THE UNIVERSITY OF CHICAGO
BIOLOGICAL SCIENCES DIVISION

THE UNIVERSITY OF CHICAGO
BIOLOGICAL SCIENCES DIVISION
University of Chicago researchers and alumni are finding new ways to harness the body’s cancer-fighting strength via immunotherapy and develop treatments that work for every patient.
To extend lifesaving advances to more people, we must deepen our commitment to research — even as new challenges arrive that threaten the pursuit of knowledge and healthcare innovation.

Mark E. Anderson, MD, PhD
Paul
and Allene Russell Professor Dean of the Biological Sciences Division and the Pritzker School of Medicine
Executive
Vice President for Medical Affairs
The University of Chicago
Dear Colleagues,
If you’ve been on our Hyde Park campus this year, you’ve likely noticed the transformation underway just north of East 57th Street, where our new cancer pavilion is taking shape.
In February, we marked another milestone in the construction of Illinois’ first freestanding center dedicated solely to cancer care and research. Together with members of our community, we celebrated the placement of the final beam a 31-foot-long piece of steel adorned with more than 3,400 signatures and messages from those who have been touched by cancer.
The beam now stands as a symbol of hope and an enduring reminder of our ultimate goal: helping people and saving lives.
This issue of Medicine on the Midway emphasizes the remarkable work happening across the Biological Sciences Division, the Pritzker School of Medicine and the UChicago Medicine health system. Our cover story explores groundbreaking advances in cancer-fighting immunotherapy, which harnesses the body’s defenses to combat the disease and improve outcomes. The U.S. Food and Drug Administration approved the first checkpoint inhibitor immunotherapy for cancer in 2011. Six years later, UChicago Medicine became the first site in Illinois to offer the revolutionary CAR T-cell therapy, which uses a patient’s own genetically re-engineered T cells to find and destroy cancer cells.
Yet, immunotherapy is effective for only about one-fifth of cancer patients, and the reasons remain unclear. To extend lifesaving advances to more people, we must deepen our commitment to research even as new challenges arrive that threaten the pursuit of knowledge and healthcare innovation.
That commitment is what inspired us to build the cancer pavilion. Set to open as the AbbVie Foundation Cancer Pavilion in 2027, this 575,000-squarefoot facility will bring together scientists, clinicians and staff who currently work under separate roofs. By creating an environment that fosters stronger collaboration, we can spark the discoveries that will define the next era of cancer care.
This issue shares other stories about the myriad ways the University of Chicago community continues to elevate the human experience. Our alumni are applying what they learned here across fields that range from shaping public policy to caring for Olympic athletes. At the Pritzker School, students are volunteering at free clinics across Chicago’s South Side, bringing our high-quality care to patients and families in need. In our labs, researchers have created bionic hands and other transformative technologies that restore possibilities for so many people.
Even as we mark our successes, we remain vigilant in addressing the challenges ahead, including the potential impact of executive orders and federal actions on our research, higher education and healthcare. While we work with a range of partners to mitigate these effects, we also take strength from the broader UChicago community and our shared commitment to the enduring value and power of science and medicine to help people and save lives.
Thank you for reading and for your steadfast support of our missions in research, education and clinical care.
Spring 2025 Volume 78, No. 1
A publication of the University of Chicago Medicine and Biological Sciences Division. Medicine on the Midway is published for friends, alumni and faculty of the University of Chicago Medicine, Biological Sciences Division and the Pritzker School of Medicine.
Email us at momeditor@bsd.uchicago.edu
Write us at Medicine on the Midway Suite 2500
130 E. Randolph St. Chicago, IL 60601
The University of Chicago Pritzker School of Medicine and Biological Sciences Division
Executive Leadership
Mark E. Anderson, MD, PhD, Paul and Allene Russell Professor, Dean of the Biological Sciences Division and the Pritzker School of Medicine, and Executive Vice President for Medical Affairs for the University of Chicago
T. Conrad Gilliam, PhD, Marjorie I. and Bernard A. Mitchell Distinguished Service Professor, Dean for Basic Science, Biological Sciences Division
Thomas E. Jackiewicz, President of the University of Chicago Health System
Vineet Arora, MD, AM’03, Herbert T. Abelson Professor, Dean for Medical Education, Pritzker School of Medicine
Editorial Committee
Chair Jennifer “Piper” Below, PhD’11
Gabrielle Edgerton, PhD’10
Dana Lindsay, MD’92
Carol Olson, PhD’82, MD’86
Loren Schechter, MD’94
Coleman Seskind, AB’55, SB’56, MD’59, SM’59 (Lifetime Member)
Carol Westbrook, AB’72, PhD’77, MD’78
Student Representative
Tony Liu (Pritzker)
University of Chicago Medicine
Communications Kevin Joy, Editor
Editorial Contributors
Emily Ayshford
Jamie Bartosch
Kat Carlton
Johannes Jaeger, PhD
Jane Kollmer
Louise Lerner
Manu
Devon McPhee
Grace Niewijk
Tamara O’Shaughnessy
Novid Parsi
Angela Wells O’Connor
Matt Wood
Photo Contributors
Argonne National Laboratory
Mark Black
Olivia Bush
John Cheng
Michael Connor
Stephen Garrett
Alastair Grant
Chris Jones
Jennifer McMenamin
Henrik Montgomery
Jordan Porter-Woodruff
Eddie Quinones
Joe Sterbenc
Rodney Wright
Design
Wilkinson Design
Immunotherapy is revolutionizing cancer care, but the journey is still far from over. University of Chicago experts are finding new ways to harness the body’s ability to fight off the disease.
How John Jumper, SM’12, PhD’17, went from ‘accidental chemist’ to Nobel Prize winner.
From homeland security to health equity, the roles of graduates go beyond the lab and bedside.
Marcia Faustin, MD’13, FAAFP, provides medalworthy care for the athletes of USA Gymnastics.

Midway News
Federal grant supports AI tools to expedite cancer drug development. 3
BSD faculty members receive named professorships. 4
BSD News
The namesake lab of Sam Light, PhD, illuminates the gut-health connection. 29 New potential for prosthetic hands: producing tactile stimulation. 30

Pritzker News
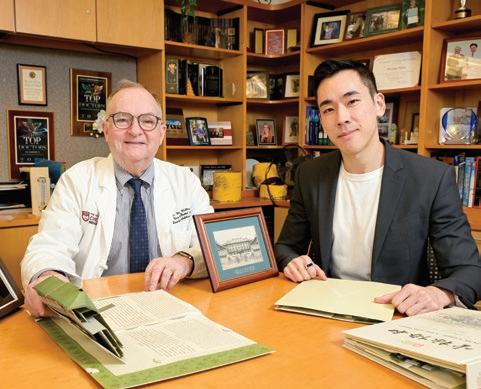
Exchanges sustain longtime link with Peking Union Medical College. 34
Match Day finds record number of grads headed to psychiatry residencies. 36

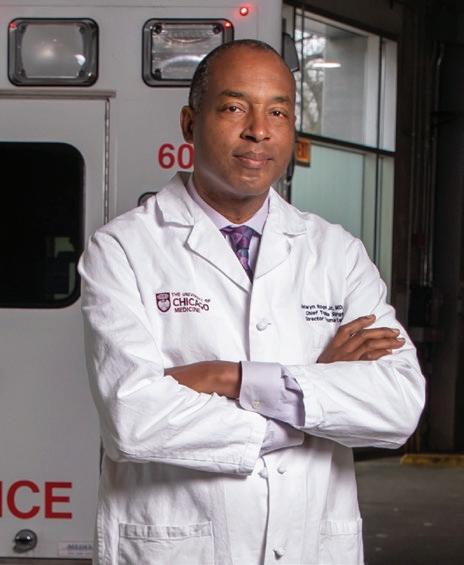
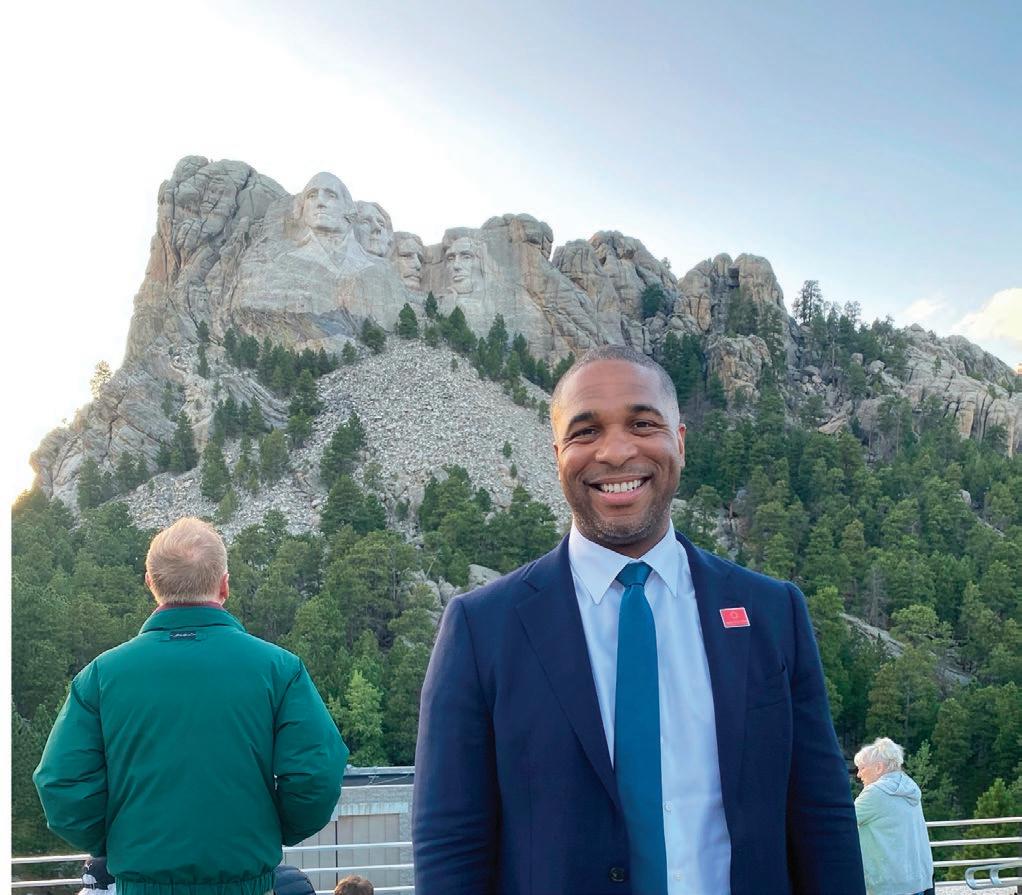
Selwyn O. Rogers Jr., MD, MPH, the Dr. James E. Bowman Jr. Professor of Surgery at the University of Chicago, was elected to the National Academy of Medicine’s 2024 class.
Rogers is one of 100 people elected to the academy last October. They are elected by current members via a process that recognizes individuals who have made significant contributions to medical sciences, healthcare and public health.
It is considered one of the highest honors in the health and medical field.
Rogers, a trauma surgeon, is also Executive Vice President for Community
Health Engagement at the University of Chicago Medicine, where he was a founding director of its adult Level 1 trauma center that opened in 2018. He was selected by the academy for his role in creating hospital-based violence interventions, including medical-legal clinics, to reduce the social drivers of gun-based trauma.
Rogers’ research focuses on understanding the healthcare needs of underserved populations, and he has published numerous articles relating to health disparities and the impact of race and ethnicity on surgical outcomes.
Catina Latham, AB’95, PhD, has returned to the University of Chicago Medicine as Senior Vice President for Community Health Transformation and Chief Equity Officer.
From 2017-2020, Latham served as Executive Director of Community Benefit Programs and Evaluation, leading the development and implementation of the community health evaluation strategy for UChicago Medicine’s Urban Health Initiative (UHI). The department administers population health and community benefit programs.
Latham also developed the evaluation framework for UChicago Medicine’s Violence Recovery Program that provides holistic support for patients and families affected by trauma from intentional violence. She started her new role in January.
What inspired your return to UChicago Medicine?
I was drawn to build on the legacy of the Urban Health Initiative and my predecessor Brenda Battle, who retired last year. The UHI encompasses the areas of interest to me and my career community focus, program design
and implementation, evaluation and quality improvements and it translates them to inform program and policy changes that advance health equity. I’m so grateful to be back.
How did you find this field?
It started when I was in college as an anthropology major. I worked on a project focused on understanding culture and health. We helped an organization design a maternal health program focused on promoting a healthy pregnancy and how to care for a baby while also respecting the rituals and healing practices of the various subcultures in the community. I have taken the lessons from that experience with me throughout my career.
What’s your approach to care?
If we are partnering to improve your health, I have to understand and respect your vantage point or point of view, and then we go from there to help you achieve your health goals. I have to also understand that your needs may be very different from what I think you need. And more importantly, for some, those needs may go beyond just healthcare.


BY JANE KOLLMER
Making a new cancer drug is a complex and resource-intensive process. It typically takes up to 15 years and more than $2 billion to go from the discovery phase to U.S. Food and Drug Administration approval.
A $6 million grant will help the University of Chicago Medicine Comprehensive Cancer Center leverage artificial intelligence and machine learning tools to expedite this critical journey.
By partnering with experts at Argonne National Laboratory a U.S. Department of Energy facility affiliated with the University of Chicago Cancer Center researchers will be able to mine vast datasets and uncover patterns that may inform treatments for drug-resistant cancers.
“Patients with cancer don’t have time to wait for new treatments, so there is a strong need to compress the drug discovery timeline,” said Kunle Odunsi, MD, PhD, who is director of the Cancer Center, as well as Dean for Oncology in the Biological Sciences Division and the AbbVie Foundation Distinguished Service Professor of Obstetrics and Gynecology.
“We aim to do that with novel synergistic approaches that take advantage of Argonne’s supercomputing capabilities and the strengths in

Be a part of Pritzker’s 100th anniversary exhibit
chemistry and cancer biology at the University of Chicago.”
The funding, which could grow to $15 million, is provided by the Advanced Research Projects Agency for Health, an agency within the U.S. Department of Health and Human Services established in 2022 to fast-track transformative biomedical research.
The need is great: Although more than 4,500 human proteins hold potential as targets for anti-cancer treatments, less than 10% of them are currently targeted by approved drugs. It’s estimated, for example, that only 14% to 28% of patients with gynecologic cancers could be matched to drugs based on their tumor’s molecular profile.
Argonne’s exceptional tools including an Aurora exascale supercomputer that can perform more than a quintillion calculations per second will screen billions of possible molecules in a matter of hours and simulate thousands of compounds within days.
Researchers plan to test this drug-discovery model on targets known to be relevant in ovarian cancer, one of the deadliest and toughest gynecologic cancers to treat. Although the pilot project will focus on ovarian cancer, it will eventually expand to include targets for any cancer type.
In celebration of the Pritzker School of Medicine’s 100th anniversary in 2027, curators are developing an exhibit at UChicago Library’s Special Collections Research Center. Do you have old photos from med school? Class notes or teaching materials? Visit tinyurl.com/Pritzker-Centennial-Exhibit to share your ideas and any memorabilia you might be willing to lend.
$75 million donation supports new cancer pavilion
The AbbVie Foundation, a nonprofit dedicated to addressing health inequities, has donated $75 million to the University of Chicago to support construction of UChicago Medicine’s new cancer pavilion.
The building, to be named the AbbVie Foundation Cancer Pavilion, will provide a hub for world-class research, pioneering clinical treatments and personalized care. The donation will help fund the $815 million, 575,000-square-foot facility, which is scheduled to open in 2027.


