A CRISIS
Howard Jones’ situation was dire and complicated, but he had a phenomenal team at Boone Health by his side.




MANAGING
Erin Wegner
COPY
Jessica Park
CONTRIBUTING
Madison Loethen
ADDITIONAL
Michelle Terhune; Hannah Williams; Jenny L. Workman
CONTRIBUTING
Lana Eklund





Please submit comments or feedback to erin.wegner@boone.health or call 573.815.3217
1600 East Broadway Columbia, MO 65201 573.815.8000

For a FREE subscription, scan the QR code, visit boone.pub/subscribe, or call 573.815.3392.



Board of Directors

Jerry Kennett, MD

Randy Morrow

Mary Beck, DNP, RN, FAONL

Judy Starr

Stacye Smith

Charles P. Bondurant, MD, FABNS, FACS

Jeffery Lashley, Ph.D.

Boone Health Neurosurgery and Spine Center offer advanced neurological procedures in a comfortable, small clinic setting, backed by the safety and technology of Boone Hospital Center.
Services include:
• Aneurysm
• Brain tumor
• Cervical, thoracic, and lumbar spine
• Hydrocephalus
• Minimally-invasive spine
• Peripheral nerve
• Surgical treatment of movement disorders
• Vascular malformation of the brain
A physician referral is required. For more information, contact us at 573.815.8242.
Preventive Care is Brain Care
This issue of My Boone Health focuses on the most complex organ in the human body. Fortunately, caring for our brains isn’t nearly as complicated — what’s good for your heart is also good for your brain.
According to the American Stoke Association, the biggest risk factors for stroke include high cholesterol, high blood pressure, diabetes, heart disease, smoking, and obesity. Seeing your primary care provider for annual check-ups, screenings, and health concerns can help prevent or identify issues early. Your provider can help you improve or maintain a healthy weight, and optimal cholesterol levels, blood pressure, and blood sugar. A healthy lifestyle that includes regular exercise, a balanced diet, stress management, and adequate sleep, benefits both your brain and your body, including our moods and cognitive functioning.
Sleep is often an overlooked contributor to our health and well-being, but it’s as necessary as food or water. According to the National Institute of Neurological Disorders and Stroke, “Sleep is important to a number of brain functions, including how nerve cells (neurons) communicate with each other. Without sleep, you can’t form or maintain the pathways in your brain that let you learn and create new memories. Lack of sleep makes it harder to concentrate and respond quickly.”
It is especially important that we get non-REM deep sleep to feel refreshed, but many of us find it difficult to get the amount and quality of sleep we need. If avoiding caffeine and alcohol late in the day, turning off your phone or tablet an hour before bed, and relaxing routines
aren’t helping, talk to your primary care provider. Sleep disruption is a common symptom of many chronic health conditions, including sleep apnea. If needed, your primary care provider can refer you for a sleep study.
Boone Health’s Sleep Center is a specialized service that diagnoses and treats sleep disorders. We offer inpatient monitoring in our sleep lab along with outpatient sleep monitoring you can do at home. Our sleep lab professionals will show you how to wear and use the monitor. A boardcertified Sleep Medicine physician will interpret the information from your study and share your results and treatment recommendations with your primary care provider who referred you and, if needed, other specialists. More information can be found at boone.health/services/ neurology-neurosurgery/ sleep-medicine.
In addition to offering excellent preventive and diagnostic care, Boone Health is proud to serve mid-Missouri as a Level I Stroke Center. Our interventional radiology team includes radiologists who specialize in neurology and can act quickly to stop a stroke before it causes further damage. Our Inpatient Rehab unit and Boone Therapy professionals help people regain function and restore their quality of life.
Remember, time is brain, so BE FAST If you or someone else has any of the following symptoms, don’t take chances, call 911. Our Emergency Medical Services team can begin treatment before you get to the hospital.

Balance: Sudden loss of balance or coordination
Eyes: Blurred, double, or lost vision
Face: Drooping on one side of the face
Arms: Weakness in the arms or legs
Speech: Slurred speech or difficulty speaking
Time: Don’t delay, call 911!
Boone Health is committed to helping you achieve your healthiest self. Brain health is vital, and we are here to assist you and your family. I strongly encourage you to maintain regular checkups and work with your healthcare team to get your vital signs and lab values within normal ranges, and to do it sooner rather than later. Be well!

Brady Dubois CEO, Boone Health
Healthgrades Recognized Boone Health With Its 2025 Outstanding Patient Experience Award
Over the past 12 months, Boone Health has been recognized with multiple national awards, solidifying its place as one of the best hospitals in the country for health care quality, patient care and employee satisfaction. Boone Health was recently awarded this new designation of Outstanding Patient Experience.
This latest recognition comes on top of Healthgrades naming Boone Health as a Top 100 Hospital in the nation, the Centers for Medicare and Medicaid Services ranking Boone Hospital as the only 5-star hospital in mid-Missouri, the American Nurses Credentialing Center giving Boone Health its fifth consecutive Magnet designation for nursing excellence, and Forbes naming Boone Health as a Top 100 place to work in the nation for mid-size employers and No. 6 in the state of Missouri. Healthgrades evaluated more than 3,000 hospitals for Outstanding Patient Experience using patient survey data from the Hospital Consumer Assessment of Healthcare Providers & Systems over a calendar year. Boone Health’s recognition puts it in the top 15% of those hospitals nationwide in patient experience.
Since September 2024, Boone Health has been awarded and/or recognized with the following:
5-Star Rating – Centers for Medicare and Medicaid Services
Forbes
• No. 1 place to work in mid-Missouri for mid-sized employers
• No. 6 place to work in Missouri for mid-sized employers
• No. 67 place to work in the nation for mid-sized employers.
American Nurses Credentialing Center
• Magnet designation five consecutive times (2024, 2019, 2014, 2009, 2005)
Magnet designation is provided to organizations that meet rigorous standards for nursing excellence; it is the highest honor for professional nursing. Only 70 hospitals in the world have received Magnet designation five times.
Healthgrades
• America’s 100 Best Hospitals three years in a row (2023-25)
• Top 15% nationally for Outstanding Patient Experience
• America’s 100 Best Hospitals for Spine Surgery (in the top 5%)
• America’s 50 Best Hospitals for both Outpatient Orthopedic Surgery and Joint Replacement (top 10%)
• Five-Star recipient for treatment of Heart Attack, Heart Failure, Knee Replacement, Hip Replacement, Spinal Fusion Surgery, Pneumonia Treatment, Abdominal Aorta Repair, Sepsis Treatment, and Respiratory Failure Treatment.
Boone Health Breast Care and Lab Services New Location
In April 2025, Boone Health Breast Care opened the door to their permanent location in Broadway Medical Plaza 2, Suite 200. This office provides comprehensive breast cancer screening, genetic risk evaluation and counseling for patients who are at an increased risk of breast cancer. To learn more or to make an appointment, visit boone.health/breast-care.
The lab in Plaza 2 has a new office. Still located on the second floor, the new office is located right across the hall from its previous location. The lab can now be found in Suite 250. To find lab locations and hours, visit boone.health/lab-services.


