Murdoch Children’s Research Institute
Prospectus 2024

To give all children the opportunity to live a healthy and fulfilled life.

Murdoch Children’s Research Institute acknowledges the Wurundjeri people as the Traditional Owners of the land on which MCRI is located. We pay our respects to their Elders, past and present.
Image: Melbourne’s biomedical precinct located on Wurundjeri land

Welcome to MCRI’s Prospectus
We are delighted to share with you an insight into the extraordinary research that we do at Murdoch Children’s Research Institute (MCRI) to improve children’s health. This Prospectus details our research and highlights examples of the crucial philanthropic investment required to help more children and families around the world.
As you read this document, we encourage you to consider how your support can make a difference in advancing our research and changing the lives of children for the better.
Investing in the health and wellbeing of children is critical. Early diagnosis of various diseases and health conditions in children is key to prevention and ensuring they receive the right care at the right time – giving hope to more families.
The projects highlighted in this year’s Prospectus represent just a small sample of our work. Carefully chosen to align with MCRI’s Strategic Plan and donor interests, they require essential financial support from generous supporters like you.
Our commitment to sustainable research ensures that our researchers have the tools and support they need in a safe, secure and well-managed environment. Each listed project includes both the direct costs and the contribution to other necessary indirect expenses. For a comprehensive understanding of our projects and the various giving levels, please reach out to us.
Thank you for considering supporting our research. We hope you enjoy learning about some of our work and seeing how you can play a meaningful role in advancing child health research.
Contact us
Engagement and Philanthropy E philanthropy@mcri.edu.au T +61 3 9936 6362
Murdoch Children’s Research Institute
The Royal Children’s Hospital 50 Flemington Road, Parkville Victoria, 3052 Australia mcri.edu.au
3 Prospectus 2024


4 Murdoch Children’s Research Institute Contents Welcome to MCRI’s Prospectus 03 A message from the Director 06 Investing in our children’s future 07 Why MCRI? 08 World-leading research changing the lives of children around the globe 10 Our story 12 Philanthropic funds 14 Scholarships, fellowships and awards 15 Introduction

5 Prospectus 2024 Together we can shape the future 54 Areas of interest 56 Contact us 57 Find out more Theme vision and leadership 16 Project 1: Centre for Population Genomics 17 Project 2: Rare Disease Now 18 Project 3: New horizons in neonatal care 19 Project 4: Mitochondrial disease research with multi-omics 20 Project 5: International Precision Child Health Partnership 21 Meet Levi 22 Genomic Medicine Theme vision and leadership 30 Project 11: Optimal brain health for every child 31 Project 12: Pain education for cerebral palsy 32 Project 13: Diabetes program 33 Project 14: Improving care for children with bronchiolitis 34 Project 15: Transforming neurodevelopmental treatment 35 Meet Emma 36 Clinical Sciences Theme vision and leadership 38 Project 16: Generation Victoria (GenV) 39 Project 17: Children’s Wellbeing Continuum 40 Project 18: ADAPT food allergies program 41 Project 19: Mental Health in Primary Schools Program 42 Project 20: Victorian Collaborative Centre for Children’s Mental Health and Wellbeing 43 Meet Sangita and Maddie 44 Population Health Theme vision and leadership 46 Project 21: Zero Dose Child 47 Project 22: Preschool Wheeze 48 Project 23: Infection-X Research Platform 49 Project 24: Pneumonia in the Asia-Pacific region 50 Project 25: Vaccine equity with a focus on the Asia-Pacific 51 Meet Gursirat 52 Infection, Immunity and Global Health Stem Cell Medicine Theme vision and leadership 23 Project 6: Cancer research discoveries 24 Project 7: Brain cancer breakthroughs 25 Project 8: Kidney disease discoveries 26 Project 9: Gene expression analysis in biomedicine 27 Project 10: Stem cell medicine and AI 28 Meet Mia 29

A message from the Director
At Murdoch Children’s Research Institute (MCRI), we are committed to advancing medical research that gives all children the opportunity to live a healthy and fulfilled life. Every day, our researchers push the boundaries of scientific knowledge, addressing the rarest and most complex conditions, as well as the common health issues affecting children and their families, to deliver better health outcomes for all.
Thanks to the unwavering passion and generosity of our community, MCRI is ranked as one of the top three paediatric institutions globally for research quality and impact.
MCRI’s story is rich, inspiring, and deeply rooted in philanthropy. Over 35 years ago, Dame Elisabeth Murdoch AC DBE and other visionary philanthropists came together to support Professor David Danks’ AO vision of a research institute that would give all children a better future.
Since then, MCRI has become a globally leading medical research institute, dedicated to saving millions of children’s lives.
When you choose to invest in our research, you are investing in the health and wellbeing of all children. Your ongoing support propels our research discoveries further and contributes to crucial knowledge that impacts the lives of children around the world.
MCRI is the place to be to change the face of child health. Your support is invaluable to us and I am genuinely excited about what we can achieve together.
Thank you.
Professor Kathryn North AC Director, Murdoch Children’s Research Institute
6 Murdoch Children’s Research Institute
Investing in our children’s future

“We stand at a pivotal moment, a unique opportunity to spearhead philanthropy and build a brighter future for all children.
What drives me to support MCRI is the unwavering passion of our researchers. They have committed their lives to finding answers for all children, investing not only their intellect but also a significant portion of their time into securing funding for their vital work. It is a paradoxical challenge – the very time they spend seeking support is time that could be devoted to groundbreaking research.
“I feel incredibly fortunate to have been part of MCRI for more than two decades. The passion and brilliance of our researchers never ceases to amaze me. Their commitment to unravelling the health mysteries for all children is truly commendable.
MCRI’s reach has brought about transformative changes in the lives of countless children worldwide. It is a legacy that I believe would make Dame Elisabeth Murdoch immensely proud. Dame Elisabeth was an extraordinary philanthropist, tireless in her support for so many causes, with children being truly at the heart of her work.
My own role at MCRI has been one of the most rewarding experiences of my life. I urge you to join us and witness the remarkable impact we have across more than 100 countries – join us and be part of something truly life-changing.”
Sarah Murdoch MCRI Board (Co-Chair), Global Advisory Board (Chair) and Global Ambassador, Murdoch Children’s Research Institute
By alleviating this burden on our researchers, we can increase the pace of discovery and impact more lives. Join us on this journey and let us ensure all children have the opportunity to live a healthy and fulfilled life.”
Miffany Blythe MCRI Board Member, Development Board (Chair) and Global Advisory Board Member, Murdoch Children’s Research Institute

Top three

1,800+
150 child health research institutes worldwide for research quality and impact*. One of the world-leading researchers working across more than research partners and 1,630 10,759 105 collaborations across diseases. countries.
World-class facilities, laboratories, and research equipment unlocking new frontiers of discovery and innovation.
Located within a globally renowned biomedical precinct of 48,000+ employees and 40+ biomedical organisations in Melbourne, Australia.
*Clarivate Performance analysis and MCRI benchmarking report, November 2023
Murdoch Children’s Research Institute

Image: Murdoch Children's Research Institute, based within The Royal Children's Hospital in Melbourne, Australia.
Photo credit John Gollings
World-leading research changing the lives of children around the globe
First-in-world to grow minikidneys from stem cells
First to grow mini-kidneys from stem cells, now used for studying kidney development and to discover new kidney disease treatments.
Revolutionary blood stem cell breakthrough for childhood cancer
Led the research to grow lab-grown blood cells resembling those in developing embryos, a significant stride towards revolutionising paediatric treatment for blood cancers like leukaemia.
Eliminating disease at a country level
Treated Solomon Islands and Fiji islands with a scabies-reducing drug, decreasing prevalence across communities to enhance quality of life, improve school attendance and reduce rheumatic fever and heart disease.
Lifesaving peanut allergy treatment and cures
Developed highly effective probiotic treatment for children with peanut allergies, inducing remission, and created the AllergyPal app for parental allergy management.
Internationally leading research for concussion
Leading international concussion guideline updates and developed the community-based HeadCheck app for diagnosing and managing concussion recovery.
Leading genomics research
Spearheading the case to incorporate DNA sequencing into healthcare in Australia, leading the national initiative Australian Genomics and also a major contributor to the Global Alliance for Genomics and Health.
First-ever care for children who suffer from stroke
Led the research and a specialist committee to develop Australia’s firstever clinical guidelines to improve the diagnosis and acute management of children who suffer a stroke.

A revolutionary state-wide mental health program in schools
Developed the Mental Health in Primary Schools model of care to support children’s mental health by building the capacity of primary schools and educators.
Rare disease diagnosis in less than three days
Leading the Acute Care Genomics study to provide rapid genomic testing for children in intensive care units across Australia and deliver answers in less than three days.
Ground-breaking rotavirus discovery
Discovered rotavirus over four decades ago and have now developed a rotavirus vaccine to protect millions of newborn babies worldwide against severe and often deadly gastroenteritis.
Helping children grow with severe dwarfism
Helped children with a severe form of dwarfism (achondroplasia) grow at a similar rate to their peers and found the drug potentially able to reduce Sudden Infant Death Syndrome (SIDS) risk.
Fighting heart disease
Creating beating heart cells from stem cells to treat congenital heart disease.


Our story
Our story began in 1986 when paediatrician Professor David Danks AO established the original Murdoch Institute with the support of Dame Elisabeth Murdoch AC DBE, her family, and other visionary philanthropists, including the late Sir Jack Brockhoff, Scobie and Claire MacKinnon Trust and the Miller family.
Professor Danks’ AO vision for an independent genetic research institute expanded from a handful of researchers to become a worldclass centre for genetics research and clinical genetics services.
The formation of the Institute crystallises a rich history of child and adolescent health research on the campus, dating back to 1936 when the first Medical Research Committee was formed within The Royal Children’s Hospital.
In the early 2000s, under the leadership of Chair, Mr Laurie Cox AO, and Director, Professor Bob Williamson AO, the Murdoch Institute and The Royal Children’s Hospital Research Institute merged to form Murdoch Children’s Research Institute, with a broader focus on child health research, including public health and clinical research.
Dame Elisabeth Murdoch AC DBE
As a founding member of the Institute in 1986, Dame Elisabeth Murdoch’s AC DBE unparalleled generosity has empowered the Institute to enhance the health and wellbeing of children worldwide.
Alongside Professor David Danks AO, Dame Elisabeth AC DBE stands at the heart of MCRI.
Until her passing in 2012, Dame Elisabeth played a pivotal role in overseeing the Institute, contributing as a generous philanthropist and esteemed patron. Her influence reached people from all walks of life – from politicians and business leaders to families and children – inspiring them to discover the joy of giving and championing the importance of medical research. She possessed the foresight to recognise the significance of investing in and developing genetic research, even during the early stages of this field.
Image: Co-founders Dame
Elisabeth Murdoch AC DBE and Professor David Danks AO at The Murdoch Institute for Research in Birth Defects
Murdoch Children’s Research Institute

“The
career of a scientist is not an easy one and it is definitely not for all of us, but they depend on our generosity. We must do all that we can within our own capacity to help them in our quest for knowledge.”
Dame Elisabeth Murdoch AC DBE Co-Founder, Murdoch Children’s Research Institute
Philanthropic funds
MCRI has established four funds, enabling supporters to adopt a portfolio approach to their giving. Each fund is designed to allow individuals to direct their contributions to a specific need that inspires them.
We invite like-minded, impactdriven organisations and philanthropists to join forces and co-invest in one of four funds that will help make an even greater difference to paediatric research, and the health of children both in Australia and around the world.
Find out more


