BRAVING THE WAVES
A COLLECTION OF PERSONAL AND CORPORATE STORIES WITHIN MEDICLINIC SOUTHERN AFRICA DURING COVID-19
2020/21













A COLLECTION OF PERSONAL AND CORPORATE STORIES WITHIN MEDICLINIC SOUTHERN AFRICA DURING COVID-19
2020/21












The COVID-19 pandemic has had a profound impact on everyone across the globe. In our case, as a healthcare provider, the impact was extremely challenging and rewarding at the same time. We needed to be part of a solution that would support our entire nation. And we wanted to work together with other role players to make sure we collectively did everything possible to meet the challenge facing us.
But first, we had to prioritise our people. This meant creating a safe environment by implementing and reinforcing all the necessary infection, prevention and control protocols, ensuring the right quality personal protective equipment was available for our hospitals, and bringing in psychological help to monitor the emotional wellbeing of our staff. We did our utmost to ensure that all our front-line healthcare workers had access to the COVID-19 vaccine as soon as possible.
Doctors, nurses, allied healthcare professionals, administrators – each and every one of you took up a role that made a difference. Team members were reallocated from Corporate Office to hospitals and, in some cases, spent many months at the localities in support. Let me emphatically say thank you to each of you who stepped outside your comfort zone to help support our efforts.
What has personally kept me going through this period was the support from the core team – knowing that I was not alone. My family were just as vital to me during this time. Even when I contracted COVID-19 myself, I knew that there was a team managing and overseeing our organisation and looking out for the staff.
They say that it is only in moments where you are truly tested that you understand your own strength. Today, I believe that we all have a better understanding of what we are truly able to accomplish. We know the challenges were not only at work. Some families suffered deep losses; others either had responsibilities after work teaching children who were home during lockdown or felt the economic

challenges of family members unable to work. I know we are asking you to climb back into the boat as this pandemic continues to trouble our community, drawing on resources you never envisioned you possessed as numbers climb and our patients seek us out. I emphasise the need to care for yourselves as well as you care for others. Please use all the resources we have made available to support you – physically, emotionally and mentally.
We are proud that the Mediclinic values of being team orientated and patient safety focused, as well as having trust and respect have shone out in our hospitals. You will find some of these stories told in this journal. I trust – despite every story not being told – that those which are featured represent your efforts along with those mentioned by name.
Take a moment to consider the stories from regions far beyond your hospital walls, and be inspired and hopeful by learning of their success. You were part of something that will be remembered for generations to come. You played your part in riding the storm and creating hope for all our communities.
As I close, I want to describe the deep hope I have for our country. I base my hope on the resilience of our people within our business and our community. When we work together, we will overcome. I base my hope on the vaccine and I base my hope on the belief that we will be able to rebuild our country economically moving ahead. Thank you once again.
KOERT PRETORIUS CHIEF EXECUTIVE OFFICER: MEDICLINIC SOUTHERN AFRICA
From early in 2020, we have faced one of the biggest battles of our lives – one that none of us could have imagined. COVID-19 spread across the world and we were not spared. Hospital teams, clinicians and supporting services immediately climbed on board to respond to this unseen enemy. This was truly an inspiring demonstration of the power that comes through unity.
I have never been so proud to be part of such a formidable team! Each of you took up the fight and fought alongside your colleagues to support family and community. Moments like these are never easy, and there is a price to pay. I would like to thank you for the long hours, the emotional commitment and the physical investment you have made in each of our patients. I trust that you have made use of the resources available, should you require support in any area.
From the onset of the pandemic in early 2020, Mediclinic began planning. A task team was quickly established to represent all areas of the business. The team met on a daily basis and spent hours planning, learning and understanding how to best support the hospitals. You will find, in coming pages, how teams in different departments stood up and were counted when and where they were needed. You will also gain insight into what they were able to learn in the process.
In Afrikaans, they say, ‘jy moet die wa deur die drif trek’ – this is a term I have used on numerous occasions within the task team. In English, this broadly means to solve a problem or master a difficult situation. It is often necessary to go through the whole process before we are able to see the outcome of our actions.
What I want you to see is that none of the stories represented in this publication would have been possible
in isolation. COVID-19 will not be overcome with one decision or one action. PPE; Medication; Training; IPC; ICT; Nursing; Doctors: Each have value on their own, but when brought together, they carried a nation. Our reward is in knowing how many lives have been saved and touched by our care, and how many families have emerged with one of their own returning home. Where we have lost patients, their friends and family can rest assured that their loved one was cared for in their most desperate need. This is you. Each of you can assuredly say, ‘I was part of the fight against COVID-19.’
I would like to personally thank our nursing staff; our attending doctors; our emergency response medics; our admin teams who kept the business moving behind the scenes; our technical teams who made physical distancing and safety measures possible; and our pharmacy teams who kept medicine and other consumables within reach. In truth, I would never be able to compile an exhaustive list of people to thank as there are so many. But what can be said with absolute certainty, however, is that collaboration was at the forefront of our success. By working together, Mediclinic and ER24 have weathered the conditions and have shown their mettle.
I am immensely proud of each of you. I appreciate your contribution, and I trust you will find encouragement in each page of this journal.

WIMPIE AUCAMP CHIEF OPERATING OFFICER: MEDICLINIC SOUTHERN AFRICA
14
Solving problems through technology and ICT

24 TRACKING FROM THE BACKLINE FOR THE FRONT LINE
20
INTERNATIONAL NURSES’ DAY 2020 & 2021
Someone who is both skilled enough to be strong and caring enough to be soft.
We look at how some of our hospitals responded to the challenges faced.

56

Driving vaccinations with a view to a healthier future.
06
07
08
09
THE TASK TEAM
Fostering accessible and agile leadership in the pandemic.
TAKING ON THE CHALLENGE
A clinical approach to fighting Covid-19.
PPE AND CRUCIAL SUPPLIES: ARMOUR AGAINST COVID-19
How procurement put the right tools in the right hands at the right time.
COVID-19 DID NOT CHANGE THE SCIENCE OF IPC
Effective IPC relies on well-established frameworks
JUMP-IN-AND DO ATTITUDE
Training and facilitating in a time of change.
10 MAKING THINGS WORK
Infrastructure became a key resource as we readied for the storm.
11 BACKING THE SCIENCE WHEN FACING THE UNKNOWN
How Pharmacy was integral to treating an unknown enemy.
12
TAKING HANDS
MHR - Bringing essential resources to hand.
13 THINKING BEYOND JUST AN AMBULANCE SERVICE
Delivering Real Help, Real Fast during a pandemic
CONTRIBUTORS
Caryn Ross
Ineke van Huyssteen
Riani Retief
Estelle Coustas
Louise Aylward
Aliné Hall
EDITORIAL
Magriet Pienaar
ART DIRECTION
Marilize Botha
DESIGN
De Wet van Deventer
15 A TIME FOR PEOPLE TO BE CHERISHED
When Human Resources are the most precious resource.
16
SERVING AS A BAROMETER FOR COVID-19 IN COMMUNITIES
Emergency care in a time of crisis.
17 INDUSTRY-BUILDING RELATIONSHIPS
Building bridges to advance our response to a crisis.
18
COMMUNICATING WITHIN
Delivering the information of value within the business.
19 ASSISTING WHERE THE NEED IS Clinical expertise you can trust.
52
54
SUCCESS IN INNOVATION
Innovating to meet the needs of business.
REASSURING THE COMMUNITY
Responding with knowledge and reassurance during uncertainty.
58 AS THE NATION RECOVERS
An overwhelming encouragement to the community was experienced through each recovery.
60
MEDICLINIC PAYS TRIBUTE
Mediclinic recognises the unwavering dedication of staff members and doctors.
PROOFREADER
Ryan Williams
PRODUCTION
Craig D’Oliveira
Lee-Ann Stoop
by Mediclinic Corporate Communication and Mediclinic Design Studio, Mediclinic Southern Africa, 25 Du Toit Street, Stellenbosch 7600 help@mediclinic.co.za | T +27 21 809 6500
Mediclinic’s response to the pandemic was spearheaded by a key strategy: Establish a core team of specialists across the business who could make immediate decisions based on the challenges facing regions or specific hospitals. The COVID-19 Task Team was born. It consisted of subject matter specialists across the business, along with regional representation and support functions. The team was headed by Wimpie Aucamp, Chief Operations Officer.
The initial intention was to establish a physical command centre at Corporate Office to function in the peak of the waves, but as the pandemic evolved the best solution became a virtual command centre, where team members met virtually throughout the various waves.
‘I believe this was a really valuable tool. It allowed us to openly share ideas, voice concerns and address priority matters swiftly. We called in additional resources as specific topics became important – allowing them to give direct feedback to the team and empowering us to make the right decisions for our staff and our hospitals,’ says Wimpie.
Through this daily interaction, the greatest needs were prioritised and appropriate decisions could be made quickly. This included availability of beds and equipment, oxygen supply, personal protective equipment and staffing resources when regions were under pressure.
‘The greatest strengths of the Task Team were the frequent meetings and open communication,’ explains Johan Geertsema, Operational Executive (OE) for the Tshwane region, ‘together with plans, policies and procedures that were timeously put in place. It really involved sharing of knowledge and experience at a high level.’
Edmund van Wyk, OE for the Western Cape Coastal region, believes the Task Team allowed feedback to be given to hospitals on a daily basis directly after each meeting, allowing hospitals to respond or implement the same day. It kept the senior management team in contact with what was happening in real time.

In exploring how this pandemic could positively impact how we manage our business going forward, Edmund believes that the direct communication from the CEO and COO to hospitals needs to remain, keeping them up to date on top-ofmind issues. Johan agrees: ‘The frequent communication must continue, with Corporate Office specialists’ direct support and involvement in solving problems.’





