BEYOND THE HEADLINES
Trends and Opportunities in Youth Mental Health in the U.S.
May2025
YouthMentalHealthOrganizationsandPhilanthropic


May2025

NewProfit,anonprofitventurephilanthropyorganization,backsbreakthroughsocialentrepreneursexpandingaccess andopportunityintheU.S.YouthmentalhealthisacriticalcomponentofourstrategyacrossEducation,Economic Mobility,andDemocracy.ForourEducationStrategy,wethinkaboutyouthmentalhealthasadvancingthewellbeingof students,educators,andfamilies.Ouryouthmentalhealthworktodatehassupportedearly-stageorganizationsin expandingaccesstoculturallyresponsivementalhealthcare,particularlyforthosefurthestfromaccess.Throughour Catalyzesupportmodel,wehaveinvested$1.6millionin16early-stagementalhealthnonprofitsandarepreparingto providethenextcohortofeightorganizationswith$880K.
Inadditiontofunding,weprovidepeerlearningcommunities,coaching,andstrategicadvisorysupporttohelp organizationsnavigatebarrierstogrowthandscaletheirimpact.Beyonddirectinvestment,wefocusonstrengthening thebroaderfieldbyconveningnewandinterestedmentalhealthfundersandleaders,joiningdiscussions,fostering collaboration,andshapingphilanthropicinvestmentstrategiesthatdrivemeaningful,community-centeredimpact.As welookahead,weaimtoexpandourinvestmentstrategytoincludeorganizationsreadytoscaleanddeepentheir impact,ensuringyouthmentalhealthsolutionsaresustainableandwidelyaccessible.
Whyalandscapeanalysisnow?
● PurposeoftheLandscapeAnalysis:Thisanalysisaimstoilluminatetheyouthmentalhealthfield,providingcritical insightstoempowerfunders,policymakers,andmentalhealthleaderstomakeinformeddecisions.
● BuildingonourWork:Overthepastfewyears,NewProfithashadtheprivilegeoflearningfromremarkablesocial entrepreneursandmentalhealthleaders.Aswelooktodeepenourimpact,thisanalysis,conductedinpartnershipwith thehuman-centereddesignfirm,PeopleRocket,buildsonworkcompletedbyourpeerswithafocusonaccesstoensure wenavigatetheyouthmentalhealthspaceresponsiblyandwithintention.
● MentalHealthasaFoundation:MentalhealthisintegraltoachievingsuccessinNewProfit’sstrategicfocusareas: Education,Democracy,andEconomicMobility.Addressingmentalhealthchallengesstrengthensindividualand collectiveoutcomesacrossthesedomains.

EmergingfromtheCOVID-19pandemic,youthmentalhealthhascomeintothespotlight.Evenbeforetheisolationofthe pandemic,theformerU.S.SurgeonGeneral,Dr.VivekMurthy,warnedofa“lonelinessepidemic”contributingtoadecline Americans’mentalhealth.Indeed,youthmentalhealthhasbeenonthedeclinefordecades.Duringthepandemic,youthmental healthchallenges,includingdepressionandsuicidality,intensifiedandcontributedtoagrowingconsensusthatinvestmentis neededatalllevels,fromfamiliesandcommunitiestopublicandprivatesectorinstitutionsandpolicies,tosupporttoday’s youth.Philanthropicorganizations,inparticular,haveauniqueopportunitytocatalyzechangebyinvestingininnovative, community-driven,andproximatesolutionsthataddresssystemicbarrierstocare,reducestigma,andfosterresiliencein youngpeople.
Inordertomakeprogress,itisimperativethatwehaveanuancedunderstandingofthediverserangeofchallengesfacedby youthtodayandtheopportunitiesforinterventionandimpact.NewProfitundertookanovellandscapeanalysisofyouthmental healthintheUnitedStates,whichisfocusedonunderstandingboththestateofyouthmentalhealthtodayandthelandscapeof nonprofitsandtheirfundersacrossthecountrythatarefocusedonaddressingyouthmentalhealthaspartoftheirmissionor coreactivities.
Itisourhopethatthisworkcanhelptomovethefieldforwardbyaddingnuancetotheheadlinesaroundyouthmental health,makingvisiblethegapsininvestmentandaccesstocriticalservicesandsupports,andshiningalightonthegood workthatisalreadybeingdonetosupportyouthmentalhealthincommunitiesacrosstheUnitedStates.


Youthmentalhealthisacomplexandevolvingissuethatisshapedbyindividualexperience,communitycontexts,and systemicfactors.Todevelopanunderstandingofthecurrentyouthmentalhealthlandscape,we:
● reviewedover300reportsandstudies
● interviewedmorethan20stakeholdersincludingnonprofitleaders,funders,researchers,advocates,andyouth
● analyzedpubliclyavailabledatatoidentifynearly7,000nonprofitorganizationsfocusingonyouthmentalhealthin theUnitedStates.
Thisapproachincorporatesabroadrangeofperspectivesandenablesusnotonlytounderstandtheextentanddepthofthe challengesfacingyouthmentalhealth,butalsotohighlightopportunitiesforthefield.
Bygroundingourworkinresearchanddiverseperspectives,weaimtomovebeyondthebroadgeneralizationsoften usedtodiscussyouthmentalhealthandinsteadofferamoreprecise,nuanced,andactionableviewoftheyouthmental healthecosystem,whichcapturesthecomplexitiesofyoungpeople’slivesandthevarietyofinterventionsthatcould supporttheirwellbeing.

● Youthcanencompassalargedevelopmentalrange, includingboththeadolescentandyoungadultstages. Thefieldofyouthmentalhealthbroadlydefinesyouth asthosefrom12-25years(McGorryetal.,2024).
● Youthmentalhealthreferstotheemotional, psychological,andsocialwellbeingofyoungpeople, shapedbytheirlivedexperiencesandthe environmentstheyinhabit.
● Forthepurposesofthisreport,wealsoinclude behavioralhealthundertheumbrellaofyouthmental health,whichrefersto“behaviorsandactionsthat affectwellness”(CDC,n.d.).Thisincludessubstance useandaddiction.
● ThestateofYouthMentalHealthisamultifacetedissue thatisinfluencedbybothindividualpsychologyand behavior,andbroadersocietalfactorssuchas socioeconomicstatus,race,gender,familydynamics, educationalpressures,accesstohealthcare, technologyinnovations,andworldevents.
● Mentalhealthcanencapsulateawidespectrum,from conceptsofwellnessandwellbeingtoahostof diagnosedmentalillnesses.
● Mentalhealthandmentalillnessareunderstood differentlyacrossculturesandcommunities,aswell asacrossgenerationsandwithinfamilies.

Thisanalysisincorporatesdatafromindustryandacademicpublications,expertinterviews,andanovelanalysisofyouthmental healthnonprofitorganizationsintheUnitedStatesusingIRSForm990data.
Areviewofacademicarticlesand industryreportswasconductedto betterunderstandtheyouthmental healthlandscape,ensuringbothdepth andbreadth.Findingsfromthisreview informedthedesignofinterview protocolsandthedevelopmentof searchcriteriaforidentifyingrelevant organizations.
Thereviewfocusedonidentifyingkey trends,gaps,challenges,and opportunitieswithinthefield,providing afoundationforaseriesof semi-structuredinterviewsto investigatetheseareasfurther.
Semi-structuredinterviewswith knowledgeablestakeholderswere conductedtodeepenunderstandingof theyouthmentalhealthfieldandto investigateasetofworkinghypotheses aboutthefield’skeydynamicsand opportunities.Theseconversations providedcontextandinsights, groundingtheanalysisinlived experiencesandexpertperspectives.
Quotesincludedinthisdocumentare drawndirectlyfromtheseinterviewsbut havebeenanonymizedtoensure confidentialityandencouragecandid input.
Almost7,000Organizations
Termsandphrasesidentifiedthrough thereviewoflandscapedocumentsand interviewswereusedtoguidethe analysisofpubliclyavailableIRSdata.
Theseinsightsinformedthesearch criteria,enablingtheidentificationof nonprofityouthmentalhealth organizationsandtheirfunders.


Youthmentalhealthdoesnotexistinisolation;itinfluencesandisinfluencedbythebroaderecosysteminwhichyoungpeople growanddevelop.Whilementalhealthisoftentreatedasitsownsilowithinhealthcare,ayoungperson’swellbeingisshapedbythe entiretyoftheircontexts—includingtheirbiology,identity,anddevelopmentalstage;theirrelationshipswithfamilyandpeers;their experienceswithinschools,workplaces,andcommunityinstitutions;thepolicylandscapethatgovernsaccesstoresources;andthe largersocietaltrendsthatinfluencecultureandnorms.Addressingyouthmentalhealtheffectivelyrequiresasystemicapproachthat accountsfortheseinterconnectedinfluences.
Atthecoreofhealthyyouthdevelopmentandmentalwellbeingisasenseofpurpose,connection,agency,andself-efficacy.Yet,many youngpeople—particularlyyoungadults—reportfeelinglonely,overwhelmedbyachievementandfinancialpressures,and disconnectedfrommeaningandpurposeintheirlives.Critically,relationshipsserveastheprimarybridgebetweenyoungpeopleand thesystemsthatshapetheirwellbeing.Strong,supportiverelationshipshelpbufferstress,buildresilience,fosterasenseofbelonging, andconnectyouthtoresources.Asweconsidersolutions,aguidingquestionmustbe:Howdoesthisenvironment,program,orpolicy supportandstrengthenthedevelopmentalrelationshipsthatareessentialtoyouthmentalhealth?
Philanthropyhasauniqueandpowerfulroletoplayincatalyzingthischange.Philanthropyhastheopportunitytotakerisks,investin innovativemodels,andsupportcommunity-drivensolutionsthataddresssystemicbarrierstocare.Byfundinginitiativesthat strengthenrelationalhealth,expandaccesstoculturallyresponsiveservices,andaddressrootcausesofmentalill-health,philanthropic organizationscanhelpcreatetheconditionsforlong-term,sustainableimprovementsinyouthmentalhealth.Strategic,coordinated investmentshavethepotentialtonotonlyfillgapsbuttoreshapetheecosysteminwaysthatcenterthewellbeingandagencyof youngpeople.

