







1. Voegeli D, LBF® “No-Sting” Barrier Wipes: Skin Care Using Advanced Silicone Technology. British Journal of Nursing, 2008; Vol. 17: No. 7. ©2023 Convatec Inc. ®/™ all the trademarks are the property of ConvaTec group companies. AP-64736-CAN-ENG
NILTAC TM and SILESSE TM are now

SILICONE BASED ADHESIVE REMOVER
Rapidly releases appliances or dressings adhered to skin

Protects skin for up to 72 hours1
For more information, please call our Customer Relations Center (Registered Nurses on staff) at 1-800-465-6302, Monday through Friday, 8:00 AM to 6:00 PM (EST), or visit our Web Site at convatec.ca
Scan for more information or to ask for samples





I am excited to introduce myself and join the Ostomy Canada team as its new Executive Director. I look forward to working with all stakeholders across the country! I share an extensive background of 20 plus years of senior national management experience in the not-for-profit sector at both a provincial and national level. As well, I have 15 years of professional and entrepreneurial leadership as part of a family owned and operated business within the health care industry dedicated to Incontinence Management.
Having recently relocated in 2021 to the Okanagan in beautiful BC after spending most of my life in Winnipeg, I enjoy spending leisure time with my wife, hiking trails, playing a round of golf, walking the dog(s), or kayaking on the lake; that is when I’m not training to run a Marathon race or watching NFL football on Sundays!
I am passionately driven to ensure that all people are treated with dignity, and provided with quality care, support, and compassion in times of need and I believe that we can unite together in providing support that enables people living with an ostomy to “live life to the fullest” ! n

Ian MacNeil (Ottawa, ON) – Ontario Region
Andrea Manson (Parksville, BC) – Pacific Region
Janet Paquet (Hamilton, ON) – Ontario Region
OFFICERS
Chair: Jacqueline Bloom (Salisbury, NB)
Vice-Chair: Janet Paquet (Hamilton, ON)
Treasurer: Stephen Maybee (Mississauga, ON)
Secretary: vacant
Executive Director: Bryan Ezako, (Kelowna, BC)non-voting
OFFICE STAFF
Office Manager / Accountant: Wilma Kohler (Toronto, ON)
Office Coordinator: Carole Pew (Oshawa, ON)
DIRECTORS
Jacqueline Bloom (Salisbury, NB)
Deb Carpentier (Regina, SK)
Troy Curtis (Ottawa, ON)
Ann Durkee-MacIsaac (Hebron, NS)
Stephanie Grace (Newmarket, ON)
Randy Hull (Winnipeg, MB)
Jayne Kerr (Thornbury, ON)
Réal Lamarche (Quebec City, QC)
Andrew Joseph (AJ) Leveille (Langley, BC)
Ian MacNeil (Ottawa, ON)
Andrea Manson RN, BSN, NSWOC, NCA (Parksville, BC)
Stephen Maybee (Mississauga, ON)
Janet Paquet (Hamilton, ON)
Joan Peddle RN BN NSWOC WOCC (C) CCHN (C) (Moncton, NB)
REGIONAL ADMINISTRATORS
Deb Carpentier (Regina, SK) – Prairie Region
Réal Lamarche (Quebec City, QC) – Quebec Region
Joan Peddle (Moncton, NB) – Atlantic Region
PILLAR ADVISORS
Sustainability – Bryan Ezako and Stephen Maybee
Advocacy & Government Relations –Ian MacNeil and Joan Peddle
Engagement and Support – Deb Carpentier and Andrew Joseph (AJ) Leveille
Marketing and Communications – Stephanie Grace and Troy Curtis
Partner and Relationship Support – Andy Manson and Randy Hull
MEDICAL LIFESTYLE ADVISORY COMMITTEE
Karen Bruton NSWOC - RN BScN, MCICS-WH WOCC(C)
Dr. Zane Cohen Senior Colorectal Surgeon, Sinai Health System - M.D., F.R.C.S.(C)
Lisa Harris Registered Physiotherapist
- BSCPT CAFCI MCPA
Rory Hornstein Registered Dietitian - RD, BED
Andrea Manson NSWOC - RN, BSN, NSWOC, NCA
Rose Raizman Personal Health Coach
- RN-EC PHCNP NSWOC WOCC(C) MSC MSCN
Dr. Tim Sproule Acting Chief Plastic Surgery, Scarborough Health Network - MD FRCSC
Dr. Shabita Teja, Naturopath and Pharmacist
- BSC (PHARM), ND
Lauren Wolfe NSWOC - RN, BSN, MCLSC (WH), NSWOC, CWOCN
OSTOMY CANADA MAGAZINE
Lisa Gausman, BA Humanities, Senior Editor
Julie Grzela, Assistant Editor
Janet Paquet, Assistant Editor
Heather Twele, BA English Honours
Assistant Editor
Tammy Hunter, Graphic Designer
Lorne Aronson, Advertising Manager
Réal Lamarche, Translator of French content
OSTOMY CANADA CONNECTS
Bryan Ezako
Tiffany Shorson
SOCIAL MEDIA/WEBSITE
Yaser Nadeem (Webmaster)
Address all Correspondence to Ostomy Canada Society, 5800 Ambler Drive, Suite 210, Mississauga, ON L4W 4J4
Tel: 1-905-212-7111
Toll free: 1-888-969-9698
Fax: 1-905-212-9002
Email: info1@ostomycanada.ca www.ostomycanada.ca
Charitable Registration No. 119277093RR0001
www.ostomycanada.ca/ our-board-and-staff/
As I sit down to write my editorial, I am feeling quite reflective of the time that has passed since the last magazine was published. I would like to offer readers an apology for the lateness of the past few magazines. I have begun to recognize that perhaps I say, ‘sure, yes I can do that for you’, too often when Ostomy Canada is involved. We all have a passion to bring more awareness to people who have an ostomy who are living life to the fullest! The next magazine will be somewhat delayed as well and it will have fewer pages in an effort to get caught back up to our regular timeline. If you are able to help in any way, please see the ‘ask’ below. The magazine is short on content. We have a great editorial team but finding the content is very time consuming with only myself seeking it out. As supporters, please send any ostomy-related stories my way, and I will follow the lead. Kindest of thanks.

Having had several ET’s and now NSWOCs involved in my medical care has been incredible. Most of us feel an absolute respect and love for NSWOCs but especially our own.
The year has been going by at lightning speed. I was honoured to be asked to be the keynote speaker at the NSWOCC 43rd national conference titled, Rising to the Challenge, hosted right here in Calgary. This title was aptly appropriate because I really found myself needing to engage in a lot of positive self-talk to try to keep my nerves under control; public speaking is not my strength! I was asked to share my evolution from being diagnosed with a chronic illness, Crohn’s disease, in the mid 80’s, which had me living in a shroud of silence and secrecy to transforming in 2006 and continuing till this date and into the future. I became an advocate who shouts from the rooftops to raise awareness and help eliminate still-existing stigmas surrounding ostomy surgery. I spoke about how I use available platforms and take opportunities in order to educate and create awareness wherever I go! If you have ridden in my car, you know that usually involves sitting on a stack of Ostomy Canada magazines. Not only are they my pride and joy, but I really do tend to meet a lot of ostomates in my every day life.
I talked about my involvement with Ostomy Canada magazine as well as about being an administrator for Ostomy Canada youth camp, having just had my 18th year as a volunteer mentor. These are two very busy positions to be involved in, even though I wouldn’t trade them for the world, some help would be welcome! Having taken control of my own life, I have learned that I can validate myself, that I don’t need to hide or feel shame, that I am not a burden, that my ostomy not only saved my life but it has enabled me to live as ‘normal’ of a life as I ever could.
Having had several ET’s and now NSWOCs involved in my medical care has been incredible. Most of us feel an absolute respect and love for NSWOCs but especially our own. They are not only nurses who are specialized in the field of ostomy care, but they are friends who are there to not only pick you up when you fall but to build you back up when you need it.
A big YAHOO goes out to the organizing committee and all those
in attendance. I believe there were approximately 400 people there and what a fun and lively group they all are! Just off the heels of the conference, I found myself visiting Vancouver for my first time! A big part of being a volunteer mentor at youth camp is striving to make connections as well as making an impression. So when a camp alumni, who has recently graduated from medical school invites you to their wedding, you have to wipe away the tears that are blurring your vision so you can reread the invitation again and again! What an amazing trip! My travel partner was one of my besties, and fortunately Janet has a sister-in-law who resides very close to the wedding venue. She was an amazing host who took us all around so I could get a good look at Vancouver! We flew out four days in advance and then raced home to begin the two-week countdown for youth camp. Our busiest time of the year. Janet and I are an amazing team and this year really proved that. Our entire team of volunteers and NSWOCs came together in ways I have not experienced before. There was a heatwave happening in Calgary during camp week, one of the hottest weeks on record. So, can you guess where I am going with this? …Heatwave, 39 kids with ostomies, outdoor activities, high energy programming, dehydration with campers, all contributed to myself and a couple of other volunteers taking trips the 50 minutes from camp to Calgary hospitals, four times! Everyone was fine in the end and said that the heat and the water fights led to the amount of fun they had. I would like to thank all of the sponsors and donors who came through this year with ‘loot’ for the kids. The kids were given ball caps from Ten Aces Medical and Ostomy Canada provided t-shirts, ballcaps, water bottles, and cinch bags to carry their supplies with them. As well, Coloplast donated ostomy kits that the campers immediately began switching their products from their makeshift kits to an ostomy specific kit that also had a different stuffie attached to each of them. In the next magazine, there will be an article telling all about camp 2024 and giving thanks to many others sponsors and donors! We appreciate each and every one of you, especially those of you who took the time to come out and ‘play’ with the campers, kicking off day one! n
Lisa Gausman, Senior Editor

EXECUTIVE DIRECTOR’S MESSAGE
Dear Friends and Supporters of Ostomy Canada Society, As we continue our journey to empower and support individuals living with ostomies across the nation, I am thrilled to share with you the latest updates and initiatives from Ostomy Canada Society.
Firstly, I’m excited to announce that Ostomy Canada Youth Camp was a very successful week. The campers happily reunited with friends made in past years and had a ton of fun forming new friendships and memories. We look forward to the thank you cards, and pictures and videos of all the excited faces!
In addition, I’m proud to introduce our new Ambassadors’ Initiative. This program intends to expand our reach and impact by engaging passionate individuals who are committed to raising awareness and promoting ostomy care and support. Look for their stories and more in the magazine and newsletters.

awareness campaign for Ostomy Canada, allowing us to continue our mission of improving the lives of individuals living with an ostomy This year was supposed to be World Ostomy Day but that has been postponed to 2025.
I’m proud to introduce our new Ambassadors’ Initiative. This program intends to expand our reach and impact by engaging passionate individuals who are committed to raising awareness and promoting ostomy care and support.
Par ailleurs, c’est avec fierté que je vous présente notre nouveau programme d’ambassadeurs, dont l’objectif est d’accroître notre rayonnement et notre retentissement en mobilisant des gens passionnés et motivés à faire de la sensibilisation et à promouvoir les soins de stomie et le soutien des personnes stomisées.
Furthermore, I’m delighted to unveil the revamped Ostomy Canada website. This modernized platform will serve as a comprehensive resource hub for those living with ostomies, caregivers, and healthcare professionals alike, offering valuable information, support, and community connections.
We are also thrilled to continue our partnership with the Nurses Specialized in Wound, Ostomy, and Continence Canada (NSWOCC) and our participation in their Summit and national conferences. This ongoing collaboration will enable us to further enhance the quality of care and support we provide to our community.
Additionally, I’m pleased to report that our Visitor Training Program continues to thrive. This vital program ensures that individuals facing ostomy surgery have access to knowledgeable and compassionate peer support during their journey.
On a somber note, I extend my heartfelt condolences to the Ivol family on the passing of Roger Ivol. Roger was not only a longterm supporter but also a valued board member of Ostomy Canada. His dedication and contributions to Ostomy Canada, locally and nationally, will always be remembered and cherished.
Lastly, mark your calendars for Step Up for Ostomy on October 5th. This annual event serves as a vital fundraiser and national
In closing, I want to express my gratitude to our chapter and group members, volunteers, and supporters for their unwavering commitment to our mission. Together, we will continue to make a meaningful difference in the lives of those affected by ostomies.
Warm regards,
Dana Ypma Executive Director, Ostomy Canada Society
*at the time of publication, Dana accepted a new role outside of Ostomy Canada Society. She extends her warmest wishes and best of luck for the future of OCS
Chers amis et sympathisants de la Société canadienne des personnes stomisées, Alors que nous poursuivons notre mission de soutenir les personnes vivant avec une stomie à travers le pays et de les aider à vivre pleinement, c’est avec un grand enthousiasme que je vous fais part des dernières actualités et initiatives de la Société canadienne des personnes stomisées.
Tout d’abord, je suis très heureux d’annoncer que le Camp des Jeunes a été une semaine réussie. Les jeunes étaient certainement ravis de retrouver leurs amis du camp et ont eu beaucoup de plaisir à nouer de nouvelles amitiés et à se forger de beaux souvenirs.
Nous avons déjà hâte de voir les cartes de remerciements, les photos et les vidéos de toutes leurs mines réjouies!
Par ailleurs, c’est avec fierté que je vous présente notre nouveau programme d’ambassadeurs, dont l’objectif est d’accroître notre rayonnement et notre retentissement en mobilisant des gens passionnés et motivés à faire de la sensibilisation et à promouvoir les soins de stomie et le soutien des personnes stomisées. Surveillez leurs témoignages et leurs articles dans le magazine et les infolettres!
Je suis également ravie de vous dévoiler le nouveau visage du
site Web de la Société canadienne des personnes stomisées. Notre plateforme modernisée deviendra un centre de ressources complet aussi bien pour les personnes stomisées et leurs aidants que pour les professionnels de la santé; ils y trouveront de précieux rensei gnements, du soutien et une communauté.
Nous sommes en outre emballés de poursuivre notre parte nariat avec l’organisme Infirmières spécialisées en plaies, stomies et continence Canada (ISPSCC) et de participer à leur sommet et à leurs conférences nationales. Cette collaboration suivie nous aidera à améliorer encore davantage la qualité des soins et du soutien que nous offrons aux membres de notre communauté.
De plus, je vous informe avec plaisir que notre programme de formation des visiteurs continue de prospérer. Ce programme cru cial permet d’assurer que les personnes en voie de subir une stomie ont accès au soutien de pairs expérimentés et bienveillants tout au long de leur parcours.
Sur une note bien triste, j’aimerais transmettre mes plus sin cères condoléances à la famille de Roger Ivol, qui nous a quittés récemment. Roger était non seulement un sympathisant de longue date, mais aussi un membre estimé du conseil d’administration de la Société canadienne des personnes stomisées. Son dévoue ment et ses contributions à notre organisme, à l’échelle tant locale que nationale, resteront à jamais dans nos mémoires et dans nos cœurs.

Enfin, c’est le temps d’inscrire à votre agenda la date du 5 octobre, jour de notre campagne de sensibilisation nationale Step Up for Ostomy. Cet important événement annuel est l’occasion pour nous de recueillir les fonds dont notre organisme a besoin pour poursuivre sa mission d’améliorer la vie des personnes stomisées. Une Journée mondiale de la stomie devait par ailleurs se tenir cette année, mais l’événement a été remis à 2025.
En terminant, j’aimerais remercier les membres, les bénévoles et les sympathisants de nos associations et groupes pour leur engagement indéfectible envers notre mission. Ensemble, nous continuerons de changer la vie des personnes stomisées et de leurs proches.
Cordialement,
Dana Ypma
Directrice générale,
Société canadienne des personnes stomisées
*au moment de la publication, Dana a accepté un nouveau rôle à l’extérieur de la Société Ostomie Canada. Elle vous présente ses vœux les plus chaleureux et bonne chance pour l’avenir d’OCS.
Personalized Ostomy care
We have a variety of ostomy brands and products.
Speak with your Pharmasave pharmacist.
As the days grow longer and the sun shines brighter, I hope you’re all basking in good health and high spirits as we anticipate the arrival of the sun-kissed days of summer. Summer is a season of vibrancy and adventure, where we embrace the warmth and cherish moments of leisure and joy.
The Board of Directors at Ostomy Canada Society (OCS) has been working hard at continuing the growth of our governance and looking to our Executive Director to manage the operations of the society.

The Governance Committee is responsible for the development of the Board’s governance framework, by-laws, policies, guidelines, and Standing Committees’ Terms of Reference which reflect current best practices. The committee also has the oversight of Board competencies, composition, and succession planning, along with development of orientation and continuous Board development programs for Directors.
The Governance Committee has been reviewing, updating, and developing new policies that reflect the work of the society. They have also taken on updating our by-laws that will incorporate some of the changes that were made around the definition of membership. We look forward to having a final draft of the By-laws and finalized policies ready for the AGM in September.
OCS has also incorporated a Finance Committee that serves as an advisory working group on all matters related to the budgeting, investment, and allocation of the Society’s Funds. This is a vital committee that is responsible for overseeing the development of an appropriate financial and investment strategy subject to approval of the Board of Directors.
Following the AGM in September, we will be embarking on developing a new Strategic Plan for 2025. We look to engage the chapters and peer support groups in the development of the plan. Stay tuned for more information on this.
The Board is proud of the work we are doing to enhance the lives of everyone living with an ostomy. I would like to express my gratitude to the volunteers in the chapters and peer support groups across the country for your ongoing support and collaboration dedicated to all people living with an ostomy, and their circles of support, helping them live life to the fullest. Together, we can create an environment that promotes growth, well-being, and success for every member of our community.
All the best,

Jacqueline Bloom Board Chair, OCS
Editor’s note: The Chair’s column was submitted in the beginning of Summer, prior to the delays.
À l’approche de la belle saison, en cette période où les jours s’allongent et où le soleil brille de plus en plus fort, j’espère que santé et joie de vivre sont au rendez-vous. L’été est une saison qui appelle à la vie et aux aventures, où il fait bon profiter pleinement de la chaleur et se repaitre de moments de détente et de joie. Le conseil d’administration de la Société canadienne des personnes stomisées travaille fort pour assurer l’amélioration continue de notre gouvernance et s’appuie sur la directrice générale pour la gestion des activités de l’organisme. Le comité de gouvernance a la responsabilité d’établir le cadre de gouvernance du conseil et ses règlements administratifs, politiques et lignes directrices, ainsi que les attributions de ses comités directeurs, en tenant compte des pratiques exemplaires actuelles. Le comité assure aussi la supervision des compétences du conseil, sa composition et la planification de la relève, tout en veillant à son orientation et aux programmes de perfectionnement continu de ses membres.
Le comité de gouvernance a entrepris d’examiner et de mettre à jour les politiques et d’en établir de nouvelles afin de mieux refléter le travail de notre organisme. Il a aussi commencé à revoir les règlements administratifs afin d’y intégrer certains des changements apportés à la définition du statut de membre. Nous avons hâte de présenter la version définitive des règlements administratifs et des politiques à l’assemblée générale annuelle de septembre.
La Société canadienne des personnes stomisées a aussi mis sur pied un comité des finances qui a pour mission de servir de groupe de travail consultatif quant à toutes les questions qui concernent l’établissement des budgets, les investissements et l’allocation des fonds de l’organisme. Il s’agit d’un comité essentiel qui a la responsabilité de superviser l’élaboration d’un plan financier et d’une stratégie d’investissement adéquats aux fins d’approbation par le conseil d’administration.
Après l’assemblée générale annuelle qui aura lieu en septembre, nous amorcerons la préparation d’un nouveau plan stratégique pour 2025. Nous entendons solliciter la participation des associations et groupes de soutien dans le cadre de cet exercice. Restez à l’affût pour en savoir davantage à ce sujet.
Le conseil est fier du travail qu’il accomplit pour améliorer la vie de toutes les personnes stomisées. En terminant, j’aimerais remercier les bénévoles des associations et groupes de soutien à travers le pays qui aident les personnes stomisées et leurs proches à profiter pleinement de la vie pour leur soutien continu et leur dévouement. Ensemble, nous pouvons créer un environnement qui favorise l’épanouissement, le bien-être et la réussite de chacun des membres de notre communauté.
Meilleures salutations,
Jacqueline Bloom
Présidente du conseil d’administration, Société canadienne des personnes stomisées
OSTOMY CANADA SOCIETY’S MISSION STATEMENT
Ostomy Canada is a non-profit volunteer organization dedicated to all people living with an ostomy, and their circles of support, helping them live life to the fullest through advocacy, awareness, collaboration and support.
OUR VISION STATEMENT
Canada’s voice and agent of change for people living with an ostomy
SOCIÉTÉ CANADIENNE DES PERSONNES STOMISÉES
ÉNONCÉ DE MISSION
La Société Canadienne des Personnes Stomisées est un organisme bénévole sans but lucratif qui se consacre à toutes les personnes vivant avec une stomie et à leurs cercles de soutien, en les aidant à vivre pleinement leur vie grâce à la défense des droits, à la sensibilisation, à la collaboration et au soutien.
VISION
La voix et l’agent de changement du Canada pour les personnes vivant avec une stomie

Greetings from the Nurses Specialized in Wound, Ostomy, and Continence Canada (NSWOCC)! As usual, there is a lot going on in the wound, ostomy and continence world, all with the goal of improving patient care and patient outcomes.
NSWOCC continues to work hard at improving access to Nurses Specialized in Wound, Ostomy and Continence (NSWOC) nationally. Summits educating health care administration, management, and provincial government officials / members on the role of the NSWOC and the beneficial impact on patient care that NSWOC involvement brings continue. To have quality care for persons living with an ostomy, access to the high level expertise of an NSWOC is essential. Lessons are learned with every Summit and slowly results are starting to be seen with some students being supported to attend the WOC Institute. Summits have happened in Nova Scotia (Fall 2022), New Brunswick (June 2023), Alberta (October 2023), Ontario (June 7, 2024).

