FIGURE 8.0 | An illustration of the Cinchona plant, a natural source of the antimalarial drug quinine.

CHAPTER 8
FIGURE 8.0 | An illustration of the Cinchona plant, a natural source of the antimalarial drug quinine.

CHAPTER 8
Here are a few essential terms used in the science of therapeutics. By the end of this chapter, you should be able to apply these terms and understand how they relate to other critical concepts.
Antibiotics
Antifungals
Antimicrobials
Antiparasitics
Antivirals
Biologics
Curative Therapeutics
Mechanism of Action
Natural Products
Side Effects
Small Molecules
Symptomatic Therapeutics
Therapeutics
Humans have used therapeutics for as long as recorded time, and the past centuries have radically enhanced our approaches to developing them. Ancient cultures began using plants, such as willow bark, as medicines, and scientists later created compounds similar to these natural products. The discovery of the drugs quinine and later penicillin transformed the fight against infectious diseases. We have since developed additional approaches to identify and design therapeutics efficiently.
Therapeutics come in many forms and can be classified in a variety of ways. Some are found in nature whereas others are designed by researchers. Some are small molecules, while others are complex and mimic biological processes. Some cure the disease, while others treat the symptoms. In the setting of infectious disease, curative therapies can be further subdivided by the types (bacteria, fungi, parasites, viruses) and range (broad, narrow) of microbes they target.
Identifying and developing a new therapeutic drug and bringing it to the market is a long and iterative process. The process begins with researchers looking into existing drugs, and learning about the disease of interest to target microbes or symptoms, and/or carrying out large screens of potential compounds for new therapeutics to test. Once they have good leads, researchers perform experiments, proceeding carefully from the bench up to human volunteers. In the US, the Food and Drug Administration (FDA) ensures that the proposed drugs have been sufficiently proven to be safe and effective before approving them for human use. As you might imagine, the process of drug testing in humans has significant ethical considerations, and must be carefully handled. After a drug has been approved, there is still more work to be done to get it safely into the hands of sick people. The drug must still be rigorously manufactured and introduced into the market. The FDA decides when a therapeutic can go to market and continues to review the drug as it’s being used by the public.
There are many factors that must be considered in developing effective and safe drugs and getting them to people. As researchers develop drugs they aim to maximize effectiveness and reduce toxicity, and carefully assess these values to determine the dose of drug to recommend. Many things affect this value including how drugs are taken and how they interact with the body. Some drugs require a prescription, while others can be approved to be sold over-the-counter, like at a drugstore. Getting drugs to the hands of a consumer –prescription or not – is a challenging process, and not everybody is able to access them equally. Just as there are downsides to a lack of drugs, there are also downfalls to their overuse and misuse.


After reading this chapter, you will recognize the main types of therapeutics and their classifications. You will understand how therapeutic drugs are designed, developed, and ultimately introduced as the medications we use to improve human health. Finally, you will begin to appreciate the challenges and rewards that therapeutics bring and their global impact.
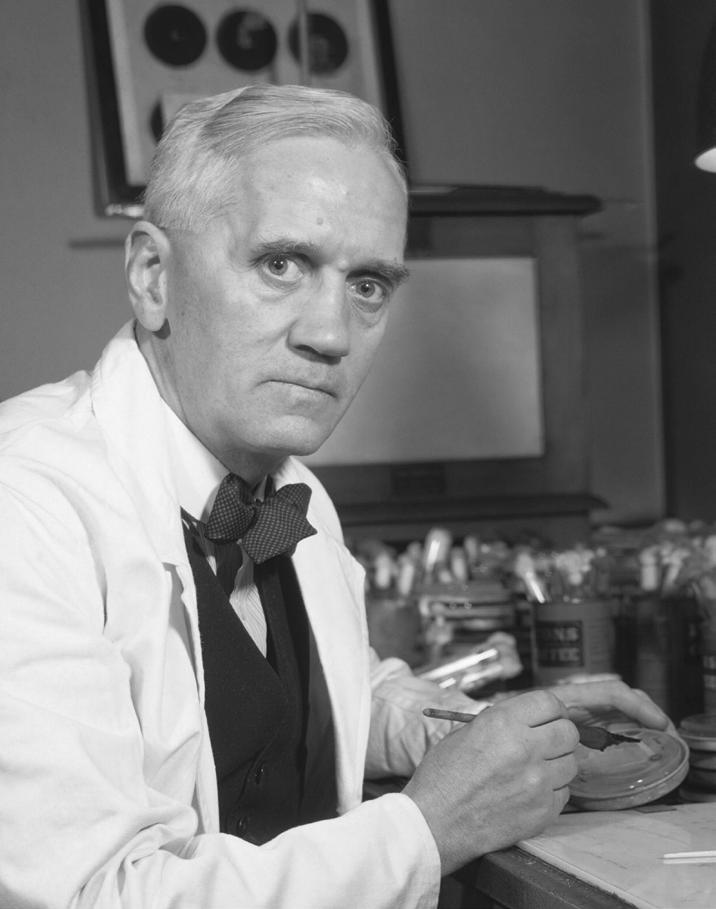
It is September 1928, and you’re rushing out of your lab to go on a much-needed holiday with your family. Scottish-born and educated, you’ve built a strong reputation for yourself as a microbiologist in the years since you moved to London and began working at St. Mary’s Hospital. By virtue of your unusually perceptive nature, as well as your somewhat busy workspace, you’ve made multiple important discoveries already, including systematically demonstrating that current treatments do not reduce the incidence of fatal infection after traumatic injuries observed during the Great War. You have also discovered a biological product, an enzyme, that kills certain bacteria, which you’ve termed a “lysozyme.”
At this point, no effective treatments for bacterial infections exist. The strategy physicians employ for a patient suffering from pneumonia, or even a basic infection resulting from a simple cut or scratch is a “wait and see” approach. You study the pathogens that cause many of these common infections in your lab,
“The trouble with being a hypochondriac these days is that antibiotics have cured all the good diseases.”
—Caskie Stinnett, American writer
including the bacteria Staphylococcus aureus (S. aureus) that causes sore throats and abscesses. Upon your post-vacation return to the lab, you realize that you left some staph-speckled Petri dishes out and uncleaned while you were gone.
As you begin to sort through the dirty dishes, one plate, in particular, draws your attention. Although this plate is dotted with bacterial colonies of S. aureus similar to the others, one detail stands out: a blob of mold with a distinct bacteria-free zone surrounding it. As you inspect the dish further, you notice a clear, gel-like secretion on the edges of the mold. This substance seems to have repelled the colonies or otherwise inhibited the growth of S. aureus.
Intrigued, you try to replicate the dish in your lab. As the bacterial colonies closest to this mystery mold continue to die, you work with your team to isolate the mold, growing larger samples of it for further testing. As you run more tests and experiments, your team examines whether the mold has the same effect on the bacteria responsible for infectious diseases like gonorrhea, meningitis, pneumonia, and scarlet fever, and you’re met with success in each case. You conclude that the isolated secretion is an effective agent to kill bacterial pathogens, and based on the fungi’s scientific name – Penicillium rubens – you decide to name your newfound agent that could miraculously kill bacteria “penicillin.”
As with most scientific progress, many more individuals and a considerable amount of work is needed to reach the full potential of this amazing compound that you’ve found. A team of women known collectively as “The Penicillin Girls” (Figure 8.1b) work diligently to “farm” the penicillium mold in order to produce penicillin in your lab, managing over 700 cartons of “mold juice,” as well as synthesizing and purifying large amounts of the antibiotic for continued study – a key contribution to the research as a whole.
The Penicillin Girls – Ruth Callow, Betty Cooke, Peggy Gardner, Claire Inayat, Megan Lancaster, and Patricia McKegney – are able to test penicillin’s effects on other organisms, including mice and even a few human patients, to see whether it is effective against a number of diseases. They also work to determine how much medication the patients need to take in order for it to be effective but not harmful. It’s hard work, but these efforts help facilitate a life-saving breakthrough. Several other advancements, led by your colleagues and supporters, pave the way for penicillin to become a safe and effective therapeutic. As World War I begins, manufacturers begin to ramp up production of
penicillin, rightly recognizing the value it would have on the war front.
You are Alexander Fleming, and you later explain this “triumph of accident, fortunate occurrence” and say, “When I woke up just after dawn on September 28, 1928, I certainly didn’t plan to revolutionize all medicine by discovering the world’s first antibiotic, or bacteria killer. But I suppose that was exactly what I did” (Figure 8.1a). Decades later, penicillin is still used to treat illnesses like meningitis, gonorrhea, and sepsis – the very diseases your purified mold samples were first tested against. Your remarkable impact is still felt around the world today, preventing millions from dying of these now-curable illnesses.
Fleming had a number of other colleagues that helped develop penicillin as we know it; Dorothy Hodgkin, a British chemist, confirmed penicillin’s structure via x-ray crystallography; Australian pharmacologist and pathologist Howard Walter Florey and German-born British biochemist Ernst Boris Chain led a team to help manufacture the new drug. Together, Fleming, Florey and Chain were awarded the 1945 Nobel Prize in Physiology or Medicine “for the discovery of penicillin and its curative effect in various infectious diseases.” Hodgkin received a Nobel Prize later in 1964 for her work in the determination of the molecular structure of penicillin and other substances.
You interact with therapeutics every day. When you get a bacterial infection, your doctor prescribes antibiotics. When you get cramps or a headache, you visit the pharmacy to purchase pain medication. But what exactly

are therapeutics? Where do these therapeutics come from? What exactly do they do in our bodies? Why don’t we have a treatment for every known illness? As we dive into the world of therapeutics, we will answer these questions, among others.
Therapeutics are therapies or treatments that have healing or health-improving qualities. The word originates from the Greek word therapeia, which means “a service given to another.”
Therapeutics (used interchangeably with therapies and treatments) support your health in many ways. Some, like penicillin, can kill an invading pathogen. Others tone down your own immune response. Some therapeutics are medical devices such as ventilators, which are machines that help patients breathe mechanically. In some cases, even rest can be considered therapeutic.
We’ll spend most of this chapter learning about therapeutic drugs, a substance or medication that is used to treat, prevent, manage, or cure a disease or medical condition. Note, that while
the terms drug and medication are often used interchangeably, not all drugs are medications – administered with the intention to treat or prevent a disease. Some, for example, can be recreational or performance enhancing. In this chapter, we will use the term drugs to mean therapeutic drugs, the ones you have probably taken as medication when you were feeling sick or diagnosed with an infection to either fight the pathogen or treat symptoms. Through this chapter, you will learn about a variety of therapeutic drugs: how they are classified, how they work, and how they are designed, developed, and distributed.
Therapeutics have been used for thousands of years to cure and prevent disease. Like penicillin, many early therapeutics derived from the natural world, often from plants. One such example can be found in ancient Assyrian and Egyptian texts, which reference concoctions made from willow bark and
leaves that were used to treat a wide variety of conditions, including fever and insect bites, as early as 3500 BCE. Hundreds of years later, in the 19th century, scientists identified the reason why the treatment was effective: a molecule called salicin. Since it is naturally occurring, salicin belongs to a class of therapeutics called natural products. Salicin was eventually structurally modified to create acetylsalicylic acid, the active ingredient of aspirin (Figure 8.2). Because aspirin is a molecule that is chemically similar to and derived from the structure of another (salicin), it is described as an analog of salicin. Aspirin is one of many successful modern drugs derived from a natural product.
Much like penicillin, another one of the world’s most powerful drugs was also discovered through a happy accident. As you may remember from Chapter 5: Biology of Infectious Agents, the compound called quinine, another natural product, found in the bark of the cinchona tree was widely used to treat malaria in the 1600s. The legend has it that this chemical compound was identified as a potential malaria remedy hundreds of years ago, when a feverish man drank from stagnant water near cinchona trees near the Andes Mountains of South America. The man assumed he was poisoned by the bitter-tasting water until his fever eventually subsided. He shared his accidental discovery with local villagers, who began using cinchona bark extracts to treat fevers. This technique eventually spread to Europe, where it was used to fight malaria. Prior to 1820, the primary treatment for malaria was ground-up cinchona bark mixed with a liquid and taken orally.
Over the next century, quinine was extracted from the bark and then isolated and purified. This isolate became the main treatment
for malaria, even though its mechanism of action, or the way that a therapeutic works and confers its benefit, was not well understood at the time. The demand for quinine, however, far exceeded the ability to produce quinine in nature, and the drug had severe side effects, which are secondary, typically unwanted adverse (negative) effects of a drug or medical treatment.. In 1934, Hans Andersag and his team in Germany, used their knowledge of quinine and its structure to create chloroquine that was safer and could be mass produced. Note that while the two drugs are structurally similar, chloroquine is not considered an analog, because its structure was not directly derived as a modification of quinine. Chloroquine became the primary antimalarial drug from the time of its approval until relatively recently, with the emergence of chloroquine resistance, a phenomenon where a given drug is no longer effective against its specific pathogen due to changes in the pathogen over time. Drug resistance will pop up a few more times in this chapter, and will have its own chapter later in the book, Chapter 14: Pathogen Evolution and Drug Resistance.

