




















20242025
Welcome to our Quality Account for 2024-25.
With the backdrop of significant change in the NHS, I am proud to see colleagues embrace this with a focus on integrated care to support our community, responding to local population health need.
Improvements to the care we provide are centred on the Government’s ‘three shifts’:
• Analogue to digital
• Sickness to prevention
• Acute to community
With high-quality care as our focus, we have set eight priorities for April 2025/26, with themes of:
• Continuing to maintain the 12-month rolling Hospital Standardised Mortality Rate (HSMR+) as ‘within expected’, and we will continue learning from every death. This will improve quality of care
• Improving patient outcomes and reducing harm from long waits in the Emergency Department (ED)
• Continuing to work with all clinical teams to reduce communication-related patient complaints
• Working to have 0 patients waiting over 65 weeks for treatment and significantly reducing the number of patients waiting longer than 52 weeks for treatment
• Continuing to roll out the national Call for Concern (Martha’s Rule) to reduce the risk of harm from clinical teams not recognising deterioration in a patient’s condition, ensuring patients, their families and carers are listened to
• Improvements in colleagues feeling safe to speak up about concerns, as demonstrated by our Staff Survey results
• Improvements in colleagues recommending PAHT as a place to work and to receive care or treatment, as demonstrated by our Staff Survey results
• Collaborating with our local system and regional partners on local health pathways, integration and infrastructure to improve patient care and experiences
Key highlights that have improved the quality of care we provide include successfully introducing our new electronic health record (EHR), Alex Health, in November 2024. Alex Health is core to the delivery of our digital strategy and substantially improves the quality of services we are able to offer to our local population. This is a fantastic achievement – thank you to all involved.
We want to be able to provide the most therapeutic physical environment for our population when they need acute hospital care. On this, in January 2025, the government confirmed the funding and timetable for a new hospital for Harlow, following a review of its New Hospital Programme (NHP). The Princess Alexandra Hospital scheme is in wave two and we are now planning to begin construction in 2032. Our new hospital will be part of the wider growth and regeneration agenda for Harlow and its neighbouring communities.
Thank you to all of the fantastic colleagues at PAHT for your commitment to providing the best care for our local population.
Best wishes

Thom Lafferty Chief executive
The Trust directors are required under the Health Act 2009, amendments published in the Health and Social Care Act 2012 and the Quality Account FAQ published in 2021/2 Annex 1, to prepare a Quality Account for each financial year.
The Department of Health has issued updated guidance regularly on the form and content of the annual Quality Account, which incorporates the above legal requirements.
In preparing the Quality Account, directors are required to take steps to satisfy themselves that:
• The Quality Account presents a balanced picture of the Trust’s performance over the reporting period
y The performance information in the Quality Account is reliable and accurate
y There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice
y The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, and is subject to appropriate scrutiny and review. The Quality Account has been prepared in accordance with Department of Health guidance
The directors confirm that, to the best of their knowledge and belief, they have complied with the above requirements in preparing the Quality Account.
Every year all NHS hospitals in England must write a report for the public about the quality of their services; this is called the annual Quality Account. The purpose of the report is to make the hospital more accountable to you the public and to drive forward improvements in the quality of our services.
At The Princess Alexandra Hospital NHS Trust, we are committed to making sure that we keep our patients and our people safe. Our focus has been to ensure we can provide all necessary care and treatment in the safest possible way, at the right time and in the right place for our patients. Through this, we are making our pledge to you about the improvements we intend to make over the period 1 April 2025 to 31 March 2026 by committing to our quality account improvement priorities.
This report will tell you how well we performed against the quality priorities and goals we set for the last year to cover 1 April 2024 to 31 March 2025 and the areas we have improved through this year.
We will describe to you the areas where we have reviewed our patient care in order to evaluate the quality of services provided. This report will contain mandated information from our Board, along with statements from our commissioners and partners. We will also provide a glossary of terms.
Our Quality Account is prepared in line with the Quality Accounts toolkit guidance with additional information included in line with advice received by NHS England as follows:
y Details of ways in which staff can speak up (including how feedback is given to those who speak up), and how the Trust ensures that staff who speak up do not suffer detriment
By order of the Board
y A statement regarding progress in implementing the priority clinical standards for seven-day hospital services

A statement that evidences an improvement plan to reduce rota gaps for NHS doctors and dentists (Schedule 6, Paragraph 11b of the terms and conditions of service for NHS doctors and dentists in training (England 2016)
The report is published following internal and external partnership engagement. The information was reviewed by the Trust Board in June 2025, with delegated authority given to our Quality and Safety Committee for final approval.
The most recent inspections of the Trust were completed by the Care Quality Commission (CQC) through unannounced focused inspections, these included a review of the Trustwide Well Led, Key Line of Enquiry in 2021. The care services inspected were:
Inspection report
y Maternity care
y Medicine (including elderly care)
The most recent specific focused inspection was completed in the Urgent and Emergency Care Department
Princess Alexandra Hospital Hamstel Road
Harlow
The CQC completed an unannounced focused inspection of the Emergency Department in March 2023 to monitor our progress against the Trust action plan and review our performance against their Key Lines of Enquiry standards.
CM20 1QX
Tel: 01279444455
www.pah.nhs.uk
Date of inspection visit : 6 to 7 July 2021, 10 August 2021, 14 July 2021, 17 August to 6 September 2021 Date of publication: 17/11/2021

Overall trust quality rating Requires Improvement
Are ser vices safe? Requires Improvement
Are ser vices effective? Requires Improvement
Are ser vices caring? Good
Are ser vices responsive? Requires Improvement
Are ser vices well-led? Requires Improvement
The recommendations received from the 2021 and 2023 CQC inspections were collated into individual projects. Each was updated by the relevant divisional team using our quality improvement methodology to enable a consistent and sustained approach to the achievement of these objectives. Each project had a designated executive, a senior responsible officer (SRO) and the Trust has a quality project management team to provide additional support.
We used our CQC quality improvement plan as a dynamic document; during the last year we have added additional improvement topics into it, as we identified further areas that we felt required improvement. The quality improvement plan is monitored monthly through the Clinical Quality Improvement Group which reports into the Trust Compliance group and onwards to the Quality and Safety Committee.
Our people use the CQC inspection outcomes as the foundation upon which to critically examine our services and focus on how we plan and deliver the fundamental aspects of safe care. We have taken decisive actions to change everyday activities, which have led to significant improvements.
We review our services against the amended CQC inspection framework (2024) and going forward the Trust has completed self-assessments against these quality statements.
The Trust is actively working across all our clinical services to measure our current performance position and identify the evidence we have in place to support each quality statement.
The Trust has set eight Quality Account priorities for delivery next year, these are identified in line with the four quality elements of the Trust five Ps strategy covering: our patients, our people, our performance and our places. We have developed these through consideration of the factors that matter the most to our patients which is to improve safety, reduce harm and waiting times and learn from their feedback. Also taking into consideration how we deliver improvements for our staff who are responsible for face-to-face patient care. This process has been supported by the clinical leadership team and members of the Trust board.
Our patients and our performance
1. We will continue to maintain the Trust 12 month rolling Hospital Standardised Mortality Rate+ (HSMR+) as ‘within expected’ and we will continue learning from every death. This will improve quality of care for all patients.
2. To improve patient outcomes and reduce harm from long waits in the emergency department, our improvement plans aim to reduce the numbers of patients within the department who are waiting for longer than 12 hours for treatment to less than 10% of the total attendances, that then are either admissions, discharged home or transferred to an alternative hospital setting.
3. We will collaborate with all clinical leaders to reduce communicationrelated patient complaints by 20% for 31 March 2026, as measured by patient feedback surveys and complaints data, through targeted staff training and regular feedback reviews, to enhance overall patient experience.
4. We will have zero patients waiting over 65 weeks for treatment and reduce the number of patients waiting longer than 52 weeks for treatment to no more than 1% by 31st March 2026 (this is
in line with national guidance). This will be delivered through improving the efficiency and utilisation of our clinical resources such as theatres, out-patient clinics and will be measured by the reported national submissions of patient waiting times and will improve experience for all of our patients.
5. Roll out Martha’s Rule to reduce harm from failure to recognise deterioration and ensure the patient’s family/carers are listened to.
Our people
6. We will improve the number of our staff who state that they agree / strongly agree that they feel safe to speak up about anything that concerns them in the organisation to over 60%. This will be measured through the annual staff satisfaction survey. This will benefit the Trust as concerns will be escalated and we will improve the wellbeing of our people.
7. We will improve by at least 10% the numbers of our staff who
• would recommend the Trust as a place to work to 55%
• would recommend the Trust as a place to receive care/treatment to 52%
This will be measured through the annual staff satisfaction survey. This will benefit the Trust through improved wellbeing of our people.
Our places
8. We will continue to work in collaboration with our local system and regional partners to improve local health pathways, integration and infrastructure to improve patient care and experience.
Our pounds - Nil
By improving the quality of care as detailed in the priorities above, we will deliver greater value for money for our patients and the Trust.
These priorities will be monitored using our existing governance structures; this will include being monitored through our Quality and Safety Committee.
PAHT is a 419 bedded hospital with a full range of general acute services, including; a 24/7 accident and Emergency Department (AandE), an intensive care unit (ICU), a maternity unit (MU) and a level II neonatal intensive care unit (NICU).
The Trust serves a core population of around 350,000 and are the hospital of choice for people living in East
Hertfordshire and West Essex. In addition to the communities of Harlow and Epping, we serve the populations of Bishop’s Stortford and Saffron Walden in the north, Loughton and Waltham Abbey in the south, Great Dunmow in the east, and Hoddesdon and Broxbourne in the west. The extended catchment areas incorporate a population of up to 500,000.
We own the main hospital site in Harlow, and operate outpatient and diagnostic services in both Herts and Essex, Bishops Stortford and St Margaret’s Hospitals. The operation of these site facilities forms part of the longer-term strategy of bringing patient services closer to where people live and making services, where appropriate, that are more accessible and easily available to patients.
We operate over 75 different services to meet the needs of our patients (the service portfolio is detailed within table 1).



Antenatal and New born screening
Early Pregnancy Unit
Children’s ward including patient at home (delivered by community provider)
Foetal Medicine
Infant Feeding support Maternity:
Antenatal clinics and ward
Bereavement services Birth Centre
Community midwifery services
Homebirth service
Labour Ward Maternity Assessment Centre (Day and Triage)
Obstetrics
Postnatal Ward Specialist antenatal services
Ultrasound scanning
Colposcopy and hysteroscopy services
Gynaecology ambulatory service
Neonatal critical care –special care baby unit and neonatal community nurses
Community midwifery
Gynaecology including Termination of Pregnancy Services
New-born Hearing Screening
Paediatrics:
Assessment
services Diabetic
Medicine
In-patients
Out-patients
Clinical Support Services
Audiology Blood tests Breast surgery Chemotherapy
Clinical Haematology Dermatology
Interventional radiology
Neurology Oncology services
Outpatients Pathology: Blood sciences and biochemistry (delivered by Health Service Laboratories)
Cellular pathology
Microbiology
Patient appliances Pharmacy services Physiotherapy
Occupational therapy Radiology
Speech and language therapy
Medicine
Transfusion services
Cardiology Diabetic medicine
Geriatrics including Frailty
Podiatry (delivered by community provider)
Surgery
Endocrinology General medicine
Medical in-patient wards Older People Assessment and Liaison
Oncology services relevant to medical care
Respiratory Medicine Rheumatology Specialist palliative care and end of life services
Day surgery
Colorectal services Ear Nose and Throat
Endoscopy services
Gastroenterology General surgery Genito-urinary medicine and Urology surgery High Dependency Unit
Intensive Care unit
Perioperative Medicine: Anaesthetics
Urology
Maxillo-facial surgery Ophthalmology Oral surgery
Surgery – in-patients Tissue viability Trauma and orthopaedics
Vascular services
Adult assessment services incorporating same day emergency care and urgent” hot” clinics
Emergency Department
Integrated Urgent Treatment Centre – in collaboration with Stellar Health, Stort Valleys Federation, Essex Partnership University Trust and Herts Community Trust
Paediatric Emergency Department
Patient at home, adult (delivered by community provider)
The review of services and all associated data is undertaken through the Trust governance structure. This includes monthly meetings reviewing information covering patient experience and engagement, patient safety, learning from deaths, vulnerable patients and the infection prevention and control committee and bi-monthly clinical effectiveness and compliance groups.
All of these groups report monthly into the Quality and Safety Committee, which is a subcommittee of Trust Board.
Review of each service’s performance within the Trust has been monitored through the Performance and Finance Committee, with external review undertaken by both Essex and Hertfordshire commissioners at the monthly Quality Assurance, Improvement and Performance Oversight Meeting.

Our patients and our performance
1. We will maintain the Trust Hospital Standardised Mortality Rate (HSMR) within the as expected range and we will continue learning from every death. This will improve quality of care for all patients.
Outcome: Achieved
The Trust has sustained the Hospital Standardised Mortality Ratio (HSMR) and Standardised Mortality Ratio (SMR), as ‘within expected’ in the national and regional position in the year December 2023 – November 2024.
During December 2023 to November 2024, the Trust consistently submitted fully coded data on a monthly basis with particular improvements noted in the capture of co-morbidity reporting and palliative care.
Continuous improvement in care for patients and robust review of deaths have seen the Trust maintain (for over two years), the “as expected” level in historical outlier categories such as acute kidney injury (AKI), chronic obstructive pulmonary disease (COPD), diabetes, fracture neck of femur and sepsis.
HSMR for the period Dec-23 to Nov-24 is 102.18 is “within expected” (see figure 3 below and HSMR for November 2024 and divided by months in the figure 4).
Figure 3: HSMR for the period December 2023 – November 2024 is 102.18 and “within expected” (confidence intervals 95.15 – 109.58)
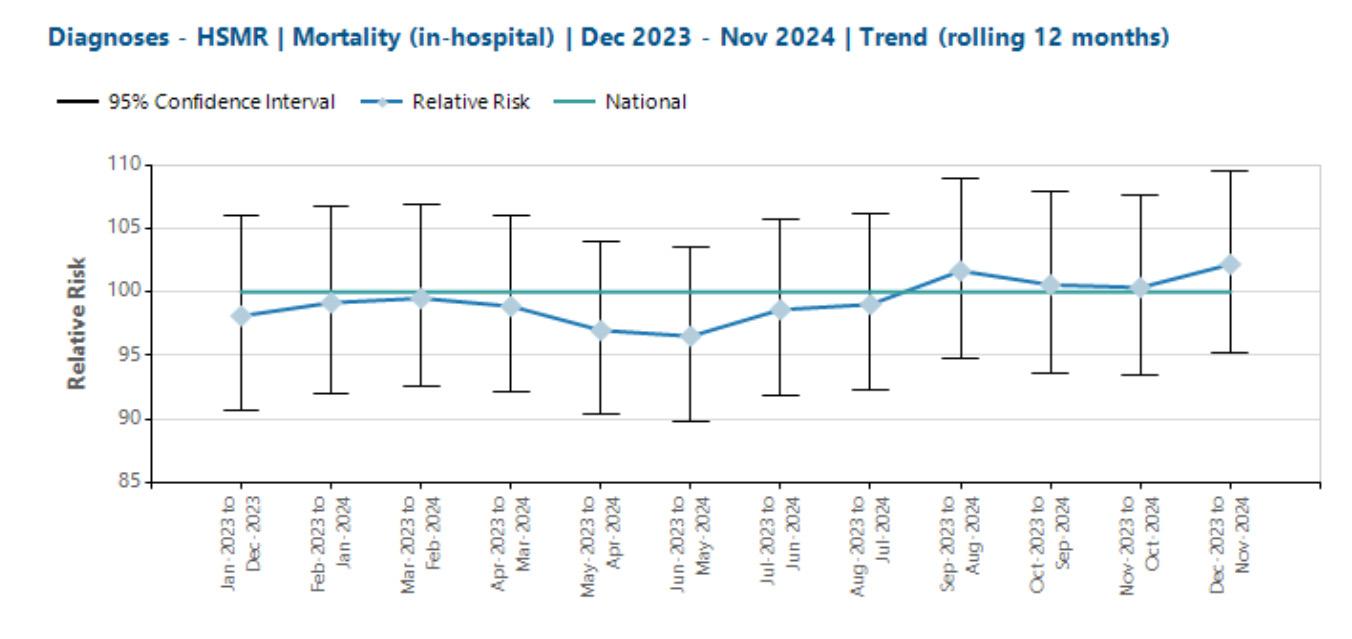
Figure 4: HSMR for November 2024 is 125.6 and “within expected”

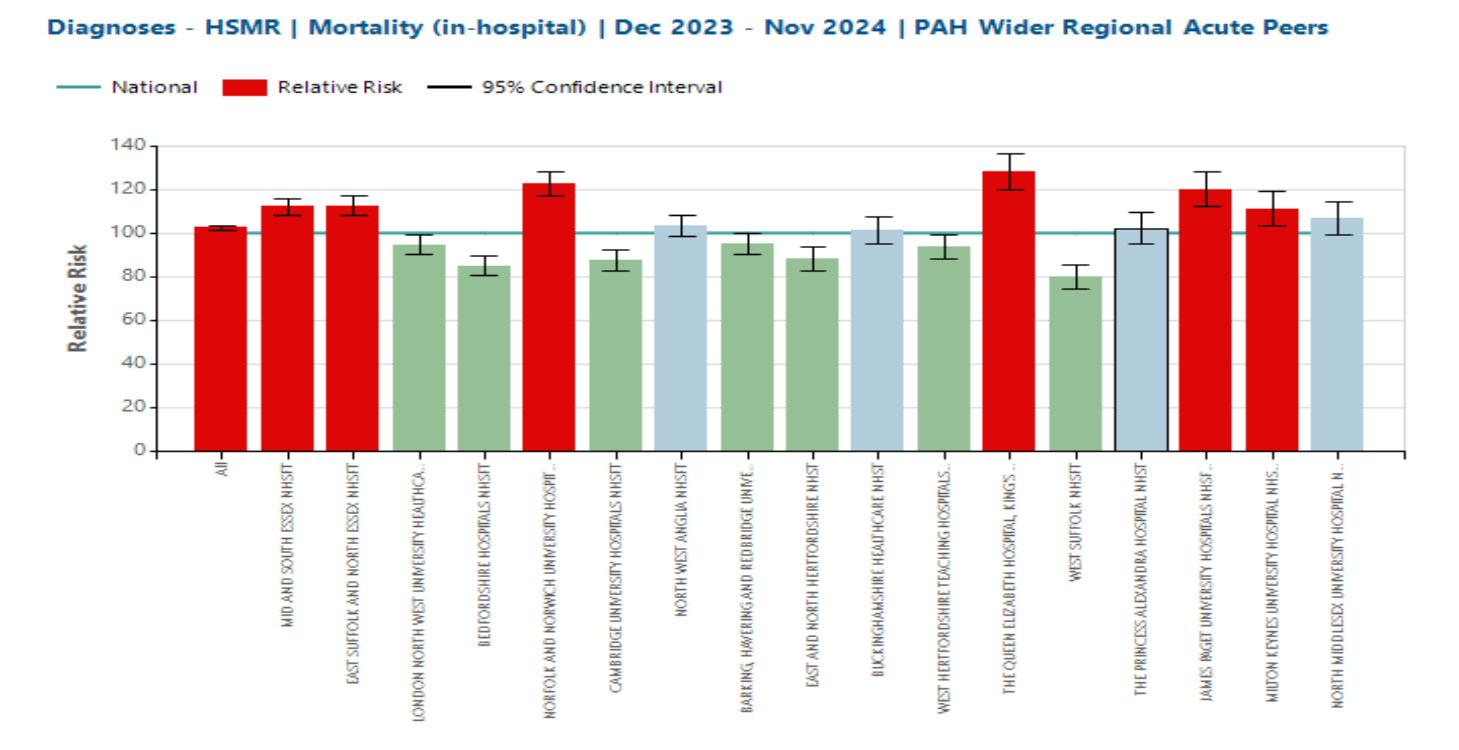
The Trust remained comparable to peers, and were not found to be statistically, significantly different to either the bespoke regional peer group, or national peers (see figure 5).
Figure 5: Regional HSMR is 102.3 and “as expected”
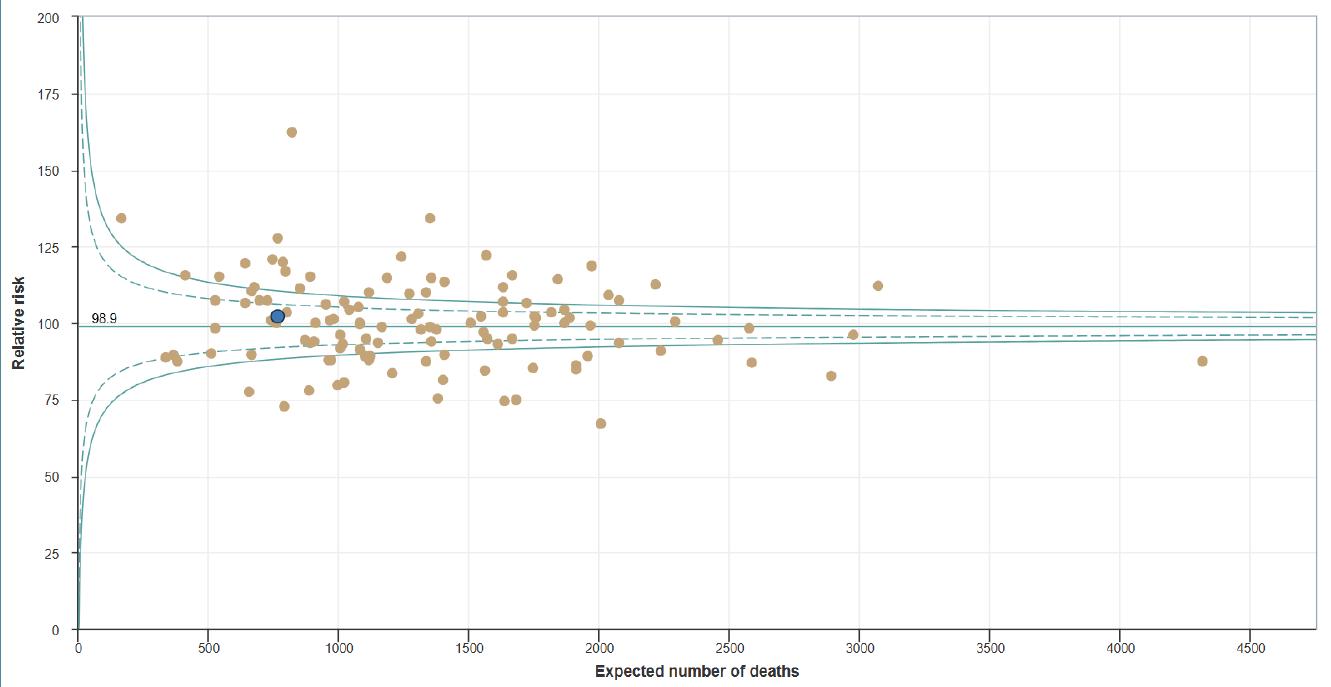
PAHT remained in a good position when compared with national data for similar types of organisations (See Figure 6, the Trust is the blue dot).
Figure 6: National HSMR for the period December 2023 – November 2024 is 102.3 and “as expected” (confidence intervals 101.0 – 103.6)
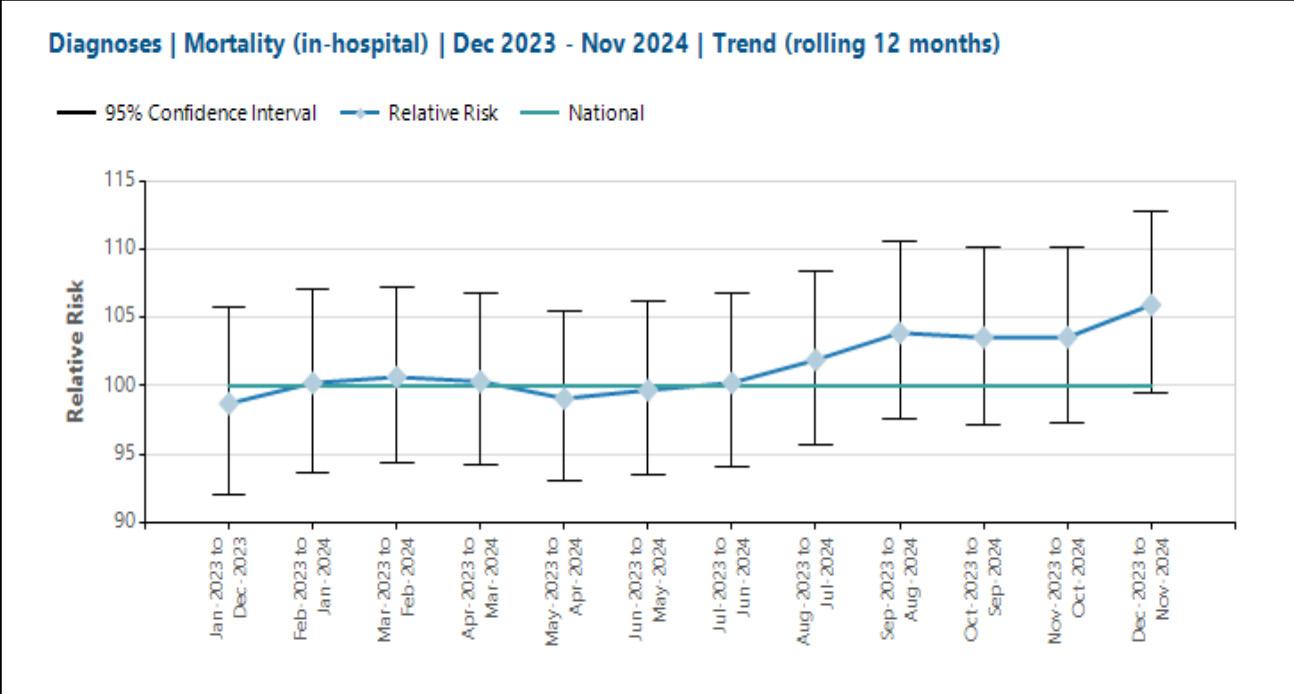
Standardised Mortality Ratio (SMR) up to November 2024 was 135.9 and “higher than expected” (see figure 7).
The number of super spells for the Trust’s SMR for Nov-24 was lower than previously, but the number of observed deaths was consistent month-on-month.
• The reason for the “higher-than-expected” outcomes is therefore pertaining to the trend in expected deaths. This had fallen to 58.9 for the month of Nov-24
• The reason for the change is believed to be two-fold:
o the amended HSMR to the newer HSMR+ model has impacted the Trust’s SMR
o coupled with the implementation across the Trust of our electronic patient record (EPR), introduced over the period 31 October to 3 November 2024, and this changed how the non-elective pathway patient data (for emergency admissions) was collected
o The most important reflection in the analysis has been that non-elective care did not appear to show signs of significant changes, due to the relationship between mortality and admission type. The majority, if not all of the Trust observed deaths are on non-elective pathways
o Elective admissions therefore carry a much lower risk of mortality and contribute a fewer number of expected deaths
o Day case admissions are automatically assigned a 0% risk of mortality. The Trust is therefore looking into the reporting of day case activity to ensure that it is reflected into the Trust’s risk-adjusted mortality values
o It is important to note that Nov-24 was the first month of mortality data received to incorporate the Trust’s new electronic patient record (EPR) activity
Figure 7: SMR for the period December 2023 – November 2024 is 105.9 and “within expected” SMR for Nov-24 is 135.9 and “higher than expected”
• The Trust continues to be in a good position during 2024/25 for the main mortality indices
• This also included the elimination of historical outlier categories seen in AKI, COPD, diabetes, fractured neck of femur and sepsis for over two years
• Since the beginning of this financial year, PAHT has remained in a good position compared to peers in our local region and nationally
• The introduction of the new HSMR+ model and our electronic patient record has affected the SMR data. We believe this is likely due to missing elective care data. This is being investigated
y Learning from deaths does not rely only on the mortality indices. The following processes complement the mortality data:
y The Telstra data set includes diagnosis specific mortality outliers. All of the patient deaths within each outlier group are reviewed by the clinical specialty leads and the coding leads
y All deaths are scrutinised by the Medical Examiner team
y 25% of deaths are further reviewed using the Structured Judgement Review approach and learning is shared through regular departmental mortality and morbidity (MandM) meetings
y In addition to the structured judgement reviews, a number of additional cases highlighted by the medical examiner were reviewed and presented by Junior Doctors at the speciality MandM meetings
y Any concerns raised through our review processes are scrutinised by the Trust Incident Management Group and reported as an incident on the Datix system
The SMART database is used for the completion of:
y Medical Examiner independent reviews
y Recording of Structured Judgement Reviews
y The database produces a mortality dashboard, which can be filtered to individual specialities or by divisions. This allows teams to review mortality over defined periods of time
y This has proved a useful tool in pulling themes and trends in order to understand the Trust’s mortality status and where improvements may be required. It also provides a useful digital platform for the management and standardisation across the Trust of the learning about Mortality and Morbidity meeting
y The SMART system has been adapted several times over the last year to incorporate tools in order for specialities to learn from deaths
y Learning from deaths is cross referenced with the Trust’s incident reporting system and patient experience team to maximise learning
y Learning from deaths of patients who die within 30 days of receiving anticancer treatments has been included in the SMART system, with a review form that reflects the national Systemic AntiCancer Therapy (SACT) tool. This has been implemented in oncology tumour sites and haematology
y Data received from the regional SACT data base assists with these reviews to ensure all appropriate patients are reviewed
y The Strategic Learning from Death Group continues to support and enable the mortality program in order to facilitate continued improvement of care of our patients
y The Deteriorating Patient Group continues to work closely with all divisions to improve both early identification and the quality of care delivered to the deteriorating patient across the Trust. The group has been integral in revising and improving the care and treatment provided to patients requiring non-invasive ventilation, to ensure accurate pathways are in place
y Patients’ deaths after a cardiac arrest have also been reviewed to ensure there is robust process in place for such deaths
y Further implementation of the SMART system will help to standardise and extend the mortality and morbidity program to all services across the Trust
y Enhanced networking with regional peers and primary care will continue to support learning across the system
Our patients and our performance
2. We will continue to deliver high quality care in the right place and at the right time for our urgent and emergency care patients working towards achieving the 76% emergency care quality standard. This will be measured and reported on national submissions of the four-hour access standard.
Outcome: Partially achieved Urgent and Emergency Care Performance
The percentage of patients that were
admitted, transferred, or discharged within four hours in the Emergency Department has significantly improved during the year and the Trust has an improving special cause variation (figure 8).
While the Trust has not achieved the national 76% within the four-hour standard during 24/25 overall for all attendances, the implementation of our electronic patient record (EPR) system in November 2024 impacted our performance.
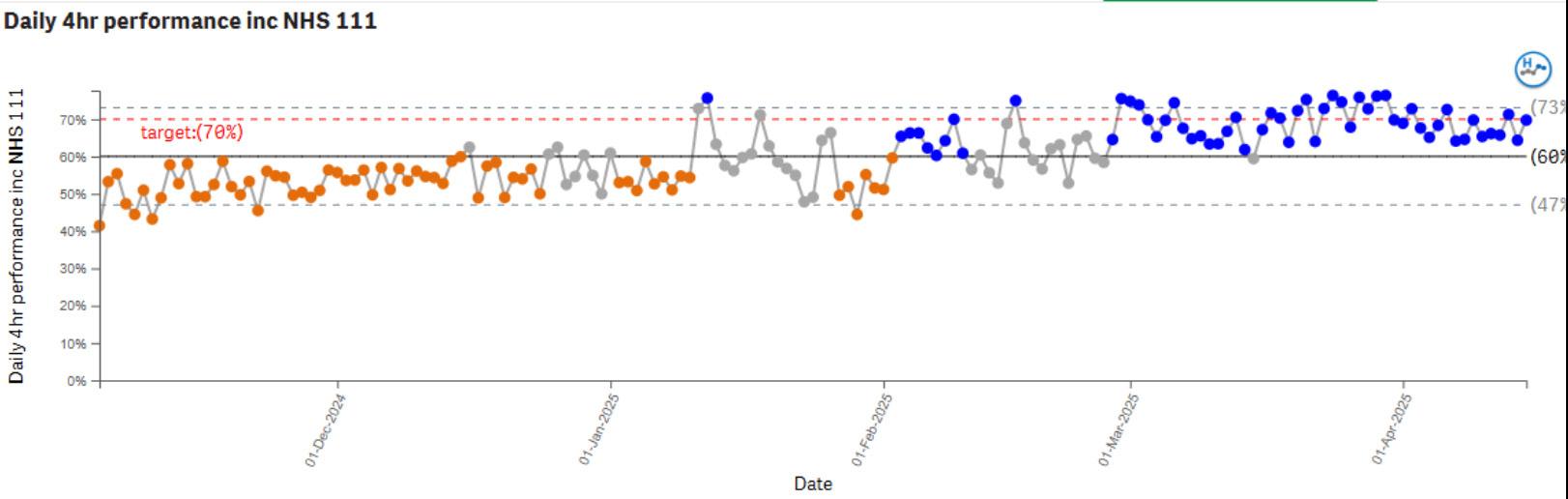
Following a recovery period, the Trust has increasingly achieved or exceeded the regionally agreed 70% four-hour standard.
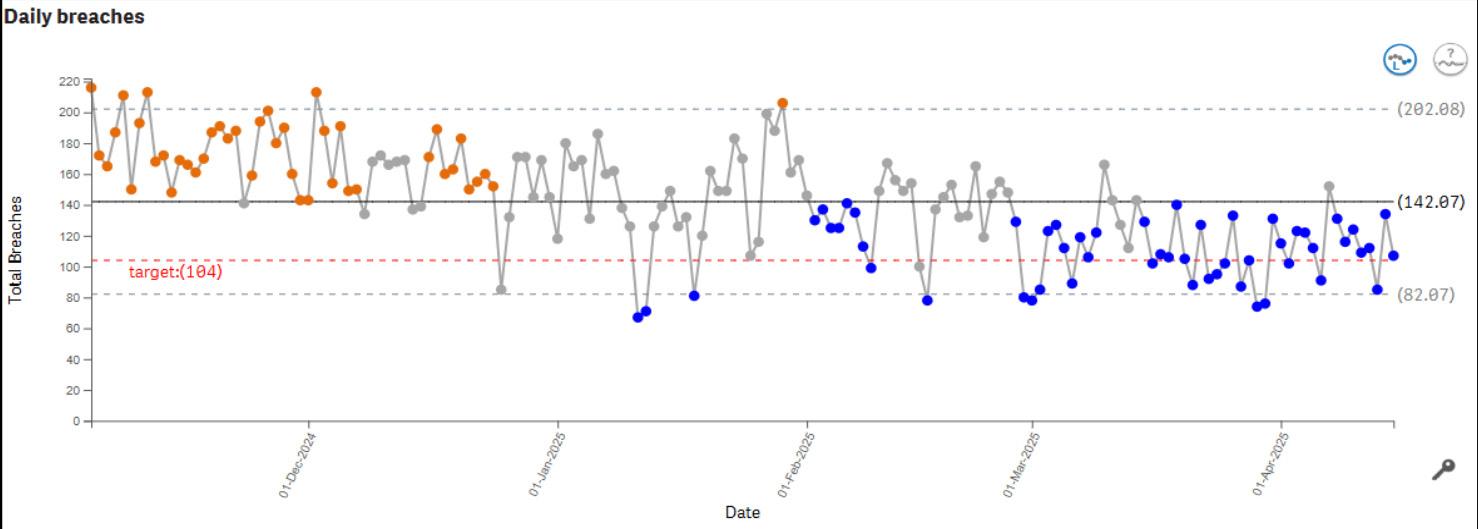
There has been consistent improvement seen with reduction in the numbers of patients who had breached the four-hour standard (figure 9).
Further to this, the Trust also saw a significant reduction in the percentage of patients who remained in the Emergency Department for 12 hours or longer (figure 10).
The Trust continues to work hard to reduce the length of time patients stay in the Emergency Department and have developed a comprehensive improvement plan to support further improvements.
Figure 10: Percentage of patients who remained in the Emergency Department for 12 hours or more

