





2 04 How Opening Up to AI Could Improve Your Mental Health 12 Growing Community Care to Ease NHS Waiting Times 20 28 About Us Embracing Remanufactured Laptops for a Greener NHS The Data Principal 16 24 Health Sector Round Up Hybrid Healthcare: Enhancing the NHS Experience For All 08 TECHNOLOGY SUSTAINABILITY

h.wintle@peloton-events.co.uk
In this our third edition of the Health Industry Leaders eMagazine, we’re pleased to bring you cutting edge technological advancements and sustainability breakthroughs that continue to shape the healthcare sector in 2024 and into the future.
Featuring exclusive insights from Stephen Critchlow into how the way we handle data could streamline everything we accomplish in healthcare, we also explore the role of AI in improving mental health, and unpack the environmental advantages of remanufactured laptops.


With sustainability targets on the horizon, the healthcare sector is continuing to deliver patient outcomes in an increasingly climateconscious world, and Health Industry Leaders is intent on covering the ongoing story.
CONTENTS
3
FOREWORD
Hannah Wintle Multi Media Journalist
Floyd March Editor
Olivia Staveley Graphic Designer
Chelsea Bailey Multi Media Journalist
How Opening Up to AI Could Improve Your Mental Health
A clinical AI chatbot could encourage people to open up about their mental health problems
The app supports NHS services by enhancing the entire care pathway, from referral to discharge
A closed-loop AI approach and ensures clinical accuracy during conversations with patients
The evolution of technology is resulting in increasingly novel and exciting healthcare innovations. The use of AI in the sector is a notable example, thanks to its valuable ability to automate tasks and free up staff for the jobs that necessitate a human touch.
4 ISSUE 3 TECHNOLOGY
Mental health is one such area of healthcare where human interaction can be helpful and rewarding, but upon exploring the role of technology and AI, some impressive results have been uncovered.
To understand how technology can be utilised to help those suffering with mental health problems and support existing mental health services, Health Industry Leaders spoke to Ross O’Brien, Managing Director of Wysa, an AI mental health app.
He said: “Wysa is also a global company that supports over 6 million people on our platform in 95 different countries. We’ve got a variety of different offers from population and prevention support to helping people through talking, talking therapies, care pathways for adult services in the NHS and in employee assistance programs and lots of lots of different things in between as well.”
A CURATED AI EXPERIENCE CAN ENCOURAGE COMMUNICATION
Working through mental health problems largely revolves around the individual communicating their struggles. Traditionally, it is a human therapist on the other end of this conversation, but Wysa have developed their own AI chatbot that not only guides users through their mental health challenges, but also ensures accessibility and anonymity.
Unlike many language model AIs, such as open AI ChatGPT, Wysa uses a closed loop approach, meaning all of the answers it can provide are pre-scripted, ensuring suitable responses, based around NICE guidance and CBT protocols, are offered in every instance.
As well as its educated and appropriate clinical delivery, the AI is programmed with natural language understanding and processing, so that it can hold a fluid and natural conversation.
For Wysa, keeping the AI running optimally for users is a big priority. Ross explained: “As an AI company, we’re very, very cognisant of how we use the AI in a manner that is safe, that we’re able to audit what we do, that where approaches aren’t working very well for patients, we can go in and make changes to the code and the text so that ultimately we give the best experience, but also we give an experience which a therapist would give.”
“The biggest thing for us with mental health is that people need to trust that interaction with the AI, they need to know that the conversation is coming from a place of clinical safety and efficacy, that it works, and that they’re actually being helped in the way that the humans would want them to, so that’s really important to us.”
AI also offers a non-judgemental approach, which can be an important factor in allowing some individuals to fully open up about their mental health concerns, and helping them to access the appropriate care.