Brilliant Minds Fund
Support the career of a talented researcher and make one of the most valuable investments that can be made for the Institute, individual researchers, and the field of child health research.
Discovery Fund
Invest in a range of promising projects and play a role in accelerating ground-breaking discoveries in medical research by providing seed funding for one-ofa-kind, proof-of-concept projects that show huge potential.
Innovation Fund
Fund projects with the greatest potential to deliver real-world outcomes. Our innovative research can be converted into life-changing improvements in the communities in which children live, learn and grow.
Future fund
Support future generations of children by contributing to the long-term endowment of Murdoch Children’s Research Institute.
14 Murdoch Children’s Research Institute
Scholarships, fellowships and awards
Our world-class facilities, strong track record of research excellence and global collaborations provide the capacity to solve complex paediatric conditions and make MCRI an attractive home for the world’s most soughtafter researchers.
In order to attract and retain these brilliant minds and stay at the cutting-edge of discovery, we need to continually invest in our people.
MCRI has developed two models to recognise generous donors wishing to establish a named research position at the Institute:
• Term-named research positions - with funding guaranteed for a minimum of three years.
• Endowed, named research positions – enabling a researcher to be supported in perpetuity.
Scholarships and fellowships have a fundamental impact on our research discoveries, allowing researchers to generate high quality pilot data and improving their competitiveness for peer-reviewed government grants.
Investment and recognition options
Early Career
We invite you to be the visionary of this inspiring initiative, to sustain excellence in paediatric research and to help transform child and adolescent health.
 Image: Professor David Thorburn (left) and researcher (right) with Eli (middle left) and Evie (middle right).
Image: Professor David Thorburn (left) and researcher (right) with Eli (middle left) and Evie (middle right).
Research position Term investment (three year minimum) Endowed investment Fellowship $750,000 ($250K p.a.) $5 Million
Researcher Award $300,000 ($100K p.a.) $2 Million Scholarship $105,000 ($35K p.a.) $1 Million Award $60,000 ($20K p.a.) $500,000

Genomic Medicine
Vision
To develop and implement the latest genetic and functional genomic technologies to transform the lives of children and their families affected by genetic disorders.
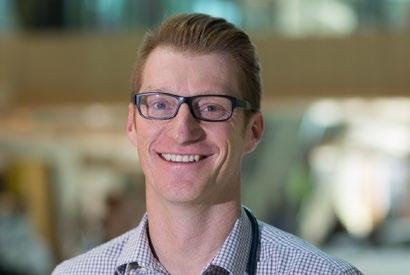
Leadership
“Our genetic research is essential for understanding and addressing child health challenges. Through early diagnosis and targeted treatments, we aim to make a practical impact on genetic disorders, infectious diseases, and non-communicable diseases, contributing to tangible improvements in healthcare for the younger generation.”
 Professor John Christodoulou Director, Genomic Medicine
Professor John Christodoulou Director, Genomic Medicine
Story of discovery and impact
Heel prick test now detects more medical conditions
Diagnosing newborns with rare but serious medical conditions enables early intervention and treatment, offering them the best chance at a healthier life. Newborn screening began as a test for one genetic condition, phenylketonuria, and has since expanded to many others. Recently, screening for a potentially fatal hormone disorder, congenital adrenal hyperplasia, was added. Additionally, our researchers have developed a screening method for Fragile X, Angelman, Prader-Willi, and Chromosome 15q duplication syndromes. We hope these can be added to the screening test in the future.
Find out more

16 Murdoch Children’s Research Institute
Project 1
Centre for Population Genomics: Paving the way for equitable genomic medicine
The Centre for Population Genomics (CPG), established by MCRI and Sydney’s Garvan Institute of Medical Research, aims to advance equitable genomic medicine for all.
Problem
Urgent investment is needed to ensure advances in genomic medicine benefit all and do not exacerbate existing health inequities.
Genomic medicine depends on being able to compare the genomic profiles of patients with those of hundreds of thousands of healthy individuals, to track down the unique changes in the patients that could cause their disease. These genetic causes of disease can be more reliably found when those healthy individuals come from as many different ancestries as possible.
Unfortunately, the existing international genomic databases contain genomic information primarily from individuals of European ancestry – many of the communities living here in Australia are largely or entirely missing from these resources. These include Aboriginal and Torres Strait Islander peoples and other Oceanic communities, as well as people from North Africa, the Middle East, South-East Asia, South Asia and Sub-Saharan Africa. This lack of representation limits the diagnostic power of genomics for everyone. It also means that families from these communities are less likely to receive an accurate diagnosis for their genetic diseases.
Solution
Led by Professor Daniel MacArthur, who previously created the world’s largest human genomic data resource at the Broad Institute of MIT and Harvard, the CPG addresses existing health inequities by collecting and analysing genomic data in respectful partnership with under-represented communities to benefit all and advance precision medicine.
CPG focuses on three core domains: Genetic diversity: Increasing inclusion of under-represented communities in genomic research
Through the ‘OurDNA’ program, we will strive to include genomic data for the 3.5 million Australians who are part of communities largely missing from existing international genomic databases. We will collect and share genetic variation data from over 20,000 Australians, including at least 7,000 participants from under-represented groups, recruited following deep community engagement and co-design.
Rare disease: Leveraging innovative genomic and analysis methods at scale to improve diagnosis
Severe genetic diseases, like muscular dystrophy or cystic fibrosis, are individually rare but collectively this group of more than 7,000 conditions affects around 2 million Australians, with a disproportionate impact on children. The near-term focus of CPG is on improving the genomic diagnosis of rare genetic disorders, and our long-term goal is to empower the development of better therapeutics
for these disorders. We have built a custom cloud-based analysis platform that allows clinicians and researchers to compare patient data with genomic reference databases to identify disease-causing genetic variants. With this approach, we have already provided more than 100 new diagnoses. For families affected by rare disease, a diagnosis opens doors to access support and possible treatments and enables these families to take ownership of future health decisions.
Gene function: Linking genetics to health outcomes to improve therapeutic development
The classic drug discovery pipeline can take up to 15 years and cost more than AU$1 billion to move from initial target identification, through drug development, to regulatory approval. Human genomics has the potential to revolutionise this process; drugs designed against targets with human genetic support are more than twice as likely to succeed in the clinic. We are driving large-scale studies linking genetics, biological assays and clinical outcomes to improve drug target discovery.
Funding will support additional genomic talent, provide critical infrastructure, and enable community engagement, consultation and participant recruitment.
Investment required AU$54,000,000 over five years
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
17 Prospectus 2024
Diversity and Inclusion Genomics Rare Disease Genomic Medicine
Project 2
Rare Disease Now: Unlocking genetic mysteries
Advancing rare disease research through cuttingedge genomic analysis.
Problem
At least one in 12 babies are born with a rare disease. There are more than 7,000 known rare diseases and around 80% have a genetic origin. They are estimated to cause 35% of deaths in children younger than one year old. Even with advances in genomic testing, half the children with a rare disease do not receive a genetic diagnosis with clinical genomic testing, and even fewer receive impactful interventions.
Giving parents an early, accurate genetic diagnosis for their child ends the diagnostic odyssey. It can help inform what will happen with the child’s condition, it can impact management by avoiding unnecessary, expensive and often invasive investigations, and can improve outcomes by identifying any available targeted therapies.
Solution
MCRI’s Rare Diseases Now (RDNow) project unites research and clinical expertise to tackle unanswered and important issues for those affected by rare diseases.
Our vision is to enable all people living with a rare disease the opportunity to receive a precise diagnosis, optimal care, and access to innovative research and available therapy. Funding genomic sequencing for 10 undiagnosed families and the crucial experiments needed to prove that a new gene causes a genetic condition, will have ripple effects that could help countless families in Australia and around the world.
Investment required
AU$120,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
At least one in 12 babies are born with a rare disease.
18 Murdoch Children’s Research Institute
Genomics Rare Disease
Project 3
New horizons in neonatal care: Revolutionising newborn screening with EpiGNs heel-prick test
Improving health outcomes for babies by checking for more childhood developmental conditions in the standard newborn heel-prick test.
Problem
Current genomic newborn screening is limited by its high-cost and lack of precision, missing key developmental conditions, including Fragile X, Prader-Willi, Angelman, Dup15q, Turner, myotonic dystrophy type 1, Beckwith-Wiedemann, Silver-Russell, XXY, XXXY and XXYY syndromes, just to name a few.
Except for Prader-Willi and myotonic dystrophy type 1 syndrome, most of these conditions don’t typically show physical signs at birth. That means early detection can prevent delayed diagnosis, lower medical expenses, and reduce stress and anxiety for families.
Diagnosing Fragile X syndrome early is also crucial. It not only helps the affected infants through providing early access to treatments, but also their mothers, who will be at high risk of having more affected pregnancies before their first newborn is diagnosed, which is typically after the child turns three years old.
Prader-Willi and Turner syndromes can be treated effectively from infancy and there are clinical trials for gene therapy for Angelman and myotonic dystrophy type 1 syndromes. Current medical treatments may also help with serious underlying conditions like intellectual disability, autism and obesity that can occur with these disorders. However, more data of real-time costs and effectiveness of the EpiGNs program are needed for these conditions to be included in the newborn screening programs using the heel-prick test.
Solution
The EpiGNs program, in collaboration with multiple universities and institutions, aims to detect a wider range of developmental conditions using advanced genomic screening techniques. This program will trial a new two-tiered screening process utilising genomics in 100,000 Victorian infants, aimed at setting actionable screening thresholds, providing accurate prevalence estimates, and assessing costeffectiveness. It aims to offer early treatment options, reduce diagnostic delays and costs, and provide parents with more informed reproductive choices.
Investment required
AU$180,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
19 Prospectus 2024
Genomic Medicine Genomics
Project 4 Into the Unknown: Transforming mitochondrial disease research with multi-omics
Revolutionising the diagnosis, prevention and treatment of mitochondrial diseases, using cutting-edge genetics and multi-omic analysis.
Problem
Mitochondrial diseases or “mito” are inherited problems in energy generation that cause severe health burdens, from chronic illness to early mortality. At least 60 children born in Australia each year will develop these life-limiting diseases. They are particularly complex to diagnose as they comprise over 400 different genetic disorders affecting any or all organ systems. Despite technological advancements, about half of all patients with suspected mito remain undiagnosed even following genome sequencing. This leaves families in prolonged states of uncertainty and without effective treatment options.
Solution
Australia is at the international forefront of developing a comprehensive “multi-omics” diagnostic approach to combine genomics, transcriptomics, proteomics, and computational methods. We are leading mitoMDT, a national Mito Multidisciplinary Team, to leverage advanced diagnostic technologies to lift diagnostic rates towards 90% and to demonstrate the health economic benefit of transitioning them from research tests to routine clinical care.
Finding the genetic answer can enable families to be able to access innovative clinical trials like ‘MitoHOPE’, which explores mitochondrial donation for preventing mitochondrial diseases, and will enable development of personalised medicine approaches through stem cell models.
Investment required
AU$180,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
At least 60 children born in Australia each year will develop these lifelimiting diseases.
20 Murdoch Children’s Research Institute
Genomics Innovation
Project 5
International Precision Child Health Partnership (IPCHiP): Harnessing genomics to transform child health
Global partnership to revolutionise the treatment of childhood diseases and deliver better health outcomes through genomic medicine.
Problem
Childhood diseases present unique challenges that demand specialised approaches. Traditional treatments often follow a one-size-fits-all model, which can be ineffective for the complex, individual needs of children with various conditions, especially for those with a rare disease. The lack of targeted therapies hampers outcomes and can lead to lifelong complications.
The average timeframe for diagnosing a child with a rare disease is approximately five years and can involve multiple rounds of testing. This prolonged process poses major challenges for the child and their family, leading to missed opportunities for timely treatment and significantly diminishing the child’s prospects of reaching their full potential – with too many children dying before they even receive a diagnosis.
Solution
Australia, Canada, the UK and the USA have joined forces to enhance healthcare for critically ill infants and children through the International Precision Child Health Partnership (IPCHiP).
This collaborative effort between four paediatric hospitals - Boston Children’s Hospital; UCL Great Ormond Street Institute for Child Health and Great Ormond Street Hospital (London); Murdoch Children’s Research Institute with The Royal Children’s Hospital (Melbourne); and The Hospital for Sick Children (SickKids) (Toronto) focuses on leveraging genomics and other transformative technologies to transform healthcare.
IPCHiP aims to accelerate the diagnosis and treatment of rare diseases, which affect a significant portion of the global population. By integrating whole genome sequencing into standard care, the partnership seeks to reduce the diagnostic odyssey for families, improving outcomes for children with rare diseases and ensuring these advanced technologies become accessible and funded within healthcare systems.
Through its commitment to precision medicine, IPCHiP envisions a future where every child receives personalised care that optimises health outcomes. This initiative not only promises to revolutionise the treatment of paediatric diseases but also to establish a new standard for healthcare worldwide.
Investment required
AU$1,000,000 over three years
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
21 Prospectus 2024
Genomics Global Health Rare Disease Genomic Medicine

