1 Evidence and Key Information for Ontario Harm Reduction Programs Ontario Harm Reduction Distribution Program
Response Drug Test Strips Fentanyl | Benzodiazepine | Xylazine
Rapid
2 contents Introduction and Context Setting ........................................................................................................................ 4 Fentanyl Drug Test Strips (FTS) .................................................................................................................................. 6 Evidence ......................................................................................................................................................................... 7 Effectiveness Of Fentanyl Test Strips 11 Limitations Of Using Fentanyl Test Strips as A Drug Checking Tool ................................................... 13 Drug Checking Process Using Fentanyl Test Strips .................................................................................... 15 Procedure For Drug Checking with Fentanyl Test Strips .......................................................................... 16 Interpreting Results 17 Benzodiazepine Drug Test Strips (BTS) ................................................................................................................ 19 Evidence ...................................................................................................................................................................... 20 Advantages Of Benzodiazepine Test Strips ................................................................................................... 22 Limitations Of Benzodiazepines Test Strips as a Drug Checking Tool 23 Drug Checking Process Using Benzodiazepine Test Strips ..................................................................... 25 Procedure For Drug Checking with Benzodiazepine Test Strips ........................................................... 26 Interpreting Results ................................................................................................................................................ 27 Xylazine Drug Test Strips (XTS) 29 Evidence 30 Advantages Of Xylazine Test Strips .................................................................................................................. 32 Limitations Of Using Xylazine Test Strips as a Drug Checking Tool..................................................... 33 Drug Checking Process Using Xylazine Test Strips 33 Procedure For Completing Drug Checking Using Xylazine Test Strips 34 Interpreting Results ................................................................................................................................................ 35 Practical Considerations for Programs ................................................................................................................. 37 Ordering Process 37 Storage And Handling` 38 Kit Configuration...................................................................................................................................................... 39 Disposal ....................................................................................................................................................................... 39
3 Recommendations For Training ......................................................................................................................... 40 Safety Planning ......................................................................................................................................................... 40 FAQs .................................................................................................................................................................................. 42 Useful Links and Further Reading 43 References....................................................................................................................................................................... 44 Appendix ......................................................................................................................................................................... 49 OHRDP Order Form ................................................................................................................................................ 49 Information and Evidence from the Toronto Drug Checking Network 50 Safety Data Sheets .................................................................................................................................................. 53
Introduction and Context Setting
The goal of this document is to provide harm reduction programs with the evidence and information needed to understand and distribute BTNX Rapid Response™ test strips. The materials to make drug test kits are made available through OHRDP to help communities in responding to the toxic drug crisis. These materials are available for a limited time.
Offering drug test strips encourages individuals who use drugs to be more informed about the drugs they are using. In many cases drug test strips lead to behaviour change and adoption of other harm reduction measures. Drug test strips can also provide opportunity for increased engagement between service-users and harm reduction staff.
The field of drug checking is ever evolving, as is the language around drug checking and drug testing. Going forward in this document, drug checking is considered the over-arching language for both rapid response test strips and advanced drug checking technologies, like Fournier transform infrared spectrometer (FTIR), Gas Chromatography-Mass Spectrometry (GC-MS) and Liquid Chromatography-Mass Spectrometry (LC-MS). Drug test strips, while useful for quick and preliminary testing, have limitations that can be addressed by these more advanced technologies.
There are numerous reasons why combining drug test strips with more advanced drug checking technologies is beneficial:
Increased Accuracy and Specificity: Drug test strips are often limited in their ability to detect a wide range of substances and may not be able to distinguish between closely related compounds. Advanced technologies such as Gas Chromatography-Mass Spectrometry (GC-MS) and Liquid Chromatography-Mass Spectrometry (LC-MS) offer a much higher level of specificity and can accurately identify and quantify a wide array of substances within a sample.
Identification of Novel Substances: The drug market is continuously evolving, with new synthetic drugs and novel psychoactive substances (NPS) emerging regularly. Many of these substances may not be detected by standard drug test strips. Advanced drug checking technologies can identify these novel compounds, providing crucial information for harm reduction and public health responses.
Quantitative Analysis: Drug test strips can typically only provide a qualitative result (presence or absence of a substance). In contrast, advanced techniques can quantify the amount of a substance, which is critical information for understanding potential toxicity and overdose risk.
4
Public Health Monitoring and Research: Advanced drug checking technologies contribute to a better understanding of drug market trends and the emergence of dangerous adulterants. This data is invaluable for public health monitoring, research, and informing policy decisions.
Adulterant Detection: While some drug test strips are designed to detect specific substances, like fentanyl, benzodiazepine, and xylazine they may not detect other harmful substances that can be present. Advanced technologies can screen for a wide range of potential adulterants, some of which may be unexpected or new to the market.
Building Credibility: The use of advanced technologies can enhance the credibility of drug checking services among users, public health officials, and policymakers. Demonstrating a commitment to accuracy and comprehensive analysis can encourage more individuals to utilize these services, thereby increasing their harm reduction impact.
Engagement and Building Trust: Drug test strips are an engagement tool like other harm reduction supplies. The importance of harm reduction staff engaging with service-users around drug test strips ensures individuals understand the strip limitations and how to interpret the results. This allows individuals to make better informed decisions about their consumption. It also opens the door to talking about drug checking services and advanced drug checking technologies.
Coupling drug test strips with advanced drug checking technologies creates a more robust, accurate, and comprehensive approach to drug checking. This combination maximizes harm reduction potential, enhances public health monitoring, and ensures that drug checking services can keep pace with the evolving nature of substance use. Drug checking services empower service-users to advocate for themselves, educate their peers, and help develop solutions that impact them.
5
Fentanyl Drug Test Strips (FTS)
Summary
● Fentanyl Drug Test Strips have low detection limit, high sensitivity, and specificity for fentanyl and some fentanyl analogues
● Test results should be interpreted with caution
● High concentrations of diphenhydramine, methamphetamine, and MDMA could potentially affect test results and lead to false positives when using FTS.
● People who use drugs and harm reduction program staff should have adequate knowledge of the test strip technology, and on how to read and interpret the result
● People who use drugs and harm reduction program staff should be aware of the limitations of FTS
● Coupling drug test strips with advanced methods like FTIR and mass spectrometry is crucial for enhancing the accuracy, specificity, and comprehensiveness of substance analysis in harm reduction efforts.
● FTS should be combined with overdose prevention strategies and naloxone distribution
● As an easy-to-use drug checking tool, FTS are well accepted among people who use drugs
● Using FTS as a drug checking tool allows individuals to make informed choices about their substance use, modify their behaviours and potentially reduce the risk of overdose
● Additional benefits of programs providing FTS include:
Direct engagement
Prevention and education
Service-user empowerment
Integration of services
Wider reach
Programs who will have staff directly assisting with drug checking need to have drug checking exemptions. For more information please see below: https://www.canada.ca/en/healthcanada/services/health-concerns/controlled-substances-precursor-chemicals/exemptions.html
It is very important that harm reduction staff engage with service-users about drug test limitations. Ensure service-users understand the recommended steps to help reduce their risk of drug poisoning regardless of a negative result.
6
Evidence
Background
Accidental drug overdoses have rapidly become a major public health crisis in Canada. The main driver of the opioid overdose epidemic is the replacement of diverted or illegally manufactured pharmaceutical pills and heroin with extremely potent synthetic opioids. They primarily present in the forms of fentanyl and its analogues (e.g. carfentanil, furanylfentanyl, acetylfentanyl) (Belzak & Halverson, 2018). Fentanyl, a synthetic opioid 50-100 times more potent than morphine, is identified as the leading opioid responsible for fatal overdose deaths in Canada (Belzak & Halverson, 2018). Fentanyl and its associated analogues (including carfentanil, furanyl fentanyl, and acetyl fentanyl) have been found mixed with heroin and cocaine and pressed into counterfeit prescription drugs (John Hopkins, 2018).
In the first half of 2023 (from January to June), fentanyl was involved in 84% of accidental opioid-related fatalities, marking a 47% rise since the initiation of nationwide monitoring in 2016, although this rate has shown signs of leveling off in recent years. Furthermore, during the same period in 2023, 80% of accidental opioid toxicity deaths were linked exclusively to nonprescribed opioids, representing a 21% increase since the commencement of national surveillance in 2018, with indications of stabilization in recent years (Special Advisory Committee on the Epidemic of Opioid Overdoses, 2023).
There were 22,828 opioid toxicity deaths registered between January 2016 to March 2021 and 1,772 opioid toxicity deaths occurred between January to March 2021 (approximately 20 deaths per day). During the height of the COVID-19 pandemic, a significant increase in the number of opioid overdose deaths was reported with 6,946 deaths between April 2020 to March 2021 in Canada. That represents an 88% increase from the same time period prior to the pandemic (April 2019 to March 2020 – 3,691 deaths) (Special Advisory Committee on the Epidemic of Opioid Overdoses, 2021).
Drug Checking – Fentanyl Test Strips
In response to the opioid overdose crisis, many harm reduction programs have incorporated some form of on-site and/or off-site “drug checking” intervention into their services. During a "drug checking" process, unregulated drugs or illegally acquired prescription pills are analyzed to determine their composition or if they are adulterated. The distribution and use of fentanyl test strips (FTS) is one method used for drug checking. Integrating drug test strips with sophisticated techniques like FTIR and mass spectrometry is essential to improve the precision, detail, and overall effectiveness of substance identification in promoting safer drug use and reducing the risk of overdose. FTS represent an emerging harm reduction intervention that helps to prevent unintentional fentanyl exposure and reduce the risk of accidental opioid overdose (Goldman et al, 2019).
7
What Are Fentanyl Test Strips?
FTS are disposable, single-use tests that can detect the presence of fentanyl or its analogues in a substance. Although, most commonly FTS are used to test the drugs for the presence of fentanyl and its analogues, FTS can also be used to check equipment or baggie residue. There are
different types of fentanyl test strips. The best FTS are those that show high sensitivity in detecting traces of fentanyl and its analogues with lowest percentage of false negative and false positive results. For example, Interior Health in British Columbia uses BTNX™ test strips, because they are tested by Johns Hopkins Bloomberg School of Public Health and show high sensitivity to fentanyl and its analogues.
The BTNX™ Rapid Response Fentanyl Test Strip is a lateral flow chromatographic immunoassay for the qualitative detection of fentanyl/nor fentanyl in urine at the cut-off concentration of 20 ng/ml. Interpretation of test results are: positive: one line, negative: two lines, invalid: no lines or no control line. It is specific for fentanyl screening with no significant cross reactivity to other opiates, such as morphine and heroin. The Rapid Response™ Fentanyl (FYL) Test is able to detect fentanyl and many other fentanyl analogues such as carfentanil, acetyl fentanyl, butyryl fentanyl, remifentanil, ocfentanil, sufentanil, p-fluoro fentanyl, furanyl fentanyl, valeryl fentanyl, and 3methyl fentanyl (BTNX website, www.btnx.com). However, FTS cannot detect all types of fentanyl analogues, or carfentanil in very small amounts.
Evidence Review of the Effectiveness of Using Fentanyl Test Strips
Numerous studies demonstrated the utility of FTS as a cheap, fast, and easy-to-use drug checking tool with high sensitivity to detect fentanyl and some of its analogues in street drugs (Green, 2020; John Hopkins, 2018; Skov-Skov Bergh et al, 2021; Marshall K, 2018). And most studies recognize the importance of coupling drug checking services, including FTS, with other more advanced drug checking technologies (FTIR and mass spectrometry), treatment, harm reduction and overdose prevention strategies.
Currently, there are various brands and types of FTS on the market. Recognizing that there might be differences between various types of FTS in how effective they are in detecting fentanyl and its analogues, Skov-Skov Behr et al. (2021) examined the ability of four commercially available brands of urine fentanyl test strips to identify fentanyl and 28 different fentanyl analogues. The study examined the differences between the following four brands of FTS:
Rapid Response Fentanyl (FYL) Test Strips from BTNX Inc. (Markham, ON, Canada)
Rapid Self-Test (RST) – Fentanyl FYL20 from Rapid Self-Test Inc. (Mississauga, ON, Canada)
8
Nal van Minden Drug-Screen ® FYL 10 from Nal van Minden (Moers, Germany) and
One Step FYL20, Rapid Test Dipstick (Urine) from Hangzhou Alltest Biotech Co., Ltd (Hangzhou, China)
The authors found that all four different urine fentanyl test strips successfully recognized a broad panel of fentanyl analogues. Three of the tests, Rapid Response, Rapid Self-Test and Nal van Minden, gave a positive test result for as many as 19–22 of the 28 fentanyl analogues tested at 1000 ng/mL and 24 analogues at 10 000 ng/mL. A major limitation for all the test strips tested was the low sensitivity for detecting the ultra-potent fentanyl analogue carfentanil, even at potentially life-threatening concentrations.
FTS showed higher sensitivity and specificity when compared to other drug checking tools (Green et al, 2020, John Hopkins; 2018) A study by Green et al (2020) examined the validity of three portable devices in identifying the presence of fentanyl in street-obtained drugs: fentanyl test strips, a hand-held Raman Spectrometer, and a desktop Fourier-Transform Infrared Spectrometer. The findings show that FTS have high sensitivity and specificity and could detect the presence of at least two additional fentanyl analogues alone or in the presence of another drug in liquid, powder, and pill forms. The authors conclude that for public health interventions aiming to detect fentanyl in “real-world” samples, FTS would be the device of choice considering that 9.6% false negative and 3.7% false positive rates, at most, were deemed acceptable. In addition, the study recommends that FTS intervention should be coupled with tailored education and naloxone distribution. The main limitation of the FTS is that they do not indicate any other information on quantity, purity and presence of adulterants or fill, which is why these interventions should be coupled with more advanced drug checking technologies (FTIR and mass spectrometry).