“[THERE ARE] TONS OF THINGS THAT WE DO TO TRY AND HELP PEOPLE WITH THEIR MENTAL HEALTH.”
BY HANNAH WINTLE HIL
5
Around 18% of children aged 7 to 16 had a probable mental health condition in 2022, up from 12% in 2017
3.25 million people accessed NHS mental health, learning disability and autism services in 2021/22
Two-thirds of people experience improvement after talking therapy, but this varies in different parts of England and between social groups
1 in 6 adults experience a ‘common mental disorder’ like depression or anxiety in any given week.
(Source: Mental health statistics: prevalence, services and funding in England, House of Commons Library, March 2023)
The NHS in England spent £14.9 billion on mental health services in 2021/22 - 13.8% of local NHS funding allocations
Waiting times for NHS talking therapies vary from 4 days to 229 days in different parts of England
6 HOW OPENING UP TO AI COULD IMPROVE YOUR MENTAL HEALTH
Ross illustrated this point: “You might be struggling with anxiety, and that might be manifesting in a way that gives you a bad stomach, and so you might go and talk to somebody and say, ‘I’ve got a really bad stomach and it’s stopping me from sleeping’.
“That interaction with the human might –because you feel slightly embarrassed to say, ‘well actually I think it’s because I’m really stressed’ – lead you down a path where you actually go and have physical health examinations before you get to a stage where you go and have mental health conversations.
“With AI, what we find is, because it’s nonjudgmental, it’s 24/7, and people are very, very clear that they’re not talking to a human, they’re talking to an AI, they’re a lot more open, so they’ll go and have that conversation straight off the bat.”
This has a knock-on-effect when it comes to referrals to mental health services, in that people are better able to access the appropriate services from the get-go due to the nonstigmatised front doorway Wysa has provided.
BOLSTERING NHS SERVICES BENEFITS PATIENTS AND STAFF
Supporting the NHS necessitates a tailored approach for Wysa, due to the unique challenges facing adult mental health services compared to children’s.
While supporting children’s services focuses largely on prevention and support provision during waiting times for CAMHS, where adult services are concerned, Wysa supports the whole care pathway.
In an attempt to drive up the number of referrals to the NHS and avoid confusion in their initial
stages of seeking NHS support, Wysa have enabled patients to onboard via their chatbot, through which they can complete assessments and give information about themselves and why they’ve presented to the service.
The AI chatbot, along with the more than 100 self-help modules available on the Wysa app, continue to help patients from the moment they refer, all the way through their wait, whilst they are accessing treatment with a therapist in the service, and post-discharge.
“All the way along that care pathway, there’s various things going on for the patient. Whilst they’re waiting, patients might not know how long they are going to wait, or they might go up and down in terms of their need,” Ross explained.
As well as supporting patients directly, Wysa can free up clinicians by guiding patients through any homework they might have been set, such as practising CBT techniques, so that therapists are freed up to do more for other patients.
Finally, while the help some patients receive through NHS services may have targeted the most pressing issue in their mental health, they may still have questions around other aspects of their life.
When their treatment on the NHS has concluded, patients can still access their earlier conversations on the Wysa app, as well as specific modules designed to guide patients through various issues, so that they can continue to work on themselves post-discharge.
As healthcare services continue to evolve in the face of rapidly advancing technology, AI is proving itself to have a seat at the table. Applying this innovation in both formal and selfcare settings promotes smoother NHS services, enhanced care provision, and most importantly, better mental health outcomes for those in need.
7
HYBRID HEALTHCARE: ENHANCING THE NHS EXPERIENCE FOR ALL
DrDoctor is a Patient Engagement Platform that streamlines NHS services between patients and staff
Giving patients digital autonomy over their healthcare can enhance their experience
The working environment of healthcare staff and clinicians could also benefit from hybrid healthcare systems
Healthcare and technology have always been two intertwined concepts. As technology progresses, further potential is unlocked in healthcare, and breakthroughs can be made for both individual patients as well as the system at large.
In an age of rapid technological advancement, we are seeing the vast potential of digital innovation and the seemingly countless ways it is changing how healthcare is practised the world over.
Take DrDoctor for example, a Patient Engagement Platform that, in its 11 years of operation, has facilitated over 150 million NHS appointments for 25 million unique patients across 72 hospitals, saving the NHS over £60 million in the process.
Importantly, it is a platform that lets patients take their healthcare into their own hands, by giving them autonomy over their appointments and the tools to book, reschedule, and cancel where necessary, as well as easing communication and patient record-sharing between Trust staff and patients.
While DrDoctor showcases the use case of technology and digital advancements, such as AI to identify potential no-show appointments, in a modern healthcare system, it has been developed to scaffold and complement the NHS and its existing structure we enjoy today, rather than rewrite it.
Health Industry Leaders spoke to CEO and Co-Founder of DrDoctor, Tom Whicher, who summarised the philosophy behind the platforms conception:

8 ISSUE 3 TECHNOLOGY
“I BELIEVE THE NHS IS THE BEST HEALTHCARE SYSTEM IN THE WORLD, BUT I BELIEVE THAT, AS IT IS, IT ISN’T SUSTAINABLE, AND WE HAVE THE OPPORTUNITY TO FIX THAT USING TECHNOLOGY.”

Tom Whicher, CEO and Co-Founder of DrDoctor
9 BY HANNAH WINTLE
HIL
INVOLVING PATIENTS IN THEIR OWN HEALTHCARE CAN ENSURE A SMOOTHER SERVICE
Empowering patients goes beyond giving them the ability to control their appointments. Sometimes, the most impactful improvements in the patient experience can be the most simple.
Tom said: “A lot of patient benefits are about clarity. Historically, most people are actually like, ‘look, if I have to wait six months, I’ll wait six months, but I want to know why I’m waiting, I want to know that you still care, and I want to know where I am on the list.’ All of those relatively simple problems are really important to people, and take a lot of stress out of their healthcare.”
POSITIVE OUTCOMES FOR PATIENTS BREED POSITIVE OUTCOMES FOR STAFF
Reducing waiting times and keeping channels of communication open for patients can directly impact staff, both in terms of treatment at work, and levels of burnout.
THE NHS EXPERIENCE FOR ALL
Reducing wait times remains one of DrDoctor’s priorities, a task accomplished through communication with patients, the appropriate utilisation of hospital capacity by reducing the nonattendance rate, and the continuous assessment of waiting patients and their health needs.
“If you can improve the efficiency of the system, you do reduce the waiting lists, and it means the patient can be seen as soon as possible, so ultimately its about control and communication with the patient.”
According to a recent study by DrDoctor, 75% of non-medical, patient facing NHS workers have been physically or verbally abused in the last 12 months, though 86% recognise and empathise that the rise in waiting lists plays a significant role in this behaviour. Tom acknowledged that in improving the experience of waiting, these members of staff could face less of the brunt of patient frustrations.
Furthermore, in an industry where burnout and stress levels are leading to clinicians leaving the NHS in alarming numbers, moving to more remote, data driven models could allow more scope for working from home.
10 HYBRID
HEALTHCARE: ENHANCING
“When you think about a flexible workforce, a large percentage of our clinical workforce is female and, if you’re a working mother, the ability to work flexible shifts is a huge thing, so decoupling having to be in the hospital to deliver a clinic is actually massive for the workforce.”
“But also,” Tom continued, “moving to data driven medicine means that you can allow clinicians much more work at the top of their practice. The vast majority of outpatient follow ups and are often not particularly value-adding interactions.
“If you can move those lower value interactions online, I don’t even mean video, I mean asynchronous messaging, it means that you fill the clinics up with high value patients, which are the ones where the clinicians can really add value, and that really counts so much in a burntout workforce.”
This hybrid healthcare approach, which utilises the beneficial aspects of digital innovation and combines it with in-person care, results in a twobirds-one-stone situation: patients receive more timely care with minimal fuss, and healthcare professionals are more enriched and fulfilled by their role.
“IT’S ABOUT MOVING FROM A MODEL WHERE EVERYONE GETS SEEN ON A TOP OF THE QUEUE TO THE BOTTOM OF THE QUEUE LIST AND YOU ALL GET THE SAME 10 MINUTES, TO MODEL WHERE WE SEE THE SICK PATIENTS FIRST AND THE DOCTOR CAN SPEND LONGER WITH THE PEOPLE THAT NEED IT. THAT IS WHAT WE’RE TRYING TO ACHIEVE HERE, THAT’S THE HOLY GRAIL.”
The ultimate goal of hybrid healthcare is to complement essential in-person services by offering virtual alternatives where appropriate and allowing patients digital autonomy over their healthcare processes. In doing so, the NHS is able to efficiently deliver its valuable and essential services in a way that is rewarding for both patients and staff.

