

CALL





Welcome
To the latest edition of Your Call
Welcome to the latest edition of Your Call.
Our magazine is a platform to celebrate the people within our service and the impact they have, both on and off duty - in uniform, in headsets, helping patients, or behind the scenes.
This edition is full of personal stories, experiences, and special moments. You’ll read about Paramedic Brent Kenny’s quick thinking and how the use of a body-worn camera helped protect a member of the public.
Education Manager Simon Buckley reflects on how sleep is often underrated, while Paramedic Bethany shares her journey to representing Great Britain at the Women’s European Baseball Championships over the summer.
We have also included a powerful, globe-trotting piece from Regional Community and Engagement Lead Mark Evans and Paramedic Paul Atherton, who volunteered their time to help strengthen ambulance services in Africa.
And you’ll also meet Fire Safety Manager Kev, who, outside of his ambulance service role, also serves as the official town crier for Sefton. It’s a unique role that reflects the diverse interests and community involvement of our colleagues beyond their day jobs.
This isn’t your typical corporate magazine or newsletter. Your Call is about people. It’s about shared human experiences. We hope it makes you smile, reflect, and maybe even feel a little prouder to be part of, or connected to, us.
Enjoy the read!
Your Call Magazine Team
Do you have a story to share with us? If so, please get in touch by emailing: communications@nwas.nhs.uk
Note:
One step at a time, from care homes to the ambulance service
Renée House joined our patient transport service after attending one of our ambulance awareness days and is now working to become a paramedic.
Lynch Syndrome and life-saving screening
Mike, from our Patient Safety Team, shares his story of being diagnosed with Lynch Syndrome, a genetic condition that increases cancer risk.
Mama bear at work Cath Boylan, EOC Shift Supervisor, become a true “work mum” to Jackie Porter, supporting her through an ADHD diagnosis which has helped her to adapt her work environment.




