Gut reactions
By diving deeply into a delicate community of bacteria, viruses, fungi and microbes, UChicago experts unlock new insights and treatments
DIVISION SPRING 2024
THE UNIVERSITY OF CHICAGO BIOLOGICAL SCIENCES
Fostering stronger connections across the University and building more interdisciplinary research programs will give us a framework to unite basic researchers and clinicians, and to connect our discovery pipeline with the human experience.

Mark E. Anderson, MD, PhD
Paul and Allene Russell Professor
Dean of the Biological Sciences Division and the Pritzker School of Medicine
Executive Vice President for Medical Affairs
The University of Chicago
Dear Colleagues,
When asked about the biggest challenges facing humanity, what comes to mind? Perhaps it is infectious diseases and the threat of another pandemic. You may think of health equity and the disparities that persist along racial and socioeconomic lines. Or you might wonder about the role that artificial intelligence, with its immense promise and potential pitfalls, is poised to play.
One of my goals is to foster and grow interdisciplinary research programs to tackle the most complex biomedical questions that cannot be answered by any one discipline, let alone a single scientist. The Neuroscience Institute and the Duchossois Family Institute whose faculty and staff focus on microbiome research are examples of how interdisciplinary research can be advanced at the University of Chicago.
These and other efforts can provide a roadmap of how to harness the expertise of departments and divisions, to leverage the University’s strengths as a multidisciplinary academic powerhouse and to grow in other research areas. The possibilities include cancer biology and therapeutics, human immunology, application of AI and urban health. We plan to discuss these ideas, as well as proposals submitted via an open call, with our faculty.
On this campus, our exceptional faculty, staff and students are just steps from the world’s foremost experts in chemistry, physics, molecular engineering and countless other fields. Fostering stronger connections across the University and building more interdisciplinary research programs will give us a framework to unite basic researchers and clinicians, and to connect our discovery pipeline with the human experience. They also will provide a valuable recruitment tool to attract more top faculty who are focused on solving big problems.
This issue of our magazine details the exciting work that is possible when great minds work together. Our cover story explores the gut microbiome, which Cathryn Nagler, PhD, describes as “the ‘Wild West’ of science.” Faculty like Nagler, Eugene Chang, MD’76, and Eric Pamer, MD, have spent years working to understand this delicate community, with the goal of finding new options for disease prevention and treatment. The pursuit involves many partners, including those at Argonne National Laboratory and the Marine Biological Laboratory University affiliates that are a key part of our strategy to grow interdisciplinary research programs.
Another feature profiles the tireless work of Samuel Volchenboum, MD, PhD, MS, who is leading an effort to collect and share pediatric cancer data from across the world. As Associate Dean of Master’s Education, Volchenboum also supported the creation of our joint MS/MBA program with the Booth School of Business to train the next generation of healthcare leaders.
If you’re reading this magazine, you understand the lifelong impact of a UChicago education. The stories in this issue illustrate different steps of that journey, from the medical students following Pritzker’s new Phoenix academic curriculum to the many alumni working at the helm of top scientific journals.
No matter where you are now, your continued engagement helps build on our work, and it ensures we can offer the very best training in medicine and the biological sciences. Thank you for being part of our community.
Dean’s Letter
Spring 2024 Volume 77, No. 1
A publication of the University of Chicago Medicine and Biological Sciences Division.
Medicine on the Midway is published for friends, alumni and faculty of the University of Chicago Medicine, Biological Sciences Division and the Pritzker School of Medicine.
Email us at momeditor@bsd.uchicago.edu
Write us at Medicine on the Midway Suite 2500
130 E. Randolph St. Chicago, IL 60601
The University of Chicago Pritzker School of Medicine and Biological Sciences Division
Executive Leadership
Mark E. Anderson, MD, PhD, Paul and Allene Russell Professor, Dean of the Biological Sciences Division and the Pritzker School of Medicine, and Executive
Vice President for Medical Affairs for the University of Chicago
T. Conrad Gilliam, PhD, Marjorie I. and Bernard A. Mitchell Distinguished Service
Professor, Dean for Basic Science, Biological Sciences Division
Thomas E. Jackiewicz, President of the University of Chicago Health System
Vineet Arora, MD, AM’03, Herbert T. Abelson Professor, Dean for Medical Education, Pritzker School of Medicine
Editorial Committee
Chair Jeanne Farnan, AB’98, MD’02, MHPE
Jennifer “Piper” Below, PhD’11
Gabrielle Edgerton, PhD’10
Dana Lindsay, MD’92
Rob Mitchum, PhD’07
Carol Olson, PhD’82, MD’86
Loren Schechter, MD’94
Coleman Seskind, AB’55, SB’56, MD’59, SM’59 (Lifetime Member)
Carol Westbrook, AB’72, PhD’77, MD’78
Student Representatives
Peishu Li, SM’22 (BSD)
Tony Liu (Pritzker)
University of Chicago Medicine
Communications
Kevin Joy, Editor
Editorial Contributors
Sabrina Arif
Emily Ayshford
Jamie Bartosch
Sigi Bischof
Diane Dungey
Ellen McGrew
Devon McPhee
Photo Contributors
Katie Dixon
Greg Dwyer, PhD
Alison Hunter, PhD
Katie H. Long
Chris Jones
Jean Lachat
Jordan PorterWoodruff
Design Wilkinson Design
Jen A. Miller
Grace Niewijk
Angela O’Connor
Sarah Richards
Anne Stein
Jack Wang
Matt Wood
Eddie Quinones
Kaylie Scorza, SB’23
Joe Sterbenc
Nancy Wong
John Zich
Heidi Zieger
Secrets of the microbiome 10
By diving deep into the gut’s delicate community of bacteria, viruses, fungi and microbes, University of Chicago experts are unlocking critical new insights on a wide range of diseases and potential ways to treat them.

FEATURES
Alumni profile 6
Alexander Yang, MD’01, MBA’01, uses his dual degrees to get promising therapies to market.
Communicators-in-chief 17
Meet University of Chicago alumni who lead prominent science and medical journals.
Healing arts 23
John E. Ellis, MD’82, is a devoted supporter and collector of Chicago Black art.



DEPARTMENTS
Midway News
First-year medical students learn the value of violence recovery care. 2
UChicago Medicine expands to Crown Point, Indiana, with its largest offsite location. 4
BSD News
Samuel Volchenboum, MD, PhD, MS, is building a global database to find new disease cures. 25
A “bionic breast” aims to recreates sensation of touch after reconstructive surgery. 28

Pritzker News
The new Phoenix Curriculum marks the medical school’s biggest update in 15 years. 8
Cheers, tears and residency destinations from Match Day 2024. 34
1
IN THIS ISSUE
COVER STORY
Letters
Your News 38 In Memoriam 38 8 34 23 25 17
37
Pritzker students learn the value of violence recovery care
Kenneth Wang and Brooke Olson, first-year students at the Pritzker School of Medicine, shadow pediatric violence recovery specialist Tre Nowaczynski, pictured at left.
BY JAMIE BARTOSCH
Lewis Oh watched closely as a young patient with a gunshot wound arrived by ambulance at the University of Chicago Medicine Level 1 trauma center. As doctors, nurses and technicians provided care, Oh also saw pediatric violence
type of care offered in the trauma center, one of the busiest in the nation.
“It’s important to me that we expose this next generation of physicians to what’s possible in healthcare,” said Nowaczynski, who coordinates the VRP shadowing program. “Since we’re embedded in the hospital, which is rare, we have the ability to do this for our students, unlike other medical schools in the U.S.” VRP specialists provide 24/7 support, tending to the emotional needs of patients and families who have experienced intentional violence.

1,835
Number of patients served by the Violence Recovery Program in 2023
40%
Percentage of UChicago Medicine adult trauma patients with penetrating injuries
20 hours
Required non-physician shadowing time under Pritzker’s new curriculum
recovery specialist Tre Nowaczynski spring into action gathering information for the patient’s family and assisting with nonmedical needs.
“Tre’s presence was really valued by the medical team,” said Oh, a firstyear student at the Pritzker School of Medicine. “To see that side of healthcare was really inspirational to me. I thought: ‘I hope I could work with a person like Tre when I work in emergency medicine.’”
Oh’s outlook came via a new option for first-year Pritzker students to shadow specialists in UChicago Medicine’s Violence Recovery Program (VRP). The two-hour observations spotlight a unique
That includes arranging for a safe discharge and connecting them with community resources. In 2023, the program helped nearly 2,000 UChicago Medicine patients, almost two-thirds of whom had gunshot wounds.
The demand has led UChicago Medicine to nearly triple the number of its trained VRP specialists. Many live on the South Side, and some have survived gun violence themselves, said Carlos Robles, LCSW, AM, the VRP’s Manager of Clinical Operations.
The shadowing experience aligns with Pritzker’s redesigned Phoenix Curriculum, launched with the matriculating class of 2023. It includes a component that requires 20 hours of shadowing non-physician hospital staff to
THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION 2 Midway News
UNIVERSITY OF CHICAGO MEDICINE
PHOTO BY JORDAN PORTER-WOODRUFF
learn about roles and responsibilities, as well as team-based communication.
This is the first year medical students could shadow VRP specialists. The opportunity was made available after students expressed interest in learning more about the trauma center service, said Tia Kostas, MD, Pritzker’s Director of Interprofessional Education.
Although it can be emotionally difficult to witness violent injuries, some of which involve children and complex social problems, Pritzker students eagerly pursue VRP shadowing slots.
“Once a few students did it, they told the rest of the class about it,” Kostas said. “And now they all want to do it.”
Kostas and Nowaczynski hope participants gain a deeper understanding of why psychological recovery from trauma is important, as well as the value of hospital-based violence recovery programs.
“We’re finally getting some traction in treating gun violence like a public health crisis,” Nowaczynski said. “But it’s going to take the next generation of physicians to push it forward.”
HEALTH EQUITY
Annual report details community impact
Over the past 10 years, UChicago Medicine’s reported community investments in Chicago’s South Side and in the south suburbs have totaled more than $5 billion, according to the 2023 Community Benefit Report.
These investments help reduce health disparities by improving access to healthcare and other resources, conducting health screenings and funding grassroots organizations working to stop community violence. They also cover medical expenses for patients, and support research and training for the next generation of healthcare professionals.
In fiscal year 2023, UChicago Medicine’s community benefit investment was $730.9 million including $636.6 million through the University of Chicago Medical Center in Hyde Park and $94.3 million through UChicago Medicine Ingalls Memorial in Harvey, Illinois.
Community benefit investments and initiatives are guided by UChicago Medicine’s Urban Health Initiative, which is its community health division, along with its two Community Advisory Councils and many key partnerships.
To view the report, visit community.uchicagomedicine.org/2023













$5 billion +
UChicago Medicine’s community investments in the past decade
Source: 2023 Community Benefit Report
New effort focused on cancer inequities
With health disparities in cancer expected to increase as rates of the disease climb, the University of Chicago Medicine Comprehensive Cancer Center’s new effort the Center to Eliminate Cancer Inequity (CinEQUITY) will work to pioneer transformative research that addresses the complex factors that adversely affect excluded or marginalized people in the Chicagoland area.
By serving as a research hub, CinEQUITY (pronounced “see inequity”) will provide core
resources to partner with community leaders, support collaboration with community-based organizations, train in best practices for conducting community-engaged research, build inclusive research teams, and disseminate findings to influence policy and practice.
“Our guiding vision is of a future where every individual, regardless of background or circumstance, has equitable outcomes when preventing, treating and surviving

cancer,” said Jasmin Tiro, PhD, MPH, Professor of Public Health Sciences and the Director of CinEQUITY.
CinEQUITY’s external advisory board includes national leaders in cancer disparities, including Otis W. Brawley, SB’81, MD’85, a renowned cancer disparities researcher and the Bloomberg Distinguished Professor of Oncology and Epidemiology at Johns Hopkins University. He delivered a keynote speech at the center’s launch event on Feb. 16.
3 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
UChicago Medicine opens new Crown Point facility

Following 20 months of construction and hundreds of hours of planning, the University of Chicago Medicine opened its two-story, 132,000-square-foot multispecialty care center in Northwest Indiana to patients on April 29.
The facility, called UChicago Medicine Crown Point, offers access to UChicago Medicine and UChicago Medicine
Comer Children’s Hospital physicians and specialists including those in cancer
Services and capabilities
■ Infusion therapy, radiation, and medical and surgical oncology
■ MRI, CT, PET, X-ray and ultrasound imaging
■ Ambulatory surgery and breast imaging centers
■ Laboratory services
■ Access to UChicago Medicine clinical trials
■ An eight-bed emergency department and eight-bed inpatient unit
care, digestive diseases, heart and vascular, neuroscience, and orthopaedic surgery.
Located at I-65 and 109th Avenue, the care center is UChicago Medicine’s first freestanding facility in Indiana and its largest offsite location. It will employ about 200 staff and is projected to accommodate 110,000 patient visits each year.
“We’re excited to bring the forefront of medicine to people in Northwest Indiana who would otherwise have to travel long distances to access highly specialized care,” said Blase Polite, MD, Physician-in-Chief for Northwest Indiana. “We look forward to joining the community and collaborating with local providers.”
Based on assessment of the market, UChicago Medicine found that about 15% of patients in Northwest Indiana travel outside the region for medical care, with roughly one in five of that group visiting the health system’s facilities in and around Chicago.
The Crown Point facility builds on a network of smaller specialty care medical offices UChicago Medicine has operated for years in the region, in Merrillville, Munster and Schererville. Last September, UChicago Medicine acquired four regional oncology centers from Michiana Hematology Oncology.
Joint partnership supports healthcare education, new jobs
The University of Chicago Medicine and the University of Chicago are partnering with City Colleges of Chicago on a project that will create new jobs, establish healthcare career pathways, and enhance and expand the capacity of clinical lab facilities on the medical center campus.
A main component involves construction of a new facility that will consolidate UChicago Medicine’s existing clinical labs on underutilized land along East Garfield Boulevard in Washington Park. The clinical lab facility will support 550 jobs including approximately 200 new positions and drive healthcare careers for South Side residents.
The other key part of the partnership involves a new learning center for Malcolm X College. Constructed by City Colleges of Chicago, the center will be adjacent to the proposed clinical lab facility and serve up to 800 students as the first clinical lab technician program in Chicago. Both facilities are expected to break ground in 2025 and open during the 2026-27 academic year.

THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION 4 Midway News
EXPANSION
PHOTO BY CHRIS JONES
UChicago Medicine receives $20M gift for cancer care and research pavilion
Susan and Tandean Rustandy have donated $20 million to the University of Chicago Medicine to support development of Illinois’ first and only freestanding facility dedicated to cancer care and research. The 575,000-square-foot space is scheduled to open in 2027.
“We believe in the power of collaborative efforts to effect transformative change, and the new cancer pavilion holds immense potential to impact not only the local community, but also the broader landscape of patient care globally,” said Tandean Rustandy, who received his master’s in business administration from the University of Chicago Booth School of Business in 2007.
The gift will support the work of UChicago Medicine’s nationally recognized clinicians,
physician-scientists and researchers to discover novel treatments, improve cancer patients’ overall care experiences and reduce health disparities in underserved communities including Chicago’s South Side, where cancer death rates are twice the national average.
Rustandy serves as a trustee on both the University of Chicago and University of Chicago Medical Center boards. He and his wife have been generous benefactors to the University, providing support for the College, the Divinity School, and Chicago Booth, where the Rustandy Center for Social Sector Innovation was established in 2013. In 2014, the couple established the Tandean Rustandy Fund for Fundamental Cancer Research in the Biological Sciences Division.
‘OR of the future’ views the brain like never before
Anew kind of operating room is designed to give University of Chicago Medicine physicians more information than ever to guide neurosurgical procedures.
“Our vibrant neurosurgery research program demanded real-time technology integration as the next logical step,” said Peter Warnke, MD, Director of Stereotactic and Functional Neurosurgery at UChicago Medicine.


An “OR of the future,” as Warnke called it, opened at UChicago Medicine’s campus in Hyde Park in January 2023. It features cutting-edge instruments and high-definition screens that allow surgeons to scan and view key areas of the brain throughout an operation.
The highlight, Warnke said, is a new intraoperative MRI that allows doctors to run functional MRI scans mid-surgery to see not only how the brain is arranged but also how it’s working in real time during surgical interventions.
The space includes two complementary mobile CT scanners, including an ultrafast, 64-slice helical scanner. HD screens project output from the MRI, CT scans and all surgical plans, including robotic trajectories and images from a patient’s medical record.
These tools can help surgeons target their approach down to the millimeter. “With precise imaging, we can use minimally invasive tools like interstitial lasers and responsive closedloop stimulation systems to reduce morbidity significantly,” Warnke said. “It’s a major paradigm shift in neurology.”
5 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
Tandean Rustandy, MBA’07
Advanced tools allow UChicago Medicine physicians to see how the brain is working in real time during surgery.
PHOTO BY JORDAN PORTER-WOODRUFF
Entrepreneur uses strategic storytelling to advance new therapies
 BY DEVON MCPHEE
BY DEVON MCPHEE
More than 90 percent of drug candidates never move forward, according to the National Institutes of Health a roadblock that saddens Alexander Yang, MD’01, MBA’01.
“It’s heartbreaking how many therapies that clearly work don’t make it to market, not because of the science but because of how their value is communicated to investors,” said Yang, founder and CEO of Xelay Acumen, a Bay Area strategy and management consulting firm focused on biotechnology, pharmaceutical and healthcare providers.
The barrier also motivates him. Yang’s firm, which develops clear medical communication programs for promising therapies in development, boasts numerous successes in moving promising new treatments further down the development pipeline.
“We challenge ourselves to uncover and develop the stories that will aid stakeholders government, insurance, physicians, investors and patients in understanding the potential role of a therapy and to secure needed funding to continue clinical trials,” Yang said. The entrepreneur’s distinct path almost never came to fruition. While enrolled in the University of Chicago’s joint MD/MBA program, Yang envisioned a career as a pediatrician and, later, an emergency department physician.
But during residency applications, he also explored consulting opportunities and received multiple job offers. One firm, McKinsey & Company, convinced him to defer residency and join their West Coast office, where biotech was burgeoning.
“I thought, ‘I’m young and single why not?’” Yang said. “It really opened my eyes to how I could leverage both of my degrees and how
I could make a difference in patients’ lives on a broad scale by helping to get groundbreaking therapies into the market for patients.”
Yang spent a decade at various biotechnology companies, including Amgen, Nektar Therapeutics and Affymax, before striking out on his own. Today, Xelay Acumen employs about 20 across the United States and Asia. Yang has also launched an investment fund and a philanthropy foundation.
“Entrepreneurship has given me the ability to work on exciting therapies that satisfy a passion for scientific inquiry and, at the same time, help others in a meaningful and impactful way,” he said.
Yang credits his UChicago education for much of his success, emphasizing an approach known as “the pursuit of why” to connect seemingly disparate concepts.
“There’s this ‘network externality’ effect, where you have different pieces of information, and if you understand the ‘why’ behind each of them, you begin to see how they are connected and can make discoveries that others overlook,” Yang said.
As a gesture of gratitude, Yang established the Alex Yang MD’01, MBA’01 and Xelay Foundation Scholarship Fund in 2018 to support students at the Pritzker School of Medicine, and he sponsored the creation of a study space at the medical school.
Yang recently funded a gift for the University of Chicago Booth School of Business Hong Kong campus, and he was appointed a member of the Division of the Biological Sciences and the Pritzker School of Medicine Council in July.
“I’m honored to give back to the institution that has played a pivotal role in my life,” Yang said.
6 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION
ALUMNI PROFILE
Alexander Yang, MD’01, MBA’01, credits his UChicago education for emphasizing “the pursuit of why,” an approach that guides his entrepreneurship.

Have you made a qualified charitable distribution in the past, or are you considering one?
A recent law allows IRA owners age 70½ or older a special, one‑time opportunity to use a qualified charitable distribution (QCD) of up to $53,000 to fund a charitable gift annuity. With this option, you can transform an IRA distribution into fixed income payments for life and leave a meaningful residual gift to the University.
As with a standard QCD, using a QCD to fund a charitable gift annuity satisfies all or part of annual required minimum distributions (RMDs). Now you can choose the charitable giving strategy that works best for you—income or no income.
Interested?
Learn more at giftplanning.uchicago.edu
Calculate your payments at giftplanning.uchicago.edu/calc.
AMERICAN COUNCIL ON GIFT ANNUITIES RATES* Single‑Life Charitable Gift Annuity
IRA donors. There’s a new spin on qualified charitable distributions. For more information, contact: Wendy Irvine, senior director of development Medicine & Biological Sciences Development EMAIL wirvine@uchicago.edu CALL 773.702.3055 DIVISION OF THE BIOLOGICAL SCIENCES AND THE PRITZKER SCHOOL OF MEDICINE OFFICE OF GIFT PLANNING AGE IMMEDIATE PAYMENT 70 6.3% 75 7.0% 80 8.1% 85 9.1% *Rates effective January 1, 2024. Certain limitations and rules apply. The minimum required to fund a charitable gift annuity is $10,000.
Attention,
Phoenix rising
 BY DEVON MCPHEE
BY DEVON MCPHEE
Pritzker curriculum overhaul builds on historic strengths, interactive learning
The Phoenix Curriculum, a revised educational framework at the University of Chicago Pritzker School of Medicine, is designed to empower students to serve as patient advocates, incorporating self-directed learning, research, clinical experience and community engagement from day one.
Current first-year Pritzker students are the first to follow the new curriculum the medical school’s most significant update in 15 years.
“Though we have made continuous quality improvements over the years, this is a major overhaul of the curriculum,” said Jeanne Farnan, MD’02, MHPE, Professor of Medicine and Associate Dean for Undergraduate Medical Education.
The name was selected to symbolize rebirth following the COVID-19 pandemic and to pay homage to the University of Chicago’s coat of arms, a shield displaying a phoenix.
Development of the Phoenix Curriculum began in 2021, when Pritzker leadership sent a needs assessment to students, staff, alumni and patients. Working in small groups to review the responses as well as ongoing objectives and national benchmarks the medical school’s education team identified growth areas rooted in the school’s core values, notably health equity and scholarship.
The result: a model focused on holistic development and shared collaboration.
“We see our students graduating with not only the strong foundation in biomedical science and clinical experience
needed to become good doctors, but also the communications skills and adaptability to embrace advances in healthcare and become leaders in their field,” said Jason Poston, MD’02, Associate Professor of Medicine and Assistant Dean for Medical School Education. “We also think it will be a great recruitment tool.”
More time to observe, explore Robust and early exposure to the clinical environment is central to the Phoenix Curriculum. Previously at Pritzker, two years of coursework were required before two years of clerkships.
“We recognized that students were coming in with a lot of biomedical knowledge and that they hungered for earlier exposure to the clinical environment,” Poston said.
Pritzker students now participate in a yearlong ambulatory and inpatient preceptorship that introduces them to healthcare settings and nonphysician staff within the first 18 months. Students also can participate in an optional Pritzker Morning Report, modeled after the morning reports held during residency, to analyze a real-world case.
Under the new curriculum, second-year Pritzker students enter their clerkships earlier in March instead of June and they have longer core clinical rotations, including a new four-week ambulatory clerkship that combines outpatient care in internal medicine and family medicine. Time is allotted both during and after rotations for electives and career exploration.
8 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION MEDICAL EDUCATION
“ We recognized that students were coming in with a lot of biomedical knowledge and that they hungered for earlier exposure to the clinical environment.”
Jason Poston, MD’02, Associate Professor of Medicine and Assistant Dean for Medical School Education
Pritzker’s education team condensed or reworked courses to accomplish this. They identified areas of overlap, such as in the legacy curriculum’s Cell Pathology and Immunology course and Microbiology course, respectively, and merged them into a single Host Defense and Invasion course taught by both instructors.
“We were very conscious of respecting our students’ time and not simply cramming the same amount of information into a shorter time frame,” Poston said. “We also wanted them to grow outside of the formal curriculum by giving them time to pursue other interests.”
The pandemic showed administrators that passive learning strategies such as lectures didn’t engage students, Farnan said, which led Phoenix Curriculum planners to incorporate more team-based learning in small groups an approach linked to higher test scores.
In the Methods of Inquiry course, for example, students first review a scientific paper and answer questions about it on their own. Then, they get together with their team to discuss and refine answers before submitting them as a group.
Health equity and scholarship
The needs assessment survey also revealed strong support for expanding health equity education.
As a result, the Phoenix Curriculum prioritizes health equity as a longitudinal thread throughout the first three years including a dedicated first-year health equity course plus foundational courses and clerkships that incorporate
patient advocacy and healthcare disparities discussions.
“Our hope is that this will allow our students to become even more committed and prepared to address this huge challenge in healthcare,” said Adam Eickmeyer, MPH, Director of Medical School Education.
There is also a continued focus on scientific examination. Through Pritzker’s Scholarship and Discovery program, every student participates in a four-year mentored research program. Ninety percent have published in a peer-reviewed journal by graduation, while 96 percent have authored an abstract or poster.
This distinguishes Pritzker graduates from their peers, said Farnan, noting that fewer than 80 percent of medical students nationally conduct mentored research.
“Other schools have reduced or removed their scholarship component, but we felt that maintaining it was core to our UChicago identity,” Farnan said. “It also gives our students an edge when it comes to the residency application process.”
To measure the success of the Phoenix Curriculum and guide modifications, the medical school has developed multiple avenues for soliciting feedback. It will also track students’ performance on internal and standardized exams, as well as their clinical performance.
So far, the reception has been positive. “Students have told us that they really like the small group learning and appreciate that we’ve moved the clinical skills curriculum much earlier in their training,” Eickmeyer said.
Pritzker Morning Report brings residency tradition to first-year students
Under the new Phoenix Curriculum, first-year students at the Pritzker School of Medicine can benefit from a learning experience that typically doesn’t happen until residency: the morning report.
As it does for medical residents, the session consists of a clinician presenting a real-world case and working though it with attendees. The group reviews lab results and physical exams, asks questions and then considers the diagnosis.
Known as the Pritzker Morning Report, these gatherings take place once or twice weekly before classes during the first quarter. Topics span the medical profession, from emergency medicine and obstetrics to oncology and pediatrics.
“The earlier you can expose students to the variety of specialties and subspecialties that exist in medicine, the more we can help them find the right fit,” said Jason Poston, MD’02, Assistant Dean for Medical School Education.
Although the Pritzker Morning Report is completely elective, almost all first-year students attended at least one session, said Jeanne Farnan, MD’02, MHPE, Associate Dean for Undergraduate Medical Education.
“It helps connect classroom learning with the students’ future as physicians,” Farnan said. “It reminds them that they’re not learning things simply for an exam, but because they’re going to be taking care of patients.”
9 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
Secrets of the microbiome
BY EMILY AYSHFORD
By diving deep into the gut’s delicate community of bacteria, viruses, fungi and microbes, UChicago experts unlock lifesaving insights and new treatments
10 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION
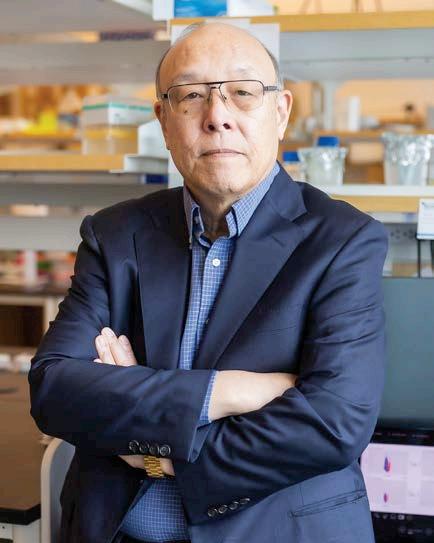
Nearly a quarter-century ago, Eugene Chang, MD’76, was studying inflammatory bowel diseases, chronic yet poorly understood conditions marked by diarrhea, pain and fatigue sometimes with life-threatening complications.
Cases of IBD had been rising for decades, but researchers at the time couldn’t determine why. The cause wasn’t just genetics, environmental factors or even one triggering pathogen. Chang suspected part of the answer could lie within our own gut microbiome an ever-changing network of trillions of microbes that has co-evolved over time to help the body digest food.
Clearly, these bacteria were doing far more than just digesting. “It dawned on us that the gut microbes were affecting our gene expression,” said Chang, Martin Boyer Professor of Medicine at the University of Chicago.
The hunch was so strong that Chang retooled his namesake lab in 2000 to focus on the microbiome, collaborating with scientists at Argonne National Laboratory and the Marine Biological Laboratory, and using the latest technologies to study microbes in detail.
Some colleagues questioned the pivot. “There was so little known about the microbiome, and most people were very skeptical that it could be studied,” Chang said. “You’re dealing with trillions of microbes. How do you sort that out?”
Today, the pursuit is booming at the University of Chicago. The gut microbiome has been implicated in a host of diseases and conditions, including those that affect the gastrointestinal tract. It has also been linked to metabolic diseases like diabetes and obesity, cancers, complex immune diseases, allergies, developmental abnormalities and neurological disorders.
As researchers untangle the web of microbiome and host, University teams are developing new breakthroughs that include management tools for IBD, metabolites to
treat allergies and probiotics to improve liver disease outcomes.
“Our microbiome medicine and research programs are incredibly strong because of robust multidisciplinary collaborations,” said Chang, who in 2008 worked with Alexander Chervonsky, MD, PhD, and Betty Theriault, DVM, to create the Gnotobiotic Mouse Facility to study microbes’ behavior in germ-free mice an effort that launched a tidal wave of research at the University.
“Our tools are getting better, and now we can model and simulate conditions to form and test hypotheses that translate into research directions that advance precision medicine.”
Delicate balance, hard questions
When the gut microbiome is healthy and functional, it lives in concert with many of the body’s biological processes, such as metabolism and immunity.
Microbes play a key role in extracting nutrients from the food we eat, but they also release metabolites (small molecules that enter the blood stream, affecting systems throughout our bodies) and produce antimicrobial substances to protect their host from external pathogens.
This microbial network is ever-evolving depending on a person’s diet, environment, genetics and whether they have recently taken antibiotics and it varies across ages and cultures.
“The gut microbiome impacts all of our physiology, and when it’s thrown off balance, that will predispose to many different kinds of diseases,” said Cathryn Nagler, PhD, Bunning Food Allergy Professor of Pathology, Medicine, Pediatrics and the Pritzker School of Molecular Engineering.
Consider the United States, where modern-day environments have removed many microbes that humans lived with for thousands of years, and diets have proliferated that lack fruits and vegetables
GUT MICROBIOME
BY THE NUMBERS
5
Phyla of bacteria constitute the gut:
■ Firmicutes
■ Bacteroidetes
■ Actinobacteria
■ Proteobacteria
■ Verrucomicrobia
500
Species of bacteria in the gut
3–4
Days in which the gut microbiome balance shifts with changes in diet
Sources: Frontiers in Nutrition, Journal of Cardiovascular Nursing, Microorganisms
11 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
100 trillion Microbes in the gut
Eugene Chang, MD’76, is credited with jumpstarting a wave of microbiome research at the University of Chicago.
PHOTO BY NANCY WONG
to help diversify the gut’s microbial membership and functions. Scientists theorize that these scenarios contribute to a rise in allergies and autoimmune conditions such as diabetes.
Over the past decade, Nagler said, microbiome researchers have moved beyond identifying which bacteria class is a target to examining host-microbiota interactions on a molecular level.
Progress and demand have led the University to create state-of-the-art microbiome research facilities and services including the Duchossois

