PEGASUS SMALL GROUP EDUCATION PROGRAMME
IMPACT REPORT
2023




This report was prepared by Pegasus Health It is not intended to compel or unduly influence independent choices made in developing health care policy or practice The resource remains the intellectual property of Pegasus Health This material is not to be redelivered, on sold to any individual or organisation, or made publicly available on any website or in any publication, without written permission from Pegasus Health (Charitable) Ltd
© Pegasus Health (Charitable) Ltd May 2024
Small group brings all the GPs, the health professionals up to speed and allows that time for reflection and support so it benefits both patients from a clinical point of view and the health professionals from a support point of view
General Practitioner

EXECUTIVE SUMMARY
We are excited to bring you the first impact report for the Pegasus Small Group Education Programme (SGEP)
The Small Group Education programme (SGEP) delivers high quality, group-based clinical education for primary health clinicians. The programme supports clinicians with up to date, evidence-based knowledge and resources about topics relevant to clinical practice. Since the inception of the programme in the early 1990s, the breadth of impact of the programme has expanded significantly beyond its initial focus on the optimal use of laboratory tests and pharmaceutical prescribing Mid 2023, with the support of Kin Strategy and Research, an external agency specialising in social impact, we embarked on a journey to better understand, measure and report on the expanded impact of the SGEP.
Our impact analysis was informed by an in-depth analysis of the SGEP 2023 output, outcome and impact data as derived from attendee interviews, meeting feedback and post-topic surveys, and was supplemented by a review of the relevant academic and practice-based literature, historical SGEP insights and conversations with key stakeholders and industry experts This impact work had several outputs which are showcased in this report

Pegasus Health Small Group Impact Report| Page 5
Our analysis provided key output highlights of the SGEP for 2023, including:
SGEP attendance grew by 15% compared to 2022, with almost 1000 clinicians attending the programme. This increase is particularly significant given the continued pressure on clinicians’ time, reflecting the value clinicians place on the programme.
Clinicians from 87% of general practices and community pharmacies in Canterbury attended the SGEP and received latest best practice knowledge. The wide coverage across general practices and community pharmacies means that the SGEP keeps much of the Canterbury primary care workforce up to date.
Attendance in multidisciplinary Small Groups increased by 90%. This increase reflects a movement towards interdisciplinary learning and ways of working, which is significant as it aligns with national initiatives around establishing comprehensive primary care teams.
Across the five topics delivered in 301 small group sessions in 2023, the quality and relevance of SGEP sessions was consistently rated highly with an aggregated score of 4.5 out of 5.
Our analysis provided further insight into the incredible value and contributions of the SGEP beyond these output statistics. It highlighted how much clinicians value having an ongoing professional development programme that provides them with up-todate, reliable, research-based evidence on topics of key relevance to their daily practice
“[In] a Small Group setting not only do you get all the research that’s gone on and the background to all that up-to-date information, but you also get other people’s ‘how to’s’ and experience and that can be as valuable as the hand-outs; a GP giving some feedback on what they did or how they managed things can be really helpful ”
- General Practitioner
“Often, sharing difficult patients or situations or just how hard it can be is a helpful thing - that peer group kind of support”
- General Practitioner
Page 6 | Pegasus Health Small Group Impact Report
The interactive, discussion-based model of delivery complements the research-based content of the SGEP, so clinicians benefit from the experience of those in their peer group.
The peer group format provides professional support, thereby increasing clinicians’ confidence and reducing a sense of professional isolation
“Primary care is incredibly isolating. We see patients every 15 minutes in this room, and you don’t really have much do with other people ”
- Nurse Practitioner
“I am part of a multidisciplinary team group, so that also allows me to see the world through the pharmacist’s eyes and that sort of thing which is always valuable”
- Practice Nurse
This, in turn, supports the retention of skilled and experienced practitioners within the health system.
The multidisciplinary nature of the content development and the opportunity to learn from others in the primary care workforce through participation in multidisciplinary Small Groups ensures that clinicians grow their understanding and connections across disciplines.
As such, the SGEP impacts not just the individual clinician but the wider workforce and the health care system as a whole It contributes to a connected, supported and more resilient clinical workforce; a workforce that is not operating in silos, is able to provide consistent messaging to patients, and can better guide patients and whānau to the right primary care providers within the wider health system.

Our analysis also shows the flow on benefits of the SGEP for quality patient care and resource-use within the primary health care system overall.
These SGEP impacts are particularly relevant given the current challenges facing the health care system (like, significant workforce shortages, high burnout rates, increase in complexity of primary, health inequity). And we advocate for expanding the programme to other regions in Aotearoa New Zealand, to grow and scale these positive impacts of the SGEP programme in the near future.
Pegasus Health Small Group Impact Report | Page 7
“Because it is the same group of people, you get to know them, you feel comfortable with them, you feel comfortable with your leader. And it just becomes this open space where you can discuss so many things – the topic, but you can also discuss other things. It’s just a really important space. A comfortable space”
- Community Pharmacist
Internally, these insights informed the development of four up-to-date impact goals for the SGEP, which our outlined in more depth in the report:
The 4 impact goals are, The SGEP;
Keeps clinicians up to date with the latest clinical evidence and support best practice decision making
Creates a more resilient primary care workforce that feels confident and supported in their clinical practice
Helps build a more connected primary care workforce that is not working in silos
Supports optimal resource use and reduces unhealthy variation
In addition, our impact analysis informed the development of a robust SGEP impact model and measurement framework, both of which will improve our ability to measure, report, communicate and grow our impact going forward.
Louise Kennedy Service Manager, Clinical Quality & Education, Pegasus Health
Page 8 | Pegasus Health Small Group Impact Report
ACKNOWLEDGEMENT
This report was written in collaboration with Puck Algera, PhD, from Kin Strategy and Research. We are very grateful for Kin’s expertise, guidance, and support.

Pegasus Health Small Group Impact Report| Page 9
Executive Summary | 5
Acknowledgement | 9
Introduction | 11
Background and History | 14
Our Unique Approach | 15
Key Programme Features
Small Group Topic Development
Our Commitment and Impact Goals |18
Our Impact Goals
Our Place in the System
Our Impact Model | 20
2023 Impact Highlights | 22
Key Output and Impact Highlights 2023 2023 Key Insights per Impact Goal
Looking ahead | 42
Summary Reflections | 43 Appendices | 45 Small group Topics delivered in 2023
Alignment with Te Whatu Ora and UNSDGs
The SGEP Theory of Change

Contents
1.
2.
3.
4.
Impact Investigations 2023
References | 50

O UC O
The Small Group Education programme (SGEP) delivers high quality clinical education for primary health clinicians. Since the inception of the programme in the early 1990s, the breadth of impact of the programme has expanded significantly beyond its initial focus on the optimal use of laboratory tests and pharmaceutical prescribing. While this initial focus led to significant savings to the healthcare system ($85 million was returned for reinvestment into healthcare programmes), participant feedback and anecdotal evidence indicated that the SGEP also provides other significant value to primary health professionals in Canterbury and beyond.
Mid 2023, we embarked on a journey to better understand, measure and report on the impact of the Small Group Education programme It was important to us to define up-todate impact goals for the programme and lay the foundations for evidence-based reporting on our impact. In addition, we wanted to grow the team’s capability around understanding and measuring social impact and identify areas or ways in which we can scale our impact
Pegasus Health Small Group Impact Report | Page 11
Understanding our impact
For the first phase of this work, to understand the breadth of impact, we did an indepth evaluation of past and current participant feedback on the programme; we held workshops with key internal and external stakeholders to discuss the value and contribution of the programme (e.g. Pegasus Clinical Quality & Education team, primary care clinicians, senior leaders from Te Whatu Ora Waitaha and Te Waipounamu, Manatū Hauora, and Pegasus Health); and we did several in-depth interviews with primary care clinicians further exploring topic and programme specific areas of impact. We also analysed the direct and longer-term impact of three specific programme topics, “Manawa Ngoikore - Heart Failure”, “Improving Early Cancer Diagnosis in Primary Care” and “Supporting Healthy Weight”, in more depth.
The output of this phase was the definition of four main impact areas and goals of the Small Group Education Programme.
The SGEP aims to:
Keep clinicians up to date with the latest clinical evidence and support best practice decision making
Create a more resilient primary care workforce that feels confident and supported in their clinical practice
Build a more connected primary care workforce that is not working in silos
Support optimal resource use and reduce unhealthy variation
These are elaborated on in the Impact Goals section of this report. We also developed an impact model (Theory of Change) for our work, which defines, based on the evidence gained in this phase, the logical steps through which the SGEP creates impact (see appendix 4)

