implementation.

These aims will be achieved through four components:
› a systematic review of published studies that used EHR data to develop or validate models for detecting dementia
› an external validation study using the NCHA’s recently developed algorithm to identify patients with diagnosed dementia using EHR data, and testing how well this algorithm performs in a more recent, unseen patient cohort at Peninsula Health
› a model development study aimed specifically at detecting undiagnosed dementia by identifying a cohort of people with clinical indicators suggestive of dementia and experimenting with different types of variables
› a stakeholder perspectives study to develop models for real-world use, addressing the implementation gap. This includes conducting 30 interviews with clinicians, people with dementia, carers, and members of the public to explore priorities, concerns, and expectations for AI-based dementia detection.
“My PhD will explore how we can best utilise both structured and unstructured EHR data to develop algorithms capable of identifying people with undiagnosed dementia,” explains Dr Lu.
“This includes evaluating different modelling approaches and balancing accuracy with feasibility, interpretability, and clinical usefulness.”
“This study will help fill a major evidence gap in the Australian context, as it is one of the first projects nationally to focus on real-world AI model development for dementia detection using EHR data,” Dr Lu concludes.

Research Governance
Research
Operations Committee
Professor Velandai Srikanth (Chair)
Professor Nadine Andrew
Associate Professor Cathleen Aspinall
Dr Gabriel Blecher
Ms Lee-Anne Clavarino
Mr Scott Cripps
Ms Monica Finnigan
Professor Terry Haines
Associate Professor Mahesh Iddawela
Dr Nathan Johns
Dr Laura Jolliffe
Mr Nicholas Jones
Dr Nisha Khot
Professor David Langton
Professor Jamie Layland
Associate Professor Shyaman Menon
Professor Richard Newton
Dr Elisabeth Nye
Dr Karen O’Brien
Associate Professor Fiona Reed
Professor Warren Rozen
Dr Kerryn Rubin
Professor Ravi Tiruvoipati
Associate Professor Ashley Webb
Ms Libby Wilson
Human Research Ethics Committee
Dr Dilinie Herbert (Chair)
Dr Melanie Benson
Dr Rosamond Dwyer
Ms Joanna Green
Ms Jo Hansen
Mr Richard Ivice
Mr Cameron Marshman
Associate Professor Shyaman Menon
Ms Gillian Oates
Dr Meghan O’Brien
Ms Sharon O’Brien
Dr Stefanie Oliver
Professor Warren Rozen
Dr Babak Tamjid
Professor Ravi Tiruvoipati
Dr Vicky Tobin
Dr Michael Wang
Scientific Review Panel
Professor Nadine Andrew
Associate Professor Ernie Butler
Dr Taya Collyer
Dr Laura Jolliffe
Dr Chris Karayiannis
Dr Sam Leong
Dr David Snowdon
Projects approved by the Human Research Ethics Committee
› Allied health assistant care for patients with acute hip fracture and cognitive impairment: A feasibility randomised controlled trial
› Development and internal validation of a prognostic model to predict personcentred outcomes following ankle fracture in adults: A feasibility study
› Documenting the learning curve when learning the percutaneous needle fasciotomy (PNF) technique
› Enhancing informed consent competency in medical personnel through video-based education
› Establishing a molecular oncology care pathway at Peninsula Health
› Evaluation of psychology registrar program
› Exploring the attitudes and experiences of maternity services staff during the implementation of a publicly funded homebirth program
› Exploring health professions educators approaches and experiences of linking learners’ emotions to learning during simulation-based education debrief
› Identifying clients’ barriers and expectations of attending the multidisciplinary persistent pain management service
› International research database for extracorporeal support – INDEX study
› RAPID residue testing and monitoring
Projects approved by the Director of Research
› A clinical audit of management, follow up and outcomes of patients with non-muscle invasive bladder cancer
› Admission outcomes for patients with per rectum bleeding at Peninsula Health: A clinical audit
› A quality improvement project evaluating current cognitive monitoring practices for older adults receiving electroconvulsive therapy (ECT) at Peninsula Health, against best practice evidence-based standards
› A retrospective audit examining the timely and appropriate administration of solid oral dosage form (SODF) medications in patients with a speech pathologist determined altered swallowing status
› Allied health electronic health record workflow efficiencies project
› Analysis of Grade 1 Perugini score cardiac amyloidosis detected on PYP bone scans, and their progression to grade 2 & 3 transthyretintype cardiac amyloidosis and cardiovascular outcomes in a tertiary hospital
› Requests for voluntary assisted dying in the Palliative Care Unit
› Southern Melbourne Integrated Cancer Services and Peninsula Health – Care Plus Project
› Staff experiences, perceptions of care and communication regarding patient goals of care
› The routine use of bedside transthoracic echocardiography in the assessment and management of patients with atrial fibrillation in the emergency department
› Validation of entrustable professional activities (EPA) created for outreach pharmacy work at Peninsula Health’s community care program
› Appraisal of adequacy of post operative nausea and vomiting risk assessment/ management within the Frankston Hospital Anaesthetics Department
› Arteriosclerotic cardiovascular disease prevention in patients with end stage renal failure
› Assessing the clinical indications of PET scans and their role in inpatient management: A retrospective study at Frankston Hospital
› Audit of indications and complications following percutaneous cholecystostomy at Peninsula Health – II
› Audit of rates of urinary retention post intrathecal morphine in patients having major lower limb joint surgery
› Audit of rib fracture management
› Audit of treatment patterns of diverticulitis presenting to Frankston Hospital Acute General Surgical Unit – II
› Clinician feedback on consult geriatric service
› Communication skills workshop for interns: Qualitative and quantitative evaluation
› Comparative analysis of robotic assisted versus conventional total knee and hip arthroplasty in patients aged 70 and above
› Documenting the journey of patients with endometriosis and persistent pelvic pain who require ambulance service and emergency department attendance
› Does cool spray reduce local anaesthesia injection pain compared to no treatment prior to percutaneous needle fasciotomy treatment of Dupuytren’s disease?
› Enhancements to the allied health governance structure
› Evaluation of the management of patients with acute nonspecific lower back pain in the emergency department at a metropolitan hospital
› Evaluating psychotropic prescription and informed consent in delirium management for inpatients in a tertiary centre
› Evaluating the precision of word triggers in identifying cancer within histopathology reports from endoscopic biopsy procedures
› Evaluating the use of mechanical prophylaxis of venous thromboembolism at a major metropolitan hospital
› Evaluation of a pharmacy and nursing inter-professional education (IPE) program: Medication moments
› Evaluation of the management of asymptomatic bacteriuria (ASB) in rehabilitation units: Compliance with evidencebased guidelines
› Evaluation of the use of valproate for mental health disorders at a major metropolitan hospital in adults of reproductive potential
› Gender differences in hand injuries among Australian rules football players: An audit study
› Healthcare utilisation in older adults with new-onset epilepsy
› Hospital osteoporosis management for patients with hip fractures: Barriers and enablers
› Identifying barriers and enablers of direct referral to hand therapy at Peninsula Health: Right care, right patient, right time
› Impact of COVID-19 on elective melanoma excision: An audit cohort analysis
› Implementation of medication duplication alerts in the electronic health record system at a major metropolitan hospital
› Inter-rater reliability of the Clinical Frailty Scale between MET calls and ICU admission
› Introducing day-case haemorrhoidectomy in a Victorian public hospital
› Long-term outcomes of Bankhart v Latarjet procedures: A retrospective analysis of single-surgeon data on the Mornington Peninsula
› Microvascular assessment in clinical practice: Correlation with patient characteristics and assessment results
› NCHA data platform - data quality audit
› Outcomes of neoadjuvant therapy in early triple-negative and HER-2-positive breast cancer: A retrospective and prospective cohort study at Peninsula Health
› Outcomes of percutaneous needle fasciotomy in treating Dupuytren’s disease at Peninsula Health
› Outcomes of surgical retroareolar biopsy prior to nipple sparing mastectomy: A single institution experience
› Peninsula Health consult geriatric service pilot
› Peninsula Health GEDI (Geriatrician in ED initiative) pilot
› Perioperative analysis of ECGs and HbA1c at the Frankston Public Surgical Centre
› Physiotherapist-led shoulder arthroplasty follow-up
› Physiotherapy involvement in the management of patients with rib fractures at Frankston Hospital
› Predictors for the administration of multiple sedative agents in palliative sedation
› Predictors of discordance between CT coronary angiography and invasive coronary angiography: A retrospective study
› Prevalence of neurological complications in patients with varicella zoster virus in cerebrospinal fluid: A Peninsula Health study
› Proactive interventions in a hospital setting to transition patients using discontinuing insulin formulations
› Prophylactic ureteric stenting in colonic resections: Retrospective review of complication rates in a single institution
› Referral and attendance rates for pulmonary rehabilitation: A retrospective audit to explore reasons for non-referrals, non-attendance and non-adherence
› Retrospective cohort study: Effectiveness and safety of intra-operative methadone
› Safety of SABR (stereotactic ablative radiotherapy) without histological confirmation in stage 1 and 2 non-small cell lung cancer (NSCLC): A retrospective audit
› Sexual dysfunction in patients with liver cirrhosis
› ST segment elevation in aortic valve replacement: Lesion characteristics and outcomes
› Standardising preoperative frailty assessments of patients undergoing emergency laparotomy: An Australian retrospective study
› The accuracy of patientreported height, weight, and BMI in anaesthetic preadmission questionnaires
