Successfulblindlungisolationwiththeuse ofanoveldouble-lumenendobronchialtube inapatientundergoinglungtransplantation withmassivepulmonarysecretion
Acasereport
YijunSeo,MDa,b,NamoKim,MD,PhDa,b,HyoChaePaik,MD,PhDc,DaheePark,MDa, YoungJunOh,MD,PhDa,b,∗
Abstract
Rationale: Preciselungisolationtechniquewithvisualconfirmationisessentialforthoracicsurgeriestocreateasafeandclear surgical field.However,incertainsituations,suchaswhenpatientshavemassivepulmonarysecretionorwhenthe fiberoptic bronchoscopy(FOB)isnotapplicable,lungisolationhasbeenperformedblindly.
Patientconcern: A52-year-oldwoman,whoseairwaywasunabletovisualizewithFOBduetomassivepulmonarysecretion, waspresentedforbilateralsequentiallungtransplantation.Extracorporealmembranousoxygenation,tracheostomy,andmechanical ventilationwereappliedtothepatientfor39dayspreoperativelyasabridgeforlungtransplantation.
Diagnosis: Patientwasdiagnosedwithanidiopathicpulmonary fibrosisandobesity.
Intervention: Initially,height-basedblindpositioningwithaconventionaldouble-lumenendobronchialtube(DLT)failedtoventilate thepatientproperly,andtheconfi rmationofDLTpositioningwithFOBwasimpossibleduetomassivepulmonarysecretion. Therefore,anovelDLT(ANKORDLT)thathasonemorecuff,locatedatapointbetweenthedistalopeningofthetracheallumenand thestartingpointofbronchialcuff,thanconventionalDLTwasusedforthelungisolationinthepatient.
Outcomes: Afterthecompletionoflunggraft,FOB findingshowedthattheANKORDLTwasoptimallypositionedatthe tracheobronchialtreeofthepatient,anditsdepthwas2.5cmshallowerthanthatoftheconventionaltube.
Lessons: ANKORDLTwouldbeafeasiblechoicetoachievesuccessfulblindlungisolationwhentheuseofFOBisimpossibleto achievetheoptimallungisolation.
Abbreviations: DLT = double-lumenendobronchialtube,ECMO = extracorporealmembraneoxygenation,FOB = fiberoptic bronchoscopy,POD = postoperativeday.
Keywords: airwaymanagement,idiopathicpulmonary fibrosis,lungtransplantation,one-lungventilation
1.Introduction
Preciselungisolationtechniqueisessentialforthoracicsurgeries tocreateasafeandclearsurgical field.Idealpositioningof
Editor:N/A.
Funding:Notapplicable.
YJOhasthepatentonthedesignofANKORTM double-lumenendobronchial tube,andlicenceditouttoInsungMedical.Co.Otherauthorshavenoconflicts ofinterest.
a DepartmentofAnesthesiologyandPainMedicine, b AnesthesiaandPain ResearchInstitute, c DepartmentofThoracicandCardiovascularSurgery,Yonsei UniversityCollegeofMedicine,Seoul,SouthKorea.
∗ Correspondence:YoungJunOh,DepartmentofAnesthesiologyandPain Medicine,AnesthesiaandPainResearchInstitute,YonseiUniversityCollegeof Medicine,(03722)50-1Yonsei-ro,Seodaemun-gu,Seoul,SouthKorea (e-mail:yjoh@yuhs.ac).
