

Transcatheter mitral valve repair with MitraClip
REDUCING DEATH AND HEART FAILURE HOSPITALIZATION
By Ahmad Edris, MD

The management of valvular heart disease has advanced significantly in recent years with transcatheter interventions emerging as a viable alternative to traditional surgical approaches. Transcatheter aortic valve replacement (TAVR) is a wellestablished, transformative technology that has enabled the treatment of a spectrum of aortic stenosis patients from appropriately selected low-risk to very complex high-risk patients.
The mitral valve is significantly more complex. Disorders of the mitral valve can involve the mitral valve leaflets, annulus, or subvalvular apparatus, including the left ventricle. It is crucial for a valve program to have physician expertise in understanding the mechanism of the dysfunction through advanced imaging technology to appropriately treat patients.
Transcatheter edge-to-edge repair of the mitral valve (m-TEER) with MitraClip has evolved significantly with expanding operator experience and device iterations since the FDA first approved the device in 2013 based on the EVEREST trials (1, 2). MitraClip has become an increasingly common technique for treating patients with severe degenerative and functional mitral regurgitation (MR).
The latest MitraClip G4 platform, with expanded clip sizes, has enabled successful treatment of a broader range of pathologies. In cases of degenerative or primary MR, it is essential to provide patients with a result close to surgical outcomes, achieving a reduction in MR severity to mild (1+) or less.
Montage Health has a significant patient population with severe
It is important for our heart team, which includes cardiac surgeons, cardiologists, and nurse practitioners, to appropriately select patients for the best treatment.
doses of guideline-directed medical therapy and cardiac resynchronization therapy if appropriate(3). Patients who underwent MitraClip experienced a significant reduction in heart-failurerelated hospitalizations and lower all-cause mortality within 24 months of follow-up compared to those on medical therapy alone. These benefits were sustained through five years of follow-up(4).
A significant number of patients on the Monterey Peninsula could benefit from this technology that is being offered at Community Hospital of the Monterey Peninsula. For any questions or referrals for treatment, please contact Dr. Ahmad Edris, Director of the Structural Heart Disease Program, at (831) 241-9200 or Elizabeth Vitanza, Structural Heart Coordinator, at (831) 625-4536.
REFERENCES
1. Feldman T et al. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial
EVEREST cohort. J Am Coll Cardiol 2009;548:686-694
2. Feldman T et al. Percutaneous repair or surgery for mitral regurgitation. N Eng J Med 2011;364:1395-1406
3. Stone GW et al. Five-year follow-up after transcatheter repair of secondary mitral regurgitation. N Engl J Med 2023;388:2037-2048
4. Stone GW et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med 2018;379(24):2307-2318
degenerative MR that may be better served by MitraClip rather than surgery. It is important for our heart team, which includes cardiac surgeons, cardiologists, and nurse practitioners, to appropriately select patients for the best treatment.
Additionally, patients with congestive heart failure and severe functional or secondary MR (caused by ventricular or atrial disease rather than mitral leaflet pathology) are being evaluated by our heart failure team and may be referred for MitraClip if they continue to have severe MR and symptoms despite optimized medical therapy.
The landmark COAPT trial evaluated patients with heart failure and reduced ejection fraction (EF of 20–50 percent) who had at least moderate-to-severe (3–4+) MR and remained symptomatic (at least NYHA class II) despite maximal
Vascular
surgery program at
Community
Hospital of the Monterey Peninsula
