Software. Consulting. Education. Results.
Proposed Rule SOFTWARE. CONSULTING. EDUCATION. RESULTS. Navigating the Price Transparency Rule Updates for 2024 09.14.23
CMS OPPS
Meet the Speakers




Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 2
Kevin Chmura
Chief Executive Officer
Panacea Healthcare Solutions
Govi Goyal President, Financial Services
Panacea Healthcare Solutions
Henry Gutierrez SVP, Financial Consulting Services
Panacea Healthcare Solutions



Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 3 Agenda 01 Opening Remarks and Introductions 04 05 02 Recent Actions by CMS and Enforcement Updates 03 How to Stay Ahead of the Proposed Requirements 04 Use of Negotiated Rate Data for Comparative Analysis 05 Questions and Answers


Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 4 Industry Updates and Recent CMS Actions
Did you participate in the CMS webinar held on July 26th or read the price transparency section of CMS OPPS proposed rule?
a. Yes, attended the webinar and read the proposed rule

b. Only attended the webinar
c. Only read the proposed rule
d. Neither, that's why I'm here!
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 5
Polling Question 1
CMS Price Transparency
Standard Charges
Public AGENCY: Centers for Medicare & Medicaid Services (CMS), HHS.

ACTION: Final rule.
SUMMARY: This final rule establishes requirements for hospitals operating in the United States to establish, update, and make public a list of their standard charges for the items and services that they provide. These actions are necessary to promote price transparency in health care and public access to hospital standard charges.
By disclosing hospital standard charges, we believe the public (including patients, employers, clinicians, and other third parties) will have the information necessary to make more informed decisions about their care. We believe the impact of these final policies will help to increase market competition, and ultimately drive down the cost of health care services, making them more affordable for all patients.
DATES: This final rule is effective on January 1, 2021.
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 6
Key Dates
Jan 1st, 2022
Increase in Civil Monetary Penalties
Nov 14th, 2022
Standard Voluntary Data Format for Machine-Readable Files

Sep 11th, 2023
End of CMS Comment Period
Mar 1st, 2024
End of Grace Period for MRF Changes*
Jan 1st, 2021
CMS Price
Transparency
July 1st, 2022
Transparency in Coverage (TiC) rule
July 13th, 2023
Release of OPPS
Proposed Rule
Jan 1st, 2024
Effective Date for Certain Requirements
*Certain proposed changes related to price transparency are effective on January 1st, 2024, without a grace period.
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 7
Recent Communication from CMS about Enforcement
In a recent article on hospital price transparency published in Health Affairs, CMS officials

Meena Seshamani, MD, PHD, and Douglas Jacobs, MD, noted that the agency is exploring how to streamline price transparency enforcement efforts, including expediting the timeframes by which it requires hospitals to come into full compliance upon submitting a corrective action plan. The authors also said that CMS plans to take aggressive additional steps to identify and prioritize action against hospitals that have failed entirely to post files.
Source: Seshamani, M., and Jacobs, D., “Hospital price transparency: Progress and commitment to achieving its potential,” Health Affairs, Feb. 14, 2023.
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 8
What is CMS’ process for enforcing the HPT rules?
The enforcement process occurs in a phased manner and typically involves a comprehensive compliance review in response to CMS audit or a complaint received through the Hospital Price Transparency website.
If CMS concludes a hospital is noncompliant with one or more of the requirements, CMS may take any of the following actions:
• Provide a written warning notice to the hospital of the specific violation(s). This step may be skipped if there is no evidence of efforts to comply
• Request a Corrective Action Plan (CAP) if noncompliance constitutes a material violation of one or more requirements. Under a current bill, hospitals would be given 45 days to submit a plan and 90 days in total to achieve full compliance

• Impose a Civil Monetary Penalty
• A public list of non-compliant hospitals that are assessed a CMP will be located on the CMS Price Transparency website: https://www.cms.gov/hospital-price-transparency. (Public Shaming)
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 9
Shorter Window to Comply

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 10 Old Enforcement Process 90 Days Warning Letter 135 Days Submit CAP 225 Days Implementation of CAP New Enforcement Process 45 Days Submit CAP Implementation of CAP 90 Days As of April 2023, CMS may “skip” warning letter and automatically impose a CMP on hospitals that fail to submit a CAP at the end of the 45-day CAP submission deadline.