Thirty-one members of the University of Chicago faculty have received distinguished service or named professorships, including eight individuals affiliated with the Biological Sciences Division. The appointments were effective January 1. Here’s a look at some of their career highlights:




RISHI ARORA, MBBS
Harold H. Hines Jr. Professor, Department of Medicine and the College
■ Chief, Section of Cardiology in the Department of Medicine
■ Cardiologist and electrophysiologist treating a wide range of heart conditions
■ Namesake lab researches heart rhythm disorders, with a focus on atrial fibrillation
Stephen Family Professor, Department of Pediatrics ✾
■ Director of neonatology research
■ Co-Director, Basic Science Track within the Scholarship and Discovery Program, Pritzker School of Medicine
■ Faculty Co-Chair, Pritzker’s Summer Research Program
✾ Denotes a newly created named professorship
DAVID FREEDMAN, PHD
Stahl Professor of Neurobiology, Wallman Society of Fellows and the Department of Neurobiology and the College ✾
■ Chair, Department of Neurobiology
■ Uses computational modeling and machine learning to study how neural networks mediate cognitively demanding behaviors
■ Co-Lead, Eric and Wendy Schmidt AI+Science Postdoctoral Fellowship Program
Lowell T. Coggeshall Professor, Department of Psychiatry and Behavioral Neuroscience
■ Appointed department chair in July
■ Public health researcher focused on evidence-based interventions, including those for HIV and substance use disorders
■ Leading efforts to integrate behavioral healthcare across UChicago Medicine
HENING LIN, PHD
James and Karen Frank Family Professor, Departments of Medicine and Chemistry and the College
■ Pioneer in chemistry, biology and therapeutic targeting of enzymes
■ Investigator, Howard Hughes Medical Institute
■ Promotes interdisciplinary work among UChicago chemists, biologists and clinicians

JAMES REIDY, MD
Adelaide M. Seeberger Professor, Department of Ophthalmology and Visual Science ✾
■ Vice Chair of Clinical Operations and Medical Director, Ophthalmology Outpatient Center
■ Specializes in corneal diseases
■ Studying stem cells in ocular surface reconstruction and artificial cornea implantation for high-risk keratoplasty patients

PABLO SANCHEZ, MD, PHD
Lowell T. Coggeshall Professor, Department of Surgery
■ Surgical Director, Lung Transplant Program at UChicago Medicine
■ Affiliated with the Latino Transplant Program for Spanish-speaking patients
■ Leader of new techniques, including ex vivo lung perfusion evaluation and bloodless lung transplantation

The University of Chicago Medicine has earned bronze-level recognition from the American Medical Association (AMA) as a Joy in Medicine health organization.
Valid for two years, the 2024 distinction from the country’s leading physicians group recognizes health systems and hospitals that are successfully reducing burnout and enhancing the well-being and professional fulfillment of doctors.
“We’re committed to nurturing the joy that each of our physicians and faculty
members have in their work from the laboratory to the bedside while also helping them when the journey is rocky,” said Bree Andrews, MD, Chief Wellness and Vitality Officer for Physicians for the Biological Sciences Division and UChicago Medicine.
UChicago Medicine was cited by the AMA for its efforts to improve wellness, resilience and ease of clinical practice, pillars of the UC Well initiatives program. Among them: ambient AI tools to streamline workflows and internal improvement
RONG
GRACE ZHAI, PHD
Jack Miller Professor for the Study of Neurological Diseases, Department of Neurology
■ Vice Chair for Research, Department of Neurology
■ Widely known for work in Drosophila genetics and human disease modeling used to understand causes of neurological diseases
■ Fostering partnerships to create a disease modeling and drug discovery platform within the BSD
programs targeting common challenges.
Other projects include the launch of internal peer-development programs for physicians, the addition of well-being directors for clinical departments, wellness grants, and surveys to ensure physicians feel more valued, respected and heard.
After peaking during the COVID-19 pandemic, the physician burnout rate has dipped under 50% for the first time in four years, according to the AMA. The rate at UChicago Medicine is just below 40%, as measured this year and last.
BY DEVON MCPHEE


A nontraditional path has always appealed to Peter Edelstein, MD’87, whose career and curiosity have taken him around the world.
Even during medical school and residency, “I wasn’t sure that I wanted to be a doctor in the traditional sense,” Edelstein said. “But I recognized that if I decided to take an unusual course in life, the University of Chicago would teach me the best way to do it.”
Edelstein, who trained in general, trauma, and colorectal surgery, initially worked at academic medical centers and private healthcare systems. His first academic position was on the surgical team at Stanford University, his undergraduate alma mater, where he also served as associate surgical residency program director and associate director of the surgical ICU.
He then spent more than a decade in the corporate world, becoming general manager of MEDai Clinical Analytics, part of Elsevier, and chief medical officer at LexisNexis Risk Healthcare.
But when others might think about retirement, Edelstein pivoted yet again by joining the armed services.
“I knew I would regret it if I didn’t serve,” said Edelstein, whose father, Jack Edelstein, MD’57, served as a pediatrician in the U.S. Army. “I told my wife, Laura, that I wanted to be a civilian with the U.S. military, and that the best way for me to do that was to go back into the hospital. Luckily, she was very supportive.”
To do this, Edelstein needed to renew his board certification and complete 100 new surgical cases. He spent one month observing at the University of California, San Diego, where he had completed his residency and an internship decades earlier, and participated in medical mission trips in Bolivia and Haiti.
He became a civilian surgeon for the Army, practicing at Bayne-Jones Army Community Hospital at Fort Johnson (formerly Fort Polk) in Vernon Parish, Louisiana, for more than a year. Edelstein impressed base leadership so much that he received the Army Civilian Service Commendation Medal and was encouraged to join the Army Reserve, which had a need for qualified surgeons.

“I told them, ‘I’m kind of old, don’t you think?’” said Edelstein, who was in his late 50s at the time. “But they told me the military has age waivers for trauma surgeons who can pass all physical requirements, and that the base commander and the hospital commander were writing letters for me.”
In 2021, Edelstein became an Army Reserve surgeon, a role that has taken him around the world.
With the U.S. at peacetime, he joined a private contracting group that provides medical support for special forces.
“My first assignment was in Niger, where, within a very short time, there was a coup,” Edelstein said, adding that a subsequent stint found him in a country harboring large terrorist forces. “I can say it’s been interesting.”
Edelstein has two more assignments in Africa on deck as part of the Warfighter Recovery Network, which supports U.S. military activity there.
“Having the opportunity at this point in my career to support these amazing young U.S. military personnel has been a tremendous surprise and honor,” he said.
Now 63, Edelstein is considering retiring in about five years to spend time with his wife, a Harvardtrained pediatric radiologist, and to enjoy hiking and horseback riding. Never to stay in one place for long, the couple has considered joining the Peace Corps program for retirees.
University of Chicago researchers and alumni are finding new ways to harness the body’s cancer-fighting strength via immunotherapy and develop treatments that work for every patient.
PHOTOGRAPHY BY MARK
Lung tumors shrinking.
Melanomas melting away.
Metastatic kidney tumors disappearing for good.
When the Food and Drug Administration approved the first immunotherapy for cancer in 2011, it ushered in a new era for care. Patients had a reason for hope: The cancers that had previously evaded immune cells could be targeted and destroyed by their body’s own defense system, similar to how it might fight off a cold.
Since then, the number and types of immunotherapies have increased, putting many patients in remission, or even curing them. But physicians and scientists continue to face a stubborn reality: Immunotherapies work best for certain kinds of
cancers, and the treatments are effective for only about 20% of patients.
“The immunotherapy field had this meteoric rise, and then it stalled a bit as we tried to figure out why it didn’t work for everyone,” said Thomas Gajewski, AB’84, PhD’89, MD’91, the AbbVie Foundation Professor of Cancer Immunotherapy in the Departments of Pathology and Medicine at the University of Chicago. “But it is starting to tick up again as resistance mechanisms are being uncovered.
“We are going to get to a point where immunotherapy works in a majority of patients.”
It’s the kind of challenge that motivates Gajewski and UChicago researchers one that involves painstaking analysis of biological systems, stateof-the-art technologies and collaboration across disciplines. As they work at the forefront of creating new immunotherapies, expert teams also hope to gain a clearer understanding of why current approaches do not cure everyone.
From ‘religion’ to reality
Cancer can evade the immune system in several ways. Some types are naturally less visible, while others have proteins on their surface that turn off immune cells. Other cancers interfere with the environment around a tumor, hindering the immune system’s ability to attack it.

Thomas Gajewski, AB’84, PhD’89, MD’91, the AbbVie Foundation Professor of Cancer Immunotherapy, has studied the groundbreaking approach since the early 1990s. “It’s come full circle,” he says.
Studies as far back as the 1890s have explored the potential of harnessing the immune system to fight cancer. But for decades, as clear answers or options remained elusive, the standard of care focused on surgery, radiation and chemotherapy.
Gajewski, an immunologist and medical oncologist, has long theorized that the immune system is relevant to every area of medicine. Looking for the hardest problem to study, he turned to cancer in the early 1990s a time when “nobody was doing cancer immunotherapy” and “the field was more on a religion level.”
He studied with Belgian scientist Thierry Boon, a distinguished immunology researcher who had discovered the first tumor-associated antigen
that would enable the immune system’s T cells to recognize cancer cells.
That informed Gajewski’s early work in understanding immune checkpoint therapy involving the CTLA-4 protein’s role in serving as the “brakes” for a key biological process. When this protein, found on T cells, binds to another protein known as B7, it prevents the T cell from killing healthy cells. Unfortunately, it can also prevent these mighty T cells from attacking cancer.
But if this checkpoint protein was blocked, scientists found, the immune system could attack and potentially eliminate tumors. This discovery led to the FDA’s approval of the first checkpoint inhibitor immunotherapy in 2011.
Another checkpoint inhibitor therapy which blocks the PD-L1 proteins on tumors that turn down T-cell responses through the inhibitory receptor PD-1 followed a few years later. The discovery led to a Nobel Prize for two scientists in 2018.
Since then, millions have received these drugs, with triumphant stories abounding in melanoma and lung cancer cases, where the approach can be effective for 30% to 60% of patients.
“That has been the biggest success, and it is now approved for 20 different cancers,” said Gajewski, who also co-leads the Cancer and Immunology Program in the National Cancer Institute-designated University of Chicago Medicine Comprehensive Cancer Center. “It’s come full circle. At first, no one in the field believed us.
“Now, immunotherapy has become first-line therapy for many patients.”
‘Home run’ ambitions
Checkpoint inhibitors aren’t the only option. CAR T-cell therapy a process in which a patient’s T cells are extracted and supercharged with a gene called a chimeric antigen receptor (CAR) helps the immune system recognize and fight blood cancers like leukemia and lymphoma once the re-engineered T cells are put back into the body.
UChicago Medicine became the first site in Illinois to offer CAR T-cell therapy in 2017. In January, it was one of nine locations for a clinical trial studying the therapy’s effect on three autoimmune diseases: systemic lupus erythematosus, inflammatory myositis and systemic sclerosis.
CAR T-cell therapy, said Satyajit Kosuri, MD, a cellular therapy physician and Assistant Professor of Medicine, “is a broad platform that we can adapt and
apply to certain patient populations with diseases that have been resistant to historically standard therapies. It may offer a new solution where previously there was none.”
Last year, another kind of cellular therapy called tumor-infiltrating lymphocyte (TIL) therapy was approved by the FDA as a treatment for advanced melanoma. UChicago Medicine was among the first places in the nation to offer it.
The therapy involves growing and activating a patient’s own TIL cells, which are specialized T cells that have moved from the bloodstream into a tumor. The body’s own small population of these cells cannot destroy a tumor, but if the cells are removed from the patient, multiplied into the billions and re-injected the same strategy as CAR T-cell therapy it creates a superpowered immune system to clear out the cancer.
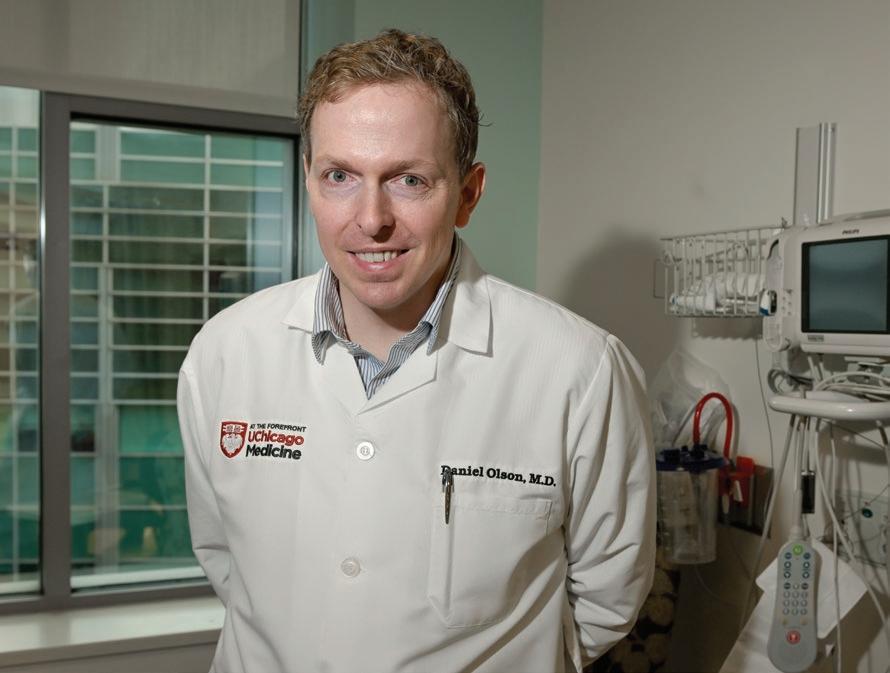
“Cell immunotherapies have given us a lot of excitement,” said Daniel Olson, MD, an oncologist and Assistant Professor of Medicine who led the TIL therapy rollout at UChicago Medicine. One of Olson’s patients, the first in the Midwest to receive the new therapy, was able to vacation in Europe after 15 years of battling skin cancer.
Although only one-third to one-half of all recipients will see a benefit, “TIL has been able to cure patients who haven’t had success with other treatments,” Olson said, noting that the therapy requires advanced coordination among oncologists, surgeons and the cell therapy team.
Daniel Olson, MD, Assistant Professor of Medicine, led the UChicago Medicine rollout of tumor-infiltrating lymphocyte (TIL) therapy for advanced melanoma.
THE KEY TO UNLOCKING the wider power of immunotherapy might lie in the ecosystem of microbes that live in our intestines.
The gut microbiome has been implicated in conditions as far-ranging as obesity and Alzheimer’s disease. In 2018, Thomas Gajewski, AB’84, PhD’89, MD’91, the AbbVie Foundation Professor of Cancer Immunotherapy in the Departments of Pathology and Medicine at the University of Chicago, wondered if a person’s microbiome
composition might influence whether they responded to immunotherapy.
For Gajewski and his collaborators, the answer was a resounding “yes”: Patients who responded to immunotherapy had much more abundant strains of good bacteria in their GI tract.
It was a result that could also be flipped. “If you took a mouse that responded to immunotherapy, you can make them not respond by putting in the wrong bacteria,” Gajewski said.
The general idea is that these bacteria help “warm up” cancers so that they can be found and destroyed by the immune system. Now, working with UChicago’s Duchossois Family Institute, scientists are finding the exact combinations of bacteria that work best, with the hopes of starting a clinical trial to offer cancer patients a probiotic treatment before immunotherapy.
“We think the microbiome could explain immunotherapy resistance in around half of patients,” Gajewski said.

Ralph Weichselbaum, MD, the Daniel K. Ludwig Distinguished Service Professor of Radiation and Cellular Oncology, has discovered ways checkpoint inhibitors can improve the effects of radiation therapy.
The potential has UChicago Medicine oncologists and scientists at the David and Etta Jonas Center for Cellular Therapy studying the wider use of TIL therapy for other tumor types, including cervical, lung and colon cancers.
“We’re aiming for a home run,” Olson said. “We’re looking for transformative therapies that can really alter a patient’s immune system to fight cancer on its own, and do it for the long term. That’s what motivates us day to day.”
As scientists continue to uncover and refine immunotherapies that work as a first-line offense, they’re also testing how to best combine them with widely used cancer treatments such as radiation which, despite its cancer-killing powers, can also suppress immune cells.
Ralph Weichselbaum, MD, the Daniel K. Ludwig Distinguished Service Professor of Radiation and Cellular Oncology at UChicago, has studied this phenomenon, as well as ways to combine therapies. In a study published in the Journal of Clinical Investigation, Weichselbaum and his team found that
DAN LEVENTHAL, SM’13, PHD’16,
was always interested in how biomedical research translated from the bench to the bedside. But as a graduate student in UChicago’s cancer biology program, he found himself studying fundamental research: how T-cell tolerance is regulated in cancer.
“It’s funny that I ended up in a more fundamental immunology research lab,” he said with a laugh. “But I moved toward trying to answer questions that needed to be addressed, ones that could have impact more broadly.”
The research paved the way for a career in biotech startups, where Leventhal has worked on engineering T cells and creating strains of immuno-modulating bacteria to fight cancer.
Today, his work involves not activating the immune system but hiding from it.
As head of immunogenicity at Xaira Therapeutics, a Bay Area biotechnology company, Leventhal is
developing protein-based therapeutics for several different diseases by using machine learning techniques to find a way to “hide” these therapeutics from the immune system so they aren’t recognized as foreign and attacked.
“It involves the same understanding of how tolerance is enforced for T cells in the context of cancer or homeostasis,” Leventhal said. “We want to design protein sequences that are less likely to be detected.”
Because the immunogenicity of biotherapeutics is a relatively new field of study, much fundamental research must be done. But thanks to his experience at UChicago, Leventhal is ready to put in the work.
“UChicago really gave me a leg up in the industry, because I was used to the high level of detail and discourse in research,” he said. “No one can surprise me with questions and critiques. My scientific training prepared me for that.”