› The effect of increasing parathyroid hormone, calcium or corrected calcium on the identification of a parathyroid adenoma
› The Southeast Melbourne Primary Care Integration Project: Understanding the GP-specialist referral pathway
› The usage patterns and complication rates associated with supraglottic airway during planned procedures under general anaesthesia
› The validity and accuracy of plain film rotation of the knee
› Timing of prophylactic antibiotic administration in relation to the induction of anaesthesia
› Treatment of necrotizing pancreatitis
› Understanding environmental conditions on the Peninsula Health Smart Ward
› Understanding the patient flow and outcomes for those who attend the Emergency Department via ambulance
› Using consumer involvement in preparing physiotherapy students for communication with patients at orientation to placement
Multisite projects authorised
› A phase 2a, randomized, double-blind, parallel-group, placebo-controlled study to evaluate the efficacy, safety, and tolerability of fexlamose (AER-01) inhalation solution in the treatment of adults with moderate to severe chronic obstructive pulmonary disease
› A phase 3, randomised, open-label study to compare the efficacy and safety of adjuvant MK-2870 in combination with pembrolizumab (MK3475) versus treatment of physician’s choice (TPC) in participants with triplenegative breast cancer (TNBC) who received neoadjuvant therapy and did not achieve a pathological complete response (pCR) at surgery
› A phase 3, randomized, double-blind, multicenter study of MK-1084 in combination with pembrolizumab compared with pembrolizumab plus placebo as firstline treatment of participants with KRAS G12C, mutant, metastatic NSCLC with PD-L1 TPS ≥50%
› A phase III, open-label, randomised study to assess the efficacy and safety of camizestrant (AZD9833, a next generation, oral selective estrogen receptor degrader) versus standard endocrine therapy (aromatase inhibitor or tamoxifen) as adjuvant treatment for patients with ER+/HER2- early breast cancer and an intermediate-high or high risk of recurrence who have completed definitive locoregional treatment and have no evidence of disease
› A randomized, double-blind, placebo-controlled, parallel, 4-arm dose ranging study of the safety and efficacy of nalbuphine extendedrelease tablets (NAL ER) for the treatment of cough in idiopathic pulmonary fibrosis (IPF)
› A randomized, double-blind, phase 3 trial of adagrasib plus pembrolizumab plus chemotherapy vs. placebo plus pembrolizumab plus chemotherapy in participants with previously untreated, locally advanced or metastatic non-squamous non-small cell lung cancer with KRAS G12C mutation
› A randomized, doubleblinded, multicentre, phase 3 clinical study of HLX22 (recombinant humanized anti-HER2 monoclonal antibody injection) in combination with trastuzumab and chemotherapy (XELOX) versus trastuzumab and chemotherapy (XELOX) with or without pembrolizumab for the first line treatment of locally advanced or metastatic gastroesophageal junction and gastric cancer
› A randomized, phase 3, open-label study to evaluate SGN-B6A compared with docetaxel in adult subjects with previously treated nonsmall cell lung cancer
› A retrospective multicentre audit on adult presentations of symptomatic Meckel’s diverticulum
› Acceptance and Commitment Workplace Training: Evaluation of a secondary prevention initiative
› An interventional, open-label, randomized, multicentre, phase 2 study of PF07220060 plus letrozole compared to letrozole alone in postmenopausal women 18 years or older with hormone receptor-positive, HER2negative breast cancer in the neoadjuvant setting
› Enterobacter species whole genome sequencing project
› Establishing the quality of home-based services on stroke survivor outcomes and quality of life
› NEt ultrafiltration prescription and targeting versus usual NEt ultrafiltration during continuous renal replacement therapy
› Personalised exercise rehabilitation for people with multimorbidity
› A phase 1/2 study to evaluate the safety and efficacy of MK-2870 monotherapy or in combination with other anticancer agents in gastrointestinal cancers
› A phase II randomised, noncomparative, 2-arm trial of neoadjuvant chemotherapy + either olaparib or olaparib + durvalumab in young premenopausal women with HRD-enriched HR+ HER2- early breast cancer
› Supplemental jejunal feeding to improve quality of life
› Targeted approach for preventing pulmonary and extra-pulmonary traits
Grants awarded
Primary Investigator Grants
Dr Marianne Coleman
$399,000
Designing a dementia-friendly eyecare pathway to help people with dementia, Dementia Australia
Dr Joanne Lundy
$125,000
Establishing a Molecular Oncology Care Pathway at Peninsula Health, Southern Melbourne Integrated Cancer Service
Dr David Snowdon
$24,554
Allied health assistant rehabilitation of people with acute hip fracture and cognitive impairment: a feasibility randomized controlled trial, La Trobe University
Co-investigator Grants
A/Prof Mahesh Iddawela
$359,000
Medication education and supportive care for rural cancer patients prescribed oral anti-cancer medicines, Cancer Council Victoria
Dr Laura Jolliffe
US$17,500
Comprehensive action for rehabilitation excellence: an implementation project –The CAREMAP Project, World Stroke Organisation Futures Leaders
Dr Oliver Klein
$5,000,000
Identifying and overcoming mechanisms of immune evasion in cancer, National Health and Medical Research Council
A/Prof Samantha Sevenhuysen, Ms Joy Davis
$30,000
Augmenting the debrief of emergency resuscitation in-situ simulation utilising artificial intelligence, Laerdal Foundation
Dr David Snowdon
$1,469,063
WaitLESS: Applying data-driven, evidence-based principles to reduce waiting lists in specialist clinics, NHMRC
Professor Velandai Srikanth
$2,999,830
Strategic development of real-time frailty monitoring technology to improve care for older Australians, Medical Research Future Fund
$2,799,901
TRANSFORM: Transitions and reform for seamless multidisciplinary care, Medical Research Future Fund
Organisation-wide Clinical Trial Income
$1,650,000
Celebrating Research 2024
Prize Winners
Presentation Session 1
Best Presentation by an Experienced Researcher
Ms Martha Turek & Ms Cathy Halmarick –Pharmacy & Women’s Services
Retrospective evaluation of methoxyflurane effectiveness and tolerability for outpatient intrauterine device insertion
Best Presentation by an Early Researcher
Ms Catherine Devanny – National Centre for Healthy Ageing
Using co-design to improve access to rehabilitation for people with dementia
Presentation Session 2
Best Presentation by an Experienced Researcher
Dr Alison Carver – National Centre for Healthy Ageing
Associations of neighbourhood air pollution and greenery with unplanned hospital admissions related to cardio metabolic disease
Best Presentation by an Early Researcher
Dr Joel van Weel – Geriatric Medicine
Persistent pain and serious falls in healthy older Australians
Keynote Speakers
Professor Justine Naylor
Conjoint Professor, Faculty of Medicine & Health, University of New South Wales
Senior Principal Research Fellow in Orthopaedics , South West Sydney Local Health District (Some) things we know and (some) things we don’t know for some orthopaedic models of care
Dr Margot Lodge
Consultant Geriatrician and Clinical Lead Geriatric Trauma Service, The Alfred
Making innovation a reality: Implementation science and models of care for older people
Poster Competition
1st Prize
Ms Man Chun Chan – Pharmacy Department
To evaluate the provision of naloxone on discharge for patients from a metropolitan hospital
2nd Prize
Mr Javier Araujo Rodriguez – Pharmacy Department
A study of patient management post-splenectomy
3rd Prize
Ms Martha Turek & Ms Cathy Halmarick –Pharmacy & Women’s Services
Retrospective evaluation of methoxyflurane effectiveness and tolerability for outpatient intrauterine device insertion
Publications
› Abhinav, S., Ishith, S., Bryan, L., Roberto, C., & Rozen, W. M. (2024). Ethical issues of artificial intelligence in plastic surgery: a narrative review. Plastic and Aesthetic Research, 11(58).
https://doi.org/10.20517/23479264.2024.108
› Anthony, O. D., Seth, I., & Rozen, W. M. (2025). Concentration of povidone-iodine pocket irrigation in implant-based breast surgery: a scoping review. Aesthetic Plastic Surgery, 49(11), 3067–3080.
https://doi.org/10.1007/s00266-025-04660-y
› Anton, A., Hutchinson, R., Hovens, C. M., Christie, M., Ryan, A., Gibbs, P., Costello, A., Peters, J., Neeson, P. J., Corcoran, N. M., & Tran, B. (2024). An immune suppressive tumor microenvironment in primary prostate cancer promotes tumor immune escape. PLOS ONE, 19(11), e0301943. https://doi.org/10.1371/journal.pone.0301943
› Bange, J., Gao, W., & Crawford, K. (2025). Graduate nurses’ experience of support, training, and education during the COVID-19 pandemic: a qualitative study. Collegian, 32(2), 120–127. https://doi.org/10.1016/jcolegn.2025.02.002
› Barnes, E., Zhao, P., Udy, A., Nguyen, N., & Burrell, A. (2025). Outcomes of pregnant and post-partum patients admitted to the intensive care unit with COVID-19 in Australia: an analysis of SPRINT-SARI Australia. Australian and New Zealand Journal of Obstetrics and Gynaecology, 65(3), 372–381. https://doi.org/10.1111/ajo.13908
› Bell, J. S., Brennan, S., Patterson, A., & Srikanth, V. (2025). Closing the evidence-practice gap in dementia: two new national guidelines. Age and Ageing, 54(1), afaf005. https://doi.org/10.1093/ageing/afaf005
› Benetti, C., Whitehead, R., & Hopkins, L. (2024). ‘I feel like they understand me a bit more’: the experiences of young people with borderline personality disorder following their parents taking part in a mentalisation-based intervention for parents and carers (MBT-FACTS). Journal of Family Therapy, 46(4), 406–422. https://doi.org/10.1111/1467-6427.1247
› 0Birhanu, M. M., Zengin, A., Evans, R. G., Kim, J., Olaiya, M. T., Riddell, M. A., Kalyanram, K., Kartik, K., Suresh, O., Thomas, N., Srikanth, V. K., & Thrift, A. G. (2025). Comparison of laboratory-based and non-laboratory-based cardiovascular risk prediction tools in rural India. Tropical Medicine and International Health, 30(1), 57–64. https://doi. org/10.1111/tmi.14069
› Bonavia, W., Ling, R. R., Tiruvoipati, R., Ponnapa Reddy, M., Pilcher, D., & Subramaniam, A. (2025). The interplay between frailty status and persistent critical illness on the outcomes of patients with critical COVID-19: a populationbased retrospective cohort study. Australian Critical Care, 38(2).