Page 12 | Pegasus Health Small Group Impact Report
Measuring our impact
For the second phase of this work, to measure our impact, we developed a measurement framework based on the goals and impact model defined in phase 1 This meant an in-depth evaluation of possible measurement indicators with internal and external stakeholders and experts, and a review of existing and potential data collection methods. The result of this phase was the creation of an impact measurement framework and strategy.
Reporting on our impact
The impact measurement framework and strategy are being implemented in the first quarter of 2024 This means that when it comes to reporting on our 2023 impact, we cannot yet provide a comprehensive impact report as it relates to our newly defined impact goals. But we can provide our output and impact highlights as derived from our 2023 feedback and attendance data These highlights can be found here. Our 2024 impact reporting will be (even) more comprehensive and aligned with our impact goals.

A new name for the programme
Alongside our revised impact goals and new impact framework, the programme is changing its name in 2024. The new name is Clinical Connect – Peer Education Programme, this honours the programme’s history and founding principles, and emphasises the ‘connection’ that is built through the people-centric and multidisciplinary nature of the programme - as also reflected in our revised impact goals. Our programme website is https://clinicalconnect.nz/.
BACKGROUND AND HISTORY
The Pegasus Small Group Education Programme (SGEP) delivers education to primary health professionals in peer groups. A peer group of 12-15 clinicians meets once every few months face-to-face to discuss a clinical topic and will go through a series of 5 topics throughout the year The same group make up is retained throughout these topics and groups often stay together for multiple years, sometimes even 20 years or more This supports reflective, interactive, and sometimes challenging discussions that benefit knowledge building, skill development and maintaining confidence in clinical practice. It also supports creating connections and (interdisciplinary) teamwork. This Pegasus programme currently attracts almost 1000 primary care clinicians in Waitaha across general practice and community pharmacy each year
While the initial programme focused primarily on peer groups for general practitioners (GPs), since its inception in the early 1990s, the SGEP has expanded to include practice nurses (1998), community pharmacists (2010) and nurse practitioners (2015). Small Groups can consist of one profession or multiple, with an increasing demand for multidisciplinary groups
Small Group topics are selected to focus on areas of clinical practice that are: complex (often with significant uncertainty about optimal practice), relevant to primary care clinicians, and of strategic importance to the wider health system.
This includes looking at the best practice use of resources, such as laboratory tests and pharmaceuticals, and exploring the wider social determinants of health that impact best practice clinical care. All Small Group topics reflect the input from clinicians with different professional backgrounds and clinical expertise By providing the same learning objectives and take-home messages across all meetings (regardless of group professional makeup), we support the development of a clinical workforce that is on the same page This approach ensures that patients and whānau receive consistent, aligned clinical messaging wherever they turn up in primary care – general practice or community pharmacy
Page 14 | Pegasus Health Small Group Impact Report
OUR UNIQUE APPROACH
Certainly, that’s what makes it different to just going to a webinar – which is usually run by a specialist who doesn’t work in general practice and doesn’t deal with patients where they are
General Practitioner

Pegasus Health Small Group Impact Report | Page 15
Key Programme Features
The SGEP uniquely brings together practising GPs, Nurse Practitioners, Practice Nurses and Community Pharmacists in small peer groups, which enables them to learn together and improve their practice. The SGEP has several key and distinctive features:
It is independent: we develop and deliver our own education topics in-house so that content can be trusted and clinical decision making in primary care is not influenced by commercial interests (such as pharmaceutical company sponsorship) (1)
It is peer-led: peer primary care clinicians are trained to research, write, and deliver the SGEP topics This unique approach ensures that content is relevant and impactful for our primary care workforce
It is evidence-based and informed by local data: we review the latest research and look at local data on laboratory tests, pharmaceuticals, and referral patterns to identify gaps between current practice and best practice evidence and areas for improvement (2)
It covers challenging and interesting topics: we focus on the uncertain areas of clinical practice, selecting topics which focus on those areas of clinical practice that will benefit from a combination of understanding the evidence, peer discussion, and shared experiences
It applies a health equity lens: we consider, highlight and discuss relevant health equity issues and/or challenges throughout the sessions for each topic
It is multidisciplinary: every professional group receives the same learning goals and take-home messages regardless of professional background, this ensures consistent messaging for patients and whanau. The multidisciplinary nature also increases connections and collaboration across different primary care providers (3, 4)
It is interactive and discussion based: our education model supports the best practice in adult learning It provides opportunities for reflective and discussion-based learning, and supports participants to identify and apply improvements into their clinical practice (5)
Page 16 | Pegasus Health Small Group Impact Report
Small Group Topic Development
Small Group topics are selected to focus on uncertain, complex areas of clinical practice relevant to primary care clinicians and of strategic importance to the wider health system. Appendix 1 provides an overview of the 2023 Small Group topics. The programme is accredited by the Royal New Zealand College of General Practice and meets the professional development requirements of nurses and pharmacists.
Small Group topics are developed by the Clinical Quality & Education (CQE) team who consult widely with other Pegasus teams, clinical experts, secondary care clinicians and other relevant parties. The content development team are peer clinicians, many with current or recent clinical experience. The multidisciplinary CQE team role models collaborative teamwork and includes perspectives from general practice, pharmacy, nursing, public health, physiotherapy, and academia
In advance of each topic, SGEP participants receive a pre-reading that summarises relevant background information on the topic in preparation for participating in the peer meeting. The meeting focuses on interactive discussion usually based around 1 or 2 case studies or scenarios A tailored handout for the topic is also provided that summarises helpful resources to use with patients and whānau, or for further learning. Continued access to these resources after the sessions is provided through our Te Rau Ako learning platform