Whilementalhealthisoftenconfinedtoitsownfieldwithinthehealth sector,youthmentalhealthimpactsandisimpactedbytheentire ecosystemsurroundingayoungperson,including:
● theirindividualbiology,identity,anddevelopmentalstage
● theirclosestrelationships(includingparents’mentalhealth)
● thecommunitiesandinstitutionswithwhichtheyinteract(e.g.,schools, youthprograms,religiousinstitutions,socialservices,employment)
● thepolicyenvironment(e.g.,insuranceandeconomicpolicies,local state,city,andschoolboardpolicies)
● thelargermacro-trendsinoursocietythatimpactournorms,values, andsocietalculture (e.g.,technologicaladvances,incomeinequality, racialandgenderinequality,politicalpolarization,climatechange).
Asystemicapproachtoaddressingyouthmentalhealthwouldinclude attentiontotheinfluencesoftheentireecosystemonthewellbeingofyouth.

● Healthyyouthdevelopmentandmentalwellbeingrequiresasenseof purpose,connection,agency,motivation,andself-efficacy.Accordingto recentresearchfromHarvard’sMakingCaringCommon,youth(and particularlyyoungadultswhoarestrugglingatevenhigherratesthanteens) reportalackofmeaningorpurpose,financialworries,andachievement pressureasthemaincontributorstotheirmentalhealthchallenges.Youth alsoreporthigherlevelsoflonelinessthananyotheragegroup.
● Relationshipsmediatetheinfluencesofayoungperson’secology.Close developmentalrelationshipshelpyouthtobuffersourcesofstressandbuild resilience,makesenseoftheirworld,developagency,connecttoresources, andfeelthattheymatter.
● Therefore,aguidingquestionforallstakeholdersinthisworkmustbe:
○ Inwhatwaysdoesthis[practice/program/policy/environment] encourage,enrich,andempowerthedevelopmentalrelationships aroundyouth?(SimpleInteractions)
○ Alternatively,arethereobstaclesthatarediscouraging,diminishing,or disempoweringrelationshipsforyouththatneedtobeaddressedor removed?
“Whatarethetwothingsthataregoing tobemostcoretoteenagersandyoung adultsmentalhealth?Ithinktheanswer [to]thatquestion…wouldbehaving meaningful,gratifyingrelationshipswith peopleandfeelingsomemeaningand purposeinyourlife.AndIdon'tmean havingasinglepurposeoracalling.Ijust meanhavingthingsyouvaluethatyou canpursue...thingsyoucareabout,that youcanpursue.”
-Interviewee

Takinganecologicalperspectiveallowsustoseenuance,complexity,context,andinterdependence, whichinformsasystemicapproachtoimpact.
● Contextmatterswhentryingtounderstandthecausesofmentalhealth challengesanddesignsolutions.Ratherthansolvingageneric“youthmental healthcrisis,”weneedtobeaskingthequestion“what[specificmental healthchallenge]areweaddressingandforwhom”?
● Race,class,culture,andotheraspectsofidentityimpacthowyoungpeople experiencetheirecosystemandtheresourcesandopportunitiesavailableto thematalllevels.
● Mentalhealthalsoimpactsmorethanjustindividualwellbeing-youth mentalhealthimpactsandisimpactedbyaccesstohighquality education,afunctioningdemocracy,economicmobility,andmore.There isalmostnosectorthatdoesnothavearoletoplayandastakeinthegame whenitcomestoyouthmentalhealth.
● Forfundersandpractitioners,it’saboutseeingthesystemasawhole,and ourpartwithinit.It’saboutconnectingthedotstocreateentiresystemsof supportaroundyouth.
Howmightwebuildcoalitionsacrossallecologicalsystemsandsectorswith improvingyouthmentalhealthasthecommongoal?


TheCOVID-19pandemicshonealightonadecades-long declineinyouthmentalhealthandcatalyzedmuch-needed conversationsinthefieldandourbroadersociety.Thisincreasedawarenessledtoanuptickinneworganizations,funding,and prioritization,yetsystemicinadequaciespersistwithregardtoensuringequitableaccesstobothpreventivesupportsandmentalhealth services.Theyouthmentalhealthsystemisfragmented,underfunded,anddifficulttonavigate,withsignificantprovidershortagesand barrierstoaccessingcare.Thisisespeciallytrueforcertainsub-groups,includingruralyouthandyouthofcolor,whoarelesslikelyto accessmentalhealthservices.
Ourinterviewswithkeystakeholdersaffirmedthatthecurrentsystemisnotmeetingtheneedsoftoday’syouth.Changemustgo beyondexpandingservicestoinvestinginyouthvoiceandproximateknowledgeaboutwhatworks,expandingapproachesto care,andaddressingrootcauses.Thereisnoone-size-fits-allsolution,andeffectivemodelsmustbedevelopmentallyappropriate, culturallyresponsive,andintegratedacrosssystems.Multigenerationalapproaches,collectivecaremodels,andcommunity-based interventions-includingpeersupport,arts-basedprograms,anddigitaltools-offerpromisingsupplementstotraditionalclinicalcare. Additionally,ourfindingshighlightatechnologyparadoxinyouthmentalhealth.Whilehighamountsofscreentimeandsocialmedia usehavebeenlinkedtopoormentalhealth,digitalplatformscanalsoprovideimportantopportunitiesforsupport,connection,and therapeuticinterventions.
Ultimately,improvingyouthmentalhealthrequiressystemicchange.Thecomplexityofcoordinatingacrosssectorsmakesthis challenging,butamoreintegrated,responsive,andholisticapproachisneeded.Byrecognizing,asoneofourintervieweesshared,“it doesnothavetobetherapytobetherapeutic,”strengtheningproximateandcommunity-basedsolutions,andfostering collaborationacrosssectors,itispossibletobuildasystemthatholisticallysupportsyouthwellbeing.

Thepandemicexacerbatedexistingmentalhealthchallengesamong many-butnotall-U.S.youth,amplifyingthedemandforservicesand bringingattentiontothegapsinthecurrentsystem. Thereisno“singlestory”ofhowthepandemicimpactedyouth mentalhealth—somestudiesshowincreasingratesofanxiety, depression,eatingdisorders,andsuicidalityamongcertainsubgroups, includinggirlsandyouthofcolor(e.g.,Bridgeetal.,2023;Prichettetal., 2024;Yard,2021),whileothersindicatelittle-to-nochangeandareturn topre-pandemiclevels(e.g.,Brunetteetal.,2023;CDC,2024). However,regardlessofthepandemic’seffects,datashowsadecline inyouthmentalhealthovertime.Forsome,schoolclosuresremoved stressorssuchasbullying,peersocialpressure,andacademic achievementdemands(Penneretal.,2021),whilethosewho maintainedclosesocialconnectionsvirtuallyreportedbettermental healthoutcomes(Jonesetal.,2022).Atthesametime,thepandemic mayhavebroughtgreaterpublicattentiontoyouthmentalhealth, amplifyingconversationsthatwerepreviouslyoverlookedor deprioritized.

Datasource:CentersforDiseaseControlandPrevention.YouthRiskBehaviorSurvey
DataSummary&TrendsReport:2013–2023.U.S.DepartmentofHealthandHuman Services,2024.

The protective effect of increased family time may be particularly true for youths from Latinx backgrounds due to familism, an important Latino cultural construct that puts family as central and prioritizes family as a main source of support and comfort, and that has been shown to be a protective influence for many adolescent outcomes.”
PENNERETAL.,2021

ThegraphsbelowshowthepercentageofhighschoolstudentsintheUnitedStateswhoexperiencedpersistentfeelingsof sadnessorhopelessnessduringthepastyear,bydemographicgroupduringandafterCOVID.Thoughratesbegintodecrease, theyremainalarminglyhigh,particularlyforfemalesandLGBTQ+youth.

Datasource:CentersforDiseaseControlandPrevention.YouthRiskBehaviorSurveyDataSummary&TrendsReport:2011-2021and2013–2023.U .S.DepartmentofHealthandHumanServices.



We had been funding areas to try and destigmatize conversations about mental health...but that became less necessary after COVID. I think COVID really changed the conversation about youth mental health, where it went from being something that no one really talked about to a broad conversation where we could all admit that we were struggling.”

COVIDshonealightonafailingyouthmentalhealthsystemandledtoasurgeinneworganizations,funding,andprioritization. Thetablebelowprovidesaviewofthenumberofnonprofitorganizationsinouranalysisfocusedonyouthmentalhealthand theirfundingflowsbeforethepandemic(2019)andasof2022.Despitegrowth,systemicinadequaciespersist.
BeforethePandemic(2019)
Asof2022
NumberofNonprofitOrganizations ~5,000 ~7,000
ContributionsfromPrivateFoundations
%ofGivingfromPrivateFoundations
Jumptothefollowingsectiontoseehowthesefigureswerecalculated:YouthMentalHealthOrganizationsandPhilanthropicFunding
SeeAppendixforamorein-depthexplanationonmethodologyandlimitations

● Equalaccesstobothproactiveandpreventativesupports,aswellasmental healthcareservicesandproviders,withinthecontextsyouthinhabitisa majorchallengefacingthefield.
● Ateveryleveloftheecosystem,complexitiesabound.Forexample:
○ Atthetheindividuallevel:Youthmaybeexperiencingmultiplemental healthchallengessimultaneouslyorsymptomsthatmaypointtomultiple possiblediagnoses.Treatmentisnotalwaysclear-cut,andthosewiththe samediagnosismayrespondverydifferentlytothesametreatment. Thereisalsotheriskofovermedicalizationofthehighsandlowsofthe humanexperience.
○ Attheinstitutional level:Thetransitionfromchildtoadultcareoften losesyouthinthemiddle.Thereisthechallengeofbureaucracy, especiallyinaccessingcoordinatedmentalhealthcareinschools,which isoftenthefirstlineofsupport.Additionally,therearenumerous challengeswithinsurancecoverageandotherbarrierstoaccessingcare.
○ Atthesocietallevel:One’sexperienceandunderstandingofmental healthandmentalillnessisinfluencedbycontextandculture.This requiresunique,culturallyandcontextuallyrelevantapproachesto prevention,support,diagnosis,andtreatment.