Several projects have been completed over the past months that may be of interest to Ostomy Canada members. The position statement on pre-operative stoma marking has been completed and is available on the NSWOC.ca website. All of us understand how crucial proper stoma placement can be in future quality of life and independence. Best Practice Recommendations on Parastomal Hernia Prevention – Assessment and Management is also available on the website. Parastomal Hernias can also have significant impacts

on quality of life. The teaching booklets for Ileostomy, Colostomy, and Urostomy have all been updated and revised. Accurate and timely education tools are important in such life changing situations.
In development at the association at present is a project on Virtual Consultations for Wound, Ostomy, and Continence. The impact such an initiative could have for patients living in underserviced areas is tremendous. There could also be a role in the care of patients with significant mobility issues for such a program. It is important to remember that all work at the NSWOCC happens with diversity and inclusivity as priorities.
Members of the NSWOCC and guests had an educational and fun-filled time at our annual conference May 1 to 5 in beautiful Calgary, Alberta. We all participated in “Rising to the Challenge”. I am happy to have seen members of Ostomy Canada as well as the Calgary Ostomy chapter in attendance and we enjoyed your participation.
This is my last submission to Ostomy Canada as NSWOCC President. I have enjoyed being in contact with all of you, but at the Annual Member’s Meeting in Calgary, I handed over the presidency to Corey Heerschap of Barrie Ontario. I know he will be terrific at the job. Thank you everyone.


by Cathy Harley, NSWOCC CEO
The Calgary Hyatt Regency Hotel was the venue for the 2024 NSWOCC national conference which took place May 1 to 5, 2024. We were thrilled to have Ostomy Canada participating with an exhibit table throughout the conference. It was good to be able to speak with Dana Ypma, the Ostomy Canada Executive Director and representatives in order to learn about current activities.

One of the highlights of the conference was having Lisa Gausman as the opening plenary keynote speaker. Lisa engaged the audience with her straight forward description on both the challenges and the positive learning from living with an ostomy. Listening to her story was not only inspirational, it was motivating for all in attendance. Lisa demonstrated the value she brings to Ostomy Canada as the Senior Editor of Ostomy Canada magazine and as the Administrator of the Ostomy Youth Camp which is held just outside of Calgary, Alberta. We thank Lisa for her willingness to share her experience with the conference delegates.

was a room where all of the posters focusing on wound, ostomy and continence topics were displayed and the honoured corporate partners also had the opportunity to feature key technologies during the event. The participants had time to learn as they made their way through the poster and product displays.
One of the highlights of the conference was having Lisa Gausman as the opening plenary keynote speaker. Lisa engaged the audience with her straight forward description on both the challenges and the positive learning from living with an ostomy.
The Sing, Stomp and Honky Tonk Lip Sync Event was enjoyed by all who attended. There were nine groups which were a mixture of Nurses Specialized in Wound, Ostomy and Continence (NSWOCs), Skin Wellness Associate Nurses (SWANs) and Industry Partners who formed teams that performed country and western themed songs. The lip synching and dancing was taken to a new level this year and it was wonderful to see so many smiling faces. The grand winner of this event was the NSWOCC Indigenous Core Program and Seven Generations Medical who was their industry partner.
Ostomy education was a part of this national conference. There was a session on basic ostomy management which was attended by many nurses who were seeking foundational education and it included proper product selection. The hernia workshop provided valuable information on the prevention and management of hernias and another education session focused on fistulas and complex cases including education on high output ileostomies, anal fissures and prolapses.
A special poster session event was held on Thursday, May 3, 2024 called “Posters, Punch and Products”. There
The annual NSWOCC Graduation and Conference banquet took place on Saturday May 4, 2024. This included the parade of NSWOC and SWAN graduates and the presentation of their graduation diplomas. This event also includes the presentation of numerous awards for academics and leadership. We were proud to see the recipients of the Ostomy Canada Awards during the NSWOCC annual Graduation and Conference banquet. The two winners of these Ostomy Canada financial awards were Alyson Wood and Ashley Hogan. We would like to congratulate these two graduates of the NSWOC Program.
We look forward to having Ostomy Canada attend our 2026 national NSWOCC conference which is taking place at the Hotel Bonaventure in Montreal from May 21-24, 2025 in Montreal, Quebec. The theme will be “IDEAS” – Inclusivity, Diversity, Equity and Accessibility – Shared” n
Please stay tuned to www.nswoc.ca for further information.


Greetings!
For many years we’ve all wished that more people knew about living with an ostomy as well as the organizations that provide support and resources such as UOAA. This year we are taking more steps to help improve ostomy awareness and education. We recently produced a Public Service Announcement commercial in both English and Spanish. Getting this commercial aired on TV free of charge is still a challenge in the United States so we are also looking at more affordable distribution options such as streaming TV channels. You can view and share the videos on our YouTube and social media. The message is a simple one and features one of our advocates, Keyla Caba, going about daily life as an ostomate. She just happens to be a model! www. ostomy.org/ostomy-advocates-in-the-room-where-it-happens/. We hope this chips away at existing stigmas and raises ostomy awareness to a broad audience of viewers.

brother who just had colostomy surgery!
Other new online resources this year are the Living with an Ileoanal Pouch Guide and soon, new webpages dedicated to children, teens and young adults living with an ostomy will be available.
We have also heard the cry that there are still too many medical professionals who do not know enough about ostomy care. Our Advocacy and Education teams are diligently working on many strategies to properly educate medical professionals such as Home Health and Floor Nurses on proper care for the ostomy patient.
For individuals and medical professionals who may want to start an ostomy clinic in their area, our advocacy team has developed a new educational course. The online Roadmap to Establishing Outpatient Ostomy Services, and our hope is that this will increase the likelihood of more outpatient clinics being opened and improve access to quality ostomy care.
I’m pleased that when we reach new people, we now have an updated New Ostomy Patient Guide to send to them and their caregivers. Since 2020 we have mailed over 50,000 copies of this publication that is also available on our website www.ostomy.org.
We take pride in this service and recently had a 91-year-old woman, who has had an ostomy for 56 years and did not know about UOAA, call our office to request one for her 96-year-old

Our next UOAA National Conference will be August 14-16, 2025 in Orlando, Florida! You’re all invited to join us at the Hyatt Regency Grand Cypress Resort for fun and education. Save the date!
UOAA President Cheryl Ory





August 9, 1942 – February 19, 2024
By Janet Paquet
It is with sadness that we announce the death of Roger Ivol, a former director of Ostomy Canada Society, Past President of Ostomy Hamilton, a long-time supporter of Friends of Ostomates Worldwide Canada and a great friend to many in the ostomy community.
I struggle on how to give tribute to a man who has done so much for our association, both locally and nationally. How can I accurately convey how monumentally important his contributions and selflessness have been to the many lives he touched?
The best way for me to express how Roger has affected so many ostomates’ lives is to tell you about the impact he had on my life.
In 1996, I was in my twenties, scared, a new mum to a premature baby, and I had just undergone ostomy surgery. I had no idea how I was going to cope. My in-laws were friends of Roger and Ann. They all taught in the school board together and my fatherin-law had met Roger when they were Cadet Officers at Camp Ipperwash back in 1965. I had just returned home from the hospital and was already having trouble with my ostomy. My mother-in-law just happened to run into Roger at a grocery store and told him of my troubles finding an appliance that would stay on for more than a day, and how I was not coping very well. Within the hour Roger had dropped his groceries off at home and was at our house and became my ‘ostomy visitor’.
I learned so much from that first visit. He answered every question I had and assured me that, given time, it would get better. I have a distinct memory of Roger telling me about the great information and assurances he had received from his visitor, Paul Penny, and how this experience helped him to accept his new way of elimination.
I had no idea what to expect when Roger picked me up and took me to my first Ostomy Hamilton monthly meeting, and I certainly

never thought that I would become an active participant in the association. Obviously, I underestimated the profound affect Roger and what we now lovingly refer to as the ‘Roger vortex’ would have on my life.
Passion. It’s just one of the many words I can use to describe what Roger had, and what he brought out in people. He had a passion to learn, and a passion to help. Roger inspired people. He inspired me.
He inspired me to become involved, not only with Ostomy Hamilton but with Ostomy Canada as well. He recognized skills in me that I wasn’t fully aware that I had. He first got me involved as a typist on the UOACanada Talks, a precursor to the Ostomy Canada magazine, of which Roger was the founding editor. Eventually, Roger once again inspired me to become his assistant editor, then senior editor, then conference program book editor and convinced me that I would be a good fit on both the Ostomy Hamilton and the Ostomy Canada board of directors. Along this journey, Roger was always there for me, always had great advice and helped guide me. As recently as this past fall, I had called Roger to ask his advice on running the ostomy visitor training. He was passionate about visitor training and helped set up the national program. He believed that this program was one of the most valuable resources that the association offered.
Roger inspired me to become pro-active in the ostomy community, and he encouraged me to become involved in the youth camp, which is my biggest passion. He tirelessly worked to send hundreds of kids from south-western Ontario to Ostomy Canada Youth Camp; he recognized the value that camp brings. These children’s lives have been changed because Roger actively sought them out and fundraised to send them to camp.

Roger was the change from Mahatma Gandhi’s famous quote; “Be the change that you wish to see in the world.” This quote serves as a call to action that empowers people to take control of their lives and become agents of positive change. Roger embodied the values and principles we wish to see in the world. He took responsibility and led by example and by doing so, he inspired so many people to join in the quest for a better world.
I know for a fact that if I hadn’t met Roger my life would have been on a very different path, I would not be the person I am without having his guidance and support. Under his mentorship I am reminded that everyone, even myself, have the ability to create positive change in my own life as well as in the community. I will miss my friend and my mentor immensely, and the entire ostomy community has lost a valued resource.
With gratitude and respect to a dear friend and mentor.
Janet Paquet, Co-President, Ostomy Hamilton; Ostomy Canada Youth Camp Administrator; Vice-Chair Ostomy Canada Society
A tribute to a friend and colleague by
Pat Cimmeck
Roger and I met in the early 1990’s at a conference in the United States.
We worked together for many years both as board members on United Ostomy Association of Canada (now Ostomy Canada Society),
FOWC, the national magazine, youth camp and international ostomy interests. Through the years we developed a friendship inside the various organizations as well as outside.
Roger was an avid fisherman and he spent leisure hours fishing in different areas around Ontario, the US and abroad.
Fishing was a stress relief and Roger was happiest spending time with his rod and reel. My husband is also a fisherman. He and Roger spent many hours after various conferences enjoying the outdoors. The Ivols were gracious hosts and we enjoyed their hospitality while we were guests in their home. After a conference in our home city of Calgary, they were able to spend time with us as part of their holiday.
Roger always wanted to experience fishing on the Bow River, famously known worldwide for trout fishing. The guys didn’t catch much that day but they did enjoy the getaway. Whether spending time together in Canada or abroad, we always enjoyed Roger’s sense of humor, knack for storytelling and gratitude and enjoyment of life.
He gave many years of devotion to ostomy awareness, patient support and truly showed living life to the fullest. This devotion will be greatly missed. He was the personification of a dedicated volunteer and my husband I are grateful to have had the opportunity to share his friendship.
Pat is the President of Calgary Ostomy Society and a Director for FOWC
Words of fondness for a valued friend from the President of Friends
FOWC has lost one of its long-time supporters, Roger Ivol, and we send our sympathy to his wife, Ann, and to his family. For many years, Roger accepted and collected donations of products from individuals, hospitals and retailers. He and Ann would often pre-sort these items, and then bring a full carload (or at times two carloads) to wherever the sorting and packing would be. Roger would then help with the sorting and packing, putting in a full day before driving the distance back home. As his health began to fail, he was no longer able to work a full day, but still supported the charity with collection and donation of products. We will miss his gentle spirit, and genuine desire to help give the gift of dignity to those less fortunate.
Témoignage d’affection pour un ami précieux, de la part du président de FOWC par Lorne Aronson FOWC a perdu un sympathisant de longue date, Roger Ivol, et nous tenons à transmettre nos plus sincères condoléances à sa femme, Ann, et à ses proches. Pendant de nombreuses années, Roger a accepté et recueilli les dons de produits offerts par des particuliers, des hôpitaux et des détaillants. Ann et lui faisaient souvent un premier tri de ces dons avant d’en apporter une voiture pleine (parfois deux) à l’endroit où le tri et l’emballage devaient se faire. Roger participait ensuite au tri et à l’emballage toute la journée, avant de reprendre la route pour rentrer chez lui. Quand sa santé a commencé à décliner et qu’il n’arrivait plus à travailler toute la journée, il a quand même continué à soutenir l’organisme en recueillant des dons.
Sa bienveillance et son désir sincère d’apporter la dignité aux moins fortunés nous manqueront.
Roger, My Friend
I was at the Ostomy Canada Society Congress when I first met Roger Ivol. Right away, I felt this was a man with great passion to help people. Shortly after this first meeting, we began to exchange opinions, ideas and ways of doing things, the main goal of which was undoubtedly to help and support people living with an ostomy.
He responded affirmatively to all the invitations sent to him for the provincial conventions of the Association québécoise des personnes stomisées (AQPS) and we spent a lot of time together discussing and imagining solutions to common problems experienced by ostomy patients in Quebec and Ontario.
As time went on, our relationship quickly turned into a friendship and we discovered that fishing was our common passion. Roger came to my house to fish for landlocked salmon (Atlantic salmon trapped behind hydroelectric dams) on Lake Kénogami. Last year, I accepted Roger’s invitation to fish and he taught me how to fly fish. We spent several days teasing brown trout along the rivers in his area that drain into Lake Erie. When I left, Roger gave me the fly-fishing rod with which this teacher had so kindly introduced me to this noble sport.
As time went on, our relationship quickly turned into a friendship and we discovered that fishing was our common passion.
Avec le temps qui passait, notre relation s’est vite transformée en amitié et nous avons découvert que la pêche était notre passion commune.
Roger has participated in many “Living with an Ostomy” days in the Gatineau area near Ottawa. These days are organized by the AQPS in regions where there is no regional association of persons with ostomies. In January 2024, Roger advised me that his health had deteriorated and that he would not be coming to our February event in Gatineau. On February 19, 2024, I went to his house to spend a few days with my friend and unfortunately Roger left... he probably went fishing with his ancestors.
Roger, if one day you hand me your line, I will know that it is time for me to join you and it will also be time for me to go fishing with you, my friend, and with my ancestors.
Jude
Ruest your friend - (Translation by Réal Lamarche)
Jude is the President of AQPS
J’étais au congrès canadien des personnes stomisées lorsque j’ai rencontré Roger Ivol pour la première fois. Toute suite, j’ai senti en cet homme une grande passion pour aider les gens. Peu de temps après cette première rencontre, nous avons commencé à échanger nos opinions, nos idées et nos façons de faire dont le but principal était sans contredit l’aide et le soutien aux personnes stomisées.
Il a répondu affirmativement à toutes les invitations qui lui étaient adressées pour les congrès provinciaux de l’Association québécoise des personnes stomisées (AQPS) et nous passions beaucoup de temps ensemble à discuter et à imaginer des solutions aux problèmes fréquents vécus par les personnes stomisées du Québec et de l’Ontario.
Avec le temps qui passait, notre relation s’est vite transformée en amitié et nous avons découvert que la pêche était notre passion commune. Roger est venu chez moi pêcher la ouananiche (saumon de l’Atlantique emprisonné derrière les barrages hydro-électriques) sur le lac Kénogami. J’ai accepté son invitation pour la pêche l’an dernier et Roger m’a appris à pêcher à la mouche. Nous avons passé plusieurs journées à taquiner la truite brune le long des rivières de sa région qui se déversent dans le lac Érié. À mon départ, Roger m’a remis la canne à pêche à moucher avec laquelle ce professeur m’avait si gentiment initié à ce noble sport.
Roger a participé à plusieurs des journées « Vivre avec une stomie » dans la région de Gatineau près d’Ottawa. Ces journées sont organisées par l’AQPS dans les régions où il n’y a pas d’Association régionale de personnes stomisées. En janvier 2024, Roger m’a avisé que sa santé s’était détériorée et qu’il ne viendrait pas à notre activité de février à Gatineau. Le 19 février 2024, je me suis rendu chez lui pour passer quelques jours avec mon ami Roger et malheureusement Roger est parti … Roger est probablement parti pêcher avec ses ancêtres.
Roger, si un jour tu me tends ta ligne, je saurai que c’est le temps pour moi de te rejoindre et ce sera pour moi aussi le temps de retourner pêcher avec toi, mon ami, et avec mes ancêtres.
Jude ton ami
Jude est le président de AQPS – Association Québécoise des personnes Stomisées

Karen Bruton RN BScN IIWCC MCISc-WH NSWOC WOCC(C)
QNext month, my 78-year-old mother is having a colostomy created due to rectal cancer. I have never heard of ostomies before – what do I need to know to prepare myself to help her post surgery?

AThis is a great question! As everyone manages differently in life, modify the following tips to meet your needs.
For you as the caregiver and for your mom as a patient:
1. 1 If your mother is in favor and you are able, plan to attend her medical appointments to both ask questions and give her needed support.
• Educate yourselves as to what a colostomy is. Ostomy Canada Society website (https://www.ostomycanada.ca ) has a wealth of information. While learning about ostomies is vital, don’t try to spend a lot of time researching colostomy care; that will come with time.
• Ostomy Canada Society has a Visitor Program. Discuss potential options with your mother. Visitors are volunteers with an ostomy who have received training for this program and will come to visit you and your mother. If an in-person visit is not available, often visitors will reach out by phone or email. There are excellent resources on the website page (https://www.ostomycanada.ca/ ostomy-canada-visitor-program/ )
2. Mental health is most important for both of you so ensure you get enough nightly sleep and even take catnaps.
3. Ensure you both eat well-balanced meals, which includes fresh fruits and vegetables, protein and carbohydrates as required to meet the Canada’s Food Guide recommendations (https://foodguide.canada.ca/en/ ). Don’t forget to stay hydrated, drink water. You should both keep a water bottle close by as a reminder.
4. Maintain an exercise routine or create one, even if it is a daily walk around the block.
As a caregiver you need support too! Ensure you discuss your feelings and concerns with a friend or a loved one to give you much needed support as you will need this!
Being mentally prepared is crucial. Before your mother is scheduled, learn about how to care for a colostomy following surgery from the NSWOC, the hospital nurse, and/or the homecare nurse.
QI am a middle aged male who has had an ileostomy for 10 years. I have a short bowel and an inoperable hernia. I seem to be having a lot of loose stools lately so I am changing my appliance more often. As well the hernia makes it more challenging for the appliance to adhere to the skin. I have lost 15 pounds in two months. My physician says to eat more but otherwise they have provided no other advice. I live in Oshawa, Ontario. What can I do?
AI empathize with the complexity of your health situation and commend you for seeking help. Here are some steps to access the care you need:
1. Dietitian Consultation: While dietitian services are generally not covered by Ontario Health Insurance Plan (OHIP), they might be included in private health plans. For dietitians in the Central East region, you can explore this link: Dietitian Services – Central East. OHIP-covered local programs might exist, but you’ll need to investigate through your physician.
2. NSWOC Nurse Access: Contact the Central East office for homecare at Central East | Home and Community Care Support Services or call 1-800-263-3877. Be assertive in your request for a Nurse Specializing in Wound, Ostomy, Continence (NSWOC) consultation. Explain your ileostomy complications, diarrhea, hernia, and the impact on your lifestyle. A physician order is not necessary, but detailed information will support your case. Initially, a general nurse might conduct an assessment, but insist on seeing a NSWOC nurse. If one is not available, then look for a nurse with experience in dealing with ostomies.
3 . Outpatient NSWOC Clinics: Although NSWOC outpatient clinics are few in your area, the Durham Medical store in Oshawa may have an NSWOC nurse available for appointments. Check their current services as the NSWOC’s presence may not be full-time.
4. Finding a NSWOC Nurse: For further assistance in locating a NSWOC nurse, visit the NSWOC website (https://memberscaet. ca/find.phtml ) or Ostomy Canada (https://www.ostomycanada.ca/ find-a-nswoc/ ).
Dealing with multiple health issues can be challenging, but the right medical and dietary guidance can significantly improve your quality of life. I encourage you to explore these options and advocate for your health needs.


