THE JOURNAL
of the New York State Nurses Association
VOLUME 49, NUMBER 1
n Editorial: Ordinary Essential by Anne Bové, MSN, RN-BC, CCRN, ANP; Audrey Graham-O’Gilvie, DNP, RN, ACNS-BC, CCRN-k; Meredith King-Jensen, PhD, MSN, RN; Alsacia L. Sepulveda-Pacsi, PhD, DNS, RN, FNP, CCRN, CEN; and Coreen Simmons, PhD-c, DNP, MSN, MPH, RN
n Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper by Cynthia Flynn, BA, RN, IBCLC and Audrey Graham-O’Gilvie, DNP, RN, ACNS-C, CCRN-k
n Venting the Truth About COVID-19 by Carol Lynn Esposito, EdD, JD, MS, RN-BC, NPD; Devneet Kaur Kainth, MPH, BS; and Shelly Lim, MPH, BA
n Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study by Annemarie Rosciano, DNP, MPA, ANP-C and Barbara Brathwaite, DNP, MSN, RN, CBN
n What’s New in Healthcare Literature
n CE Activities: Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper; Venting the Truth About COVID-19; Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
THE JOURNAL
of the New York State
VOLUME 49, NUMBER 1
Nurses Association
n Editorial: Ordinary Essential............................................................................................................................................................ 3 by Anne Bové, MSN, RN-BC, CCRN, ANP; Audrey Graham-O’Gilvie, DNP, RN, ACNS-BC, CCRN-k; Meredith King-Jensen, PhD, MSN, RN; Alsacia L. Sepulveda-Pacsi, PhD, DNS, RN, FNP, CCRN, CEN; and Coreen Simmons, PhD-c, DNP, MSN, MPH, RN n Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper 5 by Cynthia Flynn, BA, RN, IBCLC and Audrey Graham-O’Gilvie, DNP, RN, ACNS-BC, CCRN-k n Venting the Truth About COVID-19 .......................................................................................................................................................... 11 by Carol Lynn Esposito, EdD, JD, MS, RN-BC, NPD; Devneet Kaur Kainth, MPH, BS; and Shelly Lim, MPH, BA n Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study...................................................................................................................................................................................................... 28 by Annemarie Rosciano, DNP, MPA, ANP-C and Barbara Brathwaite, DNP, MSN, RN, CBN n What’s New in Healthcare Literature ..................................................................................................................................................... 39
n CE Activities: Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper; Venting the Truth About COVID-19; Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study ................................................................................... 43
THE JOURNAL
of the New York State Nurses Association
n The Journal of the New York State Nurses Association Editorial Board
Anne Bové, MSN, RN-BC, CCRN, ANP
Clinical Instructor New York, NY
Audrey Graham-O’Gilvie, DNP, RN, ACNS-BC, CCRN-k
Assistant Professor Mount Saint Mary College Newburgh, NY
Meredith King-Jensen, PhD, MSN, RN
Adjunct Professor Mercy College Dobbs Ferry, NY Nurse Consultant Veterans Administration Bronx, NY
Alsacia L. Sepulveda-Pacsi, PhD, DNS, RN, FNP, CCRN, CEN Registered Nurse III New York-Presbyterian Adult Emergency Department New York, NY
Coreen Simmons, PhD-c, DNP, MSN, MPH, RN Professional Nursing Practice Coordinator Teaneck, NJ
n
Carol Lynn Esposito, EdD, JD, MS, RN-BC, NPD, Co-Managing Editor
Lucille Contreras Sollazzo, MSN, RN-BC, NPD, Co-Managing Editor
Christina Singh DeGaray, MPH, RN-BC, Editorial Assistant
The information, views, and opinions expressed in The Journal articles are those of the authors and do not necessarily reflect the official policy or position of the New York State Nurses Association, its Board of Directors, or any of its employees. Neither the New York State Nurses Association, the authors, the editors, nor the publisher assumes any responsibility for any errors or omissions herein contained.
The Journal of the New York State Nurses Association is peer reviewed and published biannually by the New York State Nurses Association. ISSN# 0028-7644. Editorial and general offices located at 131 West 33rd Street, 4th Floor, New York, NY, 10001; Telephone 212-785-0157; Fax 212-785-0429; email info@nysna.org. Annual subscription: no cost for NYSNA members; $17 for nonmembers.
The Journal of the New York State Nurses Association is indexed in the Cumulative Index to Nursing, Allied Health Literature, and the International Nursing Index. It is searchable in CD-ROM and online versions of these databases available from a variety of vendors including SilverPlatter, BRS Information Services, DIALOG Services, and The National Library of Medicine’s MEDLINE system. It is available in microform from National Archive Publishing Company, Ann Arbor, Michigan.
Journal of the New York State Nurses Association, Volume 49, Number 1 2
©2022 All Rights Reserved
The New York State Nurses Association
Ordinary Essentials
The phrases, “Never again” and “Never forget” are etched on memorials to holocaust survivors and in the hearts of those whose loved ones were murdered in communities destroyed by violent conflicts. Uttered by people outspoken against genocide and oppression, the words forewarn of atrocities that can and will perpetuate unless actively thwarted. In light of Russia’s war in Ukraine, many ask, “Why again?” and “Did we forget?”
Today, so many seek a secure place to live and thrive. Ukrainians, Afghans, Central and South American people are fleeing violent conflict in their native countries. Individuals everywhere struggle against many kinds of marginalization. Many of us take for granted precious, simple things: running water, food choices, a safe neighborhood, home, family, pets, and the comfort of mundane daily routines—but these are privileges worth fighting for.
In “Venting the Truth About COVID 19,” a history of pandemic and disease repeats itself. Outraged by soldiers dying of minor wounds, Florence Nightingale challenged “the way things were done” in the Crimean War Hospital. She used objective methods to identify hazardous infectious practices, implement hygienic change, and reduce casualties. Her approaches contributed to the modernization of health care. Interplay among government bureaucracy, egotistical leaders, pathogens, greed, and human nature fueled the pandemic. The resultant cacophony of injustices are being addressed by nursing unions, which amplify the voices of nurses demanding PPE and calling for safe health practices based on truth, for OSHA worker protection, and for sound public policy in defense of vulnerable healthcare workers.
In “Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper,” the authors recognize complex barriers encountered by mothers, particularly from economically disadvantaged Black communities. Their challenge to marshal community and hospital resources through a breastfeeding sponsorship program empowers mothers to provide the best kind of nutrition available to their baby. Here, women and caregivers are cognizant of the oppressive social forces of racism and modern isolation that can distress the fragile and emotionally charged weeks of early motherhood and child life. The article demonstrates the wisdom of ages, calling upon “a village” to boldly, gently promote the strength and well-being of the next generation.
In “Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study,” it seems that young adults who were cultivated with certain gender norms and cultural pressures are predisposed to risk tolerance in their sexual lives. Given the ongoing HIV/AIDS epidemic, it is essential for young adults to make accurately informed decisions. Through screening and education, youth are supported by a caring, open campus health environment that challenges them to recognize and modify bodily and emotionally unsafe sexual practices.
We are struck by the hope, compassion, determination, and willingness of people who unite and stand to challenge oppression in order to retain what they hold dear. Healthcare workers support efforts to address building improved practices, equity in health care, and continued improvement in a sometimes-broken system. The articles in this issue reflect the invaluable nature of the ordinary; we applaud the efforts of those authors and readers who choose—and fight—to keep it.
Anne Bové, MSN, RN-BC, CCRN, ANP
Audrey Graham-O’Gilvie, DNP, RN, ACNS-BC, CCRN-k
Meredith King-Jensen, PhD, MSN, RN
Alsacia L. Sepulveda-Pacsi, PhD, DNS, RN, FNP, CCRN, CEN
Coreen Simmons, PhD-c, DNP, MSN, MPH, RN
n EDITORIAL
Journal of the New York State Nurses Association, Volume 49, Number 1 3
Breastfeeding Disparities Among Communities
Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper
Flynn, BA, RN, IBCLC and Audrey Graham-O’Gilvie, DNP, RN, ACNS-BC, CCRN-k
Acknowledgements
Christine Berté (MSMC School of Nursing Dean), Denise Garofalo (MSMC Librarian for Systems & Catalog Services),
Julia Flynn (MSMC Writing Center)
n Abstract
There is a significant difference in breastfeeding rates between Black and white infants, dependent upon their mother’s access to professional lactation care. According to the Centers for Disease Control and Prevention (CDC), 73.7% of Black infants are ever breastfed in comparison to 86.7% of white infants (Centers for Disease Control and Prevention [CDC], 2020a). The COVID-19 pandemic has complicated access to lactation care and illuminated the ongoing healthcare disparities in racial minority and economically marginalized populations across the United States. According to the CDC, some Black communities have higher rates of chronic diseases and also register lower breastfeeding rates. Research suggests that some chronic diseases can be mitigated by human milk consumption in infancy (Binns & Lee, 2019). In recognizing human milk’s value during infancy, the U.S. Surgeon General recommends access to international board certified lactation consultants (IBCLC) to support breastfeeding. Despite these government issued guidelines, data repeatedly demonstrates that hospitals lacking adequate lactation care in under-resourced Black communities continue to lack adequate distribution of breastfeeding information and lactation support.
A literature review was performed by the authors using the databases PubMed Central®, CINAHL, Google Scholar, and ProQuest. Sources include journal articles, books, websites, and reports (2012–2021). The authors used the topics related to general healthcare disparities, breastfeeding rates, and variances, as well as barriers to breastfeeding in impoverished communities in the United States. Access to lactation consultants during COVID-19 and lactation programs that address impoverished communities was also examined. The literature review consistently notes clear discrepancies in care. At a time when nationwide healthcare policies focus on preventative solutions to improve population wellness, this lack of equality in care in communities cannot be overlooked.
Nursing theorist Imogene King’s work on goal attainment may be applied to foster adaptation among interdisciplinary teams, IBCLC, and patients to increase breastfeeding rates among under-resourced Black communities. Guided by King’s Theory of Goal Attainment, this paper offers a proactive construction for an insidious public health dilemma. The purpose of this paper is to explore and disrupt inherent systematic healthcare inequities affecting Black communities by suggesting a new platform for lactation care. The application of theoretically-derived best practices will help to improve lifelong health outcomes, strengthen patient-provider relationships, and reduce healthcare spending across the lifespan of these currently underserved communities.
Keywords: professional lactation care, Imogene King Theory of Goal Attainment, breastfeeding sponsor, barriers to breastfeeding
Cynthia
Cynthia Flynn, BA, RN, IBCLC and Audrey Graham-O’Gilvie, DNP, RN, ACNS-BC, CCRN-k
Mount Saint Mary College Family Nurse Practitioner Program, Newburgh, New York
Journal of the New York State Nurses Association, Volume 49, Number 1 5
and
Background
The COVID-19 pandemic has brought to light racial disparities in health care prevalent throughout the United States. Systemic discrimination, already prevalent in many racial minority communities due to limited funding and healthcare access, has only grown more prevalent during the global pandemic. For example, according to data from New York State, Blacks and Hispanics make up 22% and 29% of the New York City landscape, yet their COVID-19-related death rates are 28% and 34%, respectively (New York State Department of Health, 2021). A review of national data indicates that counties with higher proportions of African Americans also have higher numbers of COVID-19 cases and deaths (Peek et al., 2021). However, inequalities in healthcare delivery run deeper than the pandemic statistics of the past 2 years. These inequalities have been documented extensively in the Black, Latinx, and other medically underrepresented communities for more than 120 years by government and academic researchers (Levins, 2019). In the United States, Black men are more likely to be diagnosed and succumb to prostate cancer, yet they are disproportionately underrepresented in prostate cancer screenings (Alexis & Worsley, 2018). Data from the Pennsylvania Medicaid system showed that managed care organizations’ poor performance with minority populations has directly correlated with greater racial differences within communities served (Parekh et al., 2017).
Healthcare Disparities Beginning at Birth
According to the Office of Disease Prevention and Health Promotion (ODPHP) Healthy People 2020 national objectives for improving lives, a health disparity is a health difference that is closely linked with social, economic, or environmental disadvantage (Office of Disease Prevention and Health Promotion [ODPHP], 2020). Healthcare disparities begin in infancy and impact health throughout a person’s lifespan. Breastfeeding is where this often begins. Denying an infant the basic opportunity to breastfeed, due to its racial and socioeconomic environment, is an unconscionable injustice.
When considering a range of infant feedings, nothing comes close to the multitude of benefits that human milk provides. Human breastmilk delivers the greatest number and quality of health benefits to mother and baby, which is why it is often referred to as “superfood.” For the pair, increased bonding and reduction in postpartum depression may foster healthier emotional environment early in life. Protection against infections and chronic diseases such as diabetes (type 1 and 2), obesity, and childhood and reproductive cancers also exists (American Academy of Pediatrics [AAP], 2020). Since 2012, the American Academy of Pediatrics (AAP), in recognition of these benefits, recommends breastfeeding exclusively for newborns in the first six months of life or more. It is estimated that if 90% of people breastfed according to guidelines, the United States would save more than $13 billion in health care costs per year (U.S. Department of Health and Human Services, 2020). Because science affirms breastfeeding as the superior choice for infant feeding, the U.S. Surgeon General created a call to action recommending access to international board certified lactation consultants (IBCLC) and breastfeeding support for every mother and baby (CDC, 2019).
Breastfeeding Data
Human milk is unequivocally regarded as the best nutrition for all infants. Yet, according to data from the CDC, a percentage of Black infants
are repeatedly missing this important early-stage development opportunity. Blacks historically have disproportionately higher rates of cancer, diabetes, and obesity than whites (CDC, 2017). Breastfeeding can help reduce these threats to health and wellness, and benefits of breastfeeding are lifelong. Convenient access to early intervention is the key to making and reaching breastfeeding goals.
In 2015, the CDC added several breastfeeding questions to their National Immunization Survey-Child (NIS-Child) to track the rates of breastfeeding among Blacks and non-Hispanic whites at birth, 3 months, and 6 months of age (Beauregard et al., 2019). The results of the NIS-Child revealed that breastfeeding initiation rates for Black infants were 16.5% lower than white infants of the same age. Furthermore, at 3 months of age, the consumption of any human milk for Black breastfeeding babies was 14.7% lower than for white babies. At 6 months, the disparity grew to 17.3% (Figure 1). The CDC reported that low-income families who receive the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) have lower breastfeeding rates (77%) compared with families who qualify, but don’t utilize WIC (82%) and those who do not qualify for WIC (92%) (CDC, 2020a).
Barriers to Breastfeeding
Generally, Black women who are in a low-income bracket, are less likely to breastfeed for several reasons, including language and cultural
0 10 20 30 40 50 60 70 80 90 100 % Initiated Breastfeeding % Any Breastfeeding at 3 Months % Any Breastfeeding at 6 Months 70% 71% 61% 45% Non-Hispanic White Non-Hispanic Black 59% 86%
Comparison of Breastfeeding Initiation and Continuation According to Race Note. Figure 1 shows the variation in breastfeeding rates of initiation and continuation between non-Hispanic white and Black people. Adapted from “Racial disparities in breastfeeding initiation and duration among U.S. infants born in 2015,” by J.
H. C. Hamner, J. Chen, W. Avila-Rodriguez, L. D. Elam-Evans, and C.
Perrine, 2019, Morbidity and Mortality Weekly
In the
6 Journal of the New York State Nurses Association, Volume 49, Number 1
Figure 1
L. Beauregard,
G.
Report, 68(34), pp. 745–748 (https://doi. org/10.15585/mmwr.mm6834a3).
public domain.
n Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper
Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper
barriers, and a lack of support at home, work, and within healthcare systems (Leruth et al., 2017). Disparities in breastfeeding knowledge and access to lactation care are also leading concerns causing these discrepancies. In fact, less than 25% of lower-income Black women receive information on breastfeeding from public health and social service venues. Hospitals that service low-income Black communities also report lower rates of breastfeeding initiation (Beauregard et al., 2019).
To further understand the impact that the healthcare industry has on breastfeeding rates, the CDC created the Maternity Practices in Infant Nutrition and Care (mPINC), a national survey for maternity wards meant to help hospital administrators celebrate existing strengths and target areas for improvement in their practices and policies that affect infant feeding. Every two years, the CDC invites hospitals to fill out the mPINC survey. In 2018 alone, 2,045 hospitals participated and were asked about early postpartum care practices; feeding practices; education and support of mothers and caregivers; staff and provider responsibilities and training; and hospital policies and procedures. Organized into six main areas of care called subdomains, policies and practices are then scored and comprise each state’s total mPINC score (CDC, 2020b).
Figure 2
In 2011, the CDC began correlating mPINC scores with U.S. Census data by ZIP codes to identify trends in maternity care and breastfeeding promotion and guidance equity. A CDC Morbidity and Mortality Weekly Report (Figure 2) revealed that hospitals were less likely to meet five of the 10 recommended mPINC indicators if they were in ZIP codes where the Black population was greater than the national average. The indicators included early initiation of breastfeeding (46.0% compared with 59.9%), limited use of breastfeeding supplements (13.1% compared with 25.8%), rooming-in (27.7% compared with 39.4%), limited use of pacifiers (30.5% compared with 37.9%), and post-discharge support (23.9% compared with 29.9%) (Lind et al., 2014). Survey findings revealed that the hospitals in question lacked common practices that typically promote lactation. Practices such as breastfeeding attempts in the first hour after birth, skin-to-skin contact, and avoidance of glucose water and infant formula when not medically indicated were inadequately implemented.
Often, despite the U.S. Surgeon General’s recommendations, these hospitals were not staffed with IBCLCs and/or staff training to support breastfeeding is inadequate (Beauregard et al., 2019). Research by Patel (2017) demonstrates the direct correlation between access to IBCLCs and
mPINC Scores Related to Racial Composition of Patient Populations
Served by Hospitals
Early initiation of breastfeeding: 20% of healthy, full-term, breastfed infants initiate breastfeeding within 1 hour of uncomplicated vaginal bir th.
Limited use of breastfeeding supplements: <10% of healthy, full-term, breastfed infants are supplemented with formula, glucose water or water.
Rooming-in >90% of healthy, full-term infants, regardless of feeding method, remain with their mother for at least 23 hours per day during the hospital stay.
Blacks < 12.2
Limited use of paci ers: <10% of healthy, full-term, breastfed infants are given paci ers by maternity care sta members
Blacks > 12.2 % Point Di erence
Post- discharge suppor t: hospital routinely provides three modes of post- discharge suppor t to breastfeeding mothers (physical contact, ac tive reaching out, and referrals).
Note. Figure 2 shows that as the percentage of Blacks in a population increases, the mPINC scores for the population’s ZIP code decreases. The mPINC score of a hospital is based on a 10-point survey that addresses the utilization of best practices for breastfeeding initiation and continuation. Adapted from “Racial disparities in access to maternity care practices that support breastfeeding – United States, 2011,” by J. Lind, C. Perrine, R. Li, K. Scanlon, and L. Grummer-Strawn, 2014, Morbidity and Mortality Weekly Report (https://www.cdc. gov/mmwr/preview/mmwrhtml/mm6333a2.html). In the public domain.
Note. Description of the various
0 10 20 30 40 50 60 70
%
60% 13% 27% 12% 12% 40% 11% 30% 30% 33%
%
ces of quantitati data used 48% 8% 8% 28% 38%
7 Journal
Volume 49, Number 1
of the New York State Nurses Association,
n
increased rates of initiation and continuation of exclusive breastfeeding in the first month of life. This data confirms that disparities in access to quality breastfeeding assistance exist in Black communities that are in a low-income bracket, which negatively affects breastfeeding rates.
COVID-19 Effects on Breastfeeding
The COVID-19 pandemic has further complicated infancy for new mothers. During a pandemic, as with natural crises like devastating hurricanes and earthquakes, the value of breastfeeding becomes clearer. In a state of uncertainty, human milk is one form of nutrition that mothers can count on. Families never need to concern themselves with finding substitutes in their local markets or worry that their water sources for preparation are contaminated or inaccessible. An Australian study (Hull et al., 2020) that examined the needs and concerns of breastfeeding mothers during the height of the COVID-19 pandemic found that mothers commonly expressed feelings of isolation, stress, and the need for professional lactation intervention. Many could not access their healthcare provider face-to-face, either because of fear of contracting COVID-19 or lack of appointments available, according to the study. Decreased access to care was common throughout the United States during the first surge of the pandemic.
Developing Solutions
Addressing the barriers to breastfeeding for Black women is one of the keys to improving care for future generations of families in America. The data describes variances in breastfeeding rates between Black and white infants in disadvantaged communities in the United States. According to a report by the American Civil Liberties Union (ACLU) Women’s Right Project, Black women face physical, emotional, and cultural obstacles to breastfeeding, many of the constraints owing to limited financial resources. Black women’s labor participation rate of 60.2% is higher than the rate for women of all other races. Additionally, Black women are oftentimes the primary economic support for their families, with 70.7% of Black mothers as sole breadwinners and 14.7% as co-breadwinners (Echols, 2019). Many Black women experience economic pressures that motivate them to return to the workplace earlier after giving birth than women of any other race. This paper highlights critical deficiencies found in the health systems of Black communities in low income brackets and the lack of lactation consultant programs and support. To disrupt this entrenched inequality, the authors propose an anticipatory approach, guided by Imogene King’s Theory of Goal Attainment. Now, more than ever, it is of utmost importance that all families have access to equitable resources that support the mother-baby dyad in breastfeeding and that families have access to tools to help them set and reach their breastfeeding goals.
A comprehensive support structure providing ongoing, professional guidance can help to improve breastfeeding outcomes.
Existing Models
Increased access to IBCLCs is supported by Sanchez et al. (2019). This work revealed that a comprehensive support structure providing ongoing, professional guidance can help to improve breastfeeding outcomes. Additionally, when access to health care is limited and internet service is unavailable (as is more likely the case in communities in a low-income bracket), mobile clinics are often used. However, infection control and social distancing concerns in mobile clinics arose during the COVID-19 pandemic, further complicating processes and solutions.
An excellent model for care already exists in the work done by Leruth et al. (2017). In this study, healthcare providers increased breastfeeding rates in a vulnerable population by partnering with a local hospital to provide intensive one-to-one education and ongoing support. By integrating inpatient and outpatient resources in hospitals that serve Black communities in a lowincome bracket, more mothers were enabled to breastfeed. The authors suggest combining ideas from Leruth et al.’s (2017) Chicago clinic with COVID-19 pandemic adjustments taken into consideration. We also suggest an additional level of support, guided by the Theory of Goal Attainment by Imogene King as described in the text, “Nursing Theories and Nursing Practice” by Marlaine Smith (2020). King’s theory is a framework by which providers can deliver modern, ongoing and effective care and focusing on incremental progress to be made by setting and achieving goals.
Application of Nursing Theory
King’s Theory of Goal Attainment begins with the concept of capturing the essence of nursing in the form of face-to-face transactions (Smith, 2020). The theory emphasizes the value of the nurse-patient relationship in communicating, setting goals, and moving both nurse and patient together to achieve goals. When used in an interdisciplinary setting, goals are achieved by the patient when each member of the team realizes and accepts their role and function in reaching chosen goals. Each member brings a specific purpose to the group, and individualized tasks are accomplished by the teammates according to their role and expertise. Communication within the group is ongoing, fluid, patient-centered, and it includes the patient as an active participant. This process promotes adaptation of the patient and team as one.
The Nurse Practitioner Leads a Multidisciplinary Team to Address Gaps in Care
In a breastfeeding model of care, applying King’s theory would entail exchanging information on breastfeeding and assisting the client in establishing a commitment to, and an initial goal for, breastfeeding. The process would begin during pregnancy and continue through infant weaning. As the process unfolds, further, measurable goals can be set in a stepwise or gradual fashion. Each goal should be accompanied by a means to attain the goal in the form of a nursing care plan. The care plan would be implemented using lactation resources through the hospital-based breastfeeding office, which would allow providers to capture newborns at birth.
A nurse practitioner would direct the service and be responsible for assessing, diagnosing, prescribing, admitting, and referring out the most complicated breastfeeding cases. To promote fiscal responsibility, IBCLCs and certified lactation counselors (CLC) can be utilized to reiterate breastfeeding best practices and help resolve varying levels of breastfeeding
8 Journal of the New York State Nurses Association, Volume 49, Number 1
n Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper
A breastfeeding sponsor would also function as a contemporary companion who could provide an outlet during the fragile and emotionally charged weeks of early motherhood.
challenges. This proposed service would operate out of the local hospital and push into the community in the form of home health visits. These visits would provide individualized care, be socially distanced, and also adhere to standard infection control practices. Care would begin in the third trimester of a pregnancy, and pinpointed care would occur at crucial times along the breastfeeding timeline such as at birth, in the first 2 weeks at home, during growth spurts and teething, as well as during a mother’s return to work, the introduction of solid foods, and weaning. Evaluation of the plan would occur weekly in early infancy, and as breastfeeding is further established, evaluations would continue monthly for the duration of the breastfeeding relationship.