The naturally-occuring salicin was eventually structurally modified to be acetylsalicylic acid, the primary ingredient in aspirin.
To understand how drugs work, we must think about their targets, which are the structures or processes that the drug alters to exert its effect. As we discussed in Chapter 5: Biology of Infectious Agents, microbial cells have many features that differentiate them from human cells. These unique features make excellent therapeutic targets, as action against them will only affect the pathogen, not the host’s cell. For example, penicillin specifically targets transpeptidase, a key enzyme involved in the formation of the bacterial cell wall, and irreversibly alters it, killing the bacteria. Transpeptidase is not found in human cells; this means that disabling transpeptidase will kill the bacteria but won’t be able to have a direct effect on the human host cells.
Paul Ehrlich, a German physician, was among the first cohort of scientists to develop systematic methods to identify pathogen targets. Ehrlich and his peers used strategies from the clothing dye industry – a significant area of chemical advancement during this era – to identify dyes that could stain specific pathogenic cells in a way that would differentiate them from the cells of the host (Figure 8.3). Ehrlich reasoned that there was an affinity between certain biological structures in the bacterial cells and the structure of the dye. He extrapolated this logic to predict that if certain chemicals could preferentially bind to the bacteria, then products could be identified that would bind to and potentially kill a specific target microorganism – a revolutionary concept at the time. By identifying specific drug targets and attacking them, researchers could combat disease with groundbreaking precision and efficiency.
Ehrlich identified drug targets by synthesizing a huge pool of related molecules and then testing them all on a single pathogen: syphilis. His work
laid the foundation for high-throughput drug discovery processes of molecular screening, and yielded one molecule that could kill the syphilitic bacteria. Called compound 606, it was widely disseminated under the name Salvarsan and even lauded as a ‘magic bullet’ for syphilis. Salvarsan and penicillin are examples of antibiotics: drugs that target bacteria. Antibiotics are a subset of antimicrobials, which are any drugs that can kill an invading pathogen. We continue to benefit from these discoveries today.
Salvarsan was revered for its power to alleviate the severity of syphilis, but it had many drawbacks as well; it had dangerous side effects, including nausea, vomiting, and even deafness. Some of these stemmed from errors in drug administration, which we will discuss in more detail later in this chapter, rather than drug composition, but the fact remains that the compound was not well understood when it was initially put on the market. Faced with the drug’s immense side effects soon after its release, Ehrlich stated that

FIGURE 8.3 | The use of dyes to stain microorganisms revealed new ways to target microbes. Paul Ehrlich is recognized for his research in the application of dyes to stain cells and target pathogens. Here we show a human cell and bacteria stained with the Methylene blue dye, a dye Ehrlich tested on malaria in pursuit of potential drugs.





























FIGURE 8.4 | Rational drug design. This method involves three main steps for designing and developing novel curative therapeutics. 1. Researchers study the biology of a pathogen. 2. Upon understanding the pathogen and the way it causes disease, scientists design a drug that will target a specific structure or function of the disease-causing pathogen.
3. Experiments are run to test the novel therapeutic.
“the step from the laboratory to the patient’s bedside ... is extraordinarily arduous and fraught with danger.” Today, modern drug discovery methods still employ some aspects of the original strategies used to develop therapeutics such as Salvarsan. However, researchers also utilize more recent chemical, biological, and computational advancements and support their work with more time and effort. The goal of this process is to maximize efficacy – also referred to as its effectiveness – which is the clinical benefit of the drug in treating the disease of interest, while minimizing adverse effects on the patient. We will discuss the clinical development of therapeutics in more depth in section 8.3: Drug Discovery, Development, and Approval.
Before the 20th century, drug discovery relied primarily on discovering a natural product through chance or broad experimentation. This changed when work began towards developing
the first antivirals – therapeutics that disrupt viral infections. To develop new antiviral drugs, American physician George Hitchings and American chemist Gertrude Elion introduced a new approach of rational drug design, in which scientists carefully study the biology of a pathogen – its structures, how it infects cells, how it spreads, and more – and use these insights to design curative therapeutics (Figure 8.4). By studying the structure and function of potential drug targets, Hitchings and Elion were able to design and test the antiviral properties of many nucleoside analogs
Nucleoside analogs are molecules that mimic the nucleotide building blocks of DNA and RNA. They structurally resemble a specific nucleoside – such as guanosine – but have structural differences that make it impossible to add another base after the analog has been
FIGURE 8.5 | Nucleoside analogs and molecular screening for drug discovery. Acyclovir, structurally resembles the natural genetic molecule guanosine. Using rational drug design, scientists can produce molecules that mimic certain building blocks of DNA and RNA, but have been engineered to have therapeutic benefit.
incorporated into the chain (Figure 8.5). This has tremendous therapeutic benefits during viral infections, where the virus is rapidly replicating within the host cells. After they are taken in the form of a drug and introduced to the host cells, the analogs halt the replication of any genome they’re incorporated into; this will disproportionately affect viral replication over host cell replication because of how much more rapidly viral replication takes up nucleosides.
This process underlies the drug acyclovir, an antiviral developed by Gertrude Elion. She and her team found that acyclovir could specifically halt the progress of herpesvirus infection as well as treat other viral infections such as chickenpox. In addition to earning her a Nobel Prize in Physiology or Medicine, this landmark discovery and the drug design strategy behind it opened the door for many of the antivirals we use today.
1. How do therapeutics relate to treatments, therapies, and drugs?
2. What are we referring to when we talk about “the target” of a drug?
3. Physicians stopped using compound 606 or Salvarsan to treat syphilis in the 1940s. Why was Salvarsan discontinued for medical use?
Therapeutics can be classified in different ways based on how they are produced (natural, semi-synthetic, and synthetic), their underlying composition (small molecule, biologic, natural biological therapy), and the range (narrow, broad) and type of pathogens (bacteria, parasite, fungus, virus) they target
Quinine has only ever been produced by extracting the compound from the bark of the cinchona tree. That is, it has always been a natural product, or natural drug. Penicillin, on the other hand, started out as a natural drug, but now has a more commonly-prescribed analog.
The original penicillin – a natural drug derived from mold – is still in rare use, and is called Penicillin G, which is directly injected into the patient’s bloodstream. However, when your doctor prescribes you “penicillin” as a pill, you are actually getting Penicillin V, an analog drug developed by modifying the basic structure of penicillin to make it more resistant to stomach acid and, therefore, more effective when taken orally. When natural compounds like penicillin are modified in the lab to improve their efficacy or allow for their mass production, these analogs are also classified as semisynthetic drugs. Other penicillin analogs and semi-synthetic drugs include amoxicillin and ampicillin. Like these, aspirin is an analog and semi-synthetic drug. While the terms are often used interchangeably, semi-synthetic drugs differ from analogs in that analogs do not necessarily have to be derived from a natural product, and semi-synthetic drugs do not have
to remain quite as structurally similar to their natural product as analogs would.
Chloroquine is considered a synthetic drug because (while related to quinine) it is entirely produced in a lab and wasn’t derived directly from a natural substance. Synthetic drugs can also spur their own analogs. For example, hydroxychloroquine involves a simple addition of a hydroxyl (-OH) group to chloroquine. Hydroxychloroquine, which has fewer side effects than chloroquine, is also used to treat malaria and certain autoimmune conditions like rheumatoid arthritis and lupus.
There are yet another group of drugs that exactly match something found in nature, but are created in the laboratory. They are neither natural, semi-synthetic, or synthetic, and are instead said to be created by biotechnology – the application of biological processes, organisms, or systems to develop functional products. As we will see shortly, many biologics fit within this category.
As their name aptly describes, small molecules are drugs categorized by their small size and weight; some small molecule drugs are so small that they are composed of only 20 atoms. Small but mighty, they are quite diverse in their ability to control biological processes through different mechanisms of action. Examples of small molecule drugs include quinine and chloroquine, acetylsalicylic acid, salvarsan, and penicillin, which you learned about in the beginning of this chapter. As you will likely notice across this chapter, the vast majority of current drugs are classified as small molecules. However, this is expected to change as we are able to develop increasingly sophisticated drug targeting approaches.
Biologics are typically large and complex drugs derived from living organisms, such as genes, proteins, or cells, and are designed to provide a therapeutic benefit, frequently using biotechnology methods. For example, insulin, the drug most people take to treat diabetes, is a protein-based hormone. At one point, it was a natural drug, back when the hormone was extracted from pigs and cows for use in humans. Now, it is made using recombinant DNA technology, a form of genetic engineering in which two portions of genetic material are combined to introduce a new function in a biological system (Figure 8.6). In the case of insulin, bacterial or yeast cells are engineered, via recombinant DNA technology, to produce the human hormone, allowing for more efficient production and collection. This form of insulin is a biologic, created by biotechnology, and is neither natural, semisynthetic, or synthetic since it exactly matches the human gene sequence but it was not produced naturally.




There are a number of biologics that are used to treat infectious diseases. Let’s learn about a few examples. To do so, it helps to first consider the natural biological process they are mimicking.
As you might recall from Chapter 6: Immune System and Host Defenses, antibodies are the key molecules of your adaptive immune system, and mark foreign bodies for elimination by other parts of the immune system. As the body learns about an invading pathogen, it produces and then releases pathogen-specific antibodies that bind to the infectious agent. This process is known as active immunity, which is achieved when the antibodies are developed in a person’s own immune system. In contrast, passive immunity is achieved when a person receives antibodies that were produced by another individual (for example from mother to baby via breast milk).
We can use naturally produced antibodies as a form of therapy called antibody therapy, to give patients passive immunity to a disease. Specifically, we use convalescent plasma, plasma from people who have survived a specific disease, which harbors antibodies. The general process








FIGURE 8.6 | Recombinant DNA technology. A bacterial cell is modified genetically to introduce a new function such as the production of insulin, a biological therapeutic. 1. The first step in recombinant DNA technology is the extraction of the plasmid DNA of a bacteria. 2. The DNA containing the information for a new function (DNA of interest) is inserted into the plasmid of the bacteria creating “recombinant DNA”. 3. The recombinant DNA is introduced into bacterial cells. 4. Bacteria divide creating multiple copies of the recombinant plasmid.
8.7 | Convalescent plasma therapy. Antibodies in recovered individuals help fight the same disease in sick patients. Antibodies in the plasma of the disease survivor may be transfused into an actively ill patient to support the recipient while they fight the infection or may be used to help prevent infection in somebody who has recently been exposed to the pathogen, but isn’t ill yet.
of convalescent plasma therapy is illustrated in Figure 8.7. It starts with a patient who has survived the infectious disease of interest, in this case, COVID-19. As you might also remember from Chapter 6: Immune System and Host Defense, antibodies to a given disease remain in the survivor’s plasma, a component of the blood. After infection, researchers can collect the recovered patient’s plasma, and then transfuse (slowly inject) it into patients who are infected with the same pathogen. This gives the newly-infected patients a head start on fighting off their infections by boosting their adaptive immune system until they are able to make their own antibodies. This approach has also been used as a preventive measure by transfusing the plasma into individuals who were not yet ill, but typically had been exposed to a pathogen, or were at a high risk of becoming infected. Though quite rudimentary and logistically challenging, this approach has been used to treat several diseases, such as Ebola and COVID-19, for which it was given rapid authorization for use by the FDA given the lack of other available treatments at the time
of significant need. We’ll discuss how drugs are approved in more detail later in section 8.4: Considerations for Therapeutic Administration and Distribution.
The early successes of convalescent therapies led to the development of biologics, antibodybased therapies in the laboratory. One of these biologics is monoclonal antibodies, which are antibodies that have been generated to be identical, and recognize a desired antigen e.g. SARS-CoV-2 spike protein (Figure 8.8). The term “monoclonal”, can be broken down into mono which means “one”, and clonal which means “created by asexual reproduction”. The application of monoclonal antibodies has emerged as a promising approach to treat infection by mimicking our immune response. Isolated from mice after their exposure to the pathogen or developed with specialized cellular systems, monoclonal antibodies are categorized as biologics due to the fact that they mimic a biological process. Since these therapeutics support the immune system, they are useful in many fields, including cancer and
Receptors