BLACK WOMEN ARE more commonly diagnosed with triple-negative breast cancer (TNBC), but they’re less likely to receive immunotherapy, even after controlling for socioeconomic factors, a study in JAMA Network Open has found. An analysis of data from the National Cancer
Database revealed that women of other ethnic groups received immunotherapy for TNBC at rates comparable to one another. It also found there was no difference in pathologic complete response and overall survival between white and Black patients who received the treatment. “Our study
the checkpoint PD-L1 protein, which turns down T-cell responses, was actually induced by radiation.
Put another way, if that protein is blocked by a checkpoint inhibitor, “you can actually improve the effects of radiation therapy,” Weichselbaum said. In another paper, published in 2023 in Cancer Cell, Weichselbaum and Chuan He, PhD, the John T. Wilson Distinguished Service Professor of Chemistry in the Physical Sciences Division and Professor of Biochemistry and Microbiology in the Biological Sciences Division, found that a reader of RNA methylation called YTHDF2 induces immune suppression. Blocking YTHDF2, they found, improved the positive effects of radiotherapy.
Weichselbaum is on the hunt to find more immunotherapy options that could enhance the positive effects of radiation. A decade ago, Weichselbaum, Gajewski and others found that mice that lacked a specific protein pathway called STING (stimulator of interferon genes) could not mount an immune response to cancer in conjunction with immunotherapy or high-dose radiation. They recently published a paper in Immunity outlining the findings.
Since then, STING has become a target to make “cold” tumors “hot” in other words, to have more T cells and therefore be more responsive to immunotherapy and radiation. Weichselbaum is currently collaborating with Wenbin Lin, PhD, the James Franck Professor of Chemistry, to develop nanoparticles that can activate the STING pathway.
“These combinations of treatments are either in clinical trials or will soon be,” Weichselbaum said. “It’s been very gratifying. It’s a real chance to help people.”
While the first immunotherapies were given to patients with metastatic cancers who had already run through other treatment options,
gave us a preliminary look at some of the systems-level factors, like insurance status and treatment facility, that create disparities in access to these medications,” said Frederick Howard, MD, Assistant Professor of Medicine and the study’s co-author.
“More work definitely needs to be done.”
physicians are now testing the opposite: trying immunotherapy first.
This neoadjuvant method, UChicago scientists have found, has improved outcomes with limited side effects for some patients.
Consider, for example, patients with head and neck cancers caused by human papillomavirus (HPV). They have high survival rates but often face side effects from chemotherapy and radiation that affect the ability to speak and swallow.

In a recent clinical trial, Ari Rosenberg, MD, Assistant Professor of Medicine, started treatment on patients with head and neck cancer by administering a checkpoint inhibitor immunotherapy along with an initial dose of chemotherapy, a strategy called chemoimmunotherapy. Patients then received a reduced dose of chemotherapy and radiation.
“The results were very promising,” said Rosenberg, whose findings were published last year in JAMA Oncology. “Patients had lower feeding tube rates and
Ari Rosenberg, MD, Assistant Professor of Medicine, is studying how administering immunotherapy with chemotherapy can benefit patients with head and neck cancer.

Akash Patnaik, MD, PhD, MMSc, Associate Professor of Medicine, says the aim of his immunotherapy research is to “flip the switch on the bad guys and make them the good guys, the anti-tumor guys that can then attack and kill cancer.
A BOUT OF CHICKEN POX once kept Avery Posey, PhD’11, home from school, but it spurred an early interest in medicine and biological research that led to graduate studies in genetics at UChicago.
After earning his PhD, Posey studied CAR T-cell therapy, which takes T cells from a patient’s body and adds a gene called a chimeric antigen receptor (CAR) to help the cells recognize and fight blood cancers like leukemia and lymphoma. But the therapy can also cause toxicity in the body.
Now, as an assistant professor at the University of Pennsylvania Perelman School of Medicine, Posey is working to find alternative targets on tumors for CARs and to alter the signaling influences of T cells.
He is also exploring how the therapy could treat heart disease. By reengineering a type of T cell to reduce
smaller changes in their weights during treatment. They also had improved swallowing outcomes.”
Next, the team decided to try the regimen with head and neck cancers not caused by HPV. Although these cancers are often caused by tobacco or alcohol use, physicians also are seeing a growing number of cases in nonsmokers. They recently published a study, also in JAMA Oncology, that showed excellent outcomes with fewer side effects for responding patients who received less radiation.
“Many of us are excited to be leveraging combi nations of immunotherapy with other drugs and treatments to help improve outcomes for patients,” Rosenberg said.
Ultimately, there is no single reason why immuno therapy might fail. Each patient is unique, and scientists must identify different strategies that consider their biological makeup.
Gajewski and many others have focused on the tumor microenvironment, the area around the tumor. Using advanced technologies like single-cell RNA sequencing and spatial transcriptomics which shows how cells interact with each other to form a community they have begun to understand the basic mechanisms behind immunotherapy successes.

inflammation and provide local immune suppression, the technique could help reduce atherosclerotic plaque and treat inflammation caused by autoimmune diseases.
Beyond that, he’s studying how CAR T-cell therapy may benefit a unique set of patients. Working with Penn’s veterinary school, Posey is developing new receptors to target cancers in dogs.
“Dogs with cancer are like humans they have a lot of the same cancer biology, and there is a lot of variability between patients,” Posey said. “Our ultimate goal is to better treat cancer and disease, and this sort of comparative medicine research can give us better confidence that the drugs will also work in humans, hopefully with better success rates.”


BENJAMIN BOYERINAS, PHD’09, didn’t envision a career in immunotherapy. As a graduate student at UChicago, he studied how microRNAS contributed to aggressive cancers.
But when his wife accepted a job in Washington, D.C., Boyerinas found a postdoctoral fellowship focused on therapeutic vaccines for cancer at the National Cancer Institute. While attending an immunotherapy conference, he saw a lecture on CAR T-cell treatments for melanoma patients.
“The external melanomas would just melt away,” he said. “That had a profound effect on me.”
Now, as the head of immuno-oncology at startup AvenCell in Massachusetts, Boyerinas is working to make CAR T-cell therapy an off-the-shelf product to help even more patients. While the traditional therapy uses a patient’s own T cells and engineers them to recognize and fight cancers, AvenCell takes donor T cells and engineers them so they can be injected into any patient.

among patients, and those who had high expression had a better clinical response to checkpoint inhibitor immunotherapy.
Akash Patnaik, MD, PhD, MMSc, Deputy Section Chief for Translational Research in Hematology/ Oncology and program leader for the Clinical and Experimental Therapeutics Program at the Cancer Center, recently found that in patients with prostate cancer who don’t respond to immunotherapy, the immune system actually promotes the growth of cancer by recruiting tumor-associated macrophages that express PD-1 into the tumor microenvironment. The findings were published in Clinical Cancer Research.
Macrophages a type of white blood cell are one key to improving immunotherapy. These cells can treat the cancer like an injury, preventing the immune system from attacking it while the body
Previously, patients needed to be immunosuppressed to take such cells, as their body would recognize them as foreign and try to fight them off. But AvenCell’s workaround means that patients would not need to be immunosuppressed. Their product is now in clinical trials.
“You have to engineer it so it won’t be rejected by the host immune system, and our goal is to be the first to demonstrate a product that has this capability,” he said. “It would allow for much more rapid treatment of patients and give people hope.”
The persistence that Boyerinas learned as a PhD student at UChicago still guides his work.
“When you do research, you always assume the worst and prepare for the best,” he said. “That allows you to never get comfortable or complacent and to focus on the right questions, and to persist in the face of adversity. And when you finally make it, it teaches you that you can accomplish anything you set your mind to.”
of Medicine.
In 2017, Patnaik and a team showed that the drug cabozantinib reprogrammed immune cells called neutrophils the first line of defense against bacterial infections. They’re now testing it in clinical trials with immunotherapies to see whether the combination improves outcomes in patients with prostate cancer.
For Patnaik, who lost an uncle to advanced prostate cancer, the quest to “crack the code” of immunotherapies is personal.
“We’re making progress each day,” he said. “It’s an exciting time, and there’s certainly a lot of promise with these approaches. As a physician-scientist, that’s the most rewarding aspect to be able to do basic research that leads to clinical trials for patients and then take what we learn from those clinical trials back to the lab.”
BY LOUISE LERNER AND KEVIN JOY
When John Jumper, SM’12, PhD’17, arrived at the University of Chicago to begin his doctoral studies in chemistry, there was one slight hitch.
“I knew no chemistry none,” said Jumper, who recalled hustling to stay one week ahead of the curriculum as a teaching assistant for an undergraduate general chemistry course. “I had to ‘speed-run’ the whole thing.”
A bigger adrenaline rush followed. In October, Jumper was awarded the 2024 Nobel Prize in chemistry.

He and Google DeepMind colleague Demis Hassabis, PhD, were recognized for creating AlphaFold a program that uses artificial intelligence to successfully predict the structure of almost all known proteins. The technology could give research teams new insights into disease and accelerate the search for new treatments.
“It can be viewed as the first real scientific breakthrough of artificial intelligence,” wrote Johan Åqvist, a member of the Nobel Committee for Chemistry.
The 40-year-old Jumper is the youngest chemistry laureate in more than 70 years.
The accolade, presented in December in Stockholm, “is a testament to the pioneering research conducted at UChicago that leads to real-world impact and the success of our mission to train future leaders in the field,” said Jiwoong Park, PhD, Chair of the Department of Chemistry.
Answering a knotty question
Much like the proteins he studies, Jumper’s academic path took its own distinct shape.
After finding little joy in pursuing a PhD in physics his first scientific love Jumper left to take a job at a company writing computational programs to model the movements of proteins in the hopes of understanding diseases such as lung cancer.
“It was so easy to see the connections; if we do this right, someone goes home from the hospital,” he said.
That fascination pushed Jumper toward a doctorate in chemistry at UChicago, where he worked with Karl Freed, PhD, the Henry G. Gale Distinguished Service Professor Emeritus of the Department of Chemistry, and Tobin Sosnick, PhD, Chair of Biochemistry and Molecular Biology and the William B. Graham Professor of Biochemistry and Molecular Biology.
And it was there that Jumper sought to answer a question that had vexed scientists for more than half a century: How do proteins fold?
“As an ‘accidental chemist,’ I wanted to go from understanding a very narrow slice of the problem to getting a better sense of the problem as a whole,” Jumper said.
Using different combinations of the same 20 building blocks known as amino acids, the body’s cells make thousands of proteins each day. And it is by spontaneously folding into different shapes that these proteins can perform a specific job such as transporting oxygen in the blood, making antibodies or enabling synapses that power thoughts in the brain.
Knowing the shapes of the proteins is essential for scientists to understand how the proteins do their job, and how to design drugs to interact with the proteins to treat diseases. But while modern DNA sequencing can pinpoint what amino acids a protein contains, it cannot determine the structure a protein will take.
At the time Jumper began his studies, the method scientists used to determine these structures was an experimental process that was laborious and expensive. Everyone in the field longed to speed up progress by asking a computer to predict a structure based on a protein’s DNA.
“We’d been at this for 60 years, and we still couldn’t predict what shape a particular protein would take,” Sosnick said.