Breastfeeding Sponsorship: A Fresh Concept
There is noted success in the literature to indicate that that peer breastfeeding sponsorship could translate for use with Black mothers to increase their breastfeeding success (Kim et al., 2017). According to the report, researchers who studied an Illinois WIC office recommended providing emotional and informational support to Black women by establishing support circles that are otherwise lacking. Adding this supportive and social aspect would contribute to increasing both breastfeeding initiation and duration rates for Black women, whose cultural background may have deterred breastfeeding. Some Black women have seen breastfeeding as reverting to “slavery days” when feeding a child by breast was the only option, according to a report in Minority Nurse (Johnson, 2016). With the introduction of baby formulas in the 1800s, campaigns led many women to believe breastfeeding was a choice only for lower-income mothers.
As an aid to addressing many of these stigmas, a breastfeeding sponsor would also function as a contemporary companion who could provide an outlet during the fragile and emotionally charged weeks of early motherhood. Mirroring other successful sponsorship programs, a one-on-one peer breastfeeding sponsor can serve as a close family member or friend for those who don’t have familial support when breastfeeding. Members of the community who have personal experience with breastfeeding can act as sponsors, thereby providing new mothers a
“chain” of support that includes a breastfeeding sponsor, IBCLC or CLC, and nurse practitioner. In keeping with the essence of King’s theory, each member in such a support team will be focused on the common goal set by the patient and her care team.
Progress, any changes, as well as the achievement of goals would be communicated within the team to allow for continued development and holistic adaptation. Professional lactation care would be accessible in the home, which will keep newborns and their mothers out of hospitals and offices and away from exposure to diseases such as COVID-19. Consideration will have been made for the use of telehealth for lactation consultations and video phone calls for sponsor support during the height of the COVID-19 pandemic, when telephones and internet services are available. A review of literature by Ferraz dos Santos et al. (2020) shows the use of telehealth as a viable option for providing lactation consultations when in-person care is not feasible. Illness and disease that are avoidable with breastfeeding could be reduced with improved breastfeeding outcomes from such measures.
Conclusion
Human milk, often touted as “liquid gold” for its beneficial health properties, is the simplest and purest of human infant needs. Although on the surface this superfood is available to all infants, data shows this isn’t always the case due to any number of factors. Applying an action-based approach to this public health call by fortifying Black communities that are in a low-income bracket with additional breastfeeding support and resources would prove beneficial in radically reducing breastfeeding and its related health discrepancies between various racial communities in the United States. Rather than relying on infant formula due to numerous environmental, cultural, and job-related obstacles, the measures discussed in this paper would support both the child’s and mother’s health, as well as a family’s financial wellness if resources focused on increased rates of breastfeeding to cut down on both formula and medical expenses. Subsidized lactation care would reduce the burden of disease due to increased adherence to the established breastfeeding guidelines. Healthcare dollars saved by decreased rates of illness could be reinvested in lactation care to allow for continued services. Applying the concepts developed originally by Imogene King allows caregivers to work as a team to help persons in need establish and meet their breastfeeding goals. Through continuous care, documentation, and evaluation of achieved goals, the proposed approach would succeed. Education and preventative, proactive work to address deficiencies in the current models of breastfeeding delivery to underserved Black communities would begin to provide equity in resources and results in breastfeeding goals as established by the CDC. Providing a structured lactation service that underscores humans caring for humans in peer networks and communities is the backbone of King’s work. Implementation of the proposals offered by this paper would enhance health and wellness for underserved black communities.
9 Journal of the New York State Nurses Association, Volume 49, Number 1
n
Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper
Alexis, O., & Worsley, A. (2018). An integrative review exploring Black men of African and Caribbean backgrounds, their fears of prostate cancer and their attitudes towards screening. Health Education Research, 33(2), 155–166. https://doi.org/10.1093/her/cyy001
American Academy of Pediatrics. (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. https://doi.org/10.1542/ peds.2011-3552
American Academy of Pediatrics. (2020). Benefits of breastfeeding. Retrieved December 1, 2020, from https://www.aap.org/en-u.s./ advocacy-and-policy/aap-health-initiatives/Breastfeeding/Pages/ Benefits-of-Breastfeeding.aspx
Beauregard, J. L., Hamner, H. C., Chen, J., Avila-Rodriguez, W., ElamEvans, L. D., & Perrine, C. G. (2019). Racial disparities in breastfeeding initiation and duration among U.S. infants born in 2015. Morbidity and Mortality Weekly Report, 68(34), 745–748. https://doi.org/10.15585/ mmwr.mm6834a3
Binns, C., & Lee, M. K. (2019). Public Health Impact of Breastfeeding. Oxford Research Encyclopedia of Global Public Health. https://doi. org/10.1093/acrefore/9780190632366.013.66
Centers for Disease Control and Prevention. (2017). African American health. Retrieved December 1, 2020, from https://www.cdc.gov/ vitalsigns/aahealth/index.html
Centers for Disease Control and Prevention. (2019). Breastfeeding: Why it matters. Retrieved December 1, 2020, from https://www.cdc.gov/ breastfeeding/about-breastfeeding/why-it-matters.html
Centers for Disease Control and Prevention. (2020a). Breastfeeding facts. Retrieved December 1, 2020, from https://www.cdc.gov/ breastfeeding/data/facts.html
Centers for Disease Control and Prevention. (2020b). mPINC 2018 National results report. Retrieved December 1, 2020, from https:// www.cdc.gov/breastfeeding/data/mpinc/national-report.html
Echols, A. (2019, August 15). The challenges of breastfeeding as a black person. American Civil Liberties Union. https://www.aclu.org/blog/ womens-rights/pregnancy-and-parenting-discrimination/challengesbreastfeeding-black-person
Ferraz dos Santos, L., Borges, R., & de Azambuja, D. (2020). Telehealth and breastfeeding: An integrative review. Telemedicine and e-Health, 26(7), 837–846. https://doi.org/10.1089/tmj.2019.0073
Healthy People. Healthy People 2020. https://www.healthypeople.gov/2020
Hull, N., Kam, R., & Gribble, K. (2020). Providing breastfeeding support during the COVID-19 pandemic: Concerns of mothers who contacted the Australian Breastfeeding Association. Breastfeeding Review, 28( 3), 25–35.
Johnson, N. (2016). African American women and the stigma associated with breastfeeding. Minority Nurse. https://minoritynurse.com/africanamerican-women-and-the-stigma-associated-with-breastfeeding
Kim, J. H., Fiese, B. H., & Donovan, S. M. (2017). Breastfeeding is natural but not the cultural norm: A mixed-methods study of first-time breastfeeding, African American mothers participating in WIC. Journal of Nutrition Education and Behavior, 49 (7). https://doi. org/10.1016/j.jneb.2017.04.003
Leruth, C., Goodman, J., Bragg, B., & Gray, D. (2017). A multilevel approach to breastfeeding promotion: Using healthy start to deliver individual support and drive collective impact. Maternal and Child Health Journal, 21(S1), 4–10. https://doi.org/10.1007/s10995-017-2371-3
Levins, H. (2019). Struggling to escape poor health: 120 Years of health disparities reports. University of Pennsylvania Leonard Davis Institute of Health Economics. https://ldi.upenn.edu/news/struggling-escapepoor-health-120-years-health-disparities-reports.
Lind, J., Perrine, C., Li, R., Scanlon, K., & Grummer-Strawn, L. (2014). Racial disparities in access to maternity care practices that support breastfeeding—United States, 2011. Centers for Disease Control and Prevention. Retrieved December 1, 2020, from https://www.cdc.gov/ mmwr/preview/mmwrhtml/mm6333a2.htm
New York State Department of Health. (2021). Workbook: Nys-covid19tracker. https://covid19tracker.health.ny.gov/views/NYS-COVID19Tracker/NYSDOHCOVID-19Tracker-Fatalities?%3Aembed=yes&%3 Atoolbar=no&%3Atabs=n%29
Parekh, N., Jarlenski, M., & Kelley, D. (2017). Prenatal and postpartum care disparities in a large Medicaid program. Maternal and Child Health Journal, 22(3), 429–437. https://doi.org/10.1007/s10995-017-2410-0
Patel, S. (2017). The effectiveness of lactation consultants and lactation counselors on breastfeeding outcomes. Journal of Clinical Chiropractic Pediatrics, 16, 1266.
Peek, M. E., Simons, R. A., Parker, W. F., Ansell, D. A., Rogers, S. O., & Edmonds, B. T. (2021). COVID-19 among African Americans: An action plan for mitigating disparities. American Journal of Public Health, 111(2), 286–292. https://doi.org/10.2105/ajph.2020.305990
Sanchez, A., Farahi, N., Flower, K. B., & Page, C. P. (2019). Improved breastfeeding outcomes following an on-site support intervention in an academic family medicine center. Family Medicine, 51(10), 836–840. https://doi.org/10.22454/fammed.2019.698323
Smith, M. (2020). Nursing theories and nursing practice (5th ed.). F. A. Davis Company.
U.S. Department of Health and Human Services. (2020). Breastfeeding: Surgeon General’s call to action fact sheet. Retrieved December 1, 2020, from HHS.gov.https://www.hhs.gov/surgeongeneral/reports-and publications/breastfeeding/factsheet/index.html
n References
10 Journal of the New York State Nurses Association, Volume 49, Number 1
n Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper
Venting the Truth About COVID-19
Carol Lynn Esposito, EdD, JD, MS, RN-BC, NPD
Devneet Kaur Kainth, MPH, BS
Shelly Lim, MPH, BA
n Abstract
Corresponding to the protestations made by Florence Nightingale more than 150 years ago during the Crimean War and in her Notes on Nursing (1960) and Notes on Hospitals (1959), this study amplifies the outcries of unionized nurses who have worked on the front lines of the COVID-19 pandemic and details their observations on the administration of nursing and the responses of healthcare organizations during the pandemic. In this article and study, we highlight key events that occurred during the pandemic that illustrate non-conformity with Nightingale’s visions for healthcare reform in the areas of organizational responses, critical thinking and problem analyses, implementation of interventions and positive outcomes, detailed documentation and statistical analysis, tenacious political advocacy to reform healthcare systems, and advancement of nursing practice based on evidence. Now, and given that the 200-year anniversary of Florence Nightingale’s birth in 2020, this article compares and explores how the appalling defects of hospitals during the Crimean War resemble and personify the appalling conditions of New York hospitals during the COVID-19 pandemic.
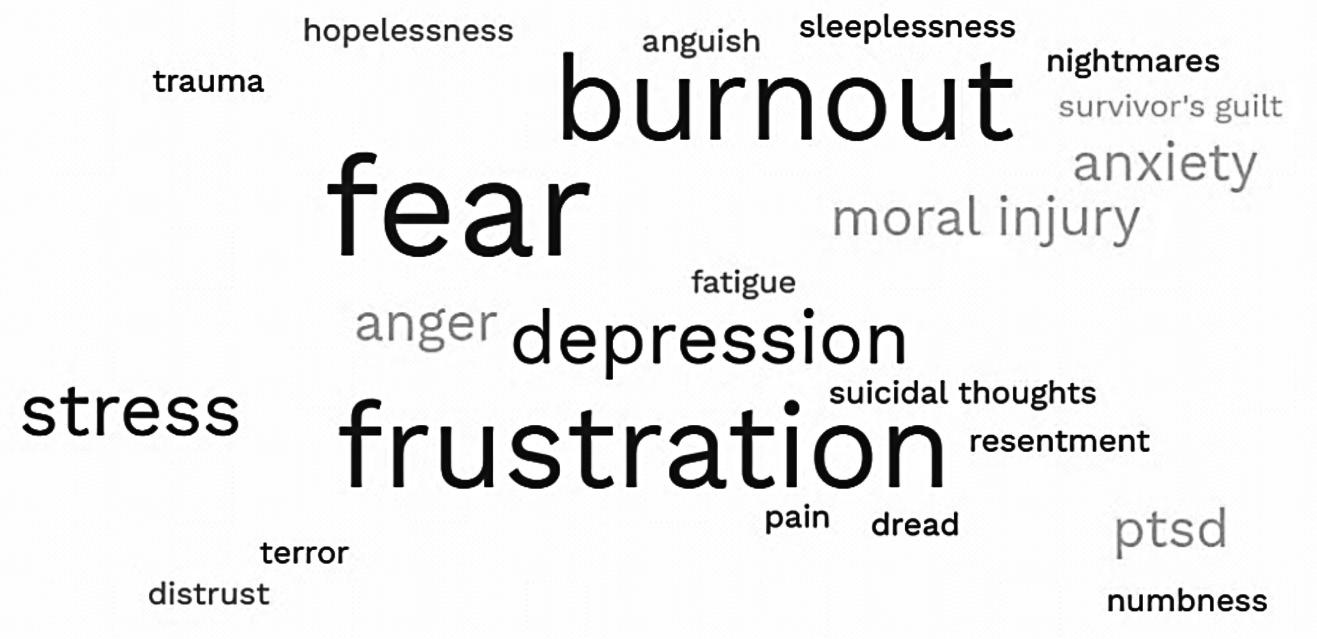
Keywords: stress, pilot study, stress-reducing intervention, work-stress impact on nurse health, contractual agreement, peer-led hospital intervention, nurse self-care
Introduction
Through her work during the Crimean War, Florence Nightingale learned the enormously important lesson that problems could be solved and high death rates brought down, even radically, when their causes were ascertained and the appropriate changes were made. Additionally, Nightingale was always conscious of the mortal risk to nurses from inferior hospital conditions and called for the incidence of deaths to be
The COVID-19 crisis unveiled many fractures in the United States healthcare system.
Carol Lynn Esposito, EdD, JD, MS, RN-BC, NPD
officially tracked, which she argued in each of the three editions of Notes on Hospitals (1959) from 1858 to 1863. In her first papers on hospitals, Nightingale identified common hospital defects, which included poor ventilation and the agglomeration of a large number of sick under the same roof (McDonald, 2020).
Background and Significance
The COVID-19 crisis unveiled many fractures in the United States healthcare system, including lack of emergency preparedness, lack of proper ventilation systems in acute care facilities, lack of personal protective equipment (PPE) for healthcare staff, lack of adequate staffing to meet the needs of the patients, cohorting of patients in inappropriate numbers and on inappropriate patient care units, distrust by healthcare staff and
Nursing Education and Practice, New York State Nurses Association, New York, New York Devneet Kaur Kainth, MPH, BS
Mailman School of Public Health, Columbia University, New York, New York Shelly Lim, MPH, BA
SUNY Downstate School of Public Health, Brooklyn, New York
Journal of the New York State Nurses Association, Volume 49, Number 1 11
the public in health officials and departments, and inequities in health determinants for minority populations. New York, the epicenter of the “first wave” of cases in the United States, was a microcosm of the devastation that resulted from the failures of the healthcare system during an emergency.
March 1, 2020, marked the first confirmed case of coronavirus disease 2019 (COVID-19) in New York State (NYS). In New York State, cases rose exponentially, reaching 76 cases by the first week of March, 613 cases by the second week, 10,356 cases by the third week, and 52,318 by the fourth week (Konda et al., 2020). By the end of the month, New York State accounted for roughly 5% of confirmed cases globally (McKinley, 2020); and by March 7, 2021, the number of positive cases of COVID-19 in New York State reached 1.7 million (Statista, 2021).
The first wave triggered unprecedented public fear and endangered the health and well-being of all people, but especially vulnerable populations. Controlling the spread of COVID-19 became a singular focus, as governmentmandated shutdowns were ordered to slow the spread of the new, highly infectious viral agent and severe acute respiratory syndrome. The pandemic precipitated social disruption, overwhelming and overly burdensome healthcare utilization, and economic instability. New York City streets became barren and ransacked grocery stores became the new “normal” for a time (Vannabouathong, et al., 2020).
COVID-19 displays a variety of clinical manifestations, ranging from asymptomatic presentation to critical illness with severe pneumonia, acute respiratory distress syndrome, respiratory failure, and/or multiple organ failure (Tsai et al., 2020). Most critically ill cases and fatalities occur in patients who are elderly, immunocompromised, and/or who suffer from comorbidities. Stark disparities in infection rates and fatalities have presented in minority populations such as Black and Hispanic communities in New York (University at Albany, SUNY, NYS COVID-19 Minority Health Disparities Team, 2020).
Moreover, long-term impacts of COVID-19, known as long, post-acute or chronic COVID illness, have been observed. Though the case definition of long COVID remains ambiguous, research suggests that one-third of patients experience symptoms that last 2–6 weeks post onset of disease, and 11–25% have symptoms that persist beyond 3 months (Alwan & Johnson, 2021). The medical community has also observed immense psychological burden on patients who suffer from COVID-19 and all those who have lived through this life-changing, traumatic pandemic (Kovner et al., 2021; Cullen et al., 2020).
As the pandemic marches on into its third year, health professionals have continued to work on the front lines to care for patients while they understand and mourn the fact that this deadly disease has no cure and the healthcare community is woefully unprepared to meet the needs of its patients or the safety needs of its practicing professionals.
Theoretical Underpinnings
Eight key components of Florence Nightingale’s work and directives for high-quality nursing that parallel registered professional nurses’ (RNs) interventions in patient care during a pandemic include:
l providing high-quality, compassionate patient care; l driving best practices based on advances in medicine and science; l implementing and monitoring of evidence-based health care;
l supporting high-quality health care for all; l understanding that health status is linked to environmental conditions that are now termed “social determinants of health”; l collaborating across disciplines in coordination of care; l advocating for the health and welfare of nurses and their work environment; and l practicing as a political advocate for changing health systems.
The role of the RN was created to meet the increasingly complex and evolving needs of patients and communities. This resembles the mission undertaken by Nightingale and her vision of nursing. The RN’s spheres of impact affect each facet in patient care, nursing and nursing practice, and healthcare systems and organizations, reflecting Nightingale’s work and beliefs about patient care, nursing standards, healthcare reform and advocacy, and training (Matthews at al., 2020).
Study Aims
The purpose of this article and study is to explore and compare how the appalling defects of the hospitals during the Crimean War resemble and personify the appalling conditions of New York hospitals during the COVID-19 pandemic.
In this article and study, we aim to highlight key events that occurred during the pandemic that illustrate non-conformity with Nightingale’s visions for healthcare reform in the areas of organizational responses, critical thinking and problem analyses, implementation of interventions and positive outcomes, detailed documentation and statistical analysis, tenacious political advocacy to reform healthcare systems, and advancement of nursing practice based on evidence.
Methods
Participants and Study Design
To assess the experience of unionized nurses during the COVID-19 pandemic, a mixed qualitative and quantitative research method approach was utilized. A mixed method approach is powerful because it encourages the synthesis of qualitative and quantitative data and, often, takes advantage of the strengths of both disciplines. However, it is an approach that lacks a standardized framework for data collection, integration, and analysis (Östlund et al., 2011). It was important for this article to capture the complexity and depth of nurses’ responses and experiences during the COVID-19 pandemic. It was equally important to assess trends in issues related to worker health and safety among the several facilities examined in this study. As such, a mixed method approach was employed.
Quantitative Data Collection
Several sources were utilized to gather quantitative data, including U.S. Department of Labor Occupational Health and Safety Administration (OSHA) employer-generated Logs of Work-Related Injuries and Illnesses (Form 300) for private sector employees; the NYS Department of Labor Public Employee Safety and Health (PESH) Logs of Work-Related Injuries and Illnesses (Form SH-900) for public sector employees; nurses’ COVID-19 daily diaries; nurses Protest of Assignment Forms (POAs); and a Nurse 2021
Journal of the New York State Nurses Association, Volume 49, Number 1 12 n Venting the Truth About COVID-19
Venting the Truth About COVID-19
Table 1
Demographics of Facilities Selected for This Study
Private hospital locations
Bronx, NY
Staten Island, NY
Somers Point, NJ Albany, NY Brooklyn, NY Flushing, NY Olean, NY Dunkirk, NY Brooklyn, NY Poughkeepsie, NY
Public hospital locations
Elmhurst, NY Valhalla, NY Buffalo, NY Bronx, NY
Long-term care facility location Buffalo, NY
Home health agency location Bronx, NY
Health department location Buffalo, NY
Correctional facilities locations
Buffalo, NY
Various NYC locations
COVID-19 Survey. OSHA and PESH injury logs were obtained via a union demand for information from 24 various healthcare facilities throughout New York State. COVID-19 daily diaries and POA forms were obtained from RNs working in New York in union hospitals and were generated voluntarily in the usual course of business and sent to the union for analysis. The Nurse 2021 COVID-19 Survey was a 34-question SurveyMonkey® survey sent via email to 44,000 unionized RNs throughout New York State. The 44,000 unionized RNs constituted a convenience sample of study population. The survey elicited 1,170 voluntary responses.
Several facilities, shown in Table 1, were selected to be highlighted in this study. These facilities constituted a convenience sample and were chosen to showcase differences in the progression of the COVID-19 crisis in New York State, taking into account variations in geographic region, COVID-19 outbreak periods, union nurse member political and concerted actions, and facility type (public/private, small/large).
The strengths and weaknesses of each data source are presented below in Table 2
Qualitative Data Collection
A convenience sample of 20 registered professional nurses working on COVID units and six nurse representatives volunteered to be interviewed by
Nurses, supported by their unions, have been at the forefront of the fight for improvements in patient care and worker safety throughout the COVID-19 pandemic.
the authors to provide firsthand accounts and insights into their experiences during the pandemic.
Nurses who volunteered to be interviewed were contacted through emails, texts, and phone calls to schedule one-on-one qualitative interviews. The interviews were conducted from June 24 to July 26, 2021, mainly over Zoom® and phone. Each interview lasted approximately 30 minutes to 1 hour. Consent was voluntary, and after consent was obtained, interviews were recorded and transcribed using the online transcript generator Otter.ai and coded using a matrix method in Microsoft Excel. The interviews were the primary form of qualitative data collected for this study.
Data analysis was conducted using Microsoft Excel and Salesforce. Tableau Desktop was used to create a map of this article’s healthcare facilities.
Results and Discussion
The following results correspond to Nightingale’s key events, which occurred during the Crimean War and that relate to events that occurred during the COVID-19 pandemic that illustrate nonconformity with Nightingale’s vision for healthcare reform (organizational responses and failures, critical thinking and problem analyses, implementation of interventions and positive outcomes, detailed documentation and statistical analysis, tenacious political advocacy to reform healthcare systems, and advancement of nursing practice based on evidence). A discussion of the results will immediately follow the reported results.
Organizational Responses and Failures
Lessons from Florence Nightingale are just as relevant today as they were more than 150 years ago. Nurses are unremittingly faced with innumerable complex healthcare delivery systems problems. While Florence Nightingale charted a path for modern nurses to become trusted and valued members of the healthcare team who employ data and evidence daily to plan patient care, our current systems of healthcare delivery are characterized by chaos and complexity. Despite a long list of health system inefficiencies that make delivering care challenging and stressful, nurses must maintain balance and ensure safe, efficient, and high-quality patient care.
This study describes nurses’ encounters with organizational and operational failures in the healthcare system that hindered timeliness of care and eroded quality and patient safety during the COVID-19 pandemic. Organizational failures fell into several broad categories: (1) lack of equipment and supplies; (2) chaotic and ever-changing communications/guidance; (3) lack of staffing; (4) inadequate training; and (5) inadequate infection control. While Nightingale identified the need for nurses to observe, assess, understand, collect data, and plan nursing care, organizational dysfunction during the pandemic and time spent on operational failures wasted
13 Journal of the New York State Nurses Association, Volume 49, Number 1
n
Strengths and Weaknesses of Study Quantitative Data Sources
Data source Description Strengths Weaknesses
OSHA and PESH Injury and Illness Logs
COVID-19 daily diaries
Standardized logs of illnesses and injuries that occur in the workplace, reported by employers, as required by the U.S. and NYS Departments of Labor.
Nurses filled out information daily about the units they worked on, number of patients in their care, staffing ratios at their facilities, and other COVID-related issues. Since 3/25/2020 an impressive 11,196 responses have been obtained.
It facilitates comparisons among workplaces because data is collected in a standardized method.
It is a rich source of data that provides insight into daily working conditions for nurses.
It is prone to underreporting because employers decide which injuries and illnesses are work-related.
It is difficult to assess validity and reliability of data, since it is self-reported by nurses.
COVID Protest of Assignment (POA) forms
Nurses submitted COVID POAs to document unsafe assignments for reasons related to unavailable personal protective equipment (PPE), lack of training, inadequate staffing, increases in patient volume, and unsafe facility protocols.
It is a rich source of data that highlights unsafe working conditions and assignments.
Request for information (RFI)
Nurse 2021 COVID-19 Survey
A union requested for information from employers. Infection rate information from 139 facilities was obtained.