https://doi.org/10.1016/j.aucc.2024.09.013
› Bonnamy, J., Bugeja, L., Morphet, J., Russo, P. L., & Brand, G. (2024). Transforming researchers into writers through a series of semi-structured writing retreats: a mixed methods study. BMC Nursing, 23(1), 611. https://doi.org/10.1186/s12912-024-02261-9
› Bonnamy, J., Calvert, S., Bennett, C., Dart, J., Molloy, R., & Brand, G. (2025). Students’ perspectives from co-designed, lived experience eating disorders education: a qualitative inquiry. Nurse Education Today 144, Article 106412. https://doi.org/10.1016/j.nedt.2024.106412
› Bonnamy, J., Carr, B., Lazarus, M. D., & Connell, C. (2025). Survey sabotage: Insights into reducing the risk of fraudulent responses in online surveys. Anatomical Sciences Education, 18(8), 767–773. https://doi.org/10.1002/ase.70015
› Bonnamy, J., Levett-Jones, T., Carr, B., Lokmic-Tomkins, Z., Maguire, J., Catling, C., Pich, J., Fields, L., & Brand, G. (2024). Australian and New Zealand nursing and midwifery educators’ planetary health knowledge, views, confidence and teaching practices: a descriptive survey study. Journal of Advanced Nursing. https://doi. org/10.1111/jan.16317
› Brand, G., Sheers, C., Hansen, A., Stephens, G., Dart, J., Shannon, B., & Bonnamy, J. (2025). How to codesign education with healthcare consumers. The Clinical Teacher, 22(2), e70039. https://doi. org/10.1111/tct.70039
› Brijnath, B., Cavuoto, M. G., Feldman, P., Dow, B., Antoniades, J., Ostaszkiewicz, J., Nakrem, S., Stevens, C., Reyes, P., Renshaw, G., Peters, M. D. J., Gilbert, A., Manias, E., Mortimer, D., Enticott, J., Cooper, C., Durston, C., Appleton, B., O’Brien, M., & Markusevska, S. (2025). Codesigning training for health providers to improve detection and response to elder abuse. The Gerontologist, 65(4). https://doi.org/10.1093/geront/gnae153
› Brown, A., Sakowski, S. A., Moran, C., Koubek, E. J., Srikanth, V. K., Zhao, L., Collyer, T., Adamson, C. L., Northam, E. A., Beare, R., Cameron, F. J., & Feldman, E. L. (2025). Identifying lifelong factors that impact brain health and functional outcomes in adults with childhood-onset type 1 diabetes: the cognition and longitudinal assessments of risk factors over 30 years (CLARiFY) - diabetes complications study protocol. BMJ Open, 15(6), e105887. https://doi.org/10.1136/bmjopen-2025-105887
› Burgess, T., Wegener, E., McClelland, B., HunterSmith, D., Werker, P. M. N., & Martin, J. (2025). Adverse events after adjuvant radiation therapy for Dupuytren’s disease in the DEPART randomized trial. Journal of Hand Surgery (European Volume), 50(7), 891–897. https://doi.org/10.1177/17531934251321393
› Burke, K. L. A., Snowdon, D. A., Milne, S. C., & Farlie, M. K. (2025). Exploring physiotherapists’ perspectives of group clinical supervision effectiveness for aquatic physiotherapy skill development: a qualitative study. Physiotherapy Research International, 30(2), e70044. https://doi.org/10.1002/pri.70044
› Callisaya, M. L., Piguet, O., Munroe, M., De Araújo, R. C., O’Bree, B., & Srikanth, V. K. (2025). Associations between dual-task walking and cognitive impairment in people attending a cognitive diagnostic clinic. Australasian Journal on Ageing, 44(1), e13372. https://doi.org/10.1111/ajag.13372
› Carver, A., Rachele, J. N., Sugiyama, T., Corti, B. G., Burton, N. W., & Turrell, G. (2024). Public greenspace and mental wellbeing among mid-older aged adults: findings from the HABITAT longitudinal study. Health & Place, 89, Article 103311 https://doi.org/10.1016/j.healthplace.2024.103311
› Ceccaroni, A., Cuomo, R., Pentangelo, P., Gentile, A., Marra, C., Rozen, W. M., Seth, I., Lim, B., & Alfano, C. (2024). Exploring reverse sural flap necrosis in lupus-like syndrome: challenges and strategies in lower limb reconstruction - A case presentation. Medicina, 60(12), 2053. https://doi.org/10.3390/medicina60122053
› Cevik, J., Rajaram, R., Pollock, M., Seth, I., & Rozen, W. M. (2025). Collagenase Clostridium histolyticum for Dupuytren’s disease: a comprehensive systematic review and comparative analysis against percutaneous needle aponeurotomy and limited fasciectomy. Journal of Plastic Surgery and Hand Surgery, 60, 27–34. https://doi.org/10.2340/jphs.v60.42750
› Cevik, J., Rostek, M., & Rozen, W. M. (2024). Anomalous anatomic variation of an absent deep inferior epigastric artery: implications for autologous breast reconstruction. Surgical and Radiologic Anatomy, 46(10), 1683–1686. https://doi.org/10.1007/s00276-024-03441-7
› Chua, M., Ratnagandhi, A., Seth, I., Lim, B., Cevik, J., & Rozen, W. M. (2024). The evidence for perioperative anesthetic techniques in the prevention of new-onset or recurrent complex regional pain syndrome in hand surgery. Journal of Personalized Medicine, 14(8), 825. https://doi.org/10.3390/jpm14080825
› Collins, I. M., Freeman, J., Ludowyk, J., McDonough, J., Ridgwell, J., Buzza, M., Corcoran, N., Campbell, D., & Thomas, B. (2025). Development of a virtual multidisciplinary meeting framework for less common cancers. Internal Medicine Journal, 55(2), 313–315. https://doi.org/10.1111/imj.16610
› Collins, M., Higgins, L., McAlister, S., & McGain, F. (2025). Siloed thinking: the case for integrating economic and environmental analysis in critical care. Critical Care and Resuscitation, 27(2), 100111. https://doi.org/10.1016/j.ccrj.2025.100111
› Collyer, T. A., Liu, M., Beare, R., Andrew, N. E., Ung, D., Carver, A., Ilomaki, J., Bell, J. S., Thrift, A. G., Rocca, W. A., St Sauver, J. L., Lu, A., Siostrom, K., Moran, C., Roberts, H., Chong, T. T., Murray, A., Ravipati, T., O’Bree, B., & Srikanth, V. K. (2025). Dual-stream algorithms for dementia detection: harnessing structured and unstructured electronic health record data, a novel approach to prevalence estimation. Alzheimer’s & Dementia, 21(5), e70132. https://doi.org/10.1002/alz.70132
› Colombo, N., Biagioli, E., Harano, K., Galli, F., Hudson, E., Antill, Y., Choi, C. H., Rabaglio, M., Marmé, F., Marth, C., Parma, G., Fariñas-Madrid, L., Nishio, S., Allan, K., Lee, Y. C., Piovano, E., Pardo, B., Nakagawa, S., McQueen, J., & Barretina Ginesta, M. P. (2024). Atezolizumab and chemotherapy for advanced or recurrent endometrial cancer (AtTEnd): a randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet Oncology, 25(9), 1135–1146. https://doi.org/10.1016/S1470-2045(24)00334-6
› Courneya, K. S., Vardy, J. L., O’Callaghan, C. J., Gill, S., Friedenreich, C. M., Wong, R. K. S., Dhillon, H. M., Coyle, V., Chua, N. S., Jonker, D. J., Beale, P. J., Haider, K., Tang, P. A., Bonaventura, T., Wong, R., Lim, H. J., Burge, M. E., Hubay, S., Sanatani, M., & Booth, C. M. (2025). Structured exercise after adjuvant chemotherapy for colon cancer. The New England Journal of Medicine, 393(1), 13–25. https://doi.org/10.1056/NEJMoa2502760
› Cunningham, C., Broadbear, J. H., Rajaram, J., Rao, S., Newton, R., & Galligan, R. (2025). Toward integrated treatment for co-occurring borderline personality disorder and eating disorders: a clinician perspective. International Journal of Eating Disorders, 58(5), 917–925. https://doi.org/10.1002/eat.24397
› Cuomo, R., Seth, I., Marcaccini, G., Lu, P. Y. J., Rozen, W. M., & O’Brien, D. P. (2025). Atypical Mycobacterium ulcerans infection with skip lesions in a 68-year-old male: a rare case and comprehensive literature review. Journal of Clinical Medicine, 14(11), 3853. https://doi.org/10.3390/jcm14113853
› Cuomo, R., Seth, I., & Rozen, W. M. (2025). Answer to: Commentary on “Can AI answer my questions? Utilizing artificial intelligence in the perioperative assessment for abdominoplasty patients.”