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 11 0 200 400 600 800 1000 1200 1400 Jan-22 Feb-22 Mar-22 Apr-22 May-22 Jun-22 Jul-22 Aug-22 Sep-22 Oct-22 Nov-22 Dec-22 Jan-23 Feb-23 Mar-23 Apr-23 May-23 Jun-23 Cumulative Trend in Warning Letters and CAPS Warning Letters Corrective Action Plans Accelerated Enforcement
Civil Monetary Penalties

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 12
$0 $200,000 $400,000 $600,000 $800,000 $1,000,000 $1,200,000 0 100 200 300 400 500 600 700 800 IL TX AR TX GA GA NH Puerto Rico NY Puerto Rico NC FL MD D.C. Community First Medical Center Falls Community Hospital Fulton County Hospital Kell West Medical Center Northside Hospital Atlanta Northside Hospital Cherokee Frisbie Memorial Hospital Hospital General Castaner Samaritan HospitalAlbany Memorial Campus Doctors' Center Hospital Bayamón Betsy Johnson Hospital UF Health North Holy Cross Hospital Saint Elizabeths Hospital CMP Bed Size CMPs by Hospital Bed Size and Location Bed Size Fine $4.6M Total Fines to Date
Dramatic Increase in Penalties Due to Non-Compliance

Hospitals equal to or less than 30 beds
Hospitals between 31 and 550 beds
Hospitals with more than 550 beds
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 13 Hospital Bed Size CY 2021 CMP CY 2022 CMP Up to $300 Per Day or $110K Per Year Up to $300 Per Day or $110K Per Year
to $300 Per Day or $110K Per Up to $10 Per Day multiplied by Number of Beds
CMP of $3,000 Per Day or $1M Per Year.
to $300 Per Day or $110K Per Year Up to $5,500 Per Day or $2M Per Year
Up
Example: A 300-bed hospital would have a maximum
Up
Common Errors on the Machine-Readable File
Showing only “%” versus “$”
• CMS advises hospitals to calculate the dollar value for ‘percent of charge payers’ at CDM and NDC level
Missing Line Items
• Hospitals must include all items and services with a standard charge, including items with zero volume, drugs at the NDC level, etc.
Not Easily Accessible
• Machine-Readable Files should be accessible to consumers, digitally searchable and displayed prominently without barriers.
Wrong Naming Convention
• CMS requires a specific naming convention and file format (<ein>_<hospitalname>_standardcharges.[json|xml|csv]).
Missing Updated Date
• Hospitals must indicate the date that the MRF was most recently updated in the file itself or associated with the file.
Rates Only at the Plan Level
• Payer-specific negotiated rates should be at the payer and plan code level and should not be averages or ranges.

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 14
Common Errors – Using Claims and Payments Data Instead of Payer Contracts


Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 15


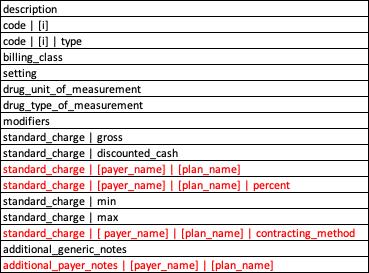
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 16 CMS Proposed Additions to Machine-Readable Files
“Static” MRF Elements

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 17 Data Element Included in 2021 CMS PT Rule? Included in 2022 Sample Template? Included in 2024 OPPS Proposed Rule? Hospital Name Yes Yes Yes Hospital File Date (FKN: Date of Last Update) Yes Yes Yes Item / Service Description Yes Yes Yes Billing / Accounting Code Yes Yes Yes Gross Charges Yes Yes Yes Cash Discounted Price Yes Yes Yes Payer Specific Negotiated Charges Yes Yes Yes Maximum Deidentified Negotiated Charges Yes Yes Yes Minimum Deidentified Negotiated Charges Yes Yes Yes
“New” MRF Data Elements

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 18 Data Element Included in 2021 CMS PT Rule? Included in 2022 Sample Template? Included in 2024 OPPS Proposed Rule? Hospital License No Yes Yes Hospital Location No Yes Yes Hospital License No Yes Yes Hospital Address No No Yes Hospital Financial Aid Policy No Yes No File Version No Yes Yes Code Type (e.g., MS -DRG) No Yes Yes Modifiers (e.g., 50, 25, TC) No Yes Yes Billing Class (e.g., Professional) No Yes No Setting (e.g., Inpatient) No Yes Yes
“New” MRF Data Elements cont.

