THE THE THE
MEDICAL MYRIAD MEDICAL MYRIAD MEDICAL MYRIAD
ARTICLES ARTICLES
Q&A’S WITH CONSULTANT DOCTORS Q&A’S WITH CONSULTANT DOCTORS
WORK EXPERIENCE REFLECTION WORK EXPERIENCE REFLECTION
MEDICAL STUDENT Q&A
MEDICAL STUDENT Q&A
OXFORD HIGH SCHOOL OXFORD HIGH SCHOOL HIGH

01 CONTENTS 2 5 7 12 16 21 24 28 30 38 39 40 Q&A WITH OBSTETRICS AND FOETAL MEDICINE CONSULTANT, DR CHRISTINA AYE Q&A WITH CARDIOLOGY CONSULTANT, DR JAMIE KITT WHAT ARE INDUCED PLURIPOTENT STEM CELLS? THE THYROID GLAND MUSIC THERAPY TREATMENT FOR ALZHEIMER’S DISEASE Q&A WITH 1ST YEAR MEDICAL STUDENT, MARYAM WORK EXPERIENCE REFLECTION: BRAIN SHUNT SURGERY FOR THE TREATMENT OF HYDROCEPHALUS REFERENCES THERISEOFULTRA-PROCESSEDFOOD MEDICAL BOOK REVIEWS Q&A WITH ORTHOPAEDIC SURGEON, DR SALMA CHAUDHURY ACKNOWLEDGEMENTS
Q&A
WITH DR CHRISTINA AYE, CONSULTANT OF OBSTETRICS AND FOETAL MEDICINE AT JOHN RADCLIFFE HOSPITAL, INTERVIEWED BY Y12 STUDENT EMMA
Q: AT WHICH STAGE IN YOUR CAREER DID YOU DECIDE TO WORK IN OBSTETRICS?
I left medical school thinking I wanted tobeapaediatrician,butafterIdidan F1inpaediatricsurgeryIrealisedthat I didn’t enjoy seeing sick children all thetime,soIwaskindofatalossas towhattodo.
Ithenspent4monthsdoingobstetrics andgynaecologyasthefirstjobofmy F2 rotation and really loved it, because it was a huge mix of things andaveryvariedcareer.
I have found in this career path that there is something for everyone : if you'reverysurgically-mindedthenyou can do gynae oncology or urogynaecology; if you’re into medicine then you can do maternal medicine; if you’re somewhere in the middle and you like a varied day-today life, you can do operating on a delivery suite or procedural based stuff such as scanning and foetal intervention. I really liked how varied itwasandhowtherewassomethingto suiteveryone.
Q: CAN YOU DESCRIBE WHAT A TYPICAL DAY LOOKS LIKE FOR YOU?
I spend most of my time in foetal medicine, which involves doing ultrasound scans of babies, either seeing new patients or making first assessments. These babies that have been referred to us have either got growth problems or structural abnormalities. Women also come in whorequireinvasiveprocedures,such as amniocentesis or CVSEs, where you sample placenta to get a genetic sample for the baby. I spend four out of five of my days doing that, but it's really nice as you never know what you’regoingtoseenext.
I do three general clinics where I see differentproblemstodowiththebaby, and then I do one special foetal cardiac clinic whereby we just do foetal echoes, which involves looking at the structure and function of the foetalheart.
02
One day a week, I am the consultant on the delivery suite or covering the elective caesarean sections so I manage the labour ward. This is very busy because Oxford is probably the 2nd biggest maternity unit in the country, so I do the caesarean sections, the instrumental deliveries which includes supervising juniors to dothat,orIdotheelectivecaesarean list.
Q: DO YOU FEEL THAT YOU HAVE A GOOD WORK-LIFE BALANCE AND HOW DO YOU MANAGE THAT?
Yes,Ido.Ihavetohaveagoodworklife balance because I have four children so I think actually working and having such an enjoyable, fulfilling job makes me a better mother.
Ithinkit’salsoreallyimportanttobea good role model because I have got two daughters myself. I want to show them that actually you can have a career but also be really present for your children. I try my best to ringfencetimeespeciallyontheweekends whereby I try not to do any work unless I’m on call over the weekends so I can concentrate on looking after them, being present for them and taking them to all their extracurricular activities.
I make sure that every so often I still do the things that I love, like do some exercise and go out with friends. We also travel quite a lot so we always make sure we have the next holiday booked which I think is really important when you’re working so hard.
03
Q: WHAT IS THE WORST THING ABOUT YOUR JOB?
When we lose babies and very rarely when we lose mothers. Part of the reason why I love this speciality is because you’re usually dealing with really young, fit people who are going through a really happy time in their life, so most of the time my job is really happy and it's such a privilege to be there to help women through their pregnancies and during their deliverywhichisaveryprivatetime
Being involved in bringing babies safely into this world is a real privilegesomostofthetimethereare lots of highs, but the lows are really low. When you have to deal with couples who have lost their baby, and very occasionally when you lose mothers, usually because of things that you can’t prevent, that’s really tough because it’s meant to be a happytime,soit'sreallydifficult
Q: IF YOU COULD GIVE ANY ADVICE TO YOUR A-LEVEL SELF TO PREPARE FOR MEDICINE AS A CAREER WHAT WOULD IT BE?
Be resilient. Realise that there is something for everyone in medicine and don’t be worried if you don’t find the thing that really grabs you in medical school. When you start working as a doctor it’s very different from the experience in medical school, and I think that you can be quite sad that you haven't found the thing that you want to do, but it will come!
I think that once you find your niche and you find your little area that you feel passionate about, which will undoubtedly happen because there's so many different careers in medicine, you will have a really fulfilling career Just stick at it!
04
What are Induced Pluripotent Stem Cells?
WRITTEN BY Y12 STUDENT BEATRIX
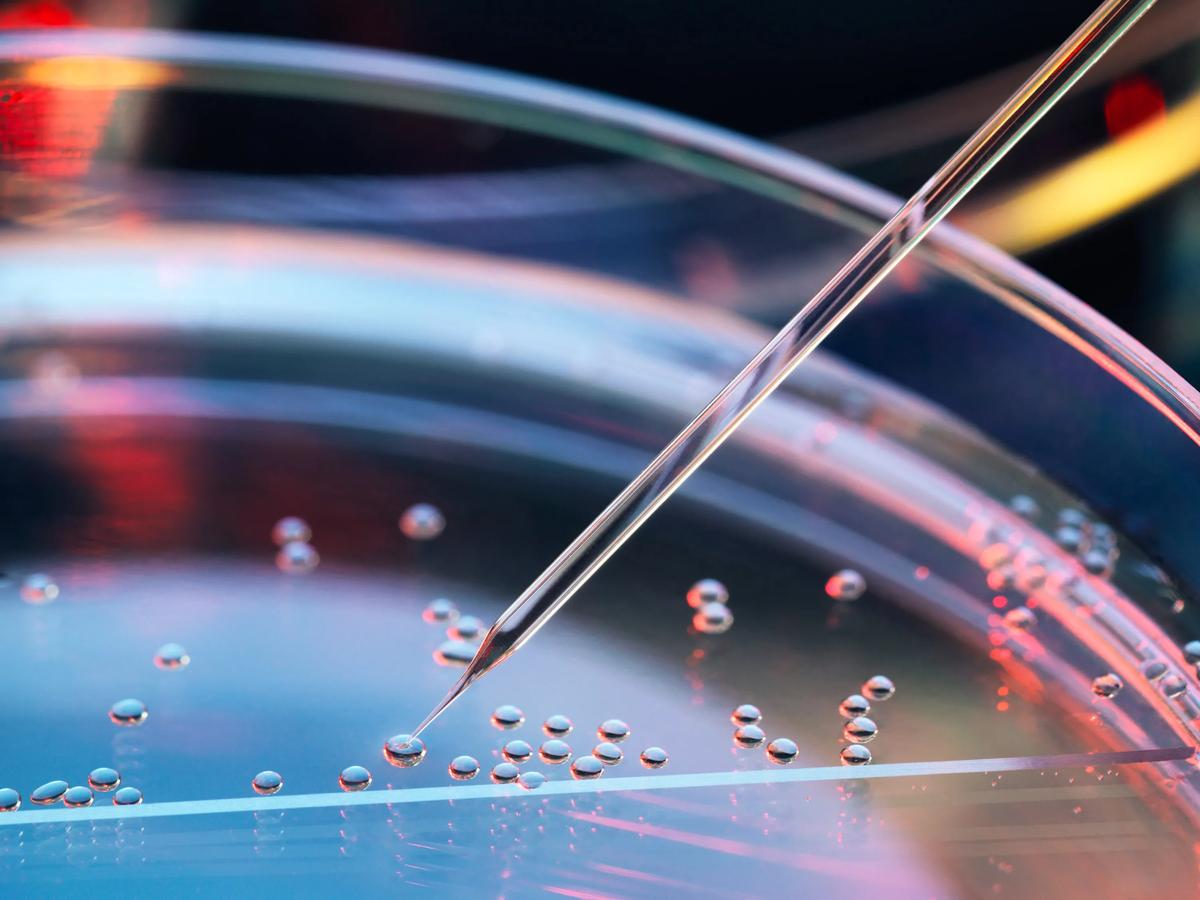
Theethicsofembryonicstemcellresearchhave always been debated amongst many medical scientists and researchers. Induced pluripotent stemcells(iPSCs)havebecomearevolutionary development in regenerative medicine, allowing scientiststocarryoutmedicalresearchwithout dealingwiththeethicaldebatesurroundingthe destructionofahumanembryo.
So what exactly are induced pluripotent stem cells? iPSCs are pluripotentstemcellstakenfromsomaticadultcellsthataregenetically reprogrammed to regain the ability of an embryonic stem cell (ESC) so that they can differentiate into different types of cells. iPSCs were first discoveredbyShinyaYamanakaandKazutoshiTakahashiin2006,where both of them reprogrammed mouse fibroblasts (a type of cell that contributestotheformationofconnectivetissue)withthehelpofseveral transcriptionfactors,inducingESCcharacteristicsinthem.

Thefourmaintranscriptionfactorsinvolvedin producingiPSCsareOCT4,SOX2,KLF4,and c-MYC, known collectively as OSKM or the YamanakaFactors.OSKMfirstbindtoregions in chromatin that other somatic cell factors cannot access, causing the regions to rearrange themselves and turning on/off the expression of some genes. For example, OSKM binds to enhancers of pluripotency genes to further induce their expression. OCT4 and SOX2 is mainly used to maintain the primitive state of the induced stem cells, while KLF4 is used to enhance the pluripotency of these cells. These processes gradually cause these somatic cells to adapt a gene expression similar to that of pluripotentESCs.
05
Now that the transcription factors used to create iPSCs have been discovered,onemaybegthequestion:howaretheydeliveredintocells? There are several methods for delivering the Yamanaka factors into somatic cells The most effective delivery method is via a retroviral vector. A retroviral vector contains sequences and gene promotors that accommodate and enhance the genes that are to be delivered into the target cells As the vector can enter the cells easily and integrate into thegenomeinthenucleus,therehavebeenraisedconcernsaboutvirusinduced tumour formation To mitigate this risk, the retrovirus-delivered transcription factors have been developed to be expressed outside the nucleus, which reduces the likelihood of integration into the human genome Despitealloftheconcernssurroundingretroviralvectors,itstill remains one of the most effective delivery methods for the Yamanaka factors