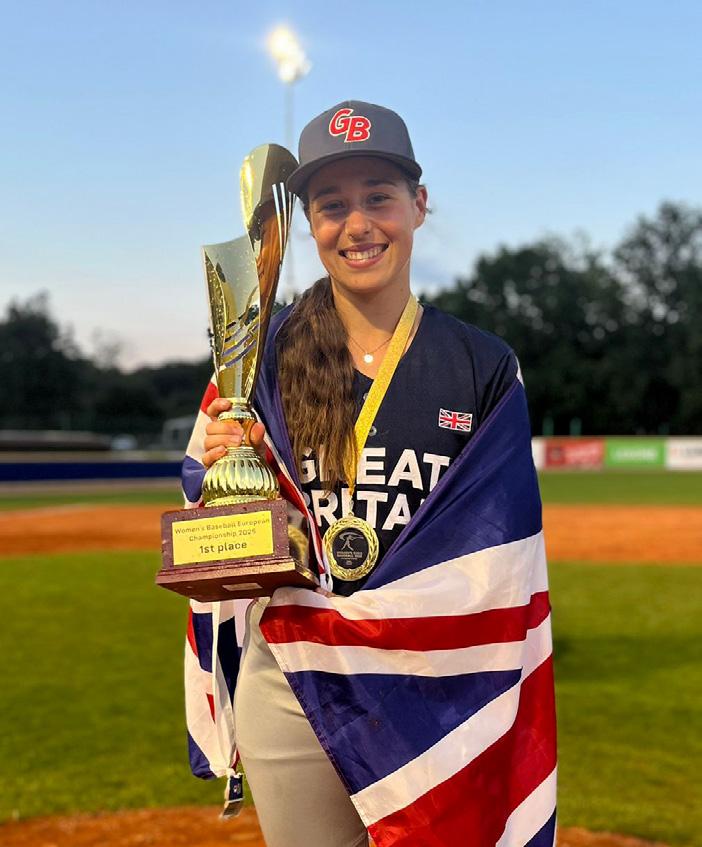
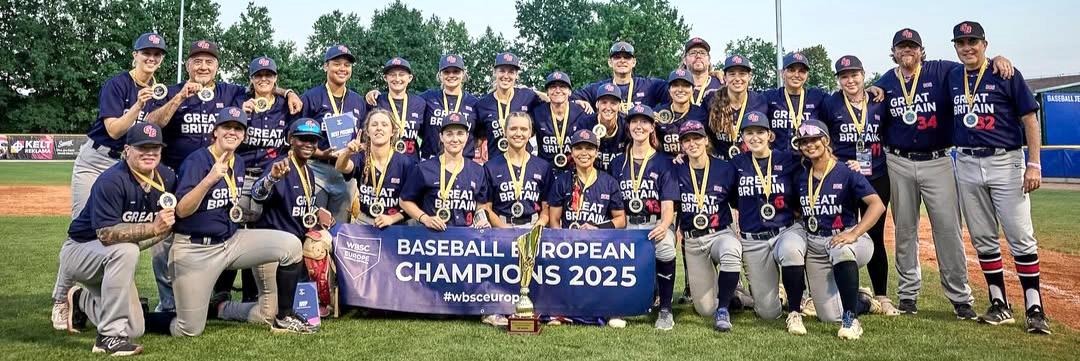
Representing Great Britain
Bethany’s journey to winning the European Baseball Championships
When she’s not responding to emergency calls in Cumbria, Paramedic Bethany Casson is usually training on the baseball field. This summer, she prepared for one of the biggest moments of her sporting life, which was representing Great Britain at the Women’s European Baseball Championships in the Czech Republic. The team went on to win the tournament.
“It was a huge honour,” she says. “And something I’ve worked incredibly hard for, balancing full-time shifts, training, and preparation over the past few years.”
Baseball first entered Bethany’s life around five years ago when she was studying for her paramedic degree at the University of Central Lancashire. A chance introduction quickly turned into a deep passion. She joined both the baseball and softball teams at university, competing in three national university championships, captaining teams, and working to get more women involved in the sport.
Since then, she’s continued to climb the ranks, playing for the Manchester Jetts women’s team and the Liverpool Trojans co-ed team in the British Baseball Federation leagues. Competing in both women’s and mixed teams has pushed her game further and developed her skills as a hitter and outfielder. For her, the sport offers something different.
“Baseball is the perfect mix of strategy, athleticism, and mental focus,” she says. “Every pitch matters. There’s a real intensity, but also a strong sense of community. It gives me balance, especially when work gets tough.”

That balance has propelled her to elite training opportunities, including the MLB EDGE training camp in London, which is an invite-only event attended by just 16 female athletes from across the UK. She trained with the GB national team coaches in Leicester and London, gaining experience and sharpening her performance in preparation for the recent international competition.
The 2025 Women’s European Baseball Championships took place from 14 to 17 August in Hluboká, Czech Republic. Team GB competed against some of the topranked teams in the sport, including the Netherlands, France, and the Czech Republic and they won. It’s the highest level of women’s baseball in Europe, and an exciting milestone not just for the team, but for the sport’s future in the UK.
For Bethany, this journey is about more than personal achievement. It’s about visibility and progress. “Women’s baseball is still an emerging sport in the UK, but with more support and awareness, I know we can grow it,” she says. “Being part of Team GB and winning this summer means I get to play a role in that. Hopefully, it encourages someone else to give it a go.”
Well done to Bethany and the GB team!

“Thankfully, I was there to help and prevent something more serious from happening.”
Paramedic saves woman from attacker