Boone Health EMS Team Receives
Generous Donation

For Emergency Medical Services Week in May, a new medical transport vehicle and trailer was generously donated by Drs. Roberta and Gary Minish. The vehicle was officially put into service and will play a vital role in supporting our EMS teams.


Anthem Blue Cross and Blue Shield and Boone Health Announce New Four-Year Contract Agreement
A new four-year agreement between Anthem Blue Cross and Blue Shield and Boone Health was announced. This ensures continued in-network access to Boone Health’s hospitals, clinics and providers for all Anthem members, including those enrolled in employer-sponsored and Medicare Advantage health plans. If you’re looking for a Boone Health provider that can meet your needs, call 573.815.3000.
Boone Health OB/GYN Elizabeth Wilson, MD Works to Empower Women Through Hormone Replacement Therapy
Dr. Wilson, of Women’s Health Associates and Boone Health is a leading expert in the Hormone Replacement Therapy (HRT) field. She is spearheading the expansion of Boone Health Partner, Women’s Health Associate’s HRT program. Dr. Wilson is an excellent resource for media outlets covering hormone health, aging and women’s wellness. She has a dual focus on education and evidence-based care.
“Hormonal imbalances can impact everything from energy and mood to sleep, metabolism, and mental clarity,” says Dr. Wilson. “With our Hormone Replacement Therapy program, we’re empowering women to take back control of their health with solutions that are customized, safe, and supported by the latest science.”
HRT is a medically supervised treatment used to address symptoms related to menopause, perimenopause, and other hormone-related conditions. It offers a variety of delivery methods tailored to each patient’s lifestyle and preferences. Options include bioidentical hormone creams, patches, oral medications, pellet therapy, and peptide therapy to provide steady, long-lasting hormone levels. Dr. Wilson works closely with each patient to determine the safest and most effective option based on individual symptoms, goals and overall health. With a career rooted in caring for women through all stages of life, Dr. Wilson brings both clinical experience and advanced training to HRT. She has continually expanded her knowledge through prestigious organizations such as The Institute of Functional Medicine and the American Association of Anti-Aging Medicine, keeping her at the forefront of hormone science and integrative health.
Dr. Wilson and Women’s Health Associates welcome patients seeking personalized hormone care. Appointments can be scheduled through wha-inc.com/ or by calling 573.443.8796.

Boone Raises the Flag for Organ & Tissue Donation

On April 15, 2025, Boone Health raised awareness for National Donate Life Month by signing and raising a Donate Life flag outside the main hospital entrance. The flag featuring handwritten messages of comfort and hope honors organ, eye and tissue donors, their families, and recipients.
Chief Nursing Executive Shannon Kuczynski addressed gathered employees and representatives from Midwest Transplant Network, our partner in organ, eye, and tissue donation.
Since its inception in 2003, the U.S. has celebrated National Donate Life Month each April to raise awareness about what donation truly means. Together, we can encourage the community to join the organ, eye and tissue donor registry. Together, we can honor those who have given the gift of life through donation. Together, we can celebrate the lives of those who have received the gift because of someone’s generosity.
There are approximately 103,000 Americans currently waiting for a life-saving organ transplant. Regardless of age and medical history, everyone 18 years old and older can join the organ, eye, and tissue donor registry. I encourage you to join the donor registry, if you have not already done so, by signing up at ShareLifeMidwest.com. Then, please tell your loved ones about your decision.

I am proud of the work all of us at Boone Health do to care for our donors and recognize the ripple effect that each donor has on their recipient’s family members, friends, community and beyond.
TAMMY GRIMES’ STROKE JOURNEY
From Crisis to Recovery

How rapid medical care and therapy helped her regain independence.
Tammy Grimes opened her eyes and found herself in a hospital bed. Her husband, Marshall, sat beside her, and she struggled to remember what had happened. Slowly, fragmented memories began to return. The night before, she had gone to bed at her usual time of 9 p.m. Around 3 a.m., she woke up with pain in her left leg. Attempting to walk it off, she found she couldn’t move properly. Though she thought it was odd, she managed to fall back asleep.
That morning at 5 a.m., she hobbled to the kitchen for her coffee, and then she realized she couldn’t drink it—her lips wouldn’t move properly. Alarmed, she called for her husband, who immediately rushed her to Boone Hospital Center’s Emergency Department. As they entered, he spotted a sign listing the warning signs of a stroke. Recognizing Tammy’s symptoms, he pointed to the sign and told the front desk attendant, “She has all of these.”
Tammy was rushed into a treatment room, where doctors quickly confirmed she was experiencing a right pontine ischemic stroke. A right pontine ischemic stroke occurs when blood flow to the right side of

Tammy Grimes and her granddaughter, Piper.
the pons, a crucial part of the brainstem, is blocked due to a clot or narrowing of the blood vessels. Tammy was stabilized and then taken to a recovery room to receive supportive care and rehabilitation.
“I stayed in the hospital for a week, but it didn’t feel like that. Everything was such a blur. My whole left side didn’t work well. I couldn’t walk or take care of myself—it was overwhelming,” Tammy recalls.
Following her discharge, Tammy was prescribed outpatient Occupational Therapy (OT) and Physical Therapy (PT) at Boone Therapy—something she describes as a blessing.
OT and PT played a crucial role in helping Tammy regain her independence. PT focused on physical movement, helping her rebuild strength, balance, and coordination so she could walk and perform daily tasks safely. OT addressed fine motor skills and cognitive recovery, teaching her how to dress, eat, and even type again—an essential skill for her job as a paralegal. Both therapies used repetitive exercises and adaptive techniques to promote neuroplasticity, allowing her brain to rewire itself and regain lost function.
“I was devastated by how little I could take care of myself,” Tammy shares. “I have a daughter and a 4-year-old granddaughter that we are very involved with. I knew I could hardly take care of myself, much less care for my granddaughter.”