Meet Levi
“The results we got through early genomic testing changed his life forever”
Levi Trowbridge was just three days old and newly released from the maternity ward when he went into convulsions.
Within a week, Levi was transferred to The Royal Children’s Hospital in Melbourne and put under the care of Dr Katherine Howell, the epilepsy team leader at MCRI and a paediatric neurologist at The Royal Children’s Hospital.
“Watching your newborn baby not breathe for periods of time, not being able to hold him due to affecting his brain waves felt like my heart was being ripped out of my chest,” said Karsha, Levi’s mother.
After taking part in a rapid genomic testing program for critically ill children at MCRI, Levi was diagnosed with a rare genetic disorder at three weeks of age.
“There is no easy way to discuss what Levi went through at the start of his life, but the results we got through early genomic testing changed his life forever,” said Karsha.
“If we had been waiting years for a diagnosis, his development and learning may never have progressed. It is likely Levi wouldn’t have walked, talked or breathed on his own. Early intervention is crucial because every seizure, no matter how small, does damage.”
Karsha said after changing medications Levi went from having five seizures a day to not having any since February 2020.
Levi improved rapidly and his multiple daily seizures stopped by the time he was three weeks old –he was more alert, started to feed well and was able to go home from the hospital. Today, Levi is healthy and seizure-free.
Levi’s treatment and diagnosis marks the dawn of the genomic revolution and provides a glimpse of what is possible through precision medicine. Prompt genetic diagnosis guided the choice of seizure medication, with dramatic effect. Most other antiseizure medications would not have worked for Levi.
22 Murdoch Children’s Research Institute
Stem Cell Medicine
Vision
To be at the forefront of stem cell research and translation globally, paving the way for a new generation of stem cell treatments.
Leadership
“Our researchers are pioneering therapies for childhood diseases once deemed incurable – be it kidney diseases, heart and skeletal muscle disorders, leukaemia, brain cancer, respiratory ailments, or juvenile diabetes. Every breakthrough is an exciting stride toward a future where no child’s health is defined by these health challenges.”
 Professor Enzo Porrello Director, Stem Cell Medicine
Professor Enzo Porrello Director, Stem Cell Medicine
Story of discovery and impact
Kidney models pave the way to better treatments
Approximately 1.7 million Australians have kidney disease. The potential toxicity of new drugs is a major problem in the search for better treatments.
We need a safer way to test new therapies, especially in children, to avoid additional risk or harm.
We created models of human kidney, paving the way for new treatments for kidney failure and possibly laboratory-grown transplants.
Find out more

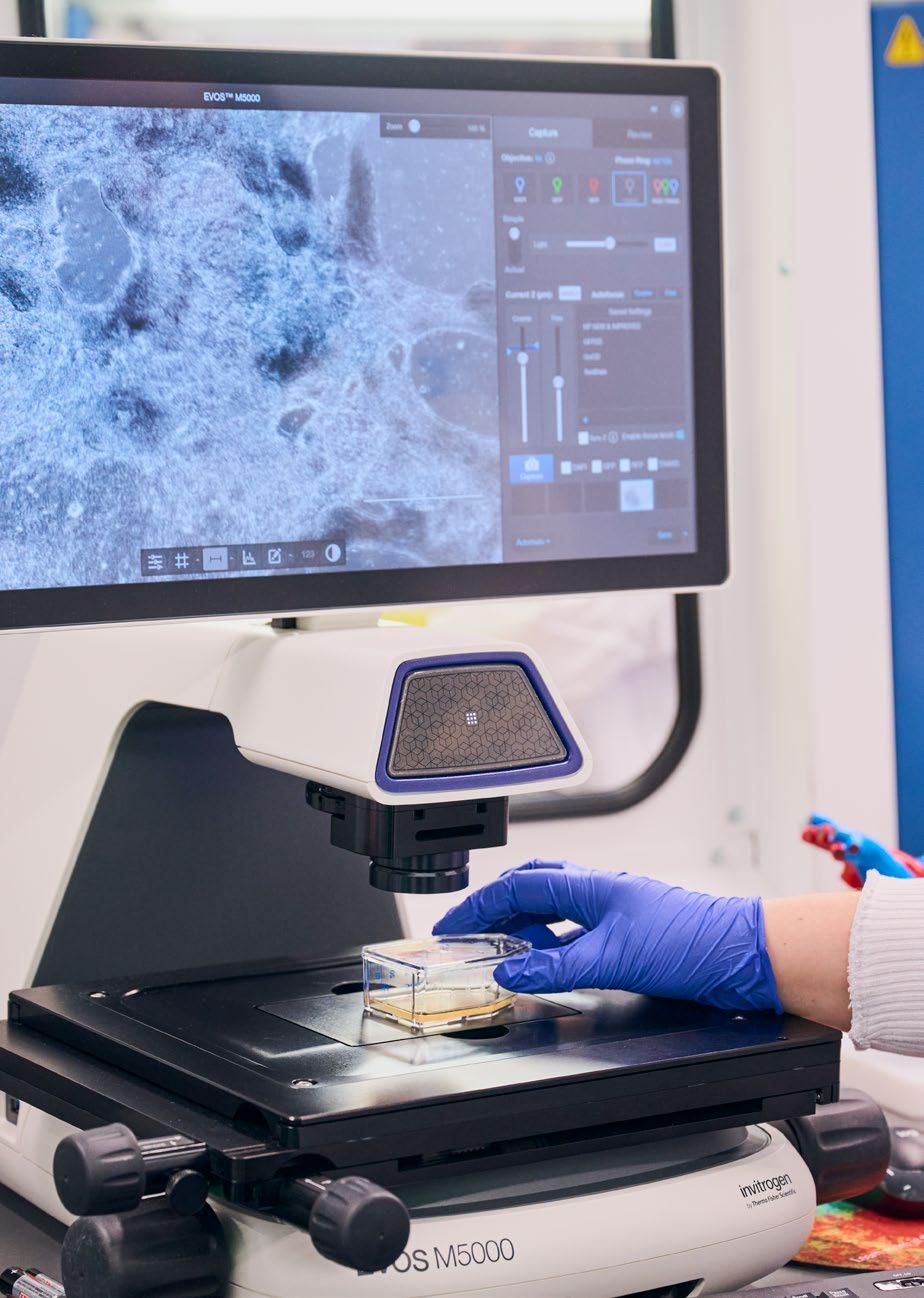
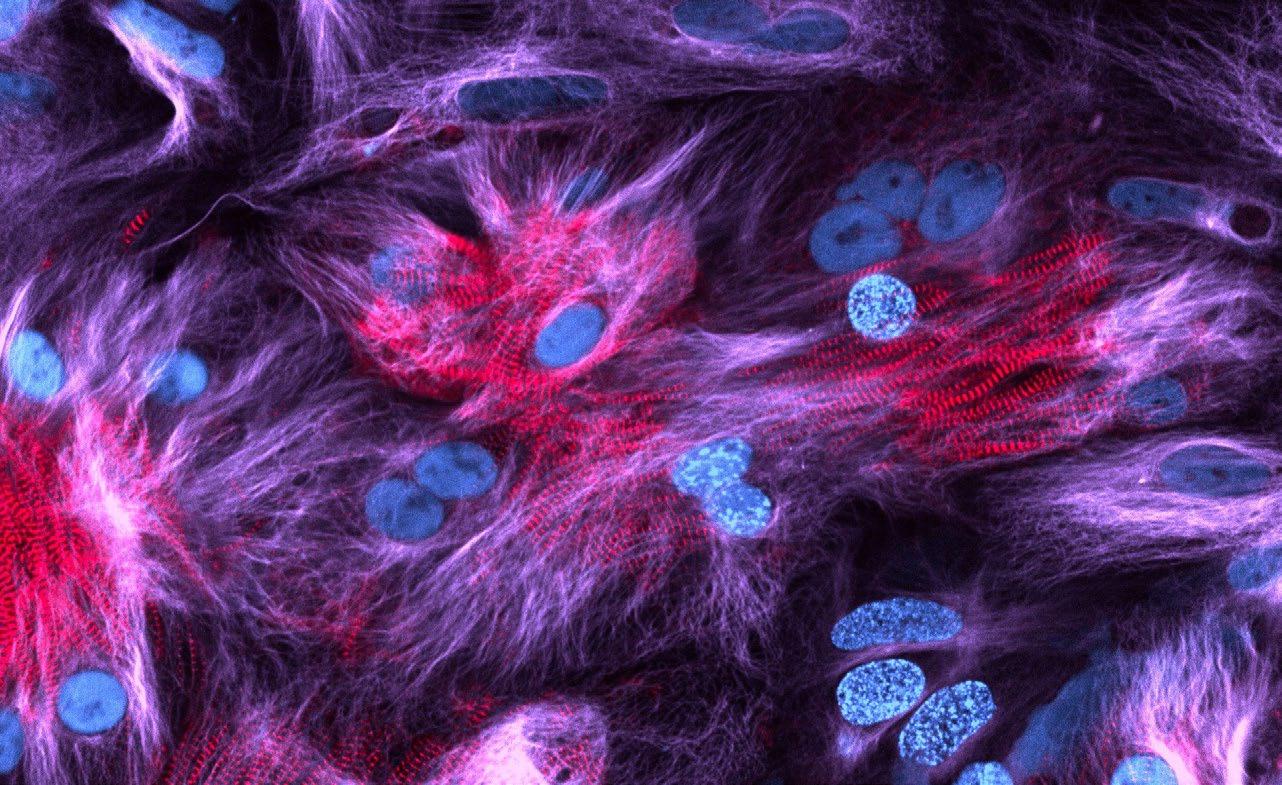
Header image: Proliferation (blue) of heart muscle cells (red) in a stem cell derived 2D cardiac model.
Credit: Dr Frankie Butera and Rachel Morris (Heart Regeneration groupProf Enzo Porrello and A/Prof David Elliott).
23 Prospectus 2024
Project 6
Cancer research discoveries: A new era for childhood cancer treatment
Developing new therapies and technologies to improve health outcomes and the quality of life for those affected by childhood cancer.
Problem
At diagnosis, nearly half of all children with cancer in Australia were aged four or under, with the number of childhood cancer cases increasing by 67% in Australia between 1983 and 2015. Survival rates for paediatric brain, bone, and soft tissue cancers are generally low, and long-term issues for survivors include heart problems or secondary cancers resulting from cancer therapy.
Solution
Our cancer team unites the expertise of research scientists, clinicians, specialists, and onsite enablers including the Children’s Cancer Centre and the Children’s Cancer Centre Biobank. This collaborative approach is necessary to make the greatest impact on the unmet needs of infants, children and adolescents with cancer in Australia and abroad.
Cell and tissue irradiator
This critical piece of equipment will allow our world-leading research team to improve paediatric cancer treatment and quality of life for children and their families. The irradiator will enable us to model the brain and blood cells of animals given cancer therapy (radiation), to understand the damaging effects of this treatment and the biological mechanisms that cause secondary cancers to develop. The irradiator can also stop cell division of living cells, allowing researchers to grow various types of cells and research different diseases.
Bioluminescence imaging system
Finding personalised cancer drug therapies for patients requires state-of-the-art in vivo imaging. This non-invasive equipment will allow our researchers to visualise and understand, in living organisms, the live progression of tumours. Researchers can alter specific molecules in tumour cells and see how these changes affect tumour growth. For example, by observing how a tumour shrinks after providing cancer treatment, researchers can begin to figure out which treatments work best. This powerful system will also allow other researchers to investigate non-cancer conditions in living organisms.
Investment required
AU$750,000
• Cell and tissue irradiator: AU$350,000
• State-of-the-art bioluminescence imaging system: AU$450,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
24 Murdoch Children’s Research Institute
Brain Cancer Equipment Stem Cell Medicine
Brain cancer breakthroughs: Accelerating drug discovery for children with brain cancer
Revolutionising the treatment of childhood brain cancers, specifically medulloblastomas, by leveraging cutting-edge mass spectrometry technologies to identify new therapeutic targets, offering hope for more effective, precise treatment options.
Problem
Medulloblastoma, the most prevalent paediatric brain cancer, presents a dire prognosis with high relapse rates and severe treatment side effects. Current treatment protocols, not tailored to specific tumour sub-groups, often lead to life-threatening outcomes. This project addresses the critical need for a nuanced understanding of medulloblastoma’s molecular basis to develop effective, targeted therapies.
Solution
Our researchers propose employing advanced proteomic technologies and live-cell imaging to investigate molecular targets in medulloblastoma. By profiling tumour samples and screening them against a library of 30,000 drug compounds, the project aims to identify new cancer treatments. A confocal live-cell automated microscope will enhance this exploration, linking molecular discoveries with potential therapeutics.
This research promises to redefine medulloblastoma treatment, shifting from generic protocols to tailored cancer medicine. By identifying precise drug targets and compounds, the project enables the development of more effective treatments for medulloblastoma sub-types, which currently lack successful interventions. The outcome will not just be life-saving therapies for young patients, but a paradigm-shift in the approach for treating paediatric brain cancers.
Investment required
AU$504,200
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
25 Prospectus 2024 Stem Cell Medicine Project 7
Brain Cancer Equipment Innovation Stem Cell Medicine
Kidney disease discoveries: Uncovering therapies for genetic kidney disease through stem cell models
Addressing currently untreatable genetic kidney disease conditions.
Problem
One in 1,000 children are born with a kidney defect, with one in 15,000 presenting with severe kidney disease.
While we can now diagnose the genetic mutations in over 50% of patients presenting with renal failure, there are currently no therapies other than renal replacement or dialysis.
Solution
We are proposing to develop a therapy which would delay the need for dialysis or transplantation, reducing disease burden and giving children the chance to attend school camps, birthday parties and live a better quality of life.
Utilising human stem cells, we will model a rare but severe paediatric kidney disease, nephrotic syndrome. We will grow the affected kidney cells in our laboratory and screen over 4,500 approved drug compounds, some of which may correct the protein defect observed in genetic nephrotic syndrome.
Investment required AU$204,720
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
One in 15,000 children present with kidney disease as a result of inherited gene variants.
26 Murdoch Children’s Research Institute Kidney Stem Cell Medicine
Project 8
Gene expression analysis in biomedicine: 3D analysis of organs
Exploring organ development and disease research in 3D.
Problem
The advancement in understanding disease and organ development has been significantly restricted, not by a lack of data, but by the critical shortage of advanced software tools necessary for interpreting complex tissue gene expressions. Irrespective of the disease or organ affected, in both children and adults, analysis of gene expression data is one of the most critical steps to understanding a path towards novel treatment. Despite the emergence of spatial transcriptomics, a revolutionary technique offering detailed insights into gene expression within tissues, a significant bottleneck persists. The full potential of this data to unveil organ and disease development, particularly in three dimensions, remains untapped due to a critical shortage of adequate software tools for biomedical researchers. This gap poses a significant challenge in the field of biomedical research.
Solution
VR-Omics addresses this gap by providing a comprehensive, intuitive data visualisation platform with an integrated, fully automated workflow.
This solution empowers biologists to independently conduct indepth analysis of spatially resolved transcriptomic (SRT) data, revolutionising their ability to extract meaningful insights. By bridging the divide for noncomputational users, VR-Omics enables more efficient and effective exploration of SRT data, leading to groundbreaking discoveries in tissue and disease development.
The anticipated impact of VROmics is profound, streamlining data integration and comparison in SRT, thereby enhancing our understanding of diseases and guiding therapeutic interventions. This democratisation of SRT analysis will not only accelerate research but also foster innovation within the biomedical community, ultimately contributing to improved patient outcomes in precision medicine.omes in precision medicine.
Investment required
AU$117,364
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
27 Prospectus 2024 Stem Cell Medicine
Project 9
Innovation Stem Cell Medicine
Stem cell medicine and AI: Pioneering the future of paediatric cardiac care
Harnessing stem cells and artificial intelligence (AI) to develop precision therapies for childhood heart disease.
Problem
Heart disease is the leading cause of death and disability in children, affecting up to one in 100 live births.
Childhood heart disease includes congenital heart defects that affect the structure of the heart, as well as cardiomyopathies of the heart muscle, both of which affect the heart’s ability to pump efficiently.
In the most severe cases, these conditions can progress to heart failure, which is a life-threatening condition where the diseased heart is unable to pump enough blood to meet the needs of the body.
Current therapies for heart failure in children do not target the root cause of disease and only offer symptomatic relief. Therefore, the only option for patients in end stage heart failure is heart transplantation. Unfortunately, heart transplantation has limitations including low donor tissue availability, poor medium to long term survival rates, lifelong immunosuppression requiring frequent hospitalisation, as well as poor quality of life for transplanted patients.
Solution
A global partnership between MCRI and Gladstone Institutes, two of the world’s leading research institutes in child health, computational machine learning and stem cell medicine, to develop precision therapies for childhood heart disease.
This new collaboration aims to transform the treatment of childhood heart disease by identifying and targeting molecular pathways predictive of patient outcomes, allowing tailored treatments for each patient to prevent progression to heart failure. This collaboration aims to:
• Utilise MCRI’s extensive stem cell technologies and patient access to drive biological understanding.
• Employ Gladstone Institute’s advanced AI capabilities to analyse extensive data sets, revealing new biological insights.
• Accelerate the development of precision therapies tailored to the unique genetic makeup of each child.
Investment required
US$5,000,000 over three years
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
Heart disease
is a critical health issue
affecting children around the world (one in 100 births).
28 Murdoch Children’s Research Institute Project 10
Heart Stem Cell Medicine