FIGURE 8.8 | Anti-SARS-CoV-2 monoclonal antibodies. Monoclonal antibodies bind to viral SARS-CoV-2 spike protein to prevent binding between it and the human cell receptor, (ideally) blocking infection. This is an example of a biologic.
hurdles for its effective use as an antimicrobial therapeutic in humans that must first be addressed; research in this field is ongoing.
Other new biologic approaches targeting a microbe’s genome have shown promise for treating infectious disease. Although they are still relatively new, genome-targeting therapies have received major attention in recent years due to abilities to select and customize microbial genomes to target. Two such examples are CRISPR and RNA interference (RNAi).
As we learned in Chapter 4: Fundamentals of Genetics, different organism cells have varied means to regulate gene expression. One such method, first discovered in plants and then observed in the helminth Caenorhabditis elegans (C. elegans), is RNAi. During this process, small interfering RNAs (siRNAs) identify specific mRNA sequences which are then cleaved and degraded, preventing their translation. As a result, protein expression is reduced or silenced. The discovery of RNAi led to a Nobel Prize in Physiology or Medicine for American scientists Andrew Fire and Craig Mello in 2006. The biomedical potential of silencing genes as a therapeutic approach was highlighted soon after, and has now been applied to develop antivirals and other therapeutics. The technology is still nascent, but you can imagine how silencing a pathogen’s genes could have great therapeutic potential.
As we discussed in Chapter 7: Diagnostic Tests, CRISPR, one of the most prominent biological technologies, was originally discovered to be E. coli’s natural defense mechanism against invading viruses. It allows bacteria to scan for circulating viral genomes, and then it creates a precise cut in the viral genome sequence to disable it. Due to this highly targeted editing ability, CRISPR, the so-called “molecular scissors,” is also of great interest as a potential antimicrobial therapy. Early observations of CRISPR’s efficacy show significant promise for targeting many viruses, including hepatitis B, HIV, influenza, and SARS-CoV-2. However, there are a number of potentially insurmountable
There are a number of other therapeutics that, like biologics, are typically large and complex and derived from living organisms, but are fully natural products. They are thus biological therapeutics, but are not defined as biologics. Convalescent plasma is one such natural biological therapy, which was initially given naturally, and then used as the basis for biologics.
Another natural biological therapeutic are the probiotics, live microorganisms that help to maintain the health of the human microbiome. As you may remember from Chapter 5: Biology of Infectious Agents, the microbiome is the ecosystem of microorganisms living on and in each person that help regulate the immune autoimmune disease treatment; this highlights how important a balanced immune system is to your overall health, beyond just protection against infectious disease.
system and digestion, and keep harmful bacteria in check. The antibiotics that we use to treat bacterial infections cannot distinguish between the harmful pathogenic bacteria and the ones that make our microbiome and that live in our bodies; so they can also take out parts or much of our microbiome. There is then a need to replenish the body’s microbiome. One way to do this is through ingesting beneficial, live microorganisms in the form of probiotics during and after taking the course of antibiotics.
In extreme scenarios, after a course of antibiotics has wiped out other bacteria in the gut, opportunistic “bad actors” like the anaerobic bacteria Clostridium difficile (C. difficile) can multiply and overwhelm the system. C. difficile infection shows up as frequent, watery diarrhea (up to 15 times per day), that can cause significant dehydration, and can be a life-threatening disease and it also causes colitis (an inflammation of the colon). While initial treatment of C. difficile infections involves antibiotics, there is a unique treatment when all else fails: fecal microbiota transplantation (FMT). FMT is the transplantation of fecal material (i.e., a poop transplant) from a healthy individual to an ill patient either via colonoscopy (which is a tube
that goes in the anus and can be advanced through the colon), or via a tube through the sick patient’s nose (less common route) (Figure 8.9). Impressively, this unconventional therapy has shown great success in restoring the balance of gut microbiota in C. difficile patients. FMT’s efficacy lies in the fact that it transplants a healthy gut microbiome back into the ill patient. The ideal donor would either live with or have similar eating and drinking habits to the recipient in order to make their microbiomes as close a match as possible.
And while you may not always think about them this way, the foods that you eat can also be biologically-based and natural therapeutics. For example, you might not be surprised to learn that malnutrition is associated with an increased risk of infection of a number of diseases (although this correlation might be influenced by other factors – like socioeconomic factors and housing options) and that during a flu infection, you should drink lots of fluids and consume sugars and electrolytes in healthy forms. However, you might be interested to learn that foods like poultry, whole grains, ginger, cinnamon, and turmeric have also been found to confer moderate anti-inflammatory effects.
An intriguing study by Andrew Wang and Ruslan Medzhitov, researchers at Yale University, and colleagues compared the effects of fasting (i.e., no food intake) and food supplementation on the inflammatory response in bacterial and viral infections in mice. They found that fasting was protective to the mice’s survival in bacterial but not viral infections. They also demonstrated the converse: that nutritional supplementation, particularly with sugar, decreased mice’s survival in bacterial infections but was protective in viral infections. This study may form the basis of the centuries old adage “feed a cold, starve a fever” since most colds are caused by viruses. However, since both bacteria and viruses can cause either, we can not use it alone, and it is a reminder of why we need better diagnostics, to know for sure what pathogen we are fending off and how to respond. In the meantime, it is generally wise to try to take in healthy foods either way, and to avoid processed sugar.
The study had an additional intriguing finding. There is an inhibitor found in avocados called D-mannoheptulose that inhibits glucose metabolism in mammalian cells. This inhibitor mimics the effects of fasting, which, as the study shows, is protective during bacterial infections, meaning that avocado intake might be beneficial in the setting of bacterial illness, and still provide nutritional supplementation that could be beneficial in viral infections. However this has not been assessed in humans, and it is important to consult with healthcare professionals before making drastic dietary changes, especially when you are ill. That said, including avocados in our diets in moderation seems to be a healthy choice, regardless (Figure 8.10).
We can also characterize therapeutics as curative or symptomatic. Curative





FIGURE 8.10 | Components of common foods can affect pathogen metabolism. D-mannoheptulose, a natural glycolysis inhibitor found in avocado, has been shown to inhibit glucose metabolism in mammalian cells. This inhibitor may mimic the effects of fasting; this could have the potential to improve infection outcomes, as fasting can improve mouse survival of bacterial infections. However, this has not been demonstrated in humans.
therapeutics eliminate infection by knocking down or killing off the pathogen of interest. Symptomatic therapeutics alleviate the associated symptoms to support infected individuals while they fend off the pathogen.
Antimicrobials are curative therapies, as they neutralize or kill off the offending pathogen. They can either target a broad variety of pathogens,

Scan this QR code or click on this link to watch the video abstract of a study showing how food affects mice’s ability to fight off bacterial and viral infections.
or a very narrow set of pathogens, which we describe as their spectrum of target pathogens.
Broad spectrum antimicrobials are effective against many different species of a given type of microbe, i.e., multiple species of bacteria. Typically they work against organisms that all have some structural similarity, like a similar cell wall or other cellular components. Broad spectrum antimicrobials are particularly useful when multiple organisms are suspected to be causing the infection, which is typically the case for wounds on people’s feet, or when multiple organisms are on the differential diagnosis, as in many early infectious disease cases. However, since they wipe out so many different organisms, they can damage the patient’s microbiome, and they run a greater risk of creating antimicrobial-resistant organisms.
On the other hand, narrow spectrum antimicrobials are effective only against one or a few groups of organisms. As a result, you have to be more sure about what specifically you’re treating before you start them, another example of the important role diagnostic tests can play. Narrow spectrum antimicrobials don’t pose as much of a risk to the microbiome, nor of developing resistance – although both of these risks are always present with all antimicrobials.
Curative therapeutic drugs are then typically subdivided by the type of pathogen that they are designed to combat. They can target bacteria, parasites, fungi, or viruses; occasionally, some may have effects on multiple different types of pathogens. Let’s
dive into these different classes of curative antimicrobial drugs. For each, we will describe them, and give some examples.
Antibiotics, also known as antibacterials, are a key group of antimicrobial drugs that target bacteria. They are the most researched and most diverse set of drugs that we have to treat infectious disease as a whole. Since the discovery of penicillin, scientists have identified many different antibiotics; this is likely due to the fact that bacterial cells have many unique features, including cell walls, specialized enzymes, distinct structural proteins, and their own cellular machinery, distinct from their human hosts. You have likely taken antibiotics at some point in your life, perhaps to treat an ear infection, strep throat, or urinary tract infection. There are many varieties of antibiotics, with varying mechanisms of action, bacterial targets, and uses, which leads to a number of different ways to classify antibiotics.
Antibiotics can target bacterial cells in a variety of ways, including inhibiting cell wall synthesis, disrupting cell membrane function, inhibiting protein synthesis, inhibiting nucleic acid synthesis, and blocking metabolic pathways. They can either be bactericidal, outright killing the bacteria, or be bacteriostatic, interfering with cellular processes to stop bacterial growth, and buying the body more time to mount its immune defenses (Figure 8.11).
There are also different “classes” of antibiotics, grouped around their structure and/or mechanism of action. Let’s take penicillin for an example. Penicillin is a narrow spectrum small molecule, and the first member of an antibiotic class called beta-lactams. Beta-lactams received their name because they contain
DISRUPTS CELL WALL SYNTHESIS Penicillin
INHIBITS TRANSCRIPTION
INHIBITS PROTEIN SYNTHESIS
INHIBITS DNA REPLICATION
Ciprofloxacin
FIGURE 8.11 | Bacterial cell targets of antibiotics. Antibiotics target bacterial cells in four main ways: disrupting cell wall synthesis, and inhibiting DNA synthesis, transcription or protein synthesis. They can either kill the bacteria (bactericidal) or stop its growth (bacteriostatic).
what is known as a “beta-lactam ring” in their molecular structure. Beta-lactam drugs work by binding to proteins that inhibit synthesis of the bacterial cell wall and activate autolytic, or self-destructive, enzymes. The combination of inhibition and activation ultimately leads to lysis of the cell wall and destruction of the bacterial cell, making beta-lactams bactericidal. As you already know, penicillin was discovered in nature, and is frequently used to treat strep throat, various skin infections, and syphilis.
Ciprofloxacin is a broad-spectrum small molecule member of the antibiotic class known as fluoroquinolones. It functions by inhibiting bacterial DNA replication and is classified as bactericidal. It was discovered via molecular screening, and is used to treat bacterial conjunctivitis (also known as pink eye) as well as some urinary tract infections.
Doxycycline is a broad-spectrum, small molecule antibacterial that belongs to a drug class called the tetracyclines. It functions by inhibiting protein synthesis and is bacteriostatic.
It was discovered via semi-synthetic drug design. It is used to treat early Lyme disease, among other tick-borne diseases. Doxycycline can also be used to treat acne, which is caused by a bacterial infection of oil-secreting glands in the skin. Interestingly, it has also found use in preventing malaria. This shows that drug classifications are not set in stone.
Rifampin is a broad spectrum, small molecule antibiotic that belongs to a class known as macrolactams. It functions by inhibiting enzymes crucial to RNA synthesis, i.e. inhibiting transcription, and is bactericidal. It was developed as a semi-synthetic drug. It is used in combination with other antibiotics to treat tuberculosis and leprosy.
Antifungals, also known as antimycotics, fight off fungal infections, as the name suggests. They have become increasingly important with the rising prevalence of life-threatening
fungal infections, like aspergillosis, which most commonly affects the lungs and organs received by transplant. Antifungals are also important topical treatments for vaginal yeast infections and fungal skin infections, such as athlete’s foot and ringworm.
Most antifungals work by targeting some part of the fungal cell envelope, which consists of the inner cell membrane and the outer cell wall. As you might remember from Chapter 5: Biology of Infectious Agents, fungi are eukaryotic, like human cells, meaning that they have several cellular structure features in common (such as nuclei, various enzymes, and other pieces of crucial cellular machinery). As a result, targeting these features on fungal cells will affect human cells as well; this makes these shared characteristics imperfect drug targets. While most existing therapies have these suboptimal targets, it’s an exciting and active area of research, and other targets are currently being researched, including fungal metabolic pathways, and gene expression.
There are different groups of antifungals, classified by various mechanisms of action, uses, chemical structure, and or side effects. They generally work by disrupting membrane function, or synthesis of the cell wall, nucleic acids, or ergosterol – a compound that is required for the structure of the cell membrane. They are also divided into polyenes, azoles, echinocandins, and pyrimidine analogues. We provide more details about two of them, amphotericin B and fluconazole below.
Amphotericin B is a broad spectrum small molecule member of the polyene class of antifungals. It specifically targets ergosterol, which is the fungal equivalent of cholesterol. Upon binding to ergosterol, which is found throughout the fungal cell membrane, amphotericin B causes pores or holes to
form in the membrane, thereby destroying its integrity. It was discovered via molecular screening. It’s a particularly potent antifungal, however, this potency can also inflict collateral damage to human cells given the structural similarities between ergosterol and cholesterol, giving rise to its nickname “amphoterrible” within the clinical community. As a result, it is recommended only in the case of serious fungal infections.
Fluconazole is a small molecule, broad spectrum antifungal, and belongs to the class of drugs called triazoles. Fluconazole works by inhibiting an enzyme required for the production of ergosterol, thereby damaging the fungal membrane. It was discovered through rational drug design, and can be used for vaginal yeast infections, as well as to avoid fungal infection in those receiving chemotherapy.
Illustrated in figure 8.12 we present some of these antifungal drugs, organized by the cellular processes or components they act upon.


