Aesthetic Plastic Surgery, 49, Article 04812. https://doi.org/10.1007/s00266-025-04812-0
› Dalli, L., Kilkenny, M. F., Olaiya, M. T., Ung, D., Kim, J., Churilov, L., Cadilhac, D. A., Sundararajan, V., Thrift, A. G., Nelson, M. R., Lannin, N. A., Barnden, R., Srikanth, V. K., & Andrew, N. E. (2025). Chronic disease management to enhance medication adherence trajectories in long-term survivors of stroke: a population-based cohort study. Pharmacoepidemiology and Drug Safety, 34(5), e70148. https://doi.org/10.1002/pds.70148
› Daneman, N., Rishu, A., Pinto, R., Rogers, B. A., Shehabi, Y., Parke, R., Cook, D., Arabi, Y., Muscedere, J., Reynolds, S., Hall, R., Dwivedi, D. B., McArthur, C., McGuinness, S., Yahav, D., Coburn, B., Geagea, A., Das, P., Shin, P., & Fowler, R. A. (2025). Antibiotic treatment for 7 versus 14 days in patients with bloodstream infections. The New England Journal of Medicine, 392(11), 1065–1078. https://doi.org/10.1056/NEJMoa2404991
› Dang, Q. M., Psaltis, P. J., Burgess, S., Chandrasekhar, J., Mukherjee, S., Kritharides, L., Jepson, N., Fairley, S., Ihdayhid, A., Layland, J., Szirt, R., El-Jack, S., Puri, A., Davis, E., Shiekh, I., Arnold, R., Watts, M., Marathe, J., Bhagwandeen, R., & Zaman, S. (2025). The Australian–New Zealand spontaneous coronary artery dissection cohort study: predictors of major adverse cardiovascular events and recurrence. European Heart Journal, 46(21), 2012–2023. https://doi.org/10.1093/eurheartj/ehaf097
› Dawes, P., Reeves, D., Yeung, W. K., Holland, F., Charalambous, A. P., David, R., Helmer, C., Keay, L., Kumaran, S., Leighton, R. E., Little, J. A., Martins, R. N., Piano, M., Politis, A., Pye, A., Robinson, G. A., Russell, G., Sheikh, S., Sohrabi, H. R., & Leroi, I. (2025). Development and validation of the Montreal Cognitive Assessment for people with vision impairment (MoCA-VI). Psychological Assessment, 37(3), 114–122. https://doi.org/10.1037/pas0001357
› Fandler-Höfler, S., Eppinger, S., Ambler, G., Nash, P., Kneihsl, M., Lee, K. J., Lim, J. S., Shiozawa, M., Koga, M., Li, L., Lovelock, C., Chabriat, H., Hennerici, M., Wong, Y. K., Mak, H. K. F., Prats-Sanchez, L., Martínez-Domeño, A., Inamura, S., Yoshifuji, K., & Gattringer, T. (2024). Sex differences in frequency, severity, and distribution of cerebral microbleeds. JAMA Network Open, 7(10), e2439571. https://doi.org/10.1001 jamanetworkopen.2024.39571
› Farlie, M. K., Coventry, J., Foo, J., Sevenhuysen, S., Shannon, B., Williams, C. M., Maloney, S., & Matthews, K. (2025). “We might be put into situations we are uncomfortable with, but not exactly told how to deal with them”: health professional students’ experiences questioning low-value care practices during work-integrated learning. Anatomical Sciences Education https://doi.org/10.1002/ase.70054
› Fiolet, A. T. L., Poorthuis, M. H. F., Opstal, T. S. J., Amarenco, P., Boczar, K. E., Buysschaert, I., Budgeon, C., Chan, N. C., Cornel, J. H., Jolly, S. S., Layland, J., Lemmens, R., Mewton, N., Nidorf, S. M., Pascual-Figal, D. A., Price, C., Shah, B., Tardif, J. C., Thompson, P. L., & Kelly, P. J. (2025). Colchicine for secondary prevention of ischaemic stroke and atherosclerotic events: a meta-analysis of randomised trials. eClinicalMedicine, 76, Article 102835. https://doi.org/10.1016/j.eclinm.2024.102835
› Foo, C. T., Langton, D., Donovan, G. M., Thompson, B. R., Noble, P. B., & Thien, F. (2025). Assessment of ventilation heterogeneity in severe asthma using phase-resolved functional lung magnetic resonance imaging. Physiological Reports, 13(12), e70423. https://doi.org/10.14814/phy2.70423
› Foo, C. T., Langton, D., & Thien, F. (2024). A case series of patients undergoing bronchial thermoplasty a second time for severe asthma. Journal of Asthma and Allergy, 17, 1239–1245. https://doi.org/10.2147/JAA.S492730
› Ford, T., Zeitz, C., Spiro, J., Yong, A., Layland, J., Watts, M., Chan, W., Girolamo, O., Marathe, J. A., Negishi, K., Sidharta, S., Singh, K., Tavella, R., Farouque, O., Khor, L., Ooi, E. L., La, S., Lau, J. K., Montarello, N. J., & Beltrame, J. F. (2025). Functional coronary angiography for the diagnosis of coronary vasomotor disorders. Heart, Lung and Circulation, 34(9), e89–e103. https://doi.org/10.1016/j.hlc.2024.09.012
› Francene, K., Warren, R., Ishith, S., & Roberto, C. (2024). Exploring the efficacy of negative pressure wound therapy in the management of Mycobacterium ulcerans wounds: a comprehensive literature review. Plastic and Aesthetic Research, 11(43). https://doi.org/10.20517/2347-9264.2024.26
› Furrer, M. A., Sathianathen, N. J., Mulholland, C. J., Papa, N., Katsios, A., Soliman, C., Lawrentschuk, N., Peters, J. S., Zargar, H., Costello, A. J., Hovens, C. M., Liodakis, P., Bishop, C., Rao, R., Tong, R., Steiner, D., Murphy, D. G., Moon, D., Thomas, B. C., & Corcoran, N. (2025). Pelvic lymph node dissection in prostate cancer: is it really necessary? A multicentric longitudinal study assessing oncological outcomes in patients with prostate cancer undergoing pelvic lymph node dissection vs radical prostatectomy only. The Journal of Urology, 214(2), 188–196. https://doi.org/10.1097/ju.0000000000004587
› Girard, N., Burotto, M., Paz-Ares, L. G., Reck, M., Schenker, M., Lingua, A., Orlandi, F. J., Naidoo, J., Beardsley, E. K., Velcheti, V., Martinengo, G. L., Felip, E., Zhang, Y., Kasbekar, P., Chowdhury, M., Spires, T., Tendolkar, A., & Cobo Dols, M. (2024). LBA53 Nivolumab (NIVO) plus relatlimab with platinum-doublet chemotherapy (PDCT) vs NIVO + PDCT as first-line (1L) treatment (tx) for stage IV or recurrent NSCLC: results from the randomized phase II RELATIVITY-104 study.
Annals of Oncology, 35(Suppl 2), S1243–S1244. https://doi.org/10.1016/j.annonc.2024.08.2295
› Gong, W., Wang, J., Deng, J., Chen, J., Zhu, Z., Seth, I., Zhang, B., Wang, X., Yang, J., Du, L., Xu, X., & He, X. (2024). Quantification of fundus tessellation reflects early myopic maculopathy in a largescale population of children and adolescents. Translational Vision Science & Technology, 13(6), Article 22. https://doi.org/10.1167/tvst.13.6.22
› Gupta, S., Tiruvoipati, R., Balachandran, M., Bolton, G., Pratt, N., Molloy, J., Paul, E., & Irving, A. (2025). A propensity matched cost analysis of medical emergency team calls led by nurse practitioners versus intensive care registrars. Intensive & Critical Care Nursing, 86, 103819. https://doi.org/10.1016/j.iccn.2024.103819
› Gurteen, H., Toomey, M., Franco, B., Bennett, R., Cenin, D., El-Saifi, N., Ferguson, M., Gu, Y., Heine, C., Keay, L., Kumaran, S., Lenzen, S., Leroi, I., Lowthian, J., Meyer, C., Mitchell, L., Newall, J., Pachana, N., Piano, M., & Dawes, P. (2025). Protocol for the process evaluation of the SENSE-Cog sensory support intervention field trial to improve quality of life for older people receiving home care in Australia. Health Expectations, 28(3), e70305. https://doi.org/10.1111/hex.70305
› Hettiarachchi Senarath, G. M., Delir Haghighi, P., Bai, L., Shannon, M. M., Andrew, N. E., Srikanth, V., Snowdon, D. A., & O’Connor, D. A. (2024). Barriers and facilitators to the uptake of electronic collection and use of patient-reported measures in routine care of older adults: a systematic review with qualitative evidence synthesis. JAMIA Open, 7(3), ooae068. https://doi.org/10.1093/jamiaopen/ooae068
› Homewood, D., Keane, K., Haridy, J., Valaydon, Z., Manning, T., Crowe, J., Tse, E., Iyngkaran, G., & Corcoran, N. (2024). Updates in digital shared care: launching into the 21st century. Australian Journal of General Practice, 53(11), 872–878. https://doi.org/10.31128/AJGP-10-23-7005
› Homewood, D., Fay, T., Tan, N., Silagy, A., Corcoran, N. M., Lawrentschuk, N., & Agarwal, D. (2024). Advances in sliding clip renorrhaphy for partial nephrectomy.
Nature Reviews Urology, 21, 703–704. https://doi.org/10.1038/s41585-024-00906-7
› Homewood, D., McDonald, J., Valaydon, Z., Ogluszko, C., Sukocheva, O., Tse, E., Corcoran, N., & Iyngkaran, G. (2024). eHealth platforms facilitate prostate cancer shared care: a systematic review. Healthcare, 12(17), 1768. https://doi.org/10.3390/healthcare12171768
› Homewood, D., Tan, N., Fay, T., Silagy, A., Lawrentschuk, N., Corcoran, N. M., & Agarwal, D. (2025). An overview of renorrhaphy techniques for partial nephrectomy.
International Journal of Urology, 32(4), 329–340. https://doi.org/10.1111/iju.15658
› Huhtanen, A., Mathew, A., Lewis, C., Martin, T., Piano, M., & Hui, F. (2025). Evaluating a collaborative paediatric eye-care model between optometry and ophthalmology: a clinical audit.
Clinical and Experimental Optometry, 1–5. https://doi.org/10.1080/08164622.2025.2460623
› Ishith, S., Bryan, L., Yi, X., Richard, J. R., Roberto, C., & Warren, M. R. (2025). Artificial intelligence versus human researcher performance for systematic literature searches: a study focusing on the surgical management of base of thumb arthritis. Plastic and Aesthetic Research, 12, Article 1. https://doi.org/10.20517/2347-9264.2024.99
› Ishith, S., Damien, G., Bryan, L., Jevan, C., Gabriella, B., Yi, X., Gianluca, M., Warren, M. R., & Roberto, C. (2024). Advancements, applications, and safety of negative pressure wound therapy: a comprehensive review of its impact on wound outcomes.