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 19 Data Element Included in 2021 CMS PT Rule? Included in 2022 Sample Template? Included in 2024 OPPS Proposed Rule? Payer Name Yes Yes Yes Plan Name No Yes Yes Payer Specific Negotiated Charge: Percent No Yes Yes Contracting Method (e.g., Fee Schedule) No Yes Yes Drug Unit of Measurement No Yes Yes Drug Type of Measurement No Yes Yes Consumer Friendly Expected Allowed Amount No No Yes Additional Generic / Payer-Specific Notes No Yes Yes
Allowable File Formats
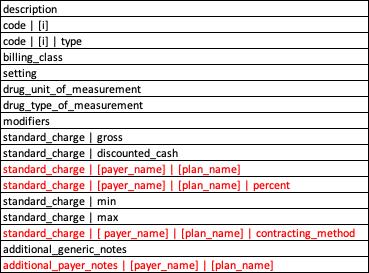


* Consumer Friendly Expected Allowed Amount has not yet been added to the data dictionary.

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 20
JSON Schema CSV “Wide” Format
CSV “Tall” Format
Additional Data Element: Contracting Method
Definition:
The type of contract arrangement used to establish the payer-specific negotiated charge.
Naming Convention:
standard_charge | contracting_method (Tall Format)
standard_charge | [ payer_name] | [plan_name] | contracting_method (Wide Format)

Valid Values:
Case Rate, Fee Schedule, Percent of Total Billed Charges, Per Diem, Capitation, Other
CSV Instructions: Select the value that most closely represents the contracting method for the payer-specific negotiated charge associated with the item or service. If the contracting method isn’t represented in the definitions, select ‘Other’ and enter a detailed explanation of the contracting arrangement in the ‘Additional Generic Notes’ for the CSV Tall sample format or the ‘Additional Payer-Specific Notes’ for the CSV Wide sample format.
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 21
Adding in the Contracting Method – Examples


Good Examples – Based on the CSV “Tall” Format

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 22 Bad Example – Contracting Method is embedded in the Service Description

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 23 *Analysis performed by Panacea in 2023 is based on 175 hospitals across the nation encompassing over 1,500 managed care contracts. 4% 73% 23% CPT 99282 – ED Visit Per Visit Per Unit Case Rate Average Negotiated Rate $820 Average Negotiated Rate $4,651 Average Negotiated Rate $1,593
We Care About Contracting Method?
Why Do
Confidence Levels Based on Frequency of Contracting Method
*Analysis performed by Panacea in 2023 is based on 175 hospitals across the nation encompassing over 1,500 managed care contracts.

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 24 High Low Confidence Level in Rate Methodology Billling Code Description Confidence Level Predominant Contract Method (Claim vs. Line Item) Frequency of Predominant Rate Methodology 80050 General health panel Primary Line Item 95% 73030 X-ray exam of shoulder Primary Line Item 87% 71550 Mri chest w/o dye Primary Line Item 85% 99282 Emergency dept visit Secondary Line Item 77% 76932 Echo guide for heart biopsy Secondary Line Item 72% 64642 Chemodenervation Tertiary Bundled Payment 68% 31625 Bronchoscopy w/biopsy Tertiary Bundled Payment 65% 27447 Total knee arthroplasty Tertiary Bundled Payment 61%
Opportunity to Comment to CMS – Align with TiC?
Negotiated Arrangement
The negotiated rate, reflected as a dollar amount, for each covered item / service that the plan has contractually agreed to pay an in-network provider
Negotiated Type
The negotiated percentage value for a covered item or service from a particular innetwork provider for a ‘percentage of billed charges’ arrangement.
The rate for a covered item that determines a participant’s costsharing liability for the item / service, when that rate is different from the negotiated rate or derived amount.
The per diem daily rate, reflected as a dollar amount, for each covered item / service that the plan has contractually agreed to pay an in-network provider
The price that a plan or issuer assigns to an item or service for the purpose of internal accounting, reconciliation with providers or submitting data in accordance with the requirements of 45 CFR 153.710(c)

