connection YOUR FREE MAGAZINE FROM PENINSULA HEALTH
•
ISSUE 5
•
AUTUMN 2016
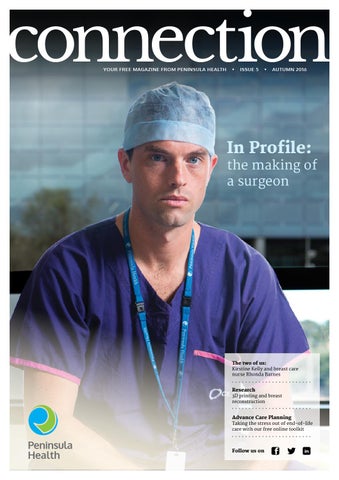
In Profile:
the making of a surgeon
The two of us: Kirstine Kelly and breast care nurse Rhonda Barnes
Research
3D printing and breast reconstruction
Advance Care Planning
Taking the stress out of end-of-life care with our free online toolkit
Peninsula Health
Follow us on