Meet
Mia was diagnosed with a complex congenital heart disease as a baby, requiring multiple surgeries during her first few years of life. Due to her condition, Mia’s heart functions with a single ventricle instead of the usual two beating chambers.
“I was born with a few holes in my heart, essentially half a heart, and needed four open-heart surgeries. Ever since I was little, I have struggled with walking and dealing with the extremities of weather because my heart struggles to pump blood around my body,” said Mia.
Mia and other patients like her are at an increased risk of developing complications in adulthood, including heart failure.
At MCRI, researchers are developing stem cell-derived heart tissue patches to boost heart function and ultimately prevent heart failure in children with a single ventricle.
“These heart patches could be the cure for heart disease and heart failure one day. This research is essential because it could save lives, and I think that’s worth investing in,” said Mia.
“It’s really exciting to watch the research being done at MCRI and see little beating heart cells down a microscope. It’s incredible to think of the potential, and my hope is that other kids with heart diseases can live a normal life without surgeries and being pricked with needles from birth.”
29 Prospectus 2024
Mia
Stem Cell Medicine
Image: Mia (left) and Lyndall (right) Cowley

Clinical Sciences
Vision
To generate and translate new knowledge to advance clinical care of babies, children and adolescents, save lives and improve health and wellbeing of vulnerable children and their families.
Leadership
“Our researchers are world renowned, and the innovation, excellence and commitment to improving the lives of sick children, never ceases to astonish!”
 Professor Vicki Anderson Director, Clinical Sciences
Professor Vicki Anderson Director, Clinical Sciences
Story of discovery and impact
HeadCheck app improves concussion care
Despite many sports modifying rules to reduce contact among younger players, concussions affect one in five individuals by age 16. However, most parents fail to recognise the severity of symptoms or seek medical attention.
Our research indicates that about one in three children and adolescents develop a mental health condition after a concussion, which can persist for several years.
In collaboration with The Royal Children’s Hospital (RCH) and the Australian Football League (AFL), we have developed the groundbreaking HeadCheck app to educate parents, coaches, first aiders, and players about when medical attention is needed.
Find out more