Like an army preparing for war, the clinical teams across Mediclinic have been trained to deliver the best possible care to their patients against various enemies. But, as with war, you can never tell how the enemy will approach; in the case of COVID-19, the enemy was unknown and its attack needed to be studied before a formal response could be launched.
‘Our response to the rapidly changing environment was multipronged, with treatment guidelines, infection prevention and control (IPC) protocols, care pathways for Emergency Centres, access control and screening guidelines, care escalation guidelines, palliative care guidelines, amongst others, being developed. Regularly during this period, new information would present and these documents would need to be revised. Agility became essential,’ explains Dr Gerrit de Villiers, Chief Clinical Officer: Mediclinic Southern Africa.
As staff wellness became an even greater priority, screening and monitoring healthcare workers became a key focus area. Personal protective equipment quality needed to be assessed and the procurement team set high standards for what was to be used in the hospitals.
Daily engagements with teams at hospital level became part of the agenda during each surge: engagements and catch-ups took place across different mediums. Zoom, WhatsApp and Skype all became valuable channels for swift response: understanding the needs at a practical level, what could be done, what could be improved.
Dr Kim Faure, Clinical Performance Manager, believes that this collaboration and teamwork encouraged (and sometimes forced) team members to step out of their operational comfort zones and take on new challenges. ‘This gave the opportunity for certain people, who are not usually at the forefront, to shine and demonstrate their unrecognised value to the team as a whole.’
A vital part of the Clinical Department’s role was to delve into the best-practice principles to overcome fake news and beliefs, both in the media and at hospital level. With the uncertainty of a novel virus, much had to be learnt. The important factor was disseminating the correct information quickly. Management broadcasts allowed information to be shared quickly, concerns to be addressed swiftly and questions to be answered.
The most valuable elements of the pandemic response were the prompt, decisive engagements from various units. ‘The IPC response. The Critical Care response in terms of triage. Critical Care Society engagement and guidelines. Experimental treatments and the role they played in the pandemic. Oxygen provision, and the support received from the infrastructure team. Procurement’s response to our needs. Information and communications technology innovation driving a streamlined approach to so many different areas of our business. Our effective media response to the pandemic. These are all areas in which I believe we have succeeded by operating across our zones and working together,’ explains Dr De Villiers.
How will this pandemic shape our way forward? Dr Faure believes that some things are here to stay. Hand hygiene will be a new normal. Mask wearing has demonstrated its effectiveness, and should remain an ingrained behaviour within hospitals. A key element she believes should be built into any route forward is the high levels of collaboration between departments. The movement back to silos is unthinkable.
Dr De Villiers believes that IPC’s core role in the hospitals has been reinforced. In addition, the importance of science behind any decision was highlighted. And, above all, he believes it is vital to retain the people-centred approach to our business: for patients, nurses, cleaning staff, porters, administrators, doctors – everyone.
HOW
The COVID-19 pandemic was a battle no one saw coming, which left many on the back foot. But, by procuring appropriate personal protective equipment (PPE) efficiently and timeously, Mediclinic could focus on ensuring the best outcomes in a challenging and unprecedented environment. Here is how the Procurement team protected staff, while keeping the patient safe and at the centre of patient care.
When the World Health Organization declared the COVID-19 outbreak a global pandemic in March 2020, all eyes turned to hospital facilities and their crucial supplies. Ventilators, surgical face masks, temperature thermometers, even bed linen – from the earliest clinical definitions of coronavirus disease, it was clear that these would be crucial. ‘This is why Mediclinic began planning for an effective in-hospital response long before COVID-19 was first reported in South Africa,’ says Annelia Bezuidenhout, General Manager: Procurement, who leads a team responsible for acquiring a wide range of essential hospital equipment.
‘We have contracts in place, and existing suppliers for crucial items and PPE. When those suppliers were unable to fulfil the need because of the unprecedented worldwide demand, then we started looking at alternatives,’ says Venesha Shunmugam, Manager: Pharmacy Procurement.
Annelia explains: ‘We had to have a central distribution point. The space was twofold: We could order stock from several places and then prepare a consolidated order in the Corporate Office, or it was where we needed to take stock urgently before it was sold out in the market. If you didn’t buy it and take delivery of it immediately, someone else would take it, especially during the early stages of the pandemic. There are videos of how we were loading boxes late at night or early in the morning. We also had testing stations set up where the teams did physical testing of PPE themselves to ensure everything was up to standard.’
Stock availability was undoubtedly the most crucial objective for the Procurement team. Although the supply chain might have been severely disrupted, Mediclinic never ran out of quality PPE.
‘There were moments where some hospitals ran short, but then we moved stock from other hospitals. Hospitals might not have had the products they were used to, but they did have stock, and we never ran out. We used anything between 800 000 and 1.6-million gloves per week. I think we recorded 6-million gloves in a month. Pharmacy was under the most pressure, but they were able to deal with all the curveballs,’ says Annelia.
The pandemic taught us a lot about resilience, tenacity, teamwork and coping
The team reviewed almost 1 000 suppliers and, in the end, bought products from fewer than 10. Organising was the key to not buying things in a frenzy, and by managing price increases well, Mediclinic was saved millions.
‘Of course, we also had to contend with lots of scams and be careful not to be duped because you trust what information is provided. We tried our best to maintain contact with reputable companies, especially in the respiratory field. We also tried to stay as close as possible to our current vendor approval and product approval process. We worked closely with our competitors so that we could collaborate and learn from one another. We were all fighting for the same resources, and it made no sense that one should end up with a lot of stock and one be compromised – we are all in the business of healthcare,’ says Venesha.
The pandemic spared no one from venturing outside of their normal scope of work. Those who saw the mountains of boxes in what our Corporate Office cafeteria was would know – you have to make do with what you have.
Annelia was also involved with Business for SA (B4SA) and Venesha with the Department of Trade and Industry (DTI). Here, they helped with product development, standards on the DTI side, and managing products on the B4SA side. ‘I had a weekly market check-in and industry meeting where we would discuss common burning points and then that was fed back to B4SA to ensure alignment in the market,’ says Annelia.
The pandemic taught us a lot about resilience, tenacity, teamwork and coping under immense pressure. For Annelia and the team, the pandemic also separated the wheat from the chaff. ‘You had to identify the most important or most valuable aspects and ignore the rest. There have been obstacles, and there will be more, but we are confident that our hospitals have what it takes to beat this challenge.’
When SARS-CoV-2 was reported as being a ‘novel’ or newly identified virus of concern, the Infection Prevention and Control (IPC) team approached, monitored and planned – as they had in the past – for the emergence of communicable disease outbreaks of local or international concern such as MERS (Middle East Respiratory Syndrome) and Ebola. The Measles and Listeriosis outbreaks in South Africa in 2017 were examples of existing IPC processes being intensified to successfully manage demands, with limited impact. When the initial and subsequent cases of SARS-CoV-2 were identified in South Africa, the IPC Managers continued to apply established surveillance processes. Hospitals identified patients, isolated them, and reported each case as a Notifiable Medical Condition (NMC), ensuring that contacts of people testing positive for SARS-CoV-2 were followed up as part of occupational and broader public health requirements. IPC was called upon for planning and input on various aspects including patient and staff access, patient placement, staff protection and monitoring, statistics, training and practical guidance related to specific patient and procedural interventions. It has been extremely positive to see IPC being recognised as a specialty which plays an adaptable and integral role within its well-established framework and across activities in all departments, supporting varied disciplines.
The IPC Managers at the hospitals must be commended for their unwavering hard work, dedication, determination, resilience, caring and sense of humour, irrespective of the challenges they faced. We are particularly appreciative for the assistance of Patient Safety Managers and other colleagues available to assist as logistical demands increased. The Regional Clinical Managers likewise provided unwavering and valued support to the hospitals, IPC Managers, and Corporate Office teams. Multiple discussions and investigations were undertaken to determine failures which may have resulted in ‘clusters’ or cases where transmission of COVID-19 occurred between staff or patients to prevent recurrence and share lessons learnt. Human behaviour remains one of the greatest challenges in attaining consistent compliance to mitigate IPC risks on an ongoing basis.
While COVID-19 provided the opportunity to reiterate and apply IPC principles, it also raised numerous challenges and complexities. Repeated explanations were required due to extensive involvement of multiple role players with no prior IPC knowledge or experience, in order to justify sound evidence-based recommendations in light of media sensationalism or hearsay from elsewhere.
Christine Smedley and Narissa du Toit from the Corporate Office IPC team are well-known faces within their area of specialty. They commented that having an IPC role during a pandemic is, in essence, the ultimate experience of an IPC career. It was challenging to continuously reinforce and substantiate reasons for IPC practices while role players with limited IPC exposure or knowledge voiced and unnecessarily exacerbated fear and anxiety about managing COVID-19. On the other hand, they were provided with such amazing opportunities to develop IPC and promote future involvement and development in this field. As time has progressed, it has been reassuring to reflect that they remain committed to the initial recommendations and basic IPC principles despite the many challenges, although each ‘wave’ or new development will undoubtedly bring new uncertainties. What was most striking was the appreciation and recognition of support that the hospitals provided to the Corporate Office IPC team despite the hardships they themselves were facing.
Significant ‘unseen’ IPC achievements and successes since COVID-19 include the initial development of the healthcare worker application. ‘Our healthcare workers are such a priority, and ensuring only healthy healthcare workers are at work further translates to less risk for colleagues or patients,’ explains Narissa. External collaboration led to the automation of data for National COVID-19 statistics reporting from Mediclinic systems directly to the Department of Health and the National Institute for Communicable Diseases. Mediclinic is currently the only private healthcare group to successfully automate the extremely labour- intensive process for mandatory reporting of COVID-19 as a Notifiable Medical Condition.
Throughout this process, communication barriers have been broken down and new relationships forged between management, staff and doctors. ‘It was rewarding to have diverse teams spontaneously engaging with us through a common need, asking for advice, seeking out guidance,’ says Christine. ‘Our task remains empowerment of individuals to apply IPC principles and develop their own solutions at ground level to best equip them for the future.’ Better knowledge and involvement across all groups of healthcare workers is essential to not only respond to the pandemic, but to address multiple IPC challenges which will continue to affect patients and communities.
And, in the end, Dr Gerrit de Villiers, Chief Clinical Officer of Mediclinic Southern Africa, hopes that one long-term outcome from this pandemic will be that the role of IPC within the business is recognised and solidified in daily operations within all Mediclinic hospitals.
The COVID-19 pandemic brought sudden and disruptive change. You had to adapt, think on your feet, and be resilient while trying to keep your head above water. Change can be unsettling, challenging and lonely. But change can also bring teamwork, new perspectives and new skills to the fore. This was Training and Development’s response to the pandemic.
‘From the get-go, our team had to jump in and do. We had to develop training material that focused specifically on COVID-19 patients from a critical care perspective. We also developed posters, as well as disaster training packs for hospitals. The posters enabled staff to have crucial information at their fingertips should this or that happen. The learning material was no longer nice to know; it was now a need-toknow. Nothing was too difficult to learn quickly. We had to upskill theatre nurses to help in the Critical Care Unit (CCU) as that was where the need was, and we made sure that we offered the necessary support to the hospitals and nurses,’ says Avril Stroh, General Manager: Training and Development.
The Learning Centres had to go from face-to-face to virtual training. An incredible feat here was that the educators who were not directly involved with the students could assist hospitals in need.
‘The educators played a crucial role in training the hospital staff. Some of them went to work in the CCUs, where others took over the Learning and Development Facilitators’ work. We identified the educators who had specific critical care skills, plus MHR enlisted its clinical facilitators. I compiled a list where I designated them to various hospitals. Every hospital had someone who could support the nurses and teach them on the spot. This was a very valuable component,’ says Kayline Coetzee, Nursing Training Manager.
The theatre and other redeployed nurses stepped into a world they did not know at all
Training and Development also got involved with the COVID-19 debrief sessions at the hospitals, which provided them with the opportunity to see what was working, what was not, and where there were needs that still needed to be met.
The theatre and other redeployed nurses stepped into a world they did not know at all. The fear of the unknown was immense, and they had to forge new relationships in the CCU. This in itself was a daunting task, but they rose to the occasion and became heroes in the eyes of many.
‘The COVID-19 training provided them with a broader perspective when it came to patient care, but they also saw that there was actually nothing to be scared of. I think the nurses who had this type of experience are going to be phenomenal post-COVID-19. Most did a complete 180 after their training and their experience in the CCU. This was one of the greatest learnings I experienced,’ says Avril.
The higher education side also had to deal with a significant change as they had barely started with their new batch of students when the pandemic hit our shores.
‘We assisted wherever we could or wherever the need was. Priorities were shifted, and the Training and Development department was led by these priorities – even if it meant you had to set aside your work. Change can be difficult, and most people aren’t comfortable with it. But we all realised that change needed to happen fast, and we had to adapt. There was great teamwork shown, and I think we managed well. Our new students, who were taught virtually, were quite successful in that they had a good pass rate at the end of the year,’ says Kayline.
Are there any changes in their department they wish to keep? ‘We would like to see if we can acquire accreditation to do more of our training virtually. We have permission now from the Department of Higher Education and Training to do it temporarily. We won’t be able to do all our training virtually, but to have at least a few programmes accredited for this would be wonderful,’ says Avril.
It can be said that relationships and experience formed the backbone of the Infrastructure team’s response to the COVID-19 pandemic. The wise and experienced heads leading the charge included Kobus Jonck, Projects General Manager; Kevin Poggenpoel, former Technical Operations General Manager; and Wiid Brett, Project Manager, who gave some insights into their team’s response.
‘Our interventions were timed when the country was in Level 5 lockdown. We were developing ventilation systems and temporary isolation structures when businesses were closed. We called on suppliers we had existing relationships with to open up warehouses, and we found ways to make things work in our hospitals,’ explains Kobus.
Three key areas were portable ventilation systems, temporary isolation units (or bubbles), and oxygen supply across very different hospital structures. These challenges can also be seen as their greatest successes.
safety. It was an amazing process.’ Their solutions took them from building portable ventilation units located in the roof to changing their approach to be floor-based as more became known about the virus. Fans – or their lack thereof during lockdown – meant importing units to ensure they operated quietly and efficiently to meet their purpose in the hospitals. Small things became big things during the decision-making process. Technical teams on the ground had to get things right.
Trial and error, is how Kevin explains their erection of the isolation units. ‘We had to identify the right materials. Functional. Practical. Durable.
In many ways, these are the silent heroes of the fight
‘We did endless calculations,’ Kobus explains. ‘We calculated air circulation in theatre, we calculated oxygen flow across different designs and points in a hospital, we developed a system to monitor oxygen levels at facility level. We kept going back to verify what information we had learned from our counterparts in Italy and the Netherlands who had already experienced some of the pandemic before us.’ Plans were made and guidelines and policies developed, then adjustments needed to be made at hospital level.
Wiid explains: ‘We had plans and we would approach a facility and they would have their own plans. We would then sit and engage, and discuss, and then develop systems to work that gave the facility ease of operation, but also met the standards we needed to maintain for everyone’s
But this was done to suit the facility, and we appreciate the work done by hospital and regional teams to get them in place.’
Oxygen supply: two enormously important words. It was not just ensuring that our suppliers, with whom we had ongoing engagements around supply, kept the deliveries up. It was about understanding what each system could safely handle. Each hospital required unique decisions on supply, infrastructure and equipment that could be added, as well as reviews of bulk storage capacity. This put enormous pressure on the technical teams, especially the smaller hospitals where oxygen cylinders could stand 100 deep and changeovers were being made every four to six hours – leaving teams at risk of burnout. But the work was done, so that the hospital could safely receive patients.
In many ways, these are the silent heroes of the fight. No one saw the oxygen cylinders – they just knew oxygen was there. But there were bodies behind the triage tents, the ventilation units, the isolation units and the endless calculations that made things work. To these bodies and minds, we give our appreciation for crucial work.

The COVID-19 pandemic brought a lot of unknowns into the industry. How do we fight the virus? How do we prevent infection from the virus? Then the introduction of fake news drove even more uncertainty in terms of the most appropriate pharmaceuticals.
Within the pharmaceutical industry, South Africa only utilises approximately 2% of the gross international market, leaving us as a small player on the larger stage. Limitations on access to products to fight the symptoms began when worldwide supply came under pressure. Consideration had to be given to balancing the acquisition of sufficient stock, while ensuring that we did not stockpile to the detriment of other role players in our country. It was vital that we were responsible in our decision-making.
As the pandemic evolved, it became easier to understand and track the needs of the hospitals as trends and patterns developed. What became a greater challenge was the demand for many unproven treatments, where no proven science was available to support the appeals for access. ‘We maintained our decision to acquire medications based on research and current legislation, and eagerly observed what evidence was available to support various treatment protocols. Many of these “popular treatments” faded as fast as they arrived,’ explains Douglas Defty, Pharmacy Executive.
They were cautious around communication to their teams, and were trying to avoid information overload as knowledge was shared across the business. ‘I was so impressed with the teams at hospital level: how ready and keen they were to share ideas and adjust to the changing landscape we faced,’ says Douglas, ‘We had to adjust shifts
to reduce risk of infection, and I was encouraged by the manner in which team members stepped across their roles to learn and take on other responsibilities in this process.’
Many of the challenges the team faced led to what Douglas sees as their big successes. ‘We proved that generics are effective. When certain drugs became scarce, generics were applied and proved their efficacy. We also proved that our processes were robust, but that they could always be improved. We demonstrated how our most valuable asset (our staff) were able to adjust and be flexible in their roles to achieve the common goal of best patient care.’ He explains how people shared ideas freely and showed insight that no one had previously recognised in some individuals.
Douglas also notes the importance of interdepartmental interaction. ‘We found new ways of doing things. We made things happen across the business. We developed solutions. It was exciting and inspiring.’
And in looking to the future, he believes a few things have also changed or come to the fore. ‘I think we have proven the value of dedicated clinical pharmacists. I also want cross-function training to continue, as well as the sharing of ideas. We have demonstrated the importance of decisions based on science. We also know that we can get by with less,’ he says.
Douglas offers some insight as a personal note: ‘I have learnt to appreciate people and their contributions, the importance of recognition for contributions and the value of people putting up their hands and moving out of their comfort zones. We can share and bring greater care and value, working in a team like this.’