At UChicago, Jumper studied protein folding in Sosnick and Freed’s joint laboratory a unique pairing of scientists tackling problems from theoretical and experimental perspectives to investigate questions at the intersection of biology, chemistry and physics.
“I think it was really an important part of my development to go from a physicist who happened to do biology to someone who could think more deeply about the question,” Jumper said. “I’m a big believer in interdisciplinary science. You learn so much more by talking to a diverse group of experts
University of Chicago
Nobel laureates
* University of Chicago alumnus
‡ Current member of faculty
to learn what they’re excited about and how they think about things.”
Under Freed’s and Sosnick’s guidance, Jumper honed his skills in computational modeling and theoretical chemistry, exploring the intricate dynamics of molecular interactions.
As part of the PhD program, Jumper rotated through different areas, including a stint in the lab of Steven C. Meredith, MD, PhD, a Professor of Pathology, where he moved from crafting computer models of proteins to actually making them in beakers.
That was long enough to realize “the lab and I were better apart,” Jumper said with a laugh, adding
John Jumper, SM’12, PhD’17, was awarded a share of the 2024 Nobel Prize in chemistry for his work creating an AI model called AlphaFold that predicts the structures of proteins.
Edward Adelbert Doisy PHYSIOLOGY OR MEDICINE
Hermann Joseph Muller PHYSIOLOGY OR MEDICINE
Bertrand Russell LITERATURE
Glenn Theodore Seaborg CHEMISTRY
Tsung-Dao Lee, PhD’50 * PHYSICS
Chen Ning Yang, PhD’48 * PHYSICS
George Wells Beadle PHYSIOLOGY OR MEDICINE
1958
Edward Lawrie Tatum, EX’31 * PHYSIOLOGY OR MEDICINE
Owen Chamberlain, PhD’49 * PHYSICS
1959
Willard Frank Libby CHEMISTRY
1960
James Dewey Watson, PhB’46, SB’47 * PHYSIOLOGY OR MEDICINE
1962
Karl Ziegler CHEMISTRY
1963
Maria Goeppert-Mayer PHYSICS
Eugene P. Wigner PHYSICS
Sir John Carew Eccles PHYSIOLOGY OR MEDICINE
1964 Konrad Bloch PHYSIOLOGY OR MEDICINE
1965 Julian Schwinger PHYSICS
Robert S. Mulliken, PhD’21 * CHEMISTRY
1966
Charles Brenton Huggins PHYSIOLOGY OR MEDICINE
1967 Hans Albrecht Bethe PHYSICS
George Wald PHYSIOLOGY OR MEDICINE
Luis W. Alvarez, SB’32, SM’34, PhD’36 * PHYSICS
1968
Murray Gell-Mann PHYSICS
1969
Paul A. Samuelson, AB’35 * ECONOMIC SCIENCES
1970
Gerhard Herzberg CHEMISTRY
1971
William H. Stein CHEMISTRY
1972
Kenneth J. Arrow ECONOMIC SCIENCES J. Robert Schrieffer PHYSICS
Friedrich August von Hayek ECONOMIC SCIENCES
1974
1975 Tjalling C. Koopmans ECONOMIC SCIENCES
Milton Friedman, AM’33 * ECONOMIC SCIENCES
1976
Saul Bellow, EX’39 * LITERATURE
1977 Ilya Prigogine CHEMISTRY
Herbert A. Simon, AB’36, PhD’43 * ECONOMIC SCIENCES
1978
Herbert C. Brown, AB’36, PhD’38 * CHEMISTRY
1979
Theodore W. Schultz ECONOMIC SCIENCES
Lawrence R. Klein ECONOMIC SCIENCES
1980
James W. Cronin, SM’53, PhD’55 * PHYSICS
Roger W. Sperry, PhD’41 * PHYSIOLOGY OR MEDICINE
1981
George J. Stigler, PhD’38 * ECONOMIC SCIENCES
1982
that he prefers working on computer simulations of proteins. “But it turned out to be a really valuable experience, to understand what experimentalists can do easily and what is hard, to know what problems they most need answered, to be familiar with the sources of uncertainty.”
BY THE NUMBERS
The number of people affiliated with UChicago to receive the Nobel Prize in chemistry 100
The number of UChicago community members to win a Nobel Prize (Jumper is the 100th winner)
For Jumper’s thesis, he developed a program that uses machine learning to simulate the process of protein folding. But the work did not predict protein structures of the size, scale and variety that AlphaFold does.
After completing his PhD in 2017, Jumper spent several months as a postdoctoral researcher in Sosnick’s lab before taking a job with Google DeepMind, a London-based AI research laboratory, where he joined colleague and future co-Nobel laureate Hassabis.
Jumper was quickly promoted to lead a team to attack the singular problem of predicting a protein’s final conformation based only on its protein sequence. After several years of development, Jumper, Hassabis and their team unveiled AlphaFold.
A user can feed any protein sequence into it whether it be from a fruit fly, a cow or a human and AlphaFold will spit out its prediction, as well as an estimate for its certainty about that prediction.
Although AlphaFold is not 100% accurate, the program marked an enormous leap forward. “It hit the level where it transformed what people thought was possible,” Sosnick said.
Since being released as an open-source program in 2021, it has been cited in thousands of scientific papers.
Researchers have used the program’s capabilities to model the interactions between the proteins involved in viruses, diseases and other health conditions. Doing so at the molecular level has the potential to revolutionize drug design by allowing for the creation of more targeted and effective therapies.
“I think [AI] is going to start to change how we approach really complicated problems,” Jumper said. “Nature is complex, and I think neural networks can handle complexity in surprisingly useful ways. I’m interested to see how far it can be pushed.”
Sosnick remembered Jumper as a generous scholar who took time to help others on their projects and papers and one who was always willing to partake in the UChicago tradition of friendly, vigorous debate.
Amid the recent celebrations of Jumper’s Nobelwinning discovery, the protein-simulating code he wrote as part of his PhD thesis at UChicago is still used regularly. Sosnick and a team recently received a grant from the National Science Foundation to broaden the code to study different scientific questions.
“He’s the graduate student that keeps on giving,” Sosnick said.
Beyond his contributions to science, Jumper has also influenced the vernacular.
Henry Taube CHEMISTRY Gerard Debreu ECONOMIC SCIENCES Subrahmanyan Chandrasekhar PHYSICS
1983
Yuan T. Lee CHEMISTRY
1986
James M. Buchanan Jr., PhD’48 * ECONOMIC SCIENCES
Leon M. Lederman PHYSICS
1988
Jack Steinberger * PHYSICS
1989 Trygve Haavelmo ECONOMIC SCIENCES
Harry M. Markowitz, PhB’47, AM’50, PhD’55 * ECONOMIC SCIENCES
1990
Merton H. Miller ECONOMIC SCIENCES
Jerome I. Friedman, AB’50, SM’53, PhD’56 * PHYSICS
AlphaFold draws from a database of more than 200,000 protein structures that have already been decoded and entered into the global Protein Data Bank. The program uses deep learning, a type of AI, to take insights from the bank of protein structures and apply them to predict what new structures might look like.
“The phrase ‘I AlphaFolded it’ is now something I hear almost every day, whether in the lab, during a thesis defense or at a scientific conference,” Sosnick wrote in 2023. “This transformation of a noun into a verb similar to ‘I Googled it’ reflects the profound changes that have taken place in the biological sciences.”
Ronald H. Coase ECONOMIC SCIENCES
1991
1992 Gary S. Becker * ECONOMIC SCIENCES
1993 Robert W. Fogel ECONOMIC SCIENCES
1995 Paul Crutzen CHEMISTRY F. Sherwood Rowland, SM’51, PhD’52 * CHEMISTRY
Robert E. Lucas Jr. * ‡ ECONOMIC SCIENCES
1996 Richard E. Smalley CHEMISTRY
1997 Myron S. Scholes, MBA’64, PhD’70 * ECONOMIC SCIENCES
Daniel C. Tsui * PHYSICS
1998
Robert A. Mundell ECONOMIC SCIENCES
1999
Daniel L. McFadden ECONOMIC SCIENCES
2000
James J. Heckman ‡ ECONOMIC SCIENCES
2002 Masatoshi Koshiba PHYSICS
John M. Coetzee LITERATURE
2003
Alexei A. Abrikosov PHYSICS
2004 Irwin Rose, SB’48, PhD’52 * CHEMISTRY
Edward C. Prescott ECONOMIC SCIENCES
Frank Wilczek, SB’70 * PHYSICS
2007 Leonid Hurwicz ECONOMIC SCIENCES
Roger B. Myerson ‡ ECONOMIC SCIENCES
2008 Yoichiro Nambu PHYSICS
Ada E. Yonath CHEMISTRY Barack Obama PEACE
2009
George E. Smith, SM’56, PhD’59 * PHYSICS
Jack Szostak ‡ PHYSIOLOGY OR MEDICINE
Thomas J. Sargent ECONOMIC SCIENCES
2011
Bruce A. Beutler, MD’81 * PHYSIOLOGY OR MEDICINE
2013 Lars Peter Hansen ‡ ECONOMIC SCIENCES
Eugene F. Fama, MBA’63, PhD’64 ‡ ECONOMIC SCIENCES
Richard Thaler ‡ ECONOMIC SCIENCES
2017
2018 Paul M. Romer, SB’77, PhD’83 * ECONOMIC SCIENCES
2019 John Goodenough, SM’50, PhD’52 * CHEMISTRY Michael Kremer ‡ ECONOMIC SCIENCES
2020 Andrea Ghez, LAB’83 * PHYSICS
2021 David Card ECONOMIC SCIENCES
2022 Douglas Diamond ‡ ECONOMIC SCIENCES
2023 Moungi Bawendi, PhD’88 * CHEMISTRY
Claudia Goldin, AM’69, PhD’72 * ECONOMIC SCIENCES
John M. Jumper, SM’12, PhD’17 * CHEMISTRY
2024
James A. Robinson ‡ ECONOMIC SCIENCES

The highly competitive Chicago Fellows Program aims to support, shape biological sciences leaders
BY NOVID PARSI
Since its launch in 2009, the Chicago Fellows Program has emerged as a premier postdoctoral fellowship for exceptional scholars in the biological and biomedical sciences offering them distinct benefits in funding, autonomy and networking.
Each year, the highly competitive University of Chicago program awards a two-year fellowship to a handful of applicants typically two or three chosen from a pool of dozens.
“We’re not looking for hired postdocs in a lab,” said Marcus Kronforst, PhD, a Professor of Ecology and Evolution who has been on the selection committee for about a decade. “We’re looking for a special connection between the fellow and the UChicago host lab someone who can use tools, techniques or ideas from the host lab to advance their research in a new and interesting way.”
Distinct opportunity
Many other programs award their funds to faculty members, not the postdocs, which typically means junior scientists must work within the faculty’s research areas. But Chicago Fellows recipients get direct funding, allowing them to pursue their own research interests.
Unlike most postdoctoral programs, Chicago Fellows comes not just with a salary but also research funding, Kronforst said. Each year, participants receive a
stipend that covers their salary plus a research budget of $10,000.
That funding model was a draw for Jenny Tung, PhD, who studied nonhuman primate genomics and behavior as a Chicago Fellow from 2010-12.
“Most postdoc positions get funding from elsewhere, often the principal investigator’s grants, which is still a wonderful opportunity but somewhat circumscribes the type of research a postdoc can do,” said Tung, now director of the Department of Primate Behavior and Evolution at the Max Planck Institute for Evolutionary Anthropology in Leipzig, Germany.
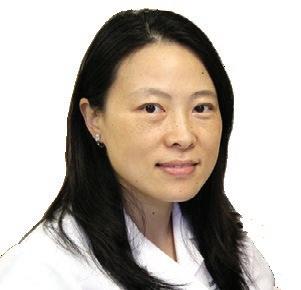
Huiping Liu, MD, PhD’06, who studied the role of microRNAs in breast cancer stem cell-mediated therapy resistance and metastasis as a 2009-11 Chicago Fellow, was able to secure additional funds and lead her own research team.
“Under my mentors’ guidance, I had the privilege to lead and supervise my own team, including a technician, which helped move the research faster,” said Liu, now an associate professor of pharmacology and medicine at Northwestern University Feinberg School of Medicine. “Chicago Fellows helped me learn not only scientific skills but also leadership and mentoring skills.”
The program has evolved in recent years. Applicants were previously required to submit a published academic paper.
Publishing a peer-reviewed paper can take a long time, however, so some applicants might not yet have their best work in print.
“But they do have great work that hasn’t yet been peer-reviewed and published,” said Connie Lee, PhD, Associate Dean for Basic Science for the Biological Sciences Division. As a result, the selection committee broadened its submission requirement to include unpublished work.
Organizers of the Chicago Fellows Program also strive to support camaraderie and career building. “Postdocs can be pretty isolated on campuses, so we try to create a sense of community for them,” said Allison Gicking, PhD, Director of Research Initiatives for the Biological Sciences Division.
For example, the program helps fellows build relationships in their fields and present their work at talks and conferences. A recent panel featured newly hired UChicago faculty speaking about their experiences applying for positions with tips on interviewing and salary negotiations.
“We want the postdocs to get up-to-date information, positioning them for success in the job market,” Gicking said.
UChicago educators also reap the benefits of a rotating crop of bright minds. “We get the chance to interact with some of the best young investigators in the world,” Kronforst said.
BY JAMIE BARTOSCH

What inspired you and your husband, Larry Hancock, PhD, to sponsor scholarships?
I’ve always wanted to give back because I received great scholarship and grant funding from the University of Chicago. Several years ago, we started the Sapphire Oak Scholarship Fund for UChicago’s Medical Scientist Training Program because we know becoming an MD and PhD takes time and money.
In 2023, we started a named scholarship just for PhD students. Many PhD students don’t have the financial support they need. We hope to help alleviate some debts for these students who really have talent and interest.
Do you recommend people earn an MD and a PhD?
If you are passionate about medical or scientific research, I think it’s the right way to go. But it’s a long haul. Young people today want to work and make money, but then they end up having to go back to school later which is OK. I was 30 when I started medical school. I worked for four years before my PhD. I decided to try research and see if I liked it. Obviously, I did.
How did you end up in the pharmaceutical world?
In the late 1980s, I was studying infectious diseases and everyone was focused on HIV, which I found interesting. At the same time, DRGs (diagnosis-related groups) came into effect. It went from not mattering how much time we spent with a patient, or how much we charged, to having to pay attention to our billing.
Carol Olson, PhD’82, MD’86, recently retired from a 30-year pharmaceutical career helping develop drugs for COVID-19, HIV and many other illnesses. A returning annual member of the Alumni Council of the University of Chicago Medical & Biological Sciences Alumni Association and Medicine on the Midway’s editorial committee, Olson spoke about her support for UChicago and shared advice for aspiring researchers.
I hadn’t considered a job in pharma. All of a sudden, I was getting calls from recruiters and I realized I could make a career change. I interviewed at the “Big 3”— Abbott, Pfizer and Bristol Myers Squibb and I liked the people at Abbott best. Plus, they were in Chicago.
What was the first drug you helped develop?
During my first year at Abbott, we were doing a new drug application for Helicobacter pylori (H. pylori), a common cause of stomach ulcers. It was really exciting. This is the first time we would have a treatment for ulcers, and I got people from across the company to work with me and do what was needed in a rapid time frame.
Most recently, you headed medical science and strategy at PPD, part of Thermo Fisher Scientific. What stands out?

What’s a memorable hurdle?
I was working as a chief medical officer for a small biotech, and we had an amazing product that was working for first-stage African sleeping sickness. We were almost ready to file with the Food and Drug Administration when we did additional safety studies that discovered some toxicity we hadn’t observed previously. We had to kill the drug, which killed the company.
We worked with the Infectious Diseases Society of America to develop 20 new antibiotics in 10 years. I also assisted with COVID vaccine and drug development, and we ran all the Moderna vaccine trials during the pandemic. I was the infectious disease specialist for our pandemic response committee, and I led programs to keep employees safe and clinical trials going forward.
Throughout my career, I always felt like I had the ability to contribute to something bigger. That’s one of the things that pharmaceutical product development does.
Applying the studies of biological science and medicine isn’t limited to the lab or the bedside. Using their deep, specialized knowledge, graduates of the Pritzker School of Medicine and the Biological Sciences Division at the University of Chicago — as well as individuals working at UChicago Medicine — are making an impact on public policy, health and safety. From homeland security to health equity, the work of these individuals helps influence lawmakers, federal agencies and everyday people. Here’s a look at five pursuits in action:

BY JAMIE BARTOSCH
Cardiologist, White House Fellow, 2023-24
From Hyde Park to the Hill: A cardiologist at the University of Chicago Medicine for most of his career, Smith was one of more than 1,000 applicants just 15 were selected for the fellowship, which he describes as “an intense one-year leadership incubator experience.” Fellows joined roundtable discussions and heard speakers from the federal government and the private sector, including Supreme Court justices and CEOs.
Action on-site: As part of the fellowship, Smith was assigned to work with the Social Security Administration to help the Oglala Lakota Sioux in South Dakota. The tribe, he said, has some of the worst health outcomes in the country. Smith organized a health fair and mobile clinic on the reservation, inviting five other federal agencies to offer screenings, CPR workshops, mental health information, disability benefits resources and more.
Transformative Pritzker class: Before his first year of medical school in 2006, Smith took a weeklong health disparities course taught by Monica Vela, MD’93, a former associate dean at Pritzker. Students drove around Chicago’s South Side, learning about disparate resources. Smith recalls future first lady Michelle Obama, then the Vice President for Community and External
Affairs at the University of Chicago Medical Center, speaking to the class. Haircuts and health: At Pritzker, Smith volunteered at Project Brotherhood, a South Side barbershop that doubles as a health clinic. Smith obtained a grant to help Pritzker students conduct educational sessions on wellness and preventive care inside the barbershop. “It became a catalyst in my career,” said Smith, noting
“If you’re going to build relationships and trust, you have to show up.”
that advocacy work completed at Pritzker informed his work in South Dakota. “If you’re going to build relationships and trust, you have to show up.”
Welcome to New York: Smith recently moved to the Big Apple, where his wife, journalist Adriana Diaz, landed her “dream job” co-hosting “CBS Mornings Plus.” Smith is looking forward to his next gig ideally “a leadership role related to health equity.”