Feedback is collected and reviewed after each meeting to ensure continuous improvement Feedback is used for identifying learning needs, choosing future education topics, and ironing out any technical or operational issues In addition, feedback is used to assess the participant's intention to change and improve practice as a result of engaging in the session. Ideas for system improvements identified within the feedback and topic development processes are actively followed up e.g. suggesting changes to processes or referral pathways that may potentially improve patient care We maintain a 4/5 or higher ranking for overall quality of our meetings and review anything lower in finer detail.
Pegasus Health Small Group Impact Report | Page 17
OUR COMMITMENT AND IMPACT GOALS
Our Impact Goals
We are committed to positively supporting our primary care workforce. We have four main impact goals for the programme:
The SGEP keeps clinicians up to date with the latest clinical evidence and supports best practice decision making
The SGEP creates a more resilient primary care workforce that feels confident and supported in their clinical practice
The SGEP helps build a more connected primary care workforce that is not working in silos
The SGEP supports optimal resource use and reduces unhealthy variation
These impact goals positively impact and support the transformation of the Aotearoa health system. The Pae Ora (Healthy Futures) Act in 2022 laid the foundation for the current health system transformation, setting the direction for a system that is equitable, accessible, cohesive and people centred.
Page 18 | Pegasus Health Small Group Impact Report
Te Pae Tata (NZ Health Plan) further outlines the plan for the next two years The SGEP promotes a connected, informed and supported primary care workforce which contributes to this transformation as it progresses.
The programme also supports the United Nations Sustainable Development Goals, and in particular Goal 3: Ensure healthy lives and promote wellbeing for all at all ages
For more detailed information on how the 2023 SGEP topics relate to these areas and goals, see appendix 2.
Our Place in the System
Our commitment and our impact goals are relevant in the current Aotearoa New Zealand health system which is facing a number of challenges
Significant workforce shortages are well recognised across general practice, practice nursing and community pharmacy and will likely worsen in the short term with high rates of retirement forecasted (50-55% of our GPs and nurses intend to retire within the next 10 years), higher pay offered in secondary care and in Australia, and many leaving the profession Burnout rates for health professionals are also high and cited as a reason for leaving (6-9).

Thresholds for accessing specialist and secondary care continue to increase, thereby raising the demand for primary care and increasing the complexity of patients. Collaborations between primary care providers are increasingly vital to continue to improve care, particularly for vulnerable populations, and to work towards health equity for all. Together these factors are driving the development and rapid uptake of new or expanded professional roles, such as nurse/pharmacist prescribers, and a need for clinicians to be supported to work at the top of their scope as well as across the full breadth of their scope
The multidisciplinary model of the SGEP supports national initiatives being introduced to manage increasing healthcare demands, such as the establishment of comprehensive primary care teams. Interdisciplinary learning is also recognised by the World Health organisation as an important strategy to support collaborative practice and respond to local health needs (4)
Pegasus Health Small Group Impact Report | Page 19
OUR IMPACT MODEL
An impact model describes the logical steps through which an activity or programme creates positive change The 2023 in-depth evaluation of the SGEP and its impacts revealed these (logical) steps for the SGEP. This impact model is elaborated on in words below. A visual representation in the form of a Theory of Change can be found in appendix 4.
Impact goal 1:
The SGEP keeps clinicians up to date with the latest clinical evidence and supports best practice decision making
TThis impact goal speaks to the impact on the knowledge and clinical practice of practitioners.
The information provided through the SGEP keeps clinicians up to date with the latest clinical evidence. Being up to date supports best practice decision making and, where relevant, leads to improvements in clinical practice. In addition, being up to date with the latest clinical evidence supports clinicians' ability to deal with complexity in primary care This in turns support the provision of improved, quality patient care
Impact goal 2:
The SGEP creates a more resilient primary care workforce that feels confident and supported in their clinical practice
This impact goal concerns the impact on the professional experience, feelings and resilience of the practitioner.
The format and the group-based nature of the SGEP creates a safe space for nonjudgemental reflection with peers about individual practice and offers an improved sense of support. By being able to share with peers and discuss difficult or complex situations, clinicians feel more confident in their own practice The group sessions further support a sense of connection with those in and outside own practice This in turn helps to reduce (or avoid) a sense of professional isolation and supports a more resilient workforce with improved retention.
These findings are supported by previous research, which shows that peer support and an opportunity to learn together improves professional connection and reduces feelings of isolation (10-17) This is particularly relevant in rural areas (12, 18) In turn, this supports the retention of the primary care workforce (13). The literature further identifies professional isolation as a red flag for professional burnout and as an antecedent to not following best practice (17, 19-21).
Page 20 | Pegasus Health Small Group Impact Report
Impact goal 3:
The SGEP helps build a more connected primary care workforce that is not working in silos
TThis impact goal concerns the impact on the primary care workforce as a whole.
The multidisciplinary nature of the SGEP supports sharing perspectives and growing interdisciplinary understanding. It also aids solving problems, continuous improvement and diffusion of knowledge across disciplines. The SGEP strengthens cross-discipline primary care connections and working relationships. This, in turn, assist clinicians in being better able to guide patients and whānau to the right people in the wider primary care team In addition, because the SGEP delivers the same messaging to all disciplines, clinicians can provide consistent messaging for patients and whānau in primary care. Finally, the multidisciplinary group nature of the SGEP also supports and assists those clinicians working in, or towards, advanced and/or top of scope practice.
This all leads to a more connected primary care workforce, which is working together and not in silos to provide consistent, quality care for patients and whānau.
Impact goal 4:
The SGEP supports optimal resource use and reduces unhealthy variation
This concerns the impact on the optimal use of resources in the health system and cost savings to the health system.
Better clinical decision making, and improved patient care (see previously mentioned impact areas) will optimise the use of resources, as well as reduce morbidity and the associated costs In addition, having up to date clinical knowledge and knowledge sharing between professionals reduces unhealthy variation in clinical practice. For example, depending on the topic, the knowledge or information provided in the sessions may lead to the early detection of new and/or worsening illness; improved management of long term conditions; prevention of harm caused by over-or underuse of resources like pharmaceuticals, tests or referrals; improved participation in screening; reduction in unhealthy variation in clinical practice; in turn leading to reduced morbidity, improved quality of life, and reduction in hospitalisation. All impacting positively on the reduction of health system costs.
Note: resource use optimisation does not necessarily mean resource or cost savings in the short term. For example, the information provided for certain topics may initially increase the use of a resource, like an increase in uptake of bowel cancer screening. This will initially lead to more costs, but prevention or early detection may lead, in the long term, to health system savings
Pegasus Health Small Group Impact Report | Page 21

2023 IMPACT HIGHLIGHTS
This initial impact report provides key statistics and impact highlights of the Small Group education programme in 2023.
For this report we drew on participation and attendance statistics, commentary provided by attendees, evaluation feedback provided after sessions, as well as several in-depth interviews with primary care clinicians (attendees), which explored topic and programme specific areas of impact. We also looked more in depth into the immediate and post-topic evaluation of three of the five topics delivered in 2023: “Manawa Ngoikore - Heart Failure”, “Improving Early Cancer Diagnosis in Primary Care” and “Supporting Healthy Weight” The reports on the topic specific investigations are available on request, see appendix 4 for more information
The first section here outlines key 2023 output and impact statistics, and the second section provides illustrative impact insights and quotes for each of the impact goals - as derived from our 2023 impact investigation
Page 22 | Pegasus Health Small Group Impact Report
Key Output and Impact Statistics for 2023
301 Small Group meetings were held across Canterbury in 2023
Five Small Group topics were developed and delivered in 2023, and On average 588 clinicians attended each topic
15% increase in Small Group attendance across Canterbury in 2023
Participation in the programme increased by a further 15% in 2023 compared to 2022. This increase is particularly significant given the continued pressure on clinicians’ time, reflecting the value clinicians place on the programme
We saw 2940 attendances compared to 2554 attendances in 2022
We saw an increase of 10% in unique primary care clinicians attending compared to 2022 (from 880 in 2022 to 968 in 2023)
Of the 968 unique primary care clinicians attending in 2023, 34% were GPs, 32% Practice Nurses, 29% Community Pharmacists, 2% Nurse Practitioner, 4% Other (see Figure 1)
Individuals attending Small Group programme 2023 by Professional Group
* ‘Other’ category includes general practice based paramedics, district nurses, school nurses, and health improvement practitioners attending a practice-based (rural) group These groups are not currently covered within programme funding GP 34% PracticeNurse 32% CommunityPharmacist 29% Other* 4% Pegasus Health Small Group Impact Report | Page 23
Clinicians from 87% of general practices and community pharmacies in Canterbury attended the SGEP and received latest best practice knowledge.
The SGEP keeps much of the Canterbury primary care workforce up to date This high coverage within the Canterbury region means that 87% of the general practices and community pharmacies in Canterbury have received, or have had access to, the latest best practice knowledge in clinical practice.
Attendance in Multidisciplinary Small Groups increased by 90%
In 2023 we offered the SGEP to four professional streams: General Practitioners and Nurse Practitioners; Community Pharmacists; Practice Nurses and Multidisciplinary groups
Attendance at the Multidisciplinary groups accounted for 21% of the programme attendances, this is a 90% increase from 2022
Participation in the Multidisciplinary stream doubled from 250 to 523 attendances (Figure 2)
Figure 2: Professional streams of Small Group education 2022 vs. 2023
Meeting Attendance per programme stream 2022 vs 2023
2022 2023 0 5 10 15 20 25 30 35 GeneralandNursePractitioner PracticeNurse CommunityPharmacist Multidisciplinary
Page 24 | Pegasus Health Small Group Impact Report
Traditionally, Multidisciplinary Small Groups have only been offered in rural areas (due to smaller numbers of clinicians in these areas) but in 2023 Multidisciplinary groups were introduced in urban areas in response to increased demand, and they are very popular. The request for Multidisciplinary groups often comes from those practitioners expanding their scope of practice and who are keen to learn from the experience of other professions, an example would be nurses or pharmacists who are moving into prescribing and practice-based roles.