It is a survey containing 34 questions related to worker health and safety, COVID-19 infection, long COVID, workers’ comp, and mental health. The number of responses obtained was 1,252.
It is a legally enforceable request that can be mandated by National Labor Bureau.
Rich source of data that assesses impact of COVID-19 pandemic on a broad range of issues for nurses.
Limitation on the generalizability of the information due to sample size, although persistence of observations increases the credibility of the qualitative data.
It is difficult to assess validity and reliability and difficult to obtain information from employers even though required by law.
Difficult to assess validity and reliability of data since it is self-reported by nurses.
Note. Description of the various sources of quantitative data used to generate this report along with strengths and weakness of each data set.
nurses’ precious time, created moral distress, and detracted from core care responsibilities (Reinking, 2020). These categories will be discussed more fully below.
Critical Thinking and Problem Analysis
Nightingale’s statistical findings indicated that most deaths during the Crimean War were due to overcrowding, poor sanitation, and improper ventilation. Her data demonstrated the merits of quality nursing care: Survival rates increased from 50% to nearly 80% under the care of Nightingale and her nurses. Attention to rigorous infection prevention, hygiene and cleanliness, nutrition and hydration, and compassionate care were integral interventions that revolutionized nursing care practices and improved clinical outcomes (Reinking, 2020).
Fast forward over 150 years to today. Although nurses are effective at identifying core operational failures in our modern healthcare system, they’re often ill-equipped and ill-resourced to complete more in-depth, system-level problem-solving. Finding solutions to the current perplexing problems in health care would require nurses to develop, maintain, and refine their critical-thinking skills. Instead, due to the nature of the work environment, nurses are forced to create workarounds and do whatever it takes in the moment to care for their patients, use trial and error to find solutions,
and only involve others who are closest work friends in problem-solving rather than counting on previously unreliable managerial or governmental resources for solutions.
Lack of Equipment and Supplies
Personal Protective Equipment (PPE). Personal protective equipment has long been used by healthcare workers to reduce disease transmission. The SARS-CoV-2 virus has been known to be detectable and viable on plastic and stainless steel surfaces and in patient rooms for hours (Stewart et al., 2020). This suggests that gowns and gloves are necessary to protect healthcare workers. Although the Centers for Disease Control and Prevention (CDC), pressured by the American Hospitals Association
Due to the nature of the work environment, nurses are forced to create workarounds and do whatever it takes in the moment to care for their patients.
Table 2
Journal of the New York State Nurses Association, Volume 49, Number 1 14
Truth About
n Venting the
COVID-19
Photo Source: Campanile & Boden, 2021. Retrieved from: https://nypost. com/2020/04/02/nurses-at-nyc-hospitalreceive-gowns-after-post-trash-bag-expose/.
and other employer groups, insisted that SARS-CoV-2 was transmitted only through contact and droplets, study after study confirmed that the virus can also be spread via airborne viral particulates (Zhang et al., 2020; Noorimotlagh et al., 2021). This means that, at a minimum, nurses and other healthcare workers should be provided with fit-tested N95 respirators (or a higher level of respiratory protection) for all patient care interactions (United States Department of Labor, Occupational Safety and Health Administration, 29 CFR 1910 Subpart I).
Based on nurses’ COVID-19 pandemic daily diaries, we compiled the responses of nurses related to the status of access to PPE at their facilities. The response options included adequate, inadequate, unsure, and blank. Of the total 65 private facilities reviewed, there were only five facilities where less than 40% of its nurses indicated that there was “inadequate PPE.” Sixty private facilities and all 24 public facilities reviewed had over 40% of its nurses respond that there was “inadequate PPE” supplies available. Some nurses indicated that they went to stores to purchase their own makeshift PPE such as overalls, gowns, and respiratory protective equipment generally used in other industries, such as construction. Several nurses resorted to wearing a black plastic bag over their uniforms (See Figure 1).
Some nurses interviewed indicated that the hospitals were not prepared for the influx of patients suffering from COVID-19 and that the scene reminded them of the casualties one might see during wartime. But
the simile does an injustice to nurses. While the COVID-19 virus might be conceptualized as an invisible enemy, it does not have any “intentions” and cannot sign a truce. Moreover, viewing hospitals as war zones and nurses as heroes who fight the virus does not constitute a fair simile, since nurses are employees of hospitals paid to do their job, but not to risk their lives, and hospitals ought to ensure that their units are safe places where security is always a primary concern (Panzeri et al., 2021).
Chaotic and Ever-Changing Communication/Guidance: Airborne Protection
Surgical masks can help decrease droplet transmission of SARS-CoV-2, but some ultra-fine viral particles can still penetrate these masks (Stewart et al., 2020). Although the CDC recommends surgical masks if respirators are not available, this should not be an excuse for healthcare employers to avoid providing respirators to its employees. The CDC alternative guidance created confusion, not only for nurses, but also for the public, regarding the use and enforcement of masks. Employers took hold of this alternative guidance, perhaps as a way to save money and supplies, and this resulted in nurses indicating on surveys that they were not given maximum PPE by their employers (See Figure 2).
Let’s be clear: Under usual and customary circumstances, the CDC and OSHA recommend N95 respirators for patient contact and aerosol generating procedures. N95s, which must be certified by National Institute for Occupational Safety & Health (NIOSH), are a type of non-powered, disposable filtering face-piece respirator (FFR), designed for protection against respirable particulates (Stewart et al, 2020). N95s are labeled as such since they are able to filter out 95% of particulates that are greater than 0.3μm in size. Nevertheless, even in the face of a pandemic crisis, N95 masks were not provided to nurses in accordance with CDC and OSHA guidance.

PPE
Figure 1 Makeshift
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Gloves Impermeable Gown Face Shield/Goggles N95 Respirator PAPR Respirator 100% 70% 69% 7% 54%
to PPE
Figure 2 Access
0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Yes No 42% 55% Are Staff currently required or will be required to reuse N95 respirators while caring for COVID
patients?
Note. Chart of survey responses for the accessibility of different types of personal protective equipment (PPE). Air-purifying respirators (PAPR) are the least accessible, and N95 respirators are the second to least accessible. Figure 3 N95 Reuse
-19
15 Journal of the New York State Nurses Association, Volume 49, Number 1
Answered 1,900 Skipped 106
n
Venting the Truth About COVID-19
Interviewee Statements Regarding N95 Reuse and Lack of Access to PPE
Nurse Interviewee Statements
“There is a lack of N95s at my facility.”
“My facility failed to ration N95s.”
“My facility did not fit test us for N95s and failed to provide us with gowns.”
“We were only given surgical masks during the height of the pandemic.”
“While caring for a ventilated, positive COVID patient with pneumonia, my manager gave me an unrecognizable N95 mask. It turned out to be a mask from a dental company. One of the straps snapped and whipped my face, exposing me to the virus.”
“Every day it seems like we are being given a different brand of N95 masks.”
“After struggling with three outbreaks since the start of the COVID pandemic, we are only just now being fitted in February 2021 for N95 masks.”
“Our hospital does not have a universal masking protocol.”
“Our hospital told us not to wear masks because it might make the patients anxious.”
“When I tried to wear a mask, my manager would question why I had one on. She would ask me if I was sick.”
“Even after my hospital was cited by OSHA for failure to provide N95 masks and failure to check mask seals, my employer continued to claim that they provided what they were supposed to for every RN.”
While many facilities have claimed that they provided adequate respiratory protection during COVID, it appears clear from the survey (Figure 3) and from interviewees (Table 3) that over 50% of nurses surveyed did not have N95 respirators and were forced to reuse their respirators, rather than having been provided the recommended N95 respirator for each patient interaction. Reusing N95 respirators can result in degraded performance, making them less effective at filtration what they are certified for (Bielcor, 2021).
Ultimately, as a result of a lawsuit filed by one nurses union against a large, public sector hospital, management was forced to borrow equipment from the Department of Health to fit test nurses and their coworkers for N95 respirators.
Inadequate Training
Work Related Injury and Illness Due to Inadequate Training: Escalating Workers Compensation. Healthcare employers owe a duty of care to their nurses. This means they must provide adequate training
Figure 4
Hierarchy of Controls
Elimination
S ubstitution Engineering Controls Administrative Controls
PPE
Note. Elimination and substitution considered the most effective of controls, whereas PPE is the least effective.
and resources to increase the safety of their employees and others involved in the day-to-day provisions of care to the public. If an employer fails to provide necessary training and safety resources, and an employee is injured as a result, the employer may be held liable for negligence. During a coronavirus pandemic, employers must provide training on physical distancing requirements; face coverings and sanitation; safe and healthy work practices and control measures; knowledge of the ability of asymptomatic individuals to transmit coronavirus; COVID-19 signs, symptoms and reporting procedures for the workplace; and quarantining/ isolating requirements. Failure to adequately train or provide safety resources can result in claims for workers’ compensation.
New York employers must carry workers’ compensation insurance to pay benefits to employees who are made ill or injured due to their employment. Nurses, who work in a healthcare environment where COVID-19 exposure risks are significantly higher than other workers, are more likely to have compensable COVID-19 workers’ compensation claims. However, underreporting of workers’ compensation cases in general has been widespread over the past decade on both the part of employees and employers.
One of the most common reasons for underreporting work comp claims is worker fear of retaliation by their employer and the potential to lose one’s job or be disciplined. Another reason for RN employee underreporting is related to perceptions of injuries as being “small” or “part of the job.” Employer underreporting compounds the issue due to corporate fear of increasing workers’ compensation costs or hurting their chances of winning contracts. The overall result is that employers now provide only a small percentage (about 21%) of the overall financial cost of workplace injuries and illnesses through workers’ compensation. Instead, the costs of workplace injuries are borne primarily by injured workers, their families, and taxpayersupported components of the social safety net (American Public Health Association, 2017).
Table 3
Journal of the New York State Nurses Association, Volume 49, Number 1 16 n Venting the Truth About COVID-19
In response to our nurse 2021 COVID-19 Survey, 70.17% of 352 nurses infected by COVID-19 while on the job did not file for workers’ compensation and 12.78% of those nurses who reported claims were told that their claims were denied. One tactic implemented by one nurses union in response to the severe underreporting of claims was to reach out to individual nurse members and to report an illness to the employer on their behalf.
Inadequate Infection Control
Hierarchy of Controls. It is essential that facilities provide appropriate PPE to healthcare workers, especially nurses. However, PPE is not enough. According to NIOSH, it is important to apply the hierarchy of hazard controls (Figure 4) in order to effectively prevent occupational exposures (CDC, 2015).
Figure 5
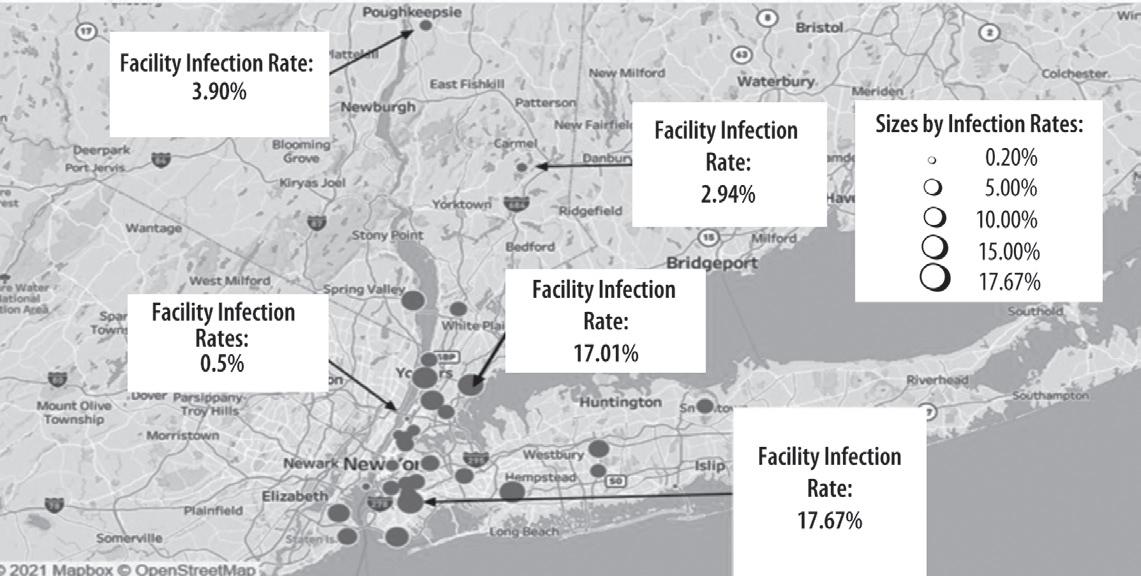
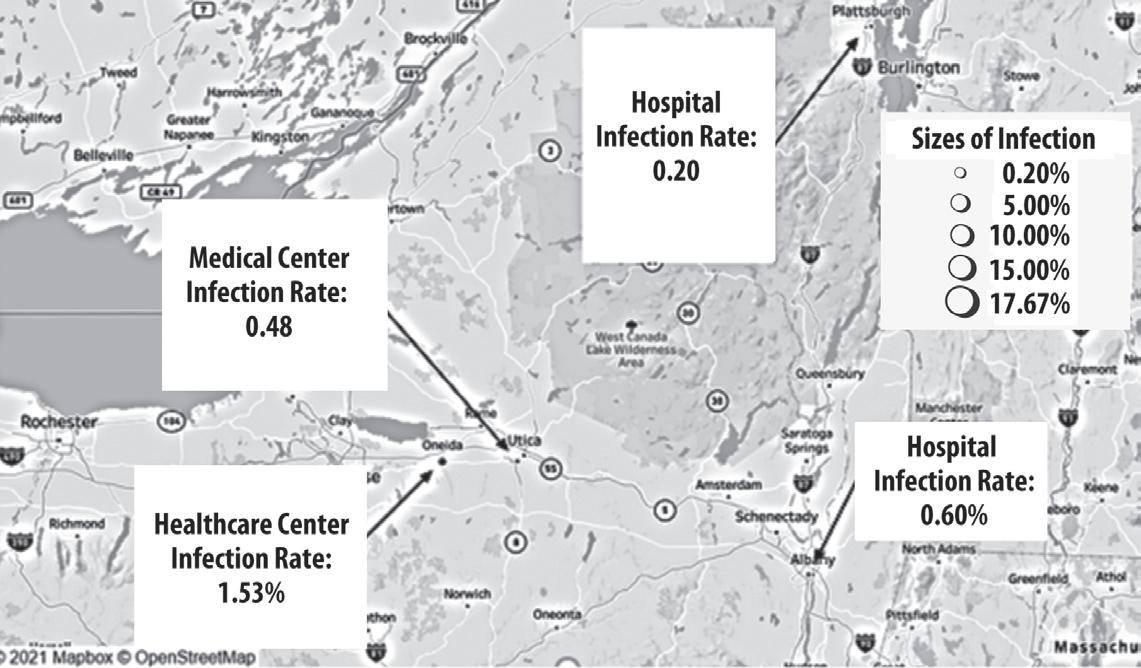
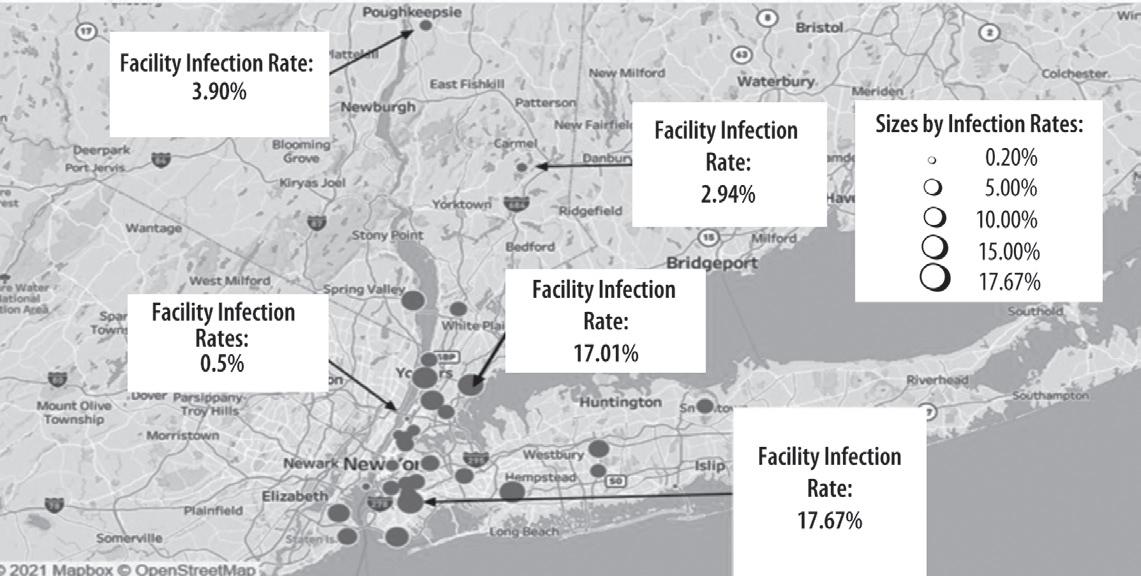
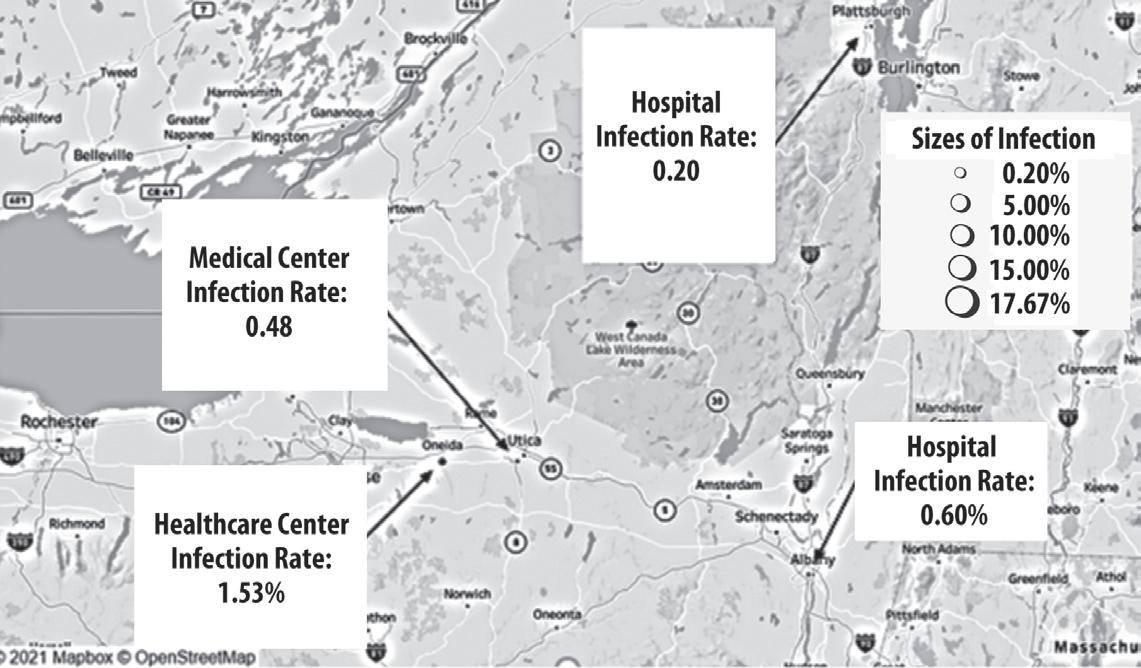
Distribution of Infection Rates of Nurses at Examined Healthcare Facilities in New York State: Top Map
Hospital Infection Rate: 0.20%
Medical Center Infection Rate: 0.48%
Healthcare Infection Rate: 1.53%
Figure 6
Sizes of Infection 0.20% 5.00% 10.00% 15.00% 17.67%
Elimination and Substitution. The Ontario Agency for Health Protection and Promotion (Public Health Ontario) created infection prevention and control (IPAC) recommendations, starting with elimination and substitution which are considered to be the most effective in the hierarchy (Public Health Ontario, 2021). Due to the Delta variant wave, the remainder of the unvaccinated within populations, and the shortage of vaccines around the world, it will be difficult to eliminate COVID-19 entirely. However, COVID-19 vaccines are effective in preventing the disease, or at least reducing the risk of COVID-19 severity. In Figures 5 and 6 (Distribution of facilities with their associated infection rates of nurses), the facilities located in the New York State Capital Region had less infection rates than facilities in other regions of New York during the first COVID-19 wave. However, the Capital Region is currently seeing the highest rate of COVID19 cases among the general population compared to the rest of New York (New York State, 2021), likely due to the region’s lower vaccination rates. Therefore, it is important to encourage more people to get vaccinated, which can help reduce transmission and also the likelihood of infection for healthcare workers.
Engineering Control Measures. Engineering measures, such as barriers between patients and healthcare workers, can help reduce the risk of exposure. Facilities should improve ventilation by utilizing airborne infection isolation rooms (AIIR) and increasing air changes in their heating ventilation and air conditioning (HVAC) systems, and improving air filtration. There should also be antechambers for changing into and out of PPE (Brosseau et al., 2021).
Hospital Infection Rate: 0.60%
Administrative Control Measures. Administrative measures include improving staffing ratios by hiring nurses or changing policies to retain current nurses. From our results, many facilities have had over two patients to one ICU nurse ratios (California’s state mandated maximum ICU ratio is 1 to 2), suggesting that there needs to be significant improvements to not only deal with the COVID-19 Delta wave, but also to prepare for the future. In addition, screening, testing, signage, and cohorting of staff and patients remain important controls (Brosseau et al., 2021), but they have been ignored by facilities. This is likely due to the incorrect assumption that, once the population is vaccinated, the pandemic will be over.
Distribution of Infection Rates of Nurses at Examined Healthcare Facilities in New York State: Bottom Map
Facility Infection Rate: 3.90%
Facility Infection Rate: 0.5%
Facility Infection Rate: 2.94%
Facility Infection Rate: 17.01%
Sizes by Infection Rates: 0.20% 5.00% 10.00% 15.00% 17.67%
Facility Infection Rate: 17.67%
Note The sizes of the points are proportional with the level of infection rates for each facility. The top of the map shows the Upstate New York region and the bottom of the map shows the Westchester/mid-Hudson Valley and Downstate regions.
Personal Protective Equipment (PPE). Although PPE should not be the only protection for healthcare workers, it is highly important that facilities maintain an adequate supply of gloves, gowns, facial and eye protection, and N95 (or higher-level) respirators. Workers should also be properly fit tested for respirators to minimize exposure. One study has described the advantages of elastomeric respirators and suggested that these are beneficial for all healthcare workers. Even half facepiece elastomeric respirators can provide respiratory protection equal to and often better than N95 respirators. Elastomerics can be safely reused multiple times and can be easily cleaned and decontaminated. Unlike N95s, elastomerics have well-established cleaning protocols. Despite being more expensive than N95s (~$20-$50), elastomeric respirators are, in the long run, less expensive than N95s (Brosseau et al., 2021). In addition, healthcare facilities should expand their use of powered airpurifying respirators (PAPRs) with hoods, as these respirators are already familiar to healthcare workers, allow the mouth to be seen by patients and staff who may be hard of hearing, and can be worn by those who cannot pass a fit test on another type of respirator (NYSNA, 2021).
17 Journal of the New York State Nurses Association, Volume 49, Number 1
About
n
Venting the Truth
COVID-19
Implementation of Interventions
Just as Nightingale experienced during the Crimean War, from PPE to staffing, nurses have struggled with various challenges throughout the pandemic. Despite their hardships, one thing remains clear: Nurses are dedicated to their work, patients, and team. They deserve the right to be treated fairly and safely and offered full protection. Nurse unions have supported their members and have helped them to raise their voices through rallies, protests, lawsuits, and more concerted actions, but more work needs to be done to win improvements for nurses.
Recommendations for Employers
Recommendation 1. Apply the hierarchy of hazard controls to improve occupational health and safety against COVID-19 for all employees in facilities.
1. Invest in engineering controls to isolate and prevent transmission of COVID-19 in workplace.
2. Enforce COVID-19 administrative controls to standardize workplace procedures.
a. Standardize and enforce procedures that comply with social distancing guidelines for triaging and cohorting patients.
b. Train nurses in evidence-based protocols for utilizing PPE, such as fit testing for N95s and donning and doffing PPE.
c. Enforce safe staffing ratios in all units.
d. Create comprehensive trainings for nursing COVID-19 patients and assess competency after trainings.
e. Limit visitation to decrease the risk of community-acquired COVID infection to enter the facility.
f. Test patients upon entry to the facility.
g. Assume patients are COVID positive until proven otherwise.
3. Invest in 90-day stockpiles of PPE, including gloves, gowns, facial and eye protection, and N95 (or higher-level) respirators.
a. Consider investment in alternative and sustainable PPE, such as elastomeric respirators and PAPRs.
b. Allow nurse representatives to view and verify 90-day stockpile.