Team Orientated. One of Mediclinic’s five core values. This value truly encompassed what was needed – and still is – to combat the COVID-19 pandemic together: The importance of supporting colleagues, going above and beyond what is expected, and working together towards the greater cause. Here’s how MHR embraced teamwork.
‘All MHR staff, not limited to any specific individual, were phenomenal during the pandemic and the subsequent waves. Staff cancelled or shortened their leave, some worked on their loved ones’ birthdays, people worked on their off days, nobody hesitated to help – even at times cross-functionally,’ says André Fourie, Chief Executive Officer: MHR.
Although MHR recruited several different types of clinical staff to various hospitals during the pandemic, nurses were the most sought after. In general, even pre-pandemic, South Africa has a shortage of registered nurses. When the pandemic hit, the need was even greater to support hospitals and ensure the staffing levels were adequate – no matter what it took.
faced the challenges head-on,’ says André. ‘There were many nurses who were willing to travel anywhere, be it to the Western Cape, KwaZulu-Natal, Southern Cape or Upington – wherever there was a need. That in itself is incredible.’
‘The Career Acquisition team and our team learned how to work closely together to search for available staff,’ says Alina.
Although MHR coordinators and call centre staff managed to help most of the hospitals needing staff, there were also times where the reality of the situation hit home.
‘On an emotional level, the coordinators also had to phone hospitals to say that they could not find any available staff for them. But we continued to try. From an agency point of view, it has been amazing to see how our clients treated our own like their own. For that, we are thankful,’ says Alina.
We had to commit ourselves to only 24 hours
‘There were a couple of challenges, especially during the second wave. One moment, a hospital was sufficiently staffed, and the next moment they would let us know that they needed more help. We searched in every nook and cranny for an available nurse. If you had a pair of epaulettes and a uniform, you had to go to work. ER24 personnel also went to work in some of the hospitals. We took hands, and we became one – all for the patient,’ says Alina van der Merwe, Quality Control Manager: MHR.
‘I felt such an immense appreciation towards the nurses because, although they were scared of the unknown, they
The orientation process of staff was another challenge MHR was faced with. Due to the immediate need for staff and supporting hospitals, they did not have the luxury of a four-day orientation process. ‘We had to commit ourselves to only 24 hours; within this period, the person had to be trained and be at the hospital ready to help. We vowed that, even if the orientation was shorter, the quality of the staff member placed would not be affected. We focused on and adapted our teaching to what they needed to know now and what they could still learn over, say, the next three months. We had to learn to be adaptable; there was no other way,’ says André.
In the end, to get on a bus, leave your family behind, and travel to another province for an unknown amount of time takes unbelievable courage and resilience. We salute all the staff who put their hands up: You are our heroes.
Teamwork, clinical excellence, communication, and shared knowledge. These are some of the ways in which ER24 transformed and improved themselves to successfully manage the challenges of the COVID-19 pandemic, by aiding not only the hospitals and patients, but also clients and staff.
Clinical excellence in the healthcare industry could not be taken for granted. You had to consider clinical excellence for your clients and your patients and stay up-to-date with the latest clinical information as the pandemic evolves. ER24’s clients’ needs have been diverse; their needs included staff screening and access control, clinical information, counselling, the COVID-19 hotline for clinical information and, of course, immediate response to any emergency. ‘It’s been a privilege to develop and support the teams who have been instrumental in maintaining these programmes for our clients, such as our Contact Centre and our operational teams,’ says Dr Holgate.
Within the clinical operations environment, staff safety has been top of mind in everything implemented or done. There was no time to think of what personal protective equipment (PPE) staff were going to be using. ‘Being in the emergency space, we needed to move on even quicker and ensure the safety of our staff every time we implemented a new process or procedure, sometimes changing these processes and procedures frequently as new information became available. An example is ensuring our operational teams had access to PPE appropriate for our environment. This included masks, visors, surgical gowns, and gloves for every patient being managed.’
Teamwork, communication, and a closer working relationship with Mediclinic were also established very early on in the pandemic. From an operational perspective, instead of handing over a patient at the hospital, paramedics often stayed and assisted the hospitals with the patients. This was especially needed where hospitals were not prepared for the influx of patients or were overburdened. ER24’s operational teams have also learnt more hospital-based clinical skills, a mutually beneficial relationship for all. ‘Our pre-hospital staff are just as exposed to COVID-19 as the in-hospital staff, because we don’t know which of our patients have COVID-19. We appreciate the support Mediclinic gave us in that our pre-hospital staff were prioritised along with the other areas of the business. It was also reassuring to meet frequently with our clinical colleagues to discuss best clinical practices,’ says Dr Holgate.
As the waves progressed and different areas of our country experienced their surge at different times, disaster management principles of doing the most for the most were implemented. ER24 established a Bed Support Unit to assist any hospital to source a bed for their patient. The realisation was that some hospitals were overwhelmed with critical care unit and high-care patient volumes at times, and others could assist with patient care. Once stabilised,
ER24 assisted by locating a suitable bed and moving patients to another location to be treated and managed if they could not be managed at their initial receiving Emergency Centre. The Bed Support and Pandemic Support lines were located in the ER24 Contact Centre. The Pandemic Support line offered up-to-date, evidence-based medical information for clients. Having excellent clinical resources in the form of nurse case managers was pivotal to ensure access to clinical information. ‘It is true to say, when looking at the advances we have made in other areas of our response, ER24 is not just an ambulance service,’ says Dr Holgate.
Support and care to ER24 staff were crucial for Dr Holgate. Staff needed to feel as protected as the patients they were caring for. Care became a key philosophy. ‘With the uncertainty of the pandemic, sometimes the only thing you could offer was care. Reaching out to staff was critical to me. We enlisted the support of our trauma support team to attend to our staff’s emotional needs. It took a lot of time to develop a culture of debriefing and speaking out about needing to talk to somebody. May this caring and attention to our staff’s emotional needs be a legacy we are proud to retain post-COVID-19.’
How will this pandemic shape our way forward? Dr Holgate reiterates that there is no place for complacency. COVID-19 has changed the way we do business. Medicine will be practised differently forever, but clinical excellence and putting our patients first will remain at the forefront of everything we do. Although we cannot go back to how things were or how we used to do certain things, she believes it is for the better. We should learn, evolve, and move forward – together.
Whether directly or indirectly involved in the care of a patient, every staff member has contributed to their care. Thank you to everybody at ER24.
The Mediclinic COVID support lines were established on 13 March 2020. These lines include the public-facing COVID support line, the bed bureau/bed support, the IFT line and diversion logs. Since March 2020 until October 2021, we have received 34 675 incoming calls.
March 2020 – October 2021: The public-facing COVID support line (an access point for the public to complete telephonic screening and request medical information): 10 023 calls
Dedicated internal support line for our hospitals during the peak COVID-19 waves: 22 647. Outbound: 47 758
Number of bed request cases opened: 2114 Specialist beds sourced: 641
Mediclinic has long put the patient at the centre of every aspect of the business, innovating and evolving to ensure expert, appropriate care across a range of fields. With the COVID-19 pandemic, Mediclinic’s Information and Communications Technology (ICT) experts had to implement innovative systems of the highest quality in the shortest amount of time to equip various departments while keeping the patient at the centre.
‘The amount of work we had to implement for COVID-19 was immense, especially during the first wave. We had to ensure that our healthcare workers, hospital teams, pharmacy staff and procurement could plan in accordance with bed, equipment and product availability. The Bed Bureau was implemented and was 100% COVID-19-focused. We developed a system where we could see per hospital all the units, patients, occupancy, COVID-19 patients, staffing and ventilator shortages, etc.
The Healthcare Worker Monitoring system was built in record time to help our Infection Prevention and Control department track the spread and pro-actively prevent and manage outbreaks of the disease among our healthcare workers. Once elective admissions resumed after the first wave, the focus shifted towards considering and applying technology solutions in collaboration with the Clinical department to reduce COVID-19- related risks to patients and staff in hospitals,’ says Minette Barkhuysen, Core Enterprise Systems Manager.
COVID-19-related requests almost simultaneously, all of them critically important at face value, requiring quick and accurate assessment to determine technical feasibility and business process fit. I had to ensure that we could prioritise and align the relevant resources to every priority. Operationally, we had to use all the resources available. The pressure was immense, and set timelines had to be met,’ says Minette.
Cost pressure was another challenge faced during the two waves. With any technology advancement, you have to be cognisant of cost. The team were pressed to develop innovative systems in the shortest amount of time, at the quality that Mediclinic expects and is known for. Balancing the golden triangle of cost, time and quality are the primary forces in a project.
Having the patient at the centre also meant keeping their families right next to them. Part of Mediclinic’s belief is that the family and visitors play a crucial role in a patient’s recovery process. Visitation was temporarily suspended due to the pandemic, and the ICT team also realised the importance of communication with the next of kin during this time. The unit administrative assistant could use the nursing dashboard system to SMS the spouse or the person listed as a contact. A roaming tablet device was also used to set up video calls with families, a small gesture that could mean a lot to the family waiting in anticipation.
During the second wave, Minette notes, most of the systems were already in place and working well to assist various departments. However, the second wave brought challenges at a clinical level as the number of patients increased exponentially, and most of the hospitals were inundated and needed a scoring system to assist them in managing and treating patients. The triage scoring system assisted the hospitals, especially those in harder hit provinces.
‘One of the biggest challenges we faced as a team was the prioritisation of our work. We would receive multiple
‘We understood that it is not just about ICT. It is about the pandemic that we are fighting together. The nurses, cleaning staff, doctors, paramedics, and our patients faced tougher battles than we could ever imagine. There is a greater cause, and I am proud of my team for working towards this with resilience and a willingness while facing challenges of their own. My rule is to attack the issue, not the person. People are tired, and they also have family members who have been ill. I believe that if you look after your team, pandemic or not, you will get the best out of people.’
In the end, we needed the best to fight COVID-19 from the backline to support the brave fighters on the front line.