This increase in Multidisciplinary groups is important because it also reflects the growing interest and acceptance of interdisciplinary learning and ways of working A multidisciplinary delivery of the programme aligns with national initiatives around establishing comprehensive primary care teams, which focus not only on improving patient care but also on managing the shortages of various professional workforces. This reflects a movement away from role specific planning and solutions to a collaborative approach to care, where members of the multidisciplinary team learn from, with, and about each other (4) In addition, Multidisciplinary groups allow for interdisciplinary connections to be made and aid in providing consistent messaging for patients and whānau across the healthcare sector. A better understanding of the roles of other clinicians within primary care further assists clinicians to better guide patients and whānau through the healthcare system
The quality and relevance of SGEP sessions are consistently rated highly among attendees with an average, aggregated evaluation score across all topics of 4.5 (on a scale of 1 to 5), see table below for individual topic scores. This aggregated evaluation score includes how attendees rate:
The quality of the information provided
The quality of the resources provided
The importance and relevance of content, and
The overall quality of the session
2023 Small Group sessions rated highly (4.5 out of 5)
Pegasus Health Small Group Impact Report | Page 25
Table 1 Aggregated evaluation scores for each topic delivered in 2023
TOPIC
In the attendee feedback, comments about the high quality of the information provided and the relevance to clinical practice were recurring
Attendees commented positively on the depth and reliability of the information provided
The breadth of information and topics addressed in the SGEP sessions are also valued highly by attendees
“My other main source would be something like the Goodfellow Unit, which gives me a lot of information on specific topics, but probably doesn’t open up the topic quite as widely as the Small Group education”
- Practice Nurse
“I like the breadth of information that I get exposed to. I know that a huge amount of research has gone in behind that and so I think I get a much bigger picture than I think I would get from anywhere else”
- Practice Nurse
“It’s all consistent information and it’s been backed up by evidence, you see it in the references and the background information, and I think that’s really important”
- Community Pharmacist
“But also having a topic that is often topical at the time. A lot of work has gone into it and you definitely notice it And if you need to go back to those resources, you’ve got that information there online to be able to do that”
- Community Pharmacist

HEART FAILURE 4.67/5 GUT HEALTH 4.45/5 IMPROVING EARLY CANCER DIAGNOSIS 4.46/5 NEURODIVERSITY WITH A FOCUS ON ADHD 4.44/5 SUPPORTING HEALTHY WEIGHT 4.49/5
EVALUATION SCORE
Page 26 | Pegasus Health Small Group Impact Report
The information package provided to clinicians at each Small Group session is considered invaluable by attendees Attendees reflected that they would otherwise not have known about these resources but importantly, they would also not have had the time to search for these themselves. The resources provided were not just helpful for the clinicians themselves but also for their patients:
“There are so many resources out there and if you have just been to a Small Group then there’s this [summary] leaflet Local resources are particularly useful”
- General Practitioner
“At the end of the session there are those lovely resources as well. So to be able to direct people [patients] to those resources is great”
- Practice Nurse
The inclusion of local data, information and resources was highly appreciated


Pegasus Health Small Group Impact Report | Page 27
2023 Key Insights per Impact Goal
While we did not yet have the new measurement framework in place in 2023 to allow us to report on each of the newly developed impact goals in depth, our evaluation of the 2023 impact of the programme provided the following impact insights and statements for each of the goals
The information provided through the SGEP keeps clinicians up to date, which supports best practice decision making and, where relevant, leads to improvements in clinical practice This in turns supports the provision of improved,qualitypatientcare.
The SGEP keeps clinical workforce up to date:
Our deep dive into several of the topics delivered in 2023 illustrates that the Small Group sessions support either gaining new information or reinforcing existing knowledge The post topic attendee survey for the session on ‘Improving Early Cancer Diagnosis in Primary Care’, for instance, showed that:
For 57% of the attendees the information provided reinforced that their existing knowledge and practices were up to date
For 36% of the attendees the knowledge gained through the sessions improved or expanded their current practice
The importance of having up to date information is illustrated by attendee reflections:
“The wide range of topics just refreshes your knowledge, refreshes what you should be doing, the areas you should be targeting”
- General Practitioner
“We went through the new pharmacological treatments [related to the management of heart failure] that I probably wasn’t hugely familiar with. That was really quite useful“
- General Practitioner
Impactgoal1:TheSGEPkeepscliniciansupto datewiththelatestclinicalevidenceand supportsbestpracticedecisionmaking.
Page 28 | Pegasus Health Small Group Impact Report
This also related to having the latest information about new medications and medication provision to patients:
“You get all the research that’s gone on and the background to all that up to date information… When you’ve got new drugs coming along all the time, it is really good to be up to date with [them].”
- Community Pharmacist
As part of the topic on heart failure management, for instance, medicine reconciliation was discussed, which is the process of ensuring that patients are clear on which medications should be taken or stopped, and when. This process reduces the risk of medication-related harm.
“We discussed the Entresto [heart failure medication] starting and the candesartan [high blood pressure medication] stopping because we see it all the time … it is so important to do those medicine reconciliations”
- Community Pharmacist
The SGEP supports better decision-making and improves patient care:
Our analysis of the impact of several topics delivered in 2023 showed clear evidence that the knowledge provided in the sessions can significantly improve patient care. For example, after the topic on ‘Supporting Healthy Weight’, the intention to improve communication with patients and to address clinician bias was reflected in the post session feedback:
87% of the clinicians indicated the intention to become more aware of their own weight bias and improve conversations with patients about weight, and 97% clinicians stated that the knowledge gained from the topic would support these conversations.
Together these factors are likely to improve understanding and shared decision making between clinicians and patients and whānau in relation to obesity and weight management As another example, in a post topic survey several weeks after the session on ‘Improving Early Cancer Diagnosis’:
66% of the respondents had either discussed their learning about safety netting practices, or had already made changes to improve safety netting practices in their workplace
Safety netting practices manage clinical uncertainty, highlight ‘red flag symptoms’ and are strategies put in place to help monitor patients until their symptoms are explained. It is strongly recommended by both the Health and Disability Commission NZ and NICE UK to use safety netting to improve early diagnosis of cancer (22, 23). Safety netting was highlighted and encouraged through the small group sessions
Pegasus Health Small Group Impact Report | Page 29
Over the long term these changes may improve cancer detection, which in turn can increase treatment options, survival rates, and improving the quality life for patients and whānau A particularly notable illustration of this, was the following The small group topic on Early Cancer Diagnosis had highlighted the symptoms that should be considered ‘red flags’ for further investigation to all professions. A community pharmacist who had attended this topic was able to recognise potentially indicative symptoms of cancer in a patient visiting the pharmacy, leading to the strong advice to visit a GP. This in turn led to an early-stage cancer diagnosis The following was shared by a Community Pharmacist Attendee:
“After attending the session, I have heard from a patient that was diagnosed with lung cancer after following up with their GP on the advice of our pharmacist. She thought she simply had lingering chest symptoms from COVID but during a discussion with the pharmacist some red flags were identified Thankfully her cancer was detected early and has a good prognosis. She is so grateful she took the advice and followed her symptoms up with the GP”
- Community Pharmacist