It is easily one of the toughest but most gratifying things I’ve ever been through …and I wouldn’t have been able to do it without both “Shawn” the Stoma giving me my life back, and Coloplast products playing a significant role in keeping my ostomy healthy.
There was a time in my life when I thought being a father and starting a family just wasn’t in the cards for me. Especially after two decades of constantly battling, not only my body’s health issues, but also the strain it took on me mentally.
Let’s rewind a little bit. I was diagnosed with Crohn’s Disease back in high school after months of not being able to make it home without having an accident.
I felt ashamed and didn’t want to talk about it. I remember when my family doctor told me that I had Crohn’s. He almost seemed annoyed about it. Like it was too much for him to deal with. I believe that this experience with my doctor along with also being bullied in school, because of my Crohn’s, led me to feel like my disease was a burden. I spent years either hiding that I have Crohn’s from people or downplaying how badly it affected me.
I had my first surgery back in 2009 and the experience honestly had me swearing off anything surgery related later in life. I felt I was pushed into it without being heard or understood. I remember having to go for a counselling session where I first learned about ostomies and was told that there was a possibility that I could wake up with one. It freaked me out and I couldn’t handle it. One of my biggest fears was how people would look at me afterwards but if I had seen all the advocacy that I’ve seen now, it would have truly helped me understand it more back then.
I didn’t end up getting an ostomy that time, but I would end up back in the hospital within a couple of months going through renal failure. After recovering I switched GI’s and went through another whirlwind of tests trying to figure out what was stopping me from finding remission. With no answers found, I was told that maybe this was the best I was going to get and that I would never find remission. The worst part is that I believed it.
Miraculously, during this time, I met the woman who would later become my wife. Together we moved into my sister’s base-
ment suite allowing me to be close to family and to see my nephews grow up. Seeing them, I quickly realized I wanted to be a dad.
Just before COVID-19 hit, my health started to crash hard. After 20 years of dealing with IBD, nothing was helping to reduce my symptoms and phone call appointments alone just weren’t cutting it. After trying new meds and nearly bleeding out due to complications, my GI dropped me onto a new doc. I was upset and hurt but it would end up being the thing that saved me. Finally, after months of fighting, the decision was made to send me to a surgeon who would conclude that it was time to remove my colon and rectum.
I went in for surgery at Eagle Ridge Hospital in Port Moody, BC without any complications. I spent the next month of my healing process trying different bags given to me by my NSWOC at the hospital from various manufacturers before deciding on Coloplast. I had been having issues with leakage as well as bad skin reactions from all the adhesives, but when I saw the sleek design of the Coloplast bag I knew I wanted to give them a try and was ecstatic to find that together with the barrier rings, they would be the product that would prevent any further issues.
The design of the Coloplast bag made it so much easier. It made me feel confident. This is easily one of the biggest reasons why I would recommend Coloplast to any ostomate. Now, a year after living with my ostomy and through 5 months of being a new dad, I can attest that my thoughts have not changed in the slightest.
From the long nights of no sleep with the newborn stage to the bouncing, swaying, and playing with my daughter as an infant; my bag has never leaked thanks to my Coloplast SenSura® Mio 2-piece click system in light convex.
The ability to switch out my bag without having to change my baseplate has come in handy a few times. Like, when I’m introducing my favourite things to my daughter at the FanExpo convention, or going on a long road trip. The flexible Brava® Protective Ring is easy to mould around the dips and bumps of my stomach around my stoma, helping to keep my skin healthy and safe from leaks. It was such a game changer when I started using them. Especially during the first month after my daughter was born. The long sleepless nights were followed by copious amounts of coffee to which my bag continued to hold up.
Bag changes are also effortless with the help of the Brava® adhesive removal spray, making the removal of my SenSura® Mio quick and painless, letting me get back to doing what I love; looking after my beautiful baby girl. To say that Coloplast has taken the worry out of being an Ostomy Dad is an understatement.
I rarely think negatively of my stoma or feel anxious about what could happen, keeping me in the moment with my new little family which I couldn’t be more thankful for. n
Brad received compensation from Coloplast to provide this information. Each person’s situation is unique so your experience may not be the same. Reprinted with permission from Brad and Coloplast.


Hydration expert Dr. Maitreyi Raman shares valuable insights on maintaining hydration, balancing electrolytes, and minimizing output for a healthier, more vibrant life.
An ostomy can have a profound impact on your body’s ability to absorb water and stay adequately hydrated. This effect is even more pronounced if you have a high-output ostomy; an ostomy that produces more than two liters (2L) of stool per day. A high-output ostomy can have a dramatic impact on your quality of life and mental health. It can also lead to problems with weight loss, low energy, low muscle mass, difficulty absorbing nutrients, dehydration, electrolyte imbalances, and kidney stones.

It’s key to understand that the fluids you’re putting into your body may affect your ostomy output. In general, there are three categories of fluids to consider. These are isotonic, hypotonic and hypertonic fluids. Isotonic fluids contain similar amounts of water, electrolytes, and sugar compared to what naturally occurs in your blood and body fluids. Hypotonic fluids either do not have any added electrolytes or sugar, or the concentration of these is lower than that found in body fluids. In contrast, hypertonic fluids contain electrolytes and sugars that are in excess to those identified in body fluids.
Water, tea, and coffee (hypotonic fluids) and sugar-containing fluids (hypertonic fluids) such as pop and fruit juices both promote ostomy output. So, how do you stay hydrated if even water can lead to increased output? The key is to create isotonic solutions, also known as oral rehydrating solutions (ORS). Isotonic fluids have a similar sugar and electrolyte composition to the cells in your body. Therefore, when drinking these, you are at lower risk of fluid shifts in the gut.
ORS should make up most of your fluid intake. How do you know how much ORS to drink? A good starting point is to calculate your total fluid intake (TFI) goal. We recommend drinking at least 30mL/kg of total fluids per day, more if your output is higher. Twothirds or more (66%) of your fluid intake should come from ORS. So, for example, if you weigh 70kg (154lbs), then you should aim to drink at least 2100mL of fluids per day, with 1400mL of fluid being ORS. Generally, for those with high ostomy output, it’s recommended to limit free water intake to a maximum of one liter (1L) per day. On top of this 1L, you can drink about 500mL of juice, tea, and fluids that aren’t oral rehydrating solutions (ORS). Any further fluids should come from ORS, keeping in mind the two-thirds rule.
If your ostomy output is greater than 2L per day, talk to your medical provider to personalize how much fluid you should be drinking. Finally, make sure to sip on your fluids and spread out your intake evenly throughout the day. Check out this page for homemade ORS recipes. www.shortbowelsyndrome.com/Content/ pdf/Recipe Book DIGITAL.pdf
In addition to the fluids you drink, there are additional factors that affect your ostomy output. Here are some tips that can help you decrease your output.
• Limit lactose. If you have undiagnosed lactose intolerance or other food sensitivities, you may face additional challenges with increased output.
• Keep a food journal. It’s worth keeping a journal that tracks your response to certain foods.
• Limit caffeine. Caffeine consumption can increase gut motil-
ity through enhanced peristalsis, and this, combined with hypotonicity (remember, since coffee is a hypotonic fluid), further increases ostomy output, especially when consumed in high volumes.
• Wait 30 minutes before consuming solids and liquids. Eating solids and liquids together, even adding a glass of water with your meals, can lead to higher output. Liquids empty from the stomach at a faster rate than solid foods. Rapid stomach emptying contributes to enhanced outputs. Spacing out your solids and liquids optimizes gastric emptying.
• Have multiple small meals throughout the day rather than fewer, larger meals. This strategy aids in optimal gut motility, leading to decreased output.
By limiting caffeine and free water consumption, being mindful of how lactose affects your body, and implementing the strategies above, you can find ways to reduce your stoma output.

You may be aware that a diet high in fibre is good for promoting regular, solid bowel movements. However, it’s important to recognize the distinction in types of fibre. Insoluble fibre includes fruit and vegetable skins, seeds, and raw vegetables. It may irritate the GI tract, leading to abdominal discomfort, high ostomy outputs, and even bowel blockages.
On the other hand, soluble fibre helps regulate output by altering the motility of the gut. Examples of soluble fibre include fruits (with peeled skins), some cooked vegetables, lentils, psyllium, barley, and oatmeal. Additionally, supplements such as psyllium fibre
(e.g. Metamucil) can also be effective if you have trouble consuming enough fibre in your diet. On average, women need 25g of fibre, and men need 38g daily. If you plan to add soluble fibre supplements to your diet, start at half the recommended dosage and work your way up to the target dose over time. This gradual transition decreases the probability of side effects such as bloating or cramping. Talk to your medical provider to discuss fibre supplementation as an option to manage your high ostomy output. www.convatec.ca/ostomy/livingwith-an-ostomy/nutritional-advice-and-diet-tips/colostomy/
Until your ostomy output slows down, you might need an oral multivitamin and mineral supplement. Most commonly, these mineral supplements should prioritize magnesium and potassium. However, keep in mind that oral magnesium supplements can contribute to increased diarrhea. So, observe your outputs





closely and talk to your doctor about magnesium options, particularly if you have low magnesium status and cannot tolerate oral supplements.
In addition to the steps listed above, it’s important to remember that medical management also plays an important role. Always talk to your medical provider about what’s best for you; these are some strategies you may discuss:
1.Increasing Imodium. You can take up to 16mg per day spread out throughout the day. Remember to time it with your meals, taking it 30 minutes before.
2.Add Lomotil. This slows down transit and reduces stoma output. Take it 30 minutes before meals.
3.Add Codeine 15-30mg. Take it 30 minutes before meals with your other medications to reduce output. This option may not be suitable for everyone, but it works effectively if you have not responded to the above strategies.
4.Add acid-lowering therapy. For example, Omeprazole may be prescribed to reduce stoma output. http://fg.bmj.com/content/13/2/140
5.Add Octreotide subcutaneous injections. These work to reduce stoma output and are administered before food.
6.Consider IV hydration. This would take place at a day medicine clinic and may be required for those with short bowel, electrolyte abnormalities, or severe symptoms.
Maintaining your diet can be challenging. In addition to talking to your medical team, consider reviewing the following resources to learn more about diet and hydration.

•LyfeMD. This is an app developed by leading medical professionals and is a holistic guide to optimal health and well-being with a chronic condition. It has specific dietary plans and recipes for gastrointestinal (GI) diseases. It also features a physical activity, yoga, and mindfulness plan to target improved mental health. www.lyfemd.ca/
•LyfeMD’s Guide to High-Output Ostomy Nutrition. This quick-read PDF is an additional valuable resource to managing high-output ostomies. It includes information on nutrition, hydration, medications, and supplements. www.lyfemd.ca/wp-content/ uploads/2021/03/EP-Managing-your-high-output-Ostomy.pdf
•Short Bowel Syndrome’s ORS Recipes. This PDF features different ORS recipes for you to try, including the World Health
Organization’s (WHO) ORS recipe. It also has a variety of juicebased and sports drink-based recipes. www.hollister.ca/en-ca/products/ostomy-care-products/two-piece-pouching-systems/high-output-pouches/new-image-two-piece-high-output-drainable-ostomypouch
•High Output Ostomy Products. Consider this pouch system from Hollister. It’s designed specifically for managing high-output ostomies and is easily drainable. Also, check out this ostomy bag from Coloplast. http://products.coloplast.ca/coloplast/ostomy-care/ sensura-hospital-assortment/sensura-high-output-pouch/
•Magnesium and Potassium. Curious about this vital mineral and electrolyte? Check out these PDFs for more information on their role in your body. http://ods.od.nih.gov/pdf/factsheets/ Magnesium-Consumer.pdf
http://ods.od.nih.gov/pdf/factsheets/Potassium-Consumer.pdf
•Food Reference Chart. Check out this food reference chart designed for those with ostomies. It’s a great place to learn how common foods can affect your output. www.ostomy.org/wp-content/uploads/2022/02/Food_Reference_Chart_2022-02.pdf
*Unless otherwise indicated, information from this article comes from Dr. Maitreyi Raman, MD MSc FRCPC*
Source - This article was written by Erika Kana, RN, in collaboration with and based on a hydration presentation by Dr. Maitreyi Raman, MD MSc FRCPC. n
Dr. Raman is a gastroenterologist, physician nutrition specialist, and hydration expert. She is the CEO and co-founder of LyfeMD and a faculty member in the Cumming School of Medicine at the University of Calgary since 2006. She is the director of Ascend (Alberta’s Collaboration of Excellence in Nutrition for Digestive Diseases) and the national medical lead for nutrition for the Canadian Association of Gastroenterology. Dr. Raman has coauthored over 90 peer-reviewed manuscripts, many in highimpact journals, on diet, nutrition, and mind-body interventions in digestive diseases. Dr. Raman has also co-authored four books on diet and digestive health. She presents her research on international, national and provincial platforms.
Erika Kana is a Calgary-based Registered Nurse and health content writer. She began volunteering with the Ostomy Canada Connects Newsletter in 2024. She has experience in geriatric and medical-surgical nursing and specializes in emergency nursing. Her diverse nursing experiences have sparked an interest in wound and ostomy nursing. Erika regularly seeks ways to learn more about ostomy management and research.

I saw a post on the Ostomy Canada Facebook Group from Crohn’s Ostomy Life (Damien Gibson) titled - Things I Wish I Could of Told Myself when I was First Diagnosed with IBD (Crohn’s disease). Damien was happy to share the wisdom he has learned through experience;
1. Have the confidence to speak up for yourself. Trust your instincts about your own body and recognize what does or doesn’t work for you.
2. Despite the initial fear surrounding steroids or any medication, you will gradually become accustomed to them.
3. Utilize alarms to help you remember to take your medication as scheduled.
4. Living with IBD doesn’t have to hinder your activities; it may just require some additional planning.
5. Despite what you may come across online, having the right kind of supportive friends won’t result in losing friendships due to illness.
6. Take the time to identify the specific foods, drinks, and emotions that trigger your symptoms. It’s possible that you may have several triggers or none at all, but it’s crucial to tune in to your body’s signals and be open to experimenting with different dietary choices.
By Damien Gibson
7. Prepare yourself for unsolicited advice from others, which can be bothersome. Remember that you have the autonomy to decide whether or not to heed these suggestions.
8. The abundance of medical terminology can be overwhelming. Take the initiative to learn and educate yourself about IBD, becoming an informed patient who possesses extensive knowledge about the condition. This self-empowerment can greatly aid you in managing your health.
9. Recognize the importance of rest in your journey. It is not only important but necessary, particularly during flare-ups and when you’re battling fatigue. Focus on pacing yourself and avoiding overwhelming demands.
10. Practice self-compassion and kindness towards yourself. Understand that you are not responsible for causing your IBD; it is not your fault. Coping with the challenges of this condition can be burdensome, so refrain from being self-critical and instead prioritize self-care and understanding.
11 . Last thing, trust me! DO NOT smoke cigarettes. It is the worst thing you can do for IBD! n
see our website at www.fowc.ca for product donation criteria or email info@fowc.ca
By Damien Gibson
Imagine being a vibrant and energetic 23 year-old, enjoying good health and happiness. Suddenly, without any warning, you find yourself plagued by excruciating chronic abdominal pains. It feels as though your stomach is being consumed by fire, burning relentlessly from within. Simultaneously, your bowels become twisted, causing severe constipation. Your abdomen bloats, making you appear as if you are six months pregnant, and your appetite completely vanishes. Adding to the distress, you become pale, drenched in sweat due to the pain, and uncertain whether you need to vomit, defecate, or both. All of this occurs while you are working seven day,12-hour gruelling shifts spent underground in the coal mines, enduring physically demanding labor and not telling anyone what you are going through, trying to cover it up and suffer in silence so you didn’t look like someone just trying to get out of work.
In such circumstances, all you desire is to retreat to your bed, curl up into a ball, and escape the misery. Unfortunately, that option is not available to you at the time. Instead, you must summon every ounce of strength to persevere. Desperate for relief, you consume pain medication like it’s candy, oblivious to the potential consequences of contributing to further constipation. After realiz-
Imagine being a vibrant and energetic 23 year-old, enjoying good health and happiness. Suddenly, without any warning, you find yourself plagued by excruciating chronic abdominal pains. It feels as though your stomach is being consumed by fire, burning relentlessly from within.
ing that the pain wasn’t subsiding, you endured days of discomfort before reaching a breaking point and informing your boss that you needed to leave work and return home.
At the age of 23, I was thrust into the world of Crohn’s disease, a realm completely unfamiliar to me. Following a two-month hospital stay, I didn’t dwell on it much until a year later when I faced my first flare-up. This marked the beginning of a recurring cycle that persisted for years. Managing the inflammation proved to be a relentless challenge, requiring a combination of medications, frequent hospital visits, and extended periods away from work. The most difficult aspect of this experience was the overwhelming sense of isolation, as it often felt like nobody truly comprehended the depth of my struggles, be it at work or at home.

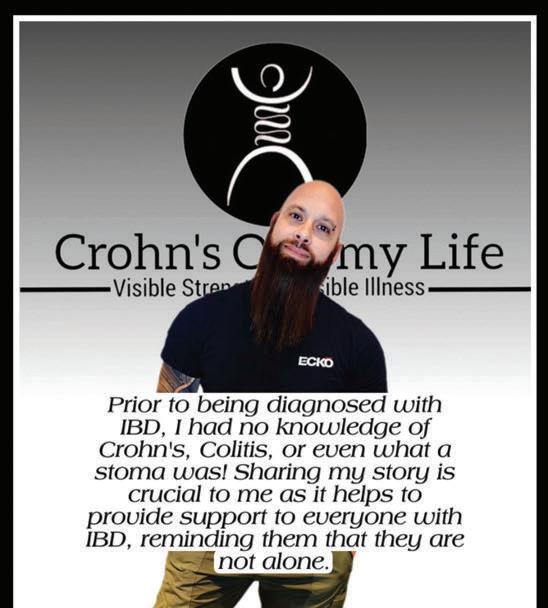

I grappled constantly with flare-ups, and in my twenties, I must admit that I was ignorant about my condition. I overlooked the warning signs and did not prioritize self-care. Fast forward to August 2022. I started experiencing intense lower back pain. This initiated a two-month odyssey spanning across three hospitals as we sought to identify the root cause. Throughout this period, I endured excruciating 10/10 on the pain scale, yet my suffering was not taken seriously by those around me. Ultimately, I was airlifted to RBWH hospital in Brisbane, Australia, for urgent surgery to address a perforated ileum and blood infections (sepsis) that had brought me to the brink of death. Upon regaining consciousness after the operation, I discovered that I now had an ileostomy bag attached to my abdomen. The emotions that overwhelmed me at that moment are beyond words. Undoubtedly, this was the most formidable challenge I have ever encountered. For weeks, the sight of my ileostomy would reduce me to tears.
Over time, I had to accept this new reality and summon the courage to progress. This period proved to be a significant mental and physical challenge for me. I experienced a notable weight loss, dropping from 92kgs (202lbs) to 69kgs (152lbs), and I realized that prioritizing fitness and exercise played a vital role in guiding me through these difficulties. This dedication has brought about positive changes in both my mental and physical health, enabling me to concentrate on the present moment.
Furthermore, I have found that openly discussing and expressing my emotions has been incredibly beneficial. I take pride in my

ostomy, as it has played a vital role in saving my life. Over time, I have learned to embrace my ileostomy and now cannot imagine life without it. While I understand that my ileostomy is reversible, I have chosen to keep it as it has greatly enhanced my quality of life and has not hindered me in any way.
I have recently departed from my home in Australia and am on an adventure in South Africa advocating for ostomy awareness, despite facing some setbacks along the way. I am making sure to take some well-deserved time to rest and recover from the ups and downs I have encountered in the past few years.
In addition to this, I am preparing to embark on a journey across various African countries to shed light on the challenges faced by ostomates living with inadequate healthcare systems. My mission is to raise awareness about chronic illnesses and the experiences of ostomates, while also seeking sponsorship from major companies to help provide essential ostomy supplies to those in need.
I have finally discovered my purpose and passion: to support, inspire, motivate, and educate others facing similar challenges, and to raise awareness for life-changing illnesses. n
Damien Gibson - @Crohn’s ostomy life – lives in Gold Coast, Queensland, Australia

When Brenda Elsagher had colorectal surgery at age 39, she made some choices about how she would live life with an ostomy.
Brenda states: after I was diagnosed with colorectal cancer in October of 1995, I made some important choices. Finding out that I would need a big operation that would require a permanent colostomy, vaginal reconstruction, and a hysterectomy was a day wrecker. I was 39 years old, married for six years, and had two children ages three and five. I was lucky in that I had never had bowel problems, like so many people who suffer greatly with Crohn’s disease and ulcerative colitis. I had a two-week pain in my butt that would not go away, even with medicated cooling pads and hemorrhoid ointment. In those years, I owned a busy hair salon and hardly had time to notice the pain, but eventually I couldn’t ignore it. I thought I just had a hemorrhoid problem, but it was much worse than that.
I chose to be as positive as possible
The day I was diagnosed with colon cancer, the doctor explained the surgery to me, and said it would be necessary to save my life. At first, I cried a lot. The next day at work, I found myself laughing and
felt a little better. Then, I chose to be as positive as possible; I wanted to see my children grow up. Over the next three weeks, I had ten different rectal and vaginal exams. I had things photographed that I never even knew about! I was quickly getting educated on body parts that I had taken for granted. I learned that my tumor may have started growing ten years earlier, and that the only thing that would have detected it was a colonoscopy; a procedure that isn’t recommended until age 50. They told me I was one in 100,000. I once won $5.00 on a scratch-off lottery ticket, so that was the closest I came to defeating the odds prior to this day.
I chose to be vocal about having an ostomy
Eventually, I made a choice to tell even more people that I had an ostomy because I thought it might save another person. I never set out to become a comedian, an author, or an international speaker. I was happy being a hairstylist. But I often joke that when my rectum was removed, it left more room for creativity. You don’t have to be vocal about having an ostomy, but it sure worked out for me. The best part is when people tell me that my urging them to get a colonoscopy saved their life. My job is done!
Brenda Elsagher has been living well with a colostomy for 25 years. She is a comic, and international speaker, and the author of five books.
Hollister is an independent, employee-owned company that develops, manufactures, and markets healthcare products and services worldwide. Hollister has been serving healthcare professionals and patients for more than 100 years - making a difference in the journey of life for people throughout the global community. n
This article was submitted by Hollister as part of their Diamond level sponsorship support of the 2023 Step Up for Ostomy Program.