F IGURE 8.12 | Fungal cell targets of antifungals. Antifungal therapeutics have multiple potentialfungal targets, including disrupting membrane function, or synthesis of the cell wall, nucleic acids, or ergosterol – a compound that is required for the structure of the cell membrane.
Interestingly, some antifungals have been found to have broader applications than just fungal infections. For example, certain antifungals target enzymes called cytochrome P450s, which are involved in fungal biosynthesis. These antifungals with activity against cytochrome P450s have also been effective in treating the bacterial infection tuberculosis (TB), as the bacteria causing TB, Mycobacterium tuberculosis, contains a very large number of the cytochrome P450 enzymes. So this antifungal has uses beyond its name. This again shows that drug classifications are not set in stone and that a drug’s function against different organisms is dependent on its target.
Antiparasitics are a group of antimicrobials used to treat parasites, such as protozoa and helminths. The mechanism of action for these














FIGURE 8.13 | Parasitic cell targets of antiparasitics. Antiparasitics have a wide range of activities given the diversity of organisms that they defend against. They typically have four main mechanisms of action: disrupting cell wall permeability, disrupting nutrient transport within the cell, inhibiting DNA synthesis, and inhibiting protein synthesis.
drugs varies dramatically, as they target cellular components in a wide variety of organisms. However, they have four main mechanisms of action: disrupting cell wall permeability, disrupting nutrient transport within the cell, inhibiting DNA synthesis, and inhibiting protein synthesis. Figure 8.13 shows four antiparasitic agents, as well as the cellular processes or components that they act upon. We provide more details about two of them, chloroquine and atovaquone-proguanil below.
You already learned about the antiparasitic chloroquine, which is a broad spectrum small molecule in the aminoquinoline class. It prevents the clearance of toxic compounds from the parasite’s body, eventually killing the parasite. As you already know, it is a semi-synthetic drug and an analog of the natural product quinine, and is used as an antimalarial; it has activity against P. vivax, P. malariae, P. ovale, and sometimes P. falciparum (depending on whether the parasite has developed resistance yet or not), all of which cause malaria.
Atovaquone-proguanil, another antiparasitic, is a broad spectrum, small molecule aminoquinoline. Atovaquone-proguanil interferes with the synthesis of pyrimidines, disrupting the ability of P. falciparum to synthesize its genetic information. Initial research began when World War II drove a shortage of quinine, motivating a rational drug design approach to develop an alternative. Like chloroquine, atovaquone-proguanil is an antimalarial drug, but unlike chloroquine, atovaquone-proguanil can be used for both malaria treatment and prevention. It can also be used to treat uncommon infections, like pneumonia from the fungus Pneumocystis jirovecii pneumonia, and the neurologic infection toxoplasmosis. The route to developing atovaquone-proguanil as we
currently know it was long, but worth it, as it has remained relatively immune to the drug resistance concerns that have plagued malaria treatment for decades.
Ivermectin is a broad spectrum small molecule in the avermectin class. It binds to the ion channels in the parasite’s cells, eventually causing paralysis and death of the parasite. It is a semi-synthetic drug, and can be used against a number of parasites, including head lice and parasitic roundworms. Some claimed it has protective effects against SARS-CoV-2, but this had little scientific support.
Antivirals, as you might remember, are therapeutic drugs that target viral infections, which are some of the most dangerous and prevalent types of infections. Since viruses invade host cells and use their host’s cellular machinery for much of their life cycle, it is hard to find unique drug targets that attack the virus without harming the human host. Antivirals function via four main mechanisms: blocking viral attachment and entry into host cells, inhibiting viral replication, blocking cellular machinery that allows particular viruses to encode themselves into host DNA, and prohibiting the release of viral particles from already-infected host cells. Figure 8.14 shows four different antivirals, as well as the cellular processes or components that they act upon. We provide more details about acyclovir, oseltamivir, and zidovudine below.
Even with multiple therapeutic strategies, our pool of approved antivirals – made up of only 90 drugs that have been produced over the last 50 years – has many challenges. The first is that only 90 antivirals have been produced over the

























F IGURE 8.14 | Viral and host cell targets for antiviral agents. Antivirals function via four main mechanisms: blocking viral attachment and entry into host cells, inhibiting viral replication, blocking cellular machinery that allows particular viruses to encode themselves into host DNA, and prohibiting the release of viral particles from already-infected host cells.
last 50 years; for comparison, there were 51 antibiotics under development in 2017 alone. Furthermore, these existing antivirals only treat nine viral diseases in total, often with limited efficacy. Another limitation is the fact that there are very few true broad-spectrum antivirals, making it difficult to prescribe antivirals without a specific diagnosis, again highlighting the need for better diagnostics.
In addition to a limited degree of efficacy, most antivirals also only have a fairly narrow window of efficacy; they tend to only be effective during the early progression of a viral infection when symptoms are not as pronounced. This leaves just a small window of time when the virus is undergoing initial replication, and the immune response is not yet at its peak. For example, influenza antivirals are only effective within 48 hours of symptoms appearing; after this point, therapeutics such as rehydration
and respiratory support, are often the only remaining course of action. Even in cases where a suitable drug target is available, high viral mutation rates often decrease the drug’s efficacy dramatically over a short period of time as the virus can adapt quickly, and develop resistance to the drug at an alarming pace. We will learn more about this phenomenon in Chapter 14: Pathogen Evolution and Drug Resistance, but for now, we want you to remember that all of these factors pose limitations to the efficacy of all antimicrobials, and in particular antivirals.
In the introduction to this chapter, you learned about acyclovir, which is a relatively broad spectrum for an antiviral, small molecule antiviral that belongs to a drug class known as the synthetic nucleoside analogs, which means that they are designed to mimic nucleosides. Acyclovir inhibits viral replication by inducing early chain termination. It was discovered during a screening process for new antivirals in 1974, and is used in the treatment of herpes virus and a similar virus, varicella-zoster virus
Oseltamivir (brand name: Tamiflu®) is a narrow spectrum small molecule in the neuraminidase inhibitor class of antivirals. It’s in this class because it works by inhibiting the enzyme neuraminidase – an enzyme that allows for the release of new viral particles – thereby
preventing the particles from exiting the host cell and replicating further in nearby cells. It was discovered through rational drug design, and is used to treat influenza A and influenza B infections.
Zidovudine (Retrovir, AZT) is part of an important subset of antivirals known as antiretrovirals, and like most antiretrovirals it is a narrow spectrum small molecule targeting retroviruses. Antiretrovirals are used to treat HIV infections, and are always used in combination (multiple drugs in a cocktail) to counteract drug resistance. They work through a number of different mechanisms, including stopping HIV entry into the cells by blocking viral attachment to the host cell, blocking viral transcription, and preventing integration of the HIV genetic material into host DNA. The original antiretrovirals were discovered through molecular screening; interestingly, the original antiretroviral compound was developed for potential use as a cancer therapy, but was found to be ineffective against cancer cells.
We hope that this section has shown you that there are many different ways to target and kill pathogens in a curative manner. We provide examples of antimicrobials, the drug class they belong to, their spectrum of activity, mechanism of action, uses and how they were discovered in Table 8.1.
Antibiotics Ciprofloxacin (fluoroquinolone)
Doxycycline (tetracycline)
Penicillin (beta-lactam)
Rifampin (macrolactam)
Antifungals Amphotericin B (polyene)
Fluconazole (triazoles)
Antiparasitics Atovaquoneproguanil (aminoquinoline)
Chloroquine (aminoquinoline)
Ivermectin (avermectin)
Antivirals Acyclovir (synthetic nucleoside analogs)
Oseltamivir (neuraminidase inhibitor)
Zidovudine (antiretroviral)
Broad Inhibits bacterial DNA replication Bacterial conjunctivitis, urinary tract infections
Broad Inhibits bacterial protein synthesis Lyme and other tick diseases, acne
Narrow Inhibits bacterial cell wall synthesis
Strep throat, various skin infections, and syphilis
Broad Inhibits RNA transcription Tuberculosis and leprosy
Broad Punctures cell membrane
Broad Inhibits production of cell membrane
Broad Prevents synthesis of genetic material
Severe fungal infections
Mild to severe candida infections, fungal meningitis
Malaria prophylaxis and treatment
Narrow Inhibits clearance of toxic compounds from parasite Malaria treatment
Broad Disrupts parasite’s ion exchange
Relatively broad Induces premature chain termination during DNA replication
Narrow Prevents the release of new viral particles from host cell
Narrow Block reverse transcriptase, and thus HIV replication
Head lice, roundworm treatment
Herpes and varicella-zoster viruses
Influenza A and B
Molecular screening
Semi-synthetic drug design
Product in nature
Semi-synthetic drug design
Molecular screening
Rational drug design
Rational drug design
Semi-synthetic drug design
Semi-synthetic drug design
Molecular screening
Rational drug design
HIV
Molecular screening
Many therapeutics are designed to alleviate the harmful symptoms caused by infection, rather than targeting the pathogen itself. These therapeutics are called symptomatic therapeutics, also known as symptomatic treatments, and providers typically recommend them for two specific purposes: 1) to counter the harmful effects of the pathogen and/or 2) to diminish excessive immune responses.
The first symptomatic therapy approach is to counteract dangerous and harmful symptoms caused by the pathogen itself. For example, if a person can’t breathe due to a respiratory infection, a symptomatic treatment would be needed, such as administering oxygen via a facemask, or supporting their breathing with a ventilator. These interventions can be lifesaving, and provide the person with the support they need to fight off the pathogen. Another example is oral rehydration therapy (ORT), an extremely important treatment for patients suffering from infections that cause severe dehydration through diarrhea and vomiting, such as cholera (Figure 8.15). ORT was developed based on an understanding that fluids must be delivered with the sugar and salts to help the body effectively absorb and retain water. There have been many documented cases of dehydrated cholera patients recovering after receiving a solution of water with sugar and salt – in some cases even delivered in the form of Coca-Cola®. ORT is sometimes sold in pharmacies as electrolyte solutions, or can be found in most grocery stores in forms such as Gatorade® and coconut water.
While rehydration is great, it’s probably even better to stop the symptoms of diarrhea altogether. One common antidiarrheal is a symptomatic therapeutic drug known as bismuth subsalicylate; you might have taken
this before, as it’s the key ingredient in PeptoBismol®. While its mechanism of action isn’t fully known, bismuth subsalicylate not only helps with diarrhea, but can also help with nausea.
Another potentially distressing symptom is a cough; coughs can be physically uncomfortable, and prevent you from sleeping or being as physically active as you’d like to be. One example of a cough suppressant is a drug called dextromethorphan, which can be found in cough suppressants like Robitussin®
The second symptomatic therapy approach is to decrease the magnitude of the immune response to a pathogen. This may seem a bit counterintuitive because the response exists to help us eradicate the invader as quickly as possible. However, as you might remember from Chapter 6: Immune System and Host Defenses, there are also times when the immune response is so extreme that it can hurt the patients rather than help them. This approach can be further broken down into two groups: antipyretics and anti-inflammatory drugs. As you will see, many drugs fall into both classes.