The Trust has achieved 100% compliance with the four-hour standard for the patients who have attended the Urgent Treatment Centre this year (called Type III attendances).
Within our Paediatric Emergency Department, the overall standard achieved was 81%.
Our patients and our performance
3. We will reduce the number of complaints or PALS concerns that detail communication as a theme by 10%.
We will focus on identifying that our feedback from patients demonstrates an improvement in communication with them. This will improve experience for all patients.
The percentage of complaints related to communication fell by exactly 10%, with 2023-24 (41%) and 2024-25 (31%).
However, in 2024/25 the overall numbers of complaints increased significantly and so this means the individual number of complaints about communication did not reduce, so this goal is only partially achieved.
Our patients and our performance
4. We will reduce inpatient falls with moderate and severe harm to less than 0.5 per 1,000 occupied bed days. The Trust will continue to learn from each of these incidents. This will improve quality of care for patients at risk of falling.
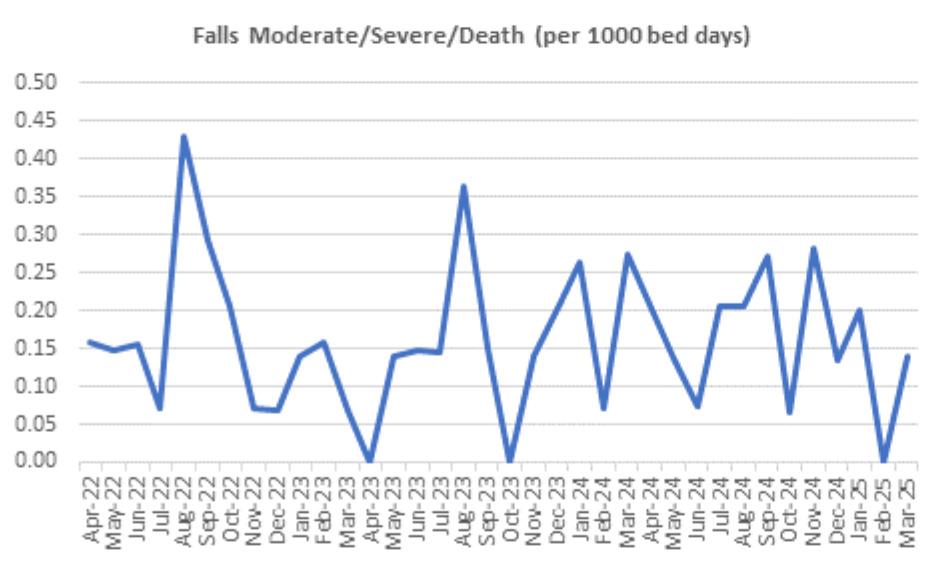
In year there was a decrease in the numbers of inpatient falls that resulted in moderate harm and a significant increase of the numbers of inpatient falls resulting in severe harm, table 2 and figure 11.
*The Trust now grades all incidents that result in a fractured neck of femur as severe harm.
All falls resulting in moderate or above graded harms are investigated individually and the reports are reviewed at the monthly Falls Investigation Oversight Meeting.
The members of the oversight meeting will determine if there is thematic learning or whether further investigation or action is required.
From work undertaken this year the following has been completed:
(i) The overall falls numbers met the objective set and were less than 0.5 per 1,000 occupied bed days.
(ii) During 2024/5 the Trust saw an increase in falls resulting in a fracture to the neck of femur to 14, each is graded as a severe harm incident.
The Trust had 10 fractured neck of femurs in 2022/23 and 8 in 2023/24.
• Following the first 8 incidents of inpatients sustaining a fracture neck of femur up to August 2024, the Trust completed a deep dive review of each of these incidents. This involved reviewing the investigation findings individually and then collating these as a thematic review
• The findings from this review did not identify any unknown care or service delivery issues outside of those areas already identified and included within the current Trust falls strategy
• During 2024 the safeguarding team become members of the Falls Investigation oversight meeting and part of the review is to determine whether or not all safeguarding requirements have been addressed. The expertise of the safeguarding team has given us greater assurance that through our incident reviews we have appropriately addressed potential safeguarding concerns. The team’s presence in the group and at the meetings enables those present to review and address any concerns in real time
The total number of inpatient falls that have occurred have reduced over the last four years.
• Comparison with total numbers in 2021/22 has reduced by 11.3%
• Patient deaths resulting from an inpatient fall during 2024/25 has increased to one
• Mandatory falls awareness training has been maintained at over 90% compliance
Figure 11: All Falls with Harm graded as Moderate/Severe/Death) per 1,000 bed days – 3-year data
Highlights and learning from 2024/25
y The Trust continued our monthly Falls Investigation Oversight group to review all moderate and above graded harms resulting from falls
y All care and service delivery themes identified from our investigations are incorporated into the Trust falls strategy
y The Trust has maintained mandatory falls awareness training compliance at over 90% each month
y We have strengthened the governance around the provision of enhanced care for patients. This included reviews of Level 4 patients (this group require close care where a staff member needs to be within arm’s reach) and the accuracy of the data recorded on Safecare
y Training on enhanced care and Safecare is now provided within the Registered Nurse preceptorship programme
y We have continued to recruit staff to the enhanced care team including the recruitment of a new band 4 team coordinator post
y We participated in the pilot phase of the NHS England collaborative looking at the provision of enhanced therapeutic observation and care
y Continued with the programme to encourage the reconditioning of our patients
y Continued to work with the lead frailty pharmacist to encourage the deprescribing of culprit medication (these are drugs believed to be the primary cause of adverse drug reactions)
y Undertaken a deep dive review of falls leading to fractures to the neck of femur
y Undertaken a small pilot study on the use of decaffeinated drinks to reduce toileting related falls. This small study was successful and is planned to be extended during 2025/26
y Refreshed the falls champions programme with regular update meetings and teaching sessions
y Developed and introduced a policy relating to the completion of neurological observations and undertaken an associated training programme to accompany this
y Commenced a review on the reasons for a rise in unwitnessed falls, we anticipate having the findings from this review over Quarter 2 (July to September 2025)
y Developed a trial programme on the completion of a vision assessment as part of multifactorial falls assessment (this is due to commence in June 2025)
y Improved Trust compliance for completion of lying and standing blood pressure (compared to 2023/24) and introduced a focused teaching programme following a small Staff Survey
y Continued with the bi-monthly meetings of the Improving Essential Care – Falls Prevention Group
Our patients and our performance
5. We will reduce the number of patients who sustain a hospital acquired pressure ulcer (HAPU) by reducing all pressure ulcers that could not otherwise be avoided to less than 3 per 1,000 occupied bed days and reduce moderate and severe harm pressure ulcers to <0.5 per 1000 bed days. This will improve the quality of care
received by our patients at risk of developing pressure ulcers.
In year 2024-2025 we reported 536 incidents of which there were 580 reportable Hospital Acquired Pressure Ulcers (HAPUs) of differing pressure ulcer categories.
These represent multiple patients who acquired more than one HAPU in the same incident. In year, the reported number of moderate harms is showing a slight increase per 1,000 bed days (Figure 12).
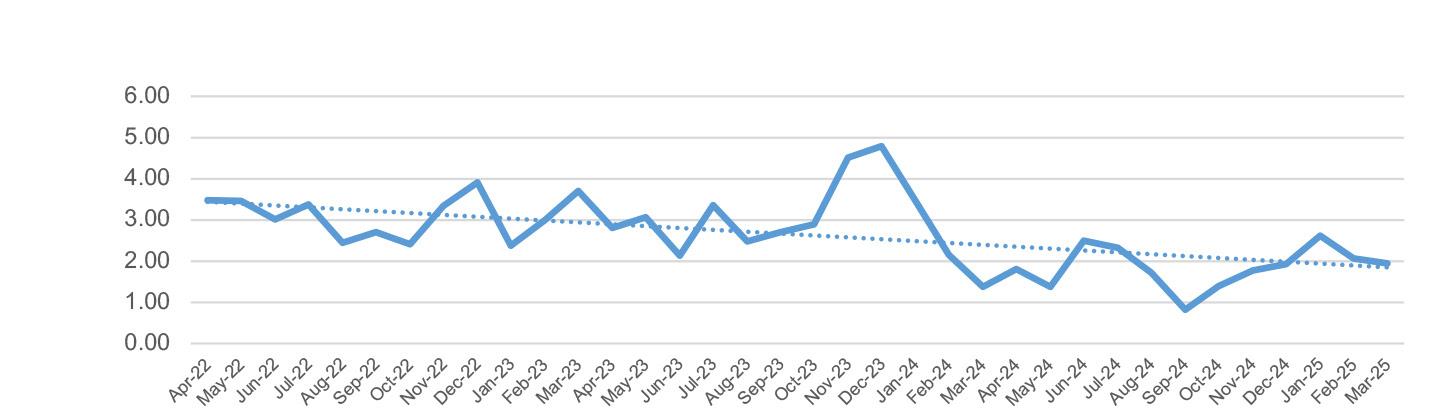
The total number of reported incidents has increased over the year, however the total HAPUs per 1,000 bed days has reduced from 3.5 in April 2022 to 2.0 in March 2025, which is below the Trust’s strategic aims to achieve less than 3 per 1000 bed days (Figure 13).
91% of HAPU incidents raised in 2024/25 have been validated and closed. There remains a further 49 incidents from 2024/25 to validate and close.
There has been no unvalidated severe harm HAPUs since November 2022 and there remains no open, unvalidated HAPU incident reports from 2022/23 and 2023/24.
Figure 13: Trust pressure ulcer rate during 1 March 2023 to 31 March 2025

Pressure ulcer reporting rate has remained within expected thresholds except for November - December 2023.
y During this time the organisation faced unprecedented demand on services, often exceeding bed capacity
y These delays contributed to the increased risk of developing pressure ulcers
y However, the reporting within 2024/25 stayed within the as expected range and did not demonstrate any special cause variation
y We continue to implement our Trust strategy on reducing hospital acquired pressure ulcers across the Trust
The data showed that hospital acquired pressure ulcers were less than 3 per 1,000 bed days since April 2024 and therefore the objective was achieved.
y Although the graph indicates there was a reduction in the total number of hospital acquired pressure ulcers, this is primarily due to the exclusion of the deep tissue injuries (DTI)
y This change is following release of national guidance recommendations in February 2024, stating that DTIs are now reported as vulnerable skin and no longer meet the requirement to be reported as pressure ulcers
y The Trust still categorised and monitored DTI incidents in year
The Trust completes an annually revised workplan aligned to our five-year comprehensive Pressure Ulcer Prevention Strategy, aiming to deliver improvement. This continues to be embedded and implemented as we aim to reduce all pressure ulcers, that could not otherwise be avoided.
The Trust’s Pressure Ulcer Investigation Oversight Group (PUIOG) as a sub group of the Improving Essential Care Group and has been established and embedded Trust wide in over the last year as part of our quality governance framework.
PUIOG has evolved to meet investigation requirements robustly and addresses quality improvement strategies in a timely manner. All clinical areas (as appropriate), have a quality improvement action plan that is reviewed by PUIOG on a regular basis. The primary focus is to review the progress of each ward’s action plans for delivery of our pressure ulcer prevention and measure improvement though the HAPU rates and fundamentals of pressure ulcer care delivery.
Validated harm levels are monitored monthly through the Pressure Ulcer Investigation Oversight Group (PUIOG) to identify areas of concern and incidents are therefore closed quicker with appropriate actions in place. The group identifies new emerging themes and ensures those themes are being addressed either, by a local action plan, a strategic action plan, quality initiative or held on the relevant risk register.
As part of the 5-year strategy, the dedicated Pressure Ulcer Prevention Practitioner is identifying early skin changes due to closer monitoring. This has resulted in an increase in current reporting (Figure 12). It should be noted that through earlier identification of skin changes, this will assist in improving the quality of care given to our patients and potentially reduce deterioration of skin and moderate harms.
Within the five-year strategy, we have also:
y Embedded the national assessment tool called Pressure Ulcer Risk Primary or Secondary Evaluation Tool (PURPOSE T). This was implemented in the last six months alongside the new electronic patient record (Alex Health), the new digital system which continues to be embedded Trust wide. The risk tool within our electronic patient record is aligned to national guideline, that is aimed to give earlier identification of those patients most at risk via early risk screening, from the start of their journey into the hospital through to discharge
y Implemented “care colour circles” that was a project introduced to provide a visual aid to assist staff with prioritising high-risk patients in relevant clinical areas
y Updated and implemented our e-learning to support national guidelines; including information on essentials of pressure ulcer prevention, Purpose T risk tool and the new categorisation of pressure ulcers
y Trust has purchased 90 footstools to assist patients to take weight off their heels (off-loading), 60 are already in place with a further 30 to be delivered
y Launched new animated teaching videos using Instagram and other digital platforms
y Collaborative project implementing inflatable trolley overlays for use in the Emergency Department as a preventative measure and to improve patient comfort
y Introduced two new Patient Information Leaflets for Pressure Ulcer Prevention; these are aimed to inform patients and their family members/carers and are aligned to national guidelines
y Conducted a Trust wide audit to give insight into our compliance with the pressure ulcer prevention care bundles and provide baseline data prior to new PURPOSE T tool
We continue to strive to deliver effective pressure ulcer care for our patients and aim to reduce pressure ulcer harms that could not otherwise be avoided. We aim to improve the quality of care received by our patients at risk of developing pressure ulcers.

Our patients and our performance
6. We will reduce the number of patients waiting longer than a year for their elective treatment by improving the efficiency and utilisation of our clinical resources such as theatres and out-patient clinics. This will be measured and reported by national submissions of patient waiting times.
The Trust remains committed to reducing long waits for elective care and has continued to prioritise this objective throughout 2024/25. A key focus for the year was on treating the most clinically urgent patients and addressing the longest waiters. As a result, the Trust successfully reduced the number of patients that were breaching 65-weeks, with only a small cohort of patients that choose to wait beyond the timeframe up to 31 March 2025.
In total, the Trust treated approximately 10,000 patients who had been waiting over 52 weeks.
This represented a 43% increase in patients treated during 2024/5 when compared with the 6,000 patients treated in 2023/24. This marks a significant improvement in access for patients experiencing the longest waits.
However, whilst performance against longwaiting patient treatment target improved, the overall number of patients waiting over 52 weeks increased during the year. This was primarily due to capacity being directed toward managing those longest waiting patients which therefore limited the ability to prevent those near the 52-week breaches from being treated.
Positively, the Trust also made targeted improvements for children and young people. Recognising the impact of long waits on this group, the Trust reduced the proportion of patients under 18 years of age waiting over 52 weeks from 18% at the start of April 2024 to 9% by year-end.
This objective will continue for next year with the priority set to work towards achieving the national guidance standard for 2025/26 which requires we:
y Sustain zero patients waiting over 65 weeks
y Prioritise the reduction of all patients waiting longer than 52 weeks for treatment to have no more than 1% of its patients waiting longer than a year by 31 March 2026
y Acknowledging the significant impact on children and young people from waiting a long time for their treatment, the Trust has set a local ambition to achieve having no more than 1% of children waiting longer than a year by September 2025 and to achieve no year long waits by no later than 31 March 2026
Our patients and our performance
7. The Trust developing change strategy is aligned with our core values of everyday excellence as we move forward on our journey to becoming a learning organisation. We will foster a culture of continuous learning, adaptability and knowledge sharing, to not only deliver successful and effective transformation but also to empower our people and teams to evolve and thrive in their delivery of everyday excellence.
Objective: Partially achieved
PAHT2030 Change Strategy
NHS Impact is the new, single, shared NHS improvement approach. NHS Impact has been launched to support all NHS organisations, systems and providers at every level, including NHS England, to have the skills and techniques to deliver continuous improvement.
There are five components that form the ‘DNA’ of all evidence-based improvement methods, these principles underpin a systematic approach to continuous improvement:
1. Building a shared purpose and vision
2. Investing in people and culture
3. Developing leadership behaviours
4. Building improvement capability and capacity
5. Embedding improvement into management systems and processes
Part of our (PAHT) response to ‘building a shared purpose and vision’ is the development of our ‘PAHT2030 Change Strategy’. The goal for this strategy is ‘deliver a change approach that enables us to achieve outstanding and sustainable results across our five Ps, ultimately ensuring that we are modern, integrated and outstanding’. The strategic driver diagram below outlines the key elements of the strategy:

Our 5 Ps consist of
y Our Patients
y Our People
y Our Performance
y Our Places
y Our Pounds
In year the Trust strategy was approved, this now needs to be fully embedded to sustain the strategy during 2025/6.
8. We will improve our people’s satisfaction measured through the annual staff satisfaction survey. This will benefit the Trust through improved wellbeing of our people and support our continued focus to drive a positive culture.
The Trust response rate to the Staff Survey was 49.33%, this was equal to the median response rate of the comparison group (49%). Although this was statistically lower than last year’s response rate of 49.7% by 0.37%.
When looked at against the headcount of eligible staff able to respond this equated to an increase of 6.6% of our staff engaging with the survey which is equivalent to 275 people.
Staff Survey results for 2024 against those for 2023 showed that we scored:
y Significantly better in 7 questions with the most improved scores relating to witnessing an error/near misses, staffing levels, level of pay and burnout
y A marginal reduction in that our people felt we are keeping them safe and healthy, however the health and safety climate score has seen an improvement, this sub score includes the question relating to my organisation takes positive action on health and wellbeing which increased by 0.76%
Figure 14: Staff Survey 2024 scores vs 2023 scores

Following the results of the annual Staff Survey (2023), the Organisational Development Department (OD) prepared survey analysis and materials for each division and subdivision. ‘Feedback To Action’ leads were appointed, with workshops held in 2024 to discuss results and generate improvement action plans.
The action plans were linked to the Trustwide Staff Survey improvement priorities which were:
1. People Promise: We are always learning
2. People Promise: We are safe and healthy
3. This is Us management practices and leadership promise
For 2025/26 the executive team has identified three key areas for all divisions to concentrate on within their 2025 engagement plans:
y People Promise: We are compassionate and inclusive
y People Promise: We are a team
y People Promise: We are recognised and rewarded
Furthermore, each division is to fully review the findings specific to their department and sub-departments and add any additional areas of focus specific to them onto their engagement plans.
The NHS People Promise continues to be important as we strive to deliver care in line with our values and our quality and patient safety strategy.
People feeling safe to speak up and creating psychological safety remains a key focus for the Trust, there are currently 29 Freedom to Speak Up (FTSU) ambassadors who have a wide range of ethnic and professional backgrounds.
y There is a split of ambassadors from the Divisions and this information is shared with the Divisions to support the update for future cohorts to ensure equity of support
y The guardians and the ambassadors continue to raise the profile of speaking up and deliver training and drop-in sessions across the organisation
y There are videos on AlexNet for staff to access to raise their awareness of how to speak up
As part of their focus on psychological support, in April 2024 the staff health and wellbeing team were successful in being awarded funding from the Trust for a psychological staff support service. This was commissioned with Here for You (HFY) via Essex Partnership University NHS Foundation Trust (EPUT) after central funding ceased from the Integrated Care System (ICS) in January 2024.
y The Here for You (HFY) staff support service is a core aspect of the health and wellbeing offer and strategic direction for staff at PAHT
y Whilst it is a specialist clinical service offering psychological assessment and intervention for staff and teams, the service also provides subject-expert led webinars and resources as well as consultation back into the wider organisation and system
As part of our ongoing commitment to building a sustainable, inclusive local workforce, the resourcing team has significantly expanded its outreach and engagement activity over the past year. Working closely with community partners, educational institutions, and employability services, we’ve strengthened pathways into healthcare careers and ensured our recruitment activity reaches a broad and diverse audience.
9. We will continue to work in partnership to improve our hospitals and health infrastructure for our patients.
Following the election in the summer of 2024, a review of the New Hospital Programme (NHP) was announced. The Trust expected the Autumn Budget Statement to say more about the degree of commitment to the NHP, but instead it trailed that a more detailed statement from the Department of Health and Social Care would be issued in the coming weeks. In late November 2024, the Chief Programme Officer for the New Hospital Programme announced that there would be a statement from the Secretary of State in January 2025 on the scope of the programme beyond the Reinforced Autoclaved Aerated Concrete (RAAC) and other schemes excluded from the NHP review. The Trust was placed in wave 1 of the New Hospital Programme.
Following the government announcement on 20 January 2025, our Trust was confirmed to be placed in wave 2 of the New Hospital Programme. This in turn has signalled a construction start date of 2032, with a budget envelope of £1.5 to £2.0 billion. NHP also confirmed that site acquisition activity could continue to “de-risk” the programme.
Our staff continue to work in partnership with a wide stakeholder group of experts to deliver a Community Diagnostic Centre (CDC) at St Margaret’s Hospital in Epping. As the lead organisation for our CDC programme, we are committed to delivering an innovative and fit for purpose Community Diagnostic Centre by refurbishing and extending the existing NHS estate at this site.
The CDC will provide additional scanning and diagnostic testing at the weekend and longer opening hours during the week. This development brings diagnostic tests closer to patients homes, increases the number of appointments and extends the days of the week that tests will be available, which will support local people.
The new CDC will receive the first patient from January 2026.
Infection Prevention and Control (IPC), and the reduction of healthcare associated infections (HCAIs) has remained a top priority for the organisation, and forms part of the Trust’s overall risk management strategy. The IPC team are supported by the Trust Board in ensuring that effective prevention and control of infections are integral to everyday practice, and this is applied consistently by everyone, promoting a culture of patient safety within the Trust. IPC is embedded into the governance processes and forums across the organisation.
The Infection Prevention and Control Committee (IPCC) meet bi-monthly (was monthly until July 2024) and is chaired by the chief nurse. The Committee has continued to maintain an overview of IPC priorities, linking to the risk management and clinical governance arrangements for the Trust, and reports to the Quality and Safety Committee. Additionally, the Infection Prevention and Control Steering Group (IPCSG), which meets monthly, increasing frequency as required (chaired by the deputy Chief Nurse), is a sub-group of the IPCC. The IPCSG has
an operational overview of IPC, and is responsible for reviewing achievements and risks against agreed performance indicators, monitoring trends of healthcare associated infections (HCAIs), reporting these to the IPCC.
Infection prevention and control key performance indicators for health care associated infections
NHS England (NHSE) sets trajectories / threshold values for all NHS Trust’s on specific organisms; these form part of the NHS standard contract to minimise infections, and reduce harm to patients including:
y Clostridiodes difficile (C.difficile)
y Meticillin-Resistant Staphylococcus Aureus (MRSA) blood stream infections (BSIs),
y Gram-Negative BSIs (GNBSIs)
The Trust’s performance on these organisms for 2024-25 is shown below in Table 3. The data in the table also shows comparative rates of infection per 100,000 occupied bed days for the 14 Trust’s within the East of England (EoE) region. The Trust demonstrated a lower rate of infection (in some organisms this is significantly lower and for others it is marginally lower) then the East of England average across all alert organisms.