Inequalityinaccesstomentalhealthcareisanenormouschallenge.Therearebothnotenoughprovidersandnumerous barrierstoseekingoutandaccessingcare.
● In2023,almost60%ofyouthwithdepressiondidnotreceiveanymentalhealthtreatment(MentalHealthAmerica,2024).
● AsofDecember2023,morethanhalfoftheUSpopulationliveswithinaMentalHealthProfessionalShortageArea(defined asapopulationtoproviderratioof30,000ormoreto1),withruralareasparticularlyaffected.Itispredictedthatthese shortageswillcontinueorgetworseoverthenext10+years(NationalCenterforHealthWorkforceAnalysis,2023).
● Disparitiesareevidentinbothaccesstoservicesandqualityofcare,withhistoricallyunderservedcommunities,particularly youthofcolorandruralyouth,facingmorebarriers.Thisiscompoundedbyalackofculturallycompetentcareandadearth ofdiversepractitioners.
○ Youthofcolorreportthatpractitionerculturalunderstandingismostimportanttothemintheirwillingnesstoengage inmentalhealthcare(Chuetal.,2022).
Itiscriticaltobothremoveaccessbarriersandbuildadiverse,culturallyresponsivementalhealthcareworkforce.

The pyramid for the mental health workforce is backwards... Most states are only skilling and licensing at the top of the pyramid, meaning we have too many highly specialized providers but not enough community-based, culturally competent care that can meet young people where they are.” INTERVIEWEE

MorethanhalfoftheU.S.populationlivesinamentalhealthprofessionalshortagearea.Whilethereisalsoaprimarycare professionalshortage


TheUSPsychologyworkforceis79%whiteand72%female.Formanyyouth,thismeanslackofaccesstoaproviderwitha sharedbackgroundoridentity.

Datasource:AmericanPsychologicalAssociation.DataTool: DemographicsoftheU.S.PsychologyWorkforce,2023.

WhencomparingRace/Ethnicitybetweenthegeneralpopulationandthepsychologyworkforce,disparitiesemerge, highlightingtheurgentneedtomakethementalhealthworkforcemorerepresentative.

Datasource:UnitedStatesCensusBureau.PopulationEstimates,July1,2024.

Ofthoseexperiencingmentalillness,communitiesofcolorarelesslikelytoreceivetreatment.
● Youthofcolorfacegreaterbarrierstoaccessingcare duetomultiplefactorsincludingstigma,discrimination, alackofculturallyresponsiveproviders,andcoverage barriers,andthereforeaccessmentalhealthcareat lowerratescomparedtothewhitepopulation.
● Duringthepandemic,thereissomeevidencethat mentalhealth(depression,anxiety,suicidality)declined atlargerthanexpectedratesforBlack,Asian,and Hispanicpopulationscomparedtothewhite population,andthatthesegroupsweresignificantly morelikelytohaveanunmetmentalhealthcareneed (Thomeeretal.,2022).

Source:CenterforBehavioralHealthStatisticsandQuality,2021

Healing can also be scary... if you don't even think that you're worthy of receiving support.”

● WhilealsoacknowledgingthatstigmarelatedtomentalhealthhasdecreasedsincetheCOVID-19pandemic,many intervieweeshighlightedpersistentculturalstigmaaroundseekingmentalhealthcare,particularlyincommunitiesofcolor (McGorryetal.,2024;Misraetal.,2021;Thornicroftetal.,2022).Culturalsensitivitiesarounddirectlydiscussingmental healthoftenleadstotheuseofalternativephrasestodescribementalhealthandmentalillness.
● Severalinterviewparticipantsexplainedthatthestigmaisn’tjustaboutwhatotherswillthinkofyou;it'salsoaboutifyou thinkyouareworthyofreceivingcare.“Thewaysinwhichwetalkaboutstigmaaredifferent...Peopleactuallywanttogoto therapy,butit'slikemakingsurethattheyfeelworthyenoughtoheal,andworthyenoughto,youknow,changethe trajectoryoftheirlife.”
● Whiletheoverwhelmingmajorityofyouthsaythattheythemselveswouldnotthinklessofsomeonewhohasreceived mentalhealthtreatment,over60%believeotherswould(Brunetteetal.,2023;Eisenbergetal.,2009).
● Theavailabilityandaccessibilityofculturallycompetentcare,aswellasthoughtfullydesignedpublicawarenesscampaigns (thatde-stigmatizementalillnesswithoutmakingitatrendtopathologizehumanemotions)areessentialstrategiesto combatstigma.
Tobeeffective,effortsmustalsoaddressinternalizednarrativesandhelpindividualsseethemselvesas deservingofcareandsupport.

It is not really a system. It is a fractured patchwork set of services.”

Theyouthmentalhealthsystemfacescriticalchallengesduetofragmentation,chronicunderfunding,andoutdatedoperations. Onethingisclear:ourintervieweesdidn’tthinkthesystemwasmeetingtheneedsoftoday’syouth.
Integratingmentalhealthservicesinto primarycareandschoolsischallenging becauseofthenecessarydifferencesin training,funding,andorganizational goals.Thiscreatesatensionbetween theneedforcomprehensive,integrated careandtherealityofthesystems currentlyinplaceandtheirunique needs.
Provided Community-basedmentalhealthcare caneffectivelymeetlocalneedsand offeraccessibleservicesinawaythat traditionalhealthsystemscannot. However,theyfacesystemicbarrierslike limitedfundinganddifferingcommunity basedapproaches,attitudes,andbeliefs towardsmentalhealth.Thesebarriers reduceaccesstocareandeffectiveness, unfairlyshiftingtheburdentothe communityandoftenleadingto inadequatecare.
Individualizedvs.UniformStandards
Addressingmentalhealthdisparities requiresattentiontotheyouthin context,ensuringallyouthhaveaccess toquality,culturallyresponsivecarefrom representativeproviders.However, there'stensionbetweenthisneedfor tailoredservicesandthepushfor uniformstateandnationalstandards, whichcanconflictwithproviding customizedcare.

It’s not just about one tool or model. We need a whole system of supports that can adapt and connect, from peer support to tech innovations to school-based care.”
INTERVIEWEE

Therewasasharedsensethatwithoutconcerted,systemicchange,theseissueswillcontinuetohinderprogress.
● Youthmentalhealthcareishighly"geographic-specific"becauselicensingandregulationshappenatthestatelevel. Thismeansthatnavigatingdifferentstaterulescanbeasignificantbarrier.
● OutdatedinsurancereimbursementandMedicarepoliciesandcodesmakeitdifficultformentalhealthservicesto adaptandgrow.
● Thecomplexityofcoordinatingwithvarioussystems,includingschools,localhealthdepartments,andstateregulators meansthatintegratingnewinitiativesintotheseexistingframeworkscanbechallenging.
● Thereisstrongconsensusthatsilosbetweenmentalhealthcaresystemsandschoolshinderthedevelopmentof comprehensiveyouthmentalhealthprograms.
○ Schoolsareunderutilizedintermsofprovidingmentalhealthsupport,yetschoolsoftenrequireextensive approvalsandstandardizedprocessesforintegratingnewmentalhealthprograms.Thisbureaucraticprocesscan actasabarrier,preventingtimelyandeffectivecollaborationsbetweenhealthcareprovidersandeducational institutions.
○ Oneintervieweegavetheexample,“Therapydeliveredinschoolswasonlyreimbursedifithappenedbehindtwo doorsfromapublicspace...Thatmeantthattherapycouldonlybereimbursedifitwasbeingdoneinacloset.”

“There is, like, no evidence.”
Changeinyouthmentalhealthwillnotonlycomefromserviceprovisionbutalsofromcreatingevidenceandscienceabout whatworks.Thisinsighttookonafewdifferentformsfromourinterviewparticipants.
1. Thefieldlacksobjectivetests,diagnostictools,andcleardataaboutbiomarkersandgeneticmarkers.
2. Thereisnotenoughresearchandevidenceunderpinningthecarebeingprovidedinthesectorrightnow.
3. Thereisalackofdefinitiveknowledgeaboutwhathascausedthedecades-longdecline.
● Intervieweesshared:
○ "Ifeellikeeveryonesaysit.Ifeellike...IwouldlookattheresearchandIwouldthink,thisisn’tastrongevidence base,butalotofdecision-makersdon’thavethetrainingthatIhad.Andso,Ithinkit’seasytosaythisis research-basedorevidence-based.Idon’tknowhowmanyreallyare."
○ "It'sconcerningthat...someofthepracticesouttherearenot,youknow,evidence-based,there'snoresearch backing.And...lessthanhalf[oftheyouthwhoreceiveservices]actuallygetevidence-basedpractices".
○ "There’slikenoevidence,particularlyinresearchingyouthofcolorinthiscountry...That’stheevidenceright there,thelackofevidence."
○ "Currently,inmentalhealth,tosomeextent,they'retryingtoreplicatewhathasbeendoneforadultsandkindof putitinaboxforyouth."
○ “Everybodyelsehasanobjectivetest.Youhaveascratchythroat,Iswab,andifyouhavestrepthroat,Iknowyou havestrepthroat.Wedon’thavethatmagicinchildpsychiatry…Wearelookingforthat.”

I feel like the mental health conversation, the narrative is pretty much like this: that the population we should be most worried about is teens, and the reason we should be most worried about them is social media…But our data…presents a very different picture…Young adults, 18 to 25, are suffering about twice the rate of anxiety and depression as teens are.”

…actually the main idea that our data supports, which is not the idea that anyone wants to hear, is that there is literally no one-size-fits-all solution for all of this.”
YOUTHINTERVIEWEEANDTEENMENTALHEALTHRESEARCHER

Partofremovingbarriersisunderstandingthat,whenitcomestoyouthmentalhealthcare,thereisnoone-sizefitsall.Weneed arangeofresponsiveapproachestotreatmentandcarethataretailoredtoyoungpeople’sneedsanddevelopmentalstage(as opposedtosimplymimickingadultmodels).
● Collaborativeandintegratedcaremodelshavebeenshowntoincreaseaccesstocareandimproveadolescentdepressive symptoms.Similarly,studiesshowthatfamilytherapymodelsareeffectiveintreatingyouthmentalhealthandbehavioral disorders.Thatsaid,theresearchdoesnotpointtotheseformsofcarebeingbetteroverall-itwilldependonthecontext (Asarnowetal.,2005;Hopkinsetal.,2017;Jiménezetal.,2019;Richardsonetal.,2014;Wrightetal.,2016).
○ Oneintervieweeshared,“Ithink,aswithallofmentalhealth,muchof[thetreatmentapproach]dependsonthe individualwhoisstruggling.Somedobetterwithindividualfocus.Othersdobetteringroups.”
● Benefitsofcollectivecareincludethatithelpsbuildsocialsupportnetworksandcanprovidescalablecare.However, concernshavebeenraisedaboutthecomplexityofrelationshipswithinthesegroups,particularlyforyouthwhose multifacetedidentitiesandexperiencesmaynotbefullyacknowledgedandacceptedamongstgroupmembers.While somepapersemphasizethebenefits,otherscautionagainstover-relianceontheseapproaches,pointingouttheneedfor personalizedcareandculturalsensitivitytoavoidalienatingindividualswithinthegroup.
● Addressingtherootcausesofyouthmentalill-health(e.g.,poverty,isolation,housinginsecurity,trauma,toxicstress) fromamultigenerationalperspectiveisalsocritical(McGorryetal.,2024).