Assistant Director, Federal Strategy, Johns Hopkins University
Front and center: Krinsky lobbies legislators on a broad swath of issues to support higher education and research, and he also informs policymakers about what’s happening at Johns Hopkins. He works on two main areas: “One is Department of Education-related student aid, accreditation and things that involve higher ed- and student-related policy,” Krinsky said. “The other is tax and finance issues, which are going to be a big deal in the current Congress.”
From academia to policy: While working as a graduate researcher at UChicago, Krinsky pondered merging his interests in science and education policy, but he wasn’t sure how. “I applied for, and was very lucky to get, the National Academies [of Sciences, Engineering and Medicine] Mirzayan Science and Technology Policy Fellowship
in 2015,” he said. The 12-week program helps early-career individuals gain skills and knowledge to work in science policy.
A mentor’s impact: While earning his doctorate in evolutionary biology, Krinsky was inspired by his dissertation adviser, Manyuan Long, PhD, from the Ecology & Evolution Department. “He’s an incredibly broad thinker and voracious in his interests,” Krinsky said. “He created a feeling of excitement and open-mindedness to any intellectual endeavor.”
Putting his degree to work: Krinsky loves the study of evolution to understand how events of the past affect the present. Graduate school also taught him how to be resourceful: “As a scientist, you have to figure a lot of things out: What is my scientific question? How am I going to carry out this project?” he said. “You also learn to be
“As a scientist, you have to figure a lot of things out. ...
You also learn to be open and know when to say, ‘I don’t know how to do this. Can you help me?’”
open and know when to say, ‘I don’t know how to do this. Can you help me?’”
Proud moment: In his previous job, as associate director for federal relations at Yale University, Krinsky helped organize a roundtable event with the director of the National Science Foundation. “It was rewarding to help our faculty have a conversation about what’s on their minds and discuss what kind of science they’re doing and how the NSF can support their work,” he said.
Full-circle moment: For the past nine years, Krinsky has participated in UChicago’s myCHOICE program, a decade-old effort that helps graduate students explore jobs beyond academia and leverage their unique skills. His target audience: those seeking careers in public policy.
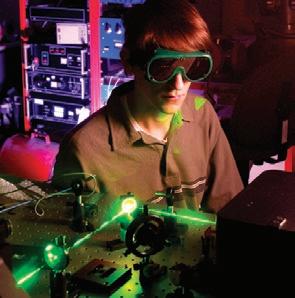
Economic Security Team Lead, American Systems Corporation
Tech whiz: A self-described “Swiss Army Knife of a scientist,” Zalisko is a contractor for the Department of Defense, where he manages a team that supports the Office of the Under Secretary of Defense for Research and Engineering. His job involves analyzing export controls and foreign investment into U.S. science and technology. “I’ll spend one day talking about lasers and directed energy weapons, and the next talking about biotechnology, human enhancement and economic security policy for AI chips,” Zalisko said.
Instant chemistry: Zalisko, a native of rural Carlinville, Illinois, grew up loving science and politics. Although he planned to get a PhD in organic chemistry and become a professor, his acceptance into the NIHsponsored Chemistry-Biology Interface fellowship landed him in a biochemistry lab. The placement was influential: For the first nine years of his career, as a graduate student and postdoc, Zalisko worked in the Kozmin, Keenan and Rock biochemistry labs at the University of Chicago.
Divine fellowship: Through UChicago’s myCHOICE program, Zalisko visited Washington, D.C., to explore nontraditional careers, and he learned about the Science & Technology Policy Fellowship. Run by the American Association for the Advancement of Science, this fellowship sponsors PhD scientists to work in the federal government. “That’s where the clouds parted and the angels sang,” Zalisko said. “I thought: ‘That’s exactly what I’d love to do.’”
Focus on national security: His first job in D.C. was working on homeland defense and disaster response within the DOD’s Office of Cost Assessment & Program Evaluation. After that, Zalisko became a senior program analyst in the State

Department, overseeing planning, training and implementation of export controls and border security. He moved on to a senior technical adviser role at CRDF Global, a foreign assistance nonprofit, where his tasks included engaging foreign countries in their peaceful use of nuclear technology to advance the United Nations’ sustainable development goals.
Public service priorities: UChicago instilled in Zalisko the importance of advancing scientific values in public service, rather
“I’ll spend one day talking about lasers and directed energy weapons, and the next talking about biotechnology, human enhancement and economic security policy for AI chips.”
than prioritizing personal acclaim or wealth. “I came to D.C. to improve the epistemology of the federal government,” he said.
Famous lookalike: Zalisko is often told he looks like Ukrainian President Volodymyr Zelenskyy, and he once dressed up as him for Halloween. “I’m one-quarter Ukrainian, and my name is phonetically close to Zelenskyy, so I just let people go with it,” he said.

Senior Professional Staff Member, Homeland Security & Governmental Affairs Committee, U.S. Senate
Watchful eye: An expert in biosecurity and countering weapons of mass destruction, Vora informs government leaders about developments and trends that could affect their constituents. She reports to U.S. Sen. Gary Peters (D-Michigan), the committee’s ranking member, and the homeland security team she serves on identifies, plans responses and develops policy related to threats that include cyberattacks, illegal drugs and viruses. She regularly meets with expert groups, such as the American Society of Microbiology, to see how their research can help save lives.
Science-focused strategy: Vora has a background that offers distinct value to the committee. “Having a PhD in cancer biology, I bring a different viewpoint,” said Vora, who previously worked at the State Department and the Department of Defense. “There’s a lot of value in not just knowing the science, but also the real-world impact.” On any given day,
she might speak to the implications of pathogens or radioactivity.
Shared mission of safety: The Department of Homeland Security involves a wide mix of law enforcement and policy groups, scientists, first responders and disaster managers, a network that can surprise people who might assume most work is done at the border or in airports. “It is a pretty incredible organization,” Vora said. “I would argue it has one of the most difficult missions in the entire government: to keep us safe from a million different threats that are complicated and growing.”
Campus connector: At UChicago, Vora was recruited to join the Dean’s Council, an experience she called “transformative” for its leadership training. She worked with all the different biology departments, their staff and Victoria Prince, PhD, Dean for Graduate Affairs in the Biological Sciences Division, to address student issues, plan outings and manage budgets.
“I don’t think people always appreciate what the value of good governance is, but it’s deeply rewarding in knowing what you can do for people.”
Smart choice: As a participant in the myCHOICE program at UChicago, Vora learned about opportunities at the National Academy of Sciences, where she met with people who had completed a training program there. “It was the experience that ultimately helped me land science policy fellowships, and it transitioned me from science to public policy,” Vora said.
Good deeds: In a previous job, Vora decided to issue a travel grant to a Tunisian woman who wanted to attend a conference on biosafety and biosecurity. The woman was so inspired that when she returned to Tunisia, she started her own biosafety organization. Years later, the woman who was never told who reviewed her travel grant application ended up inviting Vora to her own conference. “It was a full-circle moment,” Vora said. “I don’t think people always appreciate what the value of good governance is, but it’s deeply rewarding in knowing what you can do for people.”
Anthony D. Douglas II, MD
Surgery Resident, University of Chicago Medicine
Beyond the bedside: During his two years as a surgery resident in UChicago Medicine’s Level 1 trauma center, Douglas saw the effects of gun violence and high drug prices exposure that compelled him to find new interventions. “If you truly want to make a difference for people, you have to be involved in the policies that dictate their access to care and how they’re living,” he said.
Prescription for policy: Douglas took the notion to his faculty adviser, Selwyn O. Rogers Jr., MD, MPH, the Dr. James E. Bowman Jr. Professor of Surgery and the trauma center’s founding director. That led Rogers along with Andrew Benjamin, MD, SM’17, Assistant Professor of Surgery, and UChicago Medicine Government Affairs Vice President Ben Gibson to craft a custom public policy and advocacy program for him. It was a first-of-its-kind opportunity for a UChicago Medicine surgical resident.
Rising voice: Douglas has spoken about his experiences treating patients who couldn’t afford their medications, and the scramble to find less expensive and sometimes less effective alternatives. Douglas worked with Citizen Action/Illinois, and he has learned how to build coalitions with legislators and lobbyists. Last October, he testified at a U.S. Senate Judiciary Committee hearing hosted by Illinois Sen. Dick Durbin.
New knowledge: Even after many years studying science, policy research proved challenging. “I had to inform myself on things like drug purchasing and development, patent legislation, why prices have risen above inflation and more,” Douglas said. His core focus is advocating

“If you truly want to make a difference for people, you have to be involved in the policies that dictate their access to care and how they’re living.”
for the Health Care Availability and Access Board Act (HB 4472), which would protect Illinois residents, governments, healthcare providers and others from the high cost of prescription drugs.
Role models: Douglas admires physicians who have pivoted from medicine to public policy including former UChicago Medicine trauma surgeon Brian H. Williams, MD, who, as a Texas resident,
recently ran for the U.S. House of Representatives.
Continuing his mission: Douglas will earn a Master of Public Health from the University of Illinois Chicago in May. After that, he will return to his surgical residency at UChicago Medicine. Among other projects on his plate: growing Lil’ Scholars, the nonprofit he created to help South Side children with literacy.
BY JAMIE BARTOSCH
In December, Simone Biles posted a photo with Marcia Faustin, MD’13, FAAFP, to her millions of Instagram followers, offering thanks for “keeping me sane” amid the excitement and pressure of the 2024 Paris Olympics. (Biles won three gold medals.)
Biles’ teammate Sunisa “Suni” Lee called Faustin a “saving angel” for recognizing that the sudden inflammation in her body in February 2023 wasn’t allergies, but a serious kidney issue. With Faustin’s guidance, Lee navigated her health condition and went on to nab a gold medal in Paris.

These are just a few of the many praises the elite gymnasts have given Faustin aka “Dr. Marcy”— since she became co-head physician for the USA Gymnastics women’s national team in 2019.
Since then, Faustin has developed close bonds with the athletes at practice, camps, competitions and at the past two Summer Olympics, in Tokyo and Paris.
Spectators might assume her role mostly involves treating sprains and pain, but the job is also that of a confidant who helps some of the most-watched competitors on Earth maintain their mental health.
“To watch those ladies win gold medals, and to work hard and overcome their challenges, it makes my soul smile,” Faustin said. “I get teary-eyed because I know how much each of them overcame on their journey to success.”
Faustin, a gymnast and volleyball player during her high school years in Orland Park, expanded her athletic resume as a track and field star at Loyola University Chicago, where she initially intended to major in nursing. But when the nursing
program’s clinical rotations calendar didn’t align with her athletic commitments, she set her sights on medical school.
After earning a premed degree, Faustin came to the Pritzker School of Medicine on scholarship and focused on family and sports medicine.
“I was surrounded by awesome classmates and received an amazing education,” Faustin said.
Her 88-student class was tight-knit; in their free time, they played flag football and broomball and ran races across campus. Many of her classmates remain close friends, and one is now her husband, Toussaint Mears-Clarke, MD’13, MBA, FAAFP, a family medicine physician and obstetrician. Faustin’s medical school mentor, psychiatrist Elizabeth Kieff, MD’03, Pritzker’s former director of wellness, spoke at their wedding.
Through a University of Chicago Medicine connection, Faustin eagerly took an opportunity to volunteer at USA Gymnastics competitions. That effort led to her current role with the organization, a job she shares with New York-based Ellen Casey, MD, FACSM, FAAPMR.
The work is collaborative. Sometimes Faustin needs to bring in specialists like orthopaedic surgeons or physical therapists, but her main function is to take what she calls a “bio-psycho-social” approach to the athletes’ care. That means treating their muscular and skeletal issues, as well as understanding their mental health and how social surroundings can impact it.
“There are a lot of external influences they face,” said Faustin, who encouraged the Olympic gymnasts to minimize or avoid social media while in Paris and Tokyo, establishing “no-phone zones” where they could play cards and socialize. “We just stay focused.”
Faustin praises USA gymnasts for being grateful, hardworking, phenomenal competitors but she has equal respect for the collegiate athletes and everyday people she treats.
“I find as much joy in helping a patient who now can go dance at their granddaughter’s bat mitzvah,” she said.

A higher standard Faustin’s arrival to the team came after a turbulent and transformative time. In 2016, an investigation by The Indianapolis Star revealed that top executives at USA Gymnastics failed to alert authorities to many allegations of sexual abuse by coaches.
Hundreds of gymnasts came forward to say they were sexually assaulted or abused by members of the USA Gymnastics staff and medical team. Among the offenders: team doctor Larry Nassar, who pleaded guilty to federal and state charges and was sentenced to 100 years in prison.
Since then, USA Gymnastics has made many changes and efforts to rebuild trust, including new safety policies and procedures, along with the addition of a chief of athlete health and wellness position.
The most important aspect of caring for patients of all ages, levels and backgrounds is building trust. “It goes both ways; patients need to trust the physicians and vice versa,” she said. “It’s critical to have trust so we can help them make collaborative decisions when the world is watching and do what’s best for them, in the present and for their future.”
Faustin understands the influence and visibility of her role is more critical than ever.
“It’s a blessing to be their physician and to have them trust me with vulnerable information that they might not even share with their significant other or family members,” she said. “I really hold that trust to a high standard.”
Outside of her commitments traveling with USA Gymnastics, which total about 40 days annually, the Sacramento-based Faustin is an assistant clinical professor at the University of California, Davis, where she is co-head physician for the school’s 25 sports teams.
Never content to rest on the sidelines, she’s also the team doctor for the Sacramento Republic FC soccer team.
“It’s a busy life,” Faustin said. “But I love the people and the relationships I get to develop.”
As one of only a handful of Black female sports medicine doctors nationwide, Faustin knows her representation is important. Less than 3% of all U.S. physicians are Black women, and even fewer are in sports medicine, she said.
Faustin, center, on her role as co-head physician for the USA Gymnastic’s women’s national team: “It’s a blessing.”

While her schedule doesn’t leave time for much else, Faustin did speak as part of Pritzker’s Bowman Society Lecture Series in January. The topic: addressing mental health in athletes.
“I’m grateful to have gone to Pritzker, and it’s given me a great foundation to practice medicine,” she said. “So, I want to give back.”
BY MATT WOOD

Octopus arms move with incredible dexterity bending, twisting and curling with nearly infinite degrees of freedom. But how do these extraordinary creatures do it?
New research from the University of Chicago has revealed the nervous system circuitry that controls arm movement in octopuses is segmented, giving the deepsea dwellers precise control to explore, grasp objects and capture prey.
“We think it’s a feature that specifically evolved in soft-bodied cephalopods with suckers to carry out these wormlike movements,” said Clifton Ragsdale, PhD, Professor of Neurobiology at UChicago and senior author of the study, published in January in Nature Communications
Each octopus arm has a massive nervous system, and the eight arms combined contain more neurons than are found in the animal’s brain. These neurons are concentrated in a large axial nerve cord (ANC) that snakes back and forth as it travels down the arm, with every bend forming an enlargement over each of its hundreds of suckers.
Cassady Olson, a graduate student in computational neuroscience, led the study. Her goal: to analyze the structure of the ANC and its connections to musculature in the arms of the California two-spot octopus (Octopus bimaculoides), a small species native to the Pacific Ocean.
She and co-author Grace Schulz, a graduate student in development, regeneration and stem cell biology, examined thin, circular cross sections of the arms under a microscope, but the samples kept falling off the slides. After that, they tried lengthwise strips of the arms and found better luck plus an unexpected discovery.
The octopuses’ neuronal cell bodies, the pair learned, were packed into columns that formed segments resembling a corrugated pipe. These segments are separated by gaps called septa, where nerves and blood vessels exit to nearby muscles.
Nerves from multiple segments connect to different regions of muscles, suggesting the segments work together to control movement. Nerves for the suckers also exited from the ANC through these septa,
systematically connecting to the outer edge of each sucker. This indicates that the nervous system sets up a spatial, or topographical, map of each sucker.
The suckers are packed with sensory receptors that allow the octopuses to taste and smell things they touch like combining a hand with a tongue and a nose.
For comparison, the research team also looked at longfin inshore squid (Doryteuthis pealeii), which are common in the Atlantic Ocean. Squid tentacle clubs, they found, have fewer segments per sucker, likely because squid don’t use their suckers for sensation in the same way. (Squid rely more on their vision to hunt in open water; octopuses prowl the ocean floor and use their sensitive arms to explore.)
“Different cephalopods have come up with a segmental structure, the details of which vary according to the demands of their environments and the pressures of hundreds of millions of years of evolution,” Ragsdale said.
BY MATT WOOD
Age-related macular degeneration (AMD) is a leading cause of vision loss in adults over 50 in the United States. The National Eye Institute estimates about 11 million people in the U.S. are affected, a figure that’s expected to double by 2050.
Depending on the type a person has the more common dry (atrophic) AMD or wet (neovascular) AMD treatments such as lifestyle modifications, supplements and eye injections can slow its progression. Currently, there is no cure.
Now, researchers are focusing on metformin, an inexpensive drug widely used for treating Type 2 diabetes, as a potential new tool to prevent or slow down AMD at earlier stages.
55 and over with newly diagnosed AMD over a 10-year period, matched with controls who did not have AMD. The results, published in JAMA Ophthalmology, showed that patients taking metformin had reduced odds of developing AMD.
Metformin is sometimes prescribed to people without diabetes, such as patients with prediabetes and polycystic ovary syndrome. Skondra’s second study in JAMA Ophthalmology, published in 2024, showed that metformin lowered the risk of wet and dry AMD for these individuals, and that the protective effects seemed to be stronger than in people with diabetes.
Skondra’s team published a third study, in Retina, in February 2024 also showing that metformin is linked to reduced chances of developing new onset wet AMD, especially for patients without diabetic retinopathy, a damaging condition caused by high blood sugar levels.
Further research from Skondra, published in Investigative Ophthalmology & Visual Science in March 2024, showed that metformin decreased the odds of an advanced form of dry AMD called geographic atrophy by 47%.
‘A very complex disease’
That’s because diabetic patients taking metformin have a lower incidence of cardiovascular disease, cancer and cognitive decline, studies have found. And the results have led researchers to hypothesize how metformin may benefit people with eye disease.
“You need something noninvasive and safe that you can use in the early stages of disease,” said Dimitra Skondra, MD, PhD, a Professor of Ophthalmology and Visual Science at the University of Chicago.
“This is where metformin would fit perfectly: It’s already FDA approved, it’s been around for 30 to 40 years, and has a very good safety profile.”
Potential benefits of medication
Skondra has published a series of studies investigating the metformin connection.
In 2021, she and her colleagues used a nationwide health insurance claims database to study patients
Just how metformin protects against AMD is not clear. Preclinical studies in animals have shown that metformin can improve health by influencing cellular processes associated with aging, such as reducing oxidative stress and modulating inflammation.
“I think that’s why it is our best chance to stop a very complex disease,” said Skondra, who last year published another paper in Investigative Ophthalmology & Visual Science describing how mouse models with AMD lesions or damaged spots on the retina that took metformin experienced reduced lesion size and expression of genes associated with inflammation and the formation of new vessels.
“It attacks the problem from multiple routes and gives us a better chance to actually slow it down.”
This growing pool of data, Skondra said, is more than enough to justify prospective trials in humans, where subjects 55 and older with and without diabetes could be given metformin to see if it prevented or slowed AMD.
After years of tweaking their lesson plans to meet students’ changing needs, as well as developing publications and platforms used by countless physicians-to-be, two University of Chicago professors remain committed to the pursuit.
Vinay Kumar, MBBS, MD, the Lowell T. Coggeshall Distinguished Service Professor of Pathology at UChicago, is credited with the discovery of natural killer immune cells. Any doctor who completed medical school in the last few decades, however, is likely to recognize Kumar’s name as a co-author of the “Robbins books,” the internationally recognized, gold-standard pathology textbooks.
His colleague, Husain Sattar, BS’93, MD’01, Professor of Pathology, is best known for developing Pathoma, a wildly popular multimedia course beloved by medical students worldwide.
PHOTO BY MARK BLACK