Table 3: Mandatory alert organisms data for Trust and East of England 2024-2025
Clostridium difficile
y The Trust did breach its set threshold for C.difficile; as a total of 65 hospital and community onset health care associated cases were reported during the year 2024-2025. This was over the Trust’s set threshold value allocated for the year, it should be noted that PAHT was given a significantly lower threshold then many other Trust’s within both our local Integrated Care Systems (ICS) and across the EoE region (due to our previously lower-case numbers). Of the 14 acute Trust’s in the East of England region, only two had a lower trajectory than PAHT. As can be seen in Table 3, Trust infection rates were slightly lower than the regional average.
Of our cases:
y 42 were hospital-onset health care associated infections (HOHA), meaning they were detected three or more days after admission to the Trust
y 23 were community-onset healthcare associated (COHA), detected either in the community, or within two days of a hospital admission, and the patient had been an inpatient in the Trust in the previous four weeks
y The increase in cases of healthcare associated C.difficile infections is reflective of regional and national activity
y All healthcare associated cases of C. difficile are investigated to ensure that gaps in practice and corresponding actions are identified and monitored
y Management of C.difficile is further supported by multidisciplinary ward rounds completed by the microbiology consultants, antimicrobial pharmacist and the IPC nursing team
y Good antibiotic control is a key strategy for the control of this organism, however, C.difficile is multi-factorial and prevention requires a number of control measures, including hand hygiene, isolation, good environmental cleaning / deep cleaning programme, and appropriate use of personal protective equipment (PPE)
Methicillin-resistant Staphylococcus aureus (MRSA) Blood Stream
(BSIs)
For MRSA BSI, there were two cases during this year:
y Both cases had full investigations undertaken in conjunction with the clinical teams, which ensure any gaps in practice are managed appropriately and that learning is identified to help prevent future cases
y There is a continued focus on the management of peripheral intravenous lines (drips given to administer fluids), which are known to be the source of some BSIs
Methicillin-sensitive Staphylococcus aureus (MSSA) BSIs
Although there was no threshold set for cases of MSSA, cases continue to be closely monitored, with a review of each case undertaken. Over last two years, the Trust has reduced its cases of MSSA; however, it is important that there is a continued focus on peripheral intravenous catheters as they have been a contributing factor to some cases of MSSA, as well as for MRSA.
In line with the ambition to reduce the incidence of GNBSI in England, the IPC team have continued to monitor trends in these organisms throughout the year. In year there has been
y A focus on improving our local data as we reported more respiratory source GNBSIs in 2023-2024 than average;
y Trust data for 2024-2025 data is now in line with national data.
y As the largest number of patients with GNBSIs continue to be those of urinary origin, various strategies are still in place to reduce these infections including:
• sepsis prevention
• urinary tract infection (UTI)
• catheter-related UTI prevention
• dissemination of patient information (hygiene, good hydration)
• improved education and training of staff
• antimicrobial stewardship (improved antibiotic treatment of UTIs) and surveillance
• a focus on the GNBSI patient group that have hepato-pancreatobiliary (HPB) disease
Although there are no performance indicators for respiratory infections, the winter period was very challenging this year for both our Trust and most NHS organisations, particularly due to the significant increase in the numbers of influenza A cases, resulting in much higher numbers than usual. The Trust:
y Experienced eight outbreaks of influenza affecting only small patient groups, despite the significant number of Influenza A cases detected
y To reduce this infection the Trust Infection Prevention and Control Steering Group (IPCSG) recommended that our staff use fluid resistant surgical masks during January and February 2025 to reduce the impact of Influenza A on patients and our staff
y Noted other respiratory viruses were also managed in this period; whilst there was been operational impact, clinical significance for most patients was low. These viruses include:
o COVID-19
o Human metapneumovirus (hMPV)
o Influenza B (although in much smaller in numbers than influenza A).
o Respiratory Syncytial Virus (RSV)
Increasingly complex patients, with resistant organisms, are placing pressure on healthcare systems for more suitable environments (new hospital programme); there is a growing requirement for higher numbers of side rooms with en-suite facilities to be part of the Trust estate. In our wards, the bays consist of multiple beds making it more challenging to manage the transmissions of certain organisms such as those of respiratory source, and viral diarrhoea and vomiting infections.
In managing HCAIs, the key measures monitored for preventing infection are based on the guidance from the National Infection Prevention and Control Manual (NIPCM) have been implemented. Ongoing education on transmission-based precautions has continued; this supports the safe management, and reduction of, transmission of infections.
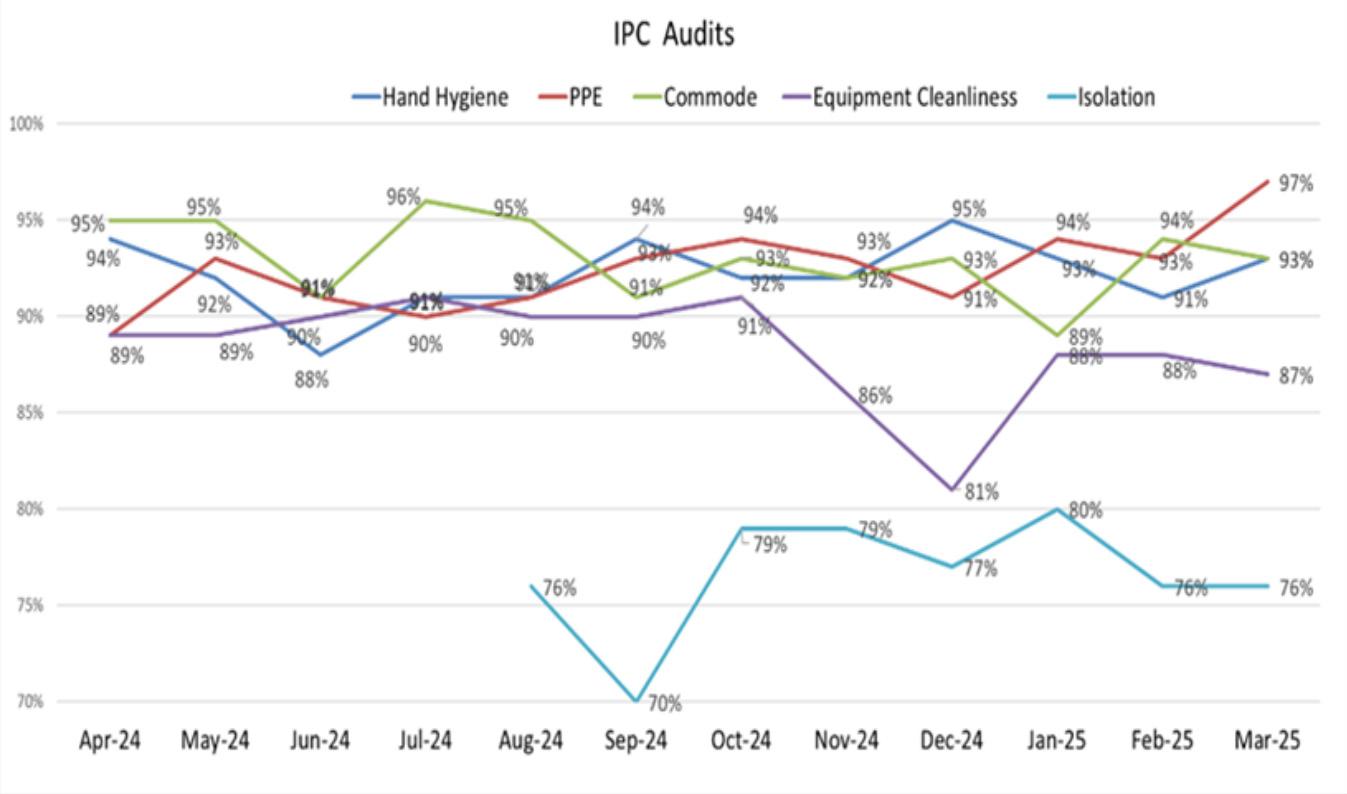
A number of IPC audits are undertaken on a monthly basis across the Trust by the IPC team, including:
y hand hygiene compliance
y personal protective equipment (PPE)
y cleanliness of equipment
y cleanliness of commodes
y More recently, compliance with isolation practices
For most audits, compliance across the Trust has been above the expected standard of 90% for the year (Figure 15), recognising there is still improvement needed for equipment cleanliness and isolation.
Expected compliance for statutory / mandatory training is 90%. As can be seen in Figure 16, there has been a gradual improvement over the course of 2024-2025 for both Level 1 (non-clinical) and Level 2 (clinical) compliance. Most divisions have achieved above 90% for Level 1, whilst for Level 2, compliance is slightly under trajectory, but has increased. This continued to be monitored with divisional leads through IPCSG and IPCC.
Figure 16: Level 1 and Level 2 IPC Training Compliance 2024-2024

In 2025-2026, the aims are to:
y Continue the improvement plans for the reduction of C. difficile cases
y Continue the daily antimicrobial stewardship across the Trust
y Focus on reducing the number of avoidable bloodstream infections for both MRSA, MSSA and GNBSI
y Ensuring that we are prepared in advance of winter to manage any surges in respiratory infections is also of great importance for the safe management of patients and the operational performance of the hospital
y Collaborative working with our Estates and Facilities teams on building and improvement projects and joint environmental audits

At The Princess Alexandra Hospital NHS Trust (PAHT) we define quality improvement as: ‘Working together in partnership to make the sustainable changes that lead to us being modern, integrated and outstanding for our patients, people, places, performance and pounds.’
The quality improvement (QI) team have two key roles. The first, is to support the Trust in building quality improvement capability and capacity by providing learning and development as well as facilitating and coaching others to achieve their quality improvement aims and objectives. The second, is to manage improvement and transformation programmes and projects that address organisational risks or the realisation of strategy. The following improvement programmes are the ones the QI Team continues to support:
y PAHT2030 Change Strategy
y Alex Health Transformation
y Outpatients Programme
y Urgent Care Programme (UEC, SDEC and discharge)
y Theatres
y Musculoskeletal (MSK) lead provider
y West Essex HCP Transformation (frailty, adult as well as children and young people)
A core part of our ‘PAHT2030 Change Strategy’ is strengthening our approach to building capability and capacity at PAHT for Quality Improvement and Transformation. The Improvement Partnership is central to achieving this. Our goal is to equip all staff at appropriate levels with the improvement training and support so that everyone at PAHT can run improvement projects and improve their daily work.
As part of our ‘PAHT2030: Change Strategy’ we need to agree a ‘dosing strategy’ with divisions and corporate teams to better ensure staff have the capability and capacity to deliver improvement. We have a proposed QI dosing model, which is based on guidance from NHSE, it includes a plan for numbers needing to be trained across PAHT, training course proposal and goals per staffing group, (figure 17).
This will encompass:
y Utilisation of those that are already trained in Improvement methodologies, this included Improvement Partners and QI Coaches
y Long-term QI training staff plan which includes roles/staff need to be trained at different levels of expertise and a trajectory for achieving this
y Plan to ensure all staff have a basic awareness of QI
Figure 17

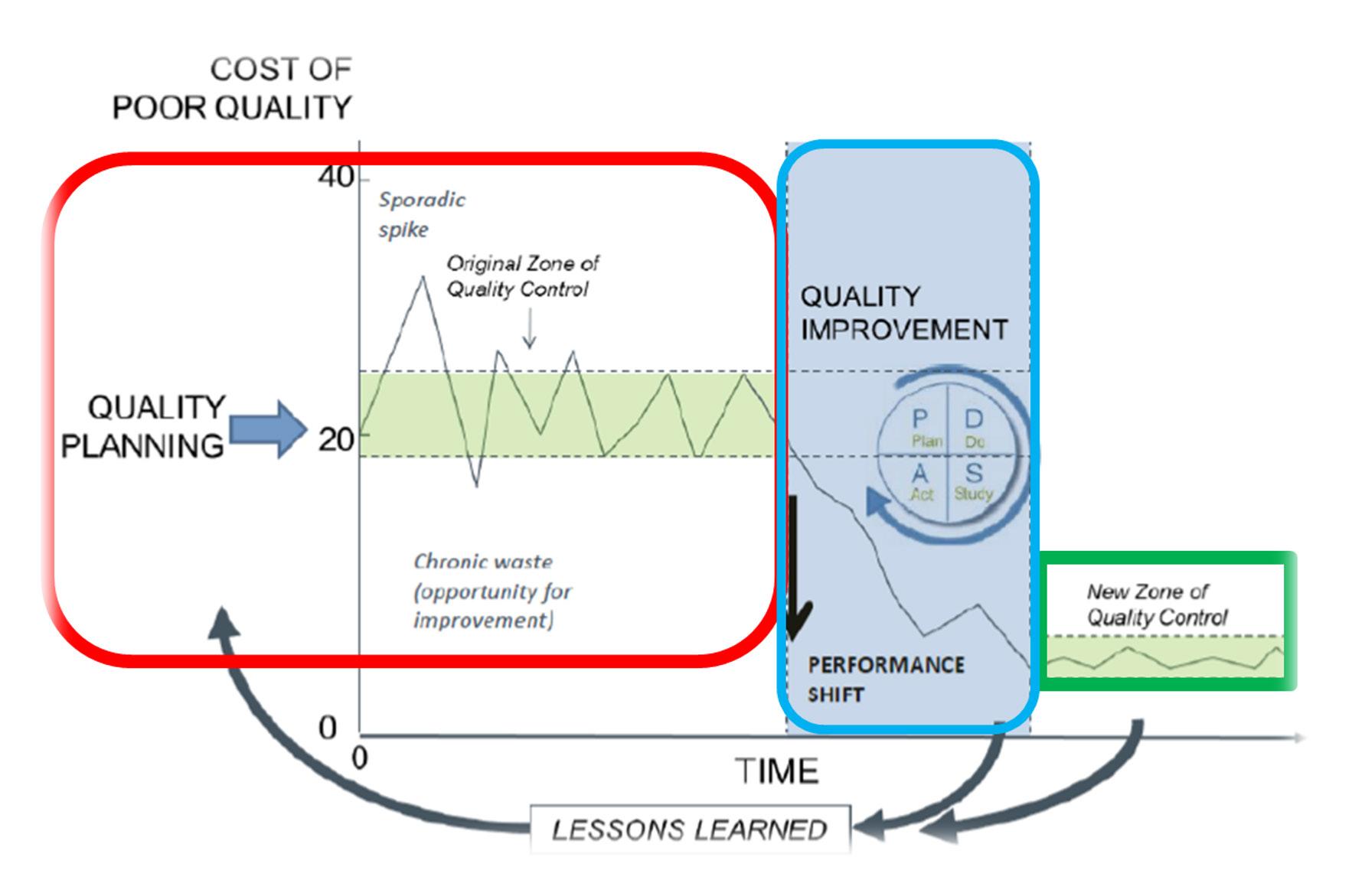
Part of the PAHT2030 Change Strategy is to formally introduce a QMS. Much of this is in place; however, this is an opportunity to formally achieve a best practice approach built on the learning from other organisations that have change and quality improvement well established and embedded. The three elements of the QMS that is proposed are quality planning, quality improvement and quality control. ‘People’ are at the centre as a way of emphasising the fact that everything we do is enabled and driven by our people, which includes patients, partners and the wider community that we serve (as summarised in figure 17).
The three elements (phases) of the QMS of quality planning, quality improvement and quality control are explained below:
y Quality planning is a strategic process whereby we evaluate how a service or clinical area is performing and plan the quality priorities that need be addressed in order to redesign or shift these to a new level of performance to best meet the needs of our service users
y Quality improvement is a consistent approach and methodologies to equip and enable us all to ‘work together in partnership to make the sustainable changes that will lead to excellence for our patients, people, places, performance and pounds
y Quality control is about setting and meeting standards, benefits realisation, operational management tools to track and monitor data over time often against agree targets and trajectories
Figure 18: The image below illustrates the three phases of quality planning (red), quality improvement (blue) and quality control (green).
i. Development of Stop, Start, Continue media (Alex Health Transformation)
ii. Leading the transformation associated with the go-live of Alex Health (change, communications and training) as well ongoing adoption and achievement of benefits realisation.
iii. Supporting the implementation of the Alex Health Ambassadors (214 members of staff) and navigators (436 members of staff)
iv. Masterclass – implementation of sessions to increase knowledge and understanding of our clinical and nonclinical teams
v. Development of ENT- SDEC service (Surgery and Critical Care Division supported by Business Change Manager)
vi. Introduction of the Vanguard Theatres (Surgery and Critical Care Division supported by Business Change Manager)
vii. Robotic assisted surgery (Surgery and Critical Care Division supported by Business Change Manager)
viii. Electronic pre-operative assessment (e-POA) - in progress in Surgery and Critical Care Division (supported by Business Change Manager)
ix. General Surgery SDEC - introduction of dedicated surgical navigator for Surgery and Critical Care Division (supported by Business Change Manager)
x. Changes to community contract and triage (MSK Lead Provider)
xi. Integrated MSK pathway developmentshoulder elective (MSK Lead Provider)
xii. MSK APP to support shoulder clinic (MSK Lead Provider)
Supporting adoption of the system and aiding clinical staff to easy use of the system
>95% of all staff trained achieved ahead of go-live.
Reduction in number of systems that clinical staff use to record care for patients
Providing at the elbow support to all staff in the early life implementation of the system to increase quality of data entry
Supporting our teams to correctly utilise the system increasing the quality of the data input and monitoring patient care
Reduction in ED waits for ENT patients, improvement in 4hr breaches for ENT service. Better patient experience
Reduced wait times for cataract surgery, reduction in cataract backlog, improved patient experience on the day of surgery
Improved health inequality as access for Harlow patients. Reduction in length of stay and post op complications.
Should lead to a reduction in on the day cancellation for surgery. Also improved patient experience and optimisation ahead of surgery
Improved flow between ED and SDEC for general surgery patients, reduction in 4-hour breaches. Improved patient experience.
Community onward referral to secondary care reduced. More patients being managed in the community
Appropriate patients being referred for surgery
Focused on discharging patients and placing those appropriate on the patient initiated follow up pathway. Reducing review lists
Table 4: Test(s) for change, intervention(s) or action(s)
xiii. Spinal MDT between community and secondary care clinicians (MSK Lead Provider)
xiv. Advice and Refer implemented in 2 pilot sites (Outpatients Transformation)
Measurable impact on quality and safety
Patients being cared for in the correct setting
Reduction in conversion to appointments, reduction in patient numbers where hospital is asked to see patient through increased advice given to GPs.
xv. Review of clinic templates to optimise with new electronic health record, Alex Health (Outpatients Transformation)
xvi. Implementation and development of monthly Quality Improvement training and support sessions
Increased capacity and smoother patient journey
Clinic rebuild in Alex Health has been completed, enabling us to focus more on aspect of transformation and improvement
From April 2024 until March 2025, Trust trained 109 staff on QI Fundamentals (part 1), 86 staff on QI Fundamentals (part 2) 88 staff on Leading Change.
A number of these staff have gone on to delivery QI projects and use QI and change methodology in their effort to improve quality and safety.
QI clinics are up and running in CHAWs supporting staff with their QI projects
xvii. Urgent care improvement programme PAHT achieved the best performance in our four-hour standard since 2021. Furthermore, we have seen a sustained improvement in our ambulance handover performance.
xviii. Multi-agency discharge event (MADE) Frailty MADE (17 – 21 March resulted in the following areas of sustained improvement:
• PAHT extended the assessments completed in older persons assessment unit (OPAL) and same dame emergency care units to 08:00 – 20:00 7 days per week
• Interface with geriatrician service is now consistently available 10:00 –18:00 (Monday – Friday)
• Direct Ambulance Offload into OPAL Chair 7
xix. Care Closer to Home (focus on Frailty)
Two workshops held (17 March and 22 April) with partners to agree how we can achieve the Care Closer to Home model of care into practice with an integrated care pathway for Frailty
The PMO is an independent, Trusted advisor and support service that enables the Trust to do the right thing, at the right time, using the best practice project management tools and techniques that support the delivery of organisational goals.
The PMO operates flexibly across all of our clinical areas, whilst maintaining an ‘engine room’ on main site to drive the PQP (Patients, Quality and Productivity) programme delivery. The PMO has expanded both its remit and responsibilities since its inception to support and respond to the Trust’s ambitions and strategic priorities.
Essentially the PMO, as part of the wider Quality Improvement team, enables the Trust to become Modern, Integrated and Outstanding.
The PMO provides assurance, oversight and governance to the Trust Board, Executive team and wider stakeholders of the key projects and programmes undertaken at the Trust.
The PMO ensures there is an effective framework and appropriate governance in place for the management of projects and programme deliverables.
The PMO ensures sustainable change is implemented and embedded and that the identified benefits are monitored, managed and ultimately realised in a timely manner. The PMO has focused on driving, embedding and sustaining quality improvement through an evidence-based approach, holding leads to account and working with a wide range of stakeholders across the Trust’s and wider system to enable and drive the successful delivery of key projects and programmes.
The PMO employs an appreciative enquiry and engagement approach which is supportive, collaborative and empowering. The PMO have embedded a standardised and best practice approach to project and programme management across the Trust. As part of this, the PMO have established clear and robust governance processes in relation to delivery, responsibility and accountability, underpinned and utilising the Trust’s Accountability Framework. The PMO works with stakeholders to codesign and co-produce programmes of work, ensuring a balance of top down and bottom-up approaches. The PMO provide and analyse benchmarking data from a variety of tools and sources including Model Health and Getting It Right First Time (GIRFT) to identify opportunities and inform the Trust’s and Divisional delivery and improvement plans. The PMO works with the Trust’s information team to track the delivery of key metrics and enable informed and evidence-based decision making. The Divisions utilise the outputs from the PMO to inform their PQP, QI and wider programmes of work.
The PMO continued to utilise a project management system called PM3 to track the delivery of projects and programmes of work. The PM3 system is fully managed by the PMO enabling project leads, project managers and project teams to effectively manage, document, report and deliver projects and programmes of work. In turn, the PM3 system enabled the PMO to track and report delivery, monitor progress, issues and risks effectively. The PM3 system enables the four members of the PMO to oversee hundreds of projects and programmes using the systems reporting functionality.
As of January 2025, there were 350 trained PM3 users, and a total of 1063 projects been captured on the system. Since we commenced use of this system 294 projects are currently active and 550 have been delivered and closed with measurable benefits delivered, with the remainder in pipeline for future delivery. The PMO also delivered a masterclass training session for projects, where to date 296 staff have successfully completed the training.
The PMO has supported and driven the delivery of the key major projects and programmes over the past two years. This included driving the delivery of the five strategic priorities of PAHT2030 (Transforming Our Care, Our Culture, Digital Health, New Hospital, Corporate Transformation) and the various projects and programme there within.
The production of the Trust’s 28 Clinical Strategies, overseeing the planning of the New Hospital, overseeing the implementation of the Trust’s new EHR (Electronic Health Record), monitoring the development of ‘Our Culture’ programme and strategy and overseeing the delivery of the Corporate Transformation programme. This complex programme involves multiple stakeholders from across the wider system and is responsible for driving transformational change at PAHT.
The delivery of PAHT2030 strategy will continue to be embedded during 2025/6.
The PMO work with the wider QI team to enable and report on the delivery of Quality improvement initiatives undertaken across the Trust, including those quality improvements led, supported and facilitated by the Quality improvement team. The PMO provide oversight, governance and support with data, including dashboards, metrics and benchmarking as well as expertise in effective programme and project management. Work is also continuing in partnership with the wider QI team, the strategy team and the business intelligence team to produce the Trust’s Outcomes Framework.
The PMO works closely with the patient safety and quality teams as part of the Quality PMO, jointly overseeing the Quality Compliance Improvement Group (QCIG), which drives the delivery of regulator improvement actions. Working collaboratively with the patient safety and quality teams and each divisional team, the PMO, through the working at QCIG, is moving from a reactive model to a proactive model whereby patient safety and quality opportunities are identified and addressed before becoming an issue. This is being made possible through the use of audit, internal and peer review inspections, data mining and national trend data reviews. Ultimately the PMO is providing the foundations for our patient safety and quality teams to deliver real improvement for patients.
The Quality PMO team have worked collaboratively with the Patient Safety and Quality teams through the Quality Compliance Improvement Group which has overseen and driven the successful adoption of the Care Quality Commission (CQC) “must and should” actions. These actions, required by the regulator, addressed identified gaps in the provision of high-quality patient care across a number of our clinical areas. One such
example is the successful adoption of the streaming programme, which is effectively streaming patients away from the Emergency Department to the most suitable and clinically appropriate service. This programme is helping to reduce the demand on the urgent and emergency care department, leading to improvements in the timeliness of care for patients thus improving quality of care.
Patients, Quality and Productivity (PQP) programme
The PMO lead, oversees and drives the delivery of the PQP programme, holding divisions to account whilst providing help and support and insight into potential opportunities. The PMO has enabled the
Listening, learning and leading
successful delivery of the Patient, Quality and Productivity (PQP) programme (formally called the cost improvement programme) for the past two years. The PQP programme has delivered significant and measurable patient safety and quality improvements across all divisions, significant and measurable improvements in operational performance against key metrics and delivered substantial financial and productivity improvements totalling £16.5m in 2023/24 (4.5% of turnover) and £18.5m in 2024/25 (5% of turnover).
The PMO have overseeing the production of the Trust 2025/26 Patients, Quality and Productivity programme which launched in April 2025.
Patient experience based on activity in 2024-25 at The Princess Alexandra Hospital NHS Trust is founded on a three-part strategy of:
a) Improving communication in all its forms to support the individualisation of care
b) The effective use of technology while also robustly tackling digital inclusion
c) Enabling kindness and cultivating compassion across all of our services
Within that work is our voluntary services and patient engagement strategy, whilst these are currently in the process of being reviewed but are founded upon:
1. Patient leadership
2. Coproduction
3. Supporting the delivery of care by listening and then
4. Individualising care processes and pathways.
Figure 19: Summary diagram showing taken from Patient engagement strategy

Listening functions enable our population to feed back
These two citizen-facing services are the listening and learning functions of the Trust, they bridge communication gaps between our population and our services and enable an intelligence led response. The patient advice and liaison service (PALS) and the complaints system are both starting points in that learning cycle.
The patient advice and liaison service are first responders when patients, families and carers are noticing that services are not operating in line with their expectations. Last year, the Trust responded to 4729 concerns in year, this has increased by 7.2%, from 4410 in 2023-24 and since 2020-21 increased by 51%.
We know we need to be more effective and so the service has been proactively working with operational and clinical teams to resolve concerns. The continuing increase in public enquiries has placed extraordinary pressure on all staff and so we have maintained a focus on receiving concerns and sharing them in a timely way with delays in care, communication and appointments being the top three issues raised for our services.
A process mapping workshop took place in March 2025 and demonstrated significant variation in processes completed between the different Trust divisions. Our next steps are to offer bespoke support for case management and to eliminate waste through the standardisation of best practices across all five divisions. We then intend to review progress of this work in September 2025.
Every year, the Trust must make a statement under section 18 of the NHS Health and Social Care Act 2009, about how many complaints were received, whether or not they were well founded, their subject, the issues they raise, and any actions taken. This report is intended to satisfy that requirement.
How many complaints were received?
The Trust received 318 complaints in 2024-25 an increase of 172 (85%) complaints when compared to those submitted in 2023-24.
While there has been a significant increase in the number of complaints, much of this has come from our escalations of patient advice and liaison service (PALS) enquiries which had not been resolved or where we had recognised pressures within a clinical specialty, resulting from the volume of work having increased in year. This was particularly evident in our surgery specialties such as trauma and orthopaedics, urology, care of the elderly for Medicine division and gynaecology care in women’s services.
Many of these concerns were associated with appointment delays and these were also associated with the introduction of Alex Health, the new electronic health records system.
How many were well founded (‘upheld’)?
Of the 226 complaints closed in this year (the point at which we determine if the complaint can be upheld) we found that:
y 11 fully upheld.
y 149 partially upheld
y 66 complaints were not upheld (including those who failed to return consent or ended contact)
By identifying a case as upheld, we mean that at least one of the concerns raised meant action was required by the Trust to address the issue.
Of 318 cases, 919 categorisations were made (each case has several categorises) cases, the most frequently occurring themes related to:
a. Medical and nursing care: 28% (n=2640)
b. Communication: 17% (n=157)
c. Waiting times: 13% (n=125)
What issues do those cases raise and what actions were taken?
The patient experience strategy relates to three core themes of improving our
y Communication
y The effective use of technology
y Centred on kindness and compassion in the services we provide Our actions in response to those themes in year were:

y 1076 nursing midwifery and Allied Healthcare Professional (AHPs) completed the three-hour SAGE and THYME Foundation Level communication skills model training, developed by University Hospitals South Manchester
y The first doctors attended the training on 9 April 2025 in agreement with the medical director
Feedback received following a recent Sage and Thyme training
y Work with the Deaf Community to improve cancer information in partnership with Cambridge based Anglia Ruskin University Masters students
y An event for people with learning disabilities working with 11 community Learning disabilities and autism services in conjunction with cancer teams across West Essex
y Outreach events in Harlow, Epping and Stortford to support access to the resolution of PALS concerns and involvement in the patient panel
y A 10-week British Sign Language (BSL) training course launched and fully subscribed with 30 trainees
y A sensory training pilot using clinical simulations to improve communication completed with Royal National Institute for the deaf (RNID) and HealthWatch Essex Disability Ambassadors
y An outreach event in children’s centres and the African community working cancer services