These findings regarding the high sensitivity and low detection limit of FTS are similar to findings from earlier studies (John Hopkins, 2018; Olson et al, 2019). Additionally, the John Hopkins study from 2018 examined the perspectives of people who use drugs on FTS and found that people who participated in the study:
are interested in fentanyl drug checking interventions and
would tend to modify one or more of their drug use behaviours if their drugs tested positive for fentanyl
The accuracy, acceptability, and the impact on behaviour of FTS was demonstrated in a joint study by Vancouver Coastal Health, Interior Health, and the BC Centre for Disease Control, where participants were provided with free take-home drug checking kits, each containing (Sukhpreet et al., 2022) five fentanyl test strips, instructions, and a survey. Results from 994 takehome fentanyl test strips used on opioid samples were compared to checks on opioids conducted at health care and community sites. The study found that:
9
89.95 per cent of opioid samples contained fentanyl for take-home drug checking, 89.14 per cent of samples contained fentanyl at on-site drug checking.
27 per cent of service-users using the take-home kit made a safer choice if their substance tested positive for fentanyl. A safer choice here was referred to as using with a friend, using less of a substance, using more slowly, or taking their substance to an overdose or supervised consumption site for use.
96 per cent of service-users said they would use the take-home checking kit again.
In August 2017 in San Francisco, the DOPE Project partnered with the Syringe Access Collaborative (SAC) (National Harm Reduction Coalition 2020) to pilot a fentanyl test strip monitoring survey in response to the growing number of opioid overdose deaths. The findings from this project, like other studies (Sherman et al, 2018; Sherman et al, 2019; John Hopkins, 2018) suggest that FTS:
are a useful engagement tool to foster discussion with people who use drugs, especially regarding universal precautions and the presence of fentanyl in their drug supply
are easy for people who use drugs (PWUD) to use with minimal instruction
are well accepted among PWUD
are detecting fentanyl and some fentanyl analogues in various drug supplies
allow PWUD to be more informed about the drugs they are buying and using
could lead to behaviour change and adoption of other harm reduction measures
allows providers to better engage with non-injectors and non-opioid users around overdose prevention (e.g., naloxone trainings with non-opioid users)
demonstrate a high likelihood of implementing one or more harm reduction strategies when learning that their drugs are positive for fentanyl
lead to an increased general awareness and understanding of fentanyl among PWUD and harm reduction workers and needle distribution sites
10
Effectiveness Of Fentanyl Test Strips
1. Accurate Drug Detection For fentanyl test strips, the vendor indicates a cut-off concentration of 200 ng/mL on the back of each test strip packet and also in the product insert information. The performance characteristics curves obtained for BTNX Rapid Response (Liquid/Powder) FTS show that when the fentanyl concentration is about 200 ng/mL the chances of observing a false-negative response are about 5%. This result is consistent with the 200 ng/mL cut-off value claimed by BTNX for their Rapid Response (Liquid/Powder) product. This indicates their reliability in detecting fentanyl in illicit substances, which is crucial in preventing harm (Rodriguez et al., 2023). In a study by Klaire, et al, (2022), take-home fentanyl test strips were distributed at ten sites providing drug checking services in British Columbia from April to July 2019. Take-home fentanyl test strips used by PWUD on opioid samples can provide similar results to formal drug checking services and are a viable addition to existing overdose prevention strategies. Test strips should be used to supplement, not replace, more advanced drug checking technologies like FTIR and mass spectrometry to enhance harm reduction efforts and decrease overdose risks. This study demonstrated that for opioid samples, there was concordance of rates of fentanyl detection between samples tested using distributed fentanyl test strips and samples tested on-site by trained individuals. This suggests that PWUD can accurately use fentanyl test strips with minimal training in their chosen location. Specifically, results from take-home drug checking yielded similar results to on-site drug checking conducted by trained staff (Klaire et al, 2022). Although the study lacked sufficient statistical power for a comprehensive comparison, its findings imply a potential variance in reliability between take-home drug checking and on-site drug checking, particularly when examining stimulants. Of note is the lower incidence of fentanyl positivity in stimulant samples tested on-site compared to those analyzed in the take-home setting.
2. Detection of Fentanyl Analogues: The cut-off level is a predetermined concentration set by the manufacturer, and it represents the minimum amount of fentanyl or its analogues that the test strip can reliably detect. If the concentration of fentanyl or its analogues in the sample is below the cut-off level, the test strip may produce a negative result, indicating that fentanyl is not present in significant amounts. If the concentration is at or above the cut-off level, the test strip may produce a positive result, indicating the presence of fentanyl. BTNX FTS are also capable of detecting several fentanyl analogues further highlighting their effectiveness in harm reduction efforts (BTNX, 2023).
3. Reducing Risky Drug Use: FTS are distributed to people who use drugs (PWUD) in various community-based and clinical settings across the country. Based on the study by Klaire et al, (2022), the use of Fentanyl Test Strips was well accepted amongst PWUD both for takehome and on-site use, and the vast majority were interested in using fentanyl test strips in the future. When PWUD receive a positive result from an FTS, some PWUD tend to modify
11
their behaviour to reduce overdose risk. These behavioural changes may include discarding drugs, reducing drug doses, using drugs more cautiously, conducting smaller "tester" shots, consuming drugs in the presence of others, keeping naloxone on hand, and sharing FTS with friends who are at risk of fentanyl exposure (Maghsoudi et al., 2021; Peiper et al., 2019; Goldman et al., 2019; Krieger et al., 2018; Weicker et al., 2020; Park et al. 2021; Reed et al., 2021; Goodman-Meza et al., 2022). Importantly, there is no empirical evidence suggesting that FTS use leads to increased drug consumption among PWUD (Betzler et al., 2020), and it is unlikely that the availability of drug checking equipment encourages drug initiation (Koning et al., 2021).
4. Potential to Reduce Overdose Risk: While further research is needed to establish a direct causal relationship between FTS use and mortality, early studies have indicated a connection between FTS use and a reduced risk of overdose. For instance, the introduction of a vending machine in Cincinnati that dispensed harm reduction supplies, including FTS, coincided with a decrease in unintentional overdose deaths in the county. Additionally, at a supervised injection facility in Vancouver where FTS were provided to service-users, those who expressed an intention to reduce their drug dose after testing experienced significantly lower odds of overdose. Even if a positive test strip result does not change opioid consumption, recent research suggests test strip use is associated with carrying naloxone (Tilhou et al., 2023), which could help prevent fatal overdoses.
5. Consideration: Another study by Tilhou et al. (2023) found, FTS use is associated with performing more safer and more riskier drug use behaviours with respect to overdose. Positive FTS results are associated with more safer behaviours and fewer riskier behaviours than negative test results. These findings suggest that FTS may help promote behaviours to reduce overdose risk among PWUD even when fentanyl penetration is high and use of fentanyl common. Negative FTS test results were associated with fewer safer behaviours. While logical, these findings raise safety concerns given risks of false negatives, especially for fentanyl analogues. These risks are particularly critical for people who primarily use stimulants and other non-opioid drugs and therefore have lower physiological tolerance to high potency opioids. It is critical that harm reduction practitioners encourage PWUD to implement multiple overdose risk reduction techniques regardless of FTS results.
Additional Benefits of programs providing FTS include:
1. Direct Engagement: Harm reduction emphasizes direct engagement with people who use drugs. By providing tools like drug strips, programs can actively involve service-users in their own safety measures, fostering a sense of participation and responsibility.
2. Prevention and Education: Drug strips allow individuals to learn the composition of their substances before use, potentially averting unintended overdoses. This educational aspect can lead to more informed choices and discussions about drug use and its risks.
12
3. Empowerment: Innovative models that include drug strips as part of harm reduction strategies can empower service-users by offering them practical tools to manage their drug use more safely. This empowerment can lead to increased self-efficacy and autonomy in making health-related decisions
4. Integration of Services: The use of drug strips can facilitate the integration of harm reduction with substance use treatment services, offering a more comprehensive approach to addressing drug use. This integration can help bridge the gap between harm reduction and treatment, providing a continuum of care that respects the individual's journey and choices.
5. Wider reach: Test strip distribution has a wider reach than spectrometry methods since they can be carried by individuals and used in any location.
In summary, FTS have demonstrated their effectiveness in detecting fentanyl and its analogues, helping to reduce risky drug use behaviours, and potentially lowering the risk of overdose among people who use drugs, making them a valuable tool in harm reduction efforts.
Limitations Of Using Fentanyl Test Strips as A Drug Checking Tool
Limited Information: These strips can only confirm the presence or absence of fentanyl (or fentanyl analogues) in a substance, providing no information about the quantity or concentration of the substance.
Potential for False Positives: False positive results may occur, especially when testing substances like MDMA or methamphetamine or in the presence of other drugs such as diphenhydramine (Benadryl) (Lockwood et al., 2021).
Practical consideration: High concentrations of diphenhydramine, methamphetamine, and MDMA could potentially lead to false positives when using FTS. Typically, many containers and small baggies contain approximately 0.75–1 mL of water. To illustrate, let's consider a scenario where there's 5 mg of methamphetamine in the container, and it's diluted with 1 mL of water. In this case, the methamphetamine concentration becomes 5 mg/mL, potentially causing a false positive on the FTS.
However, if the residue is instead dissolved with 10 mL of water, the methamphetamine concentration decreases to 0.5 mg/mL, which would yield a true negative result on the FTS. Now, let's imagine the drug residue consists of 95% methamphetamine and 5% fentanyl. With a 10 mL dilution, the methamphetamine concentration would no longer interfere with the FTS, ensuring a true positive result due to the presence of fentanyl in the sample.
For practical guidance aimed at harm reduction groups, it is advisable to dilute with at least 30mL of water. This substantial dilution provides a generous margin of error for the accurate
13
detection of fentanyl in cooker or powder residues while effectively avoiding false positives triggered by other drugs.
Diluting the drug in a larger amount of water might help mitigate the issue of false positives, but there is no nationwide consensus on the appropriate water-to-drug ratio, given variations in drug strength over time and location.
Limited Assurance of Safety: A negative test result does not guarantee that a drug is safe to use, as it may still contain other risks or unknown substances. A negative result does not at any time rule out the presence of fentanyl, as it may be present below the minimum detection level of the test.
An often-raised critique of drug checking surrounds the concerns about the limitations of tests in producing false negatives, potentially leading people to believe a drug is safe when it may not be. However, this argument contains a logical fallacy, as the risk of harm and the likelihood of someone consuming a drug are significantly higher when consumers lack any information about the drug's contents.
Drug checking services consistently emphasize the inherent risks associated with all drug use, focusing on highlighting these risks rather than guaranteeing safety. Furthermore, many of these services employ a combination of drug checking methods to minimize the possibility of false positives, thereby enhancing their overall accuracy and reliability (Barrat & Lee, 2023).
Testing Challenges: While testing the entire quantity of a drug is the ideal approach, it is often impractical due to patterns of substance use. Consequently, it is advisable to use the test strips every time you use a substance.
Inconsistent Drug Supply: Unregulated drug supplies frequently change, and drugs may not always be uniformly mixed. This can result in one part of a drug batch containing fentanyl while another part does not. This phenomenon is often referred to as the "chocolate chip cookie effect" where the cookie represents the entire drug batch, and the chocolate chips symbolize the presence of fentanyl. Even when purchasing from the same source, variations in drug concentrations or mixtures can occur between purchases.
Assume Fentanyl Presence: When uncertain or unable to test a drug, it is prudent to assume that fentanyl is present. Ensure that someone knowledgeable and capable of recognizing and responding to an opioid overdose is present in such situations.
14
Drug Checking Process Using Fentanyl Test Strips
Supplies Needed
● 1 Fentanyl drug testing strip – check the expiry date.
● 5 ml (1 teaspoon) of room temperature drinking water, and if this is not available, use sterile water from a harm reduction program.
● 1 mixing cup
● 1 micro scoop
● 2 Castile soap wipes (1 to clean hands or surface before testing, 1 to clean the surface after testing)
● 1 OHRDP Card Kit Insert to show how to do the test, and how to interpret the results
● A disposal bin like a sharps container to throw the used testing supplies away
How To Prepare for Drug Checking
It’s best to use a test strip each time you use drugs. When drug checking, it’s important that strips are at room temperature.
During drug checking, we recommend the service-user handle the substance, not staff at onsite programs.
During drug checking, we recommend the service-user handle the substance, not staff at onsite programs. Programs that have staff assisting with drug checking need to have a drug checking exemption. If staff are assisting, they should wear gloves
A few grains to one micro scoop of the drug will be needed. The micro scoop holds 5 mg-10mg and 5-10 mg is recommended by the manufacturer.
● Pills: split the pill in two, scraping the inside of the pill – not the outside coating
● Powder: shake up bag or container that drugs are in. Scoop a few granules from this supply.
● Crystal Form: break off a small piece and crush or grind into small granules
● Rock Form: break off or crush a small amount and grind into small granules
15
Procedure For Drug Checking with Fentanyl Test Strips
Step 1:
Add a scoop of drug into the mixing cup.
● Avoid adding too much of the drug because it can affect test accuracy.
● For stimulants like methamphetamine or cocaine, using more of the drug than recommended can cause a false positive or inaccurate positive result. If a stimulant test shows a positive result, add more water - up to 30 ml or 1 ounce - and redo the fentanyl test with a new test strip.
Step 2:
Add 5 mls or 1 teaspoon of the room temperature water to the mixing cup. Gently swirl the drug and water solution to dissolve the drugs.
Step 3:
Open the package at the notched end and take out the test strip.
● It’s very important to hold the strip by the blue end only. Never touch the wavy part of the test strip with fingers as it can impact your result.
● Drug checking should be performed within one hour of opening the package
Step 4:
Place the strip in the water and drug mixture holding it straight up and down. Make sure to cover the wavy lines but do not sink the strip past the single solid blue line or your test will be invalid. Hold the tip in water for at least 10-15 seconds.
Step 5:
Remove the test strip and lay it on top of the drug test strip wrapper. Wait 60 seconds for your result. If there is any doubt in interpretation, it is safest to repeat the test with a second test strip.
16
Interpreting Results
A positive result (indicated by the presence of one red line in the control region “C”) means that fentanyl or a fentanyl analogue has been detected in the drug.