Tammy’s PT Wes Glenn says many patients can be overwhelmed by the recovery before them after a stoke. The Boone Therapy team works with patients to develop individualized plans to meet their goals.
“There are so many questions that most people have in this situation: When will I get better? What is the timeline of recovery? When can I drive again? What should I do to be safe? Is there any special equipment I need? What questions SHOULD I be asking? A physical therapist may not know everything, but they are a great resource for organizing information, reducing stress, and providing direction for patients,” Wes said.
In OT, she worked tirelessly to regain her independence. Over the course of six weeks, she progressed from struggling with basic self-care to dressing herself and even typing on a keyboard again.
“OT taught me everything I needed to get my life back,” she says.
In PT, Tammy focused on rebuilding her strength and mobility. “When I started, I was in a wheelchair. Then I moved to a walker, then a cane, and now, I can walk on my own.”
Tammy’s biggest motivation in therapy was regaining the ability to care for and play with her granddaughter. She and Wes worked hard to make that happen.
“Wes was a great motivator, listener, and really cared about me. Without his help, I do not know what I would have been able to accomplish. He is the BEST in my eyes, and I am very grateful to him,” Tammy said.
Now, after eight months of PT, Tammy has regained almost all of her abilities.
“I do my exercises at home, and I can now do almost everything I could before my stroke,” she says proudly.
Her favorite milestone? Being able to play with her granddaughter.
“We go to the park, and I can climb on the jungle gym with her. We even play horsey on the floor again!” she says with a smile.
Tammy’s journey is a testament to the power of early medical intervention, determination, and therapy in stroke recovery.
Her story serves as a reminder that, with the right support and perseverance, it is possible to regain independence and return to the activities that bring joy and purpose to life. By Madison Loethen

Parkinson’s Patients Think BIG
Parkinson’s Disease is a neurogenerative disorder that a ects movement. It’s progressive, getting worse over time, and there is no cure. Common symptoms include tremor, rigid muscles, speech and handwriting changes, poor posture, and loss of balance. e movements of those with Parkinson’s may become slow and they may lose automatic movements, such as blinking or swinging their arms as they walk.
In other words, Parkinson’s makes normal movements small, which is why Boone erapy provides ways to make them big again.
Occupational erapist Leah Botkin proposed the implementation of the the Lee Silverman Voice Treatment (LSVT) BIG® in 2021. e global program requires certi cation to use its protocol. It uses occupational therapy and physical therapy to improve and maintain movement and decrease rigidity. ere’s also a speech component, LSVT LOUD®, to assist patients with those speech and swallowing issues as well.
“ e only thing that we know that helps with symptoms and helps keep symptoms at bay and maintain function over time is exercise – high amplitude, high repetition, intense exercise, which is what the LSVT BIG® intervention is,” Leah says.
High amplitude is a big part of the BIG protocol. is type of exercise involves making large, exaggerated movements.
ose help patients concentrate on overcoming small movements as the disease progresses. For example, patients may perform a series of long steps to help keep them from shu ing.
“ e program really focuses on the small movements that Parkinson’s encourages and making those bigger and more functional,” Leah says. “We’re taking small, shu ing movements and getting them to be large, functional movements.”
e LSVT exercises help with a patient’s speci c balance and rigidity problems and other functional tasks. But it’s not entirely a one-size- ts-all program.
“It’s a structured protocol that also has a lot of room for personalization,” Leah says. “ e idea is that they take that and continue doing it as a home exercise program.”



e program bene ts people across the Parkinson’s progression spectrum, although early intervention is ideal. ere are four LSVT protocols, including regular exercise, adaptive exercise, exercise done while seated, and exercise done while lying down. So, the type of exercise meets patients where they are on the spectrum of disease progression.
“Parkinson’s is a progressive disease, so the goal of the LSVT program is to take you where you are, raise that baseline up, and then ideally keep you at that new baseline,” Leah said.
Going BIG means undergoing therapy four times a week for four weeks for a total of 16 one-hour sessions. Half of the sessions are occupational therapy and the other half are physical therapy. If a patient requires intensive speech therapy, it will be scheduled either after those four weeks or prior to rather than combined. at separation helps keep therapy intensive.
e intensity of the program is what makes it e ective. But that isn’t all there is to it. Depending on the severity of symptoms, patients are encouraged to return to therapy for “tune-ups” to check on maintenance of the baseline and address any new issues as they arise. Patients may be in the tune-up phase for a period of three to 12 months.
Some patients experiencing symptoms begin the program even before a neurologist has diagnosed Parkinson’s.
“Navigating Parkinson’s can be really di cult,” Leah said. “Being able to meet with us and get our input and their questions answered before they ever meet with a neurologist often better helps them prepare for their neurology appointment.”
e outcomes for LSVT patients are solid. Improvements in functional balance and decreased fall risks are common. Gait and the ability to traverse stairs improve. Writing improves. A patient’s ability to change clothes and other activities of daily living improve.
“ e response to this program is overwhelmingly positive,” Leah said. “Everyone really enjoys it, and I honestly think a lot of them are far more con dent. Many people come in distraught after the diagnosis. But by the end of it, a lot of people feel more con dent about what they can do about it.”
“I think having a progressive disease can make you feel pretty out of control at times. Being able to have tools in your toolbox you can utilize to stay functional really helps a lot of people,” Leah said. “I think we see some really good outcomes from the program. Not just physical outcomes, but psychological and emotional outcomes as well.”
e LSVT BIG® program was designed for patients living with Parkinson’s. However, the protocols are also used for other neurological conditions, such as post-stroke, normal pressure hydrocephalus (a build up of cerebrospinal uid), and progressive supranuclear palsy (damage to nerve cells in areas of the brain.)
By Michelle Terhune
If you are interested in learning more about the LSVT BIG® Parkinson’s program at Boone Health, call 573-815-3868 or visit the website at boone.health/lsvt-big-for-parkinsons-disease
Forgetting Something?
If you or a loved one struggles with memory loss, here’s what you can do.
Whether you call it a “senior moment” or “mental-pause,” a memory lapse can be alarming. But how do you know if it’s just part of getting old or a cause for concern?
“Dementia is an umbrella term for loss of memory and other thinking abilities that is severe enough to interfere with daily life,” explained Teresa Brown, CDC, program manager with Alzheimer’s Association of Greater Missouri.
Dementia results from conditions that a ect the brain’s ability to communicate. In the brain, a network of nerve cells, or neurons, sends and receives messages to and from the body. Neurons use molecules called neurotransmitters to communicate with other neurons along neural pathways. Our memories are actually stored along these pathways. If part of a neural pathway is damaged, you might struggle to recall memories or form new ones.
Alzheimer’s disease, which is the most common form of dementia in the United States, occurs when a build up of protein deposits (amyloid plaques) and malformed proteins (tau tangles) causes neurons to stop working properly and breaks these pathways.
Other common forms of dementia include:
• Frontotemporal: Conditions that shrink frontal and temporal lobes
• Vascular: Damage after a stroke or multiple strokes
• Lewy Body: Protein deposits (Lewy bodies) on neurons
• Huntington’s: Mutation in the HTT gene causes progressive deterioration
Teresa notes other diseases can mimic dementia symptoms, including diabetes, thyroid issues, depression, vision problems, or hearing loss. If you’re concerned about your memory, talk to your primary care provider.