y The implementation of our electronic healthcare patient record (Alex Health) is linked to the My Alex Health, a patient portal for the system. This went live in March 2025, with 875 patients registered in the first month in Dermatology. Of 300 patients invited to register on the portal in the first week, 99% registered on first invitation
y There is a planned phased roll out to be completed specialty by specialty, to support staff and public confidence in the roll out to be completed by end of the summer 2025
y Digital inclusion. A project in partnership with West Essex Community Action Network (WECAN) to combat digital exclusion has enabled us to give away 160 devices, securely wiped and prepared for use by patients who do not currently have a device. WECAN helps us achieve this as they are an alliance of local voluntary organisations set up to build stronger links between the voluntary sector and statutory partners for the benefit of the community in Harlow and Epping Forest
y Friends and Family Test (FFT) data is more robust and all users who have requested access have been given it, with protections in place where issues arise which may need a follow up
y New technology driven noise at night project launches on 11 October 2025
y Development of the project plan to procure new wheelchairs for bariatric patients was agreed at Capital working group with funding of £75k
Enabling kindness and compassion
y Development of projects focussing on enabling personalised care have included:
• food and drink
• discharge support
• end of life care through the butterfly end of life volunteer’s hub
• bringing greater visibility to the challenges of marginalised groups through board stories included the topics of maternal mortality, deaf-blindness and outreach to the community
y Voluntary services development of sensory and therapeutic gardens on site
y Joint working with the Herts and West Essex Surgical Centre to support the development of adjustments for patient travelling to St Alban’s for surgery who are usually treated at The Princess Alexandra Hospital NHS Trust Case studies
These are case studies presented at the Patient Experience Group which takes place bi-monthly. At each meeting one of our divisions provides a detailed update on its current learning from complaints and its process that has taken place as a direct result of our patient’s feedback to us. The following four case studies were presented during 2024/25.
Surgery and critical care division and the challenges of clinical engagement
y A cancer patient whose family wanted to understand key elements of the care provided and wanted to understand if there had been a delay in diagnosis
y The concern included being unhappy with the experience when an inpatient, the patient had felt she was discharged without a clear clinical plan, communication was lacking and that the attitude of the consultant was dismissive when they were asked questions
y What made this worse was that when the family then raised a concern, clinical engagement remained poor and so despite offering meetings, the meetings were ineffective
Learning and actions taken
y A face-to-face meeting was set up and involved an independent consultant who had not been involved in the patient’s care but spent time reviewing all healthcare records, scans and MDT outcomes and completed a full timeline which was discussed at a second meeting
y What became clear was that the care provided had been effective but the explanation of the process and communication had been poor
y The result was an excellent conversation, with one person leading the meeting which was planned. The family were aware there was a lengthy process in diagnosing cancer. The Consultant explained that there were lots of discussions taking place with members of the multi-disciplinary team and scans needed clarification. All of this resulted from the cancer being difficult to diagnose
y Learning and reflection discussions took place within the surgical audit meetings, these were led by the consultant who attended the family meeting to explain that timely clinical engagement when given can reduce the distress experienced by families
Women’s services and a lack of empathy during a molar pregnancy
Patient had care in the Emergency Department (ED) and Early Pregnancy Unit (EPU). Sadly, after numerous reviews, attendances and following investigations, the woman was diagnosed with a molar pregnancy (gestational trophoblastic disease).
y The complaint was surrounding a lack of empathy after discovering there was not a viable pregnancy and the care pathway for molar pregnancies requiring multiple scan and blood reviews
y The patient went to theatre to remove the molar pregnancy and subsequently had to go back to theatre for a repeat procedure
Explainer: What is a molar pregnancy?
In the UK, about 1 in 590 pregnancies is a molar pregnancy. A molar pregnancy, also known as GTD or gestational trophoblastic disease, happens when the fertilisation of the egg by the sperm goes wrong. This leads to the growth of abnormal cells or clusters of water filled sacs inside the womb. Unfortunately, a molar pregnancy cannot develop into a healthy baby.
Source: Cancer Research UK Website [Accessed: 25.04.2025]
y A referral to the bereavement midwife and counselling service could have been made earlier and so will become routine in cases like this
y The speciality Matron and lead emergency consultant will be working together on how to improve the communication between the two services. This will ensure all women who are high risk can contact a specialist nurse or Matron during core business hours of Monday to Friday 9am to 5pm
y A clear plan is being developed for how to improve communication with highrisk patients attending EPU for cases like this
y Professional development time with EPU to familiarise the team with appropriate referrals and relevant information to be read by patients following USS findings of suspected or confirmed GTD or similar situations
Medicine division and finding new ways to enable the personalisation of care
y Patient’s personal care was incomplete for long periods, including oral hygiene not completed or support for patient to use their glasses and hearing aids
y Delays in being given medication causing upset and distress to the patient
y Subsequently the patient began to refuse to eat and drink
y Delays in recognising patient needed palliative care and therefore in being fast tracked
and actions taken
y A face-to-face meeting with the family took place
y The service apologised for the service failings, including in providing timely pain relief, in the breakdown in communication which meant noone was explaining the delays were caused by a struggle to get funding for accommodation to support the patient
y The long-term change implemented by the clinical team is focussed on now supports an intensive collaboration with palliative care and discharge teams
y The ward team are now working closely with the discharge team to arrange patient’s preferred place of dying. If no response from the discharge team is received within 48 hours, then the patient’s will be moved into a side room, where possible
y The consultant confirms with their junior doctors that the palliative referral has been fully completed, that the syringe driver (used for delivering medication) is reviewed every 24 hours to ensure that this is effective and medication is changed as required
y A huge number of compliments are received every year by the Trust, here we include a small selection
“I attended Princesses Alexandra Hospital on Saturday 22nd for a CT scan. I must say the young gentleman who did my scan was brilliant. Very kind caring and most helpful. Even pushed my wheelchair back to the reception area when my scan was finished. He was on his own, I wished I had taken his name. Cannot praise him enough. I do hope you find him and pass this message to him.”
“I want to extend my appreciation to all the clinicians that were involved in my care starting with the triage nurse who was very polite and attentive, a young female radiographer who was sensitive and respectful to me when preparing me for the chest X-ray, and finally to the doctor who took the time and trouble to listen to my concerns and to address them in so far as he could despite his busy schedule. Dr X was also very polite and respectful when explaining the limitations of what was available in the A&E setting as opposed to through my GP”.
“I am writing to say thank you to all of the staff working last night in the ED and Further Assessment Unit at PAHT. From the receptionist to the observation nurse, streaming clinician and phlebotomist the journey took 20 minutes. Then a wait at the Further Assessment Unit for the blood results. What a nice touch bringing sandwiches round for those waiting. The staff at the Unit were also amazing and very efficient. Once in I had medication administered and a CT scan arranged within an hour”.
“I am writing to you with nothing but praise for St Margaret’s Hospital. I was referred there from my GP early last year and have been so impressed with the efficiency of the Breast Unit in particular. Everyone including doctors, radiologists, nurses and receptionists has treated me with kindness and care on all my visits and has explained everything to me as and when necessary.
Earlier this month I had to be admitted quickly to Princess Alexandra Hospital and once again I was treated with kindness and reassurance at a rather worrying time. Miss W deserves a special mention as she went above and beyond to get my treatment done as soon as possible”.
“After many years of suffering with back and leg pain that I have not received any treatment for, I voiced my frustration and exasperation at the situation during my appointment, having persevered with me, checked my mobility/strength, identified some habits that may be contributing to my pain, and set up a home exercise programme for me to follow. I want to thank her for being so patient, understanding, and professional. She is a great asset to your hospital”.
Patient’s mother-in-law wanted to say that “I can’t thank the staff enough for the care and support they gave to my daughter in law, husband and children too. I hope you will pass this email to X and their team, to say how much everything they did meant to us all as a family. Words will never be enough to thank them all. I just want them to know we are so grateful for all they did to make sure she got back home. We, as a family, are so grateful for the care and support X and her team showed us all. We will never forget what they did, especially X. They made her final wishes possible and for that we thank them from the bottom of our hearts.
“I was very nervous and X really helped put me at ease. When I am nervous, I talk a lot and X was more than happy to listen and respond to me going off on a trail. Although I was the last of the day, he didn’t rush me or show he was eager to go home as I’m sure he was! He was very quick and didn’t hurt me when putting the cannula in which is a problem I often face and end up with so much bruising! His funny jokes and helpfulness answering my questions made today a much better experience than I was expecting. X truly is an asset to the team and I am very glad I got to meet him”.
Our service users receive a link via a text message within 24 hours of being discharged or attending the hospital for their appointment to allow the Trust to receive feedback on the Friend and Family Test.
The Trust has seen an increase in responses received due to this new way of collecting data.
y Total annual Friend and Family Test (FFT) score for 2024/25 showed that 79% of patients rated our services as good or very good
y This is compared to 76% (12,272) who gave the same rating in 2023/4)
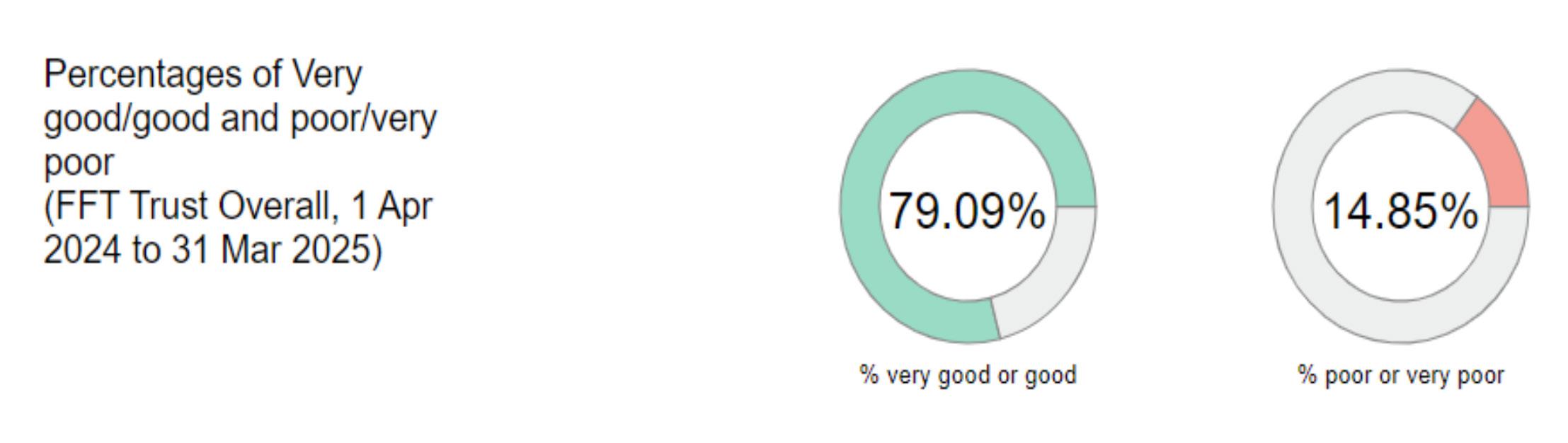

The past year has been busy and productive for the Patient Panel. As representatives of our patients, their main goal is to ensure the best possible care and experience for those using our hospital.
To connect with the wider community, our panel have visited local shopping centres to gather public feedback, which is shared with hospital management team. The panel produce an annual report to keep the community informed about the work completed in year.
Our Patient Panel Chair remains actively involved in governance, attending public board meetings and regularly meeting with the Chief Nurse and CEO. The panel also takes part in key stakeholder meetings, contributing to important decisions.
The panel members worked with our people team to provide interview skills training, allowing more panel members to join the recruitment process. Additionally, the panel have engaged with the Freedom to Speak Up Guardian lead, enabling members to train in this vital area.
A major achievement this year has been expanding the membership, working to make the Patient Panel more diverse and inclusive.
The Complaints Reference Group meets regularly where the panel review complaint themes and Trust actions to address these and in year the group has been active, recently updating its terms of reference and committing to reviewing the hospital’s complaints policy.
Patient Panel members have also attended national Health Education Through Technology (HETT) conferences, with the Vice-Chair presenting at the last two events.
Working with the Medical Advisory Committee (MAC), the patient panel have helped develop the Consultant Awards, which were well received at the MAC’s annual dinner, recognising outstanding medical contributions.
The Patient Panel hosted a half-day forum on Patient Safety Partnership and recruitment, promoting best practices and continuous improvement.
The Patient Panel proudly supported the British Legion Poppy Appeal, collaborating with the 1st Great Parndon Scout Group to create a special display featuring young people’s reflections on Remembrance Day. Over five days, hospital staff, senior managers, and panel members engaged with patients and visitors, raising £2006, a 30% increase from 2023. The event concluded with a Remembrance Service, organised by the Chaplaincy Team. Wreaths were laid on behalf of the NHS, Veterans, and the Community, with a member of the public playing the Last Post. Attendance at the service continues to grow each year. Costa Coffee, Marks and Spencer, and Harlow Hospital Radio generously supported the event.
A major highlight this year was celebrating our Patient Panel Chair’s achievement in received a British Empire Medal in the King’s Birthday Honours for services to the NHS, in addition to receiving the NHS Unsung Heroes – Volunteer of the Year Award.

Engaging with young people was also a priority. The panel welcomed a group of eightyear-olds for a hospital tour, where they visited Radiology, Paediatric AandE, the radio studio, the sensory room, and met therapy dogs. Their visit ended with treats in the restaurant and a goody bag from the Patient Panel, presented by the Chief Nurse.
Looking ahead, our panel remain committed to patient advocacy and improving hospital services. To achieve this, they held a public meeting in April 2025 to engage with the community and gather valuable insights.

Improving care for patients with delirium and dementia
PAHT has made good progress on our goal to deliver the very best possible care for our patients with dementia, in line with national policy. We have an integrated dementia strategy and delirium strategy, which has key performance indicators in the following areas and is monitored through our dementia and delirium steering group.
y Find, assess and refer pathway
y Person-centred care (recording of ‘This is Me’)
y Comparison of harm related incidents for patients with dementia (development of a dashboard)
y Training
We have recently participated in round six of the national audit of dementia care in general hospitals, The Royal College of Psychiatrists (2019), the recommendations will inform part of our strategy document.
The Trust has one Admiral nurse and their role is supported with monthly clinical supervision through Dementia UK and access to other training and learning opportunities whilst still supporting the strategic development of Dementia care at the hospital. The Admiral nurse’s role still provides that of a Clinical Nurse Specialist support.
The number of referrals received is around 45-52 per month, which are raised both internally through our staff and also from the community received from family, carers and professionals.
In response to acknowledging lack of service provision locally, Admiral Nurse Clinics have been set up on the Harlow site for staff and visitors accessing the organisation and anyone who is supporting someone living with dementia.
In 2019 we undertook a project to introduce singing for the brain into the hospital setting. The aims were to reduce the social isolation that patients often experience during a stay in hospital, to improve wellbeing and mobility. Music therapy is known to play a crucial role in the care of many people with or without dementia, helping to minimise apathy, anxiety, restlessness and depression.
Following the successful pilot, PAHT now provides a weekly music therapy session, which is facilitated by the clinical nurse specialist for Dementia and volunteers. The sessions are delivered at the bedside (if required) on a 1-1 basis or in small groups. The plan for the early part of 2025-6 is to look at expanding the variety of these sessions.
Feedback from family members and carers has been very positive; there has been a notable change in interaction, improved appetite and reduction in delirium related anxiety.
Delirium (sometimes called ‘acute confusional state’) is a common clinical syndrome characterised by disturbed consciousness, cognitive function or perception, which has an acute onset and fluctuating course (NICE 2010). The risk of mortality following a delirium episode in a person with dementia is more than 40%. To support our staff in the care of patients presenting or developing delirium in hospital, we now have established new pathways and guidelines. We also have a leaflet designed to be given to patients and their families or carers.
Dementia training is given in a face-toface session for all new colleagues as part of induction to the Trust. To support our patients, we have introduced mandatory training on delirium as well as creating dementia and delirium simulation training. This has received excellent evaluation and we have been instrumental in helping a local Trust set this up. Additional and more detailed Dementia training (a national recommendation), is available for all staff who have regular contact with people living with dementia.
We are proud of our virtual dementia tour, which enables staff to experience what it may be like to have dementia, and learn how to work with people living with dementia and is included within our dementia training programme. Additional dementia training was introduced into our Preceptorship Programme and Health Care Support worker programme, and is available for our volunteers and to all staff who have regular contact with people who have dementia.
Namaste care. “To honour the spirit within “offers a respectful and supportive approach to care for those living with advanced dementia, integrating compassionate nursing and therapeutic activities. Working closely with St Clare’s Hospice, we have introduced Namaste care in PAHT with the support of the dementia clinical nurse specialist (Namaste champion), who will develop the role of Namaste volunteers in partnership with PAHT volunteers.
Currently Namaste care sessions are delivered twice weekly and embedding a Namaste approach to delivering compassionate care in every day nursing care. The Dementia CNS works closely with St Clare Hospice and supports the Namaste Training.
The Trust has a Memorandum of Agreement in place with Action for Family Carers (AFFC) who provide support for patients living in West Essex. A member of the AFFC team host a drop in every Thursday in the hospital atrium where they aim to identify carers and support them with assessments and hospital based reasonable adjustments.
In addition to this, following the success and outcomes of a fixed term contract for a carers lead funded through National Health Service Charities Together (NHSCT) we plan to write a business case to recruit a carer’s lead in a substantive role. The Admiral Nurse Supports family carers as part of her role and may often support families who are not affected be dementia.
This project continues to provide such wonderful moments for our patients and staff. The project was developed during 2021/22 and started on 6 April 2022, supported by our voluntary services. Ward visits with therapy dogs, providing reminiscence, conversation, loving touch and comfort.

Trust has a robust focus and governance process in place to monitor safeguarding concerns. The Trust has a team that oversee provision of advice, guidance and training to staff to ensure we provide care that maintains patient’s safety. Our specialist safeguarding team work collaboratively with our community partners to ensure this important aspect of patient care is delivered to a high standard.
The Trust is in the process of the development of three therapeutic garden spaces.
1. Sensory Garden
2. Staff garden
3. Garden of reflection
This project was made possible through funding from NHS Charities Together (NHSCT) and match funding from our hospital charity. Due to relocation of the sensory garden the project has incurred additional costs and we are actively seeking additional funding of 32k. The sensory garden will be ready shortly and a grand opening is planned for 5 July 2025. The sensory garden will support our patients with Dementia, Autism, Delirium those who have a prolonged length of stay and for those who find the hospital environment overwhelming. The project will be supported by volunteers. Due to a successful application to NHS Forests, the Trust has been given a large number of free trees and hedges to improver outside spaces

We recognise the environment in hospital can be unsettling for our patients with dementia and delirium. We are working closely with our Patient Panel, our Trust Board and external companies to enhance our environment. Additional funding has been made available through the Capital Woking Group to upgrade the ward environments but there is more work to be done.
We have developed a family carers’ passport and to ensure that family carers are recognised for the contribution they can make to help support patients whilst staying in hospital.
We recognise that when a friend or loved one, who is dependent on the care provided to them at home, is admitted to hospital, that carers may have concerns so we offer a carer passport and lanyard. This aims to achieve the following:
y To enable staff to share details of care plans
y To give access to concessions such as discounted parking and refreshments in the Alexandra Restaurant
y To enable unrestricted visiting times (when appropriate)
y To provide blankets and pillows to carer needing to stay overnight unexpectedly
We recognise and encourage carers to support their friend/family member during their stay in hospital, it is important to remember that occasionally our ward staff may ask you to leave the bay/ward to maintain the privacy and dignity of other patients.
To apply for a family carers’ passport, carers can speak to the ward/department manager.
Looking to the future and the shift from analogue to digital support, the Trust Electronic Patient Records system (which we called Alex Health) was launched on 1 November 2024. The most useful impact from this system is for carers which allows us to now record carer status and report against it from these records.
This will enable us to proactively provide reasonable adjustments to carers and make sure we are able to evidence this. We expect reporting against this element to become more visible from the Summer of 2025.
A further benefit of the Alex Health system will be the implementation of My Alex Health, a patient portal available through the patient experience team. This will enable carers to use the patient portal to manage their loved one’s healthcare as a formally recorded proxy.
The functions which will be available will include the ability to:
y Confirm attendance to appointments
y View all hospital letters digitally
y Receive appointment reminders on their phone
y Request changes to appointments
y Complete assessments and questionnaires from home
y View results, reports and personal information
y Receive messages from consultants
Improving care for patients through use of the Mental Capacity Act
The Mental Capacity Act (MCA) was passed in 2005 to protect and empower people who may lack mental capacity to make their own decisions about their care and treatment. It applies to individuals aged 16 and over and emphases respecting the rights of individuals to make their own choices as much as possible.
The Trust has a policy that was developed with multiple local agencies and it has been adopted across Essex. Part of the policy MCA forms are used to provide evidence and assurance regarding the implementation of the Mental Capacity Act. MCA forms are used by the Trust when health decisions need to be made regarding an individual’s care.
There has been an increase in the use of MCAs of 52% over the last year which are all submitted to the Trust safeguarding team. Our safeguarding team are the Trust experts on the care, support and use of this act for patients being cared for within the hospital. This is highlighted through our training programme for staff and all MCA forms should be sent for an audit to the safeguarding team.
This increase in use of MCA demonstrates that more assessments are being completed and is believed to be as a result of increased awareness of using the mental capacity whilst treating patients is now integrated into our clinical staff training for allied health professionals, doctors and nurses.
The safeguarding team review each assessment and follow up the patient’s with ward teams to ascertain if a Deprivation of Liberty application is required or to assist with other support for the patient’s care.
MCA forms received by the safeguarding team will be reviewed for their overall quality and in year the team have found that this has continued improve, however the themes on the completion of the form are stated as
y evidence of documentation of the best interest decision
y details of family /friends, time /date of assessments
Training is available for staff on mental capacity, which is offered both on-line and in face to face sessions. Over the last year within our Safeguarding training programme specific training has been provided on MCA as a stand-alone training module. This is included within our Trust Level 3 training programme.
In recognition that not all planned outpatient appointments are undertaken face to face the Trust needed to look at how we complete our consent process to cover all appointment types.
The Trust launched electronic consent (e-consent) during 2022 and in year we have seen an increase in receipt of completed MCA assessments as part of e-consent.
The Trust has a specific consent process that is undertaken for patients who are being cared for under the MCA.
To support patients with a learning disability the Trust uses Hospital Passports and the Purple Folder (which contain valuable information about each patient) that will provide additional information to our staff to provide personalised care to those who have a learning disability or are autistic.
Wherever possible the Trust will support adjustments such as giving a double timeslot for an outpatient appointment to allow for a meaningful discussion, or allocating a quiet area for a patient to wait whilst in the outpatient department. Support is given to patients on our wards by allowing input from their family and carers to assist our patients to feel more comfortable when being cared for in an unfamiliar environment. This will enable patients with learning disability or autistic to access and use our hospital services.
The Trust has a learning disability team and their role is to specifically support our patients with a learning disability or autistic to ensure that we fully utilise the valuable information stored within the documents our patients bring into hospital with them, such as the passport and this will support our outpatient and ward staff to make appropriate adjustment to how they deliver care wherever they are needed.
Oliver McGowan training is a standardised training package, developed to ensure that health service staff receive learning disability and autism training appropriate to their roles. Currently, it is the preferred and recommended training for health and social care staff.
The training consists of two different levels y Tier 1: comprises an e-learning programme and is delivered online as an interactive session for all staff who require general awareness training
o The Trust has a total of 4,268 staff identified as being eligible for completion of this training level
o The tier 1 e-learning training programme was introduced at the end of June 2024 and up to 31 March 2025, a total of 1,390 staff have completed it, this is 32.5% of eligible staff
o Our Integrated Care Board (ICB) set the Trust a target trajectory to achieve by 31 March 2025 of 20% of eligible staff
o In addition, there is an on-line interactive webinar session as part of Tier 1 training. This was provided by an external agency with Trust staff required to book themselves onto the available slots. By end of March 2025, 300 staff had completed this session
o The Trust trained 20.5% of identified staff in Tier 1 during 2024/5 and achieved the compliance target set by our ICB, see table 5 below
y Tier 2 training comprises a one-day face to face (in the classroom) training day for relevant staff. Experts with lived experiences contributes to the content and running of the day. All staff with a patient facing role are required to undertake Tier 2 training
o Tier 2 training was provided by an external agency through funding received from our ICB
o The training commenced in January 2025 and up to 31 March 2025, 194 staff attended, comprising 7% of our identified staff
y The Trust learning disabilities steering group will work with each division to agree the 2025/6 trajectory to be achieved, for both tier one and tier two training compliance
o The ICB training contract was recently awarded to a new provider so the training dates from April 2025 onwards have been placed on hold pending the new provider making arrangements to cover the future sessions
o The Trust awaits receipt of the 2025/6 training dates from the ICB and once received our organisational development and training team will oversee the sharing of these dates with divisions and staff to ensure we fully utilise our booking places and training staff in this programme
o Table 5 below details our Trust progress against this training
Patient safety is a Trust priority and we continuously work to ensure that incidents are managed effectively, promptly and most importantly, that we learn from them and share the improvements arising with relevant staff members.
A patient safety incident refers to any unintended or unexpected event that could have, or did, lead to harm for one or more patients receiving NHS funded care. This includes all terms such as adverse incidents, adverse events and near misses, where an incident was recognised and averted.
For the year 1 April 2024 to 31 March 2025, 13,815 incidents were reported on the Trust’s Datix incident management system; this is comparative to the previous year’s reporting. The spread of incidents across our divisions is reflected below.
Figure 17: Incident reporting data for period 1 April 2024 – 31 March
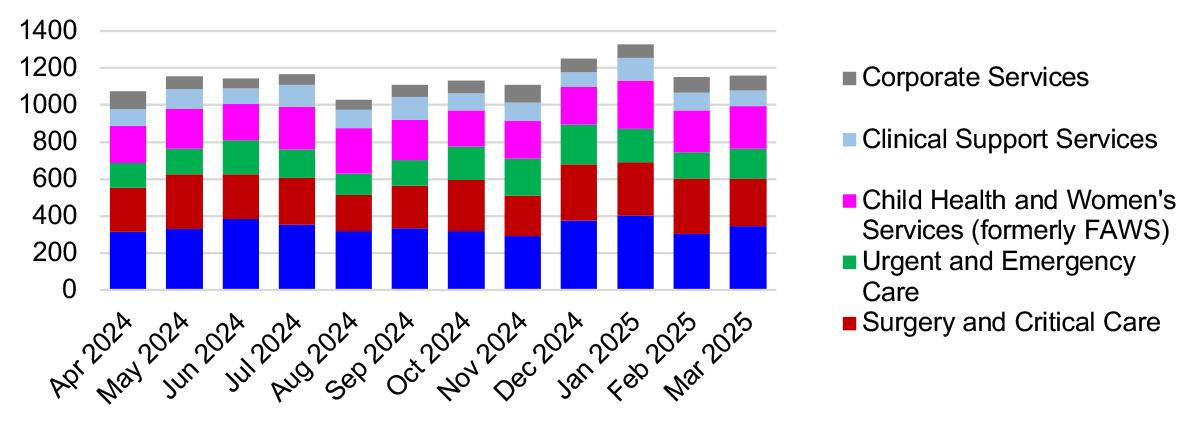
The categories of patient safety incidents reported during 1 April 2024 to 31 March 2025 are summarised in figures 17-19 along with themes of care incidents. These are reported to the National Reporting and Learning System (NRLS) to enable learning and comparison with similar sized organisations across the country to occur.
Figure 18: Top 10 categories of patient safety incidents for 1 April – 31 March 2024
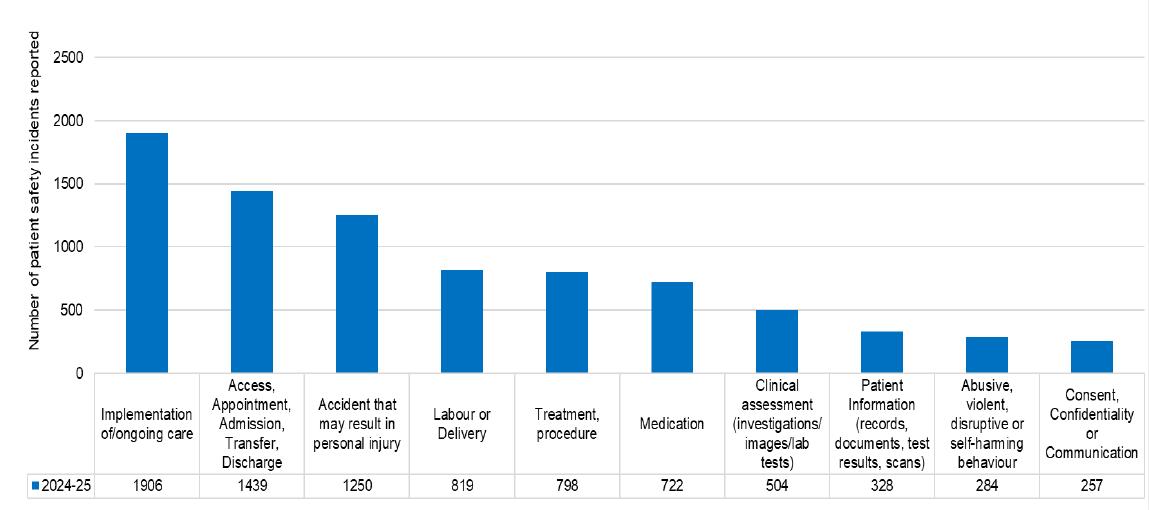
Figure 19: Top 10 themes of patient care incidents for 1 April 2024 – 31 March 2025