As a result of the SGEP, not only did the pharmacist identify that the patient needed a GP review, but the appropriate action was also taken by the GP - both now being able to recognise the ‘red flags’, and with that, potentially improving this patient’s outcome.
Page 30 | Pegasus Health Small Group Impact Report
Impact goal 2: The SGEP creates a more resilient primary care workforce that feels confident and supported in their clinical practice
Both the format and group-based nature of the SGEP sessions allow for the creation of a safe space, where practitioners can connect with one another, share experiences and feel supported. This in turn positively impacts clinicians’ ability and confidence in clinical practice This in turn helps to reduce (or avoid) a sense of professional isolation
The SGEP supports connection and learning from one another: Our 2023 interviews with clinicians from different professional backgrounds showed that the chance to discuss and exchange experiences with peers was a major attraction of the Small Group model that lifted it above most other professional development opportunities:
“[In] a Small Group setting not only do you get all the research that’s gone on and the background to all that up-to-date information, but you also get other people’s ‘how to’s’ and experience and that can be as valuable as the hand-outs; a GP giving some feedback on what they did or how they managed things can be really helpful”
- General Practitioner
“It brings all the GPs, the health professionals up to speed and allows that time for reflection and support. So it benefits both patients from a clinical point of view and the health professionals from a support point of view”
- General Practitioner

Pegasus Health Small Group Impact Report | Page 31
The SGEP increases confidence in clinical decision making:
Sharing experiences and learning from one another helps clinicians to increase their confidence in clinical practice and supports their delivery of the most up-to-date care to their patients:
“And then the next day you have a patient come in, and you’re just a bit more familiar, you’re on to it”
- General Practitioner
Our deep dive into the impact of the ‘Improving Early Cancer Diagnosis’ topic showed improvements in confidence in clinical decision making around early cancer detection as a result of attending the sessions, as illustrated in Figure 3 below. Overall improvements in confidence (36%) ranked as the second largest impact on professional practice behind knowledge improvement (57%) for all professions. Interestingly, improvement in confidence ranked highest among nurse practitioners (50%), followed by pharmacists (45%) and practice nurses (45%), and lower for GPs (23%) This may indicate the changing roles of these professions in primary care teams as the nature of their practice expands and they take on responsibilities traditionally held by the GP alone.
Improved my confidence
Overall
Other
PracticeNurses
NursePractitioners
GeneralPractitioners
CommunityPharmacists
Figure 3: Improvement in confidence after attending ‘ Improving Early Cancer Diagnosis’ topic
0 10 20 30 40 50
Page 32 | Pegasus Health Small Group Impact Report
The SGEP helps minimise professional isolation:
The SGEP attendees valued the professional support and connection provided through regular interaction with peers in their Small Groups Connection with others who work in the same or similar roles affirms that clinicians are not alone in the difficulties they encounter. This in turn helps to minimise professional isolation.
“Often, sharing difficult patients or situations or just how hard it can be is a helpful thing - that peer group kind of support”
- General Practitioner
“Just seeing how other people do it Primary care is incredibly isolating. We see patients every 15 minutes in this room, and you don’t really have much do with other people So I think it is really important just to figure out what’s going on out there”
- Nurse Practitioner
The positive impact of the programme on minimising a sense of professional isolation is particularly relevant in maintaining a sustainable and resilient primary care workforce. As mentioned earlier, burnout is a significant risk factor for health workforce, particularly those who are professionally isolated 86% GPs in the biennial 2022 RNZCGP survey on burnout agreed that GPs need strong peer networks for support and to reduce isolation and address burnout (7). The SGEP provides a strong peer network.

Pegasus Health Small Group Impact Report | Page 33
Impact goal 3: The SGEP helps build a connected primary care workforce that is not working in silos
The multidisciplinary group nature of the SGEP supports building a primary care workforce that is connected and works together. A workforce that is able to deliver consistent messaging and patient care, and that, by understanding each other's roles, is better able to guide patients and whānau through the health care system.
Learning together in the SGEP supports working collaboratively:
Our analysis of the impact of the SGEP shows that learning together supports working together. This is particularly true for the multidisciplinary groups:
“I am part of a multidisciplinary team group, so that also allows me to see the world through the pharmacist’s eyes and that sort of thing which is always valuable”
- Practice Nurse
“It was really interesting hearing what the nurses [do] – their way of blood tests, the lab way of things.… What the GPs do and what criteria to fit to reach their screening process [this helps to understand when and where to refer patients] Determining what things need to be checked for heart failure - I didn’t know what you need to check
That was really interesting”
- Community Pharmacist

The opportunity to learn about and from others right across the primary care workforce ensures that Small Group attendees have a wider view of (the impact of) their clinical decision making and are not practising in disconnected silos. The importance of learning from multidisciplinary peers is also endorsed by the World Health Organisation, who identify interprofessional education as an important strategy to create collaborative practice-ready workforce better prepared to respond to local health needs (4).
Page 34 | Pegasus Health Small Group Impact Report

Pegasus Health Small Group Impact Report | Page 35
Impact goal 4:
The SGEP supports optimal resource use and reduces unhealthy variation
This goal concerns the impact of the SGEP on the use of resources in the health system, and the financial or cost savings to the system. These impacts are generally the flow on effects of better decision making and better patient care
The cost impacts from the Small Group education programme can be:
direct (e.g. reduction in cost due to reduction of use of tests - as a result of the SGEP), indirect (e g improved productivity through better use of services/higher quality referrals/ teamwork/better communication – as a result of the SGEP), or intangible (e.g. improved patient quality of life, better patient experience or better supported clinical workforce - as a result of the SGEP) (22)
Our deep dive into the financial impacts of a few of the 2023 SGEP topics revealed the following:
Financial impact of SGEP Heart Failure Topic:
Through the analysis of the attendee feedback of the ‘Heart Failure’ sessions, we know that attendees were more up to date and understood the diagnostic process better after attending the sessions. It would be reasonable for this increased knowledge to lead to earlier identification and better management of heart failure in primary care, likely reducing the need for hospitalisation and associated costs. From Business Intelligence at Te Whatu Ora – Te Waipounamu, we know that the total cost of hospitalisation related to heart failure for Waitaha for the financial year 2022/23 (12 months) was $10,141,463.35
There were 1141 admissions
Average length of stay in hospital was 5 days
Average cost per event $9022.65 (23)
If only 2% of these admissions were avoided through the information provided in the SGEP, the financial savings to the health system would be $205,896.87. Whilst a 2% reduction in admissions is a conservative “best guess”, particularly considering the high number of Clinicians in Waitaha attending the programme, it does give an indication of the significant financial impacts of the SGEP.