Family Institute (DFI), the Microbiome Center and the Microbiome Medicine Program as well as partnerships with affiliate institutions. Established in 2017, the DFI is led by renowned infectious diseases expert Eric Pamer, MD, Donald F. Steiner Professor of Medicine, Pathology, and Microbiology.
Additionally, UChicago was selected as one of the first human demonstration projects by the National Institutes of Health (NIH) Human Microbiome Project; it has since garnered numerous research grants from the NIH and other funding agencies.
Clear link to diabetes
Although an unbalanced microbiome has been linked to diseases throughout the body, many studies show correlation, not causation. Still, the gut microbiome has the clearest connection with conditions that affect the gastrointestinal tract including IBD, liver disease and diabetes.
In a study published in Cell Host & Microbe last year, Chervonsky, Professor of Pathology and Medicine, showed that when diabetes-prone mice were given a diet based on the milk protein casein, it helped prevent them from developing Type 1 diabetes. In fact, their insulinproducing cells had improved function, and their autoimmune response was limited.
But when gluten was added into their diet, it overrode the protective effects of casein. The research team found when gluten is eaten, Enterococcus faecalis (E. faecalis), a common bacterium in the gut, secretes enzymes that digest the gluten. This process releases lipopolysaccharides (LPS) components of non-native “gramnegative” bacteria.
That, in turn, stimulates the immune system to respond to the gut, which overpowers the protection given by casein and can lead to autoimmunity.
“Finding LPS was a surprise that we definitely did not expect, but it must be coming with gluten somehow,” Chervonsky said. “There are gram-negative bacteria everywhere in the soil, so maybe it’s associated with where the grains are grown, or it is contaminated in storage.”
Many of the microbes in the gut microbiome are obligate anaerobes, meaning they cannot live in an oxygenated environment. Instead of generating energy by respiring (“breathing”) oxygen, like most cells do, microbes can respire metabolites, which can then travel throughout the body and affect health.
Sam Light, PhD, Neubauer Family Assistant Professor of Microbiology,
12 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION
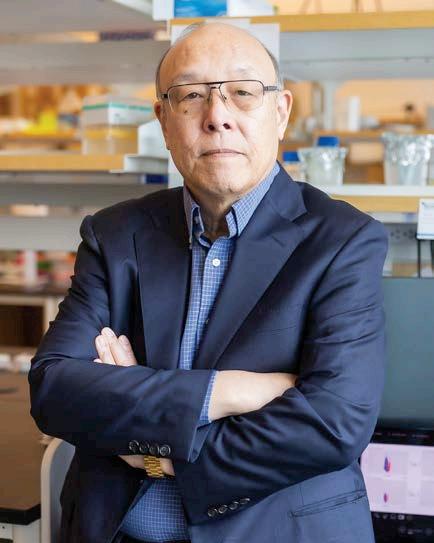
Cathryn Nagler, PhD, is developing a polymer molecule designed to deliver metabolites directly to the gut to help repair intestinal barrier function and prevent food allergies.
PHOTO BY NANCY WONG
UChicago alumni extend the microbiome research network
Stopping bad bacteria in their tracks
Jeannette Messer, PhD’13, didn’t plan for a career in microbiome research. In fact, she started out as a veterinarian. But as she cared for animals, Messer realized she was most interested in disease mechanisms, especially those of infectious diseases.
Messer enrolled in a PhD program in immunology at the University of Chicago, which cemented her interest in how the human body is constantly cooperating with and defending itself against microbes.
“It’s like a local neighborhood,” she said of the gut microbiome. “You have some people you like, who help each other out, and others are terrible. They cause damage and break things.”
A postdoctoral fellowship in the lab of Eugene Chang, MD’76, solidified Messer’s interest in host-microbiome interactions. Now, as a principal investigator at Cleveland Clinic, she conducts research on how to manipulate these interactions specifically, by preventing those bad neighbor microbes from adhering to the body in the first place.
“Blocking these adhesion events is critical for infectious and chronic inflammatory diseases,” Messer said. “If we can figure out how to block that first step, we can prevent disease from ever getting started.”
She and her team have begun testing potential therapies in cellular models, with the hope that they will be successful enough to eventually move forward to clinical trials.

“It’s a great time to be in microbiome research,” she said. “We’re getting to the point of being able to manipulate the microbiome. We’re going to make a big difference in a lot of diseases, which could help a lot of people. That’s the hope. That’s why I’m in this field.”
Understanding diet and the microbiome

When Suzanne Devkota, PhD’12, began studying dietary effects on the gut microbiome as a graduate student in the lab of Eugene Chang, MD’76, in 2008, she didn’t consider herself a “microbiome person.”
“I was interested in nutrition, and the microbiome field was very much still in its infancy,” she said. But her research found that one specific type of fat was driving inflammation in colitis, and one kind of bacteria produced a pro-inflammatory by-product.
“I was hooked,” Devkota said. “It was exciting and scary to go into a totally new field, but I felt like I had a responsibility to continue this line of work.”
Now the director of the Cedars-Sinai Human Microbiome Research Institute, Devkota has studied the role of fat tissue in gut inflammation specifically, how microbes translocate out of the gut and embed themselves into fat tissue. She found that in Crohn’s
Disease, a type of inflammatory bowel disease, fat tissue expands to trap the translocating microbes from spreading further by acting like an intestinal bandage.
She also studies how certain diets such as high-fiber diets, fermented food diets, diets that involve intermittent fasting and diets in early life affect the microbiome and immune system development. Devkota is excited about the future of the field, but she doesn’t want hype to detract from the progress.
“We need bacterial genetics and molecular biology, not just big sequencing studies,” she said. “We need actual microbiology to understand the bacterial mechanisms and why things happen.”
Still, Devkota believes those answers are within reach, especially for the next generation at UChicago. “The University of Chicago created a camaraderie of like-minded, excited scientists,” she said. “We have continued to collaborate, and that has been a lot of fun.”
13 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
Suzanne Devkota, PhD’12, is studying the effects of diets such as intermittent fasting.
Jeannette Messer, PhD’13, conducting microbiome research at the Cleveland Clinic.
recently discovered that certain anaerobic microbes convert dietary protein into a small molecule called imidazole propionate, which impairs glucose tolerance. He and his team are now studying how these microbes contribute to the development of Type 2 diabetes.

Sam Light, PhD, is studying how anaerobic microbes contribute to the development of Type 2 diabetes.
“We’re trying to find exactly which gut microbes make this compound and figure out what we can do to prevent them from doing so,” Light said. “That could be a dietary intervention that would prevent it from being produced, or we could introduce another bacteria that could compete metabolically.”
Microbiome studies explore Alzheimer’s disease in women
Insights on COVID-19, liver disease For those who already suffer from certain diseases, an unbalanced microbiome can lead to severe or even deadly outcomes. During the early days of the COVID-19 pandemic, Bhakti Patel, MD, Assistant Professor of Medicine, was trying to figure out why some relatively healthy patients ultimately died from the virus and others recovered.
A study of the microbiomes of COVID-19 patients hospitalized in the ICU at the University of Chicago Medicine between September 2020 and May 2021 offered new insights. “With the technology provided by the DFI, we can measure the microbiome function and potentially customize interventions that restore someone to a healthier state,” said Patel, who worked with Pamer and a team to analyze those patients’ fecal samples.
Their findings: the COVID-19 patients who suffered lung failure and died had more of a group of bacteria called Proteobacteria in their gut microbiome, and they also had lower levels of secondary bile acids and less of a metabolite called desaminotyrosine.
The resulting study, published in Nature Communications, showed that the composition of the gut microbiome and metabolites the microbes produce could predict the trajectory of patients with
Two University of Chicago studies investigated the gut microbiome’s role in differing rates of Alzheimer’s disease in women and men. One, published in Molecular Neurodegeneration, involved testing a drug compound on a mouse model of Alzheimer’s; female mice were less affected by the drug, and they also experienced fewer microbiome changes. The other, in Scientific Reports, examined how manipulating estrogen levels affects composition of the gut microbiome as well as amyloid deposition and inflammatory microglia levels, which are key symptoms of Alzheimer’s.
14 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION
PHOTO BY JOHN ZICH
severe COVID-19. Patel called the discovery “a paradigm shift” in microbiome research.
A microbiome-focused analysis also shed new light on liver disease patients who have a high incidence of infections from drug- or antibiotic-resistant bacteria.
Matthew Odenwald, PhD’15, MD’17, a former gastroenterology fellow in Pamer’s lab, has studied fecal samples of more than 250 patients hospitalized with liver disease. He, too, found that these patients had reduced microbiome diversity and high abundances of potential pathogens, and lacked certain metabolites that can impact immune defenses.
But a portion of those who had received lactulose a synthetic sugar commonly given to liver disease patients to treat hepatic encephalopathy had more gut bacteria called Bifidobacteria. Expansion of this group of bacteria inhibited growth of antibiotic-resistant bacteria, and it was associated with reduced rates of serious infections and prolonged survival.
Odenwald, now an Assistant Professor at the University of Chicago, along with Christopher Lehmann, MD, and Pamer, has received Food and Drug Administration approval to conduct a clinical trial that will provide probiotics strains of bacteria in oral capsules to liver disease patients. The goal: to test whether the bacteria engraft in the gut and positively affect clinical outcomes.
“To be able to do this translational work from bedside to bench to back to bedside is a pretty unique opportunity here at the University of Chicago,” Odenwald said.
‘A completely new frontier’ Identifying intricate patterns and behaviors is key to answering bigger questions. Chang and his group discovered a novel antimicrobial peptide (AMP) produced by unique immune cells of the gut called Paneth cells. The peptide was identified
as peptide YY, a known gut hormone produced by endocrine cells that is important for controlling appetite.
However, the form made and secreted by Paneth cells plays a very different and vital role that maintains intestinal fungi in a state of commensalism. “This was an important finding because so little was known about how our body controls fungi that are part of the gut microbiome,” said Chang, whose findings were recently published in Science. “We know that they’re there, but now know a bit more about how we keep them under control and in states that benefit us.”
Erin Adams, PhD, is taking a different approach to study of the microbiome by investigating the structure of microbial proteins, finding one that has the same structure as proteins created by pathogenic microbes. But this protein, she said, seems to come from normal bacterial interactions in the gut, leading to questions about the origins and roles of these proteins.
“Does this mean that this protein allowed these microbes to colonize our guts without taking over as they co-evolved with humans?” said Adams, Joseph Regenstein Professor of Biochemistry and Molecular Biology. “Was this co-opted from pathogenic bacteria to allow for some tolerance by our immune systems, or was it co-opted by the pathogenic bacteria?”
Nagler, who studies the gut microbiome as the key to curing food allergies, has analyzed bacteria in the Clostridia class down to their flagella, which propel them around the gut. A study from her research group shows that flagella on Clostridia stimulate the immune system far differently than flagella on pathogenic bacteria a link that hadn’t been identified.
“That’s what makes microbiome research so exciting,” Nagler said. “It’s the ‘Wild West’ of science, a completely new frontier. The more we find out, the more we find out we don’t know.”
Duchossois Family Institute
In 2017, a $100 million gift from Janet and Craig Duchossois and The Duchossois Family Foundation established the Duchossois Family Institute: Harnessing the Microbiome and Immunity for Human Health.
The institute brings together 18 University of Chicago faculty members and more than 30 staff members from across disciplines to study the microbiome. Faculty have access to state-of-the-art research facilities that include:
Host-Microbe Metabolomics
Facility to measure and characterize metabolites produced by microbes
Microbiome Metagenomics
Facility to provide metagenomics sequence analyses on complex microbial populations
Symbiotic Bacterial Strain Bank that contains more than 1,690 bacterial strains from healthy human donors that have been cultured and characterized
uchicagomedicine.org/midway 15 MEDICINE ON THE MIDWAY SPRING 2024
Food preservative disrupts the gut microbiome
Lanthipeptides, a class of bacteriocins with highly potent antimicrobial properties, are widely used by the food industry to kill pathogens in foods such as beer, cheese and sausage. But they can affect beneficial bacteria as well, threatening the healthy balance of the gut microbiome, according to a joint UChicago and University of Illinois Urbana-Champaign study in ACS Chemical Biology. If too many commensal bacteria are indiscriminately killed by antimicrobial food preservatives, opportunistic pathogenic bacteria could wreak havoc, researchers suggest.
Turning innovation into intervention
Although new findings and published research on the gut microbiome have increased exponentially, many questions remain.