A negative result (two red lines) means that the test did not detect fentanyl or a fentanyl analogue within the sample tested. The presence of any second line, no matter how faint, is NEGATIVE.

An invalid Result occurs when control line fails to appear. Results from any test which has not produced a control line at the specified read time must be discarded. Please review the procedure and repeat with a new test. If the problem persists, discontinue using the kit immediately and contact your local harm reduction program.

False Negatives Vs. False Positives
False Positives – positive results when the drug is not actually present. A test strip can appear positive when a substance that has a similar structure to the drug that is being detected is present. This is called cross reactivity.
False Negatives – negative results when the drug being detected is present. These can happen when the drug is present at trace quantities in the sample. It can also happen when dealing with analogues the test strip is less sensitive for and does not detect as easily. For example, the test strips are less sensitive for 3-methyl fentanyl or carfentanil, compared to fentanyl.
17
Limitations Of a Positive Result
● The test will not tell you about other drugs in your sample. Other substances found in the drugs can cause a false positive, even if there is no fentanyl in the sample.
● The test cannot distinguish between fentanyl-related drugs (e.g., fentanyl and carfentanil).
Stimulants (like methamphetamine or MDMA) can cause false positives with fentanyl test strips. Dilute in more room temperature water, up to 30ml or 1 ounce, and repeat the test with a new test strip.
Limitations Of a Negative Result
● The sample may test negative even when there is fentanyl present because the amount of fentanyl may be so low it is undetectable.
● Fentanyl can be unevenly distributed throughout the drug. The test strip only checks if fentanyl is present in the small portion tested. It cannot tell how much is present in the whole batch of drug or the strength of the batch.
● Tests do not detect all fentanyl or fentanyl related drugs. If new or unidentified fentanyl related drugs are present, the test might still show a negative result.
18
Benzodiazepine Drug Test Strips (BTS)
Summary
● Benzodiazepine test strips have a higher limit of detection relative to their fentanyl counterparts; this means that the tester will need to use more of a sample to reliably detect benzodiazepines if they are present (BTNX, 2023)
● Test results should be interpreted with caution
● Dissolving benzodiazepines in water can be challenging due to their low water solubility. As a result, when attempting to dissolve them in water, they may form clumps or remain as undissolved particles, making it difficult to achieve a homogenous solution.
● People who use drugs and harm reduction service providers should have adequate knowledge of the test strip technology, and on how to read and interpret the results
● People who use drugs and harm reduction service providers should be aware of the limitations of BTS
● Coupling drug test strips with advanced methods of FTIR and mass spectrometry is crucial for enhancing accuracy, specificity, and comprehensiveness of substance analysis in harm reduction efforts.
● Benzodiazepine test strips should be added with other overdose prevention strategies and naloxone distribution
● Using Benzodiazepine test strips as a drug checking tool allows individuals to make informed choices about their substance use, modify their behaviours and potentially prevent overdose.
● Additional benefits of programs providing benzodiazepine test strips include:
Direct engagement
Prevention and education
Service-user empowerment
Integration of services
Wider reach
● Programs that have staff assisting with drug checking need to have drug checking exemptions. For more information please see below: https://www.canada.ca/en/healthcanada/services/health-concerns/controlled-substances-precursorchemicals/exemptions.html
It is very important that the harm reduction staff talk with the service-user about these limitations and that they understand the recommended steps to reduce their risk of drug poisoning regardless of a negative result.
19
Evidence
Background
Benzodiazepines test strips are a significant advancement in harm reduction strategies, particularly in the context of the opioid crisis. These strips are designed to detect the presence of benzodiazepines in substances, offering a quick and straightforward method for individuals to test drugs for contamination or the presence of benzodiazepines. This tool is particularly relevant given the increasing prevalence of benzodiazepines in the unregulated drug supply, which poses significant risks when combined with opioids.
In Canada, benzodiazepines and related drugs have increasingly been found in the opioid supply, complicating overdose responses due to their additive sedating effects. The presence of benzodiazepines in opioids is concerning because naloxone, the opioid overdose antidote, is not effective against benzodiazepines. This situation underscores the importance of benzodiazepines test strips in harm reduction, allowing individuals to detect the presence of these substances in their drugs and potentially make safer choices.
A study by Barker et al. (2004) examined the cognitive effects of long-term benzodiazepine use. This study systematically evaluated the impact of long-term benzodiazepine use on cognitive functioning using meta-analytical techniques. It found that long-term users were significantly impaired compared to controls across all cognitive categories examined, suggesting that the cognitive effects of benzodiazepines could have broader implications for users, including potential safety risks.
Drug Checking – Benzodiazepine Test Strips
In response to the opioid overdose crisis, many harm reduction programs have incorporated some form of on-site and/or off-site “drug checking” intervention into their services. During a "drug checking" process, unregulated drugs or illegally acquired prescription pills are analyzed to determine their composition or if they are adulterated. The distribution and use of benzodiazepine test strips is one method used for drug checking.
What Are Benzodiazepine Test Strips?
Benzodiazepines test strips are rapid visual immunoassays for the qualitative, presumptive detection of benzodiazepines in various substances. They work similarly to fentanyl test strips, where the presence of the target drug causes a reaction on the strip, typically the disappearance of a line, indicating a positive result. These strips are designed to target a broad range of drugs within the benzodiazepine class, making them a versatile tool in detecting these substances in the opioid supply (Lardner & Burek, 2021).
20
Impact On Overdose Deaths and Behaviour Change
The introduction of test strips for drugs, including benzodiazepines, has shown promise in reducing overdose risks. A study evaluating a fentanyl test strip intervention among female sex workers who use drugs in Baltimore found significant reductions in drug use frequency and solitary drug use following test strip use, suggesting that such interventions could extend to benzodiazepines test strips (Park et al., 2020). These findings highlight the potential of test strips to not only inform users of the presence of dangerous substances in their drugs but also to encourage safer drug use practices.
Impact on Overdose Deaths
The presence of benzodiazepines in the unregulated drug supply, particularly when combined with opioids, significantly increases the risk of overdose and overdose-related deaths. Benzodiazepines can exacerbate the respiratory depression caused by opioids, leading to fatal outcomes. The use of test strips can inform users about the presence of benzodiazepines, potentially leading to more cautious use or the avoidance of contaminated substances. A study by Park et al. (2020) in "Addiction" highlighted the association between prescribed benzodiazepines and increased risk of fatal opioid overdose among individuals receiving buprenorphine, underscoring the dangers of concurrent use of opioids and benzodiazepines.
Behaviour Change
The availability of benzodiazepines test strips can lead to significant behaviour changes among drug users. By providing immediate feedback on the content of their substances, these strips empower users to make informed decisions, potentially leading to reduced consumption of contaminated drugs. A pilot study by Park et al. (2020) on female sex workers who use drugs in Baltimore found that the use of fentanyl test strips led to significant reductions in drug use frequency and solitary drug use, suggesting that similar interventions with benzodiazepines test strips could encourage harm reduction behaviours
Furthermore, the study by Swartz et al. (2023) on the feasibility of using mobile phone-based experience sampling to assess drug checking behaviours among street opioid users found that test strip use was associated with higher proportions reporting overdose risk reduction behaviours. This indicates that the use of test strips, including those for benzodiazepines, can lead to increased engagement in behaviours that reduce the risk of overdose (Research Square).
21
Advantages Of Benzodiazepine Test Strips
The primary advantage of benzodiazepines test strips is their ability to provide rapid and specific information about the presence of benzodiazepines in substances, which can be crucial for individuals at risk of overdose. This information can lead to more informed decisions, potentially reducing the risk of overdose when benzodiazepines are present.
Additional benefits of programs providing benzodiazdepine test strips include:
1. Immediate Detection and Informed Decision-Making: One of the primary advantages of benzodiazepines test strips is their ability to provide immediate results regarding the presence of benzodiazepines in a substance. This rapid feedback is crucial for individuals who use drugs, as it enables them to make informed decisions about their drug use in real-time. The study by Park et al. (2020) demonstrated that interventions using fentanyl test strips led to significant reductions in risky drug use behaviours among female sex workers in Baltimore, indicating that similar outcomes could be expected with benzodiazepines test strips
2. Reduction in Overdose Risk: Benzodiazepines, particularly when used in combination with opioids, significantly increase the risk of overdose due to their synergistic effects on respiratory depression. By using test strips, individuals can detect the presence of benzodiazepines and potentially avoid using the contaminated substance, thereby reducing the risk of overdose. The research by Dasgupta et al. (2016) highlighted the complex interactions between opioids and benzodiazepines and the increased risk of overdose, which emphasizes the importance of using drug checking methods like drug test strips and more advanced drug checking technologies (FTIR and mass spectrometry).