In a time where our staff were the most valuable asset and the most at risk, Mediclinic had to rely on agility to overcome the challenges facing the team. For those at Corporate Office, leadership accessibility was key to addressing changing needs and the urgent requirement of up-to-date information and knowledge.
René Nel, Human Resources Operations General Manager, believes that with this came the need for quick response to the demands of the hospitals they serve. They had to break down previous hierarchical decision-making structures and opt for flatter, more responsive ways to do business. Safety of staff was a strong motivator in any decision-making. ‘If it is what the staff need, then we get it,’ could be heard across the business.
‘During the pandemic, we began to rely less on formal guidelines and more on the values of our business. It was important to create psychological safety for our staff, by doing as much as we possibly could to support them,’ explains Gilienne Engel, Talent Manager.
There was a strong need to support employees’ wellbeing during the respective waves in a concerted and combined effort by leaders, HR Operations, Talent Acquisition, Organisational Effectiveness, volunteer organisations and Incon to support employees. Most importantly, the pandemic raised awareness of the crucial importance of employee wellbeing as a must-have in the business. The Care.Courage.Compassion website was launched to support employee wellness through a tiered support framework, from self-help wellbeing resources to access to professional psychological counselling. Feedback on the support was amazing, with one staff member noting, ‘People had the opportunity to reflect on not being alone in this, a shared experience through the crisis.’
Really meaningful initiatives launched by the staff themselves included Halls of Fame, the Jerusalema Challenge, red carpet discharges to celebrate recoveries, recovery trees and appreciation videos. We thank each of you for the role you played in supporting your colleagues and giving your all.
‘But during this flatter, more agile decision-making process that the crisis demanded, the business discovered a number of really valuable pieces of input across the business. Ideas could be shared, recognised and quickly implemented – allowing individuals to receive recognition for ideas and concepts,’ says René. That human need for
interaction and engagement also impacted on the volunteering side of the business.
Sharon Rose, Human Resources Operations Manager who championed much of the volunteerism efforts, believes that the pandemic taught her more than she realised.
‘Volunteerism is about people wanting to give back. It should not be about formalised arrangements, but about letting the communities in which we operate engage with us as they have need. It was about a braai at Mediclinic Hoogland, psychologist visits at Mediclinic Vergelegen, and prayer walks around other hospitals. It was about meal packs and letters of hope. The community responded to hospitals as they felt they needed to in recognition of our role in the community.’
And the result? A wave of re-energised teams across Mediclinic as these engagements cheered them on during really long, tough days. Give and take: We give and, sometimes, we need to receive and fill our batteries again.
In a time where fear and uncertainty about COVID-19 gripped the world, people looked to hospitals and medical professionals for help. So, Mediclinic redesigned its Emergency Centres (ECs) to manage patients presenting with COVID-19 and other medical emergencies safely and efficiently. COVID-19 accelerated the evolution of healthcare, and the ECs were ready.
‘ECs are highly specialised areas,’ explains Dr Melanie Stander, Emergency Medicine Manager. ‘We must manage complex and undifferentiated cases and traumatised patients, our staff must remain calm and clinical, and we must ensure patients are treated safely and efficiently, at all hours, even amid a pandemic.’
ECs are accustomed to short-lived, quick disasters, such as bombings, fires, and massive vehicle collisions. However, COVID-19 is a prolonged disaster, which means that staff are continually in this disaster mode for a protracted period.
‘Mediclinic staff had some disaster medicine training because of the FIFA Soccer World Cup held in South Africa in 2010, and Riani Retief and I were responsible for revisiting this training with all our hospitals.
We started the national roll-out in 2017/2018, which stood us in good stead, because many hospitals now had the framework and all we had to do was create a very comprehensive document for the hospitals. A command structure also needed to be put in place for hospitals. You need to ensure that the command structures can control all the hectic variables relating to the disaster (human resources, equipment, personal protective equipment [PPE], acute care that needs to be delivered). The activation of the disaster plan for COVID-19 and the national training certainly helped to assist the hospitals. It wasn’t a new language they had to learn; they were used to working in that type of scenario,’ says Dr Stander.
Mobile testing stations (MTSs) were another way Mediclinic wanted to assist communities by providing support and coming to the party as an acute clinical service provider – keeping the patient at the centre of everything we do. This was a complex arrangement, but the need was massive. Especially at the beginning of the pandemic in the country, there were not many options for people to get tested. Mediclinic saw a need and very quickly and creatively came up with an innovative solution.
‘Our challenge was, many of the people coming to the EC were not really that sick. They had symptoms, but they needed a test, and then they could go home and get followed up there. So, we researched and implemented policies to establish container-type setups outside of our hospitals that were easily accessible for the public. The pathology laboratories came on board and were invaluable with their assistance,’ says Dr Stander.
Our staff have worked tirelessly
Riani explains further: ‘The idea behind the MTSs was not only to avoid large numbers of people in our units, but also to avoid bringing the sick people that are not requiring hospitalisation into the facility. So, as part of access control, we divided the ECs into two separate streams: respiratory and non-respiratory systems. When there was an overflow of patients, we also created additional space for low-flow oxygen therapy. This was especially necessary in some of our facilities during the second and third waves.’
‘For a couple of months, these testing stations were running at a few of our hospitals, in areas where the options for patients to be tested for COVID-19 were very limited in the community,’ says Dr Stander.
‘When we were in the thick of things, our ECs were overrun with patients. As a result, we had to quickly adapt our normal way of work to ensure safety for all our patients and our staff,’ says Riani, Clinical Quality Specialist.
From the beginning, EC access was non-negotiable. Mediclinic regularly receives patients with trauma, potential heart attacks or strokes, chronic and deteriorating conditions, and those who may be experiencing serious COVID-19 infections.
‘Very early on, we decided there would be only two entrances where people could enter the hospital. This was the main hospital and the EC. We were very cognisant that if we restricted access to our EC, we would have unintended consequences of, maybe, someone standing at the main reception who is third in the queue with a heart attack, and no one is aware,’ says Dr Stander.
Furthermore, if one of the healthcare workers in the MTS became concerned about a patient’s clinical condition, there would be a mechanism in place to immediately alert the EC and transfer the patient to the EC for further assessment.
‘Our EC staff, doctors and nurses, and EMS staff became accustomed to the presentation of very sick patients. I think that gave them a lot of practice that by the time we got to the second wave, they were comfortable, they knew what to do with PPE, and they knew what to do with patients because they were in the front line from the very beginning,’ says Dr Stander.
Both Dr Stander and Riani are extremely proud of the Mediclinic EC staff. ‘Our staff are phenomenal and have worked tirelessly under extremely difficult and challenging circumstances, and they have continued to do the best that they can for each and every patient that they care for.’

The COVID-19 pandemic highlighted the role that all stakeholders have to play in the healthcare sector. The virus has not discriminated against any sector, impacting them all heavily during the waves.
Mediclinic was very willing to engage and establish a solid role in assisting during the pandemic. This was done through various channels and with a number of positive outcomes. Initially, we were heavily engaged with the National Department of Health’s discussions around receiving public sector patients – Mediclinic participated in good faith, providing submissions on terms, fees and transparent disclosure of costs involved in the process. Discussions also included practical operations around admissions. An agreement was concluded for the Western Cape, but levels in our hospitals meant we seldom had capacity to accept additional patients.
Mediclinic joined together with other private healthcare providers in a facilities work stream under the Business for South Africa (B4SA) umbrella to work collaboratively and in support of the government-led pandemic response, with the Hospital Association of South Africa (HASA) providing coordination in meeting and enabling critical decisions to be taken in many rapidly unfolding areas such as the provision of personal protective equipment, testing, and ventilator availability.
Dr Biren Valodia, Chief Marketing Officer: Mediclinic Southern Africa and former HASA Chairperson, explains: ‘We also engaged through HASA on key issues affecting the
industry during the pandemic, knowing that a concerted response was critical. Within weeks of the first identified case in the country, HASA approached the Ministers of Health and Trade, Industry and Competition to ask them to facilitate increased flexibility in the system. Both ministers acted quickly and hospitals were granted permission to internally organise and increase bed numbers by redesignating licenced beds and re-circumscribing units to ensure they were up to the task of caring for large numbers of infected patients if and when required.’
He continues: ‘Another key contribution we made as part of the private industry was through the creation of a dynamic online platform that provided details of available COVID-19 beds around the country. With bed numbers and locations changing constantly during the waves, this tool was of great benefit for triage and the national pandemic response.’
Corné Heyns, Chief Strategy Officer: Mediclinic Southern Africa, explains why he feels these engagements were a success. ‘We actively demonstrated our willingness and readiness to assist, concluding agreements around fees and administration of public sector patients being admitted. We were keen to be part of the solution.’
Bob Govender, Industry Affairs Executive, believes that the discussions allowed various role players to strengthen relationships between sectors. This is essential for the success of the healthcare sector as a whole moving forward.
Early on in the planning for our COVID-19 response, Mediclinic recognised the importance of effectively communicating with our staff and giving them the right information. ‘This served to both reassure and protect them as the pandemic evolved,’ explains Dr Biren Valodia, Chief Marketing Officer: Mediclinic Southern Africa.
With so much fake news being shared on social media, Mediclinic sought to provide accurate information on personal protective equipment, infection prevention and control, and other areas that impacted how we did business. While information overload was a concern, targeted messaging was chosen to speak to different stakeholders within our business.
Reassurance messaging was not just important for our patients. As knowledge became available in our industry, we shared the facts and all relevant information with our staff, allowing them to be a voice of reason in their families and communities. Information was shared via emails, posters, screen savers, mobile channels and the Intranet.
An exciting introduction was the regular audiocasts where Executive Committee members made themselves available to answer questions within the business. Quick updates were given on where the business was and what they needed to communicate to staff, followed by SMS questions submitted by staff and addressed by relevant managers. This allowed staff to receive information first-hand on issues that concerned them.
Dr Valodia says, ‘As the pandemic evolved, we realised that another key area would be how we supported our staff through the pandemic. Teams and individuals were under enormous strain, and we needed to make the right resources available to help. The Care.Courage.Compassion campaign was launched, making the website mobile-friendly to offer resources touching on mental, emotional, physical and financial wellness. Contact details were offered to access various support channels, and counselling was made available at hospital level to manage any areas where our staff needed support. This was an essential tool to ensure that, whatever our staff members needed, help was available quickly.’
He goes on: ‘One inspiring channel we discovered was our patient recovery videos – sharing our colleagues’ successes in the COVID-19 fight. These were shared far and wide and really served to show how hard our teams were fighting for each of their patients.’ The celebrations inside the hospital were revealed on social media and, in return, the public began expressing their appreciation for the work.
A more serious part of our communication fell to recognising those colleagues we had lost during our fight. Through tributes, we were able to remember friends and colleagues with kindness, recognising how hard they had worked alongside us to fight the pandemic.
As the situation evolved, we were also able to start looking to the future. #OurBestShot became a call to action for staff to protect themselves by getting vaccinated, allowing them to act as an example to their family and greater community while at the same time protecting themselves against severe illness.
‘Above all, we recognise that our staff are the key to our success. They are the hands of care, and we appreciate each staff member in this journey, particularly during these unprecedented times,’ Dr Valodia says.

The corporate office nursing team looks back on the early days of the Covid-19 pandemic when a few colleagues in the clinical team thought that the rest of the world were exaggerating the impact of this disease and naivety was the order of the day. By the second week in March there was a daily 07:30 meeting of the ‘Corona Task Team’, so named by the CEO’s secretary, Marijke Kershoff, who has provided, and continues to provide, the glue between all the departments so solidly, day after day throughout the pandemic.
Initially, Riani Retief, Clinical Quality Specialist, led the nursing charge because of the logical clinical leadership she is so respected for, as well as the urgency of the policies and documents required in the Critical Care Unit and Emergency Centre space. Since her appointment to her position six years ago, she yearned to get back to the patient’s bedside. The pandemic finally taught her (and Louise Aylward, Nursing Operations Manager) to make peace with the fact that they can touch the lives of many more patients and nurses by doing what they need to do, i.e. developing and implementing the tools required to equip the nursing units.
Riani’s contribution will be remembered for her constant reminder to ‘do the most for the most’, whether in respect of the need to allocate scarce respiratory equipment or counselling the doctors who were battling with implementing critical care triage. She quickly realised that this pandemic had to be a team sport and, in her words, ‘Everyone on the COVID-19 Task Team moved heaven and earth to support our colleagues in every possible way. Nothing was too much and no idea or plan too complicated or expensive to consider.’
As the patient numbers grew, more gaps were identified in terms of specific pandemic requirements, and more members of the Corporate Office nursing team were drawn
in. One of the challenges the team has always faced is the fact that nurses are at the heart of most activities involving the hospitals and patients, and there simply are not enough hands for everything to be done. Whether it is Patient Experience, Human Resources, Patient Administration, Procurement or Infrastructure, nursing input is required in initiatives like providing electronic platforms for communication with families, volunteerism, admission documentation and decisions on which ventilators to purchase and where to place them.
From the outset, Louise and Aliné Hall, Clinical Quality Specialist, readily threw their efforts into assisting with the pandemic activities wherever there was a need. Aliné was particularly challenged as she tried to support her unit managers in providing safe obstetric care, allowing patients to enjoy these special events in their lives amid the pandemic where nothing was normal. Apart from assisting with all the digital initiatives where the nursing team had to provide input, arranging the COVID-19 documentation and advising on the Patient Experience initiatives, Louise equipped herself with new knowledge on palliative care, which she could use to support the hospitals.
As the nursing team worked mainly from home, 14-hour days and seven days a week became the order of their lives for many months, only letting up briefly between waves. Each day started with calls to check up on colleagues with COVID-19 and to see how the unit managers in the different areas were managing. Ultimately, the team frequently reminded themselves of the need to live one day at a time and that standing together would assist in making sure that they would get through whatever came their way. Amid the sad memories, the team will forever cherish their memories of the good times, particularly the patient, family, staff and doctors’ celebrations in the hospitals on discharge of the sickest patients, as well as the Jerusalema productions in the hospitals that were so uplifting for those teams.
It takes a special person to do the job of a nurse. You have to be strong enough to handle long hours and life-or-death situations, as well as soft enough to care for patients with a sensitive and gentle touch. Nurses who defined being both strong and soft were nominated and stories were shared showcasing how they embody both these qualities. Congratulations to all nominees and the winners of 2020.

Suzette Burmeister Professional Nurse Mediclinic Bloemfontein


Marlize Liebenberg Enrolled Nursing Auxiliary Mediclinic Durbanville and Mediclinic Durbanville Day Clinic

Dineo Masemola Enrolled Nursing Auxiliary Mediclinic Heart Hospital

Vibin Varghese Senior Professional Nurse Mediclinic Kimberley and Mediclinic Gariep

Madeleine Vorster Enrolled Nursing Auxiliary Mediclinic Brits

Lizel Roeloffze Clinical Facilitator Mediclinic Emfuleni

Carryl Anne Oosthuizen Enrolled Nursing Auxiliary Mediclinic Hermanus

Ann Williams Enrolled Nursing Auxiliary Mediclinic Klein Karoo

Blanche Peens Clinical Facilitator Mediclinic Cape Gate

Sicelo Mate Enrolled Nursing Auxiliary Mediclinic Ermelo

Phelma Moagi Enrolled Nursing Auxiliary Mediclinic Highveld and Mediclinic Secunda

Poppie Moloisi Enrolled Nursing Auxiliary Mediclinic Kloof

Sethembile Makhanya Professional Nurse Mediclinic Cape Town

Emmerentia Erasmus Professional Nurse Mediclinic George and Mediclinic Geneva

Brenda Henley Smith Patient Safety Manager Mediclinic Hoogland

Sibati Ledwaba Enrolled Nursing Auxiliary Mediclinic Legae

Leach Professional Nurse Mediclinic Constantiaberg

Kgatuke Enrolled Nursing Auxiliary Mediclinic Gynaecological Hospital*

Joyce Nkala Professional Nurse Mediclinic Howick

Tebogo Motupa Enrolled Nursing Auxiliary Mediclinic Lephalale

Rina Maleka Professional Nurse Mediclinic Limpopo and Mediclinic Day Clinic

Joanne Madeley Unit Manager Mediclinic Morningside

Ashleen Titus Professional Nurse Mediclinic Paarl


Lorraine Cameron Enrolled Nursing Auxiliary Mediclinic Sandton

Cornelia Potgieter Patient Safety and Infection Prevention and Control Manager Mediclinic Tzaneen

Elisa Makhooe Enrolled Nursing Auxiliary Mediclinic Welkom and Welkom Medical Centre