Plastic and Aesthetic Research, 11, Article 29. https://doi.org/10.20517/2347-9264.2024.05
› Janssens, S., & Marshall, S. (2024). Leadership in emergency teams: time to look beyond “the leader”. Chest, 166(5), 913–915. https://doi.org/10.1016/j.chest.2024.06.008
› Jevan, C., Omar, S., Alice, H., Siyuan, P., Omar, S., Ishith, S., & Warren, M. R. (2024). The efficacy of three-dimensional printing for plastic surgery education: a narrative review. Plastic and Aesthetic Research, 11, Article 39. https://doi.org/10.20517/2347-9264.2024.65
› Jolliffe, L. A., Collyer, T. A., Sun, K. H., Done, L., Barber, S., Callisaya, M. L., & Snowdon, D. A. (2025). Geriatric evaluation and management inpatients spend little time participating in physically, cognitively or socially meaningful activity: a time-motion analysis. Age and Ageing, 54(3), afaf043. https://doi.org/10.1093/ageing/afaf043
› Jolliffe, L. A., Lannin, N. A., Larcombe, S. A., Major, B. A., Hoffmann, T., & Lynch, E. A. (2025). Training and education provided to local change champions within implementation trials: a rapid systematic review.
Implementation Science, 20, Article 8. https://doi.org/10.1186/s13012-025-01416-9
› Jolly, S., d’Entremont, M. A., Lee, S. F., Mian, R., Tyrwhitt, J., Kedev, S., Montalescot, G., Cornel, J. H., Stanković, G., Moreno, R., Storey, R. F., Henry, T. D., Mehta, S. R., Bossard, M., Kala, P., Layland, J., Zafirovska, B., Devereaux, P. J., Eikelboom, J. W., & Yusuf, S. (2025). Colchicine in acute myocardial infarction. The New England Journal of Medicine, 392(7), 633–642.
https://doi.org/10.1056/nejmoa2405922
› Jolly, S. S., d’Entremont, M. A., Pitt, B., Lee, S. F., Mian, R., Tyrwhitt, J., Kedev, S., Montalescot, G., Cornel, J. H., Stanković, G., Moreno, R., Storey, R. F., Henry, T. D., Mehta, S. R., Bossard, M., Kala, P., Bhindi, R., Zafirovska, B., Devereaux, P. J., & Yusuf, S. (2024). Routine spironolactone in acute myocardial infarction. The New England Journal of Medicine, 392(7), 643–652.
https://doi.org/10.1056/NEJMoa2405923
› Joseph, K., van der Hock, S., Seth, I., Hapangama, N., Gibson, L., Cuomo, R., Rozen, W. M., & Dhupar, N. (2025). Association of ovarian teratoma with anti-N-methyl-D-aspartate receptor encephalitis: a case report and narrative review. Archives of Gynecology and Obstetrics, 311(6), 1535–1541. https://doi.org/10.1007/s00404-024-07779-6
› Kaciulyte, J., Sordi, S., Luridiana, G., Marcasciano, M., Lo Torto, F., Cavalieri, E., Codolini, L., Cuomo, R., Rozen, W. M., Seth, I., Ribuffo, D., & Casella, D. (2024). Size does matter: mastectomy flap thickness as an independent decisional factor for the peri-prosthetic device choice in prepectoral breast reconstruction. Journal of Clinical Medicine, 13(23), 7459. https://doi.org/10.3390/jcm13237459
› Karamchandani, K., Nasa, P., Jarzebowski, M., Brewster, D. J., De Jong, A., Bauer, P. R., Berkow, L., Brown, C. A., Cabrini, L., Casey, J., Cook, T., Divatia, J. V., Duggan, L. V., Ellard, L., Ergan, B., Jonsson Fagerlund, M., Gatward, J., Greif, R., Higgs, A., & Myatra, S. N. (2024). Tracheal intubation in critically ill adults with a physiologically difficult airway: an international Delphi study. Intensive Care Medicine, 50(10), 1563–1579. https://doi.org/10.1007/s00134-024-07578-2
› Karunarathna, S., Breslin, M., Alty, J., Beare, R., Collyer, T. A., Srikanth, V. K., McDonald, J. S., & Callisaya, M. L. (2024). Associations between brain structure and dual decline in gait and cognition. Neurobiology of Aging, 143, 10–18. https://doi.org/10.1016/j.neurobiolaging.2024. 08.004
› Klein, O., Carlino, M. S., Michael, M., Underhill, C. R., So, J., Kee, D., Antill, Y., Lam, W. S., Chan, H., Harrup, R. A., Hamilton, A., Palmer, J. B., Thomas, D. M., Wilkie, K., Cebon, J., & Gao, B. (2024). 713MO Nivolumab and ipilimumab combination treatment in advanced gynaecological clear cell cancers: results from the phase II MoST-CIRCUIT trial.
Annals of Oncology, 35, S546–S547. https://doi.org/10.1016/j.annonc.2024.08.775
› Klein, O., Gao, B., Chan, H., Michael, M., Zielinski, R., So, J., Harris, S. J., Kee, D., Collins, I. M., Lam, W. S., Lyle, M., Underhill, C. R., Brown, M., Harrup, R. A., Wong, S. F., Palmer, J. B., Thomas, D., Wilkie, K., Cebon, J., & Carlino, M. S. (2024). 998MO nivolumab and ipilimumab combination treatment in advanced dMMR/MSI-H noncolorectal cancers: results from the phase II MoST-CIRCUIT study.
Annals of Oncology, 35(2), S679–S680. https://doi.org/10.1016/j.annonc.2024.08.1057
› La Hood, A., Moran, C., Than, S., Lu, A., Collyer, T. A., Beare, R., & Srikanth, V. (2025). Associations between physical activity and brain structure in a large community cohort. Scientific Reports, 15(1), Article 18896. https://doi.org/10.1038/s41598-025-04010-7
› Lannin, N. A., Crotty, M., Cameron, I. D., Chen, Z., Ratcliffe, J., Morarty, J., & Turner-Stokes, L. (2024). Cost efficiency of inpatient rehabilitation following acquired brain injury: the first international adaptation of the UK approach. BMJ Open, 14(12), e094892. https://doi.org/10.1136/bmjopen-2024-094892
› Lannin, N. A., Pellegrini, M., Smith, M. J., Jolliffe, L., & Morris, M. E. (2024). Addressing the intensity of rehabilitation evidence–practice gap: rapid review, stakeholder perspectives and recommendations for upper limb rehabilitation after acquired brain injury. International Journal of Therapy and Rehabilitation, 31(7), 1–20. https://doi.org/10.12968/ijtr.2018.0029
› Lavina, R., Eric, Y., Savannah, D., Roberto, C., Ishith, S., & Rozen, W. M. (2024). The use of generative artificial intelligence in surgical education: a narrative review. Plastic and Aesthetic Research, 11, Article 57. https://doi.org/10.20517/2347-9264.2024.102
› Layton, N., Devanny, C., Hill, K., Swaffer, K., Russell, G., Low, L. F., Lee, D. C., Cations, M., Skouteris, H., O’Connor, C. M., Collyer, T. A., Neves, B. B., Andrew, N. E., Haines, T., Srikanth, V. K., Petersen, A., & Callisaya, M. L. (2024). The right to rehabilitation for people with dementia: a codesign approach to barriers and solutions. Health Expectations, 27(5), 1112–1124. https://doi.org/10.1111/hex.70036
› Lee, D. C., Russell, G., Haines, T. P., Hill, K. D., O’Connor, C. M. C., Layton, N., Swaffer, K., Long, M., Devanny, C., & Callisaya, M. L. (2024). Dementia rehabilitation training for general practitioners and practice nurses: does it make a difference? Nursing Reports, 14(4), 3108-3125. https://doi.org/10.3390/nursrep14040226
› Lennox, A., Goodwin, D., Leavold, F., Nicol, R., Srikanth, V., Ayton, D., Berends, M., Thiessen, M., Flynn, D., & Moran, C. (2025). Understanding and integrating the needs and preferences of people living with dementia in the inpatient setting: a qualitative study. BMC Geriatrics, 25, Article 342. https://doi.org/10.1186/s12877-025-05932-7
› Levett-Jones, T., Moroney, T., Bonnamy, J., Cornish, J., Moll, E. C., Foster, A., Lapkin, S., Pich, J., Richards, C., Tutticci, N., Tulleners, T., & Young, M. (2025). Investigating the impact of the ‘healthy planet, healthy people’ educational boardgame: a multicentre pre-test - post-test study. Nurse Education Today, 152, 106753. https://doi.org/10.1016/j.nedt.2025.106753
› Li, E. Y. Y., Robinson, L. S., & Stockdale, C. (2025). Establishing the reliability and validity for GripAble: a handheld sensor-based dynamometry device. Hand Therapy, 30(2), 90–99. https://doi.org/10.1177/17589983251322537
› Li, P., Papa, N., Corcoran, N. M., & Agarwal, D. K. (2025). Comparing R.E.N.A.L., PADUA, and RPN scores: is RPN the more logical choice in the robotic era? BJU International. https://doi. org/10.1111/bju.16807
› Lim, B., Seth, I., Cevik, J., Ratnagandhi, J. A., Bulloch, G., Pentangelo, P., Ceccaroni, A., Alfano, C., Rozen, W. M., & Cuomo, R. (2024). Innovations in pain management for abdominoplasty patients: a systematic review. Journal of Personalized Medicine, 14(11), Article 1078. https://doi.org/10.3390/jpm14111078
› Lim, B., Seth, I., Joseph, K., Cevik, J., Li, H., Xie, Y., Hernandez, A. M., Cuomo, R., & Rozen, W. M. (2024). Optimal use of drain tubes for DIEP flap breast reconstruction: comprehensive review. Journal of Clinical Medicine, 13(21), Article 6586. https://doi.org/10.3390/jcm13216586
› Lim, B., Seth, I., Marcaccini, G., Susini, P., Cuomo, R., & Rozen, W. M. (2024). Regulatory frameworks in plastic and cosmetic surgery: a comparative scoping review across Australia, United Kingdom, and Italy. Gland Surgery, 13(8), 1561–1572. https://doi.org/10.21037/gs-24-244