The educators share a deep respect for one another, and also a progressive teaching approach. By championing practical knowledge and real-world application over rote memorization, they have made a big impression and become unlikely stars.
Still, the pair prefers to focus on academics rather than acclaim.
“It is my greatest honor: the chance to interact with whoever wants to listen, and to give them something they can use throughout their careers,” Sattar said.
Different direction
It wasn’t always this way. Earlier in his teaching career, before coming to UChicago, Kumar noticed gradually that students were coming to class less often.
“Faculty were angry, but I wasn’t; I knew there had to be a reason,” he said. “I told them, ‘Instead of yelling at students or penalizing them by grading attendance, why don’t we sit down and ask them
BY GRACE NIEWIJK
why they don’t come? These are intelligent, motivated people paying a lot of tuition.’”
Kumar invited students to a candid conversation, where they explained that the lectures they skipped mostly consisted of factual knowledge they could obtain on their own. What they wanted was practical ways to use that information.
“I decided we had to change our teaching,” Kumar said.
Starting in 1992, he slashed lecture times from 150 to 50 hours, with the remainder focused on case-based discussions.
“We’d do things like show them a picture of a rheumatic heart and simply ask: ‘What do you think is happening here? How did this change occur?’ And that completely changed everything,” Kumar said.
The pivot helped boost attendance, as well as students’ test and satisfaction scores. Eventually, Kumar and his co-authors published an updated pathology textbook that had just 150 pages of classic informational material, with the remainder comprised of cases built to challenge students.
Making pathology digestible
Sattar’s contributions to teaching are personal. “In medical school, I was just completely overwhelmed,” he said. “It felt like drinking from a fire hydrant.”
He went through the foundational pathology course at UChicago three times: first as a medical student, then as a teaching assistant and a pathology resident TA. Even on the third time, he was struck by the sheer amount of material students were struggling to grasp.
“This idea for Pathoma arose in my mind because we were talking about lymphoma, carcinoma, melanoma, sarcoma,” said Sattar, who used the nomenclature as inspiration when creating Pathoma in 2011. “I said to myself, ‘Students are still missing the big picture.’”
Pathoma delivers simplified, clinically integrated explanations of only the most important topics, and it’s intended to be an affordable complement to classroom textbooks and lectures. With digestible video modules (featuring narration in Sattar’s calming voice) accompanied by a concise, easy-to-read textbook, the format, Kumar said, is popular because “it’s a multimedia resource that facilitates discussion and helps students truly understand things.”
PHOTO BY STEPHEN GARRETT

BY EMILY AYSHFORD
Over the last decade, researchers have begun to untangle the network of trillions of bacteria, fungi and other microbes that live within our guts. It’s a major task that requires new thinking and specialized equipment.
In his namesake lab, Sam Light, PhD, the Neubauer Family Assistant Professor of Microbiology, and his team study these microbes and their implications in treating diseases including inflammatory bowel disease, liver disease and Type 2 diabetes and enhancing health.
Light spoke more about his work for the University of Chicago’s Inside the Lab interview series.
What is the human gut microbiome?
It comprises hundreds of species of microorganisms, primarily bacteria, that colonize our gastrointestinal tract. Our digestive systems can’t digest everything in food, so evolution came up with this clever strategy where we outsource that job to different species of microbes that have unique capacities to break down different elements in our food.
Through the digestive process, these microbes make small molecules known as metabolites, which are analogous to drugs. They can enter our bloodstream and have a variety of implications for human health.
What do we know about this connection?
The human gut microbiome has been linked to a lot of different diseases, as well as the prevention of infectious disease. Some people argue that the microbiome is essential because one of the main things that microbes do is provide colonization resistance through various mechanisms to make it harder for pathogens to cause disease.
The questions we’re tackling are trying to understand what role the microbes play. How do they produce these different metabolites that influence

our health? Can we identify the principles that will help understand why the microbiome is dysfunctional in some disease states? And can we find new ways to intervene?
How does your lab study the microbiome?
The large intestine is an anaerobic environment, which means there’s no oxygen. When we want to grow anaerobic microorganisms in the lab, we need to make environments that are free of oxygen. So, we have these big chambers where we vacuum out the air and replace it with nitrogen. It’s kind of clunky, but it’s what you have to do.
We can also take a fecal sample, extract the DNA from it and sequence that to identify microbes that are present. We also have mass spectrometers that can determine what metabolites are in the sample, and we can measure the concentrations.
What angles do you investigate?
We have specific disease-driven projects. There’s this specific microbiome dysfunction that has been shown to occur in a subset of patients with Type 2 diabetes, and it has been shown very convincingly to exacerbate their disease. But exactly which microbes are responsible for that dysfunction and why aren’t known. We’re trying to identify them.
We also ended up discovering that there are these different microbes that modify certain hormones. That includes sex and stress hormones. Microbes inactivate these hormones, and we think there’s relevance to inflammatory bowel disorders. That’s because the microbes that do it tend to appear more often in the guts of people with IBD; we think they are actively working to produce a more pro-inflammatory environment that benefits them.
How might this work affect patients?
Doctors use antibiotics to treat disease, but an unintended side effect is that it wipes out gut microbes. My lab is part of the Duchossois Family Institute, which specializes in studying the microbiome. Dr. Eric Pamer, the director, has overseen the construction of a facility where they can prepare gut microbes.
Inside the Lab offers a firsthand look at the laboratories of UChicago researchers. Read more interviews at news.uchicago.edu/inside-the-lab
They’re about to start a clinical trial administering gut microbes to people whose microbiomes have been wiped out by antibiotic treatment. Hopefully this will be a proof of principle and establish some of the critical data needed to support more widespread adoption of this approach.
BY GRACE NIEWIJK
Most people can easily complete a basic task without looking at their hands.
Put on gloves that dampen the sense of touch, however, and many actions may become frustrating. Take away proprioception the ability to sense the body’s relative position and movement and the result could be a broken object or even injury.
“Most of us don’t realize how often we rely on touch instead of vision for typing, walking, picking up a flimsy cup of water,” said Charles Greenspon, PhD, a Research Assistant Professor in the Department of Organismal Biology and Anatomy at the University of Chicago.
“We could evoke the feeling that you were touching something, but it was mostly just an ‘on/ off’ signal, and often it was pretty weak and difficult to tell where on the hand contact occurred,” Greenspon said.
But shared work among scientists and engineers at UChicago, the University of Pittsburgh, Northwestern University, Case Western Reserve University and Blackrock Neurotech has brought major advancements in using brain-computer interfaces and robotic prosthetic arms to restore motor control and sensation.
A testing participant controls a bionic hand through a brain-computer interface that allows him to feel pressure changes as the steering wheel moves in the hand.
“If you can’t feel, you have to constantly watch your hand while doing anything, and you still risk spilling, crushing or dropping objects.”
Recently, Greenspon and a team of collaborators published two papers documenting progress on a transformative technology: direct, carefully timed electrical stimulation of the brain that can create tactile feedback from prosthetic hands. The goal is to enhance independence and quality of life for people living with limb loss or paralysis.

The researchers’ approach to prosthetic sensation involves placing tiny electrode arrays in the parts of the brain responsible for moving and feeling the hand. This allows a participant to move a robotic arm by simply thinking about movement.
Meanwhile, sensors located on the limb can trigger pulses of electrical activity called intracortical microstimulation in the part of the brain dedicated to touch.
For about a decade, this method faced limitations.
The work has been underway for years, much of it led by pioneering UChicago neuroscientist Sliman Bensmaia, PhD, until his unexpected passing in 2023.
In the first study, published in Nature Biomedical Engineering, Greenspon and his colleagues focused on ensuring that electrically stimulated touch sensations are stable, accurately localized and strong enough to guide everyday tasks. By delivering short pulses to individual electrodes in participants’ touch centers and having them report where and how strongly they felt each sensation, the researchers created detailed maps of brain areas that correspond to specific parts of the hand.
The result: When two closely spaced electrodes are stimulated together, participants feel a stronger, clearer touch that can improve their ability to locate and gauge pressure on the correct part of the hand.
Exhaustive tests then confirmed that the same electrode consistently creates a sensation that corresponds to a specific location on the hand. Such reliability could allow prosthetic users to trust their motor control and sense of touch as much as they would with a natural limb.
“If I stimulate an electrode on Day One and a participant feels it on their thumb, we can test that same electrode many years later and they still feel it in roughly the same spot,” said Greenspon, the study’s lead author.
“ This is how we restore touch to people...and we’re working to expand the approach to other regions of the brain.”
Charles Greenspon, PhD
RESEARCH ASSISTANT PROFESSOR
DEPARTMENT OF ORGANISMAL BIOLOGY AND ANATOMY

Led by Giacomo Valle, PhD, a former postdoctoral fellow at UChicago, the team then took the research a step further.
“We saw that two electrodes placed next to each other in the brain don’t create sensations on side-byside parts of the hand,” Greenspon said. “Instead, the sensory locations overlap.”
That insight led the researchers to test whether prosthetic users could feel the boundaries of an object or the motion of something sliding along their prosthetic. After identifying pairs or clusters of electrodes whose “touch zones” overlapped, the scientists activated them in carefully orchestrated patterns to generate sensations that progressed across the sensory map.
The idea worked. Participants described feeling a gentle gliding touch passing smoothly over their fingers, despite the stimulus being delivered in small, discrete steps. Scientists attribute this result to the brain’s ability to stitch together sensory inputs and read them as coherent, moving experiences by filling in gaps in perception.
The approach also significantly improved participants’ ability to distinguish complex tactile
shapes and respond to changes in the objects they touched. They could sometimes identify letters of the alphabet traced on their fingertips, and they could use a bionic arm to steady a steering wheel when it began to slip through the hand.
The results were published in Science, with Greenspon and Bensmaia sharing senior authorship.
As electrode designs and surgical methods continue to improve, researchers hope tactile coverage will enable even more lifelike feedback.
The approach also holds promise for other types of sensory loss. The group has collaborated with UChicago surgeons and gynecologists on the Bionic Breast Project, which aims to produce an implantable device that can restore the sense of touch after mastectomy.
“We all care about the people in our lives who get injured and lose the use of a limb this research is for them,” Greenspon said. “This is how we restore touch to people. It’s the forefront of restorative neurotechnology, and we’re working to expand the approach to other regions of the brain.”
people living with limb loss or paralysis.