The Patient Safety Incident Response Framework (PSIRF) is the national system that supports organisations in identifying incidents that require investigation, focusing on learning to enhance patient safety.
This system replaced the Serious Incident (SI) process and was fully implemented from 1 January 2024 at The Princess Alexandra Hospital NHS Trust.
Incident investigations commissioned under the PSIRF framework are called Patient Safety Incident Investigations (PSII’s).
The Trust raised 13 PSII during the period 1 April 2024 to 31 March 2025, figure 20.
Figure 20: Comparison of Patient Safety Incident Investigations commissioned from 1 April 2023-25
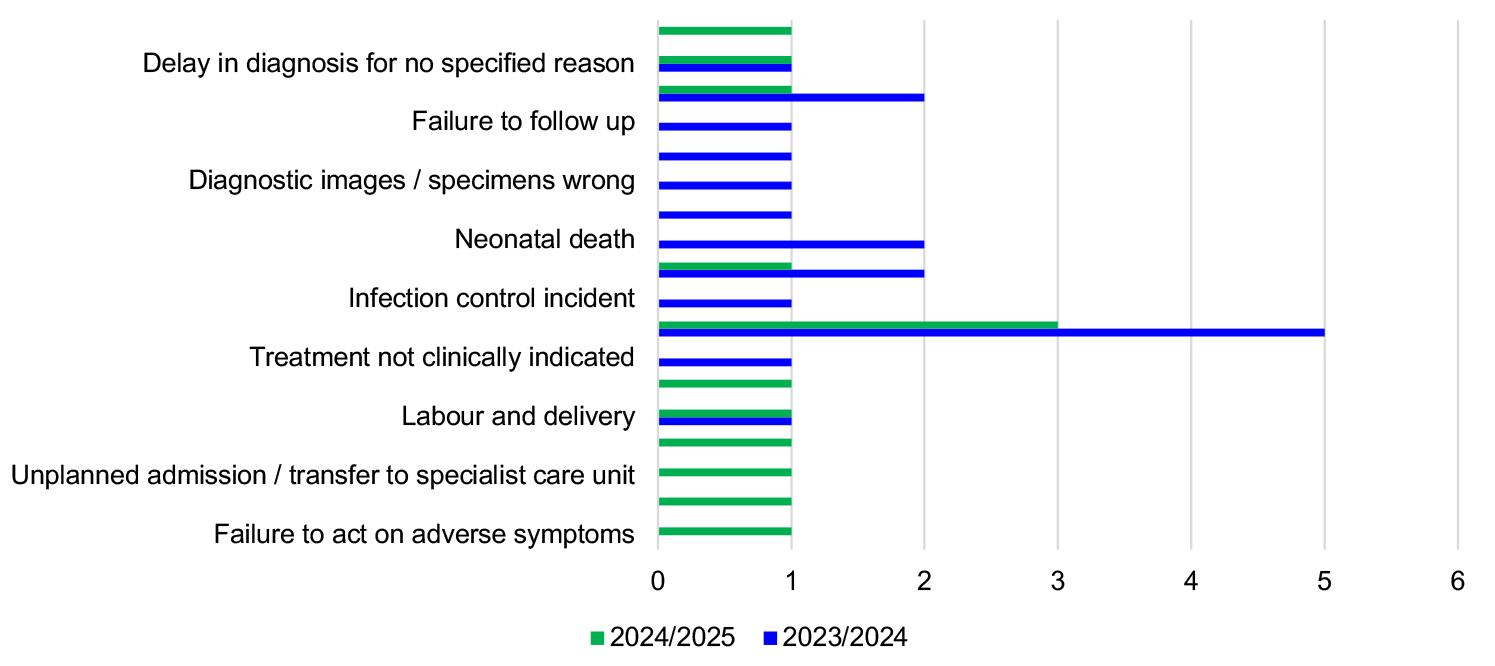
Once a PSII investigation is concluded, an action plan is developed to capture the learning and recommendations from the report for implementation to prevent a reoccurrence.
The Trust uses a sharing the learning report to ensure all relevant staff are
y aware of the key issues that occurred in this incident
y the changes to practice either implemented or being completed
y what the learning from the incident is to prevent reoccurrence
This is presented and shared widely within the local teams where the incident occurred and if relevant to other clinical areas with divisions and across the Trust. This information is reported Trust wide monthly to the Patient Safety Group and quarterly to the Trust sub-committee of Trust board called the Quality and Safety Committee.
Of the 13 PSII’s raised during 2024/5, two were categorised as Never Events.
A never event is a preventable safety incident that should never happen if robust procedures are followed. These events can cause significant harm to patients if they occur. In respect to these investigations
y One was concluded with a robust action plan developed and in place
y The remaining investigation is ongoing however, immediate actions were developed and implemented pending conclusion of the investigation
In summary, five of the 13 PSII incidents have concluded with each having a robust action plan developed and shared.
Examples of changes implemented in 2024/25 following learning from incidents
• Nerve block sites
All members of the anaesthetic team are present prior to the commencement of a surgical site nerve block being commenced. This will provide a double check process for all procedures.
Site markings are made using a single arrow close to the operation site as possible to ensure it is always visible within the operative field following the patient’s skin being cleansed and draped for their surgical procedure.
• In-patient falls
Education and training was implemented to improve compliance with the completion of lying and standing blood pressure assessments.
An additional focus to increase the frequency of documented medication reviews as the impact of medication increasing the risk of a patient falling is recognised. Finally, a pilot study for the completion of vision assessments has commenced. This will support reducing the risk of patients falling and sustaining injury whilst in hospital.
• Blood transfusion
Education about not transfusing blood components based on community blood test results taken prior to patients attending the hospital if they are not showing symptoms has been noted in year and is now included within the mandatory blood transfusion training delivered to our clinical staff. Increased knowledge will improve staff awareness and avoid giving patients unnecessary blood transfusions.
• Ophthalmology
A post-operative cataract community triage and assessment process was established, that comprises of two digital pathways for cataract care (one of the first in the country). This will support the timely treatment and follow up care for patients.
• Consent Process
Consent forms now include the need to discuss and document the potential for an unsuccessful procedure outcome with the patient. This will ensure that patients are aware that a procedure or treatment may not have the desired outcome and what that means for their ongoing care.
• Cardiac care
Development of chest pain pathway that recommends administration of aspirin at triage if a patient’s chest pain has characteristics typically associated with heart related issues such as chest pressure, tightness, squeezing or heaviness in the chest that could be sign of conditions like angina or heart attack. This supports early intervention with the correct medication.
• Sepsis care
Teaching and discussion on identifying sepsis (use of the sepsis six bundle) has been completed. This will remain an ongoing regular training session for the future. Within this training the following is included:
y To act on an increase in temperature
y Collect blood cultures as soon as possible
y Immediate management of sepsis interventions designed to improve outcomes for patients with sepsis
y The Trust Infection Prevention and Control team will deliver additional sessions for new staff as part of Trust induction to discuss invasive devices insertion and ongoing care to reduce risk of sepsis
This training will support staff in providing high standards of sepsis care.
• Safe administration of insulin
Introduced an e-learning package on insulin safety which is available on the Trust’s staff training system (TIMs). The training supports the safe prescribing and administration of insulin avoiding deterioration related to diabetes.
63% of all incidents raised within the Trust are for patient safety
37% of the incidents are not regarding patient safety, the categories for these are detailed below in table 6:
Medicines safety and reducing avoidable harm from medicines is of worldwide significance, with both the launch of the World Health Organisation’s ‘Medication without Harm’ initiative as well as NHS England’s recently launched Medicines Safety improvement programme. Regionally, medicines safety is a core priority as services and pathways begin to become more seamless in the newly formed ICS.
Despite the increased service demands and challenges around staff resource, medicines safety continues to be a clinical and quality priority for the Trust, with improvements seen throughout the organisation. Medicines safety will continue to form a key driver of improvement within pharmacy and the wider organisation, as we strive to ensure our patients receive the most appropriate, most effective, and best value treatments, free from avoidable harm.
Medicines are the most common intervention given to patients in hospitals. Medicines play a crucial role in maintaining health, preventing illness, managing chronic conditions and curing disease. In an era of significant economic, demographic and technological challenge it is crucial that patients get the best quality outcomes from their medications.
Safe medicines management within an organisation is a multi-disciplinary process, and one of our priorities has been to equip all staff with the tools, knowledge and skills they need in the medicines process from prescribing through to storage, supply and administration. By utilising the Trust learning platform, our pharmacy team developed four medicines modules designated as ‘essential learning’ for staff.
These are:
• Insulin safety
Insulin is the most commonly reported medicines related incident which results in patient harm. Nationally, 1 in 5 patients admitted to hospital have a diagnosis of diabetes, and the treatment of patients using insulin has become more varied and complex. This e-learning module, aimed at all nurses, clinicians and pharmacists, explores the pharmacodynamics and pharmacokinetics of different insulins used, helps to understand different regimens, monitoring and delivery methods used, and recognises the risks and safety precautions needed when using insulin.
• Medicines management
The storage, administration and governance surrounding medication management is a key competent of medicines safety at ward level. This e-learning update is tailored to deliver standards for storage of medicines, controlled drug record keeping, as well raising awareness of specific risks within PAHT, and how they can be mitigated in the future.
• Patient group directions
Patient group directions (PGD’s) allow different groups of healthcare professionals to administer or supply medicines to predefined groups of patients without a traditional prescription. Use of patient group directions allow improved medicines uptake without compromising patient safety. In order to use PGD’s, practitioners should demonstrate an understanding of the legal, clinical and practical aspects to a PGD, and this e-learning package allows them to do just that.
• Antimicrobial stewardship
The emergence and spread of drugresistant organisms (pathogens) that have acquired new resistance mechanisms, leading to antimicrobial resistance, continues to threaten our ability to treat common infections. Especially alarming is the rapid global spread of multi- and pan-resistant bacteria (also known as “superbugs”) that cause infections that are not treatable with existing antimicrobial medicines such as antibiotics.
In 2019 World Health Organisation (WHO) identified 32 antibiotics in clinical development that address the WHO list of priority pathogens, of which only six were classified as innovative. Furthermore, a lack of access to quality antimicrobials remains a major issue. Antibiotic shortages are affecting countries of all levels of development and especially in health care systems.
The UK Government has developed a 5-year National Action Plan (NAP), to contain and control these drug-resistant bacteria by 2040. As part of this strategy, the use of antimicrobial drugs is heavily scrutinised.
Antibiotic (antimicrobial) resistance poses a major threat to everyday life and modern-day medicine where lives could be lost as a result of antibiotics not working as they should. All health and care staff, as well as the public, have a very important role in preserving the power of antibiotics and in controlling and preventing the spread of infections. Amongst the approaches to reduce this threat includes adequate infection prevention and control practices, good antimicrobial stewardship and the use of diagnostics.
According to the benchmarking data, our Trust remains a high user of antibiotics, figure 21. However, this data has been challenged, with business informatics team tasked with identifying why around 800-1000 admissions per month are lost to our Trust reporting data

Despite the lack of clarity, our hospital has seen an 8.9% decrease in the defined daily doses (DDD) per 1,000 admissions from December 2022 to December 2024, this is reflective of a variety of interventions we have implemented, such as specialist ward rounds, reducing the course lengths for drugs and minimising dispensing wastage. Going forward, there is a number of targets within the antimicrobial agenda, these include:
Antibiotics are divided into three World Health Organisation (WHO) classifications;
y Access antibiotics (the preferred antibiotics for common infections, with a narrow spectrum of activity and low risk of side effects)
y Watch antibiotics (broader-spectrum antibiotics that are recommended for more severe infections or infections that are more likely to be resistant to Access antibiotics)
y Reserve antibiotics (Last-choice antibiotics used to treat multidrugresistant infections)
Having a high percentage of access antibiotics as first line therapy given to patients when following our clinical guidelines, along with good adherence to these guidelines across the Trust demonstrated by our audit data and reviews, demonstrates we are adhering well to our local guidelines and procedures indicating strong antimicrobial stewardship.
Previous attempts at a performance pack for clinical divisions has been difficult to interpret and escalate where needed. Through the creation of a performance dashboard, including topics such as intravenous (IV) antibiotic use, use of high-risk antibiotics, course length and guideline adherence, the intention is to allow antimicrobial stewardship to be an active topic of discussion at divisional meetings.
Currently participation by clinical leaders at monthly antimicrobial stewardship (AMS) group is low. The AMS group is exploring alternatives ways to address this, such as antimicrobial champions, consulting registrars, and linking meeting times into staff’s job planning.
The benefits of getting patients onto oral antibiotic therapy are widely documented, including earlier discharge home, reduced risk of infection from vascular devices, lower side-effects, costs and carbon footprint.
A target set within our locality of Hertfordshire and West Essex is to reduce the number of patients on IV antibiotics for over 72 hours, who are clinically stable, do not have a temperature (afebrile), are eating and drinking and do not have a deep-seated infection.
There are two metrics that are nationally reported to measure medicines safety and governance, these are
y Medication Incidents Rate per 1,000 bed days
y Percentage Medication Incidents Reported as Causing Harm or Death/All Medication Errors
A Trust that is frequently reporting medication incidents, with a low percentage of these incidents causing harm, is recognised as having a good organisational ethos with regards to patient safety, see figure 22-23. These are also reported as part of hospital pharmacy’s benchmarking process, known as ‘model hospital’.
Figure 22: Number of reported medication incidents/per 1000 bed days

23: % of medication errors that cause harm
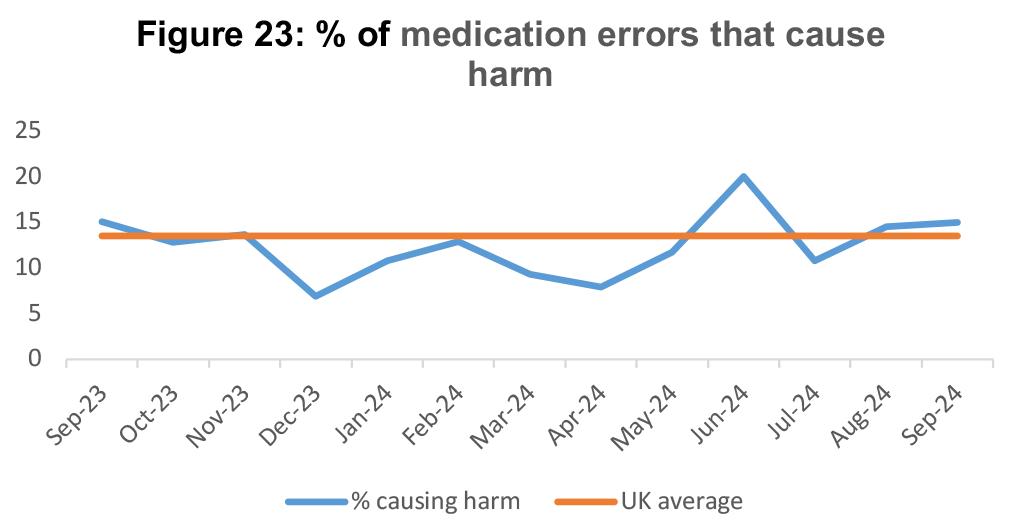
Themes:
• Antibiotics and creatine clearance
A number of incidents reported were due to the wrong dose of antibiotic being given in respect to a patient having reduced renal function. For these patients it is vital to check their blood results for creatinine clearance, particlarly if they require strong antibiotics such as gentamicin, teioplanin and temocillin, as these drugs are cleared from the body through the kidneys.
• Critical medication
Some critical medication being omitted or delayed have resulted in patient harm including the delay of c.difficile treatment as well as medication to treat Parkinson’s symptoms. Staff are reminded of the importance of prompt treatment for these conditions
• Insulin errors
Insulin remains a common theme of errors, including wrong drug administered, failure to prescribe insulin on admission, and use of intraveous insulin infusions. Staff are directed to the essential insulin e-learning on Trust learning platform.
It was recognised that there was a large number of incidents involving medication errors at admission during January. As a
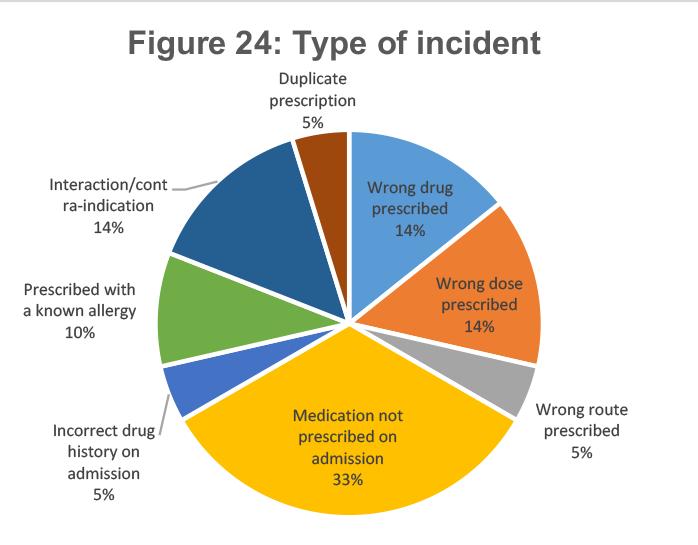
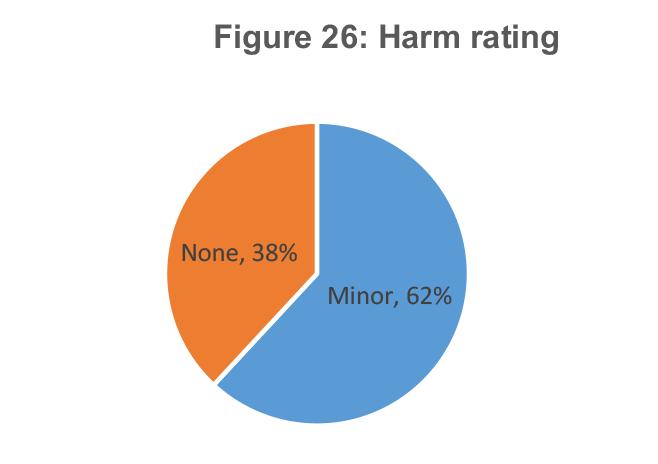
result, a thematic review was performed to evaluate all medicines incidents captured on admission, find trends and common factors, and gather shared learning, with an emphasis on how pharmacy can support incidents going forward.
A total of 21 incidents were identified in a 3-month period, and these were reviewed with key themes and shared learning extracted, see figures 24-27 below
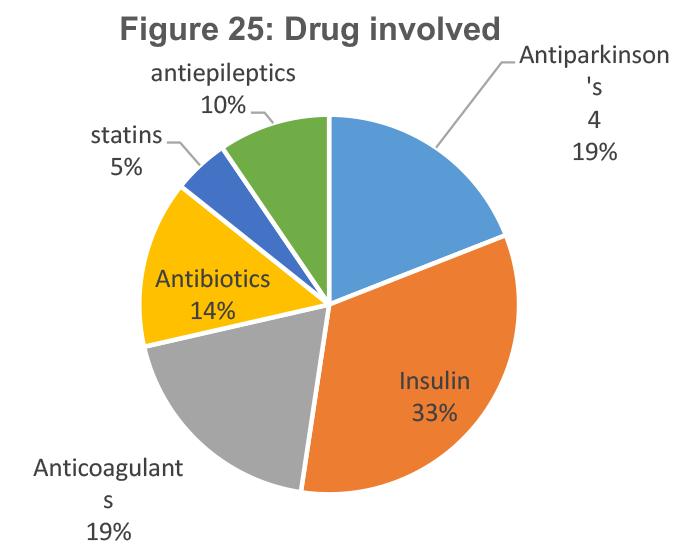

Factors that contributed to incidents included
y location, degree of pharmacy support, complexity to medication (particularly If there are multiple formulations of the same medication, or a number of similar sounding options), and recent admission status
y A number of incidents occurred within the first 24 hours of a patient’s admission, either in the Emergency Department or acute admissions unit (AAU). Those on AAU were usually identified by the pharmacist
y Three main groups of medication formed the majority of the incidents:
o Medication to treat Parkinson’s disease
o Insulin
o Anticoagulants
These three groups of medication contributed to each incident where patient harm occurred.
In addition to 10 out of 21 of total incidents, where the patient’s medicines had not been through the medicine’s reconciliation process.
y In 6 of the 21 incidents, medicines reconciliation had been performed but after the incident had taken place (> 24 hours after admission)
y A large number of incidents occurred on bank holidays and over weekends, when patients were transferred from the Emergency Department directly to a ward (and not via the AAU)
y A number of the incidents, five out of the 21), were identified by either the patient or their relative, highlighting the importance of listening to our patients. Listening to our patients, who raise a concern is vital as they are the experts in their long-term medicines and this is reinforced through our patient safety teams
y Lessons learnt in respect to medicines safety is shared at various staff forums across the hospitals from locally in individual ward areas and then Trust wide using the hospital Grand round, Medicines optimisation group and the regular weekly pharmacy forums. This is a wider piece of work undertaken within the Trust to improve how we communicate with our patients and their carers

This is Us: Our Amazing People Awards
This event is held annually to celebrate the work of our people during the year.
54 staff members were shortlisted (from almost 400 nominations received), resulting in the following individuals recognised across our 12 award categories, that included:
• Kindness Award
• Safety Award
• Speaking Up Award
• Learning Award
• Commitment Award
• Improvement Award
• Inclusion Award
• Teamwork Award
• Engagement Award
• Managing for Excellence Award
• Emerging Leader Award
• Inspiring Leader Award
• Patient Panel Champion Award













Long Service Awards Recognition – the Trust holds an annual event to celebrate the staff member Long Service Awards.
y 90 people were presented with certificates and a pin badge to mark 20 years of service at PAHT
y 25 people were presented with certificates and pin badges to mark 25 years of service at PAHT

The annual NHS National Staff Survey (NSS) is recognised as an important tool for ensuring that the views of people working in the NHS are used to help inform local improvements. The feedback is useful in helping highlight strengths, and improvements that will make PAHT a better place to both work and be treated.
The NHS Annual Staff Survey 2024 results are benchmarked nationally and show our results against the national average. The questions are aligned to the NHS People Promise which are the seven elements that would most improve working life as chosen by NHS employees.

Over 2000 employees completed the National Staff Survey in 2024:
y There was a 49% response rate, a 1% decrease on last year, however a 6% increase in actual respondents
y 5% of respondents shared a free-text comment, which offered further insights about specific issues important to our people
y We achieved an improvement on the previous National Staff Survey results across four elements including morale, however declined in other areas such as engagement
y Summary presented in table below that shows the best / median results achieved in the survey and the Trust data
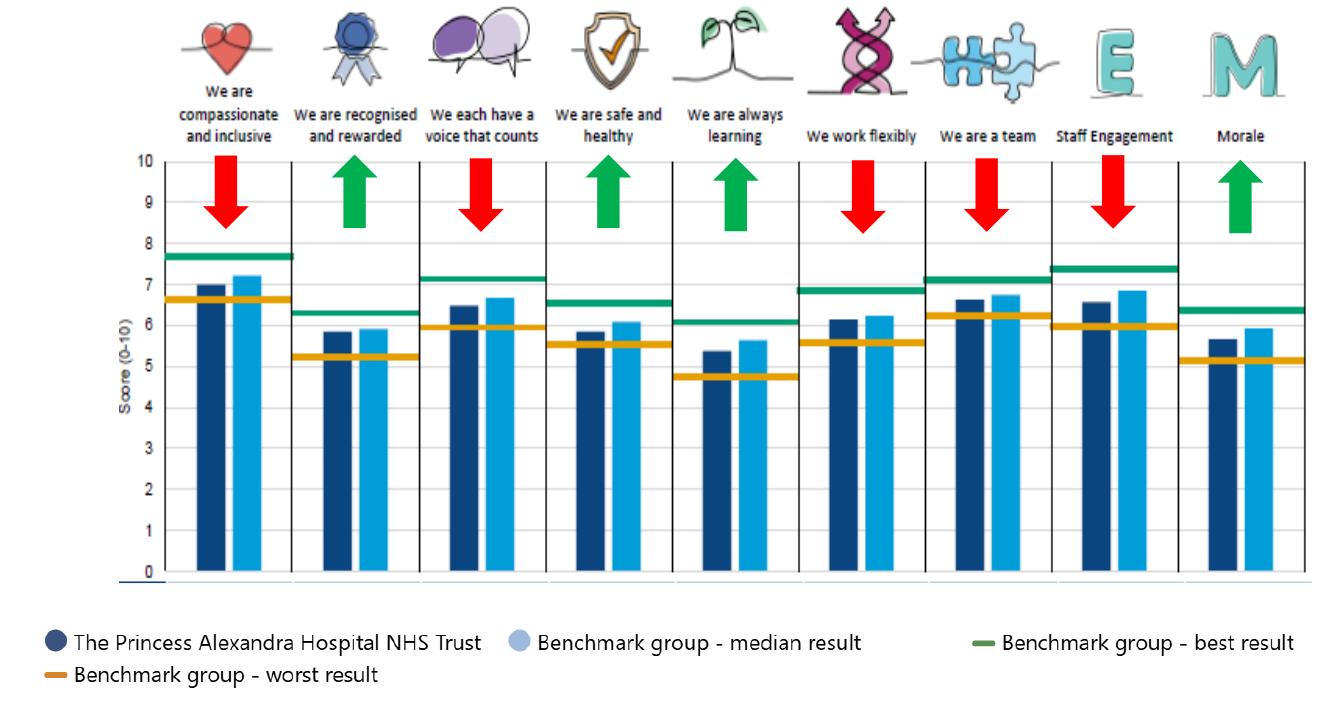
Critically, two important questions for the Trust showed no change / declined this year:
1. Would you recommend PAHT as a place to work?
This achieved 50%, which is equal to last year.
2. Would you be happy with the standard of care if a friend or relative needed treatment at PAHT?
This achieved 46%, which was a 1% decrease on last year (47%)
The executive board has identified three key areas for all divisions to concentrate on within their 2025 engagement plans:
y People Promise: We are compassionate and inclusive
y People Promise: We are a team
y People Promise: We are recognised and rewarded
Trust statistics monitored by the people team are detailed on table 7
Table 8: People Key Performance Indicators
In February 2024 we published our Equality, Diversity and Inclusion (EDI) strategy along with an EDI Delivery Plan 2024-5 that will support engagement with external partners and adherence to our commitment to diversity as a core value. This included a Governance framework and timetable to meet our regulatory reporting responsibilities. We are committed to improving the quality and extend our data and information in relation to protected characteristics. This will inform the development of equality actions and activity within the delivery plan.

To achieve this our aim is to:

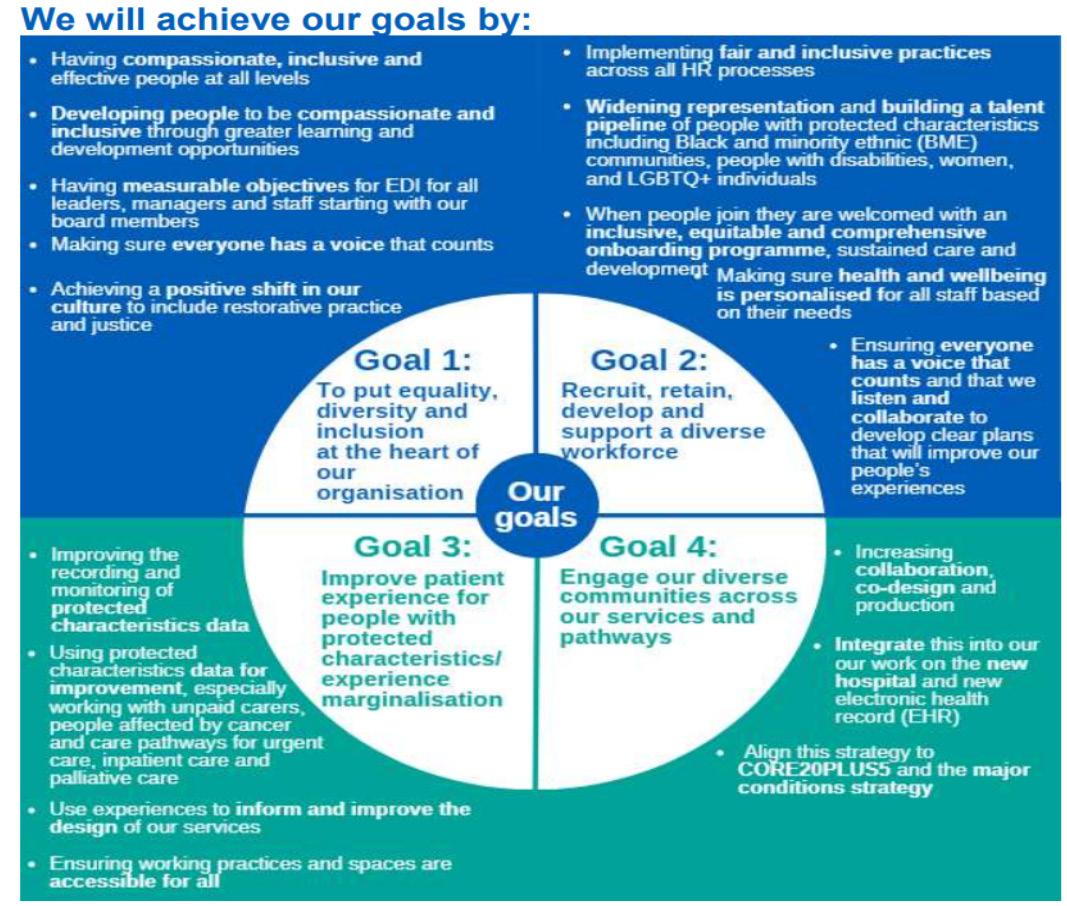
The EDI Delivery Plan details the actions we are taking to deliver the following reporting requirements:
y EDI Annual Report – (EDI goals and objectives)
y NHSE EDI Improvement Plan
y Workforce Race Equality Standard
y Workforce Disability Equality Standard
y Gender Pay Gap Report
y Ethnicity Pay Gap Report
y Equality Delivery System
y East of England Anti-racism Strategy
y Health Inequalities (from 2025 - 2026)
The outcome of the Delivery Plan will be reviewed along with new activity to create our EDI Delivery Plan for 2025 - 2026.
The EDI Steering Group (EDISG) is responsible for the monitoring of our EDI Delivery Plan and Governance framework. The EDISG consists of a diverse range of our people with representation from teams and departments across the Trust. The main aim of the group is to help shape the organisation’s strategies and policies to improve the experience of staff and patients with protected characteristics.
The Trust actively participates in the ICSwide EDI network. Strong relationships have been developed with the other participants in the ICS and PAHT is working collaboratively on a number of diversity initiatives including recruitment, leadership development, and anti-racism awareness.
A plan was developed by the patient engagement team alongside the patient panel and other stakeholders, to make some improvements to the required access to services by patients. Through our membership of the Disability Forum, we are in the process of preparing a disability audit to examine and improve policies and practices across the organisation. Further work is underway in partnership with our volunteers. Progress will be reported in our EDI Delivery Plan for 2025-26.
In addition, plans are being devised with our Estates and Facilities team, for the New Hospital and PAHT2030 strategy, to support the improvement of accessibility for all.
A plan for all year-round communications is being devised. We are also utilising our membership with the Business Disability Forum, to improve accessibility of information, throughout our communication platforms.
We have reviewed our staff networks in line with the NHS Guidance for Staff Networks 2024. The Trust currently has three staff networks; the Disability and Wellbeing Network (DAWN), the Race Equality and Cultural Heritage (REACH) staff network and the Alex Pride (LGBTQ+) staff network.
The DAWN network continues to thrive, it is now in its second year. The purpose of the network is to be an independent and effective voice for staff with long term health conditions and disabilities. The network has worked closely with the staff health and wellbeing team to raise awareness of access to work, promoted Deaf Awareness week and provoked discussions on invisible disabilities through videos and general communications.
The REACH network has supported the organisation to move forward on race equality with a focus on its three primary objectives:
(i) The promotion of Psychological Safety
(ii) Support for Continuing Professional Development
(iii) Achieving our goals through Allyship with other networks.
The LGBTQ+ staff network re-established its name to Alex Pride. The network has invited members of the LGBTQ+ community to meetings to share learning and as an opportunity to inform Trust policies and practices. The network is linked in with the East of England LGBTQ+ network.
In the coming year the Trust intends to develop two more staff networks, to represent Faith and Belief and Women.
The Trust’s monitoring of operational performance against national constitutional standards and local standards is monitored and reviewed at:
y Regular Divisional Review Meetings between members of the executive team and each division or department
y Executive Board
y Operational Board
y Operational Cell
y Strategic Cell
y Executive Cabinet
y Quality and Safety Committee
y Alex Health Operational Advisory and Readiness Board
y Patients, Quality and Productivity meetings (PQP)
y Divisional Board
y The Cancer Board
y The Performance and Finance Committee
y Trust Board meetings
An Integrated Performance Report is presented to the Performance and Finance Committee, Quality and Safety Committee and Trust Board meetings. Externally, the Trust is held to account for its operational performance by NHS England/Improvement and its commissioners.
Delivery of all national standards has continued to be impacted by the increased elective waiting lists caused by the Covid-19 pandemic, industrial action, high numbers of emergency patients requiring care and the deployment of the Trust’s new Electronic Health Care Record; Alex Health.
The Trust focussed on improving the efficiency of services to ensure that as many patients received appointments and treatment as possible with the facilities and staff available. Full elective operating was delivered during the winter period with only a 1-week closure of the orthopaedic ward to support the increased emergency admissions. Critical care capacity has been challenged during 2024-25 with a number of elective critical care cases requiring re-scheduling due to emergency pressures. Plans are being developed through completing demand and capacity modelling to update the business case to increase capacity in conjunction with the East of England Critical Care Network.
Throughout 2024-25, the 18-week Referral to Treatment (RTT) standard was negatively impacted as the Trust focused on reduction of our long waiting patients. Performance at the start of the 24/25 financial year was 51.2%, with March 25 performance at 46.2%. A recovery trajectory has been developed to achieve 60% by March 2026 (figure 33). During 24-25, the Trust successfully eradicated patients waiting over 78 weeks and our cohort of patients waiting over 65 weeks at the start of the 24/25 financial year was 583 in comparison to 17 at the end of March 25 (figure 28-29). The Trust continues to book patients in clinical priority order with urgent and cancer treatments prioritised at every opportunity.
Figure 28: Referral to Treatment access target – Incomplete standard
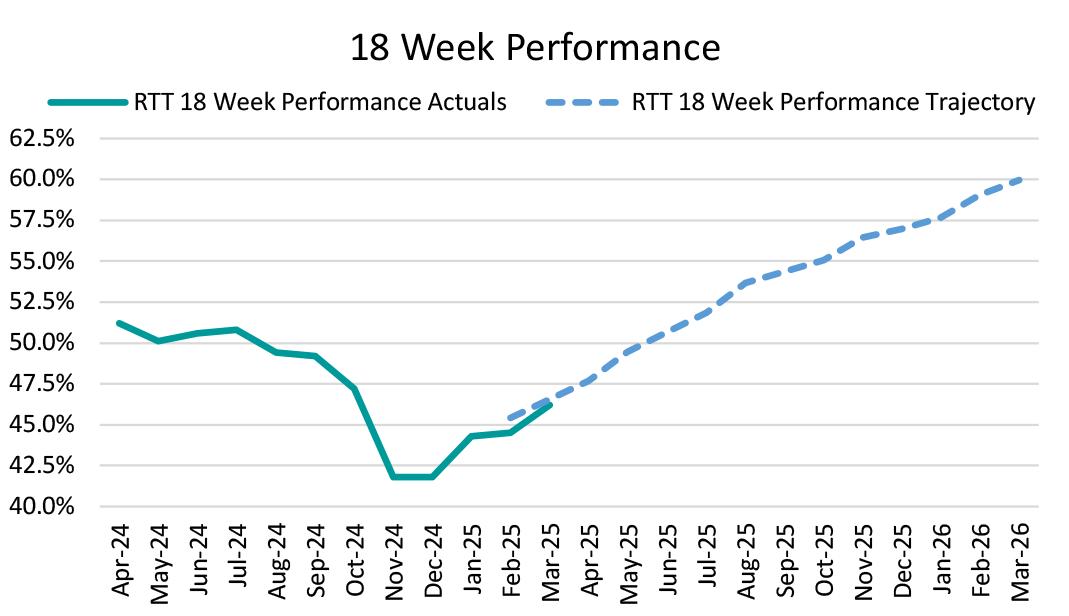
Figure 29: Referral to Treatment access target – patients waiting over 65 weeks
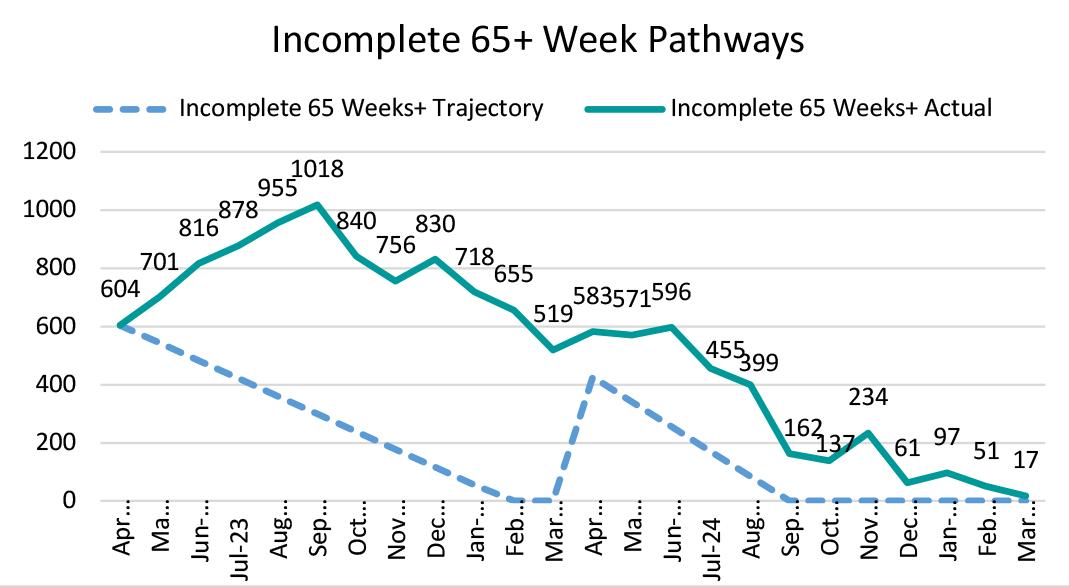
Delivery of the national cancer standards has continued to be impacted by the number of patients waiting over 62 days for their treatment, and within 2024/25 the Trust did achieve the target set by the national team for numbers of patients waiting longer than 62 days for treatment.
However, in November 2024 the backlog increased as a result of the new electronic health record implementation. Work is continuing to support bringing the backlog down and aim to exceed the target set in 25/26 (figure 30).
Figure 30: 62 Day cancer backlogs
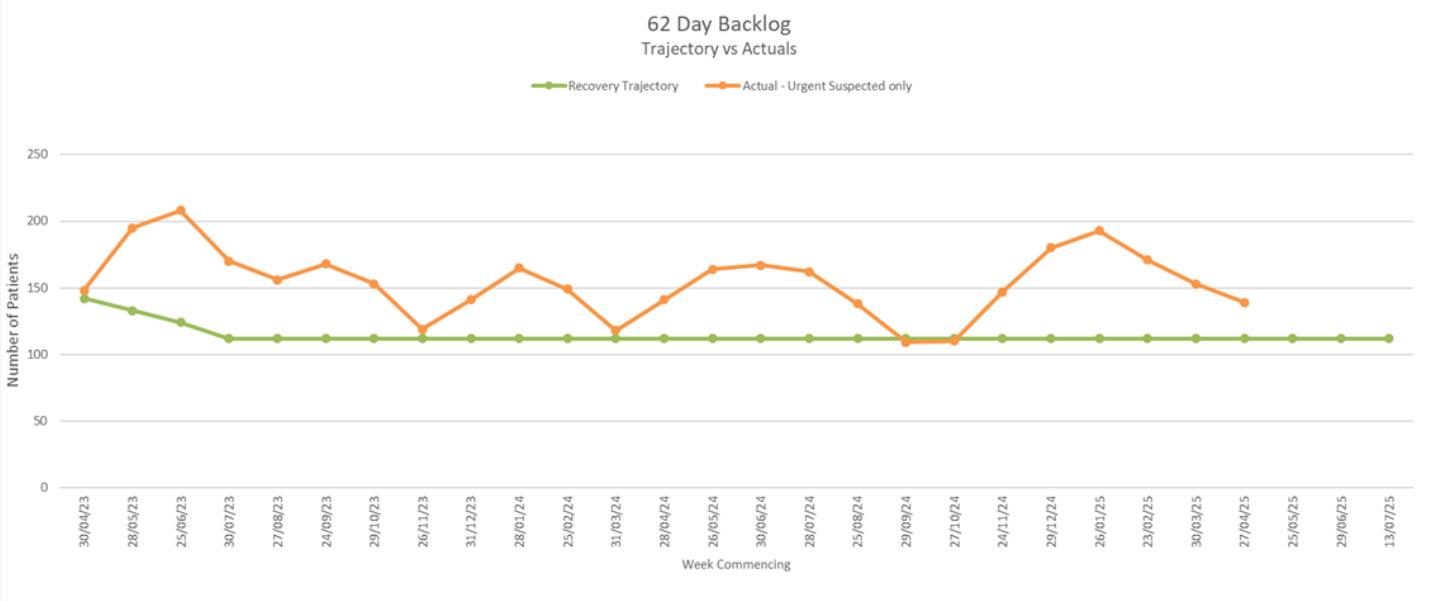
The Trust has been one of three Trust’s in the East of England to consistently achieve the clinical safety standard that ensures suspected cancer patients receive a diagnosis of cancer or no cancer within 28 days of referral, however the implementation of our EHR system in November has impacted performance. Recovery trajectories and further actions are being developed to support oversight to bring us back in line with the national standard (figure 31).
31: 28-day Faster Diagnosis Standard
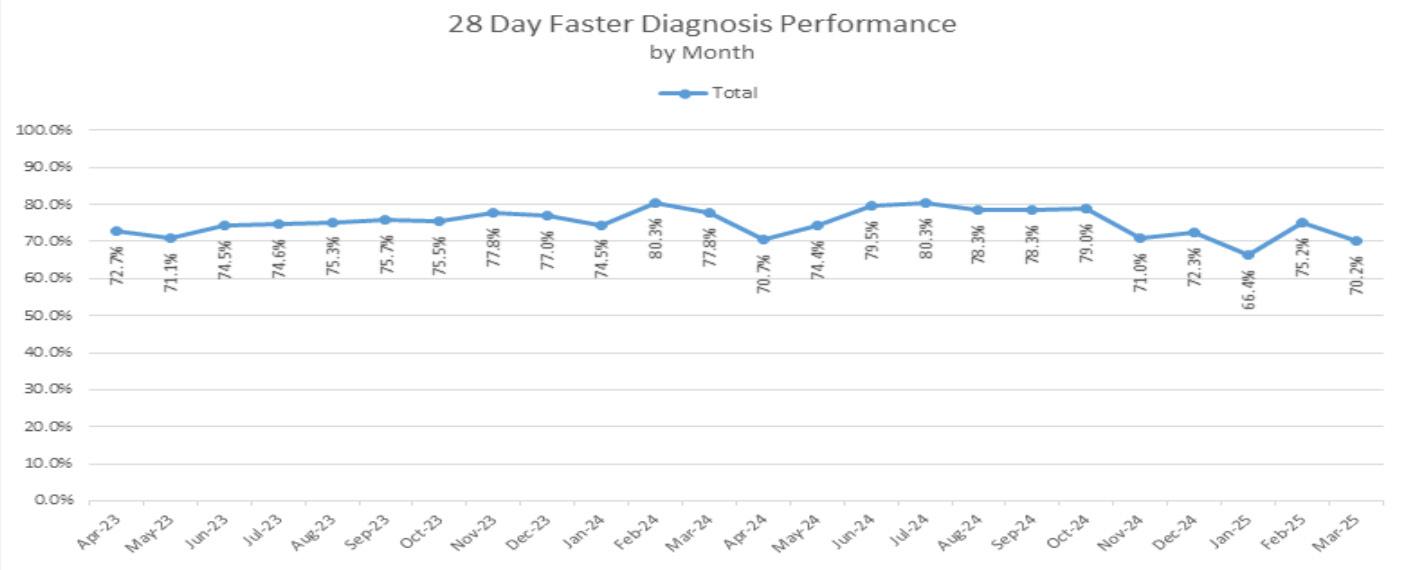
Diagnostic performance has been impacted by backlogs of routine patients waiting longer than 6 weeks for their diagnostic investigations. There have been significant increases in referrals across the radiology imaging modalities; MRI increased by 24%, 10% in Ultrasound and 20% in CT scanning.
The opening of additional capacity at the St Margaret’s Hospital site for the Community Diagnostic Centre and ongoing additional capacity from temporary diagnostic services has contributed to a steady improvement in the number of patients receiving their radiology diagnostic within 6 weeks, (figure 32). MRI and CT have achieved the monthly waiting times at 100% for a six-month reporting period within 24/25 to date.
Additional capacity in the Audiology service via the commissioning of a second Audiology booth at the Community Diagnostic Centre at Hearts and Essex Hospital has improved waiting times for paediatric assessments specifically and this has achieved 95% compliance at the end of March 2025. Adult audiology continues to be improving on an upward trajectory.
The implementation of the electronic health record in November adversely affected the reporting for Urodynamics, Colonoscopy, Flexi Sigmoidoscopy, Cystoscopy and Gastroscopy modalities. This impacted the service’s ability
to validate the position for accurate performance reporting. Significant progress has been made with performance reports available for validation going into the new financial year.
It is the Trust ambition to improve performance throughout 2025-26, with recovery of the diagnostic standard dependent on providing additional capacity, insourcing, recruitment drives, demand and capacity modelling and overall pathway efficiencies across relevant modalities. Recovery plans are in place and being regularly monitored against trajectory.
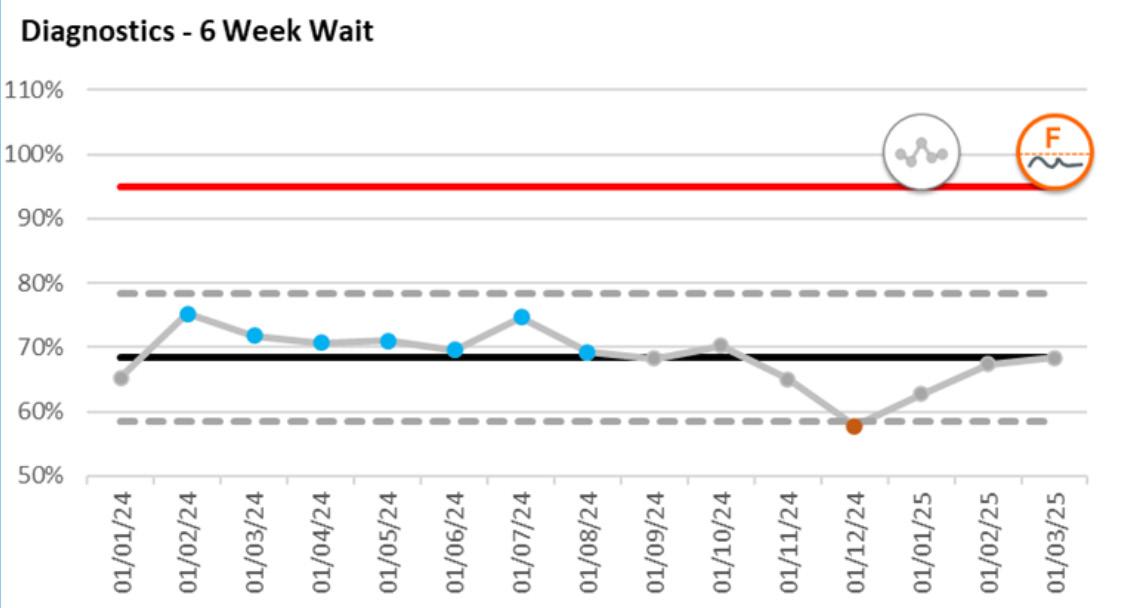
We are committed to undertaking effective clinical audit across all clinical services and recognise this is a key element for developing and maintaining high quality patient-centred services.
During 2024/25 the Trust participated in 91% of the eligible national clinical audits.
Of the three national confidential enquiries, the Trust has participated in three of the studies which it was eligible to participate in.
The national clinical audits and national confidential enquiries that the Trust participated in and for which data collection was completed during the 2024/25 period are listed below alongside the current stage / reasons for not taking part to each audit or enquiry where known.
Table 9: Project Name Workstream Name Provider Organisation Participation Stage / submission details
a) BAUS Penile Fracture Audit
BAUS Data and Audit Programme
Not applicable
b) BAUS I-DUNC (Impact of Diagnostic Ureteroscopy on Radical Nephroureterectomy and Compliance with Standard of Care Practices) Not applicable
c) Environmental Lessons Learned and Applied to the bladder cancer care pathway audit (ELLA)
British Hernia Society Registry
Case Mix Programme (CMP)
The British Association of Urological Surgeons (BAUS)
NHS Digital)
Care National Audit and Research Centre (ICNARC)
Child Health Clinical Outcome Review
Programme1
a) Emergency (non-elective) procedures in children and young people
Cleft Registry and Audit Network (CRANE) Database
a) Adolescent Mental Health
Emergency Medicine QIPs:
b) Care of Older People
National Confidential Enquiry into Patient Outcome and Death (NCEPOD)
Royal College of Surgeons of England (RCS)
Royal College of Emergency Medicine
Not applicable
a) Not due to start until 2026
b) Yes Data submission period still open
c) Time Critical Medications c) Yes
Epilepsy12: National Clinical Audit of Seizures and Epilepsies for Children and Young People1 Royal College of Paediatrics and Child Health
Falls and Fragility Fracture Audit Programme (FFFAP):1
a) Fracture Liaison Service Database (FLSDB)
b) National Audit of Inpatient Falls (NAIF)
c) .National Hip Fracture Database (NHFD)
Learning from lives and deaths –People with a learning disability and autistic people (LeDeR)
Royal College of Physicians a) Not applicable
Maternal, Newborn and Infant Clinical Outcome Review Programme1 University of Oxford / MBRRACEUK collaborative
a) Blood sodium study
Medical and Surgical Clinical Outcome Review Programme1
b) Rehabilitation following critical illness
d) Acute Limb Ischaemia
National Confidential Enquiry into Patient Outcome and Death (NCEPOD)
Mental Health Clinical Outcome Review Programme1
National Adult Diabetes Audit (NDA):1
a) National Diabetes Core Audit. Includes:
- Care Processes and Treatment Targets
- Complications and Mortality
- Type 1 Diabetes
- Learning Disability and Mental Health
- Structured Education
- Prisons and Secure Mental Health Settings
b) Diabetes Prevention Programme (DPP) Audit
c) National Diabetes Footcare Audit (NDFA)
d) National Diabetes Inpatient Safety Audit (NDISA)
e) National Pregnancy in Diabetes Audit (NPID)
f) Transition (Adolescents and Young Adults) and Young Type 2 Audit
g) Gestational Diabetes Audit
National Audit of Cardiac Rehabilitation
University of ManchesterNational Confidential Inquiry into Suicide and Safety in Mental Health (NCISH)
Not applicable
NHS England (formerly NHS Digital)
a) Yes Data submission period still open
b) Not applicable
c) Yes Data submission period still open
d) Yes Continuous data submission
University of York Not applicable
Continuous data submission
Continuous data submission
National Audit of Cardiovascular Disease Prevention in Primary Care (CVDPrevent)1
National Audit of Care at the End of Life (NACEL)1
National Audit of Dementia (NAD)1
NHS Benchmarking Network
NHS Benchmarking Network
Royal College of Psychiatrists
Not applicable
Yes
National Bariatric Surgery Registry
British Obesity and Metabolic Surgery Society
Data submission period still open
Yes 100% Round t –105 cases (target 40)
Not applicable
National Cancer Audit Collaborating Centre (NATCAN):
National Audit of Metastatic Breast Cancer (NAoMe)1
National Audit of Primary Breast Cancer (NAoPri)1
National Bowel Cancer Audit (NBOCA)1
National Kidney Cancer Audit (NKCA)1
National Lung Cancer Audit (NLCA)1
National NonHodgkin Lymphoma Audit (NNHLA)1
Royal College of Surgeons of England (RCS)
Yes
Yes
Yes
Yes
Yes
Yes
Automatic data submission from monthly Cancer Outcomes and Services Dataset (COSD)
National Oesophago-Gastric Cancer Audit (NOGCA)1 Yes
National Ovarian Cancer Audit (NOCA)1 Yes
National Pancreatic Cancer Audit (NPaCA)1 Yes
National Prostate Cancer Audit (NPCA)1
Yes
National Cardiac Arrest Audit (NCAA)
National Cardiac Audit Programme (NCAP):
a) National Adult Cardiac Surgery Audit (NACSA)
b) National Congenital Heart Disease Audit (NCHDA)
Intensive Care National Audit and Research Centre (ICNARC)
Not applicable
Not applicable
c) National Heart Failure Audit (NHFA) Yes Data submission period still open
d) National Audit of Cardiac Rhythm Management (CRM) Yes Data submission period still open
e) Myocardial Ischaemia National Audit Project (MINAP) Yes Data submission period still open
f) National Audit of Percutaneous Coronary Intervention (NAPCI)
g) National Audit of Mitral Valve Leaflet Repairs (MVLR)
h) UK Transcatheter Aortic Valve Implantation (TAVI) Registry
i) Left Atrial Appendage Occlusion (LAAO) Registry
j) Patent Foramen Ovale Closure (PFOC) Registry
k) Transcatheter Mitral and Tricuspid Valve (TMTV) Registry
National Child Mortality Database (NCMD)1
National Institute for Cardiovascular Outcomes Research (NICOR)
Not applicable
Not applicable
Not applicable
Not applicable
Not applicable
Not applicable
University of Bristol Yes 100%
National Clinical Audit of Psychosis (NCAP)1
Royal College of Psychiatrists
National Comparative Audit of Blood Transfusion:
a) National Comparative Audit of NICE Quality Standard QS138
b) National Comparative Audit of Bedside Transfusion Practice
National Early Inflammatory Arthritis Audit (NEIAA)1
National Joint Registry
National Major Trauma Registry [Note: Previously TARN. To commence data collection in 2024]
National Maternity and Perinatal Audit (NMPA)1
NHS Blood and Transplant
Not applicable
National Neonatal Audit Programme (NNAP)1
National Obesity Audit (NOA)1
National Ophthalmology Database (NOD):
a) Age-related Macular Degeneration Audit
b) Cataract Audit
National Paediatric Diabetes Audit (NPDA)1
National Perinatal Mortality Review Tool
British Society for Rheumatology
Healthcare Quality Improvement Partnership (HQIP)
Yes Continuous data submission
Yes Continuous data submission
NHS England Yes Continuous data submission
Royal College of Obstetricians and Gynaecologists
Royal College of Paediatrics and Child Health
NHS England (formerly NHS Digital)
The Royal College of Ophthalmologists (RCOphth)
Royal College of Paediatrics and Child Health
University of Oxford / MBRRACEUK collaborative
Yes Automatic data submission
Yes
Not applicable
Yes Automatic data submission
No
National Pulmonary Hypertension Audit
National Respiratory Audit Programme (NRAP):1 [Note: previously named National Asthma and COPD Audit Programme (NACAP)]
a) COPD
Secondary Care
NHS England (formerly NHS Digital)
Not applicable
b) Pulmonary Rehabilitation Not applicable
c) Adult Asthma Secondary Care Yes
d) Children and Young People’s Asthma
Royal College of Physicians Yes 147 cases
Secondary Care Yes 123 cases
National Vascular Registry (NVR)1
Out-of-Hospital Cardiac Arrest Outcomes (OHCAO)
Paediatric Intensive Care Audit Network (PICANet)1
Royal College of Surgeons of England (RCS) Yes Continuous data submission
University of Warwick Not applicable
University of Leeds / University of Leicester Yes
Perioperative Quality Improvement Programme Royal College of Anaesthetists
Prescribing Observatory for Mental Health (POMH):
a) Rapid tranquillisation in the context of the pharmacological management of acutely disturbed behaviour Royal College of Psychiatrists
Yes
Not applicable
b) The use of melatonin Not applicable
c) The use of opioids in mental health services
Not applicable
35 cases
a) Oncology and Reconstruction
b) Trauma
Quality and Outcomes in Oral and Maxillofacial Surgery (QOMS):
Not applicable
No
c) Orthognathic Surgery Not applicable
d) Non-melanoma skin cancers
British Association of Oral and Maxillofacial Surgeons (BAOMS)
Yes Data submission period still open
e) Oral and Dentoalveolar Surgery No
Sentinel Stroke National Audit Programme (SSNAP)1
Serious Hazards of Transfusion (SHOT): UK National Haemovigilance Scheme
Society for Acute Medicine Benchmarking Audit (SAMBA)
King's College London Not applicable
Serious Hazards of Transfusion (SHOT)
Society for Acute Medicine Yes
UK Cystic Fibrosis Registry Cystic Fibrosis Trust Not applicable
UK Renal Registry Chronic Kidney Disease Audit
UK Kidney Association Not applicable
UK Renal Registry National Acute Kidney Injury Audit UK Kidney Association

There were eight commercial portfolio studies and 60 non-commercial studies open throughout 2024/25. Of the eight commercial studies, one is still open to recruitment, six are closed to recruitment and in follow-up and one is closed, see figure 33 below. The Trust had 60 non-commercial studies open in 2024-25, Figure 34. From these 39 are still open to recruitment, 21 are closed to recruitment but in follow up and five are closed.
33:
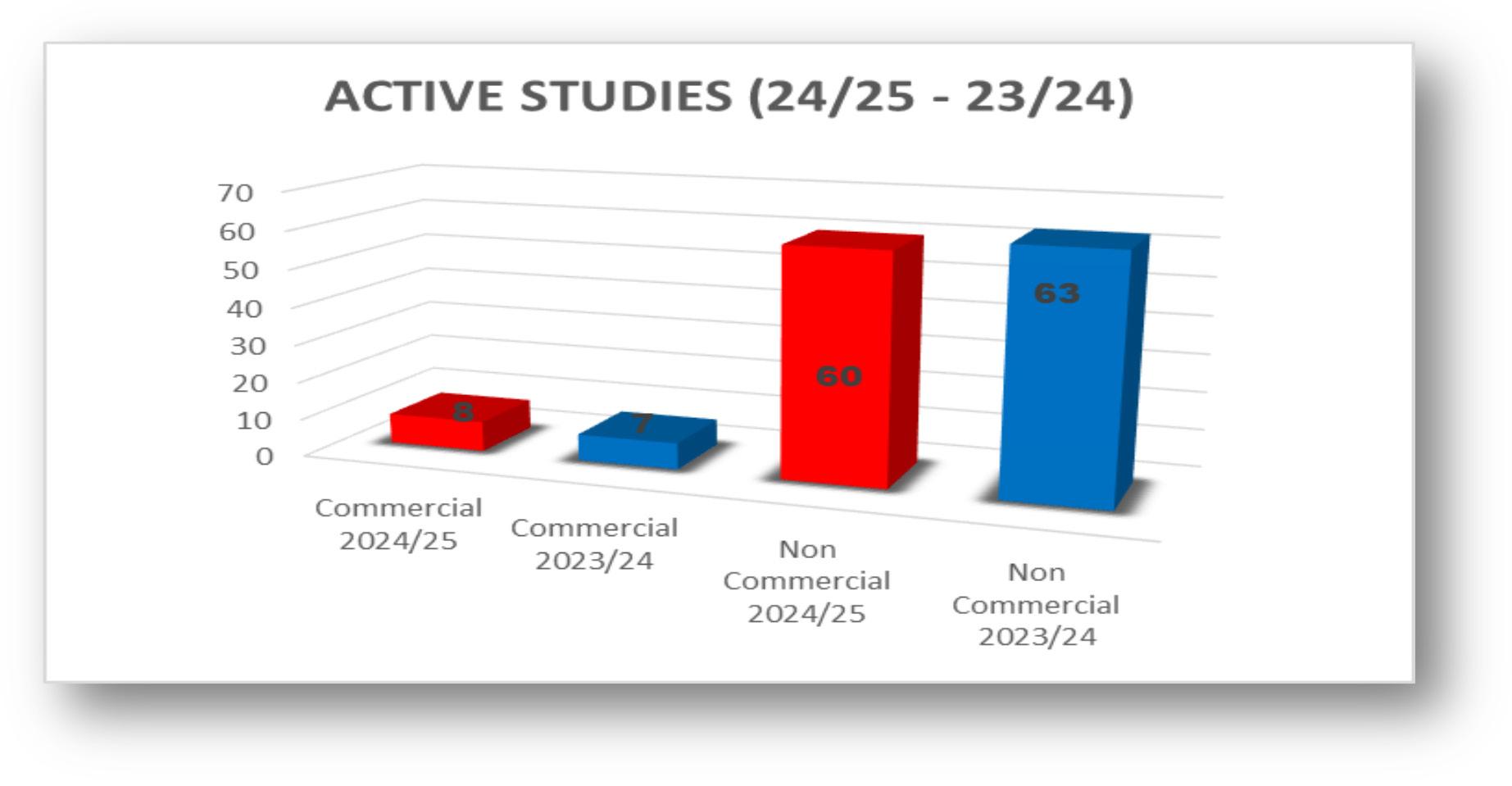
34:
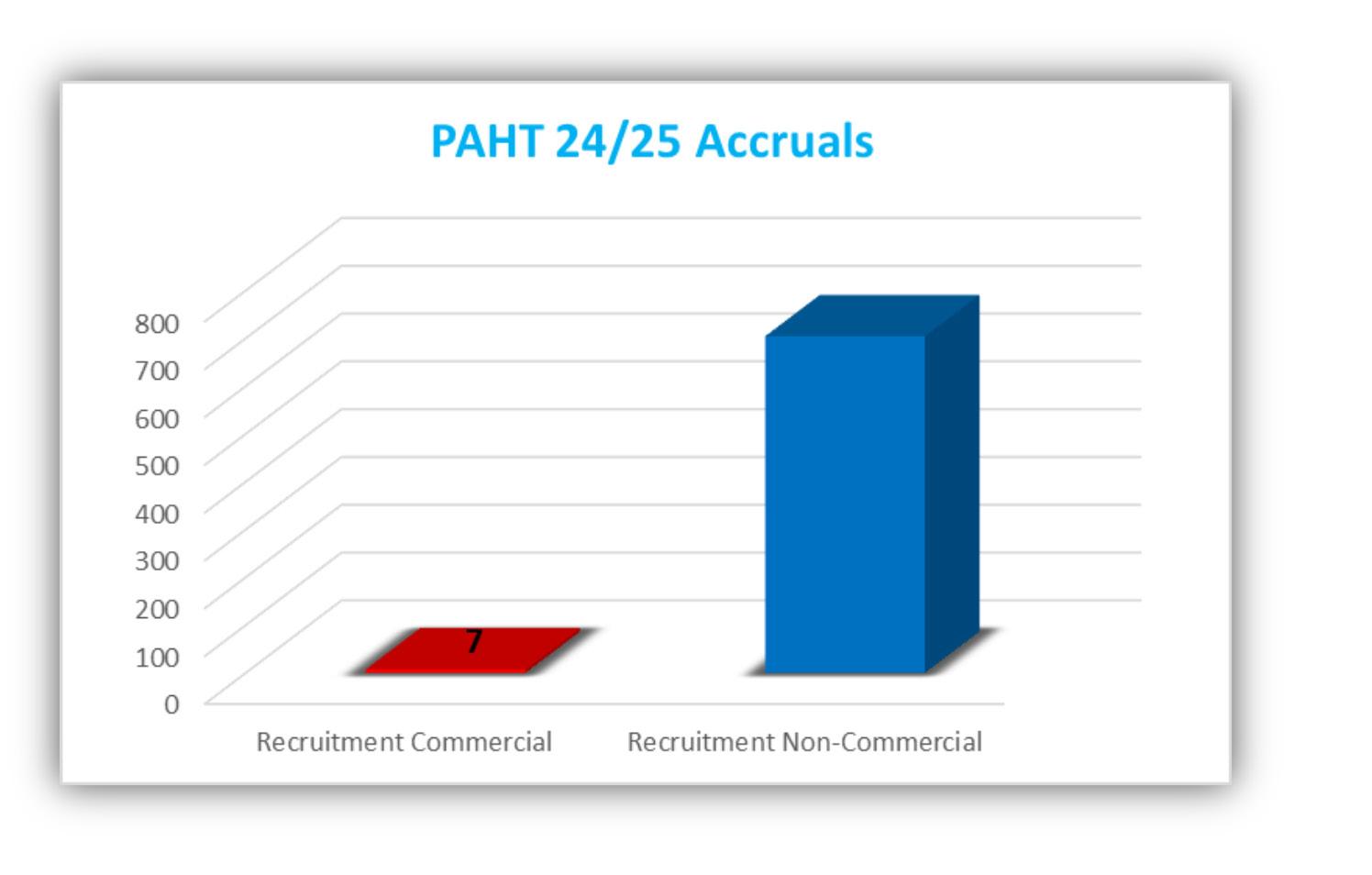
The overall recruitment for 2024-25 is 711, made up of 7 recruits to our commercial studies and 704 to our non-commercial, see Table 10.