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 25 Fee Schedule Fee for Service Negotiated Derived Capitation Bundled Per Diem Percentage Fee Schedule Negotiated Derived Percentage


Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 26 Opportunity to Comment to CMS – Add More Methods?
Additional Data Element: Consumer Friendly Expected Allowed Amount
Definition:
The average dollar amount a hospital expects to be paid by the payer and required in situations where the payer-specific negotiated charge cannot be expressed as a dollar figure or payment varies from patient to patient.

Naming Convention:
Expected Allowed Amount
Valid Values:
TBD - CMS will provide technical instructions for hospitals to display standard charges expressed in dollars, percentages, and algorithms in order to ensure consistency and machine-readability.
CSV Instructions:
TBD - Currently Proposed only and not included within data dictionary. Requires the combination of claims and payment contracts.
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 27

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 28 0 50 100 150 200 250 300 350 Under $3K $3K - $4K $4K - $5K $5K - $6K $6K - $7K $7K - $8K $8K - $9K $10K - $11K $11K - $12K Greater $12K Variability in Charges for Colonoscopy (N = 900 claims) (“soft-coded” 45378) Median Mean Total Billed Charges for Colonoscopy Claims # of Claims Conceptualizing the Consumer Friendly Expected Allowed Amount
Consumer Friendly Expected Allowed Amount – Examples
Further clarification will be required from CMS to determine if the contracted % should be displayed within the “Payer Specific Negotiated Charge: Percent” data element
Additionally, clarification necessary on the requirement to display the Standard_Gross Charge (i.e., average charge) for Payers and Products using a % of Total Billed Charges Contract Method
Confirmation that claims data should only be used for situations where the payer-specific negotiated charge cannot be expressed as an exact dollar figure. Source of all other Payer Specific Negotiated Charges should come from 3rd party payer contracts or fee schedules.

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 29
Additional Data Elements: Payer Name + Plan Name
Definition:
The name of the third-party payer that is, by statute, contract, or agreement, legally responsible for payment of a claim for a healthcare item or service and that payer’s specific plan associated with the standard charge.

Naming Convention:
Payer_Name
Plan_Name
Example
Values:
Cigna, Aetna, Humana, etc. (payer name)
PPO, HMO, All Managed Care Plans, etc. (plan name)
CSV Instructions:
Only applies to the CSV “Tall” sample format and JSON schema. We recommend that hospitals use the full name of the payer organization, absent any abbreviations. (On the CSV “Wide” sample format the payer and plan name is combined with other data elements such as Contracting Method)
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 30
Why it Matters – Meaningless Variation Between Plan Types
*2023 comparative rates study by Panacea using cleansed hospital machine-readable files from over 15 hospitals in Texas and over 500 hospitals across the nation.

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 31 Same Payer but Different Plan Types Different Payers but Same Plan Types $0.00 $200.00 $400.00 $600.00 $800.00 $1,000.00 $1,200.00 $1,400.00 PPO HMO Medicaid Medicare Average Negotiated Rates by Product Type CT Head w/o Dye United HealthCare Texas National $0.00 $200.00 $400.00 $600.00 $800.00 $1,000.00 $1,200.00 $1,400.00 $1,600.00 $1,800.00 $2,000.00 Cigna Humana
Average Negotiated Rates by Payer CT Head w/o dye PPO Product Type Texas National
BCBS UHC Aetna


Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 32
Opportunity to Comment: Classification to a Standard Payer and Plan
Additional Data Element: Drug Unit and Type of Measurement

Definition:
The unit value that corresponds to the established standard charge for drugs.
The measurement type that corresponds to the established standard charge for drugs.
Naming
Convention:
drug_unit_of_measurement
drug_type_of_measurement
Valid Values:
Positive Numbers (unit type)
GR – Gram, ME- Milligram, ML – Milliliter, and UN – Unit (measurement type)
CSV Instructions: Enter the unit value, or amount, of the drug for that particular standard charge. If the description is “aspirin 81mg chewable tablet – each” then the drug unit value is “1” and the type of measurement is “UN” since the standard charge is established per tablet.
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 33
Why Do We Need Additional Fields for Pharmacy?

