





A practical benefits guide for embedding and sustaining digital transformation in health and care.
Developed by Dr Rebecca Casey and Dr David Wainwright, Newcastle University in collaboration with the Great North Care Record team, North East and North Cumbria Integrated Care System.
This Playbook focuses on how digital innovation changes the way people work across health and care. It is designed for those leading or enabling frontline and operational transformation - programme leads, digital champions and implementation teams working to embed shared care records like the Great North Care Record (GNCR) into everyday workflows, decision-making and collaboration. This Playbook complements traditional benefits management approaches such as the Statement of Planned Benefits (SoPB) and the use of tools like the Benefits Analysis and Realisation Tool (BART) available to download from the NHS Futures Platform. It provides practical prompts, real-world use cases, and frameworks that support ongoing delivery.
Who is it for?
Designed for project teams, digital champions and frontline health and care professionals across primary and secondary care, mental health, social care and emergency settings.
Senior leadership teams and system-level decision-makers can also use the Playbook to support investment, assurance and benefit oversight.
How to use this playbook?
Follow this step-by-step guide, enriched with real-world case studies from the adoption of GNCR shared care record, to drive successful digital integration in your organisation.
Note: This playbook is based on findings from a mixedmethods research evaluation of the GNCR, specifically conducted around user-reported benefits. While it highlights positive and promising practices and user case studies, it has not incorporated real-world usage data, which the GNCR records. Quantitative claims about system-wide impact should be interpreted with this in mind.

Key takeaways:
• Without strategic alignment, sponsorship and buy-in are almost impossible.
• Digital adoption must map to organisational goals to ensure long-term impact.
Action points:
• Identify your organisation’s digital transformation objectives.
• Clarify how your project contributes to NHS priorities (e.g. analogue to digital, hospital to community-based care, focus on prevention over treatment).
• Secure senior sponsorship early.
• Where possible, map digital initiatives to actual usage data (e.g. login frequency by clinical role, function and task) to test alignment between strategic goals and adoption patterns.

In mental health settings, GNCR enables rapid access to crisis plans. With usage data, the extent of this impact could be measured across the health and care system. Embedding monitoring tools that track real-time usage by service could help validate these benefits and guide prioritisation.
1
Top layer
National and regional NHS priorities
These will show alignment with wider NHS strategy and policy.
NHS Long Term Plan Priorities:
• Digitally-enabled care
• Integrated care systems
Patient safety and care quality
• Cost reduction and operational efficiency
Regional Digital, Data and Technology Strategy
• Seamless, real-time data sharing across sectors
• Interoperability across NHS and social care
2
Middle layer
GNCR investment objectives and benefits
These will be extracted from the business case and underpinned by strategic drivers
3
Bottom layer
Organisational objectives
You can map GNCR benefits to the organisational objectives

Safety and quality
• Real-time patient history access
• Fewer medication errors
Safer maternity care and mental health crisis management
• Better safeguarding
Operational Efficiency
Reduced duplicate tests
• Reduced hospital attendances
• Time saved in clinical and social care workflows
NHS Foundation Trusts
• Patient flow improvement
• Safer discharge
• Operational cost reduction
Patient experience
• Less need for patients to repeat history
Continuity across organisational boundaries
Financial and environmental value
• Cost avoidance benefits
• Reduced patient transport requests
• Reduced carbon footprint
Mental Health Trusts
• Crisis intervention support
• Access to physical health information
• Safeguarding data integration
Ambulance Services
• Real-time access to care plans
• Medication history in emergencies
Social Care
• Faster care planning
• Better safeguarding decisions
• Less duplication in referrals
• Joined up care
Key takeaways:
• Stakeholders don’t just need information - they need a role in shaping the change.
• Effective change management is key to adoption and continuous improvement
Action points:
• Use stakeholder mapping to identify influencers, decision-makers and concerned stakeholders.
• Share survey tools through newsletters, digital champions and advocacy groups for higher response rates.