Stomas come in different shapes and sizes. Choosing a skin barrer with a soft convexity design can provide exibility to t the curves of your body and move with you throughout the day. The CeraPlus TM Two-Piece Soft Convex Skin Barrier* helps achieve a secure and comfortable t that protects from leakage for all stoma types. Your barrier stays in place and helps your skin stay healthy, so you can feel free to live your life.
Priorto use,besuretoreadtheInstructions forUse forinformationregardingIntendedUse,Contraindications, Warnings,Precautions,and Instructions. Hollister,the Hollister logo andCeraPlusaretrademarksof Hollister Incorporated. ©2023 Hollister Incorporated.


By Hannah Spencer
Hi my name is Hannah, I’m 24 and I have an ostomy. This past month I was sponsored by Coloplast Canada to compete in my first ever pageant, the Miss Calgary 2024 pageant!
So what made me want to compete and how exactly did I come to the decision to compete?
The idea of being in a pageant had definitely crossed my mind many times as a child. I loved watching the show Toddlers & Tiaras and have always thought it would be cool to be in a pageant myself, but I was never presented with the opportunity and I didn’t seek it out either.
Fast forward to October of last year. I was scrolling on Instagram as I do each evening when an ad popped up for the 2024 Miss Calgary pageant. I clicked on the ad and read through the details and on a whim I filled out the application to compete. I honestly wasn’t sure if anything was going to come of it or if I was going to go through with it but I thought, “what’s the harm in applying?” A few days later I had a phone interview and was accepted as a delegate!
But why exactly did I decide to compete? The simple answer is that I wanted to represent the ostomy community, raise awareness and show the younger generation that beauty is not just about the ‘perfect body’. Beyond that I also wanted to push myself out of my comfort zone and show that I am capable of showing myself and everyone else my authentic self. If you told me when I first had surgery, that three years later I would walk across a stage in front of a crowd of strangers showing my ostomy I would not have believed you, but I did it and my younger me is so proud of myself.
Coloplast Sponsorship
Once I was accepted into the pageant I began looking for sponsors to help me with the entrance fee. I reached out to a few local businesses but that didn’t lead to anything, and then I realized that I needed to find a sponsor who was meaningful to me. So I reached out to Coloplast, as I exclusively use their products and really like them. A few weeks went by and I sort of forgot that I had approached them, but then I received an email wanting to set up a call from their marketing team! I couldn’t believe it when I received the email that they were going to pay my entrance fee in full! I have had the pleasure of working closely with the marketing team the past few months to come up with an influencer agreement and work on content creation for Coloplast as part of the deal. I am so grateful, not only for their sponsorship, but also for the opportunity to
work with them and get to know some of their team. Thank you Coloplast!
The weeks leading up to the pageant
February and March were filled with events, rehearsals, fittings, meetings and different competition segments like the live speech and the inter view. It was so incredible to learn so much from the 2023 Miss Calgary and to practice our walks and routines!
My ostomy certainly doesn’t define me, but it is part of me. In my journey of self-love and being my authentic self, I thought this was an important step in the process.

During my live speech I had the chance to talk about disability accessibility in the city of Calgary, which, as an area in need, is an important issue for me to shed light on. During my interview I was able to talk about my experience living in Calgary and who I am as a person. This was also a great opportunity to work on my public speaking before the big day.
The Big Day!
Finally, after months of preparation, the day of the competition came around. It started on Friday night with a fashion show and silent auction, which was so much fun! The main event was held on Saturday where we got our hair and make-up done. We had a ton of photos taken and really got to know each other.
We started with introductions to the audience and judges, then went straight to the swimwear category! I have worn bathing suits to the beach before which show my ostomy, but I sometimes also wear bathing suits that cover it. However, I made the decision to specifically showcase my ostomy and not hide it, as my main reason for doing this pageant was to represent the ostomy community and show up as




my authentic self. Leading up to it, I was so nervous to walk the stage in front of a huge audience and camera crew, because I didn’t know how people would react or how I would feel, but as soon as I got on stage my nerves melted away and I absolutely killed it.
Here is a photo of me wearing my blue and orange bikini for the swimwear category! My ostomy certainly doesn’t define me, but it is part of me. In my journey of self-love and being my authentic self, I thought this was an important step in the process.
Overall, the pageant was an incredible experience that I would happily do again. I had the privilege of meeting many amazing women and also had the chance to push myself out of my comfort zone, allowing me to truly embody who I am as a person. Afterward, I was approached by people who thanked me for my representation and for showing my ostomy. I even had the incredible privilege to win ‘Miss Inspirational’ which is awarded to the contestant whose story inspired the judges the most, as well as ‘Miss Natural’ which is awarded to a first time competitor who the judges felt showcased the most natural talent.
I am so honored and incredibly proud of myself for trying something new and winning these awards in the process.
All this is to say, having an ostomy does not make you any less worthy, beautiful, or loveable, so stay true to who you are! n

I had
prior to the pageant to get to know about her as well as about the pageant. Hannah graduated from the Okanagan College in kinesiology. Hannah is now in Calgary obtaining her acupuncture certificate. Pageant participants were involved in every aspect including arranging baskets for the auction, collecting jewelry for Gems for Gems, selling tickets, having the highest media views about the pageant, etc. These young ladies strive to become role models who exude confidence. Part of the pageant involves a scholastics test graded per segment. Hannah gave a big shout out to Coloplast for their support with her registration fee. Because Hannah is open, approachable and comfortable, many guests thanked her for bringing awareness to ostomies and Ostomy Canada Society. It was a real pleasure to be able to be there in person to support and encourage her.
Calgary’s pageant system (Little Miss to Mrs.) was created by Patti Falconer over 50 years ago. Patti believed the pageant experience was the best opportunity for females to develop poise and confidence. Through public speaking, special events and interviews she watched the pageant delegates develop grace and courage.
By Tori Judson
Hi, my name is Tori and I have a very rare condition called Hereditary Sensory Autonomic Neuropathy (HSAN) which causes continual degeneration to my autonomic nervous system. I am, ‘One in the World’. I can’t feel pain or temperature, can’t sweat, can’t feel hunger, can’t hydrate naturally, and have never been able to feel when I need to go to the bathroom. I have endured three years of malnutrition and gut discomfort, suffer from joint hypermobility, and as well I have mild skin hyper extensibility. I bruise easily, and because I’m immunocompromised, it takes longer for cuts or wounds to heal. My veins are scarred and are hard to find. I have had complications from surgeries, I have autism, I also have a mild intellectual disability, several eye disorders, and infertility due to an inversion of chromosome 10. I have autonomic nervous system degeneration, and the list goes on. It took 19 years to get a diagnosis after many misdiagnoses over the years. My neurologist said something happened in utero or it could be a gene mutation that has not yet been discovered. My autonomic nervous system started worsening in 2018 and I would have seizures or I would suffer meltdowns from overheating. Sometimes I would pass out due to my hydration issues. When I was 20, my bladder and my colon both quit working due to complications of HSAN (neurogenic bladder - a small bladder capacity of 100ml, slow colon transit, and borderline gastroparesis). On September 25, 2020, I had surgery that left
Since being on daily IV hydration
I’ve been able to maintain weight for over a year now. I have energy, I am able to walk more and can exercise. I am able to live and function and I can do so many things! The power port which is inserted in my chest wall is a true lifesaver!
me with both an urostomy as well as a colostomy. Unfortunately, the colostomy failed but thankfully I have an ileostomy now! I’ve had my urostomy for four years and my ileostomy for a year and a half. My hydration issues became severe after I got my ileostomy because my autonomic nervous system reacted badly to the surgery and I now need more hydration than is orally possible. Because of my condition, I now get most of my hydration through a central line. Before I started doing daily IV hydration treatments I was



literally wasting away. For three years I was rapidly losing weight, I almost needed a feeding tube, and I needed to use a walker or sometimes use a wheelchair. I really couldn’t function, I wasn’t aware or present in my own life, I had no energy and was lethargic. On weekends I would literally drop six pounds from not getting any IV hydration. If I go longer than a day without IV hydration, things
go downhill and become life threatening very fast. During the three years of being malnourished, my mom and I would go from doctor to doctor and no one was overly concerned. They didn’t tell us why this was happening, and labeled me as anorexic. I lost 33% of my body weight. Although I was eating 2000-3000 calories a day, I was still losing weight. Since being on daily IV hydration I’ve been able to maintain weight for over a year now. I have energy, I am able to walk more and can exercise. I am able to live and function and I can do so many things! The power port which is inserted in my chest wall is a true lifesaver! My mom was my caregiver during my years of not being well and of my needing to have a lot of surgeries and hospital stays. She did my ostomy appliance changes, administered IV antibiotics three times a day, gave me lovenox injections, and did wound dressing changes. My mom did all of the different things needed to take care of my port. She was and still is an amazing advocate and more! Now she’s my medical advocate when I can’t advocate for myself. She makes phone calls when I can’t, helps with transportation, finances, and is my guardian. A nurse comes to our house each week to access my port. It must be conducted under a sterile technique, so it is nice a nurse comes to me. Due to my autism and mild intellectual disability, I wasn’t emotionally ready or able to become involved with my medical stuff until
last year. Taking care of everything surrounding my rare condition and trying to remain infection free is a full-time job. It is so much work and most people don’t realize this unless you actually live with me and see what I do from day to day. Life still moves on after needing lifelong medical devices and you should always have hope! I’m very thankful for God and for my wonderful support system! I love sharing my medical journey in the hope of helping others and encouraging them on their journey! I’m an ostomy advocate, HSAN advocate, I work with the HSAN IV foundation to promote the foundation and I’m a guest speaker to juniors and seniors! I have made so many friendships through the Instagram community. My account has grown a lot and it’s truly the best community! I wouldn’t be where I am today without God and He keeps opening up doors for me! I am living proof that just because you have rare conditions doesn’t mean that it should stop you from pursuing your goals and dreams even though they may change! n
Tori lives in Rosemount, MN.
Editor’s note: After reading several of Tori’s Instagram stories, I reached out to ask if she would like to share her story. She was very happy to do so! She is an amazing advocate.



Facilitator,
It started with a question from Deborah Hurley, “How can we improve on the care provided by healthcare professionals for people learning to live with an ostomy?” Deborah has been a strong supporter and advocate for people learning to live with an ostomy.
The first “Living With an Ostomy” for nursing students and Visitor Training Program.was organized. Anne provided a PowerPoint on the ostomy basics, which was delivered before we talked about our personal journeys. This process was well received and the PowerPoint was more visually interesting and professional.
I met Anne while I was at a post op appointment as an inpatient. Anne was my ‘stoma nurse’ and I immediately connected with her, feeling her genuine caring and benefiting from her extensive knowledge and teaching skills. I had questioned both my surgeon and the nurses at the pre admission clinic as to whether there was a support group and/or individuals who I could speak to pre and post op. There was neither option available. During my first visit to the outpatient stoma clinic, I broached this topic again and coincidentally Anne Le was in the process of forming a Peer Support group in Edmonton. I attended her first meeting and since then the group has grown and has engaged in several initiatives, including presenting “Living With an

Ostomy” for nursing students and for the Visitor Training Program. My ‘new normal’ began near my 70th birthday in the middle of the pandemic (2021) when I required urgent surgery to remove my sigmoid colon and two thirds of my rectum, with a temporary loop ileostomy to allow for healing.
P.S. it took me two years to muster the courage to go in a pool and ocean!!

I had been diagnosed with diverticular disease many years before and medical management had run its course. I had several episodes of diverticulitis resulting in pain, unpredictable bathroom trips and lengthy courses of antibiotics, plus surgery to remove my cecum in 2015. In 2020 my disease worsened with the development of fistulas, and additional symptoms that could not be resolved with medications, putting me at a high risk of perforation of the bowel.
The path has not been easy. I learned that the section where the surgical join was had become blocked and that a reversal would be a huge challenge. With my family and friends’ support, my faith, and my positive attitude, I have moved forward through the stages, similar to the stages of the grieving process. My quality of life has improved, and I have resumed travelling, golfing, swimming and can enjoy my grandchildren, food, and ‘life’! We celebrated our 50th wedding anniversary in Maui recently and I can’t remember when I last felt so well!
As a post-op inpatient, I encountered some nurses who were not comfortable and/or knowledgeable with providing ostomy care.


Months later, I had coffee with two recent nursing graduates who clearly stated they were taught nothing about ostomies! My mission now is to help others dealing with ostomies and to bring awareness to this ‘different way’ of life.
In February of 2023, Brittany Specht attended an Edmonton Peer Support Meeting. Brittany spoke openly about her own experience and added a positive outlook.
I was one of those people who thought “that will never happen to me”, until something did happen, suddenly and unexpectedly. In the Fall of 2022 I became very ill and was diagnosed with an aggressive and severe case of Crohn’s Disease. The next three months I spent in and out of the hospital for a total of forty-five days. I was 22 pounds underweight, malnourished, and anaemic. My team of specialists trialled many medications, but unfortunately my body did not respond. I had multiple bruises from all the needles and IV medication.
My ostomy saved me and I am forever grateful!
In October of 2022, in order to prevent my disease from getting worse, I had an urgent subtotal colectomy with an ileostomy. In layman’s terms, I had 70percent of my large intestine removed and my waste is now diverted through an opening in my abdomen, called a stoma. I lost everything during those three months of being sick. I lost my ability to parent (I had a 10 month old and two-year old at this time), I lost my identity, I lost my physical health, my body image was compromised, and I struggled greatly with my mental health. I was thrown a huge learning curve as I learnt how to care for my stoma and ostomy. This involved dealing with bag leaks, blockages, and learning how to do bag changes.
Brittany Specht, Registered Nurse

It took awhile to become confident in caring for my stoma but one day it became my new normal. With all the dark that came with my illness, a new strength was discovered. I started living my life to the fullest and did not let my illness define me.
Since getting my ostomy I really strived to continue pursuing my passion and things that bring me joy. It has taken some navigation and trial and error. Since my surgery, I have started working out again, travelled to many places including Hawaii, ran a 5km race, hiked two mountains and I started to become an ostomy advocate. I have had the pleasure of teaching second year nursing students at Grant Macewan about what an ostomy is and about my personal experience of living with one.

Society has given us a vision of what normal looks like. I want to highlight that just because someone looks different, or doesn’t function the way a ‘normal’ person does, doesn’t mean they can’t enjoy life, it doesn’t mean that they aren’t beautiful, and it doesn’t mean they can’t excel.
Anne Le, an NSWOC at the Grey Nuns Community Hospital spoke to a Grant MacEwan University instructor about the need for nursing students to increase their awareness and comfort level in caring for patients undergoing ostomy surgery, and to develop an appreciation for the potential challenges patients may experience. With these connections and identifying as a facilitator of the Edmonton Ostomy Peer Support Group, Anne was able to help arrange a teaching session.
In May of 2023, Deborah and Brittany presented to second year nursing students at Grant MacEwan University, sharing their personal experience on living with an ostomy. The students overwhelmingly agreed that their current curriculum required improvement and the information presented was invaluable and enlightening!

As soon as the day after surgery, I felt like a weight had been lifted from my body as the severe disease affecting my large intestine was gone. Ostomy surgery significantly improved my life and brought me back to my sense of self.
Both Deborah and Brittany are amazing advocates as they bring a unique perspective because they are both nurses themselves and are able to speak from a patient perspective with an appreciation of the current challenges of our hospital system, with the goal to improve care for people undergoing ostomy surgery.
As a result of the positive feedback from the Grant MacEwan instructors, there are more opportunities for Deborah, Brittany, and/or Justin to continue to advocate with our future nurses on how to care for patients learning to live with an ostomy.
When I was 16 years old, my image of being a teenager was flipped upside down as a diagnosis of Crohn’s Disease was given to me after months of enduring various symptoms. My high school experience was sprinkled with medications, bloodwork, and lifestyle changes that my peers were not dealing with. Eventually, in my second year of university (at 19 years old), it came to the point where I was unable to leave my house. Physically and mentally, I was at my
lowest. I was admitted to the hospital and after a week-long stay, a surgery for a permanent ileostomy was scheduled for just days soon approaching.
Having an ostomy surgery happen so quickly was surprising to say the least. Recovery was not straightforward due to blockages, but as soon as the day after surgery, I could felt like a weight had been lifted from my body as the severe disease affecting my large intestine was gone. Ostomy surgery significantly improved my life and brought me back to my sense of self. I didn’t struggle too much with having the appliance on me (thankfully the NSWOC nurses had been great for exposing me to that prior to surgery), but I did have issues with what others thought if they saw my ostomy bag. Over time, I realized that it is not a negative thing in my life and that it has allowed me to truly live again. I took my chances and through an opportunity with my university, I went abroad (alone) to work in Germany the following summer. I was able to keep up with my peers in terms of activity, food, and travel. This experience with an ostomy was a huge turning point in my life and I credit it to be one of the best decisions I have ever made.
Coming back home, I had once again been exposed to the joys and freedoms of living, all of which were evidently capable with having a permanent ostomy. Taking that risk to challenge myself and step outside my comfort zone while travelling helped in changing how I think about my ostomy every day. I am now ready to share my story, help others, and raise awareness. Being a part of the Edmonton Ostomy Peer Support Group and being able to educate nursing students has been extremely fulfilling. What I’ve learned is that you most often regret the chances you didn’t take! n
Note from the editor: On March 27th), Justin was able to give another presentation for MacEwan nursing students with the help of Anne Le. This was his second presentation there. As well, I am 23 now and have just passed the three-year mark with my ostomy and have educated many of my friends at school about it!
Brittany and Deborah and Justin are members of the Edmonton Ostomy Peer Support Group.

By Tabitha Wilson

February 26th, 2024, the start of eating disorder awareness week which is one journey I never thought or even saw living with a digestive motility disorder to bring me on. Yet here I am, and it is time awareness is made about just how much having a digestive disorder and an ostomy can impact one’s eating and relationship with their body and food. My journey begins at the age of 18 when my digestive disorder became concrete. I would eat but it made me violently ill and would often send me to the emergency room because the pain and nausea were uncontrollable to manage at home. This led me to have a difficult relationship with food and I would avoid it because I associated food with pain and nausea and hospitals. Prior to having my ostomy surgery, it became apparent that I had a motility disorder. We were trying every medication, diet and therapy with hopes of something helping me however, the only thing that became beneficial for me was switching to an all-liquid diet. I tolerated this enough to gain weight and I lived like this for five years. Then my doctors brought up having colostomy surgery. We hoped that by removing the part of my GI tract that was the most affected and was causing the rest to move slowly, would manage my symptoms enough so that I would be able to tolerate solid food with minimal pain and nausea. However, the colostomy was not an answer to my problem and my symptoms only worsened. I became unable to tolerate full liquids and clear liquids which were the only thing I felt safe enough to eat. I ended up needing a picc-line to receive infusions and hydration to keep my iron, electrolytes and hydration up because I could not get enough

in orally. Those five years of struggling from 2017-2022 this is when I truly believe developing Avoidant Restrictive Food Intake Disorder (ARFID) gripped hold of my life.
In March of 2021 I was admitted to the hospital for a fourth time through the COVID-19 pandemic and it was then when doctors realized I had a bigger problem than just my motility disorder and a colostomy that was not helping give me the quality of life it was supposed to. While I was admitted to the hospital I was supposed to be on clear liquids as my intestines were impacted and I only had my ileus. I was on clear liquids, where they bring food trays with juice, Jell-O, and Italian ice; however, I was not brought a tray during my first three days of being admitted. Because of how sick I was, I really did not care but on day three the hospital dietitian came in to see me and she had some questions. At the time, even at home, me going three days with having only water was my normal. She questioned why that was my normal and I said because the pain and nausea is hard enough with just water that I don’t think about food or anything until I start to feel dizzy and weak. I ended up getting referred to an eating disorder clinic. It did not bother me because in my eyes it was not an eating disorder that I had, it was the harsh reality of pain and nausea and having a paralyzed digestive tract causing me to be incapable of eating. June 30th, 2021, I remember it like it was yesterday, I got diagnosed with ARFID. http://kidshealth.org/en/parents/arfid.html#:~:text= What%20Is%20ARFID%3F,poor%20growth%20and%20 poor%20nutrition. I had my intake at the eating disorder clinic that
I was referred to and it was an almost three-hour appointment. so many questions and I could not understand everything that was thrown at me. Body-image was among the top questions I was asked. When it got to the point of being asked about what eating looked like for me, it became apparent for them that I had an eating disorder, but it was nothing like typical eating disorders. The act of eating was torture for me due to my motility disorders, but I had learned to cope by avoiding food in an attempt to try to make myself feel safe because doctors did not know how to help me. They decided I needed treatment as I was on a piccline and struggled to maintain a healthy weight and would only consume the same four foods (ice cream, pudding, yogurt, peanut butter). I was put on a waitlist for treatment which now looking back at how things turned out, I am thankful for.
When it got to the point of being asked about what eating looked like for me, it became apparent for them that I had an eating disorder, but it was nothing like typical eating disorders. The act of eating was torture for me due to my motility disorders, but I had learned to cope by avoiding food in an attempt to try to make myself feel safe because doctors did not know how to help me.
Throughout my time waiting to start treatment which I was not hopeful on helping me, I continued to search for answers, going through more medication trials and testing. Eventually we found ourselves in the year 2022 and it was decided that I needed to go see my colorectal surgeon again and that the only option for a better quality of life for me with managed pain and nausea was to switch my colostomy to an ileostomy. It was a rather easy decision to decide we were putting me through another major intestinal surgery and September 26th, 2022, I had surgery. The day before Thanksgiving I got the call just two weeks post ileostomy surgery that I would be starting treatment for ARFID in two weeks. I am thankful that my name came up so soon after surgery as it was apparent ileostomy surgery was the right decision. I would need help to learn to eat as it had been ten years since I had done so sufficiently.