Ziyanda Fokazi Professional Nurse Mediclinic Louis Leipoldt

Athira Gopalakrishnan Professional Nurse Mediclinic Muelmed

Ralph Lekay Enrolled Nursing Auxiliary Mediclinic Panorama

Carina de Kock Nurse Educator Mediclinic Southern Africa Learning Centre

Emmie Jacobs Professional Nurse Mediclinic Upington

Maria Nakambunda Unit Manager Mediclinic Windhoek
*Before closure in November 2020

Mpho Ditshego
Enrolled Nursing Auxiliary Mediclinic Medforum

Yolyn Segopane Senior Professional Nurse Mediclinic Nelspruit

Monde Nduku Professional Nurse Mediclinic Pietermaritzburg

Nontando Matulela Enrolled Nursing Auxiliary Mediclinic Stellenbosch, Mediclinic Stellenbosch Day Clinic and Winelands Orthopaedic Hospital

Riekie Holder Clinical Facilitator Mediclinic Vereeniging

Nardia Molaoa Molosiwa Infection Prevention and Control Manager Mediclinic Midstream

Joyce Dananai Matsikidze Registered Nurse Mediclinic Otjiwarongo

Thea Ferreira Professional Nurse Mediclinic Plettenberg Bay

Tanja Fischer Unit Manager Mediclinic Swakopmund


Abronise van Rhyn Enrolled Nursing Auxiliary Mediclinic Worcester

Mandy du Plessis Senior Professional Nurse Mediclinic Milnerton

Zarina Ali Enrolled Nursing Auxiliary Mediclinic Newcastle and Day Clinic

Valencia Campbell Senior Professional Nurse Mediclinic Potchefstroom


Anmari Lourens Senior Professional Nurse Mediclinic Vergelegen and Mediclinic Strand

Maureen Mothobekhi Senior Professional Nurse Wits Donald Gordon Medical Centre
Bongi Mogweng Enrolled Nursing Auxiliary Mediclinic Thabazimbi




Melanie Govender Professional Nurse Mediclinic Victoria

Masike Professional Nurse Mediclinic Brits

Thandiwe Ramathibela Professional Nurse Mediclinic Emfuleni


Solomon Mahlangu Professional Nurse Mediclinic Highveld

Eunice Malinda Enrolled Nursing Auxiliary Mediclinic Lephalale

Nathi Ntshangase Professional Nurse Mediclinic Morningside

Jobin John Senior Professional Nurse Mediclinic Cape Gate and Mediclinic Cape Gate Day Clinic

Valentia Ndisina Enrolled Nursing Auxiliary Mediclinic Ermelo

Jenee Wanliss Clinical Facilitator Mediclinic Hoogland

Mancha Mothomogolo Enrolled Nursing Auxiliary Mediclinic Limpopo

Tondi Mashele Enrolled Nursing Auxiliary Mediclinic Muelmed

Williams Professional Nurse Mediclinic Cape Town

Genevive Carelse Clinical Facilitator Mediclinic George and Geneva

Bongiwe Hlongwane Professional Nurse Mediclinic Kimberley and Mediclinic Gariep

Sane Tshabalala Professional Nurse Mediclinic Medforum

Sibeko Professional Nurse Mediclinic Nelspruit and Mediclinic Nelspruit Day Clinic

Brits Unit Manager Mediclinic Constantiaberg

Edwin Chepape Professional Nurse Mediclinic Heart Hospital

Mpho David Tshepang Mphuthi Professional Nurse Mediclinic Kloof

Mataboge Unit Manager Mediclinic Midstream

Ngubeni Professional Nurse Mediclinic Newcastle

Nurse Mediclinic Durbanville

Krishna Pai Professional Nurse Mediclinic Hermanus

Nkambule Enrolled Nursing Auxiliary Mediclinic Legae

Peter Enrolled Nursing Auxiliary Mediclinic Milnerton

Mudadi Registered Nurse Mediclinic Otjiwarongo











Elize Powell Learning Centre Manager Mediclinic Southern Africa Learning Centres









WE LOOK AT HOW SOME OF OUR HOSPITALS RESPONDED TO THE CHALLENGES BROUGHT ON BY COVID-19.

By Louise Aylward
Lynette Louw, retired Nursing Manager of Mediclinic Pietermaritzburg, nominated Clinical Facilitator Suzan Mntambo who ‘is definitely an extraordinary person’. Yet, Suzan commends the leadership of her hospital, who showed their trust in her and the team. ‘This boosted our confidence. The Critical Care Unit (CCU) team was very involved in the preparation for the first wave,’ Suzan says. ‘We used guidelines from the Corporate Office team to plan our response, discussing possible scenarios and writing protocols, while nursing procedures were tested and changed.’ What stood out for her was the teamwork: ‘Help was always there to address practical issues. It sounds like I am including everyone, but everyone was involved,’ Suzan continues, listing the CCU, Emergency Centre (EC) and Medical Unit managers, CCU staff, doctors, as well as technical, patient safety and
infection prevention and control managers. ‘We felt that we were trusted and our views valued despite having to be upskilled ourselves.’
She is confident that they are better prepared to handle further waves of infections
When the Cardiac CCU had an outbreak, a number of staff, including the Unit Manager, were isolated and Suzan was asked to manage the unit during this stressful time. ‘It was during this period that this helpful, competent and disciplined practitioner’s leadership qualities became even more pronounced,’ Lynette explains. As the CCU staff returned to work, she assisted in the medical unit to upskill the staff, while nursing highdependency patients. ‘Yet,’ Suzan explains, ‘when we wanted to roll out the hospital training programme, I realised that the staff were not ready to be trained. They were fearful, and myths and fake news abounded. I


realised that staff needed listening to, and their questions answered, to allay anxieties.’ Managing her own fears amid the unknown, she made an effort to understand the science of COVID-19, specifically with the support of Riani Retief, Clinical Quality Specialist, and Dr Richard von Rahden, Intensivist/Anaesthesiologist.
Lynette says: ‘This humble individual unfortunately got infected and was nursed in our CCU for eight days.’ ‘I was terrified,’ Suzan says. ‘I went to the EC, where I received care for 12 hours while awaiting a bed in the CCU. I refused to be admitted to another hospital but my own. I had full confidence in the systems and skills that my team helped establish.’ Thinking of the upskilled registered nurses caring for her, Suzan was reminded of the words of Mrs Bomvana, her CCU tutor at the Chris Hani Baragwanath nursing college, encouraging her to ‘pull the others in the class with her’ to also do well in the exams. ‘One day you will need them, when you are the patient in the CCU bed.’
Encouraging her colleagues, Suzan reminded them that they had done it before without prior knowledge and experience. She mentions her Nursing Manager referring to HIV as an example: ‘Initially, we were all terrified of HIV, but look where we are now.’ Although staff are emotionally and mentally fatigued, she is confident that they are better prepared to handle further waves of infections.

By Aliné Hall
Sizakele Mlotshwa, Unit Manager of the Hepato Renal Critical Care Unit (CCU), and Vanessa Moodley, Unit Manager of the Medical CCU at Mediclinic Wits Donald Gordon Medical Centre (WDGMC), were interviewed together. We chatted for well over an hour, which can be summed up as: ‘Why me?’, isolation and lockdown, fear, resilience, and teamwork.
COVID-19 did not arrive at WDGMC as early in the pandemic as at other Mediclinic hospitals. Preparations began and worst-case scenarios were discussed. Vanessa says when she was told she would be in a COVID-19 area, her first thoughts were: ‘Why me and my unit?’ The initial isolation came with fear – fear of the unknown, fear for one’s own

wellbeing and of one’s families. The wait between COVID19’s coming and for it to get to WDGMC was long; a time in which to be anxious and wonder what it would bring. Both say the questions in their heads were: ‘How can I tell my staff to do something when I am afraid and do not know myself? How will I make them okay when I am not okay?’
Initially, the social distancing felt like seclusion away from everything that was normal work behaviour, such as daily meetings, chatting in tea rooms and moving around with no cares. Now it was masks, visors, learning to don and doff, and isolation from your colleagues and friends. In this time, Vanessa lost her best friend at work when her colleague emigrated. She said it felt like her umbilical cord

They were grateful to the nursing profession for their jobs

had been cut. Despite the isolation from each other and familiar routines, they felt the COVID-19 changes actually brought everyone closer together.
‘COVID-19 taught us to actually get to know the strengths and weaknesses of each member of the team; it was an opportunity to really get to know your staff.’ They became a close-knit team and more aware of each other’s needs, all pulling together on the same journey.
Both mention the comprehensive mental and social care of the WDGMC management team and, in particular, Deputy Nursing Manager Hester Swart. Alternative meeting places were found for the ability to socialdistance but still be able to see each other, and that was comforting. Tea times now consisted of a walk outside, which became essential for their mental wellbeing. After an uncertain start, life as they knew it was gone and life in a COVID-19 pandemic became the new normal.
When asked whether there was anything positive she could take from COVID-19, Sizakele immediately relates that their hospital-acquired infection (HAI) rate went to zero. It took a while to realise the HAIs were gone in the face of heightened hand washing and increased infection prevention and control principles. In all the fear and change, there was a lesson to learn.
Vanessa says she gained confidence in her staff, feeling a little like a bird throwing her fledglings out of the nest. She
was forced to grow and gain confidence in her role as Unit Manager, and delegate and trust that the work would be done. She sees now that before COVID-19, she would check and oversee everything the staff did, while now she had to let them go and they flew.
In addition to the management team, two doctors stood out for them. Dr Gitti Bertelsmann, who worked in the COVID-19 CCU, checked on all the staff daily, chatted to them, and allayed their fears. She also reported back to the Unit Managers if she felt someone was in trouble and needed more help. And Dr Gunther Schleicher – in his normal manner – ensured everyone knew what was happening and what was expected of them. Both Sizakele and Vanessa note his interactions and continuous updates to the family of each COVID-19 patient. They also say how important closure was for families. Sizakele recalls assisting a family member with the donning and doffing and explaining the process to them, when they came in to say farewell to a patient.
They both say they are grateful to the nursing profession for their jobs, in uncertain times. At the end, they say talking about it had actually been cathartic, showing them what they had accomplished and accomplished well. When discussing the negatives of COVID-19, they both quickly go back to the positives they could take away, sometimes surprising themselves that in looking back, they had done well for themselves, their staff and their patients.
By Riani Retief
When Mapule Maria Dlamini arrived for her first day at Mediclinic Legae as Deputy Nursing Manager on 15 July 2020, she had no idea of the roller coaster ride that she was about to face. Her first day at the hospital was the first time she had actually seen the inside of the hospital, and without really knowing anyone, except for Matlhogonolo Segale, this was quite a journey. Her Mediclinic Legae journey started during COVID-19, during a time when the Nursing Manager fell ill, the Infection Prevention and Control Manager was in isolation and the Patient Safety Manager was on maternity leave. Despite it being a challenge, her overwhelming feeling was that of excitement. Reflecting on those early days, she is happy and proud to have been part of such an amazing opportunity to not only learn with the team, but also to lead them. ‘God’s timing is perfect, as He groomed

me for this position and placed me there for the experience and the growth, masterfully so. I am forever grateful for the way the team at Mediclinic Legae took me in and accepted me during those very trying times.’
Matlhogonolo started the COVID-19 journey as the Unit Manager (UM) of the Surgical Unit. During this time, SPN Thandi Radebe (at that stage acting UM) fell ill with COVID-19, and was admitted to her own Critical Care Unit (CCU) where she was nursed until she passed away on 25 July 2020. Matlhogonolo still remembers the day Thandi passed away as if it was yesterday. She clearly remembers the way in which everyone just got together. Matlhogonolo kept a watchful eye over both the Surgical Unit and CCU while Thandi was critically ill and was appointed as the new UM of the CCU in August 2020.


There was so much happening during the wave. You got up in the morning, went to work, and before you knew it, the whole day had passed in what felt like a fleeting moment. They worked with minimum staff, everyone just pushing through and doing their best for the patients.
‘COVID-19 brought along a silent fear that crept into people’s minds and I decided early on that I would not surrender to this fear. I will do my best despite all the doubt and the uncertainty.’ While trying to do everything in her power for her new team and the patients, the pandemic found a way to get to her. One morning at 02:00, she got up to go to the bathroom, and there, on her own, she just started to cry, not really knowing why. But suddenly, the pressure and all the trauma that she had endured with COVID-19 came
Despite it being a challenge, her overwhelming feeling was that of excitement
washing over her. Her husband and two children sat with her until she managed to work through the storm and, for the first time since the beginning of COVID-19, she felt at ease. She is forever grateful to her family who allowed her to let go and created a safety net for her.
Mapule Maria and Matlhogonolo are not only grateful for their blood family who encouraged them through this turbulent journey, but also their work family, who were incredibly supportive and did everything humanly possible to do the best for the patients and team at Mediclinic Legae.
Thank you Mapule Maria, Matlhogonolo and every single person working at Mediclinic Legae for everything you did during the COVID-19 pandemic. We salute you.
By Riani Retief
Mediclinic Midstream’s COVID-19 journey was like many of our other hospitals – one of turbulence, but with the added chill factor of our own staff ending up in the Critical Care Unit (CCU). Their story starts with Tauhierah Tavares, Deputy Nursing Manager (DNM). According to Dr Shane Kotzé, Hospital General Manager: Mediclinic Midstream prior to her own illness, Tauhierah took it upon herself to be the embodiment of the nurses’ pledge: ‘She facilitates family visits for our dying COVID-19 CCU patients through the windows of the unit; she calls the families to allow them to say goodbye and she holds the hand of the dying patient to ensure that the family has comfort that their loved one doesn’t die alone. I don’t have words to express this humility.’ Not only did Tauhierah do the coordination with family members, she also functioned as a stand-in Unit Manager: being a runner in the CCU, mixing medication and getting staff, equipment and other very scarce resources. On 13 August 2020, her life changed in a way that she had never imagined. During the course of the day she realised that her voice sounded funny. She went to her Nursing Manager, Diane van Schoor, who confirmed the changes to her voice. Tauhierah went for her COVID-19 test, then home and off to bed. Waking up from that nap, she realised that something was going on. She felt substantially worse than before, and later that day her test results came back positive. She was admitted to the unit later that day, but moved to the CCU that night. Little did she know that she would only see her home again on 20 November 2020.
With Tauhierah in hospital, Elana Lamprecht, Emergency Centre Unit Manager, went to Diane to offer her services to assist wherever she could. She was appointed as acting DNM and fell right in where Tauhierah had left. With Midstream’s second wave, things were dramatically worse. The hospital phoned Elana on 25 December 2020 to ask for assistance, as the EC was totally overwhelmed – the very day that Avril Kundasamy, Financial Admin Manager, (who later passed-away) was admitted. Elana helped to sort out the constant influx of patients, getting more staff and much-needed equipment. On 2 January 2021, she started feeling ill, and was admitted the next day. She was blissfully unaware that she, too, would end up on a ventilator.
Liz Dunstan, who had been appointed as CCU Unit Manager in the meantime, walked into a 15-bed CCU with 15 ventilated COVID-19 patients. And everything was new: a new role, new staff and a new virus creating havoc throughout South Africa. Liz saw this as her opportunity to create stability, strength and clinical objectivity for her team. When asked about the one thing that will stay with her for the rest of her life, she mentions ‘the day Tauhierah went to rehab. The staff formed a guard of honour to the ambulance that did the transfer, singing, dancing and celebrating her life. At that very moment, I realised exactly how fragile life is.’