It does not have to be therapy to be therapeutic.”

Community-basedinterventions,peersupport,arts,anddigitaltoolscanallprovidetherapeuticbenefits,presentingabroader, moreaccessibleapproachtomentalhealth.Thisideashiftsperspectivesfromamedicalizedviewofmentalhealthtoamodel whereeverydayactivitiesandcommunityconnectionsalsoplayvitalroles.
● Non-traditionalapproachescanbemoreaccessibleandrelatable,particularlyforyouthwhomightnotengagewith traditionaltherapy.
● Buildingsupportive,youth-centeredenvironmentsincludedtheexpansionofdigitalhealthtoolsandcommunity-based servicesthatprovideaccessiblementalandbehavioralhealthsupportandopportunitiesforhealthyconnectionand engagementoutsidetraditionalclinicalsettings.
● Interventionsthathelpyouthtoformstrong,supportiverelationships,findmeaningorasenseofpurpose,manageor mitigatestressorsintheirenvironments,andfeelcompetentandagentivecanallbeseenasaddressingrootcausesof youthmentalhealth.
○ Oneexpertshared,“Howdoyouhelpkidsdevelopmeaningfulrelationships?Howdoyouhelpthemdothingsthatare meaningful?I'mverybigonservicethesedaysandcollectiveservice,workingtogether.BecauseIthinkithelpswith loneliness;helpswithmeaningandpurpose;ithelpswithanxietyanddepressionforyoungadults.”

I think something that's really important is to consider the factors that are driving youth to go on their phones and breed that disconnection. And maybe [it’s] not as much that the phones are the root cause of that disconnection. I think that, in so many situations, youth are turning to their phones because there's not space to [connect] otherwise.”
YOUTHINTERVIEWEEANDTEENMENTALHEALTHRESEARCHER

Socialmedia,screentime,anddigitalplatformscancontributetoanxietyanddepression,buttheyalsoofferavenuesfor support,connection,andinnovativetherapeuticinterventions.
● Researchandinterviewsemphasizedtheneedforabalancedapproach,ensuringthatdigitalplatformsareusedeffectively andsafelytosupportyouthmentalhealth(Weinstein&James,2022).
● Socialmediacanexacerbatementalhealthissueslikedepression,anxiety,andlowself-esteem,particularlythrough cyberbullying,negativesocialcomparison,andexcessivescreentime.Thenegativeimpactisespeciallypronouncedfor girls(Achterbergetal.,2022;Boersetal.,2019;Brunetteetal.,2023;Odgers&Jensen,2020;OSG,2021;Orben& Blakemore,2023;Twenge&Farley,2021;Twengeetal.,2022;Usborne&Taylor,2010).
● But,asourintervieweesshared,nuanceisnecessary."There'smixedfindings...somestudiesshowpositiveimpacts, especiallyforyouthfrommarginalizedbackgrounds...[who]getasenseofbelongingfromsomeonlinespaces."For LGBTQ+youth,“it’salifeline.”
Singularnarrativesthatpointtotechnologyasthesolecauseofyouthmentalhealthproblemsleadtooverlysimplisticand single-mindedsolutions(e.g.,simplybanningorrestrictingyouth’saccesstotechnology),ratherthantakinganuanced approachthatidentifiesrootcauses,teacheshealthytechhabits,andleveragesthepotentialbenefitsoftechnologyin serviceofthosewhoneeditmost.

There's so much more pressure that teens are facing now from so many areas. And like, the fact that we have to be on the clock. I would [be] in middle school, [and] I was getting emails from my teachers on the weekends, and then high school, these random deadlines [over the weekend]. Like this is also something that's so new to the generation and has obviously never happened before. That's also important to consider.”
YOUTHINTERVIEWEEANDTEENMENTALHEALTHRESEARCHER

So
I think what we need to look at is not banning kids from social media or the digital ecosystem, but empowering them with the knowledge of how to use this power tool and to recognize it as a power tool, not as a toy, not as a playground, but as a tool that can do great good or great harm.”

Whiletechnologyisoftenseenaspartoftheproblem,telehealthanddigitalmentalhealthtoolshavethepotentialtoprovide solutions.Thesetoolsareviewedascrucialforincreasingaccessibilitytomentalhealthcare,especiallyforunderserved populations.
● Technologyhasthepotentialtobeusefulfor:expansionoftelehealthservices;coordinatingcare;offeringadditional supports;andprovidingdigital peersupportandcommunity.
● Thereisinterestintheuseoftechnologytoincreaseaccesstomentalhealthcarefrombothyouthandpractitioners,and evidencethatinternet-basedCBTandotheronlinementalhealthpromotionandpreventioninterventionscanbeeffective inpromotingyouthmentalhealth.Thosethatinvolvearelationalorface-to-facecomponenthavebeenshowntobe evenmoreeffective(Alvarez-Jimenezetal.,2021;Anderssonetal.,2019;Belletal.,2022;Brunetteetal.,2023;Clarkeetal., 2015;D’Alfonsoetal.,2017;Halletal.,2022;McGorryetal.,2024;vanDoornetal.,2023;Worsleyetal.,2022).
● Telehealthmaybeanespeciallypromisingwaytogetyouth“inthedoor”toaccessmentalhealthservices.Oneclinician shared,“...beforethepandemic,wehada25to30%noshowrateonfirstvisits…InMarch2020,wewentallvirtualovernight, andournoshowratedroppedtozerobecausethey'recomfortableandmasterfulinthisenvironment.”
● AIchatbotshavealsoenteredthesceneasalow-barrierentryintomentalhealthandcounselingsupport,butmustbebuilt toeffectivelyconnectyouthtorealhumanrelationships,ratherthansupplantthem.Oneintervieweeshared,“We’recoming upwithanother[tool]calledMirror,becauseAmy'sgotdepression...Thisistherapeuticjournaling,andthere’sawaythatif shegetsworsewecanalerther,saying,‘Yoursymptomsseemworse,reachouttothiscrisislineoryourmother.’”

We draw artificial boundaries between the real world and the virtual world. For kids, this is a single world. They’re seamlessly in and out of the screen environment, and we have to recognize and respect that, but do it in a way that allows them to learn how to be good citizens in this space, how to show respect for each other and for themselves, how to be healthy, and how to be optimistic, as opposed to dystopian.”
INTERVIEWEE


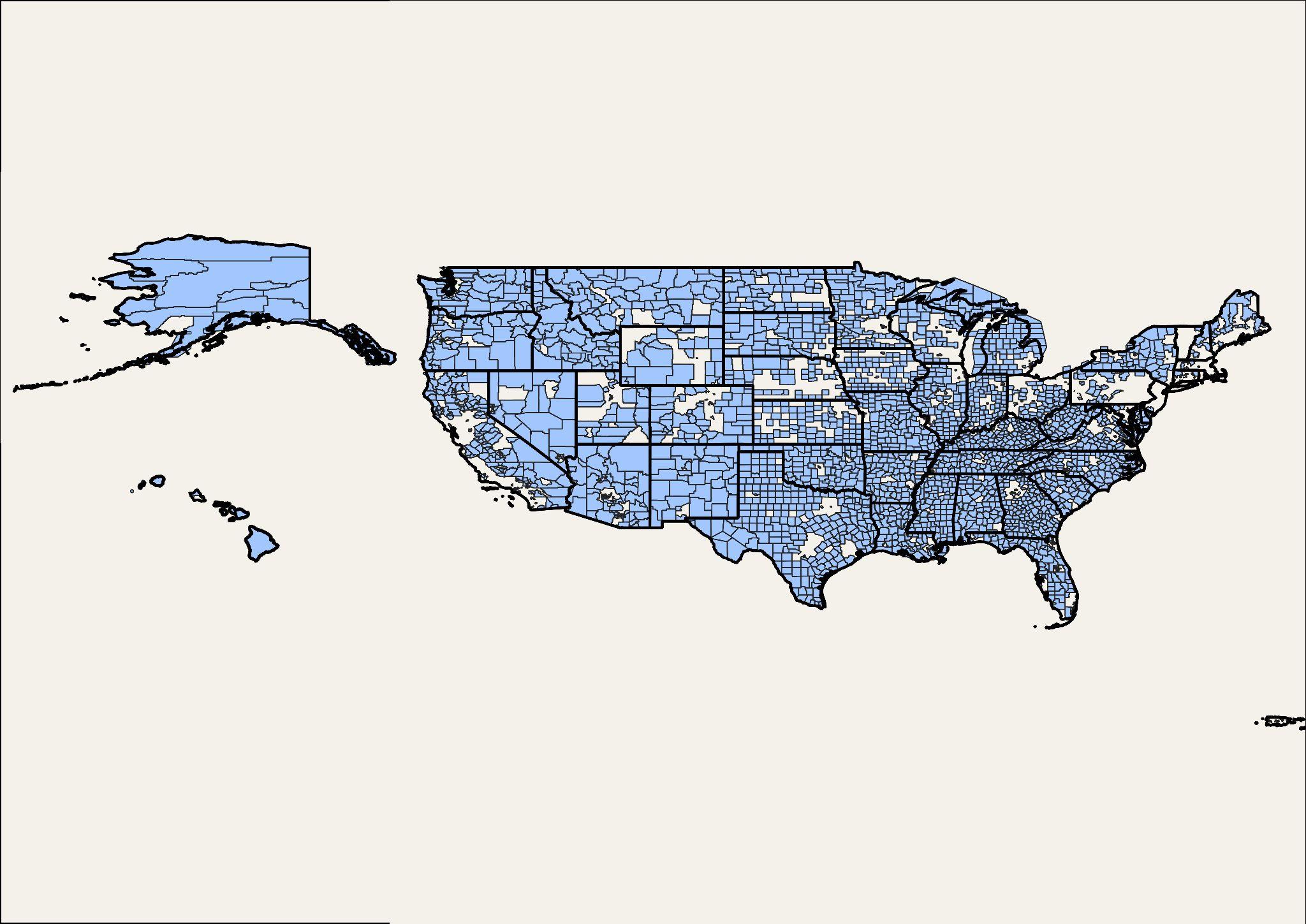
YouthmentalhealthnonprofitsintheUnitedStatesvarywidelyintermsofprogrammaticfocus.Thisvariabilitymakesit difficultfortraditionalclassificationsystemsliketheNationalTaxonomyofExemptEntities(NTEE)tocaptureallofthe organizationsworkinginthisspace.Toaddressthisgap,usingpubliclyavailableIRSForm990dataandakeywordanalysis,we identifiednonprofitsthatalignedwithourexpansivedefinitionofyouthmentalhealthandtheirprivatefoundationfunders. Thisanalysisprovidedinsightsintothegeographicdistributionofbothorganizationsandphilanthropicfunding.Aheatmapof youthmentalhealthnonprofitsshowsthatthehighestconcentrationsareontheWestCoastandtheNortheast,withafew clustersdistributedthroughouttherestofthecountry.However,whenlookingatthedistributionoffunding,thepicture becomesmorestark.Fundingisevenmoreconcentratedthantheorganizationsthemselves,witharelativelysmallnumberof geographicareasreceivingadisproportionateshareofresources.
Inadditiontogeographicdisparities,ourfindingssuggestabroaderchallenge:thephilanthropicfundinglandscapeof youthmentalhealthisfragmented,withmostfundersgrantinglessthan$100Kpergrant.Lackofsustainable,long-term investmentpreventsmanyorganizationsfromachievingtheirobjectives.Additionally,tensionsemergebetweenphilanthropic supportandlong-termsustainability,short-termwinsversuslong-termsystemicchange,andtheneedforbettercoordination topreventduplicationofefforts.Thissectionconcludeswithacloserlookathowfocusareaswithinmentalhealthreceive varyinglevelsofsupport,underscoringtheneedtoalignfundingwithneed.