Header image: Professor Mimi Tang (right) and patient Chevy, 6.
30 Murdoch Children’s Research Institute
Optimal brain health for every child: Pioneering tomorrow’s solutions today
Problem
Understanding the many complex pathways of childhood brain development, including how individual differences in neurodevelopment impact health and the process of recovery from neurological conditions, remains a significant challenge. Current diagnostic and research methods often fall short in providing the depth of information needed to fully grasp these complexities. This limitation hampers the development of targeted, effective interventions for young individuals facing brain health challenges, leaving a critical gap in paediatric neurological care.
Solution
In order for this sophisticated medical technology to be utilised to its fullest potential, the Developmental Imaging Research Group was formed by MCRI over a decade ago; a multidisciplinary team of developmental imaging experts with strong structural links to RCH clinical services. The productive relationship between RCH Medical Imaging Department and the MCRI Developmental Imaging team enables high quality imaging capture and analysis for delivery of excellence in clinical care, the prompt translation of research evidence and new technologies into clinical care (including machine learning/AI and innovative imaging capture and analytics).
Our mission is to translate the rich insights gained from our research into significantly improved diagnostic and therapeutic care. We are dedicated to pioneering new pathways in paediatric brain health, offering more precise, effective and personalised treatment options for children and adolescents.
Investment required
AU$1,500,000 over three years
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
31 Prospectus 2024
Project 11
Brain Clinical Sciences Clinical Sciences
Project 12
Pain education for cerebral palsy: Improving pain management for children with cerebral palsy
Developing an online platform for pain education, specifically designed for children with cerebral palsy and their families, to improve pain management and enhance their quality of life.
Problem
Many children with cerebral palsy have to deal with chronic pain, which is often not adequately recognised or treated in this population. Conventional pain management approaches fail to address the unique challenges of these children, particularly those with complex communication needs. The absence of specialised, accessible pain education restricts effective self-management, adversely affecting the child’s participation, emotional wellbeing, and overall health. This initiative targets the critical need for relevant and accessible pain education tailored for children with cerebral palsy and their families.
Solution
Our solution involves a synergistic approach where we partner with children and young people with cerebral palsy and their families to create an online pain education and self-management platform that truly resonates with their experiences and needs. This involves delving into a comprehensive needs analysis, including literature reviews and gathering first-hand insights through surveys, interviews, and focus groups.
The heart of the project lies in the iterative development of a prototype online system, shaped by the voices of those with lived experiences. This is followed by a critical evaluation phase through a pilot study, ensuring the platform’s efficacy for children with cerebral palsy experiencing chronic pain.
Investment required
AU$36,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
32 Murdoch Children’s Research Institute Clinical Sciences Education
Project 13
Diabetes program: Innovative diabetes therapy solutions for children
Combining expertise in immunology, stem cell medicine, and clinical trials, to transform the lives of children affected by type 1 diabetes (T1D).
Problem
Type 1 diabetes (T1D) is a condition in which the immune system attacks the part of the pancreas that makes insulin, leaving affected children with the need to regularly inject this hormone or to be permanently tied to glucose monitoring and insulin pump devices. Not only is this treatment difficult for children, but it also places a substantial burden on families. Despite many technological advancements, modern treatment methods using insulin pumps do not fully compensate for the loss insulin made by the body, meaning clinical outcomes have seen little improvement over the last century. The emergence of immunotherapy as a potential intervention for T1D highlights the need for innovative approaches to fundamentally change the treatment landscape for affected children.
Solution
Immunotherapies have the potential to arrest the development of T1D while stem cell medicine provides hope for those already affected. Our program brings all of these cuttingedge approaches into one clinically focussed effort.
Our program seeks to pioneer T1D immunotherapy clinical research in Australasia. By leveraging our collective expertise in immunology, stem cell medicine, and clinical trials, we aim to establish a comprehensive framework for T1D treatment. This includes creating baseline immune profiles for future trials, developing a ‘diabetes in a dish’ stem cell model to explore patient-tailored therapies, and initiating clinical trials at Melbourne Children’s Campus. These efforts are directed towards implementing cutting-edge immunotherapies, with the goal of creating lasting changes in the immune system and eliminating the need for daily insulin therapy.
We can initiate a transformative program in T1D research, focusing on immune profiling and stem cell models to search both causes and cures. This investment will lead to improved understanding and innovative treatments for T1D, enhancing the quality of life for children.
Investment required
AU$374,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
33 Prospectus 2024 Clinical Sciences Clinical Sciences Diabetes Stem Cell Medicine
Breathing hope into children’s health: Improving the care of children with bronchiolitis
Problem
Bronchiolitis is the leading cause of infant hospital admissions in Australia and presents a dual challenge. First, clinicians struggle to stay current with evolving evidence for managing this condition. Traditional guidelines lag, hindering the delivery of the most effective treatments. Second, the poorly designed discharge information leads to confusion, stress for families, and unnecessary Emergency Department revisits, compounding the socioeconomic burden, especially in disadvantaged areas.
Solution
Our research proposes a twopronged approach. We will introduce living guidelines that dynamically evolve with the latest research, placing up-to-date, evidencebased recommendations at the fingertips of frontline clinicians ensuring clinicians can offer cutting-edge care.
We will develop discharge communication materials through a co-design process with parents and clinicians, aiming to enhance understanding and improve care after hospital discharge. The co-designed discharge information will provide clear, understandable instructions for caregivers, significantly improving patient safety and reducing the stress associated with home care post-hospitalisation.
Investment required
AU$120,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
34 Murdoch Children’s Research Institute Clinical Sciences Respiratory
Project
14
Project 15
Transforming neurodevelopmental treatment: Stem cell medicine and clinical care for neurodevelopment disorders
Combining expertise in stem cell medicine and clinical care to change the trajectory of treatment for children with neurodevelopmental disorders.
Problem
Neurodevelopmental disorders are a large group of conditions characterised by impaired functioning of the nervous system, stemming from early brain development. The developmental impact initiates in the womb and persists, influencing brain maturation and behaviour throughout childhood. These disorders include autism spectrum disorder (ASD), intellectual disability, cerebral palsy (leading to motor disabilities), seizures, learning disabilities (such as dyslexia), and attention-deficit/hyperactivity disorder (ADHD).
Affected children can have difficulty regulating emotions, learning, socially integrating, and movement. The causes and mechanisms of why they develop are not fully understood, which poses challenges for developing effective and targeted treatments.
Solution
Our vision is to develop personalised treatments to improve the lives of children with neurodevelopmental disorders. Our team is internationally leading in this field, with expertise across clinical care, neuroimaging, and lab disease modelling.
Our research in the underlying mechanisms causing autism has two key aspects – understanding the detailed clinical and behavioural aspects of autism, and understanding the effects that different genetic conditions have on brain development in the lab, using advanced modelling in patient derived induced pluripotent stem cells (iPSC). We are now seeking additional researcher support on the clinical aspects of autism, and on stem cell models of brain development in the laboratory.
Investment required
AU$260,000 over three years
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
35 Prospectus 2024 Clinical Sciences Brain Clinical Sciences Stem Cell Medicine
Meet Emma
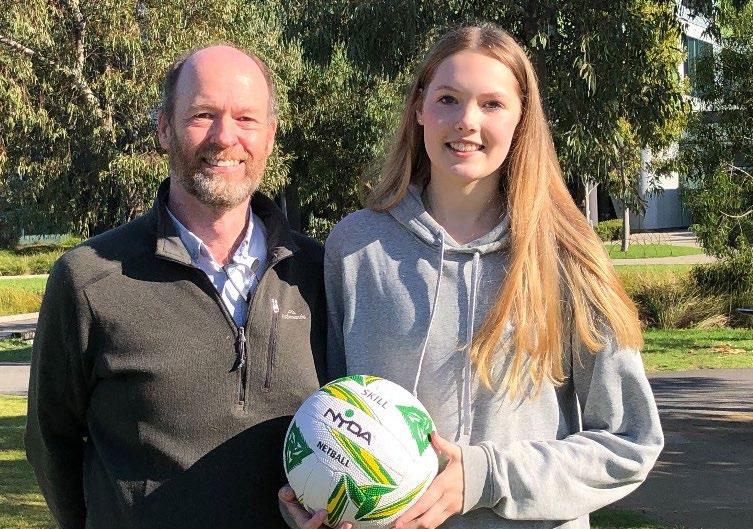
Emma has been seeking mental health support after experiencing two concussions, a year apart. In 2019, while playing netball, Emma knocked her head on a goal post and was later hit with a ball in the back of the head. Emma stated that after the second concussion, she developed anxiety, headaches, a sense of hopelessness, and had trouble concentrating.
“After my last concussion, I found it very hard to be motivated for school and everyday life. Doing the simplest of tasks, such as a walk, was difficult for me. Not being able to complete these tasks got me quite disheartened, which impacted my mental health,” she said.
Emma’s dad, Bruce Henry, welcomed the push for mental health to be part of pediatric
concussion assessment and management, as many cases would be going untreated.
“When a child has a concussion, they might look fine, but you can’t see the underlying impact. It’s crucial for mental health to be part of concussion management, which has been essential to Emma’s recovery process,” Bruce said.
MCRI’s Director of Clinical Sciences, Professor Vicki Anderson, emphasised that assessment, prevention, and intervention of mental health difficulties after a concussion should be integrated into standard concussion management.
“Mental health is central to concussion recovery. Concussion may both precipitate and exacerbate mental health difficulties, impacting delayed recovery and psychosocial outcomes,” she said.
“Incorporating mental health risk into post-injury management represents an opportunity to engage children and adolescents with mental health services to either prevent unnecessary problems emerging or to treat already existing issues.”
Developed by world-leading concussion experts at MCRI and The Royal Children’s Hospital, and in collaboration with the AFL, the HeadCheck app helps parents, coaches, and first aiders recognise the signs of concussion and manage the child’s safe return to school, play, and organised sports.
For more information, visit www.headcheck.com.au or download the app from the Apple Store.
Image: Bruce (left) and daughter Emma (right)
36 Murdoch Children’s Research Institute


Population Health
Vision
To understand the determinants of health at the population level and translate knowledge appropriate to diverse populations, particularly those affected by social disparities.
Leadership
“In Population Health, we focus on the common chronic conditions in childhood – mental health, allergy, developmental problems; these are the conditions that are going to impact the lives of our future generations. Our research strives to create better systems, services and policies that will truly make a difference to children and their families to prevent, intervene early and cure these conditions.”
 Professor Sharon Goldfeld Director, Population Health
Professor Sharon Goldfeld Director, Population Health
Story of discovery and impact
Teaching babies to sleep is safe and improves parental wellbeing
Sleeping problems are common in babies with over one-third having trouble settling to sleep at the start of the night, waking overnight, or both.
We found that from about six months of age, babies can be taught to fall asleep by themselves and not cry out for mum or dad when they wake during sleep using the strategies of ‘controlled comforting’ or ‘camping out.’
Our evidence-based sleep intervention program is now embedded in Victoria’s free Maternal and Child Health Service as an eightmonth intervention and is available online to health professionals and parents throughout the globe.
Find out more

Header image: Joining the world’s largest-ever birth and parent cohort studies. Dad, Patrick, 11-month-old baby, Violet, and mum, Paige, joined GenV in June 2022 at Frankston Hospital when Violet was born.
38 Murdoch Children’s Research Institute
Generation Victoria (GenV): Transforming the health and wellbeing of an entire generation
Generation Victoria (GenV) is Australia’s largest child and parent longitudinal cohort internationally unique in its diversity and ability to enable real-time trials. With recruitment remaining open to families with a child born in the birth window, GenV is ideally placed to help solve the complex health, wellbeing and social issues affecting children and parents worldwide.
Problem
Each child has their own individual health and wellbeing challenges underpinned by their unique combination of genetic, behavioural, environmental and clinical factors. These problems carry on into adulthood. Many diseases and disorders in adult life, including major public health concerns and complex issues such as obesity, heart disease, climate change, equity, entrenched disadvantage and mental health problems, are linked to processes and experiences that happen in very early childhood. It is not one single factor that starts a child on the path to adult disease and disorder, it is the interaction between their genes, the environment and the context in which they live and grow. Changing children’s environment and their context for the better offers a chance to improve the health and wellbeing of all children, not just in childhood but across their entire lifespan.
Solution
GenV is a ground-breaking national research and data asset, aiming to transform the health and wellbeing of children and parents. With two years of recruitment in every birthing hospital in Victoria complete, GenV has established an incredible cohort of 115,000 participants representing Australia’s rich social, cultural and geographic spectrum. This includes communities usually missed by traditional research methods such over 7,000 participants whose primary language spoken at home is not English (across 72 languages) and over 25,000 participants from regional Victoria.
This ambitious national initiative of international significance is creating a comprehensive research and data platform, guided by the concept of collecting population data once and using it many times. Multiple researchers can use GenV to identify patterns, enable trials and discover how to predict, prevent and treat health and wellbeing problems faster and better than we can today.
Translating this research to enhance the way health, education and social services are delivered will change the trajectories of children and parents for generations to come.
Investment required
AU$50,000,000 over five years Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
39 Prospectus 2024
Project 16
Genomics GenV Innovation Population Health
Children’s Wellbeing Continuum: Amplifying children’s voices and partnering with front-line clinicians
Problem
Childhood is a critical period to promote good mental health for both its immediate impact on quality of life and its lasting influence on children’s development. However, the Australian mental health system for children remains extremely fragmented, with many barriers preventing families from seeking timely and appropriate support for their children; it is a service system in urgent need of reform.
Traditionally, mental health has operated within a binary framework – the presence or absence of a mental illness based on diagnostic guidelines. However, this approach has been increasingly criticised for its limitations and contribution to ongoing service system barriers for parents and children, given it is a) inherently stigmatising and restrictive, and b) fails to address the reality of the fluid and often dynamic nature of the child’s mental health experiences.
Solution
Our researchers have developed the Children’s Wellbeing Continuum: an evidence-based, visual tool to support conversations about children’s wellbeing. The visual tool incorporates four ‘traffic light’ like colours and emojis to help describe a child’s wellbeing from Good through to Coping, Struggling and Overwhelmed. By enabling parents, teachers, healthcare providers and children to discuss and reflect on wellbeing (via a shared language), the Children’s Wellbeing Continuum can better support health literacy, and early identification and action when children are struggling.
Investment required
AU$132,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
40 Murdoch Children’s Research Institute Mental Health
Project 17
ADAPT: Transforming the lives of children afflicted with food allergies
Targeting all stages of allergy development, from prevention in infancy to managing existing allergies and fostering tolerance.
Problem
Australia’s unprecedented high rates of food allergies affect approximately one in every ten infants and present a major public health challenge. The current lack of effective treatment options, coupled with the standard practice of allergen avoidance, imposes considerable emotional and social stress on affected families and communities.
Solution
The ADAPT Program’s strategy is to shift the existing paradigm from merely managing allergies to actively promoting tolerance development in infants. Utilising a novel care model, it integrates dietitian and nurse-led interventions in the familiarity of the patients’ homes, complemented by digital tools like the AllergyPal app, offering a proactive solution to this widespread issue.
It combines the expertise of dietitians, nurses, and allergists to create a multidisciplinary approach. Focused on early interventions and telehealth support, the ADAPT Program strives to make classrooms allergy-free. ADAPT represents a beacon of hope, promising to significantly diminish the allergy burden and enhance family wellbeing.
The program’s pilot plans to enrol 300 infants, assessing the effectiveness and safety of its innovative approach. The primary objective is to establish a sustainable, scalable model that can be adopted nationwide, setting a new standard in allergy care.
The ADAPT Program is poised to significantly reduce the prevalence of food allergies among Australian children. By reshaping clinical practices and informing public health policies, it aims to enhance the lives of children with allergies, offering them a future free from the constraints and fears associated with food allergies
Investment required
AU$384,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
10 per cent of one year olds and one in 20 children aged between 10 and 14 years old, have a food allergy.
41 Prospectus 2024
Project
18
Population Health Allergy Education
Mental Health in Primary Schools: Support the national research strategy
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact. Project 19
Upskill experienced teachers to become Mental Health and Wellbeing Leaders. This will increase the capacity of primary schools to support the mental health and wellbeing of their students and ensure no child slips through the cracks.
Problem
Many children experience mental health issues. In Australia, around 13.6% of children between four and 11 years old have dealt with these issues in the past year which can lead to academic underachievement and missed classes. Despite available effective sources of help, children’s mental health issues are rising, especially post-COVID-19, and primary schools lack the support and resources to adequately address these escalating problems.
We know less about the problem than we should. A national coordinated process for gathering data on mental health and wellbeing in primary schools, and the development of bespoke tools to measure student, teacher and school based mental health and wellbeing outcomes, is critically needed.
Solution
Our Mental Health in Primary Schools (MHiPS) initiative, which includes having a Mental Health and Wellbeing Leader (MHWL) in every primary school, was successfully piloted in 100 Victorian Primary Schools and is now being rolled out across the state and expanding interstate. Over 90% of staff from participating schools agreed that the MHiPS initiative had increased whole-school capacity to support student mental health and wellbeing.
The next research phase requires a part-time Research Officer to help coordinate the development of a national research strategy and infrastructure to support the design, analysis, synthesis and dissemination of findings from the MHiPS project on a large scale. This will allow us to communicate the outputs of the project to as wide an audience as possible and to provide critical insights into the mental health and wellbeing of Australian children aged 5-12 years.
Investment required
AU$120,000
42 Murdoch Children’s Research Institute
Education Mental Health
Project 20
Victorian Collaborative Centre for Children’s Mental Health and Wellbeing
Problem
Good mental health in childhood is a crucial element in living a quality life. It contributes to a child’s ability to develop and maintain fulfilling relationships, adapt and cope in the face of adversity and ultimately reach their full potential over their lifespan.
When identified late or left untreated, child mental ill health is linked to poor social functioning, school dropout, substance abuse, unemployment, violence and suicide. The existing mental health system is unable to adequately support the sharp increase in frequency and severity of child mental health problems over the last decade, and the COVID-19 pandemic has exacerbated this issue.
Child mental health care differs from youth and adult approaches, with a child and family-centred perspective and early-intervention at its core.
Solution
The Centre for Child Mental Health and Wellbeing (‘The Centre’) is a virtual, state-wide Centre dedicated to informing the support of mental health and wellbeing of children aged 11 years and under. The Centre was catalysed by the Royal Commission into Victoria’s Mental Health System.
At its core, The Centre will embed the vital contribution of children, carers and families with lived and living experience of mental illness or psychological distress to:
• Support the implementation of child and family-centred care in a consistent way across the state.
• Generate evidence for prevention and early intervention and explore barriers and enablers to research translation.
• Train the current and future workforce to offer innovative, consistent, high quality, child and family-centred care in urban, regional and remote communities across Victoria.
• Focus on promoting mental health wellbeing across the tiers from prevention, treatment and care maintenance.
• Respond to equity and access by having a focus on those at-risk groups who experience barriers.
Investment required
AU$360,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
In Australia, one in 12 children aged four to 11 years have a diagnosed mental health disorder.
43 Prospectus 2024
Population Health
Education Mental Health