Diane van Schoor, Nursing Manager, started her career at Mediclinic in January 2020 after 30 years at another private hospital group in South Africa. Once there, things happened very quickly and she realised that they were all in uncharted waters. The one thing that stands out for Diane is the amazing team that she walked into, and that nothing was ever too much to ask. They surrounded her with support and they all adapted quickly to the constantly changing goal posts.
I realised exactly how fragile life is
‘Even though this was an uphill journey, we’ve learned so much. We’ve learned how to care differently. Suddenly, your smile and eyes were not visible anymore, so we had to think how we can still care in a way that’s different.’
Thank you, Tauhierah, Elana, Liz and Diane, for stepping up and leading your teams through the storm despite multiple tsunamis.
By Riani Retief
Writing articles for this journal has been one of my favourite activities. To hear their stories, and see the emotion wash over their faces, has deeply touched me. What a privilege to meet the two people whose stories I am about to share. During the interview, there was just so much energy and I could feel their warmth and compassion, albeit across 1 692km and through a computer screen.
Samson Modiba has worked at Mediclinic Limpopo for the past seven years and four months. He is an Enrolled Nursing Auxiliary (ENA), and is currently working in the Medical Unit. According to Matlou Sathekge, Nursing Manager, Samson is a role model and patient experience champion. Patients’ basic needs are his priority, and no patient will ever be dirty, uncomfortable or untidy when he is around. This was

constantly true during the COVID-19 pandemic. The one thing that he did without fail was to keep on doing the little things for patients, like mouth care. ‘You know, the patients are struggling to breathe – all different forms of oxygen devices, but I tried to keep their mouths clean and fresh to make it easier for them.’ For Samson, it was all about being brave, being present and taking each day as it came. Teamwork, learning and adapting, togetherness, and perseverance despite the fear are but a few of the things that will always stand out for him when thinking back on those times.
Isaac Mashigo is also an ENA and works in the Surgical/ Orthopaedic Unit. Looking back on the pandemic, Isaac remembers how they quickly learnt to ‘see’ the sick COVID-19 patient when they came into the unit. For someone who is usually looking after medically healthy

I am proud of myself – I stood my ground despite being scared

patients who undergo surgery, this was quite new. ‘We had to learn quickly how to look after these patients and all the different machines. And together, we were not only a team, but we became friends who supported each other through the difficult days.’ Isaac is not only a team player with his colleagues but is also well known for the way in which he can reassure anxious patients, and therefore it is not uncommon for patients to speak highly of his compassionate demeanour. Add to this his smile that
is one of his trademarks and you will understand why he was nominated for this interview.
Samson says, ‘I am proud of myself. I stood my ground despite being scared.’ What a privilege to know that we have these special souls around us as part of our nursing family. Thank you, Samson and Isaac, for making us proud to be nurses – you are true heroes. We are so grateful for the stability that you bring to the rest of us.
By Louise Aylward
Mirinda Coertzen, Nursing Manager of Mediclinic Durbanville, says, ‘During this pandemic, we saw everybody taking strain and struggle to cope with the unknown.’ With some knowledge but very little experience, their admitting physician team decided to form proning teams to work more effectively to conserve personal protective equipment, to ensure the safety of the patient during this high-risk procedure, to be respectful of the time it took everybody involved and to limit the exposure of staff and doctors to infected patients.
This meant that proning happened at a set time in the Critical Care Unit, and the team, including nursing staff, doctors and physiotherapists, would move from patient to patient and turn them as needed.
Proning is the process of turning patients with precise, safe motions onto their stomach. This position allows for better expansion of the back lung regions and enhanced removal of secretions which may ultimately lead to advanced breathing.
Very soon, Careworker Lushandre Jordaan emerged as the counter, directing the team by counting out loud to synchronise their actions while watching over the safety of the patient, tubes and devices. A proning master recipe was developing.


Renay Jacobs, Senior Professional Nurse, remarks: ‘We learnt to figure things out together, as a team. And with Lushandre’s counting and leading, we are like an oiled machine.’
The next ingredient was music. One morning, Professional Nurse Danielle Veldsman turned the volume up on her cell phone and ‘Pens en Pootjies’ by Snotkop set the proning tone. Everybody had a good laugh. ‘Our spirits were lifted and proning became a fun event.’ This song became the call to the proning round, even convincing some resistant patients to take part to ‘draai en swaai’. A very precious camaraderie was developing.
If I may choose only one positive aspect to keep post COVID-19, it would be the teamwork and respect for each other
Dr Pierre Tredoux, Physician, agrees that the pandemic situation was extremely emotionally taxing. It stands out for him that everyone worked as a team, was equal and
knew their roles. ‘We got to know and appreciate our colleagues in these difficult times. We see when a colleague is ‘off’ and pull them aside; listening, encouraging and praying. We know this is a temporary situation; this too will pass. We’ll get the strength to get through this.’
What inspires them? Renay says, ‘Knowing we did this and can do it again. We rely on the team – checking on each other to put safety first, to work away the pain, to encourage, to sing together.’ Dr Tredoux adds: ‘It’s so rewarding to celebrate the discharge of a patient we cared for.’
Mirinda says: ‘If I may choose only one positive aspect to keep post COVID-19, it would be the teamwork and respect for each other. It was humbling to see.’
By Louise Aylward
Behaviours such as walking the extra mile, an affinity for helping and teaching (staff and patients), and being exemplary, knowledgeable and flexible were mentioned in the nominations for Blanche Peens when she was awarded the Nursing Excellence Award in 2020. At that time, she was still a Clinical Facilitator. She was recently appointed as Obstetrics Unit Manager at Mediclinic Cape Gate. Her journey over the past several months highlights the vulnerability she experienced, and the caring colleagues who stepped in to assist during difficult circumstances.
Despite increasing COVID-19 admissions and hectic shortages in the Critical Care Unit (CCU), she rose to the challenge and mastered her fears by doing the CCU upskilling programme. She was terrified at first, but willing
and eager to learn. The appreciation showed by the CCU team was encouraging, while the group who participated in the upskilling programme pulled together for mutual support; they understood what their mates were going through. This made the CCU challenge easier, and Blanche was soon one of the Professional Nurses (PNs) the team requested to be placed there.
Blanche remembers her first ‘talking’ CCU patient very well. The patient wanted to go home to bury her husband, who had died due to COVID-19 a few days prior. She had refused to put her CPAP mask back on, despite decreasing saturation levels. In a state of panic, Blanche called on PN Leandro Storm, who was able to remedy the situation, talking calmly with the patient and eventually convincing her to wear her mask. Sadly, the patient died in the next few days.

Blanche needed to be isolated from her elderly parents for months – the longest time ever – due to concerns of COVID-19 infection. ‘It caught up with me when I had to nurse an elderly man with my father’s name, John, who was ventilated. I broke down in tears.’ Bernie Maralack, Night Manager at that time, provided her with a kind, understanding shoulder to cry on.
When the wave subsided, reallocated staff looked forward to returning to their home units. Nevertheless, the training staff were still allocated to other units. It was emotionally taxing to accept yet another new challenge, this time as acting Unit Manager of the Obstetrics Unit.
Wide-eyed and anxious, but willing to develop further, she was kindly guided by Nursing Manager Ray Husselmann and the nursing management to develop in this role.
‘I was raised to adapt and cope under all circumstances; yet, I needed additional help to cope during the past months,’ says Blanche. ‘I was not the person I used to be.’ She describes the random calls from Human Resources colleagues inviting staff to individual counselling sessions, the psychologist placed in the CCU; and group sessions by Anlé D’Emiljo, Organisational Effectiveness Specialist, which provided a safe environment to talk.
Her journey shows what an individual can achieve when surrounded by caring colleagues who are ready to help but also open to receiving help and support.
Blanche’s advice to colleagues? ‘Keep calm; you don’t always have to be perfect. And keep checking on each other to ensure everyone’s safety.’

By Aliné Hall
Working in a smaller hospital, the units often cover many different disciplines. Marcia Izatt initially led the Surgical Unit, which included maternity, neonatology, gynaecology, urology, and general surgery. At the beginning of the COVID-19 pandemic, the hospital was divided into COVID-19 and non-COVID-19 units. Paediatrics, neurosurgery and orthopaedics were added to her unit

and she became the leader of all non-COVID-19 units Marcia is a very positive, energetic person and a passionate midwife, who grasped this new challenge with enthusiasm.
Marcia repeatedly mentions teamwork – COVID-19 taught them to work as a team. She had a young team working in their very diverse unit of many different disciplines, including an occasional high-care patient, and had to also factor in all the PUI (patient under investigation) patients, with some testing positive. Knowing that nurses do not like mixing disciplines, initially she had to motivate them daily and eventually found there was a growing pride in them and a feeling of ‘We can do this.’ Working 18 or even 24-hour shifts during December and January, often with minimal staff, was done as a team, and if one offered to work late, they all did. The obstetricians and paediatricians worked with them, feeding and changing babies, doing observations. Together, the team managed whatever was thrown at them. This made them work better as a team. The nurse and doctor shared the same experience, and there was more freedom of speech. In true midwife spirit, she says it was like going through childbirth. After you managed labour and the delivery, you feel you can manage anything.
When asked what changed for the better due to COVID-19, this was an immediate answer: technology and fewer meetings.
COVID-19 also took its toll, seeing mothers deliver alone with no partner in the beginning, watching people die alone with no family, watching your colleagues in the COVID-19 unit surrounded by critically ill patients. Initially, seeing the fear in the staff and their first time contact with COVID-19.
To motivate and encourage the staff every day, Marcia would give them a number to pick, and this was linked to a Bible verse they would read together. Sometimes they needed to pick a few numbers until everyone felt calm and ready to face the shift.
From a reluctance to nurse all the disciplines, there is a reluctance now to return back to the ‘normal’ units.

Marcia repeatedly mentions teamwork –COVID-19 taught them to work as a team
By Caryn Ross
Dr Ighsaan Carr, Specialist Physician and head of the COVID-19 Clinical Response team at Mediclinic Constantiaberg, believes that teamwork and communication were the basic tenets of their hospital’s successful response to the pandemic. ‘For many years, we have operated a successful Antibiotic Stewardship Programme (ASP) where clinical cases, particularly focusing on infections, are discussed. This ASP includes physicians, paediatricians, microbiologists, clinical pharmacists, laboratory support staff, and our nursing team leaders,’ Dr Carr says. ‘We developed a solid working relationship over the years, which formed the basis of our COVID-19 pandemic response.’