Page 36 | Pegasus Health Small Group Impact Report
Financial impact of SGEP Early Cancer Diagnosis Topic:
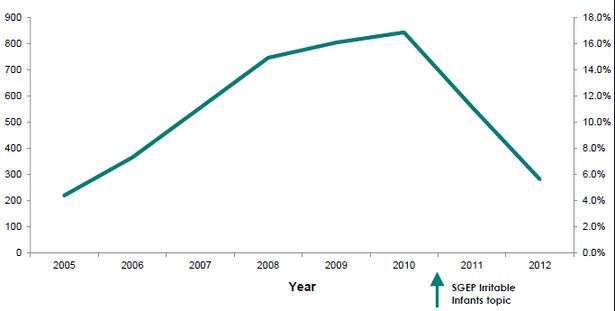
In terms of the SGEP topic on ‘Improving Early Cancer Diagnosis’, we know from the National Bowel Screening Service Project Manager in Canterbury that referrals for bowel screening test kits increased immediately after the delivery of the session on this topic, the arrow in figure 4 below shows when the impact of the topic on referrals for test kits (24). This suggests that the information provided in the SGEP sessions has increased the awareness of the process of accessing kits for priority populations through general practice. And it also suggests that primary care clinicians were encouraging and supporting the uptake of this relatively new national screening programme
Bowel Screening Kits ordered in Waitaha by General Practices
Increasing the screening of eligible patients for bowel cancer will have increased costs for the health system in the short term; however, in the longer-term increased uptake of the national bowel screening programme supports better population health through earlier diagnosis and treatment While we did not analyse, for instance, the cost of the kits and further investigations (colonoscopy, surveillance, false positives etc.), evidence shows that bowel cancer screening is likely to avoid approximately 1 in 6 colorectal cancer deaths (27). In turn, this may lead to savings for the health system.
2023 0 50 100 150 200 April May June July August September
SGEP Early Cancer Diagnosis topic
Figure 4: Bowel screening test kits ordered by Canterbury General Practices
Pegasus Health Small Group Impact Report | Page 37
It is important to note that while every topic in the SGEP focuses (in part) on better resource use and ultimately savings to the system (direct, indirect, or intangible), not every topic lends itself to the actual measurement of resource use or financial savings.
An historic example (pre-2023) of a SGEP topic that lent itself for measurement was the reduction in the overdiagnosis of reflux and a reduction in the use of omeprazole for infants (which is an unlicensed medication for this indication). The arrow in Figure 5 below shows the impact on omeprazole use in Canterbury for infants after the topic was run (26, 27)
Canterbury Unique Patients Under 1yrs Old dispensed Omeprazole
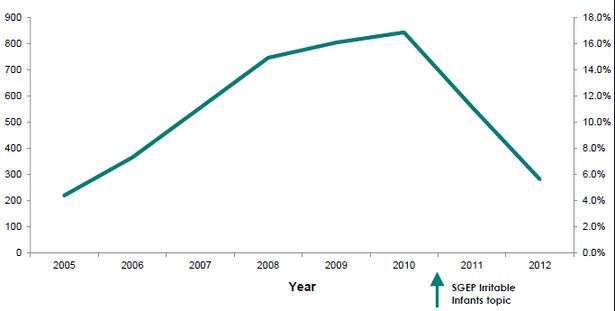
The impact of the information provided in the SGEP session on medication use was measurable, in this case, through analysis of the Ministry of Health pharmaceuticals claims data before and after the sessions were run But this kind of information and measurement is not always available for SGEP topics and/or takes time.
Figure 5: Omeprazole use for infants over time
Page 38 | Pegasus Health Small Group Impact Report
As we developed our new impact measurement framework, our analysis identified the four main challenges:
The lack of available data: e.g. we only have access to dispensing information on funded medications; internal analysis capability shortages; variable access to laboratory data - test data can be held at individual laboratory level or nationally; delays in data reporting from third parties
The delayed impact on resource use or costs: e.g. a SGEP topic may lead to improved knowledge about how to support healthy weight but reduced morbidity and costs from obesity related illnesses will happen in the longer term
The difficulty of attribution or causality: it is often not clear how much of a change can be attributed to SGEP or other factors, and M th d l i i th (fi i l) l f lif i k d d th

Pegasus Health Small Group Impact Report | Page 39
Table 2. Small Group topics 2023 areas of financial impact through optimising resources
Topic
Impact
Heart Failure Best practice use of new medications for treating heart failure
Improved diagnosis of early heart failure
Best practice testing for heart failure using BNP
Gut Health Reduction in antibiotic prescribing for diverticulitis
Which in turn reduces risk of antibiotic resistance
Areas of potential financial impact through optimising resources
Improved morbidity (= better control of heart failure, fewer exacerbations, identification and treatment of earlier, less severe disease)
Reduction in need for secondary care and hospitalisation
Improving Early Cancer Diagnosis
Increased uptake of bowel cancer screening
Multidisciplinary approach to safety netting to detect early cancer
Increased likelihood of early or earlier cancer diagnosis through better safety netting systems and uptake of screening
Effectiveness of antibiotics to treat infections is maintained, providing cost-effective treatment options when needed
Reduction in need for secondary care and hospitalisation
Improved morbidity/mortality
Short term increase in screening costs but longer-term population gains through early detection and treatment, increased survival rates
Increased earlier diagnosis of cancer improves quality of life and saves money through reduced morbidity and treatment costs
Improved morbidity/mortality
Reduction in need for secondary care interventions and hospitalisation
Neurodiversity with a Focus on ADHD
Improved diagnosis of ADHD
Reduced morbidity from disease
Improved productivity and quality of life for the individual and whānau
Supporting Healthy Weight (obesity)
Improved conversations and knowledge to support healthy weight and obesity management
Reduced morbidity from obesity related illnesses long term
Reduction in need for secondary care and hospitalisation because of fewer longer-term health impacts related to obesity
Page 40 | Pegasus Health Small Group Impact Report
Further explanation of the cost measurement challenges
Throughout the impact analysis, extensive efforts were made to gain further data and research that would allow a further specification of the impact of the SGEP on resources and costs This included (but was not limited to) a review of the published and grey literature on the valuation and costs of health, sickness and death; a review of the literature on the effectiveness and value of health education for health professionals; an exploration of the data available at Statistics New Zealand and Te Whatu Ora on relevant health related statistics and costs; countless emails to (international) experts in the field of healthcare, statistics and health economics