Copyright © 2019theAuthor(s).PublishedbyWoltersKluwerHealth,Inc. ThisisanopenaccessarticledistributedundertheCreativeCommons AttributionLicense4.0(CCBY),whichpermitsunrestricteduse,distribution,and reproductioninanymedium,providedtheoriginalworkisproperlycited. Medicine(2019)98:33(e16869)
Received:21February2019/Receivedin finalform:17June2019/Accepted: 24July2019 http://dx.doi.org/10.1097/MD.0000000000016869
double-lumenendobronchiallumen(DLT)hasbeenconfirmed by fiberopticbronchoscope(FOB).[1,2] Alternatively,blindlung isolationtechnique,suchasthelungcompliance,[3] bronchialcuff pressurechange,[4] orheight-basedassumption,[5] hasbeenused whenFOBisunavailableornotapplicableincertainsituations. Here,wereportthesuccessfulblindlungisolationbyusinga novelDLTwhichhasonemorecuffthantheconventionalDLT, developedbyoneoftheauthors,inapatientundergoinglung transplantationwithmassivepulmonarysecretion.Thiswouldbe the firstreportdescribingtheclinicaluseofanovelDLTinthe literature.Writteninformedconsentforthepublicationofthe clinicaldetailsandclinicalimagewereobtainedfromthepatient postoperatively.
2.Casereport
A52-year-oldwoman(height159cm,weight94kg)with idiopathicpulmonary fibrosisandobesitywaspresentedfor bilateralsequentiallungtransplantationwithrightlunggraft first underextracorporealmembraneoxygenation(ECMO).Preoperativepulmonaryfunctiontest(%,predicted)showedforced expiratoryvolumein1second,0.88L(37%);forcedvital capacityin1second,0.92L(30%);forcedexpiratoryvolume
in1second/forcedvitalcapacity,95%;anddiffusingcapacity ofcarbonmonoxide,8.3L/mmHg/min(28%).Veno-venous ECMO,tracheostomy,andmechanicalventilationwere appliedtothepatientfor39dayspreoperativelyasabridge forlungtransplantation.Preoperativechestradiography showedseverediffuselungconsolidations(Fig.1A).Preoperativecardiacechocardiographyshowedreducedrightventricle systolicfunction,mildpulmonaryhypertension(rightventricularsystolicpressure47mmHg),D-shapedleftventriclewith slightlydecreasedleftventriclesystolicfunction(ejection fraction56%).
Theanesthesiawasinducedwithmidazolam3.0mg, sufentanil50 mg,androcuronium50mg.Initially,a35Fr left-sidedDLT(Shiley,Covidien,Mans fi eld,MA)wasinserted viaoralrouteforlungisolationandblindlyplacedat28.5cm depthatthelevelofupperincisorofthepatientaccordingtothe height-basedblindpositioningofDLT.[5] However,bothlungs wereunabletoventilate,andthecon firmationforthe positioningofDLTwithFOB(FIVE4.0,KarlStorz,Tuttlingen, Germany)wasimpossibleduetomassivepulmonarysecretion (Fig.1B).Despitetheefforttosuckoutthepulmonarysecretion withthesuctioncatheterandFOB,anyanatomicstructuresof tracheobronchialtreewereinvisible.Wedecidedtouseanew DLT(ANKOR,InsungMed,Wonju,SouthKorea)ofleft-sided 35Fr(Fig.2A).Afterthecarinalcuffofthetubepassedthrough thevocalcordofthepatient,thetubewasturnedtoleftside,and carinalcuffwasinfl atedwith6mLofair(Fig.2B).Thetubewas advancedfurthertowardleftmainbronchus,anditstoppedat 26.0cmofdepthatthelevelofupperincisorofthepatient.After thede fl ationofthecarinalcuff,thetrachealcuffandthe bronchialcuffofthetubewereinfl atedwith5and2mLofair, respectively(Fig.2C).Afterthecompletionofrightlunggraft, bronchoscopic findingshowedthatthetubewasproperly positionedatthetracheobronchialtreeofthepatientshowing theuppermarginofthebronchialcuffwasslightlyseenat betweenthecarinaandtheleftmainbronchialori ficewithout theobstructionofthetracheallumen(Fig.2D). [6] Surgeons indicatedthattheuseofthenewDLTprovidedexcellent operatingconditionsduringbothlunggrafts.Theoperation timewas10hoursand50minutesunderveno-arterialECMO. ThepatientwastransferredtointensivecareunitwithvenovenousECMO.ECMOwasappliedforpostoperativeday
(POD)13,andthepatientwasmovedtothegeneralwardat POD37.