Normal Age-Related Forgetfulness
• You forget something that happened 20 years ago.
• You misplace your car keys, but find them by retracing your steps.
• You can’t recall a name or word in the moment but remember it later.
• You need a second to remember where you left off after an interruption.
• You enter a room of your house and briefly forget what you wanted there.
• You accidentally put 2024 when dating a check in 2025.
• You ask a family member to help you set up your new smart TV.
Possible Indicator of Dementia
• You forget something that happened 20 minutes ago.
• You frequently misplace items, sometimes in unusual places, and can’t retrace your steps.
• You forget names of close family members or everyday objects.
• You struggle to tell a story, often repeating yourself.
• You feel lost in familiar places, including your home.
• You lose track of what day, season, or year it is.
• You struggle to complete daily tasks, like paying bills, running errands, or self-care.

Dementia or Forgetfulness?
“Normal forgetfulness is misplacing your car keys or not being able to readily come up with a word, but you’re able to retrace your steps or recall the word later,” Teresa said. But memory loss due to dementia can make everyday tasks di cult and impair judgment and speech. Alzheimer’s can also cause vision problems, social withdrawal, and changes in mood, behavior, or personality. If forgetful episodes worry you, Teresa recommends keeping a log and bringing it with you when you see your primary care provider. You can also do this if you’re concerned about a loved one’s forgetfulness.
Diagnosis, Treatment, and Prevention
While there is currently no cure for Alzheimer’s disease, there are options that may slow progression if detected early. e single best step to take if you suspect you or a loved one has dementia is to make an appointment with a primary care provider. Your provider can review your medical history and medications, conduct a depression screening and neurological exam, and refer you for additional testing. Alzheimer’s is diagnosed through multiple tests, including imaging the brain with a CT or MRI scanner, and lumbar puncture to test cerebrospinal uid for Alzheimer’s markers.
“Recently, the FDA cleared the rst blood test to aid in diagnosis of Alzheimer’s which could make it easier for individuals to receive an accurate diagnosis earlier in a less medically invasive way,” Teresa said.
While some risk factors for dementia, like age, can’t be avoided, taking good care of your overall health and wellbeing can potentially lower your risk. Annual checkups, a balanced diet, regular exercise, maintaining a healthy weight, and adequate sleep can bene t your entire body.
“What is good for the heart is good for the brain,” Teresa said, adding that Alzheimer’s is often comorbid with heart disease.
Another tip Teresa shared is to use your head. Learning something new helps your neurons form new neural pathways and strengthen existing ones. Challenge your mind by reading, completing challenging puzzles, or learning new skills.
Support for Patients and Caregivers
Dementia a ects more than the people who have it – nearly 12 million Americans provide unpaid care for family members with Alzheimer’s and dementia.
“No one wakes up with all the knowledge you need to take care of a parent or a spouse with dementia,” Teresa said. “Your relationship has changed.
RESOURCES
Alzheimer’s Helpline
1.800.272.3900
Alzheimer’s Association
Greater Missouri Chapter alz.org/greatermissouri
Find the My ALZ Journey app on the iOS App Store or Google Play.
Join the Columbia Walk To End Alzheimer’s on October 4 alz.org/comowalk
Now you need to take on many roles, like attorney, accountant, or dietitian.” e Alzheimer’s Association website provides resources for people with earlystage Alzheimer’s and their caregivers, including a new, free app called My ALZ Journey. e app can be personalized based on the user, location, and age, and is available for Android and iOS devices. Other resources include education about the disease, real life stories, and links to local community resources including virtual and in-person support groups for patients and caregivers. e association also runs a 24/7 phone hotline to answer questions and provide support. All services are o ered free of charge.
Caregivers can struggle with social isolation. If you know someone caring for a parent or spouse with dementia, check in on them and o er to help with errands if you can.
“Be patient and empathetic not only with the person who has the disease, but with their family. is disease will turn worlds upside down and they are doing the best they can,” Teresa said. By Jessica Park
Calm & Collected AMID A CRISIS
Charles “Howard” Jones doesn’t know when he started having cardiovascular symptoms. e shortness of breath he was experiencing began a couple of years ago and was getting progressively worse. Howard was receiving care from another cardiologist in the region, but moved his care to Martin Tibuakuu, MD at Missouri Heart Center after his son, Chris Jones, joined Boone Health as Chief Operating O cer in 2024.
A pacemaker was implanted in December 2024, but it didn’t seem to help much. en, towards the beginning of February, Howard started showing other concerning symptoms.
“My wife Dona and my son noticed some changes in my speech patterns. I was also having di culty with balance as well as endurance. I declined so much that I became confused and couldn’t get myself out of bed. ey got really concerned and called the ambulance to take me to the emergency room to have me checked out,” Howard said. “And that’s when the fun began,” he said with more than just a hint of sarcasm.
Getting loaded into the ambulance was the last thing Howard remembered until he woke up in the ICU two weeks later, following open heart surgery. In his conscious absence, many things happened.
Howard was originally admitted as an inpatient for sepsis. Doctors determined the source of the infection was streptococcus which destroyed his mitral valve. Howard then spent two weeks in the ICU while they were getting the infection under control so the heart valve could be replaced. But that wasn’t all that was occurring with Howard’s health.
A CT revealed Howard had a brain hemorrhage caused by clots thrown by the infection described as a “showering e ect.” e hemorrhage was complicated by the occurrence of roughly two dozen mini strokes which they tracked with an MRI. If all that weren’t enough for this 81-year-old patient, he needed blood thinners to prevent further strokes but those couldn’t be administered due to the brain bleed.
One month before this photo was taken, I wasn't able to stand on my own. The staff at Boone Health got me to where I am today. This hospital saved my life.