Conduct targeted interviews with key stakeholders to capture real-world benefits, which are user relatable, though, for example, a day in the life of narratives.
Engage non-users by highlighting how GNCR helps them (e.g. For emergency department clinicians, it reduces unnecessary calls to GP practices and hospital admissions can be verified without waiting for callbacks).
Understand barriers to adoption such as time pressures, interface usability or lack of awareness.
Address areas of lower digital adoption in your mapping - roles or departments with low GNCR interaction and explore reasons why.
When GNCR engaged frontline staff in interviews and feedback loops, it revealed practical barriers to adoption - like login issues and training gaps - which were easily addressed before wider rollout.
NET BENEFITS
Should champion the project - but must be aware of implications for others and use their influence.
“Collaborators” [HELP]
BENEFITS BUT … CONCERNED
Need help with changes - ensure sufficient enabling changes are identified to offset any resistance.
“Compromisers” [HELP/MAKE]
Prioritising your stakeholders according to what’s in it for them versus the extent they are expected to change how they work.
FEW BENEFITS BUT …
Must be kept supportive by removing any inertia/apathy which may influence others.
“Accommodators” [NEUTRAL]
NET DISBENEFIT
Likely to resist the changes - must ensure all aspects of resistance dealt with by enabling projects.
“Sceptics” [ALLOW/HELP]
Change required
A&E consultants, mental health crisis teams
These stakeholders experience clear and immediate benefits from GNCR, such as faster access to patient records, reducing duplicate tests, and enabling quicker clinical decisions
They should champion GNCR adoption and influence others to use it.
GPs, social care professionals
While GNCR provides benefits (e.g. reducing admin burden, improving care coordination), these groups face workflow disruptions due to interoperability issues or usability challenges. Engagement should focus on enabling change, ensuring GNCR is integrated seamlessly with existing EHR systems and providing role-specific training.
Prioritising stakeholders based on the benefits they gain versus the level of change required in their workflow.
Administrative staff, some allied health professionals (e.g. physiotherapists)
These groups may have less direct interaction with GNCR, but their support is needed to prevent inertia or passive resistance.
Efforts should focus on keeping them informed and supportive of GNCR’s wider impact on patient care.
Some Secondary Care Specialists
While this group may not yet see direct benefits, they are well-placed to gain from improved efficiency and information access. Targeted engagement –including peer examples and success stories – can build confidence and address concerns around usability, interoperability, and data quality
Change required









Keep questions simple, clear, and concise, especially for time-limited stakeholders.
Secure an executive sponsor to endorse the survey and encourage participation.
Provide a brief project information sheet and ethics clearance if needed.
Ensure confidentiality and anonymity where required.
Structure questions around tasks, value, benefits, challenges and digital system impact.
Encourage discussion on benefits realisation and role process changes.
Consider social/cultural factors related to digital adoption.
Share a summary of key findings with respondents.
Use online tools for convenience and seek consent for recordings.












Keep it simple, clear, and concise, especially for time-limited stakeholders.
Focus on key areas: tasks, value, benefits, challenges and digital system issues.
Use a mix of question types:
• Yes/no and likert scales (1-5 or 1-7) for quick responses Open-ended questions for nuanced insights.
Secure an executive sponsor to endorse the survey and encourage participation.
Include a brief project info sheet and ethics statement if needed.
Set a short response window and send reminders.
Ensure confidentiality and anonymity if required.
Use online survey tools for efficiency.
Pilot the survey first, gather feedback, then launch at scale.
Share key findings in a short summary report with respondents.

Define investment objectives. Why are you doing this?
• Identify the strategic goals (e.g. Improving efficiency, enhancing patient care, reducing costs).
• Align objectives with national priorities (e.g. NHS digital strategy, integrated care goals).
“To improve efficiency by reducing time spent accessing patient records.”

Define business changes. How will workflows evolve?
• Determine the new ways of working introduced by digital enablers.
• Focus on how teams will interact with the system and what will change in daily operations.
“Clinicians can access test results instantly, reducing duplicate requests.”