› Lim, B., Seth, I., Maxwell, M., Cuomo, R., Ross, R. J., & Rozen, W. M. (2025). Evaluating the efficacy of large language models in generating medical documentation: a comparative study of ChatGPT-4, ChatGPT-4o, and Claude. Aesthetic Plastic Surgery https://doi.org/10.1007/s00266-025-04842-8
› Liu, J., Harewood, L., Bagguley, D., Dundee, P., Mirmilstein, G., Murphy, D. G., Chan, Y., Moon, D., Kearns, P., Satasivam, P., Perera, M., Woon, D. T. S., Reeves, F., Agarwal, D. K., Peters, J., Katz, D., Raj, M., Eapen, R., Sengupta, S., & Lawrentschuk, N. (2025). Early results from the CONFIRM trial: utility of prostatespecific membrane antigen positron emission tomography/computed tomography in active surveillance for prostate cancer. European Urology Oncology, 8(4), 1118–1125. https://doi.org/10.1016/j.euo.2025.02.010
› Liu, R. K., Green, J., & Newton, R. (2025). A scoping review of treatment for factitious disorder (imposed on self). Psychiatry Research Communications, 5(2), 100216. https://doi.org/10.1016/j.psycom.2025.100216
› Lodge, M. E., Dhesi, J., Andrew, N. E., Srikanth, V. K., Ayton, D. R., & Moran, C. M. (2024). Implementing a perioperative medicine for older people undergoing surgery (POPS) service: a guide for clinical leaders. Australasian Journal on Ageing, 44(1), e13376. https://doi.org/10.1111/ajag.13376
› Lodge, M. E., Dhesi, J., Shipway, D. J. H., Braude, P., Meilak, C., Partridge, J., Andrew, N. E., Srikanth, V. K., Ayton, D. R., & Moran, C. M. (2025). Core elements of the perioperative medicine for older people undergoing surgery (POPS) model of care. European Geriatric Medicine, 16(2), 435–446. https://doi.org/10.1007/s41999-024-01122-7
› Lora, L., & Foran, P. (2024). Nurses’ perceptions of artificial intelligence (AI) integration into practice: an integrative review. Journal of Perioperative Nursing, 37(3). https://doi.org/10.26550/2209-1092.1366
› Lu, A., Than, S., Beare, R., La Hood, A., Collyer, T. A., Srikanth, V., & Moran, C. (2024). Interactions between muscle volume and body mass index on brain structure in the UK Biobank. Frontiers in Dementia, 3, Article 1456716. https://doi.org/10.3389/frdem.2024.1456716
› Machado, P., Le, T., Rozen, W. M., Hunter-Smith, D. J., & Niumsawatt, V. (2025). An optimal scalp rotation flap design: mathematical and bio-mechanical analysis. JPRAS Open, 43, 251–264. https://doi.org/10.1016/j.jpra.2024.10.007
› Marcaccini, G., Seth, I., Lim, B., Sacks, B. K., Novo, J., Ting, J. W., Cuomo, R., & Rozen, W. M. (2025). Management of burns: multi-center assessment comparing AI models and experienced plastic surgeons. Journal of Clinical Medicine, 14(9), Article 3078. https://doi.org/10.3390/jcm14093078
› Marcaccini, G., Seth, I., Novo, J., Bautista, M., Ruhunage, L., Bhat, S., Cuomo, R., & Rozen, W. M. (2025). Myopericytoma masquerading as Dupuytren’s disease: a case report and systematic literature review. Journal of Clinical Medicine, 14(11), Article 3703. https://doi.org/10.3390/jcm14113703
› Marcaccini, G., Seth, I., Novo, J., McClure, V., Sacks, B. K., Lim, K., Ng, S. K., Cuomo, R., & Rozen, W. M. (2025). Leveraging artificial intelligence for personalized rehabilitation programs for head and neck surgery patients. Technologies, 13(4), Article 142. https://doi.org/10.3390/technologies13040142
› Marcaccini, G., Seth, I., Xie, Y., Susini, P., Pozzi, M., Cuomo, R., & Rozen, W. M. (2025). Breaking bones, breaking barriers: ChatGPT, DeepSeek, and Gemini in hand fracture management. Journal of Clinical Medicine, 14(6), Article 1983. https://doi.org/10.3390/jcm14061983
› Marcaccini, G., Susini, P., Xie, Y., Cuomo, R., Pozzi, M., Grimaldi, L., Rozen, W. M., & Seth, I. (2025). Enhancing patient education in breast surgery: artificial intelligence-powered guidance for mastopexy, augmentation, reduction, and reconstruction. Translational Breast Cancer Research, 6, Article 99318. https://doi.org/10.21037/tbcr-24-67
› Marshall, S. (2024). Usability comparison scoring of video and direct laryngoscopes. Anaesthesia, 79(11), 1257-1288. https://doi.org/10.1111/anae.16397
› Marshall, S., & Eppich, W. (2025). Aspiring to mastery: clinical skills learning in regional anaesthesia. British Journal of Anaesthesia, 135(1), 26–30. https://doi.org/10.1016/j.bja.2025.04.008
› Martin, P., Kumar, S., Ducat, W., & Snowdon, D. (2024). Interprofessional supervision: strengthening clinical supervision by utilising commonalities across professions. The Journal of Practice Teaching and Learning, 22(1–2), 97–114. https://doi.org/10.1921/jpts.v20i3.2152
› McErlean, G., Hui, H., Crawford-Williams, F., Hart, N. H., Krishnasamy, M., Koczwara, B., Walwyn, T., Iddawela, M., McIntosh, R., Chan, R. J., & Jefford, M. (2025). Quality cancer survivorship care: a modified Delphi study to define nurse capabilities. Journal of Cancer Survivorship https://doi.org/10.1007/s11764-025-01804-6
› McShane, E., Furness, K., Hanna, L., Connell, K., Haines, T., Huggins, C., Zalcberg, J., Carey, S., Pilgrim, C. H. C., Lundy, J., Metz, A., Kissane, D., Franco, M., Coutsouvelis, J., De Boo, D. W., Bell, J., Iddawela, M., Dodson, T., Pereira, I., & Croagh, D. (2025). Assessing the impact of an intensive dietitian-led telehealth intervention focusing on nutritional adequacy, symptom control and optional supplemental jejunal feeding, on quality of life in patients with pancreatic cancer: a randomised controlled trial protocol. Nutrition Journal, 24(1), Article 54. https://nutritionj.biomedcentral.com/ articles/10.1186/s12937-025-01113-9
› Medland, J., Garcia, N., Seth, I., & Rozen, W. M. (2025). Dupuytren’s disease percutaneous needle aponeurotomy: does grip strength improve post procedure?
Journal of Clinical Medicine, 14(12), Article 4171. https://doi.org/10.3390/jcm14124171
› Molloy, R., Bonnamy, J., Brand, G., Pope, N., Schweizer, R., & Sevenhuysen, S. (2025). Harnessing lived experience in health professions simulation-based education: a scoping review. Advances in Health Sciences Education. https://doi.org/10.1007/s10459-025-10432-9
› Mon, Y., Seth, I., Medland, J., & Rozen, W. M. (2025). Effectiveness of splinting after percutaneous needle fasciotomy for Dupuytren’s contracture. Journal of Hand Surgery (European Volume). https://doi.org/10.1177/17531934251350463
› Muthusamy, S., Phan, A. L. G., Seneviratne, U., Beare, R., Srikanth, V., Ma, H., & Phan, T. G. (2025). Identifying hotspots of seizure-related hospital admissions in Australia. Seizure, 129, 70–76. https://doi.org/10.1016/j.seizure.2025.03.017
› Nagamalla, V., Verghese, J., Ayers, E., Barzilai, N., Beauchet, O., Lipton, R. B., Shimada, H., Srikanth, V. K., & Blumen, H. M. (2024). Distinct patterns of brain atrophy in amnestic mild cognitive impairment and motoric cognitive risk syndromes. Neurodegenerative Diseases, 24(3–4), 117–128. https://doi.org/10.1159/000540512
› Naito, Y., Koshino, Y., Ota, H., Piano, M., Watanabe, A., Inagaki, Y., Tokikuni, Y., & Sawamura, D. (2025). Short-term effect of prism adaptation treatment on severity of unilateral spatial neglect following right hemispheric stroke: a systematic review and meta-analysis. Journal of Rehabilitation Medicine, 57, Article 42542. https://doi.org/10.2340/jrm.v57.42542
› Naude, K., Snowdon, D. A., Parker, E., McNaney, R., Srikanth, V., & Andrew, N. E. (2025). Sharing data matters: exploring the attitudes of older consumers on an emerging healthy ageing data platform using electronic health records for research. BMJ Health & Care Informatics, 32(1), e101126. https://doi.org/10.1136/bmjhci-2024-101126
› Nguyenhuy, M., Chan, X. Q., Homewood, D., Ogluszko, C., Dundee, P., & Corcoran, N. (2024). Utility of multiparametric prostate MRI to predict regional or distant metastatic disease against conventional staging using CT and bone scintigraphy or Ga-PSMA PET in intermediate-tohigh-risk prostate cancer. Cureus, 16(11), e10032. https://doi.org/10.7759/cureus.10032
› Nielsen, S., Cheetham, A., Grist, E., Jackson, J., Lord, S., Petrie, D., Jacka, D., & Morgan, K. (2025). A multisite implementationefficacy trial of pharmacist-led collaborative care for medication assisted treatment for opioid dependence: 3-month outcomes from the EPIC-MATOD trial. Drug and Alcohol Dependence, 267, 112163. https://doi.org/10.1016/j.drugalcdep.2024.112163
› Noble, P. B., Langton, D., Foo, C. T., Thompson, B. R., Cairncross, A., Hackmann, M. J., Thien, F., & Donovan, G. M. (2024). Beyond bronchial thermoplasty – where to now?