11
Growing Community Care to Ease NHS Waiting Times

RMI operate all over the world in the most remote locations
Community care can take pressure off an at capacity NHS
Mobile care can help communities most in need

12 ISSUE 3 TECHNOLOGY
The demand for remote and mobile care has always simmered in the discourse surrounding the NHS, but as we emerge from a post-pandemic world, the need for this has been exacerbated and is at the forefront of conversations in the public sphere.
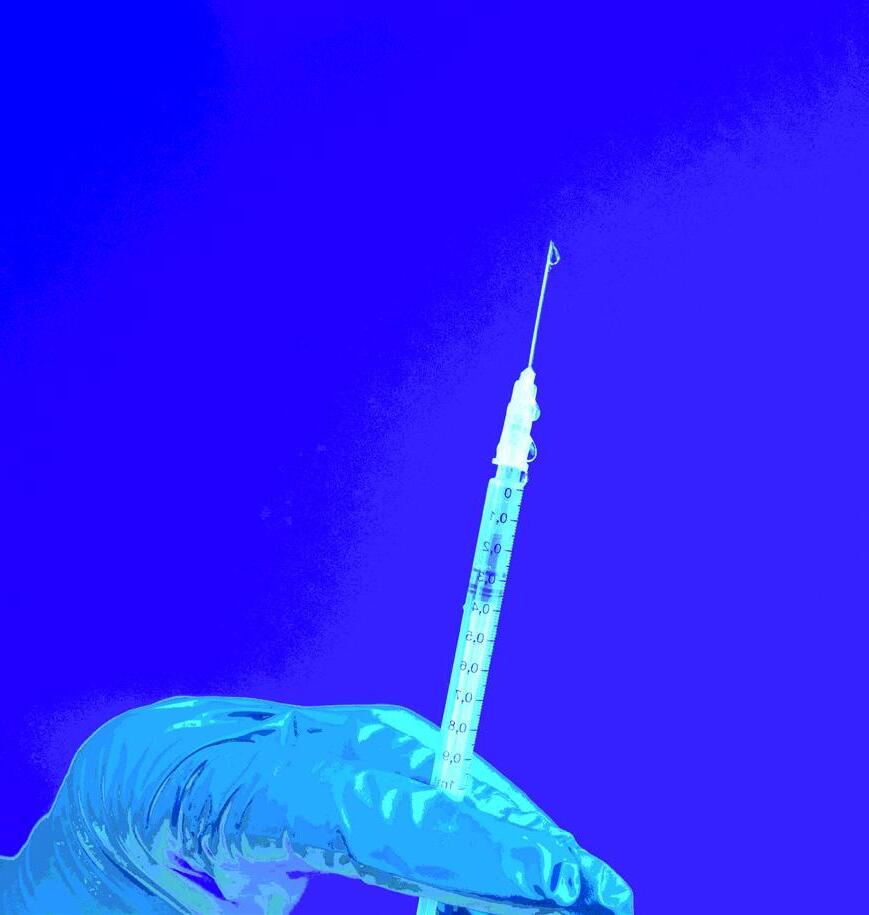
During the pandemic, RMI supported the NHS to deliver testing and vaccination services directly into the heart of the community, utilising mobile medical units as the health service looked to accelerate the rollout of its mass inoculation programme.
In addition to this, RMI has further experience in providing medical provisions to some of the most remote locations on the planet.
Both these facts coupled, highlight how such practice could be implemented on a wider NHS scale. They believe that their mobile medicine solutions could be utilised in the NHS to help deliver medical care to communities across the UK and bring down waiting lists.
With the NHS backlog growing and A&E waiting times hitting record levels, rolling out mobile medical units to provide community healthcare could save costs, time, reduce the waiting lists and improve the healthcare experience of patients in remote locations and particular mobility issues.
Echoing all of this, Health industry Leaders spoke to Simon Le Clerc, Director of NHS Business at RMI about this topical issue. He said: “We see it in the news all the time regarding patient flow, blockages in the departments and failure to discharge patients home. So we came up with a solution to try and ease this problem.”
PANDEMIC RESPONSE HAS LED TO A NEW ERA OF DELIVERING CARE
In 2021, RMI delivered that capability and closed the capacity gap that suddenly arose with COVID and where they needed to provide mobile testing in real-time and very efficiently.
“ “ “ “
Off the back of that, we started to think there’s a lot more that could be done in a mobile setting if you apply the right kind of mindset to do it.
13 BY FLOYD MARCH HIL
“To do this we asked ourselves, where are the issues, where are the challenges, and how could we address them? In terms of diagnostics specifically, how do we ease the workflow in an overcrowded setting, where people are funnelled through these departments.”
These solutions extend just this with additional options including primary care. This solution is about redistributing resources to be fairer across the board, rather than trying to meet all the needs of patients through already stretched hospitals.
Simon added: “If we can take it [care] to patients, if we can take it to people in the community, then why don't we? It's not an easy challenge but that shouldn’t and doesn’t deter us.”
Addressing these challenges head on, RMIs mobile solution has the ability to offtake routine appointments and check ups, ranging from physiotherapy to delivering government standards for screening certain age groups.
Simon explained that it makes perfect sense to: “Take our solution to those people in the community and do it there rather than people trying to make arrangements for hospital visits.”
These forms of mobile services can also be pop up, addressing regional specific needs for instance; or in rural communities where this care isn’t always accessible. Simon added: “We can move a mobile physiotherapy section to a GP practice once a week where the patients can be pre-booked by the GP's into that physio clinic; so they just come into their practice or a local environment and have the same treatment they would have had in the hospital.”
COMMUNITY HEALTHCARE CAN OFTEN BE NEGLECTED WHEN DISCUSSING THE NHS
With the demographic of the UK constantly changing, people living longer and more people entering retirement age the need for sustainable community healthcare is growing exponentially.