PAHT’s new electronic health record called Alex Health went live on 2-3 November 2024.
Alex Health continues to be a major transformation project for the Trust, with a significant amount of work underway to stabilise and sustain the system and provide appropriate training and support for staff. Alex Health is a key deliverable in PAHT’s strategic ambition to be modern, integrated and outstanding, and during the coming year the programme will gradually move into a business-as-usual as part of the Trust’s broader digital strategy. Alex Health is a single digital record of a patient’s care. This includes a patient’s health history, treatments, medical conditions, and allergies. Hospital clinicians now get fast and easy access to this data, and soon patients will too as we roll out the My Alex Health patient-facing portal during 2025.
During the last twelve months, work has been split into two phases: getting ready for golive and responding to and resolving issues and ongoing usability needs after the go-live, including business as usual changes.
With the design and functionality of Alex Health agreed and locked-in following months of design, various cycles of testing were carried out and the process for migrating data from old systems to Alex Health identified.
A wide range of face-to-face engagement activities took place across the Trust to prepare PAHT staff for Alex Health and how it would change their ways of working. These were supported by information campaigns such as Stop, Start, Continue that showed staff how specific daily tasks would change, helping them prepare for the huge training programme which ran during August to November 2024, in a new purpose-built training centre on the main site. Over 95% of staff were trained by go-live; a significant achievement for the Trust to ensure safety and compliance.

Alongside the training programme, the Trust recruited a team of in-house Alex Health ‘Navigators’ and ‘Floorwalkers’ - pre-trained staff who would provide hands-on support to staff during go-live and the days thereafter, helping with adoption and troubleshooting.
During Autumn, the training continued and detailed preparations were put in place for ‘cutover’ - the period in which existing systems went down before Alex Health went live – and the go-live weekend itself. There was an event organised with system partners to improve patient flow across the system to reduce acute hospital bed occupancy and patient attendance at the hospital before, during and after cutover and go-live of Alex Health.

A two-week ‘Your Access Fair’ helped staff register their smartcards and set up Alex Health to their individual needs before go-live. Alongside this, various ‘dress rehearsals’ took place to make sure every aspect of Alex Health – from technical to clinical to operational – was fully prepared for.




During the go-live weekend all clinical specialties and wards went live in a carefully planned sequence, starting with the Emergency Department on Saturday afternoon. By the Monday morning, all wards and departments were live on Alex Health

During Winter, system configuration and staff engagement were ongoing to embed new ways of working and support continuous learning, including additional training, masterclasses led by subject matter experts, floorwalking support and quick reference guides.
With a programme of this scale, post-implementation challenges were anticipated and prepared for. With ‘early life support’ from Oracle Health and working closely with inhouse teams and system partners, the Alex Health platform continued to be refined and improved, with over 250 system configuration changes made to tailor Alex Health to meet the specific clinical and operational needs of PAHT.
Alongside the widespread staff engagement programme, system partners, patient groups, GPs and clinical leaders in Herts and West Essex were also engaged during the year. During cutover and go-live, patient engagement started to increase, with engagement beginning to raise awareness of My Alex Health - the web-based, secure digital ‘portal’ where patients can see information relating to their care with us.

1 and 2: Front and back of patient QR code card. Photo 3: Patient Engagement Day in Harlow Harvey Centre supported by the Patient Panel.
Further information about My Alex Health is included on the main homepage of the external Trust website, you can access the Alex Health page through the button on the front (yellow button): Alex Health patient portal | Princess Alexandra Hospital
www.pah.nhs.uk/alex-health


Patients can register for My Alex Health at any time; however, they will only be able to use it effectively when they are an active patient and when their specialty area has gone live on the portal. All specialty areas are expected to go-live by Summer 2025.
y The My Alex Health patient portal, launched in March 2025 and has enabled 89% of those patients invited to get registered following just one invitation. This is being rolled out in a phased process by clinical speciality
y In the first 6 weeks since the portal was available, 4,489 patients registered
y This compared favourably to the national average of 67% of patients responding to the first invitation and has been achieved through a communications campaign and outreach completed through local voluntary sector groups, our award winning patient panel and events in our local community
y As stated before, we have established a partnership with local voluntary sector organisation West Essex Community Action Network (WECAN) who are helping us by recycling electronic devices to combat digital exclusion in areas known to have digital deprivation. Through WECAN donated devices can be shared with people to use in their day-to-day outreach to support citizens in our local community who have lost access or cannot afford to purchase an up-to-date device
y The team have spent time in local shopping centres, the Harvey Centre in Harlow, an event in the Civic Centre with the leader of the Council and Chief Executive of the Hospital, Jackson Square in Stortford
y Our team are planning to continue the outreach work by hosting digital inclusion sessions in Harlow Library and other public spaces
People in our community that do not wish to use digital technology can request and still receive their hospital communication through letters and will receive appointments in the post.
To be a modern, integrated and outstanding hospital, our estate requires significant ongoing investment to enable us to provide the best services possible. During the last year the Trust invested in the estate, transforming a number of key sites that have since brought significant improvements to our operations. This is not just about investing in spaces and places, it is about investing in our people and our patients; listening to their needs, understanding what we can do better to provide and maintain the very best environment to deliver and receive care.
We have a responsibility to invest to improve the health of the planet too, and during the last year have introduced a number of initiatives to reduce our environmental impact in line with wider NHS green targets.
In 2024-25, the Harlow hospital buildings were maintained with the view to improve the experience for everyone in the hospital by:
y improving the management of buildings and engineering systems
y providing excellent and sustainable facilities
y ensuring safety and security at all times
y Specific and appropriate power supply was installed for both our neonatal intensive care unit and Emergency Department completed in year with planning for theatres. This provides clean electrical supplies that are uninterrupted, to key electrical sockets serving medical equipment to ensure the safety of our patients should a full mains failure or power occur and the Trust electrical generators do not kick in
y Remedial works were completed to the water supply and our pipework this year to update and remove redundant dead leg pipework (these allow microorganisms to grow), renewal of the heating and hot water systems serving key areas of the hospital. This upgrade provides for improved monitoring and is in line with all recent safety regulations
y The alarm systems to the medical gas supply (oxygen, medical air etc) were renewed across the site to ensure that each ward and departments systems are linked to hospital our main switchboard. This ensures that the pressure monitoring for compliance with safety regulations
y Upgrade of the Emergency Department that included new coved sealed flooring, renewal of wall cladding to aid cleaning, full decoration throughout, door protection and frames installed


y Upgrades to the Discharge Lounge in the Emergency Department and creation of a second space in the old physiotherapy gym area that received new heating, disabled toilet, kitchenette, flooring, decoration and new air conditioning
y Funding agreed for commencing work on our physical barriers for fire stopping, that included fire door renewal and a detection system across the site again in line with the most recent regulations and to aid compliance
y Hospital main kitchen fridges and freezers upgrade, along with completed upgrade of the main hospital restaurant
y Completion of new in-house fit testing room for infection prevention and control team to complete staff tests on the Harlow site
y Creation of new mental health side room on Charnley Ward to ensure the ward is safer for this group of patients


y Upgrading project for our x-ray equipment at Herts and Essex Hospital
y New x-ray equipment to the Interventional Suite in the Radiology dept
y We have appointed the main contractor and are in the final design stage to complete the new community diagnostic centre at St Margaret’s hospital, aiming for completion by December 2025
y Supporting Pharmacy department by the creation of a temporary dispensing area ahead of the installation to our new pharmacy dispensing robot that will be in place during 2025/26
y Supporting our information technology team and the Trust with installation of our 4G equipment in the telephone switch room
y Installation of new sitewide wayfinding signage to common areas of the Trust, both externally and internally
y Creation of screened, controlled and enlarged storage areas to meet service demands and national waste regulation guidance
y Upgrade to the care of elderly wards were completed to brighten up the common areas, provide new lightings, supporting handrails with door protection from advice from the Trust Dementia lead. The wards now have a quite area and staff rooms
y Creation of the charity funded sensory and dementia garden for patient and staff use, work not yet fully completed.
y Funding secured and worked commenced to create a new Emergency Department same day emergency care area anticipated to be completed by end of June 2025
y New ventilation systems installed to the hospital Cellular Pathology building to allow full compliance against latest guidance
y New two storey electronic health record Training building
y New Anaesthetic Gas Scavenging System put in place that will actively monitor these gas mixtures from the operating theatres and other clinical areas fitted with nitrous oxide terminal units. This will ensure safety of staff users and be overseen by the Medical Gas Committee
y Upgrade works within Fleming and Harvey Wards to the Clean / dirty utility rooms, staff room upgrade and creation of a new store room
y Creation of additional parking bay, including disabled bay provisions to Gibberd ward and Williams Day Unit

In line with targets set by Greener NHS and targets already within our green plan, we continued working towards achieving net zero by 2040 for emissions we control directly and by 2045 for emissions we can only influence i.e. supply chain emissions.
y NHS National Energy Efficiency Fund (NEEF) – Phase 2.
The Trust was successful in our application to the National Energy Efficiency Fund (NEEF) to procure, install and commission LED lighting and Solar PV grant. The Trust was awarded £170,765 for LED lighting upgrade across the hospital site. It is estimated that this yield benefits in reducing our energy consumption by 119,277 kWh so will reduce our carbon footprint and give cost savings. A completion date is planned by end of June 2025
y NHS National Energy Efficiency Fund (NEEF) -BMS
The Trust was successful with its application for NEEF funding to install Building Management System controls to our air conditioning systems. The Trust was awarded £259,932 for the procurement, install and commission 90 units for BMS expansion and again it is anticipated that it would reduce the energy consumption by estimated saving of 643,429kWh so give both a cost saving and carbon foot print saving
y Heat Decarbonisation Plan (HDP)
Following approval for funding to develop our heat decarbonisation plan for the Trust, the estates team have commissioned Low Carbon Europe (LCE) to produce the HDP. The trajectory to achieve net zero by 2040 and recommend decarbonisation actions are planned
y Electric vehicles
The transport team within facilities have Electric vehicles which are used to transport medical records, Central Sterile Supply Department instruments, pharmacy items; between the main hospital site and to both St Margaret’s and Herts and Essex Hospitals
Following the financial penalties imposed by our clinical waste supplier (Stericycle), the Trust implemented the following actions to resolve the waste segregation issues, which have improved the segregation of items. A new audit was completed and the penalties were removed.
To deliver this improvement we completed the following:
y Increased face-to-face and one to one staff training for staff working both clinically and our facilities colleagues
y Staff induction training given for nursing staff
y Weekly awareness raised by completion of regular road shows
y Weekly meetings with our contractor
y Contractors’ (Stericycle and Sharpsmart) support the Trust through educational material provisions and participation in the roadshows

Response to PAHT’s Quality Account 2024-25 from Healthwatch Essex
Healthwatch Essex is an independent organisation that works to provide a voice for the people of Essex in helping to shape and improve local health and social care. We believe that health and social care organisations should use people’s lived experience to improve services. Understanding what it is like for the patient, the service user and the carer to access services should be at the heart of transforming the NHS and social care as it meets the challenges ahead of it.
We recognise that quality accounts are an important way for local NHS services to report on their performance by measuring patient safety, the effectiveness of treatments that patients receive and patient experience of care. They present a useful opportunity for Healthwatch to provide a critical but constructive, perspective on the quality of services, and we will comment where we believe we have evidence – grounded in people’s voice and lived experience – that is relevant to the quality of services delivered by Princess Alexandra Hospital NHS Trust (PAHT).
We offer the following comments on the PAHT Quality Account:
y We are pleased to see Martha’s Rule will be implemented as a priority for 2025-26. The Healthwatch network have publicly welcomed this because patients and their loved ones know the patient’s behaviour best
y There has been an increase in concerns and complaints this year, which is disappointing, but the proactive steps taken to address these are positive. In particular, we note the efforts to improve communication with the Deaf Community and those with learning disabilities. PAHT have engaged with our ambassadors with lived experience in training this year and we will continue to offer support with this going forward
y We welcome the initiatives to support carers. Using Carers Passports can be a great tool for improving communication and support for carers. Introducing a Carers Lead would also be a worthwhile step
y It can be more challenging to engage with young people so the work of the Patient Panel in engaging eight-year-olds through a hospital tour is positive. It would be great to see this expanded to other age groups in the future
y Waiting times are an ongoing challenge for many Trust’s and a concern for many people who feedback to us. It is positive to see the partial improvements in waiting times, with the goal of reducing these to meet the national guidance
Listening to the voice and lived experience of patients, service users, carers, and the wider community, is a vital component of providing good quality care and by working hard to evidence that lived experience we hope we can continue to support the work of PAHT.
Chloe Dench
Communications Manager, Healthwatch Essex
May 2025
Healthwatch Hertfordshire’s response to The Princess Alexandra Hospital NHS Trust (PAHT) Quality Account 2024/2025
Healthwatch Hertfordshire is pleased to provide a response to PAHT’s Quality Account 2024/25, particularly as a significant number of residents from East Hertfordshire, Hoddesdon and Broxbourne are treated at the Trust.
PAHT demonstrates a learning culture with a level of openness in the Quality Account through the work on the PAHT2030 Change strategy for example. We look forward to seeing how the impacts of this relate to an improved culture and working environment and improved outcomes for patients.
The Quality Account priorities have clear targets and monitoring arrangements, and we are pleased to see that Martha’s Rule, also known as Call for Concern (a patient safety initiative for families and staff to call for an independent review if they are concerned about a patient’s deterioration) has been included as a priority as this is so important for patient safety. We look forward to seeing the full roll out and assessment of this priority.
We welcome that there is a focus on reducing elective care waiting times in next year’s objectives so that patients can receive their care in a timelier manner. Whilst we know it’s a challenge, people’s situations and circumstances, including their need for information, advice and support about ‘waiting well’ need to be carefully considered and clearly communicated during this period.
The case studies and deep dives from the Patient Experience Group (which we regularly attend) shows a level of listening and learning about people’s experience and a commitment to improvement. We know that complaints have increased (partly due to the difficulty with outpatient appointments with the introduction of the new Electronic Patient Record: Alex Health) but that the Trust has

introduced positive initiatives to address communication concerns including working with the Deaf Community and people with learning disabilities to improve cancer information, looking at ways to minimise digital exclusion and training staff in positive ways to communicate with patients.
We commend the work of the Patient Panel in engaging with the local community and expanding its reach and representation including several outreach visits to Bishop’s Stortford. We also note their work on engaging with young people. Children and Young People is a focus area of our work programme this year and we will be happy to collaborate and share insights from our research with PAHT. We are pleased to see the focus on Dementia and the work being done to support these vulnerable patients and their families to promote wellbeing and reduce social isolation during their stay in hospital. It is important that the specific care needs of people with dementia are fully understood, and it is good to see the training and support being provided for staff and volunteers who have contact with people with dementia. Support for carers and the carers passports is also welcomed.
While it is good news that PAHT has been confirmed in Wave 2 for new hospital funding, we have concerns that ongoing estates issues may impact on patient care in the meantime. We recognise that this is a challenging time for the Trust, and it is good to see that this concern has been included in the Quality Account.
We welcome the focus on psychological support for staff and the work on Freedom to Speak Up ambassadors. Our research on the experience of International Recruits in the NHS has shown the importance of peer support and open conversation. Retaining and supporting staff to provide high quality care is crucial to ensuring patient safety and experience.
Collaboration and partnership working is evident in the Quality Account, and it will be important to maintain and strengthen these relationships during this period of change in the NHS.
We look forward to continuing to work closely with the Trust to help enhance opportunities for patient voices to be heard and services to be improved, including supporting the quality priorities outlined in this Quality Account.

Neil Tester, Chair Healthwatch Hertfordshire
June 2025



NHS Hertfordshire and West Essex Integrated Care Board (HWE ICB) response to the Quality Account of Princess Alexandra Hospital NHS Trust for 2024/2025
NHS Hertfordshire and West Essex Integrated Care Board (HWE ICB) welcomes the opportunity to provide this statement on The Princess Alexandra Hospital NHS Trust (PAHT) Quality Account for 2024/25. The ICB would like to thank PAHT for preparing this Quality Account, developing future quality priorities, and acknowledging the importance of quality at a time when they continue to deliver services during ongoing challenging periods. We recognise the dedication, commitment and resilience of staff, and we would like to thank them for this.
HWE ICB is responsible for the commissioning of health services from PAHT. During the year the ICB has been working closely with PAHT in gaining assurance on the quality of care provided to ensure it is safe, effective, and delivers a positive patient experience. In line with the NHS (Quality Accounts) Regulations 2011 and the Amended Regulations 2017, the information contained within the Quality Account has been reviewed and checked against data sources, where this is available, and confirm this to be accurate and fairly interpreted to the best of our knowledge.
The Trust has identified priorities for 2025/26 that are fundamental elements of their ‘Five P’ strategy covering: our patients, our people, our performance, our places, and our pounds. This includes continuing the work to reduce the mortality rate, improve patient outcomes, reduce harm from long waits in the Emergency Department and improve staff well- being. The Trust has provided transparent information regarding the 2024/25 priorities that were not met and remain ongoing, as well as the next steps going forward for these priorities. Progress against all the priorities will be monitored through the Trust’s Quality and Safety Committee.
The Trust has provided an account of the Care Quality Commission (CQC) inspections they have received, and the Trust continues to focus on their improvement plans and regularly report progress to the Trust’s Quality and Safety Committee, to the ICB and to the CQC.
In November 2024 PAHT introduced Alex Health, a new Electronic Health Record (EHR) system. This is a significant transformation project and continues to be embedded Trust wide. It is a key deliverable of the Trust’s strategic ambition to be modern, integrated and outstanding. The Quality Account gives a detailed summary related to the progress of Alex Health and the ongoing areas of work, including the roll out of the My Alex Health patientfacing portal during 2025.
Regarding the delivery of the national cancer standards, these have continued to be impacted by the number of patients waiting over 62 days for treatment, however, progress has been made in reducing the long waits. The Trust is one of the top performing Trust’s in the East of England for the faster diagnosis standard and where there has been an impact from the implementation of the new EHR system, recovery trajectories and actions are in place.


In 2024/25, the Trust experienced an 85% increase in complaints compared to the previous year. In response, several improvements have been implemented, particularly in communication and the use of technology, to enhance patient experience and address concerns more effectively.
The Trust has identified many departments and speciality teams within which improvements have been made in the last year, including the teams caring for patients with dementia, and the continued wide ranging and constructive work of the patient panel.
The 2024 NHS National Staff Survey results demonstrated the Trust achieved improvements across four areas including morale and the ICB recognises the ongoing work and commitment within the Trust in progressing the Staff Survey findings.
The Trust reported two “Never Events” in 2024/25, of which, one investigation has been completed with significant learning and changes in practice to mitigate against a recurrence. The second Never Event remains under investigation at the time of writing this statement and immediate actions have been developed and implemented pending conclusion of the investigation.
Significant learning from patient safety incidents has been demonstrated, including in relation to establishing a post-operative cataract community triage and assessment process, development of a chest pain pathway, and training in relation to identifying sepsis.
The ICB acknowledges PAHT for their dedication in implementing the Patient Safety Incident Response Framework (PSIRF), strengthening how the NHS learns from patient safety incidents to enhance care and
outcomes. We will continue our joint working with PAHT and system partners as part of continued progression with PSIRF and the National Patient Safety Strategy and recognise that evidencing key principles
such as compassionate engagement, proportionality, and system-wide approaches will be vital to ensure its ongoing success.
Looking forward to 2025/26, the ICB supports PAHT quality priorities and we look forward to a continued collaborative working relationship, including through building on existing successes and collectively taking forward needed improvements to deliver high-quality services for this year and thereafter.

Toni Coles Place Director, West Essex
Hertfordshire and West Essex ICB
Dr Jane Halpin, Chief Executive
Rt.
Hon. Paul Burstow, Chair

Following the recent County Council elections we now have a new Health Scrutiny Committee and they are yet to have their first meeting.
As such the Committee is not able to provide specific feedback on the Quality Account however the Chairman has asked me to acknowledge receipt with thanks and to say that the Committee will note the contents and looks forward to working with the Trust over the coming term.
Could I ask that the final version be circulated to me please and I will ensure it is circulated to all Health Scrutiny Committee members.