TheNationalTaxonomyofExemptEntities(NTEE)isa classificationsystemthefederalgovernmentusesto classifynonprofits.Someexamplesub-categoriesfor MentalHealthandCrisisInterventionareprovidedtothe right.
Ourexperienceworkingwithourmentalhealthequity cohortrevealedthatmanyoftheorganizationswewere workingwithandspeakingtowerenotclassifiedintoanyof theseMentalHealthandCrisisInterventioncategories.
ClassificationsystemslikeNTEEprovideahelpfulbaseline, butfallshortincapturingthebreadthoforganizations workinginaparticularsector.
Challenge:howmightweidentifyamorerepresentative setoforganizationsworkingtoaddressyouthmental healthintheUnitedStates?

Createadataset:procuremillionsofIRSForm990filingsfor nonprofitorganizationsandprivatefoundationsthatcontain descriptiveprogrammaticandgrantinformation.
Developbagofwordssearchterms:synthesizefindingsfromdesk researchandinterviewstocreateasetoftermsthatcanbeusedto identifyyouthmentalhealthnonprofitsandtheirfunders.
Identifyorganizations:complementexistingclassificationsystems byapplyingthebagofwordssearchtermstoprogrammatic descriptionstoestablishasetofyouthmentalhealthnonprofits.
Identifyfundingflows:identifytheprivatefoundationfunding sourceandamountbycheckingthegrantrecipientinformation providedbytheprivatefoundation.
Theresultinglistoforganizations reflectNewProfit’sdefinitionofthe youthmentalhealthlandscape. Pleaseseeappendixforadditional information.

Thewayyouthmentalhealthworkisdiscussedoften divergesfromjargon-heavy,field-specificlanguage.This disconnectcanmakeitchallengingtoidentifyandengage withorganizationseffectivelyaddressingyouthmental healthneeds.Inconversationswithleadersinthisspace, severalexamplessurfacedthatprovidedclarityandhelped bridgethisgap.Theseexamplesnotonlyhighlightedthe diversityofapproacheswithinthefieldbutalsoenabledus torefineourbagofwordssearchtermstoidentifyabroader andmorerepresentativerangeoforganizations.
"JoyisprobablyoneofthebestwaysthatIhear mentalhealthtalkedabout,particularlywithin theBlackcommunity,aslikefindingjoy,or,you know,harnessingyourjoy,empoweringyour joy.Joy,isonewaythatIhearalotofpeople talkaboutmentalhealthwithoutlikesaying mentalhealth.”
Interviewee

Theheatmapbelowillustratestherelationshipbetweenpopulationandnumberofyouthmentalhealthorganizationsatthe countylevel.Evenwhenaccountingforpopulationdisparities,muchoftheUnitedStateshaslimitedaccesstotheyouthmental healthecosystem.Thisrepresentsakeyopportunityforsocialentrepreneursandphilanthropicleaderstosupporttheseareas.
NumberofYouthMentalHealthOrganizations
Limitations of GeographicalAnalysis:This analysis relies on addresses reported in filings, but many nonprofits serve beyond their listed locations.As a result, the map may not fully reflect their true service catchments. For more details, jump to the slide on limitations in the appendix.


Whenwelookbeyondtheorganizationsandexaminethefundingflows,weseethesameunderlyingthemeamplified.Theflows areevenmoreconcentrated,presentingfunderswithacriticalopportunitytorefinetheirfundingstrategiestosupportemerging opportunitiesinlow-accessareas.
ConcentrationofFunding
$0-$1k
Limitations of GeographicalAnalysis:This analysis relies on addresses reported in filings, but many nonprofits serve beyond their listed locations.As a result, the map may not fully reflect their true service catchments. For more details, jump to the slide on limitations in the appendix.


Fundingremainsacomplexissue,withmanyyouthmentalhealthinitiatives,particularlysmaller,proximate,andcommunity -basedorganizations,strugglingtogrowbeyondacertainlevelduetoalackofsustained,long-termfunding. Whilethere hasbeenanincreaseinphilanthropicinterest,thefocusoftenleanstowardsshort-termwins,ratherthansystemicchange.
Short-termfundingfromphilanthropic organizationsiscrucialbutcreates tensionbetweenimmediateresource needsandlong-termsustainability. Wheninitialfundingends,manymental healthprogramsstruggletocontinue, leadingtoinstabilityanddiscontinuityin care.Manyorganizationsaredependent onrelativelysmallgrants(e.g., $100k-$200k),whichmakesitdifficult forthemtoplanlong-termandexpand theirservices.
Fundersandpolicymakersoften prioritizeinitiativeswithimmediate results,likecrisisinterventionand short-termtherapy.Thiscreatestension betweenseeingfastimpactand investinginlong-termsolutions,suchas prevention,earlyintervention,and systemicchange.Manyfundersare perceivedascautious,whichcan preventinnovative,early-stage nonprofitsfromgettingthenecessary backingtoscale.
Thementalhealthsystemis fragmented,withfundersoften supportingsimilarinitiativeswithout coordination.Thiscreatestension betweentheneedforacohesive, effectivesupportsystemandthereality ofindividualfunderswantingtomove quicklyandfundcausestheycareabout. Thisleadstoduplicateefforts, inefficiencies,andunevensupport.

“
I would say the biggest dynamic is that the the field is so dramatically under-resourced… you spend all these time in philanthropic convenings, where everyone's talking about a culture of abundance, and all of that doesn't exist in mental health because you have very good people who've been working really hard for a long time with very, very little money.”
INTERVIEWEE

Ouranalysisindicatesthattherearemorethan6,000privatefoundationsmakingcontributionstoyouthmentalhealth organizations.Fewerthan100ofthesefundersaccountfor50%ofthetotalgivingtoyouthmentalhealthorganizations.
Theaveragecontributionamountis~$23k.


Improvingyouthmentalhealthrequiresamulti-facetedapproachthatenhancesaccesstocare,strengthenscoordination acrosssystems,andbuildsrelationalenvironmentsinwhichyouthcanthrive.Thismeansbothimprovingaccesstomental healthcareforallyoungpeopleandstrengtheningtheecosystemssurroundingyouthsothatitsupportstheirwellbeing,aswell asthewellbeingofthosewhocareforthem.Thislookslikesupportingfamiliesandworkingtoreducebarrierstoaccessingcare suchasstigma,geographicandsocioeconomicbarriers,andlackofculturallyresponsiveandyouth-centeredservices,aswellas greaterintegrationacrosseducation,healthcare,andcommunityorganizationsisessentialtocreatingasystemofcare.
Youthareuniquelypositionedtobothprovideinsightintotheirexperienceswithmentalhealthandwellbeingandto designinnovativesolutionstomeettheirneeds.Inpartnershipwithsupportiveadults,youthhavethepotentialtoleadon theseissuesandtoreimaginethecontextsthatsupporttheirpositivedevelopment.
Philanthropyhasauniqueroletoplayincatalyzingsolutionsinpartnershipwithyouth,frominvestinginproximate organizationsandsocialentrepreneurstoleveragingitsconveningpowerandfillingfundinggaps.Byprioritizinglong-term, sustainedinvestment,supportingeffectivepolicydevelopment,andcatalyzingnewknowledgeofwhatworksandforwhom, philanthropycanhelptransformtheyouthmentalhealthecosystemintoonethatismoreaccessibleandeffective.Nowisthe timetomovebeyondfragmentedeffortsandinvestinsolutionsthatenableallyoungpeopletothrive.

“
There are a lot of really smart people out there who know what we can do to improve mental health in our country. But...there wasn't anybody really focused on building power to do the systems change work.”
INTERVIEWEE

Theserecommendationsfocusonstrategiestoimproveaccesstomentalhealthcareforallyoungpeople,including usingtelehealth.
● InvestinBuildingaDiverse,CulturallyResponsiveWorkforce:Increasethenumberanddiversityofmentalhealth providers,particularlyforunderrepresentedgroupsandinmentalhealthshortageareas.Ensurethatallprovidersareskilled inprovidingculturallyresponsivementalhealthcare.
● ExpandDigitalandTelehealthServicesResponsibly:Increaseavailabilityoftelehealthandotherdigitalservicesto provideremotementalhealthcare,especiallyinunderservedareas.LeveragetheaffordancesofAIanddigitaltechnologies, whilecontinuouslyprioritizingstrengthenedhumanrelationshipsasthecoreobjective.
● EnhanceCrisisInterventionServices:Improvecrisisinterventionserviceslikehotlinesandmobilecrisisteamstooffer immediatesupportforyouthindistress.
● SimplifytheReferralSystem:Makethereferralsystemeasierforparentstonavigatewhenseekinghelpfortheirchildren.
● ContinuedTrainingforPrimaryCareClinicians:Provideongoingeducationandtrainingforprimarycarecliniciansto betteraddressmentalhealthneeds.
● FocusonPreventionandEarlyIntervention:Emphasizeearlyidentificationandpreventionofmentalhealthissuesthrough universalscreening,crisisintervention,andpromotingresilienceandcopingskills.