EClinicalMedicine, 79, Article 103017. https://doi.org/10.1016/j.eclinm.2024.103017
› Novo, J., Seth, I., Mon, Y., Soni, A., Elkington, O., Marcaccini, G., & Rozen, W. M. (2025). Use of robotic surgery in plastic and reconstructive surgery: a narrative review. Biomimetics, 10(2), Article 97. https://doi.org/10.3390/biomimetics10020097
› Ong, S. W. X., Pinto, R., Rishu, A., Tong, S. Y. C., Commons, R. J., Conly, J. M., Evans, G. A., Fralick, M., Kandel, C., Lagacé-Wiens, P. R. S., Lee, T. C., Lother, S. A., MacFadden, D. R., Marshall, J. C., Martel-Laferrière, V., Mayette, M., McDonald, E. G., Neary, J. D., Prazak, J., & Daneman, N. (2025). Identifying heterogeneity of treatment effect for antibiotic duration in bloodstream infection: an exploratory post-hoc analysis of the BALANCE randomised clinical trial. EClinicalMedicine, 83, Article 103195. https://doi.org/10.1016/j.eclinm.2025.103195
› Pang, R. K., Shannon, B., Collyer, T., Srikanth, V., & Andrew, N. E. (2025). Community care navigation intervention for people who are at risk of unplanned hospital presentations. Cochrane Database of Systematic Reviews, 6(6), Article CD014713. https://doi.org/10.1002/14651858.CD014713.pub2
› Paynter, J., Qin, K., Hunter-Smith, D., Brennan, J., & Rozen, W. M. (2024). Rural general surgical provision from the perspective of twenty-two rural general surgeons: a thematic analysis. ANZ Journal of Surgery, 94(12), 2231–2237. https://doi.org/10.1111/ans.19229
› Pearce, B., Uribe, S., Cowling, C., Pinson, J. A., Smith, W., & Sim, J. (2024). Can radiographer regulatory compliance contribute to patient safety in the emergency department fast-track pathway? A retrospective pilot study. Radiography (London), 31(1), 53–65. https://doi.org/10.1016/j.radi.2024.04.012
› Phan, T. G., Srikanth, V. K., Cadilhac, D. A., Nelson, M., Kim, J., Olaiya, M. T., Fitzgerald, S. M., Bladin, C., Gerraty, R., Ma, H., Thrift, A. G., Nurses of the STANDFIRM Trial, & Doctors for Improved Risk Factor Management Collaborative (2025). Framingham Risk Score prediction at 12 months in the STANDFIRM randomized control trial. Journal of the American Heart Association, 14(10), e040254. https://doi.org/10.1161/JAHA.124.040254
› Phillips, B. T., Abi-Rafeh, J., Brown, S., Datta, S., Graziano, F. D., Ma, X., Molle, M., Naga, H. I., Othman, S., Remy, K., Seth, I., Mardan, Q. N. M. S., Taskindoust, M., & Williams, S. (2025). Spotlight in plastic surgery: January 2025. Plastic and Reconstructive Surgery, 155(1), 223–226. https://doi.org/10.1097/PRS.0000000000011718
› Piano, M., Jarden, R. J., Hastings-Ison, T., Lawford, B. J., Diemer, K., Hui, F., Kefalianos, E., & McKibbin, G. (2024). Exploring early- and midcareer academic work wellbeing challenges through a diversity and inclusion lens. BMC Medical Education, 24(1), Article 1048. https://doi.org/10.1186/s12909-024-05967-1
› Quick, S., Lawler, K., Shannon, M., Soh, S., McGinley, J., Snowdon, D., & Callisaya, M. (2025). What is effective physiotherapy for dementia and how do we get there: a qualitative study. Physiotherapy Theory and Practice, 41(7), 1447–1457. https://doi.org/10.1080/09593985.2024.2426181
› Rahman, M. M., Jahan, S., Koczwara, B., Iddawela, M., Chan, R. J., Thornton-Benko, E., Garvey, G., & Hart, N. H. (2024). Utilisation of Medicare chronic disease management item numbers for people with cancer in Queensland, Australia. Australian Health Review, 48(6), 626–633. https://doi.org/10.1071/AH24121
› Rajaram, R., Cevik, J., Bhindi, N., & Rozen, W. M. (2024). The anatomy of the superficial inferior epigastric artery: cautious optimism and rightful reluctance for the championing of a minimally morbid abdominal flap. Journal of Plastic, Reconstructive & Aesthetic Surgery, 96, 69–71. https://doi.org/10.1016/j.bjps.2024.07.004
› Ralota, K., Dagan, M., Lee, J., Gowda, V., & Layland, J. (2025). Cardiac medication nonadherence: the elephant in the room. Internal Medicine Journal, 55(4), 690–691. https://doi.org/10.1111/imj.70042
› Ralota, K. K., Layland, J., Han Win, K. T., & Htun, N. M. (2025). Myocardial viability: evolving insights and challenges in revascularization and functional recovery. Journal of Cardiovascular Development and Disease, 12(3), Article 106. https://doi.org/10.3390/jcdd12030106
› Raspovic, A., Duck, R., Synnot, A., Caldwell, B., Phillipou, A., Castle, D., Newton, R., Brennan, L., Jenkins, Z., Cunich, M., Maguire, S., & MiskovicWheatley, J. (2024). A peer mentoring program for eating disorders: improved symptomatology and reduced hospital admissions, three years and a pandemic on. Journal of Eating Disorders, 12(1), Article 99. https://doi.org/10.1186/s40337-024-01051-7
› Reeder, S., Stanley, M., Jolliffe, L. J., & Lannin, N. A. (2025). Study protocol for a nested process evaluation of a complex discharge planning intervention (HOME Rehab) to improve participation after first-stroke. Frontiers in Neurology, 15, Article 1483245. https://doi.org/10.3389/fneur.2024.1483245
› Rehan, R., Virk, S., Wong, C., Passam, F., Layland, J., Keech, A., Yong, A., White, H., Fearon, W., & Ng, M. (2024). Intracoronary thrombolysis in ST-elevation myocardial infarction: a systematic review and metaanalysis. Heart, 110(15), 988–996. https://heart.bmj.com/content/110/15/988
› Ridley, E. J., Bailey, M., Chapman, M. J., Chapple, L. S., Deane, A. M., Gojanovic, M., Higgins, A. M., Hodgson, C. L., King, V. L., Marshall, A. P., Miller, E. G., McGuinness, S. P., Parke, R. L., Paul, E., & Udy, A. A. (2025). The impact of a tailored nutrition intervention delivered for the duration of hospitalisation on daily energy delivery for patients with critical illness (INTENT): a phase II randomised controlled trial. Critical Care, 29(1), Article 8. https://doi.org/10.1186/s13054-024-05189-3
› Rohan, R., Jevan, C., & Rozen, W. M. (2025). Non-vascularised lymph node transfer: future directions for the minimally invasive surgical management of lymphoedema. Plastic and Aesthetic Research, 12, Article 6. https://doi.org/10.20517/2347-9264.2024.147
› Savage, S. A., Seth, I., Angus, Z. G., & Rozen, W. M. (2025). Advancements in microsurgery: a comprehensive systematic review of artificial intelligence applications. Journal of Plastic, Reconstructive & Aesthetic Surgery, 101, 65–76. https://doi.org/10.1016/j.bjps.2025.07.008
› Schmid, P., Cortes, J., Dent, R., McArthur, H., Pusztai, L., Kümmel, S., Denkert, C., Park, Y. H., Hui, R., Harbeck, N., Takahashi, M., Im, S. A., Untch, M., Fasching, P. A., Mouret-Reynier, M. A., Foukakis, T., Ferreira, M., Cardoso, F., Zhou, X., & O’Shaughnessy, J. (2024). Overall survival with pembrolizumab in early-stage triple-negative breast cancer. The New England Journal of Medicine, 391(21), 1981–1991. https://doi.org/10.1056/NEJMoa24099
› Scrivener, K., Ada, L., Pellegrini, M., Nicks, R., Kramer, S., Christie, L. J., Jolliffe, L. J., Dean, C., & Lannin, N. A. (2024). Is there room for improvement? Stroke rehabilitation environments may not reflect home environments in terms of chair, toilet, and bed heights. Archives of Rehabilitation Research and Clinical Translation, 6(3), Article 100352. https://doi.org/10.1016/j.arrct.2024.100352
› Seth, I., Bulloch, G., Seth, N., Fogg, Q., HunterSmith, D. J., & Rozen, W. M. (2023). Efficacy and safety of different trapezium implants for trapeziometacarpal joint osteoarthritis: a systematic review and meta-analysis. Hand, 19(8). https://doi.org/10.1177/15589447231183172
› Seth, I., Lim, B., Lu, P. Y. J., Xie, Y., Cuomo, R., Ng, S. K., Rozen, W. M., & Sofiadellis, F. (2024). Digital twins use in plastic surgery: a systematic review. Journal of Clinical Medicine, 13(24), Article 7861. https://doi.org/10.3390/jcm13247861
› Seth, I., Lim, B., Phan, R., Xie, Y., Kenney, P. S., Bukret, W. E., Thomsen, J. B., Cuomo, R., Ross, R. J., Ng, S. K., & Rozen, W. M. (2024). Perforator selection with computed tomography angiography for unilateral breast reconstruction: a clinical multicentre analysis. Medicina, 60(9), Article 1500 https://doi.org/10.3390/medicina60091500
› Seth, I., Lim, B., & Rozen, W. M. (2025). Response to “Letter to the Editor - Exploring the Unknown: Evaluating ChatGPT’s performance in uncovering novel aspects of plastic surgery and identifying areas for future innovation.” Aesthetic Plastic Surgery, 4(9), 2638–2639. https://doi.org/10.1007/s00266-024-04210-y
› Seth, I., Lim, K., Chang, E., Rozen, W. M., & Ng, S. K. (2025). Evaluating the clinical utility of robotic systems in plastic and reconstructive surgery: a systematic review. Sensors, 25(10), Article 3238. https://doi.org/10.3390/s25103238
› Seth, I., Marcaccini, G., Lim, K., Castrechini, M., Cuomo, R., Ng, S., Ross, R. J., & Rozen, W. M. (2025). Management of Dupuytren’s disease: a multi-centric comparative analysis between experienced hand surgeons versus artificial intelligence. Diagnostics, 15(5), Article 587. https://doi.org/10.3390/diagnostics15050587
› Seth, I., McClure, V., Lim, B., Cuomo, R., Ross, R. J., & Rozen, W. M. (2025). Collagenase Clostridium histolyticum versus percutaneous needle fasciotomy for Dupuytren’s disease: a systematic review and meta-analysis. Life, 15(2), Article 259. https://doi.org/10.3390/life15020259
› Shen, A., Seth, I., Marcaccini, G., Rozen, W. M., & Ross, R. J. (2024). Basal cell carcinoma arising in a previous full-thickness graft donor site: a case report and comprehensive literature review. Journal of Clinical Medicine, 14(2), Article 591. https://doi.org/10.3390/jcm14020591
› Siostrom, K., Snowdon, D., Sriamareswaran, R. K., Law, Y. M., Jolliffe, L., & Moran, C. (2024). Experiences of healthcare staff caring for hospitalised people with delirium: a qualitative systematic review. Age and Ageing, 53(7), Article afae159. https://doi.org/10.1093/ageing/afae159
› Snowdon, D. A., Marsh, L., Srikanth, V., Beare, R., Barnden, R., Parker, E., & Andrew, N. E. (2025). Feasibility of implementing a codesigned patient reported outcome measures (PROMs) collection system for older adults in acute and sub-acute hospital settings.