Recommendation 2. All patient-facing staff must be provided with N95 or higher-level respirators.
1. Sufficient numbers of N95s or higher-level PPE for all staff to use as intended (single use, for each patient care session)
2. No reprocessing of N95 respirators
3. Incorporation of elastomeric respirators or elastomeric respirator programs with a sufficient supply of respirators and cartridges for key frontline staff to use during pandemic surges or other emergency situations
Recommendation 3. Create a working group of administrators, managers, and frontline nurses that meets regularly to facilitate communication and collaboration regarding unsafe working conditions and other nursing concerns. Involve nurses in decision-making meetings and processes.
Recommendation 4. Open units that were closed during the pandemic, such as psychiatric services.
Recommendation 5. Provide all employees with free, independent, and accessible mental health resources.
Recommendation 6. Prioritize the retention of experienced nurses.
1. Offer COVID-19 pay to nurses who worked throughout the pandemic.
2. Recognize achievements of experienced nurses in facilities, such as the number of years in the profession or leadership roles taken.
3. Create incentives for full-time nursing staff.
4. Create and encourage mentorship programs between experienced nurses and nurses new to the profession.
Recommendations for Government
Recommendation 7. Mandate and enforce numeric safe staffing ratios for nurses in all types of facilities, similar to those enforced by California’s Department of Health Services (DHS).
Recommendation 8. Incentivize the domestic production of PPE.
Recommendation 9. Enact a permanent airborne transmissible disease standard for healthcare workers, modeled on the California OSHA standard.
Recommendation 10. Improve data collection on occupational health and safety hazards in workplaces.
1. Mandate that employers record and report all worker occupational exposures and illnesses related to transmissible diseases to a central body in real time, and make the data available to the public to ensure transparency.
2. Audit facilities to ensure the accurate and consistent reporting of hazards.
3. Create educational tools to help workers understand their rights and when and how to report unsafe conditions.
Recommendation 11. Invest in research into long COVID-19, specifically its potential disparate impacts on nurses and other healthcare professionals.
Detailed Documentation and Statistical Analysis
While NYS governors Andrew Cuomo and Kathy Hochul promulgated executive orders that eased RN recordkeeping requirements to the extent necessary in response to the COVID-19 outbreak, this directive can be juxtaposed with Florence Nightingale’s zeal for statistics, which not only saved lives during the Crimean War, but formulated the basis for today’s evidence-based practice. Nightingale’s groundbreaking work in data collection and visualization should have been replicated during the COVID19 pandemic. Data, including the composition of patient characteristics data (e.g., sociodemographic, disease severity, comorbidity); clinicianrelated factors data (e.g., center volume, patient load distribution among physicians, hospitals, and health systems); resource utilization data (e.g., intensive care unit [ICU] admission), and clinical outcomes data (e.g., patient-reported outcomes, mortality, readmissions) was lost due, in large part, to Executive Order No. 4, which declared that any RN (or other licensed practitioner) acting reasonably and in good faith would be immune from liability for failure to keep accurate records. This lessening in record-keeping responsibilities included allaying the recording and maintenance of fully accurate records, which otherwise would be required under law and evidence-based practice (New York State, 2021, September 27; Shioda et al., 2020).
Journal of the New York State Nurses Association, Volume 49, Number 1 18 n
the
Venting
Truth About COVID-19
Venting the Truth About COVID-19
COVID-19 Infection Rates in NY Union Nurses
“First-Wave” COVID-19 Infection Rates: Employer Request for Information vs. OSHA/PESH Logs
10 15 20 25 30
Note. Data regarding RN COVID-19 infection rates were obtained from employer reports and OSHA/PESH logs via union requests for information (RFI). The data was analyzed and infection rates between March 2020 and July 2020 were calculated and compared. Infection rates were calculated by obtaining the number of COVID-19 positive cases and dividing this number by the total bargaining unit member numbers. Out of the 19 facilities highlighted in this report, only nine employers fully responded to the union’s requests for information.
Although Nightingale called statistics the most important science in the world, New York limited its data collection during the pandemic. Whereas Nightingale broke new ground with her use of data, using it to understand the current state, evaluate priorities, and assess progress in improving patient outcomes, the pandemic brought abrupt changes in New York’s healthcare system. As the number of patients who sought health care during the pandemic for emergency cardiovascular conditions declined, as outcomes of certain diseases, such as cancer, worsened, and as surgical procedures were reserved for patients with emergency conditions, such changes will inevitably be reflected in the healthcare data for future research (Shioda et al., 2020).
Let’s be clear. The ability to compare data sets from different places is critical to understanding outbreaks. One of the challenges in monitoring the COVID-19 pandemic in New York has been the lack of standardized data sets for experts studying the pandemic to compare regarding the numbers and comorbidities of people infected.
Infection Rates of RNs
Nightingale was versed in the correlation between the contagion of disease and its proximity to unsanitary conditions. She emphasized sanitization and ventilation practices that led to the creation of the 1848
British Public Health Act, and implemented into practice what would become the first tenets of germ theory in disease prevention (Gill & Gill, 2005). These tenets were ignored during the COVID-19 pandemic.
Poor reporting of healthcare worker infection data has been a major issue both preceding and throughout the COVID-19 pandemic (National Nurses United, 2020). OSHA logs are notorious for poor recordkeeping due to a variety of reasons, such as business practices that incentivize low injury rates and limited communication between workers and employers (Wuellner & Bonauto, 2014).
Figures 5 and 6 show the infection rates of nurses between March and April 2020 that resulted from poor infection control and ventilation practices. This information was provided by facility employers through a union request for information (RFI). The map does not suggest a visible There were discrepancies between the data documented in the OSHA/PESH logs and the data obtained from the employer via RFIs.
Figure 7
05
Bronx
Staten
al
Upstate Medic al Center Q ueens Medic al Center Western New York General Hospital Mid-Hudson Medic al Center NYC Health + Hospitals Facility Public County Medic al Center Correc tional Health Services Infec tion
8.4 7.70 2.2 0.09 7.40 1.78 0.40 0.40 7.40 11.7 0.60 2.8 12.60 11.4 0.13 8.4 3.90
19 Journal of the New York State Nurses Association, Volume 49, Number 1
Medic al Center
Island Medic
Center
Rate from RFI Infec tion Rate from OSHA/PESH Logs 28.4
Number of c ases per bargaining unit member
n
difference in infection rates between the different regions across New York City. The map does denote two 250–300 bedded facilities in the lower New York region that had the highest infection rates, whereas one 900 bedded facility in the lower New York region and one 300 bedded facility in the upper New York region had the lowest infection rates.
As can be observed in Figure 7, there were discrepancies between the data documented in the OSHA/PESH logs and the data obtained from the employer via RFIs relative to the COVID-19 infection rates for nurses. The largest discrepancy was observed in correctional health data; however, the issue was persistent across public and private facilities. These discrepancies highlight the lack of reliable data on occupational health and safety hazards in healthcare workplaces. The reporters had difficulty in accessing data in 10 of 19 facilities.
Tenacious Political Advocacy for the Health and Welfare of Nurses Within Their Work Environment Inconceivable Lack of Staffing
Nightingale worked at the Scutari Hospital during the Crimean War under grueling circumstances, up to her neck in infectious risks, with little-to-no staff, much as healthcare workers have been doing during the coronavirus pandemic. Like many nurses today who are rapidly becoming infected with COVID-19 from working conditions, Nightingale fell ill shortly after arriving to Crimea with brucellosis, otherwise known as “Crimean fever.”
Contagious illnesses like COVID-19 bring into stark relief the fact that there are many stakeholders who are accountable to the health of a community and its constituents, and who are a part of the equation that adds up to social determinants of health: the hospital, the nurse, the patient, and the population. Nightingale asserted that the entire healthcare team should be held accountable for safe, high-quality care and that every stakeholder in the healthcare system contributes to quality and safety. There is no doubt that the COVID pandemic strained our system’s resources, supplies, communications, and delivery of medical care.
Staffing Shortages During the Pandemic
Nurses are employed in a variety of settings, from traditional hospitals to correctional health centers and in a variety of clinical practice areas, such as emergency units, behavioral health units, labor and delivery units, surgical units, and maternal child units. In response to the clinical needs of the COVID-19 patient, facilities were required to set up new units such as COVID ICUs, COVID step-down units, and COVID medical units. The resilience of hospitals to pandemic cases depends on the preparedness of the institutions, and not all hospitals have the same resilience. A lower resilience will affect the sustainability of a hospital’s health services. Likewise, the resilience of nurses to the patient who is admitted during a pandemic depends on the competencies of the individual nurse and the acuity level of the patient (Al Thobiaty & Alshammari, 2020).
Considering the fact that nurses constitute the majority of healthcare providers, they have a critical function in healthcare systems. During a pandemic, nurses must be well-equipped with essential knowledge and skills in managing crises involving clinical treatment, decontamination, isolation, communication, triaging, psychological support, and palliative
care if necessary. Thus, nurse-to-patient ratios are an important variable influencing the outcome of the acutely ill patient.
For decades, nurses around the world have struggled with understaffing and meeting the demands of their profession. Nurse understaffing has been associated with increased risk of healthcare-associated infections in patients (Cimiotti et al., 2012). Shortages of registered professional nurses can lead to missed care, poorer quality of patient experience, and poorer medical education for patients (Cho et al., 2020). The enormous numbers of nurses who became sick with COVID-19, who had to quarantine at home, or who became hospital patients themselves has further exacerbated the nursing shortage. The pandemic has aggravated this situation as many national nurses associations (NNA) have reported the following (International Council of Nurses, 2020):
l Ninety percent of NNAs are concerned that heavy workloads and insufficient resourcing, burnout, and stress related to the COVID19 pandemic response are the drivers resulting in increased numbers of nurses who have left the profession, and increased reported rates of nurses’ intention to leave this year and when the pandemic is over.
l Twenty percent of NNAs reported an increased rate of nurses leaving the profession in 2020, and studies from associations around the world have consistently highlighted increased rates of nurses’ intention to leave.
l Due to existing nursing shortages, the aging of the nursing workforce, and the growing COVID-19 effect, the International Council of Nurses estimates up to 13 million nurses will be needed to fill the global nurse shortage gap in the near future.
Determining nurse-to-patient ratios in New York State healthcare centers has been the subject of collective bargaining and demands for legislative action in recent decades. A plethora of research has supported the notion that nurse-to-patient ratios are one of the most important factors in providing quality care and achieving optimal patient outcomes, and particularly so during the COVID-19 pandemic (Lasater et al., 2021a; Lasater et al., 2021b; McHugh et al., 2021). Nevertheless, New York hospitals and the New York State Legislature have never agreed to institute across-theboard nurse-to-patient ratios, and research indicates that just before the COVID-19 pandemic, staffing in medical-surgical units varied from 3.3–9.7 patients per nurse, with the worst average mean for staffing being in New York City. Hospital nurses were burned out and working in understaffed conditions in the weeks prior to the first wave of COVID-19 cases, which posed increased risks to the public’s health. Such risks could be addressed by safe nurse staffing policies (Lasater, et. al, 2021b). Currently, California is the only state to have patient to nurse staffing standards required by law.
Staffing Ratios in New York ICUs
ICUs host the most acutely ill patients and are prepared to provide concentrated cardiovascular and respiratory monitoring, mechanical ventilation, and artificial life support. The recommended nurse-to-patient ratio in ICUs, based on California State standards, is one nurse to two patients. Step-down units are a transition between ICU and general nursing for patients who require close monitoring by expert staff. The recommended nurse-to-patient ratio for step-down units, based on California State standards, is one nurse to three patients. Medical units are for patients
Journal of the New York State Nurses Association, Volume 49, Number 1 20 n Venting the Truth About COVID-19
recovering from surgery or acutely ill medical conditions. The recommended nursing ratio, based on California State standards, is one nurse to five patients (National Nurses United, n.d.; Health Facilities: Nursing Staff Act, Cal. Assemb B 394 [1999-2000]). Throughout the COVID-19 pandemic, many of these ratios were disregarded by employers and extremely unsafe staffing ratios were reported in the POAs that were filed by New York nurses (NYSNA, 2021a).
POA forms are used by nurses to notify their employers and the union of unsafe conditions for either patients, nurses, or both. Issues reported on COVID POA forms included, but were not limited to, inadequate RN staffing, inadequate PPE, inadequate training, inadequate testing and screening of patients and/or staff, and inadequate access to needed supplies. Nurses reported on their 2020 COVID POAs patient-to-nurse ratios as high as 4.5 for ICUs and 9.5 for medical-surgical units. One ICU nurse employed at a NYC H+H hospital said that his worst assignment consisted of four critically ill ICU patients. Most nurses agree that the ideal nursing ratio in the ICU, particularly during the COVID outbreak, should be one patient to one nurse, or, maximally, two patients to one nurse (Anders, 2021). The California ICU patient-to-nurse safe-staffing ratio is currently two patients to one nurse (National Nurses United, n.d.).
When nurses fought for increased staffing in March 2020, their employers tried to recruit outside nurses who had ICU experience and encouraged retirees to come back. Additionally agency nurses from all around the United States were solicited. However, these recruits ended up being a “blessing and curse,” since not all of the nurses temporarily hired by New York employers had ICU experience. One New York nurse expressed that it was a difficult experience because the inexperienced temporary nurses were only provided a basic crash course in the care of ICU patients, as were many of the New York nurses who were floated from their motherbaby, behavioral health, and labor and delivery nursing specialty units to temporary, makeshift COVID medical and ICU units (Aziz et al., 2020).
In our study, the nurse-to-patient ratios in New York hospital ICUs were compared with the infection rates of nurses in 2020 to determine a possible correlation. In Figure 8, which compares infection rates, public facilities are marked with an arrow and private facilities are marked with a solid dot. Although there was not a significant statistical difference, private facilities displayed a greater range in ICU nurse-to-patient ratios than that of public facilities. Many factors, including the drive for profits, may have contributed to these differences. This factor may suggest that nurses employed in private facilities may be exposed to poorer staffing ratios.
In an interview, one nurse who works in homecare, states she used to have a good experience when her employer was a not-for-profit agency. When it was converted to a for-profit agency, the management began cutting assigned patient care hours per client. Aides, who had formally been assigned to work three shifts for one patient, were limited to one shift. This change hurt the patients who needed total care around the clock. Management continued changing policies and procedures without much input from the nursing staff, which led to frustrated nurses who, in turn, left the homecare workforce.
“They lay off all the union aides,” one interviewee stated, “and the feeling is that they don’t want a union representing nurses any longer.” Many of the nurses at this facility had resigned or retired after struggling with heavy caseloads and responsibilities from the pandemic. Yet, this facility was expanding its ZIP code eligibility to cover almost every area of the Bronx.
Figure 8
ICU Staffing Ratios Compared to Nurse Infection Rate
Infec tion Rates R Members in 2020 vs Patientto -Nurse Ratios in Intensive Care Facility
Infec tion Rates of Nurses for Each Fa cilit y Facilities Private Public
0 0.5 1.0 1.5 2.02.5 3.03.5 0.00% 2.00% 4.00% 6.00% 8.00% 10.00% 12.00% 14.00% 16.00% 18.00% 20.00%
ICU Patient-to -Nurse Ratio
Note: Sta ng ratios in home care diminish during COVID.
y = 0.01x + 0.05 R2 = 0.01
Deficiencies in the Provision of Mental and Emotional Support
Nightingale believed not only in the importance of good hygiene and adequate nutrition, but also helped improve the emotional health of soldiers by writing letters home for them. As an eminent and natural problemsolver, we can only imagine how Nightingale would respond to transform today’s trends around how the mental and emotional well-being of nurses are handled.
Research has shown that healthcare professionals are at a significant risk of experiencing negative mental health impacts from stressful workplaces. For nurses, stressors such as understaffing, high workloads, and intense emotional labor have been linked to high anxiety, depression, and burnout (Jenkins & Elliot, 2004). Work-related stress is intensified by a lack of control in the workplace, since nurses are often excluded from decision-making processes by facilities. The COVID-19 pandemic has not only increased the presence of workplace stressors, but also the resulting mental burden on nurses.
In the 2021 Nurses COVID-19 Survey, 93.2% of respondents reported that pandemic working conditions had an impact on their mental health, with 43.5% citing the pandemic as having a “major impact” on their mental health. This finding was further investigated through in-depth interviews with 20 nurses. After inquiring about mental health, the top five most commonly reported symptoms were fear, frustration, stress, burnout, and depression, as depicted in Figure 9.
Fear
Fear was consistently expressed by nurses from all facilities. One emergency department (ED) nurse described her debilitating fear. She saw “seasoned nurses and newer nurses...waiting in their cars, crying in their cars, terrified to come into the job that would not provide what they needed (to protect themselves).” Lack of preparation for the COVID-19
21 Journal of the New York State Nurses Association, Volume 49, Number 1
n
Venting the Truth About COVID-19
Figure 9
Figure 10
on the Mental Health of Nurses
Impact of COVID-19 Pandemic
Pressure to Return to Work
Among the long-COVID nurse respondents, how many of them feel pressure to return to work before their symptoms are gone?
67 (34%)
Note. In-depth interviews were conducted with 20 nurses and seven nurse representatives, in which interviewees were asked about the impact of the COVID-19 pandemic on their mental health. Results were coded and this word diagram was created using an online word cloud generator (www.freewordcloudgenerator.com). The top five most commonly reported symptoms were fear, frustration, stress, burnout, and depression.
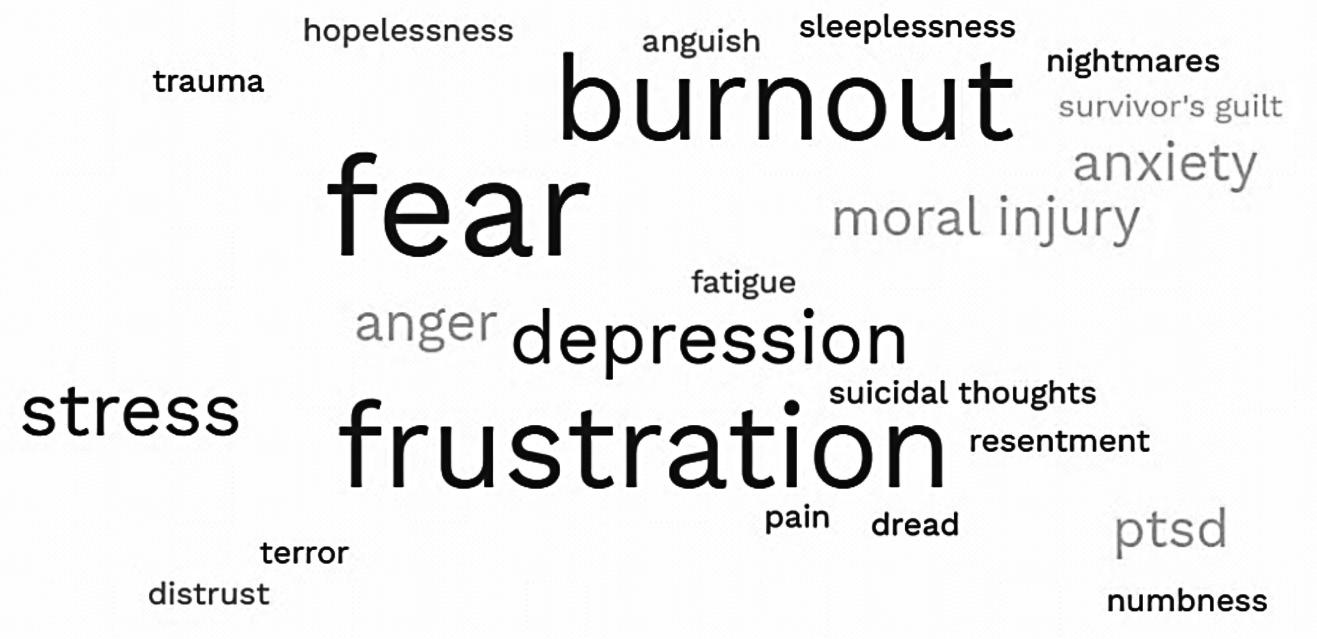
surges resulted in chaos, which left nurses without the necessary resources, training, or testing to appropriately care for COVID-19 patients. They were not only scared of failing their patients daily, but also contracting the virus themselves and bringing it home to their families.
Nevertheless, even in the face of fear, nurses heeded the call to action and duty to serve. As commented upon by one nurse representative, while most people were going into their homes and locking their door “the overwhelming majority of nurses wanted to run into this pandemic to help. [Nurses] were running into the fire, versus running away from it.” Despite their fears, to this day, nurses continue to work on the front lines of the pandemic.
Frustration and Stress
Nurses continue to experience constant frustration and persistent stress due to a lack of support from their facility administration and management. They shared troubling stories of N95 masks being removed from their faces, orders to reuse PPE for unsafe periods of time, and monthslong assignments worked without comprehensive training or support caring for COVID-19 patients. They grappled with constantly changing clinical information, the spread of misinformation, and a lack of standardized protocols from hospital administration and the government. These conditions were especially frustrating in COVID-19 medical-surgical units and ICUs. As one nurse had described it:
It was basically a disaster. None of the ancillary staff would enter the units to help us with anything...so, we were doing everything ourselves. We had 5-minute crash courses on how to start an IV, how to draw bloods, how to do our own EKGs, how to load our own pyxis, and how to stock the storeroom. It got to the point where we were cleaning our own floors.... We were having a lot of issues with dietary, who wouldn’t come in to pass out, take, or remove the trays....
Note. Pie chart of survey responses among the nurses who had reported experiencing long COVID symptoms and who had felt pressure to return to work after their acute symptoms ended. The number and the percentage of the responses are shown in order. There was 1 blank response included in the total. Among the long COVID nurses, nearly a third had reported that they had felt pressured to return to work when their acute symptoms were gone, even though they were experiencing long COVID symptoms.
They changed the way we donned and doffed PPE. It was so wrong that I personally felt it left everybody at much more risk of exposure.... There was no good algorithm of care for the patients. And, once my manager and I developed one, it was almost like nobody cared.... Initially, staffing was good for the first wave, but by the second wave it was trash. We were taking care of six or seven COVID patients each, which is completely unsafe. Meanwhile, we were taking two to three to four in the first wave.
This horrific account sheds light on the increased presence and intensity of workplace stressors that nurses experienced during the COVID19 pandemic. They have worked long and intense hours with insufficient training, inappropriate resources, and inadequate staffing ratios. Unsafe work conditions and severe overburdening have led to prolonged frustration and stress for months on end.
Burnout and Depression
Unsurprisingly, many nurses are experiencing burnout and depression from the trauma of the COVID-19 pandemic. This has come from the increased amount of workplace stressors, along with the volume and acuity of COVID-19 patients seen during the initial surge. As one of the nurses interviewed said:
The ICUs were awful. They were windowless. Every patient, usually between 9 to twelve patients, was typically on a ventilator.... It was just
128 (65%) 1 (1%) Yes No Blanks
Journal of the New York State Nurses Association, Volume 49, Number 1 22
n Venting the Truth About COVID-19
Figure 11
Diagram of Long COVID-19 Symptoms
in nurses. Nurses have seen the deaths of patients their age and their children’s ages. They have seen the deaths of their coworkers and loved ones. A major stressor for nurses has not been just bearing these emotional burdens, but also not being able to perform their jobs appropriately and with dignity, as they had been trained to do so for years. Some continue to experience burdens beyond burnout and depression, ranging from post-traumatic stress disorder (PTSD) to suicidal thoughts. It has been a continuous, traumatic process that nurses continue to shoulder out of fidelity to their profession.
Long COVID and Pressure to Return to Work
The consequences of understaffing can be far-reaching. Nearly a third of nurses who are reported to have experienced or are experiencing long COVID symptoms feel pressure to return to work before their symptoms are gone (Figure 10). New York State and local governments wanted staff back at work to care for the increasing COVID-19 patient load. Some nurses have even described in our interviews instances where their managers consistently called sick workers at home to pressure them to return to work. One nurse described their concern for their coworkers as well as the stress of understaffing saying, “Nurses, especially sick nurses with long COVID symptoms, deserve the time to rest, but understaffing makes it difficult for them.”
Note. In-depth interviews were conducted with 20 nurses, in which they were asked if they were infected with SARS-CoV-2 and experienced long COVID-19 symptoms. The symptoms, along with two direct quotes, were incorporated into a diagram that was created using an online figure generator (www.BioRender.com).

nurses, wrapped up in plastic and barely recognizable, moving from one silent bed to another where patients were just in a row, on machines, with every type of machine possible performing every function for them.... We never saw death on this scale before and death where we were the only ones with them. You’re not just the nurse when it comes to the COVID patient. You’re there as surrogate family, the surrogate friends, and I think that’s what got to a lot of nurses.