Identify digital and organisational enablers. What enables change?
• Technology: Introduce innovative platforms like GNCR while modernising legacy infrastructure
• Process: Align workflows with shared digital pathways to streamline care delivery.
• People: Support staff with targeted training and peer learning to embed new ways of working.
• Governance: Strengthen data access and sharing policies to build confidence and trust.
““GNCR doesn’t just give us access to records – we can rethink how we deliver care across boundaries.”
Map to business benefits. What measurable improvements will occur?
Link business changes to tangible benefits, such as:
• Time savings for clinicians Fewer GP referrals
• Faster decision-making in emergencies Include specific, quantifiable targets where possible.
“Assess the reduction in duplicate tests enabled by GNCR (e.g. through local audit or baseline comparison).”
Enablers
Organisational enablers
Training and Adoption (Improving staff competency)
Improved Data Governance and access control (rolebased access)
Leaders ensure GNCR adoption aligns with ICS digital transformation goals
Digital enablers
GNCR health information exchange (Centralised patient data sharing)
Integration with Provider Systems
Business changes (new ways of working)
Faster access to discharge summaries, test results, and patient history
Fewer unnecessary GP referrals and calls to other providers.
Better coordination for safeguarding, mental health, and elderly care
Enhanced remote triage for 111 services and virtual wards
Business benefits
Investment objectives
Time savings: e.g. GPs (3-5 min per consultation), A&E clinicians (5-10 min per patient), social care and mental health professionals (avoiding multiple calls for patient records)
Reduced duplication of assessments and reduced need for patients to repeat their histories
More informed and timely decision-making by practitioners
Enhanced safety and continuity of care through shared access to discharge summaries, crisis plans, and
To improve efficiency (time and cost savings) in health and care workflows
Enable Seamless, real-time information sharing across health and social care

Enhancing digital value (EDV) for A&E (ED) departments: GNCR dependency network
Digital technology enablers GNCR data sharing
Trust data displayed in: dedicated widgets items included:
• Allergies and adverse reactions
• Blood sciences
• Care plans Cellular pathology
• Clinical correspondence
• Encounters
• Future appointments
• Maternity information Microbiology
• Problems and diagnosis
• Procedures
• Radiology
GP Connect (SystmOne and EMIS) data displayed in: GP Records widget only information included:
• Administrative items
• Allergies and adverse reactions
• Clinical items
• Encounters
• Immunisations
• Medications Observations
• Problems and issues
• Referrals Summary
• Vital signs Local authority council data displayed in: Social care items included:
• Demographics Assessment details
• Care package information
• Case notes
• Contact details Warnings
• Worker relationships
• Communication needs
• Assessment details
• Safeguarding details
• Service user details
• Social worker details
Enabling changes
GNCR education and training (both face to face and virtual)
Enhancing digital value and benefits management education and training
Training of clinical professions on new advances in testing and diagnostics
Process analysis, review and co-design of health and care pathways and services
Develop and implement GNCR continuous improvement programmes
Refine GNCR widgets for quick use and access to key patient details
Avoid and eliminate data duplication
Hospital digital systems education and training
Benefits
Identify frequent and serial attenders
Holistic view of patients – safer clinical decision making
Increased levels of patient satisfaction and experience
Increased levels of patient trust and reassurance
Enhanced levels of communication between clinicians
Reduced levels of stress and anxiety for clinical team
Accelerated and enhanced learning/ training for junior doctors
Benefits
Reduction in duplicate and/or unnecessary tests
Reduction of clinical adverse outcomes
Decrease in hospital ward admissions
Target average time savings between 5 to 10 mins per patient consultation
Increase in patient throughput
Increase access to social care client details for safeguarding
Decrease in time spent making telephone calls & waiting for patient notes to GP practices or other NHS providers
Clinical and organisational drivers