For 30 years, Pritzker School of Medicine students have lent their time and skills to the Maria Shelter Health Clinic, a haven for homeless women and their children on Chicago’s South Side.
Pritzker students can take part as early as their first year. A student-led executive board oversees clinic operations that include scheduling volunteer physicians, managing a referrals system, maintaining medical supplies and organizing the annual Englewood Health Fair.
“They do the heavy lifting,” said Andrew Davis, MD’80, MPH, a Professor and Associate Vice Chair for Quality in the Department of Medicine, who began volunteering at the Maria Shelter Health Clinic when he returned to Pritzker to teach in 2000.
Margaret’s Village, a nonprofit that operates the shelter, recently honored Pritzker’s three decades of service and its many students who, with the supervision of faculty volunteers, conduct patient interviews, collect vital signs and present cases to attending physicians.
The medical school, along with Davis and Wei Wei Lee, MD, MPH, a Professor of Medicine and Associate Dean of Students at Pritzker, received
50th annual gala in October.
“If we can give back in some way and also help students get some clinical experience while learning about how some of the issues in our system impact people, that’s a win,” said Davis, faculty adviser to the clinic a role he now shares with Sonia Oyola, MD, Assistant Professor of Family Medicine.
The partnership provides a critical resource for Englewood residents facing physical and emotional traumas, said Angela Hicks, executive director of Margaret’s Village.
And the work continues to evolve. Recently, Pritzker students led a successful effort to establish a psychiatric clinic at the shelter to provide mental health services to residents.
The Maria Shelter Health Clinic is one of Pritzker’s six student-run free clinics. Pritzker students also engage the South Side through numerous groups, including Chicago Street Medicine, the Health Professions Recruitment and Exposure Program (HPREP), and Medical Careers Exposure and Emergency Preparedness (MedCEEP), and several school outreach programs.
6 student-run free clinics
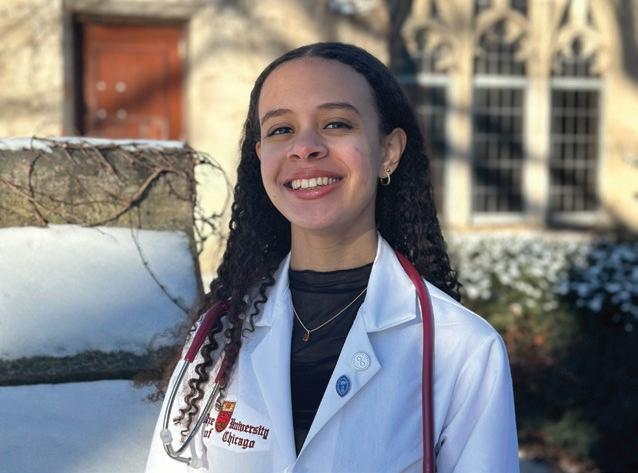
Janelle Herring, a second-year student at the Pritzker School of Medicine, is a co-director of the Maria Shelter Health Clinic in Englewood.
Why get involved with the clinic?
The Association of American Medical Colleges (AAMC) has presented the 2024 Spencer Foreman Award for Outstanding Community Engagement to the University of Chicago Medicine and the Pritzker School of Medicine.
The award is given annually to an AAMC-member medical school or teaching hospital with a sustained commitment to addressing community needs through engagement, partnership and collaboration. It was presented in a virtual ceremony in October.
715 patients served
241 student volunteers 179 clinic sessions held 63 individual preceptors 41 resident volunteers
Our mission of serving women of the South Side aligned perfectly with my own. I’m from this area, and I ultimately want to work in women’s health. I also love that the clinic is located within Maria Shelter. This allows us to form long-term relationships with a meaningful impact.
What’s a typical day like for you?
Our offerings rotate between primary care and psychiatry clinics. At each one, we address any urgent issues, while also getting individuals connected to long-term care for chronic conditions. Our work also has a strong educational focus for patients.
Why is this partnership so important?
We are a touchpoint for people who have had to put their health needs on the back burner. By bringing our services to the shelter and reducing barriers to care, we are hopefully playing a small role in overcoming systemic inequalities that South Side women have historically faced.
How has the clinic informed your career?
It taught me how to advocate. While this year has gifted me skills of creativity and resilience, witnessing the context of individuals’ lives outside of a normal healthcare encounter has been just as impactful. It has strengthened my resolve to go above and beyond for future patients.
In a statement, the AAMC lauded Pritzker and UChicago Medicine for embedding those pillars “into every aspect of medical education, research and clinical care.”
“Through our mission, vision and values and across all of our strategic initiatives, UChicago Medicine and the Pritzker School of Medicine are committed to advancing health equity within the communities we serve,” said Mark Anderson, MD, PhD, Dean of the Biological Sciences Division and of the Pritzker School of Medicine.
Last year, Pritzker launched an updated educational framework called the Phoenix Curriculum that incorporates clinical experience and community engagement from Day One.
Additionally, residents across specialties collaborate via the Graduate Medical Education Community Champions program in partnership with the Urban Health Initiative, UChicago Medicine’s community health division that serves Chicago’s South Side and south suburbs.
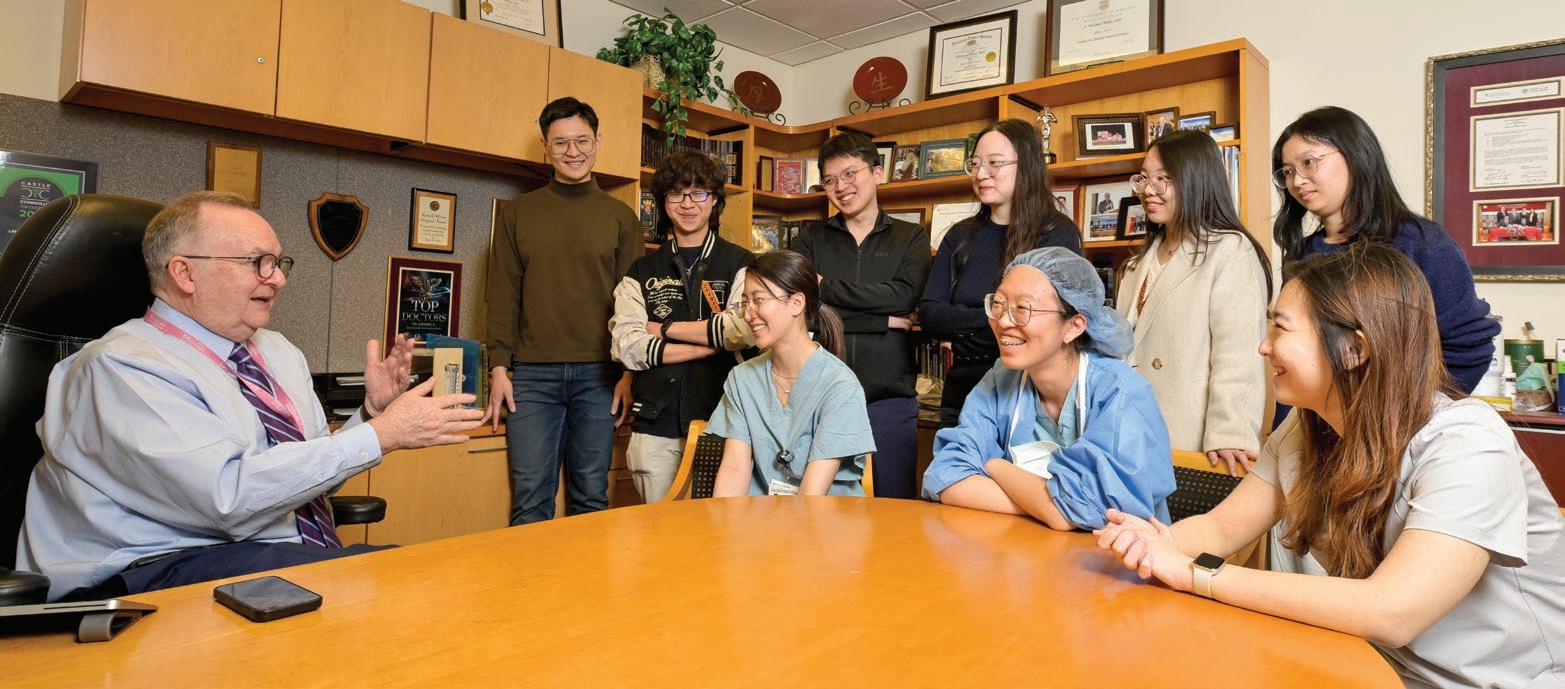
BY NOVID PARSI
Nearly 7,000 miles separate the University of Chicago Pritzker School of Medicine and Peking Union Medical College (PUMC) in Beijing, but the two institutions have been intertwined for more than a century.
In 1921, the Rockefeller Foundation sought to establish a world-class medical school in China, and it tapped Franklin C. McLean, MD, SB’07, SM’12, PhD’15 an Illinois native and the son and grandson of physicians to help set up the college.
Two years later, McLean drew on his experiences at PUMC when blazing another trail: directing UChicago’s brand-new medical school.
Today, Pritzker and PUMC are linked via myriad programs that foster cross-continental collaboration and travel among students, residents, fellows and faculty a rare arrangement for medical schools, said J. Michael Millis, MD, a Professor of Surgery at Pritzker.
The efforts help teams on opposite ends of the world discover “new and different ways to address illness and health,” Millis said.
‘Life-changing experience’
For a few weeks each year, Pritzker hosts about 15 senior medical students from PUMC to complete their rotations at the University of Chicago Medicine, an exchange in place since 2008. Two years ago, PUMC began hosting about 15 senior medical students from Pritzker.
“The students we took from Pritzker last year felt it was a life-changing experience,” said Millis, who is also Vice Chair of Global Surgery for UChicago Medicine. “Similarly, the students who come here from PUMC enjoy learning how the U.S. healthcare system works and how we teach.”
Millis holds conferences at PUMC once or twice annually where UChicago Medicine residents and fellows give talks and, in some instances, conduct clinical research. Pritzker also hosts PUMC residents and fellows who observe UChicago Medicine’s clinical operations and also pursue their own clinical and academic interests.
Zain Talukdar, MD, a second-year resident in pediatrics at UChicago Medicine Comer Children’s Hospital, spent time at PUMC last spring. The staff
there, he said, were “gracious” in helping translate handouts and conversations for visiting clinicians.
The cultural differences were also notable.
“It was interesting to see how outpatient clinics allowed multiple extended family members to actively participate in well-child checks, as well as the cooperation from families and young children during more academic processes, such as attending rounds,” Talukdar said. “I learned there are many ways patients view their health.”
PUMC sends about 10 faculty members to Chicago each year to spend three weeks observing how Pritzker educates its medical students. Some Pritzker faculty members attend conferences and spend time at PUMC.

Fromme, MD, Professor of Pediatrics and Associate Dean for Faculty Development.
“I learn a lot from my PUMC colleagues and they learn a lot from me about different diseases and different presentations of diseases both in China and the U.S.,” said Millis, noting that PUMC is generally regarded as the top medical school in China. “Our intertwined history and strong working relationship make accepting each other’s students easy.”
Several exchanges focus on the executive level. The Clinical Leadership Development Fellowship hosts faculty from PUMC and other elite teaching hospitals in China for an academic year at UChicago. With coursework in clinical medical ethics and hospital management, the intensive program offers a certificate in clinical trials management and regulatory compliance.
The fellowship, established in 2018, “dramatically impacts the scholars’ careers in their home institutions,” Millis said. “It allows them to gain leadership positions and increases their confidence in their leadership when they go back to China.”
A similar mission guides UChicago’s International Medical Educators Program (IMEP). During two weeks in Chicago and three months virtually, Pritzker faculty help clinical educators from China hone their teaching skills covering effective ways to give lectures, conduct small-group discussions and design courses. One-third of spots go to PUMC faculty; the rest are given to faculty at other Chinese institutions.
“A lot of participants are in positions of leadership, so they have an outsize influence on how education is conducted at their hospitals,” said Jonathan Lio, MD, Associate Professor of Medicine at Pritzker, who established IMEP in 2019 with Renslow Sherer Jr., MD, Professor of Medicine, and H. Barrett
“There’s a robust exchange,” Lio said. “We show them our best our newest, most innovative teaching techniques. And we help them develop new curricula for medical students and residents, so the program impacts countless trainees down the road.”
Evolving partnership
The modern era of the PritzkerPUMC relationship dates back more than two decades.
In the early 2000s, China began modernizing its liver transplant system, and over a decade ago, the country standardized its medical training and residency programs. Physicians from both PUMC and Pritzker played critical roles in these processes.
In addition to providing on-site medical education, the exchanges give visiting students, residents and faculty the change to explore culture and community.


Millis and his PUMC colleagues helped establish regulations for liver transplants as China stopped using organs from executed prisoners, for example. Lio and other Pritzker physicians helped PUMC implement competencies for training residents including patient care, communication, teamwork, teaching and professionalism.
“We’ve seen a number of institutions pull back from their interactions with China because of geopolitical issues,” Millis said. “Fortunately, our leadership has continued to support these interactions.”
One sign of PUMC’s standing in China today? Many of the Chinese government’s health appointees are PUMC faculty members, Millis said.

BY JAMIE BARTOSCH
As Jillian Bowman, AB’20, opened the envelope, her hands shook. But the University of Chicago Pritzker School of Medicine student saw what she had hoped for: a match with Boston Children’s Hospital for her pediatric residency.
“I just started crying,” said Bowman, who hugged her parents and her grandmother Glenda Ashley, MD, a retired Chicago pediatrician.

Bowman was among 85 Pritzker students who learned their residency placements on March 21 during the annual Match Day celebration in Ida Noyes Hall.
After applying and interviewing at multiple hospitals, the students ranked their top picks. On Match Day, they learned where they’ll spend the next four years or more. Some jokingly call it “employment day” because it means the start of full-time jobs after nearly a decade.
After tearing open their envelopes, people hugged, cried, high-fived and shared their news with classmates and family members.


“I’m so happy,” said Adaora Ekwonu, AB’20, who matched with the University of Pennsylvania for psychiatry. “This is such a surreal moment.”
Ekwonu is one of a record-high 17% of Pritzker students who matched for a psychiatry residency this year, mirroring a growing interest in the field.
Armaan Singh, who also will head to UPenn for his psychiatry residency, was inspired by shifting needs driven by the pandemic. “During COVID, mental health really came to the forefront,” he said.
The specialty goes far beyond psychoanalysis; it folds in neurology, policy, education and research on new medications, substance abuse, depression, dementia and much more, said Deborah Spitz, MD, Professor of Adult Psychiatry, Director of Residency Training and Vice Chair for Education and Academic Affairs.
Vineet Arora, MD, AM’03, Pritzker’s Dean of Medical Education, congratulated the class for having a profound impact on the South Side, where they staffed free clinics and did community engagement and health research.
With convocation coming up June 7, many in the close-knit class felt bittersweet about having to say goodbye and disperse around the country. Still, “you are always part of our family,” Arora told them.
Most popular specialties
Internal medicine (22 students)
Psychiatry (14)
General surgery (7)
Pediatrics (6)
Orthopaedic surgery (5)
Most popular institutions
University of Chicago Medical Center (20)
University of California system (8)
Harvard University programs (5)
Northwestern University programs (5)
Stanford University programs (4)
University of Illinois College of Medicine (4)
Fourteen fourth-year students of the University of Chicago Pritzker School of Medicine
Class of 2025 were inducted into the Gold Humanism Honor Society in February. Nominated by their peers, these students exemplify compassionate patient care and serve as role models, mentors and leaders.
Jillian Bowman, AB’20, was the student recipient of the Leonard Tow Humanism in Medicine Award. Lolita Alkureishi, MD, was the faculty recipient.

Nineteen members of the University of Chicago Pritzker School of Medicine
Class of 2025 were inducted into the Alpha Omega Alpha (AΩA) Honor Medical Society. The AΩA constitution calls for students to be recognized not only for academic achievement, but also achievement in research and scholarship, leadership, ethical behavior, professionalism and service to the school and community at large.
Each AΩA class elects alumni, faculty and housestaff to the Illinois Beta Chapter (the University of Chicago) in recognition of their leadership and accomplishments. Alumni are eligible 10 years after graduation. Faculty are elected based on demonstrated commitment to scholarly excellence and medical education. Housestaff are elected for their continued achievement, promise and mentorship qualities.
The 2025 honorees are:
Alumni: Kammi Henriksen, AB’02, MD’07, Department of