By Emaad Farooqui MD, MHA, RPVI, FSVS
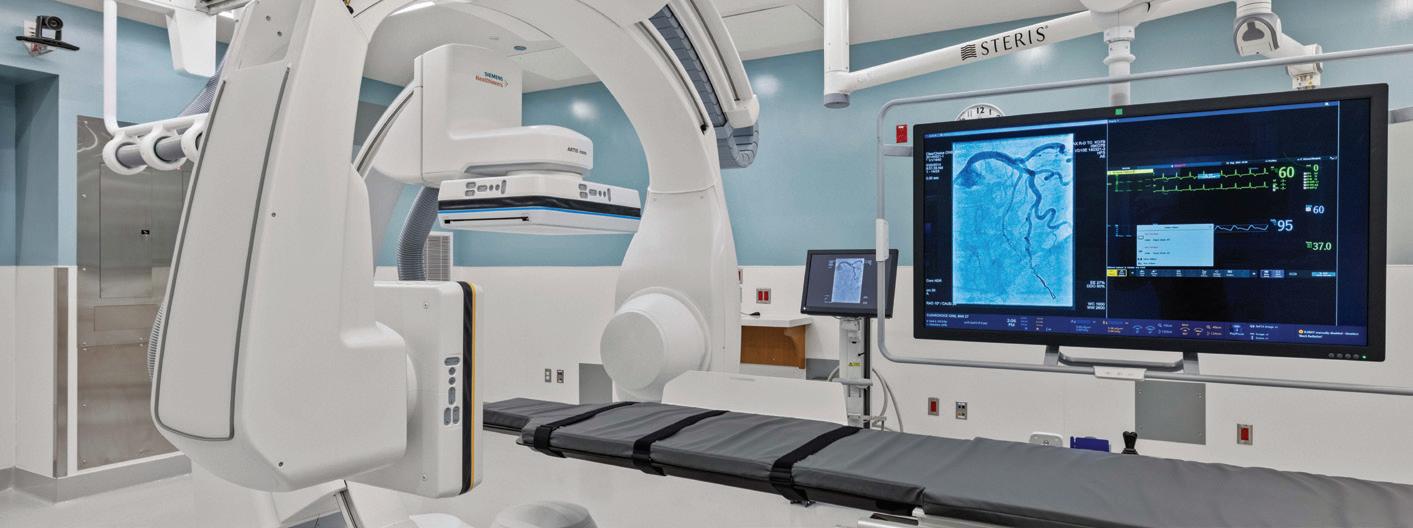
Endovascular surgery is a minimally invasive technique using X-ray imaging to treat various vascular conditions involving arteries and veins throughout the body. This innovative approach has revolutionized the treatment of both standard and complex vascular diseases including arterial aneurysms, peripheral arterial disease (PAD), carotid stenosis, and venous disorders. Vascular surgery encompasses both traditional open surgical techniques in addition to minimally invasive endovascular surgeries.
Endovascular procedures offer numerous advantages over traditional surgical methods. Patients often experience reduced pain, shorter hospital stays, decreased operative time under anesthesia, and faster rehabilitation. The minimally invasive nature of these procedures generally leads to fewer complications such as pain, infections, or significant blood loss. Additionally, endovascular techniques can be performed under local anesthesia or sedation, further enhancing patient comfort.
For conditions such as abdominal aortic aneurysms (AAA), endovascular aneurysm repair (EVAR) has become the gold standard for repair in most of the patient population and is now at the forefront of treating complex thoracic and abdominal aortic repairs. We plan to bring the ability to treat complex thoracic and abdominal aortic disease using fenestrated aortic endografts which broadens the patient population that can benefit from minimally invasive treatments. Our vascular surgery program will also provide minimally invasive methods of treating carotid stenosis
to reduce overall stroke risk. We will be able to offer patients both traditional carotid endarterectomy in addition to a newer and less invasive approach known as transcarotid artery revascularization (TCAR) which is a hybrid operation that involves placing a carotid stent through a small incision above the collarbone. This has allowed high-risk patients who were not candidates for carotid endarterectomy to undergo carotid interventions that reduce stroke risk.
TCAR has shown to result in a 12-fold decrease in nerve injury, decreased risk of perioperative myocardial infarctions, and shorter anesthesia time, with equal stroke rate compared to carotid endarterectomy.
Endovascular options may not always be the optimal treatment for your patients long-term, and it is best to refer them to a vascular surgeon to
decide what treatment approach they would benefit from most.
SERVICES THAT THE VASCULAR PROGRAM WILL OFFER
n Dialysis access surgery
n Carotid surgery (open and minimally invasive)
n Minimally invasive treatment of thoracic aortic dissections and aneurysms
n Minimally invasive treatment of complex abdominal aortic aneurysms
n Limb salvage operations in patients who have failed open bypass surgery in addition to failed endovascular management
n Treatment and management of venous diseases (May-Thurner syndrome, DVTs, venous insufficiency, varicose veins, etc.)
n Minimally invasive treatment of mesenteric ischemia and acute limb ischemia
As technology continues to advance, vascular and endovascular surgery is likely to evolve further. Innovations such as enhanced imaging techniques alongside lower-profile medical devices promise to improve precision and outcomes for our patients.
Both open and endovascular surgery options are vital components of modern vascular care. By combining advanced technology with a multidisciplinary approach, these programs offer patients effective treatment options that can significantly improve their quality of life.
Please feel free to contact me directly if you have questions.
Emaad Farooqui MD, MHA, RPVI, FSVS emaad.farooqui@ montagemedicalgroup.org (818) 554-1773
We will be able to offer patients both traditional carotid endarterectomy in addition to a newer and less invasive approach known as transcarotid artery revascularization (TCAR).