A number of infectious diseases cause severe dehydration, which can cause serious complications and even death, if not treated quickly. ORTs include water mixed with salt and sugar. They are sometimes sold in pharmacies as electrolyte solutions, or can be found as drinks at most grocery stores.
Antipyretics are used to treat one of the most common infectious disease symptoms: fever. It makes sense then that antipyretics derive their name from the Greek pyr, meaning fire. Antipyretics are some of the most commonly used symptomatic treatments that target the immune response. Fever occurs when cyclooxygenase (COX) enzymes catalyze the synthesis of prostaglandins. Prostaglandins accumulate in the central nervous system – an organ system that includes your brain, spinal cord, and surrounding fluid – and signal the rest of your body to raise its temperature. Since pathogens often grow best at normal body temperature, this increase in temperature makes it harder for them to survive. Fever also encourages the production of white blood cells, which further help the body to fight off disease. The precursor COX enzymes are often the target of antipyretics, preventing this rise in temperature from the very beginning of the pathway.
can even be life-saving. In this way, even basic antipyretics such as Advil® (ibuprofen) and Tylenol® (acetaminophen) can be instrumental in recovery from various infections. In addition to medications, there are also many home remedies that people use to treat fevers, such as using cold compresses, taking a warm bath, or drinking cool to warm water.

But if fevers are so helpful, why would we try to lower them at all? In short, high fevers can cause stress to the body that outweighs the immunological benefits, particularly at extremely high temperatures. For example, if too high or sustained for too long, fever can also cause brain damage. Therefore, antipyretics can often support a patient when they’re fighting off a pathogen, and in extreme cases, they
Anti-inflammatory drugs reduce another component of the immune response: inflammation, which is part of the body’s nonspecific response to disease or injury. Inflammation comes from the Latin word inflammare, meaning “to set on fire with passion”; as you might remember from Chapter 6: Immune System and Host Defenses, inflammation causes increased heat, redness, swelling, and pain at the afflicted area. Subsequent increased blood flow to the area brings more white blood cells to the site of infection or injury, which is very useful in moderation, but can cause harm in excess. There are two categories of anti-inflammatory drugs: nonsteroidal anti-inflammatory drugs (NSAIDs) and steroidal anti-inflammatory drugs.
NSAIDs include many medications with which you are familiar, such as aspirin (acetylsalicylic acid), Advil® (ibuprofen, which is also an antipyretic) and Aleve® (naproxen). These drugs each block the COX enzymes we previously mentioned in different ways that all ultimately result in directly blocking production of prostaglandins. Prostaglandins also assist in the inflammation process and bring white blood cells to the infected areas, but sometimes they can recruit too many and subsequently damage the non-infected human cells in the vicinity. The recruited immune cells – like macrophages – can do their job too well, “eating” not just the pathogens or the infected cells, but also the healthy cells, causing intense swelling and
discomfort. Like antipyretic drugs, the alleviation of symptoms from anti-inflammatory drugs can sometimes come at the cost of worse disease progression due to a weakened immune response. Therefore, it is still important to be mindful in their use. You might also recognize these drugs as “painkillers” that you might have taken when you last had a headache.
Steroids, also known as corticosteroids, are a synthetic derivative of some of the hormones your body naturally produces, and make powerful anti-inflammatory drugs. They tone down the immune system by binding to a molecule called the glucocorticoid receptor, which then allows them to suppress the genes that facilitate the inflammatory response. This makes them very useful in a number of autoimmune conditions. While their use in infectious disease has sometimes been considered controversial because there are concerns about suppressing the immune
response when it’s needed most, steroids have been shown to improve long-term outcomes in some types of infections, particularly with severe symptoms. More specifically, the corticosteroid dexamethasone is very useful in treating bacterial meningitis.
Many infections also cause some form of pain or discomfort, which could be either from the pathogen itself or our immune response to it. Analgesics are a type of medication used to relieve pain; the word also has Greek origins of “an-” (without) and “algos” (pain). Common analgesics used in infectious disease are ones that simultaneously reduce our immune responses, including Aspirin, Advil® (ibuprofen), Tylenol® (acetaminophen), and Aleve® (naproxen).
In Table 8.2, we provide examples of symptomatic therapeutic drugs, their types, uses, mechanisms of action, and how they were discovered.
Drug Name (Compound)
Advil® (Ibuprofen)
Aleve® (Naproxen)
Aspirin (Acetylsalicylic Acid)
Ozurdex® (Dexamethasone)
Tylenol (Acetaminophen)
Antipyretic, & Anti-inflammatory (NSAIDs)
Antipyretic, & Anti-inflammatory (NSAIDs)
Antipyretic, Anti-infammatory (NSAIDs)
Anti-inflammatory (Steroid)
Antipyretic
Ease fever and relieve minor aches associated with common cold, muscle pain, headaches, or toothaches
Relieve the symptoms of arthritis, which include inflammation, swelling, stiffness, and pain of joins
Reduce fever and relieve mild to moderate pain from muscle aches, toothaches, and headaches
Relieve inflammation of body parts and allergies
Reduce fever and relieve mild to moderate pain from muscle aches, menstrual pain, toothaches, and headache.
Inhibition of prostaglandin synthesis
Molecular screening
Inhibition of prostaglandin synthesis Molecular screening
Prevents prostaglandin synthesis by blocking host response to tissue damage
Suppresses genes that facilitate the inflammatory response
Inhibition of prostaglandin synthesis in only the central nervous system
Semi-synthetic drug design
Semi-synthetic drug design
Semi-synthetic drug design
1. What are the four main types of curative therapeutics and how do they broadly function?
2. Give two examples of symptomatic treatments for infectious disease.
3. Why do we use oral rehydration therapy rather than just water to treat dehydration?
We have now introduced you to the many types of therapeutics, their classification, their targets, their mechanism of action, their effects, and some examples of therapeutics that are used frequently. But what is the process of therapeutic drug design from the moment a researcher begins to search for a new drug to the moment they discover a promising new drug to the moment it is available on the market? In the US, this latter process is overseen by the US Food and Drug Administration (FDA), which you may remember is a federal agency that is responsible for ensuring human and veterinary drugs, medical devices, and human biological products are safe and effective. It was established by the 1906 Pure Food and Drugs Act, which was implemented partially with the goal of curbing excessive claims from those selling “medicines” (Figure 8.16). In this way, they help safeguard public health. The industry that develops, manufactures, and brings drugs to market is referred to as the pharmaceutical industry Its origins are in the Greek word pharmakeia, which means “the use of drugs, medicines, potions, or spells”.
In Chapter 6: Diagnostic Tests, you learned that the main goal of a diagnostic is to find the microbe responsible for a disease. Similarly, the main goal of many (curative) infectious disease therapeutics is to target and neutralize or kill the microbe. Therefore the primary focus in infectious disease drug development is centered around the “bug”. As you’ve already learned, researchers design new drugs via one or both of two approaches: running screenings using large libraries of compounds (molecular screening)

F IGURE 8.16 | FDA regulation of medical claims and substances. In the 1870s, William Clarke was selling Hunt’s Remedy, which he claimed cured an incredibly wide range of ailments, shown in its promotional materials as beating off death. The introduction of the 1906 Pure Food and Drugs Act was commemorated with a stamp referencing the advertising for Hunt’s Remedy. This time, it could be interpreted as the Act’s beating off harm from medical misrepresentation. Image credit: “1906 Pure Food and Drugs Act, ©1998 United States Postal Service®. All Rights Reserved. Used with Permission.”
or studying the biology of the microbe to find potential targets (rational drug design). These processes of drug discovery and development involve many stages, and it can take up to 15 years, or even longer, from the initial research stages to the launch of a drug. The FDA regulations encompass the following steps:
1. Drug Discovery and Development
2. Preclinical Research
3. Clinical Research
The drug approval process then follows these additional steps:
4. FDA Drug Review
5. FDA Post-Market Drug Safety Monitoring
6. Post-Market Clinical Research (Phase IV)
The aim of this step is to identify and validate two factors: 1) drug targets, i.e., what a potential drug will act on, and 2) drug candidates, i.e., what compounds might be able to exert the desired effect. Since our current drug discovery process tends toward rational drug design, researchers typically start by reviewing existing patents and already-published data on molecular compounds and existing treatments and technologies, to help identify potential targets and candidates. Once they have identified a group of compounds that they suspect will have the desired effect on the chosen target (e.g., inhibiting an enzyme involved in bacterial cell division or blocking the release of viral particles from a host cell), researchers begin to perform molecular screening, designing and running experiments to assess whether the drug will actually have the desired effects. These are known as validation experiments, and involve screening assays, which are qualitative procedures that allow for the characterization of the effect of compounds on selected targets at the cellular, molecular, and biochemical levels.
Screening assays help determine whether a given compound is a ‘hit’ molecule, i.e., whether it induces the desired effect efficiently. Molecular screening most commonly uses high-throughput automated experiments to
allow for efficiency of testing several small molecules at once, using robots and systematic analysis. In high-throughput automated experiments, very large compound libraries are tested against the identified drug target in plates containing 365 or more wells – which are hollow areas that can be filled with the chemicals needed for the reaction, and serve as small, space-efficient test tubes (Figure 8.17).
Researchers used this high-throughput molecular screening approach in their efforts to find new therapies to treat COVID-19. Studies published in 2020 and 2021 detailed screening of a library of 12,000 biologics, which were already FDA-approved for other diseases. Of these, 21 hits were identified as SARS CoV-2 replication inhibitors.
After being classified as a drug candidate, the selected compound will enter preclinical trials. These experiments aim to collect more information about the individual compounds such as their effects in cells, and whether it has any harmful effects. Trials in this stage assess the safety of the drug. The FDA requires two types of experimental research as part of the preclinical trials for each drug candidate: in-vitro (experiments in blood or tissue under laboratory conditions) and in-vivo (experiments in animal models, typically mice, rats or zebrafish). Where available, this stage may also include experiments in animals that can manifest the disease of interest in response to a pathogen infection, to further examine drug effects.
As you might imagine, there is substantial controversy around the use of vertebrate animals, particularly primates, in biomedical research. While many people agree that drugs, vaccines and other medical interventions should be














F IGURE 8.17 | High-throughput experiments screen multiple drugs. High-throughput drug screenings have revolutionized drug discovery as automated systems can perform hundreds of tests in parallel and provide rapid results to identify novel candidate drugs.
validated on animals before use on humans, there remains discomfort around the use of animals. There are strict protocols that researchers must follow to ensure compliance with ethical standards when working with animals.
Once preclinical experiments are completed, researchers evaluate their findings and decide whether the drug should move on to clinical trials, and be tested in people.
Clinical research is the stage at which human subjects participate. There are two types of clinical research: observational studies and clinical trials. In observational studies, researchers gather information about people in normal settings. These can involve the collection of medical data such as medical and test results or medical surveys, which can be helpful in understanding the population’s lifestyles or identifying common medical
concerns that could provide new prospects for therapeutic development. In contrast, clinical trials are research studies in which new treatments are tested in human volunteers.
To understand the effect of a drug, it is necessary to compare what happens with patients who take the drug to what happens with patients who do not. To accomplish this, clinical trials assign volunteer human subjects to an “experimental” group or a “control” group. Individuals in the two groups have similar preexisting conditions and demographic features. The experimental group is given the treatment of interest, while the “control” group is given either a placebo – a treatment that does not have any therapeutic effect on the patient – or the standard-of-care –a treatment or drug already recognized as effective by the medical profession. Most well-designed drug trials employ a ‘doubleblind’ approach, meaning that neither the clinician nor the experimental subject are
aware of whether the subject is receiving the experimental or control treatment. Rather, this information is stored in a coded document, to which the study team does not have access for the duration of the study. However, those not involved in analyzing the study results will have access to this coded document in the event of adverse reactions that require immediate intervention. Importantly, the study team will be required to switch any participant that is receiving the experimental drug or placebo over to the standard-of-care drug, should their condition fail to improve. Compliance with strict protocols and consent procedures is required to meet ethical standards for clinical trials with human subjects. These standards are considered in a separate section of this chapter entitled Ethics in Clinical Trials.
Clinical trials are a crucial part of the drug development process; they help us determine whether the drugs truly have the desired effect in the human body, and assess whether it’s safe for the general public to take them. As required by the FDA, clinical trials involve four phases in which the novel therapies are tested in different groups of people. As the phases progress, the number of participants increases.
Phase I: studies safety in a group of 20-100 participants; runs over the course of several months. Frequently, these first participants are healthy individuals, although some trials might start with people who have the disease of interest.
Phase II: studies the efficacy and side effects with hundreds of participants with the condition or disease; runs over the course of several months to two years.
Phase III: studies the efficacy and side effects in a group of 300 to 3000 volunteers
with the condition or disease; runs over the course of one to four years. If these first three phases are deemed successful, at this point the FDA will likely approve the drug.
After a drug is discovered and found to be safe and effective in humans, how does it make its way to the shelves of your pharmacy?