Dr Carr believes that the dedication of every doctor, nurse, pharmacist and allied healthcare worker, along with non-clinical support staff in various departments such as administration, maintenance, cleaning and security, resulted in the successful team strategy. Mediclinic Constantiaberg’s COVID-19 clinical response was led by their core hospital committee (HMIMS committee), a unique COVID-19 disaster management team led by the Hospital General Manager and representatives from each clinical and non-clinical division.
‘The backbone of our multidisciplinary COVID-19 teams was formed by the army of highly skilled and extremely dedicated nursing staff at Mediclinic Constantiaberg, particularly those working in the dedicated COVID-19 Critical Care Units (CCUs) and other nursing units. This was supported by various teams. Clinical teams involved with the management of COVID-19 patients include an Emergency Medicine doctor team in the Emergency Centre, a specific on-call CCU and an Airway Team roster, consisting of a specialist physician with two to three anaesthetists. Similar multidisciplinary teams were set up for the COVID-19 unit’s patient management, each team being led by a physician. Others included our teams of dieticians, physiotherapists, speech therapists, pharmacists and volunteers. Each knew their core responsibilities and were focused on serving our acute patients both in the COVID-19 dedicated CCUs and general COVID-19 units,’ he explains. A team of psychiatrists and psychologists ensured their healthcare worker teams were coping emotionally and psychologically.
‘An ethics committee was comprised of specialists, general practitioners, religious leaders and other key representatives to ensure we could make the right decisions regarding escalation and de-escalation of care. These were crucial for those ethical challenges encountered during the pandemic,’ Dr Carr says.
‘Clinical support by TEST teams, which were independent specialists tasked to objectively assess the management of complex COVID-19 patients, allowed for independent assessment of cases. These created a foundation of support, reassurance and confidence in the healthcare

workers on the front line, resulting in the best care within the circumstances they were facing,’ he explains. ‘All of the above multidisciplinary teams and the treatment protocols were set out in a unique booklet created specifically for our hospital, called the Mediclinic Constantiaberg COVID-19 Clinicians’ Response (2020-2021).’
All teams and committees communicated via dedicated channels (e.g. WhatsApp groups and emails), along with committee meetings. This was bolstered by a well-attended weekly academic COVID-19 online symposium, specifically focusing on the COVID-19 pandemic data.
community members often convened at hospital entrances to convey messages of support and prayers. This created a true sense of community and a united front.’
Dr Carr says this teamwork and dedication was the reason they could successfully manage two separate streams of patients, concurrently managing COVID-19 and nonCOVID-19 patient loads. Specialty silos were broken down. Every clinical and nonclinical role player had important roles to play. Communication remained a vital part of steering the management plan.
This created a true sense of community and a united front
Understanding and appreciating every team member’s opinion and experience during the COVID-19 pandemic fostered ongoing relationships within the hospital environment.
Dr Carr continues: ‘There were so many people that helped us. Volunteers from our community, General Practitioners and other specialist doctors volunteered to work in our COVID-19 CCUs and units alongside our nurses to deliver care during the different waves. Religious groups and
Dr Carr emphasises, ‘We had a strong, integrated foundation to start with. Our network was there – we just had to learn how to use it the best way possible. Teamwork. Sharing. Communicating.’
By Caryn Ross
The approach at Mediclinic Swakopmund was quite different from many other hospitals. Dr Wolfgang Tietz, representing private practitioners in the community, explains the close cooperation between Mediclinic Swakopmund and Welwitschia Hospital, another local private hospital. The process stalled for a period as the private sector awaited permission from the Namibian government to treat COVID-19 patients. Once this was granted, a strong working relationship allowed the hospitals to separate and delegate streams of patients.
Dr Tietz views this collaboration in the private sector as a key success of their response in the region.
A voluntary doctors’ group was formed and treatment protocols were quickly established with the assistance of one of the local physiotherapy practices. This dedicated team of doctors working at Mediclinic Swakopmund made the team’s task easier to manage due to the consistency of



the doctors. Doctors incorporated the Unit Manager of the CCU, Tanja Fischer, in the morning rounds to quickly identify patients who were improving or likely to deteriorate.
She believes that the team members enjoyed a positive working relationship, allowing humour to relieve the stress. A tight apron was met with a jovial ‘Flatten the curve,’ an attitude that was shared with the patients they assisted. Dr Tietz also feels that open communication and cooperation were key to their response.
leave. This was truly appreciated by all the staff and doctors,’ Tanja says.
Emiley Niilenge, Unit Manager of the Emergency Centre and Surgical Unit, says they had to adjust their ways of doing things as the Surgical Unit managed all non-COVID-19 patients since the traditional Medical Unit operated as a dedicated COVID-19 unit. She says this was a huge challenge for her, but they overcame it.
me to be upfront with patients and to discuss their fears
‘There was a lot of fear amongst the staff as the pandemic arrived, but I think this was overcome quickly. Staff adopted and embraced COVID-19 and infection prevention and control protocols, which in turn made them feel more motivated to support patients and worried family members,’ explains Helga Richter, Unit Manager of the Medical and Paediatric Unit. ‘Daily updates to designated family members was a great communication tool to support families.’
Teams in the COVID-19 unit were boosted by theatre staff, allowing more hands to take care of the workload. Emergency units created outpatient areas to assist with the correct flow and treatment of patients. ‘Corporate Office support was essential, and Riani Retief, Clinical Quality Specialist, was invaluable in helping me with equipment we had not used before. Our Hospital General Manager, Peter Sander, also came on a daily basis during the December holidays to see how we were coping, even though he was on
Tanja shares that ‘this experience taught me to be upfront with patients and to discuss their fears, while I was kneeling in front of their beds with them in a prone position. Patients were so willing to share their emotions and fears. It made me realise what a big responsibility we have managing patients’ physical and emotional wellbeing.’
Emiley says she saw the success of the hospital in patients recovering and walking out of the hospital. ‘We witnessed a lot more recovery than death.’ Helga agrees, saying: ‘The appreciation and happiness of family members and patients gives us the feeling that our task was accomplished with a positive outcome.’
Dr Tietz believes that his retirement in October 2020 was eased with the role he was able to play during the pandemic. He also believes that the medical profession, with the clinical expertise that has been gained, should play a pivotal role in the continued response in the country. We wish him well and thank him for his efforts.
The uniqueness of each hospital’s response has created a precious legacy. We look at how they triumphed, celebrated and mourned.

Employees of Mediclinic Panorama celebrated each long-term critical care COVID-19 patient who was discharged with a red carpet celebration and a guard of honour.

Panorama took part in the worldwide Jerusalema
challenge. Lots of fun, exercise and laughter for all.

officially unveiled a memorial bench
feel the need for some reflection and

Mediclinic Panorama celebrated staff, doctors and auxiliary and contract service workers who were COVID-19 survivors with a leaf on the Tree of Hope.
From left: COVID-19 survivors Almarie Hendricks (Unit Manager: Medical and Oncology Unit) and Ursula Verrooi (Unit Manager: Critical Care Unit).

Mediclinic Panorama’s employees and doctors were invited to sign a commitment to fight the COVID-19 pandemic as a team. Riaan Vorster (Hospital General Manager) was one of the first to pledge his commitment.
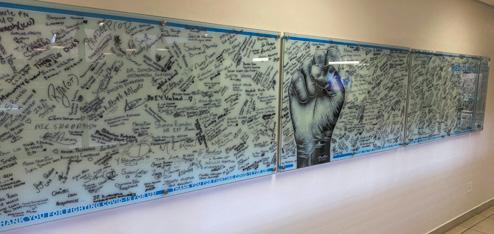
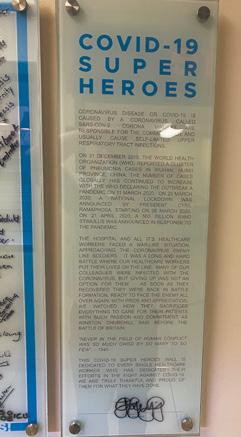
After the




Before the COVID-19 pandemic, Mediclinic Klein Karoo used 15 oxygen cylinders per week. But, during the COVID-19 waves, the demand increased to 15 cylinders every six hours. Ensuring a safe and constant oxygen supply was certainly one of the greatest challenges at the hospital. Besides the frequent loadshedding, during which a technical staff member had to be on-site, they also had to manually facilitate every cylinder bank change, whether during the day or at night.

Hannes Stegmann (Hospital General Manager) and Andrie Wiese (Nursing Manager) of Mediclinic Klein Karoo with the COVID-19 Tree of Hope in the hospital’s main corridor, which symbolises all the lives saved at the hospital during the first wave (as at August 2020). This is a visual reminder to all employees and patients that we can and will beat the virus.

Among all the daily challenges, Mediclinic Klein Karoo’s theatre employees kept their spirits high and were willing to adapt by working in the COVID-19 units when required.
From left: EN Jacky Opperman, SPN Christa Serfontein, Maria Wagener (CSSD Technician), ENA Ronel Southey, ENA Magda Claassen, Herculine Vermaak (HR Practitioner), EN Gleneaze Rabie, PN Danika Kleyn, PN Hanna Strydom and Hannes Stegmann (Hospital General Manager)



hospital activities of daily life during the COVID-19 pandemic, acknowledging the team’s contributions to show that everyone matters.

The Oudtshoorn community came together to pray for the employees, doctors and patients of Mediclinic Klein Karoo on several occasions. Seeing how the community appreciated all the hospital’s hard work provided encouragement and lifted employees’ morale.


Mediclinic Potchefstroom created its own COVID-19 Tree of Hope and held three different ceremonies for it. The employees (and contractors) who had tested COVID-19-positive and recovered (which were all of them) were each given a green leaf to sign and received a certificate of appreciation. They then placed their leaf on the tree. The hospital held a separate ceremony for all employees who had stayed healthy and supported their ill colleagues and patients. They were all given a water drop to sign and place on the wall. The final ceremony was for the volunteers who had supported the hospital in various capacities – they were given either a white or pink blossom to sign and place on the tree. They also received a small gift and a certificate of appreciation.

Johan von Wielligh, a COVID-19 patient who had been on a ventilator in Mediclinic Paarl’s Critical Care Unit (CCU) for 29 days, made a wonderful recovery and came back to the hospital to show his gratitude to the employees who had ‘helped save his life’. He thanked them for the ‘enormous task they’re doing under very difficult circumstances’, adding that it could only be possible because nursing was their true calling.





behind
Assistant: Medical Unit).
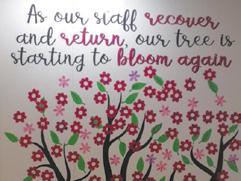
was the first staff member to place her blossom on the COVID-19 Tree of Hope as
employees who had recovered from

Nursing employees of Mediclinic Bloemfontein received cakes from Shoprite/Checkers.

Two support sessions were held at Mediclinic Bloemfontein for employees on 15 October 2020. The goal was to share personal experiences and stories of hope and inspiration through challenging times. Dr Poly Orji (Paediatrician) coordinated the project in collaboration with Dr Michelle Myburgh (Emergency Centre Head) and the Health and Wellness team. COVID-19 experiences were shared, songs of hope sung, poems of grace read, dances of celebration performed (see above) and talents of bravery displayed.

INNOVATING TO MEET THE NEEDS OF BUSINESS
Necessity is the mother of invention. And nothing could be more demanding than a pandemic hitting a hospital, a nation and, indeed, the whole world.
Mediclinic’s innovative approach in managing our response to the pandemic required a new level of teamwork between operations, clinical, infrastructure, procurement and many other teams. It also required regular and interactive engagement between hospitals and Corporate Office.
Dr Kim Faure, Clinical Performance Manager, outlines some of the innovation driven by the pandemic. “Our preparedness plan served as a blueprint to guide all policies and guidelines. It was designed and functioned as a disaster plan, and operated as a backbone for all other related decisions.”
Dr Gerrit de Villiers, Chief Clinical Officer, highlights the role infection prevention and control played in setting out
policies and guidelines. The science-based guidelines served as a solid base to develop further responses to the various challenges.
Access control became an essential tool, tracking risk for staff members and reducing risk from members of the public accessing our hospitals. Information and communications technology became an essential part of streamlining operations, such as reporting to the national Department of Health and screening – with the introduction of the WhatsApp bot and HCW monitoring systems as just a few of these elements.
Even Zoom and Microsoft Teams became everyday business tools. This simplified engagements during peak periods when large portions of the administrative employees were working from home. Meetings could be hosted with the touch of a few buttons and internet access. Daily engagements between the Task Team and regional
representatives were a prime example. Engagement and training with doctors highlighted the evidence and science behind clinical decision-making. Core committees meeting daily, such as the vaccine committee, meant staff were able to continue their working roles from home while actively participating in decision-making.
Our Care Campaign for staff also went digital, making it accessible to as many of our staff and attending doctors as possible, ensuring that our greatest resource – our staff – had access to the support measures they needed at any time. We created videos by our own staff and shared them via different channels to encourage other team members.
SMS hotline and reassurance or more detail given where needed. These broadcasts opened the door for accessible leadership – key to responding to the pandemic.
Our hospitals began producing their own content for social media, filming on cell phones and submitting their pieces for editing in our in-house studio. This content served to reassure our clients that we were ready for them. Videos were streamed of patients leaving hospitals, spreading a message of hope to others impacted by COVID-19.
Our preparedness plan served as a blueprint to guide all policies and guidelines
The need for direct communication to staff was heightened during this time and we pushed the development and launch of the app to assist with communication needs on the ground, providing a one-stop shop for colleagues who did not have direct online access.
Voice broadcasts from Corporate Office on a weekly or bi-weekly basis allowed for immediate and relevant updates across the business. Questions could be addressed via an
Patient visits were facilitated via the Wi-Fi and tablet devices available in hospital. Family is an essential part of recovery and these engagements served to encourage, inform and, sadly sometimes, bid farewell to loved family members. Even “window visits” were adopted where COVID-19 units were based on the ground floor, allowing family members to see patients through the glass for brief periods.
Changing the way we did business was the most effective way we could meet the needs of our community. To each one who contributed to these big and small innovations: We recognise your role in assisting our clients.