iPSCs hold significant potential in the future of medical research. For one,patient-specificiPSCscouldbecreatedfromthepatient’sowncells so that new, identical tissues can be formed for transplantation therapy. This allows doctors and researchers to overcome a hurdle in organ transplantation, as tissues formed from iPSCs from the patient’s own cells are less likely to experience rejection from the immune system In addition, iPSCs allow animal models to be replaced in clinical trials Animals have a very different genetic makeup from humans, and cannot mimic the microenvironment of a typical human cell On the other hand, iPSCs are able to model diseases more effectively as they can replicate human physiological conditions since they are derived from human adult cells. iPSCs are also far more cost-effective than using animal models, making them a suitable option for any future clinical trials in medical researchers
In conclusion, iPSCs are a powerful tool in the field of medicine Through their ability to differentiate into many types of body cells, they open up many opportunities in understanding diseases and regenerative medicine, benefiting the future of medical research
06
Q&A
WITH DR SALMA CHAUDHURY, ORTHAPAEDIC SURGEON AT NUFFIELD ORTHOPAEDIC CENTRE, INTERVIEWED BY Y12 STUDENT HAJIRA
Q: HOW DID YOU CHOOSE THE MEDICAL SCHOOL YOU WENT TO AND WHAT DID YOU ENJOY AND DISLIKE ABOUT YOUR EXPERIENCES THERE?
A: I wanted to go to Cambridge because I aspired to go to a medical school with quite an academic focus, but also that small campus feel of being in a college within the larger university environment; it was incredibly friendly and fun because it meant you could socialise with plenty of people studying different subjects. Of course there was also the fact that it’s a beautiful city and not very far from home In terms of what I disliked about my experience, I would say, and they’ve changed it since I graduated, but the fact that we had to do really big exams at the end of each year with a lot of pressure in having to memorise a lot of content and going into a level of detail that I realise, looking back, was not very necessary when it comes to actually being a doctor
Q: WHAT PROMPTED YOU TO BECOME A SURGEON AS OPPOSED TO A HOSPITAL DOCTOR?
A: I think I always knew I wanted to be a surgeon. I liked the idea of doing something practical, with my hands. I also liked the prospect of being able to directly influence the outcome of a patient’s medical case, more so than a prescription can sometimes.Thefactthattherearen’t long ward rounds and that when you’re in the theatre you can immediately see if you’ve fixed an issue or not struck me. So the rewarding nature of it was quite appealing. Also I liked the variation that comes with the job, with every surgery being different. And I admiredthementalityofsurgeons,in that getting things done quickly and seeingresultsisemphasised.

07
Q: WHAT WOULD YOU SAY IS THE MOST CHALLENGING THING ABOUT BEING A SURGEON?
A: Iguessit’sthefactthatthingsrest on your shoulders and when you’re in the theatre it can be difficult sometimes because you’ve got to rely onyourselftodealwitheachsituation; there’s a big responsibility there. There are times when you’ve done your best, but you don’t know if the patient will have the best outcome necessarily, which brings about a feeling of personal responsibility for everything good or bad that may happentoapatientafterwards
Q: WHAT DIFFERENCES ARE THERE BETWEEN HAVING A MEDICAL CAREER IN THE UK AND WORKING IN THE US?
A: The training in the US is shorter, but much more intense There's a very structured progression to going ‘higher up in the ranks’ and becoming more specialised In terms of the environment, what's positive is that the Americans have quite a ‘can do’ kind of attitude towards work

The negatives about the States are probably the poor work-life balance but also especially in the hospital I was working in in particular, which is a leading hospital there, there was a lot of pressure to operate whereas in the NHS you can manage patients cooperatively and patients are much more willing to consider non-operative treatment
As well as this, in the UK patients don’t really have to consider the financial pressures of operating so I think people’s decision-making is different compared to in America. Equally in the US another benefit is that patients can get access to specialists sooner.

The reason why comparing the two systems is complex is because the healthcare system I was working in is in essence equivalent to working in the private healthcare system e in the UK I think the NHS wever offers amazing value for ney. I'm really proud of the fact t we offer everyone here atment when they need it, it ht be more timely for some ople but it’s a very equitable tem, it doesn’t differentiate ed on wealth I think it’s really od that we do things like clinical ls here which you couldn’t really licate in the US because they n’t have something like the NHS re.

08
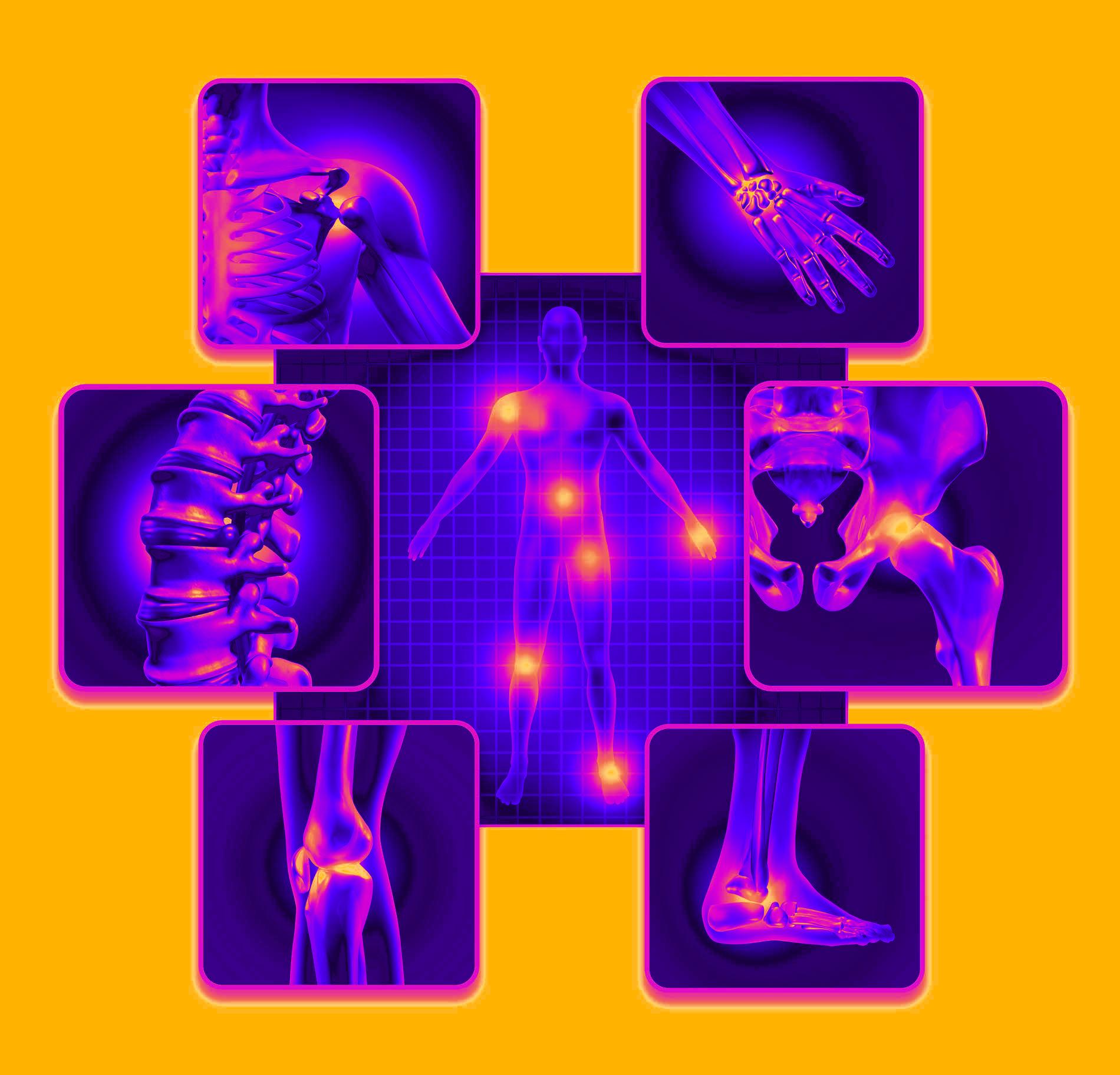
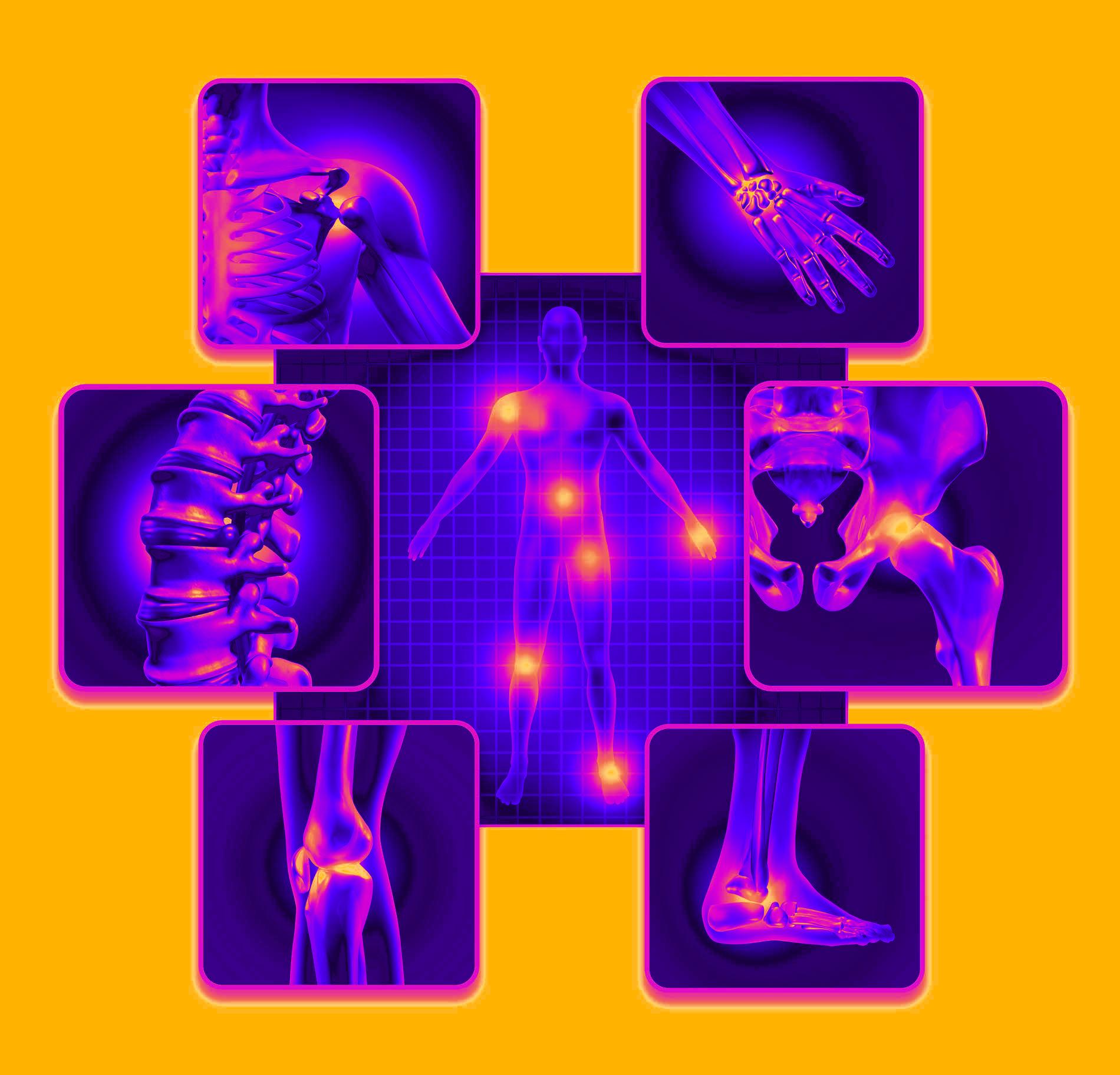
Q: WHAT ARE THE MOST COMMON PROBLEMS THAT YOU SEE GENERALLY?
A: I mostly see older people with fractures and breaks of their shoulders, but I also see some younger people with shoulder complications or fractures of their clavicles. I also see some soft tissue problems so quite a few people with tendon-related issues. Those are mostly the things I come across most often.
Q: HOW DID YOU COME TO THE DECISION TO SPECIALISE IN ORTHOPAEDICS?
Q: CAN YOU DESCRIBE A ‘TYPICAL’ DAY FOR YOU?