A paramedic is advocating the use of bodyworn cameras after his intervention led to the conviction of a man who assaulted a woman in the street.
Advanced paramedic Brent Kenny was stopped at traffic lights in his response vehicle on Talbot Road in Blackpool when a member of the public knocked on his window, alerting him to an attack taking place in a nearby alleyway. Brent got out to help, managing to pull the man away from his victim, suffering punches and kicks from the assailant.
He also switched on his body-worn camera and asked control to listen to what was happening through his radio. As a result, he was able to secure evidence of the assault and a confession from the man before police arrived.
He says, “Thankfully, I was there to help and prevent something more serious from happening. Fortunately, I only suffered a few scratches as a result of the attack on me.
“However, I’m a big advocate of body-worn cameras. This is a great example of how they can be used to protect patients and the clinicians wearing them. While they don’t always deter people from acting violently and aggressively, as in this case, they can be used to collect vital evidence. Which means a violent offender has received the justice they deserve.”
Last December in court, the attacker pleaded guilty to charges including intent to commit sexual assault, assault occasioning actual bodily harm, and assault on an emergency worker. He was sentenced to ten weeks in prison.
Natalie Samuels, NWAS Head of Violence Prevention, Reduction and Security says, “We are incredibly proud of Brent and the brave actions he took to protect a member of the public while also ensuring his own safety. Paramedics, emergency medical technicians, and other emergency workers should never be subjected to violence or abuse while doing their jobs, and this incident highlights just how crucial body-worn cameras can be in supporting prosecutions and keeping our staff safe.”
She added, “Colleagues have the right to work without fear of harm, and we are committed to doing everything we can to reduce violence against them. We promote the use of body-worn cameras across our service and work closely with police to ensure that any acts of aggression or violence are dealt with swiftly and appropriately.”


Sleep is underrated!
Simon Buckley shares his struggles with sleep and routine


“I’ve suffered from various health conditions over the years, including anxiety and depression, which can affect sleep, mood and general health and wellbeing.
“To try and improve my sleep, I implemented a sleep routine, which I believe has changed my life for the better. This includes avoiding caffeine after a certain time, reducing sugary drinks and alcohol intake, limiting device usage, and minimising blue light exposure before bedtime. When you have a clear idea of what to do, when to do it, and how to do it, it all contributes to improving your sleep.
“As part of the NWAS sleep, fatigue and recovery wellbeing project for staff, I was invited to wear a device, similar to a fitness tracker, which provides vital biometrics in terms of sleep and movement. Whilst the device alone isn’t a game changer, the app that goes with it gives me information and advice on how to make improvements.”
Education Manager Simon Buckley has had a fraught relationship with sleep, having worked as a paramedic for over ten years with irregular shift patterns and night shifts.
“For me, improving my sleep is still a work in progress, even without doing shift work. It can be difficult to have that ‘bedtime routine,’ but I now know what to do to get a good sleep, I have noticed a difference.
“One of the biggest takeaways for me is to realise that everything you do from the minute you wake up leads to you having a good (or bad) night’s sleep.”
Search ‘how to fall asleep faster and sleep better’ online to access the Every Mind Matters guide.
Connecting care beyond the call: social prescribing
When the blue lights fade and the emergency is over, the challenges many of our patients face don’t stop. Loneliness, housing issues, money worries, and lack of community support can still impact their health; it might even be the reason they called 999 in the first place.
That’s where social prescribing comes in. It’s a simple but powerful idea: connecting people with local, non-medical support to improve their overall wellbeing. Think benefit advice, debt counselling, help with cold or damp homes, community groups, or simply someone to talk to.
And it’s not just for GP surgeries anymore. Social prescribing is part of our wider efforts as an ambulance service to provide high-quality, person-centred care to our patients.

Our social prescribing initiative is championed by Public Health Manager Claudia SoilandReyes and in Greater Manchester by Sector Clinical Lead Natalie Ashcroft.
Natalie has worked in Team NWAS for 12 years, starting as a student paramedic and progressing to an advanced clinical role.
Despite having dyslexia, Natalie was determined to pursue her dream. With the support of her university family, friends, and a lot of determination, she successfully gained her diploma and paramedic registration.