Eli Falk, Evan Neczypor, Reilly
Pathology; and Yanina PurimShem-Tov, AB’94, MD’98, Rush University Medical Center.
Faculty: Ethan Molitch-Hou, MD, Department of Medicine; and Alejandro Palma, MD, Department of Medicine.
Housestaff: Ross H. McMillan, MD, Department of Medicine; Dhruvil A. Patel, MD, Departments of Medicine and Pediatrics; and
Dagher.
Greg Raster, MD, Department of Surgery.
Cherrell Triplett, MD, MBA, program director of the OB/GYN residency program at Illinois Masonic Medical Center, received the Clinical Faculty Award, which recognizes a community physician who contributes with distinction to the education and training of clinical students.
Robert Gallo, MD, renowned for co-discovering HIV, has joined the University of South Florida Health Morsani College of Medicine as director of the new USF Health Virology Center. Additionally, USF has been selected as the international headquarters of the Global Virus Network, an organization Gallo co-founded. Gallo, who earned an MD at Jefferson Medical College, completed an internship and his residency at the University of Chicago.
Fernando Ugarte, MD’65, retired after being in medicine for 52 years. His hobby of photography transformed into his full-time job and passion. He travels extensively around the United States, Peru and Europe, and he documents everything. Ugarte, a published and award-winning photographer, looks at the world from a different perspective and finds beauty everywhere. His pictures are used by businesses, and he has created 150 books for friends and family.
Allison August, MD’93, was named one of Endpoint News’ 20 Women Leading Biopharma in 2024. This list celebrates over 120 women breaking boundaries in biopharma research and development. August is the chief medical officer at Comanche Biopharma, where she is focused on developing a treatment for preterm preeclampsia. Comanche Biopharma won a Fast Track designation from the Food and Drug Administration for its Phase 1 lead candidate, a siRNA investigational drug injected into patients.
Imelda Dacones, SB’92, MD’96, was appointed to the National Medical Fellowships (NMF) board of directors in December 2024. The NMF is committed to supporting underrepresented students and practitioners in medicine and healthcare professions. Dacones is the Pacific Northwest market president for Optum, overseeing the company’s Washington and Oregon markets. She is an internist/hospitalist and is
widely recognized for her leadership in driving value-based care models, innovation and transformation.
Jonathan Dowell, MD’93, received an Institutional Service Award for his years of outstanding clinical service at the UT Southwestern Medical Center. This award recognizes individuals who share time and expertise in service to internal committees, task forces and other institutional activities impacting patient care. Dowell is a professor of internal medicine in the Division of Hematology and Oncology at UT Southwestern.
Amy Derick, MD’02, was elected to serve the state of Florida as the chairwoman of the Florida Board of Medicine, starting in January 2025. She is the first woman to chair the board in at least a decade, and she is one of two women on the board. Derick served as the Illinois State Medical Disciplinary Board chair from 2019-21.
Share news about your life and accomplishments: mbsaa.uchicago.edu/update-contact-info Send letters to the editor regarding a memory or a story in this issue: momeditor@bsd.uchicago.edu
Guillermo “Guillo” Mateo, SB’45, MD’48, died on December 6, 2024. After serving in the U.S. Air Force during the Korean War, Mateo settled in Minnesota, where he established a private medical practice that welcomed patients regardless of their ability to pay. His late wife, Grace “Bunnie” Mateo, SM’45, who died in 2012, joined his practice as a nurse practitioner. The couple later taught in the University of Minnesota’s nurse practitioner program. After retiring to South Carolina, Mateo enjoyed skiing and playing tennis into his 90s.
Eugene Halpert, MD’56, died on October 31, 2024. Halpert was a clinical professor in the Department of Psychiatry at NYU Medical Center for over four decades. He earned a bachelor’s degree from Union College and an MD from the University of Chicago. After serving as a captain in the U.S. Army from 1957 to 1959, he embarked on a distinguished career
as a psychiatrist and psychoanalyst. Halpert was president of the Long Island Psychoanalytic Society from 1975-76. While proud of his accomplishments, Halpert’s family also cherished his kindness, generosity, curiosity, humor and dedication to loved ones.
James Huffer, AB’53, SB’55, MD’58, died on October 23, 2024. Huffer’s credentials are a testament to a lifetime spent caring for people. While serving in the U.S. Air Force, stationed at Clinton-Sherman Air Force Base in Oklahoma, Huffer served as the base’s sole physician. He joined the Department of Orthopedics and Rehabilitation at the University of Wisconsin-Madison and eventually became a partner at Bone and Joint Surgery Associates. A doctor and mentor to many student-athletes, he was twice presented with the studentgiven UW Medical School teaching award. Huffer will be remembered as a loving husband, father, grandfather and great-grandfather.
Herbert Rothenberg, SB’49, MD’51, died on October 7, 2024. Rothenberg transferred to the University of Chicago
from the University of Michigan, and he earned his bachelor’s degree at 20, followed by his MD. Rothenberg worked as chief resident at Denver General Hospital, served as a U.S. Air Force captain and joined the University of Colorado Medical School faculty. He believed his major contributions were the development of the internal medicine teaching program at Rose Medical Center and serving on the board of directors for Denver Opportunity, where he helped develop the Denver Neighborhood Health Program.
Alan M. Weintraub, MD’56, died on July 20, 2024. Early in his career, Weintraub joined the Navy Medical Corps and cared for U.S. senators while stationed at the Capitol in Washington, D.C. As a cardiologist, he practiced at Georgetown University Medical Center and Sibley Memorial Hospital. He also cared for patients who underwent some of the first artificial heart valve operations performed by Charles Hufnagel, MD, who pioneered the technology. In his free time, Weintraub competed in carriage driving events and became a certified scuba diver.
EXECUTIVE COMMITTEE
Karyl S. Kopaskie, AB’07, PhD’14 President
Doriane C. Miller, MD’83
Immediate Past President
Sapana Vora, PhD’14
Vice President
Rajiv Jauhar, MD’91
Chicago Partners Program Chair
Courtney K. Burrows, PhD’15, MBA’17 Alumni Awards Committee Chair
Jennifer “Piper” Below, PhD’11
Editorial Committee Chair
Sydney S. Yoon, MD’86 Regional Programs Chair
ALUMNI COUNCIL
Shahriar Alikhani, MD’91
Lampis D. Anagnostopoulos, SB’57, MD’61 ✱
Allison August, MD’93
Margaret “Peggy” Barron, MD’78
Jennifer “Piper” Below, PhD’11
Anita Blanchard, MD’90
Jillian Bowman, AB’20 ✤
Kenneth Bridbord, MD’69, MPH
Ava Ferguson Bryan, AM’10, MD’18
Courtney K. Burrows, PhD’15, MBA’17
Arnold “Arnie” Calica, SM’61, MD’75 ✱
Ruth Carlos, AB’89, MD’93
Gabrielle Edgerton, PhD’10
Arash Emami, MD’94
Katherine Given, AB’08, PhD’13, MBA’16, MD’16
Jeffrey M. Goodenbour, PhD’09
Stanton Greenstone ✤
Andrew Hack, AB’95, PhD’00, MD’02
Theresa He, MD’03
Rajiv Jauhar, MD’91
Suejin Kim, MD’04
Clifford Ko, AB’87, SM’89, MD’91
Karyl S. Kopaskie, AB’07, PhD’14
Peter McCauley, MD’86
Jennifer A. McPartland, PhD’08
Doriane C. Miller, MD’83
Vincent Nelson, MD’98, MBA, MPH
Carol Olson, PhD’82, MD’86
Aneesha Sahu, PhD’19
Loren Schechter, MD’94
Coleman R. Seskind, AB’55, SB’56, MD’59, SM’59 ✱
Puneet Singh, MD’11
Maggie Steiner ✤
Anne L. Taylor, MD’76
Cynthia Thaik, MD’90
Vishruth “Vish” Venkataraman ✤
Sapana Vora, PhD’14
Sydney S. Yoon, MD’86
Rostik “Russ” Zajtchuk, SB’60, MD’63 ✱
✱ LIFE MEMBER
✤ STUDENT/RESIDENT REPRESENTATIVE
John Carpenter, MD’66, died on August 25, 2024. He attended Oberlin College, where he met his beloved wife, Peggy. After graduation, the couple moved so Carpenter could earn his MD at the University of Chicago. He later joined the Public Health Service in Boston, where he cared for patients in the U.S. Coast Guard. He then worked at Neponset Health Center and Brockton Hospital. The family moved to Norwell, Massachusetts, in 1975, where Carpenter served on the city’s board of health. He later started his practice at North River Medical Associates. He was an avid tennis player and fly fisherman who enjoyed vacations in St. John, volunteering and walking on the beach.
Robert E. Porter Jr., MD’60, died on September 10, 2024. He served as a flight surgeon in the U.S. Air Force before joining Mary Hitchcock Memorial Hospital in Hanover, New Hampshire, as an orthopaedist in 1972. He later became an associate professor of surgery at Dartmouth Medical School, and he took on leadership roles in various professional organizations, including the Federation of State Medical Boards. After retiring to
Florida, he enjoyed an active lifestyle that included sailing, skiing and scuba diving.
Joseph Simpson, PhD’67, MD, died on October 24, 2024. A graduate of Cornell University, Simpson received his PhD in psychopharmacology at the University of Chicago in 1967. After that, he worked on his postdoctoral fellowship at Yale University and earned an MD from Harvard University Medical School. After his training, Simpson started at Washington University School of Medicine and BarnesJewish Hospital in St. Louis, where he specialized in treating head and neck cancer. He was a dear cousin, colleague, mentor and friend to many.
Leslie Cohen, MD’76, died on November 23, 2024. Cohen solidified his desire to join the medical profession as a research student at the Jackson Laboratory in Maine. After attending Johns Hopkins University and the University of Chicago, he became a physician, specializing in radiology. He began his practice in 1980 in Flint, Michigan, where he also served as an assistant clinical professor at Michigan
John Reinitz, PhD, a Professor in the Departments of Statistics; Ecology and Evolution; and Molecular Genetics and Cell Biology at the University of Chicago, died on January 23 after a battle with metastatic cancer. He was 66.
Reinitz helped pioneer new thinking in the early 1990s when genetic research in developmental biology relied heavily on qualitative, hypothesis-driven experiments. His approach involved constructing an “atlas” a large, unbiased pool of data with no clear hypothesis behind it.
His later work leveraged data-driven modeling to train predictive models of gene regulation using these atlases, a method now widely practiced across disciplines and found in countless large quantitative datasets, such as The Cancer Genome Atlas.
“John was a fiercely independent thinker,” said Stefano Allesina, PhD, Professor and Chair of the Department of Ecology and Evolution at UChicago. “He went where the science brought him, without caring about the opinions of others, and he attempted to crack problems that seemed insurmountable.”
As a PhD student at Yale University, Reinitz’s path began when mathematical modeling was considered irrelevant to biological discovery. He devised a model that revealed the known mechanisms of viral gene regulation weren’t enough to account for all of a virus’s behaviors, a finding that dismayed researchers who considered the topic to be fully understood.
After a postdoctoral stint at Columbia University, Reinitz launched a major project with David Sharp, PhD, a nuclear physicist at Los Alamos National Laboratory, and Eric
State University. Cohen was chairman of the imaging department at Sturdy Memorial Hospital in Attleboro, Massachusetts. He took great pride in his family’s closeness and holds a special place in the hearts of all who called him a friend.
Lee Leserman, MD’73, PhD’73, died in 2024. He obtained his MD and a PhD in pathology from the University of Chicago. After completing his residency at Duke University, Leserman became a clinical associate/investigator in 1976. In 1979, he joined the Centre d’Immunologie de Marseille-Luminy in Marseille, France, where he and his team developed multiple applications using monoclonal antibody-coupled liposomes to target distinct cell surface molecules. This led to more cellular interactions in the immune response to vesicular antigens. Leserman is fondly remembered as an open-minded, wellread and rigorous scientist, as well as a thoughtful and gentle human being.
John G. Albertini, MD’93, died on January 17, 2025, after fighting cancer. Albertini graduated from the University of Notre Dame before pursuing his
Mjolsness, PhD, of Yale. Their connectionist model a computational method that simulates developmental data and provides insights could learn or infer the structure of a gene network.
Such data-driven modeling came to be known as “systems biology” by the early 2000s, and the National Institutes of Health began investing in this field.
After more than a decade at Stony Brook University, where his work was used to challenge the then-prevalent French flag model of cellular behavior, Reinitz came to UChicago as part of a systems biology initiative in 2011.
Reinitz expanded his model beyond developmental biology to include evolutionary biology, stochastic gene regulation and machine learning and he leveraged statistics across his work.
“John brought statistical modeling into his laboratory, and he enthusiastically brought his insights from the DNA laboratory into his teaching of statistics,” said Stephen Stigler, PhD, the Ernest DeWitt Burton Distinguished Service Professor Emeritus in the Department of Statistics.
Reinitz was known as a demanding boss who valued straight talk and an open exchange of ideas. Still, he knew his experience as an outsider in biological modeling meant his trainees faced an uphill battle. Many trainees learned later that Reinitz’s letters of recommendation were unusually long and offered detailed arguments supporting their candidacy.
A lifelong Grateful Dead and Phish fan, Reinitz also enjoyed reading science fiction and global travel. He is survived by his wife, Ilene, and daughter, Julia.
medical degree at the University of Chicago. He then served in the U.S. Air Force and was devoted to his profession as a Mohs surgeon. As president of the American College of Mohs Surgery, he was nationally recognized as a gifted surgeon and leader who put his patients first. He was a beloved husband to Laurie Wong Albertini, MD’93, and an incredible father to their three children.
Jaime Molden, MD’02, died on October 18, 2024. He earned a degree in biology from the University of California, Berkeley, and then conducted HIV research before discovering his calling in medicine. After attending medical school at the University of Chicago, he completed cardiology training at Harbor-UCLA Medical Center and an advanced fellowship in electrophysiology at Cedars-Sinai in Los Angeles. As a cardiologist and electrophysiologist, he was known not only for his expertise but also for his deep compassion. Molden’s legacy reaches beyond his medical career. He was a devoted father who cherished every moment with his sons, a loving husband, a humble leader and a steadfast friend.

“ John personified a major tenet of our department: Statistics flourishes when engaged with serious scientific problems, and vice versa.”
Stephen Stigler, PhD Ernest DeWitt Burton Distinguished Service Professor Emeritus, Department of Statistics
Robert Haselkorn, PhD, Distinguished Service Professor Emeritus in the Department of Molecular Genetics and Cell Biology, died at home on February 10. He was 90.
Haselkorn was widely known for his work on plant viral RNA, which carries genetic information for making new viruses that infect plants and can devastate crops, as well as for his work on the molecular genetics of nitrogen fixation and photosynthesis in cyanobacteria and purple bacteria.
He was also known for his research on acetyl-CoA carboxylase, which catalyzes the first step in the synthesis of fatty acids.
“Bob was among the group of people who developed the paradigm that we still use today to think about how genes control biochemical reactions,” said Bernard Strauss, PhD, Professor Emeritus of Molecular Genetics and Cell Biology, who served as chair of the Department
of Microbiology from 1969 to 1985. “He was popular in the research community and a very respected scientist.”
After joining the University of Chicago in 1961 as an assistant professor in biophysics, Haselkorn rose through the ranks, ultimately being named the Fanny L. Pritzker Distinguished Service Professor. He was the founding chairman of the Department of Biophysics and Theoretical Biology, which was succeeded by the Department of Molecular Genetics and Cell Biology, and he held an academic appointment in the Department of Chemistry. Haselkorn maintained an active lab and continued his research after retiring in 2009.
Teacher and connector
A two-time recipient of the University’s Quantrell Award for Excellence in Undergraduate Teaching, Haselkorn encouraged students at all levels to pursue projects that interested them. His approachability, colleagues said, made him a popular mentor for budding scientists.
In 2003, Haselkorn and his wife established the annual Margot and Robert Haselkorn Visiting Lecture series

to host molecular genetics and cell biology leaders on campus for a week. The series, which turns 18 this year, supports public and scientific lectures, and the opportunity for visitors to meet and interact extensively with students and postdocs.
“The series has been extremely valuable, not just for learning about the science, but also for giving our students exposure to leading scientists from around the world,” said Laurens Mets, PhD, Associate Professor Emeritus of Molecular Genetics and Cell Biology, who worked with the Haselkorns to establish the event.
This year’s lineup will feature one of Haselkorn’s former postdocs, Susan Golden, PhD, now a professor at the University of California, San Diego, and an expert in cyanobacteria.
Distinguished career
A native of Brooklyn in New York, Haselkorn received a bachelor's degree from Princeton University in 1956 and a PhD in biochemistry from Harvard University three years later.
He completed a postdoctoral fellowship at the Agricultural Research Council in Cambridge, England. While there, he was inspired by the work of Francis Crick and James Watson, who discovered the structure of DNA, to focus his own research on molecular biology and biophysics.
Haselkorn was a member of the National Academy of Sciences, the American Academy of Arts and Sciences, and the American Philosophical Society. He received the Gregor Mendel Medal in Biological Sciences from the Czech Academy of Sciences, and he was also awarded a Guggenheim Fellowship. Haselkorn served on the Marine Biological Laboratory Board of Trustees from 2003-10 and 2012-15, receiving the title of trustee emeritus in 2015. A co-founder of two biotechnology companies and a scientific adviser to many others, he held several patents in the biochemical field.
Haselkorn met his wife of 67 years, Margot (née Block), on a blind date while at Harvard. The pair married in 1957. They have two children, Deborah and David, four grandchildren and four great-grandchildren.
Those who wish to honor Haselkorn’s memory may contribute to the National Academies Committee on Human Rights.
“ He got off to a great start scientifically, which allowed him to climb the ladder quickly. He was also one of the most loyal University of Chicago citizens I have known. He cared enormously about the University and served it well in multiple ways.”
Theodore Steck, MD Professor Emeritus of Biochemistry and Molecular Biology
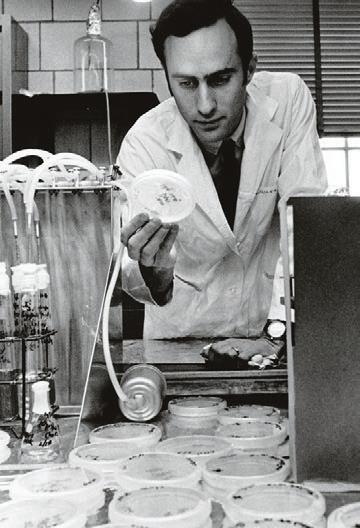

One of the most powerful and personal ways to show your support is to plan a future gift from your estate.
Your bequest to UChicago Medicine, the Biological Sciences Division, or the Pritzker School of Medicine reflects the important role these institutions play in your life and to the generations of people who have valued their excellence in research, education, and patient care.
When you add a provision to your will or trust, you can provide unrestricted support or designate its purpose. Plus, a bequest allows you to update your wishes if your priorities change, and to retain your assets for as long as you may need.
Not sure where to start or need help with the appropriate language?
Email Wendy Irvine, senior director of development, at wendyirvine@bsd.uchicago.edu.
Let us know.
If you've already planned a bequest, sign up to become a lifetime member of the Phoenix Society at phoenixsociety.uchicago.edu
Explore further.
giftplanning.uchicago.edu/statement25
The University of Chicago does not discriminate on the basis of race, color, religion, sex, sexual orientation, gender identity, national or ethnic origin, age, status as an individual with a disability, protected veteran status, genetic information, or other protected classes under the law. For additional information, please see uchicago.edu/about/non_discrimination_statement.
A steel beam with more than 3,400 messages of hope and tribute was lifted into UChicago Medicine’s new cancer pavilion by construction crews on Feb. 4. Set to open as the AbbVie Foundation Cancer Pavilion in 2027, it will be the first freestanding center in Illinois dedicated solely to cancer care and research.

BY