Meet Sangita and Maddie
Generation Victoria (GenV), one of the world’s largest parent and birth studies, is making significant strides in advancing the understanding and management of health outcomes for parents and children worldwide.
Among the thousands of Victorian families contributing to GenV is Sangita and her daughter, Maddie.
“I think it’s important for children’s health, now and later on, that we gather as much information from as many parents as possible. The more information researchers have, the more they can find. It’s important to get as many people as possible into this kind of study,” said Sangita.
GenV brings together information and samples already collected by services and combines them with parent-reported information, aiming to transform the health and wellbeing of an entire generation of Victorians – with inclusivity and equity at its core.
For Sangita, child health conditions such as autism and diabetes hold particular interest.
“For me personally, autism is something I’d really like to know more about – it’s something that there’s currently no way of knowing about until kids are slightly older. If there’s anything that could be done during pregnancy to identify if there’s an issue, that’s something I would like to see happen,” she said.
“Diabetes is the other condition because it’s hereditary in my family. I had gestational diabetes during my last pregnancy, so it would be good if there were ways to identify these types of conditions early on – before they become a bigger problem.”
To find out more about GenV, please visit: www.genv.org.au
Image: Mother Sangita holding daughter Maddie
44 Murdoch Children’s Research Institute


Infection, Immunity and Global Health
Vision
To improve the health and wellbeing of children by better understanding infections and their immune response, both in Australia and internationally, especially in less developed countries.
Leadership
“Our researchers are on the front lines, actively safeguarding children from avoidable threats like allergies, common infections, and immune conditions. Our concentrated efforts extend globally, with a particular dedication to disadvantaged populations, especially in low- and middle-income countries. We are committed to defending every child’s health, ensuring a practical impact where it matters most.”
 Professor Andrew Steer Director, Infection, Immunity and Global Health
Professor Andrew Steer Director, Infection, Immunity and Global Health
Story of discovery and impact
New rotavirus vaccine could save millions of babies worldwide
In 1973 in Melbourne, MCRI’s Professor Ruth Bishop AC identified rotavirus as the cause of severe gastroenteritis.
Years later, a safe rotavirus vaccine enabled gastroenteritis wards in Australian hospitals to close, but worldwide the diarrhoeal disease still kills almost 250,000 children aged under five every year.
Find out more

46 Murdoch Children’s Research Institute
Zero Dose Child: Improving vaccine uptake across the lifespan and around the world
Develop and assess targeted community-led vaccine communication and communityengagement programs to boost vaccine confidence, trust and uptake in the Asia-Pacific region, with a focus on areas with high ‘zero-dose children’ rates.
Problem
The pandemic has disrupted routine childhood immunisation, leaving global coverage at its worst level since 2008. Between 2019-2021, 67 million children globally missed out on routine vaccines. This has sadly resulted in greater rates of preventable diseases in children such as nine million measles cases and over 100,000 deaths in 2021. Of most concern, there were 48 million zero-dose children who received no vaccines during this time, and they account for more than half of the vaccine preventable deaths.
Finding children who missed vaccines during the pandemic and restoring immunisation confidence and coverage in the Asia-Pacific region are critical priorities for global health organisations, with WHO and global partners making an urgent call to catch-up children who missed vaccines during COVID-19, restore routine immunisation coverage and strengthen primary health care.
Solution
At MCRI, we have internationally recognised expertise in risk communication and the social, behavioural and equity aspects of vaccination in Australia and the region. Working closely with UNICEF and local country partners, we have spent two years developing and evaluating tailored communication and community engagement programs to increase vaccine confidence and uptake in Fiji, Tonga and Vietnam. Our current priority areas are the Philippines and Indonesia, where rates of zero-dose children are high.
Philippines
We are currently completing a study with the University of the Philippines to understand the barriers to vaccine uptake in three low coverage regions. Using data, we will co-design a vaccine education and communication program for trained and lay health workers, and pilot the intervention in a lowcoverage region. To achieve sustainable implementation and integration with other primary healthcare programs, we need to ensure the effectiveness and cost-effectiveness of the program. We are seeking support to evaluate this vaccine education and communication program for trained and lay health workers in a cluster randomised controlled trial in three low coverage regions to improve uptake and ascertain effective implementation factors to reduce zero-dose children.
Indonesia
In Indonesia, we are currently partnering with UNICEF and the University of Gadjah Mada to develop and pilot a train-the-trainer vaccine education and communication intervention.
This intervention will target health workers, religious leaders and youth leaders to address vaccine hesitancy and drive demand in 10 low-coverage provinces. The inclusion of religious and youth leaders is novel and needed in Indonesia. With additional funding, we can conduct a hybrid study that blends design components of clinical effectiveness and implementation research to enable more rapid translational gains, more effective implementation strategies, and more useful information for decision makers. This hybrid study would allow simultaneous testing of the clinical intervention (through an RCT) and implementation strategy (using an implementation science framework including economic data) to optimise scale up and sustainability of this program.
Investment required
AU$1,740,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
One in five children worldwide are now zerodose or under-vaccinated. In the Asia-Pacific region; the Philippines, Indonesia and Vietnam are among the top 20 countries with the largest numbers of zero-dose children.
Zero-dose children account for more than half of the vaccine preventable deaths.
47 Prospectus 2024
Project 21
Education Global Health Infection Vaccines
Infection, Immunity and Global Health
Project 22
Preschool Wheeze: solutions for preschool wheeze management
Changing the way preschool wheezing is diagnosed, treated, and managed at The Royal Children’s Hospital (RCH), extending its impact nationally and internationally.
Problem
Wheezing in preschool children is a prevalent health issue, affecting nearly half of this age group. It is a leading cause of emergency department visits and hospital admissions, with a high frequency of re-admissions, particularly among children aged three to five years. The current “one size fits all” management strategies are significantly outdated, not reflecting the diverse nature of wheezing in young children. This has led to sub-optimal care and outcomes, highlighting a critical need for a revised approach that considers the distinct clinical characteristics and underlying causes of preschool wheezing.
Solution
The Wheeze Wise Kids group represents a groundbreaking consortium approach, aiming to harness the collective expertise and resources available at RCH, the Murdoch Children’s Research Institute (MCRI), and the University of Melbourne. The strategy is multifaceted, focusing on the development of personalised treatment pathways, the implementation of healthcare improvements, the introduction of novel treatments, and an overall reduction in hospital admissions and readmissions. This comprehensive solution involves conducting multiomic studies, establishing novel trial platforms, creating new data linkages, and developing targeted health services programs for vulnerable populations.
This initiative seeks to address the significant challenge of managing preschool wheeze more effectively and efficiently, delivering significant improvements in the management of preschool wheezing and ultimately setting a new standard of care that could be adopted worldwide.
Investment required
AU$180,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
48 Murdoch Children’s Research Institute
Global Health Respiratory
Infection-X Research Platform: Data and research solutions for infectious diseases
Rapidly analyse and respond to emerging infectious diseases in children, integrating real-time clinical data, biosample analysis, and cutting-edge research to inform clinical and policy decisions.
Problem
Infections are the leading cause of paediatric hospital admissions globally, with respiratory viruses like Influenza and Respiratory Syncytial Virus (RSV) causing significant morbidity. Despite the prevalence, there remains a substantial gap in our understanding of these infections’ immune responses, clinical profiles, and the impact of vaccinations, especially in the postCOVID-19 era. This project aims to fill these critical knowledge gaps by collecting and analysing data on these diseases in real-time.
Solution
The Infection X platform proposes an innovative solution to tackle infectious diseases through a multifaceted approach: a real-time electronic medical record tracking system, a prospective clinical data repository, and a biosample research repository. By leveraging The Royal Children’s Hospital Electronic Medical Record, the platform will enable near-instantaneous analysis of hospitalizations and clinical data, crucial for understanding and preparing for diseases of interest and future pandemics.
This comprehensive platform will not only describe current and emerging infectious diseases but also facilitate an advanced understanding of immune responses, especially in light of new vaccines for RSV, Human metapneumovirus (HMPV), and parainfluenza virus. A research team is needed to collect and analyse data, offering immediate insights into infection patterns and vaccine efficacy.
The anticipated impact is significant. We expect the platform to influence clinical practice and policy by providing real-time data on infection trends, vaccine responses, and clinical outcomes. This will enhance our ability to identify atrisk children and tailor interventions more effectively.
Investment required
AU$180,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
49 Prospectus 2024
Project
23
Infection, Immunity and Global Health Global Health Innovation
Project 24
Saving precious lives: Addressing Pneumonia in the Asia-Pacific region
Addressing the urgent issue of childhood illness and death caused by Streptococcus pneumoniae (pneumococcus) in the Asia-Pacific region.
Problem
Pneumonia is the single largest infectious cause of death in children worldwide. Streptococcus pneumoniae is a common cause. Although pneumococcal vaccines have been available for over 20 years half of the world’s children remain unvaccinated.
Nearly half of all pneumonia deaths occur in the Asia-Pacific. The Asia-Pacific region has extremely high levels of antibiotic resistance, making treatment a challenge and underscoring the importance of preventing disease through vaccination.
Solution
Across the Asia-Pacific region we are leading a broad program of work. Discoveries or new methods uncovered in one region can be rapidly translated into other countries. Investment is needed to drive our programs forward and accelerate progress.
Our most urgent priorities in our program are:
Papua New Guinea
We have access to a unique sample set from children with pneumonia, their contacts and caregivers from Papua New Guinea. In this project we will apply state-of-
the-art microbiology including whole-genome sequencing. From one data set we will be able to address critical questions to understand pneumococcal transmission, identify the most appropriate population and tools for monitoring vaccine impact, and assess the impact of vaccine introduction on the pneumococcal population over time including the emergence of non-vaccine types and antimicrobial resistance. We are currently undertaking wholegenome sequencing with existing funding but are seeking support to undertake the analysis and experimental components.
Mongolia
We will use cutting-edge microbiology to monitor the longterm changes in pneumococci occurring following vaccine introduction, to look at the success of vaccination and to inform future vaccine design. This data will provide the first long-term pneumococcal carriage data from the region, inform policy makers in Mongolia and in similar settings regarding the benefits of long-term use of this vaccine.
Vietnam
Application of a novel immune assay to measure long-term protection from reduced dose schedules of pneumococcal vaccines.
We will apply our novel flow cytometric assay to measure pneumococcal serotype-specific B cell response as a marker of longterm protection following reduced dose Pneumococcal Conjugate Vaccine schedules in Vietnam.
Fiji
Although vaccines are one of the most effective ways to save lives, there many important microbes for which there is no safe and effective vaccine available. Therefore, we are testing a new approach to prevent maternal and newborn bacterial infections. To investigate simple and low-cost approaches to prevent maternal and newborn infections, we have undertaken a randomised controlled trial to measure the effect of a single oral dose of Azithromycin antibiotic given to women in labour. Now, we will extend this work by testing previously collected samples to understand the effect of Azithromycin on the bacteria and microbiome of mothers and their babies.
Investment required
AU$1,560,000
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
Pneumonia has been estimated to cause ~800,000 deaths in children aged under five years annually, and the majority occurring in lowincome countries.
50 Murdoch Children’s Research Institute
Global Health Infection Respiratory
Vaccine equity with a focus on the Asia-Pacific: Developing the Centre for Vaccine Research, Policy and Practice
Improve Australian and global health outcomes through equitable access to existing vaccines and the development of new vaccines – with a special focus on the Asia-Pacific.
Problem
Infants, children, adolescents and people of all ages continue to suffer from vaccine preventable diseases due to:
• Suboptimal access and acceptance of existing vaccines including pneumococcal, typhoid, human papillomavirus vaccine, rotavirus, Bacille Calmette-Guerin, measles and rubella, COVID-19, dengue, influenza vaccines; and
• A lack of new vaccines for priority pathogens and that prevent antimicrobial resistance including respiratory syncytial virus, group B streptococcus, group A streptococcus, cytomegalovirus, enteric diseases, emerging pathogens and others.
Solution
A Centre for Vaccine Research, Policy and Practice, with worldleading research underpinned by strong state-wide government and community, regional and global partnerships, will deliver a sustainable impact on the unique needs of people of all ages in Victoria, Australia and across the Asia- Pacific.
The Centre will work in partnership with the Australian Institute for Infectious Disease (AIID) in the Melbourne Biomedical Precinct. Strategic alignment with the AIID and the state’s recent investment in new vaccine development, will be key to accelerating Australia’s preparation and response to infectious disease challenges. Together, they expand the breadth of vaccine research and offer a united voice in real-time – that will be integral to informing policy and decision making, particularly within the proposed federal Centre for Disease Control (CDC).
The Centre’s first mission is to identify how we can use existing partnerships and Victorian data to build confidence and inform decision-making for a united research strategy across Melbourne Biomedical Precinct partners and key national stakeholders on the unique needs of children and families across Victoria and the Asia-Pacific.
Investment required
AU$420,000-AU$1,000,000 (depending on scope)
Some research projects will require additional funding for future phases of the research and can be scaled up to have an even greater impact.
51 Prospectus 2024
Project 25
Infection, Immunity and Global Health Education Global Health Infection Vaccines