Since then, she has completed her Master of Science in advanced practice.
“I always wanted to be a paramedic,” Natalie shares. “I love helping people and working in environments where you have to think on your feet.”
Claudia has worked with us for two years. Originally from Mexico, Claudia has lived and worked in the UK for half of her life. She did her master’s degree in mathematics and statistics, with a focus on practical methods to optimise resources. She has worked in health services research for over 10 years.
Claudia shares, “My dad worked in the Mexican Social Security Institute, a similar government organisation to the NHS, so having the opportunity to work at the NHS, I feel proud of following his steps.”
The duo is now collaborating with colleagues to help improve how ambulance crews support patients, long after the initial emergency.
Claudia explains, “Social prescribing is a way to help patients with issues that affect their health but aren’t necessarily medical. Things like housing problems, isolation, or financial stress. These can’t be solved with medicine, but they impact someone’s health. We connect people to the support already available in their communities. It’s about treating the whole person, not just the symptoms.”
Traditionally, social prescribing referrals were made by GPs. However, ambulance crews often visit patients in their own homes, giving them a unique insight into the daily struggles people face.
“The Public Health team began looking at social prescribing during the pandemic, with a pilot in Bolton, Greater Manchester, in partnership with Age UK. It’s now active across much of Greater Manchester, Cumbria, and Lancashire, and continues to expand. Our clinicians can now refer patients directly to social prescribing services 24/7, 365 days a year across these areas of the North West.”
“This gives us a real opportunity to make a difference,” says Natalie. “Sometimes, with just one referral, we can help stop a cycle that might otherwise lead to more 999 calls.
“The social prescribing service supports our wider strategies around health inequality, community care, and preventing repeat emergencies.”
Our crews can use Service Finder, which provides health and social care professionals with accurate and up-to-date information on available services within a specific locality through a mobile-friendly interface that is quick and easy to use. They can check if a patient’s area has a social prescribing pathway. Most referrals are processed through our Support Centre, with others being routed through local providers.
“Every area is slightly different,” explains Claudia. “That’s why we’ve worked hard to simplify the process so that frontline crews can act quickly, even during busy shifts.”
“From helping someone get essential heating repairs to connecting a lonely patient to a social group or tackling long-standing debt, the outcomes of a simple referral can be life-changing.”
Social prescribing not only helps patients, but it also helps the wider NHS. Reducing repeat 999 calls, lowering pressure on A&E, and offering long-term, sustainable support for those most in need. It’s a great example of how we can optimise and integrate resources by linking our patients to the services available and supporting them to take small steps to improve their health and wellbeing.
“We always prioritise our patient and their emergency,” Natalie says. “But we never lose sight of the person behind it, and social prescribing helps us support them beyond their call.”
Want to know more?
For members of the public, speak to your local GP if you think social prescribing could help you or someone you know. NWAS staff can find guidance on the Green Room on how to refer.


Making a lifesaving difference overseas
Our staff and volunteers don’t just work for the ambulance service, caring for people when they need us the most becomes a part of who they are.
In a shining example of this, selfless colleagues, Regional Community and Engagement Lead Mark Evans and Paramedic Paul Atherton, earlier this year volunteered their own time to support a project in Kisii County, Kenya. This was part of an initiative led by colleagues from the University of Manchester aimed at improving emergency care in one of the country’s most deprived areas.
Over the course of three weeks, a team of six health professionals, including Paul’s wife and former NWAS Paramedic Mandy Atherton, trained 24 local people in vital clinical skills such as trauma response, maternity care, and CPR. Some of the students walked miles each day to attend the programme and by the end of the course were ready to take on emergency roles in their community.
Whilst in Kisii County, a region where just two operational ambulances serve a population of 1.2 million, the team also introduced new health and safety procedures, as well as medicine management protocols to improve patient care.
“It was extremely humbling to experience a completely different way of life and to have the opportunity to make a
real difference,” says Mark. “We were welcomed with open arms, and I’ve made some friends for life.”
The work doesn’t stop there, Mark has since returned with colleague Fiona Larkin, who is a community resuscitation engagement officer in Team NWAS. They trained a further 26 emergency responders, taking the total to over 50 people trained. They also focused on developing some of the original responders as trainers who can carry the programme forward and help the service grow substantially.
“We’re keen to make sure the improvements we’ve introduced have a lasting impact,” Mark explains. “By training trainers, the knowledge can be shared more widely, which helps build a stronger, more resilient service. We’re also very conscious of respecting and embracing cultural differences in the way we approach our work.”
Mark is also planning a charity fundraising event to raise money for essential kit bags and equipment for the local ambulance teams. In the meantime, he’s keeping in close contact with his new colleagues in Kisii County, and the feedback has already been inspiring.
“They’ve been keeping me updated, and it’s amazing to hear how the changes we made are already helping to save lives,” says Mark.
“It was extremely humbling to experience a completely different way of life and to have the opportunity to make a real difference,”