Acute coronary syndrome - refers to a group of conditions where the heart muscle suddenly stops receiving enough blood with symptoms being chest pain or pressure, shortness of breath or dizziness. Includes conditions such as angina, myocardial infarction (heart attack)
Allied health professionals - Healthcare professionals working in dietetics, occupational therapy, physiotherapy, operating department assistants, radiography and speech and language therapy. This is distinct from nursing, medicine, pharmacy and healthcare scientists
Ambulatory care - Medical care provided on an outpatient basis, includes diagnosis, observation, consultation, and treatment
Antenatal – This is the care you receive from health professionals during your pregnancy
Antimicrobial resistance - The ability of a bacteria to resist the effects of medication (antibiotics) that once could successfully treat the infection
Antimicrobial stewardship - A coordinated intervention designed to improve and measure the appropriate use of antimicrobials by promoting the selection of the optimal antimicrobial drug regimen, dose, duration of therapy, and route of administration
Audiology - The study of hearing and balance
Bacteraemia – An infection of bacteria in the blood
Best interest decision – making a decision in someone’s best interest and in respect to hospital care it means that a specific decision will be made by at least two clinical staff about care / treatment for a person deemed to lack the mental capacity to make that decision for themselves
Cardiac arrest – Sudden loss of blood flow from failure of the heart to pump effectively
Cardiology - The branch of medicine that deals with diseases and abnormalities of the heart
Care Quality Commission (CQC) - CQC is an executive non-departmental public body of the Department of Health United Kingdom. Established in 2009, it is the independent regulator of all health and social care services in England
Chemical pathology – A branch of pathology dealing with biochemical basis for disease
Chemotherapy - The treatment of disease by the use of chemical substances, especially the treatment of cancer by cytotoxic and other drugs
Chronic obstructive pulmonary disease (COPD) - The name for a collection of lung diseases including chronic bronchitis, emphysema and chronic obstructive airways disease
Clinical audits - A process aimed to improve quality of patient care and outcomes through systematic review of care against explicit criteria and the implementation of change
Clinical coding - The process by which patient diagnosis and treatment is translated into standard, recognised codes that reflect the activity that happens to patients
Clostridium difficile (C.difficile)Clostridium difficile, also known as C. difficile, or C. diff, is a type of bacterial infection that can affect the digestive system
Community-onset healthcare associated infection (COHA) – is when an infection is detected when a patient is a home but they have only arrived home within two days of admission to hospital, and the patient was an inpatient in the Trust in the previous four weeks.
Colorectal care - Treatments for patients with symptoms of the gastrointestinal tract including colorectal cancer and inflammatory bowel disease
Colposcopy and hysteroscopy services
- A procedure used to examine the cervix and inside of the womb (uterus)
CQUIN - Commissioning for Quality and Innovation is a system introduced in 2009 to make a proportion of healthcare providers’ income conditional on demonstrating improvements in quality and innovation in specified areas of care
Creatinine clearance – this is a calculation that allows clinicians to assess the impact of renal impairment on medicine safety
Datix - Software used in healthcare to collect patient safety incidents and for reporting adverse events
Deep tissue injury – is damage to the subcutaneous tissue that results from externally applied load/pressure. This is distinct from a pressure ulcer and is not always associated with broken skin
Delirium - Is a state of mental confusion that can happen if you become unwell. It is also known as an acute confusion
Dementia champions - A group of staff who have had specific training in dementia care. Their aim is to make other colleagues more understanding of why a patient may be more challenging and encourages them to tailor therapies accordingly
Deprivation of liberty – taking away a person’s freedom, specifically their freedom to leave and so placing them under continuous supervision and control. This typically occurs when a person lacks the capacity to make decisions about their own care and treatment and so they will not be free to leave a place where they are being cared for.
Dermatology - The branch of medicine concerned with the diagnosis and treatment of skin disorders
Diagnostics - Tools used to help identify disease and illness
Dietetics – A branch of healthcare concerned with the diet and its effects on health, especially with the practical application of a scientific understanding of nutrition
Endocrinology - The branch of physiology and medicine concerned with endocrine glands and hormones
Endoscopy - A procedure that allows a view the inside of a person’s body
ENT clinics – An area where diagnosis and treatment are provided to conditions of the ear, nose and throat
Escherichia coli (E.coli) bacteraemia - Type of bacterial infection and a blood stream infection
Frailty service – Reviews frail older people using a holistic assessment of physical, mental and social needs
Friends and Family Test (FFT) - Test aimed at providing a simple headline metric which, when combined with follow-up questions, is a tool to ensure transparency, celebrate success and galvanize improved patient experience. It asks “How likely are you to recommend our services to friends and family if they needed similar care or treatment?” with answers on a scale of extremely likely to extremely unlikely
Gastroenterology - The branch of medicine which deals with disorders of the stomach and intestines
Genito-urinary - The branch of medicine relating to the genital and urinary organs
Governance - Establishment of policies, and continuous monitoring of their proper implementation, by the members of the governing body of an organisation
Gram negative blood stream infections (GNBSIs) - Type of bacterial infection and a blood stream infection
Gynaecology - The branch of physiology and medicine that deals with the functions and diseases specific to women and girls, especially those affecting the reproductive system
Haematology - The branch of medicine involving the study and treatment of the blood
Healthcare associated infections (HCAI) - Infections that are acquired as a result of healthcare. The burden of healthcare-associated infections has mainly been in hospitals where more serious infections are seen
Health Overview and Scrutiny Committee – Local authority committees that scrutinise health issues and care in their area
Healthwatch – Obtain the views of people about their health needs and experiences of having care and social services
Hepato-pancreato-biliary (HPB)involved in the management of gallstone disease along with benign and malignant diseases of the liver, pancreas and gall bladder
Hospital acquired pressure ulcer (HAPU) – a type of pressure ulcer that developed during a person’s stay in hospital so not there on admission
Hospital onset healthcare associated infection (HOHA) – this is an infection that is detected three or more days after admission to hospital therefore considered to be hospital acquired.
Hospital Standardised Mortality Ratio (HSMR) - Calculation used to monitor death rates in a Trust
Hospital Standardised Mortality Ratio+ (HSMR+) – Is an updated model of HSMR, and includes more accurate, comprehensive assessment of hospital mortality, building upon the original HSMR model by including new variables to address: socio-economic influences on mortality and co-morbidity to include the Global Frailty Index. These were introduced in November 2024
Integrated Care Partnership and System (ICP and ICS) – are alliances of NHS providers that work together to deliver care by agreeing to collaborate rather than compete
Inflammatory bowel disease – The name for a group of conditions that cause the digestive system to become inflamed
Intravenous – Giving fluids or drugs directly into a vein
Klebsiella bacteremia - Type of bacterial infection and a blood stream infection
Laparotomy - A surgical incision into the abdominal cavity, used for diagnosis or in preparation for major surgery
Maternal and Fetal Assessment UnitOutpatient Antenatal Unit offering planned appointments for assessment of the mother and unborn baby in pregnancy
Maternal and newborn Safety Investigation (MNSI) – is a national programme to improve maternity safety across the NHS in England and the team conduct investigations following specific hospital incidents
Maxillofacial department – An area where diagnosis and treatment are provided to conditions of the mouth, face and adjacent structures
Medical examiner – senior medical doctors who are contracted for a number of sessions a week to undertake medical examiner duties outside of their usual clinical duties. They are trained in the legal and clinical elements of death certification processes
Medicines optimisation - Is the process of ensuring patients are on the most effective and fewest medications
Medicines reconciliation – the process of identifying an accurate list of a patient’s current medicines
Methicillin-Resistant Staphylococcus Aureus (MRSA) / Methicillin-Sensitive Staphylococcus Aureus (MSSA) – A specific bacterial infection
Morbidity and mortality (MandM)Meetings established to review deaths as part of professional learning
Musculoskeletal (MSK) – Encompassing the muscles, bones, joints and associated tissue
Myocardial ischaemia - When blood flow to your heart is reduced, preventing the heart muscle from receiving enough oxygen
National Confidential Enquiries (NCEPOD) - National Confidential Enquiry into Patient Outcome and Death
National Reporting and Learning System (NRLS) - A central database of patient safety incident reports
Neonatal (NICU) - New-born children and new-born intensive care unit
Neurology - The branch of medicine or biology that deals with the anatomy, functions, and organic disorders of nerves and the nervous system
NHS Digital – the national information and technology partners to the health and social care system
NHSE/I - NHS England and Improvement is responsible for overseeing Trust’s and NHS services, as well as independent providers that provide NHS-funded care
NICE - The National Institute for Health and Care Excellence provides guidance, which supports healthcare professionals and others to make sure that the care they provide is of the best possible quality and offers the best value for money
Non-Invasive Ventilation – is a breathing support method that uses a face mask instead of an endotracheal tube delivering gas into the lungs. Commonly used to treat those with chronic lung conditions and can be given in designated ward areas.
Obstetrics - The branch of medicine that deals with the care of women during pregnancy, childbirth, and the recuperative period following delivery
Oesophago-gastric care – Treating patients with problems of the gullet (oesophagus) and stomach
Oncology - The study and treatment of cancer and tumours
Ophthalmology - The study of the structure, functions, and diseases of the eye.
Orthopaedic - The branch of medicine that deals with the prevention and correction of injuries or disorders of the skeletal system and associated muscles, joints, and ligaments
Paediatrics - The specialty of medical science concerned with the physical, mental and social health of children from birth to young adulthood
Palliative care - An approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual
Pathogen – microorganisms that cause disease
Pathology - The scientific study of the nature of disease and its causes, processes, development and consequences
Patient Advice and Liaison Service (PALS) - Offering confidential advice, support and information on health-related matters. Provides a point of contact for patients, their families and their carers
Patient Panel - A group of volunteers who represent patients, families and carers of The Princess Alexandra Hospital NHS Trust
Perioperative medicine - care of patients from the time of contemplation of surgery through the operative period to full recovery.
Personal protective equipment (PPE) - will protect the user against health or safety risks at work examples are FFP 2/3 face masks medical grade
Pressure ulcer – injury to the skin and underlying tissue primarily caused by prolonged pressure on the skin
Pseudomonas – a specific bacterial infection
Pulmonary embolus – is when a blood vessel in the lung is blocked by a blood clot
Rapid Assessment and Treatment (RAT) - A treatment model used in emergency care to provide an early senior assessment and early treatment
Radiology - The branch of medicine that deals with the use of radioactive substances used in diagnosis and treatment of disease.
Referral to Treatment (RTT) – A constitutional standard that Trust’s are measured against in which a person’s waiting time starts on the day the hospital receives the referral letter from a GP to the time of first appointment or treatment
Reinforced autoclaved aerated concrete (RAAC) - It’s a light-weight form of concrete that was used across the public sector which is now found to have significant risk of failure. Many hospitals contain RAAC hence the urgent need to replace them
Renal impairment (kidney impairment) - refers to a condition where the kidneys are not functioning properly, this can range from mild to severe with the kidneys failing to adequately filter waste, excess fluids and drugs from the blood. The kidneys are vital for maintaining the body’s fluid and electrolyte balance.
Respiratory medicine – The branch of medicine that deals with the act of breathing
Respiratory Syncytial Virus (RSV) –Respiratory syncytial virus is a contagious infection causing infection of the respiratory tract
Rheumatology - The study and treatment of arthritis, autoimmune diseases, pain disorders affecting joints, and osteoporosis
SAFER care bundle – practical tool that uses five elements of best practice
Septicaemia - Sepsis is a serious blood stream infection. A serious complication is septicaemia, which is when inflammation occurs throughout the body, which can be life-threatening
Serious Incidents (SIs) - An unexpected or unplanned event that caused harm or had the potential to cause harm to a patient, member of staff, student, visitor or contractor
SMART – mnemonic for objectives that are Specific, Measurable, Achievable, Realistic and Timely
Special cause variation – unpredictable fluctuations in a process that are caused by a specific, identifiable factors not part of routine and so indicate that something unusual or abnormal has occurred.
Stakeholders - A stakeholder is anyone with an interest in a business. Stakeholders are individuals, groups or organisations that are affected by the activity of the business.
Standard Operating Procedures – A set of step-by-step instructions compiled to help workers carry out complex routine work, aimed to achieve efficiency and uniformity of performance
Standardised Mortality ratio (SMR) and Summary Hospital-level Mortality Indicator (SHMI) - Ratio between the actual number of patients who die following treatment at the Trust and the number that would be expected to die, based on average England figures given the characteristics of the patient’s treated there
Structured judgement review (SJR) –allows trained reviewers to identify and describe the quality of care received and in so doing can create a score of that quality
Super spell – refers to a continuous period of hospital care per patient, especially if this required multiple hospital stays even if across different hospitals so comprising the whole of the patient’s journey. This gives an accurate representation of the hospital’s overall performance.
Trauma Audit and Research Network (TARN) – An audit where information is collected and analysed for patients who are moderately or severely injured after an injury. Data is submitted by Trust’s and a comparison can be undertaken
UK Health Security Agency (UKHSA) –responsible for protecting every member of every community from the impact of infectious diseases
Urology - The study of urinary organs in females and the urinary and sex organs in males
Vascular surgery – Specialists that treat people with diseases of the circulation, which can be conditions affecting arteries, veins and where there are blockages to the flow of blood.
Venous thromboembolism (VTE) - A condition where a blood clot forms in a vein, most commonly in a leg where it is known as deep-vein thrombosis (DVT), a blood clot in the lungs is called a pulmonary embolism (PE)
VTE prophylaxis/ thromboprophylaxis
- The giving of a medicine or treatment to prevent a VTE
Prescribed information Form of statement
1. The number of different types of relevant health services provided or subcontracted by the provider during the reporting period, as determined in accordance with the categorisation of services:
(a) Specified under the contracts, agreements or arrangements under which those services are provided or
(b) In the case of an NHS body providing services other than under a contract, agreement or arrangements, adopted by the provider.
1.1 The number of relevant health services identified under entry one in relation to which the provider has reviewed all data available to it on the quality of care provided during the reporting period.
1.2 The percentage that the income generated by the relevant health services reviewed by the provider, as identified under entry 1.1 represents of the total income for the provider for the reporting period under all contracts, agreements and arrangements held by the provider for the provision of, or subcontracting of, relevant health services.
During 2024/25, The Princess Alexandra Hospital NHS Trust (PAHT) has provided a range of health services listed in the directory of services, table 1. Services are provided by the Trust to Integrated Care Partnership (ICP) and are usually commissioned under standard form NHS contracts.
Subcontracted activity: During the year 24/25, the Trust has subcontracted arrangements in place from our local mental health provider Essex Partnership University Trust (EPUT) The Trust has subcontracted arrangements in place from our local mental health provider (EPUT).
We have reviewed all the data available on the quality of care provided by the services listed in table 1.
In 2024-25, £361m (84%) of the total income of £430m was received for patient care activities for services listed in table 1. Including this reimbursement, 85% of income related to patient care.
The most significant element of non-patient income, £12m related to provision of education and training.
2. The number of national clinical audits and national confidential enquiries which Trust collected data during the reporting period and which covered the relevant health services that the provider provides or subcontracts.
2.1 The number, as a percentage, of national clinical audits and national confidential enquiries, identified under entry two, that the provider participated in during the reporting period.
2.3 A list of the national clinical audits and national confidential enquiries, identified under entry 2.1, that the provider participated in.
2.4 A list of each national clinical audit and national confidential enquiry that the provider participated in, and which data collection was completed during the reporting period, alongside the number of cases submitted to each audit, as a percentage of the number required by the terms of the audit or enquiry.
2.5 The number of national clinical audit reports published during the reporting period that were reviewed by the provider during the reporting period.
During 2024-25 there were 56 national clinical audits and 3 national confidential enquiries covering relevant health services that are provided.
During 2024/25 the Trust participated in 91% (51) national clinical audits and 100% of those national confidential enquiries that were relevant to the Trust where we were eligible to participate in.
The national clinical audits and national confidential enquiries that we have participated in during 2024-25 are detailed in Table 9.
The national clinical audits and national confidential enquiries that we have participated in, and for which data collection was completed during 2024-25, are listed alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry.
Detailed in Table 9
The reports of 20 national clinical audits were reviewed by the provider in 2024-25.
2.6 A description of the action the provider intends to take to improve the quality of healthcare following the review of reports identified under entry 2.5.
• To support implementation of recommendations set out in Dementia Care Pathway the Trust has a person with lived experience on the Dementia and Delirium Steering Group
• Dementia screening tool on new electronic health record with hard stop in place to ensure completed for specific patient groups within 48 hours
• To support care of people with dementia, work taking place to enable completion of personal information including preferences and needs by families via a website
• To support ensuring older hospital inpatients are enabled to be as active as possible, various work streams are in place to address deconditioning and inactivity
• Governance processes are in place to understand when post-fall checks fail to correctly identify a fall-related injury
• The Trust are participating in the Falls and Fragility expansion and were a pilot site to assess suitability of the dataset and process
2.7 The number of local clinical audit reports that were reviewed by the provider during the reporting period.
2.8 A description of the action the provider intends to take to improve the quality of healthcare following the review of reports identified under entry 2.7.
3. The number of patients receiving relevant health services provided or subcontracted by the provider during the reporting period that were recruited during that period to participate in research approved by a research and ethics committee within the National Research Ethics Service.
The reports of 13 local clinical audits were reviewed by the Trust in 2024-25.
• Review of clinic times to support family history menopause consultation times
• Review of booking process to support ENT patients seeing same consultant
• Development of documentation to support compliance with national guidance for the management of ankle fractures
Action being taken to ensure that relevant patients have been given / sent NICE patient decision aid relating to chemoprevention.
The number of patients receiving relevant health services provided or subcontracted by PAHT in 2023-24 that were recruited into research studies during the period and approved by a research ethics committee was 704
4. Whether or not a proportion of the provider’s income during the reporting period was conditional on achieving quality improvement and innovation goals under the Commissioning for Quality and Innovation (CQUIN) payment framework agreed between the provider and any person or body they have entered into a contract, agreement or arrangement with for the provision of relevant health services.
4.1 If a proportion of the provider’s income during the reporting period was not conditional on achieving quality improvement and innovation goals through the CQUIN payment framework, the reason for this.
4.2 If a proportion of the provider’s income during the reporting period was conditional on achieving quality improvement and innovation goals through the CQUIN payment framework, where further details of the agreed goals for the reporting period and the following 12-month period can be obtained.
5. Whether or not the provider is required to register with the CQC under Section 10 of the Health and Social Care Act 2008.
In 2024-25 the Commissioning for Quality and Innovation (CQUIN) payment was included within the fixed element of the contract.
Not applicable
Not applicable
PAHT is required to and is registered with the Care Quality Commission.
5.1 If the provider is required to register with the CQC: whether at end of the reporting period the provider is:
(i) registered with the CQC, with no conditions attached to registration (ii) registered with the CQC with conditions attached to registration If the provider’s registration with the CQC is subject to conditions, what those conditions are, and whether the CQC has taken enforcement action against the provider during the reporting period.
The Trust was not subject to any enforcement action during 2024/25
6. Removed from the legislation by amendments made in 2011
7. Whether or not the provider has taken part in any special reviews or investigations by the CQC under Section 48 of the Health and Social Care Act 2008 during the reporting period.
PAHT has not participated in any special reviews or investigations by the CQC during the reporting period.
7.1 If the provider has participated in a special review or investigation by CQC:
(a) the subject matter of any review or investigation
(b) the conclusions or requirements reported by the CQC following any review or investigation
(c) the action the provider intends to take to address the conclusions or requirements reported by the CQC and
(d) any progress the provider has made in taking the action identified under paragraph (e) prior to the end of the reporting period.
8. Whether or not during the reporting period the provider submitted records to the secondary uses service for inclusion in the hospital episode statistics, which are included in the latest version of those statistics published prior to publication of the relevant document by the provider.
PAHT submitted records during 2024-25 to the secondary user service for inclusion in the hospital episode statistics, which are included in the latest published data.
8.1 If the provider submitted records to the secondary uses service for inclusion in the hospital episode statistics which are included in the latest published data: (a) the percentage of records relating to admitted patient care which include the patient’s:
(i) valid NHS number
(ii) General Medical Practice Code
(b) the percentage of records relating to outpatient care which included the patient’s:
(i) valid NHS number
(ii) General Medical Practice Code
(c) the percentage of records relating to accident and emergency care which included the patient’s:
(i) valid NHS number
(ii) General Medical Practice Code
9. The provider’s Information Governance Assessment Report overall score for the reporting period as per the Data Security Protection Toolkit (DSPT) grading criteria.
10. Whether or not the provider was subject to the payment by results clinical coding audit at any time during the reporting period by the audit commission.
The percentage of records in the published data which include valid percentage:
(a) the percentage of records relating to admitted patient care which include the patient’s:
(i) valid NHS number - 99.8%
(ii) General Medical Practice Code – 100%
(b) the percentage of records relating to outpatient care which included the patient’s:
(i) valid NHS number – 99.9%
(ii) General Medical Practice Code - 99.9%
(c) the percentage of records relating to emergency care which included the patient’s:
(i) valid NHS number - 99.3%
(ii) General Medical Practice Code - 100%
PAHT Information Governance: Assessment Report via the Data Security Protection Toolkit is anticipating an overall score for 2024-25 as Standard Met.
The Trust received a green low risk with high confidence rating outcome for the associated internal audit.
PAHT was not subject to the payment by results clinical coding audit during 2024-25 by the audit commission.
However, an internal clinical coding information governance audit was undertaken by an NHS Digital qualified clinical coding auditor
10.1 If the provider was subject to the payment by results clinical coding audit by the audit commission at any time during the reporting period, the error rates, as percentages, for clinical diagnosis coding and clinical treatment coding reported by the Audit Commission in any audit published in relation to the provider for the reporting period prior to publication of the relevant document by the provider.
11. The action taken by the provider to improve data quality.
Not applicable for 2024/25.
PAHT has taken the following actions to improve data quality:
a) a full suite of data quality reports produced daily/weekly and circulated to divisional teams for resolution of issues
b) data quality issues are monitored and addressed through the data quality group and operational board
c) data quality updates are provided to the Performance and Finance Committee, Information Governance steering group and System Access Board
d) respond in full to externally reported data quality issues from NHS England, ICB and our commissioners.
The NHS England Data Quality Maturity Index score is 90.2% for December 2024; the national average is 86.5% (covering APC, ECDS, MSDS and OP datasets)
e) Conducts full user and refresher training to support the capture and recording of good quality data, operational processes are reviewed and aligned to system functionality. Furthermore, system user training guides are regularly reviewed and updated
f) Complies with the data quality standards within the data security and protection toolkit
12. (a) The value and banding of the summary hospitallevel mortality indicator (‘SHMI’) for the Trust for the reporting period; and (b) The percentage of patient deaths with palliative care coded at either diagnosis or specialty level for the Trust for the reporting period.
17. Applies to Mental health Trust’s Applies to Ambulance Trust’s Applies to Ambulance Trust’s
Applies to Ambulance Trust’s
Applies to Mental health Trust’s
18. The Trust’s patient reported outcome measures (PROMs) scores for:
(i) groin hernia surgery
(ii) varicose vein surgery
(iii) hip replacement surgery and (iv) knee replacement surgery during the reporting period.
(a) SHMI banding published by Telstra in April 2025 covering the period November 2023 –October 2024 was 106.11 “within expected”
(b) From the Telstra mortality report the Trust Palliative care coding data was 2.08% (the national figure was 2.22%)
Not applicable to our Trust
Monitoring of PROMs for groin hernia and varicose vein surgery was paused in 2022, therefore no data is available
Latest data published was in February 2025 and covered the period 2023-24
EQ5D Index
Hip replacement: 76.41%
Knee replacement: 63.30%
EQ-VAS
Hip replacement: 75.93%
Knee replacement: 65.22%
National EQ5D Index
Hip replacement: 77.03%
Knee replacement: 73.36%
EQ-VAS
Hip replacement: 74.71%
Knee replacement: 72.84%
19. The percentage of patients aged:
(i) 0 to 15 years
(ii) 16 years and over
That were readmitted to the Trust within 28 days of being discharged from our hospital, that forms part of the same organisation during the reporting period.
20. The Trust’s responsiveness to the personal needs of its patients during the reporting period.
(i) Percentage of 0 to 15 years readmitted was 7.0%
(ii) 16 years and over readmission rate was 13.6%
21. The percentage of staff employed by, or under contract to, the Trust during the reporting period who would recommend the Trust as a provider of care to their family or friends.
22. Friends and Family Test – patient. The data made available by the National Health Service Trust or NHS Foundation Trust by NHS Digital for all acute providers of adult NHS funded care, covering services for inpatients and patients discharged from accident and emergency (types 1 and 2)
Please note: there is a not a statutory requirement to include this indicator in the Quality Accounts reporting, but provider organisations should consider doing so.
The Patient advice and Liaison service are our first contact and point of care resolution service. In year they received and responded to 4729 concerns.
This has increased by 7.2%, from 4410 in 2023-24 Increased by 51% from 3129 in 2020-21.
The Staff Survey 2024 results found that 46% of staff would be happy with the standard of care provided by the organisation if a friend/relative needed treatment.
The patient friends and family test results continued throughout 2024/2025. Our service users receive a link via text within 24 hours of being discharged or attending their appointment.
The Trust has seen an increase in responses received due to this new way of collecting data.
• Total annual FFT for 2024/2025 showed that 79% of 13,336 patients rated services as good or very good (up from 76% and 12,272 in 2023-24).
• Accident and Emergency were rated good and very good by 72.5% based on 6408 ratings.
• Hospital Inpatient services were rated good and very good by 80.6% based on 1480 ratings.
23. The percentage of patients who were admitted to hospital and who were risk assessed for venous thromboembolism during the reporting period.
24. The rate per 100,000 bed days of cases of C.difficile infection reported within the Trust amongst patients aged 2 or over during the reporting period.
25. The number and, where available, rate of patient safety incidents reported within the Trust during the reporting period, and the number and percentage of such patient safety incidents that resulted in severe harm or death.
26. Statement on seven-day hospital services
Data for the period 2024-25 was 67.85%
27.1 The number of its patients who have died during the reporting period, including a quarterly breakdown of the annual figure.
There were 42 hospital onset cases of Clostridium Difficile reported to the national surveillance database for period April 2024 to March 2025
Rate per 100,000 bed days is 24.21 (based on our own Trust data) as this information has not been published by UKHSA)
During the period April 2024 to March 2025 there was a total of 13815 incidents raised. From the 13,815 incidents 8650 were classed as patient incidents.
Validated harms:
Severe harm incidents: 19 (0.138%) Death incidents: 2 (0.014%)
The Trust is reviewing the workforce and service requirements across the 7-day week. This will identify where service gaps exist, whether there is a service need to operate across 7 days and the resources required.
This will feed into future business and service plans in line with the PAHT2030 strategy
From 1 April 2024 to 31 March 2025, 1052 of The Princess Alexandra Hospital NHS Trust patients died.
This comprised the following number of deaths each quarter:
Quarter 1: 249
Quarter 2: 233
Quarter 3: 263
Quarter 4: 307
27.2 The number of deaths included in item 27.1 which the provider has subjected to a case record review or an investigation to determine what problems (if any) there were in the care provided to the patient, including a quarterly breakdown of the annual figure.
In relation to 1052 deaths (item 27.1):
• 218 SJRs requested of 184 were completed. 34 of the SJRs still to be completed
• 26 incidents were raised on Datix for patients that died
• 20 are closed with two incidents confirmed as a death harm resulting from care or service delivery issues.
• 6 remain under investigation
Quarter 1:
• 36 case record reviewed
• 9 clinical incidents were raised:
• 1 concluded as moderate harm, 1 concluded minor harm, 4 concluded no harm
• 1 remains under investigation
• 2 concluded as death harms: PAWEB146737: was identified and reported in 2024 but related to care given in 2022. PAWEB147170
Quarter 2:
• 54 case record reviews,
• 6 incidents were raised:
• 1 concluded moderate harm
• 1 concluded minor
• 4 concluded no harm
• 0 remains under review
Quarter 3:
• 40 case record reviews
• 5 incidents were raised:
• 1 concluded moderate harm
• 1 concluded minor harm
• 2 concluded no harm
• 1 remain under review
Quarter 4:
• 54 case record reviews
• 6 incidents raised:
• 1 concluded minor harm
• 1 concluded no harm
• 4 remain under review
27.3 An estimate of the number of deaths during the reporting period included in item 27.2 for which a case record review or investigation has been carried out which the provider judges as a result of the review or investigation were more likely than not to have been due to problems in the care provided to the patient (including a quarterly breakdown), with an explanation of the methods used to assess this.
Of the 2024/25 completed case studies and incident investigations into patients who had died one was found to be a result of problems in the care provided to the patient.
In relation to each quarter, this consisted of Quarter 1: (April 2024 = 2)
1 sepsis (SI) PAweb146737
1 neonatal death (SI/MNSI) PAweb147170
Quarter 2: None
Quarter 3: None
Quarter 4: None
Cases referred for a structured judgment review (or called case record review) have data captured on Trust electronic system called SMART. All of these cases are rated with an avoidability rating of:
Score 1: Definitely avoidable
Score 2: Strong evidence of avoidability
Score 3: Probably avoidable (more then 50:50)
Score 4: Possibly avoidable, (less than 50:50)
Score 5: Slight evidence of avoidability
Score 6: No evidence of avoidability
All cases with an avoidability score of 1, 2 or 3 are followed up by:
• a review by the Trust’s learning from deaths panel
• are logged on Datix as a clinical incident and investigated through this process
• Reviewed by the Trust’s Incident Management Group – level of investigation decided.
• For discussion and learning at the specialty mortality and morbidity meeting
27.4 A summary of what the provider has learnt from case record reviews and investigations conducted in relation to the deaths identified in item 27.3.
Learning identified from completed case record reviews:
• Improvements required for earlier identification of DNACPR, TEP and end of life care completion.
• Improvements required with timely involvement of Specialist Palliative Care Team.
• Delays in responding to investigation outcomes.
• Improvements required with clinical documentation
• Develop CD competencies for our staff and not just focus on the current oral and IV ones
• Medication incidents have a robust feedback process in place and all incidents are reviewed with the EPMA team to see if new learning should be identified.
• To improve clinical documentation in order to better understand drug amendments for patients
• Provided support to nursing staff on escalation of medication concerns and the importance of the second checker role.
• Information provided to staff on the requirements of a positive incident reporting culture and importance of governance
• Cerner electronic prescribing systems have been reviewed with a view to providing an alert when controlled drug medications are amended. This supports support safe prescribing of controlled drugs.
• The importance of supervision and clinical reflection for clinical staff
Learning identified from the confirmed death harm incident investigations: (sepsis case 146737 and neonatal case 147170)
27.5 A description of the actions which the provider has taken in the reporting period, and proposes to take following the reporting period, in consequence of what the provider has learnt during the reporting period (see item 27.4).
The following actions from case reviews that continues to be embedded:
• Engagement with speciality Mortality and Morbidity (MandM) meetings have improved, allowing junior clinical staff to attend and present cases to senior clinicians. These meetings also involve teaching from senior/specialist clinicians/ teams on clinical care and treatment.
• Continued sharing the learning from case reviews at wider forums where clinical staff of all levels are invited.
• Extensive training for clinical staff on using ‘SMART’, the Trust mortality system used to undertake mortality reviews.
• Extensive work with the SMART team to improve the electronic SMART system to provide the Trust with information on mortality data and to store mortality reviews and minutes of MandM meetings
• A specific mortality form has been created on SMART for oncology and haematology teams to review patients who die within 30 days of receiving Speciality Anti-Cancer Therapy
• Clinical engagement at the deteriorating patient group to share and improve patient care across all specialities.
• Improvements continue with the Non-invasive ventilation service, including a new local process with cross speciality clinical engagement
• Monthly meetings are held to discuss the Trust’s mortality indices, in order to gain a greater understanding of the Trust’s mortality data and identify medical outlier groups, which are reviewed monthly, in order to identify care and treatment concerns or issues with coding.
• A sepsis and Acute Kidney Injury clinical lead has been recruited to ensure that patients are receiving correct and timely treatment via regular audits and provides training to clinical teams.
• The second level mortality panel has been revised, which now includes the compulsory attendance of the Medical director who chairs this meeting and has sight of all potential avoidable deaths with action plans.
• The CUSUM outlier alerts, identified by the Telstra system (which helps identify unusual patterns or changes to Trust data), are thoroughly reviewed for issues with care and treatment. The data is presented and discussed at the Sharing the Learning from Death Group, with actions plans developed where necessary.
27.6 An assessment of the impact of the actions described in item 27.5, which were taken by the provider during the reporting period.
The impact of the actions from reviews of cases are as follow:
• There is a greater understanding of inpatient deaths across all specialities due to dissemination of information across M and M’s and involvement from the multidisciplinary team
• Fewer incidents logged for delays of patients receiving endoscopies due to enhancement of that service
• Reduction of incidents logged due to in appropriate use of antibiotics due to the dissemination of the antimicrobial guidelines across numerous forums
• Relaunch of the Nasogastric tube (NG) placement check list, to follow the criteria for confirming placement and a legible signature
• NG feeding protocol was reviewed, amended and shared with clinical teams.
• Empower staff to escalate the need for extra support during periods of high acuity of care
• Teaching was undertaken on the importance of accurate interpretation of radiology images at M and M
• Further training provided to clinical staff on the diagnosis and risk factors of pulmonary embolism
• Learning was shared with clinical teams, regarding incomplete prescribing of protocols i.e. Venous thrombosis (VTE) and Acute Coronary Syndrome (ACS) to be escalated appropriately
• The Pulmonary Embolism (PE) policy was reviewed and amended to include additional information that verifies that a possible or probable PE will be treated until ruled out (risk versus benefit).
• Learning was shared with medical teams to ensure that blood tests are completed and results available in a timely way.
• Ensure the prescription bundles for ACS and PE include regular prescriptions of anticoagulation (in absence of contraindications or a bleeding risky manner
• Introduction of Electronic Health Records system at PAH has improved single access to clinical documentation to ensure that all clinical information can be found on one system while reviewing a patient, reducing the likelihood of missing important clinical data.
• Despite planning for industrial action, it was not possible to predict the volume of patients that may require unplanned attendance and the impact that this had on the appropriate clinical staff to patient ratio. This may have impacted the timeliness of patients being treated due to high volume of locum medical staff.
27.7 The number of case record reviews or investigations finished in this reporting period which related to deaths during the previous reporting period but were not included in item 27.2 in the relevant document for that previous reporting period (2022/23).
4 incident investigations were closed during 2024/25 relating to deaths and incidents raised in previous years:
• PAweb137585 – Unexpected death of a baby at 38 weeks. Death harm confirmed (approved in March 2025)
• PAweb142356 – Patient died of an untreated PE despite it being part of the differential and awaiting inpatient diagnostics – Death harm confirmed (approved in Nov 2024)
• PAweb142464 – Unexpected death of a baby – investigation completed by Maternity and newborn Safety Investigation team (MNSI) Death harm confirmed (approved in March 2025)
• PAweb146264 – Patient fed through Nasogastric tube which was in a lung resulting in death. (Never Event – closed in September 2024)
27.8 An estimate of the number of deaths included in item 27.7 which the provider judges as a result of the review or investigation were more likely than not to have been due to problems in the care provided to the patient, with an explanation of the methods used to assess this.
27.9 A revised estimate of the number of deaths during this reporting period stated in item 27.3, and for that previous reporting period, taking account of the deaths referred to in item 27.8.
4 as detailed in 27.8
2 cases in 2024/24 detailed in 27.3
4 cases detailed from before 1/4/2024 detailed in 27.8
Total of 6 identified in 2024/25
28. In response to the Gosport Independent Panel Report, provide details of ways in which staff can speak up (including how feedback is given to those who speak up) and how we ensure staff who speak up do not suffer detriment. This disclosure should explain the different ways in which staff can speak up if they have concerns over quality of care, patient safety or bullying and harassment.
There are a number of ways in which our people can speak up.
One of these may be via the Freedom to Speak up Service (F2SU).
This may be to raise concerns, about behaviours, patient or staff safety either as an individual or as a witness or to give suggestions for improvements.
There is a lead guardian who is clinical with a further two clinical guardians and two non-clinical guardians.
We have now trained a total 29 Freedom to Speak Up Ambassadors. Their role is to support staff to speak up, raise the profile of the service and be accessible to a wider range of staff. They come from a wide range of ethnic backgrounds and a variety of roles within the Trust.
We have a Freedom to Speak up vision and strategy and the vision states: “We are striving to ensure that our people feel enabled to speak up in order to support and improve patient safety and quality, the health and wellbeing of our people, and staff experiences”
A number of initiatives have continued raise the profile of speaking up. These include:
• Junior doctor drop-in sessions.
• FTSU newsletters
• Increasing number of ambassadors
• Presentations for all new staff
• Sessions on preceptorship
• Video on intranet of example of speaking up
• Attending wards/departments
• Posters with contact details
• Listening events
• Support at health and well-being events
The Guardians submit a quarterly report to the National Guardians Office detailing the numbers of referrals and themes.
A more detailed report is presented to the People Committee and the Trust board bi-annually. This shares numbers and themes of concerns raised to them but also the actions taken or required to happen to improve staff and patient experience and safety. The number of referrals continues to increase which is a good indication that more staff are feeling supported and safe to speak up.
29. Following the terms and conditions of service for NHS Doctors and dentists in training (England) 2016 requires a consolidated annual report on rota gaps and the plans to reduce rota gaps.
The Trust endeavours to triangulate all speaking up avenues and the lead guardian collaborates with a range of key individuals across the Trust to promote this.
Staff can also contact a range of people directly within the organisation who can sign post them for advice and support. These include:
• The people team
• Staff side
• Equality, Inclusion and Diversity Lead
• Line managers
• Tutors
• Organisational development team
• Staff Health and Well Being
• Mental Health First aiders
• Professional Nurse/Midwife Advocates
• Guardian for Safer Working
• Freedom to speak up ambassadors
Anyone who speaks up is always thanked for doing so. They are assured of confidentiality and encouraged to report immediately if they suffer any detriment from speaking up. This is taken very seriously and will be formally investigated. They are kept informed of progress of any actions taken to improve or resolve issues and asked to feedback on their experience.
An internal audit was undertaken to review the Freedom to Speak up service within the Trust in February 2024 and the findings were that the design of the service was green (substantial evidence) and design effectiveness was amber (moderate evidence). We will focus to ensure the evidence on the services effectiveness is also substantial.
Staff Surveys and regular Pulse surveys are undertaken to monitor impact of any changes made to improve experience and actions are monitored locally and centrally for themes and improvements.
The Trust did not complete a consolidated annual report on rota gaps for NHS doctors in training during 2024/25.

The Princess Alexandra Hospital NHS Trust, Hamstel Road, Harlow, Essex, CM20 1QX



01279 44 44 55 NHSHarlow @princessalexandranhs @PrincessAlexandraNHS The Princess Alexandra Hospital NHS Trust