Matthew Odenwald, PhD’15, MD’17, has received federal approval to conduct a clinical trial that will provide probiotics to liver disease patients.
First, there is no universal agreement on what constitutes a healthy microbiome, since it can vary so much across age and cultures. Second, scientists still hope to disentangle the relationship between the gut microbiome and diseases beyond the GI tract.
The one thing scientists agree on is that prevention is easier than treatment. Which is why University experts are hopeful that more answers are within reach. “There has been a lot of hype and maybe some disappointment, but now we’re beginning to figure out exactly the ways in which these microbes interact with our bodies,” Light said.
Researchers know, for instance, that delivering key bacteria and the metabolites they produce to the gut is essential in rebalancing the gut microbiome. But it can be difficult to get bacteria to engraft in the gut.
Nagler and Jeffrey Hubbell, PhD, Eugene Bell Professor in Tissue Engineering, solved this problem by developing a polymer molecule designed to deliver metabolites directly to the gut.
The polymers, called micelles, are suspended in water and travel through the stomach to the small intestine and cecum, where they release the metabolite butyrate. Once there, butyrate helps repair intestinal barrier function and helps prevent food allergies.
The treatment was successful in mice, and the team formed startup ClostraBio
to bring it to clinical trials to treat food allergies.
Chang, meanwhile, has developed a marker panel to assess how well a person’s microbiome is functioning. His startup, Gateway Biome, has filed provisional patents and is negotiating with manufacturers to produce home collection kits for the stool samples needed for the panel. The team is also conducting clinical studies to develop marker panels for all stages of life.
“We think this will be not only diagnostic but a very effective management tool that can guide physicians in making medical decisions and determining the right therapy to help repair and restore the health of their patients’ microbiomes,” Chang said.
Finding solutions to restore the microbiome is the next logical step and it’s already underway, said Lehmann, an Assistant Professor of Medicine, who has also studied the connection between a healthy microbiome and reduced postoperative infections after liver transplant.
The Biological Sciences Division has a biobank containing thousands of bacteria, analyzed and categorized based on their genomes and what metabolites they produce. The University of Chicago is also building a Good Manufacturing Practicescompliant facility, where scientists can produce, filter and freeze-dry key gut bacteria from healthy donors and pack them into pharmaceutical-grade capsules.
Large or small, every step in the journey has a shared purpose. “Understanding the microbiome, testing the microbiome’s health and restoring the microbiome are all crucial new tools we can add to our arsenal,” Lehmann said.
16 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION
PHOTO BY NANCY WONG
Five questions with Milda Saunders, MD, MPH
BY DEVON MCPHEE
What is the mission of Pritzker Pathway?
What sets Pritzker Pathway apart?
Each summer, the eightweek Pritzker Pathway tracks Pritzker School of Medicine Experience in Research (PSOMER) and Chicago Academic Medicine Program (CAMP) match faculty mentors with undergraduates who are underrepresented in the health-related sciences.
Milda Saunders, MD, MPH, Associate Professor of Medicine and Director of Health Equity, Diversity and Inclusion Pathways Research Training, has directed the program since 2021. She spoke about its evolution and continued mission over the past two decades.
Our mission is to increase the number of underrepresented-in-medicine candidates who pursue medical school, particularly at the Pritzker School of Medicine.
The programs allow us to identify promising students and give them research opportunities and exposure to faculty and medical students. In turn, we get to know them and help them strengthen their candidacy for medical school.
Could you describe a typical summer?
Both programs begin with a daylong orientation, where students meet their mentors and learn the basics of conducting research. After that, the summer varies: Some participants work in the lab, some are doing data analysis in the library or looking through medical records to abstract data, while others interview research participants in the clinic or wards.
On Wednesdays, each program gathers separately to discuss their projects, and then everyone meets for didactics on research topics such as research ethics, analyzing data or healthcare disparities. CAMP participants also attend MCAT prep sessions. Our work culminates in an end-of-summer presentation session. It’s phenomenal what undergraduates can do in just eight weeks.

Our programs are run by clinician-researchers who have the same background as many of our students individuals who are Black or Hispanic/Latinx and who may have come from an educationally or economically disadvantaged backgrounds.
I lead CAMP, which is funded by the Pritzker Office of Health Equity, Diversity and Inclusion; PSOMER is led by Drs. Sola Olopade and Alejandra Lastra, and it’s funded through a grant from the National Heart, Lung and Blood Institute.
In addition to their mentors, participants get to know medical students, people from admissions, and even Dr. Vineet Arora, our Dean for Medical Education. We want them to feel like they’re now a part of us and to know that we are here to help in any way we can.
How have the programs changed?
We have worked to better integrate the programs so participants have a larger peer group and support network. These are the people that they’re going to see on the interview circuit, in medical school and throughout their careers.
We’ve also adapted our MCAT prep course, transitioning it from in person to online so participants can access the materials after the summer is over. My main goal is to continue the good work that leadership has done. We have a lot of great components that just work.
Why is exposure important for undergrads?
It allows them to see that medicine and research are not these completely impossible, abstract things. It also allows them to get to know current medical students and physicians, and realize that they are normal and approachable, which may not have been their perception.
Equally important, we know that patients get better care from clinicians who are culturally aware and share a similar background. So, we are not only making our students better, but we’re also making our medical workforce better for patients.
Q&A 17 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
PHOTO BY JORDAN PORTER-WOODRUFF
Communicators-in-chief
Editors share their paths from the University of Chicago to overseeing the pages of the world’s most prestigious scientific journals
All researchers strive to see their work in a prestigious journal. The people who decide which papers to publish are journal editors, some of whom are alumni of the Biological Sciences Division and/ or the Pritzker School of Medicine. Read about their passion for the work and how they vet submissions that can become game-changers for scientific progress.
Seth Thomas Scanlon, PhD’10
Editor, Science Immunology
STORY BY JAMIE BARTOSCH
PORTRAITS BY SIGI BISCHOF


Accolades for Albert: Scanlon’s thesis advisor, the late Albert Bendelac, MD, PhD, had an infectious love for immunology. “I’ve never met someone who appreciated an elegant experiment so much,” said Scanlon, who served as a teaching assistant in Bendelac’s University of Chicago immunology course and was one of three Bendelac trainees who became chief editors of prominent biomedical journals.
Happy in Holland: Although Science Immunology’s international office is in Cambridge, U.K., Scanlon mostly works from home in Ede, Netherlands, where he lives with his wife, Eva Heinen, a professor. The couple met in Cambridge while completing postdocs at the Medical Research Council’s Laboratory of Molecular Biology and Epidemiology Unit, respectively.
Timing is everything: Scanlon started a second postdoc at the University of Manchester, but he
quickly realized it wasn’t a good fit. While figuring out his next step, he heard Science’s immunology editor was leaving a rare vacancy. He got the job, rising to senior editor before leaving to become chief editor at Science Immunology in September 2023. Today, Scanlon publishes papers on such trending topics as cancer immunotherapy, immunometabolism, next-generation vaccines and neuroimmunology.
The top 7.4%: Science Immunology, launched in 2016, received 1,550 submissions last year (Science, by comparison, receives more than 10,000). Of those, about 15% are chosen for review and just 7.4% are accepted, said Scanlon, whose team works with academics from different subspecialties to decide what makes the cut. “It’s remarkable that such a young journal has been able to publish this many high-profile and cuttingedge immunology papers,” he said.
18 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION
JOURNAL EDITORS
Trailblazing research: Scanlon helped publish seminal early papers on COVID-19 transmission in mice. But his favorite paper answered a long-standing question: whether Charcot-Leyden crystals were pathologic or symptomatic in severe eosinophil-associated diseases like asthma and chronic rhinosinusitis. It also described the development
of antibodies that could pinpoint and dissolve the proteins that formed these crystals. “I find papers like this which finally answer centuries-old questions using new technologies immensely satisfying,” he said.
Memory lane: Scanlon served on a student committee that regularly
organized art exhibitions. He also has fond memories of his trivia team, led by Stephen Meredith, MD, PhD, which found moderate success at the Pub’s notoriously tough quiz. “It was so emblematic of life on campus: a heady mixture of intellectual challenge, camaraderie and good cheer,” Scanlon said.
Katie M. Given, AB’08, PhD’13, MBA’16, MD’16
Contributing Editor, Dermatologic Surgery
That’s a lot of maroon: Given’s extended family has a combined 17 degrees from the University of Chicago, including five relatives with Pritzker MDs.
Killer chemistry: While enrolled in a notoriously tough first-year chemistry course, Given once studied for an exam on the bus ride home after a volleyball tournament (she played for UChicago her first two undergraduate years). “The test was so hard, I thought: ‘Goodbye, medical school,’” she said. “I got a 48, but it ended up being the high score for the class!”
Winding career path: Given intended to be a physician-scientist and maybe run a lab. But after completing her PhD as part of a joint MD/PhD program, she returned to clinical rotations and pursued an MBA at Chicago Booth between her third and fourth years of medical school. “My path kept evolving,” she said. “The MBA helped me understand that my skills could be applied in different ways.” Ultimately, she chose dermatologic surgery.
Passion for research: As a chief resident at Yale New Haven Hospital, Given was awarded a T32 training grant funded by the National Institutes
of Health. That same year, she landed a competitive resident representative position on the American Society for Dermatologic Surgery’s Board of Directors, a group that included the editor of Dermatologic Surgery. Given emailed the editor to ask how a young person with her background could get more involved. His response? “You should be one of our editors.”
A pioneering field: A perk of an editor’s job, Given said, is getting an early look at cutting-edge research and innovation. In her case, that’s new devices, therapeutics and imaging techniques, as well as scientific understandings of newly discovered and understood pathways and mechanisms of action in immunology and pharmacology. Developments on the horizon include new targeted therapies for melanoma, and innovations in aging and skin rejuvenation, she said.
Now podcasting: Dermatologic Surgery recently launched a monthly podcast, Derm Surgery Digest, where editors and contributors discuss the latest issue. “You can listen in your car or while you’re running,” Given said. “Dermatology is a fast-changing, innovative field. If you don’t stay on top of it, you fall behind.”

Trust matters: In an era when scientific misinformation looms large, Given feels a deep responsibility to publish trustworthy information. “The University of Chicago taught me that we’re the gatekeepers, so pure, rigorous research matters,” she said. “It’s one of the reasons I pursue continuous learning while contributing to scholarship by taking editorial responsibility.”
19 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
Thomas Gajewski, AB’84, PhD’89, MD’91
Founder and Consulting Editor, Journal for ImmunoTherapy of Cancer ; Editor, Cancer Research
That’s ritzy: Gajewski helped rename his professional society to the Society for Immunotherapy of Cancer, or SITC (pronounced “sitsy”). It was cheekily chosen to rhyme with FITC (pronounced “fitsy”), the acronym for a common light-emitting conjugate in immunotherapy. The wordplay continued in 2013 with the launch of the Journal for ImmunoTherapy of Cancer, or JITC (aka “jitsy”). “It was all about marketing but it worked,” Gajewski said.
list receives monthly emails with links to published papers.


Keeping pace with progress: In the late 2010s, as the field of immunotherapy exploded and discoveries moved out of the lab, JITC began including guidelines that offered doctors evidence-based recommendations on how and when to introduce new therapies. “The pace of progress is pretty fast, so this has become an important component of the journal,” Gajewski said. “We want to be the go-to resource for everything connected to immunotherapy.”
Open to all: Gajewski felt strongly about making JITC an open access journal, making it available at no cost to researchers around the world who couldn’t afford access. It’s free to subscribe, so anyone on JITC’s email
Fabiola “Faby” Rivas, PhD’03
Deputy Editor, Immunity
Finding her path: A chat with the late UChicago immunologist Frank Fitch, MD’53, SM’57, PhD’60 who also served as The Journal of Immunology’s editor-in-chief had a career-changing effect on Rivas during her fourth year of graduate study. Fitch suggested that she pursue a postdoc position.
“It was fantastic advice,” Rivas said. “It gave me a lot more of the scientific breadth and expertise I needed, and it positioned me to get a very good editorial job.”
Eye-opening interview: The first journal job she applied for was scientific editor at Cell, and it involved an
Why he loves journals: As an editor, Gajewski a longtime UChicago Medicine cancer immunology physician-scientist hopes to share his expertise and maintain high standards in his journals. He also likes to get a peek at work that isn’t yet published, because it can change the way he thinks about a scientific problem. “The new information tweaks a detail of the working model you have in your head,” he said. “It keeps you at the forefront.”
Rigorous thinker: The late Frank Fitch, MD’53, SM’57, PhD’60, was Gajewski’s PhD mentor at the University of Chicago and helped guide his career as a cancer immunology researcher. Fitch, a former editor-in-chief at The Journal of Immunology, “was inspirational on the science side but also demonstrated how to be active in your society journal and to make an impact,” Gajewski said. “He basically taught rigorous thinking and gave me freedom to explore.”
extensive interview process. “I learned that an editor’s role is more about scientific discussion and teamwork,” said Rivas, who landed the position. “Working on many manuscripts, you get a landscape view of what’s happening in the field and can interact with many experts. You’re always learning.”
20 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION


The editorial process: At Immunity, Rivas and a five-person editing team select submissions that go out for peer review. She also guides the next steps
John Fung, PhD’80, MD’82
for each manuscript, advising authors on how to revise and present their findings. “We select what’s moving the needle in every field of immunology,” she said.
Why journals matter: After nearly 15 years as an editor, Rivas takes pride in the fair, thoughtful evaluation that goes into every paper. This means not only knowing the science, but also the authors and reviewers. “We can say, ‘OK, this person has this perspective, and the other one has this perspective,’ so we can integrate that to provide a fair assessment,” she said. “We focus on the science.”
Your friend, Immunity: Every research journal has a unique identity, and Immunity is no different. “It’s like a thoughtful friend,” Rivas said.
Editorial Board Member, Journal of the American College of Surgeons
Journal pioneer: Fung was president of the International Liver Transplantation Society when it launched Liver Transplantation, a firstof-its-kind journal in the late 1980s, in partnership with the American Association for the Study of Liver Diseases. Few journals were focused on transplant at the time; Fung served as its editor-in-chief from 2005 to 2010.
Impactful papers: As editor of Liver Transplantation, Fung greenlit early research papers on game-changing topics, including normothermic machine perfusion (NMP), which allows donated livers to be stored at body temperature for up to four days improving the organs’ function prior to transplant. “When we first published it, people said: ‘This is kind
of boring.’ They didn’t understand the ramifications of the technology,” Fung said. “But we were setting the foundation of how NMP would work.” Today, NMP is routinely used for transplants.
Making the cut: In his current role, Fung reviews between 30 and 40 papers a year for roughly two dozen journals. Sometimes he helps authors rewrite papers, especially if they struggle with English. “I’ve been doing this for 40-plus years, so at this point in my career, I want to help people publish,” he said. “It’s an obligation I have to the field. Because if you don’t publish, then it doesn’t exist.”
Open access advocate: With print ad revenue drying up, some journals have put up paywalls a practice Fung calls immoral. “Knowledge should be open to everybody,” he said.
“We’re a friendly journal, even though we reject a lot of papers. We like being part of the immunology community.”
Favorite journals: Two of Rivas’ favorite scientific journals as a student were The Journal of Immunology (aka “JI”) and Cell. “JI has a special place in my heart because they published my first paper as a grad student,” she said. “But Cell is probably my favorite. I like that it covers all aspects of biology. Their papers have findings that would be interesting to any scientist.”
Married to immunology: Rivas’ husband, Peter Savage, PhD, is an Associate Professor of Pathology at UChicago, where he was recently appointed chair of the Committee on Immunology.