Theserecommendationsemphasizetheimportanceofintegratingmentalhealthcareacrossdifferentsystemsand sectors.
● CreateaFrameworkofConnectedness:Establishaframeworkconnectingeducationalinstitutions,families,and healthcareprovidersthroughdigitalhealth.
● EnhancePost-HospitalizationSupport:Ensureyouthreceiveadequatesupportandfollow-upcareafterbeing hospitalizedformentalhealthissues.
● CoordinateCareAcrossSystems:Developsystemsthatcoordinatementalhealthservicesacrossvariousagencies, includingeducation,healthcare,andjuvenilejustice.
● IncreaseCross-SectorCollaboration:Takepracticalstepstoenhancecollaborationacrossdifferentsectorstoimprove youthmentalhealth.
● SupportTransition-AgeYouth:Providespecializedservicesandsupportforyouthtransitioningfromchildtoadultmental healthservicestoensurecontinuityofcare.

Theserecommendationsemphasizetheneedforgap-fillingresearch,strengthenedcollaborationbetweenandwithin researchandpractice,andtheimplementationofinterventionsgroundedinproximityandevidencethattheymakean impactonwhatmattersmostforyouthmentalhealth.
● ImproveDataSystems:Enhancesystemstobetteridentifypersonsatriskforsuicideandothermentalhealthcrisesand advanceourknowledgeofriskfactorsandeffectiveinterventionoptions.
● EnhanceDataCollectionandAnalysisMethods:Improvethecollectionandanalysisofdatarelatedtomentalhealthcrisis preventionefforts.Investinunderstandingheterogeneityinmentalhealthdeterminants,diagnoses,treatment,and outcomes.Ask,arewemeasuringwhatcounts(e.g.,relationships),orjustwhatcanbecounted?
● StrengthentheResearchandPracticeCommunity:Enhancecollaborationandeffectivenesswithintheresearchand practicecommunitiessothatpracticeandlivedexperienceinformswhatweknow,andwhatweknowinformspractice.
● IncreaseFundingforInnovativeApproachestoEvidence-Building:Allocatemorefundstowardsunderstandingthe experiencesofthosefarthestfromaccessandtherangeofinterventionsthateffectivelyservetheirneeds.Focuson understandingthemechanismsofchangeandtheirfunctioninanintervention,ratherthanreplicatingoneparticularform.
● TranslateandShareKnowledge:Createcontinuousknowledgetranslationandsustainablementalhealthprevention strategies,literacy,anddigitalnavigationtools.Createopensciencenetworks.Sharewhat’sworkingandwhatwaslearned infailure.

We really need to get on the prevention front…the analogy that comes to mind…it's like you have a highway where there are a lot of car accidents. You can get more ambulances, you can build more hospital beds, or you can fix the highway. I feel like we're not fixing the highway.”
INTERVIEWEE

Theserecommendationsfocusoncreatingsupportiveenvironmentsinschools,communities,andhealthcaresettings tofostermentalwellbeing.
● SupportEducatorsandSchoolStaff:Providetrainingandsupportforteachers,counselors,andschooladministratorsto recognizeandappropriatelyrespondtomentalhealthissues.
● FosterYouthIdentity,Agency,andResilience:Assistyoungpeopleinforminghealthyidentities,gainingindependence,and feelingasenseofagency.Buildsocialandemotionalskillstohelpmanagestressandemployhealthycopingstrategies.
● AddressBullyingandCyberbullying:Implementanti-bullyingprogramsandpoliciestocreatesafeenvironmentsforyouth bothinpersonandonline.Explicitlyteachyouthhealthytechhabitsandprovidestrategiestoavoidharmfultechuse.
● CreateSafeandSupportiveSchoolClimates:Createschoolenvironmentsthataresafe,supportive,andconduciveto learning,socialandemotionaldevelopment,andmentalwellbeing.
● FocusonRelationships:Ensurethatallyouthfeelconnectedtocaringadultsintheircommunities.
● AdoptaYouth-CenteredApproach:Makementalhealthservicesmorerelevantandaccessibletoyoungpeople.
Whenweaskyouthandlistentotheirexperience,wecanco-designsolutionsresponsivetotheirlivedreality.

Theserecommendationsemphasizetheroleoffamiliesandcommunitiesinsupportingyouthmentalhealth.
● ProvideParentalEducationandSupport:Offerculturallyresponsiveprogramsthathelpparentsrecognizementalhealth issuesandsupporttheirchildren.Theseprogramsshouldencourageopendiscussionswithoutfearorshame.
● DeliverServicesbyParentsforParents:Createandfundservicesdeliveredbyparentsforparents,buildingasupportive communityofpeers.
● ProvidePlanningAssistance:Offerassistancewithplanningformentalhealthsupportatboththefamilyandcommunity level.
● HelpYoungPeopleBelongandConnect:Aidyoungindividualsinfeelingasenseofbelongingandconnectingwith appropriatesocialcircles,includingfamily,friends,andneighborsinthecommunity.
● NormalizeMentalHealthConversations:Encourageopendiscussionsaboutmentalhealthinallsettingstonormalize seekinghelpandreducestigma.
● IncreasePublicAwarenessCampaigns:Educatethepubliconmentalhealthissuesthroughtailoredcampaigns.

Theserecommendationsfocusonaddressingunequalaccesstomentalhealthservicesandsupportsandopportunities forinvestinginproximateinterventionsthataddressrootcausesandareasofhighestneed.
● AddressSocioeconomicBarriers:Recognizeandaddresspovertyasarootcauseofmentalhealthchallenges.Reduce barrierssuchaslackofinsuranceortransportationthatpreventyoungpeoplefromaccessingmentalhealthservices.
● RecruitandRetainEthnicallyDiverseStaff:Employmethodstorecruitandretaindiversestaffsoallyouthhaveaccessto providerswithsharedbackgroundsandlivedexperiences.
● DevelopProgramsforUnderservedGroups:Create(withyouth!)targetedprogramsforsub-groupsofyouth,suchas LGBTQ+youth,toaddresstheiruniquementalhealthneedsandpreferredmodesofintervention.
● EmphasizeInclusiveandCulturallyResponsivePractices:Focusonculturallyresponsiveandinclusiveapproachesin training,practice,research,andpolicy.
● FocusonRootCauses:Tacklebroadersocialdeterminantsofmentalhealth,includingsocioeconomicstatus,structural inequality(e.g.,unequalaccesstohousing,qualityeducation,employment,developmentalrelationships,socialties), politicalpolarization,andmarginalizationthatleadtodisparateexperiencesofmentalhealthandwellbeing.
● ReinventInstitutionalStructures:Raiseawarenessandtakeactiontoidentifyandreformorreinventinstitutional structuresthatmaintaininequalityatalllevelsoftheecosystem.

Philanthropyhasmultipleleversatitsdisposaltomakeacrucialdifferenceforyouthmentalhealth.Thefollowing recommendationsareacalltoactionforphilanthropytostepup,fillgaps,andhelptocatalyzetheeffortsof organizationsandsocialentrepreneursdoingtheessentialworkofcreatingecosystemswhereallyouthcanthrive.
● Co-designwithyouth: Alltoooften,prioritiesaresetandsolutionsaredevelopedwithouttheinputofyouth,whoaremost proximatetothechallengesandopportunitiesimpactingtheirmentalhealth.Ensureyouthareatthetabletoco-createsolutions thatareresponsivetotheirlivedrealities.
● Investinproximateorganizationsandsocialentrepreneurs:Organizationsontheground,incommunities,thatunderstandand incorporatethelivedexperienceofthosetheyserveintotheirprogrammingareuniquelypositionedtomakeanimpactonyouth mentalhealth.Thisrequireslong-term,sustainedinvestmentandcapacitybuilding.
● Leveragephilanthropy’sconveningpower:Bringfolkstogethertocoordinatestakeholdersacrosstheecosystem,share innovativeideas,investinsystemsbuilding,andshinealightonthegoodworkbeingdoneincommunitiesacrosstheU.S.
● Supporteffectivepolicydevelopment:Local,state,andfederalpoliciescanpromoteorinhibitgrowthinthementalhealthsector, andtherearepeopleworkingatalllevelsofthesystemtohaveanimpact.Statesarefindinginnovativewaystoestablish sustainablefinancingformentalhealth,includingcoverageformobilecrisisservices.
● Fillgaps:Whilegovernmentfundingisessentialandhastraditionallymadeupthemajorityoffundingformentalhealthservices, giventhecurrentpolicylandscapeintheUS,philanthropywillbeincreasinglycriticaltoensurecareisavailabletoall,particularly sub-groupslosingaccesstospecializedcare,suchasLGBTQ+youth.Intervieweesalsosharedthechallengeofleveragingpublic dollarstosupportnew,innovativeprogramswiththepotentialforhighimpact,whichisakeyplacewherephilanthropycanstepin.
● Catalyzenewknowledge:Investinbuildingtheevidencebasebyfundingnewresearchandinnovationinthefield, withaparticularfocusonthetranslationofresearchtopracticeandraisinguplocalfundsofknowledge.
● Engageinsystem-buildingacrossalloftheabove!


WeextendoursinceregratitudetotheCarnegieCorporationofNewYorkforfundingthiswork.
Aspecialthankstothe20+intervieweeswhogenerouslysharedtheirtimeandperspectives,helpingshapethisanalysis.Weare alsodeeplyappreciativeofthePeopleRocketandNewProfitteamsfortheirdedication,collaboration,andcommitmentto refiningandstrengtheningthisworkateverystage.
AndaheartfeltthankyoutothePeopleRocketteam—JakeHale,EmilyMeland,andTessaForshaw—aswellasthecoreteam fromNewProfit—TezetaTamrat,ShrutiSehra,andJulieAsher—whoseleadershipandcontributionswereinstrumentalin bringingthislandscapeanalysistolife.