“It was a delicate balance,” Chris said.
Once the infection was resolved, cardiothoracic surgeon Richard Mellitt, MD, was able to perform open-heart surgery to replace the damaged heart valve.
“In my follow-up appointments, I’ve had several healthcare people tell me they weren’t optimistic I’d make it,” Howard said. “It was that dire of a situation.”
Howard still faced a ght to recover. He said that after surgery, he was unable to even roll over in bed. He would undergo inpatient rehabilitation with all modalities, occupational therapy, physical therapy, and speech and cognitive therapy.
“I went from that position to them teaching me how to sit up and eventually stand. I then did physical therapy, occupational therapy and speech therapy several hours each day. My PT and OT activities were primarily me using a walker while in the hospital,” Howard said. “I used the walker for a little bit at home for balance then I switched over to a cane. Now I don’t use anything, so my physical abilities have improved signi cantly. I would say I’m at 80% or more of where I was before I went to the hospital.”
Howard’s path took him from the ER to the cardiac unit, to ICU, to surgery back to the cardiac unit then to inpatient rehabilitation over ve weeks. He graduated to the outpatient cardiac rehab program at Boone Hospital. His follow-ups with neurology have shown the brain bleed to have totally resolved and he’s regaining cognitive function and physical strength. roughout the process, Howard says everyone at Boone Hospital was great, and there are too many to mention. Dr. Mellick, Dr. Tibaukuu, and infectious disease specialist Phillip Beck, MD, were key problem-solvers.
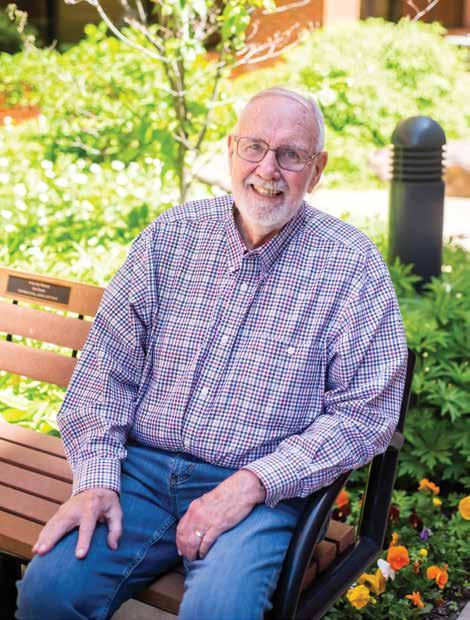
“ e care that I have received from when I arrived to now has been really exceptional,” Howard said. “When I left the hospital after ve weeks, I felt like I was leaving family. From the rehab crew, the housekeeping people, to the RNs, the therapists, were just unbelievable.”
“ e physicians all checked on him often and explained what was going on,” Dona said. “His situation was dire and complicated. We had the hospitalist, neurosurgeon, neurology, infectious disease, cardiology, and cardiothoracic surgery all on his case. ey all communicated well, explained what was going on, and next steps. Dr. Mellitt and Dr. Beck were fantastic in summarizing what was going on in simple terms and communicated frequently.”
And he bonded in personal conversations with his nurses, therapists, and other sta . e two weeks in rehab were especially meaningful as Physical erapist Rashmi and Occupational erapist Patty addressed not only physical challenges, but emotional/psychological challenges as well. Howard also thought fondly of Alayciah, a Patient Care Technician. “Alayciah would pop her head into my room several times a day to see if I needed anything or to see if I wanted to talk. I really appreciated that,” Howard said.
“ ey all had a special ability to encourage him to participate with his care plan and work hard, even though he rarely felt up to it at rst,” Stacy, Howard’s daughter said. “Later, as his energy and condition improved, he looked forward to his treatments and was encouraged by how he was improving.”
“ rough it all, what struck us the most was how quiet and calm it was. Everyone was focused and reassuring,” said Ashley Jones, Physician Assistant, Chris’s wife.
“I don’t know what the long-term e ects of the strokes or the heart surgery will be,” Howard said. “But I continue to receive follow up care from many of the specialist physicians at Boone Health who are ensuring that I continue the road to recover.”
“ ere are still a lot of questions out there that I have that only time will answer.”
One thing Howard does know is that his life was in the hands of a phenomenal team at Boone Health who will help him nd those answers as they arise. By Michelle Terhune

All Shook Up
What to Expect After a Concussion
Y our niece collided with an opponent at a soccer game. Your friend was rear-ended on the Business Loop. You fell from a ladder and hit your head. What do the three of you have in common? Probably a concussion! A concussion is a mild traumatic brain injury that affects the brain’s function temporarily. This can be caused by any impact or jolt to the head. You don’t have to hit your head to sustain a concussion. A sudden stop such as in a car accident can cause your soft brain to hit the hard skull encasing it, resulting in a concussion. Those at
risk include athletes, older adults who have fallen, military personnel exposed to a blast, victims of violence and anyone involved in a car accident.
Some immediate signs you have a concussion are loss of consciousness, nausea or vomiting, confusion, clumsiness and difficulty remembering recent events. Seek medical care if you feel these symptoms or observe them in a loved one. X-rays, MRIs and CT scans won’t show a concussion. However, your provider can assess you for symptoms of concussion and check your head and neck for any other injuries.
Symptoms may change in the days following a head injury, including:
• thinking and memory changes
• headache
• sensitivity to light or sound
• feeling more tired than usual
• imbalance
• dizziness
• blurred vision with head movement
• neck pain
• mood or behavior changes






Hannah Williams, PT, DPT
Nicole Tunink, PT, DPT
Rachel Beanland, PT, DPT
Shae Gilbert, PT, DPT
Ben Engelbrecht, PT, DPT
If you’ve been diagnosed with a concussion, keep in mind that your brain has sustained an injury. Just like a pulled muscle, it will need a combination of rest and symptom-limited activity and exercise to recover. For the first 24 hours or so, you can rest and take it easy. After that, try to gradually return to your normal activities. High quality, adequate sleep is important during this time frame. You should also avoid activities that put you at risk of falling or hitting your head. Having a second injury to your head can complicate recovery significantly. Return to activity will vary based on the individual. The general rule of thumb is to let symptoms guide your activity level. For example, if you go to work and after one hour of focusing on your computer screen your symptoms have returned or worsened, it’s time to take a break. You may need to sit or lay down in a dark, quiet room to allow symptoms to go away. When you’re feeling better, you can try returning to the activity. If your symptoms get worse again, take another break or consider stopping that activity for the day. Sometimes this requires your workplace or school to make accommodations. Don’t hesitate to advocate for yourself. After all, what’s more important than your brain?
Keep in mind that work and exercise aren’t the only things that can stress your recovering brain. Phone time, video games, reading, driving and household chores can all also bring on symptoms. These should be gradually increased over several days to weeks until you are back to tolerating your normal activities.
Has it been over a week and you are still dealing with symptoms of your concussion? It’s time to seek help. A physical therapy referral from your doctor will get you started. We have 5 physical therapists at Boone Therapy who treat concussions and dizziness. Nicole Tunink works with patients at our South location at the Nifong Medical Plaza, and Rachel, Shae, Ben and Hannah see patients at our Main clinic located in the lower level of Broadway Medical Plaza 1. We would love to help you get back on track.
Your first visit will consist of testing your eyes, balance, vestibular or inner ear system, and neck movement. We will also ask you about your symptoms and goals. You’ll receive targeted exercises and guidance to help your brain recover and allow full return to your favorite activities. Over the course of a few weeks, we will help guide you through progressed activities and exercises to decrease your symptoms and recover normal function.
The good news: even though a concussion is a brain injury and should therefore be taken very seriously, the prognosis is good. Most people with concussions will make a complete recovery By Hannah Williams, PT, DPT, Physical Therapist at Boone Therapy
A STROKE occurs when the blood flow that carries oxygen to the brain is cut off by a blockage or ruptured artery. Without oxygen, brain cells begin to die, causing a loss of function and potentially death. Stroke is the leading cause of adult disability and the fifth-leading cause of death in the United States. Stroke is a medical emergency, but fast treatment can save lives and brain tissue.
If you notice stroke symptoms, call 911 immediately! EMS professionals can start your care before you get to the hospital.
Stroke symptoms happen suddenly and can include
• Numbness or weakness in your face, arms or legs, usually on one side
• Trouble seeing in one or both eyes, including double vision
• Confusion, trouble speaking or understanding speech
• Loss of balance or coordination, dizziness, and trouble walking
• A severe headache that feels like the worst headache of your life
If you have any of these symptoms, BE FAST!
Balance
Watch for sudden loss of balance
Eyes
Check for vision loss
Face
Look for uneven smile
Arm
Check if one arm is weak
Speech
Listen for slurred speech
Time
Call 911 immediately