Why is it Important to Show the Type + Unit of Measurement?
Why is it Important to Show the NDC?
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 34 description Code | 1 Code | 1 | type drug_type_of_measurement drug_unit_of_measurement Standard_charge | negotiated_dollar Aspiring, 81mg chewable tablet 41250-0780 NDC UN 1 50.25 CMS Example description Code | 1 Code | 1 | type Code | 2 Code | 2 | type drug_type_of_measurement drug_unit_of_measurement Standard_charge | negotiated_dollar gentamicin 80 mg/100 mL in NaCl(iso) intra piggy 338050348 NDC J1580 HCPCS ML 100 75.50 gentamicin 100 mg/100 mL in NaCL(iso) intra piggy 338050548 NDC J1580 HCPCS ML 100 85.20 gentamicin 120 mg/100 mL in NaCl(iso) intra piggy 338050748 NDC J1580 HCPCS ML 100 91.25 **Same HCPCS, type and unit of measurement but different NDC clarifies different strength
description and NDC
different type of measurement
negotiated rate
units
**Same
BUT
and
(200mg billing
for the HCPCS code)
description Code | 1 Code | 1 | type Code | 2 Code | 2 | type drug_type_of_measurement drug_unit_of_measurement Standard_charge | negotiated_dollar gemcitabine 1-gram intravenous solution 25021023550 NDC J9201 HCPCS GR 1 75.25 gemcitabine 1-gram intravenous solution 25021023550 NDC J9201 HCPCS GR 2 150.50
Extracting Data from Drug File and Transform into MRF
HCPCS code J9015 Injection, aldesleukin, per single use vial
HCPCS code J2765 Injection, metoclopramide hcl, up to 10 mg

CMS HPT CSV Sample Format (Wide)
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 35 description code | 1 code | 1 | type code | 2 code | 2 | type billing_class setting drug_unit_of_ measurement drug_type_of_ measurement modifiers standard_charge | gross aldesleukin 18 million u/mL Solr 1 Each Vial 76310-022-01 NDC J9015 HCPCS facility both 1 UN 18292.85 metoclopramide 5 MG/ML Soln 2 mL Vial 0409-3414-18 NDC J2765 HCPCS facility both 2 ML 5.13

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 36 Most Hospital Formulary Exports do NOT Align with the Measurement Values Found in CMS PT Data Dictionary GR – Gram ME – Milligram ML – Milliliter UN – Unit CMS Valid Measurement Types Typical Hospital Formulary Measurement Values ML – Milliliter MG – Milligram MC – Microgram GM – Gram EA – Each UN – Unit VS. Pharmacy – Opportunity to Comment?
Do you feel that you will be ready by March 1st, 2024, to implement all the required changes?
Polling
Question 2
a. Yes, we implemented to the voluntary data format released last November, including Contract Method, and are preparing for the other updates

b. Possibly, we have made some updates to align with the new formats and continue to do research
c. No, we have not yet implemented any of the proposed changes yet and may need assistance
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 37
Which of the below additional data elements do you feel will be the greatest challenge?
Polling
Question
a. Contracting Method
b. Consumer Friendly Expected Allowed Amount
3
c. Pharmacy (type and unit of measurement)
d. Payer and Plan Name
e. Payer Specific Negotiated Charge: Percent

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 38
Other Proposed Changes to MRF
Proposal to Improve the Accessibility of Hospital MRFs
• Hospitals must include a .txt file in the root folder with direct link to their MRF on their public website
• The .txt file must include a standardized set of fields such as;
• the hospital location name that corresponds to the MRF
• the source page URL that hosts the MRF

• a direct link to the MRF (the MRF URL)
• hospital point of contact information
• Hospitals must include a link in the footer of their website (i.e., homepage) that links to their HPT page
• The link should be labeled "hospital price transparency" and links directly to the webpage that hosts the link to the MRF
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 39
Other Proposed Changes to MRF
Proposal to Improve and
Enhance Enforcement
• Requires an authorized hospital official to submit to CMS a certification to the accuracy and completeness of the standard charges' information posted in the MRF at any stage of the monitoring, assessment, or compliance phase.