The conclusion of this comprehensive and in-depth review is that there is not yet agreement on how to conduct a methodologically solid and evidencebased financial impacts evaluation for an intervention like the SGEP. (24, 30). Cost of illness studies in New Zealand, but also internationally, are rare, and much of this literature is old and out of date from a cost perspective (24) A 2021 evidence review for the Ministry of Health was also unable to estimate the overall social and economic cost of long-term conditions in New Zealand (24)
It is important to consider that the primary impact of the SGEP is focused on supporting primary care clinicians in Canterbury, which we are currently able to demonstrate evidence for, and to measure. As the data and methods for the economic evaluation of health and sickness evolve, we will be able to better measure the secondary impacts from this important professional development programme.
Pegasus Health Small Group Impact Report | Page 41
LOOKING AHEAD
In 2024 we will continue our impact work in several ways
Our redefined impact goals and our SGEP impact model (our evidence-based understanding of how the SGEP creates positive change) allows us to grow and scale our impact intentionally We will embed our impact goals more purposefully within the processes of topic selection and development of content, supporting best practice and, collaborative patient care
In addition, the implementation of our new impact measurement framework and strategy will drive the (further) improvement of the evaluation and reporting of the direct impacts of the SGEP This implementation process includes improving and adding to our data collection methods and maximising the value of our feedback processes, as well as exploring ways to strengthen financial impact reporting. The implementation of our new measurement strategy will also streamline our data collection (e.g. reduce over measuring of non-relevant data) and improve ease of impact reporting.
The Clinical Quality & Education team will use the growing impact evidence to inform the continuous improvement of the programme. In addition, the growing body of impact evidence will make it easier to communicate the value of the programme to our key stakeholders.
This improved understanding of the value of the SGEP will allow us to better share the story of the programme with other regions of Aotearoa New Zealand and inform future conversations on regional and national expansion opportunities within the health system transformation. Ultimately, we hope this will enable more clinicians in primary care (and their patients and whānau) to benefit from the SGEP
Finally, through this impact work and a number of practice-based workshops the team has grown their understanding of social impact (measurement). Going forward, we will continue to build the internal capability in relation to impact-focussed thinking and analysis. Our growing capability in the social impact space allows us to be an (pro-) active participant in conversations with funders and other stakeholders about impact measurement in the health sector In addition, we hope to inspire and inform social impact work within Pegasus as a whole.
This work will be complemented by the new name for the programme – Clinical Connect
Page 42 | Pegasus Health Small Group Impact Report
SUMMARY REFLECTIONS
Our report demonstrates the significant value of the Pegasus Small Group Education Programme.
Our impact analysis shows the positive impact on the knowledge, capability and confidence of individual clinicians in Waitaha Canterbury and how it contributes to a connected, supported and more resilient clinical workforce. A workforce that is not operating in silos, provides consistent messaging to patients, and can better guide patients and whanau to the right primary care providers within the wider health system. Finally, it highlights the flow on benefits of the SGEP for quality patient care and resource-use within the primary health care system overall
The interviews, meeting feedback and post-topic surveys showed how much clinicians value having an ongoing professional development programme that provides them with up-to-date, reliable, research-based evidence on topics of key relevance to their daily practice The interactive, discussion-based model of professional development complements the research-based content of the Small Group SGEP so that each practitioner benefits from the experience of those in their peer group, bringing a wealth of knowledge and experience into a single session. The peer group format provides professional support and affirmation for attendees, thereby increasing clinicians’ confidence and reducing a sense of professional isolation This, in turn, supports the retention of skilled and experienced practitioners within the health system The multidisciplinary nature of the content development and the opportunity to learn from those right across the primary care workforce ensures that Small Group attendees have a wider view of the impact of their clinical decision making and are not practising in disconnected silos
The value and relevance of the SGEP cannot be underestimated in the context of the current challenges facing the health care system as a whole. Increased thresholds for specialist and planned secondary care and significant workforce shortages increase the demands on primary care and require clinicians to work to the top and across the breadth of their professional scope
Pegasus Health Small Group Impact Report | Page 43
In a sector where burnout rates are already high, the professional support that the SGEP offers for practitioners is of key importance In addition, growing understanding and collaboration between primary care providers through the SGEP is increasingly vital to improve care and work towards health equity for all. In the future, by expanding the programme to other regions in Aotearoa New Zealand, we hope to grow and scale these positive impacts of the SGEP programme.
Internally, the insights of this impact work led to four new impact goals for the SGEP; the SGEP
Keeps clinicians up to date with the latest clinical evidence and support best practice decision making
Creates a more resilient primary care workforce that feels confident and supported in their clinical practice
Helps build a more connected primary care workforce that is not working in silos
Supports optimal resource use and reduces unhealthy variation
In addition, the impact analysis informed the development of a robust SGEP impact model and an impact measurement framework and strategy. This in turn improves our ability to measure, report, communicate and grow our impact going forward.

Page 44 | Pegasus Health Small Group Impact Report
APPENDICES
Appendix 1: Small Group Topics Delivered in 2023
1 - Heart Failure
2 - Gut Health
Heart failure is a complex clinical syndrome caused by a variety of cardiac diseases. It affects approximately 1.6% of Aotearoa New Zealand’s population (around 66 000 people) This topic explores the aetiology, diagnosis and management We discuss the most recent guidelines and examine the latest evidence supporting the new available therapies and how we can strengthen our current care of patients with heart failure
A highly requested topic Key developments in recent years, driven by advances in technology, have led to a deeper understanding of the gut-brain connection This has led to the re-naming of functional gastrointestinal disorders as disorders of gut-brain interaction (DGBI) and has improved our approach to their management This topic promotes current best practice in relation to irritable bowel syndrome (a DGBI) and diverticulitis (including a focus on reducing antibiotic use for this condition, which in turn reduces antibiotic resistance)
3 - Improving Early Cancer Diagnosis
There are known disparities and inequities in cancer diagnosis and treatment In primary care we have an important role to play in encouraging screening, advocating for patients, communication (patients, family, secondary care), and safety netting
4Neurodiversity with a Focus on ADHD
5 - Supporting Healthy Weight (obesity)
Neurodiversity involves a difference in processing of the world around us. The topic focusses on the challenges of making a diagnosis, treatment and approach for adult patients who may have ADHD, an area where there is new and growing evidence that often differs to what clinicians have previously been taught The impact of undiagnosed symptoms on outcomes and the evidence for both non-pharmacological and pharmacological options are discussed, aiming to reduce morbidity and improve quality of life for those with ADHD
Obesity is a major worldwide health challenge impacting on quality of life and life expectancy Continued high prevalence suggests that current approaches are not working The topic highlights the latest evidence for treatment of obesity, and the impact of stigma and bias, including from health professionals Addressing bias and promoting conversations about healthy weight management in clinical practice are key elements in the topic to support reduce weight-related morbidity and improve patient and whānau quality of life 534 4 49/5
Topic About Number of attending clinicains Evaluation Score (aggregated) 1 = poor, 5 = excellent
568 4 67/5
595 4 45/5
597 4 46/5
610
44/5
4
Pegasus Health Small Group Impact Report | Page 45
Appendix 2: Alignment with Te Whatu Ora Indicators & UNSDGs
The table below outlines how the SGEP topics of 2023 support the key areas of Te Pae Tata;Te Whatu Ora Health System Indicators; and the United Nations Sustainable Development Goals
2023
Topic
1 - Heart Failure
2 - Gut Health
3 - Improving Early Cancer Diagnosis
Te Pae Tata Interim New
Zealand Health Plan areas
Māuiuitanga taumaha – People living with chronic health conditions
Improve equity of health outcomes –Deliver on improving pae ora for Māori, Pacific people and Tāngata whaikaha | Disabled people
Māuiuitanga taumaha – People living with chronic health conditions
Improve equity of health outcomes –Deliver on improving pae ora for Māori, Pacific people and Tāngata whaikaha | Disabled people
Te Whatu Ora Health System Indicators
Better primary healthcare – people report being involved in the decisions about their care and treatment
United Nations Sustainable Development Goals
Goal 3 Ensure healthy lives and promote well-being for all at all ages
4Neurodiversity with a Focus on ADHD
Mate pukupuku – People living with cancer
Improve equity of health outcomes –Deliver on improving pae ora for Māori, Pacific people and Tāngata whaikaha | Disabled people
Better primary healthcare – people report being involved in the decisions about their care and treatment
5 - Supporting Healthy Weight (obesity)
Māuiuitanga taumaha – People living with chronic health conditions
Oranga hinengaro – People living with mental distress, illness and addictions
Improve equity of health outcomes –Deliver on improving pae ora for Māori, Pacific people and Tāngata whaikaha | Disabled people.
Improving wellbeing through prevention –participation in bowel cancer screening (in development)
Better primary healthcare – people report being involved in the decisions about their care and treatment
Improving mental wellbeing Better primary healthcare –people report being involved in the decisions about their care and treatment
3 4 By 2030, reduce by one third premature mortality from noncommunicabl e diseases through prevention and treatment and promote mental health and wellbeing
Pae ora – Better health and wellbeing in our communities
Improve equity of health outcomes –Deliver on improving pae ora for Māori, Pacific people and Tāngata whaikaha | Disabled people
Improving wellbeing through prevention
Page 46 | Pegasus Health Small Group Impact Report
Appendix 3: Impact Investigations 2023
The following documents are available on request: The impact review of the Heart Failure Small Group topic 1 Follow up impact survey of the Improving Early Cancer Diagnosis in Primary Care topic 2 The analysis of the participant interviews focused on the impact of attending the SGEP 3
Pegasus Health Small Group Impact Report | Page 47
Appendix 4: The SGEP Theory of Change
A Theory of Change (TOC) describes the path to impact of an activity, programme or
SGEP Theory of Change 2024
Outputs
Up to date clinical knowledge
Inputs
Content based on local data analysis and latest, best practice knowledge
Relevant, need-based topics
High quality, evidencebased resources
Health equity lens applied to each topic
Peer developed and led Human resources
Financial resources