Twoseparateapproachesweredevelopedtoidentifynonprofitorganizationsworkingintheyouthmentalhealthfieldusinga combinationofpre-existingclassificationschemesandtext-basedanalysis.Thefirstmethod(Approach1)usedtheNational TaxonomyofExemptEntities(NTEE)codes.Specifically,organizationscategorizedunderNTEEcodegroup“F”,meaning MentalHealthandCrisisInterventionorganizations.Anextrafilterwasthenappliedtodescriptionsoftheseorganizationsto checkwhethertheyusedyouth-specificterms.Thisapproachisconsistentwithtraditionalanalysesofthesystemandis improvedbyaddingtheyouth-specifictermstothetextanalysis.However,thisapproachisconstrainedbythelimitationsofthe NTEEclassificationsystem.
AllnonprofitorganizationshaveasingleNTEEcode.Whilethesecodesaredescriptive,theyfailtofullyaccountforthescopeof servicesanorganizationprovides.Thismeansthatthesystemisincapableofcapturingthefullbreadthoforganizationsworking inasector.Analternativeapproach(Approach2)wasdevelopedtoaddressthisconstraint.First,Form990filingswereanalyzed forage-appropriatekeywordsinthesamewayasApproach1,andthencross-checkedagainstasetoftermsalignedwithour definitionofyouthmentalhealthandbasedondocumentreviewsandconversationswithsystemstakeholders.Formore informationonthishuman-centeredmethodology,pleaseseeourotherreport:UnlockingtheBlackBox.Thisapproachenabled theidentificationoforganizationswhichmaynothavebeencapturedinthefirstmethod;thesemaybeorganizationsthatare operatinginrelatedorsimilarfields,butarestillmakingacontributiontoyouthmentalhealth.
Aftertheyouthmentalhealthorganizationswereidentified,additionalstepsweretakentomaptheirfundingflows.Inorderto achievethis,organizationswerecross-referencedwithprivatefoundationForm990filingsinordertodeterminetheamount andsourceoffinancialsupporttheyreceived.Throughtheassociationofthe identifiedorganizationswiththefundingflowinformation,thisprocessofferedabetterunderstandingofhow privatefoundationssupportyouthmentalhealthprojectsandrevealedfundingopportunitieswithinthesector.

Modelformulationandkeytermscanbeviewedbyvisitingtheview-onlyspreadsheet.
SheetNames:
● AgeTerms
● TopicTerms

Themethodsusedinthisreporthaveafewlimitationsthatconstitutefutureareasofresearch.Thefirstlimitationisthe availabilityofForm990filingdata.Someestimatesreportaprocessingdelayofmorethanthreeyears.Therefore,somefilings werenotavailableforthisanalysis.Althoughthedatasetusedforthisresearchiscomprehensive,itisnotexhaustive.Future analysesusingnewlyreleasedfilingsmayresultindifferentfindings.
Thesecondlimitationisthescopeoforganizationsincluded.Thisanalysisislimitedtononprofitorganizationsandtheirprivate foundationfunders.TheseareorganizationsthatprioritizeyouthmentalhealthbasedontheirForm990programmatic descriptions.Theremaybeotherorganizationsthataddressyouthmentalhealthaspartoftheirlargermission,butthose wouldn’tbecapturedunlesstheyexplicitlymentionitintheirForm990.Therefore,someimportantactorsinthementalhealth ecosystemarenotaccountedforsuchasfiscallysponsoredorganizations,for-profitorganizations,andgovernmentagencies.In addition,thefundinglandscapeexploredinthisstudyislimitedtoprivatefoundations,thus,organizationsthatprovidefunding throughdonoradvisedfunds(DAFs)werenotcaptured.Includingotherorganizationtypesandfundingsourcesintheanalysis wouldimprovetheutilityofthefindingspresented.
Therearealsolimitationsassociatedwithtext-basedanalysis.Thetextanalysiscomponentwasdevelopedtoidentify additionalorganizationsthatgetoverlookedintraditionalanalysesthatrelyonNTEEcodesalone.Whileadditional organizationswereidentified,thisapproachisunabletoclassifywithperfectaccuracydespiteeffortstoimproveandvalidate themethod.Furthermore,thegeographicanalysisinthisreportisbasedontheaddressreportedbyorganizationsintheir filings.However,manynonprofitorganizationsprovideservicesbeyondcountyandstateboundaries.Identifyinganalternative waytocapturethefullextentofanorganization’sservicecatchmentwouldrevealadditionalinsightsforthefield.
Lastly,thefindingspresentedinthisreportarebasedonresearchthatconcludedinlate2024.Changesinthelandscape thathaveoccurredafterthistimeareoutofthescopeofthisanalysisandthusrequirefurtherinvestigation.

PrimaryCareProfessionalShortageAreasarelesswidespreadthanMentalHealth,butstillaccountformostofthe UnitedStates.

Achterberg,M.,Becht,A.,vanderCruijsen,R.,vandeGroep,I.H.,Spaans,J.P.,Klapwijk,E.,&Crone,E.A.(2022).Longitudinalassociations betweensocialmediause,mentalwell-beingandstructuralbraindevelopmentacrossadolescence.DevelopmentalCognitiveNeuroscience, 54,101088.https://doi.org/10.1016/j.dcn.2022.101088
Alvarez-Jimenez,M.,Koval,P.,Schmaal,L.,Bendall,S.,O’Sullivan,S.,Cagliarini,D.,D’Alfonso,S.,Rice,S.,Valentine,L.,Penn,D.L.,Miles,C.,Russon, P.,Phillips,J.,McEnery,C.,Lederman,R.,Killackey,E.,Mihalopoulos,C.,Gonzalez-Blanch,C.,Gilbertson,T.,…Gleeson,J.F.M.(2021).The Horyzonsproject:Arandomizedcontrolledtrialofanovelonlinesocialtherapytomaintaintreatmenteffectsfromspecialistfirst-episode psychosisservices.WorldPsychiatry,20(2),233–243.https://doi.org/10.1002/wps.20858
AmericanPsychologicalAssociation(APA).(2021).DataTool:DemographicsoftheU.S. PsychologyWorkforce. https://www.apa.org/workforce/data-tools/demographics
Andersson,G.,Titov,N.,Dear,B.F.,Rozental,A.,&Carlbring,P.(2019).Internet-deliveredpsychologicaltreatments:Frominnovationto implementation.WorldPsychiatry,18(1),20–28.https://doi.org/10.1002/wps.20610
Asarnow,J.R.,Jaycox,L.H.,Duan,N.,LaBorde,A.P.,Rea,M.M.,Murray,P.,Anderson,M.,Landon,C.,Tang,L.,&Wells,K.B.(2005).Effectiveness ofaQualityImprovementInterventionforAdolescentDepressioninPrimaryCareClinics:ARandomizedControlledTrial.JAMA,293(3), 311–319.https://doi.org/10.1001/jama.293.3.311
Bell,I.H.,Thompson,A.,Valentine,L.,Adams,S.,Alvarez-Jimenez,M.,&Nicholas,J.(2022).Ownership,Useof,andInterestinDigitalMental HealthTechnologiesAmongCliniciansandYoungPeopleAcrossaSpectrumofClinicalCareNeeds:Cross-sectionalSurvey.JMIRMental Health,9(5),e30716.https://doi.org/10.2196/30716
Boers,E.,Afzali,M.H.,Newton,N.,&Conrod,P.(2019).AssociationofScreenTimeandDepressioninAdolescence.JAMAPediatrics,173(9), 853–859.https://doi.org/10.1001/jamapediatrics.2019.1759
Bridge,J.A.,Ruch,D.A.,Sheftall,A.H.,Hahm,H.C.,O’Keefe,V.M.,Fontanella,C.A.,Brock,G.,Campo,J.V.,&Horowitz,L.M.(2023).Youth SuicideDuringtheFirstYearoftheCOVID-19Pandemic.Pediatrics,151(3),e2022058375.https://doi.org/10.1542/peds.2022-058375
Bronfenbrenner,U.&Morris,P.A.(2006).Thebioecologicalmodelofhumandevelopment.InR.M.Lerner&W.Damon(Eds.),Handbookofchild psychology:Theoreticalmodelsofhumandevelopment(pp.793-828).Hoboken,NJ:JohnWiley&SonsInc.

Brunette,M.F.,Erlich,M.D.,Edwards,M.L.,Adler,D.A.,Berlant,J.,Dixon,L.,First,M.B.,Oslin,D.W.,Siris,S.G.,&Talley,R.M.(2023).Addressing theIncreasingMentalHealthDistressandMentalIllnessAmongYoungAdultsintheUnitedStates.TheJournalofNervousandMental Disease,211(12),961.https://doi.org/10.1097/NMD.0000000000001734
CenterforBehavioralHealthStatisticsandQuality.(2021).Behavioralhealthequityreport2021:Substanceuseandmentalhealthindicators measuredfromtheNationalSurveyonDrugUseandHealth(NSDUH), 2015–2019(PublicationNo.PEP21-07-01-004).Rockville,MD: SubstanceAbuseandMentalHealthServicesAdministration. https://www.samhsa.gov/data/sites/default/files/reports/rpt35328/2021NSDUHBHEReport.pdf
CentersforDiseaseControlandPrevention(CDC).(n.d.).AboutBehavioralHealth. https://www.cdc.gov/mental-health/about/about-behavioral-health.html
CentersforDiseaseControlandPrevention.(2024).YouthRiskBehaviorSurveyDataSummary&TrendsReport:2013–2023.U.S.Department ofHealthandHumanServices.https://www.cdc.gov/yrbs/dstr/index.html
CentersforDiseaseControlandPrevention.(2022).YouthRiskBehaviorSurveyDataSummary&TrendsReport:2011–2021.U.S.Departmentof HealthandHumanServices.https://www.cdc.gov/yrbs/dstr/pdf/YRBS_Data-Summary-Trends_Report2023_508.pdf
Chu,W.,Chorpita,B.F.,&Becker,K.D.(2022).Race,racialmatching,andculturalunderstandingaspredictorsoftreatmentengagementinyouth mentalhealthservices.PsychotherapyResearch,33(5),669–682.https://doi.org/10.1080/10503307.2022.2150582
Clarke,A.M.,Kuosmanen,T.,&Barry,M.M.(2015).ASystematicReviewofOnlineYouthMentalHealthPromotionandPreventionInterventions. JournalofYouthandAdolescence,44(1),90–113.https://doi.org/10.1007/s10964-014-0165-0
D’Alfonso,S.,Santesteban-Echarri,O.,Rice,S.,Wadley,G.,Lederman,R.,Miles,C.,Gleeson,J.,&Alvarez-Jimenez,M.(2017).Artificial Intelligence-AssistedOnlineSocialTherapyforYouthMentalHealth.FrontiersinPsychology,8.https://doi.org/10.3389/fpsyg.2017.00796
Eisenberg,D.,Downs,M.F.,Golberstein,E.,&Zivin,K.(2009).StigmaandHelpSeekingforMentalHealthAmongCollegeStudents.Medical CareResearchandReview,66(5),522–541.https://doi.org/10.1177/1077558709335173
Hall,J.,Jordan,S.,vanOmmeren,M.,Au,T.,Sway,R.A.,Crawford,J.,Ghalayani,H.,Hamdani,S.U.,Luitel,N.P.,Malik,A.,Servili,C.,Sorsdahl,K., Watts,S.,&Carswell,K.(2022).SustainableTechnologyforAdolescentsandyouthtoReduceStress(STARS):AWHOtransdiagnostic chatbotfordistressedyouth.WorldPsychiatry,21(1),156–157.https://doi.org/10.1002/wps.20947