Exercise Your Brain
Taking care of your brain’s health can also be fun! Problem-solving activities like crosswords, word puzzles, or brain teasers can help your brain maintain healthy cognitive function (how the brain perceives, interprets, stores, and retrieves information). Reading, favorite hobbies, and trying something new can also help keep your mind sharp. Each of these nine images represents a common phrase or expression. Don’t worry if some of them are difficult – just like lifting heavier weights helps you build muscles, challenging yourself builds cognitive strength. For more fun, try solving these puzzles with family or friends. See the answers on page 28. Illustrations by Jessica Park
That’s why our Behavioral Crisis Center (BCC) provides 24/7 access to mental health and substance-use services for when you need it most.
Groundbreaking for a new, larger and more expansive BCC (rendering pictured below) is set for Spring 2025.

By helping over 2,500 individuals last year, the BCC is estimated to have saved our community $2,960,503 from diverting community members from jail and the hospital and saving law enforcement's time.
Virtual tour available at burrellcenter.com/columbiabcc
Visit our current location at 1805 E. Walnut St., Columbia, MO 65201
Are you or someone you know in a crisis? Call, text, or video call 988.

2024
LEADER OF THE YEAR
Leslie Duckworth

Our 2024 Leader of the Year, Leslie Duckworth, has guided Boone through a pandemic and our transition to an independent health organization without losing sight of what matters most: safety, quality, and patient experience. The impact of her leadership is visible in our quality, outcomes, and patient experience measures.
EMPLOYEE OF THE YEAR
Jimi
Barbarotta

Our Employee of the Year, Jimi Barbarotta, not only keeps important systems up and running; he’s happy to help when things don’t work as they should. We are grateful for Jimi’s creative approaches to developing and implementing solutions that make it easier for us to complete our work and keep information secure.
Lauren O’Brien, AGACNP-BC
Neurosurgery, Boone Health Neurosurgery and Spine Center
Iwas born and raised in Springfield, Illinois. I am the second of three children, and both of my parents were in the medical field before they retired. I got my Bachelors of Science in Nursing from Illinois State University; then married my high school sweetheart, Tyler. I worked in a Surgical/Trauma/Neuro ICU for approximately 5 years before deciding to return to pursue my master’s degree as an Adult-Gerontology Acute Care Nurse Practitioner through Goldfarb School of Nursing in St. Louis. We then had our first daughter. From there, my husband’s job took us to midMissouri and I began working at University of Missouri in the neurosurgery department, where I fell in love with the specialty. I did that for about 5 years, but later took a job in orthopaedics to better accommodate our growing family. I worked in that specialty for about 5 years but ultimately felt drawn to return to neurosurgery. I have been lucky to be at Boone for the last 1 1/2 years.
Why did you get into the health care field? I have always felt drawn to medicine. Even as a child, I was fascinated by how the body worked and I enjoyed learning about what could be done to help it. My parents were always a wealth of knowledge and encouragement. In college, I began volunteering in a local emergency department and immediately felt fulfilled by helping others both physically and emotionally, which solidified my career plans in nursing.
What interested you in your particular specialty? Neurosurgery has always been a fascinating and challenging field for me. I enjoy coordinating people’s symptoms with their pathology and have always been in awe by how our body functions and adapts. I also love that the field provides opportunity for learning and growth. Out of all my experiences in many parts of medicine, Neurosurgery has always left me feeling both personally and professional satisfied.
What is the most rewarding part of your job? I love many parts of my job including assisting in surgery, helping people to better understand their medical condition and feeling appreciated by my collaborating physicians Drs. Ryan and Bondurant; but the most rewarding part of my job is seeing patients improve after both surgical and non-surgical interventions.
What is the most challenging aspect of your job? The most challenging part of my job is helping people with multiple complex medical issues navigate their neurosurgical challenges.

What do you see changing in health care in the next 5 to 10 years? Without a doubt, the next major change in healthcare will be the incorporation and ethical use of Artificial Intelligence into medicine.
What advice would you give someone looking to become a nurse practitioner? I advise everyone to first get experience as a bedside nurse, to shadow an advanced practice provider and to prioritize lifelong learning. It is also important to choose a program that fits where you want your career to go.
What do you enjoy doing outside of work? Outside of work, when I am not spending time with my husband and 2 daughters (Harper and Hayden), I enjoy exercising, cooking, gardening, caring for my house plants, leading two Girl Scout troops and cuddling with our wonderful dog Roxie.
What advice would you give to someone who is going to be a patient in a hospital for a period of time? Do not be afraid to advocate for yourself! Ask clarifying questions, take notes and repeat back what you are understanding. Also, bring a pillow and blanket from home
Pamela Evans-Smith, PhD, FNP-C
Neurosurgery, Boone Health Neurosurgery and Spine Center
Igrew up in a small town south of Cape Girardeau. I moved to Columbia to go to nursing school. I met my husband here in Columbia. He is from Iowa. We decided to stay in Columbia as we both did not want to move farther away from our families. My husband Kevin is a pharmacist who works at the University full time and at Boone inpatient pharmacy part time. We have 3 sons and 1 daughter who are grown now, and I have a grandson who is 15 months old. We also have 2 golden retrievers.
Why did you get into the health care field? There was a television show about a female neurosurgeon (ironic that she was a neurosurgeon) and she had a sassy nurse. I wanted to be that sassy nurse. I actually wanted to be a paramedic when I was graduating high school, but my father was a telephone lineman and did not want me to have to work out in the weather. He told me he would help me financially if I went to nursing school.