A: So generally my days consist of one of three ‘types’. One is a clinic day where I see a mixture of fracture patientsandelectives,whicharelongstandingproblems.Thesecondkindof day is when I actually perform the elective operations, so basically dealing with non-traumatic injuries. The third type is where I operate on trauma patients, so today, for example, I operated on someone who brokeboththebonesintheirforearm, and then somebody who broke their shoulder so they needed a shoulder replacement. Earlier in the week I did a surgery for tendon repairs and dislocationonanelectivewrist,soit’s amixtureofthingsreally.
A: Initially I really wanted to do cardiac surgery because I did a cardiac rotation at a hospital in Cambridge,inwhichIhadtodealwith life or death situations pretty much. I also did an elective in the US and I really enjoyed it. Based on these experiences though I learned that cardiac surgery is incredibly long and intense,sothewayIsawit,ittakesa big toll on your life. As well as this, with things like stents and such being introduced, the need for bypass surgeries was decreasing. Overall I didn’t envision a life of being a cardiac surgeon to be an interesting one for me. With orthopaedics, however, I really like how you’re able tofixthings,it'sabitlikeplayingwith LEGO in the way you put bits and pieces back together. With the surgeriesyouperformtherearelotsof interesting different instruments and pieces of equipment you get to work with.

09
I find it really rewarding that you’re helping people to regain function, and independence especially, which is such a key aspect for maintaining a good quality of life. When making my decision, I appreciated that it’s a specialitynotreallytodowithlifeor death situations. In the orthopaedic surgeon community I appreciate that they are quite light-hearted, don’t take themselves too seriously, as well as the fact that it’s quite an academic field in that it involves biological knowledge as well as aspectsofengineering.
Q: HAS ANYTHING PARTICULARLY DIFFICULT TO MANAGE EVER HAPPENED TO YOU WHILST PERFORMING AN OPERATION AND IF SO HOW DID YOU DEAL WITH IT?
A: I can’t think of anything particularlydifficultbutIwillsaythat certain operations will be more complicated than you thought, some are just hard to perform. When it comes to that kind of situation you’ve just got to get through it, finish the operation, and do the best that you can. Sometimes you see terrifying things, like big open fractures from car crashes, so the nature of the injuries you come acrosscanbequitedifficult.
It’s important to remember that although as an orthopaedic surgeon you want every bit and piece to be perfect it’s not always that predictable.Ithinkanotherdifficulty is that sometimes patients might have complications that are not necessarily related to surgery but it stillfeelsverypersonal,youalways feelreallyguttedanddevastatedfor your patients because of the responsibility you hold as a surgeon. But I guess that’s the nature of being a good medic in general, most of us feel incredibly responsible for all aspects of our patients.

Occasionallyinsurgery, complications,suchasafracture thatyouoperatedonnotfully healing,forexample,oranother complicationthatwasdirectlylinked toyourinterventioncanfeelquite tough.Youdealwithit,butyoufeel badaboutwhatthepatienthasto gothroughforyoutofixyour mistake.

10
Q: ARE THERE ANY QUALITIES THAT YOU BELIEVE YOU NEED SPECIFICALLY TO BE A GOOD SURGEON THAT YOU DON’T NECESSARILY NEED TO HAVE TO BE A GOOD DOCTOR?
A: I think the key to being a good surgeon is to be resilient You need to be willing to and capable of working under pressure, and have a reallyhealthyabilitytotakeonrisks, withtherightleveloffocus,butalso understand your limitations and not exceed appropriate risks. So you want to always be developing your skills but not work outside of your competency level Also sometimes surgeons can be a bit harsher than doctors in that the environment of the surgical field can feel harsherperhaps harsh isn’t the word but in thevarioussub-specialtiesof



surgery, to do well generally the standards are really high and you’ve got to be willing to work hard to maintain those standards That’s not tosaythatsurgeonsaren’tgenerally nice people, but they can be a lot more direct perhaps At the end of the day though, it’s all very rewarding in a slightly different way toworkingasadoctor
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE TO SAY?
A: I think something important to mention is that especially for girls, orthopaedics generally has a bad reputation for being full of really sporty and confident men who can be a bit exclusive, but the truth is that the field’s really changing; it’s lovely, it’s welcoming and it’s fun. There are an increasing number of women, minorities, and other groups of people working in the orthopaedic surgery space So the reality of being an orthopaedic surgeon is quite different to what it’s often stereotypically portrayed as and anywayyoushouldn’tletstereotypes affect the decisions you make in where you want to go and what you wanttoachieve

11
the thyroid gland
WRITTEN BY HAJIRA
The word ‘thyroid’ is probably familiar to you. You may have heard the term being used in a human anatomical context by reading the odd page here or there out of interest. You may simply know it as a gland that produces hormones Or, it may well be a completely foreign term to you but you have a growing suspicion that it’s all to do with things that can go horribly wrong…
The truth is the thyroid gland is a part of human anatomy that has a lot more significance than many people realise. Located in the neck, it is described as being ‘butterfly-shaped’ and is responsible for producing hormones that regulate metabolic rate, development and growth. By just listing these three functions, the extent of its value is severely undermined So, in order to battle the overlooking of this intriguing anatomical phenomena, I’ve decided to shed some light on a topic that is arguably not talked about enough.



The thyroid gland’s main function is controlling metabolic rate, i.e. the rate at which energy is consumed by the body. It produces two key hormones, triiodothyronine (T3) and thyroxine (T4). The principle difference between them is that thyroxine (T4) is considered the biologically ‘inactive’ form of thyroid hormone, whereas T3 is considered the ‘active’ form - this is because T3 is better received by receptors in body cells than thyroxine. These hormones are released via a ‘feedback loop’ system in which the hypothalamus (a structure actingasalinkbetweenthebody’sendocrineandnervoussystems)inthebrain releases thyroid-releasing hormone (TRH) which, in turn, stimulates the pituitary gland to produce and release thyroid-stimulating hormone (TSH). The ‘feedback loop’ system applies in this case because, to regulate thyroid hormones, when T3 and T4 levels increase, TRH (and therefore TSH) is not releasedandviceversa.TSHthentriggersthethyroidglandtoproduceT4and T3-oftheamountofhormoneproduced,around80%isT4and20%T3atthis stage. With this system, the thyroid gland is able to release hormones that are able to be transported to cells in practically all organs, as they are needed everywhereinthehumanbody.
12
Some of our specialised cells are able to produce T3 from T4, in a process knownasenzymaticouterringdeiodination,whichoccursinthedigestivetract -the term may sound rather complicated, but essentially it conveys that the processoccursinthepresenceofenzymes,andthataniodineatomisremoved from the outer tyrosyl ring (the T4 chemical structure). One of the contributing factors to thyroid complications, therefore, is iodine deficiency. Hence, it is important to consume enough iodine from your diet to support your thyroid gland,oftenfoundinfoodssuchasfish,seaweed,eggs,dairyandiodisedsalt.

Alongsidelowblood-iodinelevels,various diseases can trigger thyroid complications. The two most commonlyknown (but fortunately, not very commonly-occuring)onesareHashimoto’s thyroiditis disease and Graves’ disease. These are both auto-immune conditions that, to put it simply, are caused by the unusual presence of antibodies which attack thyroid cells - the reasons as to why these antibodies are produced are unknown. Hashimoto’s thyroiditis involves cells in the immune system leading to the death of the thyroid's hormone-producing cells. This usually results in a decline in thyroid hormone production, known as hypothyroidism. Graves' disease, on the otherhand,isinessencetheopposite-it is the severe over-production of T3 and T4. The disease can be a cause of hyperthyroidism, a term used to refer to any kind of overproduction of thyroid hormones.





Despitethefactthattheycan sometimespresentthemselvesas aresultofhavingrareautoimmune conditions,hypo-andhyperthyroid-relatedissuesthemselves areactuallyquitecommon, especiallyinwomen(mostoften causedbythenon-autoimmune conditionfactors).
13
Hyperthyroidism can cause symptoms such as an unusually rapid heartbeat, weight loss, tremors, and anxiety. Common symptoms of hypothyroidism, on the other hand, include constant fatigue, unprecedented weight gain, depression, dry skin, and hair loss. All of these symptoms, as you can imagine, can be significant obstacles to managing daily activities.




As well as the factors mentioned already, certain medications, radiation exposure, and genetics can increase the risk of being affected by these disorders.
Diagnosing thyroid issues typically involve a combination of blood tests to measure hormone levels, imaging studies such as ultrasound, and sometimes biopsies to evaluate thyroid tissue. Treatment options vary depending on the underlyingcauseandseverityofthecondition.Forhyperthyroidism,treatments may include medications to block hormone production, radioactive iodine therapy,orsurgerytoremovepartorallofthethyroidgland.Hypothyroidismis usually managed by taking daily medications (such as Levothyroxine) to increasethelevelsoftherelevanthormonesinthebody-thiskindoftreatment isknown,morecomplexly,assyntheticthyroidhormonereplacementtherapy.

So with regards to thyroid complications and indeed, the aforementioned potential suspicion that the thyroid gland is ‘to do with things that can go horriblywrong’,‘yourfear’waspartiallyjustifiable-thisis,afterall,amedical magazine. And when it comes to this gland in particular, where, according to the NHS, an estimated one in 50 women have either a diagnosed or undiagnosed thyroid condition, and with Levothyroxine being the third most prescribed drug in the UK, it becomes increasingly apparent that raising awareness of thyroid issues and looking out for potential symptoms earlier rather than later is paramount to prevent unnecessary suffering as much as possible.

14
You may know a relative, a friend, a neighbour, or anyone else that suffers from thyroid complications My own mother, for example, has hypothyroidism and is one of the many people who needs regular prescriptions of Levothyroxine. The way I see it, with regards to any medical condition, it is best not to try to empathise, as it is rather difficult to imagine yourself in a position where you would have to manage a condition that you have no idea what the symptoms feel like. What can sometimes be more important, I think, is in fact the seemingly more ‘trivial’ things, the small, meaningful acts that show you maintaining consistent support If it is a family member who is affected, it could be things like offering to help them around the house more or making them their favourite meal once in a while, for example Even if it’s ‘just simply’ asking them how they are. You never truly know the extent to which these ‘trivial’ things you do alleviate some of the stress that inevitably arises from having a long-term medical condition



Of course, often (and hopefully) not every day is going to be an absolutely dreadful experience for them, especially if they are receiving treatment. However, ensuring that you are there for them during the harder times and having a sense of awareness and compassion in your daily interactions with them can sometimes be the most unparalleled solace you can provide. Overall, actively try to be a source of comfort for that person, whoever they may be to you, because, at the end of the day, it matters.