When the first wave hit our country, the nation was put into lockdown. This meant that elective surgeries were postponed, and only emergency medical cases, together with COVID-19 patients, were being treated in our hospitals.
Positive messaging was communicated through detail on safety measures in place: how Mediclinic was prepared and how we were using new tools to assist our community throughout the patient journey. This was essential in combatting the increasing fake news appearing on social channels. Recovery videos from hospitals proved to be gems, as those on social media witnessed the hope and celebration and saw that our hospitals were working hard to support every patient.
As lockdown levels eased, Mediclinic needed to reassure the community that it was safe to seek out care. Many continued to delay chronic care and neglected their health in fear of infection within the hospital. A reassurance campaign was launched, allowing us to communicate across a number of different channels to carry out the message of #HereForYou – a hashtag designed to let patients know we were prepared and ready to safely receive them.
Social media formed an essential tool in this campaign, using articles, infographics and videos to inform and
encourage people to prioritise their health. Hospitals were agile and quickly began filming preset scripts within their facilities, which were quickly edited and posted to social media – providing a local glance into our hospitals with recognised doctors and management sharing the reassurance message.
The Corporate Communication team managed an influx of questions and queries relating to information on COVID-19, testing stations, visiting loved ones, and admissions for necessary medical care during the pandemic. This was crucial in reassuring the public in a timely and sincere manner.
In addition, radio and print adverts were placed, providing key information on elective surgeries and measures in place to limit infection. Doctors were interviewed on radio, sharing their confidence in the measures implemented. The results were dramatic, and hospital occupancies were able to recover, with elective surgery lists once again being filled.
The reassurance efforts were multipronged and really required collaboration across departments and hospitals. Never before had teams at hospital level been asked to do their own filming, and we were delighted by how quickly they took on the challenge and provided great content.
Following the second wave, which had placed hospitals under great pressure, it was once again essential to bring our clients in and reassure them of the capacity and measures in
Mediclinic Southern Africa (Mediclinic Legae)
– February 24 2021
Mediclinic Legae is, once again, safely performing elective surgery. All necessary precautions are in place to reduce the risk of COVID-19, with strict screening protocols in place, as well as the provision of all necessary PPE for staff members working in our facilities. If you have been delaying seeking care, please consult your doctor to ensure that your health is not placed at further risk. Mediclinic Legae is #HereForYou: http://bit.ly/3bDhFZ6

The messaging was supported by links to our current service offerings, such as Care Expert and Private Fixed Fees, as a means of making care accessible. The localised content and links to unique community detail allowed hospitals to engage with their community on a more personal level.
Mediclinic social media has a large role to play in reassuring the public. The fake news generated through social media meant that we also had to combat disinformation regarding
Mediclinic Southern Africa (Mediclinic Hermanus)
– February 10 2021
Mediclinic Hermanus offers a 24-hour Emergency Centre catering for all medical emergencies. All necessary precautions are in place to reduce the risk of COVID-19, with strict screening protocols in place, as well as the provision of all necessary PPE for staff members working in our facilities. Our multidisciplinary team ensures that any medical emergency can be safely managed. Mediclinic Hermanus is #HereForYou: http://bit.ly/36ZPTop

place. The focus for the second campaign included posts on hospital-level Facebook pages, as well as a look at the Emergency Centre measures for safely receiving patients.
Mediclinic Southern Africa – May 6 2021
Mediclinic hospitals are home to world-class emergency centres. Highy skilled multidisciplinary teams can triage a range of health emergencies. We are prepared and ready to help you. Mediclinic emergency centres can safely receive both COVID-19 and non-COVID-19 patients within designated treatment areas. For more information: http://bit.ly/3tnz7l1

the COVID-19 vaccine. #OurBestShot became a call to action, both internally and externally, where we acknowledged that the best opportunity we have to fight the pandemic is by enabling herd immunity through vaccination.
Whatever the challenge, we continue to reassure, inform and invite our community to engage with us, and to trust us for their care. #HereForYou
Mediclinic Southern Africa (Mediclinic Medforum)
– March 15 2021
Mediclinic Medforum is ready to provide urgent medical care should you require it. Our staff have taken every precaution to ensure that you receive the best possible care. Visit our website: http://bit.ly/2ZCTAMm

Avital part of our efforts to fight the pandemic was the roll-out of COVID-19 vaccines for our staff, and later, members of the public.
To ensure we responded promptly and in the best manner possible for our staff and community, a Vaccine Committee was established, meeting regularly to discuss, approve and implement elements of the vaccination roll-out. This team consisted of Clinical, Human Resources, Management, Information Communication and Technology and other representatives to meet the demands of an evolving process.
In conjunction with the National Department of Health, more than 9 000 staff members received vaccinations, alongside doctors, allied healthcare professionals and our colleagues at MHR and ER24. Further colleagues received vaccines as we rolled out Phase 2 alongside the public vaccination process.
Achieving herd immunity through vaccination has been key to overcoming any pandemic, and Mediclinic strongly supports this initiative. From the initial vaccinations in

February through to the roll-out of Phase 2, Mediclinic operated vaccine centres in some of our hospitals or operated in a support level at other facilities.


‘While the roll-out initially experienced some delays as authorities sought to ensure the safety and efficacy of the vaccines, once initiated, the Sisonke trial was efficient and we are extremely proud of the number of staff members who took the opportunity,’ says Dr Gerrit de Villiers, Chief Clinical Officer. ‘We congratulate the team involved in this trial for the amazing work they have done in supporting the healthcare workers during the pandemic.’
We also initiated a campaign to encourage both internal and external audiences to register and receive the vaccine. #OurBestShot has become a call to action to our staff and community members to be vaccinated, highlighting the benefits for the individual and community.
In support of the groundswell of public interest in the vaccination process, ER24 was brought in to assist with a vaccination support line, reducing the pressure at hospital level to provide immediate information on the process.
Our involvement in the public roll-out of the vaccine was just as inspiring, with many of our facilities hosting vaccination centres. Our community has been able to rely on our expertise to safely assist in the drive towards herd immunity. Forty-three vaccination centres were identified across South Africa to deliver both Pfizer and Johnson & Johnson vaccines. We have had some inspiring stories reach us from these sites, and it is encouraging how our community is demonstrating their appreciation for this service.
We would like to thank all the staff involved, for the training sessions and other work that went into making the roll-out a success from our side. We are in this together.


The global pandemic pummelled the health, hearts and spirit of too many people in the world. As South Africans, we were not spared as we watched our colleagues and loved ones fight for their lives against COVID-19. While healthcare workers worked tirelessly to help those who needed medical assistance, we remembered that they had been doing so long before we had the hope of the vaccine being administered. Despite the mental and emotional tolls taken, we acknowledge the kindness and hope all healthcare workers gave in their calling to care and restore.
As we progressed through 2020, we had many miraculous recoveries and discharges, and we celebrate these victories. While we can never forget those we lost, we must keep our eyes on the success and progress we have made in overcoming our adversities.
Mediclinic’s management team created a special tribute to show their appreciation to Mediclinic staff and associated healthcare workers for their dedication and commitment during the COVID-19 pandemic. Here are some of our noted triumphs as a team who stood together regardless of age, gender, background, ethnicity or religion.
Strength in age

At 103, Bertha Meltzer was one of our country’s oldest COVID-19 discharges. After being admitted with pneumonia and COVID-19, she recovered sufficiently for a marvellous discharge from Mediclinic Cape Town. Special moments during admission included Zoom calls with her 80-year-old twin sons.
Strength in teamwork
Mediclinic Midstream saw many hard-fought COVID-19 recoveries. One of the most emotional and remarkable of these was that of Deputy Nursing Manager Tauhierah Tavares, who spent seven weeks in the Critical Care Unit receiving care. After dedicating her career to caring for those in need, her colleagues were able to provide this care for her when she was infected with the virus. The
emotion-laden discharge of a respected colleague demonstrates a victory for every front-line worker who has dedicated themselves to the fight against COVID-19.

Strength in numbers

Mediclinic Hoogland celebrated its 100th COVID-19 recovery when 57-year-old Pinki Motloung from Ficksburg was discharged. The Tree of Hope featured in the video of the occasion has a leaf for every patient who has recovered in the facility, inspiring others to strive for recovery.
Strength in community

Mr Arnoldus was used to fighting to help other people. He is a firefighter for the City of Cape Town, but this time it was our turn to help him. Mr Arnoldus’ condition was very serious when he was admitted to Mediclinic Durbanville with COVID-19. Dr Pierre Tredoux and team stood beside him and fought.
Strength in new beginnings

Staff member PN Christine Williams was admitted to Mediclinic Panorama as a COVID-19 patient. She was also pregnant at the time of her admission. Following her treatment in the Critical Care Unit, she delivered baby Luca via a caesarean. Mom and baby received the red carpet treatment when they left the hospital.
Strength in hope

In sickness and in health, as they say. The Magubanes experienced a unique milestone in their marriage. Staff at Mediclinic Newcastle lined the halls to wish Mr and Mrs Magubane well when they were discharged together.
Strength in positivity

Sanjidibany Malek was admitted to Mediclinic Midstream on Monday, 1 June 2020 with difficulty breathing, burdened with the knowledge that her husband and young son were also infected with the virus. While she is only 41 years old with no comorbidities, Sanjidibany developed a severe form of COVID-19 disease. We celebrate her recovery.
Strength in gratitude

Johannes Kortje, 48, was discharged from Mediclinic Paarl after spending almost a month in the hospital. He felt well enough to refuse a wheelchair on discharge, wanting to show his good health to the staff supporting him. Johannes expressed his thanks to the staff and doctors for their admirable work during this time and for the role they played in his recovery.
Strength in perseverance

Marius Fourie came to Mediclinic Vergelegen not thinking that he had COVID-19, but soon was critically ill and spent an extended period of time in the Critical Care Unit. The doctors and nurses were astounded by his level of positivity. Marius celebrated his 20th wedding anniversary while in hospital and was reunited with his family soon after.
Strength in the face of adversity

Ms Tisane was discharged from Mediclinic Legae facility, accompanied by beautiful singing. She had spent three weeks in the hospital. While recovering from the virus, Ms Tisane started encouraging others around her – and this was why the staff chose to sing a particular song of hope upon her discharge.
MEDICLINIC RECOGNISES THE UNWAVERING DEDICATION OF STAFF MEMBERS AND DOCTORS
As a result of the COVID-19 pandemic, we have continued to experience illness and deaths in the Mediclinic family, and we have, unfortunately, lost a number of employees and admitting doctors. The commitment of each person to their career in healthcare is recognised, and our heartfelt condolences are expressed to their colleagues, friends and family.



Ralph Adams MEDICLINIC CONSTANTIABERG

Dr Pierre Botes MEDICLINIC WORCESTER

Dr Deon du Toit MEDICLINIC BRITS




Alex Craven MEDICLINIC NELSPRUIT

Dr Nolan Dreyer MEDICLINIC KLEIN KAROO








Shonisani Mabara MEDICLINIC MEDFORUM




Stoney Makgoane Worked at Mediclinic Brits for many years, and was an MHR panel member at the time of her passing


Pauline Khuduga MEDICLINIC KIMBERLEY AND MEDICLINIC GARIEP


Florence Makhele ER24 CORPORATE OFFICE (TSEBO CLEANING SOLUTIONS)












Worked at Mediclinic Nelspruit for many years, and was an MHR panel member at the time of his passing

















‘When we help ourselves, we find moments of happiness. When we help others, we find lasting fulfillment.’ — Simon Sinek, author and inspirational speaker
A few years ago, I experienced the epitome of our ‘Patients First’ philosophy when I was scheduled for a coronary angiogram at one of our hospitals. Lying in the hospital bed before the procedure, I was cold and anxious. An enrolled nursing auxiliary walked past and stopped when she saw me. ‘You look cold and scared,’ she said, before covering me with another blanket and striking up a conversation on everyday topics. She diverted my attention from the impending procedure and eased my mind. Her situational awareness enabled her to recognise my physical and psychological discomfort. To this day, I remember how her actions, warmth and empathy comforted me.
My experience predates the COVID-19 pandemic, but I have heard many similar accounts since then. In caring for more than 41 800 COVID-19 patients, many of whom have extended hospital stays and limited means to communicate with their loved ones, you have become part of their families – you have become their voice. There is no better example of what it means to pursue our Mediclinic purpose of enhancing the quality of life.
I practised medicine for more than 24 years with countless hours spent in emergency centres. I assure you that I have a deep appreciation for the work you do every day, and I understand your concerns. One of the biggest challenges you face is the increase in deaths due to the pandemic that is not only jarring, but also traumatic. This is why we established enhanced support mechanisms at each hospital. When you are overwhelmed, please use these channels and reach out to your colleagues for support.
Dr Ronnie van der Merwe, our Group Chief Executive Officer, often refers to the pandemic as ‘a marathon, not a sprint’. You may be accustomed to working in a high-stress environment, but you have undoubtedly experienced the telltale signs of exhaustion nipping at your heels. Working as a front-line healthcare worker requires selflessness,

DR RENÉ TOUA GROUP CHIEF CLINICAL OFFICER
adaptability, resilience, and an underlying motivation to make a difference. These are the traits that have helped us overcome seemingly insurmountable odds in the past, and I believe these continue to be critical to our success.
Another reason we are able to face these unique challenges is the value we derive from our international footprint. At the onset of the pandemic, the first wave reached each of our geographies at different times – first Switzerland, then the United Arab Emirates and, finally, Southern Africa. We could learn from Hirslanden and Mediclinic Middle East before the pandemic struck here and that bridged our biggest gap – knowledge. No one knew how the virus would behave or how best to treat its symptoms. Through our cross-divisional Critical Care Unit collaborative, experts across our geographies pooled their expertise and experience to benefit each of our facilities. During the second wave in Southern Africa, we assessed our challenges together. Each Chief Clinical Officer had a role to play – whether by offering support or proactively researching solutions to anticipated challenges. I am extremely proud of the camaraderie of the management team. When we work together well and we learn from one another, we truly live our organisational value of being ‘Team Orientated’.
You have shared many stories of how collaboration and compassion have increased in your teams since the onset of the pandemic as the high-stakes, high-stress, high-intensity conditions have forced us to forge relationships that are authentic and steadfast. Each story inspires me when I go about my responsibilities, many of which revolve around ensuring not only your physical and psychological wellbeing, but also empowering you to do your best work by reducing fragmented care and redundancies. You are the heart of Mediclinic, and we are working hard to build an optimal future for you and our patients.
Stay safe.