Improve and standardise urgent care at the front door of the hospital
Improve treatment clinical outcomes, quality and safety
Rapid access to patient medical history and details
Access to information 24/7 outside normal hours
Improved communication between MDT and clinicians
Reconciliation of medication and drug prescriptions and dosage
Investment objectives
Efficiency drive to cope with high patient throughput and demand in A&E with up to 150 to 200 patients per day
Speed up hospital discharge times
Reduce length of stay in hospital and ensure that patients are cared for in the most appropriate setting
Reduce ED waiting times
Achieve cash releasing efficiency gains in productivity
GOV and NHS policy imperatives
Improve A&E waiting times and ambulance response times compared to 2024/25, with a minimum of 76% of patients seen within 4 hours by March 2026.
Category 2 ambulance response times should average no more than 30 minutes across 2025/26.
Improve higher proportion of patients admitted, discharged and transferred from A&E within 12 hrs across 2025/26 compared to 2024/2025
NHS strategic priorities for 2025 onwards
Enhancing digital value (EDV) for social care departments: GNCR dependency network
Digital technology enablers GNCR data sharing
Trust data displayed in: dedicated widgets items included:
• Allergies and adverse reactions
• Blood sciences
• Care plans Cellular pathology
• Clinical correspondence Encounters
• Future appointments
• Maternity information Microbiology
• Problems and diagnosis Procedures
• Radiology
• Vital signs
GP Connect (SystmOne and EMIS) data displayed in: GP Records widget only information included:
• Administrative items
• Allergies and adverse reactions
• Clinical items
• Encounters Immunisations
• Medications
• Observations
• Problems and issues
• Referrals Summary
Local authority council data displayed in: Social care items included:
• Demographics
• Assessment details
• Care package information
• Case notes Contact details
• Warnings
• Worker relationships Communication needs
• Assessment details
• Safeguarding details
• Service user details Social worker details
Enabling changes Benefits
GNCR education and training (both face to face and virtual)
Education and briefings on medical terminology for social workers and carers
Training of social workers on GDPR and data privacy, security and confidentiality delivered in accessible formats
Hands on training in technology assisted care (gadgets, home monitors and systems and mobile tech etc.)
Enhancing digital value and benefits management education and training
Process analysis, review and co-design of health and care pathways and services
Refine GNCR widgets for quick access to key sections of the social care assessment
Holistic view of clients –safer social, economic and clinical decision making
Increased levels of client and family/ carers satisfaction and experience
Increased levels of client trust and reassurance
Enhanced levels of communication between social workers and clinicians
Early identification of key information such as potential suicidal tendencies
Greater access to safeguarding information for vulnerable clients and pregnant persons
Improved production of viable care plans with contextual health information
Benefits
Reduction of social care adverse outcomes
Decrease in hospital ward admissions
Decrease in length of hospital stays
Increase access to social care client details for safeguarding
Decrease in time spent making telephone calls and waiting for patient information from gp practices or hospital clinicians
Reduced levels of stress and anxiety for social work team
Development of personal budgets for clients
Clinical and organisational drivers
Shift toward intervention care and focus on early intervention
Increase the adoption and use of mobile digital technologies, wearables and TEC in the home or facilitated care settings
Develop multidisciplinary care teams (MDT) with appropriate levels of funding and support
Access to information 24/7 outside normal hours
Improved communication within and between MDTs
Improve joint commissioning of services, shared budgets and integrated systems

Investment objectives
Expand availability of community based services
Speed up hospital discharge times
Reduce unnecessary hospital visits
Reduce length of stay in hospital and ensure that patients are cared for in the most appropriate setting
Expand Technology Enabled Care (TEC) and virtual consultations to support care at home
Increase investment in reablement services
Achieve cash releasing efficiency gains in productivity
GOV and NHS policy imperatives
Promotion of independent living for as long as possible through provision of community-based services
Foster integration and collaboration between NHS services and social care to improve patient outcomes and streamline services
Develop innovative models of care to cope with demographic changes and increasing service demands
NHS strategic priorities for 2025 onwards
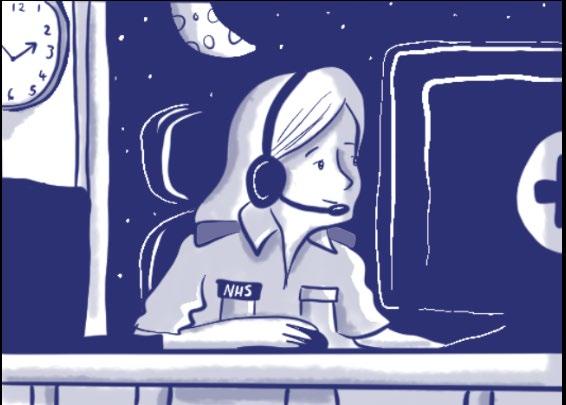
Meet Val, an advanced nurse practitioner who handles urgent calls for NHS 111, on 12-hour shifts. She makes important, critical care decisions every single day.

Calls come in any time. Especially overnight, when their usual GP may be unavailable.


Patients may be anxious, scared, confused. Val needs instant access to detailed medical histories, medications, allergies, past treatments, to make safe, informed and fast decisions.