Treatment helped me to learn to eat solid food again. I was one of only a few patients with an ileostomy that the clinic ever had. This made it harder because part of having an ileostomy and motility disorder and ARFID have me scared of eating foods like fruits, vegetables, and harder to digest things because I fear that my ileostomy will have a blockage, and then because I have a motility disorder I fear that my intestine would never work the same again. This is one area in which the eating disorder clinic’s dietician could not help me. I had to reach out to my surgeon and arrange to see the dietitian through the ostomy clinic, who reassured me that I could try and eat whatever I desired; however, my problem would be with my motility disorder not allowing things to pass through my GI tract. My ileostomy would be the least of my problems.


One of the many things I want people to learn through reading this is just how often having a digestive disorder and eating disorder can go together. Many people think that eating disorders come from a desire to be thin; however, in my experience, eating disorders are a way to cope and control and find comfort when everything else in one’s life seems to be falling apart. www.waldeneatingdisorders.com/blog/8warning-signs-of-orthorexia/. Anorexia can become something that comes along with having a digestive disorder because so often with having a chronic illness we are told “well your weight is stable so it can’t be that bad.” Some people may take extreme measures and develop unhealthy habits because they want their pain to be validated. Often people with a digestive disorder are told, “Maybe if you ate healthier.” People are so desperate to feel better that that comment, although said with the right intention, is taken the wrong way and can cause unhealthy eating to become more extreme. Eating is the hardest part for many with digestive disorders when it’s a continuing negative experience; however, when we are diagnosed with an eating disorder, many blame that as a cause for the GI issues, disease/ disorder. This needs to change.
April 17th, 2024, marked one year of me being out of treatment for ARFID and as much as I would like to say that I am doing
amazing and living with food freedom, this will forever be something I struggle with. I had a double hernia repair surgery in August 2023 that led to complications and with my motility disorder flaring, it has again caused my ARFID and mindset around food to be difficult. Recovery is not linear and because I was left to my own devices for so long, learning not to avoid food is hard. To this day, I do not commonly have hunger cues or a desire for food; however, when something appeals to me, I make sure I enjoy it because for so long my digestive disorder and ARFID made eating impossible. Recovery is hard and my motility disorders definitely make things more of a challenge, but I am fighting.
If you’re battling a journey like this, please know you are not alone and it’s something you should not be ashamed of. I know it takes a lot of effort and strength to ask for help and to go through treatment. At times it may feel unfulfilling because you are still going to be living with the illness and symptoms that have caused the eating disorder in the first place. Know that recovery is tough but so are you and you have fought through chronic illness and an eating disorder and these things are shaping you into becoming who you are. A true fighter never gives up, and this journey will take you through some really hard times; however, these experiences allow the best moments to have profound meaning and importance because you have been through a dark, and grueling journey. n
Below are two links for the therapist Tabby saw that you may find helpful:
www.lhsc.on.ca/news/truths-and-misconceptions-eating-disorders www.facebook.com/LHSCCanada/ videos/2389825544551786
There was a Regina area man, Al Wolfe, who had his ostomy surgery in 1965. While in the hospital he received a brochure about the UOAA (United Ostomy Association of America). He decided to become a member because he could see that there was information and support for his own recovery. A few years later he was approached by the UOAA and they asked Al to start a group in Regina. Over the 1973-74 winter Al, his wife Vickie and friends Alva and Orval Lewis, started working on organizing a gathering. They did not know how many people there were in the area who might be interested in an ostomy support group.
On May 4, 1974, 24 people attended a meeting following a small ad that had been placed in the Leader Post, Regina’s local newspaper. Could they have imagined that we would be celebrating its impact 50 years later?


In 2024, Regina Ostomy didn’t want to miss an opportunity to celebrate the 50th Anniversary, to remember and recognize all the people who have contributed over the years and to acknowledge all those who continue to be part of the organization to help it grow and become stronger. It was a great event with some fun entertainment by a local artist. One highlight was having one of the original group members, Muriel Matchet, join us for the evening. Muriel was the one who started the first newsletter and it continues to this day. During the evening, a slide show of photos from scrapbooks going back decades and a display of ostomy equipment from the 70’s to the present was shown. We used the opportunity to have a ‘basket’ raffle which raised money for Ostomy Canada youth camp held at Camp Horizon in Alberta. Individuals and businesses donated themed baskets filled with a lot of great goods.
Our nurses, our suppliers and advertisers were there, many of whom donated to the function or baskets. We had members and family members from throughout the province. It was a big collaborative event.
There were 130 of us in attendance and we had a great evening of meeting friends, both new and old. We shared a great meal together and listened to all of the greetings and congratulations from the City, the Province and from Ostomy Canada Society. We also received congratulations from the Lieutenant Governor of Saskatchewan on behalf of King Charles. Sometimes it’s easy to forget how many people are impacted by the support and encouragement that comes from the support group, and this celebration was a reminder to all of us that what we do is important.
Fifty years as a non-profit organization doesn’t happen without the hard work of many people. Thank you to all of you who have been a part of this great organization. Thank you to those who are new members and all those who continue to be members, year after year, enjoying our newsletter and providing support to new members. This may mark the end of the Regina Chapter as we know it, but as we move into the future, we become Ostomy Saskatchewan, a proud entity within Ostomy Canada Society, where we will continue with awareness, support and advocacy just like it began 50 years ago. n
Submitted by Deb Carpentier of Ostomy Saskatchewan
www.ostomysaskatchewan.ca/may-4-a-50th-celebration/

By Gayle Knights-Redman
Imagine the scene. It’s a warm day, despite the grey sky. You’ve just crossed the finish line of a half marathon, the cheers of the crowd ringing in your ears, the medal bouncing around your neck. You collect your baggage, start to change into dry clothes and you become vaguely aware of an odour. You sniff a couple of times and quietly say to your husband, “can you smell that?” You pull away the top of your running tights to investigate and realise your stoma bag is no longer glued to your tummy, at all!
Yes, this actually happened to me. Twenty weeks after my stoma was formed, I ran my first half marathon as an ostomate and my bag fell off. I didn’t even realise it had come unstuck. Luckily, my sportswear was holding the bag in place and Delilah (my stoma) had not been active in the time since the bag came unstuck. Still, this was going to be a problem. If I can’t even get to half marathon distance without sweat dissolving the adhesive, how am I possibly going to complete a full marathon?
Delilah is a permanent end colostomy and she was formed in April 2021, as a result of endometriosis. The surgery has also left me having to permanently perform intermittent self-catheterisation six times per day. I knew I had endometriosis 20 years ago, whilst working as a junior doctor. I had all the typical symptoms during my periods of pelvic and lower back pain, pain radiating into my legs, constipation, pain passing stools, pain with intercourse, dizziness, nausea, even pain passing urine. In between my periods, I was exhausted, much more exhausted than even a junior doctor should be. Despite my absolute certainty that endometriosis was causing my symptoms, it still took three years for me to get a referral to a gynaecologist for a definite diagnosis.
I was really very ill by that time. I had completed my post-

graduate training and was working as a GP. My life consisted of work, sleep, and many cancelled plans with friends. I was taking a lot of painkillers and using heat packs just to get through the day, and I was pretty fed up. I was also trying to plan a destination wedding in Canada and was wondering how I was possibly going to get through the day without doubling over in pain or flooding body fluid straight through my wedding dress. It seemed sensible to buy a very big, very red dress!
My treatment course was difficult, as all attempts at surgery were hampered by excessive bleeding. I ended up with a hysterectomy at 33 years old. Of course, this was only after spending two years on hormone treatments that should have reduced some of the disease but only served to make me gain weight and retain a lot of water. I was the Matron of Honour at my sister-in-law’s wedding during that time, and I am unrecognisable in the photos. The endometriosis was also significantly worse by the time I had my hysterectomy and my four surgeons, despite six hours of trying, were unable
5 November 2023 By Paul Pigott, BBC News
Awoman has pulled out of running the New York City Marathon after organisers said she could not wear a vest carrying supplies for her stoma and water.
Gayle Redman, a GP from Flint, Flintshire, said the vest had allowed her to safely run marathons in London and Paris. She said she believed she had been discriminated against.
New York Road Runners (NYRR), which organises the race, said the vest did not adhere to rules set by police. Gayle has a stoma and needs to self-catheterise six times a day follow- ing surgeries for endometriosis. A stoma connects to the diges- tive or urinary system and allows waste to be diverted from the body and into a bag. Gayle has found certain aids to help her race and has competed in numerous events over the last decade. “New York Marathon’s been on the bucket list for quite some time,” she said.
She recalled her delight when an email arrived six months ago saying she had been registered as a disabled competitor for the 2023 race. She sent organisers pictures of her vest, which has pouches on the back for a 1.5 litre water bag and a straw so she can drink continuously, as her condition makes her susceptible to dehydration. The vest also has a pocket on the back where she carries supplies for her stoma.
Gayle most recently ran the the Great North Run 2023, a half marathon in Newcastle “I carry huge volumes of fluids when I go out on my really long training runs,” she said. On a competition day the supplies she carries in her vest is all she will have for up to 13 hours. But Gayle was told by the NYRR that only waist belts would be allowed, a type of aid that would affect her stoma. “I emailed them again and said this is a dis- ability issue, this is really important,” she said. “I can’t take part if we can’t figure something out.”
The organisers sent her a type of clear ruck sack for carrying water, but she said it would not work because it had no room to carry stoma supplies.
Eleven days before the race she got another email saying she could use front water bottles in a vest, but nothing about where she could carry her stoma supplies. She said she was left with no choice but to cancel the trip, losing £500 in entry fees that she and her husband paid to run in the race. Gayle says she and her hus- band Tim, who is also a disabled runner, have lost £500 in entry fees “I’m disappointed that they couldn’t find a way of including me,” she said. “I feel like I’ve been discriminated against.
“I’ve got a disability that is recognised... the Equality Act in

the UK, and as far as I can tell the Americans with Disabilities Act (ADA) is very similar, says that reasonable accommodations should be made. “I have gone out of my way to try to meet them halfway and see what I can do. “They’ve made accommoda- tions, but they’re not accommodations that suit me.” Redman says she feels like she has been “discriminated against”
NYRR said in a statement: “We work with intention to pro- vide reasonable accommodations in accordance with local laws and federal ADA guidelines to ensure runners of all abilities have access to our races while making sure that each and every runner, spectator, volunteer and staff member are safe.” It said it went “above and beyond to provide this runner with options including purchasing two hydration packs for her, in addition to our 20 course-based hydration stations”.
“It is unfortunate that her requests didn’t align with local law enforcement restrictions and that she has chosen not to join us this year,” the organisers said, pointing to hydration vests being on a prohibited items list. Gayle said she understood the concerns about security after three people were killed and 260 injured in the Boston Marathon bombing. “I would have quite happily had a conversation with New York Police Department about what their concerns are,” she said.
“I’ve repeatedly asked [NYRR] what other suggestions they have to help me with this, and they’ve not come forward with anything.”
So will she be watching the NYC Marathon on television this Sunday? “No,” she said, because it is “all a bit too raw right now”. “We’re already exploring what we can do in the next few weeks to get into another marathon that will welcome us and accommodate us,” she said. “The reality is [on the day of the race] we’ll probably go out and do a long run.”
Reprint permission from BBC News at bbc.co.uk/news
to remove all the disease.
We knew it was going to come back, but I had ten years’ respite, where I was able to start living my life, socialising, travelling, and discovering that I liked to run. In fact, it turned out that I love to run! So, when the symptoms of endometriosis started to creep back and I knew I was going to have to have more surgery, my one proviso to my surgeons was that I had to be able to get back to running long distances afterwards. An MRI had failed to identify the extent of the disease, but my Gynaecologist was sure it was all located in my lower rectum, and I was going to need bowel surgery. I went into the operating theatre not knowing exactly which surgery I would be undergoing but having given consent for several variations.

This time I had five surgeons working on me for ten hours. “Bit greedy, aren’t I?” Waking up in recovery, my first question was about the time and if my husband was ok, as he had clearly had a very long wait for news, and I felt badly for making him worry. Then I surreptitiously placed my hand on my tummy and knew I had a colostomy. It turns out that I had endometriosis patches all over my abdomen, but the largest patch was embedded in my rectal wall and there just wasn’t enough tissue left to join the bowel back together. Delilah is with me permanently now and I am completely fine with that because the surgeons believe they have removed all the disease, and I am entirely pain free now.
Anyway, back to that half marathon finish line and the disaster of the dissolving glue. This was a huge problem for one very specific reason; ten weeks before I got the call saying I was finally going in for surgery, I found out I had won a place in the London Marathon, for October 2021. I had waited seven years to win my spot in the ballot and I was so excited to finally have my chance to run the marathon in London. As soon as I woke up from surgery and ‘met’ Delilah, I knew I would never be marathon ready in six months and was going to have to defer to October 2022, but I was absolutely determined that I was going to take my place at the starting line and run the race I had been dreaming of for so many years. That half marathon was the start of trying to work out how I would achieve my marathon goal with both a stoma and catheters. It was time to get creative, with the help of my stoma nurse. First up, making sure the bags stick properly for as long as possible, when I’m running. I started applying non-perfumed roll-on deodorant under the flange and sticking flange extenders on top and it worked. Half marathon number two completed the very next weekend, thanks to Covid deferrals, and the bag was still well and truly stuck at the finish line.
Next problem, pancaking. The tightness of my sportswear was turning the bags into vacuum packs and blocking the output, which was not only causing leaks but was also painful. So, we changed bags to ones with filters and stickers and, after a few false starts, found ones that would retain some air in the bag and stop the pancaking.
Oh wait, now I was experiencing ballooning issues. I used closed bags due to my thick output, but hey, let’s try drainable bags
so I can release the air. Brilliant idea, right? That’s how I found myself in the middle of a coastal path, with my tights around my knees, trying to open the end of Delilah’s bag and release air without releasing anything else. My husband was gallantly trying to keep a look out for passers-by and protect my modesty.
Right…, this time we’ll try two-piece bags. Brilliant idea! I can open the top of the seal easily and discretely; I don’t even have to stop running whilst I do it. I just must make sure there is no poor, unsuspecting runner downwind of me when I do.
And so, the training runs got longer, and my hydration and fuel needs got higher. It was time to start plotting routes that took me past shops where I could refill my hydration bladder and start practising with various nutrition options. On my longest training run, of 22 miles, I needed three litres of water. As for nutrition, let’s just say there were a few smelly mishaps before I finally found a combination that worked for me. I guess I had better start finding public bathrooms. Oh dear! There are no hooks to hang Delilah’s pack from, often no toilet paper and, well it’s probably best if I just say I became an expert at catheterising whilst hovering and with Delilah’s pack swinging precariously from one of the chest pockets of my hydration vest. Overall, it was perfect practice for carrying everything I would need and for the disgusting portaloos found on marathon courses.
On the 2nd October 2022 I lined up at the start of the London Marathon, feeling nervous, excited but also relieved to have made it through training. I had no time expectations, I just wanted to enjoy myself. And enjoy myself I most certainly did. The atmosphere was amazing, the course was beautiful, I felt strong, and I ran every step, stopping only to see my husband and parents, who were there to cheer me on. I crossed the finish line crying, because I could not believe that Delilah and I had made it, and I was so proud of myself for overcoming all the challenges and proving I could run a marathon with a stoma. I sent my husband a truly ugly crying selfie with my medal, which is still one of my favourite photos. Oh, and in case you were wondering, Delilah’s bag stayed put to the very end.
Since then, Delilah and I have also completed the Paris Marathon and the Lanzarote International Marathon, and I am now preparing for our biggest challenge yet. For 2024, I have won a place in the Marathon Pour Tous, which is the public event being held during the Paris Olympics. It is also an overnight race, starting at 9pm. I have no idea how to start fuelling for this or how Delilah will behave with the upset to our usual routine, but this is a once in a lifetime opportunity that I do not want to miss. I have also, unbelievably, won a ballot place in the Chicago Marathon, which is being held only seven weeks after the Marathon Pour Tous. I have never completed two marathons so close together, so it will be interesting to see how I fare with Delilah and I certainly plan to have fun finding out. n



In the next issue of Ostomy Canada, read about how our campers embraced change, made new friendships and built lifelong memories.