3. Empowerment and Engagement in Harm Reduction: Benzodiazepine test strips empower users by providing them with a tool to actively engage in harm reduction. This empowerment can lead to increased awareness and education about the risks associated with drug use, particularly the dangers of polydrug use involving benzodiazepines and opioids. The study by Swartz et al. (2023) using mobile phone-based experience sampling to assess drug checking behaviours among opioid users found that test strip use was associated with increased overdose risk reduction behaviours, highlighting the role of these strips in promoting harm reduction (Swartz et al., 2023).
4. Contribution to Public Health Data and Research: The use of benzodiazepine test strips can contribute valuable data to public health research, particularly in understanding the prevalence and patterns of benzodiazepine contamination in the unregulated drug supply. This information can inform policy decisions, harm reduction strategies, and targeted interventions to address the opioid crisis and reduce overdose deaths.
5. Wider reach: Test strip distribution has a wider reach than spectrometry methods since they can be carried by individuals and used in any location.
22
In summary, Benzodiazepine test strips have demonstrated their effectiveness in detecting certain compounds of benzodiazepine and, helping to reduce risky drug use behaviours, and potentially lowering the risk of overdose among people who use drugs, making them a valuable tool in harm reduction efforts.
Limitations Of Benzodiazepines Test Strips as a Drug Checking Tool
While benzodiazepines test strips offer significant benefits in harm reduction and individual safety, they are not without limitations. Understanding these limitations is crucial for effective use and for guiding future improvements in drug testing technologies. They cannot determine the concentration of benzodiazepines or identify specific types within the class, which varies in strength and effects. Moreover, some benzodiazepine analogues, like etizolam, may not be detected due to their different chemical structures. This limitation highlights the need for continuous development and improvement of these testing tools to cover a broader range of substances The following elaboration on the limitations of benzodiazepines test strips is supported by additional sources.
Specificity and Sensitivity Issues
One of the primary limitations of benzodiazepines test strips is their variability in specificity and sensitivity. Not all test strips are equally effective at detecting all benzodiazepines or their analogues, which can lead to false negatives. For example, some strips may not detect newer or less common benzodiazepine analogues like etizolam, which has been increasingly found in the unregulated drug supply. This limitation can give users a false sense of security, potentially leading to unsafe drug use behaviours. The study by Laing et al. (2021) in "The International Journal on Drug Policy" highlighted the challenges in detecting novel psychoactive substance benzodiazepines in the unregulated drug supply, underscoring the need for improved detection methods (Laing et al., 2021).
Inability to Quantify Drug Concentration
Benzodiazepines test strips can indicate the presence of benzodiazepines in a substance but cannot quantify the amount present. This limitation means that even if a strip indicates a positive result, the user has no information about the concentration of the drug, which can vary widely and significantly impact the risk of overdose. The lack of quantitative data limits the user's ability to assess the true risk associated with using the substance.
Potential for False Positives and False Negatives
Like any rapid testing method, benzodiazepines test strips are subject to potential false positives and false negatives. False positives can occur due to cross-reactivity with other substances, while false negatives can result from the test's sensitivity threshold, or the presence of benzodiazepine analogues not detected by the strip. These inaccuracies can lead to misinformed decisions by users, potentially increasing the risk of harm. The detection of benzodiazepine adulteration
23
within an unregulated drug supply sample highlights additional dangers exacerbating the ongoing synthetic opioid epidemic. A study by Laing et al. (2021) found a significant occurrence of both false positives and false negatives when using point-of-care detection techniques and emphasized the need to exercise caution by employing a combination of these methods alongside confirmatory drug testing. This approach can facilitate early identification and continuous monitoring of unregulated drug markets, consequently informing the development of targeted harm reduction strategies and healthcare policy initiatives.
User Interpretation and Decision-Making
The effectiveness of benzodiazepines test strips relies heavily on the user's ability to correctly interpret the results and make informed decisions based on those results. Misinterpretation of test outcomes or a lack of understanding about the implications of a positive or negative result can lead to risky behaviours. Furthermore, the decision to use or not use a substance based on test strip results may be influenced by various factors, including addiction, peer pressure, and the availability of alternative substances.
Dependence on a Single Harm Reduction Tool
Relying solely on benzodiazepines test strips for harm reduction can be problematic. These strips should be part of a comprehensive harm reduction strategy that includes education, access to healthcare and treatment services, and other drug checking technologies. Overreliance on test strips without considering other harm reduction measures may not adequately address the complex issues associated with drug use and overdose risk. Use of benzodiazepines test strips should always be coupled with other ham reduction strategies and overdose prevention strategies to minimize the risks and identify trends in the drug market. A study by Tobias et al. (2020) examined the contents of counterfeit alprazolam tablets in the unregulated drug market in British Columbia, Canada, using drug checking services. It underscored the importance of coupling methods like mass-spectrometry and benzodiazepines test strips, in identifying counterfeit and potentially dangerous and novel substances in the drug supply.
Continuous Improvement and Research: Ongoing research and development are essential to address the limitations of current test strips and to adapt to emerging challenges, such as the detection of novel psychoactive substance (NPS) benzodiazepines in the unregulated drug supply.
Education and Training: Harm reduction staff should receive education and training on the proper use of benzodiazepines test strips, including how to interpret results and counsel drug users on risk reduction strategies based on test outcomes.
Policy and Practice Implications: The findings from research on benzodiazepines test strips have implications for policy and practice, including the need for guidelines on the use of test strips in harm reduction settings and the integration of drug checking services into broader public health initiatives.
24
Collaboration and Data Sharing: Collaboration between harm reduction organizations, researchers, and policymakers is crucial for sharing data and best practices related to the use of benzodiazepines test strips. This can enhance the effectiveness of harm reduction strategies and inform the development of evidence-based policies.
Dissolving benzodiazepines in water can be challenging due to their low water solubility. These compounds are typically hydrophobic, meaning they have an aversion to water. As a result, when attempting to dissolve them in water, they may form clumps or remain as undissolved particles, making it difficult to achieve a homogenous solution (Shapiro et al. 2020).
Drug Checking Process Using Benzodiazepine Test Strips Supplies Needed
● 1 Benzodiazepine drug testing strip – check the expiry date.
● 5 ml (1 teaspoon) of room temperature drinking water, and if this is not available, use sterile water from a harm reduction program
● 1 mixing tube
● 1 micro scoop
● 2 Castile soap wipes (1 to clean hands or surface before testing, 1 to clean the surface after testing)
● 1 OHRDP Card Kit Insert to show how to do the test, and how to interpret the results
● A disposal bin like a sharps container to throw the used testing supplies away
How To Prepare for Drug Checking
It’s best to use a test strip each time you use drugs. When drug checking, it’s important that strips are at room temperature 15-30°C (59-86°F).
Benzodiazepines do not dissolve well in water so vigorous mixing and concentrated solutions must be used to minimize the chance of not detecting the drug when it is present in a sample.
During drug checking, we recommend the service-user handle the substance, not staff at onsite programs. Programs that have staff assisting with drug checking need to have a drug checking exemption. If staff are assisting, they should wear gloves.
A few grains to one micro scoop of the drug will be needed. The micro scoop holds 5mg-10mg and 5-10 mg is recommended by the manufacturer (BTNX, 2023).
• Pills: split the pill in two, scraping the inside of the pill – not the outside coating
• Powder: shake up bag or container which drugs are in. Scoop a few granules from this supply.
• Crystal Form: break-off a small piece and crush or grind into small granules
• Rock Form: break off or crush a small amount and grind into small granules
25
Procedure For Drug Checking with Benzodiazepine Test Strips
Step 1:
Add a scoop of drug into the mixing tube. Avoid adding too much of the drug because it can affect test accuracy.
Step 2:
Add 5 mls or 1 teaspoon of the room temperature water to the mixing tube. Close the lid and shake the tube for 30 seconds.
Step 3:
Open the package at the notched end and take out the testing strip.
It’s important to hold the strip by the orange end only. DO not touch the wavy part of the test strip with fingers as it can impact your result.
Drug checking should be performed within one hour of opening the package
Step 4:
Place the strip in the water and drug mixture holding it straight up and down. Make sure to cover the wavy lines but do not sink the strip past the solid orange line or your test will be invalid. Hold the tip in water for at least 10-15 seconds.
Step 5:
Remove the test strip and lay it on top of the drug test strip wrapper. Wait 60 seconds for your result.
If there is any doubt in interpretation, it is safer to repeat the test with a second test strip.
26
Interpreting Results
When obtaining a positive result, only one coloured line appears in the control region (C). No apparent coloured line appears in the test region (T).
A negative result occurs when two coloured lines appear on the membrane. One line appears in the control region (C) and another line appears in the test region (T). Even faint lines are considered negative.

An invalid result occurs when the control line (C) fails to appear. Results from any test which has not produced a control line at the specified read time must be discarded. Please review the procedure and repeat with a new test. If the problem persists, discontinue using the kit immediately and contact your local harm reduction program.