14 GROWING COMMUNITY CARE TO EASE NHS WAITING TIMES

“We're getting an older population with more complex medical needs and there's an enlarging demand, which leads to a bigger impact on finances which is a finite resource. The NHS needs to work smarter and not necessarily harder which is what currently seems to be expected.”
“The pressure on the NHS staff is horrendous and that's from CEOs downwards. Everybody's getting pressure and they are being pushed to work harder. Well, you can't push somebody to work more than 100%. And if they've been working 100% since before COVID and that lapse that we hoped would happen after COVID, that little bit of space to reconfigure and regenerate ourselves never happened.”
COMMUNITY ENGAGEMENT IS NECESSARY TO BUILD TRUST IN NEW SYSTEMS
To engage with these communities and ensure that the right care is going to the right places, RMI use the latest data and research including the National Audit Office statistics to highlight the disparities in care, both regional and socioeconomic etc.
Health Industry Leaders heard: “We look at those [statistics] to see where the biggest need is. However, we're also trying to engage locally with the ECB and the Trust.”
However this is not always as easy as it seems, particularly when it comes to procurement and tender processes across the NHS. Often delays, legislation hurdles, and policy direction changes can prove to be a bottleneck to implementing new solutions.
Simon explained: “That's our biggest challenge. We know where the issues are, we know the areas they are happening, we know the type of issues, and we have the partners already in place to help us deliver it.”
Proving the business case in other fields Simon rounded up by explaining: “We're all over the world, so we work with big industries and medical providers all over the place. We provide a managed service so we can go onto a ship in the middle of the ocean that might be doing a hydrographic service or an eye team in the Antarctic or people on exploratory rigs. We have the ability to have a medic on site who's fully trained to look after their staff and have that reach back to consultants based all around the world to give them advice.”
15
The Data Principal

Imagine a world where all your health data is accessible wherever you are. Not only will our healthcare system be completely transformed, but the health and happiness of the population will also dramatically improve. And the good news is that the prospect of achieving this ideal (and avoiding the pain of not doing so) is closer than you may think.
THE DATA
At Evergreen Life we refer to this datacentred approach as ‘People Powered Health’. It empowers people to access and control their own health record, and add to it their own records, which include changes to diet and lifestyle that will enable them to avoid disease and improve wellbeing.
A cornerstone of this personal data will be your DNA. Widespread testing – ideally at birth – would enable everybody to understand how their DNA impacts on their wellness, and know what diet, exercise and medication would be best for them.
DNA data and information about any health-related assessment or intervention would be recorded in one place, and this would be curated by us all and include information about the diet and lifestyle changes we make. From this individuals and medical professionals will get a full picture of a health position, what’s influenced it, likely outcomes and what can be done to change the outcome. It’s not necessary to try everything to stay healthy – people can instead understand what’s likely to be most effective for them using AI driven from the complete data set.
16
ISSUE 3