Renée House, from Carlisle, has always had a passion for health and social care. While studying for her Level 3 Diploma in the subject, she worked as a mentor care assistant in a dementia care home, gaining valuable experience supporting patients and families.
“I realised early on how important it is to look after one another,” Renée says. “I’ve always been interested in health, especially anatomy and physiology, and college confirmed this was the path for me.”
Her long-term goal is to become a paramedic, but her journey took shape after attending one of our ambulance awareness day events in Cumbria last year. Originally, she was there to learn more about emergency roles. However, she spoke to one of our staff members working at the event, who introduced her to our non-emergency patient transport service. That same day, Renée applied for a role.
“I love chatting to people and being out in the community. This felt like the perfect way to get my foot in the door to progress,” she says.
After researching the service, Renée prepared for her interview and was thrilled when she was offered the job. “My family was so supportive throughout the process,” she adds. Now working in our patient transport service, Renée takes
One step at a time from care homes to the ambulance service

patients to and from appointments, ensuring their journeys are safe and comfortable. “No two days are the same; some patients need extra support, and compassion is a huge part of the role.”
From easing an anxious patient’s nerves who is blind to seeing familiar faces return looking healthier, Renée finds the work deeply rewarding.
“I would love to be a paramedic eventually. Before this, I hope to gain more experience and develop my skills, and then I’d like to apply for the apprenticeship emergency medical technician role.”
Her advice? “Do your research and go to events that NWAS hosts. One conversation has changed my life, and I’m so glad it did.”
We are hosting a series of five events across the North West from September 2025 to April 2026. They are public events designed to provide more information about our role as an ambulance service, as well as volunteer and career opportunities with us. Details will be shared on our website and social media channels, which can be found on page two.
Knowledge
is power.
Mike’s journey with Lynch Syndrome and life-saving screening

Meet Mike from our Patient Safety Team. Last year, he was diagnosed with Lynch Syndrome, a genetic condition that runs in families and can increase some people’s risk of developing bowel, pancreatic, and gynaecological cancers.
Around one in 400 people in the UK are believed to be affected, although only around five percent are aware. Mike was tested for the condition after his dad was found to carry the gene during his treatment for stomach cancer. He says, “My dad has survived stomach cancer twice now, but sadly, this was the cause of death for his brother, father, uncle, aunt, and grandmother, who all died in their 30s or 40s. We suspected there was a genetic link, but because he avoided cancer in their age group, we thought all was well.
“He still had regular colonoscopy and endoscopy screenings because of this, which detected his first stomach cancer at age 72. During his second bout, advances in genetics testing saw him being tested for Lynch Syndrome, and the genetics team also recommended that my brother and I be tested.
“It was a shock to find out that I also had the gene.
As my dad said to me, ‘knowledge is power’, and the diagnosis now means I’m on a two-yearly bowel screening programme.
“I’ve also explained to my GP how important an endoscopy was for me, and I had my first one in December. So far, both screenings have been clear.
“Now I know I have Lynch Syndrome, I know to be vigilant for symptoms, and to keep myself as healthy as possible. The GP has also prescribed me a daily dose of aspirin as research has shown this reduces bowel cancer risk.
“I’m also part of ‘Lynch Syndrome UK’ Facebook support group, and I am under regular review by the genetics team in Manchester.
“Screening has saved my dad’s life twice so far and could well save mine.”
From fire safety to public declarations, meet our very own town crier
When you think of a town crier, you might picture a brightly dressed figure ringing a bell and calling, “Oyez, oyez, oyez!” What you might not expect is that same voice also oversees fire safety in the ambulance service. That’s all part of a week’s work for Kev Ruane.
As our fire safety manager with a career spanning 33 years, Kev is responsible for ensuring compliance with fire legislation across all our sites, from Carlisle to Crewe and everything in between. He conducts risk assessments, delivers training, and develops personal evacuation plans for those who need them. “It’s a mammoth task,” he says.