False Negatives Vs. False Positives
False Positives – a positive results when the drug is not actually present. A test strip can appear positive when a substance that has a similar structure to the drug that is being detected is present. This is called cross reactivity.
False Negatives – negative results when the drug being detected is present. These can happen when the drug is present at trace quantities in the sample. It can also happen when dealing with analogues the test strip is less sensitive for and does not detect as easily.
27
Limitations Of a Positive Result
• The test will not tell you about other drugs in your sample.
• Other substances found in the drugs can cause a false positive, even if there is no benzodiazepines in the sample.
Limitations Of a Negative Result
• False negatives can occur easily due to the benzodiazepine not being dissolved in the water.
• The test cannot distinguish between the many different types of benzodiazepines.
• Although a benzodiazepine may be present, there are types of benzodiazepines that the strips cannot detect.
28
Xylazine Drug Test Strips (XTS)
Summary
• Xylazine not approved for human application and can lead to adverse outcomes including significant skin damage, suppression of the central nervous system, cardiovascular complications, and even fatality
• The presence of xylazine in the unregulated drug supply has been recognized in Canada
• Naloxone is not effective for reversing a xylazine related overdose
• XTS have low detection limit, high sensitivity, and specificity of xylazine. Drug samples that may also have high levels of substances like diphenhydramine, lidocaine, levamisole, MDMA, or methamphetamine might trigger a false positive result for xylazine.
• Test results should be interpreted with caution
• People who use drugs, and harm reduction program staff should have adequate knowledge of the test strip technology, and how to read and interpret results
• People who use drugs and harm reduction service providers should be aware of the limitations of xylazine test strips
• Coupling drug test strips with advanced methods like FTIR and mass spectrometry is crucial for enhancing the accuracy, specificity, and comprehensiveness of substance analysis in harm reduction efforts.
• XTS should be added with other overdose prevention strategies and naloxone distribution
• Using XTS as a drug checking tool allows individuals to make informed choices about their substance use, modify their behaviours and potentially prevent overdose.
• Additional benefits of programs providing XTS include:
Direct engagement
Prevention and education
Service-user empowerment
Integration of services
Wider reach
● Programs who will have staff directly assisting with drug checking need to have drug checking exemption. For more information please see below:
https://www.canada.ca/en/health-canada/services/health-concerns/controlledsubstances-precursor-chemicals/exemptions.html
It is very important that harm reduction staff engage with service-users about drug test limitations. Ensure service-users understand the recommended steps to help reduce their risk of drug poisoning regardless of a negative result.
29
Evidence Background
Xylazine, a non-opioid sedative, analgesic, and muscle relaxant primarily used in veterinary medicine, has increasingly been detected in the unregulated drug supply, raising public health concerns due to its potential to exacerbate the effects of opioids and complicate overdose reversal efforts. The emergence of xylazine test strips represents a significant development in harm reduction strategies, offering a means to detect the presence of xylazine in substances.
Xylazine, which is not approved for human use, can lead to adverse outcomes including significant skin damage, suppression of the central nervous system, cardiovascular complications, and even fatality. Initial reports from the Office of the Chief Coroner of Ontario indicate that xylazine was detected in approximately 2% to 4% of opioid-associated fatalities from the fourth quarter of 2021 to the third quarter of 2022 (Canadian Centre on Substance Use and Addiction, (2023). The danger of xylazine lies in its non-opioid nature. The toxic dose range for humans spans from 40 mg to 2,400 mg. The challenge in analyzing drug-related deaths is determining whether xylazine alone or in conjunction with other contaminants caused the fatality, especially when multiple adulterants are present in a drug sample. Recorded xylazine levels in lethal cases vary widely, from mere traces to 16 mg/L, partly because even minimal quantities of xylazine can amplify the potency of other substances, such as heroin. The considerable overlap between doses that can lead to death and those that might not highlights the absence of a "safe" xylazine blood level, making it challenging to know whether a specific amount of xylazine in a drug sample will be lethal (Ayub et al. 2023)
In Canada, the presence of xylazine in the unregulated drug supply has been recognized, with test strips being made available as part of harm reduction initiatives. These strips are used in various settings, including healthcare facilities and community harm reduction programs, to test substances and provide immediate information on the presence of xylazine, thereby aiding in the prevention of potential harm (Canadian Agency for Drugs and Technologies in Health, 2023)
Drug Checking – Xylazine Test Strips
In response to the opioid overdose crisis, many harm reduction programs have incorporated some form of on-site and/or off-site “drug checking” intervention into their services. During a "drug checking" process, unregulated drugs or illegally acquired prescription pills are analyzed to determine their composition or if they are adulterated. The distribution and use of Xylazine Test Strips is one method used for drug checking.
30
What Are Xylazine Test Strips?
XTS are rapid, visual immunoassays designed for the qualitative, presumptive detection of xylazine in drug samples. They operate on a principle like other drug test strips, where the presence of the target substance leads to a visual change on the strip, indicating a positive result. These strips are intended to provide immediate feedback to individuals about the presence of xylazine in their substances, enabling informed decision-making (BTNX, 2023)
Evidence Review of The Effectiveness of Xylazine Test Strips
In March 2023, a Philadelphia-based study (CFSRE, 2023) aimed to evaluate the efficacy of drug checking test strips. This laboratory investigation utilized samples obtained through public health collaborations, alongside lab-generated controls to validate the findings. The tested "real-world" samples, derived from unregulated drug use, were analyzed using both gas chromatography-mass spectrometry and liquid chromatography quadrupole time-of-flight mass spectrometry. These analyses confirmed the presence of various drug components, including xylazine, fentanyl, and other contaminants. The xylazine test strips were found to be reliable for drug checking, exhibiting high sensitivity (100%), specificity (85%), and precision (91%). However, lidocaine was noted as a potential source of false positives.
Preliminary findings from the John Hopkins Bloomberg School of Public Health (Sisco et al., 2023) on the xylazine test strips indicated good sensitivity and minimal cross-reactivity, with lidocaine being the only exception. The strips were capable of detecting xylazine in solutions at concentrations as low as 0.5 mcg/mL, consistently yielding positive results for concentrations starting from 2.5 mcg/mL. In practical applications involving actual drug residues, xylazine was reliably identified in samples with concentrations above 2 mcg/mL. However, the results were variable for samples with concentrations between 0.1 mcg/mL and 2 mcg/mL, highlighting the strips limitations at lower concentrations. These insights, combined with the Philadelphia study's outcomes, suggest that BTNX test strips are effective for use in drug checking initiatives.
Shuda & Lam (2022) found that Xylazine test strips are effective in providing indicative results for the presence of xylazine in drug samples. These strips accurately identified all genuine samples with xylazine as positive and those without as negative. Preparing the samples involved simply dissolving a small quantity of the residue or powdered substance in 1 mL of water, which was enough to achieve a concentration detectable by the test strips.
However, drug samples that are suspected or confirmed to have high levels of substances like diphenhydramine, lidocaine, levamisole, MDMA, or methamphetamine might trigger a false positive result for xylazine. During evaluations, false positives did not occur in samples containing these substances. In cases where drug samples contain such interfering substances, alternative testing methods might be necessary to accurately identify the presence or absence of xylazine.
31
Impact On Overdose Deaths and Behaviour Change
The introduction of xylazine test strips has the potential to impact overdose deaths and user behaviour significantly. However, specific studies evaluating the impact of xylazine test strips on overdose deaths and behaviour change are currently limited, indicating a need for further research in this area.
Advantages Of Xylazine Test Strips
The primary advantage of xylazine test strips lies in their ability to provide rapid and specific information about the presence of xylazine in substances. This can empower individuals to make informed decisions about their drug use, potentially reducing the risk of harm associated with xylazine-contaminated substances. Additionally, these strips can contribute valuable data to public health research, helping to understand the prevalence and patterns of xylazine contamination in the unregulated drug supply.
Additional benefits of programs providing Xylazine test strips include:
1. Direct Engagement: Harm reduction emphasizes direct engagement with people who use drugs. By providing tools like drug strips, programs can actively involve service-users in their own safety measures, fostering a sense of participation and responsibility.
2. Prevention and Education: Drug strips allow individuals to learn the composition of their substances before use, potentially averting unintended overdoses. This educational aspect can lead to more informed choices and discussions about drug use and its risks.
3. Empowerment: Innovative models that include drug strips as part of harm reduction strategies can empower service-users by offering them practical tools to manage their drug use more safely. This empowerment can lead to increased self-efficacy and autonomy in making health-related decisions.
4. Integration of Services: The use of drug strips can facilitate the integration of harm reduction with substance use treatment services, offering a more comprehensive approach to addressing drug use. This integration can help bridge the gap between harm reduction and treatment, providing a continuum of care that respects the individual's journey and choices.
5. Wider reach: Test strip distribution has a wider reach than spectrometry methods since they can be carried by individuals and used in any location.
In summary, Xylazine test strips have demonstrated their effectiveness in detecting xylazine helping to reduce risky drug use behaviours, and potentially lowering the risk of overdose among people who use drugs, making them a valuable tool in harm reduction efforts.
32
Limitations Of Using Xylazine Test Strips as a Drug Checking Tool
Despite their benefits, xylazine test strips have limitations. They cannot quantify the amount of xylazine present or identify specific analogues, which may vary in potency and effects. Furthermore, the effectiveness of these strips can be influenced by the complexity of the drug sample matrix and the presence of other substances, which may lead to false positives or negatives. These limitations highlight the need for continuous development and improvement of testing technologies.
Drug Checking Process Using Xylazine Test Strips
Supplies Needed
● 1 Benzodiazepine drug testing strip – check the expiry date.
● 5 ml or 1 teaspoon of room temperature drinking water, and if this is not available, use sterile water from a harm reduction program
● 1 mixing cup
● 1 micro scoop
● Castile soap wipes (1 to clean hands or surface before testing, 1 to clean the surface after testing)
● OHRDP Kit Insert to show you how to do the test, and how to interpret the results
● A disposal bin like a sharps container to throw the used testing supplies away
How To Prepare for Drug Checking Using Xylazine Test Strips
It’s best to use a test strip each time you use drugs. When drug checking, it’s important that strips are at room temperature 15-30°C (59-86°F)..
During drug checking, we recommend the service-user handle the substance, not staff at onsite programs. Programs that have staff assisting with drug checking need to have a drug checking exemption. If staff are assisting, they should wear gloves.
A few grains to one micro scoop of the drug will be needed. The micro scoop holds 5mg-10 and 5-10 mg is recommended by the manufacturer (BTNX, 2023)
● Pills: split the pill in two, scraping the inside of the pill – not the outside coating
● Powder: shake up bag or container that drugs are in. Scoop a few granules from this supply.
● Crystal Form: break-off a small piece and crush or grind into small granules
● Rock Form: break off or crush a small amount and grind into small granules
33
Procedure For Completing Drug Checking Using Xylazine Test Strips
Step 1
Add a few grains to one mini scoop of drug into the cup. Avoid adding too much of the drug because it can affect test accuracy. (The mini scoop holds 5-10 mgs, and the The manuafacturer recommends 5-10mg)
Step 2
Add 5 mls or 1 teaspoon of the room temperature water to the mixing cup. Gently swirl the drug and water solution to dissolve the drugs.
Step 3
Open the package at the notched end and take out the testing strip.
● It’s very important to hold the strip by the red end only. Never touch the wavy part of the test strip with fingers as it can impact your result.
● Drug checking should be performed within one hour of opening the package
Step 4
Place the strip in the water and drug mixture holding it straight up and down. Make sure to cover the wavy lines but do not sink the strip past the solid red line or your test will be invalid. Hold the tip in water for at least 10-15 seconds.
Step 5
Remove the test strip and lay it on top of the drug test strip wrapper. Wait 60 seconds for your result.
If there is any doubt in interpretation, it is safer to repeat the test with a second test strip.
34
Interpreting Results
When receiving a positive result (Xylazine Detected) only one coloured line appears in the control region (C). No apparent coloured line appears in the test region (T).
A negative result occurs when two coloured lines appear on the membrane. One line appears in the control region (C) and another line appears in the test region (T).