And to build on this, everybody should have the opportunity to volunteer their data for research to help them and others like them - to be ‘data donors’. No longer will it be necessary for clinics to recruit people onto trials and request records from GPs. Instead, it will be easier to select and engage with data donors, who’s health information will be stored online, enabling small trials for rare diseases up to high volume programme research.
Where this approach materialises is almost irrelevant, whether it be through an app, the cloud, or maybe in the future a virtual reality headset. What’s important is the accessibility of the data so that it can be easily shared, when and where needed.
THE PAIN
Today this accessibility to data is something we don’t have. People don’t have complete health records – even in the NHS when the opportunity should be greater than anywhere else. And the situation is getting in the way of providing good healthcare. For example, it’s estimated that 70 per cent of people in hospital are impacted by an error in relation to healthcare professionals not having access to the full picture. And lack of data can result in more inpatient days in hospital, or even be the reason why someone is there in the first place.
It's easy to see how this has come about. As our ability to do more diagnostic testing increases so does the amount of data that’s produced. What’s limited is our knowledge of what to do with it. We’re doing a fraction of what’s possible – no individual can deal with the sheer volume of data available. However AI can. And it can translate it into a usable format that enables us to take positive action as a result.
In some cases, it’s not even necessary to delve into the detail to that degree. It’s more a case of enabling enhanced visibility and sharing insights already available. One particular example of this really sticks in my mind. Back in 2017 when Evergreen Life was working with a test cohort for our app, one individual lady was under the care of seven different specialties across Greater Manchester –ranging from treatment for rheumatoid arthritis to being fitted for a pacemaker and even having had one eye removed. When her condition deteriorated and she was due to have the second eye removed we suggested sharing her personal health record on the app with health professionals at her multi-disciplinary meeting. As a result it was uncovered that she actually only had one condition, which she then received treatment for, and was able to regain and retain sight in her remaining eye for the rest of her life.
17 BY STEPHEN CRITCHLOW HIL
STEPHEN CRITCHLOW
Health records can be merged today, however often not in a way that makes it efficient to analyse the millions of pieces of data available about DNA, diet and lifestyle, medications and interventions.
The potential benefits of intelligently and innovatively applying AI and capabilities of large language models are twofold. Firstly, people will know more about themselves than ever before. And not just the facts, but also what they mean for them and what action they can take to improve. At the same time, medical professionals will have all the information needed for effective decision making, in front of them, in a language they understand. Together this will prevent disease, improve outcomes and reduce pressure on our struggling NHS.
THE TREATMENT
Everybody has a part to play in making this a reality. Namely just by believing that it is possible and worthwhile – and I believe both to be true today.
Health professionals will begin to behave like better access to more complete records is the norm by asking people “Have you got your personal health record with you?”. Similarly, hospitals, care organisations and private clinics will start to think, how can I give this person all the information that will be helpful in the future as they leave the service?
IT providers will enable it to happen by focusing on personal health records (PHRs) rather than electronic patient records (EPRs) or electronic health records (EHRs). However, this doesn’t need to be an instead of. EPRs have a purpose defined by the healthcare provider that’s for them. But as well as this they do need to think about the PHR interface. For example, development of a standard transfer of care document would help. And as large language models are increasingly adopted the need for this would decrease. The ideal is for systems to link in a seamless and automated way which reduces effort and increases efficiency.