Scan this QR code or click on this link to watch a video about the four phases of clinical trials for drug discovery. This video names cancer drugs but the same phases apply in clinical trials for infectious disease drug discovery.
Once the preclinical and clinical research is completed and there is enough data proving that the drug is safe and effective to be used as therapeutic, the drug developers can file a new drug application (NDA) to the FDA for approval to put the drug on the market. An NDA presents all of the information the developers have collected about the drug, from preclinical data to Phase III results and analysis of the clinical trials.
The FDA first confirms that the application is complete and then it reviews the documents to decide whether or not to approve the drug for use in the US. Receipt of FDA approval marks an end to the years-long drug development process, at least within the US. To be used in other parts of the world, pharmaceutical companies must file for approval by the respective drug regulation agency of each region or nation, such as the European Medicines Agency, EMA, or Nigeria’s National Agency for Food & Drug Administration, NAFDAC.
Not all drugs must pass through all of the many stages of trials, testing, and review prior to this stage. Drugs that are the same or similar to previously approved drugs have an abbreviated approval process, as they are already proven to be trusted. These drugs need only show that they have nearly identical biological effects as the previously approved drug, and are effective and safe for new medical uses.
While clinical trials aim to provide a comprehensive evaluation of the safety and efficacy of a drug, it is challenging to have a complete understanding of all its effects and safety at the time of approval, as no clinical trial can last forever or include every person. Therefore, it is important to continue to monitor the effects the new drug has on the general population over the course of months and years after the drug is launched in the market.
The FDA reviews reports of adverse events, if any, and adds warnings to dosage or usage information as it becomes available. The FDA also reviews drug advertisements and labels, ensuring that they provide information that is correct and does not mislead consumers. As part of their efforts, they also monitor for the sale of drugs that have not been approved.
This is the final step, and the Phase IV of clinical trials, in which the manufacturer continues to monitor the efficacy and safety of the drug.
Phase IV: studies the safety and efficacy in a group of thousands of participants with the condition or disease. These run from the point
that the drug or medical device is approved by the FDA, and continue after it becomes available on the market. This is also called post-marketing surveillance of the drug.
You’ve now been introduced to all of the steps of therapeutic development, from intellectual conception to post-market surveillance. These are represented in Figure 8.18.
Identification and validation of drug targets Investigation of drug targets Drug screening
Selection of canditates
Selection of hit
2
3
4
Evaluation of drug safety and e cacy in humans
Examination of toxicity, pharmacokinetics, and responses in animal models
PHASE I
Verification of drug safety in 20-100 healthy participants, and some participants with the condition
PHASE II
Verification of safety and e cacy in hundreds of participants with the condition
PHASE III
Verification of safety and e cacy in up to 3,000 participants with the condition
Filing of new drug application with the FDA
5 Ensuring of accurate advertising of approved drugs and their risks
6
Presentation of the drug’s safety and e cacy data
Evaluation of the application by the FDA
Approval or rejection of the drug by the FDA
Monitoring and reporting of adverse events
Revision of drug advertisement and labels for transparency and accuracy
POST-MARKET CLINICAL RESEARCH
Post-marketing surveillance of the drug PHASE IV
Continued monitoring of drug safety and e cacy
Response to adverse outcomes
FIGURE 8.18 | Complete timeline for the drug development process established by the FDA. This process is divided in six steps and can take more than 17 years under normal conditions, from the moment researchers initiate the discovery and exploration of novel drug targets and candidates to the moment a therapeutic makes it into the market for human use and beyond.
But what happens in the outbreak setting, when time is of the essence?
The FDA and other major drug regulatory agencies like the EMA have the ability within their respective regions or nations to give approval for medications during public health emergencies, such as infectious disease outbreaks, without the full process of testing that is used at other times. This is called an Emergency Use Authorization (EUA) – the approval process by which the FDA authorizes drugs, and other countermeasures, to address public health emergencies.
Although there is urgency in getting these drugs to the market, the regulatory agency still performs its due diligence when evaluating available data on benefits and risks. As an additional protection, any medications that receive EUA are only eligible for use if they treat a serious or life-threatening disease for which the FDA stipulates “there are no adequate, approved, and available alternatives.” The EUA is an extremely valuable tool in an outbreak setting because it allows the rapid use of potentially life-saving medications; however, it comes at the cost of shortened testing and oversight, and may not be able to identify long-term effects (if any). That said, the FDA is unlikely to approve a drug that is suspected to pose long-term threats, regardless of any present benefits.
There are huge ethical responsibilities in carrying out clinical drug trials. Since they involve volunteer human subjects to determine drug efficacy, bioethical considerations are of great importance. While there are now many rules and regulations to ensure that individuals are treated properly in modern-day trials, these
protective regulations have not been in place for as long as you’d hope, and have not always been as protective as we’d want them to be. Some trials were devoid of beneficence, the moral charge to do good for patients, and/or nonmaleficence, the moral charge to avoid harming patients – two ethical principles that are now ingrained in regulatory practices for all human clinical trials. These principles state that the researchers must not only prioritize the health of test subjects, but they must also consistently ensure that they are doing no harm.
In Chapter 2: Epidemiology, you learned about the Tuskegee Syphilis Study, conducted on black men in Alabama. It was purportedly designed to observe the natural course of syphilis in black men. This egregious study followed individuals who were infected with syphilis for 40 years, without telling them their diagnosis, and the people running the trial barred the men from accessing treatment –penicillin – when it became available. This led to the death of many participants, as well as endangering their partners, and therefore children, and further spreading of the disease within the community. The Tuskegee Syphilis Study is a widely-recognized example of unethical withholding of therapeutics, and prompted a revolution in the regulations for research studies in the US.
There have been many other instances of ethically questionable research in drug development; one widely investigated example is a clinical trial for the broad-spectrum antibiotic trovafloxacin (brand name: Trovan). This trial took place in 1996 during an outbreak of meningitis in Kano, Nigeria, that would ultimately kill 1,500 people. Two hundred children were enrolled in this trial. Of these 200 participants, 100 were given trovafloxacin and the other 100 were given the standard-
of-care, ceftriaxone. Five children taking the experimental drug died, and were not moved to the standard-of-care, as they are expected to be in ethical trials, when they did not show signs of improvement (though six patients also died in the ceftriaxone group). According to authors Belinda Archibong and Francis Annan, there were existing concerns regarding Trovan’s safety before the pharmaceutical company began to test the antibiotic in the Nigerian children, and according to writer Nicole Perlroth, parents reported that they were not made aware that their children were receiving an experimental drug. Further, according to journalist Joe Stephens, it was later indicated that the pharmaceutical company’s ethical approval documents sent to the FDA for the approval of Trovan were written a year after the study had taken place by an ethics committee that did not exist. Despite these ethical issues with the trial, Trovan eventually received approval by the FDA, and arrived on the market as an antibiotic to treat meningitis in December, 1997. In the following years, however, the FDA withdrew Trovan’s authorization due to
concerns of liver injury. The incident sowed distrust of the pharmaceutical industry in some African communities, leading many to unfortunately, but understandably, reject critical drugs and vaccines. We will discuss vaccine hesitancy in chapter 9: Vaccines and Immunizations, but for now we want you to know that unfortunate events during trials of therapeutics and other medical interventions can have long-lasting effects, particularly when they induce medical distrust.
We share this history not to make you worried about taking therapeutics or vaccines, or to compromise your confidence in medications. Rather, we aim to show you that while clinical trials have strict regulations to prevent unethical actions from occurring during a study, it is important to recognize that this has not always been the case, and that these inappropriate trials have downstream effects on not only the participants but the public’s trust in pharmaceuticals overall.
1. Based on your knowledge of the biology of pathogens, describe two potential targets researchers could address in the drug discovery and development phase.
2. Why are clinical trials so critical to the drug discovery process to treat human disease?
3. Why are ethical considerations crucial during clinical research?
At this point, we have reviewed the six steps that take place during the discovery, development and approval for a novel drug, and you now know that determining the efficacy and safety of a drug are key to being on the market for public use. But what does it take to make a drug effective and safe in humans? There are many factors that influence how the drug interacts with the human body, how much of the drug actually arrives in the area or tissue where it needs to be, and what effects it causes, both good and bad. Other contributing factors include drug dosage, which is how much medication patients should take at what time, and the side effects identified during clinical research.
A drug’s effects, both good and bad, depend on and are influenced by its pharmacokinetics and pharmacodynamics. Pharmacokinetics can be conceptualized as “what the body does to the drug” and pharmacodynamics as “what the drug does to the body”. Both of these factors affect how effective a drug is, as well as how safe it is to take.
One component of a drug’s pharmacokinetics is its drug metabolism, or how a drug is chemically altered in the body. Drugs are often processed by the body after they are absorbed, leading to a change in the drug’s concentration or structure. One important phenomenon associated with drug metabolism is first-pass metabolism, in which drugs are chemically altered in a specific part of the body, often the
liver, before entering the bloodstream. This chemical alteration can inactivate part of the drug, reducing the concentration of the active drug. This leads to a lower drug bioavailability, which is the percentage of the drug that ultimately enters circulation where it can be clinically effective. Notably, some drugs are delivered in the inactive state and need first-pass metabolism to produce the active drug.
Side effects are inherent to most therapeutic interventions. You’ve probably experienced these effects at some point in your life; allergy medications can make you drowsy, antibiotics can make your stomach upset, and asthma inhalers can make you feel jittery. Side effects arise both because it’s difficult to only affect exactly one part of the human body when all of our cells have so many similarities, and also because our bodies are often not well-suited to handling substances that came from other organisms or that were produced synthetically.
Side effects are an example of a drug’s toxicity, which describes any harmful effects that it may have on the host. While all drugs can have some level of toxicity, side effects can vary greatly depending on several factors, including how the drug is administered, the specific drug’s mechanism of action, and its dosage. Even when antimicrobials are designed to only target cell components that human cells don’t have, dosage is still important. This is due to a few factors, the first being that the drug can be metabolized down to products that are somewhat harmful to the host. For example, antimalarials are known to cause muscle pain, likely from disturbance of the enzymes that help execute muscle function. Additionally, nearly any substance can overwhelm the body in high enough quantities, even water.
F IGURE 8.19 | Therapeutic window. This graph depicts the efficacy and toxicity of increasing doses of Drug X. The relationship between these values determines the TI.
The key goal of dosage determination is balancing the efficacy and toxicity of a drug. You might remember efficacy as being the clinical benefit of the drug in treating the disease of interest. Toxicity, conversely, occurs when a drug renders harm to the host, which can be dependent on dosage, and can occur even when taken at the advised dosage.
As dosage is increased from 0, so should the efficacy of a drug. However, at some point, those taking the drug will begin to experience adverse side effects. The sweet spot between the two is the dosage at which the drug level is high enough to be effective, but low enough to only produce manageable side effects. This range is known as the therapeutic window (Figure 8.19). Drug concentrations above the therapeutic window are toxic, while concentrations below the therapeutic window are ineffective.
Though the ideal range or sweet spot can be described qualitatively as we’ve just done, it can also be quantified using the therapeutic index (TI). To calculate TI, you need to know two numbers:
• The drug’s median toxic dose: TD50
• The drug’s median effective dose: ED50
The TD50 is the concentration of the drug needed to induce a toxic effect in 50% of those who take it. At doses lower than the TD50, fewer than 50% of the subjects would be experiencing these symptoms, and at higher dosages, more than 50% would be, hence the term “median”. The higher the TD50, the better. Similarly, the ED50 is the concentration needed to induce a therapeutic benefit in 50% of those who take it; the lower the ED50, the better. TI is thus TD50 over ED50.
Test subjects are given a therapeutic at a range of dosages
Therapeutic Index = TD50/ED50 = 24/8 = 3
F IGURE 8.20 | Determining TD50, ED50, and TI of a drug. This flowchart shows the calculation of the TI, as defined by TD50/ED50.
Therapeutic Index (TI)
A high TI indicates that a given dosage is more likely to provide benefit than harm; thus, the higher the TI, the better. Widening this margin between effective and toxic doses enables the treatment to avoid crossing the sometimes razorthin line between positive and negative effects. Ideally, a safe but effective drug would be toxic only in incredibly high doses, while maintaining its effectiveness in extremely low doses. As you might imagine, this is not always possible.