15
Q&A
WITH DR JAMIE KITT, CARDIOLOGY CONSULTANT AT JOHN RADCLIFFE HOSPITAL, INTERVIEWED BY EMMA
Therefore I did some work experience during my summer holiday, and I went and worked at some GP practices, including some hospital work in various specialties. I applied to graduate medicineasIreallyenjoyedusing science to help people and so came into medicine via that route toOxford.
Q: HOW DID YOU COME TO THE DECISION TO PURSUE MEDICINE?
Iinitiallyappliedtonaturalsciences in Cambridge because I loved BiologyandChemistry,andIwasn’t certainat18ifMedicinewasforme. Ihadn’thadahugeamountofwork experience and I liked David Attenborough,soIthoughtI’dgooff and see how I found natural sciences!
During that course structure you overlap with Medicine and Vets, so that includes courses in pathology and pharmacology, as well as cellular level courses of evolution behaviour of animals. Halfway through the course I realised that I actually like the medical side of it more and discovered that a science careerwas trickyasyouhadtodoa self-funded PhD - it was difficult to getabreaklikeDavidAttenborough!
Nowadays, there’s over 25 graduate courses throughout the UK, so I’d say that if you’re not sure now, you still have the chance to explore something else because you can change your mind. I think that there’s quite a few people who do natural sciences and come back, as well as other people who do subjects like biomedical sciences or even lawthatcomebacktomedicine!
Q: CAN YOU DESCRIBE WHAT A TYPICAL DAY LOOKS LIKE FOR YOU AS A CONSULTANT?
The great thing about medicine is thatthereisnodaythesame.Some job plans have a certain structurefor example, having a clinic on one dayandalistintheafternoon.I’ma cardiologistsomyscheduleincludes activities like taking pictures of people’sheartsusingaCTscanner.
16
However, even if you follow that same timetable every Monday it’s slightly different because there’s a differentsetofpatientswithdifferent problems-eventhoughyou’llhavea variety of tests that you’ll do which are similar, you’ll adjust the test accordingtothepatient.
Anotherelementthatyouhaveisoncallrotas-ontheweeksyouareon call, you’re seeing a new set of patientswho’vebeenadmittedtothe hospital unwell with various conditions,andthisincludesworking with a different team of junior doctors, so each day is slightly different. Some days you’re on call, andyou’llbedoingawardroundon the acute unit, other days you’re more clinic-based or running an imaginglist.Ifyou’readifferenttype of doctor like a surgeon you might be in the theatre, and other days you’ll be making a ward round. I thinkthegreatthingaboutmedicine isthevariety.Ifyoulikevariety,and yougetboreddoingthesamething, medicineisagoodoption!
Q: DO YOU FEEL THAT YOU HAVE A GOOD WORK-LIFE BALANCE AND HOW DO YOU MANAGE THAT?
Going into medicine you have to realisethatthework-lifebalanceis reallyhardtoachieve.Ijustfinished mytrainingnowandittookmefrom 2009-2023,whichis14years,and duringthatIwouldn’tsaythatIhad agreatwork-lifebalance.It’squite hardtocontroltherotabecauseit’s often written by rota managers rather than doctors, and it’s at random-youcan’tcontrolifyouget putontherotaonyourbirthday, Christmas,Easter,Diwaliorother religiouscelebrationsthatyoufollow -sometimes you have colleagues whoareniceandwilldoswaps,but there’s a fair number of family celebrations that you’ll miss and unfortunatelyyouhavetodonights andweekends.
Asaconsultantit’sslightlybetteralthough you still have to do weekends,theshiftsareshorterand normallyyoudon’thavetodonights asaconsultant.Howeverifyoudo specialties like paediatrics or if you’reonintensivecare,oftenyou willstillbeonatnight,butforthe vastmajority,onceyou’vefinished yourtraining,thework-lifebalance isslightlyeasier.
17
The other thing that I’ve done is research during my training. If you introduce research alongside working NHS it gives you a slightly nicerbalancebecausethedaysthat youaredoingresearch,you’remore incontrolofyourhours
Q: AT WHICH STAGE IN YOUR CAREER DID YOU DECIDE TO WORK IN CARDIOLOGY?
During your F1 year, you are provisionally registered and everyone is nervous to see where they’re signed off to, to become a fullpartoftheGMCregister!During that time, you tend to go on three month medical and surgical rotations ThisisthesameinF2,but at that point you can decide what specialtyyouwanttogointo
When picking your specialty, different factors do come into play. PeoplewanttobecomeGPsbecause training is quicker, they can lead their own practice and have more control over the work-life balance. Others decide that they want to do core surgical training because they arehands-onpeople
Some decide to become a medical specialist because they realise that they like the diagnostic conundrum, being a detective and piecing together different pieces of informationtomakeadiagnosis.
For me, I wanted to be a medical doctor and I already knew that I liked two particular specialtiescardiologyandinfectiousdiseases I had dreams of doing infectious diseasesandgoingofftothetropics andfindingacureformalaria,TBor workingonHIVvaccines
Iwasfortunateenoughtobeoffered both, so I had to weigh up what to do For me, infectious diseases meant doing a PhD abroad; if I hadn’t been married and had childrenonthewayIprobablywould have done that as it would have been quite exciting, but going for 3 years wouldn’t have been possible Therefore, I opted for cardiology because it had procedural stuff and a variety of specialties which I enjoyed,includingimaging, working on heart failure, doing interventions inthelabandworkingondevicesfor people that have cardiac arrest Cardiology also fixes people quite fastsothere’sasenseoffeel-good fromquickfixesasopposedtocare oftheelderly,whichisoftenamuch slower,moreholisticprocess.
18
Q: WHAT DO YOU ENJOY MOST ABOUT WORKING IN CARDIOLOGY?
You do make a lot of people bettercardiology is very heavily funded for research, including by charities like the British Heart Foundation - I was funded by them myself Therefore, you can bring about change in practice very quickly due to the amount of money that has gone into research
There are also a lot of treatments that work; you now know that if you’ve been up a blocked blood vessel that’s causing a heart attack, the sooner you open it up, the more likely you are to have a normal life expectancy; similarly we know that if you’ve had a cardiac arrest on the football field, like we’ve seen in the press, if you put a defibrillator in, that can save your life if it happens again
We have lots of drugs that treat heart failure now and keep people living many more years than they would have in the past. So I think for me, the fact that it's always pushing the boundaries of science and that you’re always implementing the latest technology into clinical practice is something I enjoy the most.
Q: WHAT IS THE WORST THING ABOUT YOUR JOB?
The worst thing, no matter what speciality that you’ll do, is that you can’tsaveeveryone.Theworstthing is those difficult conversations that you have to have with family membersatthetimethatpeopleare ill,breakingbadnewstothepatient themselves and then trying to steer them on that journey towards their end of life That's a specialism withinitselfandit’sarealskilltobe a palliative care doctor and it's a very important part of medicine. Personally,Iliketofixpeople Ifind that the hardest part for me is approaching the end of life discussions and helping people on theirjourneybecauseinaway,even thoughit'snotafailure,itfeelslike afailureattimes.
19
Q: IF YOU COULD GIVE ANY ADVICE TO YOUR A-LEVEL SELF WHAT WOULD IT BE?
Dowhatyouthinkyou’regoingtoenjoythemostinuniversity.University was definitely the best time I’ve ever had in my life and I was fortunate enoughtogoto2greatuniversitiesandbetherefor7years.Ifyou’regoing tobedoingmedicineyou’llbedoinganywherebetween5and6yearsthere, so a big chunk of some of your late teens and early twenties is spent in university
Medicine is a very competitive process coming from A levels and despite thefactthatit'sreallyhard,thereisstillmorecompetitionforplacesthan ever, which is a real testament to how many people want to do the job. Makesuretogointoitwithyoureyesopen;don’tjustgoanddoafewdays on a ward round with someone you know, but try to get a variety of experience GotoaGPpractice,goonanambulancecrew,donightshifts ifyoucan,seesomepaediatricA&E,getahugebreadthofexperienceso yougoinwithyoureyesaswideopenaspossible,becauseitwon'tbefor everyone,butitisagoodcareer.
It’sobviouslyimportanttoworkhard,butit’salsoreallyimportanttohave extracurricular activities whether it's music or sport or the arts or theatre becauseyouneedtohaveareasoutsidemedicinethatcanlateroninlife actasescapemechanismsatstressfultimes Iwouldalsosaythatifyou're not completely certain about doing medicine don’t be scared to go for anotherdegreethat'srelated,likenaturalsciences,orbiologyorbiomedical science,becauseyoucanalwayscomebacktomedicineifyou’renotseton itatthistimeinyourcareer
20
Music therapy treatment for alzheimer’s disease
WRITTEN BY EMMA
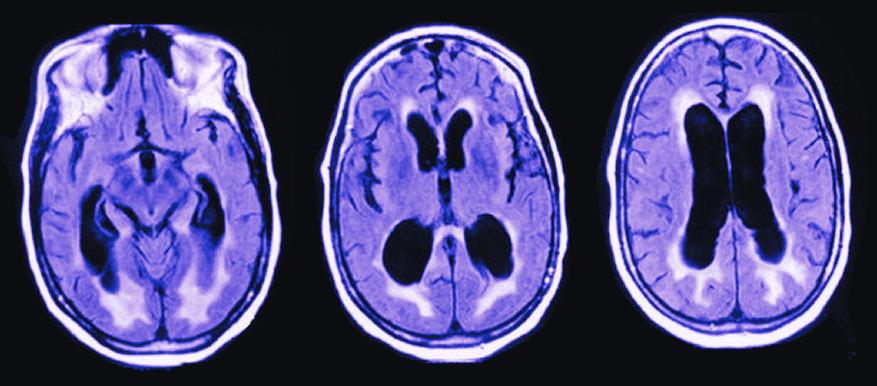
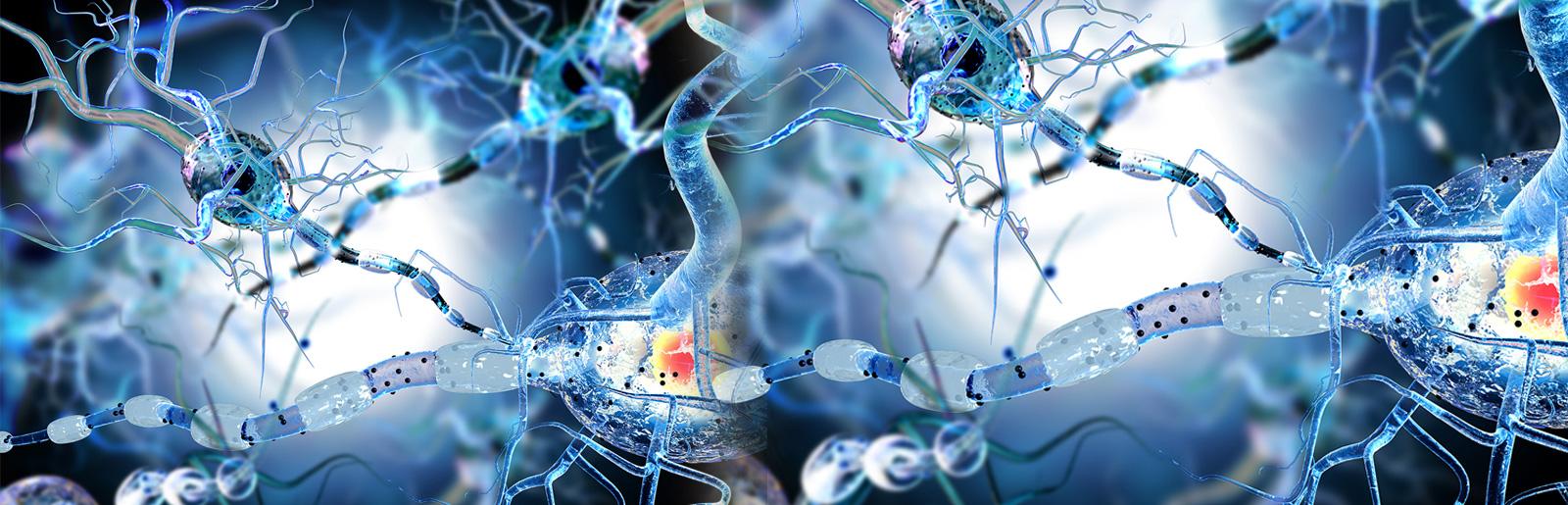
Dementia is defined by the NHS as ‘a syndrome associated with an ongoing decline of brain function’ and the most common cases of dementia are accounted for by Alzheimer's disease and vascular dementia There are further subtypes of dementia which fall under this ‘umbrella term’, including Lewy body dementia and frontotemporal dementia In the UK, 1 in 11 people over the age of 65 have dementia, and Alzheimer’s disease in itself is estimated to affect 5% of men and 6% of women worldwide, with Alzheimer’s disease being a cause for 60-80% of dementia cases overall. Although there is no cure for Alzheimer’s disease, pharmacological therapies have been used to manage the neuropsychiatric symptoms, but due to their inability to have long-lasting success, other non-pharmacological therapies have been used alongside these treatments, which includes music therapy. Music therapy has gathered momentum over the last few decades as a complementary treatment to manage symptoms of Alzheimer’s
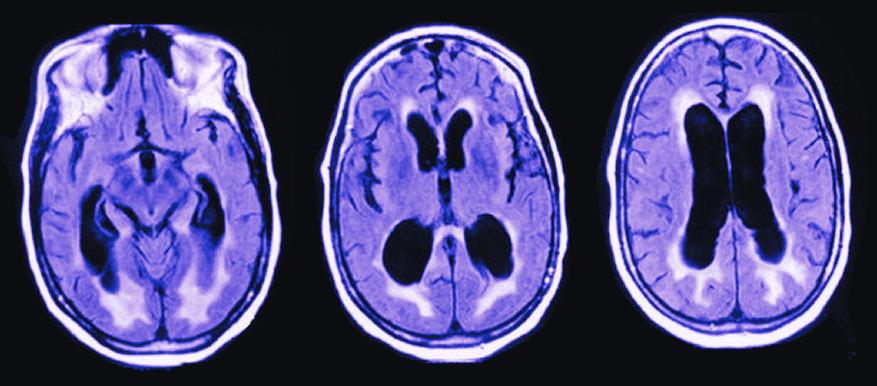
The causes of Alzheimer’s disease are still not fully understood by scientists, but are generally attributed to an abnormal build-up of proteins in and around the brain; this includes deposits of amyloid which forms plaque around brain cells, and deposits of tau which form tangles within brain cells This disruption of brain cells can result in a decrease in neurotransmitters, most notably of acetylcholine in Alzheimer’s disease patients, resulting in a reduced ability to send messages between brain cells, affecting communication, metabolism and repair Over time, different parts of the brain shrink, normally affecting the connections of neurons involved with memory first, such as the entorhinal cortex and hippocampus, and eventually affecting the brainstem, which is critical in heart and lung control, alongside swallowing Factors that can increase the risk of Alzheimer’s disease are a family history of Alzheimer’s, ageing, smoking, obesity, high blood pressure and high cholesterol levels
21
The symptoms of Alzheimer’s disease can be divided into three parts, and as the disease progresses, many aspects of a person’s life can deteriorate, including memory loss, the extremity ofmoodswingsandlossofspeech Somepeople alsohaveexperiencesofhallucinations,paranoia and in the later stages they can have dysphagia (difficultyinswallowingoreating)whichresultsin verypersonalisedcarebeingrequired
MusictherapyforAlzheimer’sdiseasecanbeusedtoaddressthephysical, emotional, cognitive and social needs of individuals, and incorporates differenttechniquessuchassinging,clappinganddancing,orlisteningto music with the intent of having an emotional response. Although the evidencefortheeffectivenessofmusictherapyforpeoplewithAlzheimer’s disease is inconsistent, music has been previously found to have positive effects on the patient, including reducing agitation, improving care-giver relationships and evoking memories or emotions Some studies have demonstrated that music therapy increases hormones such as cortisol, alongside promoting neurotransmitters such as endorphins, dopamine and endocannabinoids.
The long-term memory of music, in the salience network of the brain, remainsintactuntiltheverylaststagesofAlzheimer’sdiseaseprogression beforeitattacksthebrainstem,resultinginagreaterlikelihoodofmusicto evoke memories even in later stages of the disease; researchers in the UniversityofUtahHealthwhoplayedpersonalisedplaylistsforparticipants with dementia under a functioning MRI found that music activated whole areas of the brain, causing regions to communicate, including the visual network,thesaliencenetwork,theexecutivenetworkandthecerebellarand corticalcerebellarnetworkpairstoallshowingsignificantlyhigherfunctional connectivity. Using individualised playlists are a crucial part of music therapy,withstudiesshowingthatmusicenjoyedfromtheagesof10to30 yearsoldismoreenduringandrekindlingforpatientswithAlzheimer’s.
22
Thetechniqueswhichareusedinmusictherapycanalsobeusedforaiding movement Physiotherapists can use music to aid regular movement exercises,whichisimportantinAlzheimer’spatientsduetotheirdeclineof visuospatialskillsasthediseaseprogresses Occupationaltherapistsalso advise and train care workers in how to use music and singing for reminiscence Thiscanalsobeaspecialexperienceforboththecaregivers and the individuals with Alzheimer’s, with singing and dancing together creatingaveryspecialexperienceandenvironment.
Overall, the benefits of music therapy forpatientswithAlzheimer’sareclearly seen; due to its economical, nonpharmacological and non-invasive nature, it is important that it is more widely used The International LongevityCentreestimatedthatincare homesonly5%ofpeopleincarehomes have access to music, despite 80% of peopleincarehomeshavingdementia, and this needs to change, due to the beneficialeffectsofmusictherapy