With GNCR, an unnecessary trip to A&E can be avoided, she prescribes a more targeted antibiotic based on updated test results.







No ambulance needed. Paramedics often call in, Val relays patient histories, where mobile access may be difficult. For Val, GNCR enables faster care, safer decisions and better outcomes.

Key takeaways
• Move beyond conventional “benefits tracking” to focus on learning and adaptation.
• Identify both quantitative (time savings, cost reductions) and qualitative (staff morale, decisionmaking speed) benefits.
Action points:
• Consider live tracking dashboards alongside traditional benefits spreadsheets such as the BART tool.
• Use a combination of quick-win metrics (e.g. Reduced duplication of tests) and long-term impact measures (e.g. Improved patient flow).

• Build a feedback loop - learning systems should evolve based on user experience.
• Incorporate numerator/denominator analysis - how many eligible users have access? How many actually use the system daily or weekly?
• Layer self-reported data with system access logs to differentiate between perceived and actual impact.
Patient journey mapping has the potential to highlight real impact - faster A&E decisions, fewer duplicate tests. This qualitative evidence can be as powerful as costsaving metrics in driving adoption.
A GNCR dashboard can model time savings by incorporating granular usage. Future iterations must incorporate granular usage logs and data (e.g. Total staff with access by setting) to calculate actual benefit realisation.
Operational efficiency Faster access to records, reducing clinician admin time. Streamlined handover to A&E