What interested you in your particular specialty? A lot of our patients are either in chronic pain with back and neck issues or scared by the diagnosis of a brain mass. I like helping educate them about their disease process and treatment plan. By educating patients, I feel it helps them realize a sense of power.
What is the most rewarding part of your job? Talking with a patient after a scan has shown improvement in a brain mass or following up after their neck or back pain has improved.
What is the most challenging aspect of your job? Working with patients when you have to deliver a devastating diagnosis such as a brain tumor.
What do you see changing in health care in the next 5 to 10 years? I hope to see more treatment options available for brain tumors. Unfortunately, I feel that insurance companies are going to continue to have bigger control over treatment options in the future.
What advice would you give someone looking to become a nurse practitioner? Really do some introspection before you set your trajectory. There are many different specialties available, choose one that you feel may be your passion. It is a lot easier to do a job every day if you are passionate about it. Be open to new experiences. I never realized I would enjoy the operating room as much as I do.
What do you enjoy doing outside of work? I like to spend time with my family playing games. I like to read and go to movies- I especially like Disney movies, horror, and action. I try to travel to Disney World yearly. I also enjoy going to the beach.
What advice would you give to someone who is going to be a patient in a hospital for a long period of time? Don’t be afraid to discuss your plan of care with your providers, your nurses and your whole care team. Set daily goals for yourself whether that is walking 50 feet or increasing your water intake.
Kathy Caviness, BSN, RN
Neurosurgery
I’m originally from New Florence, Mo., a small town that really taught me the value of community. I earned my Bachelor of Science in Nursing from the University of Missouri-Kansas City. My family is my biggest support system. I married my wonderful husband Tyler in 2019, and we have two daughters — Octavia, 5, and Payton, 3. They keep us on our toes, and their energy and curiosity remind me every day why I love what I do.
Why did you get into the health care field? I’ve always wanted to provide hands-on care and be challenged every day, but I was initially hesitant because I didn’t think I was cut out for the clinical aspects like dealing with blood. But my college advisor encouraged me to meet with the nursing school, and I gained a whole new perspective on the diversity of the nursing field. It was then that I discovered the many different ways I could contribute to patient care. Here I am, 8 years later, loving every moment of it!
What interested you in your particular specialty? What initially drew me to this role was the opportunity to work in neurosurgery. I was excited about handling referrals and knew it would give me valuable insight into the complexities of neurosurgery. Plus, I had the chance to work alongside an incredible nurse practitioner who is a fantastic teacher and a highly skilled provider. That mentorship and the chance to learn from someone so experienced made this role especially appealing.
What is the most rewarding part of your job? The most rewarding part of my job is seeing patients come full circle. Often, they start in the clinic with the nurse practitioner (NP), then move on to meet with one of the surgeons when surgery is needed. After the procedure, many return for their post-op appointment with the NP. It’s amazing to hear patients report an improved quality of life. To me, that’s absolutely priceless.
What is the most challenging aspect of your job? The most challenging aspect of my job as a referral nurse is managing the urgency in getting every patient in to be seen quickly, especially knowing they’re in pain or have just received a life-changing diagnosis. It’s tough to see people in difficult moments, but it motivates me to do everything I can to get them the care they need as quickly as possible.
What has changed in your field since you started practicing? I feel like everything has shifted since the

pandemic. Patients are now more involved in their own care. They come prepared with insightful questions and have the ability to research information before they even step into the office. I think it’s wonderful to see patients take on more autonomy in their healthcare. It’s empowering and leads to better collaboration between patients and providers.
What do you see changing in the next 5 to 10 years? I think social media has given the world the ability to see more than we ever have before. We are able to challenge ourselves, think outside the box, collaborate, and create positive change. Looking ahead, I expect to see greater advancements in treating and curing diseases as people can collaborate globally with ease.
What do you enjoy doing outside of work? I love spending time with my family, and we’re always looking for new adventures. Whether it’s playing outside, taking road trips, watching live sports, trying new restaurants, or discovering new parks and playgrounds, we’re always up for something exciting. Our daughters love to dance and play t-ball, so we stay busy cheering them on and making memories together.
What advice would you give someone looking to become a nurse? Be open to change. Challenge yourself. Find joy in your passion. Establish a work-life balance. Practice self-love. Never forget that the person you’re taking care of is someone else’s whole world.
Nursing at Stephens College.


Our nursing program is a partnership with Boone Health, offering early access to a broad range of clinical experiences and individualized attention. Continue your nursing career at Stephens College.
Brain-Boosting FOODS
Eating certain foods can significantly support brain health by providing essential nutrients that enhance cognitive function, memory, and emotional well-being.
Fatty fish, such as salmon, are rich in omega-3 fatty acids, which are crucial for building brain cell membranes and reducing inflammation.
Antioxidant-rich foods like blueberries and dark chocolate help protect the brain from oxidative stress and aging, while vegetables such as broccoli provide vitamin K, important for memory function.

Nutrient-dense foods like pumpkin seeds and nuts offer minerals like magnesium and zinc, vital for nerve signaling and mood regulation.
Additionally, eggs supply choline, which supports neurotransmitter production, and fruits like oranges deliver vitamin C, a key antioxidant that defends against cognitive decline.
Incorporating these brain-boosting foods into your diet can enhance mental clarity, focus, and long-term brain health.
Here are some of the most brain-healthy foods and why they’re beneficial:




Fatty Fish
(e.g., salmon, sardines, trout)
Rich in omega-3 fatty acids, which are essential for building brain and nerve cells and are linked to slower age-related mental decline and reduced risk of Alzheimer’s.

Dark Chocolate
Contains flavonoids, caffeine, and antioxidants, all of which enhance brain function by improving memory and focus.
Blueberries
Packed with antioxidants, particularly anthocyanins, which reduce inflammation and oxidative stress that can contribute to brain aging and neurodegenerative diseases.

Nuts
(especially walnuts)
Rich in DHA, a type of omega-3 fat, and antioxidants that have been linked to improved cognitive performance and slower cognitive decline.
Broccoli
High in antioxidants and vitamin K, which is essential for forming sphingolipids, a type of fat that’s densely packed into brain cells.

Eggs
Excellent source of choline, which is used to produce acetylcholine, a neurotransmitter important for mood and memory regulation.
Pumpkin Seeds
Contain magnesium, iron, zinc, and copper, which are critical for nerve signaling and brain function; deficiencies in these can impair cognition and mood.