Meet Gursirat
Sandeep Kaur’s daughter, Gursirat, 1, spent almost two months in intensive care after contracting a Strep A infection.
“Gursirat had a mild fever, but otherwise was fine, so we gave her pain relief and kept an eye on her,” Sandeep said.
“But three days later she fell suddenly very ill. Her hands, lips and feet turned blue and her skin was discoloured,” Sandeep said.
After being admitted to the hospital, Gursirat’s condition worsened. She was diagnosed with kidney failure, a liver infection, and necrosis on seven of her fingertips, all linked to the Strep A infection.
“It was such a difficult time, our baby had drains in her leg, two operations and required dialysis for 12 days. Thankfully, her fingertips were saved but she is yet to fully recover. I hope that a vaccine can be made for Strep A so no other child has to endure this.”
Professor Steer, MCRI’s Director of Infection, Immunity, and Global Health, along with his team, is testing candidate Strep A vaccines developed by researchers in Australia and overseas in a groundbreaking human challenge model, a first of its kind.
Image: Gursirat, age 1
52 Murdoch Children’s Research Institute


Murdoch Children’s Research Institute
Together we can shape the future
Board of Directors
Patrick Houlihan (Chair)
Sarah Murdoch (Co-Chair)
Miffany Blythe
Brandon Carp
Steven Casper
Prof Jane Gunn
Bernadette McDonald
Rajeev Natarajan
Prof Kathryn North AC
Paul Rayner
Simon Rothery
The Hon Nicola Roxon
Dominic Stevens
Andrew Wilson
Development Board
Miffany Blythe (Chair)
Trent Blacket
Georgia Danos
Tanya Hamersfeld
Zara Hines
Vas Katos
Clark Kirby
Tahli Koch
Tamara Lasky
Peter Mastos
Kaajal Prasad

Global Advisory Board
Sarah Murdoch (Chair)
Trent Blacket
Miffany Blythe
David Calvert-Jones
Suzi Carp AO
Sue Collyns
Sarah Harden
Tristen Langley
Chelsey Martin
Kate Mohr
Katie O’Reilly
Erica Packer
Nicholas Stone
Lauren Thurin
Global Ambassadors
Suzi Carp AO
Sarah Murdoch
Council of Ambassadors
The Honourable Dame
Quentin Bryce AD CVO
Janet Calvert-Jones AO
Paula Fox AO
Jean Miller
Kathryn North AC
Lady Primrose Potter AC
Jeanne Pratt AC
Frances Underwood
Prospectus 2024
Areas of interest
Allergy 39
Brain 22, 23, 29, 33
Cancer 22, 23
Clinical Sciences 29, 30, 31, 32, 33
Diabetes 31
Diversity and Inclusion 15
Education 30, 39, 40, 41, 45
Equipment 22, 23
Genomics 15, 16, 17, 18, 19, 37
GenV 37
Global Health 19, 45, 46, 47, 48, 49
Heart 26
Infection 45, 48, 49
Innovation 18, 23, 25, 37, 47
Kidney 24
Mental Health 38, 40, 41
Rare Disease 15, 16, 19
Respiratory 32, 46, 48
Stem Cell Medicine 22, 23, 24, 25, 26, 31, 33
Vaccines 45, 49
Image: Kidney tissue made from stem cells using 3D bioprinting. It contains tangled tubes known as nephrons which are important parts of the kidney for filtering blood and keeping the body healthy.
Credit: Ker Sin Tan and Jessica Vanslambrouck (Kidney Regeneration group –Prof Melissa Little)
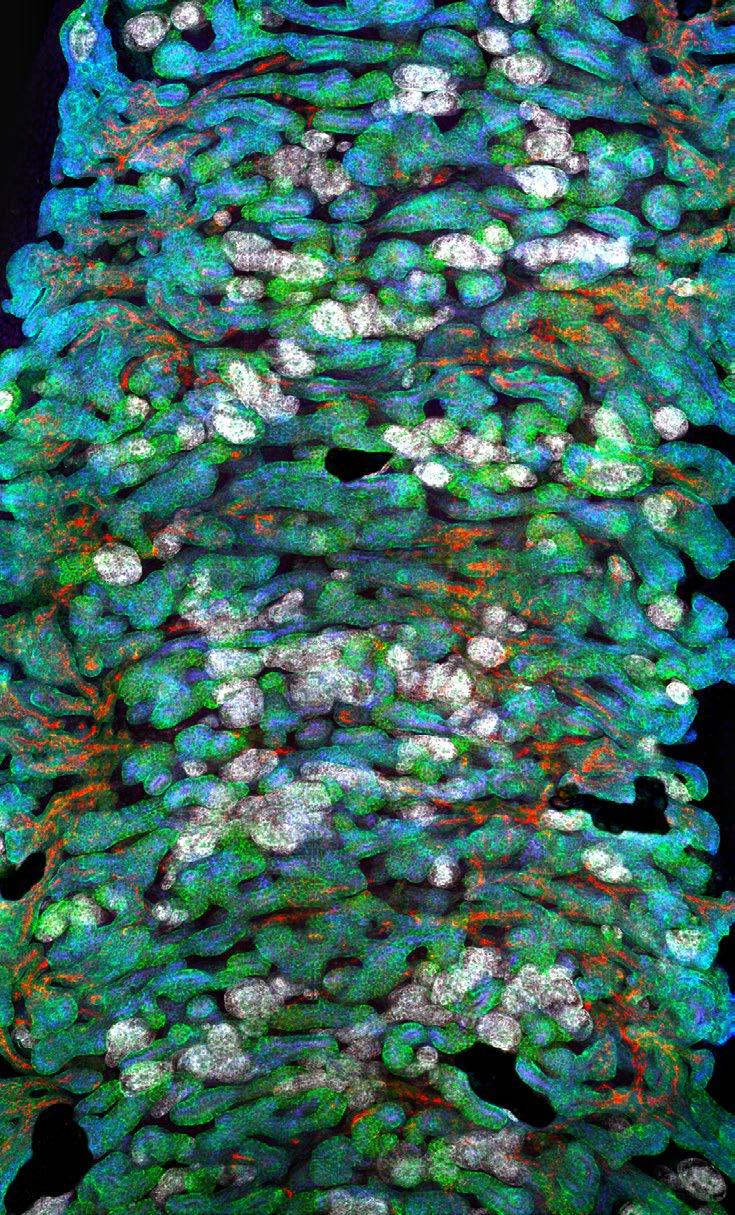
56 Murdoch Children’s Research Institute
Contact us
We would love to learn more about you and how we might work together to deliver ground-breaking research that has a long-lasting, positive impact. To discuss further, please contact:
Engagement and Philanthropy
E philanthropy@mcri.edu.au
T +61 3 9936 6362
Engagement and Philanthropy leadership

Matthew
Hannan Director, Engagement and Development
 Rebecca Harford Head of Philanthropy
Rebecca Harford Head of Philanthropy

Thank you to all the children who participated in our ‘Children at the Heart’ photo shoot, images of which have been incorporated throughout this prospectus.