Clinical safety Double-checking prescriptions, allergy alerts, safeguarding flags.
Reduced duplication
Improved MDT working
Avoid duplicated tests (blood tests, scans, etc.).
Better information flow between primary, secondary, and social care.
Faster Decision Making More informed diagnosis and treatment planning.
Patient satisfaction Patients trust clinicians more when they are well-informed.
Cost savings Fewer hospital admissions/ referrals.
Social care integration Shared care records improve home care planning.
Mental health support Better visibility of past crisis episodes, medication, and safeguarding.
Time saved per patient
Reduction in errors and adverse events.
GP, A&E, Social care, Pharmacy GPs, nurses, consultants, social workers, ambulance services
GP, A&E, Pharmacy, mental health GPs, nurses, pharmacists, social workers, ambulance services
Reduction in duplicate tests. Hospitals, GPs, A&E GPs, consultants, radiologists
Clinician feedback, case study analysis. MDTs, social care GPs, social workers, mental health teams
Time savings in clinical settings. GP, A&E, hospitals GPs, consultants, nurses
Patient surveys. GP, A&E, hospitals Patients, carers, families
Reduction in hospital costs per patient.
Social worker feedback, case study analysis.
Reduction in mental health emergency escalations.
Finance NHS digital, commissioners
Social care Social workers, local authorities
Mental Health, GP
Mental health nurses, social workers
GNCR are developing a live dashboard which will be able to model time savings and continuously improve GNCR.
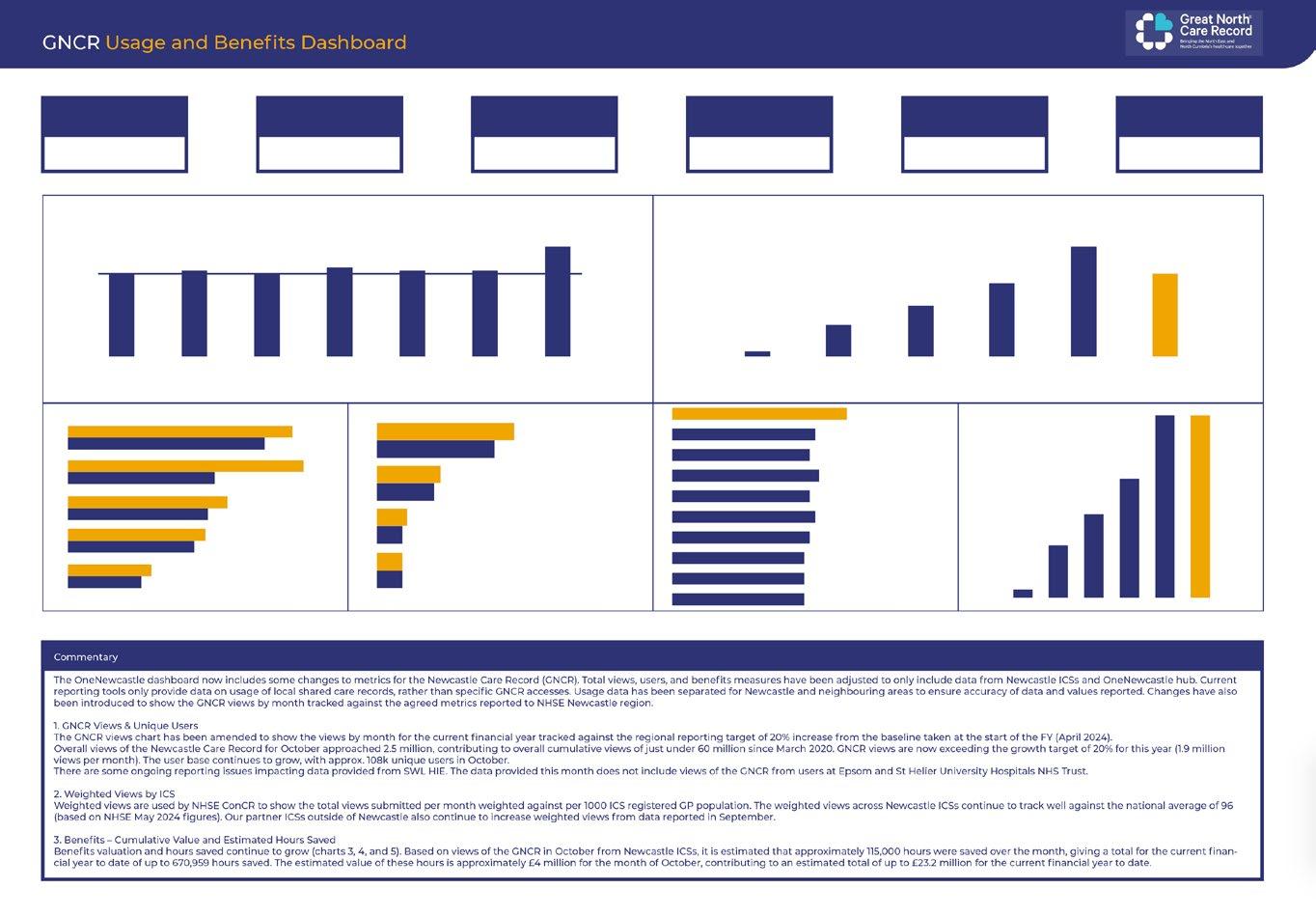