21 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
“If you have a new treatment for, say, pancreatic cancer, and someone writes a paper about it and you can’t read it, you’re not doing the patient any favors.” Open access does have drawbacks, Fung said, including the growing “threat” of low-quality, payfor-play online journals.
A way to learn: Fung, who recently stepped down as Chief of the Section of Transplant Surgery at UChicago Medicine, but continues as Co-Director of its Transplant Institute, devotes 40 to 50 hours a month to reviewing and rewriting papers, simply because he loves to learn. He appreciates journal
Angela Colmone, PhD’06
summaries and subscription services that scour credible publications and email him a curated list of papers on a chosen topic. “Anything that makes it easier to read and digest journals makes it more likely that you’ll incorporate it into your practice,” Fung said.
Assistant Executive Director, Science and Publications, Radiological Society of North America (RSNA)


Career mentor: University of Chicago graduate advisor Chyung-Ru Wang, PhD, opened Colmone’s eyes to a journal editing career by pinpointing her strengths in science writing and project planning. “She had a giant impact on my life,” Colmone said. “She always had a lot of enthusiasm, and she encouraged exploration and innovation.”
First time in print: She had her first paper published in The Journal of Immunology while working as a graduate student in a UChicago lab. When the issue arrived, her colleagues gathered to see it, celebrating with cheers and hugs. “It was fantastic,” said Colmone, who earned her doctorate in immunology and went on to hold editorial roles at Science Immunology, Science Translational Medicine, The American Journal of Pathology and The Journal of Molecular Diagnostics
Passion for journal editing: “It’s the best job in the world if you’re interested in science,” said Colmone, who now works on the business side of the enterprise. “You can work with authors and researchers doing the work and help them find connections across fields.” One of her career highlights: publishing a paper by Carl June in Science Translational Medicine in 2011 on the first in-human studies of CAR T-cell therapy, paving the way for wider clinical use.
Privilege and duty: Scientists can easily share unvetted work online, but there may be issues of accuracy or even fraud, Colmone said. Which is
why she and other journal editors feel a deep responsibility to deliver content reviewed by third-party scientific experts. “To know that someone else has taken the time to go in-depth and do vetting you can trust is critical,” she said.
Drilling down the data: Increased attention is being given to the large data sets used in studies, Colmone said. Incorporating diverse patient populations (“not just patients from large hospitals and cities, but from a variety of areas and demographics around the world”) in her journals is necessary to avoid biases from affecting AI algorithms that play an increasingly pivotal role in healthcare settings.
Expanding her reach: This year, Colmone will oversee a major expansion of RSNA’s research journals by increasing the number of publications and taking new distribution approaches to reach larger audiences.
“Radiology is at the cutting edge of AI implementation in medicine,” she said. “There’s a lot of really exciting research going on and we’re hoping to share it broadly.”
22 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION

Healing arts
Vibrant collection of John E. Ellis, MD’82, celebrates community, opportunity
BY DIANE DUNGEY
The boy, stylishly dressed in aviator sunglasses, a tracksuit and sneakers, leans against a barrier outside the Loew’s Theatre in Harlem in a 1976 Dawoud Bey portrait. Another image, taken by Kwame Brathwaite in 1965, shows women and boys crowding a convertible at a parade celebrating political activist Marcus Garvey.
For John E. Ellis, MD’82, the photos are therapeutic.
“Some works are simply beautiful, others help me reminisce, some are matters of cultural pride, others are inspirational,” said Ellis, retired faculty at the University of Chicago’s Department of Anesthesia and Critical Care and an Alumni Board executive committee member. “I also like helping to support careers, especially those of younger emerging artists.”
Since moving to Hyde Park 47 years ago to enroll at the Pritzker School of Medicine where he was the only Black student in his graduating class Ellis
has amassed more than 130 pieces of contemporary art by Black creators, primarily photography. He also became an arts ambassador. Today, he heads the board of directors of the Hyde Park Jazz Festival and he is a board member at the Smart Art Museum. Recently, the 66-year-old served as a juror at UChicago’s Arts + Public Life, an initiative that provides artist residencies, education, programming and exhibitions.
And he made a promise to the Art Institute of Chicago: the Kwame Brathwaite parade photo, loaned to the museum last year for an exhibit, one day will reside there.
From New York to Chicago
Raised in Queens by a family that valued the arts, Ellis’ first love was the stage. He acted regularly in plays while attending The Hotchkiss School, a boarding school in Connecticut, while preparing to enter Harvard University.

The collection includes “Vision Painting: No. 2, 2020” by Candida Alvarez.
23 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
PHOTOS BY JORDAN PORTER-WOODRUFF
As a college sophomore studying biochemistry, Ellis appeared in “Simple’s Harlem,” a production based on Langston Hughes’ short stories, but he gave up acting to focus on academics.
In 1977 at age 19, Ellis enrolled in the Pritzker School of Medicine, which he chose for its “record of producing physician scientists.” (Ongoing progress to diversify medical education has been gratifying: “It’s amazing to me to see how many AfricanAmerican residents and attendings are at the University of Chicago now,” he said.)

After a residency at the University of Virginia, Ellis returned for a fellowship with Michael Roizen, MD, then Chair of UChicago’s Department of Anesthesia and Critical Care.
Impressed by the breadth of research and advanced technology, Ellis joined the faculty in 1987 as a cardiovascular anesthesiologist, where he helped to create one of the first electronic records platforms for anesthesiology patients.
“It almost became the de facto pre-op note for the surgical residents before there was Epic and all this stuff,” said Ellis, noting that the effort predated the Health Insurance Portability and Accountability Act of 1996.

Cultural connoisseur
Amid the demands of medicine, Ellis stayed drawn to Chicago’s art scene.
He joined a young professionals group through the nonprofit Urban Gateways, where members would gather at the homes of established art collectors including James Jones, MD, UChicago’s first Black physician granted admitting privileges.


A visit to the Isobel Neal Gallery in River North prompted Ellis to purchase his first work by his favorite artist, Roy DeCarava. The black-and-white photo of four boys on the fire escape and steps of a brownstone in 1950 captivated Ellis with its rich tones.
Decades later, he bought another DeCarava at a fundraiser for former President Barack Obama. Chicago names are prominent in Ellis’ collection. Among them are Bey, a professor at Columbia College Chicago, and Amanda Williams, whose series “Chicago Is Iraq?” is represented. Both artists have been awarded the MacArthur Fellowship.
Supporters like Ellis are vital for their “commitment to supporting Black artists early on and developing relationships,” said Williams, a UChicago Laboratory Schools graduate. Her first solo museum exhibit, in 2017 at the Museum of Contemporary Art Chicago, was co-sponsored by Ellis.
Vivid, meaningful collection
Art lines the walls at Ellis’ sun-drenched 38th-floor apartment overlooking Jackson Park and Lake Michigan.
A corner of his living room is vibrant with a painting by Chicago-based Caroline Kent, flanked by “Chasing Snakes in the Grass” by Duhirwe Rushemeza and a Patrick Alston piece that invokes the “colors and abstraction one sees in graffiti,” Ellis said.
Bey’s photo “Couple in Prospect Park” is part of a hallway display near “Untitled (Altar No. 10),” a graphite-on-paper work by Nate Young of Chicago.
Ellis’ collecting style is simple. It comes down, he said, to buying pieces that “are meaningful to me.”
Ellis retired from practicing medicine in 2008 after his second surgery for cervical myelopathy. Between developing a continuing education platform for anesthesiology professionals and teaching, he continues to invest in art.
A work’s future valuation doesn’t drive the pursuit, and he has not sold a single acquired piece.
“I never tire of seeing the works that I have in my home,” Ellis said, with a smile.
24 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION
Strength in numbers
A global pursuit to unite health data is helping Samuel Volchenboum, MD, PhD, MS, find answers that inform new treatments
BY JEN A. MILLER

Developing therapeutics for rare diseases is an uphill battle, Samuel Volchenboum, MD, PhD, MS, knows.
Researchers may struggle to obtain funding to study diseases that affect a small segment of the population such as neuroblastoma, a pediatric cancer diagnosed in about 800 children each year in the United States. And rare diseases often lack enough standardized patient data to identify trends and biomarkers, evaluate treatments and stratify risk.
“Even the busiest hospitals will have only a few cases of any particular kind of pediatric cancer,” said Volchenboum, Professor of Pediatrics and Associate Chief Research Informatics Officer for the Biological Sciences Division (BSD) at the University of Chicago.
“To make any headway, the community really has to come together and share clinical trials and data.”
With the help of advanced computational tools and partnerships, Volchenboum is leading a
collaborative charge to collect and analyze pediatric cancer data from across the world.
As principal investigator of the fittingly named Data for the Common Good (D4CG), a group headquartered in the Department of Pediatrics at UChicago, Volchenboum facilitates sharing of health data from a wide range of institutions, groups and countries.
His goal is twofold: to support research breakthroughs and also to compile massive, highly detailed data troves that can do everything from helping tackle other rare diseases to aiding patients with more routine problems, like potential complications from being in the ICU.
“The work we do supports the entire spectrum of health research from facilitating better ways to analyze genomic data to helping discern which patients are at risk for developing sepsis in hospital,” he said. “By harnessing the power of high-quality
Samuel Volchenboum, MD, PhD, MS, says high-quality big data will “revolutionize how we treat millions of patients.”
25 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
PHOTO BY NANCY WONG
The Pediatric Cancer Data Commons
BY THE NUMBERS
43,285
Total participants in the PCDC Data Portal
35 Number of countries portal users logged in from
6
Types of pediatric cancer with data in the portal, with 5 more planned by the end of 2024
35 Research projects now approved or in progress
Source: Data for the Common Good
big data, analytics and new technologies, we can revolutionize how we treat millions of patients.”
The pursuit began decades ago. A lifetime of dual interests in computing and medicine led Volchenboum to consider throughout his MD and PhD studies how to become a “doctor who did computer science, rather than a computer scientist who dabbled in healthcare.”
His passions grew during a pediatric hematology/ oncology fellowship at the Dana-Farber Cancer Institute and Boston Children’s Hospital, and while pursuing a fellowship in informatics and a master’s degree in biomedical informatics at the Massachusetts Institute of Technology.
Today, the concept of biomedical informatics which Volchenboum describes as “leveraging data, information and knowledge to improve human health” supplies the foundation for his complex mission.
Data-driven discoveries
Pooling data resources to fuel breakthroughs isn’t new. In the 1960s and 1970s, hospitals all over the world treating pediatric cancers coalesced into cooperative groups to learn more about these deadly diseases and to collaborate on clinical trials.
“Pediatric oncologists could use the same treatment protocols in a consistent way and learn from every patient by bringing all the data together,” Volchenboum said. Over time, he noted, “many pediatric cancers that once were a death sentence are now cured 80 percent, and sometimes 90 percent, of the time.”
But they could do better, he thought, especially with more computing power.
Volchenboum joined the University of Chicago faculty in 2007, where he started a research group that would become D4CG. Initially targeting neuroblastoma, the team broadened their focus in 2019 to include other pediatric cancers.
This led to the creation of D4CG’s flagship project, the Pediatric Cancer Data Commons (PCDC), which collects cancer data from around the world. The PCDC Data Portal, launched in 2021, makes the data available in a single platform for researchers.
“Imagine the power of taking data collected all over the world on these rare pediatric cancers over the past 30 years and harmonizing it all into a unified standard for researchers,” Volchenboum said. “We have over 43,000 kids’ data in the Commons, and we expect this number to grow considerably.”
Patterns and trends found in the data can inform progress. “Until recently, there weren’t
many new drugs to treat pediatric cancers, but the way we use the drugs has changed dramatically,” Volchenboum said. “The ability to stratify patients based on genetic testing has also changed, allowing patients to receive the most appropriate treatment for their cancer. Further, new sensitive approaches to detecting residual tumor cells have made disease surveillance during and after treatment much more effective.”
In March, the White House Office of Science and Technology Policy named the PCDC as one of five Champions of Open Science. Selected from a nationwide pool, the effort was cited in a statement from the White House for its mission “to push the boundaries of research and improve health” and its potential to aid the Cancer Moonshot.
Progress and partnerships
Not only does D4CG bring data together through international consortia, members also work carefully to standardize the information a critical step for accurate, actionable analysis.
“Groups may collect data differently for features like biological sex or race and ethnicity, making it difficult to combine and aggregate data sets,” Volchenboum said. “Extrapolate that to much more complicated concepts like tumor stage or adverse events from chemotherapy, and it can be nearly impossible to bring these data sets together in a meaningful way.”
By addressing this issue, the PCDC has enabled substantial advancements in the ways children with cancer are treated, including:
■ Better treatment approaches in pediatric non-rhabdomyosarcoma soft tissue sarcomas
■ Molecular testing in rhabdomyosarcoma soft tissue sarcomas to improve risk stratification and outcomes
■ Improved surgical management of paratesticular rhabdomyosarcoma
■ Proof that clinical trial participation leads to better outcomes for children with intermediate- or highrisk neuroblastoma
With growing interest from non-pediatric cancer groups in building similar platforms, Volchenboum’s group last year rebranded as D4CG to reflect a wider mission and to tackle other diseases, particularly rare ones and rarer subtypes of common diseases.
Recently, D4CG has spearheaded work in monogenic diabetes and monogenic epilepsies, with the latter made possible in part by a grant from the
26 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION
Chan Zuckerberg Initiative DAF, an advised fund of Silicon Valley Community Foundation.
In addition to his international work, Volchenboum is deeply involved in bioinformatics efforts in Chicago. For six years, he ran the Center for Research Informatics at the University, providing support for the BSD as well as private industry including high-performance computing, applications development and access to HIPAAcompliant storage.
He’s also the informatics core leader for the Institute for Translational Medicine (ITM), a partnership between UChicago and Rush in collaboration with Advocate Aurora Health, the Illinois Institute of Technology, Loyola University Chicago and Endeavor Health.
The institute, founded in 2007, is among about 60 sites in a nationwide network supported by the National Institutes of Health. It is currently leading a multidisciplinary consortium using D4CG’s expertise to build the Sociome Data Commons, a research platform for large-scale data analysis, including publicly available geocoded data sets about such nonclinical aspects affecting public health as social and economic factors.
New ideas, programs ahead
Volchenboum credits the University for supporting bold, cross-organizational collaboration, as well as guidance from faculty in public policy, computer science and precision health.
“Within the University community, there are very few constraints to trying a new approach,” he said. “Given the audacity of trying to create a worldwide resource for data sharing, one would expect pushback. On the contrary, there has been universal support for this important work, and I think this is a unique feature of the University of Chicago.”
Volchenboum, who also serves as Associate Dean of Master’s Education for the BSD, recognizes that the future of bioinformatics depends on new blood and ideas.
In 2023, the BSD and the University of Chicago Booth School of Business announced a new joint master of science in biomedical sciences and master of business administration program to pair foundational biomedicine training with leadership and management skills.
And this summer, Volchenboum will launch the Center for Data Democratization, a centralized resource for researchers worldwide. By convening interdisciplinary experts, the center will accelerate
the understanding of fundamental questions in health and disease, build novel analytic tools and foster cohorts of clinical informaticians committed to scholarly investigation.