• Hospitals must acknowledge receipt of warning letter notices (instructions within the letter)
• CMS may request payer contract information from hospital to assess compliance
• CMS may publicize on its website, info related to CMS assessment of hospital compliance, any actions taken against hospital, status and outcome of those actions.
Proposal to Specify Formatting Requirements for MRF Information
• Hospitals must conform to the CMS template layout, data specifications, and data dictionary to be compliant with 42 CFR 180.50(c) and avoid risk to compliance action.
• Technical guidance to encode standard charge information is made available thru a data dictionary and within CMS template
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 40
Other Proposed Changes to MRF
Proposal to Affirm Accuracy and Completeness of MRF

• Requires each hospital affirm directly in its MRF (using a CMS template) that it has included all applicable standard charge information in its MRF as of the date in the MRF.
• Each hospital would be required to add a statement affirming that, to the best of its knowledge and belief;
• the hospital has included all applicable standard charge information in its MRF, in accordance with the requirements of §180.50, and that the information displayed is true, accurate, and complete as of the date indicated in the file.
• Example: if a hospital does not have a cash discount price it needs to "affirm" that directly in the MRF so there is no question about whether that hospital is compliant. Do not insert “N/A” as a value.
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 41
Additional Tips
If using CSV format, any values that include commas should be enclosed in quotation marks. (ex., “OR Level 5, First 15 Min”)
Do not insert “N/A” if you do not have applicable data. This is a retraction from CMS original guidance back from 2021.
Percents should be displayed as a whole number (e.g., 50% should be displayed as 50)
Keep in mind some proposed requirements do not have a 60-day grace period (e.g., affirmation)
Hospitals must encode standard charge information that corresponds to each data element

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 42
Panacea’s Compliance Status w/ Proposed MRF Requirements

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 43 Proposed ”New” Requirement1 Applicable Data Sources Panacea MRF Status Addition of Consumer Friendly “Expected Allowed Amount” Requires Claims and Payment Processing in Conjunction w/ Payer Contracts Meets Proposed Requirements Payer Specific Negotiated Charge Percent Requires Payer Contract Rate and Term Sheets Meets Proposed Requirements Addition of Contracting Method (e.g., Fee Schedule) Requires Payer Contracts, Chargemaster, etc. Exceeds Proposed Requirements Additional Fields for Drugs (Unit and Type of Measurement) Requires Pharmacy Formulary, Chargemaster, Payer Contracts, etc. Exceeds Requirements Clarification of Payer Name and Plan Type (e.g., “Aetna” and “PPO”) Requires Payer Contracts Meets Proposed Requirements Addition of Setting (inpatient vs. outpatient) Requires Payer Contracts, Chargemaster, etc. Exceeds Requirements Addition of Billing Class (facility vs. professional) Requires Facility and Professional Payer Contracts, Chargemaster / fee schedule, etc. Meets Proposed Requirements Addition of Modifiers and/or Revenue Codes Requires Payer Contracts, Chargemaster, etc. Meets Proposed Requirements Addition of Financial Aid Policy Requires Review of Financial aid or cash price policy
to the items and services in the MRF. Meets Proposed Requirements
new
2024
applied
1Proposed
requirements listed here are only a subset of all proposed requirements in the CMS
Proposed rule
Tools and Resources
The proposed rule can be found on the CY2024 OPPS/ASC Proposed Rule Federal Register Page
• https://www.federalregister.gov/public-inspection/2023-14768/medicare-program-hospitaloutpatient-prospective-payment-and-ambulatory-surgical- center-payment
Voluntary sample formats, FAQs, etc. can be found on the CMS HPT Resources Page
• https://www.cms.gov/hospital-price-transparency/resources
CMS Validator Tool to Confirm MRF Alignment with CMS Voluntary Sample Format
• https://cmsgov.github.io/hpt-validator-tool/

Comment Period is Open Until September 11th, 2023
• https://www.regulations.gov (follow the “submit a comment” instructions)
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 44


Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 45 Strategies for Using Negotiated Rate Data
Have you leveraged the publicly negotiated rate data in contract negotiations?