Scan this or click on this link to discover information about any therapeutic through the website DrugBank
Let’s work through a made-up example. Let’s say that participants in a clinical trial of a new drug were given a range of increasing dosages of the drug. At a dose of 8 grams/milliliter (g/ mL), 50% of the recipients are observed to have the desired outcome of the drug (ED50). The dosage continues to increase, and by the time it reaches 24 g/ml, 50% of the subjects are showing symptoms of a toxic effect (TD50). Using these results, we can calculate the TI. The TI is the ratio of these two numbers, so to calculate it, you divide the TD50 by the ED50. We summarize this example in the flowchart (Figure 8.20).
One factor that greatly affects the metabolism and efficacy of drugs is the route of administration There are many different ways to administer drugs, which we’ll detail below, starting
with routes that are more common in selfadministered medications (Figure 8.21).
• Oral: this is the one you’re probably most familiar with. For oral medications, you swallow the drug, which is generally in the form of pills or liquids. This is how you took ibuprofen for your last headache, or swallowed liquid antibiotics for an ear infection as a child.
• Sublingual: for this route, you place a pill under your tongue and wait for it to dissolve rather than swallowing the pill itself; this typically results in faster absorption than the oral route. Examples of sublingual medications include ergotamine, which some people take for migraines, as well as nitroglycerin, which is used to help relieve chest pain in a person with a heart attack, both of which you want to start working very quickly.
• Intranasal: this is where you take a deep breath to take in the dose of the drug through your nose. You might be familiar with this route if you’ve ever used some types of allergy medications that you sniff in through your nostrils.
• Topical: this is when the drug is applied (frequently as a cream or gel) to your skin, which is how you would use neosporin, antifungal creams, or many acne medications.
Other routes of administration typically require more oversight from healthcare providers. These include:
• Intravenous (IV): as the name suggests, IV medications are introduced directly into the bloodstream via a small needle that pierces the skin, and enters a vein. Frequently people with more severe bacterial or fungal infections need to receive their antibiotics