“A collaborative, standards-focused approach to collecting and using data has the potential to accelerate research in so many areas,” Volchenboum said. “Our ultimate vision is that access to highquality data should never be a barrier to improving human health.”
New joint degree program trains healthcare leaders
TVolchenboum spends time with UChicago Medicine Comer Children’s Hospital patient Alexander Brown, 5.
he University of Chicago Biological Sciences Division and Booth School of Business have teamed up to offer a new joint Master of Science in Biomedical Sciences (BMS) and Master of Business Administration (MBA) degree.
The two-year program teaches students to combine business expertise with foundational knowledge in biomedicine, preparing them for careers in such fields as biotechnology, policy, government and pharmaceuticals.
The BMS program one of four master’s degree programs offered by the BSD provides a core curriculum focused on applications and innovations in clinical care and medical treatment, statistics, bioethics and the American healthcare system. The new joint program also includes 14 courses from Booth’s MBA program and an experiential leadership development course.
27 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
PHOTO BY NANCY WONG
Building a ‘bionic’ breast
Implantable device aims to restore the sense of touch after reconstructive surgery
About one-third of the 3.5 million breast cancer survivors in the United States have had a mastectomy to remove one or both breasts. Although a majority of these women report sexual dysfunction following surgery, few patients receive the opportunity to weigh the long-term sensory effects with their doctor beforehand, Stacy Tessler Lindau, MD, AM’02, said.
“For many people, it’s not just a physical loss, but also a psychological and even an existential one,” said Lindau, Catherine Lindsay Dobson Professor of Obstetrics and Gynecology and Medicine at the University of Chicago, who has spent her career studying how to preserve sexual function in women after cancer treatment.
Lindau is now working with neuroscientists and biomedical engineers to build an implantable device that can restore sensation to the breast after surgery.
The Bionic Breast Project, launched with exploratory funding from the
UChicago Medicine Comprehensive Cancer Center and the National Cancer Institute, has received nearly $4 million from the National Institutes of Health to begin an early clinical trial that will test components of the device in patients.
Recreating natural sensations
The Bionic Breast device is based in part on research by Sliman Bensmaia, PhD, a pioneering neuroscientist at UChicago who died unexpectedly in August 2023. His lab published influential studies that offered blueprints for creating fully “embodied” prosthetic limbs that feel like a natural part of the body and produce the same sensations by connecting devices either directly to the brain or to remaining nerves in an amputated limb. These devices send and receive electrical signals that are translated into movements and sensory feedback from the prosthetic.
In 2016, after Lindau heard about Bensmaia’s work, the pair began

C
collaborating. Today, Lindau and her team are sustaining Bensmaia’s legacy and the bionic breast idea with help from collaborators at UChicago, Case Western Reserve University and other institutions.
The device will include a sensor being developed by Sihong Wang, PhD, Assistant Professor of Molecular Engineering at the Pritzker School of Molecular Engineering. Implanted under the nipple and areola or the central part of the reconstructed breast, it will respond to touch, pressure and other stimuli by routing electrical output to the nervous system interface.
Restoring
a sense of self
Lindau will soon work with surgeons at UChicago Medicine to recruit patients who are set to undergo a mastectomy and willing to test early iterations of the device.
An electrode will be implanted at the time of a patient’s mastectomy and first stage of breast reconstruction via thin, flexible electrical leads inserted through skin under the arm. A lab team will test the device by delivering electrical impulses through the leads, with recipients reporting how different sensations feel. The device will be removed at the time of the second stage of reconstructive surgery.
Lindau says the project addresses a critical physical function issue that too often is an afterthought.
“Even if their breasts are cosmetically restored, women still have many of the same experiences as a person who loses a limb,” she said. “Patients want frank but compassionate communication, with the recognition that what’s being lost is not just the feeling of sensation in the breast, but also of a vital organ with sexual and many other functions.”
28 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION BSD News
BIOMEDICAL TECHNOLOGY
Pressure sensor
Electronic circuit
A
B
Electrode array ILLUSTRATION BY KATIE H. LONG
Nutrient in beef, dairy products may fight cancer
Trans-vaccenic acid (TVA), a long-chain fatty acid found in meat and dairy products from grazing animals, improves the ability of CD8+ T cells to infiltrate tumors and kill cancer cells, according to a new study by researchers from the University of Chicago.
The study, published in Nature, also shows patients with higher levels of TVA circulating in the blood responded better to immunotherapy, suggesting that TVA could have potential as a nutritional supplement to complement clinical treatments for cancer.
“There are many studies trying to decipher the link between diet and human health, and it’s very difficult to understand the underlying mechanisms because of the wide variety of foods people eat,” said Jing Chen, PhD, Janet Davison Rowley Distinguished Service Professor of Medicine at UChicago and a senior author of the study.
“By focusing on nutrients that can activate T cell responses, we found one that actually enhances anti-tumor immunity by activating an important immune pathway.”
The research team fed mice with diverse tumor types a diet enriched with TVA, which significantly reduced the tumor
growth potential of melanoma and colon cancer cells compared to mice on a control diet. TVA also enhanced the ability of CD8+ T cells to infiltrate tumors.
A series of molecular and genetic analyses were performed to understand
analyze blood samples from patients undergoing CAR T-cell therapy for lymphoma. Patients with higher levels of TVA, they learned, responded better to treatment. And with help from Wendy Stock, MD, Anjuli Seth Nayak Professor of

how TVA was affecting the T cells. These included a new technique for monitoring transcription of single-stranded DNA developed by Chuan He, PhD, John T. Wilson Distinguished Service Professor of Chemistry and another senior author of the study.
Finally, the group worked with Justin Kline, MD, Professor of Medicine, to
Medicine, the researchers also discovered that TVA enhanced the ability of an immunotherapy drug to kill leukemia cells. Chen emphasized the study shouldn’t be an excuse to eat more hamburgers and pizza. Still, he said early data shows that there may be other nutrients including plant-based fatty acids that also can promote T cell activity.
An oral alternative for diabetes treatment
An existing drug could be repurposed to treat Type 1 diabetes, potentially reducing dependence on insulin injections as the sole treatment. A new study led by researchers at the University of Chicago and Indiana University centers on a medication known as α-difluoromethylornithine (DFMO), which inhibits an enzyme that plays a key role in cellular metabolism.
The new study, published in Cell Medicine Reports, reflects years of work. In 2010, while corresponding author Raghu Mirmira, MD, PhD, was at Indiana University, he and his lab performed fundamental biochemistry experiments on beta cells in culture.
They found that suppressing the metabolic pathway altered by DFMO helped protect beta cells from environmental factors, hinting at the possibility of preserving and even restoring these insulin-producing cells which, for people with Type 1 diabetes, are attacked and destroyed by their immune systems. A subsequent clinical trial found that the drug, taken orally, is safe for Type 1 diabetes patients and can stabilize insulin levels by protecting beta cells.
DFMO has been FDA-approved as a high-dose injection for treating African sleeping sickness since 1990, and the
medication received breakthrough therapy designation for neuroblastoma maintenance therapy after remission in 2020. This could enable its use in Type 1 diabetes.
“The approval timeline can be a matter of years instead of decades once you have solid clinical evidence for safety and efficacy,” said Mirmira, who is now Professor of Medicine and an endocrinologist at UChicago Medicine. “It’s exciting to say we have a drug that works differently from every other treatment we have for this disease.”
29 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
RESEARCH
Moth man tackles insects’ growing threat amid climate change
BY SABRINA ARIF
Under the right conditions, insect infestations can cause defoliation the removal of leaves from trees that sets off a domino effect of big problems.
Among them: dead trees, halted timber production and excess carbon in the atmosphere from decomposition that, in a vicious cycle, causes warmer temperatures ultimately more favorable to the insects.


Greg Dwyer, PhD, Professor of Ecology and Evolution at the University of Chicago, and his students are modeling the delicate relationship between forests, the spongy moth and its naturally occurring pathogens, including nucleopolyhedrovirus (NPV), that infect and kill spongy moth caterpillars.
“I have been fascinated by ecological problems since high school,” said Dwyer, a self-described country kid who has studied the topic for 30 years.
Moth populations boom when environmental factors cause predators such as mice and squirrels to decrease. But higher densities of the insects allow NPV to help curb the infestation. A 2004 study by Dwyer published in Nature was the first to fold these factors into one model.
In 2013, another study published by Dwyer and his colleagues found that spongy moth outbreaks can be more severe in areas with oak trees. A mildly toxic molecule produced by the tree after defoliation, they found, makes spongy moth larvae less susceptible to a baculovirus infection.
‘Making little epidemics’
Still, as global temperatures rise, even the most sensitive models may become inadequate, according to a study by Dwyer and his former students Colin Kyle, PhD’15, SM’15, and Jiawei Liu, PhD’22, SM’22.
In 2020, Kyle and Liu designed models that explored how host density and weather conditions influence outbreaks of another spongy moth pathogen, Entomophaga maimaiga.
“We learned that modest changes in temperature and humidity can have very big changes on interactions between species,” Dwyer said. “I didn’t see that coming.”

A key challenge in uncovering the relationship between defoliation, insect populations and climate change, Dwyer said, is defining the variables that shape a model’s predictive power.
After refining the list of inputs, researchers must find a way to mathematically simulate real-world scenarios a tall order when the data are longitudinal and ever-changing. But even the most reliable models are of little use without quality input data.
The solution? “We collect insects from naturally occurring populations, bring them back to the lab and see who’s infected, and what strain they’re infected with,” Dwyer said. “We put them together on a branch, and we see how and what fraction gets the virus.
“It’s making little epidemics on branches.”
Branching out
The capabilities of Dwyer’s lab have led to collaborations with climate scientists at Argonne National Laboratory, as well as researchers investigating human viruses, such as HPV. Dwyer has also worked with researchers at the University of Chicago Harris School of Public Policy to study how spongy moth outbreaks affect housing values.
Most notably, he’s providing guidance to the U.S. Forest Service about how and where to spray NPV to help curtail the destructive cycle. Armed with loads of federal data, Dwyer is tackling ways to forecast moth infestations across different areas and populations and how to scale other hurdles ahead.
“Climate change will likely reduce the ability of the disease to control the insect,” Dwyer said. “And that, of course, is a huge problem.”
30 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION BSD News ECOLOGY
Top: Greg Dwyer, PhD, works with doctoral student Bonnie Mendelson. Bottom: Douglas-fir tussock moth caterpillars are seen on their preferred foliage.
An adult female spongy moth perched atop an egg mass.
PHOTO BY GREG DWYER, PHD
PHOTO BY ALISON HUNTER, PHD
PHOTO BY KATIE DIXON
Emily Rogalski, PhD, awarded professorship, research center to study ‘SuperAgers’
Emily Rogalski, PhD, a clinical and cognitive neuroscientist who joined the University of Chicago in September, has been named the first Rosalind Franklin PhD Professor in the Department of Neurology.
She also has been tapped to lead the new UChicago Healthy Aging and Alzheimer’s Research Care Center, which will house a diverse group of scientists and health experts to accelerate breakthroughs in aging, dementia and cognitive resilience.
Early in her career, Rogalski operationalized the term “SuperAgers” to describe people over the age of 80 whose memory still functions as well as that of someone in their 50s or 60s. Today, she leads an international team whose research methods encompass a wide range of assessments to understand the intricate factors contributing to healthy brain aging.
Shyam Prabhakaran, MD, MS, James Nelson and Anna Louise Raymond Professor of Neurology and Chair of the Department of Neurology, called Rogalski “a catalytic leader” at a time when aging
and dementia are top concerns among surveyed Americans surpassing cancer, heart disease and stroke.
“Research is better when we do it together,” Rogalski said. “In collaborations, some people are deep specialists, while others are go-betweens who bridge disciplines, and we need both.
“At the center, we want to be those go-betweens integrating rich expertise in cognition, imaging and neuroscience with genetics and other key disciplines.”
Rogalski has also made significant contributions in the field of Alzheimer’s and related dementias, especially primary progressive aphasia, and she has helped pioneer telehealth interventions for individuals affected by these disorders.
In February, she was one of two multiple principal investigators awarded a grant from the National Institutes of Health to advance the Communication Bridge Research Program for primary progressive aphasia.
Peter Savage, PhD, appointed chair of Committee on Immunology
Peter Savage, PhD, Associate Professor of Pathology, has been appointed Chair of the Committee on Immunology (COI), effective April 1.
He fills the role previously held by Bana Jabri, MD, PhD, who chaired the committee from July 2020. Jabri will become Director of Institut Imagine in Paris beginning in January 2025.
Savage’s research focuses on the cellular and molecular mechanisms regulating immune tolerance and the immune response to cancer, with special emphasis on the biology of Foxp3-expressing regulatory T cells, self-reactive conventional T cell populations and tumor-associated T cells.
He has been an active member of the COI, the Committee on Cancer Biology, and the University of Chicago Comprehensive Cancer Center. Since 2018,
he has served as the Director of the Interdisciplinary Training Program in Immunology that supports graduate education in COI.
From 2016 to 2023, Savage served as Co-Leader of the Immunology and Cancer Program within the Comprehensive Cancer Center. He has also directly mentored graduate students and taught numerous graduate courses, including a Cancer Immunology course developed with Professor of Medicine Justin Kline, MD.
Savage received a BA in biochemistry from the University of Virginia and a PhD in cancer biology from the Stanford University of School of Medicine. Following postdoctoral fellowships at the University of California, Berkeley, and Memorial SloanKettering Cancer Center, he joined the UChicago faculty in 2009.