23
Q&A
WITH MARYAM J, 1ST YEAR MEDICAL STUDENT AT LEEDS UN I VER S I T Y , I NT ERV I EWED B Y HAJIRA
Q: WHAT ARE SOME MAIN DIFFERENCES BETWEEN THE WAY YOU LEARN AT MEDICAL SCHOOL AND AT A LEVEL?
A: I think the main difference is that there’s a lot more independent learning at university than at school, you’re expected to do things like taking notes, revising as you’re going, and doing reading before lectures without being told. The volume of content is a lot larger and so you go through content a lot faster. The majority of the things you learn are taught in the form of lectures which is why reading before-hand on the topics covered is important


Alongside lectures, we have seminars where we work in small groups to do cooperatively-based activities. In a lecture-type environment though there are many more people learning alongside you and so there’s less room for you to compareyourselftootherstudentsmost of the time you’re just focused on yourself, which is actually a less difficult aspect in comparison to doing A Levels at school. The content in the first year is split up into modules such as ethics, and science, and you have 6-7 modules that you cover, which are basically like 6 or 7 subjects, so what you learn in each is targeting distinctly different pieces of content. Some people struggle in the first term if they haven’t developed a good foundation for independent learning skills at A Level. But overall, in my experience, the first year of medical schoolisn’tparticularlydifficult.
Q: HOW DIFFICULT IS THE CONTENT COVERED AT MEDICAL SCHOOL COMPARED TO AT A LEVEL?

A: I would say that the content is not massively difficult at this stage, the difficult thing is probably the volume of content as I mentioned before, rather than the content itself being conceptuallychallenging.


24
Q: HOW DID YOU COME TO THE DECISION THAT YOU WANTED TO PURSUE MEDICINE?
A: I think the main reasons for me choosing to study medicine are that I wanted a degree with quite clear job prospectsandquiteadefinitivecareer path. Obviously I really enjoyed Biology and Chemistry. I also really wantedtoholdabasisarounddoinga job involving interactions with people; that was quite an important factor when making my decision to apply for ahealthcaredegree.




Q: WHY DO YOU THINK MEDICAL SCHOOLS PLACE SO MUCH IMPORTANCE ON CHEMISTRY A LEVEL WHEN APPLYING AND DO YOU THINK IT’S JUSTIFIED?
A: At this stage in medical school, whichisonlytheverybeginning,no, I don’t think that it’s completely justified. I don’t really see a direct link between the content I’m studyingandthecontentIlearnedat Chemistry A Level. So I haven’t really experienced any parts of the medical course where A Level Chemistry knowledge is particularly useful. But I think the reason that medicalschoolsplaceimportanceon takingitismoretodowiththeskills that you get from studying it rather than the content you learn. In my experiencethewayIlearnedtowork through problems critically, understandconceptsandapplythem to different situations has been useful when learning things at medical school. So overall I’d say the skills you gain from it are more importantthanthecontentandthat’s whatmedicalschoolsarelookingfor whenyou’reapplying.


25
Q: DO YOU FEEL THAT YOU HAVE A GOOD BALANCE BETWEEN YOUR STUDIES AND EVERYTHING ELSE IN YOUR LIFE?
A: Yes, I do think so It’s not really challenging for me to have a good balancebetweenmystudiesandmy day-to-day life because although I havetolearnalotofcontentthere’s always plenty of time in the day to do other things. I think bearing in mind that at medical school everyone's goal is the same, to become a doctor, is important because you’re not in competition with anyone else and you can study atyourownpace-it’sreallyforyou to decide how and when you get things done, because as I mentioned before you’re mainly relying on independent learning rather than instruction from teachers. So I’d say it’s quite flexible in how you can plan your time and we’re not overwhelmed with work to the point where we can’t have a good balance between studies and other things we want to do

Q: CAN YOU DESCRIBE WHAT A TYPICAL DAY LOOKS LIKE FOR YOU?
A: So typically for medical students it’s different than for people studying other courses because we usually have morning lectures every day which start at around 9:00 AM Between lectures we have 10 minute breaks And it’s different every day but sometimes I have a seminar in the afternoon or evening which lasts around 2 hours The seminars are usually for one of the modules so I might have a group work session on communicationorethics,forexample On the busiest days I sometimes have another 1 hour lecture or seminarstraightafter.Usuallyweget alunchbreakfrom12:00PMto13:00 PM.IwouldsayIhavearound5or6 hours of a combination of lectures, seminarsandotherlearningactivities in terms of classes, at the maximum for any given day On Tuesday mornings, from 9:00 AM to 12:00 PM we get assigned to a hospital or practice to observe some work - we have to get there on time and be quite strict with that, because getting there can take up to an hour sometimes, so organisation is key of course


26
Q: WHAT HAVE YOU ENJOYED THE MOST ABOUT STUDYING MEDICINE SO FAR?
A: Ilikedthecontentthatwecovered in the 2nd term which included body systems in particular, so things like the cardiovascular and respiratory systems which we went into a lot of detail in, one by one. I love the anatomical aspect of the medical course the most and find it super interesting. In my 1st term we did a medical sciences module which started off with a bit of a recap of some Biology A Level content and then we had some lectures on blood anddiseases,soIenjoyedgettingto grips with the foundational kind of knowledgeinthescientificmodules.

In terms of wider university life, I’ve enjoyed the fact that you get to meet so many different people and socialisingissortofeasierthanitwas at school I’ve also liked joining societies and doing activities, such as medicine society, Muslim society, horse riding, baking, things like that There are just so many options that you can choose from so there’s a real varietywhenitcomestoactivitiesthat you can do at university to help destress
Q: WHAT ABOUT STUDYING MEDICINE ARE YOU LOOKING FORWARD TO IN THE FUTURE?
A: I would say I’m excited to reach the level where, during a placement at a hospital, I can start to really understandwhat’sgoingonandstart to form some kind of potential diagnosis in my head when a patient starts to explain their situation I’ve heard about people’s experiences of thisfrompeopleintheirthirdyearof medicine and they’ve said medical school really starts to get exciting when you reach this stage of being able to understand more of what’s going on in the actual hospital environment Generally I’m also looking forward to, over the next few years, getting closer to becoming a junior doctor and working at a hospital; of course that’s something that will constantly be on my mind, especiallyjustbeforeIgraduate.