COS History - In 1966 a small group of ostomates began meeting in Calgary to provide support to one another. The Holy Cross Hospital and the British American Oil Company (BA Oil) auditorium were early meeting sites. Meetings were later held at various medical sites free of charge, predominantly being held at the Canadian Cancer Society. Currently, COS rents community halls to host its quarterly meetings.
An early supporter was pharmacist Ron MacLean, who was then working at Penley Drugs and later was a partner at Blain MacLean Pharmacy. Ron was first to bring ostomy appliances to Calgary from the United States, as they were unavailable in Canada. He attended many meetings, helped write the original constitution, and was responsible for originating the provincial program for adding ostomy supplies to those appliances being paid for by the Alberta government, known today as AADL(Alberta Aids to Daily Living).
In 1967 the Calgary group affiliated with the US-based United Ostomy Association of North America. It was the twenty-fifth chapter to join the UOA and among the first half-dozen Canadian chapters to join. In 1968 the Calgary Ostomy Society applied for and was granted its charter as a non-profit charitable organization.
The first president of the Calgary Ostomy Society was Anne O’Brien, a nurse. There is a long list of presidents who followed. Pat Cimmeck has been elected President four different times, and is the current President.
Gwen Drew, an early President of COS, was the first NSWOC (previously known as Enterostomal Therapy Nurse or ET) in Calgary, graduating from the Cleveland Clinic in 1973. Gwen is also an ostomate, having undergone ostomy surgery in 1954. She was chair of the United Ostomy Association regional meeting held in Calgary in 1985 and honorary co-chair of the tenth annual conference of the United Ostomy Association of Canada Inc held in Calgary in 2007.
COS has been fortunate to have received support from NSWOCs in both the hospital and community settings since 1973, when Gwen began her work at the Provincial Cancer Clinic and began to visit at local hospitals. The Foothills Hospital was the next to employ an ET, followed by the Calgary General and the Holy Cross. Later the Rockyview, Alberta Children’s, and the Peter Lougheed Hospitals hired NSWOCs, as did Calgary Home Care.
COS offers an effective service through its visiting program, which is often an ostomate’s first contact with COS. Its goals are to assist people with rehabilitation by providing emotional and technical support. The visiting program began in 1968 and continues today. The current coordinator of the visiting program is Kaylee Janse.
Since its inception, COS has endeavoured to maintain communication with its members and the general medical community. A newsletter was published for 55 years. This was done under the editorship of many differenct volunteers, the last being Tiffany
Shorson. In 2018, COS revamped its website, www.calgaryostomysociety.com, and now accepts online membership payments and donations. Over recent years a Facebook page and group, as well as Instagram, YouTube, and virtual meeting technology have been added. In addition to quarterly general membership meetings, support group meetings provide a more individual focus. They are held several times a year via hybrid meetings. In 2018 the local J-Pouch group and visitor program was incorporated into COS’ programming. COS also recognized the differing needs of its younger members. It was the first chapter to hold regular meetings of the Young Adults group, originally called the 20/40’s, as its focus was on ostomates who fell within that age group.
55 th Anniversary Celebration
Deanna Desramaux, VP of the Calgary Ostomy Society (COS), began the celebration of the fifty-fifth anniversary by introducing the Executive Committee: herself, as VP; Pat Cimmeck, President who was called away on a family emergency; Kaylee Janze, Volunteer Visiting Coordinator; Pris Squibb, Secretary; and Tiffany Shorson, Newsletter editor, and webmaster. Lisa Gausman, who formerly held executive positions and is Ostomy Canada Youth Camp’s Administrator, was among the attendees.
Deanna stated “Everyone here today either has an ostomy, or knows someone with an ostomy. There are over 150,000 people in Canada living with an ostomy. How lucky are we to be here today to celebrate the knowledge and expertise of the many doctors, nurses, manufacturers and suppliers who have dedicated their lives to ensuring that we can all live comfortably. She added: did you know that Napoleon Bonaparte was thought to have had an ostomy? I figure that is why he’s standing with his hand over his abdomen in all the paintings of him – don’t we all tend to stand that way in photos? We are all checking to make sure our pouch is flat against our abdomen and not showing. A few other famous people also had an ostomy. There was Ike Eisenhower, President of the USA, the Queen mother who had her operation in 1967 and twinkle toes himself, Mr. Fred Astaire was also an ostomate who danced his way through life! We are in excellent company! But today is not about them, it’s about you! Our members, the volunteers who help out at our functions, who have taken the training to visit ostomates in the hospitals or by phone. Today is about thanking the NSWOC’s who are there for any questions or concerns we may have. Like our own Amanda Shelvey who patiently listens to our concerns and alleviates our fears about proper fit, nutrition, weight, exercise, leaks, etc. Today is about thanking the suppliers who tirelessly deliver supplies to us and help us when we are trying new pouching systems and who teach us about the importance of skin care, food, exercise, gut health and proper nutrition.
Today is about the great caring community that is the Calgary Ostomy Society! We are 55 years young and are still going strong. Members may come and go but COS continues to thrive by offering programs such as the volunteer visiting program, the youth camp, the 20-40 group, and help for spouses and significant others. Through our membership drive, and our fun and bonding event, Step Up for Ostomy Walk, as well as other gatherings, we fundraise to help others who are new to ostomy living.
Everyone on the executive committee donates their time and
resources to helping ostomates both in Canada and worldwide via our commitment to supporting Friends of Ostomates Worldwide Canada (FOWC) which in turn helps others to live a better life with an ostomy. We provide this help through fund-raising, by sharing knowledge through Zoom meetings, Education seminars, visiting program training sessions and peer support group meetings.
One of our proudest moments was when, on May 6, 2020 Pat and Lisa were awarded the Canadian Sovereign’s Medal for Volunteers by the Lieutenant Governor General of Alberta. Pat has been volunteering with COS for over 30 years and was the camp administrator for most of that time. Lisa is now the Youth camp administrator as well as the Ostomy Canada magazine Senior Editor. Deanna presented certificates of appreciation to several members who have made significant contributions and volunteered their time to many projects. Those not able to be in attendance we mailed their certificates of appreciation.
Two long-time members were present, Gloria Reid and Doug Abraham, who both volunteered in leadership in the early days. Honorable mentions were given to several volunteers who each received a rose and a certificate of appreciation. A special mention was given to member Fay Martin who turned 100 this year. COS owes its longevity to its member’s support and many contributions. It looks forward to serving the community for another 55 years.
A special toast (below) was presented by long-time member Gloria Reid, who has had her ostomy for fifty-three years.
Gloria toasted: I have been asked to propose a toast to the Calgary Ostomy Society (COS) on its 55th anniversary. This is an honour as I have watched COS grow, and educate and support ostomates and their supporters, spouses, partners, families and friends over the years. It is a group where experiences can be shared in hopes that help can be provided to people trying to live their daily lives.
I give thanks to Jane, Gwen and others who saw a need when the Calgary Ostomy Society was formed. I have seen many changes in appliances and products over the years; these all help to make it easier to lead normal, active lives.
Thanks to the work done by many volunteers, the Youth Camp has evolved, and this life-changing experience has been offered to many youth, who each endure their own, different set of struggles. This is something to be very proud of! It is important to show ostomates of every age that an ostomy does not need to slow you down from leading an active lifestyle.
I congratulate all of you for supporting the COS. This is why we are able to celebrate 55 years. Through education and support you continue to be a growing and active society.
Please raise a glass with me as we toast the Calgary Ostomy Society on their 55 years as a community which offers education, caring and support.
The Garry Doyle Memorial Award, established by the Calgary Ostomy Society in 2023, honors Garry’s legacy by assisting RNs in NSWOC training. Garry had ostomy surgery in 1967 and lived his life supporting others via his involvement with COS. Recipients of this $1000 award are encouraged to engage in community involvement. Join us in contributing to this fund today. The first award was issued in June 2023 to volunteer and NSWOC student, Alyson Wood.
The afternoon concluded with snacks, a special cake, and time to visit together. n
One of the most common ostomy complications is the parastomal hernia. The literature varies greatly on the incidence of developing a parastomal hernia, as well as having mixed reviews for identifying risk factors that could lead to developing a hernia. In addition to its medical consequences, parastomal hernias have a significant impact on a person’s psychological health, everyday activities, and quality of life, including their financial situation.
Ostomy Canada defines a parastomal hernia as: “A portion of the intestine that bulges out of a weakened area of the abdominal muscle wall. Some individuals with an ostomy may be susceptible to hernia formation around the stoma.”
By Karen Bruton RN BScN MCISc-WH WOCC(C)
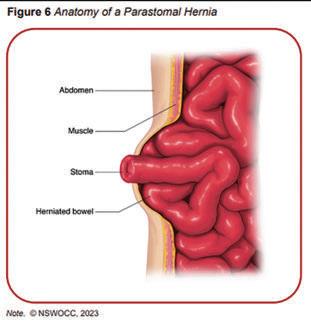
Nurses Specialized in Wound, Ostomy and Continence Canada (NSWOCC) has written the following Canadian Best practices, Parastomal Hernia Prevention, Assessment, and Management: Canadian Best Practice Recommendations which can found on the NSWOC website (https://www.nswoc.ca/bpr). Research shows the incidence for developing a parastomal hernia is between 25.6% to 58%.
Even though parastomal hernias usually develop within two years after a stoma is created, diagnosis may not happen for up to twenty years after surgery. Some of the predisposing risk factors for developing a parastomal hernia include:
• 70 years of age and older
• Obesity
• Manual labour occupation
• Moderately active, including physical exercise
• Lifting young children
• Previous history of a parastomal hernia repair
• Certain diagnoses (e.g. malignancy, connective tissue disorders, diabetes)
• Conditions causing increased intra-abdominal pressure (e.g. Congestive obstructive lung disease, constipation)
• Smoking
• Steroid medications
The type of ostomy surgery may also impact developing a parastomal hernia, but ultimately all persons undergoing ostomy surgery are at risk. There is no standardized method to diagnose a parastomal hernia except by undergoing a thorough examination by a healthcare professional, computed tomography, and an ultrasound.
Reducing the likelihood of developing a parastomal hernia may be accomplished through changing one’s modifiable risk factors.
Preventative measures may include:
• Pre-operative stoma ostomy siting by a NSWOC or a qualified health care professional
• Pre-operative and post-operative education covering the following subjects:
> Smoking cessation programs
> Avoiding intra-abdominal pressure (e.g. acute or chronic cough, vomiting, and conditions causing intra-abdominal pressure)
> Weight management
> Increasing physical activity gradually post-surgery
Most people can manage their parastomal hernias with lifestyle changes, which include losing weight, smoking cessation and wearing an abdominal support belt. Some will require hernia repair because symptoms affect their quality of life or in emergency cases when the hernia becomes strangulated or incarcerated. Not everyone is an appropriate candidate for hernia repair due to pre-existing health conditions (e.g. respiratory, cardiovascular).
Surgical candidates should meet with the surgeon to discuss and weigh the benefits and potential negative outcomes. Hernia repair literature states that it is highly likely the hernia will develop again. Surgeons will consider hernia repair for those with:
• Urgent issues (e.g. bowel obstruction, strangulated bowel, ischemic bowel)
• Symptomatic concerns (e.g. pain or discomfort, inability for appliances to adhere or constant leakage from appliance)
• Complications (e.g. vomiting, chronic skin breakdown)
For a non-surgical approach or while waiting for hernia repair, one may consider purchasing and wearing a hernia ostomy belt, also known as a hernia support garment. These are supporting devices that help to compress and support the stoma site, improving the adherence of the appliance and reducing pain. Hernia support garments come in different widths and sizes and offer different degrees of support. The kind of clothing a person wears might vary depending on their stoma type, function, pouch type, stoma size and shape, as well as their personal traits and comorbidities. These clothes should ideally fit well, be comfortable, offer the required amount of support, and be tailored to the wearer’s needs.
It is wise to investigate and ask questions when purchasing a hernia belt because there are many varieties on the market. It can be difficult to find a vendor that sells hernia ostomy belts and may be even harder to find qualified experienced fitters for measuring a


Left: Fulcionel-Adjustable-Hole-Anti-Roll-Hernia-Support-Belt; Right: Fulcionel-Anti-Roll-Wraparound-Ostomy-Hernia-Support-Belt
References
– Antoniou, S. A., Agresta, F., Garcia Alamino, J. M., Berger, D., Berrevoet, F., Brandsma, H. T., Bury, K., Conze, J., Cuccurullo, D., Dietz, U. A., Fortelny, R. H., Frei-Lanter, C., Hansson, B., Helgstrand, F., Hotouras, A., Jänes, A., Kroese, L. F., Lambrecht, J. R., Kyle-Leinhase, I., López-Cano, M., … Muysoms, F. E. (2018). European Hernia Society guidelines on prevention and treatment of parastomal hernias. Hernia : the journal of hernias and abdominal wall surgery, 22(1), 183–198. https://doi.org/10.1007/s10029-017-1697-5
– Haas, R., Horton, J., & Hamson, A. (2024). Hernia Support Garments for Parastomal Hernia Following Ostomy Procedure: Rapid Review. Canadian Agency for Drugs and Technologies in Health. https://pubmed.ncbi.nlm.nih.gov/38564550/
– Manole, T. E., Daniel, I., Alexandra, B., Dan, P. N., & Andronic, O. (2023). Risk Factors for the Development of Parastomal Hernia: A Narrative Review. Saudi journal of medicine & medical sciences, 11(3), 187–192. https://doi.org/10.4103/sjmms.sjmms_235_22
– MyOstomy.ca. https://myostomy.ca/
– Nightingale Medical Supplies Ltd. https://nightingalemedical.ca/
– Nurses Specialized in Wound, Ostomy and Continence Canada. (2023, May). Parastomal Hernia Prevention, Assessment, and Management: Canadian Best Practice Recommendations. 1st Ed. https://www.nswoc.ca/_files/ugd/9d 080f_35f5f525ff6944da831af9fdd1793bf5.pdf?index=true
– Ostomy Canada. https://www.ostomycanada.ca/
person for a hernia ostomy belt. Researching what vendors are available in your area is important to ensure you purchase the right product. Consider searching for companies such as home medical sales stores, online ostomy sales sites, and pharmacies.
When considering purchasing a hernia ostomy belt, the following questions should be asked:
• Type of material, breathability, lightweight and comfort level
• Adjustability, and customizable straps
• Durability and the garment’s lifespan
• No hole vs hole for ostomy appliance
• Cost (varies)
Hernia ostomy belts vary in size depending on the manufacturer and design; some require specific measurements, while others sell them in general sizes based on hip and waist dimensions. Researching the best possible product that suits your needs is important to ensure a positive quality of life.
Living with a parastomal hernia can be managed effectively with lifestyle changes, but at times surgical intervention is warranted, especially when it affects your quality of life. Complications caused by parastomal hernias can cause emotional turmoil, so it is important to reach out to family members, NSWOC and/or Ostomy Canada (Chapter or peer group) for support. n - A ordable - Pain Free - Saves Time















































































Stretch your dollars, with our high quality, cost e ective products






For more information to acquire locally or to request a sample please call







In Canada Contact - Peter West 519-726-5959 peter@westcaremed.com 844-767-6334 www.sns-medical.com




















By Liz Hiles
I am nearing my eight-year ‘cancerversary’ (the date I received my bladder cancer diagnosis). I still feel the same sensation as that initial moment whenever I think back on it: entirely and utterly floored. I didn’t even know that bladder cancer was a thing. How could I even have it?! By that point, I had been going to the emergency room on and off for over two years with increasing symptoms. At the time, I was told that my symptoms were atypical, but I’ve since talked to others who have had similar experiences; primarily young women. Some time after my treatment ended, I had a candid conversation with my urology oncology surgeon, stating; ‘I don’t understand how it was repeatedly missed for so long that my tumor progressed to that size and the cancer to be such a late stage.’ He stopped shuffling the stack of my records in front of him, looked at me earnestly, and replied, ‘There’s no way they could have even been looking for it. If you had not gotten diagnosed when you did, you’d definitely be dead by now, and honestly, I’m surprised you’re still alive.’ After being ignored, shuffled off, and feeling gaslit for as long as I had, I had encouraged all of my medical providers to be blatantly honest with me. Still, that statement hit below the belt, so to speak.
Let me paint a better picture for you. Throughout my mid to late 30s, I had been having increasing urinary issues: increased frequency, urgency, and nocturnal accidents. Much of this I attributed to the fact that I was approaching 40, drank more water than the average person did, and I thought that these things just come with age, or with weakness of the bladder muscles and pelvic floor weakness after delivering a baby (although I had never given birth).
Eventually, I was having pain, burning, and discomfort during urination. Despite numerous urinalyses coming back without any traces of infections, I was told it was a UTI (urinary tract infection) or bladder infection. I was given prescriptions and shuffled out of the door despite my questions about how it could be an infection without signs of infection in the tests.
My last trip to the emergency department (ED) in July 2016 was in the middle of the night. I was doubled over in so much pain that I could barely breathe. I had been urinating blood clots for months without outright blood in the toilet bowl water. I sometimes ran to the toilet urgently, as often as every five minutes. I could not sleep through the night due to all the pain, discomfort, and urgency. More tests were ordered, and the middle-aged white male doctor came in and dared to postulate that the symptoms I was describing were caused by my menstrual cycle. I was offended and appalled at the blatantly inappropriate response to what I was experiencing. Fighting back enraged tears, I looked him in the eyes

From the moment of my diagnosis, I knew it was going to change my life permanently and that I had no choice; I had to speak out and share my experiences with the disease.
and said, ‘Those are two different holes! If you had blood clots traveling through your urethra, you would know it.’ He laughed and responded, ‘Yeah, I guess you’re right. I’m going to go check on your other results. I’ll be back.’ I never laid eyes on that person ever again. He sent a PA in to discharge me, again without any referral and only a couple of prescription medications. I burst into tears. She did not know how to react, and I was at the end of my rope. She asked me why I was having such an ‘over-the-top’ reaction to being told that I was being discharged. I told her that I’d been through this all before. The meds did not help. I was back in the Emergency department with worsening symptoms, and it was not my job to figure out what was wrong with me. IT WAS THEIR JOB! I told her that if they weren’t going to do their job, they should at least refer me to someone who would figure out what was wrong with me. Baffled, she said, “You’ve been here before?” When I responded in the affirmative, she went to the nearest computer and started digging through my chart. She returned with a list of physicians for me to call to get an appointment with as soon as possible. The next day, I was meeting a urologist for the first time. On Tuesday, a week and a half later, I was having my only cystoscopy, and the following Friday, the urologist’s colleague, sounding like one of the adults from Charles Schulz’s Peanuts cartoon, was telling me I had bladder cancer and informing me of my next steps. My best friend’s mother was sitting beside me, and she was in as much disbelief as I was in. The following eight months were a blur. Due to the advanced diagnosis and size and placement of my T4 tumor, my first interven-
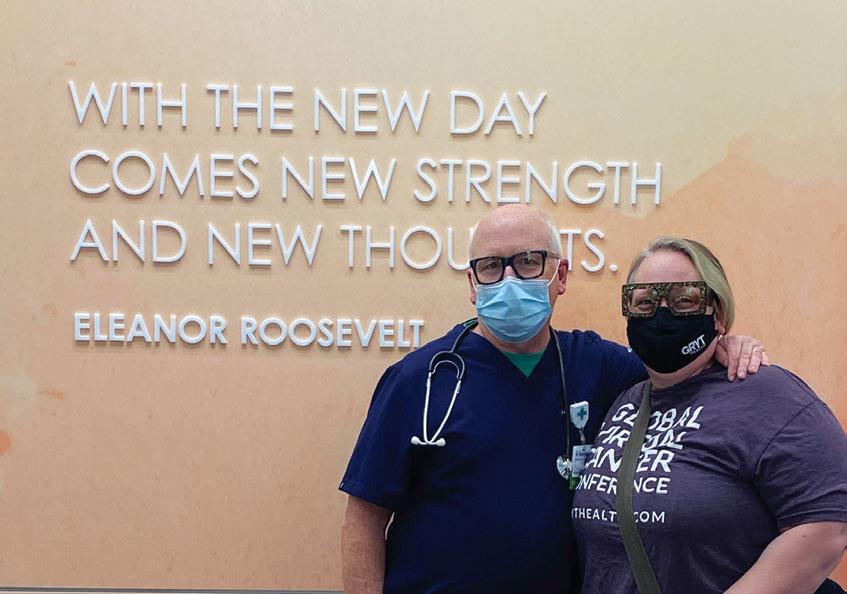
tions included a radical cystectomy with a radical hysterectomy and an ileal conduit/urostomy placement. The grapefruit-sized tumor had grown through my bladder wall and had started to attach to my cervix, so part of that was removed as well. My original plan of being hospitalized for a week and then going to a rehabilitation facility for two weeks was rather quickly abandoned after experiencing several complications. I bounced back and forth between the two facilities for two months. When I was finally discharged, I was able to go home and enjoy my birthday and Thanksgiving before seeing my oncologist in the office. In the week after the American holiday, I had my port placed, my head shaved, and I had started chemo. I was scheduled for six rounds of MVAC over the next three months. I completed four of those rounds on schedule. The fifth round was postponed a week, and the sixth round was canceled altogether. I never got to ring the ‘treatments completed’ bell like so many before and after me did, but I honestly didn’t care. I had been sleeping on a friend’s couch for a week because I was too weak to make it up the steps to my apartment. About a week later, I collapsed at said friend’s house and was taken to the emergency room. Despite being done with treatment, my blood decided I was due for one last hurrah and plummeted. My hemoglobin dropped to 5.7, and I was admitted for a blood transfusion and was sent back to rehab for another three weeks to rebuild my strength before I could go home. When I was finally discharged on a Friday afternoon, after arguing with the rehab doctor, I returned to work the following Monday morning so that I would not lose my job at a local hospital. One would think they would be more flexible, understanding, and supportive of medical crises’ unexpected paths. But they were not.
From the moment of my diagnosis, I knew it was going to change my life permanently and that I had no choice; I had to speak out and share my experiences with the disease. I had been a caregiver to my father, and I had been working in a medical office for sev-

July 2020—Liz wearing a World Ostomy Day shirt that reads, “Speaking out saves lives.”
eral years at the time of my diagnosis. I didn’t know what bladder cancer was, I didn’t know the signs and symptoms to look for, I had repeatedly been ignored and gaslit by medical personnel, and I quite literally did not check any of the boxes for risk factors of the disease. If this was happening to me, I was certain it was happening to others.
Since I completed treatment in 2017, I consciously chose to dive into multiple overlapping communities to share my story and guide others just embarking on this bizarre and challenging adventure. During the pandemic, I shifted my career to full-time, to try to make a difference in both the cancer and ostomy communities. I traveled to the 2019 UOAA National Conference in Philadelphia and spoke on a panel of superheroes. I have spoken on several virtual panels for conferences and one-time events. I have presented virtual and in-person educational presentations for my local UOAA Affiliated Support Group. I have written numerous personal story articles for various online and in-print publications. I am determined and committed to making a difference and educating the public about bladder cancer and ostomies alongside all my fellow cancer and ostomy club members; a couple of the ‘shittiest’ clubs with some of the coolest people!
Liz Hiles was born and raised in Cincinnati, Ohio, in the US. She was diagnosed with stage III-b bladder cancer in August 2016 and had an ileal conduit/urostomy placed the following month. She is a full-time advocate and writer. She is a former contributor and moderator for BladderCancer.net. Currently, she hosts Elephants and Tea magazine’s weekly Happy Hours on Fridays at 6:30 pm ET. She has just begun training as a Diabetes and Ostomy Peer Support Coach at Better Health, a US-based DME supply company. She is the volunteer President of the Greater Cincinnati Ostomy Association and actively volunteers with the United Ostomy Associations of America (UOAA). She has had the honor and privilege to lead and participate in several in-person and virtual panels. If you want to connect with Liz or read other articles, you can access that information through her linktree. n
https://linktr.ee/mirleta
Our first meet and greet of the Ostomy Red Deer group (Second Edition) was a small group, as anticipated, which resulted in the four of us coming away with great expectations for what we know will be bigger and better things. Aside from our sharing of backgrounds and experiences, we were able to put our heads together and come up with a few ideas on how to further expand and strengthen the group.
Those ideas include reaching out to those who were involved with the original Red Deer group, putting up a few more posters in those pharmacies who supply ostomy related items, and ensuring that we find ways to stay in touch with those who may not necessarily use or have access to the Facebook page.
All in all with approximately sixteen people signed up, we consider the #1 gathering to be what we’d hoped for and we look forward to our next meeting TBD. n
Best Regards,
Kurt Koch and Pat Machan

Pineapple is high in Bromelain - Bromelain is a group of enzymes found in the fruit and stem of the pineapple plant. Pineapple is native to the Americas but is now grown throughout the world in tropical and subtropical regions. Historically, natives of Central and South America used pineapple for a variety of ailments, such as digestive disorders. It is often used to reduce inflammation from tendonitis, sprains and strains, and other minor muscle injuries. Studies of people having dental, nasal, and foot surgeries found it reduced inflammation.