Throughout the COVID-19 pandemic, nurses have cared for an endless number of acutely ill patients, often until their final hours. The direct emotional burden has been exacerbated by lack of support at facilities. Many nurses felt that poor working conditions made it impossible for them to adequately care for patients, leading to moral distress and intense guilt, as outlined by one interviewee:
We lost about 60 people to COVID during the whole thing, but we lost so many more people this year. The fact that they couldn’t have visitors, the fact that our staffing had been so poor. We didn’t have staff to get people out of bed. A lot of times, we didn’t have ample people to feed residents. We were feeding everybody, but were rushing those meals. All my sickest people didn’t make it through this year, people who had been in my nursing home 10 years.... And there were more than a couple days when I’d be driving to work and I would, not intentionally, think, “Boy, you know, if I got in a car accident today, I wouldn’t have to go in.”
The devastating working conditions over the past year have caused severe depression, burnout, and even more serious mental health conditions
A lasting impact of the COVID-19 pandemic is long COVID illness. In our report, long COVID illness is defined as symptom(s) lasting more than 2 months past acute COVID-19 illness. In the 2021 Nurses COVID-19 Survey, 55.8% of nurses infected with SARS-CoV-2 experienced long COVID symptoms. Additionally, 28.9% of nurses reported needing more than 20 days off of work due to their illness, which could be used as a measure of disease severity. Long COVID was also assessed in the qualitative interviews. Of the 20 nurses interviewed, four nurses reported long COVID symptoms. Figure 11 includes the range of long COVID symptoms reported by the four nurses.
Interestingly, the four nurses who discussed their long COVID illnesses worked at different facilities and on different units, ranging from non-COVID to ICUs. Common long-term symptoms included shortness of breath, difficulty breathing, fatigue, vomiting, and mental health burdens. Three nurses reported that their symptoms have lasted over a year.
There were many differences between the clinical manifestations of long COVID in the four nurses. Two nurses reported being hospitalized for their acute infection period; one nurse had been hospitalized for 14 days in the ICU, whereas the other tested positive after an unrelated surgery and remained in the hospital for a few days. One nurse, aged 54 with comorbidities, experienced mild symptoms during her acute infection period, but continues to suffer from shortness of breath, diminished smell, and vomiting. Another nurse reported long-term gastrointestinal symptoms.
The rate of long COVID in nurses in the survey is greater than what has been found in the general public. Current research suggests that onethird of patients infected with SARS-CoV-2 experience symptoms 2–6 weeks beyond their acute infection, and 11–25% have symptoms that persist beyond 3 months. The 2021 Nurses COVID Survey found 55.81% of respondents experienced long COVID symptoms. This may be related to viral load, as some evidence indicates that a greater viral load is correlated to increased COVID-19 disease severity (Fajnzylber et al., 2020).
23 Journal of the New York State Nurses Association, Volume 49, Number 1
n
Venting the Truth About COVID-19
Many healthcare workers worldwide have had to work with COVID-19 patients. One study suggests that the estimated worldwide prevalence of SARS-CoV-2 infection among healthcare workers was 11% (Gómez-Ochoa et al., 2021). Out of that study, the most frequently affected personnel were nurses (48%), compared to most of the COVID-19-positive medical staff who worked in hospital non-emergency wards during screening. In a study of an English teaching hospital, published on behalf of the London Society of Occupational Medicine, 45% of 138 healthcare workers who responded to a questionnaire reported long COVID symptoms, with 32% struggling 3–4 months after the peak of the wave (Gaber et al., 2021).
The fact that 55.8% of the nurse respondents from our survey had reported having long COVID symptoms, suggests that nurses often have had to deal with the brunt of care for COVID-19 patients and, thus, may have been exposed to higher viral loads. Poor COVID-19 protection by facilities exacerbated these consequences. In addition, reports from our nurse interviews have confirmed the struggles that nurses have faced with physical and mental exhaustion and difficulty with care for COVID-19 patients.
Advance of Nursing Practice Based on Evidence
Nightingale wrote “The three things which all but destroyed the army in Crimea were ignorance, incapacity, and useless rules; and the same thing will happen again, unless future regulations are framed more intelligently, and administered by better informed and more capable officers.”
Similarly, during the COVID-19 pandemic, New York’s nursing workforce, which is habitually overburdened even in the best of times, was pushed to its limits. Countless employer violations in worker health and safety ultimately led to preventable losses of patients and nurses lives.
A study conducted in 2018 revealed that as a patient, if you’re admitted to a bed where the previous patient had an infection, you are six times more likely to acquire the same infection. And on any given day, one in 31 hospital patients has at least one healthcare-associated infection (HCAI) (Haque et al., 2018; Steinhoff, 2021). According to the CDC, nearly 1.7 million hospitalized patients annually acquire HCAIs while being treated for other health issues and more than 98,000 patients (one in 17) die due to an HCAI (Haque et al., 2018).
Nightingale noted “how very little can be done under the spirit of fear.” Her courage in speaking up and challenging the traditional medical authority was instrumental in advancing collaborative, high-quality care, and defining necessary elements for cultures of safety.
Nurses Unions have played an integral role in supporting nurses throughout the COVID-19 pandemic. Nurses, supported by their unions, have been at the forefront of the fight for improvements in patient care and worker safety throughout the COVID-19 pandemic. Even before the first COVID-19 case was identified in New York, nurses were outspoken advocates for improved staffing and more PPE stockpiles in anticipation of COVID-19 (NYSNA, 2020a).
In February 2020, New York health and safety experts urged for better administrative and engineering controls in hospitals to protect workers
and patients (NYSNA, 2020b). Nurses advocated for increased patient screening and cohorting procedures, as well as improved ventilation and usage of negative pressure rooms to reduce the airborne transmission of the virus (NYSNA, 2021b).
Contrary to the concerns of New York nurses, federal and New York State and local governments did not adequately prepare our health systems or the public for the first COVID-19 wave. Indeed, the first COVID-19 patient was identified in New York in March 2020, but then-Governor Andrew Cuomo was quoted as saying New York had “been through this rodeo before” with other viral outbreaks, and pointed out that the common flu posed a more widespread threat than COVID-19 (4 New York, 2020). But by March 7, 2020, Cuomo had declared a state of emergency and by March 13, 2020, then-President Donald Trump had declared a national emergency (Kerr, 2021). Even then, there were opposing ideas about the severity of the pandemic and the level of responses needed to fight it. Nurses were burdened with massive exposure to the virus and lack of personal protective gear to combat exposure to the COVID-19 while they cared for COVID-19 patients.
In response, New York unionized nurses came together to speak out against their mistreatment by employers. Rallies were held and, as more nurses joined the movement, nurse power grew stronger. Nurses began urging the federal government to ramp up supplies of personal protective equipment by activating the Defense Production Act. One NY nurses’ union filed three lawsuits: the first against the New York State Department of Health, the second against a large public sector hospital, and the third against a large private sector hospital in New York State. Nurses at those hospitals claimed these facilities failed to protect them while they were treating COVID-19 patients as evidenced by the thousands of COVID protest of assignment forms and multiple OSHA complaints that were filed at that time. These courageous actions exemplify Nightingales vision of a public healthcare system based on health promotion and disease prevention and her spirited efforts to challenge outdated systems and practices, be they from the military, medical, or political establishment.
Conclusion
We report that nurses have, and continue to face, many occupational health and safety hazards, including unsafe staffing and lack of PPE, mental health burdens, and symptoms of long COVID-19. The COVID-19 pandemic has been a painful experience, and it cannot be forgotten if we are to adequately prepare for and respond to the next pandemic crisis. Nursing’s most pressing concerns must be especially prioritized to build an effective, viable, and sustainable pandemic mitigation management plan.
We need more nurses with the mettle and competence of Florence Nightingale—passionate and tenacious, unafraid to take risks, willing to challenge the powerful, driving genuine change, building strong teams, and inspiring and bringing others with them. The best of Nightingale’s legacy, “less of the icon and more of the iconoclast,” deserves to endure for another 200 years.
Journal of the New York State Nurses Association, Volume 49, Number 1 24 n Venting the Truth About COVID-19
Al Thobaity, A. & Alshammari, F. (2020). Nurses on the frontline against the COVID-19 pandemic: An integrative review. Dubai Medical Journal, (3), 87–92. https://doi.org/10.1159/000509361
Alwan, N. A. & Johnson, L. (2021). Defining long COVID: Going back to the start. Med (NY), 2(5), 501–504. https://doi.org/10.1016/j. medj.2021.03.003
American Public Health Association. (2017, November 7). The critical need to reform workers’ compensation . https://www.apha. org/policies-and-advocacy/public-health-policy-statements/ policy-database/2018/01/18/the-critical-need-to-reform-workerscompensation
Anders R. L. (2021, October/December). Patient safety time for federally mandated registered nurse to patient ratios. Nursing Forum, 56(4), 1038–1043. https://doi.org/10.1111/nuf.12625
Associated Press. (2020, March 1). Manhattan Woman, 39, Is NYC’s First COVID-19 Case; Husband’s Test Results Are Pending. NBC 4 New York. https://www.nbcnewyork.com/news/coronavirus /person-innyc-tests-positive-for-covid-19-officials/2308155/
Aziz, S., Arabi, Y. M., Alhazzani, W., Evans, L., Citerio, G., Fischkoff, K., Salluh, J., Meyfroidt, G., Alshamsi, F., Oczkowski, S., Azoulay, E., Price, A., Burry, L., Dzierba, A., Benintende, A., Morgan, J., Grasselli, G., Rhodes, A., Møller, M. H., Chu, L., … & Christian, M. D. (2020). Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Medicine, 46(7), 1303–1325. https://doi.org/10.1007/ s00134-020-06092-5
Bielcor. (2021). Do N95 facemasks expire? https://www.bielcor.com/don95-face-masks-expire/
Brosseau, L. M., Jones, R. M., & Harrison, R. (2021). Elastomeric respirators for all healthcare workers. American Journal of Infection Control. 49(3), 405–406. https://doi.org/10.1016/j.ajic.2020.09.008
Campanile, C. & Boden, E. (2020, April 2). Nurses at NYC hospital receive gowns after Post trash bag exposé. NY Post Online. https://nypost. com/2020/04/02/nurses-at-nyc-hospital-receive-gowns-after-posttrash-bag-expose/
Centers for Disease Control and Prevention. (2015, January 13). Hierarchy of controls. https://www.cdc.gov/niosh/topics/hierarchy/default.html
Cho, S. H., Lee, J. Y., You, S. J., Song, K. J., & Hong, K. J. (2020). Nurse staffing, nurses’ prioritization, missed care, quality of nursing care, and nurse outcomes. International Journal of Nursing Practice, 26(1), e12803. https://doi.org/10.1111/ijn.12803
Cimiotti, J. P., Aiken, L. H., Sloane, D. M., & Wu, E. S. (2012). Nurse staffing, burnout, and health care-associated infection. [Correction published in] American Journal of Infection Control, 40 (7), 680. [Original] American Journal of Infect Control, 40 (6), 486–490. https:// doi.org/10.1016%2Fj.ajic.2012.02.029
Cullen, W., Gulati, G., & Kelly, B. D. (2020). Mental health in the Covid19 pandemic. QJM: An International Journal of Medicine, 113(5), 311–312. https://doi.org/10.1093/qjmed/hcaa110
Fajnzylber, J., Regan, J., Coxen, K., Corry, H., Wong, C., Rosenthal, A., Worrall, D., Giguel, F., Piechocka-Trocha, A., Atyeo, C., & Fischinger, S. (2020). SARS-CoV-2 viral load is associated with increased disease
Venting the Truth About COVID-19
severity and mortality. Nature Communications, 11(1), 1–9. https:// doi.org/10.1038/s41467-020-19057-5
Gaber, T., Ashish, A., & Unsworth, A. (2021). Persistent post-COVID symptoms in healthcare workers. Occupational Medicine, 71(3), 144–146. https://doi.org/10.1093/occmed/kqab043
Gómez-Ochoa, S. A., Franco, O. H., Rojas, L. Z., Raguindin, P. F., RoaDíaz, Z. M., Wyssmann, B. M., Guevara, S. L. R., Echeverría, L. E., Glisic, M., & Muka, T. (2021). COVID-19 in Health-Care Workers: A living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. American Journal of Epidemiology, 190 (1), 161–175. https://doi.org/10.1093/aje/kwaa191 Haque, M., Sartelli, M., McKimm, J., & Abu Bakar, M. (2018). Health careassociated infections—an overview. Infection and Drug Resistance, 11, 2321–2333. https://doi.org/10.2147/IDR.S177247
Health Facilities: Nursing Staff Act, Cal. Assemb. B 394. (1999 –2000) Chapter 945 (Cal. Sta. 1999). https://leginfo.legislature.ca.gov/faces/ billTextClient.xhtml?bill_id=199920000AB394
International Council of Nurses. (2020). The global nursing shortage and nurse retention https://www.icn.ch/sites/default/files/inlinefiles/ICN%20Policy%20Brief_Nurse%20Shortage%20and%20 Retention_0.pdf
Jenkins, R., Elliott, P. (2004). Stressors, burnout and social support: nurses in acute mental health settings. Journal of Advanced Nursing. 48(6): 622-631. doi:10.1111/j.1365–2648.2004.03240.x
Kerr, A. (April 5, 2021). Investopedia. A Historical Timeline of COVID-19 in New York City. Retrieved from https://www.investopedia.com/ historical-timeline-of-covid-19-in-new-york-city-5071986
Konda, S. R., Dankert, J. F., Merkow, D., Lin, C. C., Kaplan, D. J., Haskel, J. D., Behery, O., Crespo, A., & Ganta, A. (2020). COVID-19 Response in the Global Epicenter: Converting a New York City level 1 orthopedic trauma service into a hybrid orthopedic and medicine COVID-19 management team. Journal of Orthopaedic Trauma, 34(8), 411–417. https://doi.org/10.1097/BOT.0000000000001792
Kovner, C., Raveis, V. H., Van Devanter, N., Yu, G., Glassman, K., & Ridge, L. J. (2021). The psychosocial impact on frontline nurses of caring for patients with COVID-19 during the first wave of the pandemic in New York City. Nursing Outlook, 69(5), 744–754. https://doi.org/10.1016/j. outlook.2021.03.019
Lasater, K. B., Aiken, L. H., Sloane, D. M., French, R., Anusiewicz, C. V., Martin, B., Reneau, K., Alexander, M., & McHugh, M. D. (2021a, May 1) Is hospital nurse staffing legislation in the public’s interest?: An observational study in New York State. Medical Care, 59(5), 444–450. https://doi.org/10.1097/MLR.0000000000001519
Lasater, K. B., Aiken, L. H., Sloane, D. M., French, R., Martin, B., Reneau, K., Alexander, M., & McHugh, M. D. (2021b, August 13). Chronic hospital nurse understaffing meets COVID-19: an observational study. BMJ Quality & Safety, 30 (8), 639–647. https://doi.org 10.1136/bmjqs2020-011512
McDonald, L. (2020). Florence Nightingale: The making of a hospital reformer. HERD: Health Environments Research & Design Journal, 13(2), 25–31. https://doi.org/10.1177/1937586720918239
n References 25 Journal of the New York State Nurses Association, Volume 49, Number 1
n
McKinley, J. (2020, March 22). New York City region is now an epicenter of the coronavirus pandemic. The New York Times https://www. nytimes.com/2020/03/22/nyregion/Coronavirus-new-York-epicenter. html
McHugh, M. D., Aiken, L. H., Sloane, D. M., Windsor, C., Douglas, C., & Yates, P. (2021) Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals. The Lancet, 397(10288), 1,905–1,913. https://doi.org/10.1016/S0140-6736(21)00768-6
Matthews, J. H., Whitehead, P. B., Ward, C., Kyner, M., & Crowder, T. (2020, May 31). Florence Nightingale: Visionary for the role of clinical nurse Sspecialist. OJIN: The Online Journal of Issue, 25(2), Manuscript 1. https://doi.org/10.3912/OJIN.Vol25No02Man01
National Nurses United. (n.d.). What does the California ratios law actually require? https://www.nationalnursesunited.org/what-doescalifornia-ratios-law-actually-require
National Nurses United. (2020, September). Sins of Omission: How government failures to track Covid-19 data have led to more than 1,700 health care worker deaths and jeopardize public health https://www.nationalnursesunited.org/sites/default/files/nnu/graphics/ documents/0920_Covid19_SinsOfOmission_Data_Report.pdf
New York State (2020, March 7). At novel coronavirus briefing, Governor Cuomo declares state of emergency to contain spread of virus. https:// www.governor.ny.gov/news/novel-coronavirus-briefing-governorcuomo-declares-state-emergency-contain-spread-virus
New York State (2021, August 12). Governor Cuomo updates New Yorkers on state’s progress during Covid-19 pandemic https://www.governor. ny.gov/news/governor-cuomo-updates-new-yorkers-states-progressduring-covid-19-pandemic-218
New York State (2021, September 27). No. 4: Declaring a statewide disaster emergency due to healthcare staffing shortages in the state of New York. https://www.governor.ny.gov/executive-order/no-4-declaringstatewide-disaster-emergency-due-healthcare-staffing-shortages-state
New York State Nurses Association (n.d.a). About NYSNA. Accessed August 13, 2021. https://www.nysna.org/strength-at-work/aboutnysna#.YRXx9PKSk2x
New York State Nurses Association (n.d.b). NYSNA Represented Facilities Accessed August 13, 2021. https://www.nysna.org/strength-work/ about-nysna/nysna-represented-facilities#.YRXyOPKSk2w
New York State Nurses Association. (2021). NYSNA 2020 Annual Report https://issuu.com/nystatenursesassociation/docs/2020nysnaannlrptf inal?fr=sYzA5YzE5OTMyMjc
New York State Nurses Association. (2020a, August 8). We need sustainable PPE strategy! https://www.nysna.org/blog/2020/08/08/ we-need-sustainable-ppe-strategy#.YWWgFqQpCUk
New York State Nurses Association. (2020b, March 27). Safe nurses, safe communities: The union approach to managing the COVID19 crisis https://www.nysna.org/blog/2020/03/17/safe-nursessafe-communities-union-approach-managing-covid-19-crisis#. YWWneqQpCUk
New York State Nurses Association. (2021a, February 24). New York State Nurses Association announces over 26,000 official complaints were filed by nurses about not enough staff in Hospitals and Nursing Homes during the last two years. Retreived from https://www.nysna. org/press/2021/new-york-state-nurses-association-announces-over26000-official-complaints-were-filed#.YWWywaQpCUk
New York State Nurses Association. (2021b, July 22). NEW! Position Statement: On the COVID-19 Vaccine, July 21. https://www.nysna. org/blog/2021/07/22/new-position-statement-covid-19-vaccinejuly-21#.YWWpGaQpCUk
Nightingale, F. (1859). Notes on hospitals, being two papers read before the National Association for the promotion of social science at Liverpool, in October 1958: With evidence given to the Royal Commissioners on the state of the army in 1857. J. W. Parker.
Nightingale, F. (1860). Notes on Nursing: What It Is and What It Is Not (new ed., rev., enlarged). Harrison.
Noorimotlagh, Z., Jaafarzadeh, N., Martínez, S. S., & Mirzaee, S. A. (2021). A systematic review of possible airborne transmission of the COVID19 virus (SARS-CoV-2) in the indoor air environment. Environmental Research, 193, 110612. https://doi.org/10.1016/j.envres.2020.110612
Östlund, U., Kidd, L., Wengström, Y., & Rowa-Dewar, N. (2011). Combining qualitative and quantitative research within mixed method research designs: A methodological review. International Journal of Nursing Studies, 48(3):369–383. https://doi.org/10.1016/j.ijnurstu.2010.10.005
Panzeri, F., Di Paola, S. & Domaneschi, F. (2021, April 28). Does the COVID-19 war metaphor influence reasoning? PLOS One. https://doi. org/10.1371/journal.pone.0250651.
Public Health Ontario. (2021). IPAC Recommendations for Use of Personal Protective Equipment for Care of Individuals with Suspect or Confirmed COVID -19. https://www.publichealthontario.ca/-/media/ documents/ncov/updated-ipac-measures-covid-19.pdf?la=en Reinking, C. (2020, May). Nurses transforming systems of care: The bicentennial of Florence Nightingale’s legacy. Nursing Management, 51(5), 32–37. https://doi.org/10.1097/01.NUMA.0000659408.49349.59
Shioda, K., Weinberger, D. M., & Mori, M. (2020) Navigating through health care data disrupted by the COVID-19 pandemic. JAMA Internal Medicine, 180(12), 1569–1570. https://doi.org/10.1001/ jamainternmed.2020.5542
Statista. (2021). Cumulative number of positive cases of COVID-19 in New York State from March 4, 2020 to March 7, 2021, by day https://www.statista.com/statistics/1109721/new-york-state-covidcumulative-cases-us/ Steinhoff, A. (2021, August 18). Innovators must embrace the COVID pandemic’s “Florence Nightingale” moment. Crunch Base News. https://news.crunchbase.com/news/innovators-must-embrace-thecovid-pandemics-florence-nightingale-moment/
Stewart, C. L., Thornblade, L. W., Diamond, D. J., Fong, Y., & Melstrom, L. G. (2020). Personal protective equipment and COVID-19: A review for surgeons. Annals of Surgery, 272(2), e132–e138. https://doi. org/10.1097/SLA.0000000000003991
Journal of the New York State Nurses Association, Volume 49, Number 1 26
the
COVID-19
n Venting
Truth About
Tsai, P.H., Lai, W. Y., Lin, Y. Y., Luo, Y. H., Lin, Y. T., Chen, H. K., Chen, Y. M., Lai, Y. C., Kuo, L. C., Chen, S. D., Chang, K. J., Liu, C. H., Chang, S. C., Wang, F. D., & Yang, Y. P. (2020). Clinical manifestation and disease progression in COVID-19 infection. Journal of the Chinese Medical Association, 84(1), 3–8. https://doi.org/10.1097/ jcma.0000000000000463
United States Department of Labor, Occupational Safety and Health Administration, 29 CFR 1910 Subpart I. (2021). Healthcare Workers and Employers. https://www.osha.gov/coronavirus/control-prevention/ healthcare-workers
NYS COVID-19 Minority Health Disparities Team. (2020). Differential impacts of COVID-19 in New York State: Understanding and eliminating minority health disparities in a 21st-century pandemic (Issue Brief 1). University at Albany, SUNY. https://www.albany. edu/communicationsmarketing/covid-19-documents/Racial%20 Disparities%20in%20COVID-19%20Bonus%20Briefing%20 Paper%5B2%5D.pdf
Venting the Truth About COVID-19
Vannabouathong, C., Devji, T., Ekhtiari, S., Chang, Y., Phillips, S. A., Zhu, M., Chagla, Z., Main, C., & Bhandari, M. (2020). Novel Coronavirus COVID-19. The Journal of Bone and Joint Surgery, 102(9), 734–744. https://doi.org/10.2106/JBJS.20.00396.
Wuellner, S. E., & Bonauto, D.K. (2014). Exploring the relationship between employer recordkeeping and underreporting in the BLS Survey of Occupational Injuries and Illnesses. American Journal of Industrial Medicine, 57(10), 1133–1143. https://doi.org/10.1002/ajim.22350
Zhang, R., Li, Y., Zhang, A. L., Wang, Y., & Molina, M.J. (2020). Identifying airborne transmission as the dominant route for the spread of covid-19. The COVID-19 Reader, 21–35. https://doi. org/10.4324/9781003141402-3
27 Journal of the New York State Nurses Association, Volume 49, Number 1
n
Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
Annemarie Rosciano, DNP, MPA, ANP-C Barbara Brathwaite, DNP, MSN, RN, CBN
n Abstract
Background: College-aged students engaging in risky sexual behavior are placed at risk for sexually transmitted infection and altered health and sexual well-being.
Purpose: Identify risky sexual behaviors among college-age students and explore their plans to change behaviors using brief action planning.
Method: Retrospective quantitative study
Results: Revealed high-risk sexual behaviors among 70% of students, with 62% having multiple partners, 37% not using protection, and 71% not having sexually transmitted infection testing. A brief action planning model was used by 100% of the students and 100% who screened positive for risky sexual behaviors chose not to modify these behaviors. Students prioritized changes in diet and sedentary behaviors.
Conclusions: Students disclose risky sexual behaviors but lack a propensity to change their behaviors. This suggests students may require knowledge about their behaviors and their associated health risks. Campus health centers can place emphasis on knowledge assessment of risky behaviors and plan how to strengthen behavioral change.
Keywords: brief action planning, health belief model, Partnership to Advance Collaborative Education (PACE) Health and Wellness Screening Instrument
Introduction
College-age students should be considered a high-risk and vulnerable population due to the stressors of their age and academic and psychosocial demands as they transition to their college environment (Benson & Ellis, 2019). They are at a critical developmental stage, undergoing changes, exploring and navigating sexual relationships, and learning about themselves (American College Health Association, 2020). Engaging in high-risk sexual behaviors, such as having multiple partners and sex without protection, place them at risk for sexually transmitted infections (STIs) (Dolphin et al., 2017) and altered health and sexual well-being. Increasing awareness of risky sexual behaviors creates opportunity to achieve a healthful life (Visalli et al., 2019).