27
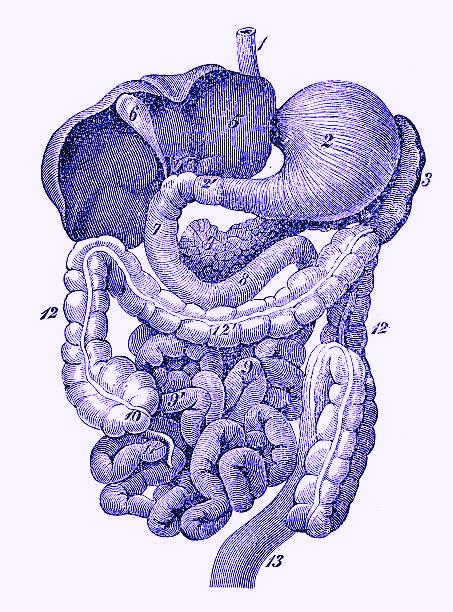
the rise of ultraprocessed food
WRITTEN BY EMMA

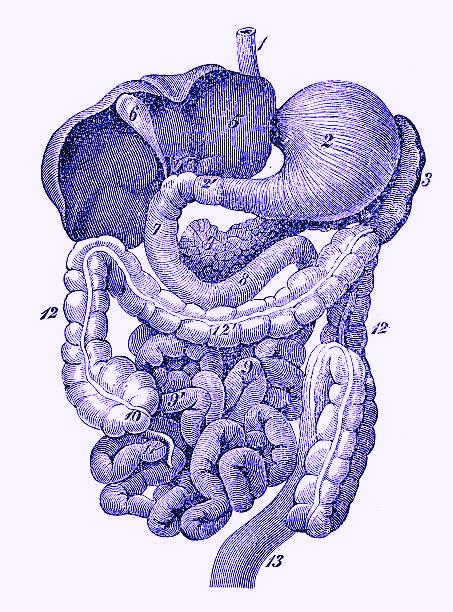
The term ‘ultra-processed food’ comes from the NOVA food classification system, which was created by Carlos Monteiro, Professor of Nutrition and Public Health at the University of Sao Paolo. His research into processed food had been prompted by the rising rate of type 2 diabetes and obesity in Brazil. This research conducted alongside his colleagues showed that although the direct purchase of sugar was decreasing, the consumption of sugaranddietaryfatwasincreasingduetolargerquantitiesbeingcontained inindustrialproducts.
This NOVA system has four categories for food, based on the level of processing. Group 1 is unprocessed or minimally processed food, Group 2 is processed culinary ingredients, Group 3 is processed food and Group 4 is ultra-processed food. Ultra-processed food includes sugar-sweetened beverages, reconstituted meat products, pre-prepared frozen dishes and packaged snacks, and is defined as formulations made from a series of processes, including extraction and chemical modification, containing very littleintactGroup1foods.
In some developed countries, such as the United Kingdom and United States, ultra-processed foods account for more than half of all calories consumed. These products are highly appealing due to their affordability, strong flavourings and high profit for producers. The food is cleverly marketedwithbrightcolours,appealingtochildren. Marketingtechniquesareusedtomaketheseultraprocessedfoodslooktempting;onetechniqueused by cereal companies is to have their cereal mascots looking down, to form eye contact with children. Researchers at Cornell found that characters on children's cereal boxes look down at an average of 9.6 degrees. Ultra-processed food also has a sense of continuity around the world as recognizable products can be found in supermarketsanywhere.
28
Highly processed foods lose many of the nutrients that were present in the original ingredients, as they go through several industrialised processes. Multiple studies have linked the consumption of these ultra-processed foods with the development of a variety of metabolic diseases; this includes asthma, depression,obesityandcardiovasculardisease.
The overconsumption of ultra-processed food is common, and this excessive calorie intake has resulted in an increasing problem of obesity. Obesity increases the risk of high blood pressure, high cholesterol levels, and atherosclerosis. The British Heart Foundation states that heart and circulatory diseases associated with excess weight or obesity total around 31,000 deaths peryear.AstudypresentedattheEuropeanSocietyofCardiologyCongressin August 2023 tracked 10,000 Australian women over 15 years. The diets with the highest proportion of ultra-processed food in their diet were 39% more likelytodevelophighbloodpressurethanthosewiththelowest.
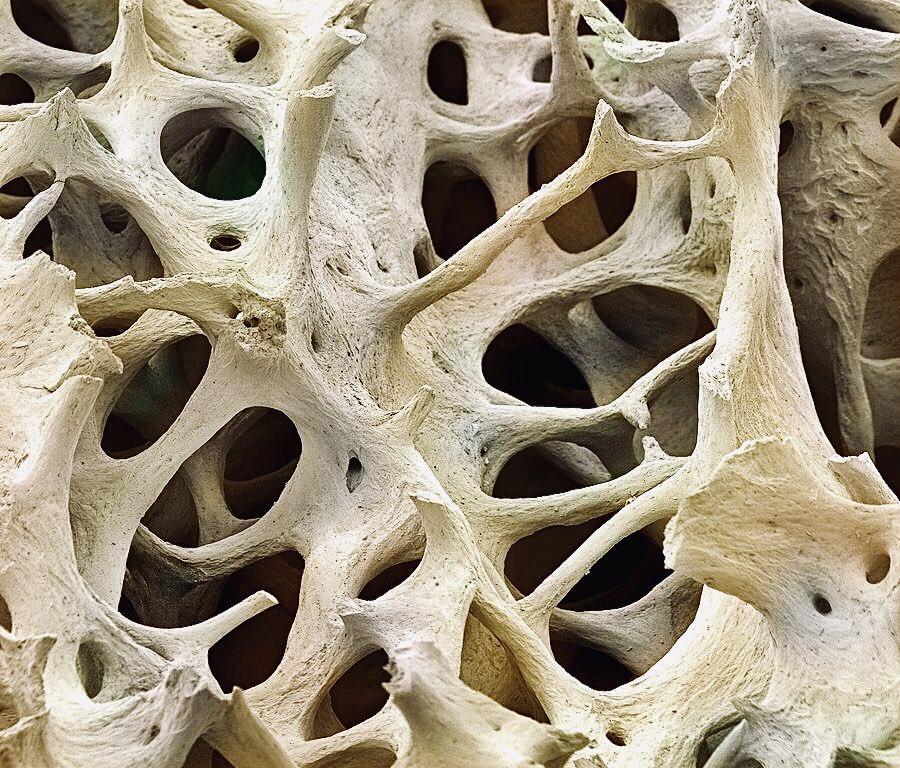
The excess weight gained as a result of obesity puts more pressure on the musculoskeletal and respiratory system; this can cause joint pain, osteoarthritis, asthma, sleep apnea and obesity hypoventilation syndrome.
Obesityalsoincreasestheriskofhormone-relatedproblemssuchaspolycystic ovary syndrome, infertility, and cancers including breast and prostate cancer. The risk of fatty liver disease is also higher, which is an excessive fat deposit in the liver, sometimes leading to serious liver damage, known as liver cirrhosis, which is scarring of the liver which prevents the liver functioning properly and can lead to liver failure and life-threatening complications. The NHSstatesthatobesityreduceslifeexpectancyby3to10yearsdependingon severity.
Ultra-processed food is also destructive in its devastating effects on the environment. Food production overall contributes to one third of the world’s total greenhouse gas emissions, and 75% of these are made by food processing and transportation, waste disposal, and commercial agricultural practices.
Overall,thetrendinincreasedconsumptionofultra-processedfoodposesrisks to human health and the environment. It is essential that we improve availability of low-processed and fresh food to everyone at a fair price, to tackle the growing problems associated with the consumption of ultraprocessedfood.
29
work experience reflection: Brainshuntsurgeryforthe treatmentofhydrocephalus
WRITTEN BY HAJIRA
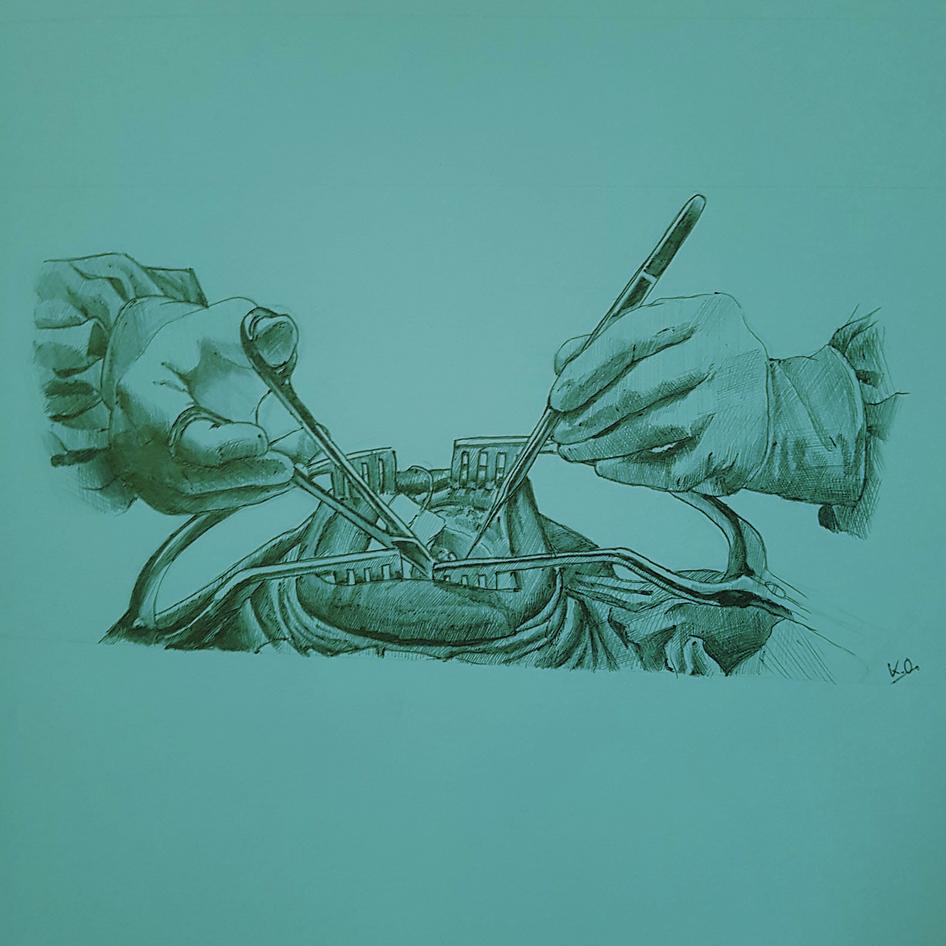
OBSERVATION OF A BRAIN SHUNT SURGERY
AT A HOSPITAL IN ANKARA, TURKEY FOR A PATIENT SUFFERING FROM ACQUIRED HYDROCEPHALUS
14TH JULY 2023
I observed the neurosurgeon’s consultation with the patient, who was a 76 yearold man, at a hospital in Ankara, Turkey. I was fortunate enough to be with a very experienced senior neurosurgeon who spoke English, and to have a translator from the hospital be present during the consultation to fill me in on what the patient was saying in Turkish without the doctor himself having to say everything back to me translated. Looking back, the language barrier, I imagine, would have made the interaction rather awkward and the overall experience not nearly as insightful or valuable
As the patient walked into the room, the doctor told me to observe his movements and explained that the patient had issues with his coordination and memory, and that he had suffered many severe headaches over the last few years. Indeed, I could tell the patient was having physical difficulties as he walked noticeably slowly and had to hold onto furniture and other things in the room to stabilise himself The neurosurgeon then told me that these symptoms had previously not raised concerns about a potential neurological issue, and so the patient had unfortunately been misdiagnosed with Alzheimer’s a few years prior, at a different hospital in the city
However, to the patient’s relief I would imagine, the neurological department were able to get to the root of the patient’s issue, discovering a case of acquired hydrocephalus having conducted an MRI.