18
Earlier in my career my role as a Pharmacist involved in electronic prescribing and medicines management crossed many interfaces of a hospital and the wider care system. Different departments were unfortunately rarely motivated to speak with each other about findings – and consequently, systems didn’t talk to each other and levels of care suffered as a result. Today solutions are increasingly being put into place to integrate, however with there often being over 200 different department systems, the challenge is immense.
Central to my move to build Ascribe (the largest supplier of secondary care software to the NHS) to help solve this problem and later set up Evergreen Life, is the realisation that the answer lies in putting the person at the centre of everything.
THE OUTLOOK
In short, an approach focused on data will enable us to predict the future, know what to do to prevent disease, and improve outcomes.
In terms of when we can achieve this – at Evergreen Life we’re doing it, right now. Our app-based PHR enables people to control their own health records, access personalised wellness advice, discover actionable insight from their DNA and offer data for costeffective research to help them and others like them, today.
This just needs to happen on a wider scale across the whole healthcare system.
Of course, striving for improved outcomes is always a journey. Over a million people have downloaded the Evergreen app so far. And as for People Powered Health being the norm, I expect we’ll see that fully in about 10 years.
There’s no need for us to be content at imagining a world where all data about your health is accessible by you. Together we can make it happen, simply by putting the person at the centre of all health information.
WIDESPREAD TESTING WOULD ENABLE EVERYBODY TO UNDERSTAND HOW THEIR DNA IMPACTS ON THEIR WELLNESS, AND KNOW WHAT DIET, EXERCISE AND MEDICATION WOULD BE BEST FOR THEM
19
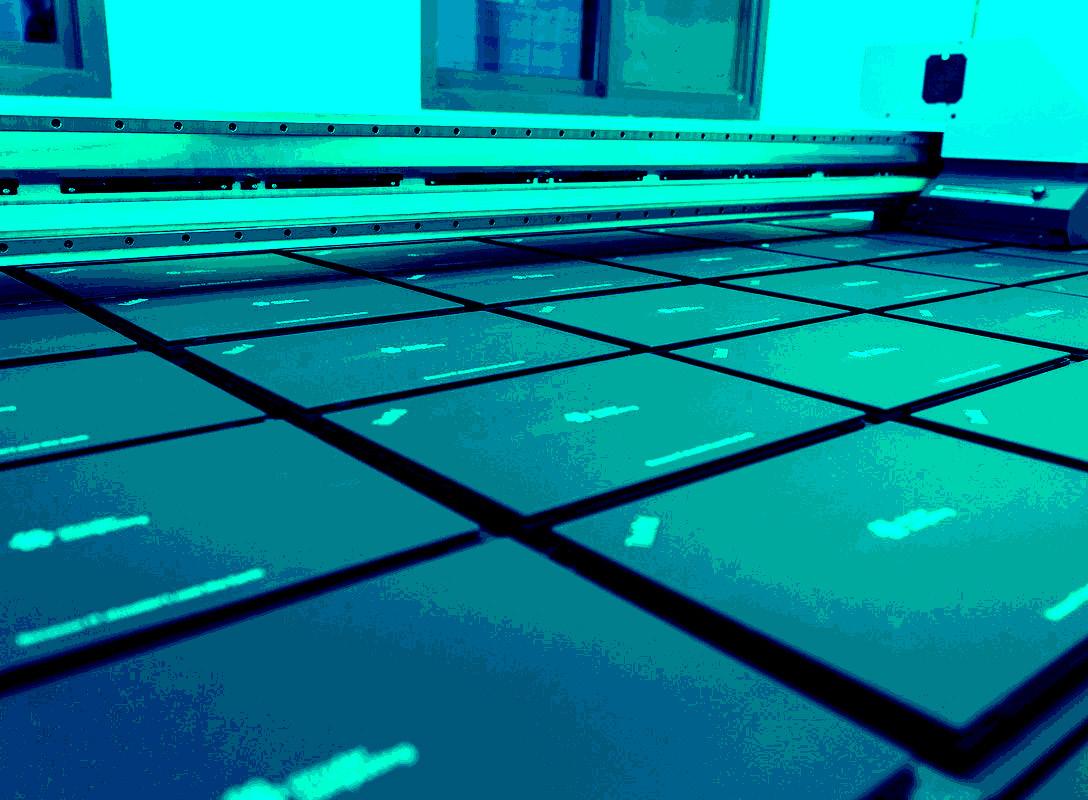
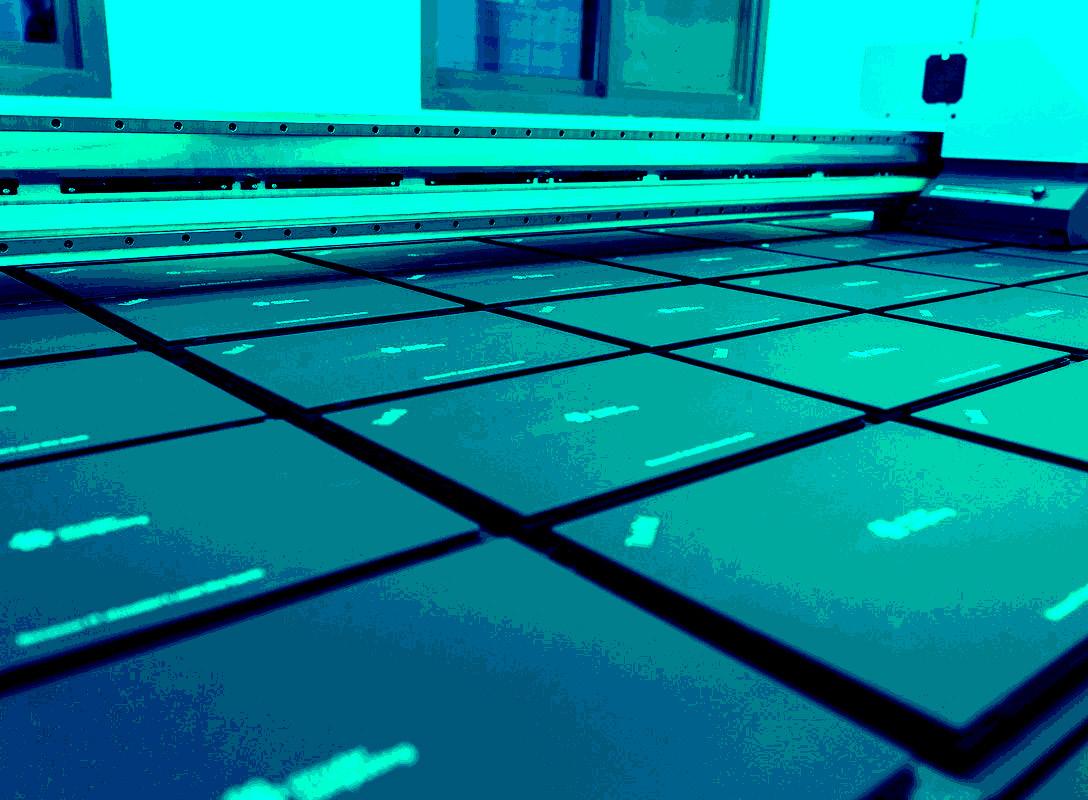
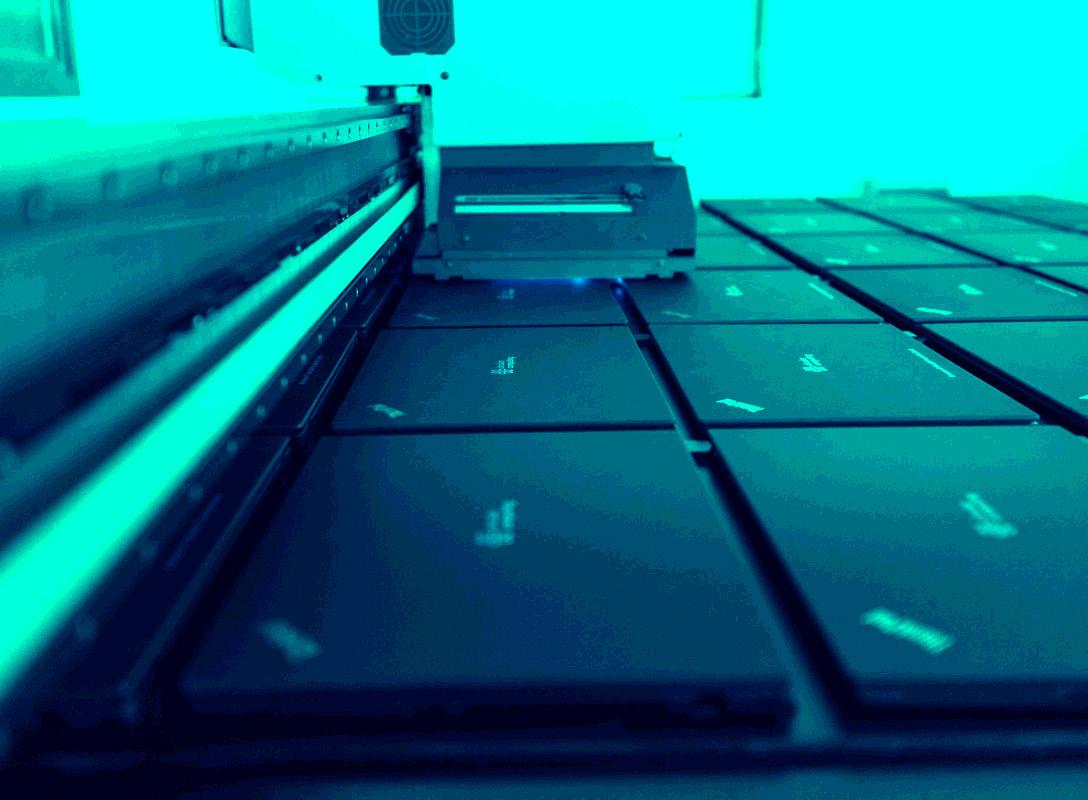
EMBRACING REMANUFACTURED LAPTOPS FOR A GREENER NHS