Key metrics:
• How many views per organisation?
• Estimated time saved per role?
• Where adoption is highest/lowest?
“This will help us tailor support, identify champions, and scale impact.”
Data sources:
• GNCR usage data → tracks access frequency by role (GPs, A&E, etc.)
• Salary data → links professional roles to average pay bands
• Time-saving calculations → uses lookup benchmarks to estimate time saved
• Financial benefits → converts time saved into monetary value
Technical requirements:
• Data pipeline for cleaning, transforming, and analysing GNCR data
• Secure integration with GNCR databases
Security and compliance:
• NHS information governance and GDPR compliance
Dashboard features
• Bar charts: time savings by organisation and professional group
• Line graphs: cumulative time & financial savings over time
• Heatmaps: high-utilisation departments
Comparative analysis
• Savings trajectory of GNCR implementation
• Organisation-level benchmarking
Summary metrics
• Total time saved
• Total financial benefit (£)
• Breakdown of organisations and associated savings
Customisation features
• Filter by date range, organisation, and role
• Export options (csv, pdf)
Navigation and accessibility
• Intuitive dashboard with tabs for time savings, financials
• Drill-down insights for deeper analysis
• Cross-platform compatibility (desktop, tablet, mobile)

Adoption alone isn’t enough. True digital value comes when use is purposeful, embedded and measurable. Focus on high-impact use cases (e.g. A&E, maternity, social care discharge) and build team routines that integrate digital tools into everyday decision-making.
Key takeaways
• Digital transformation is not a one-time project. It requires cultural adaptation.
• Focus on integrating digital tools into daily workflows not just delivering technology.
Action points:
• Adapt focus from technical implementation to habit formation and workflow changes.
• Train and empower digital champions within teams.
• Encourage peer-to-peer learning and cross-team collaboration.
• Add case studies from frontline users
• Address user interface and experience challenges and the need for continuous training (e.g. Using the “Train the Trainer” model).
• Provide workflow integration tips, ensuring GNCR aligns with daily clinical practices.
• Use team huddles or ward rounds to review how GNCR is being used - or not used - in specific workflows.
Instead of one-time training, GNCR primarily adopted a ‘Train the Trainer’ approach where experienced users mentored new adopters. This sustained digital adoption is far better than one-off workshops.
GNCR’s most impactful uses were in urgent decision-making, (e.g. Confirming medication in A&E). These workflows should be documented, repeated and scaled. Areas of high potential such as clinician to clinician referral may need targeted support.
Key takeaways
• Digital transformation is ongoing - embed a mindset of continuous improvement.
• Success stories drive further adoption - celebrate wins and scale what works.
Action points:

• Regularly revisit and adjust benefits tracking methods - keep them relevant.
• Share success stories widelystaff forums, internal blogs and leadership updates.
• Identify next-phase innovations - how can digital tools evolve further?
• Establish quarterly review sessions where users share insights on usability, system gaps and impact improvements.
When early GNCR adopters shared real-world stories of faster A&E triage, it convinced hesitant teams to engage. Peer testimonials were more effective than top-down mandates.

Focus on 2–3 key use cases (e.g. ED triage, mental health discharge, maternity triage) for in-depth case studies using real metrics and frontline feedback.
Share quarterly usage data, celebrating top teams and helping those who need support.
Consider the use of innovative tools such as natural language queries within user guidance to enhance user training and drive adoption.

Why do we want improvement?
What improvement could we get?
Improve clinical decision-making, reduce administrative burdens, enhance patient safety, and streamline communication between primary, secondary and social care.
Faster access to patient records, reduced duplication of assessments, more informed clinical decisions, improved coordination between teams. What benefits will be realised?
• Time savings per patient (3–5 minutes for GPs, 5–10 minutes for A&E consultants). Reduced phone calls and letters.
• Enhanced safeguarding and mental health support.
• Improved multidisciplinary team (MDT) coordination.
• Greater confidence in care planning
Can it be measured?
Can it be quantified?
Can a financial value be put on it?
Where will the benefits occur?
Who is responsible for delivery?
Who is affected?
What changes are needed?
How and when can changes be made?
Yes, through:
• Reduction in phone call time chasing patient data. Reduction in duplicate assessments/procedures.
• Improved speed of patient triage in A&E and GP out-of-hours.
• Patient and clinician satisfaction surveys.
Yes, through:
GP time savings: 3–5 minutes per patient.
• A&E time savings: 5–10 minutes per patient.
• Reduction in administrative delays for hospital discharges and GP referrals.
Yes, through:
• Cost savings from fewer repeat assessments.
• Reduction in hospital admissions (£25k per patient avoided).
• Savings from reduced administrative time.
Across primary care (GPs), secondary care (A&E, hospitals), mental health services, pharmacy, and social care. Ambulance services
GNCR project team, NHS digital leads, clinicians, IT system managers.
All health and social care staff using GNCR.
• More flexible training on GNCR functionality.
• More intuitive user interface and experience to streamline workflows.
• More flexible data governance policies.
• More integration with pharmacy systems
• Training and onboarding plans.
• Short-term: User interface updates and training.
• Medium-term: Integration with other health IT systems.
Long-term: Expanding functionality for social care and pharmacy.
Level Stage Description Checklist - Are you doing this?
1 Initial adoption Team is aware of the Playbook and has started using it for local planning.
2 Active Implementation Playbook is being used to structure benefits mapping, stakeholder engagement and workflow redesign.
3 Integrated practice Playbook is part of routine transformation delivery and benefits are being tracked with local data.
4 Co-produced evolution Playbook is actively maintained and expanded to include wider perspectives (e.g. patients, carers, ICS stakeholders).
• Shared Playbook with key project leads
• Mapped local use cases to playbook examples
Identified quick wins for digital workflow improvement
• Benefits mapped using dependency networks, BART or SoPB
Staff engagement (interviews, workshops)
• Evaluation framework applied to 1+ use cases
• Playbook included in project governance/assurance
• Real-time data used to track benefits
• Playbook used in business cases or funding bids
Outputs shared with senior leadership
Lessons logged and shared with other teams
• Patient and carer voice embedded in future versions
Links to wider ICS transformation plans
Playbook iterated based on feedback

• The goal is not just adoption but digital transformation that evolves.
• Use this playbook as a living document - adapt it based on your organisation’s needs.
• The real value of digital is in how people use it, not just the technology itself.