30
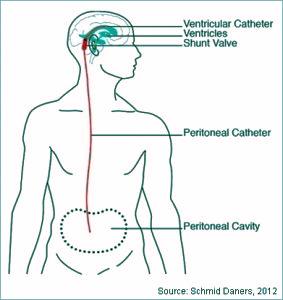
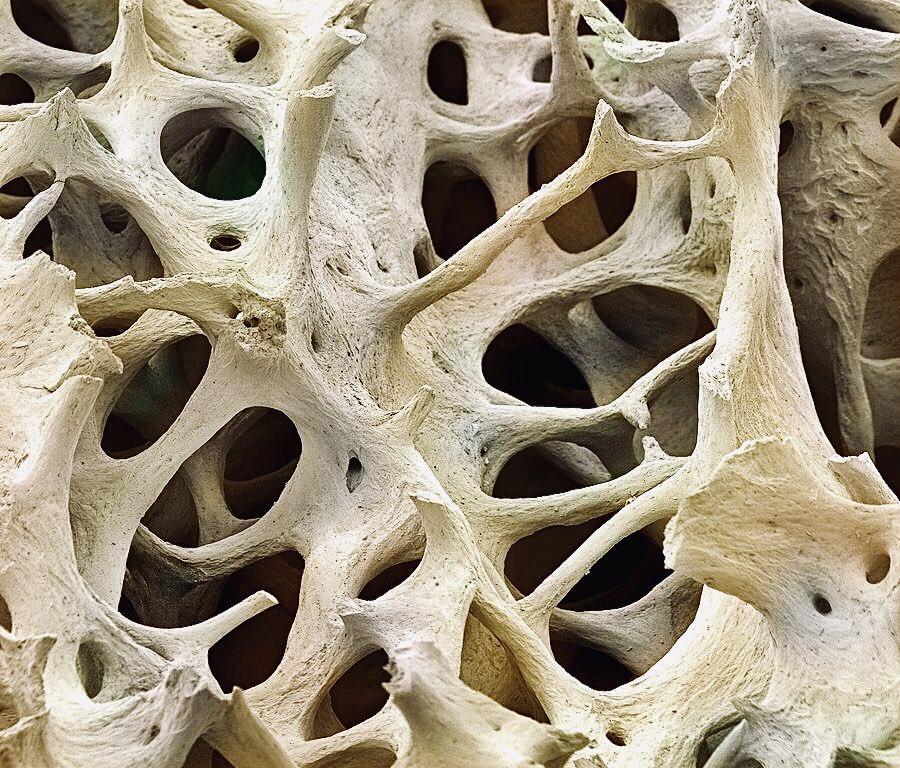
Hydrocephalus is a neurological condition in which excess cerebrospinal fluid (CSF)accumulatesinthebrain-thisfluidcausespressuretobeexertedonthe brain, which can damage it over time and can result in the symptoms that I mentioned this particular patient was experiencing, as well as blurred vision and sometimes epileptic-like symptoms. Typically, cases of hydrocephalus are found in younger individuals, with some babies being born with the conditionthis results in an enlarged head and developmental issues However, in the case of acquired hydrocephalus in particular, the condition usually develops in older children or adults, primarily as a result of the formation of blood clots (which is what occurred to the patient I was with) or infections of the nervous systemsuchasmeningitis



The neurosurgeon introduced me to the patient and his wife and I smiled politely,nothavingacluewhathejustsaidaboutme(itwasallnicethings,I’m sure) However, what I was able to decipher was that he told the patient that I’m British-Pakistani. I found out more about the patient’s life (thanks to the wonderfultranslator),andwasintriguedtohearthathehadbeenaprofessorin Turkish literature for a very long time until his health had sadly begun to deteriorate.Asthepatientnostalgicallyexpressedvariousanecdotesabouthis interests in historical literature, he turned to the neurosurgeon unexpectedly and asked him to ask me if I’d heard of a figure who connected Turkish and Pakistani history (I had not) The patient seemed jokingly disappointed in my evident lack of education about the history of my motherland and it lightened the mood a bit. It was lovely that he was interested in my perspective as well andquiteafewlaughsweresharedduringthatconsultation
The surgeon gave the patient and his wife an outline of what was going to happen in the operating theatre and how it was going to help mitigate the patient’ssymptoms
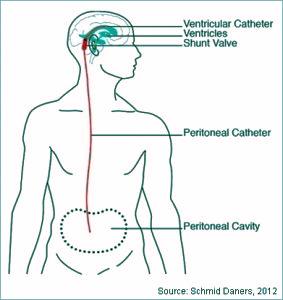
31
Essentially,itwouldinvolvetheinsertionofavalveintotheaffectedfluid-filled ventricle in the brain, connected to a ventriculo-peritoneal shunt (basically a long, thin tube - ‘ventriculo’ refers to the brain’s ventricle that is affected and ‘peritoneal’referstotheabdomen)alongtheneck,undertheskin,downtothe abdomen,wheretheendoftheshuntisfitted.Thissystemissetuptodrainthe excess cerebrospinal fluid so it can be transported from the brain down to the abdomen and absorbed into the bloodstream to eventually be filtered out. This wouldideallyenablethepatienttogainmorecontroloverhiscoordinationand mobility,asthefluid-filledventriclewouldputlesspressureonthebrainhaving beendrained.
21ST JULY 2023
Aweekaftertheconsultation withthepatient,Iarrivedat thehospitalat9:00AM.I hadnotreallyprocessedthe prospectofwatchingthis surgerybeingperformed, anditwasonlywhenIgotto thechangingroomstobe ‘suitedup’didnervesbegin tofillmeslightly.


Would I flinch at seeing pools of blood spew out as a result of the scalpel slicing into the patient’s head? Would I feel nauseous seeing the shunt being inserted into the abdomen? Or would there, perhaps, be a need to actively ‘numb’ myself to the whole situation? These concerns had arisen with me having been informed in more detail about the nature of the procedure by the neurosurgeon.HehadaskedmeifthiswasgoingtobethefirsttimeIwouldbe in an operating theatre, and I had feebly responded ‘yes’, quickly becoming worried that the evident lack of confidence in my response would make him concernedthatIwouldnotbeabletowithstandobservingtheprocedurefortwo andahalfhours,withoutbeingabletositdownonce.However,becauseofhis light-hearted demeanour, and through remembering the lively moments during the patient consultation, I was made to feel more at ease about the whole situation - after all, I would not be the one performing the surgery, and with suchaseniordoctorperformingarelativelylow-riskoperationIknewtherewas nomajorreasontogetworried.Equally,Ifeltexcitedabouthavingtherareand lucky opportunity to watch something like this. I put on a pair of clean scrubs thenursegaveme,aswellassurgeon’sclogsandasurgicalcapandheadedto theoperatingarea.
32

The maintenance of hygiene is, as you would imagine, an incredibly, if not the mostparamountaspectofsurgery.Everysurface,pieceofclothingandsurgical instrument must be kept as strictly sterilised as possible to prevent spreading infections to the patient. The first step, then, was to learn how to wash my hands properly for an operation - as I soon naively discovered, it was not the typical ‘sing happy birthday in your head whilst interlacing the fingers and scrubbing the nails, hang on, don’t forget to rotate around the thumbs’ kind-of jazz.Instead,Iwashandedasmallplasticpacketvisiblybrimmingwithabrown liquid by the surgeon - probably noticing a sense of concern growing on my face, he told me it was povidone iodine solution, an antiseptic. What was contained inside the packet was no soap bar - it was a sponge filled with the povidone solution and a soapy substance that foamed, with silicone bristles attached underneath to scrub the handsand armsall the wayuntil the elbows. When demonstrating the perfect handwashing technique, the surgeon emphasised that it is important to keep your arms slanted downwards towards the sink to remove water rather than move them up horizontally as normal and have it dripping further up your arms with potential germs that you’ve just washedoffyourhands.Icanconfidentlysaythatmyhandswillneverfeelmore cleanthanafterwashingthembeforethatsurgery.


Weenteredtheoperatingtheatre,wherethepatientwaslyingontheoperating table having been administered a general anaesthetic, and was covered in a large surgical cloth, with everywhere except the side of his head being concealed. Nurses and the other surgeon who were to be involved in the operationpacedthroughouttheroom,gettingthesharpsurgicaltoolssterilised and ready in trays lined with sanitised cotton cloths. The first step before operatingwastosterilisetheskinonthepatient’sheadforthefirststageofthe process(insertingthevalveandshuntintothebrain)soImovedbacktoletthe nurses do their thing. His head was cleaned thoroughly with povidone iodine andthenwithisopropylalcohol(anotherkindofantiseptic).Afterthiswasdone, oneofthenursescameinholdingatraywith…apairofbarberclippers?Ifelt slightly confused at first, but then quickly realised that I had been somewhat imprudentlyenvisioninganincisiontobemadedirectlyontothescalp,withthe hairstillbeingpresent,andthatthiswouldreallyhavebeenquiteanunfeasible situation. The patient’s hair was shaved on the side of his head and the area thencleanedoncemore.Theoperationwasnowreadytobegin.
33
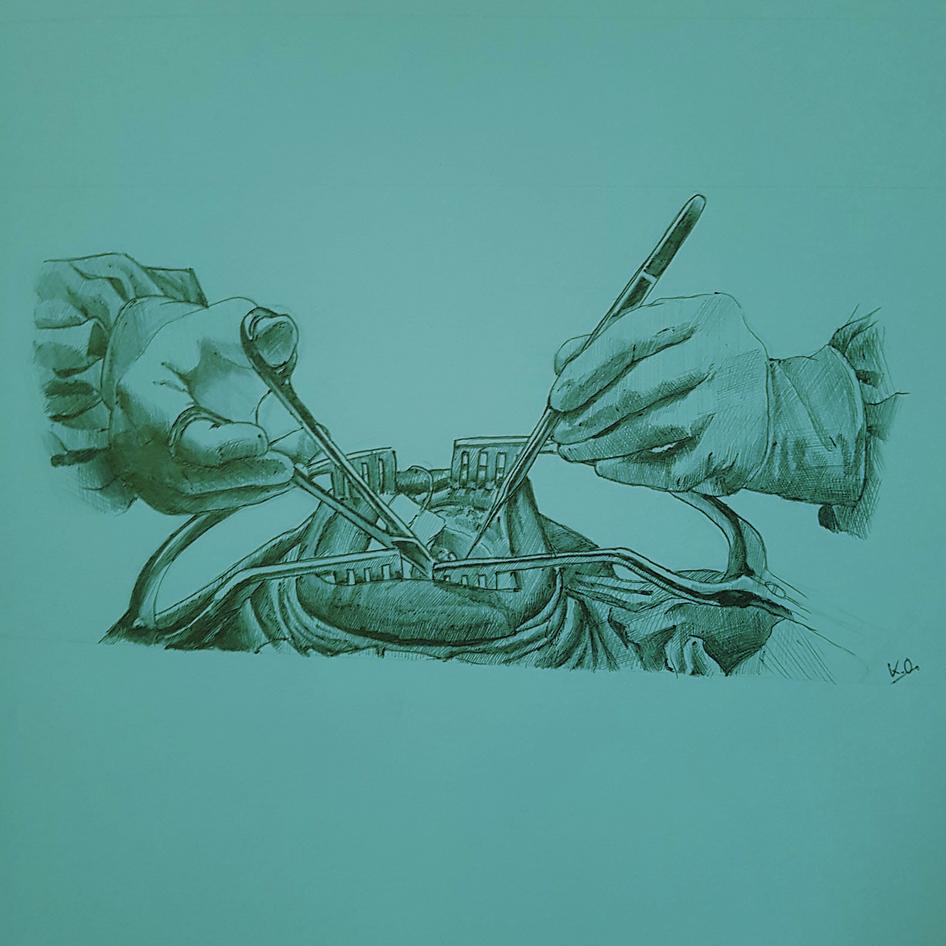
The overhead lights were switched off and the surgical lightheads above the patient switched on, swampingeveryoneinawaveofdimnessallabout the room, to spotlight the patient in the operating area. The neurosurgeon began by using a scalpel to make a curve-shaped incision into the head. This resulted in a flap of skin with a small area of the patient’s skull underneath becoming slightly visible Surprisingly, I did not, in fact, flinch or become overwhelmed with nerves upon seeing the sheervolumeofbloodthatwasgushingout Itwas probably the fact that the patient’s face and entire rest of his body were covered with the surgical drape, and so I was not necessarily thinking about him as a person in the moment - of course, this sounds rather dehumanising, but even from the perspective of someone who was simply observing the procedure being performed, I was incredibly focussed and my eyes rarely left the surgeon’s glovesashedelicatelyslicedintotheskin.Aswell as this, with the patient being under anaesthetic, ofcourse,Ididnotbecomeanxiousaboutanypain he could be feeling. With every stroke while making the incision, the surgeon pressed the area with sponges around the curve in a tender manner thatcomfortedme Withafewmoretoolsthesmall areaofvisiblecraniumwasenlargedslightly.