Hopkins,L.,Lee,S.,McGrane,T.,&Barbara-May,R.(2017).Singlesessionfamilytherapyinyouthmentalhealth:Canithelp?Australasian Psychiatry,25(2),108–111.https://doi.org/10.1177/1039856216658807
Jiménez,L.,Hidalgo,V.,Baena,S.,León,A.,&Lorence,B.(2019).EffectivenessofStructural–StrategicFamilyTherapyintheTreatmentof AdolescentswithMentalHealthProblemsandTheirFamilies.InternationalJournalofEnvironmentalResearchandPublicHealth,16(7), Article7.https://doi.org/10.3390/ijerph16071255
Jones,S.E.(2022).MentalHealth,Suicidality,andConnectednessAmongHighSchoolStudentsDuringtheCOVID-19Pandemic—Adolescent BehaviorsandExperiencesSurvey,UnitedStates,January–June2021.MMWRSupplements,71.https://doi.org/10.15585/mmwr.su7103a3
MakingCaringCommon.(2021).LonelinessinAmerica:HowthePandemicHasDeepenedanEpidemicofLonelinessandWhatWeCanDo AboutIt.https://mcc.gse.harvard.edu/reports/loneliness-in-america
MakingCaringCommon.(2023).CaringfortheCaregivers:TheCriticalLinkBetweenParentandTeenMentalHealth. https://mcc.gse.harvard.edu/reports/caring-for-the-caregivers
MakingCaringCommon.(2023).OnEdge:UnderstandingandPreventingYoungAdults’MentalHealthChallenges. https://mcc.gse.harvard.edu/reports/on-edg
MakingCaringCommon(2024).LonelinessinAmerica:JusttheTipoftheIceberg? https://mcc.gse.harvard.edu/reports/loneliness-in-america-2024
McGorry,P.D.,Mei,C.,Dalal,N.,Alvarez-Jimenez,M.,Blakemore,S.-J.,Browne,V.,Dooley,B.,Hickie,I.B.,Jones,P.B.,McDaid,D.,Mihalopoulos,C., Wood,S.J.,Azzouzi,F.A.E.,Fazio,J.,Gow,E.,Hanjabam,S.,Hayes,A.,Morris,A.,Pang,E.,…Killackey,E.(2024).TheLancetPsychiatry Commissiononyouthmentalhealth.TheLancetPsychiatry,11(9),731–774.https://doi.org/10.1016/S2215-0366(24)00163-9
Misra,S.,Jackson,V.W.,Chong,J.,Choe,K.,Tay,C.,Wong,J.,&Yang,L.H.(2021).SystematicReviewofCulturalAspectsofStigmaandMental IllnessamongRacialandEthnicMinorityGroupsintheUnitedStates:ImplicationsforInterventions.AmericanJournalofCommunity Psychology,68(3–4),486–512.https://doi.org/10.1002/ajcp.12516
NationalCenterforHealthWorkforceAnalysis.(2023,December).BehavioralHealthWorkforce,2023. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/Behavioral-Health-Workforce-Brief-2023.pdf

Odgers,C.L.,&Jensen,M.R.(2020).AnnualResearchReview:Adolescentmentalhealthinthedigitalage:facts,fears,andfuturedirections. JournalofChildPsychologyandPsychiatry,61(3),336–348.https://doi.org/10.1111/jcpp.13190
OfficeoftheSurgeonGeneral(OSG).(2021).ProtectingYouthMentalHealth:TheU.S.SurgeonGeneral’sAdvisory.USDepartmentofHealth andHumanServices.http://www.ncbi.nlm.nih.gov/books/NBK575984/
OfficeoftheSurgeonGeneral(OSG).(2023).OurEpidemicofLonelinessandIsolation:TheU.S.SurgeonGeneral’sAdvisoryontheHealing EffectsofSocialConnectionandCommunity.USDepartmentofHealthandHumanServices. https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf
OfficeoftheSurgeonGeneral(OSG).(2024).ParentsUnderPressure:TheU.S.SurgeonGeneral'sAdvisoryontheMentalHealth&Well-Beingof Parents.USDepartmentofHealthandHumanServices.https://www.hhs.gov/sites/default/files/parents-under-pressure.pdf
Orben,A.,&Blakemore,S.-J.(2023).Howsocialmediaaffectsteenmentalhealth:Amissinglink.Nature,614(7948),410–412. https://doi.org/10.1038/d41586-023-00402-9
Penner,F.,HernandezOrtiz,J.,&Sharp,C.(2021).ChangeinYouthMentalHealthDuringtheCOVID-19PandemicinaMajorityHispanic/Latinx USSample.JournaloftheAmericanAcademyofChild&AdolescentPsychiatry,60(4),513–523.https://doi.org/10.1016/j.jaac.2020.12.027
Prichett,L.M.,Yolken,R.H.,Severance,E.G.,Carmichael,D.,Zeng,Y.,Lu,Y.,Young,A.S.,&Kumra,T.(2024).COVID-19andYouthMentalHealth Disparities:IntersectionalTrendsinDepression,AnxietyandSuicideRisk-relatedDiagnoses.AcademicPediatrics,24(5),837. https://doi.org/10.1016/j.acap.2024.01.021
Reinert,M,Fritze,D&Nguyen,T(July2024).TheStateofMentalHealthinAmerica2024.MentalHealthAmerica,AlexandriaVA. https://mhanational.org/wp-content/uploads/2024/12/2024-State-of-Mental-Health-in-America-Report.pdf
Richardson,L.P.,Ludman,E.,McCauley,E.,Lindenbaum,J.,Larison,C.,Zhou,C.,Clarke,G.,Brent,D.,&Katon,W.(2014).CollaborativeCarefor AdolescentsWithDepressioninPrimaryCare:ARandomizedClinicalTrial.JAMA,312(8),809–816.https://doi.org/10.1001/jama.2014.9259 SearchInstitute.(2025).DevelopmentalRelationships.https://searchinstitute.org/developmental-relationships
Thomeer,M.B.,Moody,M.D.,&Yahirun,J.(2023).RacialandEthnicDisparitiesinMentalHealthandMentalHealthCareDuringTheCOVID-19 Pandemic.JournalofRacialandEthnicHealthDisparities,10(2),961–976.https://doi.org/10.1007/s40615-022-01284-9

Thornicroft,G.,Sunkel,C.,AlikhonAliev,A.,Baker,S.,Brohan,E.,ElChammay,R.,Davies,K.,Demissie,M.,Duncan,J.,Fekadu,W.,Gronholm,P.C., Guerrero,Z.,Gurung,D.,Habtamu,K.,Hanlon,C.,Heim,E.,Henderson,C.,Hijazi,Z.,Hoffman,C.,…Winkler,P.(2022).TheLancetCommission onendingstigmaanddiscriminationinmentalhealth.TheLancet,400(10361),1438–1480.https://doi.org/10.1016/S0140-6736(22)01470-2
Twenge,J.M.,&Farley,E.(2021).Notallscreentimeiscreatedequal:Associationswithmentalhealthvarybyactivityandgender.Social PsychiatryandPsychiatricEpidemiology,56(2),207–217.https://doi.org/10.1007/s00127-020-01906-9
Twenge,J.M.,Haidt,J.,Lozano,J.,&Cummins,K.M.(2022).Specificationcurveanalysisshowsthatsocialmediauseislinkedtopoormental health,especiallyamonggirls.ActaPsychologica,224,103512.https://doi.org/10.1016/j.actpsy.2022.103512
Usborne,E.,&Taylor,D.M.(2010).TheRoleofCulturalIdentityClarityforSelf-ConceptClarity,Self-Esteem,andSubjectiveWell-Being. PersonalityandSocialPsychologyBulletin,36(7),883–897.https://doi.org/10.1177/0146167210372215
vanDoorn,M.,Monsanto,A.,Boeschoten,C.M.,vanAmelsvoort,T.,Popma,A.,Öry,F.G.,Alvarez-Jimenez,M.,Gleeson,J.,Jaspers,M.W.M.,& Nieman,D.H.(2023).Moderateddigitalsocialtherapyforyoungpeoplewithemergingmentalhealthproblems:Auser-centered mixed-methoddesignandusabilitystudy.FrontiersinDigitalHealth,4,1020753.https://doi.org/10.3389/fdgth.2022.1020753
Weinstein,E.,&James,C.(2022).BehindTheirScreens:WhatTeensAreFacing(andAdultsAreMissing).TheMITPress. https://doi.org/10.7551/mitpress/14088.001.0001
Worsley,J.D.,Pennington,A.,&Corcoran,R.(2022).Supportingmentalhealthandwellbeingofuniversityandcollegestudents:Asystematic reviewofreview-levelevidenceofinterventions.PLOSONE,17(7),e0266725.https://doi.org/10.1371/journal.pone.0266725
Yard,E.,Radhakrishnan,L.,Ballesteros,M.F.,Sheppard,M.,Gates,A.,Stein,Z.,Hartnett,K.,Kite-Powell,A.,Rodgers,L.,Adjemian,J.,Ehlman,D. C.,Holland,K.,Idaikkadar,N.,Ivey-Stephenson,A.,Martinez,P.,Law,R.,&Stone,D.M.(2021).EmergencyDepartmentVisitsforSuspected SuicideAttemptsAmongPersonsAged12-25YearsBeforeandDuringtheCOVID-19Pandemic—UnitedStates,January2019-May2021. MMWR.MorbidityandMortalityWeeklyReport,70(24),888–894.https://doi.org/10.15585/mmwr.mm7024e1