He’s also had to improvise on the spot, making spontaneous birthday shout-outs and messages for passers-by.
In his spare time, Kev has taken on a rather unique role outside of his job in Team NWAS. Earlier this year, he was officially appointed Southport’s Town Crier by Sefton Council, the first in 36 years.
The idea came after seeing a town crier in Knaresborough and feeling inspired. When he learned that Southport, the town where he lives with his wife, didn’t have one, he pitched the idea to the council, and the rest is history.
Entirely voluntary, the role varies week to week. Kev’s appearances have included the Armed Forces Festival, the British Musical Fireworks Championships, and even wedding anniversaries, writing bespoke proclamations and poems for each occasion.
Being a Town Crier may seem theatrical, but there’s real skill involved. Confidence in public speaking is essential, of course, but creativity is equally important.
“Writing a proclamation is a craft,” Kev says. “They need to be short, relevant, engaging, and, where possible, fun! People think AI can do it these days, but each one takes real thought. I rewrite them several times before I’m happy.”
“It’s nice to do something that brings people joy. Being part of something that brings pleasure to people and adds value to their experiences is a real privilege.”
Kev’s ceremonial outfit, or livery as it is known, is based on a Georgian military tunic, complete with gold braid, breeches, and a tri-corn hat. He owns multiple versions to suit the occasion and the weather.
While balancing NWAS duties, Kev also finds time to represent the service as a town crier. He participated in the VE Day 80th anniversary event at Estuary Point earlier this year and is set to appear at the opening of the new Hazardous Area Response Team official station in Anfield. He says, “There are strict protocols about attending events in other areas, so I’m limited as to where I can attend outside of the Sefton area without following specific protocols.”
With around 200 town criers across the UK, mainly in the South, the North West has a handful, including in Chester, Darwen, Lytham St Annes and now Southport, thanks to Kev.

“Mama bear at work, how Cath helped Jackie find answers and strength”
Work mums are a special group of people. The type who take you under their wing, the person you go to when you’ve had a tough day, who celebrates your achievements like they are their own, or makes every day working life that little bit better just by being around.
For Outbound Desk Specialist Jackie Porter, that person is Cath Boylan, Shift Supervisor in our Integrated Contact Centre. Cath is someone who has guided Jackie over the seven years they’ve worked together, while bonding over their shared childhood experiences growing up in the 80s. But it was when Jackie suspected she had ADHD that Cath truly took on that “work mum” role.
Jackie says, “I suspected that I had ADHD in January of 2022 and confided in Cath regarding this. Instead of just dismissing me and telling me it was just a ‘fad’ or ‘we’re all a little neurodivergent’ (all things that have happened to me), she encouraged me to seek a formal diagnosis. She referred
me for an occupational health assessment.
“When I was formally diagnosed, she shared the happiness that I finally had an answer to so many questions that had plagued me throughout my life.”
Following Jackie’s diagnosis, Cath helped make adjustments to Jackie’s working environment. She also fought for Jackie to be able to use a different room for those times when she was really struggling with the noise in the call handling suite, meaning Jackie could calm down, focus, and continue working.
Sadly, Jackie and Cath no longer work directly together, but with only two months between them, they will be celebrating their 50th birthdays together this year.
Jackie says: “I think Cath needs celebrating as she has truly been in my corner and will do this for anyone who needs it. She’s a Mama Bear!”

CAREERS WITH HEART.



When you join our teams, you’re at the heart of something amazing. No matter what part you play, from call handler to paramedic, you’re making a real difference, every day. There are all sorts of people in over 300 different roles behind those bright yellow vehicles and blue flashing lights. But we all have one thing in common. We care. nwas.nhs.uk/careers