Polling
a. Yes, we have had some success in using the machine-readable files and plan on using comparative analysis for negotiations
b. Not yet, need support in acquiring, aggregating, and / or cleansing the data
c. No, still not confident about the reliability and / or accuracy of the data
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 46
Question 4
Hospital Analysis – Meaningful Variation in Negotiated Rates Within Same PPO Product Type
*Comparative rates study performed by Panacea in 2023 using available and cleansed hospital machine-readable files from 7 hospitals in similar size and geography and within PPO based products.

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 47 $201 $168 $90 $171 $92 $216 $131 -40% -20% 0% 20% 40% 60% 80% Average Negotiated Rates for 80053 Comprehensive Metabolic Panel Mean = $137 Hospital A Hospital B Hospital C Hospital E Hospital D Hospital G Hospital F
Payer Analysis

Target Hospital: ABC Medical Center
Patient Class: Outpatient (SDS, POP, etc.)
Payers: Big 5, excl. Managed Medicare / Medicaid
Plan Type: PPO only
Outlier Logic Included: Yes
Confidence Level for Rate Methodology:
Primary
Secondary
Tertiary Peer Group
(w/ Primary Confidence Level)
*Negotiated Rate Position is based on a weighted average. 0% is the average.
**Peer Group Rank is based on Negotiated Rates and not Gross Charges (i.e., price)
Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 48 Payer and Plan Type Negotiated Rate Position Peer Group Rank (1=Highest) Gross Charge Position BCBS PPO 5% 2/5 120% Aetna PPO 30% 1/5 Cigna PPO 10% 2/5 UHC PPO -10% 4/5 Humana PPO -15% 5/5 Overall 8% 2/5 Overall
10% 2/5
1. Peer Hospital A
2. Peer Hospital B
3. Peer Hospital C
4. Peer Hospital D
5. Peer Hospital E
Service Line Analysis: Raise Prices or Negotiate Better Rates?

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 49 -40% 35% 10% -25% 25% -25% -25% 20% 30% 10% 13% 8% 10% 14% 9% -50% -40% -30% -20% -10% 0% 10% 20% 30% 40% Gross Market Position Negotiated Rate Position Contribution Factor Dx Radiology Cardiology Surgery Emergency Lab

Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 50 Importance of Removing Outlier Rates – CBC Lab Test Payer Average Hospital A Hospital B Hospital C Hospital D Hospital E Hospital F Hospital G BCBS HMO 120 $ 100 $ 140 $ BCBS HMO 163 $ 150 $ 160 $ 180 $ BCBS HMO 120 $ 120 $ BCBS HMO 165 $ 130 $ 200 $ BCBS HMO 120 $ 100 $ 140 $ BCBS HMO 140 $ 140 $ Average 178 $ 110 $ 135 $ 160 $ 140 $ 180 $ 140 $ 200 $ After Removing Outliers Payer Average Hospital A Hospital B Hospital C Hospital D Hospital E Hospital F Hospital G BCBS HMO 120 $ 100 $ 140 $ BCBS HMO 163 $ 150 $ 160 $ 180 $ BCBS HMO 1,560 $ 120 $ 3,000 $ BCBS HMO 165 $ 130 $ 200 $ BCBS HMO 120 $ 100 $ 140 $ BCBS HMO 140 $ 140 $ Average 416 $ 110 $ 135 $ 160 $ 140 $ 180 $ 1,570 $ 200 $ Before Removing Outliers






Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 51 How
Engage
Panacea On the web www.panaceainc.com Email: contact@panaceainc.com Phone: (866) 926-5933 Panacea Insights™ Thought Leadership Portal Watch a short explainer video https://www.panaceainc.com/rateanalyzerexplainer-video/ Learn more about Panacea’s Price Transparency Suite of Services www.cmspricetranparency.com Visit Panacea’s www.panaceainc.com/rateanalyzer to request a demo
To
with


Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 52
Featured in HFM Magazine! September & October 2023 Issues
Panacea


Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 53 Questions?


Software. Consulting. Education. Results. © 2023 Panacea Healthcare Solutions, LLC 54 www.panaceainc.com