If you find pineapple too fibrous, you can substitute it for apples, oranges, or strawberries.
500 mL (2 cups) pineapple chunks
2- 3 large mangos, chopped
½ med onion, finely diced
1 large red pepper, chopped
1 fresh serrano pepper, finely chopped Serrano peppers are notably hotter than Jalapeños, packing a more intense and fiery punch.
1 fresh jalepeno pepper, finely diced
3-4 green onions (scallions) white and green parts, chopped
30 mL (2 Tbsp) cilantro, chopped, plus more sprigs for garnish
1 mL (¼ tsp) sea salt
Juice of 2 limes
Add all the chopped and diced ingredients to a large bowl. Sprinkle with sea salt and squeeze the lime juice over the top. Toss to combine and transfer to a serving dish. Garnish with cilantro sprigs. Makes 9 servings.
Recipe
by Pat Nyswonger (savorthebest.com)
My story started in 2001. I was 41 years old. For a few months I was having alternating constipation and diarrhea which I chalked up to my eating on the run as is common to happen when one is a nurse. Then, for a few years I was having colicky-type abdominal cramps which appeared out of nowhere and resulted in explosive diarrhea. Because of my knowledge as a nurse I decided to feel around my belly and when I thought I felt a bump on my lower right side, I decided I needed to see my doctor. Funnily enough my family doctor didn’t feel anything unusual, gave me peppermint pills for my gas, and planned to book me for a colonoscopy. So off we went on our planned vacation to Nova Scotia with our daughter and her friend. It was the worst trip I ever took. The abdominal cramping got progressively worse. One day, after lying in the RV all day, my husband was worried enough to ask me to be taken to a hospital in Halifax. But me, being the neverending nurse and thinking I would be fine, told him I would be all right until I got home. Now that I look back, my husband Dave was much more insightful than me to recognize that if I was not constantly moving, it was a worrying sign. He was so right!

On the way back to Newfoundland I slept most of the drive as well as on the ferry. That was very unusual for me, because I was always full of energy. I was unusually tired and a few days after we returned, I felt like something awful had happened in my belly. I immediately went to the hospital. I soon found out there was a five cm tumor on my right side that required emergency surgery and a possible colostomy. My first thought was “This is it for me.” I don’t think I ever remembered being so upset, but who wouldn’t be with this kind of news?
Back then, where I lived, there were no NSWOCs to mark the site or to do any post-operative teaching like there is today. So off I went for the surgery hoping for the best but expecting the worst. After surgery I was told that cancer had perforated through the colon and was causing infection inside my abdomen. I woke up to a six-inch incision down the middle of my abdomen. On one side was a pouch and on the other side, a mucous fistula. But I was awake and that was a positive start. I was also so blessed to have a fantastic female surgeon who knew right where to place my stoma. Bless her heart. She will be rewarded!
I spent ten days in the hospital. My husband was and still is, my greatest support. He stayed in the hospital with me every minute that he was not working. At one point the surgeon said he should go home for a break but he told her he really would rather stay. What a guy!
For days I was not permitted to eat anything until my stoma started to expel air. I could not believe how long a day could be when you cannot eat. When I did start eating, it was worth more than a million dollars. But what was worth even more to me was the news that there was no cancer found in my lymph nodes and that it had all been removed. The surgeon recommended I take six months
By Sharon Mercer
of preventative chemotherapy. I’m sure glad I did, because here I am 23 years later.
I don’t recall not accepting my colostomy. My philosophy was “I am still alive and I will be okay with some lifestyle adjustments”. I completely understand that not everyone feels this way. It is very personal and depends on their circumstances.
We had no Ostomy Chapter in my community so support seemed almost non-existent. I didn’t know of anyone else in my community who had an ostomy, though I was sure that there had to be more people than just me. Back then, it was not really talked about and was kept ‘hushed’. I attempted but failed to get any interest in starting a support group in my community.
I decided I would make the necessary adjustments and live my life as best I could. I had to make diet changes after a few blockages. For a few years I struggled to find the proper ostomy products. I’ve had pouches blow off during the night from a build-up of gas, leakages from not having a pouch fully clicked in, wafers peeling off after two days of wear, and filters on the pouch not functioning leaving me smelling like crap. Though I was very happy to have health insurance which paid 80% of the cost of these essential ostomy products, I still had to pay 20% of the cost. I have never understood why these vital products are not covered 100% federally.
When I returned to work as a nurse, I was much more aware of patients who had ostomy surgery. I just could not help myself to pop in and see if these new ostomates might need some support. Back then we didn’t have ostomy visitors. When my coworkers noticed I was taking a special interest in new ostomy patients, they often reached out to see if I could visit new ostomates. I was always so happy to do this. I think those visits helped me as much as it helped the new ostomates.
We moved to Moncton 14 years ago when my husband’s employer, Abibiti Consolidated, shut its doors for good. I can say without a doubt that this was the best move we could have made. A few years after we arrived, I learned there was an ostomy chapter which I have been a member for about the last ten years. I also became a Certified Ostomy Visitor with Ostomy Canada and continue to enjoy providing support to new and existing ostomates.
Ostomates are a very unique group who have learned to make many lifestyle changes to live life to the fullest. Our chapter members feel like family to me and I am always so happy to see them. Since I became President of Ostomy Moncton, I have been even more involved in advocating for things that would make life better for ostomates in our province. Our awareness campaign will continue because there are still so many people who are not aware of what an ostomy is. This is my passion, so I will continue on to do my best to represent us ostomates. n
Sharon is the President of Moncton & District Ostomy Association
By Susan Kydd-Haynes
1988 was to be an incredibly exciting year for Martin and me! We had been together for two years and were very happy. On Christmas Day 1987, we told our families that we had become engaged and would be married in the fall of the following year. We were so excited and had so much to plan and put in place. Life had been good. I was really enjoying both my nursing career and those who I worked with. I had travelled across Canada a couple of times and enjoyed an extended trip of four months to Europe. I had lived in Vancouver and worked on the Burn Unit at the Vancouver General Hospital while I was there. That was a tremendous experience which I really enjoyed.
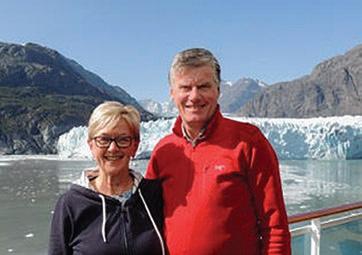
soft diet. I was given instructions about my ileostomy and how to change my appliance.
The nursing staff were excellent. Ruth Kenney, ET (*as NSWOC was known then), was extremely knowledgeable and a wonderful ostomy teacher. I learned so much from her. I began to slowly regain strength and my weight was also slowly improving. I knew my recovery period would take time, but I felt good about the positive improvement. Martin visited me each day, often having to work late evenings afterwards as he was an accountant, and it was tax season. My goal was to be on a plane to England in mid-June to attend Martin’s brother’s wedding.
I was extremely fortunate to have been a very healthy individual. Except for the odd cold or flu and the usual childhood illnesses, I was extremely healthy. I didn’t know that that was about to change. In January 1988, I began to experience what I thought were symptoms of the flu; nausea and vomiting. These symptoms would stop and start and then became more frequent, to the point where I began being absent from work and was losing weight. My GP referred me to Dr. Wil Henderson, a GI surgeon, who later told me that upon our first meeting, he knew from how I looked and from reviewing my previous test results that I would require surgery. By then, I was frequently sick and vomiting. I was very nervous about what was about to happen. I was told that I would require an ileostomy. There was a large ulceration on my colon, which needed to be removed. It was thought that I had either Crohn’s Colitis or ulcerative colitis.
I was admitted to the Victoria General Hospital in Halifax. Martin told me that my having an ileostomy wouldn’t change his love for me and our plans to marry. That meant so much. Martin and my parents were with me for long periods each day. Friends and those who I worked with visited me regularly. It was hoped that I would gain strength and regain some weight before going for surgery. Despite everything, that didn’t happen. I kept getting weaker and weaker to the point that I was only able to get up to use the commode if it was placed beside my bed; the rest of my time was spent in bed. I was scared, depressed, and going through a lot of Kleenex to wipe my tears. I had lost so much weight that I no longer wanted to look in the mirror! Dr. Henderson visited me daily and phoned the nursing station in the evenings to see how I was. He admitted to me later that he wasn’t sure if I would make it through surgery.
On Easter weekend, I was taken to the OR as an emergency case. My colon was removed, and an ileostomy was created. After several days in ICU, I was transferred back to the floor and remained at the hospital for about two more weeks. I began mobilizing with assistance, and gradually moved from a liquid diet to a
After about two weeks, I was discharged to my parents’ home, in Bridgewater, Nova Scotia. My parents were wonderful and supportive. My dad and I would go for daily walks outside. Eventually I was strong enough to stand up on my own. It took time for me to regain my strength. I had to be very conscious about changes, such as being careful with what I lifted and to be sure to use proper body mechanics. I also had some dietary accommodations.
I joined the Halifax United Ostomy Association (UOA) soon after my discharge from the hospital. I found the members of the chapter very supportive and the guest speakers to be wonderful teachers, and I certainly benefited from my participation in the chapter.
Despite only being two months’ post-op, Martin and I make it to England in mid-June 1988, to attend his brother’s wedding, visit his parents, and enjoy our holiday away, visiting friends in Scotland, as well as travelling to France. We had a wonderful time away! When we got home, we continued to prepare for our own wedding. I returned to work in September and was glad to be back. Our wedding took place as planned on October 29, 1988, in my hometown of Bridgewater. We had photos taken in the town park, followed by a dinner and dance at the Legion Hall. Everyone enjoyed themselves very much. I had suffered a small bowel blockage a few days before our wedding, which fortunately passed comfortably on its own, although it did mean I had to be hospitalized the week before our wedding. We were all hoping I would be discharged in time to be at my own wedding (which, fortunately, I was…just!) Although, it did mean I was not on a full diet, so while everyone enjoyed a beautiful wedding dinner and wedding cake, I had a bowl of beef broth.
In early 1989, we moved to Moncton. I joined the UOA chapter where knowledge, support, and friendship continue. I have been active in the chapter and have always found it rewarding, not only for the information you gain from speakers and each other, but for the long-term friendships and camaraderie with the other members. I became an ostomy visitor and have visited many new ostomates throughout the years, hoping to have helped them adjust to their new lives with their ostomy. I was president of our chapter on two occasions, for a total of five years. It was an enjoyable experience. While I was a member, our chapter hosted the national conference where members from many provinces as well as the US attend-
ed; a highlight was taking a group to the famous Hopewell Rocks and having lunch there afterwards. That was so much fun! We also travelled to attend several conferences in the Atlantic region, and enjoyed meeting fellow ostomates from across the country. We were also involved in advocacy. I met the Mayor of Moncton, explained our chapter to him and its importance in the community and how we help others experiencing ostomy surgery. He told me he wasn’t going to give us any money, but our picture was taken together and placed in the newspaper! I also worked with our chapter in advocating with the local hospital about the importance of having, (as they were known as then), ET nurses to support ostomates and their support system.
Life has been good. We adopted and raised three, now grown daughters and a son. We travelled across the continent and to Europe and enjoyed time in our own beautiful Atlantic region. Of course, nothing goes smoothly in life, with or without an ostomy. I have had my share of leaks, sometimes requiring me to conduct an emergency change in the front seat of a car! Unfortunately, over time, I developed four hernias, which were all surgically repaired. My stoma was moved from the right side of my abdomen to the left side of my abdomen during the third hernia repair. After the fourth hernia repair, I was told that I could have no more surgery. I have been lucky with my medical team, and my current surgeon, Dr. Shakerania, is an excellent and supportive individual. My husband, Martin has been by my side every step of the way as well. I am really
fortunate to have the support that I have!
I am still a member of the Moncton & District Ostomy Association (formerly known as the Moncton chapter of the UOA). The meetings are informative, fun, and provide an opportunity to meet others who have gone through similar experiences, who are knowledgeable and doing well. I should also say that we are so very fortunate to have NSWOCs present at the Moncton Hospital and the Georges Dumont Hospital, as well as in the community. I have received assistance from these professionals when I have had questions or problems, and they are an invaluable resource in the community. They also devote their spare time to supporting the chapter and its activities. We are so very lucky to have caring professionals like them in our community. I have had my ileostomy for 36 years now. I know that I must be careful about some things that I eat and some things that I do, but overall, life has been good. It hasn’t held me back and, if I do encounter an issue now and then, I know who to contact to put me on the right path. Thinking back to 1988, and the state of my health at that time, I am pretty happy with the way things turned out! n
*note: Enterostomal Therapists were called ET’s and are now known as NSWOC’s
Susan is a member of the Moncton & District Ostomy Association

By Jenny Jones
My life as I knew it changed when I was nine years old and looking back, there’s so much I know now that I wish I knew then, so much that I see drastically different now 30 years later.
I was diagnosed with the rare, hereditary colon cancer syndrome, Familial Adenomatous Polyposis (FAP), when I was eight. FAP affects a lot more than just the colon with many associated cancers and extra-colonic manifestations. My family has a long blood-line of FAP. I was fortunate to grow up with both my mother and my grandfather, who also inherited FAP and required permanent ileostomies as a result.
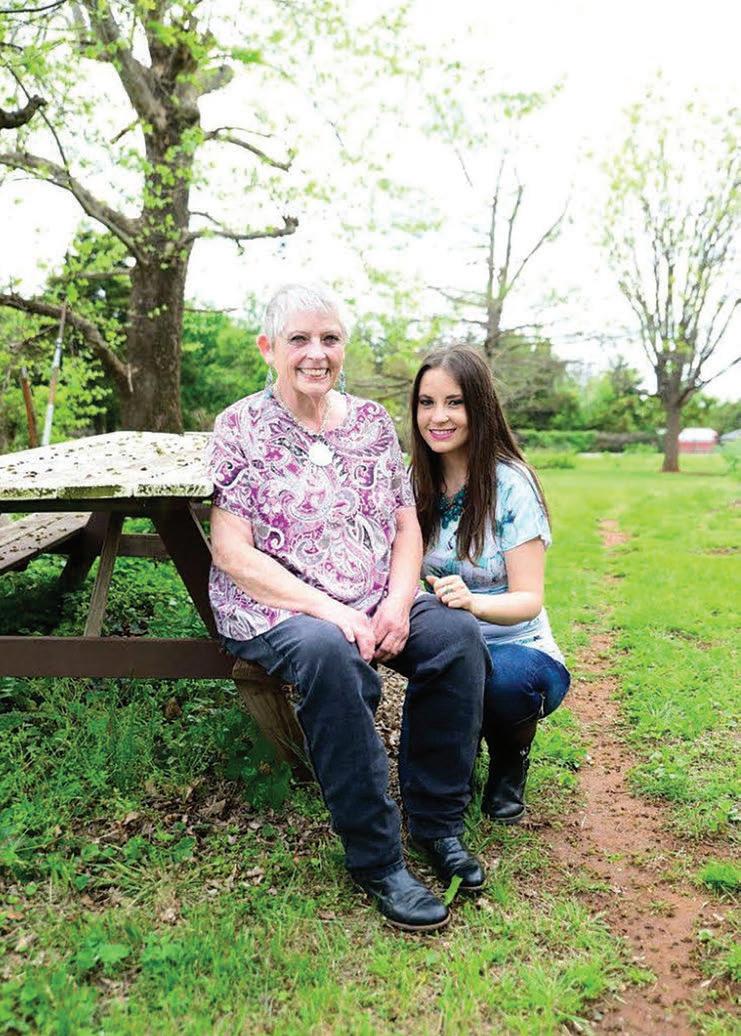
At nine, I underwent a colectomy to remove my colon as my polyps were starting to turn cancerous. However, I experienced surgical complications that left me traumatized, barely alive and with an ileostomy that was expected to be permanent. I was familiar with ostomies before then, watching and helping my mom change hers and I knew grandpa had one too. I think if it hadn’t been for all of the medical trauma I endured during the span of a year following my first surgery, I would have accepted my ostomy.
I still remember the first time my ostomy bag needed to be emptied. In any situation, there’s something about when it’s you and your body that changes your perspective and your reactions. I never felt grossed out by my mom or grandpa’s ostomies. But the idea of emptying my own grossed me out. I can still hear my dad telling
me that I had to get over it and I was going to have to learn to take care of it myself; after all it was now part of me. I laugh every time I relive that memory, if only that nine-year-old girl knew just how much feces and urine she’d eventually touch throughout her lifetime, and that she would think nothing of it now.
By the end of that first year of surgeries, there wasn’t much laughter left in me and there wouldn’t be for several years to come. I changed from being an outgoing, carefree child to becoming excruciatingly shy. I was depressed and was full of rageful hate. I was consumed by my medical Post-Traumatic Stress Disorder. I was ashamed of my body and my medical history. I was terrified of anyone knowing anything about my medical condition in fear that I wouldn’t be accepted. I wore extremely baggy clothing for my small frame hoping it hid everything about me, including my ostomy. I couldn’t accept myself much less love myself. I didn’t think anyone else would either if they knew the truth. Fearful of being bullied, I changed schools only to end up being bullied anyway. I saw this as

confirmation that no one would accept or love me if they knew about my ostomy. I became suicidal and felt homicidal, blaming my parents, medical team, and bullies for all my pain. My nightly ritual for sleep was to sob for hours, unceasingly begging for death until I could no longer keep my eyes open. For six years, I lived in constant mental anguish until I had my ostomy reversed at age 15.
I attended the local ostomy support groups but found it hard to relate as everyone else was so much older than me. It wasn’t until I was old enough to attend The Youth Rally summer camp for teens with bowel and bladder disorders that I started to feel accepted. There I met others with similar experiences and developed lifelong friendships as a camper and later as a counselor. At age 14, I requested mental health counseling to start processing my medical trauma and to learn healthier coping skills. After my reversal, I now found my body acceptable and I began to embrace my scars. I was still highly guarded about my medical details and the secrets behind my scars, although I was still fearful that I wouldn’t be accepted or loved if someone knew the entire truth about my body. It took until I was in my thirties to fully accept my body and my medical conditions.
Things I never once thought about anyone else with an ostomy, I thought about myself. I didn’t care that an ostomy is lifesaving. I didn’t care that for many people, it is also life-giving as it can drastically improve one’s health and quality of life. I felt fine before my ostomy, it was after it that my life changed, and I couldn’t see how








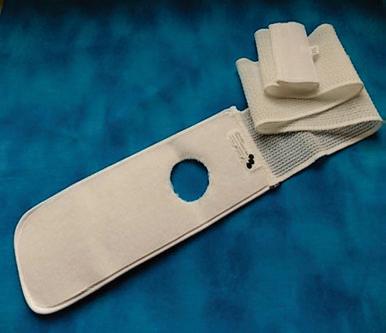



it changed for the positive.
But it did change for the positive. All the life choices I made while living in fear because of my ostomy and my health, where I went to school, what career field I entered, where I lived, are all choices I am extremely grateful for making now. They led me to a life I love, and I probably would have a completely different life without having made those decisions.
Looking back, I see that I just wanted to feel loved and accepted but because I was so fearful, I didn’t believe I could voice those needs. No one knew just how much I was hurting inside, how much love I needed that I wasn’t giving myself. I didn’t let anyone close. I didn’t share my thoughts with anyone. I lashed out in anger towards everyone around me, I self-isolated out of fear and anger. I was just a little girl needing love because she couldn’t find value in herself and thought no one else would be able to either. This is something I’m still working on to this day. The difference now is that I know my worth, and that my lovability doesn’t reside in my body or my medical conditions; it resides in my inner self, and I am loved, by many, even when I don’t love myself.
It’s these experiences that shaped my life into what it is now, it has given me purpose, for which, I am forever grateful. I established my rare disease advocacy platform, Life’s a Polyp, in 2012 focus-
ing on awareness, empowerment and funding FAP research. Through it, I’m afforded incredible opportunities to connect with an entire world of amazing individuals with similar medical experiences. I am able to build deep friendships with people I may never even have gotten to meet in person, yet who have captured my heart all the same. I’m honored to help others navigate their new lives with similar or even the same medical conditions, providing them with the love and support that I didn’t let anyone give me after my life changed. Now I’m working to change how FAP is treated through starting and funding the NORD FAP Research Fund.
I know now that my power resides within me, and that no one can take it from me unless I give it away. I know now that if someone can’t accept my body, or my medical history then they’re doing me a favor because that’s not who I want in my life. I know now that as difficult as it can be to accept and adjust to life changes, it’s possible. I know now that I’m more than what my body looks like. I know now that it’s good to use my voice and to ask for help when I need it. I know now that I’m not alone, I am loved and supported even on my darkest days when I can’t see anything good about myself and feel utterly alone. I know now that even when today is hard, that tomorrow can be better even if it’s just by a little bit. Life doesn’t stay the same and we don’t have too either.
If you’re struggling with your ostomy, your body, or your new life, you don’t have to believe it yourself right now, but I hope you hear the voices of the millions of people who currently have or previously had an ostomy telling you that you’re loved and supported. Fortunately, with the internet, we’re just a keyboard away and we look forward to embracing you, we just need you to reach out.
Jenny is a Rare Disease Advocate for Familial Adenomatous Polyposis (FAP) and Short Bowel Syndrome. Due to life threatening complications, Jenny has undergone eight surgeries, developed medical PTSD, and lived with an ileostomy before having it reversed into a Straight Pull Thru. Due to her medical experiences, Jenny established Life’s a Polyp in 2012 with the focus of awareness, empowerment, and funding FAP research. Her ultimate goal in life is to help others avoid the same medical and mental health experiences she did as a child with rare diseases and to empower others in the navigation of their own chronic illnesses. She started the National Organization for Rare Disorders FAP Research Fund in 2015, to which she donates profits from Life’s a Polyp Shop and her FAP Children’s Book - Life’s a Polyp with Zeke and Katie.
You can find Jenny at www.LifesaPolyp.com and across social media platforms @LifesaPolyp n
Jenny lost her mama, her best friend- Ina Jones to FAP shortly after the submission of this article.
www.LifesaPolyp.com
By Louise Levesque-Burley
My ostomy story began in 2021. My life story began when I was born with extremely low vision and chronic juvenile rheumatoid arthritis. I became totally blind at the age of thirty. I have worked in management, and I run my own business as an author, speaker, and coach. I have had two knee replacements and one hip replacement, and I have a guide dog, Mr. Fig. I have lived a full life and intend to continue to do so.
What else could happen? In May 2020, I had a colonoscopy and was diagnosed with ulcerative colitis. A few months later I began to have massive diarrhea and stomach pains. Three months later I was told that I had C-difficile. My best friend was the toilet and I felt like I was back to my baby-hood wearing diapers. I had absolutely no quality of life. Everything that I put in my mouth, a few minutes later, was dropped into the toilet.