Conditions
Small groups of optimal size
Group environment is safe
All disciplines feel valued SGEP meets professional development standards
Non-judgemental reflection with peers
Discussion of difficult or complex situations
Strengthened (crossdisciplinary) primary care connections


Conditions
Clinician applies learning in practice
Clinician has resources to put learning into practice
Attendees connect with one another
Page 48 | Pegasus Health Small Group Impact Report
Impacts Short Term
Outcomes
Clinicians are up to date with latest best practice
Improved clinical decision making and practice*
Clinician has improved sense of support
Clinician feels more confident in practice
Improved interdisciplinary understanding
Improved ability to work to top of scope and/or full breadth of scope

Better patient care
Improved ability to guide patients to right people in primary care
Consistent messaging for patients and whānau across primary care
Clinician experiences less professional isolation
Less clinician burnout
Optimised use of resources
Reduced unhealthy variation


Conditions
Information and best practice is consistently applied
Professional connections are valued and maintained over time
Impacts Long Term
A more connected health care system (not working in silos)
Better patient health and reduced morbidity
A more resilient primary care workforce
Improved retention in primary care
Resource/cost savings across system

Pegasus Health Small Group Impact Report | Page 49
REFERENCES
Trayer J, Rowbotham NJ, Boyle RJ, Smyth AR Industry influence in healthcare harms patients: myth or maxim? Breathe 2022;18(2):220010.
Meeker D, Linder JA, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, et al Effect of Behavioral Interventions on Inappropriate Antibiotic Prescribing Among Primary Care Practices: A Randomized Clinical Trial Jama 2016;315(6):56270.
Saint-Pierre C, Herskovic V, Sepúlveda M Multidisciplinary collaboration in primary care: a systematic review Family Practice 2017;35(2):132-41
S
Betty B, Scott-Jones J, Toop L State of general practice in New Zealand The New Zealand medical journal 2023;136(1582):8-10
RNZCGP Royal New Zealand College of General Practitioners 2022 Workforce Survey 2022 [updated 27 Feb 2023
Available from: https://www rnzcgp org nz/resources/data-and-statistics/2022-workforce-survey/
8 Pharmacy Council of New Zealand Pharmacy Workforce Demographic 2023 2023 [Available from: https://pharmacycouncil org nz/wp-content/uploads/2023/12/Pharmacy-Council-Workforce-Demographic-Report2023 pdf
10
New Zealand Nurses Organisation NZNO Strategy for Nursing 2018 - 2023 2018 [Available from: https://www nurses org nz/Portals/1/2018%20Nursing%20Strategy/NZNO%20Strategy%20for%20Nursing%202018-2023 pdf
9 Barnett S, Jones SC, Bennett S, Iverson D, Bonney A Usefulness of a virtual community of practice and web 2 0 tools for general practice training: experiences and expectations of general practitioner registrars and supervisors Australian journal of primary health 2013;19(4):292-6
11.
12
Counselman EF, Weber RL. Organizing and maintaining peer supervision groups. International journal of group psychotherapy 2004;54(2):125-43
Dowling S, Last J, Finnegan H, O'Connor K, Cullen W Does locally delivered small group continuing medical education (CME) meet the learning needs of rural general practitioners? Education for primary care : an official publication of the Association of Course Organisers, National Association of GP Tutors, World Organisation of Family Doctors 2019;30(3):145-51
13. Lancaster J, Prager S, Nash L, Karageorge A Psychiatry peer review groups in Australia: a mixed-methods exploration of structure and function BMJ open 2020;10(11):e040039
Hussan A, Satheeskaran M, Dho H, Basu A, Fazaldin Y, Tariq S, et al. GP perceptions of informal peer support in primary care: a qualitative study BJGP open 2024
14 Nash L, Karageorge A, Lancaster J, Prager S How peer review groups support learning and wellbeing in psychiatrists Australasian psychiatry : bulletin of Royal Australian and New Zealand College of Psychiatrists 2022;30(4):556-63
Palermo C, Hughes R, McCall L A qualitative evaluation of an Australian public health nutrition workforce development intervention involving mentoring circles Public health nutrition 2011;14(8):1458-65
Christie C, Bidwell S, Copeland A, Hudson B Self-care of Canterbury general practitioners, nurse practitioners, practice nurses and community pharmacists Journal of Primary Health Care 2017;9(4):286-91
Koppe H, van de Mortel TF, Ahern CM How effective and acceptable is Web 2 0 Balint group participation for general practitioners and general practitioner registrars in regional Australia? A pilot study The Australian journal of rural health 2016;24(1):16-22
Mandy A, Tinley P Burnout and occupational stress: comparison between United Kingdom and Australian podiatrists Journal of the American Podiatric Medical Association 2004;94(3):282-91
RNZCGP Burnout: Let's understand it and find solutions 2022 [Available from: https://www rnzcgp org nz/resources/dataand-statistics/burnout-survey/ 20
Wasoski RL. Stress, professional burnout and dentistry. Journal - Oklahoma Dental Association. 1995;86(2):28-30.
Hogan S; Song Z The Cost of Long-term Conditions in New Zealand: Review of the evidence – 2021 update Wellington2022 [Available from: https://www health govt nz/publication/cost-long-term-conditions-new-zealand
23. Zang T. The costs associated with Heart Failure Admissions in Canterbury 2022/23. Business Intelligence Data & Analystics; Te Whatu Ora; Te Waipounamu - Health New Zealand; 2024
23. Jackson S Dashboard requests for bowel cancer screening testing kits : Bowel Screening Project Manager Canterbury ; 2024.
National Screening Unit National Bowel Screening Programme 2023 [Available from: https://www nsu govt nz/healthprofessionals/national-bowel-screening-programme
25 Hudson B, Alderton A, Doocey C, Nicholson D, Toop L, Day AS Crying and spilling--time to stop the overmedicalisation of normal infant behaviour The New Zealand medical journal 2012;125(1367):119-26 26
Toop L; Alderton A; Hudson B Overdiagnosis and dangerous overtreatment of irritable infants with "reflux" 2014 27 Abelson P Establishing a monetary value for lives saved: issues and controversies 2007
1
2
3 WHO Framework for action on Interprofessional Education & Collaborative Practice 2010 4
of clinical education in primary care 2015 5
6
Bidwell
Effective methods
7
15
16
17
18
19
21.
22
24
28 Page 50 | Pegasus Health Small Group Impact Report