Benefits realisation
Business change
Digital champion
Digital transformation
Health information exchange (HIE)
Interoperability
Patient journey mapping
Process mapping
Realising digital value
Stakeholder mapping

A process that ensures projects deliver intended improvements and measurable outcomes aligned with strategic goals.
New ways of working introduced through digital transformation, such as changes in workflows or data access.
A frontline staff member who advocates for and supports digital adoption within their team or organisation.
The integration of digital technology into all areas of health and care, fundamentally changing how care is delivered and outcomes are achieved.
A system that enables the secure, electronic sharing of patient information across organisational boundaries.
The ability of different IT systems and software to communicate, exchange data, and use the information that has been exchanged.
A method to understand and visualise how patients move through services and how digital tools influence their care experiences.
A tool to visually describe the workflow and identify areas for improvement and digital enablement.
A framework for aligning digital investments with measurable impact in healthcare settings
The process of identifying key individuals or groups affected by a digital initiative and planning engagement strategies.
Term Definition
Advanced Nurse Practitioner
BDN Benefits Dependency Network
Term Definition
Governance
Multi-Disciplinary Team ED Emergency Department
North East and North Cumbria EHR Electronic Health Record
EPR Electronic Patient Record
GNCR Great North Care Record
National Health Service
Project Initiation Document
Summary Care Record HIE Health Information Exchange



We would like to sincerely acknowledge and thank all the professionals and organisations who generously contributed their time, experiences and insights to this evaluation. Although anonymised in this report, each participant played a crucial role in shaping our understanding of the Great North Care Record’s impact in practice. Your openness, honesty and reflections have not only informed this research but also helped to illuminate the real-world value of shared care records across the region. We are deeply grateful for your engagement and we hope this report reflects the significance of your contributions. This evaluation project by Newcastle University has been made possible through funding from the Economic and Social Research Council (ESRC) impact acceleration account –strategic fund, awarded to the lead researcher Dr Rebecca Casey following a successful competitive bid. The grant of £14,448 supported the engagement of a second researcher to co-lead data collection and analysis and has primarily funded the professional graphic design of the enhancing digital value playbook for the GNCR. The support from the ESRC has been instrumental in enabling a high-impact evaluation that is both analytically robust and accessible to a wide audience.
Casey, R. and Wainwright, D. (2023). Realising Digital Value Playbook. Available at: https://realisingdigitalvalue.co.uk [Accessed 10 Apr. 2025].
Casey, R and Wainwright, D The Great North Care Record: An Evaluation of Effectiveness and Benefits for the NENC Integrated Care System, Newcastle University, ESRC Impact Acceleration Award Report 2025.
Waring T, Casey R, Robson A. Benefits realisation from IT-enabled innovation: A capability challenge for NHS English acute hospital trusts?. Information Technology and People 2018, 31(3), 618-645. Health Foundation (2025). Electronic Patient Records: Are We Realising Their Strategic Potential? Available at: https://www. health.org.uk/reports-and-analysis/analysis/electronic-patient-
records-nhs-strategy
NHS England Digital. (2025). Benefits management. NHS England. https://digital.nhs.uk/services/benefits-management. North East and North Cumbria Integrated Care System (2023). Digital, Data and Technology Strategy 2023–2026. Newcastle upon Tyne: NENC ICS. Available at: https://northeastnorthcumbria. nhs.uk/media/p5hhd25x/digital-data-and-technology-2023-26.pdf [Accessed 10 Apr. 2025].
Ward, J. & Daniel, E. (2012). Benefits Management: How to Increase the Business Value of Your IT Projects (2nd ed.). Chichester: Wiley.
For more information about the Realising Digital Value research visit: https://www.realisingdigitalvalue.co.uk/