June 13, 2014
MEDICAL UNIVERSITY of SOUTH CAROLINA
Vol. 32, No. 41
Neurosurgeons and psychiatrists join ranks Brain stimulation therapies open new fields of research, treatment and career paths BY DAWN BRAZELL Public Relations
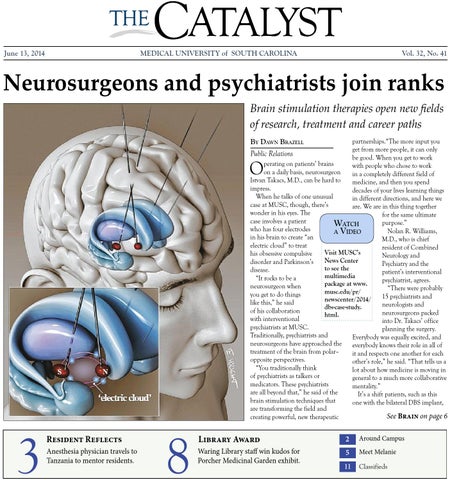
partnerships.“The more input you get from more people, it can only be good. When you get to work perating on patients’ brains with people who chose to work on a daily basis, neurosurgeon in a completely different field of Istvan Takacs, M.D., can be hard to medicine, and then you spend impress. decades of your lives learning things When he talks of one unusual in different directions, and here we case at MUSC, though, there’s are. We are in this thing together wonder in his eyes. The for the same ultimate case involves a patient purpose.” WATCH who has four electrodes Nolan R. Williams, A VIDEO in his brain to create “an M.D., who is chief electric cloud” to treat resident of Combined Visit MUSC’s his obsessive compulsive Neurology and News Center disorder and Parkinson’s Psychiatry and the to see the disease. patient’s interventional multimedia “It rocks to be a psychiatrist, agrees. package at www. neurosurgeon when “There were probably musc.edu/pr/ you get to do things 15 psychiatrists and newscenter/2014/ like this,” he said neurologists and dbs-case-study. of his collaboration neurosurgeons packed html. with interventional into Dr. Takacs’ office psychiatrists at MUSC. planning the surgery. Traditionally, psychiatrists and Everybody was equally excited, and neurosurgeons have approached the everybody knows their role in all of treatment of the brain from polar– it and respects one another for each opposite perspectives. other’s role,” he said. “That tells us a “You traditionally think lot about how medicine is moving in of psychiatrists as talkers or general to a much more collaborative medicators. These psychiatrists mentality.” are all beyond that,” he said of the It’s a shift patients, such as this brain stimulation techniques that one with the bilateral DBS implant, are transforming the field and See Brain on page 6 creating powerful, new therapeutic
O
3
Resident Reflects Anesthesia physician travels to Tanzania to mentor residents.
8
Library Award
2
Around Campus
Waring Library staff win kudos for Porcher Medicinal Garden exhibit.
5
Meet Melanie
11
Classifieds