Thisallowedthesurgeontothenuseasurgicaldrilltocarefullycreateasmall hole (known as a Burr hole) into the cranium, being directed by the other surgeonastowheretoplaceit.
Oncethishollowareawascreated,theareaoffocusofthebrain(theenlarged, fluid-filled ventricle) was now visible With the use of an endoscope, with its camera’s vision being projected onto a large screen that was positioned right behindthetable,aventricularcatheterandvalvewerefittedontothebrainand then pushed down into the patient's neck under the skin. It was then that the slightlymorecomplextaskneededtobedone,whichwastoconnecttheshunt itself to the catheter It was cut to the marked, pre-determined, appropriate length by a nurse and then threaded through, with a considerable amount of force,tobeconnected
34
Theseniorneurosurgeonstruggledabitwithfullyinsertingtheshuntalongside theinsideoftheneckandfittingitintothecatheter.However,after voicingthe difficulties he was facing, the assistant surgeon intervened and took over the surgery for around 20 minutes, using silk tie (essentially, small silk threads used in surgery) to secure the catheter to the tube, aiding the senior neurosurgeon.Throughthis,theeffectivecommunicationbetweenthesurgeons andnursesintheoperatingtheatrewasevidenttomeintheirinteractionswith each other (despite me not being able to understand what was being said), leadingtothetubebeinginsertedsuccessfully.Itwasalsovaluabletoobserve that even the most skilled surgeons can face difficulties with managing certain aspectsofanoperationandthateveryonehascertaincompetencieswhichare stronger than others, even in the environment of the operation theatre. Now thatthetubewaspartiallytunnelledundertheskinalongtheribs,preparations forthesecondstageoftheoperationbegan.


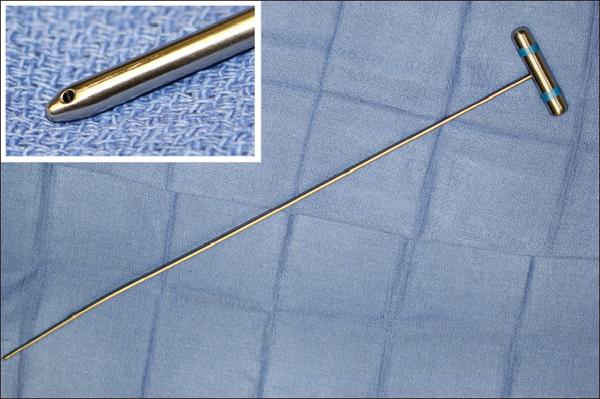

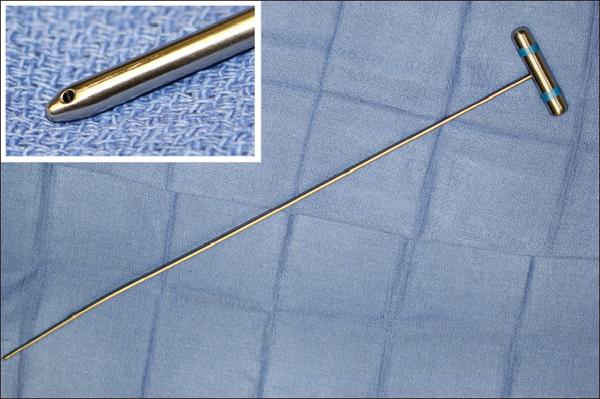
Withthecatheterhavingbeenplacedintotheventricle,theareawascleansed toremoveanybloodstains,readytocloseupthelaceration.Thetwosurgeons cooperatively fixed up the curved incision with one using forceps to hold the two parts of the skin close together, whilst the other employed the use of the surgical stapler to insert staples to bring the skin together. Staples were used in particular as they are generally faster to insert into the scalp and produce similar cosmetic results (whilst having a similar healing time) in comparison to stitches.Theareawaswipedandapatchplacedoverit.Thelargeclothwhich had been concealing the abdomen was now shifted to allow the surgeons to begin making small incisions into the side of the patient to access the peritoneal cavity. A shunt passer (a long, thin metal rod to help move shunts intoplace)wasslowlyinsertedintotheincision,andtheendofthetube,which tunnelled underneath the patient’s skin, was brought to the abdomen. A valve was placed into a pocket in the abdomen and secured to the shunt tube using silktie.Withtheuseoftheendoscope,theseniorsurgeonmovedaroundtothe end of the operating table where the patient’s head was, whilst his colleague gentlypressedontheareawiththevalve.
35
On the screen projecting the endoscope’s camera view, I could see a liquid movingdownthetubefromtheendconnectedtotheventricleofthebrain.This was the cerebrospinal fluid being drained from the head to the end to the incision in the peritoneal cavity. Having now ensured that the drainage system was working properly with the shunt having been fully installed, the surgeons diligently threaded stitches into the abdomen to close up the laceration The nursesappliedantisepticstogauze,cleanedthestitchesandtheareasaround themthoroughly,andfinallycoveredthemwithapatchtoletthemheal



U s not able to meet the patient in person following his operation,howeveramonthafteritoccuredIwasinformedbytheneurosurgeon that I worked with that the patient had recovered well (having had his head staplesremovedoncetheskinhealed)andhisphysicalstabilityhadmassively improved Although I had expected (and hoped) for this outcome, it was nonethelessrelievingandIwasverypleasedtohearthathisqualityoflifehad beenchangedinquiteasignificantwayforthebetter,especiallysinceIgotto witnessitfirsthand.Overall,themostsubstantialthingsthatIlearnedfromthis remarkableexperienceincludedthatmaintainingapositiveattitudeandforming good patient rapport is essential and that communication and making the best useoutofyourskillsetarekeytodevelopingastrongsenseofcooperation.I hadadmiredthesurgeons’abilitytoremaincomposedandmakeeverystagea very involved process for everyone in the theatre so that they could refer and direct each other to ultimately ensure the best outcome for the patient I had also admired the surgeons’ ability to stand for such long periods of time (my back had essentially given up around ¾ of the way into the procedure and, noticing my discomfort, a lovely nurse brought me a chair - it was slightly embarrassing, but I was able to focus more on the operation and, more importantly,allowthe surgeons tofocusmoreontheoperation)

36
Inallseriousnessthough,Iamreallyindebtedtotheseniorneurosurgeon,who allowedmetogainaccesstothebehind-the-scenesofsomethingthatnotvery manypeopleareableto Iwillalwaysfeelgratefulforhispatienceinanswering my endless myriad of questions and for informing me about all of the medical terminologytodowiththeprocedurethatImentionedwhilstwritingthis

Toconclude,workexperienceinanoperatingtheatreisquitedifferenttowardround work experience, expectedly - the focuses are, of course, rather dissimilar With ward rounds you gain a lot more insight into the way that doctors and nurses interact with patients and determine what tests need to be done tomakediagnoses-withoperations,ontheotherhand,yougainabetter understandingofthephysicalmedicalinterventionsthatareemployedtoacton thosediagnosesaswellasrecognisethelevelofskill,(bothmotorandmental) needed to perform a surgery effectively and successfully from start to finish Anysortofworkexperienceisabsolutelyinvaluablethough,anditisimportant toremembertoactivelyreflectonhowitimpactedyourperceptionofworkingin thatcertainmedicalfield.Trytofocusonhowyouplanonusinganyinspiration that you gain from a work experience placement in a healthcare sector to facilitate your medical aspirations, and above all, cherish the wonderful memoriesyouwillmakeduringit.



37
Medical Book reviews
WHEN BREATH BECOMES AIR - PAUL KALANITHI
REVIEW BY Y12 STUDENT ANGELA
Thisisaninspirationalmedicalmemoirabout a resident neurosurgeon’s reflection on his journey through lung cancer. This book has truly captured the highs and lows of dealing with the disease, displaying how it changed his thoughts and feelings on the purpose of lifeanddeathleadingtoachangeintheway hechosetospendthefinalyearsofhislife.I recommend everyone to read this book, as eventhoughitisamedicinebasedmemoir,it teaches the importance of doing the most thatyoucanwiththelifeyouhave.Itshowed his adjustment to understanding and acceptinghiscircumstances,withhimstating ‘I hadn’t expected the prospect of facing my own mortality to be so disorienting, so dislocating’.

Throughout the novel, I found his insight to be really valuable in understanding what a doctor’s purpose is, which I think is especially seen through this quote : ‘The physician’s duty is not to stave off death or return patients to their old lives, but to take into our arms a patient and family whose lives have disintegrated and work until they can stand back up and face, and make sense of, their own existence.’
THE MAN WHO MISTOOK HIS WIFE FOR A HAT - OLIVER SACKS
REVIEW BY
EMMA
This book is a brilliant collection of 24 short stories about different patients with neurological disorders Although it is outdated, having been published in 1985, the stories told are just as useful for today. The narrative style delivers the stories amusingly, but deals with heart-breaking cases. The cases vary from agnosia to autism to Tourette’s syndrome to amnesia Dr Sacks provides detailed scientific and clinical information alongside the stories, which allows the reader to start to learn some of the terminology used in this specialty
38
acknowledgements
many thanks to:
Y12 STUDENT CASS FOR THEIR WONDERFUL DRAWING FOR THE COVER
DR AYE, DR CHAUDHURY, MARYAM AND DR KITT FOR THEIR TIME AND INSIGHTFUL ANSWERS TO OUR Q&A’S
BEATRIX FOR HER INTRUIGING ARTICLE
THE NEUROSURGEON THAT HAJIRA WORKED WITH, THE PATIENT WHO THE SURGERY WAS FOR, THE TRANSLATOR AND HAJIRA’S MEMORY
ANGELA FOR HER GREAT BOOK REVIEW
OUR PRECEDING CO-EDITORS, Y13 STUDENTS FRANCESCA, JESSICA, ANJALI AND AHYOUNG FOR GIVING US THE PRIVILEGE OF TAKING OVER THE MAGAZINE
MRS M RHODES FOR PUBLISHING OUR MAGAZINE
MISS STEER FOR PROVIDING GUIDANCE WITH PUBLISHING THE MAGAZINE
FORMER OHS STUDENTS SHREYA AND GABBY WHO CREATED THE MEDICAL MYRIAD IN THE FIRST PLACE, IN 2020!

39
references:
What are induced pluripotent stem cells?
https://doi.org/10.2174/15734031380507 6278
https://www.britannica.com/science/in duced-pluripotent-stem-cell
https://www.genome.gov/geneticsglossary/Fibroblast#:~:text=A%20fibrob last%20is%20a%20type
https://doi.org/10.3389/fcell.2022.10508 56
https://www.ncbi.nlm.nih.gov/pmc/arti cles/PMC1186965/#:~:text=A%20retrovir al%20vector%20consists%20of
https://doi.org/10.3389/fcell.2015.00002
https://doi.org/10.3389/fcell.2015.00002
MusicTherapyTreatmentfor Alzheimer’sDisease
https://www.nia.nih.gov/health/alzhei mers-causes-and-risk-factors/whathappens-brain-alzheimers-disease
https://www.ncbi.nlm.nih.gov/pmc/arti cles/PMC7248378/
https://www.england.nhs.uk/blog/musi c-and-dementia-a-powerfulconnector/
https://alzres.biomedcentral.com/artic les/10.1186/s13195-023-01214-9
https://www.nm.org/healthbeat/health y-tips/emotional-health/music-asmedicine-alzheimers-
dementia#:~:text=Music%20evokes%2 0emotions%20and%20memories,impr ove%20communication%20and%20car egiver%20relationships.
https://www.sciencedaily.com/releases /2018/04/180428145111.htm
TheRiseofUltra-Processed Food
https://www.nhs.uk/conditions/ obesity/#:~:text=Obesity%20red uces%20life%20expectancy%20 by,on%20how%20severe%20it% 20is
https://regulatory.mxns.com/en/ ultra-processed-foods-novaclassification
https://www.bmj.com/content/3 84/bmj-2023-077310
https://news.cornell.edu/stories /2014/04/food-psychologistseyeball-cereal-characters
https://www.nature.com/article s/s43016-021-00225-9.epdf?
https://www.bhf.org.uk/informa tionsupport/heart-mattersmagazine/news/behind-theheadlines/ultra-processedfoods#definition
https://www.nhs.uk/conditions/ osteoarthritis/

40