31 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
LEADERSHIP
Emily Rogalski, PhD
Peter Savage, PhD

Signaling their intent
Virtual tokens to help applicants court their top residency programs are also helping administrators streamline the process
Anew tool for residency applicants to express strong interest in a specific program could be compared to another kind of match process: online dating.
Virtual tokens known as “signals” which are sent to confirm that a program is among a person’s top choices are “kind of like ‘swiping right,’” said Olivier Joseph, MD’23, a first-year psychiatry resident at NewYork-Presbyterian/ Columbia University Irving Medical Center and the New York State Psychiatric Institute.
Signaling was introduced in 2020 as part of the otolaryngology residency application process, and it has since been widely adopted (although the allotted number and influence of tokens vary by specialty).
But the goal is universal: to reduce the colossal volume of applications that many
residency administrators receive every year and to help improve the likelihood of a strong match.
“Instead of looking at a sea of applications and having to go through all of them with a fine-tooth comb to guess the level of interest, programs have a very clear indicator attached to individual applications that expresses a higher level of interest,” said James Woodruff, MD, Dean of Students at the Pritzker School of Medicine.
For Joseph, who sent signals to his five preferred residency programs including Columbia as part of his 30 applications, signaling was useful after he had decided where in the country he wanted to be and which programs aligned with his goals and values.
“I had very specific programs in mind,” Joseph said, “and it was my hope that one way or another I jumped onto their radars.”
BY SARAH RICHARDS
Application overload
Before signaling, which is now part of the Electronic Residency Application Service (ERAS), graduating medical students desperate to match anywhere were applying to more and more residency programs.
The resulting tsunami did more than overwhelm administrators like Woodruff, who, as a former director of the internal medicine residency program at the University of Chicago Medicine, would some years receive up to 4,000 applications for 31 spots.
Applicants who could afford to pursue dozens of programs ended up fueling an arms race, said Tyler Lockman, Pritzker’s manager of career advising and student services.
“There were students who would basically have to put $3,000 or more on a credit card just to apply to the programs, and most of the programs they were
Dean’s Letter 32 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION Pritzker News
applying to weren’t going to interview them anyway,” Lockman said.
Today, professional organizations, such as the Society of Neurological Surgeons, determine how many signals will be available for a specialty in a given year. Calculations are based in part on the average number of applicants and available residency spots.
More competitive specialties typically dole out more signals. Orthopaedic surgery applicants, for instance, received 30 signals each this year; neurology applicants got only three.
The types of signaling also can vary. Some specialties, including dermatology and anesthesiology, use tiered signaling, where applicants use ‘gold’ and ‘silver’ tokens to indicate preferred choices. Many specialties include geographic signaling that allows applicants to choose a set number of regions where they are most interested in training.
Highly powerful tool
Data from the Association of American Medical Colleges, which developed ERAS, report a drop in average application numbers for many specialties a sign suggesting that signaling may be having its intended effect.
Lockman said Pritzker students are still securing a “pretty good” yield of interviews from their signals but noted that “we’re going to have to keep on our toes, because this process is just going to keep changing.”
Still, he considers signaling to be the most powerful tool for generating an interview offer after taking an applicant’s experience into consideration.
Lockman and Woodruff recommend students take a candid outlook about their abilities and the programs best suited to their goals when choosing where to signal. They also advise signaling a diverse range of institutions; the token isn’t a golden ticket, after all.
“Each signal adds significant value to a student’s success, so using them all to apply to the most competitive programs in the country risks wasting signals,” Woodruff said.
Signaling can present a unique challenge for couples hoping to match in the same place. Fewer interviews, even if they carry greater weight, could mean there is less chance both applicants’ interviews will geographically overlap.
‘It’s a good thing’
Fourth-year Pritzker student Ashley Diaz was eager to match in the same internal medicine program or the same city as Daniel Bujnowski, her partner of six years, who is studying at Loyola University Chicago’s Stritch School of Medicine.
With Lockman’s guidance, Diaz used six of her seven individual signals on the same programs that Bujnowski did and both signaled for the same geographic region.
“ Sending applications to 70 schools just doesn’t make sense. I’m happy that my list is nice and condensed, and it’s only places that I’m definitely interested in.”
Sharbel Romanos, fourth-year student, Pritzker School of Medicine
The couple scored interviews at six of their preferred programs, while also receiving many interviews elsewhere.
Sharbel Romanos, also a fourth-year at Pritzker, is hoping to match this spring in neurosurgery. He found signaling to be “a little stressful,” and it forced him to consider where he would best match early in the application process, but the results have been promising.
Romanos, who had 25 signals and applied to 45 residency programs, chose not to signal for geographic preference. He’s pleased to have earned 10 interviews all at places he signaled.
“It’s a good thing we’re kind of getting the numbers down, because sending applications to 70 schools just doesn’t make sense,” Romanos said. “At the end of the day, I’m happy that my list is nice and condensed, and it’s only places that I’m definitely interested in.”
Federal funding thaw expands residency slots
The University of Chicago Medicine is one of a handful of academic medical centers to be awarded new residency positions as part of a five-year national plan to add 1,000 new Medicare-supported residency slots to teaching hospitals in geographic areas with underserved communities.
UChicago Medicine will add one additional position each to the diagnostic radiology and urology residency programs, bringing the organization’s total number to 174 incoming residents per year.
The effort marks a welcome boost for hospitals affected by a 1997 federal law that limited funding of residency programs, essentially stunting the number of doctors who can begin their training after completing medical school.
“While many focus on medical school slots, it is important to know the major bottleneck in the U.S. is actually at the residency level,” said Vineet Arora, MD, AM’03, Dean for Medical Education at the Pritzker School of Medicine. “Nationally expanding graduate medical education in areas with a workforce shortage is desirable, because there’s a strong association between where people train in residency and where they end up practicing.”
The Association of American Medical Colleges estimates a doctor shortage that could reach 124,000 jobs by 2034.
“Unless we significantly expand training positions so that people have a place to train, we’re not going to fix our workforce shortage problem,” said Christine Babcock, MD, Associate Dean for Graduate Medical Education. UChicago Medicine will be applying to receive additional Medicaresupported residency positions over the next three years, she said.
33 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
Pritzker’s ‘COVID class’ takes the next step forward
BY JAMIE BARTOSCH
Ida Noyes Hall fell silent at 11 a.m. on March 15 as 91 students at the University of Chicago Pritzker School of Medicine simultaneously tore open their envelopes to learn which hospitals they matched with for their residency training.
The room, heavy with nerves, erupted with joyful screams.
Students popped out of their seats and shouted in excitement. Some raised their fists in the air and tearfully hugged friends and family in attendance for Match Day an annual event that includes speeches, senior superlatives, photo montages, prize giveaways and, finally, a countdown to the big reveal.
“All of you going through this are ready and poised to make the world a better place,” said Mark Anderson, MD, PhD, Dean of the Biological Sciences Division and the Pritzker School of Medicine. “For those of you leaving, you’ll always be part of the Pritzker family.”
The group was informally nicknamed “the COVID class” because they started medical school in 2020 with masks, face shields and

social distancing, said student Melinique Walls Castellanos, one of the Pritzker Chiefs, who spoke at the festivities.
Leslie McCauley cried after seeing she’d matched with her first choice, Northwestern Medicine’s OB-GYN program. Her father wept as well.
“I’m just so proud of my daughter,” said Peter McCauley, MD’86. “Watching her go through all of this, and seeing this day, is such a sense of relief and pride.”

Peter McCauley, MD’86, joins his daughter, Leslie, who is headed to Northwestern Medicine’s OB-GYN program.

Romy Peña, AB’20, joked that her mind went blank as she stared at the paper saying she’d matched with the University of Chicago Medical Center for internal medicine. “When I saw UChicago, I was just so relieved and so happy,” she said. “I did my undergrad here, too, and I just love the patients we serve.”
Nationally, there was a record high number of applicants to residency programs, according to the National Resident Matching Program. That number is largely attributed to an increase in non-U.S. citizen international medicine graduates and osteopathic (DO) seniors.
Most popular specialties
Internal medicine
(22 students)
Anesthesiology (12)
Family medicine (11)
General surgery (6)
Psychiatry (6)
Most popular institutions
A group of Pritzker students show where they’ll be doing their residencies during a Match Day celebration on March 15.
Allen Chengzhi Zhu, SB’16, PhD’21, and his friends are all smiles after learning he matched with BarnesJewish Hospital in St. Louis.
University of Chicago Medical Center (12)
University of California system (9)
Northwestern University programs (7)
Harvard University programs (6)
NewYork-Presbyterian Hospital/Columbia
University Irving Medical Center (5)
University of Illinois College of Medicine (5)
Washington University in St. Louis (5)
34 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION Pritzker News
PHOTOS BY JOE STERBENC
MATCH DAY 2024
AWARDS
UChicago and Pritzker School of Medicine receive AAMC honors
Three members of the University of Chicago community have been recognized by the American Association of Medical Colleges (AAMC) for making significant contributions to medical education, research, clinical care and community engagement. Their achievements were highlighted at the AAMC Annual Awards in November.

Selwyn O. Rogers, Jr., MD, MPH
Department of Surgery
Rogers, James E. Bowman, Jr. Professor of Surgery and the Executive Vice President for Community Health Engagement, received the Louis W. Sullivan, MD, Award which honors a healthcare leader committed to workforce diversity. Rogers was recognized for his work as founding director of the UChicago Medicine Trauma Center and for ensuring its staff reflects the community.
Amani Allen Pritzker School of Medicine
For her work addressing obesity and diabetes disparities, and for helping launch a student-run clinic on the South Side of Chicago, Allen was awarded a Herbert W. Nickens Medical Student Scholarship, one of five awards given to incoming third-year medical school students who have shown leadership in efforts to eliminate inequities in medical education and healthcare.


Tyler Lockman
Pritzker School of Medicine
Lockman is the manager of career advising and student services. He was honored with the Careers in Medicine Excellence in Medical Student Career Advising Staff Award given to an individual who provides advising or programmatic support for a career advising program for his work with fourth-year students during the residency application process.
Pritzker receives DEI honor from AΩA
The Pritzker School of Medicine has received the 2023 Alpha Omega Alpha (AΩA) Honor Medical Society Award for Excellence in Inclusion, Diversity and Equity in Medical Education and Patient Care. The honor recognizes medical schools whose values are transformed into successful programs for students and employees.
“The shared belief in serving our community on the South Side of Chicago is a tremendous point of pride for everyone at Pritzker, and this award is a testament to many years of hard work to create a welcoming and supportive culture for everyone,” said Vineet Arora, MD, AM’03, Dean for Medical Education.
AΩA’s review committee selected Pritzker as one of three recipients among a national pool of applicants. Pritzker will receive a cash prize to advance DEI initiatives.
Pritzker consistently ranks among the nation’s most diverse and selective medical schools. In 2023, Pritzker announced that more than half of incoming students would receive full-tuition scholarships. That same year, Pritzker recruited its most diverse class with respect to both economic diversity and students from backgrounds underrepresented in medicine.
1 in 3
Pritzker students from underrepresented backgrounds
6
Free clinics in Chicago run by Pritzker students
400+ College students reached by Pritzker’s summer programs
Since 2019, students from underrepresented backgrounds have made up an average of 34% of Pritzker’s incoming classes. In addition to formal coursework in health equity, advocacy and anti-racism, Pritzker students immerse themselves in service projects including running six free clinics that provide care for hundreds of patients across Chicago.
Pritzker is also committed to training future physicians via two summer programs for undergraduates. Since their creation in 2007, the Pritzker Pathway programs have reached more than 400 participants, with 17 matriculating to Pritzker for medical school.
35 MEDICINE ON THE MIDWAY SPRING 2024 uchicagomedicine.org/midway
Gold Humanism Honor Society
Fourteen fourth-year students of the University of Chicago Pritzker School of Medicine Class of 2024 were inducted into the Gold Humanism Honor Society in February. Nominated by their peers, these students exemplify compassionate patient care and serve as role models, mentors and leaders.
Emily Feuka was the student recipient of the Leonard Tow Humanism in Medicine Award. Sonia Oyola, MD, was the faculty recipient.

Alpha Omega Alpha Honor Medical Society

Twenty members of the University of Chicago Pritzker School of Medicine Class of 2024 were inducted into the Alpha Omega Alpha (AΩA) Honor Medical Society. The AΩA constitution calls for students to be recognized not only for academic achievement, but also achievement in research and scholarship, leadership, ethical behavior, professionalism and service to the school and community at large.
Each AΩA class elects alumni, faculty and housestaff to the Illinois Beta Chapter (the University of Chicago) in recognition of their leadership and accomplishments. Alumni are eligible 10 years after graduation. Faculty are elected based on demonstrated commitment to scholarly excellence and medical education. Housestaff are elected for their continued achievement, promise and mentorship qualities.
The 2024 honorees are:
Alumni: Scott Mendelson, MD’11, PhD’10; Access TeleCare; and Renée Rodriguez Paro, MD’10, Palo Alto Medical Foundation.
Faculty: R. Parker Ward, MD, Department of Medicine; and Doriane C. Miller, MD’83, Department of Medicine.
Housestaff: Ezinne (Zee) Akpara, MD, Department of Medicine; Yaeji Park, MD, MPH, Department of Surgery; Tony Gonçalves Da Lomba, MD’22, Department of Orthopaedic Surgery and Rehabilitation Medicine.
Ayush N. Shah, DO, internist at Endeavor Health NorthShore University HealthSystem, received the Volunteer Clinical Faculty Award, which recognizes a community physician who contributes with distinction to the education and training of clinical students.
Alpha Omega Alpha Honor Medical Society inductees with faculty, from left, front row: Nikhil Umesh, Maria Paz, Ashley Diaz, Santiago Avila, Sharbel Romanos, AB’19. Middle row: Willa Li, Dean for Medical Education Vineet Arora, MD, AM’03, Saara-Anne Azizi, PhD’21, Katie Long, PhD’21. Back
Thomas Cyberski, Meytal Chernoff, PhD’21, Melinique Walls Castellanos, Mohan Chennakesavalu, AΩA Chapter Councilor Poj Lysouvakon, AB’92, MD, Jason Xiao, AB’19, P. Cody He, PhD’21, Samantha Morris, Grace Hansen, PhD’21, Rohan Shah, SB’18, SM’22, PhD’22, Siddhi Ramesh, Sukarn Chokkara. Not pictured: Kristen Chalmers

Campaigning for Latino health
To push for closing the health equity gap that exists for Latinos, Sonia Oyola, MD, Assistant Professor of Family Medicine, joined doctors from across the country in Washington, DC. Their top concerns: limited available mental health treatment, disproportionate effects of climate change and pollution, and healthcare workforce diversity. The group met with Sen. Elizabeth Warren, among other leaders, during their visit.
Dean’s Letter 36 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION Pritzker News
Gold Humanism Honor Society inductees, from left, front row: Madison Weigand, Gabriela Betancourt, Meera Sakthivel, Rachel Son, Emily Feuka, Saara-Anne Azizi, PhD’21, Isra Hasnain, Cassandra Daisy. Back row: Murtala Affini, Melinique Walls Castellanos, Samantha Morris, Alex Rains, Daniel Dolan. Not pictured: Nikhil Umesh
row:
PHOTO BY PRITZKER SCHOOL OF MEDICINE
PHOTO BY EDDIE QUINONES

We want to hear from you!
LETTERS
Is there a story in this issue that inspires you to comment? Do you have a memory or reflection to share? Medicine on the Midway is open for feedback. Letters must be signed and may be edited for AP style, space, clarity and civility. To provide a range of views and voices, we encourage letter writers to limit themselves to 300 words or fewer.
Please send letters via email: momeditor@bsd.uchicago.edu.
Discovery of old notebook — twice — inspires meeting, memories
In November 2023, my medical student colleague Vincent Tornabene, MD’70, and I had the extraordinary opportunity to enjoy lunch with our University of Chicago neuroanatomy professor, Robert Yates Moore, MD’57, PhD’62, and his wife, Jane De Young.
Dr. Moore is internationally known for his research, particularly for the discovery of the suprachiasmatic nucleus, the “master circadian clock” (according to Wikipedia). We remember Dr. Moore as a wonderful teacher and mentor. Our recent meeting came as a result of Dr. Tornabene going through old boxes and coming across a student neuroanatomy notebook of Dr. Moore’s circa 1954.
When we were medical students, Dr. Tornabene had found it in the trash in the Anatomy Building and kept it. He recently did some research of his own and was able to contact Dr. Moore and his wife, Jane, who expressed the wish to give the notebook to their
granddaughter, who had written a science report about her grandfather. Hence our meeting and notebook handoff! Wonderful seeing Dr. Moore again after all these years.