3.Discussion
One-lungventilationisusuallyachievedbyexactlungisolation techniquewithDLTorbronchialblocker(BB).[7] IdealpositioningofDLTorBBisusuallyconfirmedbyFOB.[1,2] DLTismost commonlyusedtoachievelungisolationforlungtransplantation.However,usingDLTrequirestheanesthesiologist’s proficiencyandpreference.TheDLThasbeendescribedas “difficulttubes” becauseofanincreasedrigidityandtheirlarge outsidediameter.[8] Moreover,39%ofanesthesiologistswith limitedthoracicanesthesiaexperiencewereunabletoachieve successfullungseparationregardlessofthetypeoflungisolation deviceduetopoorknowledgeofendoscopicbronchialanatomy.[9] Itrequiresalsonormalanatomyofpatientandconfirmationofbronchoscopy.BlindpositioningofDLTissometimes usedinadifficultairwaypatientorcondition,confirmedbyusing thecomplianceofbothlungsorprescribedformula(12.5+[0.1 height]cm).[4] However,thesuccessrateofblindlungisolation technique,donebydedicatedthoracicanesthesiologists,wasonly 63%.[1] However,ifthepatientshaveend-stagelungdisease combinedwithamassivepulmonarysecretion,bronchoscopic confirmationofexactlungisolationwiththeuseofFOBorthe blindlungisolationwithlungcompliancewouldbeimpossible. TheANKORDLTwasdevelopedtoprovidethesimplemethodof lungisolationforthoracicsurgery.Comparedwiththeconventional DLT,ithasonemorecuffthatislocatedatapointbetweenthedistal openingofthetracheallumenandthestartingpointofbronchialcuff. Thecarinalcuffwasdesignedtoexpandtowardtheoppositesideof bronchiallumenofthetube.Consequently,itistransientlysupposed toformaninverted “Y” shapewiththeinflatedcarinalcuffandthe distalpartofbronchiallumenofthetube,whichfunctionallyanchors thetubeatthekeel-shapedcarinalridge.OncetheANKORDLT stopsatsomedepthoftracheobronchialtree,thatpointisconsidered asanidealdepthofDLTpositioningforlungisolation.Afterwards, thedeflationofthecarinalcuffoftheANKORDLTrendersthetube functionasaconventionalDLT.Therefore,asshowninthiscase,the useofANKORDLTwouldhelptheanesthesiologiststoperformthe moresuccessfullungisolationtechniquewhichusuallytakesabout1 minuteaslongasthestructureofmaintracheobronchialtreeof
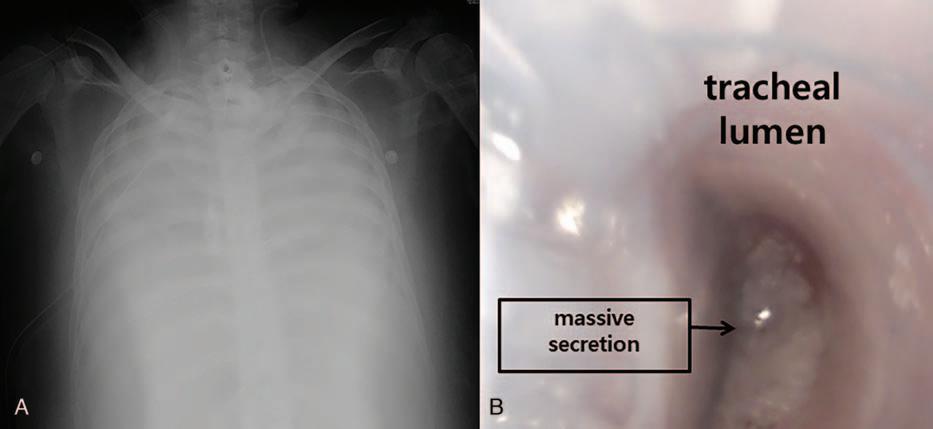
Figure1. Perioperativeimagesofthepatient.A,Preoperativechestx-ray,showingseverediffuselungconsodiation.B,Bronchoscopic finding,showingmassive pulmonarysecretionwithintheconventionaldouble-lumenendobronchialtube.