The IT industry contributes 2% of global carbon emissions per year
The NHS must move away from using single-use products
The healthcare sector could introduce a circular economy through implementing remanufactured technology

At a time when budgets are being cut and healthcare staff are under pressure to deliver high levels of service with a lack of resources, the NHS needs to make sure it applies its limited resources carefully to ensure it is able to deliver the best possible care to its patients.
20 ISSUE 3 SUSTAINABILITY

When it comes to its technology use, it is estimated that the NHS probably has a million laptops within the organisation. With the average cost of a new laptop being anything up to around £1,000, it needs to find a way that it can save on its technology.
Seeing savings here could free up money to be invested directly into main areas of its service like public healthcare.
One promising solution to mitigate cost is opting to remanufactured laptops rather than purchasing new ones. With this, there will be a 40% saving straight away against the cost of buying brand new.
THE MAJORITY OF CARBON EMISSIONS FROM LAPTOPS COMES FROM PRODUCING THEM
According to Circular Computing, more than 272 million new laptops are manufactured annually. This equates to it contributing 2% of global carbon emissions.
Steve Haskew, Head of Sustainability & Social Leadership at Circular Computing explained that the application of remanufactured technology presents the possibility to transform the healthcare sector into a circular economy.

Emphasising this transformation potential, Steve said: “NHS England’s strategy is looking to drive sustainability into their business and that filters all the way through it. One of those workstreams is IT, which is itself particularly linear as we have a habit of refreshing our technology with new. However, this is bad for the environment.”
It is carbon-intensive to make a laptop, and through Circular Computing’s research of 230 specific laptops, it discovered that “the average CO2 emissions during production of a new laptop is 331 kgs.”
Manufacturing a laptop is between 75% to 85% of the overall carbon footprint, with most of the emissions coming from the production and materials used to create the laptop.
TRANSITIONING TO REUSING PRODUCTS IN THE HEALTHCARE SECTOR WILL BE A GRADUAL SHIFT
Elaborating on the need to become more sustainable, Steve expressed: “There are thousands of different materials involved in the production of a laptop. These materials need to be refined, smelted, and processed. These then need to come together to be made into the laptop, and then shipped. That is about a third of a tonne of carbon per laptop, and around 190,000 litres of water required.”
BY CHELSEA BAILEY HIL
21
“IF THE MAJORITY OF YOUR WORKFORCE DON’T NEED THE LATEST TECHNOLOGY TO DO THEIR JOB, WHY NOT USE REMANUFACTURED TECHNOLOGY?”
This amount of carbon being created by laptop production highlights the urgency for a shift towards reusing materials, as without laptop technology, the healthcare sector can’t operate and therefore, can’t provide the care it needs to.
Steve expressed how the NHS could make a gradual transition away from producing waste: “It is going to be a generational shift, and won’t happen overnight. We need to think of how we can minimise single-use products like gloves, gowns, bed curtains, and heavy-duty and intensive technology.”
The environmental impacts and health risks that are associated with healthcare waste have increased the demand for reuse and recycling. By ensuring that the NHS moves away from using single-use products, it could reduce its carbon emissions greatly.
CIRCULAR COMPUTING HAS SUPPORTED KING’S COLLEGE HOSPITAL TRUST IN REDUCING ITS EMISSIONS
Showing the potential of utilising remanufactured technology, King’s College Hospital Trust was recently tasked with delivering a new Electronic Patient Records system (EPR).
Being one of the biggest NHS Trusts in the UK, King’s College Hospital Foundation Trust services a population of over 1 million people.
To implement this new system, it identified that training would be needed for 12,000 of their frontline support staff on the new EPR system. However, found that there were no spare laptops available for this training
On how Circular Computing supported the Trust with this project, Steve illustrated: “It is a big organisation so adopting change for them wasn’t going to be an overnight thing, it had to be managed. To train the 12,000 people on its new system, we rented them 400 Dell Latitude Laptops in one of the hospitals in South East London over the course of a year. With this, they were able to train all of their staff.”
Not only did the implementation of this technology help the Trust with its operational
22 EMBRACING
REMANUFACTURED LAPTOPS FOR A GREENER NHS
performance and cost-savings, but benefited the Trust with significant sustainability benefits, helping them to reduce their environmental impact.
IMPLEMENTING REMANUFACTURED TECHNOLOGY WON’T HAVE A DETRIMENT ON GOOD PATIENT HEALTH
Addressing concerns regarding patient care, Steve clarified that established technologies like laptops will not compromise the quality of healthcare when remanufactured.
He said: “When it comes to specialist technology that requires the latest innovations that aren’t available via old technology, then absolutely you require the latest technology. However, when it comes to established technology like laptops, all the work is done via the cloud.”
Therefore, unless the member of staff needs to use the best technology to deliver their service, implementing remanufactured technology would present no problem for them.
To provide confidence for healthcare professionals using remanufactured technology, there are certifications in place.
Giving an example, Steve revealed: “Generators that hospitals use may be a remanufactured device from the provider, it won’t be brand new all of the time. However, with this, the hospital has to have the assurance that this technology is reliable. The only way you can guarantee that is by being told by a third party, and that is where the BSI Kitemark for us plays an important role.”
According to Circular Computing “the awarding of the BSI Kitemark™ certifies that our Circular Remanufacturing Process produces products ‘equal to or better than new’ as required by the BS standard BS8887-220 and BS8887-211.”
This confidence will be fundamental to ensuring that remanufactured technology is being implemented into the NHS more consistently, and therefore, can really make a difference to reducing its carbon emissions.