Pritzker Alumni Weekend | May 17-18, 2024
All Pritzker School of Medicine alumni are invited to attend Pritzker Alumni Weekend an occasion to reconnect, reminisce and celebrate the achievements of the Pritzker community. Come together on campus for a weekend filled with camaraderie, engaging programs and alumni celebrations. Pritzker Reunion Class Dinners will take place on Friday evening for the following classes: 1964, 1974, 1979, 1984, 1989, 1994, 1999, 2004, 2009 and 2014.
Learn more at mbsaa.uchicago.edu/alumniweekend
uchicagomedicine.org/midway 37 MEDICINE ON THE MIDWAY SPRING 2024 Your News FALL 2023 Flipping the switch on cancer Studying epigenetics, UChicago scientists search
LETTERS
Anthony Philipps, AB’66, MD’70
Jane De Young and Robert Yates Moore, MD’57, PhD’62, reconnect with Vincent Tornabene, MD’70, and Anthony Philipps, AB’66, MD’70.
1960s
Barry D. Kahan SB’60, PhD’64, MD’65, has now retired. He was the founder and director of the Organ Transplant Center at the University of Texas at Houston and at the interinstitutional Program in Immunology in the Texas Medical Center in 1977. After gaining emeritus status in 2009, Kahan served as editor-in-chief of the print journal Transplantation Proceedings and online venue Transplantation Reports. He was one of the first physicians to administer Rapamune and served as a primary investigator in the Phase 1, 2 and multicenter Phase 3 U.S. trials, as well as subsequent treatment of hundreds of patients with the drug over the next decade. In retirement, he has begun to write “Rapamune: The Miracle Drug.”
IN MEMORIAM YOUR NEWS
1970s
Mark Friedman, AB’73, MD’77, is the co-founder and chief clinical officer at First Stop Health, a medical concierge service. First Stop Health offers 24/7 access to assistance and information for their members’ healthcare needs.
2010s
Bryan Smith, MD’10, has been appointed a 2023-24 White House Fellow. Founded in 1964, the White House Fellows program offers exceptional young leaders firsthand experience working at the highest levels of the federal government. Fellows spend a year working with senior White House staff, cabinet secretaries and other top-ranking officials, equipping them to serve as better leaders in their communities.
Share news about your life and accomplishments: mbsaa.uchicago.edu/update-contact-info

Bryan Smith, MD’10, at the White House, where he will work for one year as part of a fellowship program.

Sumner Kraft, MD’55, F. Thomas Wilson, MD’55, John Benfield, MD’55, and Bill McColl, MD’55.
1950s
William F. McColl, MD’55, died on December 28, 2023. During his senior year at Stanford, McColl finished fourth in the 1951 Heisman Trophy voting. Transitioning to the NFL, he played for the Chicago Bears from 1952 to 1959, while completing medical training. In 1973, he was elected to the College Football Hall of Fame. Once retired from football, McColl became a distinguished orthopedic surgeon, practicing in Korea’s leprosy hospital. He later ran three times as a Republican candidate for the U.S. House of Representatives.
1960s
Joseph F. Just, MD’64, died on October 4, 2023. Just practiced medicine in the Chicago area until his retirement in 1994, when he moved with his family to Minnesota. During this time, he wrote several editorials printed in the Chicago Sun-Times. In his retirement years, Just hosted a weekly radio show in Ely, Minnesota, “Just About Everything,” and in his later years, he wrote a monthly informal editorial, “Thoughts,” which he shared via email with his friends and family. He is survived by his wife, Cynthia Larson, and their children, Elisabeth Anne, Thomas Keith and Joseph Leslie.
2023-2024 ALUMNI COUNCIL
EXECUTIVE COMMITTEE
Karyl Kopaskie, AB’07, PhD’14
President
Doriane Miller, MD’83
Immediate Past President
Sapana Vora, PhD’14
Vice President and Chicago Partners Program Chair
Mark Aschliman, MD’80
Alumni Awards Committee Chair
Jeanne Farnan, AB’98, MD’02, MHPE Editorial Committee Chair
Michael Prystowsky, MD’81, PhD Regional Programs Chair
ALUMNI COUNCIL
Lampis Anagnostopoulos, SB’57, MD’61 ✱
Margaret “Peggy” Barron, MD’78
Jennifer “Piper” Below, PhD’11
Anita Blanchard, MD’90
Jillian Bowman, AB’20 ✤
Kenneth Bridbord, MD’69, MPH
Ava Ferguson Bryan, AM’10, MD’18 ✤
Courtney Burrows, PhD’15, MBA’17
Arnold Calica, SM’61, MD’75 ✱
Ithaar Derweesh, MD’95
Gabrielle Edgerton, PhD’10
Arash Emami, MD’94
Gail Farfel, PhD’93
Jonathan Fox, AB’79, PhD’85, MD’87
Katherine Given, AB’08, PhD’13, MBA’16, MD’16
Jeffrey Goodenbour, PhD’09
Stanton Greenstone ✤
Andrew Hack, AB’95, PhD’00, MD’02
Rajiv Jauhar, MD’91
Clifford Ko, AB’87, SM’89, MD’91
Lucy Lester, MD’72
Peter McCauley, MD’86
Jennifer McPartland, PhD’08
Vincent Nelson, MD’98, MBA, MPH
Carol Olson, PhD’82, MD’86
Loren Schechter, MD’94
Coleman Seskind, AB’55, SB’56, MD’59, SM’59 ✱
Adhir Shroff, MD’96
Puneet Singh, MD’11
Abby Stayart, AB’97, PHD’12
Margaret Steiner ✤
Anne Taylor, MD’76
Cynthia Thaik, MD’90
Vishruth “Vish” Venkataraman ✤
Sydney Yoon, MD’86
Russ Zajtchuk, SB’60, MD’63
38 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION Your News
✱ LIFE MEMBER ✤ STUDENT OR RESIDENT REPRESENTATIVE
✱
In Memoriam
Faculty
David Frim, MD, PhD
David Frim, MD, PhD, an internationally known pediatric neurosurgeon and researcher, died August 22. He was 63.
Frim, the former Chief of Neurosurgery at the University of Chicago Medicine, treated a wide range of illnesses, but his niche was congenital disorders that can be difficult to manage. Pediatric patients from around the world came to see Frim, and he cared for many into their adult years.
“He would spend so much time with each patient and each family, and they adored him,” said Jeffrey B. Matthews, MD, Chair of the Department of Surgery and Frim’s classmate at Harvard University and Harvard Medical School.

Frim arrived at UChicago Medicine in 1996, where he built a robust pediatric neurosurgery program, said Bakhtiar Yamini, MD, Interim Chair of the Department of Neurological Surgery and Director of Neurosurgical Oncology. (Frim headed what was then known as the Section of Neurosurgery from 2007 to 2020.)
“He took pride in being able to solve the most complicated fluid dynamic problems in patients,” Yamini said.
Frim was named Ralph Cannon Professor of Surgery in 2008. He was a fellow in the American Academy of Pediatrics and the American College of Surgeons, a member of numerous medical
Emeritus faculty
Ursula Storb, MD
Ursula Storb, MD, immunologist and Professor Emerita of Molecular Genetics and Cell Biology at the University of Chicago, died on December 15. She was 87.
Over nearly three decades at UChicago, Storb was a member of the Committees on Immunology; Cancer Biology; and Genetics, Genomics and Systems Biology; as well as Development, Regeneration and Stem Cell Biology. She taught graduate and undergraduate courses until she retired from the active faculty in 2015.
Storb was regarded for her work on somatic hypermutation (SHM) of the immunoglobulin light chain encoding genes. She helped create the first mice with transgenic expression of an immunoglobulin gene, and her lab identified multiple key transcriptional regulators that impact SHM which has broad and critical functions in immune cell regulation.
societies and associations, past president of the Chicago Neurological Society, and former editor-in-chief of the journal Pediatric Neurosurgery
An author on more than 150 scientific papers, Frim mentored Pritzker School of Medicine and graduate medical education students.
Many remember Frim for his kind demeanor and tireless advocacy. Margaret Hackett’s parents found Frim after other doctors told them they could do nothing more for their daughter’s hydrocephalus and craniometaphyseal dysplasia. That began a relationship that continued for many surgeries and many years, with Margaret now in her thirties. Her family gave $2.5 million to establish the Margaret Hackett Family Center Program in CNS Congenital Anomalies in 2019 at UChicago Medicine to support research and resources for patients and families. Frim served as program director. Frim also teamed with Janet Hutcheson, another patient’s mother, to found Discovery Camp, giving UChicago Medicine neurosurgery patients and their families a special camp experience for those advised to avoid recreational activities. Frim is survived by his wife of 34 years, Tammy Claman, and sons Daniel, Adam and Michael.
“ He would spend so much time with each patient and each family, and they adored him.”
Jeffrey B. Matthews, MD
Chair,
Department of Surgery

Colleagues remember Storb as a storyteller and an advocate.
She became one of the first members of the Association of Women in Science in 1971. And, in 1993, she founded a faculty committee to support graduate students from underrepresented minorities in science.
“She was a major figure in the field, but she took the time to ask me questions about my research and offered suggestions and encouragement,” said Barbara Kee, PhD, Professor of Pathology and Chair of the Committee on Cancer Biology at UChicago. “One of the benefits of choosing UChicago for a faculty position was knowing that Ursula would be a rigorous but supportive colleague.”
Storb was named a fellow of the American Academy of Arts and Sciences in 1992 and a fellow of the American Association for the Advancement of Sciences in 2007. Her longtime partner and fellow professor emeritus of molecular genetics and cell biology, Terry Martin, PhD, died in April 2023.
“ She was a major figure in the field. One of the benefits of choosing UChicago for a faculty position was knowing that Ursula would be a rigorous but supportive colleague.”
Barbara Kee, PhD Professor of Pathology Chair, Committee on Cancer Biology
uchicagomedicine.org/midway 39 MEDICINE ON THE MIDWAY SPRING 2024
Faculty
Albert Bendelac, MD, PhD

AService Professor of Pathology at the University of Chicago, died at his home on August 23, surrounded by family. He had just celebrated his 67th birthday.
Known for his passion for immunology, his mentorship of students and young faculty, and his broad scientific thinking, Bendelac joined the faculty in 2002 as an established investigator.
His research had already demonstrated that CD4 and CD8 T cells were required for the development of Type 1 diabetes, and it described a novel subset of T cells that expressed natural killer cell (NKT) antigens, discovering CD1d as their restricting element.
Bendelac’s seminal discovery came in 1995, when he first described NKT cells in the journal Science. Another, in 2005, found that lysosomal glycosphingolipid ceramide is the natural ligand for NKT cells.
“There is little doubt that he remained the leader in the field of NKT cell biology,” said Vinay Kumar, MBBS, MD, Lowell T. Coggeshall Distinguished Service Professor of Pathology and Chair Emeritus.
More largely, Bendelac explored the fundamental question of thymic selection of innate lymphocytes. He published more than 100 papers, several of which are cited more than 1,000 times. He also made immeasurable contributions toward establishing UChicago’s Committee on Immunology (COI) as a cutting-edge home for multidisciplinary research and a premier training program for young scientists.
Coworkers and students praised Bendelac’s advanced immunology course regarded by many trainees as the most demanding and rewarding course of their graduate tenure as well as his popular undergraduate immunobiology course for setting high standards.
“He was incredibly invested in and supportive of the next generation of immunologists, from undergraduate teaching, to conceiving of the graduate teaching curriculum
and helping them thrive,” said Daria Esterhazy, PhD, Assistant Professor of Pathology, whom Bendelac recruited to UChicago in 2018.
The former chair of the COI, Bendelac received multiple accolades, including a Llewellyn John and Harriet Manchester Quantrell Award for excellence in undergraduate teaching in 2019.
“You want to excite students and inspire them,” Bendelac said at the time. “My mission is to cover all the key aspects of the field but not go into excruciating detail, like knowing the music but not necessarily all the words.”
It was an award that his wife, Bana Jabri, MD, PhD, Sara and Harold Lincoln Thompson Distinguished Service Professor of Medicine, Pediatrics and Pathology, and current Chair of the Committee on Immunology, won in 2017. Colleagues described the spouses as a formidable team.
“Albert had a vision of scientific excellence that was deeply infectious he challenged and inspired others to dig deeper both conceptually and technically,” said Peter Savage, PhD, Associate Professor of Pathology. “He had high expectations of his colleagues and trainees and led by example. I never saw him flinch or hesitate to tackle a problem, or to put in the hard work necessary to do so. Ultimately, this made an indelible impression that was inspiring to many of us.”
Bendelac earned his MD from University of Paris VI in 1985 and his PhD in immunology from University of Paris VII in 1992. He previously worked at Princeton University as an associate professor and an assistant professor of molecular biology, and he also served as a visiting fellow and visiting scientist at the National Institutes of Health.
Outside of work, he enjoyed morning runs with his border collies along Lake Michigan, European cinema, literature, good food and wine, and cooking. In addition to his wife, Bendelac is survived by their children, Aude, Raphaëlle and Julien.
Albert had a vision of scientific excellence that was deeply infectious he challenged and inspired others to dig deeper both conceptually and technically. I never saw him flinch or hesitate to tackle a problem, or to put in the hard work necessary to do so.”
Peter Savage, PhD Associate Professor of Pathology
He was incredibly invested in and supportive of the next generation of immunologists, from undergraduate teaching, to conceiving of the graduate teaching curriculum in immunology, to recruiting multiple junior faculty members and helping them thrive.”
Daria Esterhazy, PhD Assistant Professor of Pathology
40 THE UNIVERSITY OF CHICAGO MEDICINE AND BIOLOGICAL SCIENCES DIVISION In Memoriam
PHOTO BY JEAN LACHAT

in
inyurl.com/MBSAA-Contact-Update
Hey, alumni!
Let’s stay
touch. Update your contact information to stay informed about the latest news and events for Biological Sciences Division and Pritzker School of Medicine alumni. t
alumni@bsd.uchicago.edu (888)303-0030 @UChicagoMBSAAmbsaa.uchicago.edu
This image, captured by research technician Kaylie Scorza, SB’23, began as gut bacteria growing in broth. As the culture dried, the bacteria metabolites formed structures that react with polarized light to create vivid, kaleidoscopic patterns when viewed under a microscope. Scorza submitted the image to the University of Chicago’s annual Science as Art contest.

Nonprofit Organization U.S. Postage Chicago, IL Permit No. 5179 PAID Suite 2500 130 East Randolph Street Chicago, IL 60601 LAST LOOK
Inner beauty
The University of Chicago does not discriminate on the basis of race, color, religion, sex, sexual orientation, gender identity, national or ethnic origin, age, status as an individual with a disability, protected veteran status, genetic information, or other protected classes under the law. For additional information, please see uchicago.edu/about/non_discrimination_statement FPO
“HIDDEN CITY” BY KAYLIE SCORZA, SB’23






















 BY DEVON MCPHEE
BY DEVON MCPHEE

 BY DEVON MCPHEE
BY DEVON MCPHEE