An invalid result occurs when a control line fails to appear. Results from any test which has not produced a control line at the specified read time must be discarded. Please review the procedure and repeat with a new test. If the problem persists, discontinue using the kit immediately and contact your local harm reduction program.
False Negatives Vs. False Positives
False Positives – a positive results when the drug is not actually present. A test strip can appear positive when a substance that has a similar structure to the drug that is being detected is present. This is called cross reactivity.
False Negatives – negative results when the drug being detected is present. These can happen when the drug is present at trace quantities in the sample. It can also happen when dealing with analogues the test strip is less sensitive for and does not detect as easily.
35
Limitations Of a Positive Result
• The test will not tell you about other drugs in your sample.
• Other substances found in the drugs can cause a false positive, even if there is no Xylazine in the sample (such as lidocaine).
Limitations Of a Negative Result
• The sample may test negative even when there is Xylazine present because the amount of Xylazine may be so low it’s undetectable.
• Xylazine can be unevenly distributed throughout the drug. The test strip only checks if Xylazine is present in the small portion tested. It cannot tell how much is present in the whole batch of drug or the strength of the batch.
• Tests do not detect drugs that are similar to xylazine. If new or unidentified xylazine related drugs are present, the test might still show a negative result.
36
Practical Considerations for Programs
Ordering Process
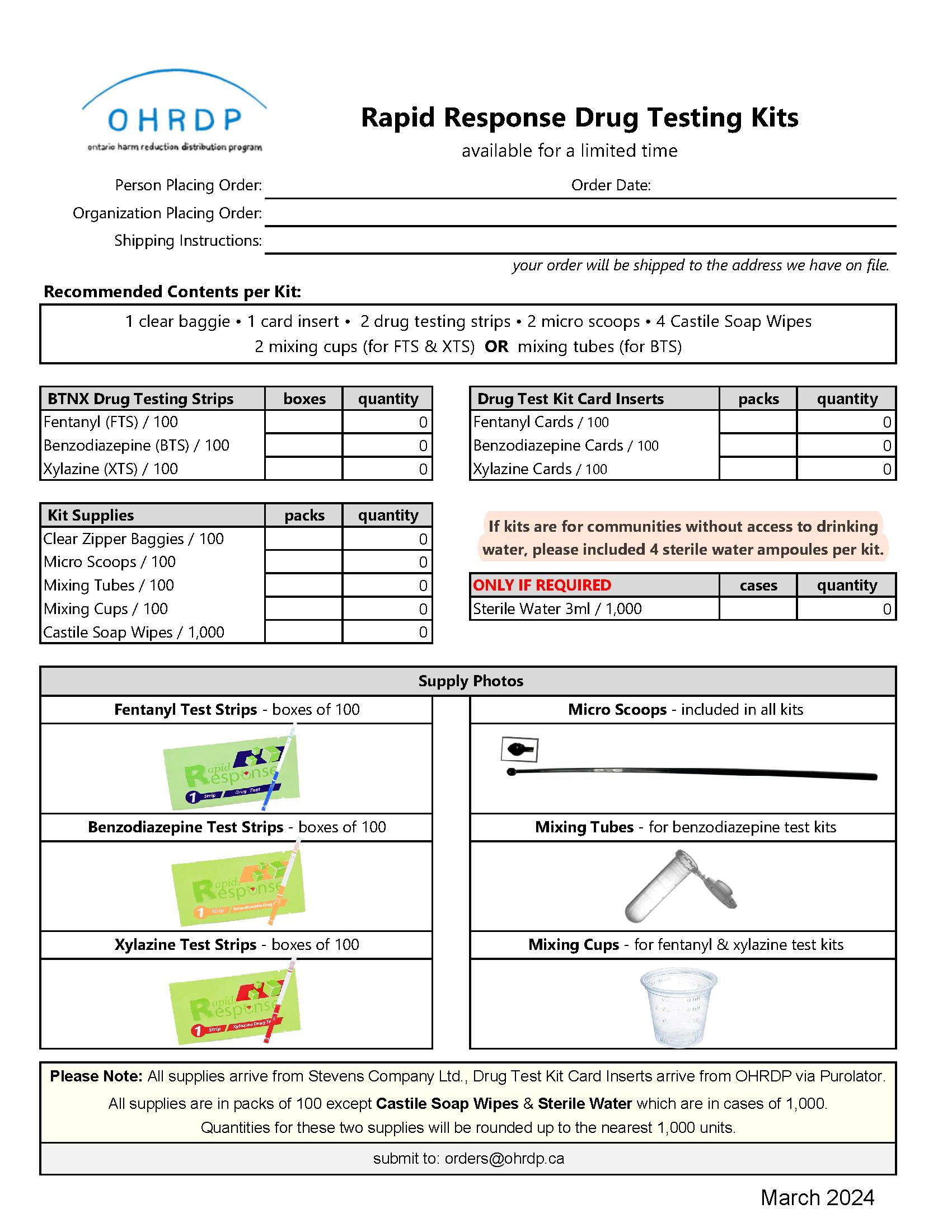
Ordering drug test strips through OHRDP will be the same process as ordering all other harm reduction supplies. Because Drug Testing Strips are not permanently added to the OHRDP catalogue, they will have their own order form. This order form will list all the supplies needed to create drug checking kits. The Core Program will be able to identify the quantities of each BTNX Drug Testing Strip and corresponding kit supplies desired.
OHRDP’s current Core Programs will order through OHRDP on behalf of their region by submitting the order form to orders@ohrdp.ca. All Rapid Response Drug Testing Kit orders will be reviewed by OHRDP to ensure Core Program’s maximum allotments are not exceeded and monitor the form calculations for best practice ratios for the corresponding items. The approved request will be processed as two separate shipments. The Drug Test Kit Card Inserts will be shipped from OHRDP (Kingston ON) and the other supplies will be shipped from our medical distributor. Please allow 2-weeks for all supplies to be delivered.
It will be up to each Core Program to decide the frequency of ordering, up until their allotment (one large order for entire allotment, weekly, monthly, etc.) is met.
We encourage programs to keep the drug test kit ordered supplies separate so that your regular harm reduction supply needs are not impacted. (Order Form can be found in the Appendix).
In terms of receiving, tracking and storage, please follow the instructions and steps from Your OHRDP Toolkit - Stocked & Ready to Support Your Community.
37
Storage And Handling`
Storage
Kits should be stored at 2-30°C (36-86°F). If not kept within this temperature range, results may not be reliable. Storing in a car in the winter or summer or use outside in colder temperatures for example may not be appropriate.
Remember to check expiry dates on kits prior to giving them out. Do not use after expiration date indicated on the package. Results may not be accurate.
See Fentanyl test strip Safety Data Sheet in Appendix
Handling
Programs who will have staff assisting with drug checking need to have drug checking exemptions. For more information, visit: https://www.canada.ca/en/healthcanada/services/health-concerns/controlled-substances-precursorchemicals/exemptions.html
Test strips should be brought to room temperature 15-30°C (59-86°F) before use.
Humidity and temperature can adversely affect results.
Do not eat, drink, or smoke in the area where the test samples and kits are handled.
Do not use the test if the foil pouch is damaged.
Kits must be used within 10 minutes of opening for accurate results.
Do not reuse tests. Use a new test every time.
The used testing materials should be discarded in accordance with local, provincial and/or federal regulations. See disposal section for further information.
38
Kit Configuration
It is recommended to use room temperature drinking water to complete drug checking with test strips. If drinking water is not available, sterile water may be used as an alternative.
Drug Test Kit contents should include:
• 1 clear plastic 6x9” zip lock baggie
• 4 Castile soap wipes (1 to clean hands or surface before testing, 1 to clean the surface after testing)
• *4 sterile waters (order only if no room temperature drinking water available)
• 2 drug test strips
• 2 micro scoops
• 2 mixing cups
• 1 OHRDP Card Kit Insert
Please DO NOT add test strips into regular injection and/or inhalation kits. Drug checking supplies should always be an individual kit. It is important that engagement takes place between harm reduction worker and service-user around these drug test strips.
Disposal
Programs should follow protocol, procedures, and regulations that each specific program/organization has in place for discarding hazardous substances.
Disposal technique for service-users using take-home drug test kits could include:
To dispose of the test-water use a paper towel to absorb the water. Wipe down the drug checking space, to avoid cross contamination or exposure of others to substances
Put all the used supplies in the clear baggie that the test and test supplies came in. Dispose of the baggie in a bio bin.
39
Recommendations For Training
Programs that participate in distributing drug test kits should be able to:
● Properly store and handle test strips
● Learn and be aware of the limitations of drug checking strips.
● Have the knowledge to perform drug checking using test strips and be able to provide teaching to service-users on how to perform drug checking using test strips
● Communicate findings back to service-users, including the provision of relevant harm reduction information
● Have a process for disposing samples and test equipment
Appropriately trained harm reduction workers should be able to communicate the following to service-users:
● Proper storage and handling of test strips
● The process for performing drug checking using test strips
● How to interpret drug checking results using test strips
● Limitations of drug checking with test strips
● Proper disposal of test strips and drug samples
● Inquire if service-users have a safety plan
Safety Planning
Encourage the importance of a safety plan when service-users are using any type of substances where quantity and types of drugs within the substance are unknown. The following information can be discussed:
1. Carry and Know How to Use Naloxone
Carry and have Naloxone readily available for someone to use. Ensure people around you know where your naloxone is located (in your bag, in your pocket) and that they know how to use it.
2. Do not use alone
Promotion of the National Overdose Response Service at 1-888-688-NORS (6677) or a regional safety app if being around others is not possible. Being around people you trust should also be a consideration when possible.
3. Start Low and Go Slow
Start with a small amount.
Trial test doses.
40
4. Plan Ahead
Be in a comfortable seated position. If you fall asleep or are ‘out’ you do not want to be in a compromised position. For example: risk for cutting off circulation to a body part which can lead to further complications like paralysis or compartment syndrome
Prepare personal belongings so that there is less of a chance of losing them/having them stolen if you are incapable of watching them while you are high or ‘out.’
Ensure you are in a safe space away from harm (harmful people, harmful situations). A CTS or OPS are recommended safe spaces if they are available.
If you are using outside, ensure you are dressed appropriately for the climate (warm clothing in winter, sunscreen in summer).
5. Consider 911 Response Time in Your Area
Rural areas have much longer 911 response times. Consider this when picking up naloxone kits as multiple kits may be needed.
Using with someone who is comfortable performing CPR
Knowing places that have access to AEDs/first aiders who know how to use AEDs – especially when a person is not responding to naloxone.
In northern Ontario where 911 may not be readily available, call your nearest emergency healthcare provide or nursing station.
6. Do Not Mix Drugs
example: mixing drugs with alcohol, using speed balls
When multiple drugs are mixed, overdoses may be more difficult to treat .
7. Know The Signs of Overdose
It’s important to recognize the signs of an overdose and call for help if you think someone needs assistance.
8. Encourage Safe Use Of Supplies According To Best Practice
See OHRDP’s Connecting – A Guide for Using Harm Reduction Supplies as Engagement Tools for the best practices in user-friendly format.
41
FAQs
Can our organization/program allow service-users to check their drugs onsite with the help of staff?
Programs who will have staff assisting with drug checking need to have a drug checking exemption. For more information, visit: https://www.canada.ca/en/healthcanada/services/health-concerns/controlled-substances-precursor-chemicals/policyregulations/policy-documents/subsection-56-1-class-exemption-urgent-public-health-needssites-provinces-territories.html
If a service-user chooses to discard their substance(s) after drug checking – how do we do that?
Staff/service-users should follow the protocol and procedures that each specific program/organization has in place for discarding unwanted/forgotten drugs/substances. Dispose of the used testing supplies in accordance your program’s protocols. (Disposal, pg. 21)
If a service-user overdoses after utilizing Rapid Response™ Test Strip is there a liability concern?