23

Health Sector Round Up
SYSTEMS AND INFRASTRUCTURE


The next generation of nurses and healthcare staff are set to benefit from the launch of a new lab at Solent University.
The Human Health Lab has been built with funding from the Office for Students and will be crucial to making sure more world-class nurses bolster NHS workforces across the country.
Moving away from on-site facilities, digital-first home healthcare provider Cera have partnered with Google Cloud to enhance real-time insights and better address the UK’s home healthcare needs.
Utilising Google Cloud’s technology has enabled carers to access near-instant insights into a patient’s condition, allowing them to act accordingly and appropriately.
The ability to access long-term historical changes to patients’ wellbeing, as opposed to only assessing data from the previous visit, offers greater insights into how their health is evolving and changing over time.

PROFESSIONAL INSIGHTS

And, as the NHS approaches its net zero goals, Surrey and Sussex NHS Trust have set their sights on reducing their carbon footprint and saving money by targeting paper and lighting in two climate-friendly initiatives.
Together, the two initiatives are saving the trust approximately 86 tonnes in carbon emissions, as well as monetary savings of around £45,000 a year.

The NHS Confederation has said it is launching new research to better understand the barriers to harnessing preventative healthcare within integrated care systems.
As part of the work, prevention measures being carried out at system, place, and neighbourhood level will be mapped out, with a focus on what stops collaborative prevention.
The NHS Confederation’s final report will be accompanied by a toolkit that will feature practical examples of how to overcome these challenges and drive population health.
Digital skills were also a topic of conversation over the last month, with the NHS North London Mental Health Partnership is helping to upskill its workforce and progress in digital transformation through the launch of a new digital academy.
Currently, the academy has trained more than 50 staff across every area of its organisation, with another 50 expected to enrol by March 2024 as the partnership looks to maintain momentum in its digital journey.

Finally, the way clinicians approach sepsis has been reviewed, as The National Institute for Health and Care Excellence (NICE) has stated that the use of antibiotics for possible sepsis should be more targeted.
NICE has recommended that clinicians use the NHS England-endorsed National Early Warning Score that was developed by the Royal College of Physicians to identify acutely ill patients.

ISSUE 3 SUSTAINABILITY
24

PATIENT IMPACT


In the patient news over the past month, the NHS has seen their first patients have received an experimental vaccine which health leaders think could revolutionise c ancer care and treatment.
Using mRNA technology, the therapy is being delivered, and it will target melanoma, lung cancer and other ‘solid tumour’ cancers.
For a broader demographic of patients, a study has shown that an NHS-led charity has helped to tackle health inequalities through its work to deliver digital inclusion services to more than 2,000 vulnerable people in London.
The digital inclusion programme has three pilots with the aim of improving digital access to health, care, and community resources.

And, in an attempt to bolster primary care services, NHS England has launched a new campaign aiming to drive awareness of the new capabilities in high-street pharmacies.
It announced that pharmacies would begin offering treatment for seven common conditions, including sinusitis, sore throat, earache, infected insect bite, impetigo, shingles, and uncomplicated urinary tract infections.


25 HIL
WEBINARS
Finding the Quick Wins in the Hunt for Net Zero


How Technology Can Reduce A&E Waiting Times

Building New Hospitals With Net Zero in Mind

Coupling Social Value With Decarbonisation
26 UPCOMING
27 PODCAST OUT NOW PODCAST OUT NOW PODCAST OUT NOW
We believe in providing comprehensive insights that transcend industry boundaries. We invite you to delve into the expertise offered by our other publications - Hydrogen Industry Leaders and Housing Industry Leaders - each dedicated to the pursuit of net zero solutions.
You can also follow us on LinkedIn and X (Twitter) to keep up to date with all the latest news in the Health sector.
ABOUT US WE ARE
28
ISSUE 3

29 HIL
PREVIOUS ISSUES
PREVIOUS ISSUES
PREVIOUS ISSUES
PREVIOUS
PREVIOUS

ISSUES
ISSUES
PREVIOUS ISSUES

30
PREVIOUS PREVIOUS PREVIOUS