Quality of Life Research, 34(6), 1809–1822. https://doi.org/10.1007/s11136-025-03931-0
› Soliman, C., Walz, J., Corcoran, N. M., Wuethrich, P. Y., Lawrentschuk, N., & Furrer, M. A. (2025). Risk prediction tools for estimating surgical difficulty and perioperative and postoperative outcomes including morbidity for major urological surgery: a concept for the future of surgical planning.
European Urology Open Science, 75, 55–60. https://doi.org/10.1016/j.euros.2025.03.012
› Sordi, S., Kaciulyte, J., Marzouk El Araby, M., Luridiana, G., Marchesi, A., Gatto, A., Seth, I., Rozen, W. M., Casella, D., & Cuomo, R. (2024). Streamlining outpatient prepectoral breast reconstruction: the role of polyurethane oxygenenriched bra cups from pandemic innovation to standardized cost analysis.
Giornale di Chirurgia - (Journal of the Italian Surgical Association), 44(6), e59. https://doi.org/10.1097/IA9.0000000000000059
› Tay, Y. T., Purcell, E., Seth, I., Marcaccini, G., & Rozen, W. M. (2025). Use of COX inhibitors in plastic surgery fibroproliferative disorders: a systematic review. Journal of Personalized Medicine, 15(6), Article 257. https://doi.org/10.3390/jpm15060257
› Taylor, N. F., Rimayanti, M. U., Peiris, C. L., Snowdon, D. A., Harding, K. E., Semciw, A. I., O’Halloran, P. D., Wintle, E., Williams, S., & Shields, N. (2024). Hip fracture has profound psychosocial impacts: a systematic review of qualitative studies. Age and Ageing, 53(9), Article 194. https://doi.org/10.1093/ageing/afae194
› Thirugnanasundralingam, V., McGrath, S., Roberts, J., & Corcoran, N. (2024). A peculiar distribution on (18)F-DCFPyL-PSMA PET scan for a patient with prostate cancer and protein S deficiency. Radiology Case Reports, 19(10), 4122–4126. https://doi.org/10.1016/j.radcr.2024.06.021
› Tiong, J., Nguyen, P., Sritharan, M., Lundy, J., Shen, H., Kumar, B., Swan, M., Jenkins, B., & Croagh, D. (2024). Evaluation of needles in endoscopic ultrasound-guided tissue acquisition of pancreatic cancer for genetic yield and quality. Cureus, 16(9), e68431. https://doi.org/10.7759/cureus.68431
› Tiruvoipati, R., Akkanti, B., Dinh, K., Barrett, N. A., May, A., & Conrad, S. A. (2024). Extracorporeal carbon dioxide removal with the Hemolung in patients with acute-on-chronic respiratory failure: a multicenter retrospective cohort study. Critical Care Medicine, 51(7), 892–902. https://doi.org/10.1097/ccm.0000000000005845
› Tiruvoipati, R., Kansal, A., & Panwar, R. (2025). High mean arterial pressure (MAP) targets in septic shock: one size does not fit all. Intensive Care Medicine, 51, 1559–1560. https://doi.org/10.1007/s00134-025-07997-9
› Tiruvoipati, R., Reddy, M. P., Paul, E., Gupta, S., Subramaniam, A., Zhang, D., & Haji, K. (2025). A comparison of conventional high-flow nasal cannula vs the Duet high-flow nasal cannula in extubated patients: a randomized crossover trial. European Journal of Medical Research, 30(1), Article 205. https://eurjmedres. biomedcentralcom/articles/10.1186/s40001-02502447-0
› Toomey, M., Gurteen, H., Franco, B., Wilson, L., Coleman, M., El-Saifi, N., Gu, Y., Heine, C., Keay, L., Kumaran, S., Lenzen, S., Leroi, I., Meyer, C., Mitchell, L., Pachana, N., Scanlan, E., & Dawes, P. (2025).
“Aged care is more than wiping bums and giving medication”: a qualitative study of the sensory support care needs of older Australians with hearing and/or vision impairment. Disability and Rehabilitation, 1–10. https://doi.org/ 10.1080/09638288.2025.2523971
› Touyz, S., Aouad, P., Carney, T., Ong, S. H., Yager, J., Newton, R., Hay, P., Maguire, S., & Bryant, E. (2024). Clinical, legal and ethical implications of coercion and compulsory treatment in eating disorders: do rapid review findings identify clear answers or more muddy waters? Journal of Eating Disorders, 12(1), Article 163. https://doi.org/10.1186/s40337-024-01120-x
› Touyz, S., Carney, T., Yager, J., Newton, R., Hay, P., & Aouad, P. (2024). Finding the balance between respecting autonomy and life-saving anorexia nervosa care: an Australian perspective. Psychiatry, Psychology and Law, 31(4), 1–15. https://doi.org/10.1080/13218719.2024.2416643
› Urquhart, S. B., Webb, G. I., Leong, S., & Webb, A. (2025). The validity of self-reported smoking status on day of surgery in a mixed elective surgery population. Anaesthesia and Intensive Care, 53(5), 307–314. https://doi.org/10.1177/0310057x251315764
› West, D. A., Killick, C., & Jones, D. (2025). Use of point-of-care ultrasound during cardiac arrest in the intensive care unit: a cross-sectional survey. Australian Critical Care, 38(1), Article 101058. https://doi.org/10.1016/j.aucc.2024.04.003
› Wheatcroft, J., Nicks, R. J., Jolliffe, L., Sansonetti, D., Unsworth, C., & Lannin, N. A. (2024). Applying implementation science theories to support practice change in the assessment of cognition by occupational therapists. Brain Impairment, 25, Article IB23105. https://doi.org/10.1071/IB23105
› Yamaguchi, T. N., Houlahan, K. E., Zhu, H., Kurganovs, N., Livingstone, J., Fox, N. S., Yuan, J., Sietsma Penington, J., Jung, C., Schwarz, T., Jaratlerdsiri, W., van Riet, J., Georgeson, P., Mangiola, S., Taraszka, K., Lesurf, R., Jiang, J., Chow, K., Heisler, L. E., & Boutros, P. C. (2025). The germline and somatic origins of prostate cancer heterogeneity. Cancer Discovery, 15(5), 988–1017. https://doi.org/10.1158/2159-8290.CD-23-0882
› Yee, S., Teo, A., Reddy, M. P., Paul, E., Haji, K., & Tiruvoipati, R. (2024). Comparing quality and barriers to sleep in non-mechanically intensive care patients in intensive care unit and in hospital ward.
Sleep and Breathing, 29(1), Article 4. https://doi.org/10.1007/s11325-024-03180-4
› Zhao, X., Brand, G., Kovach, N., & Bonnamy, J. (2024). Escape rooms in nursing education: a systematic review. Nurse Educator, 49(5), E238–E243. https://doi.org/10.1097/NNE.0000000000001641
› Zhao, X., Yu, L., Bonnamy, J., Brand, G., Kovach, N., & Huang, M. (2025). Challenges faced by international nursing students undertaking graduate research: contemporary issues. Nurse Education Today, 146, 106556. https://doi.org/10.1016/j.nedt.2024.106556
Peninsula Health Research Report 2025

Peninsula Health acknowledges the contribution made by all staff involved in research. The Research Report 2025 showcases some of these projects, and recognises the many ongoing projects and commercially sponsored, collaborative group and investigator-initiated trials across the health service that fulfill our vision of exceptional healthcare driven by excellence in research.
Manager, Office for Research: Lee-Anne Clavarino
Writers: Debra Pearce, Isla Brown, Kylie Sprague, Jessica Mills. Design: Jasmine Richards. ©Peninsula Health 2025.