The purpose of this study was to explore unhealthy sexual behaviors among campus students and help them create a plan to modify risky behaviors to promote health and reduce future risk of disease. In 2017, a northeastern public university school of nursing created and commenced the Partnership to Advance Collaborative Education (PACE). This clinical preventative screening program was offered weekly at the campus recreation and wellness center. It included screening for disease and mental health, provided education to increase awareness of risky behaviors, and referred students for medical and/or psychological services. The focal point of this study was to examine and modify risky sexual behaviors among college students.
Annemarie Rosciano, DNP, MPA, ANP-C and Barbara Brathwaite, DNP, MSN, RN, CBN
Stony Brook University School of Nursing, Stony Brook,
New York
Journal of the New York State Nurses Association, Volume 49, Number 1 28
Background
In 2020, the World Health Organization (WHO) addressed several sexual health concerns and defined sexual health as a state of sexual wellbeing (World Health Organization [WHO], 2020). Sexual health requires a positive, respectful approach to relationships, as well as having pleasurable and safe sexual experiences free of coercion, discrimination, and violence. Sexual well-being and safety are essential to overall health and wellness and are rooted in the framework of social determinants of health (Bedree, 2019). It is important to understand how students define sexual health and what supports or hinders their well-being (Bedree, 2019).
Bedree (2019) found that students felt safe to disclose sexual activity if their community was open and nonjudgmental. Sexual behaviors may be concealed among those with marginalized identities, such as the lesbian, gay, bisexual, transgender, and the queer-plus (LGBTQ+) community. This population often lacks access to health care and may be uncomfortable and/or not forthcoming with disclosing their sexuality out of fear of discrimination. Elimination of sexual barriers must be a focus to support all individuals’ diverse needs and provide opportunities for them to change risky behaviors. Minimal knowledge and lack of affirmation of one’s sexuality increases the risk of sexually transmitted infections (STIs) (Jahanfar et al., 2021; Visalli et al., 2019).
Jahanfar et al. (2021) found that sexual education received by people in high school was inferior and had little influence on sexual behaviors once a student was in college. A person’s first sexual encounter occurs, on average, at age 18, with most people reporting their first sexual relationship as casual. Gardner and Amankwaa (2020) found that young adults between the ages of 19 and 25 were not concerned with using protection or inquiring about the sexual history of their partners. The riskiest sexual behaviors were found among 24-year-olds. Fehr et al. (2018) found that male students were twice as likely to use condoms as female students, and upper division students were less likely to use condoms regularly. Race did not influence condom use. Most students reported that they did not use condoms while having anal sex and the risk of pregnancy was not cited as a concern among many college students.
Young adults are especially inclined to participate in risky behaviors as a result of masculinity norms advocated in early teenage years and peer pressure (Amin et al., 2018). Such behavior can result in increased unwanted pregnancies and STIs (DeLacy, 2019). Data published by the Center for Disease Control (CDC) “estimates that in 2018, 1 in 5 people in the United States had an STI,” with “nearly 68 million STIs on any given day in 2018,” at a total lifetime medical cost of “nearly $16 billion” (CDC, 2021, p. 1). Young adults remain disproportionally affected by STIs (Gardner & Amankwaa, 2020).
Students entering college have more freedom, including greater access to alcohol and drugs, multiple sexual partners, and opportunities to explore their sexual identity and sexual relationships (DeLacy, 2019). According to the 2018 American College Health Association-National College Health Assessment (ACHA-NCHA), 11.1% of male and 8.5% of female college students had “four or more sexual partners within one year” (p. 10). Twenty two percent of male and 21.4% female students reported having unprotected sex when drinking (p. 9). Alcohol and gender are known to be obstacles to sexual well-being (Bedree, 2019) and increase the risk for contracting and spreading STIs (ACHA-NCHA, 2018).
Students seek knowledge related to sexual issues as their age and curiosity mutually increase (Visalli et al., 2019) and young adults often look to their peers or social media for sexual health information if they feel disconnected from providers (Ericksen, 2018). Healthcare illiteracy can often be the cause of anxiety and most students do not bring their sexual health concerns to a parent (Visalli et al., 2019). Young females report an increase in autonomy when they are comfortable asking questions and obtaining information from their healthcare provider without a parent present (Richards, 2020). However, apprehension may occur if a student (a) lacks confidence in their health care provider, (b) if confidentiality is breached, or (c) if any type of discrimination occurs (Ericksen, 2018). Providers can also negatively affect student’s health outcomes when assumptions about sexual orientation are made or a patient feels a safe environment is nonexistent (Bedree, 2019).
Sexual health resources that are readily available and accessible to college students can result in reduction of STIs and unplanned pregnancies. Screening for risky sexual behaviors, communicating, and promoting safe sex education are essential in all-inclusive health care (DeLacy, 2019). Failure to support the sexual and reproductive health (SRH) needs of young adults can result in serious social, cultural, economic, and health issues which can include unplanned pregnancy, STIs, sexual intimidation, bullying, violence, and infertility. These consequences, along with limited access to SRH information and resources, puts an economic burden on families, communities, and societies (DeLacy, 2019).
Establishing equitable access and a supportive campus environment helps ensure that all students feel safe and protected (DeLacy, 2019). Mobile campus preventative screening programs offer students access, evaluation to identify risky behaviors, and provide an opportunity to change unhealthy behaviors. There is a dearth of literature concerning the significance of screening and addressing young adults’ risky sexual behavior in campus settings. Therefore, the aim of this study was to understand the sexual practices of college students and assist them in modifying these behaviors using a brief action plan (BAP) model.
Action Planning and Changing Risky Behaviors
Brief action planning is an evidenced-based motivating support tool grounded in the principles of motivational interviewing. BAP incorporates the psychology of behavioral change theory, which is aligned with selfefficacy and action-planning theory and research. Action planning has been shown to facilitate the intention-behavior relationship, thereby increasing the likelihood of behavior change. The BAP framework guides in assisting and creating an action plan and builds self-efficacy to fulfill the goals outlined in the action plan (Connell et al., 2020; Gutnick et al., 2014). Fifty to 75% of patients developed a plan with their primary care practitioners to change risky behaviors, using BAP (Gutnick et al., 2014). Weisberg et al. (2021) reported a decrease in pain and disability after instituting BAP. The BAP technique implemented during a screening event when time is limited, is effective for modifying risk factors and changing health behaviors (Gutnick et al., 2014).
One of the most frequently used models for exploring behavior change is the health belief model (HBM). The HBM is a health-specific model that aims to predict and describe why individuals modify or maintain their health behaviors. The underlying assumption is that preventive behaviors depend
Journal of the New York State Nurses Association, Volume 49, Number 1 29
n
Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective
Study
Adoption of safe sex practices by college students requires their understanding that they are susceptible and likely to develop complications (perceived susceptibility); that unsafe sexual practices lead to infection (STIs) and do harm to health.
on the individual’s expectations and beliefs (Mercadante & Law, 2022; Wang et al., 2021). The HBM suggest that an individual’s belief regarding a threat of disease and the belief in the effectiveness of the suggested health behavior will predict the possibility that the individual will adopt a new behavior. This model assumes that individual involvement in healthy behaviors depends on understanding six constructs of the individual’s perceived belief: severity, susceptibility, benefit, barrier, cue to action, and self-efficacy (Houlden et al., 2021).
Based on this model, adoption of safe sex practices by college students requires their understanding that they are susceptible and likely to develop complications (perceived susceptibility); that unsafe sexual practices lead to infection (STIs) and do harm to health (perceived severity); that healthy sexual behaviors have some benefits for them (perceived benefits); that there are some barriers against behavior alterations (perceived barriers); that healthcare professionals, peers, and social media encourage them to adopt healthy behaviors (cues to action); and, finally, that they can control unhealthy sexual practices through healthy behaviors (self-efficacy). This model supports importance of health education interventions to improve sexual health knowledge, health belief, and sexual behaviors.
Purpose
The purpose of this study is to identify risky sexual behaviors among college-age students utilizing standardized evidenced-based clinical screening instruments. A secondary aim is to explore students’ brief action plan creation and completion to change behaviors using BAP.
Methods Design
The protocol was reviewed by the university’s internal review board (IRB) and it was determined that the activity was not a systematic investigation and therefore did not meet the definition of human subjects’ research, thus the proposal did not require approval by the IRB or consent. A retrospective cohort study collection of data was used to examine sexual behaviors and gender and the application of BAP to change risky unhealthy behaviors. This was a single site study at a northeastern university in New York State. All data collection items were de-identified during their collection and responses could not be linked to any participants. This retrospective data collection was anonymously and confidentially collected from September 2017 through May 2019 using the PACE Health and Wellness Screening Instrument built by the PACE team. The data included demographic questions, height, weight, pain, vital signs, body mass index (BMI), immunization history, and screening for smoking, depression (PHQ9), anxiety (GAD-7), trauma (TSQ), alcohol (Audit-C), and drugs (DAST).
Five sexual health questions were developed by the PACE team that focused on (a) sexual activity, (b) multiple sexual partners, (c) use of protection, (d) sexually transmitted infection testing and treatment, and (e) unintended pregnancy. Sexual health questions required yes or no answers. The BAP guide was used to facilitate goal-setting and action-planning (Gutnick et al., 2014), and included open-ended questions consisting of (1) creating an action plan, (2) choosing from a behavioral menu of options, (3) reviewing of the plan, (4) rating the confidence level in creation of the plan, and (5) completing plan documentation at a 2-week follow-up phone call.
Sample
This study used a voluntary convenience sample of 603 undergraduate and graduate college-aged students who were attending the university. Participants resided both on and off campus and were at least 18 years of age and able to comprehend English. Exclusion criteria included students who were unable to complete the full screening process.
Using G*power, a statistical power analysis program, the minimum total sample size was calculated using an effect size of 0.30, a probability error of 0.05, and a power of 0.95 to determine the difference between two categorical variables within the same population required a minimum total sample size of n = 220 (HHU, 2007).
Procedure
Recruitment of students occurred at the screening location in the campus recreation and wellness center. Students were provided with an overview of the components of the screening using a vision board. Adult and family nurse practitioner (NP) students screened participants in a confidential setting. The NP students and faculty huddled to discuss identified risky behaviors. The BAP model was used by the NP students to guide the participants to identify a modifiable behavior and devise a plan. Based upon the screening results and BAP, resources, referrals, and education were provided to participants by the NP students with faculty oversight. Two weeks post screening, a follow-up phone call was implemented with an NP student to determine the level of plan completion. Throughout the process, all documents were anonymized, maintained in a sealed envelope, and collected by the primary investigator.
Data Analysis
Data was maintained in a software collection site known as RedCap, a secure web application for managing online databases (Sciences, 2018). All data was downloaded and analyzed to a protected computer and backed up on flash drive using the Statistical Package for the Social Sciences version 26 (SPSS) (IBM, 2013). Descriptive statistics were computed from the scores of the screening and BAP data. A chi-squared test of independence was performed to examine the relationship between sexual activity, unprotected sex, multiple sexual partners, and gender.
Results Sample
PACE Health and Wellness Screening demographic data was completed by 603 undergraduate and graduate participants ranging from age 18 to 24 (Table 1). Students reported their sexual practices (Table 2).
Journal of the New York State Nurses Association, Volume 49, Number 1 30
n
Sexual
Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective
Relationship Between Sexual Activity and Gender
The chi-squared test for independence was conducted to assess the association between sexual activity, unprotected sexual behavior, multiple sexual partners, and gender. Males were more likely to engage in sexual activity (Table 3); females were more likely to have unprotected sex (Table 4); and males were more likely to engage with multiple partners (Table 5).
Brief Action Planning
Analysis of behavior change indicated that 100% of the participants created a plan to change risky behaviors (Figure 1) with the top behaviors students chose to alter being exercise and diet. Seventy-five percent completed their plan to change (Figure 2); however, students did not choose to change their sexual behaviors.
Table 1
Discussion
Sexual Activity and Gender
The findings of the current study revealed that most college students engaged in sexual activity, with males reporting having more sex than females.
Unprotected Sexual Activity
The current study found 37.5% of the participants had unprotected sex at least once within the most-recent one-year period. Females reported more unprotected sex (p = .02); however, males were less apt to use any method of birth control despite reporting having more multiple sexual partners than females. In the current study, 71% of participants reported that they did not have any testing for STIs in the past year. One-third of students had unprotected sex, while often disclosing they frequently obtained STI testing.
Demographic Data Sexual Well-Being and Screening for Risky Sexual Behaviors (n = 603)
Question Category Mean n %
Age 23 100
Age 18 to 19 137 23.0 20 to 21 271 45.0 22 to 24 120 20.0 No response 75 12.0
Race Asian/Asian American 254 42.0 Black/African American 93 15.4 Hispanic/Latinx 102 17.0 American Indian/Alaska Native/Pacific Islander 1 1.5 White 177 29.4
Gender Male 324 53.7 Female 279 46.0 LGBTQ+ 44 7.3
Country of origin International 121 20.0 United States 481 80.0
Employment status Part-time 32 5.3 Full-time 225 42.3 Not employed 346 52.4
Year in college
Freshman 105 17.5 Sophomore 87 14.4 Junior 159 26.4 Senior 175 29.0 Graduate student 69 11.4 Continuing education student 6 1.0 Not employed 346 52.4
Note. N = 627. Of participants, 5.3% chose to identify as more than one race.
Journal of the New York State Nurses Association, Volume 49, Number 1 31
n
Study
2
Reported Sexual Practices (n = 603)
Sexual Practices (n) Yes %
Are you sexually active? 423 70.1
Have you had unprotected sex in the last 12 months? 226 37.5
Have you used condoms as protection in the last 12 months? 325 53.7
Have you engaged in sexual activity with multiple partners in the last 12 months? 95 15.8
Have you had oral, vaginal, and/or anal sex in the last 12 months with one partner? 248 41.1
Have you had oral, vaginal, and/or anal sex in the last 12 months with two partners? 64 10.6
Have you had oral, vaginal, and/or anal sex in the last 12 months with three or four partners? 90 15.0
Have you had any STI testing in the last 12 months? 171 28.4
If you were tested for STIs, did you test positive? 8 1.3
Have you experienced unintended pregnancy? 7 1.2
Have you received the (HPV) immunization? 324 53.7
Multiple Partners
The current study found most respondents reported having had oral, vaginal, or anal sex in the last 12 months with one partner (n = 248, 41.1%), 62% of males (p = .06) had multiple partners. Fifteen percent of the students reported having had multiple sexual partners in the last 12 months.
Lifestyle Modification
In the current study, 33% of students had a body mass index (BMI) greater than 25, poor dietary habits, and a sedentary lifestyle in addition to a high level of risky sexual behaviors. Despite this, students did not choose to modify risky sexual behaviors. They prioritized exercise (32%) and diet (24%) in attempts to lose weight.
Sexual Activity and Gender
The findings from Scull et al. (2020) coincided with this study’s findings in that male students were inclined to have more sex, a greater number of casual sexual relationships, sex while intoxicated, and practice
Table 3
Association of Sexual Activity and Gender
Reported Sexual Activity Group No Yes n (%) n (%)
Male 51 (62.2%) 156 (51.3%) Female 31 (37.8%) 148 (48.7%) χ2 (1, n = 386) = 3.07, p = .08
Table 4
Association of Unprotected Sexual Activity and Gender
Reported Unprotected Sexual Activity Group No Yes n (%) n (%)
Male 95 (57.9%) 81 (45.5%) Female 369 (42.1%) 97 (55.5%) χ2 (1, n = 342) = 5.27, p = .02
Figure 1
80
70
60
50
40
30
20
10
75% 11% 5%
Creation of Behavioral Plan (n = 603) 0
No (Up par tial to 50%) Total
more high-risk sexual behaviors. Sexual relationships are shaped by traditional stereotypes that have historically associated “masculinity” with assertiveness, violence, sexual play, and emotional distance, and
Table
Journal of the New York State Nurses Association, Volume 49, Number 1 32
n Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
“feminity” with passivity and emotional intimacy (Siegel, 2019). In Western cultures, males have traditionally been taught from a young age to associate masculinity with the initiation and experience of having sexual encounters and by acting “strong.” Males have also traditionally been under peer pressure to demonstrate masculinity through sex. Females have traditionally had greater restrictions placed on their sexuality and are more likely to have been taught from a young age that sexual activity is “saved for marriage” (Scull et al., 2020).
As a result, males tend to initiate sex at a younger age, likely due to the cultural double standard. Those who have sexual experiences at an earlier age tend to be more sexually active and incur more risky sexual behaviors (Scull et al., 2020). Siegel and Meunier (2019) found that cultural stereotypes influenced respondents’ sexual relations and the conception of sexual acts in the context of “domination–submission” (p. 1). Adolescent boys have been reported to more likely endorse unequal gender norms than girls (Amin et al., 2018). As per Amin, as boys grow older, peers appear to be very important in shaping and maintaining masculinity norms. Male peers may challenge each other physically or verbally, encourage risk-taking behaviors (such as substance use or unsafe sex), and practice sexual dominance over others. Peer relationships seem to reinforce traditional sexual stereotypes. Any breach of masculinity norms is punished by ridicule and intimidation (Amin et al., 2018; Kågesten et al.)
Figure 2 Completion of Behavioral Plan 0 10 20 30 40 50 60 70 80 No (Up par tial to 50%) Total 75% 11% 5% Table 6 Brief Action Plan (Chosen Plan Type) (n = 603) Type of action plan n % Exercise 192.9 32.2 Healthier diet 144.7 24.2 Improve sleep 72.4 12.1 Lose weight 48.2 8.7 Attend counseling 24.1 4.0 Seek medical attention (for pain) 18.0 3.4 Marijuana smoking cessation 16.2
Meditate 16.2
Cut down on smoking or cessation
2.7
2.7
12.1 2.0 Gain muscle mass 12.1 2.0 Seek assistance at student health 12.1 2.0 Study daily 7.8 1.3
Table 7 Post Screening Statistics (n = 603)
n %
Reason for attending
Convenient 349.7 58.0 Looked interesting 205.0 34.8 Worried about having a medical issue 247.2 41.2 Concerned about overall health 241.2 40.8 Wanted free items 156.0 26.8 Wants assistance to manage stress 132.0 22.0 Bothered by something physically and/or mentally 132.0 22.0 Concerned about sleep problem 114.5 19.4
n (Yes) %
Journal of the New York State Nurses Association, Volume 49, Number 1 33
Well-Being and Screening
Risky Sexual Behaviors: A Quantitative
Study n
Table 8 Post Screening Exit Survey (n = 603) Post screening
Was the experience what you expected? 578.8 96.5 Were all your concerns addressed? 584.9 97.3 Did you learn anything? 542.0 90.8 Would you recommend the screening to a friend? 578.0 96.2 Are you confident you will make changes? 494.0 82.5
Sexual
for
Retrospective
Unprotected Sexual Activity
Consistent with this study and as documented in other studies, females are known to have unprotected sex. Yi et al. (2018) assessed sexual behaviors among college students and found that females were significantly more likely to have unprotected sex. Dolphin et al. (2017) found females who reported body discontent also reported having less control during sexual activity and were more likely to defer to their partner regarding use of protection to avoid rejection.
Fairfortune et al. (2020) discovered that 67% of female students did not use condoms. Females under 20 years of age used condoms when first introduced to sexual intercourse, but condom use decreased as sexual experience increased. Those older than 20 years of age reported using condoms less frequently for their first sexual interaction, even though they used oral birth control for pregnancy prevention. Females who had sexual intercourse with experienced partners were more likely to use condoms out of fear of STI transmission. Alam et al. (2021) found that expression of relationship concerns and making decisions about condom use was suppressed for females, who were more often silenced and/or made to experience shame and guilt for requesting condom use, resulting in lack of power in their relationships and over their health.
Fehr et al. (2018) found males used condoms more regularly than females. Partners in an exclusive relationship indicated a high degree of trust in their partner to remain monogamous. (Fehr et al., 2018; Scull et al., 2020). Although the current study did not explore the type of protection used by students, future studies should focus on measures of prevention and sexual education for all genders.
Students may not value using protection because they feel safe knowing that free STI testing and Plan B contraception was available on campus. Understanding students’ viewpoints about the availability of STI testing, contraception, and unprotected sex needs further examination.
Multiple Partners
Findings from the 2018 ACHA-NCHA revealed that it was common for young adults to have multiple sexual partners within a 1-year period. This behavior increases the risk for contracting an STI and the potential to spread it to other students (ACHA-NCHA, 2018). Sexual well-being may require further exploration to understand if there is a relationship between lack of sexual satisfaction and multiple partners. The desire for multiple partners might be explained by the fact that many males were found to have more liberal attitudes about sex, which in turn were associated with an increased number of sexual partners. Young adults who initiate sexual activity at an early age have been found to exercise a higher frequency of sex and a greater number of multiple partners (Scull et al., 2020). As outlined in a systematic review by Kågesten et al. (2016), young adult males exhibit their sexual prowess by having multiple sexual partners and demonstrate dominance over their partners in relationships. Sexual education can empower young adults to make informed decisions about early intercourse.
Lifestyle Modification
By 2030, obesity in adults is estimated to increase by 50% due to diets low in fruits and vegetables and high in sugar (Opoku-Acheampong et al., 2018). Early identification of poor dietary behaviors can facilitate
Lack of knowledge pertaining to risky sexual behaviors may have influenced students’ prioritization of diet and exercise modifications instead of altering risky sexual practices.
change to promote health and prevent chronic illness. Fakhria et al. (2019) assessed college students’ perceptions toward physical activity and sedentary behaviors. Most students who chose to engage in physical activity wanted to improve their physical appearance, have fun, relax and socialize with peers, and decrease stress. Benefits of physical activity included improved physical appearance, concentration, self-assurance, and academic performance (Christianson et al., 2019). It may be that for these reasons students largely chose plans that supported exercise.
Using a Brief Action Plan to Change High-Risk Behavior
The current study supported the hypothesis that students would create an action plan to change a high-risk behavior. Most students were conscious of their poor diet habits, lack of exercise, and obesity, and chose to formulate an action plan to change their diet and begin an exercise program. Although students reported having multiple sexual partners and being deficient in using contraceptive protection, none of the participants chose to change these risky behaviors. Lack of knowledge pertaining to risky sexual behaviors may have influenced students’ prioritization of diet and exercise modifications instead of altering risky sexual practices. Many students reported participating in the health screening out of concern for their health (n = 603, 41%). Screening for diabetes and hypertension among students with a family history of these issues was a common request. While family history of disease, BMI, and diet was not included in this study, students evidenced a great need to focus on diet and exercise through their choices.
Compliance With Safe Sexual Health Practices
Education on safe sex practices can help increase knowledge and compliance. Education includes discussion of sexual health facts, disease information, and ways students can take control of their sexual health. The most reliable way to avoid sexual disease is through abstinence, vaccinations, decreasing one’s number of sexual encounters, getting tested regularly and sharing results, agreeing to be sexually exclusive with one partner, having open and truthful discussions, and consistently using a condom every time engaging in anal, vaginal, or oral sex (CDC, 2020).
Educational Approach
Sexual health education requires a positive and respectful attitude toward both sexuality and sexual relationships and a holistic and genderneutral approach. It is evident that health education services are essential to providing holistic health care for college students, not only on campus,
Journal of the New York State Nurses Association, Volume 49, Number 1 34
n Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
but throughout the community (ACHA, 2020). Healthcare providers are in a privileged position to offer educational resources and programs that target risk misperceptions and address the ways students can be empowered to make safer sexual health decisions. This study found that 90% of students reported that they learned something new through the sex education provided during their screening for this study.
Among college students, identity, culture, and ethnicity determine the values, attitudes, beliefs, knowledge, and ways in which an individual communicates about health, sexuality, relationships, contraception, and pregnancy. Healthcare providers must have an awareness and a thorough understanding of the diverse and equitable needs of college campus students. Counseling that addresses personal risk, high-risk behaviors, and the use of individual action plan strategies, such as BAP, can assist in prevention and education about risky behaviors for diverse student communities (Bowman et al., 2018).
Strengths and Limitations
This study highlighted the importance of student access to clinical preventative screenings, education, resources, and referrals. The sample size was 603 students, who voluntarily participated, with 75% of students agreeing to make changes in their lifestyle to improve identified risky behaviors other than high-risk sexual behaviors. The data suggest student assessment, family history, and interventions are essential to improving short- and long-term health outcomes. The PACE team unexpectedly identified unhealthy sexual practices in this population and educated student participants accordingly. Using the BAP model helped to close the educational gap, ultimately preventing disease for this diverse and vulnerable population.