F IGURE 8.21 | Common routes of administration for therapeutics. There are different ways to administer therapeutics, including oral, sublingual, intranasal, topical, intravenous, intramuscular and subcutaneous routes. Different routes may be selected by how they affect the pharmacokinetics or bioavailability of the drug, as well as patient experience.
or antifungals via an IV. You might be familiar with the concept of IV delivery by hearing about or receiving IV fluids. This is also how we deliver convalescent plasma.
• Intramuscular: the name is also a clue here, with the drug being delivered via a small needle straight to the muscle. A common example of an intramuscular medication is the EpiPens that are used in severe allergic reactions.
• Subcutaneous: some medications can also be administered in the layer beneath the skin, which is known as the subcutaneous tissue. Examples of these subcutaneous medications include insulin, and some blood thinners. Some antibiotics can also be delivered subcutaneously if IV administration is not possible.
You might not be surprised to learn that the same drug can be designed to be administered via different routes. For example, most antibiotics come in both an oral and IV version; oral for when the infection is mild, and people can take their medication safely at home, and IV for when the patient is severely ill, and needs to be admitted to the hospital. These routes are not just limited to therapeutic administration; you’ll see them again in Chapter 9: Vaccines and Immunizations.
Beyond just considerations of patient comfort, and how easy it will be to administer the drug, the route of administration is very important because it can cause dramatic variation in the resulting bioavailability and pharmacokinetics impact of the drug. Since IV injections administer drugs directly into the bloodstream, they have 100% bioavailability while other routes are less efficient. For example, a 40 mg oral dose of a hypothetical heart medication could be equivalent to a 1 mg dose injected
directly into the bloodstream; despite being very different dosages, both would ultimately deliver approximately the same volume of the drug to the bloodstream.
After they’ve been approved, some drugs are only on the market as prescription medications (Rx), which means that they need to be prescribed by a healthcare professional and dispensed by a pharmacy, while others can be obtained as over-the-counter medications (OTC) like ibuprofen and aspirin, which are available without a doctor’s prescription. OTC drugs are monitored separately from Rx drugs and can only include a small list of accepted ingredients, doses, formulas, and labels. Drugs can transition from Rx to OTC if the drug producer is able to demonstrate the following:
1. There is low risk for abuse of the substance
2. It can be taken effectively and safely without a doctor’s instruction
3. It is used for conditions that can be selfdiagnosed.
Rx drugs must be approved for specific indications (uses) one by one. However, it is a relatively common practice for providers to prescribe Rx drugs for unapproved conditions. This practice is called off-label usage, and it is often reserved for cases in which there may not be an approved treatment, or the patient has tried other treatments without success. One example of off-label use in the world of infectious disease is naltrexone. Naltrexone is currently approved for treating alcohol and opioid dependence, but there is some evidence that it might make antiretrovirals more effective in treating HIV. Off-label usage can also apply to drugs given in an unapproved dose, route of
entry, or specific population, such as children or the elderly. Like the EUA, off-label usage can be a valuable tool in treating people with life-threatening or terminal conditions. It’s important to realize that off-label usage is never meant to be risky, reckless, nor unethical; prescribers would never prescribe a drug for off-label usage without sufficient evidence that it is both effective and safe to use as treatment for the off-label condition. Off-label usage is always supported by the data even if the drug just has not yet passed through the formal approval process for this second usage.
As you’ve already seen within this chapter, many ethical and technical challenges may arise as drugs are developed, distributed, and used by the public. Many of these concerns revolve around access and availability to different groups of people, particularly to do with fair distribution and drug pricing.
Distributing a drug and ensuring that patients have access to it is often a more difficult battle than developing the drug itself. Many obstacles can impede the widespread use of a drug, including manufacturing difficulty, scarcity of resources, or limitations in the number of companies having production rights.
The routes that a given drug takes from being produced at a factory to being taken by a patient are known as distribution channels Most drugs take a few familiar stops along these channels, although it does vary by region of the world. They start by going from the drug manufacturer’s production line, then being sent to a drug wholesaler, who sells the drug to a hospital, pharmacy, or grocery store, who
then either administers or sells the individual packages of medication to sick patients.
Some people won’t be reached by these channels for varying reasons. There may not be any hospitals or pharmacies near where they live, any roads for trucks full of medication to travel on, or enough staff to safely run a health center, or a given drug wholesaler may not sell to a particular region because there aren’t enough potential customers to earn back their investment. This is a particular barrier in remote regions. Modern science has already created many life saving drugs for diseases that infect people all around the world; however, these treatments often simply do not reach those who need them the most. In this way, investment in distribution infrastructure is equally important as investment in drug development.
The challenge of drug pricing goes hand-inhand with availability. Even if a treatment’s manufacturing process becomes more efficient and some of the difficulties with access are resolved, many treatments remain extremely high-priced – for many reasons that are not solely market-based – and are unavailable to those who need them. This cycle creates negative, avoidable health outcomes we often see in low-income and low-resourced areas around the globe, which are frequently the communities where therapeutics are initially tested.
One well-known and egregious example of drug price exploitation, outside of infectious disease, is insulin pricing in the US (Figure 8.22). Insulin has been lauded for years as a lifesaving treatment for those who live with diabetes, and more than 100 million Americans – 30 percent of the US population – are afflicted
with diabetes or pre-diabetes today; 7.4 million of those people depend on insulin to stay alive.
Although insulin was discovered nearly 100 years ago, its price has skyrocketed in recent years due to legal loopholes in drug patent laws that enable predatory companies to charge exorbitantly high costs for their product. Despite recently-implemented price caps, many Americans still struggle to afford their life-saving treatments, at times being forced to ration medication or go without it entirely, frequently with deadly consequences. In addition to being inhumane in general, this practice has additional detrimental effects in the outbreak setting, as unmanaged diabetes reduces the capacity of the patient’s immune system to fight off infections.
antibiotics. Tuberculosis causes over 1.3 million deaths each year, over 95% of which occur among individuals from developing or lowincome nations. The price for a full course of TB treatment can reach several thousand dollars, and triple in price if the TB is found to be drug resistant. In many cases, the people who need the treatment simply cannot afford to pay and have to go without, risking not only their own health but also the potential of infecting others. While certain companies and distributors are attempting to address these concerns by subsidizing and lowering costs in various endemic regions, large-scale, structural changes are necessary to ensure individuals everywhere receive the drugs they require. While this may de-incentivize investment from pharmaceutical companies, ideally, these initiatives will be paired with prevention campaigns, in order to preserve communities’ health and alleviate the future need of drugs.
F IGURE 8.22 | Therapeutic price exploitation. Insulin prices have increased exponentially over recent decades, causing the insulin market to reach tens of billions of dollars in profit, despite no change to the underlying formula and no increase in production prices.
This situation is not unique to the US, nor to insulin alone; in the world of infectious disease, the price of tuberculosis (TB) treatments poses major barriers to their use worldwide. As you may recall, TB is a serious bacterial respiratory infection caused by the bacteria Mycobacterium tuberculosis, which is frequently resistant to the available
The inequities don’t stop with pricing; there are also significant disparities in the diseases for which we have therapeutics in the first place. For example, Lassa virus is estimated to cause up to 300,000 infections per year, and around 5,000 deaths. However, antivirals are notoriously difficult to develop, and no drug has ever been specifically developed to treat Lassa fever. Our only treatment is an off-label use of a drug called “ribavirin,” which was originally developed to treat hepatitis C.
Lassa fever is an example of a larger group of diseases, Neglected Tropical Diseases (NTDs), which typically occur in tropical regions and primarily impact developing countries. The WHO estimates that NTDs impact over 1 billion people worldwide. NTDs also include diseases like Hansen’s disease (leprosy), dengue fever, trachoma, mycetoma, and Chagas disease.
NTDs are extremely common, but their mitigation receives little funding since they impact some of the world’s most socioeconomically disadvantaged people. This likely indicates some level of bias (conscious or otherwise) against the populations that NTDs frequently affect, in addition to the limited financial incentive to develop appropriate therapeutics.
While the inability to access drugs, or concern about their use, has detrimental effects worldwide, there are also downsides to overusing drugs. For example, in areas like the US, drugs may be overused in comparison to preventative care and non-drug treatments. In fact, over 15% of total healthcare spending in the US is on prescription drugs alone. This skew towards treatment rather than prevention is evident on the research side as well, given that funding tends to predominantly support research geared toward treating illness after it’s already occurred rather than preventing it. This may be most grounded in the desire to help sick people, but we must also be aware that there may be financial motivations, as treatments are more profitable than prevention.
Prescription overuse and misuse is a particular issue for antibiotics, where antibiotic resistance can emerge and spread, threatening the effectiveness of antibiotics themselves – you’ll learn more about this concerning phenomenon in Chapter 14: Pathogen Evolution and Drug Resistance. Examples of antibiotic misuse would be taking antibiotics for non-bacterial illnesses (like the flu, which is caused by a virus). Antibiotic overuse would be prescribing an antibiotic for an infection that is, in fact, bacterial but will likely run its course on its own, such as most sinus infections.
Healthcare providers have a duty to be good antibiotic stewards to protect the efficacy of these incredible resources, as this will improve patient outcomes over the long term. It is also imperative that manufacturers and distributors ensure that there is equitable access worldwide. Beyond the moral imperative, lack of equitable access to antibiotics increases the risk that a pathogen spreads unchecked, evolving with each new infection, and running the risk of developing resistance to existing antibiotics and threatening global health. Importantly you also play a role in antibiotic stewardship when choose to take or not take antibiotics and when you take your full course of antibiotics as they have been prescribed to you.
Beyond overuse and misuse, we must be increasingly mindful of how the drugs we use interact with other substances. The effects of drugs are often dependent on other treatments used in conjunction with them, or other substances to which the body is exposed. Sometimes, doctors advise medications to be taken with others to produce synergistic interactions (interactions that result in a greater benefit than the sum of each medication alone). However, one drug can also detract from the efficacy of another, or even become toxic in combination. For example, some antibiotics consumed orally require an acidic stomach environment for absorption. This means that antacids, which decrease the acidity of the stomach, may prevent the drug from being effectively absorbed. As another example, Paxlovid®, the medication used to treat COVID-19 should not be taken with a drug class known as the statins, which are used to treat high cholesterol. This is because Paxlovid® can block the enzyme that clears statins out
of the body, allowing toxic levels of the statin to accumulate and cause tissue damage. This is notable, given that one of the statins, atorvastatin, is among the most prescribed drugs in the US, particularly for older adults who are at higher risk for severe COVID-19 infection.
A particularly harmful combination is that of many prescription drugs with alcohol. This drug interaction can be extremely dangerous, causing a range of symptoms from headaches to impaired breathing, and even death. It is crucial for researchers to understand and test for these interactions during clinical studies and
for doctors prescribing them to review what other medications or substances the patient is using before prescribing a new medication. Similarly, consumers must be mindful of their own use of drugs, as well as how the effects of the drugs they’re taking may be impacted by other behaviors.
A core theme of prescription drug use is that starting, stopping, or combining medications – or even supplements – should happen with the oversight of a healthcare provider, and you should never share prescription medications with others.
1. How does the dosage of a drug relate to its therapeutic index?
2. Name three different ways therapeutics are administered.
3. Name three challenges that arise as therapeutics are distributed and used by the public.
4. What is one of the most concerning consequences of misuse or overuse of drugs for treating infectious diseases?
1. “Therapeutics,” “treatments,” and “therapies” can all be used interchangeably and drugs are substances that make a subset of therapeutics that treat disease.
2. The target of a drug is the structure or process that the drug alters in order to exert its effect. For curative drugs in infectious disease, it is usually a structure or process that impacts the life cycle of the microbe, or its ability to damage the human body.
3. Answers may vary. Salvarsan causes dangerous and often painful side effects. Penicillin was adopted in the 1940s as the major therapeutic alternative to treat diseases like syphilis.
1. The four main types of curative therapeutics are antibiotics, antifungals, antiparasitics, and antivirals. They broadly function by directly targeting and killing the pathogen.
2. Answers may vary but might include:
a. administering oxygen via a facemask
b. using a mechanical ventilator to support their breathing
c. oral rehydration therapy
d. antipyretics
e. anti-inflammatory drugs
5. Oral rehydration therapy adds sugar and salts to water to help absorption of water by the body and balancing of nutrients.
1. Answers will vary, but may include things like the following: enzyme involved in bacterial cell wall synthesis, ion channels in a parasite’s cells, enzyme involved in viral nucleic acid replication, viral surface proteins.
2. Clinical trials are critical to the drug discovery process because they test whether the new drug is effective and safe in human volunteers, and allow researchers to identify potential side effects.
3. Answers may vary; ethics are central to clinical trials as they preserve the health and autonomy of not only the participants in the trial, but also all those who will eventually take the drug. Ethical trials will also help preserve public trust in therapeutics and medical interventions.
1. The dosage of the drug is informed by therapeutic index, as the manufacturers aim to balance effective levels of the drug with toxic side effects.
2. Any three of the following: oral, sublingual, intranasal, topical, intravenous, intramuscular, and subcutaneous
3. Answers may vary, but can include things like:
a. manufacturing difficulties
b. scarcity of resources
c. limitations in number of companies having production rights
d. limitations in distribution channels, especially in remote regions
e. pricing
f. public trust in the drug
4. The main issues of drug use and misuse include the emergence and spread of antibiotic resistance, threatening the effectiveness of our countermeasures.
Analog: A drug whose physical structure is very similar to the structure of another drug, although they have different chemical and biological properties; can be thought of as a therapy’s “relative”.
Analgesics: Type of medication that relieves pain or discomfort by targeting pain signals to the brain.
Antibiotics: Type of antimicrobials that target bacteria; also known as antibacterials.
Antifungals: Type of antimicrobials that target fungal infections; also known as antimycotics.
Anti-Inflammatory Drugs: Symptomatic therapeutics that reduce inflammation. Examples include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil®) and naproxen (Aleve®), and steroids.
Antimicrobials: A broad term that refers to drugs that target pathogens (i.e., curative therapeutics).
Antiparasitics: Type of antimicrobials used to target parasites.
Antipyretics: Symptomatic therapeutics that reduce fever. Examples include aspirin, ibuprofen (Advil®), and acetaminophen (Tylenol).
Antivirals: Type of antimicrobials that target viruses.
Bacteriostatic: Antibiotics that halt bacterial grown by targeting the bacteria’s reproduction or other cellular functions.
Bactericidal: Antibiotics that directly kill the target bacteria.
Beneficence: The moral charge to do good for patients; one of two ethical principles ingrained in regulatory practice for all human clinical trials, as well as healthcare more broadly.
Bioavailability: The fraction of a drug that reaches the bloodstream after administration; varies by route.
Biologics: Typically large and complex drugs derived from living organisms, such as genes, proteins, or cells. They are designed to provide a therapeutic benefit, frequently using biotechnology methods.
Biotechnology: The application of biological processes, organisms, or systems to develop functional products.
Broad Spectrum: A drug that is effective against many different organisms, typically by targeting a common feature among them.
Clinical Trial: Research study in which a new treatment is tested in human volunteers to assess its safety and efficacy.
Curative Therapeutics: Class of therapeutics that target the actual pathogen of interest to neutralize or kill it, ultimately eliminating the infection.
Dosage: How much and at what frequency a drug is taken in order to provide the maximum beneficial therapeutic effect with minimal toxic side effects.
Drugs: Chemical substances, synthetic or derived from nature, that are used as therapeutic agents to prevent, treat, or relieve symptoms of a disease or health condition.
Drug Candidates: The most promising molecules that emerge from the drug discovery process.
Drug Metabolism: The processes by which drugs are chemically altered by our bodies.
Efficacy: A drug’s ability to provide clinical benefit in treating the disease of interest; also sometimes referred to as its “effectiveness”.
Emergency Use Authorization (EUA): The process by which the FDA authorizes drugs for use to address public health emergencies; it requires less testing than standard approval, in order to allow for rapid action while aiming to maintain rigor.
Fecal Microbiota Transplantation (FMT): The transplantation of fecal material from a healthy individual to an ill patient in order to treat bacterial infections; a poop transplant.
Food and Drug Administration (FDA): US government agency that oversees the development, approval, and regulation of drugs.
Intranasal: A route of administration involving inhalation via the nasal cavity.
Intramuscular (IM): A route of administration involving direct injection into the muscle.
Intravenous (IV): A route of administration involving direct injection into the vein.
Mechanism of Action: The molecular/ biological process by which a drug produces its desired effect.
Molecular Screening: A technique in drug discovery in which a library of molecules is assayed for a biochemical or physiological response that is predicted to correlate with a desired therapeutic benefit.
Monoclonal Antibodies: Antibodies that have been produced in a large volume by cloning the desired antibody, typically within the lab or in non-human animals; used as a biologic therapeutic.
Narrow Spectrum: A drug that is effective only against one or a small number of organisms.
Natural Products: A class of drugs discovered in the diversity of existing nature; examples include quinine and the original penicillin.
Nonmaleficence: The moral charge to avoid harming patients; one of two principles that define ethical regulatory practices for all human clinical trials, as well as healthcare more broadly.
Off-Label Usage: A practice in which drugs are prescribed for an indication for which the drug was not approved; off-label usages are still evidence-based and regarded as safe.
Oral: A route of administration involving swallowing.
Oral Rehydration Therapy (ORT): Type of symptomatic therapeutic in which patients are given water mixed with sugars and salts, allowing their body to readily absorb fluids and obtain nutrients; used to aid those suffering from dehydration.
Over-the-Counter Medications (OTC): Medications that can be purchased without a prescription.
Passive Immunity: The receipt of antibodies against a disease that were produced by another individual, e.g., antibody therapy, babies receiving maternal antibodies via breast milk.
Pharmaceutical Industry: The business sector that researches, develops, manufactures, and markets drugs for use as medications.
Placebo: A substance used as a control in a clinical trial that is chosen to have no clinical effect; helps to evaluate the efficacy of a new drug by ensuring that its benefits are due to the drug itself rather than additional, psychological factors.
Preclinical Trials: Research study in which a new treatment is tested in animals for toxicity, safety, mechanism of action, and dosage.
Prescription Medications (Rx): Medications that may be purchased only with a prescription from a health care provider.
Probiotics: Live microorganisms, usually bacteria, that help restore the gut microbiome; often taken as a supplement during and after taking a course of antibiotics.
Prophylaxis: A measure aimed at preventing the occurrence or progression of a disease.
Rational Drug Design: Drug discovery method that utilizes the principles of biology to identify and design specific drug candidates.
Recombinant DNA Technology: A form of genetic engineering in which two portions of genetic material are combined to introduce a new function in a biological system.
Routes of Administration: Ways in which drugs and other medicines can be administered. They include oral, sublingual, intranasal, topical, intravenous, intramuscular, and subcutaneous.
Screening Assays: Qualitative procedures that allow for the characterization of the effect of compounds on selected targets at the cellular, molecular, and biochemical levels.
Semi-Synthetic Drugs: Drugs derived from a natural product that have been chemically modified to create a new therapeutic with improved or altered properties, such as increased effectiveness, better absorption, fewer side effects, or allowing for mass-production.
Side Effects: Secondary, typically unwanted (adverse) effects of a drug or medical treatment.
Small Molecules: Drugs that are characterized by their low molecular weight, with diverse mechanisms of action.
Standard-of-Care: The current standard treatment, that has been established to be effective, that a healthcare provider should provide to treat a disease.
Subcutaneous: A route of administration; the drug is injected into the tissue layer between the skin and the muscle.
Sublingual: A route of administration: the drug is placed under the tongue of the patient who waits for it to dissolve. This route typically results in faster absorption than the oral route.
Symptomatic Therapeutics: Class of therapeutics that alleviate the uncomfortable symptoms and signs which accompany a disease; also known as symptomatic treatment
Synthetic Drug: A drug created entirely in a laboratory, not derived or modified from natural substances, and designed to have specific therapeutic effects.
Targets: The structures or processes that a drug alters to exert its effect.
Therapeutics: Therapies or treatments that have healing or health-improving qualities. These can include interventions like a ventilator, or drugs like penicillin and chloroquine.
Therapeutic Index (TI): A measure of a drug’s safety margin, calculated by the ratio: TD50/ ED50, where TD50 is the median toxic dose of a drug and ED50 is the median effective dose of a drug.
Therapeutic Window: The range of therapeutic dosages that is high enough to effectively combat disease, while low enough to only produce manageable side effects; the sweet spot between efficacy and non-toxicity.
Topical: A route of administration involving application directly on the skin or mucous membranes.
Toxicity: A drug’s capacity to cause adverse (non-therapeutic) side effects; can be dependent on dosage, and can even occur at the advised dosage.