Some of you will be able to relate to that! After those long nine months and many visits to the emergency room, it was decided that I try a stool transplant. It worked to get rid of the C-difficile; however, thirty days later, I was brought back to the hospital by ambulance. I was there for five weeks. Initially the gastrologist wanted to try different options of medications. I kept having pain and diarrhea. By this time, I had dropped from 144 to 107 pounds. I felt like I was dying. After two weeks of this, I told the doctor, “I need surgery now. I want my life back.” During all of this time I felt that the hospital staff were not doing enough to ‘fix me’, until one doctor explained, ‘The medical team and I are concerned about you having an ileostomy because you cannot see. We are not sure how you will be able to handle the post-surgery care of your stoma, changing the bag, and so on.’ Not knowing what was ahead, I replied, “Let me make that decision. I have been totally blind for the past 31 years and have adapted to everything that came my way. I want to have better quality of life and, therefore, ileostomy surgery is the answer for me.” I had the surgery which meant removing most of my large bowel and five feet of small bowel. When the pathology report came back, I no longer had a colitis diagnosis, it was Crohn’s disease.
The hospital NSWOC (Nurses Specialized in Wound, Ostomy and Continence), Denise Nicholson visited. I felt that she cared
about what had happened to me. She asked a few questions and began to guide me through my very first ostomy change. Denise was so thorough that I did the change with great success. At that moment, I felt confident that I would be okay in caring for my stoma, as I have always been a very independent person. Returning home involved a huge adaptation for me, my husband, and my dog. I needed to accept that my daily routine would never be the same. I wanted to give my stoma a name; I chose ‘Betsy’. Naming her helped me in accepting my new life. When it came to doing a pouch change, I found it totally disgusting, as I had to learn to touch Betsy in order to make sure she was clean. In addition, I had to deal with leakage, finding the right products and suppliers, finding someone to precut my pouches, organizing my different products so I could find them quickly, and ensuring I had good nutrition. I had to learn what, when, and how to eat. To this day, I still have to pre-plan every time I leave the house. On top of it all, I developed a parastomal hernia, which means I need to lie down when changing my pouch and also need to wear a hernia belt.
Now Betsy and I are best friends and it only takes us 12 minutes to make a successful ostomy change. Two years later, I wanted to give back to the ostomy community. I joined our local Moncton chapter to help in any way I could. I am currently Vice President of our ostomy chapter. I have recently completed the Ostomy Canada’s Visitor program certification so now I can support others who are on the ostomy journey. The President of the chapter and myself are actively working on getting a solid commitment from the New Brunswick Government for financial coverage to help pay for medical ostomy products. New Brunswick is the only province in Canada that does not have an adequate financial program to support persons living with an ostomy.
Living with Crohn’s disease, Betsy, my husband, and Mr. Fig has given me a second chance in life. I am trying to make a difference wherever I can contribute. Each day I live my life to the fullest, helping people make the Impossible Possible! n
Louise (and Mr Fig) is the vice President of Ostomy Moncton

By Michelle Gamage
‘The
most effective advocacy I do is to be seen as a person with a disability and a sexual person simultaneously’
B.C. sex worker GoAskAlex likes to lure men to her online profiles with thirst traps, and then pepper them with social justice content. This helps spread her “leftist politics” to her followers, who she says are mainly men from the eastern and central U.S. The strategy is working. As of this summer she’s built a following of more than 253,000 subscribers on platforms like Tiktok, Twitter and Reddit plus the folks who pay to view her content on OnlyFans and Suicide Girls. The Tyee has agreed to use GoAskAlex’s first name only in order to protect her safety. “Maybe I’ve got a fan who works in the
oilfields who doesn’t otherwise hear about environmental issues,” she says. “I’m exposing them to totally new ways of thinking and hopefully radicalizing them. Roughly one-third of Alex’s posts include some form of advocacy, like raising awareness about being an ostomate due to her ulcerative colitis, neurodivergent and Métis.
But she’s also outspoken against Amazon, is working to improve workplace safety for sex workers and spent time at the Fairy Creek blockades protesting old-growth logging.
“I feel like if I chose one niche to focus on it’d be better for my brand,” she says, shrugging. She also knows moving to Los Angeles or New York would be good for her career, but says she’ll never leave her home province of B.C. with its mountains, ocean and cloudy skies.
“I don’t want to live in a city. I want to go live by the ocean with six dogs,” she says.
Alex says she was raised with strong social and environmental justice values but her childhood and work in the non-profit sector was regularly disrupted by her ulcerative colitis, a type of inflammatory bowel disease where your immune system attacks your colon.
Inflammatory bowel disease affects around one in 150 Canadians and 25,000 British Columbians and is an incurable disease that inflames the lining of the gastrointestinal tract, disrupting the body’s ability to digest food, absorb nutrition and perform normal gastrointestinal functions, according to Crohn’s and Colitis Canada.
Alex says throughout her life she spent a lot of time in the hospital, trying different treatments and sometimes ending up back at the hospital due to the side effects.
Before she started sex work, she struggled to manage her pain and energy while working eight-hour shifts and “had eight roomies with eight cats and still had to ride my bike to the food bank to fill up a backpack with noodles and beans.”
Then a roommate recommended camming, a type of online sex work where you perform in front of a webcam for paying clients.
“I gave it a try and the rest is history,” she says. “The earning potential was greater than anything I’d experienced. I could log on and earn a couple hundred in a couple of hours.” The flexible schedule also allowed her to rest when she had a health flare-up. Because she made her own hours, she didn’t need to request time off or bank sick days for future illness.
The job had its ups and downs. It allowed her to afford necessary medication, travel internationally for the first time and buy herself a hybrid car. But she also spent up to 12 hours a day interacting with people online alone in her room, which she found isolating and emotionally exhausting. “I ended up very burnt out, but I remember it fondly,” she says.
Nowadays Alex focuses more on her OnlyFans website than camming.

‘People with disabilities do have sex, consume porn and are sexual’
By 2019, Alex’s health had taken a turn for the worse, sending her to hospital every couple of months. This was her “breaking point,” she says. She told her doctor she wanted to get surgery.
Patients need to be young and healthy to reduce the risk of potential complications from this kind of surgery, says Dr. Brian Bressler, co-founder of the IBD Centre of BC and clinical associate professor at the University of British Columbia. Bressler is not Alex’s doctor. Doctors will “try to align treatment with how a patient would like to live” and around one in seven will choose surgery, Bressler says.
Alex had a total abdominal colectomy. Surgeons removed her entire colon and created a small opening in her abdomen where she now has an ileostomy appliance on her lower abdomen.
Recovering and getting back to work had the added challenge of adjusting to living with a visible disability. While the adjustment was “difficult,” Alex says sex work helped her dive into body acceptance.
Alex also realized how underrepresented disabled people were in the porn industry.
Which she found weird, because “people with disabilities do have sex, consume porn and are sexual people but not represented as such,” she says.












The IBD Centre of BC’s Bressler says it’s common for patients to feel uncomfortable with their post-surgery bodies, which can impact their life and intimate relationships.
Alex says she chose to reject the discomfort with the fact her body was no longer “conventional” and be “loud” instead.
She is now the only ostomate porn star in North America. She produces videos that show her being sexual without hiding her ostomy appliance.
“I’m not here to fetishize my disability. I’m here to normalize it,” she says.
“I think the most effective advocacy I do is to be seen as a person with a disability and a sexual person simultaneously. Just being able to be visible as a person with a disability is advocacy in itself because it’s not something people are exposed to.”
Alex hasn’t been offered a role in a mainstream porn production yet and she wonders if it’s because producers are afraid of her disability or worried customers may fetishize it. She shrugs, adding she’ll focus on working with independent producers who do want to work with her.
Supporting
Many sex workers live with chronic illness, disability or struggle with mental health, Alex says. When she was diagnosed with ADHD and told her colleagues, “everyone said, ‘Oh yeah, me too,’” she says. Sex work is low-barrier, has a flexible schedule and is attractive for “creative brains,” she says.
This is why it’s important to support “farm-to-table” porn and not just websites that host free videos, which are almost always stolen or pirated.
“You get a better-quality product which is often made just for you. The consumer and creator can enjoy knowing the product is created safely, ethically, consensually and with a fair wage,” she says.
A typical work day isn’t as sexy as you’d expect — mostly Alex says she’s on her phone and laptop updating her various social media feeds, making and editing short clips and reels, answering emails, doing taxes and sexting her fans. This takes up a lot of her time because she’s on more than 10 sites, she says.
When Alex wants to create new content, she organizes a “shoot day” with several other colleagues. They’ll all get tested for sexually transmitted infections, hire a photographer, find dog sitters, turn someone’s house into a set and dive in. “It feels a bit like you’re working for 24 hours,” she says.
cost, access and options for ostomy appliances
A lot of Alex’s advocacy around ostomy appliances focuses on the lack of colours the medical device comes in.
“Ostomy supplies look like they’ve come right out of a hospital. Technology is improving function but not aesthetic,” she says.
All devices in Canada are either a pinkish beige, orange or “cement grey,” which don’t match people’s skin tones. They’re also transparent when wet.
“I feel like this is hinged on the belief that people with disabilities don’t need to look good or sexual,” she says. “That’s ableist, assuming I don’t need to look sexual while swimming or that I’m going to cover up my body and be ashamed so it doesn’t matter what the device looks like.”
A company in the United Kingdom makes ostomy appliances in black and powder white so Alex knows it’s possible — but says the company doesn’t sell overseas, and in the U.K. you need a prescription to buy them. There isn’t a sustainable way to get the supplies she needs from the U.K., she says.
Ostomy appliance covers can be bought to conceal the device, but Alex says that adds extra bulk to her abdomen and extra cost. Even with PharmaCare coverage ostomy supplies cost around $1,000 per month, Alex says. Depending on what province you’re in it can cost more she says, adding that she’s heard from health-care workers who say patients in the U.S. without health insurance have had to make their own.
“I’m lucky that I earn enough where I can afford basic supplies, but it’s still very expensive,” she says.
Porn festivals, university visits and conferences
Alex’s films have recently debuted at the San Francisco Porn Film Festival and screened at film festivals in Romania, Slovenia, Seattle and Rome. They’re forthcoming at the Berlin International Film Festival and Porn Film Festival Barcelona in October.
The Confession, which features a church booth that was “made out of an old armoire we found in an alley,” a confession to a priest and an orgy, won best in show in Seattle. It’s “very female gaze,” Alex says.
Alex says she’s also speaking at a conference about sex work in October, and recently spoke with a university class in California about sex, porn and disabilities.
Her future could include sex education or writing, she says, which she enjoys despite the fact it “doesn’t pay the bills the way porn does.”
“There’s so many things I want to do — I really need a couple assistants,” she says. “That would free up some time do work on advocacy which, really, brings me the most joy.” n
Naked Truths from Sex Worker GoAskAlex written by Michelle Gamage September 5, 2023. First appeared in The Tyee and reprinted with permission.
STUCK Film Premiere Recap - We are thrilled to share the exciting news about our short film, STUCK, about ostomy awareness. On Sunday, June 23rd, we had the honour of premiering the film at the Dances With Films Festival at the historic Chinese Theatre in Hollywood, California. The event was a resounding success, exceeding all our expectations!
A Night to Remember - The theatre was sold out, with enthusiastic supporters taking every seat. The atmosphere was electric as the audience eagerly awaited the screening. When the film started, it was clear that our ostomy awareness message resonated deeply with everyone present.
Spreading Awareness Through Cinema - Our goal with STUCK has always been to spread ostomy awareness through the powerful medium of cinema, and we delivered in spades. The film’s narrative struck a chord, compelling and empathetically bringing attention to the realities and experiences of individuals with ostomies.
Insightful Q&A Session - After the screening, we held a Q&A session, adding another layer of depth to the evening. Rai shared his personal connection to the character with an ostomy, offering heartfelt insights that moved many in the audience. He also took this opportunity to thank the Ostomy Canada Society for their unwavering support.
Praise and Recognition - STUCK received an overwhelming amount of praise from the audience and critics alike. The positive feedback was both humbling and encouraging, and we are proud to announce that the film is now being considered for several awards. This premiere marks the beginning of our festival journey, with many more exciting events to come!
Video footage from the STUCK Hollywood premiere can be seen here: www.ostomycanada.ca/blog/2024/stuck-hollywood-premiere/


Thank You for Your Support - We extend our deepest gratitude to everyone who has supported us in this endeavour. Your encouragement and backing have been instrumental in helping us spread positive ostomy awareness.
Stay tuned for more updates as we continue our festival tour and bring STUCK to wider audiences.
Raimo Strangis is an author, screenwriter, and songwriter from Toronto, Canada. His debut novel, “The Kingdom of Grape,” was widely praised for its charm, wit, and adventure. “With Little Means” continued to showcase his exceptional talent for crafting engaging stories. His third novel, “As We Know It” is set to be released in 2024. Raimo is an executive producer of the short film “Stuck,” a story inspired by his life experiences. Raimo is also an accomplished songwriter, with his original songs earning a devoted following. Despite facing significant challenges, including living with an ostomy after years of suffering from ulcerative colitis, Raimo remains dedicated to his creative pursuits and inspiring others to follow their dreams.
Follow Raimo online! Visit his website at www.raimostrangis. com, or follow him on social media! ! n
www.raimostrangis.com
TikTok star Bella Brave, whose real name is Bella Thomson, passed away in July. She was 10 years old. Bella’s mom, Kyla Thomson, shared the news of her passing on TikTok alongside a video of her daughter dancing. Kyla wrote in the caption, ‘Our brave girl left her legacy here on earth to dance on streets of gold. Bella passed peacefully in our arms.’ Bella was inspirational to so many in the medical community. We had hoped to get her to youth camp but her health battles kept that from happening. We were hopeful after Bella underwent a life-saving bowel transplant earlier this year. Bella and her family enjoyed a few wonderful months, getting to do so many things they had long wished to experience. Sadly, a viral lung infection landed Bella in the ICU for her last time. It was there that she took her last breaths, with her family holding her closely. Please check out some of Bella’s social media features and inspirational roles she played in so many lives, helping those of us struggling with a bad day, simply follow her attitude, of, “;;;;”it’s all ‘meh’ there have been better and there have been worse. Just remember to always be Brave!”
“Bodies Are Cool” by Tyler Feder
A wonderful book that celebrates the uniqueness and beauty of individuals. Written for children, it provides a much-needed platform to celebrate different types of bodies, helping to break down stigma and raise awareness. Each page is filled with inspiring pictures and empowering messages, showing that life with any type of body can be full and rich. The book is not only informative but also uplifting, offering a powerful message of acceptance and positivity. One of the most remarkable aspects of the book is its inclusivity. It features a picture of a person with an ostomy, and the activity they are doing is a powerful image of freedom, joy and ability. Additionally, there is a page dedicated to scars, highlighting their stories and the beauty in their healing. This book is a must-have for any library, especially those with children or grandchildren. It teaches valuable lessons about body positivity, diversity, and acceptance, encouraging readers to love and appreciate their bodies just the way they are. n ~ Book review by Andy Manson
Editor: Let’s play I spy / Where’s Waldo and try to find the ostomy pouch in the photo shown. Did you find it?
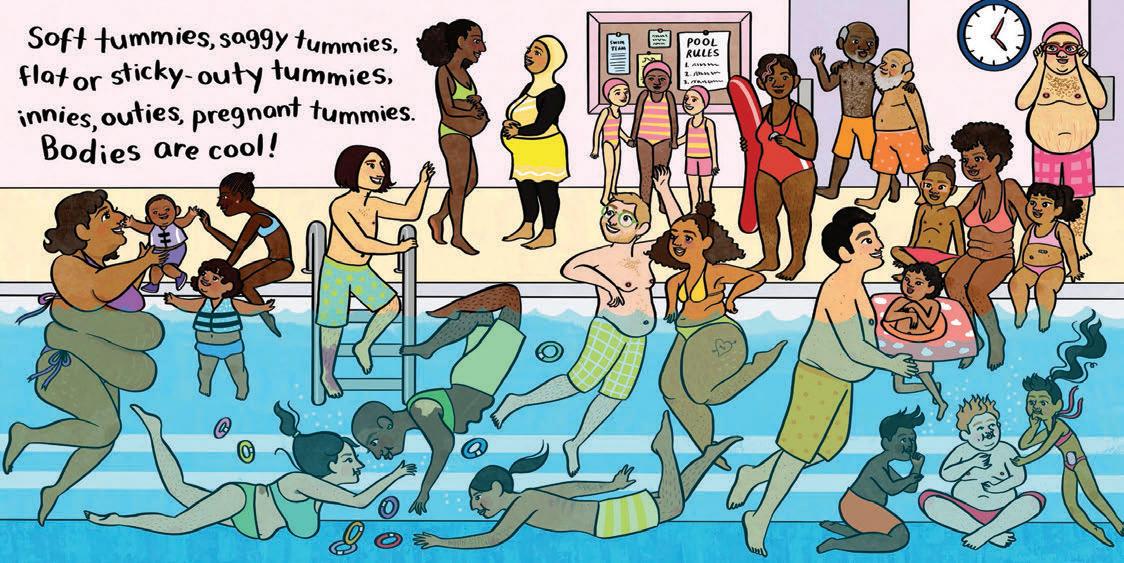








Did you know that the word ‘ostomate’ is commonly used and appears in the dictionary?!
Mirriam Webster Dictionary – definition of the word ‘ostomate’
: an individual who has undergone an ostomy
: an operation (such as a colostomy, ileostomy, or urostomy) to create an artificial passage for bodily elimination
Collins Dictionary – definition of the word ‘ostomate’
: a person who has had an ostomy
: a surgically created opening, the surgery that creates such an opening

Lego - Have you seen that LEGO has a new friend?
Meet Sara, a lego figure with an ostomy, and she even has the scar many of us are left with after surgery. I love that this will create more awareness for our ostomy/IBD community, especially for children! Being able to play with a figure that looks like them while showing them they can do anything while living with an ostomy is powerful and priceless. This figurine is only sold with the Heartlake City water park theme set!


1 out of 3 people who experience itchy skin around the stoma have healthy looking skin.†
The CeraPlus skin barrier may help. It helps protect against dryness, a possible cause of itching, by working to protect your skin’s natural moisture barrier. To learn more about the ceramide-infused CeraPlus skin barrier, or to request a FREE sample, contact us at 1.800.263.7400 or visit us at www.hollister.com.
Prior to use, be sure to read the Instructions for Use for information regarding Intended Use, Contraindications, Warnings, Precautions, and Instructions. † Consumer Survey of Pruritus, Hollister Incorporated, 2016. Data on file. The Hollister logo, CeraPlus, and “Healthy Skin. Positive Outcomes.” are trademarks of Hollister Incorporated ©2019 Hollister Incorporated. Sometimes you see it,



www.hollister.com



The CeraPlus skin barrier comes in a range of fit options including one-piece, two-piece, flat, firm convex, soft convex, tape border, and tapeless