Oranges
A single orange gives nearly all your daily vitamin C, which is key for preventing mental decline and protecting against age-related cognitive deterioration. By Jenny L. Workman
Caring for Your Neck
Sometimes the weight of your head can just feel like too much for the column of bone, muscle and important vasculature, airway, and other structures that make up your neck. If you feel like your neck needs some TLC, try these exercises. If you are having numbness and tingling down one or both arms along with your neck pain, or your pain is interfering with your quality of life, see your doctor and ask about physical therapy for your neck.

Levator Scapula Stretch
With your left hand grasping the edge of your chair, turn your head to the right and tuck your chin down toward your chest, as if you are taking a surreptitious sni of your armpit. You should feel a gentle stretch of the back of your neck on the left side. Hold for 30 seconds, then switch sides.

Upper Trapezius Stretch
With your left hand grasping the edge of your chair to help anchor your shoulder down, tilt your head to the right, keeping your nose pointing straight ahead. You should feel a gentle stretch of the left side of your neck down to your shoulder. Hold for 30 seconds, then switch sides.
Exercise Your Brain: Answers


Cervical Range of Motion
Perform these movements slowly and within a range that does not increase your pain. Move your head up and down ten times. Turn your head side to side ten times. Tilt your ear to your shoulder on each side ten times. Try to do these with your head positioned right on top of your shoulders.


Chin Tuck
While lying on your back, sitting up, or standing, pull your head back gently with your nose pointing straight ahead as though you are trying to give yourself a double chin. Your chin should feel like it is tucking back into your neck or upper throat. You might feel a gentle stretch at the base of your skull. Perform 10x.

Diaphragmatic Breathing
Sometimes, your neck and shoulders ache just because you are holding stress and tension in that area. is isn’t necessarily an exercise of your neck, but it is great at relieving stress and grounding you in your body and in the moment. Sitting in a chair with a back that is supportive (though you can really do this anywhere once you have the knack), place one hand on your stomach and one hand on your chest. Take a deep breath in through your nose, allowing your belly to rise into your hand while your chest stays relatively still. Once you have taken the biggest breath you can, slowly blow the air out, allowing your belly to compress down to help expel the air. Repeat 3x, then take a short break. Do 4 cycles. for an extra dose of relaxation, try the 4-7-8 method: breathe in for 4 counts, hold the breath for 7 counts, then breathe out for 8 counts.

Suboccipital Release
Place two tennis balls into a sock and tie the end. Lie down with the tennis balls positioned at the base of your skull where your head meets your neck so that they are on either side of your spine. If this feels relieving, you can either just let gravity do the work or gently tuck your chin back or rock your head side to side slightly for a little extra pressure. Try this for 2-3 minutes. For a more gentle alternative, you can place the sock between your head and the wall standing up so you can control the pressure more easily. By Hannah Williams, PT, DPT
Neurology Care Spotlight: Helping Patients Heal Through Compassion, Training & Innovation
Supporting Neurology Care at Boone Health
The Boone Hospital Foundation is making a big impact on patients and providers through its support of neurology services at Boone Health. Whether it’s helping stroke survivors heal, funding lifesaving training for emergency responders, or creating a calming environment in the hospital, the Foundation is making every moment count.
Stroke Recovery & Therapy Services
Boone Health’s Stroke Center provides expert care through neurology, neurosurgery, and rehabilitation services. With the Foundation’s help, patients receive even more personalized, healing care.
• Therapeutic Massage: In 2024, the Foundation funded just under $10,000 in therapeutic massage services for 172 post-stroke, postsurgical, and high-risk maternity patients. These services aid in recovery, reduce pain, and promote well-being.
• Therapy Scholarships: The Foundation offers scholarships to help Boone Health employees gain more knowledge in physical and occupational therapy by assisting with tuition and certification exam costs, as well as sending them to pertinent conferences and trainings.
Training Lifesavers: Emergency Services Support
When seconds matter, training saves lives. The Foundation invests in the skills and confidence of Boone Health’s Emergency Services Teams, both in and out of the hospital.
• Advanced Training & Conferences: Scholarships and funding support emergency services staff in attending advanced training and critical care conferences to sharpen their lifesaving skills.
• Community CPR & AED Training: By helping purchase training AEDs, the Foundation supports life-saving CPR and AED sessions for the public—empowering more people to act fast in critical situations.
In-Hospital Comfort & Care
Healing is about more than medicine. The Foundation’s Opportunity Fund supports programs that bring comfort and calm to patients and families.
• The CARE Channel: Soothing music and visuals in patient rooms help reduce stress and anxiety during hospital stays.
• Care Notes: Thoughtfully written materials placed throughout the hospital offer information and emotional support to patients and their loved ones facing difficult moments.
Building a Healthier Future
From bedside to community, the Boone Hospital Foundation continues to strengthen neurology care at Boone Health. Every gift, scholarship, and program helps to ensure that patients receive the best care possible — and that those caring for them have the support they need to succeed.
Stay Connected
Learn more or donate today at boone.health/foundation
2025 Boone Hospital Foundation Board of Directors
Officers
Arlene Heins, President
John Franken, Vice President
Drew Wilkinson, Treasurer
Valerie Ninichuck, Secretary
Dr. James Roller, Past President
Boone Representatives
Jan Beckett
Boone Board of Trustees
Representative
Stacye Smith
Boone Health CHAS
Board Representative
Directors
Dr. Mark Adams, Director
Dawn Daly, Director
Stephanie Goans , Director
Pat Hostetler, Director
Dr. Angela Hull, Director
Erica Pefferman, Director
John Pile, Director
Jolene Schulz, Director

22nd Annual BHF Charity Golf Classic
We are so grateful to our generous sponsors:




Player Gift Sponsor Presenting Sponsor Lunch Sponsor




Player Cart Sponsor Snack Sponsor Prize Sponsor 19th Hole Sponsor

Score Card Sponsor



Refresh Station Sponsor Marketing Sponsor Refresh Station Sponsor
A HUGE thank you to our hole sponsors and in-kind sponsors.
Hole Sponsors:
Boyce and Bynum • Midwest Alarm Services • Cardinal Elevator • Orscheln Industries • MFA Oil • Columbia Insurance • TIG Advisors Logboat Brewing/Waves Cider • House of Brokers • Healthcare Services Group • Harold G Butzer • FSA • United Mechanical Services Missouri Cancer Associates • Columbia Landcare • PEAK Sport and Spine • Ensemble
In-Kind Sponsors: Macadoodles • Logboat Brewing/Waves Cider • Fast Yowi • American Document Solutions • Shelter Insurance
