Providing risks and test limitations messaging to the service-user is important. Staff should never use terms like “safe” when discussing test results. If you have further questions about liability, it is best to speak with your insurance provider or the legal team associated with your program or organization.
If a service-user completes a fentanyl drug test using FTS, can they use the same sample to drug check with other drug checking test strips (such as Xylazine or Benzodiazepine Test Strips)?
Yes, the same testing sample can be used for multiple drug tests. It’s best to do a test one at a time to ensure proper technique of each test strip.
Can we put the individual drug test strips into our injection, inhalation, or naloxone kits? We strongly recommend making independent drug test kits as suggested in this document. To get the most accurate results for use of drug test strips – engagement and teaching are crucial. If drug test strips are added to a naloxone kit, they could go unnoticed for a long period of time with service-users not opening a kit until naloxone is needed. Test Strips could easily expire if the naloxone kit is not opened.
Is there anything else we should make sure service-users are aware of around drug test strips?
Inquiring if service-users have a safety plan is important. Encouraging individuals to have a plan in place will decrease the risk they are exposed to when using drugs.
42
Useful Links and Further Reading
1. Toronto drug checking service: Fentanyl Test Strips
https://drugchecking.community/resource/fentanyl-test-strips/
2. Toronto Drug Checking Service: Reports
https://drugchecking.community/reports/
3. BTNX: Rapid Response Fentanyl Test Strip - Instructions
https://www.btnx.com/files/HarmReduction/Instructions%20(EN)%20H10110336601FYL-18S7-100%20FYL-18S7-10.pdf
4. Harm Reduction Journal: High concentrations of illicit stimulants and cutting agents cause false positives on fentanyl test strips
https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-02100478-4
5. Language Matters: Create a safer space with less stigma
https://towardtheheart.com/reducing-stigma
43
References
Ayub S. Parnia S.Poddar K.Bachu AK, Sullivan A, Khan AM, Ahmed S, Jain L. Xylazine in the Opioid Epidemic: A Systematic Review of Case Reports and Clinical Implications. Cureus. 2023 Mar 29;15(3):e36864. Doi: 10.7759/cureus.36864. PMID:37009344; PMCID:PMC10063250
Barker MJ, Greenwood KM, Jackson M, Crowe SF. Cognitive effects of long-term benzodiazepine use: a meta-analysis. CNS Drugs. 2004; 18(1):37-48. Doi: 10.2165/00023210-200418010-00004. PMID:14731058
Barratt, M. & Lee, N. (2023). What Works: Drug checking and related interventions. Melbourne: 360Edge
Belzak, L., & Halverson, J. (2018). The opioid crisis in Canada: a national perspective. La crise des opioïdes au Canada : une perspective nationale. Health promotion and chronic disease prevention in Canada : research, policy and practice, 38(6), 224–233. https://doi.org/10.24095/hpcdp.38.6.02
Bergh MS, Øiestad ÅML, Baumann MH, Bogen IL. Selectivity and sensitivity of urine fentanyl test strips to detect fentanyl analogues in illicit drugs. Int J Drug Policy. 2021 Apr;90:103065. doi: 10.1016/j.drugpo.2020.103065. Epub 2020 Dec 14. PMID: 33333419.
Betzler F, Helbig J, Viohl L, Ernst F, Roediger L, Gutwinski S, Ströhle A, Köhler S. Drug Checking and Its Potential Impact on Substance Use. Eur Addict Res. 2021;27(1):25-32. doi: 10.1159/000507049. Epub 2020 Jun 12. PMID: 32535605; PMCID: PMC7845440.
BTNX (2023). "Rapid Response Fentanyl Test Strip (Liquid / Powder)." Available at:
https://www.btnx.com/files/HarmReduction/Instructions%20(EN)%20H10110336601-FYL-18S7100%20FYL-18S7-10.pdf
BTNX (2023). “Rapid Response Xylazine Test Strip (Liquid/Powder).” Available at:
https://www.btnx.com/files/HarmReduction/Instructions%20(EN)%20H10110397901-XYL-18S2100%20&%2010.pdf
BTNX (2023). “Rapid Response Benzodiazepine Test Strip (Liquid/Powder).” Available at:
https://www.btnx.com/files/HarmReduction/Instructions%20(EN)%20INS02_1-BZO-18S3-100.pdf
Canadian Agency for Drugs and Technologies in Health. (2023, July 17). Xylazine test strips for drug checking. CADTH.
https://www.cadth.ca/xylazine-test-strips-drug-checking
44
Canadian Centre on Substance Use and Addiction. (2023, July). CCENDU bulletin: Update on xylazine in the unregulated drug supply. https://www.ccsa.ca/sites/default/files/202307/CCENDU-bulletin-update-on-Xylazine-in-the-unregulated-drug-supply-en.pdf
Dasgupta N, Funk MJ, Proescholdbell S, Hirsch A, Ribisi KM, Marshall S. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. (2016) 17:85–98. 10.1111/pme.12907
Goldman E., et al. “Perspectives on Rapid Fentanyl Test Strips as a Harm Reduction Practice Among Young Adults Who Use Drugs: A Qualitative Study.” Harm Reduction Journal 16, no. 3 (2019). https://harmreductionjournal.biomedcentral.com/track/pdf/10.1186/s12954-018-02760.pdf.
Goodman-Meza D, Arredondo J, Slim S, Angulo L, Gonzalez-Nieto P, Loera A, et al. Behaviour change after fentanyl testing at a safe consumption space for women in Northern Mexico: a pilot study. Int J Drug Policy. 2022;106:103745. doi: 10.1016/j.drugpo.2022.103745.
Green TC, Park JN, Gilbert M, McKenzie M, Struth E, Lucas R, et al. (2020) An assessment of the limits of detection, sensitivity and specificity of three devices for public health-based drug checking of fentanyl in street-acquired samples. Int J Drug Policy (Internet). 2020;77:102661. https://doi.org/10.1016/j.drugpo.2020.102661.
Health Canada. (2022, March 14). Exemptions from provisions of the Controlled Drugs and Substances Act. Canada.ca. Available at: https://www.canada.ca/en/healthcanada/services/health-concerns/controlled-substances-precursor-chemicals/exemptions.html
Johns Hopkins Bloomberg School of Public Health. Fentanyl overdose reduction checking analysis study [internet]. Johns Hopkins Bloomberg School of Public Health; 2018 Feb. Available from:
https://americanhealth.jhu.edu/sites/default/files/inlinefiles/Fentanyl_Executive_Summary_03201 8.pdf
Klaire S, Janssen RM, Olson K, Bridgeman J, Korol EE, Chu T, Ghafari C, Sabeti S, Buxton JA, Lysyshyn M. Take-home drug checking as a novel harm reduction strategy in British Columbia, Canada. Int J Drug Policy. 2022 Aug;106:103741. doi: 10.1016/j.drugpo.2022.103741. Epub 2022
Jun 4. PMID: 35671687; PMCID: PMC9970175.
Koning RPJ, Benschop A, Wijffels C, Noijen J. Visitors of the Dutch drug checking services: profile and drug use experience. Int J Drug Policy. 2021;95:103293.
https://doi.org/10.1016/j.drugpo.2021.103293.
45
Krieger MS, Goedel WC, Buxton JA, Lysyshyn M, Bernstein E, Sherman SG, et al. Use of rapid fentanyl test strips among young adults who use drugs. Int J Drug Policy. 2018;61:52–58. doi: 10.1016/j.drugpo.2018.09.009.
Laing MK, Ti L, Marmel A, Tobias S, Shapiro AM, Laing R, Lysyshyn M, Socías ME. An outbreak of novel psychoactive substance benzodiazepines in the unregulated drug supply: Preliminary results from a community drug checking program using point-of-care and confirmatory methods. Int J Drug Policy. 2021 Jul;93:103169. doi: 10.1016/j.drugpo.2021.103169. Epub 2021 Feb 22. PMID: 33627302.
Larnder, A., & Burek, P. (2021, March 4). Benzodiazepines, Etizolam and the Test Strips. Substance Drug Checking. https://substance.uvic.ca/blog/benzodiazepine-strips/
Lockwood, TL.E., Vervoordt, A. & Lieberman, M. High concentrations of illicit stimulants and cutting agents cause false positives on fentanyl test strips. Harm Reduct J 18, 30 (2021). https://doi.org/10.1186/s12954-021-00478-4
Maghsoudi N, Tanguay J, Scarfone K, Rammohan I, Ziegler C, Werb D, et al. Drug checking Services for People who use Drugs: a systematic review. Addiction. 2021
Marshall K. Fentanyl Test Strip Pilot Factsheet. (2018). DOPE Project Available at: https://harmreduction.org/issues/fentanyl/fentanyl-test-strip-pilot/
National Harm Reduction Coalition. (2020, October 5). Fentanyl test strip pilot. Harm Reduction. https://harmreduction.org/issues/fentanyl/fentanyl-test-strip-pilot/
Olson K, Young S, Klaire S, Janssen R, Bridgeman J, Korol E, Jedrzejowski H, Payan S, Chu T, Ghafari C, Buxton J, Lysyshyn M. (2019). Take Home Drug Checking in British Columbia. Public Health Association of British Columbia’s Annual Conference & AGM. Available at: https://phabc.org/wp-content/uploads/2019/11/BCCDC-Research-Week-Poster-FTS-Pilot.pdf
Park JN, Frankel S, Morris M, Dieni O, Fahey-Morrison L, Luta M, et al. Evaluation of fentanyl test strip distribution in two Mid-Atlantic syringe services programs. Int J Drug Policy. 2021;94:103196. doi: 10.1016/j.drugpo.2021.103196.
Park JN, Tomko C, Silberzahn BE, Haney K, Marshall BDL, Sherman SG. A fentanyl test strip intervention to reduce overdose risk among female sex workers who use drugs in Baltimore: Results from a pilot study. Addict Behav. 2020 Nov;110:106529. doi: 10.1016/j.addbeh.2020.106529. Epub 2020 Jun 27. PMID: 32683172; PMCID: PMC8214920.
Peiper NC, Clarke SD, Vincent LB, Ciccarone D, Kral AH, Zibbell JE. Fentanyl test strips as an opioid overdose prevention strategy: findings from a syringe services program in the Southeastern United States. Int J Drug Policy. 2019;63:122–128. doi: 10.1016/j.drugpo.2018.08.007.
46
Reed MK, Roth AM, Tabb LP, Groves AK, Lankenau SE. “I probably got a minute”: perceptions of fentanyl test strip use among people who use stimulants. Int J Drug Policy. 2021;92:103147. doi: 10.1016/j.drugpo.2021.103147.
Rodriguez-Cruz SE. Evaluating the sensitivity, stability, and cross-reactivity of commercial fentanyl immunoassay test strips. J Forensic Sci. 2023; 68: 1555–1569. https://doiorg.myaccess.library.utoronto.ca/10.1111/1556-4029.15332
Sherman, S. G., Morales, K. B., Park, J. N., McKenzie, M., Marshall, B. D. L., & Green, T. C. (2019). Acceptability of implementing community-based drug checking services for people who use drugs in three United States cities: Baltimore, Boston and Providence. International Journal of Drug Policy, 68, 46–53. 10.1016/j.drugpo.2019.03.003
Sherman, S.G., Park, J.N., Glick, J., McKenzie, M., Morales, K., Christensen, T., Green, T.C. (2018) FORECAST Study Summary Report. Johns Hopkins Bloomberg School of Public Health.
Shuda S, Lam H. Characterization of xylazine test strips for use in drug checking. The Center for Forensic Science Research & Education. Accessed August 14, 2023. https://www.cfsre.org/npsdiscovery/drug-checking