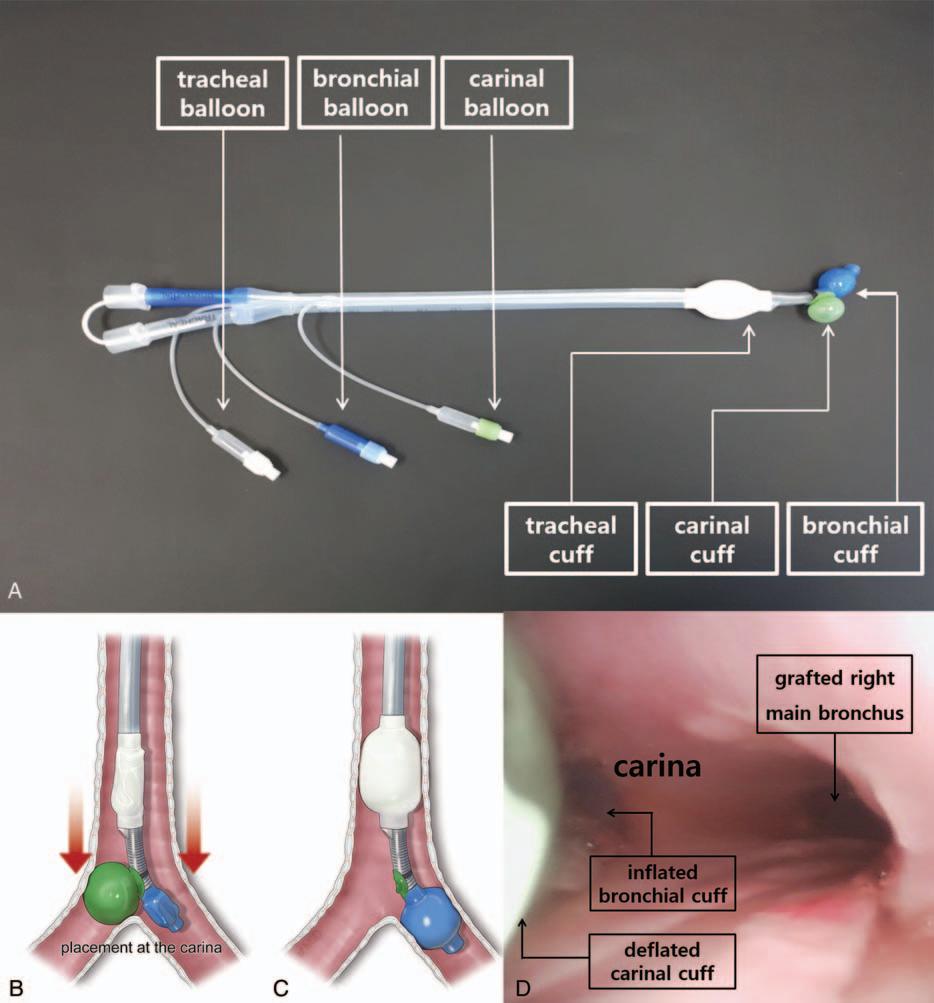
Figure2. Thedesignofanoveldouble-lumenendobronchialtube(ANKORDLT)anditsapplicationtothepatient.A,ComparedwithconventionalDLT,ANKOR DLThasonemorecuff, “carinalcuff,” thatislocatedatapointbetweenthedistalopeningofthetracheallumenandthestartingpointofbronchialcuff.B,Oncethe carinalcuffofthetubepassedthroughthevocalcordofthepatient,itwasturnedtotheleft,andcarinalcuffwasin flatedwith6mLofair.Itwastransientlysupposed toformaninverted “Y” shapewiththeinflatedcarinalcuffandthedistalpartofbronchiallumenofthetube,whichfunctionallyanchoredthetubeatthekeel-shaped carinalridge.C,Afterthedeflationofthecarinalcuff,thetrachealcuffandthebronchialcuffofthetubewereinflatedwith5and2mLofair,respectively.D,Afterthe completionofrightlunggraft,bronchoscopic findingshowedthatthetubewasproperlypositionedinthetracheobronchialtreeofthepatientshowingtheupper marginofthebronchialcuffwasslightlyseenatbetweenthecarinaandtheleftmainbronchialorificewithouttheobstructionofthetracheallumen.