Murdoch Children’s Research Institute The Royal Children’s Hospital
50 Flemington Road, Parkville Victoria, 3052 Australia mcri.edu.au












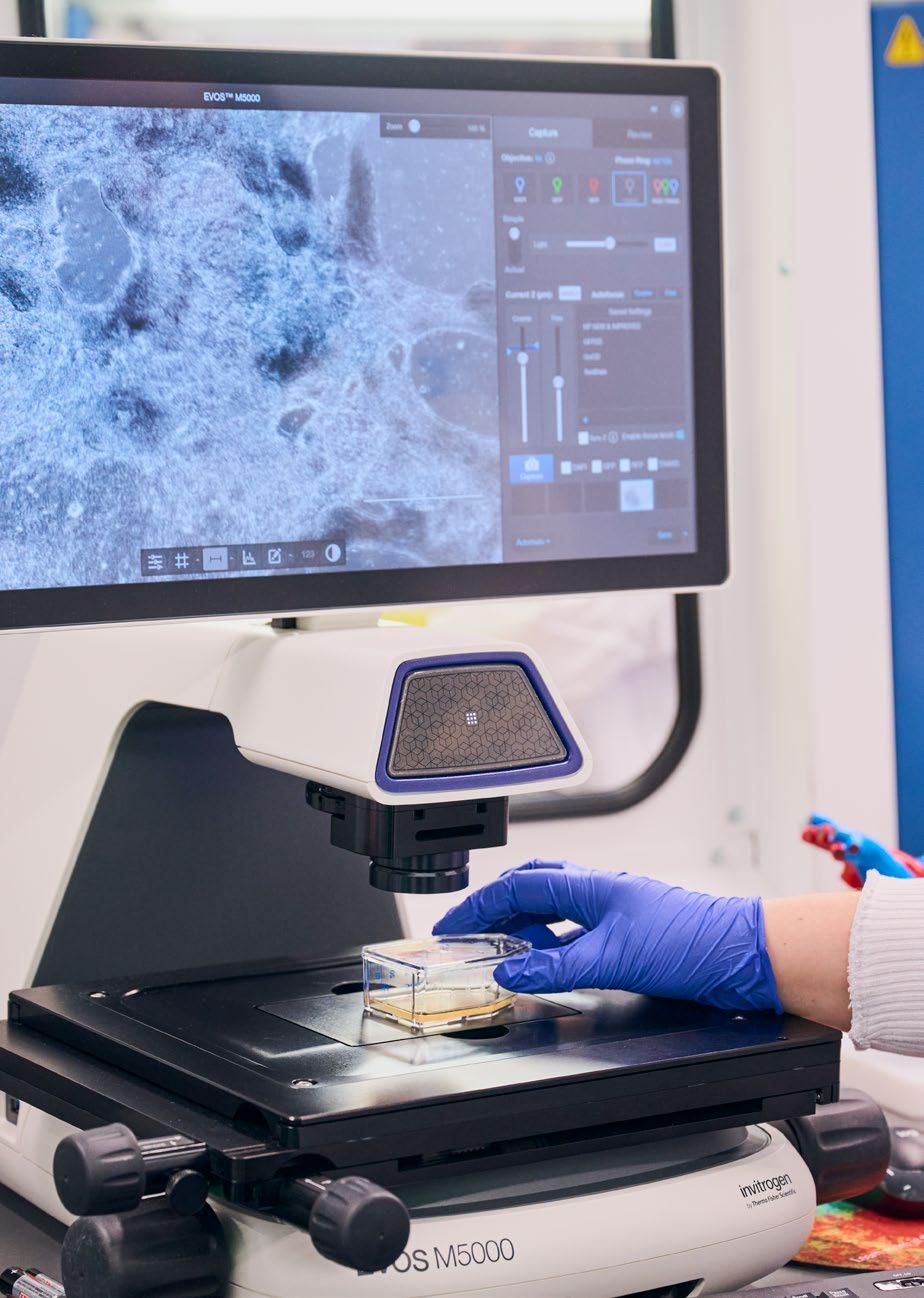





 Image: Professor David Thorburn (left) and researcher (right) with Eli (middle left) and Evie (middle right).
Image: Professor David Thorburn (left) and researcher (right) with Eli (middle left) and Evie (middle right).

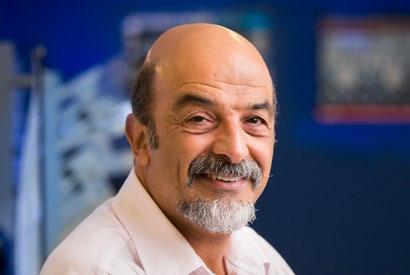 Professor John Christodoulou Director, Genomic Medicine
Professor John Christodoulou Director, Genomic Medicine

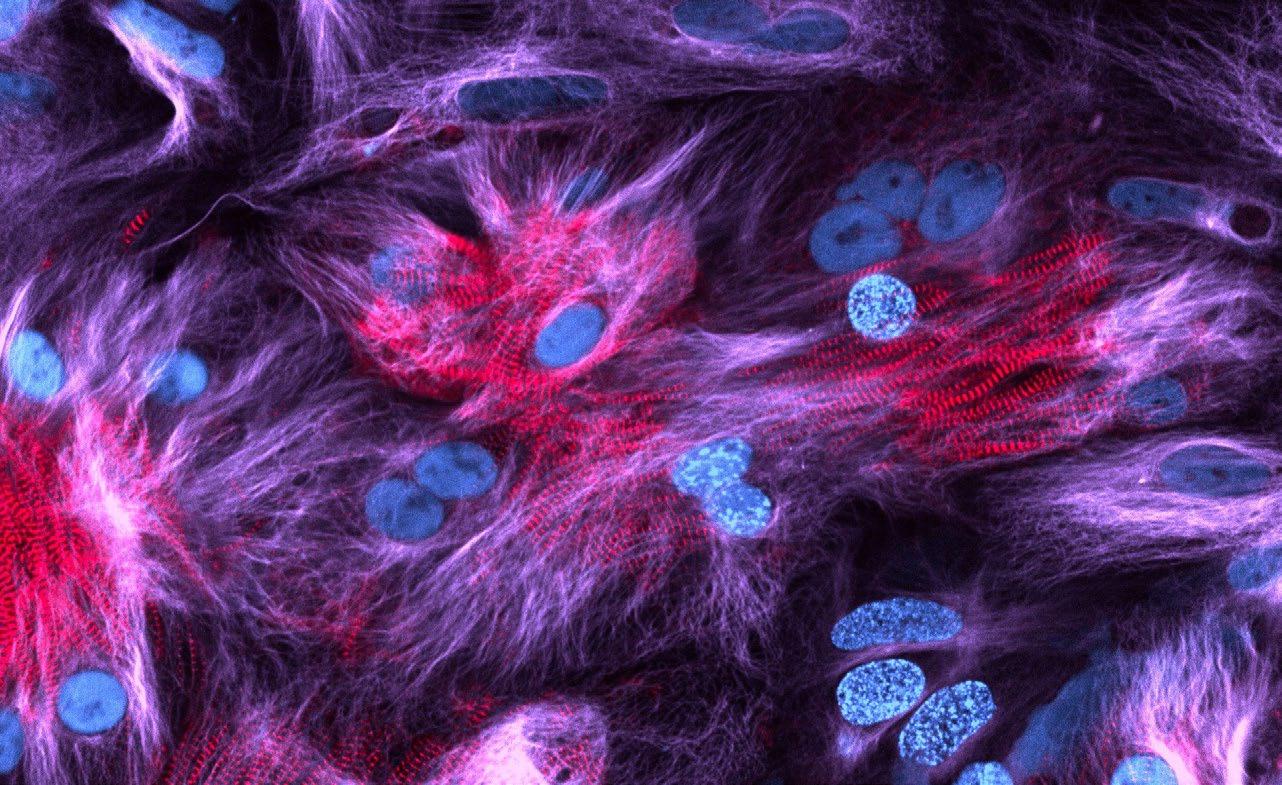
 Professor Enzo Porrello Director, Stem Cell Medicine
Professor Enzo Porrello Director, Stem Cell Medicine


 Professor Vicki Anderson Director, Clinical Sciences
Professor Vicki Anderson Director, Clinical Sciences
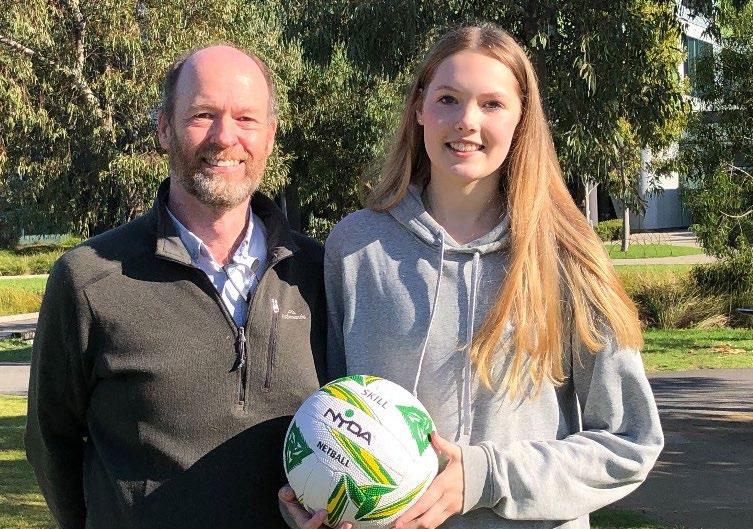


 Professor Sharon Goldfeld Director, Population Health
Professor Sharon Goldfeld Director, Population Health



 Professor Andrew Steer Director, Infection, Immunity and Global Health
Professor Andrew Steer Director, Infection, Immunity and Global Health




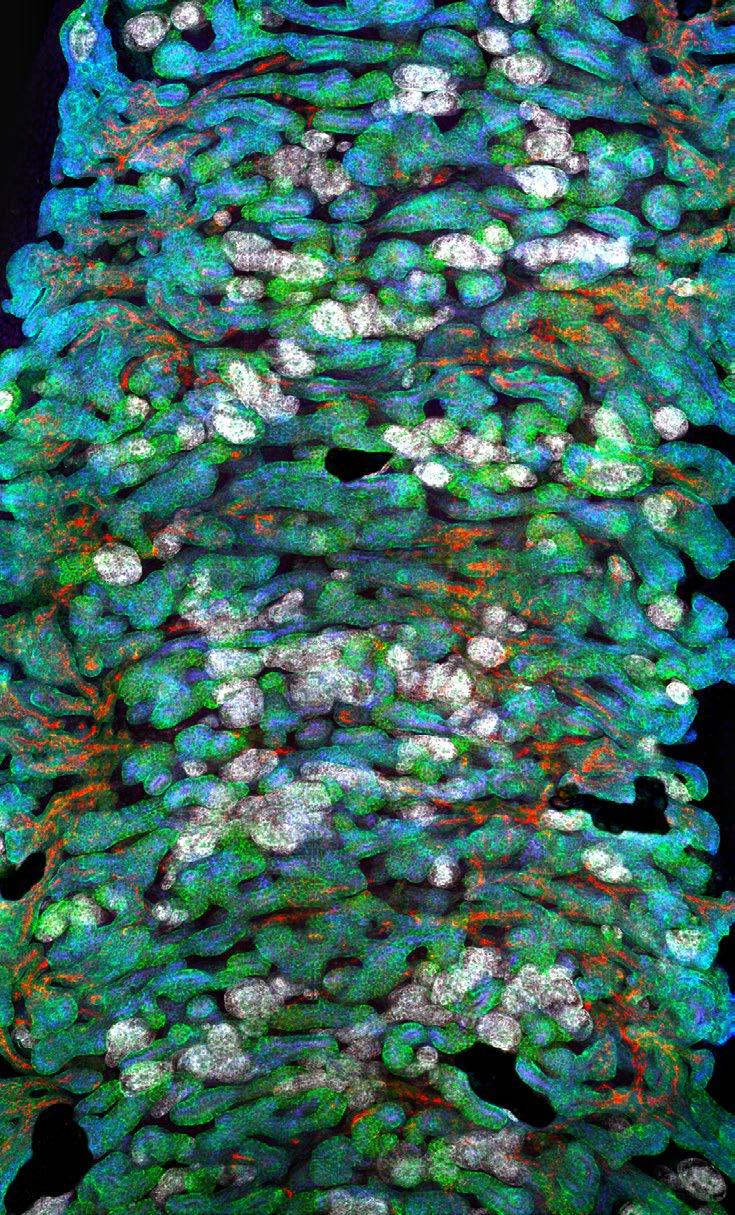

 Rebecca Harford Head of Philanthropy
Rebecca Harford Head of Philanthropy