This study lacked preassessment of students’ sexual health knowledge. Results of this study support the need to increase easy access to screenings that can support modifying students’ unhealthy practices.
The study effect sizes were relatively small and future studies are warranted to replicate these results. Self-reported data may be influenced by social desirability bias. Data was collected from a small participant pool from one university making the study geographically limited. A convenience sample was used and is not as generalizable.
Implications for Nursing Practice and Research
This study identified many variables that place college-age students at risk for poor health outcomes. Assessment of college-age patients’ existing knowledge and beliefs is vital for all nurse practitioners and educators to employ, as it may help change a student’s belief system that their behaviors are inconsequential. Strategies such as the application of a health belief model to develop educational programs should be explored to avoid the consequences of unsafe sexual practices and improve students’ well-being.
Conclusion
PACE has effectively built a strong foundation for generating the delivery of screenings to improve the health outcomes of college-age students. This study has revealed that most college students between the ages of 18–24 engage in sexual activity, males tend to have more sex than females, one-third of the students have unprotected sex (more females than males), many have multiple partners, and the majority of those who are sexually active choose not to test for STIs. Students lack the predilection to change unhealthy sexual behaviors. There is a lack of understanding by the PACE team as to why this transpired. This study demonstrated that it is vital to understand campus students’ baseline beliefs about sexual health. Replication of this study using a larger sample to include appraisal of students’ knowledge about unhealthy behaviors and ensure that representation of the effects health education has on this vulnerable population is recommended.
Journal of the New York State Nurses Association, Volume 49, Number 1 35 Sexual
n
Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
n References
Alam, N., & Alldred, P. (2021). Condoms, trust and stealthing: The meanings attributed to unprotected hetero sex. International Journal of Environmental Research and Public Health, 18, 4257. https://doi. org/ 10.3390/ijerph18084257
American College Health Association. (2020). Guideline: Best practices for sexual health Promotion and clinical care in college health settings. Guidelines Recommendations and White Papers. https:// www.acha.org/ACHA/ACHA/Default.aspx?hkey=af8fdb4e-1b51-40fdbd11-9280907b838d
American College Health Association (ACHA-NCHA). (2018). Sexual Health/STIs https://w ww.acha.org/NCHA/ACHA/Resources/Pap_ STI_Survey.aspx
Amin, A., Kågesten, A., Adebayo, E., & Chandra-Mouli, V. (2018). Addressing gender socialization and masculinity norms among adolescent boys: Policy and programmatic implications. Journal of Adolescent Health, 62, S3–S5. http://dx.doi.org/10.1016/j jadohealth.2017.06.022
Bedree, H., Moller-Mullen, M., Rose, E., & Flanders, C. (2019). Sexual well-being among college students: A qualitative study. Sexuality & Culture, 24. http://dx.doi.org/10.1007/s12119-019-09631-5
Benson, T., & Ellis, J. (2019). High-risk sexual behavior and reasons for living in a college population. Journal of Psychology and Psychotherapy, 9(3). http://dx.doi.org/10.35248/2161- 0487.19.9.361
Bowman Heads, A. M., Glover, A. M., Castillo, L. G., Blozis, S., & Kim, S. Y. (2018). Dimensions of ethnic identity as protective factors for substance use and sexual risk behaviors in African American college students. Journal of American College Health, 66(3), 178–186. http:// dx.doi.org/10.1080/07448481.2017.1400975
Brathwaite, B., Marino, M., & Bruckenthal, P. (2018). Nurse practitioner confidence and attitudes towards brief motivational interventions to improve compliance with health and wellness recommendations. Journal of Community Public Health Nursing, 4(212). http://dx.doi. org/10.4172/2471-9846.1000212
Buzayehu, F. W., Lemessa, O., Melake, D., Lemma, D. R., & Wakgari, B. D. (2021). Risky sexual behavior and associated factors among sexually experienced secondary school students in Guduru, Ethiopia. Preventive Medicine Reports, 23, Article 101398. doi.org/10.1016/j. pmedr.2021.101398
Center for Disease Control. (2019). Sexually transmitted diseases (STDs): Data & statistics https://w ww.cdc.gov/std/stats/default.htm
Center for Disease Control. (2020). How can you prevent sexually transmitted diseases (STDs)? https://www.cdc.gov/std/prevention/ default.htm
Center for Disease Control. (2021). CDC estimates that 1 in 5 people in the U.S. have a sexually transmitted infection. https://www.cdc. gov/media/releases/2021/p0125-sexualy-transmitted-infection.html
Christianson, J., Kattelmann, K., Riggsbee, K., Moret, L., Vilaro, M. J., Olfert, M. D., … & Colby, S. (2019). Promoting wellness on college campuses: Identifying and addressing the wellness needs of college
students. Topics in Clinical Nutrition 34(2), 125–137. http://dx.doi. org/10.1097/tin.0000000000000169
Connell, G., Verville, L., Cancelliere, C., Wong, J. J., Yu, H., & Shearer, H. M. (2020). Brief action planning targeting prognostic factors for an adult with persistent low back pain without radiculopathy: A case report . Clinical Case Reports 8(12), 2777–2781. doi:https://doi. org/10.1002/ccr3.3280
DeLacy, J., Saheb, R., Garcia, Raul., & Dune, T. (2019). Sexual and reproductive health services and promotion in tertiary institutions: A systematic content review. Journal of the Australian and New Zealand Student Services Association, 27(1). http://dx.doi. org/10.30688/janzssa.2019.05
Dolphin, L., Fitzgerald, A., & Dooley, B. (2017). Risky sex behaviors among college students: The psychosocial profile. Early Intervention in Psychiatry, 12(6), 1203–1212. https://doi.org/10.1111/eip.12526
Ericksen, M., Hirt. K., Rice, M., & Cedergren, A. (2018). Let’s talk about sex: Development, implementation, and evaluation of a sexual health promotion program of college students. The Health Education Monograph Series, 35. http://dx.doi.org/10.1521/aeap.2012.24.4.327
Fairfortune, T. S., Stern, J. E., Richardson, B. A., Koutsky, L. A., & Winer, R. L. (2020). Sexual behavior patterns and condom use in newly sexually active female university students. Archives of Sexual Behavior, 49(3), 1053–1065. http://dx.doi.org/10.1007/s10508-019-1411-z
Fakhria Jaber Muhbes, S. K. (2019). A study of self-reported physical activity and sedentary healthy behaviors among Babylon nursing students. Indian Journal of Forensic Medicine & Toxicology, 13(3), 230–236. http://dx.doi.org/10.37506/ijfmt.v13i3.358
Fehr, S. K., Vidourek, R. A., King, K. A., & Nabors, L. A. (2018). Relationship factors’ impact on condom use among college students. Sexuality & Culture, 22(3), 724–739. http://dx.doi.org/10.1007/s12119-018-9503-9
Gardner, L., & Amankwaa, L. (2020). Sexual behavior of young adults with sexually transmitted infections. Association of Black Nursing Faculty, Inc. 31(1), 35–43.
Gutnick, D., Reims, K., Davis, C., Gainforth, H., Jay, M., & Cole, S. (2014). Brief Action Planning to facilitate behavior change and support patient self-management. Journal of Clinical Outcomes Management, 21(1). http://ww.w.turnerhite.com/pdf/jcom_jan14_facilitate.pdf
Houlden, S., Hodson J.,Veletsianos, G., Reid, D., Thompson, C. (2021). The health belief model: How public health can address the misinformation crisis beyond COVID-19. Public Health in Practice. 2, 100151. https:// w ww.ncbi.nlm.nih.gov/pmc/articles/PMC8411835/pdf/main.pdf
HHU. (20 07). G*Power Analysis. https://www.psychologie.hhu.de/ arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/ gpower.html
International Business Machines. (2013). Statistical Package for the Social Services. https://www.ibm.com/analytics/spss-statistics-software
Jahanfar, S., Abedi, P., & Siahkal, S. F. (2021). Sexual behavior prevalence and its predictors among students in an American university. Sexuality & Culture. http://dx.doi.org/10.1007/s12119-021-09816-x
Journal of the New York State Nurses Association, Volume 49, Number 1 36
n Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
Kågesten A., Gibbs S., Blum R. W., Moreau, C., Chandra-Mouli, V., Herbert, A., & Amin, A., (2016). Understanding factors that shape gender attitudes in early adolescence globally: A mixed-methods systematic review. Public Library of Science One, 11(6), e0157805. https://doi.org/10.1371/journal.pone.0157805
Laranjo, L. (2016). Social media and health behavior change. Participatory Health Through Social Media, Elsevier, 83–111. https://doi.org/10.1016/ B978-0-12-809269-9.00006-2
Mercadante, A., & Law, A. (2021). Will they, or won’t they? Examining patients’ vaccine intention for flu and COVID-19 using the Health Belief Model. Research in Social and Administrative Pharmacy, 17(9), 1,596–1,605. https://doi.org /10.1016/j.sapharm.2020.12.012
National Research Council. (2015). Committee on improving the health, and well-being of young adults. Investing in the Health and WellBeing of Young Adults. Washington (DC): National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK284787/
Opoku-Acheampong, A. A., Kidd, T., Adhikari, K., Muturi, N., & Kattelmann, K. (2018). Assessing physical activity, fruit, vegetable, and sugar-sweetened beverage intake patterns of college students in Kansas. Journal of Nutrition Education and Behavior, 50 (10), 977–983 https://doi.org/10.1016/j.jneb.2018.02.001
Richards, N., Crockett, E., Morley, C., & Levandowski, B. (2020). Young women’s reproductive health conversations: Roles of maternal figures and clinical practices. Public Library of Science One. https://doi. org/10.1371/journal.pone.0228142
National Center for Advancing Translational Sciences. (2018). REDCap. https://ncats.nih.gov/expertise/clinical/redcap
Rosenstock I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the health belief model. Health Education Q., 15(2):175–183. https://doi.org/10.1371/journal.pone.022814210.1177/10901981 8801500203
Saghafi-Asl, M., Aliasgharzadeh, S., & AsghariJafarabadi, M. (2020.) Factors influencing weight management behavior among college students:
An application of the Health Belief Model. Public Library of Science One, 15(2): e0228058. https://doi.org/10.1371/journal. pone.0228058
Scull, T. M., Keefe, E. M., Kafka, J. M., Malik, C. V., & Kupersmidt, J. B. (2020). The understudied half of undergraduates: Risky sexual behaviors among community college students. Journal of American College Health, 68(3), 302–312. https://doi.org/10.1080/07448481.2 018.1549554
Siegel, K., & Meunier, E. (2019). Traditional sex and gender stereotypes in the relationships of non-disclosing behaviorally bisexual men. Archives of Sexual Behavior, 48(1), 333–345. https://doi.org/10.1007/ s10508-018-1226-3
Visalli, G., Cosenza, B., Mazzù, F., Bertuccio, M. P., Spataro, P., Pellicanò, G. F. & Facciolà, A. (2019). Knowledge of sexually transmitted infections and risky behaviours: A survey among high school and university students. Journal of Preventive Medicine and Hygiene, 60(2), E84–E92. https://doi.org/10.15167/2421-4248/jpmh2019.60.2.1079
Wang, D., Li, C., Wang, Y., Wang, S., Wu, S., Zhang, S., & Xu, L. (2021). Health education intervention on hearing health risk behaviors in college students. International Journal of Environmental Research and Public Health, 18, 1560. https://doi.org/10.3390/ijerph18041560
Weisberg, J., Conell, G., Verville, L., & Cancelliere, C. (2021). Brief action planning to facilitate the management of acute low back pain with radiculopathy and yellow flags: A case report. The Journal of the Canadian Chiropractic Association, 65(2), 212218. http://www.ncbi. nlm.nih.gov/pmc/articles/pmc8480372/World Health Organization. (2020). Sexual and reproductive health. https://www.who.int/ reproductivehealth/topics/sexual_health/sh_definitions/en/ Yi, S., Te, V., Pengpid, S., & Peltzer, K. (2018). Social and behavioural factors associated with risky sexual behaviours among university students in nine ASEAN countries: A multi-country cross-sectional study. SAHARA-J: Journal of Social Aspects of HIV/AIDS, 15(1), 71 –79. https://doi.org/10.1080/17290376.2018.1503967
Journal of the New York State Nurses Association, Volume 49, Number 1 37
n
Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
WHAT’S NEW IN HEALTHCARE LITERATURE
n Are You Up to Date on Cardiopulmonary Resuscitation Guidance?
n Brooks, M., & Vega, C.P. (2022, March 11). https://www.medscape.org/ viewarticle/969753
The American Heart Association, in collaboration with the American Academy of Pediatrics, the American Association for Respiratory Care, the Society of Critical Care Anesthesiologists, and the American Society of Anesthesiologists, have issued the 2022 Interim Guidance for Basic and Advanced Life Support in Adults, Children and Neonates with Suspected or Confirmed COVID-19. The updated guidance was published online January 24, 2022, in Circulation: Cardiovascular Quality and Outcomes.
Since the beginning of the pandemic, survival from cardiac arrest has declined. The severity of SARS-CoV-2 related cardiac arrest, termination of resuscitation guidance, crisis standards of care or delays in patients seeking medical care are some factors which may explain this decline. The goal of the guidance was to fully protect healthcare providers who perform resuscitation and emphasizes specific recommendations for in-hospital resuscitation.
Updates in the interim guidance focus on three principles:
1. Incorporating the most recent Centers for Disease Control and Prevention and World Health Organization guidance
l All healthcare providers should wear a respirator (e.g., N95) along with other PPE (gown, gloves, and eye protection) for patients with suspected or confirmed COVID-19 infection before performing aerosol-generating procedures (AGPs) or in a setting where such procedures are regularly performed. This may also apply to patients in cardiac arrest who tested negative for COVID-19 on admission. In
the event initial responders are not already wearing appropriate PPE, they should immediately don it and then begin CPR. (AGPs include chest compressions, defibrillation, bag-mask ventilation, intubation, and positive-pressure ventilation.)
2. Reinforcing resuscitation best practices
l Cardiac arrest survival is dependent on early initiation of CPR and performing chest compressions as soon as it is safely possible is recommended. Patients with confirmed or suspected COVID-19 should receive the best resuscitative efforts possible.
l Endotracheal medications should be avoided, as disconnections may be a source of aerosolization resulting from unfiltered exhalation.
l Manual compressions can be initiated while patients are in the prone position, with hands centered over the T7-T10 vertebral bodies.
l Suction should not be performed routinely for neonates with clear or meconium-stained amniotic fluid.For maternal resuscitation, if spontaneous circulation is not achieved within 5 minutes of arrest, perimortem cesarean delivery should be performed.
l Oxygenation with intubation should be prioritized earlier among pregnant women with COVID-19.
3. Ensuring adequate PPE supply
l Effective use of PPE is critical for the safety of healthcare providers performing resuscitations, and at this time, all healthcare providers should be following appropriate precautions and should have access to PPE in all clinical settings, regardless of the potential of encountering resuscitation events. (Brooks & Vega, 2022)
n New Contact Lens Elutes Antihistamine for Ocular Allergy
n Harrison, L. (2022, March 11). https://www.medscape.com/viewarticle /970151
The U.S. Food and Drug Administration has approved a new contact lens that slowly releases the antihistamine ketotifen as a treatment for ocular allergy. Already on the market in Canada and Japan, Acuvue Theravision With Ketotifenis are daily disposable contacts that can prevent ocular itch from allergic conjunctivitis. While able to correct vision, it is indicated for people who do not have red eyes, who are candidates for wearing contact lenses, and who do not have more than 1.00 D of astigmatism. Treatment with antihistamine eye drops for itching eyes due to allergies is contraindicated because eyedrop preservatives could interact with the lenses.
After over ten years of research, Johnson & Johnson developed an antihistamine drug (combination of ketotifen and etafilcon A) that integrates
into the contact lens polymer during manufacturing. Upon eye contact, sustained drug release from the contact lenses enter the tear film, then is absorbed into the ocular tissue. There are several beneficial effects. Typically, eye drops are quickly introduced to the eye, but the active drug is flushed out quickly. The slowly released drug has demonstrated several beneficial effects. Ketotifen, a well-established treatment of ocular allergies, blocks histamine receptors and stabilizes mast cells so they don’t release cytokines and prevents inflammatory cells from rushing to the site of irritation. With 20–40% of America’s population having seasonal allergies, Acuvue Theravision With Ketotifenis may offer significant relief from ocular allergy symptoms.
The lens contains no irritating preservatives and demonstrated minor brief discomfort when placed in the eye during clinical trials. Johnson & Johnson is researching other drugs that may be delivered through contact lens.
Journal of the New York State Nurses Association, Volume 49, Number 1 39
New In Healthcare Literature n
What’s
n
n ‘Bigorexia’: Why Teenage Boys Are Obsessed With Bulking Up
n Hochwald, L. (2022, March 10). https://www.medscape.com/viewarticle /970084
Teenage boys are under as much social pressure to have extreme bodies as girls. New studies point to a combination of factors, including the pandemic and social media, which have influenced adolescent boys to build superhero-size buff bodies. Beyond pursuit of a healthy body, boys often use supplements or steroids in order to grow muscle mass. Mental health professionals have used a new term ‘Bigorexia,’ which involves spending excessive time at the gym, preoccupation with protein diets, and having intense muscle-building goals. A concerning one-third of U.S. adolescents are trying to bulk up, according to a study published in the Journal of Adolescent Health.
“An everyday teen can become a celebrity,” says Jason Nagata, MD, a pediatrician who specializes in adolescent medicine at the University of California, San Francisco. “Then, thanks to social media algorithms, if a teenage boy likes or interacts with a post that features a muscular guy or is all about fitness, they’ll start getting all sorts of related content. They’ll get bombarded with tons of ads for protein shakes, for example,
as well as bodybuilding equipment, and that will further distort reality. Some of the most popular Instagram posts among teens feature people who have experienced a massive body transformation,” Nagata says. “It’s usually someone who lost a lot of weight or someone who was scrawny and then got muscular. The most drastic changes tend to get the most likes and are perpetuated the most and shared the most often with friends” (Hochwald, 2022).
Idealized before and after body pictures mislead viewers to believe extreme changes are real. These images can damage teenagers’ self-esteem and lead to anxiety, stress and poor body perception.
Red flags to watch out for
l Obsession with appearance, weight, food, or exercise.
l Withdrawal from friends and family out of concern for appearance
l Spending more time at the gym than with friends
l Asking parents to buy protein powder and no longer eating family meals because the food’s protein isn’t high enough or is too fatty.
n Resistance Exercise May Be Best Workout for a Good Night’s Sleep
n Wendling, P. (2022, March 10). https://www.medscape.com/viewarticle /970082
Recent research suggests resistance exercise yields better sleep than other workouts among inactive adults, especially those who are poor sleepers. Study results were presented at the Epidemiology, Prevention/ Lifestyle & Cardiometabolic Health (EPI|Lifestyle) 2022 Conference sponsored by the American Heart Association (AHA).
Even before the pandemic and bedtime “doom scrolling” became habitual, a third of Americans regularly had less than 7 hours of sleep. Aerobic exercise has been long known to improve sleep and promote cardiovascular health. However, little is known on how it compares with other types of exercise in the general population.
Researchers recruited 406 inactive adults, aged 35 to 70 years, who were obese or overweight (mean body mass index, 31.2 kg/m 2) and had elevated or stage 1 hypertension. They were randomly assigned to complete no exercise or 60 minutes of supervised aerobic, resistance, or
combination exercise three times per week for 12 months. Adherence to exercise over the year was 84%, 77%, and 85%, respectively. Participants also completed the Pittsburgh Sleep Quality Index (PSQI) at baseline and 12 months. Among the 386 participants (53% women) with evaluable data, 35% had poor-quality sleep and 42% regularly slept less than 7 hours per night. Sleep duration at 12 months, on average, increased by 13 minutes in the resistance-exercise group, decreased by 0.6 minute in the aerobicexercise group, increased by 2 minutes in the combined-exercise group, and increased by 4 minutes in the control group.
Among participants who got less than 7 hours of sleep at baseline, however, sleep duration increased by 40 minutes, compared with increases of 23 minutes in the aerobic group, 17 minutes in the combined group, and 15 minutes in the control group. Among poor-quality sleepers at baseline, resistance exercise significantly improved sleep quality and duration, compared with the control group. It also improved sleep efficiency by 9.0%, compared with 0.9% in the control group and 8.0% for the combinedexercise group.
n Clinical Guidelines for the Prevention and Control of MRSA in Healthcare Facilities
n Healthcare Infections Society (HIS) and Infection Prevention Society (IPS). (2022, February 1). https://reference.medscape.com/viewarticle/967593
“In October 2021, the Healthcare Infection Society (HIS) and the Infection Prevention Society (IPS) jointly published clinical guidelines for the prevention and control of methicillin-resistant Staphylococcus aureus (MRSA) in healthcare facilities.”
Patient screening
l At a minimum, patients should be screened for MRSA, based on certain criteria.
l Universal screening may be indicated, depending on local circumstances.
l If a patient undergoes decolonization therapy, consider determining
Journal of the New York State Nurses Association, Volume 49, Number 1 40 n What’s New In The Healthcare Literature
the success of decolonization with repeat MRSA screening 2–3 days after therapy. Surgery should not be delayed if repeat screening remains positive.
Staff screening and management
l For employees with positive test results, consider also screening the throat, hairline, and groin/perineum, because if positive, the risk increases for shedding into the environment and MRSA transmission.
l Develop workplace policies regarding exclusion from work and return of staff colonized with MRSA incorporating the worker’s risk for transmission to patients.
Decolonization therapy
l To decolonize the skin, moisten the skin, apply 4% chlorhexidine wash, and leave for 1–3 minutes before washing off. If using 2% chlorhexidine wipes, do not rinse off.
Environmental sampling and cleaning/disinfection
l Although routine screening/sampling of the environment is not necessary, surveillance should be performed in accordance with the hospital’s infection control strategy and in compliance with mandatory national requirements.
Standard vs. contact precautions and the use of isolation/cohorting
l Consider placing these patients in a single room and on contact precautions, based on the extent of their colonization or infection and their risk for transmission to others.
n Knee Osteoarthritis
Patient transfer and transport
l Unless it is clinically necessary, patients should not be transferred between hospitals, hospital wards and units, or other clinical settings. If transfer or transport is needed, the receiving party and the ambulance/ transport service should be notified that the patient is colonized/ infected with MRSA.
Shared equipment
l Shared equipment should be cleaned and disinfected after each use.
l All healthcare workers should know cleaning and decontaminating requirements.
l Staff, patients, and visitors must clean hands before and after using shared equipment.
Patient information
l Patients should be notified of their screening result as soon as possible.
l Patients who are MRSA positive may be informed about the difference between colonization and infection, the microorganism, how MRSA is acquired and transmitted, how it is treated, and the reasons for contact precautions or isolation.
l Discharge planning and education should include thorough information about risks to household members, friends, and family, as well as the implications for the patient’s future health and health care.
Clinical Practice Guidelines
n American Academy of Orthopaedic Surgeons. (2021, November 2). https://reference.medscape.com/viewarticle/961808
“Clinical practice guidelines on knee osteoarthritis (nonarthroplasty) were published in August 2021 by the American Academy of Orthopaedic Surgeons (AAOS).”
To improve pain and function for patients with osteoarthritis of the knee, the following are recommended:
l The use of canes and braces
l Unless contraindicated, topical application of nonsteroidal antiinflammatory drugs (NSAIDs) or oral administration of NSAIDS or Tylenol
l Exercise routines (i.e., supervised, unsupervised, and/or aquatic) are recommended versus no exercise.
l Balance, agility, and coordination programs can be used in combination with traditional exercise practices to improve walking speed and performance-based function.
l Education programs on self-management and general education of the condition
l In patients who are overweight or obese, sustained weight loss is beneficial.
Not recommended:
l Oral narcotics (including tramadol), as they are not effective at improving pain or function and their use results in a significant increased risk of adverse events
l Routine use of intra-articular injection(s) of hyaluronic acid: Intraarticular injections of corticosteroids may provide some short-term relief for symptomatic knee osteoarthritis.
Journal of the New York State Nurses Association, Volume 49, Number 1 41
n Big Missed Opportunities for BP Control in Premenopausal Women
n Wendling, P. (2022, March 11). https://www.medscape.com/ viewarticle/970183#vp_2
A recent report suggests limited regular access to health care has widened gaps in the awareness, treatment, and control of hypertension in premenopausal women in the United States. In a large, inclusive sample from the National Health and Nutrition Examination Survey (NHANES) of 3,343 women aged 35 to 54 years with no prior cardiovascular disease, representing an estimated 31.6 million American women, hypertension prevalence increased 8%. This represents an estimated increase from 15.2 million women between 2011 and 2014 to 16.4 million women between 2015 and 2018.