patientswereintact,eveninthepatientswithanend-stagelung diseasecombinedwithmassivepulmonarysecretion.Inthiscase, minimizingthetimewastingforlungisolationmighthavebeen crucialfortheviabledonorlungsduringthesurgery,although ECMOappliedtothepatientpreoperativelymighthaveprovided oxygentothepatientinthiscase.Therefore,weexpectthatthisnew DLTwouldworkwellinpatientswhohaveseveredestructivelung parenchyma,hemothorax,orforanesthesiologistswithlimited experienceinlungisolation.
Inconclusion,theANKORDLTwouldbeafeasiblechoiceto achievesuccessfulblindlungisolationwhentheuseof fiberoptic bronchoscopyisimpossibletoachievethepreciselungisolation asshowninthiscasereport.Furtherwell-designedclinicalstudies arerequiredforitseffectivenessonblindlungisolationinvarious clinicalcircumstances.
Acknowledgments
TheauthorsthankMID(MedicalIllustration&Design),apart oftheMedicalResearchSupportServicesofYonseiUniversity
CollegeofMedicine,forallartisticsupportrelatedtothis work.
Authorcontributions
Conceptualization: HyoChaePaik,YoungJunOh. Datacuration: NamoKim. Investigation: DaheePark. Resources: YijunSeo. Supervision: YoungJunOh. Validation: DaheePark. Visualization: NamoKim,HyoChaePaik. Writing – originaldraft: YijunSeo. Writing – review&editing: YoungJunOh.
References
[1]deBellisM,AccardoR,DiMaioM,etal.Is flexiblebronchoscopy necessarytocon firmthepositionofdouble-lumentubesbeforethoracic surgery?EurJCardiothoracSurg2011;40:912–6.
[2]KleinU,KarzaiW,BloosF,etal.Roleof fiberopticbronchoscopyin conjunctionwiththeuseofdouble-lumentubesforthoracicanesthesiaa prospectivestudy.Anesthesiology1998;88:346–50.
[3]KimSH,ChoiYS,ShinS,etal.Positioningofdouble-lumentubesbased ontheminimumpeakinspiratorypressuredifferencebetweentheright andleftlungsinshortpatients:aprospectiveobservationalstudy.EurJ Anaesthesiol2014;31:137–42.
[4]JenkinsAV.Anendobronchialcuffindicatorforuseinthoracicsurgery. BrJAnaesth1979;51:905–6.
[5]TakitaK,MorimotoY,KemmotsuO.Theheight-basedformulafor predictionofleft-sideddouble-lumentrachealtubedepth.JCardiothorac VascAnesth2003;17:412–3.
[6]CamposJH.Whichdeviceshouldbeconsideredthebestforlung isolation:double-lumenendotrachealtubeversusbronchialblockers. CurrOpinAnesthesiol2007;20:27–31.
[7]BrodskyJB.Lungseparationandthedif ficultairway.BrJAnaesth 2009;103(suppl):i66–75.
[8]BenumofJL.Difficulttubesanddifficultairways.JCardiothoracVasc Anesth1998;12:131–2.
[9]CamposJH,HallamEA,VanNattaT,etal.Devicesforlungisolation usedbyanesthesiologistswithlimitedthoracicexperience:comparisonof double-lumenendotrachealtube,Univenttorquecontrolblocker,and Arndtwire-guidedendobronchialblocker.Anesthesiology2006;104: 261–6.