Sisco E, Nestadt DF, Bloom MB, Schneider KE, Elkasabany RA, Rouhani S, Sherman SG. Understanding sensitivity and cross-reactivity of xylazine lateral flow immunoassay test strips for drug checking applications. Drug Test Anal. 2023 Dec 3. doi: 10.1002/dta.3612. Epub ahead of print. PMID: 38043944.
Skov-Skov Bergh M, Øiestad, ÅML, Baumann, MH, Bogen IL (2021) Selectivity and sensitivity of urine fentanyl test strips to detect fentanyl analogues in illicit drugs. International Journal of Drug Policy , 90.
Special Advisory Committee on the Epidemic of Opioid Overdoses. (2023, December). Opioidand Stimulant-related Harms in Canada. Public Health Agency of Canada. https://healthinfobase.canada.ca/substance-related-harms/opioids-stimulants/
Swartz, J.A., Mackesy-Amiti, M.E., Jimenez, A.D., Robinson-Taylor, L., & Prete, E. (2023). Feasibility study of using mobile phone-based experience sampling to assess drug checking by opioid street drug users. Pilot and Feasibility Studies, 9:9. Online publication. https://doi.org/10.1186/s40814-023-01321-2
Tilhou AS, Zaborek J, Baltes A, Salisbury-Afshar E, Malicki J, Brown R. Association of fentanyl test strip use, perceived overdose risk, and naloxone possession among people who use drugs. Subst Use Misuse. 2023;3:1–4.
Tilhou AS, Zaborek J, Baltes A, Salisbury-Afshar E, Malicki J, Brown R. Differences in drug use behaviours that impact overdose risk among individuals who do and do not use fentanyl test
47
strips for drug checking. Harm Reduct J. 2023 Mar 28;20(1):41. doi: 10.1186/s12954-023-007670. PMID: 36978170; PMCID: PMC10053743
Tobias S, Shapiro AM, Grant CJ, et al. Drug checking identifies counterfeit alprazolam tablets. Drug and Alcohol Dependence. 2021 Jan;218:108300. DOI: 10.1016/j.drugalcdep.2020.108300. PMID: 33127185.
Weicker NP, Owczarzak J, Urquhart G, Park JN, Rouhani S, Ling R, et al. Agency in the fentanyl era: exploring the utility of fentanyl test strips in an opaque drug market. Int J Drug Policy. 2020;84:102900. doi: 10.1016/j.drugpo.2020.102900. [PubMed] [CrossRef] [Google Scholar]
48
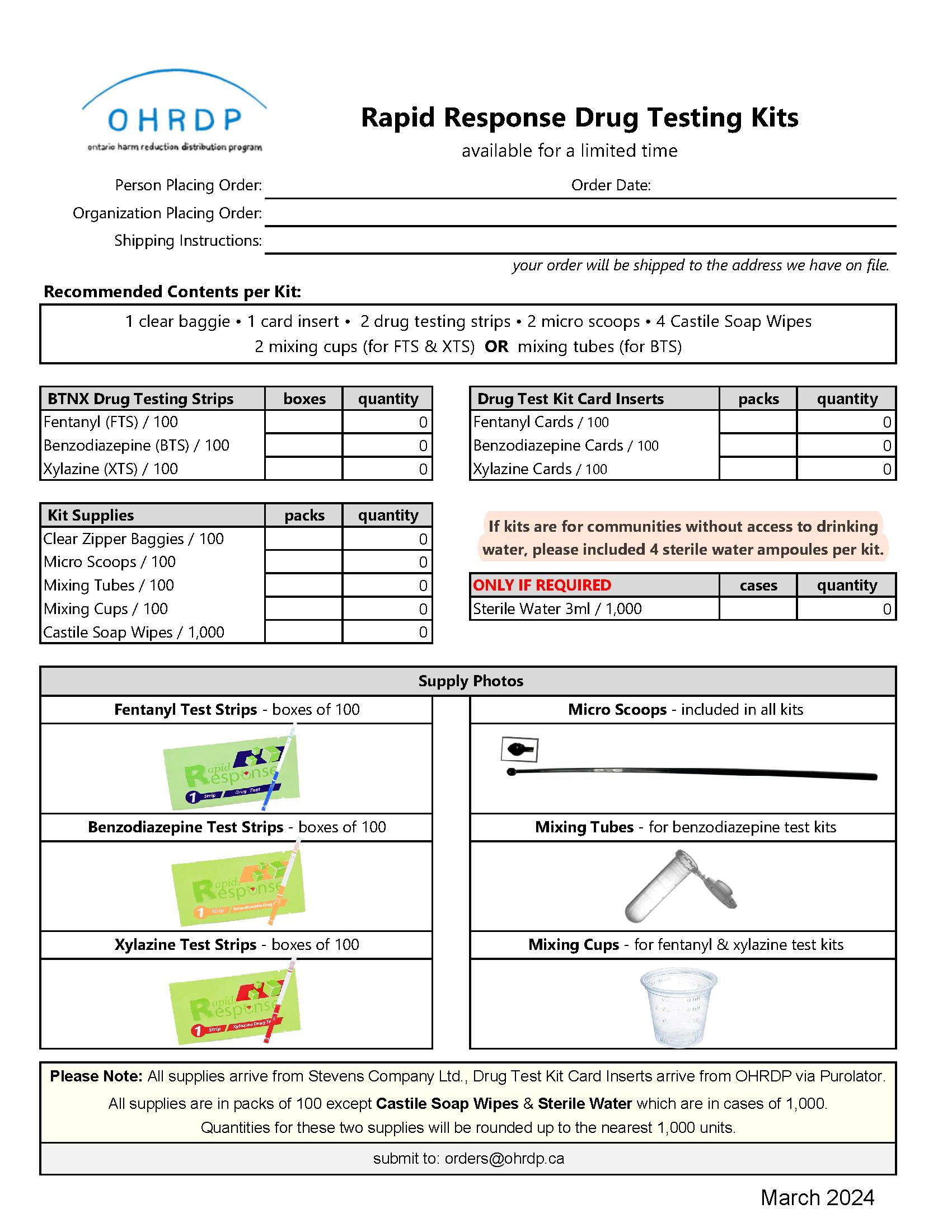
49
Appendix
OHRDP Order Form for Rapid Response Drug Testing Kits
Information and Evidence from the Toronto Drug Checking Network
Fentanyl Drug Test Strips
• Fentanyl tests strips are most valuable:
o For checking drugs that aren’t expected to be fentanyl. For example, for checking stimulants, psychedelics, dissociatives, depressants, or other opioids, like heroin, unregulated Percocet, etc. While checking drugs from the unregulated supply is always recommended, it is very infrequent that drug checking services find highpotency opioids, like fentanyl, in other drug types. When fentanyl is found unexpectedly in other drug types, there is consensus in the drug checking community that is likely the product of accidental cross contamination rather than intentional adulteration. Regardless, the unexpected presence of fentanyl in drugs poses significant health risk. Between October 2019 and December 2023, fentanyl was confirmed in less than 0.2% of 5,500 stimulant, psychedelic, dissociative, or depressant samples checked by Toronto’s Drug Checking Service. Finding fentanyl in other opioids is much more common. For example, during that same period, Toronto’s Drug Checking Service found fentanyl unexpectedly in more than one third of the heroin samples checked, as well as in samples expected to be Percocet and oxycodone (OxyContin).
o When checking fentanyl using more sophisticated drug checking technologies that cannot detect the presence of fentanyl and other drugs in trace amounts. For example, currently, the most commonly used onsite (i.e., point of care) drug checking technology for overdose prevention is the FTIR (Fournier transform infrared spectrometer). The FTIR has what is known as a limit of detection of 5%. This means that any drugs presenting in less than 5% of the sample will likely be missed by the instrument. Toronto’s Drug Checking Service has determined that fentanyl, as well as fentanyl analogues, often account for less than 5% of an expected fentanyl sample and therefore could be missed. To offset this limitation, those using FTIR couple the instrument with test strips, which have a higher likelihood of picking up drugs in trace amounts. Test strips are also strongly encouraged in combination with emerging and innovative onsite drug checking technologies whose limitations are in the process of being determined and therefore currently unknown.
• Fentanyl test strips on their own have limited value to people who intentionally use fentanyl and are at highest risk of overdose. This is because people at highest risk of overdose are often choosing to use fentanyl, therefore it is crucial that harm reduction programs
50
providing fentanyl test strips advice people who use drugs (PWUD) to employ a variety of overdose risk reduction strategies, irrespective of the outcomes provided by fentanyl test strips (FTS). The limitations fentanyl test strips for people to people who use fentanyl are:
o Inability to detect novel fentanyl-related drugs: Which fentanyl-related drugs are circulating in unregulated opioids is constantly changing. At the time of publication of this resource (spring 2024), Toronto’s Drug Checking Service had found 13 different fentanyl-related drugs in expected fentanyl samples, including 4Fluorobutyrylfentanyl (4-FBF)/4-Fluoroisobutyrfentanyl, acetyl fentanyl, bromofentanyl, butyryl fentanyl/isobutyryl fentanyl, carfentanil, fentanyl, fluorofentanyl, furanyl fentanyl, furanylethyl fentanyl, methylfentanyl, ocfentanil, valeryl fentanyl, and β-Hydroxy fentanyl. Many of these drugs cannot be detected by fentanyl test strips.
o Inability to differentiate between fentanyl-related drugs: Fentanyl test strips may be able to report if a fentanyl-related drug is present but cannot report which fentanylrelated drug is present. Knowing which fentanyl-related drug is present is crucial since their strength can vary significantly.
o Inability to report if multiple fentanyl-related drugs are present: Multiple fentanylrelated drugs are often found in a single fentanyl sample. For example, at the time of publication of this resource (spring 2024), about 50% of the expected fentanyl samples checked by Toronto’s Drug Checking Service contained more than one fentanyl-related drug. Fentanyl test strips cannot report how many fentanyl-related drugs are present in a sample.
o Inability to report the amount of fentanyl and fentanyl-related drug(s) present: Fentanyl test strips may be able to report if a fentanyl-related drug is present but cannot report the amount of a fentanyl-related drug present. Because fentanylrelated drugs are so strong, knowing how much of a fentanyl-related drug is present is crucial for attempting to reduce harm and inform dosing decisions.
o Possibility of missing fentanyl-related drugs found in trace amounts: Fentanylrelated drugs are often found in amounts that could be detected by fentanyl test strips. However, in many cases, Toronto’s Drug Checking Service has found fentanyl accounting for as little as 0.2% of an expected fentanyl sample checked. Furthermore, carfentanil generally accounts for about 0.5% of an expected fentanyl sample checked. Fentanyl test strips may not be sensitive enough to detect the fentanylrelated drugs that are present.
o Inability to detect other high-potency opioids: Other synthetic high-potency opioids are increasingly presenting in the unregulated opioid supply, including nitazene
51
opioids. Nitazene opioids were synthesized in the 1950s to relieve pain but were never clinically approved for market. They began presenting in the unregulated drug supply throughout Europe, the Unites States, and Canada around 2019. They are considered to be up to 20 times stronger than fentanyl. At the time of publication of this resource (spring 2024), Toronto’s Drug Checking Service had found 7 different nitazene opioids in expected fentanyl samples, including 5-Aminoisotonitazene, etodesnitazene, etonitazene, etonitazepyne, isotonitazene/protonitazene, etonitazene, and N-desethyl isotonitazene. Early in 2024, Toronto’s Drug Checking Service was finding nitazene opioids in about 3% of the fentanyl samples checked. That said, the presence of nitazene opioids in expected fentanyl samples can vary significantly. For example, between January and March 2022, Toronto’s Drug Checking Service found nitazene opioids in over 20% of the fentanyl samples checked. Fentanyl test strips cannot detect other high-potency opioids, like nitazene opioids.
• While fentanyl test strips should be made available to people who use fentanyl, we recommend using them when checking other opioids, stimulants, psychedelics, dissociatives, and depressants.
https://drugchecking.community/report/january-1-december-31-2022/ (page 16).
www.drugchecking.community.
https://drugcheckingbc.ca/what-is-drug-checking/overview-oftechnologies/#:~:text=The%20detection%20limit%20of%20the,sensitive%20to%20the%20target%20compound
https://drugchecking.community/#amount-of-substances-found
https://drugchecking.community/resource/fentanyl-test-strips/ www.drugchecking.community
https://drugchecking.community/resource/fentanyl-test-strips/
https://drugchecking.community/#noteworthy-drug-trends
https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-023-00911-w
www.btnx.com/files/HarmReduction/Instructions%20(EN)%20H10110397901-XYL-18S2-100%20&%2010.pdf
https://drugchecking.community/#amount-of-substances-found
https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-023-00911-w
https://www.btnx.com/files/HarmReduction/Instructions%20(EN)%20H10110336601-FYL-18S7-100%20FYL-18S710.pdf
https://drugchecking.community/#amount-of-substances-found
https://drugchecking.community/alerts/
https://drugchecking.community/#noteworthy-drug-trends
52

53
–
Safety Data Sheets
Drug Test Strips | Fentanyl

54

55
56

57
58

59 Safety Data Sheets – Drug Testing Strip | Benzodiazepine

60

61

62

63

64

65 Safety Data Sheets – Drug Testing Strip | Xylazine

66

67

68

69
Ontario Harm Reduction Distribution Program is a program of Kingston Community Health Centres, Kingston Ontario info@ohrdp.ca
March 2024

70