Study author Susan Hennessy, PhD, said at the Epidemiology, Prevention/Lifestyle & Cardiometabolic Health 2022 Conference, “There’s been no improvement over the past decade and there is evidence of race/ ethnic disparities.” Among non-Hispanic Black women and Hispanic women, over half of the missed opportunities to control hypertension occurred because these women have no regular access to health care. In women who identified as “other,” which includes non-Hispanic Asian and mixed-race populations, the uncontrolled prevalence reached 70%.
Dr. Hennessy reminded conference attendees that cardiovascular disease (CVD) is the number-one killer of women in the United States and
that CVD risk, mediated through hypertension, increases after menopause. Thus, managing hypertension prior to this life event is an important element of primary prevention of CVD and should be a priority.
Missed opportunities for hypertension control in these premenopausal women were:
l Lack of awareness of their hypertension in 23%
l Ineffective treatment in 34%
l Lack of healthcare access in 43%, increasing to 51% in non-Hispanic Black and 56% in Hispanic patients
l Prevalence of uncontrolled hypertension was 54% in non-Hispanic Black women and 66% in Hispanic women.
Conference session moderator Sadiya S. Khan, MD, said that the findings should raise “alarm and concern that hypertension is not just a disease of the old but very prevalent in younger women, particularly around the time of pregnancy. And this is a clear driver of maternal morbidity and mortality as well.”
Authors called for access to community-based blood pressure screening, home blood pressure machines with appropriate-sized cuffs as well as increased access to health care, particularly for women.
Black Patients Still Underrepresented in Clinical Trials
n Carroll, L. (2022, March 11) https://www.medscape.com/viewarticle /970050
A recent study finds that Black patients remain underrepresented in U.S. clinical trials despite the Food and Drug Administration (FDA) 2015 initiation of a 5-year plan to improve the situation. Clinical trials are the source of data on new medications, guiding regulatory approval and public use. To ensure new medicines are safe and beneficial for all, participants in clinical trials must represent the broader population.
The study, based on data extracted from the FDA’s Snapshots program included the drug’s name, the manufacturer, the approval date, the indication, the National Clinical Trial identifier number, the trial start date, the numbers of Black and white participants, and racial differences, if any, in benefits and side effects. The researchers found that Black participants
were underrepresented in 85% of the trials and in all disease categories except for psychiatry. Trials for cardiovascular disease treatments had the lowest Black participation.
“There’s no question that more diversity is needed in clinical trials,” said Dr. Otis Brawley, professor of oncology and epidemiology at the Johns Hopkins School of Medicine and the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland. “And we need to keep an eye out for side effects and how various populations respond to our medications,” Dr. Brawley told Reuters Health by phone.
“Race, however, is a sociopolitical categorization, not a biological categorization. The FDA rules imply that race is biological. To assume race is biological is racist. Rather than race, researchers should be focusing on diversity based on geographic origin,” Dr. Brawley said.
Journal
49, Number 1 42
of the New York State Nurses Association, Volume
n CE Activity: Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper
Thank you for your participation in “Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID19 Pandemic: A Theory-Guided Paper” a new continuing education (CE) activity offered by NYSNA. NYSNA members and nonmembers are invited to take part in this activity, and you do not need to be a resident of New York State.
INSTRUCTIONS
In order to receive contact hours for this educational activity, participants are to read the article presented in this issue of The Journal, complete and return the post-test, evaluation form, and earn 80% or better on the post-test.
This activity is free to NYSNA members and $10 for nonmembers. Participants can pay by check (made payable to NYSNA) or credit card. The completed answer sheet and evaluation form may be mailed or faxed back to NYSNA; see the evaluation form for more information.
The New York State Nurses Association is accredited as a provider of nursing continuing professional development by the American Nurses Credentialing Center's Commission on Accreditation.
This program has been awarded 1 CH through the New York State Nurses Association Accredited Provider Unit.
The New York State Nurses Association is accredited by the International Accreditors for Continuing Education and Training “IACET” and is authorized to issue the IACET CEU.
The New York State Nurses Association is authorized by IACET to offer 0.1 CEUs for this program.
Declaration of Vested Interest: None
NYSNA wishes to disclose that no commercial support or sponsorship was received.
NYSNA Program Planners, Presenters, and Content Experts declare that they have no financial relationship with an ineligible company.
In order to receive Contact Hours and CEUs, participants must read the entire article, fill out the evaluation, and get 80% or higher on the post-test.
INTRODUCTION
Breastfeeding during infancy is associated with lower rates of obesity, diabetes, and certain kinds of cancers later in life. Racial minority and economically marginalized Black infants are at a disproportionately higher risk for several preventable health problems than white infants. According to the Centers for Disease Control and Preventions (CDC), 73.7% of Black infants are breastfed in comparison to 86.7% of white infants. This disparity stems from healthcare system inequities and non-supportive maternal social networks. COVID-19 disrupted healthcare delivery and social networks, leaving mothers and infants in an even more vulnerable position. Disparities in breastfeeding knowledge, inadequate access to lactation care, limited or inadequate staff training, unsupportive hospital policies and procedures, lack of social network support, and COVID-19-related challenges are all
significant barriers to breastfeeding. Currently, nurses and advanced practice nurses lack knowledge about how or why they may promote breastfeeding for underserved Black communities. Nurse practitioners are in the position to lead a comprehensive support structure aimed to promote breastfeeding. This theory-guided paper proposed breastfeeding sponsorship program and links outpatient with inpatient services, as well as social support. This would be a plausible way to increase infant access to breastfeeding.
LEARNING OUTCOME
Participants will identify some of the benefits of a professional lactation assistance program.
OBJECTIVES
By completion of the article, the reader will be able to:
1. Identify barriers to infant breastfeeding in economically disadvantaged Black communities.
2. Recognize components of a breastfeeding sponsorship program.
Please answer either True or False to the questions below. Remember to complete the answer sheet by putting the letter of your corresponding answer next to the question number. Each question has only one correct answer.
The 1.0 contact hour and 0.1 CEU for this program will be offered until June 1, 2025.
1) A mother’s social support network has minimal impact on successful breastfeeding. a. True b. False
2) Hospitals that serve high-income Black communities have lower rates of breastfeeding initiation occur during a new mother’s hospital stay. a. True b. False
3) Disparities in access to professional lactation assistance negatively affects impoverished Black communities’ ability to breastfeed.
a. True b. False
4) The employment rate for Black mothers is the highest for women of all races.
a. True b. False
Journal
Volume 49, Number 1 43
of the New York State Nurses Association,
5) A support structure that includes increased access to professional lactation consultants can help improve breastfeeding outcomes.
a. True
b. False
6) Peer-based breastfeeding sponsorship has been successfully applied to increase a mother’s chance for successful breastfeeding..
a. True b. False
7) Commercial baby formula campaigns during the 1800s adversely influenced people’s perceptions of infant feeding, stigmatizing breastfeeding as a choice for women who could not afford baby formula.
a. True b. False
8) A breastfeeding sponsor, serving as a contemporary companion, can provide critical support during early motherhood for those who lack social support when breastfeeding.
a. True b. False
9) Communication among mothers and members of their support team is not necessary for successful breastfeeding.
a. True b. False
10) Breastfeeding protects infants against infections and childhood obesity, while reducing postpartum depression for mothers.
a. True b. False
Journal of the New York State Nurses Association, Volume 49, Number 1 44
Theory-Guided Paper
First Name: MI: Last Name: Street Address: City: State: ZIP Code: Daytime Phone Number (Include area code): Email: Profession: Currently Licensed in NY State? Y / N (Circle one) NYSNA Member # (if applicable): License #: License State: ACTIVITY FEE: Free for NYSNA members/$10 nonmembers
PAYMENT METHOD Check—payable to New York State Nurses Association (please include “Journal CE” on your check). Credit Card: Mastercard Visa Discover American Express Card Number: Expiration Date: / CVV# Name: Signature: Date: / /
Journal of
Association, Volume 49, Number 1 45
the New York State Nurses
The Journal of the New York State Nurses Association, Vol. 49, No. 1 Answer Sheet Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A
your answers
the spaces
1._________ 6._________ 2._________ 7._________ 3._________ 8._________ 4._________ 9._________ 5. _________ 10._________
print legibly and verify that all information is correct.
Note: The 1.0 contact hour and 0.1 CEU for this program will be offered until June 1, 2025. Please print
in
provided below. There is only one answer for each question.
Please complete the answer sheet above and course evaluation form on reverse. Submit both the answer sheet and course evaluation form along with the activity fee for processing. Mail to: NYSNA, attn. Nursing Education and Practice Dept. 131 West 33rd Street, 4th Floor, New York, NY 10001 Or fax to: 212-785-0429 Please
The Journal of the New York State Nurses Association, Vol. 49, No. 1
Learning Activity Evaluation
Breastfeeding Disparities Among Communities Lacking Access to Lactation Consultants During the COVID-19 Pandemic: A Theory-Guided Paper
Please use the following scale to rate statements 1–7 below:
Poor Fair Good Very Good Excellent
1. The content fulfills the overall purpose of the CE Activity.
2. The content fulfills each of the CE Activity objectives.
3. The CE Activity subject matter is current and accurate.
4. The material presented is clear and understandable.
5. The teaching/learning method is effective.
6. The test is clear and the answers are appropriately covered in the CE Activity.
7. How would you rate this CE Activity overall?
8. Time to complete the entire CE Activity and the test? ____ Hours (enter 0–99) _____ Minutes (enter 0–59)
9. Was this course fair, balanced, and free of commercial bias? Yes / No (Circle one)
10. Comments:
11. Do you have any suggestions about how we can improve this CE Activity?
Journal of the New
State
Volume 49, Number 1 46
York
Nurses Association,
n
CE Activity: Venting
the Truth About
Thank you for your participation in “Venting the Truth About COVID19: A Report on the Struggles of NYSNA Nurses During the COVID-19 Pandemic,” a new continuing education (CE) activity offered by NYSNA. NYSNA members and nonmembers are invited to take part in this activity, and you do not need to be a resident of New York State.
INSTRUCTIONS
In order to receive contact hours for this educational activity, participants are to read the article presented in this issue of The Journal, complete and return the post-test and evaluation form, and earn 80% or better on the post-test.
This activity is free to NYSNA members and $10 for nonmembers. Participants can pay by check (made payable to NYSNA) or credit card. The completed answer sheet and evaluation form may be mailed or faxed back to NYSNA; see the evaluation form for more information.
The New York State Nurses Association is accredited as a provider of nursing continuing professional development by the American Nurses Credentialing Center's Commission on Accreditation.
This program has been awarded 1 CH through the New York State Nurses Association Accredited Provider Unit.
The New York State Nurses Association is accredited by the International Accreditors for Continuing Education and Training “IACET” and is authorized to issue the IACET CEU.
The New York State Nurses Association is authorized by IACET to offer 0.1 CEUs for this program.
Declaration of Vested Interest: None NYSNA wishes to disclose that no commercial support or sponsorship was received.
NYSNA Program Planners, Presenters, and Content Experts declare that they have no financial relationship with an ineligible company.
In order to receive Contact Hours and CEUs, participants must read the entire article, fill out the evaluation, and get 80% or higher on the post-test.
INTRODUCTION
During Florence Nightingale’s service in the Crimean War, she determined that problems such as high mortality could be reduced when the causes were determined and specifically addressed. She advocated for real-time monitoring of mortality incidence rates and holding healthcare entities accountable for patient outcomes. Aware of how inferior hospital conditions impacted nurses and patients, she called for reforms such as better hospital ventilation and reducing overcrowding. The COVID19 pandemic brought to light the many fractures in the United States’ healthcare system, including lack of emergency preparedness, inadequate critical supplies, limited capacity within various patient care settings, inequities in health determinants for minority populations, and mistrust among healthcare staff, the public, and the government. The article bears witness to the events of the COVID-19 pandemic through the lens of Florence Nightingale’s call for healthcare reform.
COVID-19:
A Report on the Struggles of NYSNA Nurses During the
COVID-19 Pandemic
LEARNING OUTCOME
Participants will identify and compare areas of similarity between nursing during the Crimean War as observed by Florence Nightingale and the COVID-19 pandemic, representing non-conformity with Florence Nightingale’s visions for healthcare reform.
OBJECTIVES
By completion of the article, the reader will be able to:
1. Identify New York State healthcare facilities’ organizational responses and failures in emergency preparedness and the COVID-19 pandemic.
2. Identify critical thinking and problem analyses needed in emergencies and public health crises such as pandemics and times of conflict.
3. Identify interventions that can create positive outcomes related to emergency preparedness and the ongoing COVID-19 pandemic.
4. Identify common deficiencies in documentation, the collection of data, and the use of statistical analysis to make improvements in patient care and worker safety through the ongoing phases of the COVID-19 pandemic and the Crimean War.
5.Identify existing deficiencies in the NY Healthcare system that can lead to further negative outcomes for the nursing workforce.
6. Identify the methods of political advocacy needed for the survival of nursing and healthcare reform.
Please answer either True or False to the questions below. Remember to complete the answer sheet by putting the letter of your corresponding answer next to the question number. Each question has only one correct answer.
The 1.5 contact hours and 0.2 CEU for this program will be offered until June 1, 2025.
1) The article highlights that the prevailing work culture of medical institutions currently prevent nurses’ participation in system-level problem-solving and forces them to create work arounds in collaboration with close work friends to deliver timely, needed patient care.
a. True b. False
2) The application of administrative controls, such as standardization and enforcement of procedures for triaging and cohorting patients, could reduce employee workplace acquired COVID-19 infection.
a. True b. False
3) Worker occupational illness and injury were recorded accurately by employers during the Crimean War and COVID-19 pandemic.
a. True b. False
Journal of the New
Association, Volume 49, Number 1 47
York State Nurses
4) Instituting state-mandated safe nurse-to-patient ratios would reduce nurse infection rates and improve patient outcomes.
a. True b. False
5) Nurse unions helped members overcome fear during the pandemic, enabling them to advocate for patients and themselves.
a. True b. False
6) Nurse unions amplified nurses’ voices and obtained needed support through advocacy for federal law and filing lawsuits.
a. True b. False
7) Facility infection rates of nurses at examined healthcare facilities in New York State were higher in rural areas than in urban areas.
a. True b. False
8) The majority of nurses who experienced long COVID were pressured to return to work before their symptoms were gone.
a. True b. False
9) Early COVID-19 viral transmission classification as airborne vs. droplet was clearly communicated and did not create confusion.
a. True b. False
10) Creation of 90-day stockpiles for personal protection equipment and vital equipment would ensure supply availability during times of supply chain disruption or surge in demand for supplies.
a. True b. False
Journal of the New York State Nurses Association, Volume 49, Number 1 48
First Name: MI: Last Name: Street Address: City: State: ZIP Code: Daytime Phone Number (Include area code): Email: Profession: Currently Licensed in NY State? Y / N (Circle one) NYSNA Member # (if applicable): License #: License State: ACTIVITY FEE: Free for NYSNA members/$10 nonmembers
PAYMENT METHOD
Check—payable to New York State Nurses Association (please include “Journal CE” on your check). Credit Card: Mastercard Visa Discover American Express Card Number: Expiration Date: / CVV# Name: Signature: Date: / /
Journal of
Volume 49, Number 1 49
the New York State Nurses Association,
The Journal of the New York State Nurses Association, Vol. 49, No. 1 Answer Sheet Venting the Truth About COVID-19: A Report on the Struggles of NYSNA Nurses During the COVID-19 Pandemic
the
1._________ 6._________ 2._________ 7._________ 3._________ 8._________ 4._________ 9._________ 5. _________ 10._________
print legibly and verify that all information
Note: The 1.5 contact hours and 0.2 CEU for this program will be offered until June 1, 2025. Please print your answers in
spaces provided below. There is only one answer for each question.
Please complete the answer sheet above and course evaluation form on reverse. Submit both the answer sheet and course evaluation form along with the activity fee for processing. Mail to: NYSNA, attn. Nursing Education and Practice Dept. 131 West 33rd Street, 4th Floor, New York, NY 10001 Or fax to: 212-785-0429 Please
is correct.
The Journal of the New York State Nurses Association, Vol. 49, No. 1
Learning Activity Evaluation
Venting the Truth About COVID-19: A Report on the Struggles of NYSNA Nurses During the COVID-19 Pandemic
Please use the following scale to rate statements 1–7 below:
Poor Fair Good Very Good Excellent
1. The content fulfills the overall purpose of the CE Activity.
2. The content fulfills each of the CE Activity objectives.
3. The CE Activity subject matter is current and accurate.
4. The material presented is clear and understandable.
5. The teaching/learning method is effective.
6. The test is clear and the answers are appropriately covered in the CE Activity.
7. How would you rate this CE Activity overall?
8. Time to complete the entire CE Activity and the test? ____ Hours (enter 0–99) _____ Minutes (enter 0–59)
9. Was this course fair, balanced, and free of commercial bias? Yes / No (Circle one)
10. Comments:
11. Do you have any suggestions about how we can improve this CE Activity?
Journal of the New York State
Association, Volume 49, Number 1 50
Nurses
n CE Activity: Sexual Well-Being and Screening
for Risky Sexual Behaviors: A
Quantitative Retrospective Study
Thank you for your participation in “Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study,” a new continuing education (CE) activity offered by NYSNA. NYSNA members and nonmembers are invited to take part in this activity, and you do not need to be a resident of New York State.
INSTRUCTIONS
In order to receive contact hours for this educational activity, participants are to read the article presented in this issue of The Journal, complete and return the post-test and evaluation form, and earn 80% or better on the post-test.
This activity is free to NYSNA members and $10 for nonmembers. Participants can pay by check (made payable to NYSNA) or credit card. The completed answer sheet and evaluation form may be mailed or faxed back to NYSNA; see the evaluation form for more information.
The New York State Nurses Association is accredited as a provider of nursing continuing professional development by the American Nurses Credentialing Center's Commission on Accreditation.
This program has been awarded 1 CH through the New York State Nurses Association Accredited Provider Unit.
The New York State Nurses Association is accredited by the International Accreditors for Continuing Education and Training “IACET” and is authorized to issue the IACET CEU.
The New York State Nurses Association is authorized by IACET to offer 0.1 CEUs for this program.
Declaration of Vested Interest: None NYSNA wishes to disclose that no commercial support or sponsorship was received.
NYSNA Program Planners, Presenters, and Content Experts declare that they have no financial relationship with an ineligible company.
In order to receive Contact Hours and CEUs, participants must read the entire article, fill out the evaluation, and get 80% or higher on the post-test.
INTRODUCTION
In a 2018 report, the Centers for Disease Control and Prevention (CDC) indicated that 1 in 5 people in the United States had a sexually transmitted infection (STI). College-aged students or young adults are disproportionately affected by STIs, resulting in preventable illnesses, unplanned pregnancies, and billions of dollars in medical costs. This age group seeks health information from peers and social media if they feel disconnected from their healthcare providers. Misinformed young adults may have a false perception of low risk regarding sexually transmitted infection and unplanned pregnancy, rendering them vulnerable to otherwise preventable consequences. Sexual health resources that are readily available and accessible to young adults can result in reduction of STIs and unplanned pregnancies. Nurse practitioners and nurses are well positioned to provide educational resources and programs that target risk misperceptions and address ways to empower young adults to make safe
sexual health decisions. Characteristics of students who practice high-risk sexual behaviors is explored by the authors in this article. The use of brief action planning (BAP) as a method to modify risky sexual health behaviors among college-age students is studied in this article.
LEARNING OUTCOME
Participants will identify characteristics of college-age students with risky sexual behavior with regard to efficacy of brief action planning as a tool for changing risky behaviors.
OBJECTIVES
By completion of the article, the reader will be able to:
1. Identify risky sexual behaviors among college-age students.
2. Identify characteristics of students engaging in risky sexual behaviors.
3. Identify a method for changing risky behaviors.
4. Identify efficacy of BAP in reducing risky sexual behavior among college-age students.
Please answer either True or False to the questions below. Remember to complete the answer sheet by putting the letter of your corresponding answer next to the question number. Each question has only one correct answer.
The 1.0 contact hour and 0.1 CEU for this program will be offered until June 1, 2025.
1) Most students who reported risky sexual behaviors at their wellness screening were willing to modify health behaviors other than risky sexual health behaviors. a. True b. False
2) The authors suggest that having an open and nonjudgmental community allows students to feel safe enough to honestly disclose sexual activity a. True b. False
3) The riskiest sexual behaviors were found among 19-year-olds. a. True b. False
4) Young adults develop gender norms early in teenage years, which can predispose them to participate in risky sexual behaviors.
a. True
b. False
Journal of the New
Association, Volume 49, Number 1 51
York State Nurses
5) Young adults feel apprehensive toward healthcare providers if any type of discrimination occurs and can lead them to seek out sexual health information from peers or social media instead.
a. True b. False
6) Use of brief action planning (BAP) decreases the likelihood of behavior change.
a. True b. False
7) The Health Belief Model (HBM) attempts to predict and describe why individuals modify or maintain their health behaviors.
a. True b. False
8) The HBM suggests that a person’s perception of a threat from disease and the belief in the effectiveness of the recommended behavior will predict the likelihood that the individual will adopt the new behavior. a. True b. False
9) The authors suggest that students may not value using protection because they feel safe knowing that free STI testing and Plan B contraception is available on campus. a. True b. False
10) The study found that females were more likely to have unprotected sex and that males were more likely to have multiple partners. a. True b. False
Journal of the New York State Nurses Association, Volume 49, Number 1 52
Sexual
The Journal of the New York State Nurses Association, Vol. 49, No. 1
Answer Sheet
Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
Note: The 1.0 contact hour and 0.1 CEU for this program will be offered until June 1, 2025.
Please print legibly and verify that all information is correct.
First Name: MI: Last Name: Street Address: City: State: ZIP Code: Daytime Phone Number (Include area code): Email: Profession: Currently Licensed in NY State? Y / N (Circle one) NYSNA Member # (if applicable): License #: License State: ACTIVITY FEE: Free for NYSNA members/$10 nonmembers
PAYMENT METHOD
Check—payable to New York State Nurses Association (please include “Journal CE”on your check). Credit Card: Mastercard Visa Discover American Express Card Number: Expiration Date: / CVV# Name: Signature: Date: / /
Journal
Volume 49, Number 1 53
of the New York State Nurses Association,
1._________ 6._________ 2._________ 7._________ 3._________ 8._________ 4._________ 9._________ 5. _________ 10._________
Please print your answers in the spaces provided below. There is only one answer for each question.
Please complete the answer sheet above and course evaluation form on reverse. Submit both the answer sheet and course evaluation form along with the activity fee for processing. Mail to: NYSNA, attn. Nursing Education and Practice Dept. 131 West 33rd Street, 4th Floor, New York, NY 10001 Or fax to: 212-785-0429
The Journal of the New York State Nurses Association, Vol. 49, No. 1
Learning Activity Evaluation
Sexual Well-Being and Screening for Risky Sexual Behaviors: A Quantitative Retrospective Study
Please use the following scale to rate statements 1–7 below:
Poor Fair Good Very Good Excellent
1. The content fulfills the overall purpose of the CE Activity.
2. The content fulfills each of the CE Activity objectives.
3. The CE Activity subject matter is current and accurate.
4. The material presented is clear and understandable.
5. The teaching/learning method is effective.
6. The test is clear and the answers are appropriately covered in the CE Activity.
7. How would you rate this CE Activity overall?
8. Time to complete the entire CE Activity and the test? ____ Hours (enter 0–99) _____ Minutes (enter 0–59)
9. Was this course fair, balanced, and free of commercial bias? Yes / No (Circle one)
10. Comments:
11. Do you have any suggestions about how we can improve this CE Activity?
Journal of the New York State Nurses Association, Volume 49, Number 1 54
THE
JOURNAL
of the New York State Nurses Association
Call for Papers
The Journal of the New York State Nurses Association is currently seeking papers.
Authors are invited to submit scholarly papers, research studies, brief reports on clinical or educational innovations, and articles of opinion on subjects important to registered nurses. Of particular interest are papers addressing direct care issues. New authors and student authors are encouraged to submit manuscripts for publication.
Information for Authors
For author’s guidelines and submission deadlines, go to the publications area of www.nysna.org or write to journal@nysna.org
Call for Editorial Board Members
Help Promote Nursing Research
The Journal of the New York State Nurses Association is currently seeking candidates interested in becoming members of the publication’s Editorial Board.
Members of the Editorial Board are appointed by the NYSNA Board of Directors and serve one 6-year term. They are responsible for guiding the overall editorial direction of The Journal and assuring that the published manuscripts meet appropriate standards through blinded peer review.
Prospective Editorial Board members should be previously published and hold an advanced nursing degree; candidates must also be current members of NYSNA. For more information or to request a nomination form, write to journal@nysna.org
Journal of the New York State Nurses Association, Volume 49, Number 1 55
131
1073 NON-PROFIT ORG. US POSTAGE PAID CENTURY DIRECT
West 33rd Street, 4th Fl., New York, NY 10001